

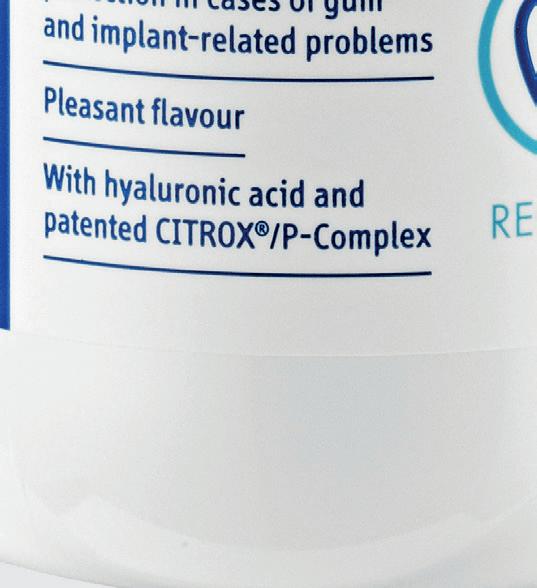
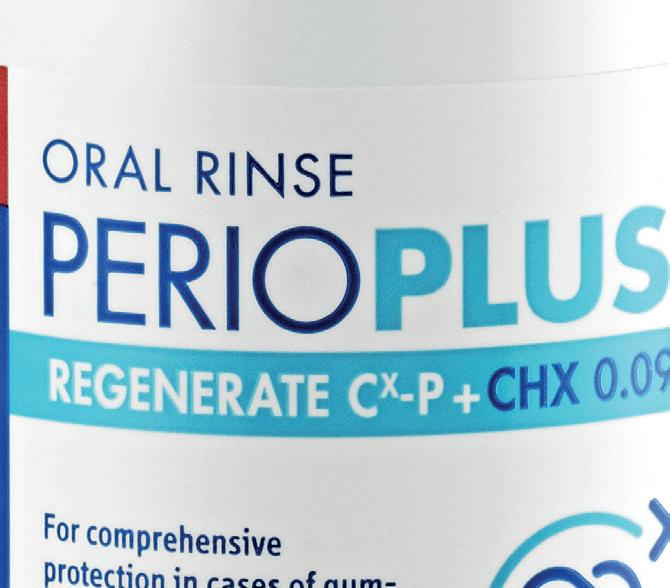
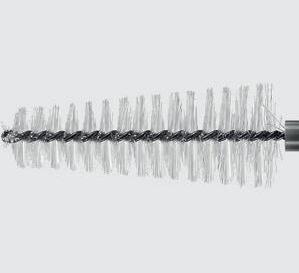
TARGETED IMPLANT PROTECTION
The Curaprox Implant Care Kit contains everything patients need to care for their implants a er surgery and for ongoing maintenance and protection.













































■
■
■
















GDC revises fitness to practise processes following report into causes of death during investigations
The General Dental Council (GDC) has revised its fitness to practise processes to improve proportionality and timeliness in investigating clinical practice concerns. The news comes following the report released by the GDC in early November, exploring the causes of death during fitness to practise investigations.
The report, the first of its kind for the GDC, covers the period 2019 to 2022. During this time, 20 dental professionals died while their cases were active, with causes of death categorised as natural, external, or unspecified, and one subcategory of suicide. The GDC has taken steps to ensure that individuals cannot be identified.
The report has included deaths in the subcategory of suicide when “suicide” was listed on the death certificate or notification. By convention, death certificates in Scotland and Northern Ireland do not use the word “suicide” or any synonym of it. Deaths that occurred overseas have been categorised as unspecified.
Lord Toby Harris, GDC Chair, said: “The report serves as a call for everyone in the dental sector to reflect on the environment, systems and processes involved in being a dental professional. It took longer than we expected to complete the work and some of the issues have been complex, but we have delivered process improvements in parallel and taken care to ensure we can be confident in the data reported.
“Every death is a tragedy, and when the data and what we are doing to improve FtP are put aside, what is left is the death of people, some in tragic circumstances, and we must consider the
families, loved ones and colleagues for whom the pain and hurt are still very raw, and we offer them our condolences.”
The GDC has reportedly prioritised improvements to its FtP process to minimise the significant negative health and wellbeing impacts of investigations on dental professionals. Recent improvements include revised communications and staff training, and the regulator is currently piloting the use of initial inquiries to enable the assessment of clinical practice concerns earlier in the process and improve timeliness.
The GDC engaged with relevant stakeholders and Sir Louis Appleby, Chair of the National Suicide Prevention Strategy Advisory Group, in the production and reporting of the data.
The latest move to refine FtP investigations follows the successful pilot of a revised process for handling fitness to practise concerns raised about dental professionals with no previous allegations of fitness to practise impairments in the previous 12 months.
Launched in September 2023, the main aim of the pilot was to reduce the time taken to investigate single patient concerns about clinical practice. These were cases where the likelihood of closure at the assessment stage was high – the process change was designed to help ensure investigations were proportionate to the potential risks involved.
The regulator limited the information requested at the initial stages of an investigation to relevant clinical records only during the pilot. The pilot has demonstrated that this more proportionate approach can significantly reduce the average time it takes to conclude an investigation.
Feedback from caseworkers highlighted quicker responses from registrants to requests for information. Concluding cases took an average of 13 weeks during the pilot, more than half the 30-week key performance indicator for single clinical incident cases to reach the end of the assessment stage.
Theresa Thorp, Executive Director of Regulation at the GDC, said: “The success of the pilot has depended on the cooperation of dental professionals in promptly providing their relevant records, and we are grateful for the positive response from them and their representatives.
“While investigations into fitness to practise concerns are an important part of the regulatory system that maintains public safety and confidence, reducing the negative impacts of investigations is a priority for us. The pilot has shown the potential to streamline investigations for certain types of concerns while upholding the GDC’s commitment to public protection.”
The pilot, which initially covered approximately 250 clinical concerns, has achieved promising results. Of the cases completed, 84% were closed at the assessment stage with no further action. Allegations were raised in only 16% of cases and referred to case examiners for consideration.
“By taking a different approach with certain types of cases, we are working to reduce the negative health and wellbeing impacts of our investigations for all participants in regulatory proceedings. Ongoing research is helping us understand the difference these changes make, and we are committed to further improvements based on the insights gathered,” Thorp added. n
New Mouth Cancer Charter launched at House of Commons
Anew Mouth Cancer Charter has been launched last Thursday by the Oral Health Foundation at the House of Commons.
Created as part of November’s Mouth Cancer Action Month, the charter aims to show the necessary steps to reduce cases of mouth cancer and its mortality in the UK.
The charter recommends seven measures aimed at raising awareness, improving early detection, and enhancing patient care. This includes a government-funded mouth cancer campaign, improving access to routine dentistry and improving training for non-dental healthcare staff to recognise signs of mouth cancer.
Professor Tim Newton, President of the Oral Health Foundation says: “As we strive to reduce the number of people affected by this devastating disease, we require coordinated action at many levels. Our charter is a call to action for everyone from the government to healthcare providers to the public at large.
The Oral Health Foundation believes that improving education on the signs and symptoms of mouth cancer, as well as enhancing training for non-dental healthcare providers, can ensure more cases are detected earlier. The charity says this will not only improve the chances of survival, but also significantly enhances the quality of life for those affected.
Other steps included highlighted in the charter include improving referral pathways, supporting the development of better technology, and introducing free dental check-ups and treatment for mouth cancer patients.
“Streamlining referral pathways can only benefit mouth cancer care,” adds Professor Newton. “By

enabling faster access to specialists through direct referrals and one-stop clinics, we can reduce delays and ensure timely treatment, which is vital for improving survival rates.
“We also believe advancing diagnostic technologies such as AI and biosensors could play a significant role in helping detect cancer earlier, providing faster, more accurate results and improving patient outcomes.”
The House of Commons reception was hosted by Grahame Morris, MP for Easington. The event featured speeches by Bill Brodie, CEO of Vigilant Biosciences and Mahesh Kumar, Oral and Maxillofacial Surgeon and President of the Mouth Cancer Foundation.
Joe Butler, a mouth cancer survivor from Sheffield, shared his story with the room during the afternoon session. Diagnosed at just 26 years old, his recurring tongue ulcer was detected during a routine dental appointment.
Joe highlighted how that visit to the dentist ultimately saved his life.
Earlier this month, the Oral Health Foundation released its new State of Mouth Cancer Report that laid bare the rise in mouth cancer cases.
The latest data collected by the charity shows 10,825 new cases of mouth cancer diagnosed in the UK a year, marking a staggering 133% increase compared to 20 years ago.
The seven measures outlined in the Mouth Cancer Charter include:
1. Government-funded awareness campaign to educate the public about mouth cancer, its risk factors, and the importance of early detection.
2. Improved access to routine dentistry to facilitate early detection through regular dental check-ups, particularly in underserved areas.
3. Enhanced training for General Practitioners (GPs) to identify mouth cancer symptoms and facilitate faster referrals, alongside updates to NICE guidelines.
4. Improved training for all healthcare professionals (including nurses, carers, and pharmacists) to identify mouth cancer signs and make timely referrals.
5. Free dental check-ups and treatment for mouth cancer patients, including restorative care, to reduce financial barriers and support recovery.
6. Supporting the development of better diagnostic technologies, such as AI, biosensors, and non-invasive devices, for quicker and more accurate detection.
7. Improved referral pathways to speed up diagnosis and treatment, including direct referrals from pharmacists and the adoption of ‘one-stop clinics’ for comprehensive care. n




AJames Cooke T: 01732 371 581
E: james.cooke@purplems.com
Follow us : @SmileOHMmag
nd so, we come to the end of another year. And what a 12 months 2024 gave us! The biggest news this year on the dental hygiene and therapy front was undoubtedly the legislation pushed through back in the late spring/early summer, granting dental therapists and hygienists new powers to supply and administer particular courses of treatment. You could say the direct access road was widened further, allowing for addition traffic (apologies for the clunky metaphor).
SUBSCRIBE TO SMILE
Rates: UK £39.95 per year; Overseas £83 - all cheques in sterling drawn on a UK bank made payable to ‘Smile’. 8 issues including 16 hrs CPD £39.95

Published by Purple Media Solutions
The Old School House, St Stephen’s Street Tonbridge, Kent TN9 2AD Tel: 01732 371 570
Managing Editor James Cooke james cooke @purplems.com Tel: 01732 371 581
Commercial Director Gary Henson gary.henson@purplems.com Tel: 07803 505208
Production and Designer 1 Lorna Reekie lorna reekie @purplems.com Tel: 01732 371 584
Production and Designer 2 Rob Tremain rob.tremain@purplems.com








To see the year out, we have some fantastic content in this issue, including a piece from new BSDHT President Rhiannon Jones on page 8. We also have an interview on page 10 with Celso da Costa from EMS, who explains how to boost your practice with GBT insights, while Victoria Wilson discusses mental clarity and focus on page 20.
There’s plenty more in store, so I’ll let you get to it. Just one more thing: don’t forget to register for the Dental Awards by 12th January to qualify for an early bird entry rate. It takes two minutes and the rest of your entry doesn’t need to be completed until 24th February. Further info can be found on page 40 and at the-probe.co.uk/awards.
Merry Christmas and a Happy New Year!

ORAL HEALTH
Divisional Administrator Francesca Smith francesca.smith@purplems.com Tel: 01732 371 570
Circulation Manager Andy Kirk
Managing Director Ed Hunt ed.hunt@purplems.com Tel: 01732 371 577
liability for any consequential loss or damage, however caused, arising as a result of using information printed in this magazine. The views expressed in Smile OHM Magazine are not necessarily the views of the magazine, nor of Purple Media Solutions Editorial Advisory Board: Dr Barry Oulton, B.Ch.D. DPDS MNLP; Dr Graham Barnby, BDS, DGDP RCS; Dr Ewa Rozwadowska, BDS; Dr Yogi Savania BChD, MFGDP; Dr Ashok Sethi, BDS, DGDP (UK), MGDS RCS; Dr Paroo Mistry BDS MFDS MSc MOrth FDS (orth); Dr Tim Sunnucks, BDS DRDP; Dr Jason Burns, BDS, LDS, DGDP (UK), DFO, MSc; Prof Phillip Dowell, BDS, MScD, DGDP RCS, FICD; Dr Nigel Taylor MDSc, BDS, FDS RCS(Eng), M’Orth RCS(Eng), D’Orth RCS(Eng); Mark Wright BDS(Lon), DGDP RCS(UK), Dip Imp Dent.RCS (Eng) Adv. Cert, FICD; Dr Yasminder Virdee, BDS.

MATTERS

in association with:

Other titles include:

















The reality of mouth cancer: an increasing illness in the modern world

Every year, mouth cancer statistics have been increasing. Anecdotally, it was often said that dental professionals could go their entire career without coming across a case of mouth cancer. Over recent years, this picture has sadly changed.
The latest data collected by the Oral Health Foundation shows that 8,864 people in the UK were diagnosed within a year, more than doubling since 2000. Worldwide the figures diagnosed have now reached 650,000 of diagnosed cases. Therefore, not only is it more likely that you will be referring more suspected mouth cancer cases, but you will also have to treat and support patients living with the aftereffects of treatment.
Treatment and dry mouth
One of the most common complaints of mouth cancer survivors is dry mouth. Radiotherapy and some chemotherapy can cause damage to salivary glands, often stopping saliva production completely or making saliva thick and sticky.
As well as being extremely uncomfortable for patients, lack of a good saliva flow can leave them at a higher risk of dental decay. Saliva replacement products are available but may not necessarily be the solution for all patients.
Patients should be encouraged to try sugar-free chewing gum, if possible, take frequent sips of water and consider a change in diet to avoid salty, dry, or acidic foods.
Patients with dry mouth may benefit from using a high-fluoride toothpaste to help to reduce the risk of decay.
Trismus and reduced access
Trismus can range from mild to severe depending on the complexity and area that needs to be treated. This can impact the range of movements of the jaw that the patient is able to complete, which then affects not only how you carry out dental treatment, but also the patient’s ability to care for their teeth.
Having restricted opening of the jaw will make the use of regular oral hygiene products very difficult. Recommending a soft, baby toothbrush with a long, thin neck can help to reach more areas of the mouth. Interdental brushes with long handles will hopefully enable the patient to clean in-between their teeth effectively too.
Other changes to patients’ care routines may be necessary, such as the use of a fluoride mouthwash to help to reach areas that a toothbrush or interdental tools cannot.
What are the psychological effects of treatment?
The psychological effects of the diagnosis and treatment of mouth cancer can be devastating for any individual. The scars of cancer from surgery are often visible, which can adversely affect selfesteem and confidence. It can impact every part of their life, from going out socialising or eating and drinking with friends and family, to personal relationships with partners and children.
This may make them less inclined to visit the dentist due to social anxiety. It can be a reminder for some of when they were first put onto the cancer journey, making it difficult to accept the help they need.
It is something to be mindful of when interacting with previous mouth cancer patients. Helping patients reach out to those who can help discuss these feelings is an excellent way to help them overcome some of their worries and anxiety.
These are national support groups that they may find helpful:
• The Mouth Cancer Foundation gives information and support to people affected by head and neck cancers.
• The Swallows Head and Neck Cancer Support Group has a 24-hour support line for those affected by head and neck cancer - 07504 725 059.
• The Young Tongues is a support group made up of young people who have been diagnosed
with Tongue Cancer or a cancer diagnosis that involves similar treatment.
• Heads2together provides peer support for patients and their caregivers for mouth, nose, throat, ear, neck, and face cancers.
• NALC (National Association of Laryngectomee Clubs) provides online and telephone (0207 730 8585) for support and information.
• Macmillan also runs an online forum for those who are suffering from mouth cancer and their loved ones.
People who have had mouth cancer face more complex issues than regular patients. They may struggle with maintaining oral health, be at higher risk for oral diseases, and deal with various mental health challenges. This makes their relationship with the dental team even more crucial. By providing personalised care, and offering reassurance, you can make them feel valued and confident. With a few adjustments, there is no reason why these patients cannot continue visiting their regular dentist, who can support them in their recovery.
Mouth Cancer Action Month is an annual campaign organised by the Oral Health Foundation to raise awareness about mouth cancer. It takes place throughout every November.
For more information on how you and your practice can support this important cause, please visit www.mouthcancer.org n
ABOUT THE AUTHOR
KAREN COATES


Experience exceptionally lightweight loupes with crystal clear optics, designed and optimised




For a t as unique as for you. • you are.
Custom Measurements
Custom Fitting


Custom Fabrication




Guided by care, driven by purpose
New BSDHT President Rhiannon Jones shares her career journey, her passion for the profession, and her commitment to promoting health, preventing disease, and championing dental hygienists and dental therapists
When I first qualified as a dental hygienist and in 1999, I could never have imagined the path my career would take. Over the years, I have worked in a variety of settings, and each experience has shaped my understanding of what it means to make a true difference in oral health.
Now, as President of the BSDHT, I reflect on the core values that have guided me throughout my journey: promoting health, preventing disease, and supporting the profession. These principles are not just ideals; they are the foundation of everything we do as dental hygienists and dental therapists.
Promoting health
At the heart of our work lies a simple but powerful mission: to help people live healthier lives. Promoting oral health is about more than clean teeth – it is about educating patients on how their oral health impacts their overall wellbeing. Preventing disease and promoting health is at the core of everything we do.
Raising awareness is vital, and we aim to build on the hard work of the current team while exploring new ways to help members reach those who cannot, will not, or do not attend surgeries. Addressing these inequalities will require collaboration, and we plan to work with stakeholders to support existing projects and develop new initiatives.
The success of our ‘75 Hours for 75 Years’ volunteering initiative showed how willing our members are to share their knowledge. To build on this, we will provide training and establish a volunteer network to enable more outreach.
Initiatives like ‘First Smiles,’ in partnership with Oral-B, and visits to local groups such as Brownies, Scouts, and Women’s Institutes showcase how we can raise awareness of oral health’s vital role in overall well-being.
Preventing disease
From the moment I began practising, I understood the importance of helping patients avoid disease before it starts. Prevention is not just a service we offer – it is a philosophy that underpins our entire approach to care.
This focus on prevention also drives our collaborations with other dental organisations, like our upcoming Oral Health Summit in partnership with the British Society of Periodontology and Implantology. This event will bring together the dental team to share knowledge, learn and grow, all with the goal of improving patient outcomes.
Today, the associations between oral health and systemic conditions like diabetes and cardiovascular disease are clearer than ever. This gives us an even greater responsibility to educate patients and advocate for preventive care. My goal is to ensure that every dental hygienist and dental therapist feels empowered to take a proactive role in preventing disease, armed with the knowledge, skills, and support they need to succeed.
To learn more about how the BSDHT supports dental hygienists and dental therapists, and to discover resources that can help you promote health and prevent disease in your community, visit www.bsdht.org.uk.

Supporting the profession
Our profession is filled with passionate, skilled individuals who are committed to making a difference. But to thrive, we need support – not only from within but from the wider healthcare community.
Over the years, I have frequently heard from members about the challenges they face in employment and contractual arrangements. With so many variations in how dental hygienists and dental therapists are employed, misunderstandings can arise, and some practitioners feel undervalued. It is critical to raise awareness of our full scope of practice and ensure that everyone works in a safe, supportive, and compassionate environment.
I am also committed to fostering collaboration across the profession. Whether it is through joint events, mentorship programmes, or initiatives that spotlight our contributions, my aim is to ensure dental hygienists and dental therapists are seen and celebrated for the essential roles they play in the dental team.
Looking ahead
As I reflect on my career and my vision for the future, I am filled with optimism. Our work as dental hygienists and dental therapists has never been more important, and I believe we
are poised to make an even greater impact in the years to come.
Promoting health, preventing disease, and supporting the profession are not just goals – they are commitments that guide us every day. Together, we can shape a future where every patient receives the care they need and every member of our profession feels valued and supported. n
ABOUT THE AUTHOR
RHIANNON JONES

Rhiannon is President of the BSDHT, holds dual dental hygienist and dental therapist qualifications. With experience spanning general practice, NHS hospitals and academia, she is dedicated to empowering patients, promoting health, and supporting the profession.

Boost your practice with GBT insights!
Why were ‘GBT IS A PRACTICE BUILDER’ and the ‘EMS Financial Guide UK’ created, and how do they complement each other?
Celso: The ‘GBT IS A PRACTICE BUILDER’ guide helps dental practices improve clinical efficiency, patient satisfaction and profitability by integrating the Guided Biofilm Therapy (GBT) protocol. Alongside the ‘EMS Financial Guide UK’, it provides a comprehensive strategy for clinical excellence and financial success, equipping practices with the tools to optimise patient care and streamline operations.
There is an emphasis on the importance of assessing every clinical case and implementing hygiene measures as the first step. How does this assessment phase impact treatment outcomes and patient satisfaction?
Celso: The assessment phase is crucial for understanding a patient’s oral health and setting a foundation for effective, personalised treatment. Conducting thorough evaluations helps identify and address issues early on, reducing infection risks and leading to improved outcomes and higher patient satisfaction.
The importance of disclosing biofilm to patients is also stressed. How does this step enhance patient understanding and treatment effectiveness?
Celso: Disclosing biofilm is a key element because it makes the invisible visible, allowing patients to see where biofilm has accumulated. This not only educates them about their oral health but also actively involves them in their treatment journey. When patients visually understand the need for biofilm removal, their cooperation increases, enhancing the effectiveness of treatments. It also enables clinicians to target biofilm more precisely, leading to more successful outcomes.
Motivating patients to maintain good oral hygiene is highlighted in the guide. What strategies do you recommend for dental professionals to engage patients effectively?
Celso: To engage patients effectively, dental professionals should emphasise prevention and provide personalised oral hygiene education. Reinforcing the benefits of regular GBT sessions and explaining how they support long-term oral health can motivate patients to maintain good practices at home and attend regular check-ups.
How does the GBT protocol’s focus on patient comfort and satisfaction translate into longterm practice growth and patient retention?
Celso: The GBT protocol’s focus on comfort and satisfaction directly supports practice growth by fostering a positive patient experience. Patients appreciate the gentle, pain-free nature of GBT, making them more likely to return for regular cleanings and recommend the practice to others. Many practices have reported significant increases in appointments after implementing GBT,


demonstrating the protocol’s impact on business growth through enhanced patient satisfaction and loyalty. For example, in Dr. Gianandre A Poggi’s practice, the number of appointments tripled within a year of adopting GBT, showcasing the protocol’s impact on business growth.
How do the recommended recall appointments tailored to individual risk assessments help to improve patient outcomes and practice efficiency?
Celso: Personalised recall appointments based on individual risk assessments ensure that patients receive care tailored to their specific needs, preventing the progression of dental issues. This approach improves practice efficiency by optimising resource use and scheduling appointments based on necessity rather than a one-size-fits-all model. It also enhances patient outcomes by providing timely interventions and reducing the likelihood of severe problems.
Employee satisfaction and continuous education are mentioned as benefits of adopting the GBT protocol. How does the Swiss Dental Academy support practices in maintaining high standards and motivating staff?
Celso: The Swiss Dental Academy (SDA) supports practices by offering continuous education tailored to their needs, keeping dental teams trained in the latest techniques and technologies. This ongoing training boosts the quality of care and helps staff feel competent and confident, leading to higher job satisfaction and retention. Additionally, working in practices that adopt advanced methods like GBT attracts skilled professionals eager to be part of a modern, innovative environment.
The guides mention the financial benefits of implementing GBT, including oral health optimisation for business growth. How does GBT contribute to a more profitable practice?
In this interview, Celso da Costa shares his excitement about the transformative potential of two new guides that offer dental professionals a powerful strategy for clinical excellence and financial growth To explore the comprehensive
Celso: GBT contributes to profitability by creating recurring revenue streams through regular recall appointments, reducing treatment times, and enabling the bundling of multiple treatments in one visit. The guide highlights that a significant proportion of dental work is referred after GBT, demonstrating its role in identifying additional treatment opportunities. Practices that have implemented GBT report significant turnover increases without raising prices, proving that GBT not only enhances patient care but also drives financial growth. n
Celso da Costa Director of Global SDA EMS Switzerland
Ultrasonic Inserts
DuraTip ® inserts deliver unprecedented like new performance for the entire life of the insert.
We have been using the Parkell DuraTip inserts for 7 months on over 200 patients and they are as efficient as when we first got them. I have seen a lot of things over the years, but nothing compares to the Parkell DuraTip insert.
— Cathy Hendrickson, RDH
Patented Design and Structure
Proprietary internal geometries work synergistically to create DuraTip's signature consistent performance and unprecedented peak scaling efficiency.
Ergonomic, Anti-Slip Soft Grip
Optimized 12mm Outer Diameter Texturing for maximum ergonomic support and ease of handling.
Innovative W-stack
Precision-cut nickel alloy stacks are pressed into a novel W-stack configuration, which results in substantially increased handling durability and optimized vibrational energy transfer across the entirety of the insert. This translates into previously unimaginable consistency of scaling power at the tip.


Performance Guides


DuraTip inserts are paired with their own color coordinated Performance Guide (included with every insert). While DuraTip inserts maintain consistent peak efficiency up to an unprecedented 3mm of wear, it is important to regularly check tip wear so that use beyond this point is minimized.
DuraTip inserts are compatible with any magnetostrictive scaler device. Contact us for an exclusive introductory offer.



Linzy Baker: ADI Board Member

Dental hygienist and therapist, Linzy Baker, started her career training as a dental nurse at The Eastman Dental Hospital in 2011 and graduated from Queen Mary University of London in Dental Hygiene and Dental Therapy in 2017. She is passionate about delivering high-quality patient care, and regularly attends conferences to stay up to date with the latest treatments.
Linzy is a member of the Association of Dental Implantology (ADI) Board as DCP Rep. She shares a little bit about herself and her experience with the ADI:
“I joined the ADI in 2018 after qualifying from university, and attended my first Team Congress in 2019. I joined the ADI Board in 2021 as the DCP Rep, and have since completed three years which have included aiding the organisation’s social media presence, curating content for the Team Congress in 2022, organising and running the DCP programmes in 2023, building connections with other organisations, and contributing to the Board to ensure DCPs are accounted for in all decisions being made.
























“The ADI has always provided top quality education and great networking opportunities to its members, and I have always been grateful for the insights delivered

at Masterclasses and Team Congresses, as well as online member information and recommendations.”
On her position on the ADI Board, Linzy comments:
“I wanted to get involved with the ADI Board as I saw an opportunity to expand reach to DCPs and not just being an organisation for dentists and the historically male-dominated field. There have been many positive changes since entering the Board, and it is great to have the team involved with improving our educational reach to the supporting team.
“We have instigated collaboration between organisations such as the BSDHT and BADN to broaden our reach and align with likeminded associations. I was keen to enter into this second term to continue the hard work that has been undertaken and to keep the organisation moving in a positive direction. I have loved working with the ADI Boards both previous and current, and I’m excited to see where we take this in the new term.”
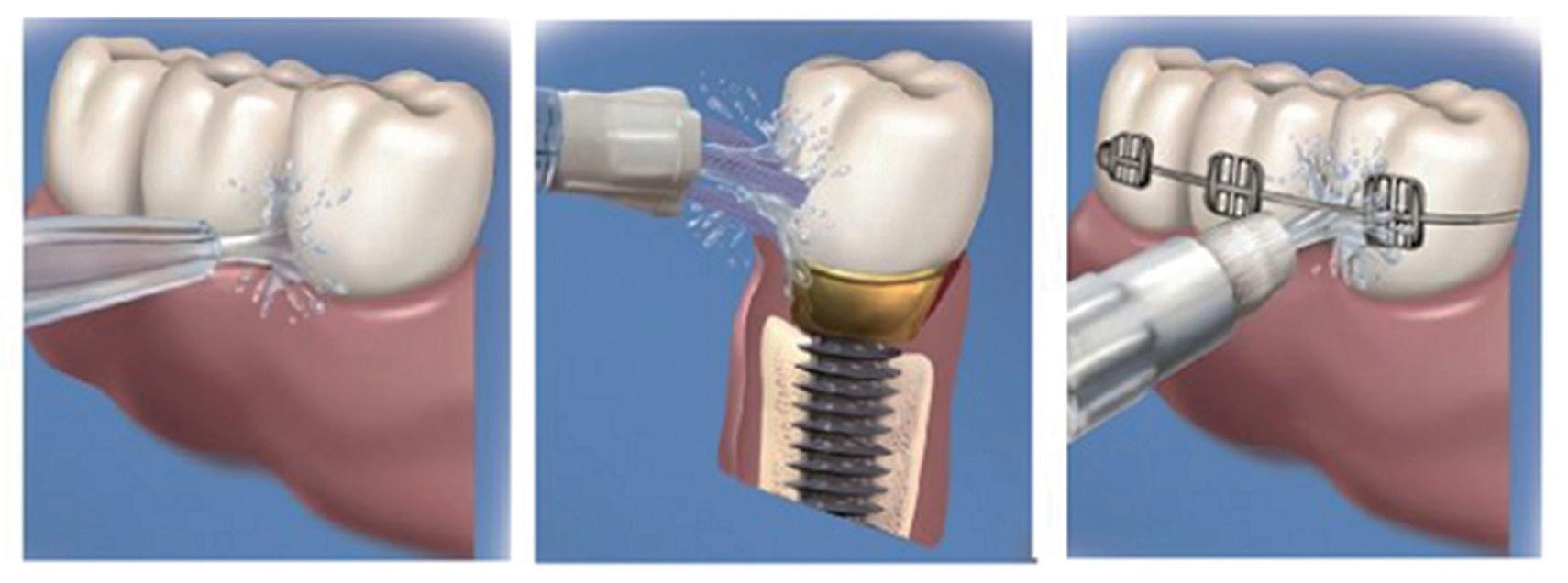
With dental implant treatment becoming more commonplace, Linzy shares advice for the dental team:
“I think education around implants is super important, knowing how common the treatment modality now is with most patients opting for this as a replacement for a lost tooth. Therefore, although imperative that dentists are at least aware of the treatment
and when it is appropriate to recommend or refer, it is my opinion that it is even more important for dental hygienists and therapists to be aware of the maintenance of implants. This is because they will be carrying most of this out and seeing them regularly, alongside the various types of prostheses. Dental hygienists and therapists are also well placed to refer patients for the assessment of missing or poor prognosis teeth that may benefit from dental implant treatment.

“It is also crucial that dental nurses are
“It is also crucial that dental nurses are knowledgeable in aseptic procedures and the different stages of implant appointments. Other dental support staff, such as treatment coordinators, should be included in the world of dental implants so they can best understand what patients may need or want to know when enquiring about or undergoing implant treatment.
“My top tip for DCPs entering into the world of implants is to join the ADI and be a part of a supporting organisation that can help and guide on the latest information, technology, and procedures. This will enable us to collectively work within our teams to deliver the highest standards of patient care.”
For more information, please visit www.adi. org.uk, and become a member today
Linzy Baker

Make your patients oral health experts
Biofilm control is key for preventing disease and keeping the mouth clean and healthy. As such, it’s important that patients have a good understanding of how to keep their plaque levels down at home. Whilst it is helpful for patients to have a deep clean when they visit a dental hygienist, it is not enough to rely on this. Optimal oral hygiene using effective biofilm control techniques at home is essential for disease prevention.
Curaden understands this, which is why it hosts Individually Trained Oral Prophylaxis (iTOP) events around the globe, providing clinicians with the latest advanced biofilm management techniques and behaviour change strategies. The leading educational programme in the profession incorporates the latest research in biofilm control. Available in four levels: Introductory, Advanced, Recall, and Educator, iTOP provides clinicians with a transformative educational journey.
iTOP Introductory
The Introductory programme explores shortcomings found in daily dental prophylaxis. The foundational level of the programme teaches delegates to improve oral health using the proper tools and techniques. This oneday course gives delegates an understanding of the iTOP concept and philosophy.
iTOP Advanced
The two-day Advanced seminar offers a deep dive into the implementation of techniques in the dental practice. This course offers more time for discussions, Delegates will also get an understanding of Touch to Teach, learning the methods and techniques for daily biofilm management in small groups. The course prepares attendees to become effective oral hygiene instructors.
iTOP Recall
This annual seminar acts as a refresher for those who already hold an iTOP certification. The seminar recalibrates delegates’ skills and updates their knowledge of iTOP principles. iTOP Recall provides certification revalidation for another year.
iTOP Educator
The intensive four-day seminar is specially designed for dentists and dental hygienists who would like to become iTOP instructors. Highly trained experts hold Touch to Teach sessions across the course, aiming for delegates to achieve certification as an iTOP instructor,
But what is Touch to Teach training?
Touch to Teach training is a core element of the iTOP programme. The hands-on aspect enables participants to
master oral hygiene using different tools and techniques. It is an effective method of correcting, improving, and guiding towards excellent oral health for their patients. Revolutionise patient care with a focus on prevention Make prevention the priority in your practice. iTOP enables you to discover strategies to address oral health issues before they become serious problems. This proactive approach to care improves patient outcomes and their satisfaction with treatment.
Participants gain science-based in-depth knowledge of biofilm control techniques, understanding how
plaque forms and how to manage it to prevent disease. By becoming an oral hygiene expert, delegates become proficient in delivering patient-centred care, focussing on each individual’s needs and preferences.
iTOP seminars are appropriate for everyone. Whether you’re a seasoned practitioner or are just starting your career in dentistry, iTOP principles aim to expand your knowledge of oral hygiene and patient care, enhance your skills, and impact your patients’ wellbeing.
So, no matter what stage of your career you’re in, take part in an iTOP course, and help your patients become oral health experts.
For more information, please visit https://curadenacademy.com/en/






Varnish






Farewell food adverts
For TV channels, the 9pm watershed is designed to help parents protect their children from harmful material. 74% of adults think 9pm is the right time; with children hopefully in bed and away from the screen.i Along with things like bad language, the watershed will have a new category added to it from October 2025: junk food adverts.
The long-gestating ban on junk food adverts, originally set for January 2023, is an attempt to curb the country’s obesity problem: more than one in five children are overweight or living with obesity when they start primary school; this rises to one in three by the time they leave.ii As advertising influences eating preferences, the daytime removal of these from both TV and online platforms hopes to reduce the daily presence of unhealthy foods for children.iii This is also a victory for dentistry as obesity and oral health diseases are both influenced by diet.iv

How it will work
To classify junk foods the government has set up two qualification systems. The first is a list of 13 categories deemed junk food: soft drinks, savoury snacks, breakfast cereals, chocolates and sweets, ice creams, cakes, biscuits and bars, morning goods, desserts and puddings, yoghurts, pizzas, potatoes, and ready meals.iii
The second is a unique scoring system that analyses the salt, sugar, protein and other nutrients within a food or drink, with the ‘less healthy’ foods deemed illegible to advertise.iii For companies that do wish to advertise but can’t, their junk food products will need healthier recipes that pass the scoring system. Famous fast-food chains can still promote their healthy products even if the brand as a whole is commonly associated with junk food.v
The oral health impacts
Whilst designed to combat obesity and its £6 billion impact on the NHS each year, the ban is also of great benefit to oral health.vi Increased body mass index is associated with a greater risk of periodontitis due to the presence of inflammationpromoting cytokines. Unhealthy diets are also less likely to include the nutrients and antioxidants that help maintain a strong immune system, increasing the risk of gingival diseases by failing to fight infection.vii Tooth decay is the biggest reason for hospital admissions for children aged 5-9, and so limiting junk food exposure could further reduce the financial strain of the NHS.viii
However, both children and adults may assume certain foods are deemed completely healthy just because they will still be advertised during the day. Despite their sugar content, foods like fruit and
jam will not be banned, as will zero sugar drinks.v Whilst better for the body and able to reduce the risk of obesity, these can still be damaging to oral health when consumed in excess due to their acidity. Zero sugar drinks can be highly erosive, making them a threat to the enamel, whilst regularly snacking on fruit and jam can cause decay, sensitivity, and discolouration.vii A consistent oral hygiene routine can mean consumers can enjoying the health benefits of acidic fruits without compromising their dental health.
Protecting the oral cavity
The advert ban does not stop people from buying and eating junk food, and its impact may not be fully seen for years to come. Consumers can still enjoy the affected treats by moderating their dietary intake and ensuring that they are regularly cleaning their teeth twice a day, and ensuring their remove interdental plaque and food debris. By doing so, the risk of gingival diseases and tooth decay from acidic and sugary foods is lowered.
An effective way of keeping the oral cavity clean is with the Cordless Advanced water flosser from Waterpik™. Able to remove up to 99.9% of plaque from treated areas, the Waterpik™ Cordless Advanced is a reliable part of the daily oral hygiene routine.ix When compared with string floss, the water flosser is up to 50% more effective for improving gum health, deterring the risk of infection.x With 4 tips, 3 pressure settings and a 360-degree tip rotation, the Cordless Advanced can be customised to match the patient’s preference during their oral hygiene routine.
The junk food advert ban represents a push to tackle obesity, and one that will also improve oral health by reducing the exposure to sugary and acidic foods. By encouraging consistency with the daily oral hygiene routine, practitioners can help promote a healthier future for all.
For more information on WaterpikTM water flosser products visit www.waterpik.co.uk. WaterpikTM products are available from Amazon, Costco UK, Argos, Boots and Tesco online and in stores across the UK and Ireland.
References
i. www.ofcom.org.uk. (2016). What is the watershed? [online] Available at: https://www.ofcom.org.uk/ tv-radio-and-on-demand/broadcast-standards/ what-is-the-watershed/#:~:text=There%20are%20 strict%20rules%20about [Accessed 25 Sep. 2024].
ii. Campbell, D. (2024). Junk food TV ads to be banned pre-watershed in UK from October 2025. [online] the Guardian. Available at: https://www.theguardian. com/politics/2024/sep/12/junk-food-tv-ads-to-bebanned-pre-watershed-in-uk-from-october-2025.
iii. Sandeman, G. (2024). Junk food ban: What is included under new advert rules for online? [online] BBC News. Available at: https://www. bbc.co.uk/news/articles/cp3d33l53r9o.
iv. Issrani, R., Reddy, J., Bader, A.K., Albalawi, R.F.H., Alserhani, E.D.M., Alruwaili, D.S.R., Alanazi, G.R.A., Alruwaili, N.S.R., Sghaireen, M.G. and Rao, K. (2023). Exploring an Association between Body Mass Index and Oral Health—A Scoping Review. Diagnostics, [online] 13(5), p.902. doi:https://doi. org/10.3390/diagnostics13050902.
v. British Dental Association (2021). Dentists support ban on junk food advertising. [online] British Dental Assocation. Available at: https:// www.bda.org/news-and-opinion/news/ dentists-support-ban-on-junk-food-advertising/ [Accessed 25 Sep. 2024].
vi. Holland, C. (2022). Obesity, oral health and the role of the dental profession. British Dental Journal, [online] 233(9), pp.712–713. doi:https://doi. org/10.1038/s41415-022-5242-2.
vii. www.colgate.com. (n.d.). Periodontal Disease & Obesity. [online] Available at: https://www. colgate.com/en-us/oral-health/threats-to-dentalhealth/periodontal-disease-and-obesity.
viii.Soffe, E. (2021). Provision of UK healthcare for children in hospital | Interweave Healthcare. [online] Interweave Textiles Ltd. Available at: https://www.interweavetextiles.com/childrenin-hospital/.
ix. Gorur, A., Lyle, D.M., Schaudinn, C. and Costerton, J.W. (2009). Biofilm removal with a dental water jet. Compendium of Continuing Education in Dentistry (Jamesburg, N.J.: 1995), [online] 30 Spec No 1, pp.1–6. Available at: https://pubmed.ncbi. nlm.nih.gov/19385349/.
x. Mancinelli-Lyle, D., Qaqish, J.G., Goyal, C.R. and Schuller, R. (2023). Effectiveness of a SonicFlosser Toothbrush with a Different Size Brush Heads and Manual Toothbrush plus Dental Floss on Plaque, Gingival Bleeding and Inflammation in Adults with Naturally Occurring Gingivitis: A 4-Week Randomized Controlled Trial. International Journal of Dental Hygiene. [online] doi:https://doi.org/10.1111/idh.12675. n
ABOUT THE AUTHOR
ANNE SYMONS

Anne is a Dental Hygienist currently working in a specialist periodontal/implant practice and also a busy NHS surgery. She has previously worked in a max fax unit, and also taught oral health care to staff in nursing and residential homes
Getting to know lupus
With an increasing number of celebrities sharing their diagnosis for lupus, awareness for the autoimmune condition is growing. Given the broad range of symptoms that can be linked to the disease, and the lack of cure, it can be a difficult condition to manage. With implications for oral health, it is necessary for dental professionals to understand potential links.
Causes and symptoms
It is not yet fully understood what causes lupus – medically known as systemic lupus erythematosus. It has been linked to various potential sources, including viral infections, certain medications, sunlight, puberty, childbirth and menopause, though the exact mechanisms are not known. It most commonly affects women, who are nine times more likely to suffer than men. Those aged 15-45 years are typically most at risk. Symptoms vary between individuals and may include: arthritis; fever; fatigue; a rash on the face; sensitivity to the sun; hair loss; change of colour in the fingers and toes; swelling in the legs or around the eyes; pain when breathing deeply or lying down; and headaches, dizziness, or confusion; abdominal pain.
There are also several oral symptoms associated with lupus: swollen salivary and lymph glands; and sores, usually painless, in the nose and mouth.
Of course, these alone can be a sign of many different things, so it’s important to ask patients broader questions. Where multiple symptoms are identified and lupus suspected, they should be signposted for a medical screening.
Left untreated it can lead to more significant problems for sufferers. These include kidney damage, seizures and memory problems, heart problems, vasculitis and blood clots, among other concerns. Those with lupus are also more likely to develop atherosclerosis and coronary artery disease.
Management techniques
Although there is no cure for lupus, symptoms can typically be managed effectively. Medications such as non-steroidal anti-inflammatory drugs (NSAIDs), hydroxychloroquine, corticosteroids, immunosupressants, rituximab and belimumab may be administrated. Unfortunately, some of these are associated with negative side effects that affect the mouth. For example, corticosteroids can reduce bone health, while immunosuppressants can cause swollen gingivae.
It is also generally recommended that those diagnosed with lupus avoid prolonged sun exposure. Covering the skin and using high SPF to prevent sunburn are beneficial for many sufferers. In some situations, vitamin D consumption should be optimised trough diet or supplements to prevent increasing the risk of osteoporosis.
Part of the support network
Ultimately, there is little dental professionals can do to help patients prevent lupus. Our role is more about helping those with a diagnosis to alleviate any oral symptoms they might be experiencing. For more information about lupus and how to support those diagnosed, you can visit the Lupus UK website. n





ABOUT THE AUTHOR
DR MICHAEL SULTAN

EndoCare, led by Dr Michael Sultan, is one of the UK’s most trusted Specialist Endodontist practices




For dry mouth – when just water is not enough


New




























































1 in 5 suffer from dry mouth, and water is usually the standard remedy. But for many people, water only provides brief relief.







TePe’s new hydrating mouthwash and mouth gel ease the feeling of dry mouth, provides comfort, and protects teeth. We recommend the gentle, unflavoured products for those with a very dry mouth and mildly flavoured products for those with moderate problems.











TePe® Hydrating Mouthwash - TePe’s mouthwash moistens the mucosa and leaves a pleasant feeling in the mouth. Not only does it help with dry mouth, but the added 0.2 % fluoride also gives that extra protection against caries.



TePe® Hydrating Mouth Gel - TePe mouth gel gives immediate and long-lasting comfort*, moistens and soothes the oral mucosa and is convenient and easy to use whenever needed – great for on-the-go.
Available from dental wholesalers. Find out more at tepe.com.






*The duration of the comfort is individual; people with no or very little saliva usually experience a more prolonged effect.









Why do women experience TMD more than men?
Temporomandibular dysfunction (TMD) has a prevalence reported to be as high as 25%, making it a common clinical feature, arising from dysfunction of the temporomandibular joint (TMJ) and the associated jaw and facial muscles. Whilst it is common, it has often been seen as a simple mechanical joint dysfunction, rather than the complex chronic pain disorder it now appears to be. As such, past research has focussed on physical interventions, and has discarded the psychological and socials impacts.ii As with many conditions, there is an increased prevalence in one gender when compared to another. It’s important that professionals recognise this, and take it into account when assessing patients and forming a diagnosis. TMD affects more women (15-26%) than men (8-15%).iii Clinicians should explore the reasons why this may be, and offer specific advice to help women manage their condition, in a way which is tailored to their specific needs.
Why do women suffer more?
With this in mind, it’s important to understand why women may be more likely to experience TMD, and suffer disproportionately both in terms of frequency and severity.iv In doing so, clinicians will be able to more effectively assist their patients with their specific needs and concerns, and offer the most appropriate advice. Factors that may make women more susceptible to TMD include:
Stress
TMD and stress are directly linked, causing the muscles to tense, jaw to clench, and teeth to grind, including during sleep. Generally, women report higher levels of stress and anxiety compared to men, and women are more likely to be deficient in magnesium, the mineral which helps to regulate stress.v
Jaw structure
Men and women’s jaw structures can be different. Women’s jaw muscles can be more prone to injury and inflammation, leading to reduced blood and oxygen reaching the face, including the jaw. This is in addition to the increased levels of lactic acid, leading to cramping and pain, as well as headaches.vi
Hormones
Some research suggests that a misaligned jaw may interfere with oestrogen receptors in the jaw, making the symptoms of TMD more painful. Further, an imbalance of progesterone could negatively impact bone, collagen, and cartilage, and hormone fluctuations during each month can mean that the way women experience pain can change at any point in time, with oestrogen generally relieving pain. Because of the potential role that hormone imbalances can have on pain, some women may benefit from talking to their doctor, particularly if they are taking hormonal contraceptives.vii
Understanding and managing TMD
TMD can lead to a number of complications, each of which can drastically impact patients’ quality of life. These include chronic pain, limited chewing function, and bruxism wear and tear on the teeth. Its symptoms include jaw and facial pain, shoulder or neck pain, jaw stiffness, difficulty opening the mouth, jaw popping or clicking, headaches, migraines, earaches, toothaches, and tinnitus.viii
Management of TMD can vary from patient to patient. However, as it can result in trismus in the long-term, having significant impacts on patients’ quality of life, it’s important to recommend

management techniques which nourish the jaw and facial muscles, and expand the mouth opening.
The Royal College of Surgeons makes a number of lifestyle recommendations for patients experiencing TMD, these are:
• Avoid stimulants like caffeine as they lead to stress and muscle tension
• Perform self-care exercises and relaxation techniques each day
• When experiencing TMD pain adopt a softer diet to reduce strain
• Do not chew gum, pen tops, nails etc. as this exerts extra strain on the jaw
• Keep the teeth apart, except for when chewing
• Try to maintain good posture, with head up and shoulders back and adopt an ergonomic workspace where possibleix
Jaw exercises are a great way to help patients expand their mouth opening, by repeatedly and gradually stretching the facial muscles.x To help with this, recommend the use of the OraStretch® Press Rehab System. When it is used as recommended for a patient’s specific situation, it can increase the mouth opening by an average of 26mm. The use of this jaw exercise rehab device helps to improve patients’ quality of life, by strengthening and stretching the jaw muscles to enable more normal function and reduced pain and stiffness.
In order to make the most appropriate recommendations to patients, it is important to understand their condition well, and why they may be predisposed to the symptoms they are experiencing. As with many conditions, one gender often statistically experiences it more than another. As such, when examining women, in particular, consider TMD as a possible diagnosis, and start preventative therapy where appropriate.
For more details about Total TMJ and the products available, please email info@totaltmj.co.uk
References
i. Camfield, D., Wilson, C. & Loescher, A. Sociodemographic trends in a UK temporomandibular joint disorder clinic. Br Dent
J (2022). https://doi.org/10.1038/s41415-022-3932-4
ii. Camfield, D., Wilson, C. & Loescher, A. Sociodemographic trends in a UK temporomandibular joint disorder clinic. Br Dent J (2022). https://doi.org/10.1038/s41415-022-3932-4
iii. Yakkaphan P, Smith JG, Chana P, Renton T, Lambru G. Temporomandibular disorder and headache prevalence: A systematic review and meta-analysis. Cephalalgia Reports. 2022;5. doi:10.1177/25158163221097352
iv. Camfield, D., Wilson, C. & Loescher, A. Sociodemographic trends in a UK temporomandibular joint disorder clinic. Br Dent J (2022). https://doi.org/10.1038/s41415-022-3932-4 v. https://www.tmjplus.com/why-womenexperience-tmj-more-than-men/ vi. https://www.smilebeautification.com/blog/atmj-dentist-explains-why-more-women-sufferfrom-tmj-than-men/ vii. https://www.tmjplus.com/why-womenexperience-tmj-more-than-men/ viii. https://my.clevelandclinic.org/health/ diseases/15066-temporomandibular-disorderstmd-overview ix. https://www.rcseng.ac.uk/-/media/FDS/TMDPatient-support-document-March-2024.pdf x. https://www.rcseng.ac.uk/-/media/FDS/TMDPatient-support-document-March-2024.pdf n
ABOUT THE AUTHOR
KAREN HARNOTT

Karen is Operations Director at Total TMJ
The role of parent education in preventing childhood tooth decay
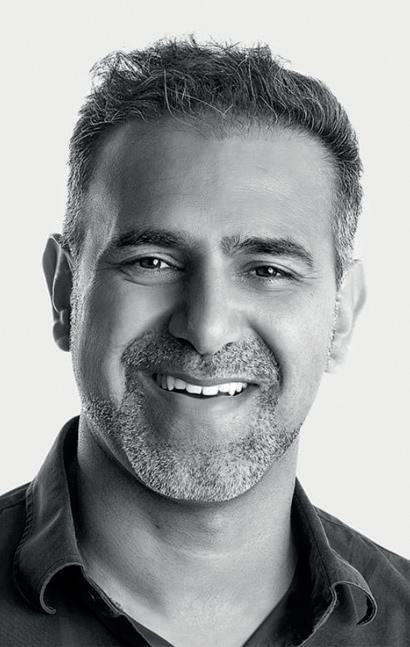
Award-winning dental hygienist and therapist and Philips KOL Sakina Syed is running an oral health education programme for local parents in her community. In this piece, she shares her advice about speaking with parents about childhood tooth decay.
“I am running a local project, educating parents at local schools near me in Tower Hamlets about their children’s oral health”, says Sakina Syed. “Tooth decay is the number one reason for hospitalisation in children, which is shocking, and preventable. I started the project because my child goes to school in a low socio-economic area.
There are a high number of children in the area with decayed and missing teeth.
I’ve always gone into schools to teach young children how to brush, and tell them about healthy foods for our teeth.
But I realised we don’t talk to parents directly, who are the decision makers in the family.”
Sakina outlines the key elements of her education programme.
“I host a coffee morning with the parents at local schools and nurseries”, she says. “I do a short presentation about how sugar affects teeth. We talk about the simple measures parents should take at home to look after their children’s teeth, and the foods which contain hidden sugars that parents may not know about, such as fruit yogurts. Awareness is the first step; there is so much hidden sugar in our foods now. I encourage parents to give their children healthier snacks like breadsticks, cheese on crackers, or fruit.
Some children are looked after by other family members, so we talk about how parents can pass information onto them, or implement healthy habits when they are the primary carers. Some parents need to be told that, even though children lose their baby teeth, they still need to be looked after. Decay spreads so much faster in baby teeth compared with adult teeth, and this has an impact on the developing teeth too. I speak with parents about the role of teeth – they don’t just help us eat our food. Teeth provide facial shape, they help us to talk and swallow.”
Sakina’s oral health education goes beyond nutrition.
“I talk with parents about going back to basics –brushing twice a day and using a fluoride toothpaste. It can be very difficult to find an NHS dentist, but in the Tower Hamlets area, there are often community dental services parents can access.
The uptake of fluoride application in this area is very low because the fluoride varnish contains alcohol and many residents are Muslim, so avoid alcohol. I encourage parents to understand that the Muslim Council has ruled that fluoride varnish is absolutely fine for your child to have because the alcohol is used as a preservative, and is of benefit to your child.”
As with adult patients, Sakina emphasises the importance of prevention in oral healthcare.
“Prevention at home is key to preventing wider oral health. I encourage parents to brush their teeth
with their children, and not position brushing as a chore, but see cleaning your teeth like having a shower – it’s a key part of looking after your body. Some parents are anxious about their own oral health. It’s so important not to transfer this to their child.”













1/3 the time





















Eyes wide shut
We are more sleep deprived than ever before. Almost 1 in 5 UK residents aren’t getting enough sleep, and the consequences of this are far greater than we think.i Natural sleeping patterns have been changed by the digital world, with the ideal 7-9 hours of daily rest feeling a lot harder to achieve. Sleep deprivation can be caused by numerous factors, such as obstructive sleep apnoea (OSA). By understanding the wider impacts of sleep deprivation and the links with dental hygiene, practitioners can be better equipped to help patients who may be suffering, or at risk from, sleep deprivation. As constant tiredness can impact overall health, a good night’s sleep can improve quality of life.
Sleepless screens
Patients with OSA may wake up repeatedly in the night, preventing a full night’s sleep and limiting their productivity the following day due to extra tiredness.ii Prevalence of OSA in adults is between 9% and 38%; its impact on sleep is bolstered by the disruptive patterns of the digital world that affect all ages.
The influx of new technology has radically altered our sleeping patterns in the 21st century. The UK population spends more time looking at screens – phones, computers, tablets, TVs – than they do sleeping.iii Among 16–24-year-olds, multiple devices are used simultaneously so that an average of 14 hours and 7 minutes of media activity are compressed into 9 hours every day.iii
Technology is not just used in the daytime: 50.09% of Britons have a TV in their bedroom to lay and watch something before sleep.iv Overall, 70% of adults use electronics of some description in their bedroom before they go to sleep.v Screens impact how we sleep, with prolonged exposure to blue light disrupting sleepiness.vi This means that OSA sufferers are even less likely to properly rest.

Rhythm and blues
The circadian rhythm is a 24-hour internal clock that regulates alertness and sleepiness according to changes in light. There are many biological clocks in the body, composed of proteins encoded by thousands of genes that switch on and off.vii The suprachiasmatic nucleus in the brain is the master clock; it releases melatonin based on the amount of light the eyes receive, and the melatonin causes sleepiness.vii The blue light from sources like TVs and phones suppresses melatonin, delaying tiredness.vi
The circadian rhythm can also be affected by food intake, stress, physical activity, social environment,

and temperature.vii As sleep supports memory consolidation, body healing and metabolic regulation, a disrupted circadian rhythm from OSA or technology use can have major health impacts. viii Short-term disruptions can include memory issues, delayed wound healing and digestion problems, whilst long-term health conditions like cardiovascular disease can be caused by an altered sleep pattern.ix
Besides the health risks, sleep deprivation impacts relationships and mental wellbeing. Insufficient rest is associated with poor mood, struggling to judge other people’s emotions, and an inability to control emotions – we have all felt irritable when tired and may be more argumentative.i For younger demographics, sleep deficiency can reduce concentration and creativity, whilst adults may be impacted at work, and while driving are more likely to have a serious injury.x Tackling sleep deprivation can lower the chances of these risks.
Sweet dreams
With sleep deprivation having a damaging effect on daily life and long-term health, a greater focus is needed on treating this issue. Dental sleep medicine (DSM) considers disorders such as OSA and snoring, but bruxism, hypersalivation, orofacial pain and xerostomia are other sleeping disorders that all impact dentistry.xi
To gain a detailed understanding of the overlap between sleeping disorders and dental hygiene, IAS Academy offers the Dental Sleep Medicine course. Led by Dr Paul Reaney, an international lecturer on DSM, the one-day course covers various therapies for OSA and snoring, fitting mandibular advancement devices, and using a digital clinical workflow with Envista technologies – among many more topics. Completing the course will give you a greater awareness of natural sleeping patterns and how sleep deprivation impacts quality of life. It will also educate you on how to identify warning signs of sleep-disordered breathing in children, preventing the problem in its early stages.
Consistent sleep is essential for overall health. With sleeping patterns altered by technology and breathing disorders, learning about new ways to help restore an uninterrupted night’s sleep can change lives for the better.
For more information on upcoming IAS Academy training courses, please visit www.iasortho.com or call 01932 336470 (Press 1)
References
i. Mental Health UK. (n.d.). Sleep and mental health. [online] Available at: https://mentalhealth-uk.org/help-andinformation/sleep/#:~:text=Almost%20 1%20in%205%20people.
ii. Watson, S. (2017). The Effects of Sleep Apnea on the Body. [online] Healthline. Available at: https://www.healthline.com/health/sleepapnea/effects-on-body.
iii. Britons spend more time on tech than asleep, study suggests. (2014). BBC News. [online] 6 Aug. Available at: https://www.bbc.co.uk/ news/technology-28677674#:~:text=Britons%20 spend%20more%20time%20using [Accessed 25 Jul. 2024].
iv. www.time4sleep.co.uk. (n.d.). 50% of Brits have a TV in their bedroom: Sleep expert comments on if you should watch TV to go to sleep. [online] Available at: https://www. time4sleep.co.uk/blog/50-of-brits-have-a-tvin-their-bedroom-sleep-expert-commentson-if-you-should-watch-tv-to-go-to-sleep [Accessed 25 Jul. 2024].
v. Bhat, S., Pinto-Zipp, G., Upadhyay, H. and Polos, P.G. (2018). ‘To sleep, perchance to tweet’: in-bed electronic social media use and its associations with insomnia, daytime sleepiness, mood, and sleep duration in adults. Sleep Health, 4(2), pp.166–173. doi:https://doi. org/10.1016/j.sleh.2017.12.004.
vi. Harvard Health Publishing (2020). Blue Light Has A Dark Side. [online] Harvard Health. Available at: https://www.health.harvard.edu/ staying-healthy/blue-light-has-a-dark-side.
vii. National Institute of General Medical Sciences (2023). Circadian Rhythms. [online] www. nigms.nih.gov. Available at: https://www.nigms. nih.gov/education/fact-sheets/Pages/circadianrhythms.aspx.
viii. Reddy, S., Sharma, S. and Reddy, V. (2018). Physiology, Circadian Rhythm. [online] Nih. gov. Available at: https://www.ncbi.nlm.nih.gov/ books/NBK519507/.
ix. Healthline. (2020). Circadian Rhythm: What It Is, How it Works, and More. [online] Available at: https://www.healthline.com/health/ healthy-sleep/circadian-rhythm#when-totalk-with-a-doctor.
x. National Heart, Lung, and Blood Institute (2022). Sleep Deprivation and Deficiency - What Are Sleep Deprivation and Deficiency? | NHLBI, NIH. [online] www.nhlbi.nih.gov. Available at: https://www.nhlbi.nih.gov/health/sleepdeprivation#:~:text=Sleep%20deficiency%20 is%20linked%20to.
xi. Lobbezoo, F., Nico de Vries, Jan de Lange and Ghizlane Aarab (2020). A Further Introduction to Dental Sleep Medicine. Volume 12, pp.1173–1179. doi:https://doi.org/10.2147/nss.s276425. n
ABOUT THE AUTHOR
DR TIF QURESHI
Dr Tif Qureshi, founder and a clinical director at IAS Academy.
Centrix Innovations

Many dental manufacturers claim their products make Dentists’ lives easier, but not every manufacturer makes it their mission. That’s unless it’s Centrix, the 50-years old dental innovator which launched the first direct-to-prep delivery system back in 1970. Centrix continues to produce single-patient-use products designed to make dentistry easier. This includes the ubiquitous Benda Brush and Benda Micro brush; Tempit temporary filling materials; FluoroDose sodium fluoride varnish, which is now available in six patient-pleasing flavours and can be applied in less than a minute via its innovative LolliTray dispenser; NoMix moisture-activated temporary cement, which is designed for use in
the surgery and at home in emergencies; Exposé disposable caries indicators which eliminate the need for measuring and mixing, and the risk of spillages; and many others.
Free sample of NEW DraganBerry flavoured FluoroDose!
Centrix have extended their range of Award Winning Fluorodose varnishes by launching NEW DraganBerry flavour! To obtain a free sample contact your local Trycare representative, telephone 01274 885544 or email dental@trycare.co.uk
Centrix’s FluoroDose 5% sodium fluoride varnish is easy to apply in less than a minute.
To make life easier, its packaging has patented features to enhance handling, comfort and patient safety. Containing a single dose of varnish, each LolliTray includes a Benda Brush applicator and is designed so that it “pops up” with one hand, making removal simple and safe.
Drying in seconds when contacting saliva, FluoroDose remains in situ for up to six hours for optimum fluoride uptake. It offers a smooth nonstringy or clumpy consistency, fast application and six patient-pleasing flavours – caramel, bubble gum, mint, cherry, melon and NEW DraganBerry! It is supplied in Introductory Packs containing all six flavours and refills of each individual flavour.
Freshly mixed prior to application it always has the optimum fluoride distribution, unlike syringes which frequently separate out leaving inconsistent mixes of ineffectively low and dangerously high fluoride concentrations. Each LolliTray contains enough varnish to protect a full adult dentition. Non-gritty and easy to apply in undetectably thin films, it is colourless so does not affect the appearance after bleaching etc.
Quick-drying and long-lasting, FluoroDose is suitable for adults with caries risk factors and children. Applied as often as needed it is FDAapproved for treating dentinal sensitivity.
Exposé
With today’s emphasis on minimally invasive dentistry, Clinicians want to ensure that their direct restorations remove as little healthy tooth tissue as possible. One thing that can help ensure this is a caries detection dye.

Exposé caries indicators make the use and application of a caries detection dye simple, messfree and precise. Its well-known Benda Micro brush applicator, available in either fine or extra-fine, is prefilled with a dry blue dye, which is simply touched onto a wet tooth to activate. The dye, which acts by staining caries by-products, stains active caries lesions thereby enabling the Clinician to identify precisely the tooth material to be removed.

Plus, because it does not become liquid until it has touched the wet tooth there are no drips to stain clothing or soft tissue.
Benda Brush and Benda Micro brushes
While a brush is a seemingly simple tool, it’s important to have the right one for the job.
When applying a precise amount of material to a broad surface, the one-piece Benda Brush with its bendable brush head is ideal. The Benda Brush smoothly places and spreads fissure sealants, bonding and etching agents, whitening agents and other materials. Benda Micro brushes are perfect for applying smaller amounts of materials or when precise placement is required, such as with selective etching or single point placement.
Both brush heads can be angled with ease and remain in position without bouncing back. Their chemical-resistant, non-absorbent fibres are suitable for harsh substances. Disposable for easy clean-up, Benda Brush and Benda Micro brushes are available in two sizes and assorted colours, so they can be colour-coded to avoid cross-contamination.
All of these exciting innovations are now available from Trycare, the UK’s fastest growing dental dealer, who have been appointed sole UK Distributors for the complete range of Centrix problemsolvers. This expands further the comprehensive range of products available from Trycare, which includes everything you need from all the major manufacturers. Yet another reason to contact Trycare and “Discover the magic” for yourself!
For further information about the complete Centrix range contact your local Trycare representative, call 01274 885544 or visit www.trycare.co.uk/centrix. n Exclusively available from Trycare!
A thriving practice needs energised, focused leaders
and team members – how do you score yourself?
How do you score yourself? asks Victoria Wilson
In a dental practice setting, mental clarity and focus are required to make critical decisions. This means remaining calm as we navigate challenges, and having the headspace to let creativity flow and be able to ‘think outside the box’.
A thriving practice should foster a positive work environment where everyone aspires to contribute to the success of the business, while also meeting their personal goals and ensuring their wellbeing. A happy team will prioritise effectively, and this will lead to improved productivity in a collaborative way. For this to become a reality, everyone needs to make time to develop the necessary emotional intelligence. The practice owner needs to stay attuned to the needs and feelings of members of the team. Communication and empathy within the workplace are of paramount importance.
In this process, individuals also need to make themselves accountable to the practice owner and their colleagues, showing care on a daily basis. The dental setting can be stressful and lead to frustration and anger at times. Everyone should be encouraged to take a step back, analyse given situations objectively, and respond thoughtfully and in a kind manner.
So, here is the paradox: We are all too busy with impending deadlines and endless to-do lists constantly occupying our minds, and yet I am going to talk about meditation, knowing it can be perceived as counter-productive. Feel free to cringe, but please keep reading…
I am also far too familiar with comments that some personalities don’t inherently lend themselves as easily to the idea of slowing down and developing the mindset to readily accept the concept of meditation, and that is fine. Busy dental professionals often struggle to sit still and quiet their racing minds. Meditation might therefore seem almost antithetical to being a suitable solution for individuals used to handling daily complex multitasking and always undertaking responsibilities at speed.
I recently came across a fascinating study that compared the neural oscillatory and physiological correlations between meditation-naïve individuals and long-term meditators, in relation to their meditation depth. It was surprising to observe that, even through different styles of meditation practices (and I can show you that meditation does not need to be on a mat!), the first group could experience the same deepest levels of concentration and relaxation as meditation converts.1
The crux of the matter is that tired, stressed individuals who might be experiencing Impostor Syndrome will not drive any dental practice forward. Instead, this environment will only foster low morale, poor motivation and performance, which will, in turn, impact on patients.
I have recently conducted a series of wellbeing roundtables with Claire Frisby, and our findings confirmed that promoting wellbeing among dental professionals should be at the core of every dental practice. Dental professionals report2 feeling pressurised to constantly deliver, having concerns about professional regulation, fear of litigation from patients, and working in a high-stress environment with relentless challenges along the way. This often results in feeling overwhelmed and reaching a state of toxic resilience.
Regularly checking in with colleagues must become a daily routine within these settings. 3 It’s essential to recognise that caring for

individual wellbeing is a shared responsibility among all dental professionals, and access to support resources should be clearly signposted. Furthermore, establishing systemic approaches within dental settings to promote wellbeing is vital, representing a significant opportunity for future growth and enhancement.
Regardless of whether meditation is on anyone’s agenda, I encourage my peers to stop and reflect for as little as two minutes about whether their current life prioritises their physical and mental health, and if it aligns with their vision 10 years ahead if they were asked to look into the future? What do you envision for yourself? Does your current work-life balance support this ideal future? If the answer is yes, that’s wonderful! However, if the answer is no, this presents an opportunity to pause and reflect on the small, cost-effective adjustments that can be made now to realistically achieve a future vision and aspiration.
Professional reflection among dental professionals is an ongoing process. However, incorporating additional reflection that prioritises our wellbeing should also be a daily consideration. This approach aligns with the need for primary prevention in the realm of mental health for dental professionals.4
From the recent, rapid, evidence-based review commissioned by the GDC, one thing that was highlighted was that dental professionals would potentially be more receptive to uptake something specifically tailored to their needs. This would mean looking into the challenges they commonly face, like the fear of litigation, the need for perfectionism, time constraints, the constant pressure of high expectations on themselves, phobic patients, writing comprehensive notes, the fear of whistleblowing, and the fear of not being competent or confident, to name but a few.
If meditation could be tailored to be more meaningful to the profession, in a configuration that made sense to individuals, amongst a community of like-minded professionals, then I think people would be a lot keener to engage and at least give it a go. I have observed this over the last four years from delivering mindful movement and meditation classes online on a weekly basis.
Philips has supported me for years, as the company recognises the importance of helping practices that place an emphasis on individual and collective growth to ensure they thrive in clinic and maintain high value to patients, while making personal happiness a priority.
Kimberley Lloyd-Rees, Philips Professional Relations and Education Manager, also strongly believes in upskilling oneself to expand one’s career and reach optimal job satisfaction.
I am thrilled that Philips wholeheartedly agreed to work collaboratively with me to raise awareness of my recent wellbeing roundtables, and now with my meditation initiatives tailored specifically to dental professionals to help the profession deal with the challenges of daily life.
With this in mind, Philips and I would like dental professionals to take ownership of their wellbeing, reflect upon what meditation could mean to them, and question how and if this could address their needs. It is about helping them acknowledge and interpret stressors in their lives, finding ways to help them function as optimally as they can. If individuals constantly feel overwhelmed, this naturally dilutes their ability to focus, excel and reach their full potential, so how can they possibly deliver the highest levels of care for their patients?
Primary prevention can prevent the need for fullon interventional support. It starts by recognising what our bodies interpret as stress and how it shows up in our body, and when one is stressed and learning how one can skilfully manage pressures. Engaging in meditation can take as little time as three minutes a day as a starting point and can be incorporated into established habits (like time taken to brush one’s teeth!).2NOW4
I would like to highlight that practising meditation should be part of a multi-pronged strategy to help individuals.
A series of complimentary meditation mindfulness videos to prepare for a New Year, New You will soon be available on my Smile Revolution platform. For more information contact Victoria, email info@smile-revolution.net, www.smile-revolution.net/yoga n
References available upon request
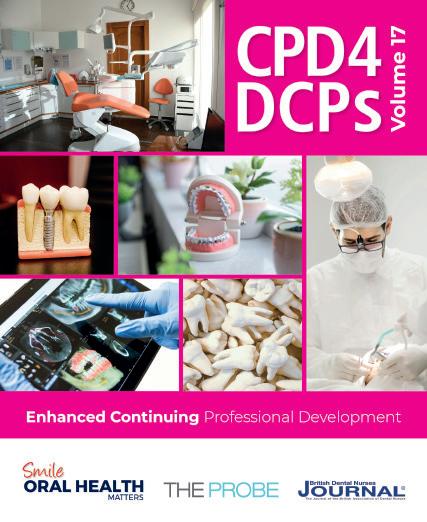
ECPD for your whole practice
CPD 4 DCPs is a fully veri able ECPD programme that enables each member of the dental team to complete one year’s ECPD requirement in a highly cost-effective manner. Covering all the highly recommended subjects, each volume is specially designed to cover the ECPD needs of up to 10 DCPs.
Providing 10 hours of veri able ECPD, one Volume covers the annual veri able ECPD needs of most practices.
VAT
Subjects covered:
• Early diagnosis of oral cancer: raising awareness of symptoms to improve outcomes
• Tackling safeguarding in dentistry
• When asthma attacks!
• Quality assurance of photostimulable phosphor plates




• How to handle a GDC investigation and come out the other side intact
• Radiographs and radiation safety in clinical dentistry
• Working with bloodborne viruses
• Complaints in the dental practice
• Patient education and communication: tackling gingival disease
• How can deafness and hearing loss impact dental care?
Just one Volume per practice per year, up to 10 people
10 hours veri able CPD including all recommended subjects
Ongoing modular learning programme
The whole team learning from the same information at the same pace
Saves time and money
Can be used by GDPs
Enhanced CPD Compliant
Choosing the right steriliser for your practice
Choosing sterilisation, disinfection and decontamination methods that effectively prevent and control the spread of pathogens in accordance with HTM 01-05 is an essential responsibility of every practitioner. With exposure to blood, saliva and the oral cavity – a natural habitat for a large number of microorganismsii – the dental setting presents a high number of opportunities for infection.
Dental handpieces can be particularly difficult to sterilise due to the complex internal structures which are considered particularly prone to contamination. To maintain a safe practice and prevent cross-contamination, a dental autoclave is an essential commodity for any busy practice, ensuring all instruments that could present a risk are safe for reuse.
Due to other pressures on the modern dental practice, choosing the right steriliser will increasingly involve other considerations, such as energy consumption, speed and efficiency, and intuitiveness/ease of use. Ideally, any member of the dental team should be able to reprocess handpieces quickly and effectively to meet appointment schedule demands as well as the needs of patients.
Infection control
The main infections that can be contracted in the environment are caused by bacteria, mycobacteria, fungi and viruses and prions – all of which can present a real danger to health.ii Contamination can be bidirectional, during treatment and afterwards, from patient to clinician and vice versa, and can be transmitted by inhalation, injection, ingestion, or absorption through the mucosa or skin.iii
Potential bloodborne diseases include human immunodeficiency virus (HIV), hepatitis B virus (HBV) and hepatitis C virus (HCV). Due to gingival bleeding, saliva should be treated with the same caution as blood.iv Without the proper mitigations in place, pathogens also have the potential to be transferred from patient to patient through shared access to poorly disinfected environments, as well as inadequately decontaminated devices and instruments.v
Autoclave types – a summary
The steriliser of choice must be fit for purpose in terms of consistent infection control.
The ‘N’ type autoclave is appropriate for flat, unwrapped, solid medical tools. It is not suitable for sterilising hollow, porous or wrapped loads, but may be useful if your practice has a large number of solid instruments to sterilise.
The ‘S’ type autoclave is considered the intermediate choice between ‘B’ and ‘N’ type options for dental practices, and can be highly useful for sterilising porous, bagged products, although it can’t process textiles. The S class autoclave usually has a range of drying cycle options, and is generally very quick and straightforward to use, but not considered optimal for hollow instruments.
Dental air turbines and straight and contra-angle handpieces can draw in contaminants during their operation. The small parts and long, narrow cavities make these instruments particularly challenging to keep free from infection.vi Once they have been cleaned and lubricated, the sterilisation process is essential to ensure they are free from infection.
‘B’ type sterilisers are considered the ideal autoclave for managing these instruments. They use a pump to create a vacuum, enabling a highpressure environment at a temperature too high for microbial survival.vii The resultant pressure when introducing boiling steam into the vacuum leads

to an increase in the boiling point of the water. In addition, the sudden pressure-change creates very hot steam at high speeds, forcing heat through the instrument, penetrating the interior more effectively than other methods.vii
Speed, energy efficiency and the audit trail
Energy efficiency is a vital concern both to save money and to reduce the carbon footprint of the operation. Of equal importance to any busy practice will be the speed and efficiency of the workflow. Sterilisation must also be validated, tested, documented and audited. Sterilisers that integrate these considerations, offering ease of use as well as speedy, effective function, are hugely beneficial for the efficiency of every practice.
Choosing the right autoclave for the practice will also require consideration of the appropriate capacity and size needed for regular use. Do you have limited space, and need a compact design? Or is your operation busy and large enough to warrant a larger unit? Do you need specialised support if things go wrong? If so, is this provided by the manufacturer?
W&H has a range of sterilisers, in compact, large and extra-large sizes to meet the needs of every dental practice. The Lisa steriliser from W&H, for example, provides both ‘S’ and ‘B’ cycles for flexibility, and offers the operator intuitive control for comprehensive and reliable sterilisation. EliTrace automates the vital audit function, meaning every instrument is automatically logged and tracked, so practices know where every instrument is in its decontamination schedule. Eco Dry+ technology also reduces the cycle time, optimising energy consumption for a more costeffective sterilization process. And ProService from W&H provides additional peace of mind, with total technical support.
Infection control is an important concern for all dental professionals, as procedures are carried out in an environment that exposes staff and patients to significant risk. Choosing a high-quality steriliser represents an opportunity to invest in the safety of your practice, as well as its overall efficiency.
To find out more visit www.wh.com/en_uk, call 01727 874990 or email office.uk@wh.com
References
i. https://www.england.nhs.uk/wp-content/ uploads/2021/05/HTM_01-05_2013.pdf
ii. Laheij AM, Kistler JO, Belibasakis GN, Välimaa H, de Soet JJ; European Oral Microbiology Workshop (EOMW) 2011. Healthcare-associated viral and bacterial infections in dentistry. J Oral Microbiol. 2012;4. doi: 10.3402/jom.v4i0.17659. Epub 2012 Jun 12. PMID: 22701774; PMCID: PMC3375115.
iii. https://www.england.nhs.uk/national-infectionprevention-and-control-manual-nipcm-forengland/
iv. Bromberg N. Brizueka M. Preventing Cross Infection in the Dental Office. March 2023. Available at: https://www.ncbi.nlm.nih.gov/ books/NBK589669/. Accessed August 2024
v. Laheij AM, et al. Healthcare-associated viral and bacterial infections in dentistry. Journal of Oral Microbiology 2012;4:1-10.
vi. Jun-Ichi Sasaki, Satoshi Imazato, Autoclave sterilization of dental handpieces: A literature review, Journal of Prosthodontic Research, Volume 64, Issue 3, 2020, Pages 239-242, ISSN 1883-1958, https://doi.org/10.1016/j.jpor.2019.07.013. vii. Laneve E, Raddato B, Dioguardi M, Di Gioia G, Troiano G, Lo Muzio L. Sterilisation in Dentistry: A Review of the Literature. Int J Dent. 2019 Jan 15;2019:6507286. doi: 10.1155/2019/6507286. PMID: 30774663; PMCID: PMC6350571. n
ABOUT THE AUTHOR
JON BRYANT

Jon is National Sales & Marketing Manager, UK & Ireland, W&H UK.
Buy 2 get 1 free (while stocks last)
Directa’s ProphyCare, is one of the most well-known brands of prophylaxis paste worldwide, offering reliable results ranging from regular cleaning of the teeth to more complicated implant maintenance procedures.ProphyCare pastes are available in different grits from coarse to extra-fine and are colour coded for easy identification. All ProphyCare pastes have a mild minty taste and do not splatter, it stays in the polishing cup during the treatment.


Learn to love lunch
Acommon saying is how ‘breakfast is the most important meal of the day’, but for those working long hours, lunchtime is crucial. In the current working world, employees are often likely to skip their midday meal – 40% more workers skipped their lunch break in 2023 compared to the previous year.i
Dentists, like other healthcare workers, often put the needs of their patients before their own, with 35% of dental practitioners unable to take breaks during the day to eat or drink.ii By focusing too much on work productivity, the current workforce is overlooking the value of rest and wellbeing.iii This can be detrimental to the practitioner’s health and their work results, reinforcing the necessity of a lunchbreak.
Promoting health
The concept of being well can comprise numerous factors: physical health and mental health, feeling happy and satisfied with life, having a sense of purpose, and managing stress effectively. iv Nutrition and a consistent diet are a crucial aspect to supporting these factors, providing the energy needed to get through the day. As the average employee spends one-third of the day in the workplace (or one-half of their time awake at work), sustaining the body with healthy food lowers the risk of exhaustion.iv
Working through lunch is also unhealthy as it can cause a deficiency in certain essential food groups. Research has shown that individuals who skipped a meal, like breakfast or lunch, did not fully compensate later in the day, leading to a negative net effect on total daily energy intake.v As some meals have a higher prevalence of food groups than others, such as dairy at breakfast or fruit at lunch, skipping them and not compensating for it later can impact health.v
Eating and drinking during a work break reduces mental fatigue, boosts brain function and promotes focus for longer periods.vi Seeing patient after patient may present a variety in the quality of their dental health, but the repetitive nature of examining the oral cavity and stooping in the dental chair can be physically and mentally draining. Taking the time to step back, stretch and eat a snack or lunch can provide the fuel needed to energise the body for the rest of the afternoon. This means returning to the practice room with a fresh perspective and a positive outlook, ensuring excellent treatments and communication for a better patient experience.
Beat burnout
Working throughout the day and neglecting food can lead to an exhaustive slump in productivity, impacting mood and increasing the chance of error. This may worsen the workload and lead to overtime, bringing dentists further towards the risk of burnout. Some of the warning signs of burnout include a lack of regular meals, working late or through lunchtimes, a lack of concentration, and chronic tiredness.vii A regular lunchbreak that incorporates healthy, energy-rich foods such as fruits, nuts or yoghurts, can remedy those warning signs, giving dentists a needed break that rejuvenates the body. A study of workers revealed that 48% feel less burned out when they eat lunch; a 26% increase from the previous year.v Similarly, over half also agree that lunch breaks help them focus and be more productive, making it an essential part of a dentist’s working day.viii
Socialising benefits
As well as the health benefits of eating lunch, another positive reason is for how a shared



lunchbreak can enhance the atmosphere in the practice. Those who engage in social eating have reported feeling more socially and emotionally supported by their co-workers, building strong bonds that make them better at their jobs.viii Talking with another staff member over lunch can be a great way of escaping work for a short time, making friendly connections that turn the workforce into a productive and effective team.iv
Saving time
Improving efficiencies in the daily workload can ensure there is more time to comfortably take a break from work. Kiroku can help; as an automated AI system it can help dentists write their notes 60% faster. The Kiroku Co-Pilot is an exciting addition that listens to the appointment then transcribes the conversation in real-time. This transcription is used to automatically write the dental notes using the preferred, customised templates. The efficiency of this service allows dentists to streamline their workloads so that they can give more attention to both the patients and, through essential lunchbreaks, themselves.
Finding the time to take a lunchbreak is essential for the physical and mental health of dentists, as well as for the continuation of excellent treatments and a successful long-term career.
To find out more about Kiroku, or to start your free trial, please visit trykiroku.com
References
i. Fortune. (n.d.). Stressed-out workers are skipping lunch—and forgoing their only chance to tame the chaos. [online] Available at: https:// fortune.com/2024/03/06/stressed-out-workersskipping-lunch-careers-health-well-being/. ii. New survey reveals impact of staff shortages on dental nurses’ wellbeing. (2023). BDJ Team, [online] 10(9), pp.5–5. doi:https://doi.org/10.1038/ s41407-023-2001-4.
iii. Cording, J. (n.d.). New Survey Shows Many Workers Aren’t Taking A Lunch Break. [online] Forbes. Available at: https://www.forbes.com/ sites/jesscording/2023/12/12/new-survey-showsmany-workers-arent-taking-a-lunch-break/.
iv. Aleksandra Hyży, Jaworski, M., Cieślak, I., Gotlib-Małkowska, J. and Panczyk, M. (2023).

Improving Eating Habits at the Office: An Umbrella Review of Nutritional Interventions. Nutrients, 15(24), pp.5072–5072. doi:https://doi. org/10.3390/nu15245072.
v. Zeballos, E. and Todd, J.E. (2020). The effects of skipping a meal on daily energy intake and diet quality. Public Health Nutrition, [online] 23(18), pp.1–10. doi:https://doi.org/10.1017/ s1368980020000683.
vi. Tan, J. (2021). Why Taking a Lunch Break Boosts Productivity, Mental Health Benefits | ThoughtFull. [online] Thoughtfull.world. Available at: https://www.thoughtfull.world/ mental-health/why-taking-your-lunchbreaks-seriously-boosts-your-mentalhealth#:~:text=Our%20minds%20and%20 bodies%20run [Accessed 17 Sep. 2024].
vii. Bradley, N. (2018). 3 Tips to Avoid Dentist Burnout and Achieve a Healthy WorkLife Balance. Colgate, [online] Accessed via: https://www.colgateprofessional.com/dentistresources/career-development/avoid-dentistburnout#
viii. Rao, D. (2024). Council Post: The Key To Workplace Productivity Isn’t Late Nights— It’s Lunch. Forbes. [online] 12 Aug. Available at: https://www.forbes.com/councils/ forbesbusinesscouncil/2023/01/03/the-key-toworkplace-productivity-isnt-late-nights-itslunch/ [Accessed 17 Sep. 2024].
ABOUT THE AUTHOR
HANNAH BURROW

Hannah is CEO of Kiroku
A Revolution in Oral Care
The most effective and body-friendly way of healing soft tissue and oral wounds.
















Patient Case Study – Before

Patient presented with Stage 4 Grade B Generalised Periodontitis.
Treatment: RSD Q&Q. blue®m TOOTh protocol










Patient Case Study – After

Recall at 12 months
Case study and photographs courtesy 0f Pat Popat BSc(Hons), PTLLS, RDH, RDT
Oxygen for Health
Maximising your skills as a dental therapist

The dental therapist is a crucial member of the practice team today. There are several factors that need to be considered for individuals to fulfil their potential and build a long and successful career. These include properly utilising their full scope of practice, being valued for their skills across the practice team and having access to first-class education and training. We all have a part to play in increasing awareness of the dental therapist’s role among the professional team, ultimately improving patient care, enhancing skill mix in practices and boosting job satisfaction for individuals in this role.
Promoting a team approach
To ensure dental therapists feel valued and able to fulfil their potential, it’s important that dentists understand their clinical remit. Not only do they need to know which treatments dental therapists can provide directly to patients, but they also need to consider how they may work in tandem with dental associates. Effective collaboration between team members can facilitate smoother daily workflows, create a more clinically diverse working day and ensure a less isolated working environment for other clinicians. It can also streamline emergency appointments and free up precious time for dentists to focus on other areas of dentistry such as implantology or endodontics.
Of course, is it just as relevant to consider how dental therapists can impact the patient experience. For a start, improved teamwork among all practice practitioners means faster, more efficient and often more effective dental care for patients. The majority of patients are already happy to see the dental therapist for a simple restoration, so there should be few barriers from them as a practice increases their dental therapy services. Patient satisfaction with treatment provided by dental therapists has been positive as well.ii Many
of the same factors apply as would impact patient satisfaction with care from a dentist – with trust and familiarity proving essential. These can be established and developed through professional behaviours and attitudes, good communication and smooth continuity of care.
Once dentists and other colleagues really understand how the dental therapist works, they can all operate within a workable business model that enhances patient care and boosts business profitability.
Although there has historically been a lack of understanding in the field, perceptions are gradually evolving. Regulatory changes are also being implemented that broaden the scope for both dental hygienists and therapists, who may now supply and administer specific medicines without a prescription from a dentist, once they have sufficient training and experience.iii
Being the change we want to see
In order for dental therapists to use their entire scope of practice, they must be confident and competent in their skills. For those who are new to the profession, or who have been unable to practise dental therapy in recent years, it can be difficult to adjust. That’s why it’s beneficial to access tailored training and support that will consolidate, develop and refresh your capabilities in a positive environment.
At Clyde Munro, we strive to be the change we want to see in the profession. We understand the importance of the dental therapist role and aim to remove barriers so that professionals may fully utilise their expertise. Our dedicated Therapist Support Programme has been designed specifically to help dental therapists to consolidate and expand their skills, covering a broad range of topics in training sessions and offering hands-on assistance from a clinical support team.
Skill, confidence and success
For many dental therapists, the chance to fully utilise their skills is important. Not only is job satisfaction improved, so too is the quality of patient care that can be delivered by the whole practice team. If you are feeling under-utilised, now is the time to make a change.
Want to know more? Please visit the relevant webpage here, or contact us on joinus@ clydemunrodental.com
References
i. Dyer, T., Humphris, G. & Robinson, P. Public awareness and social acceptability of dental therapists. Br Dent J 208, E2 (2010). https://doi. org/10.1038/sj.bdj.2010.1
ii. Dyer, T., Owens, J. & Robinson, P. What matters to patients when their care is delegated to dental therapists?. Br Dent J 214, E17 (2013). https://doi. org/10.1038/sj.bdj.2013.275
iii. New prescribing exemptions for dental hygienists and dental therapists. BDA. June 2024. https:// www.bda.org/news-and-opinion/news/newprescribing-exemptions-for-dental-hygienistsand-dental-therapists/ [Accessed August 2024] n
ABOUT THE AUTHOR
NORA GARCIA TBABAA

Nora is a Marketing Executive at Clyde Munro.
Middleton, Dental Therapist and Founder of London Hygienist
• A dentolegal advice line, with out-of-hours advice available for emergencies 24/7, 365 days of the year
• A huge range of CPD, including live webinars, online modules, and more
• Help responding to and resolving patient complaints
• Access to our confidential counselling service to support you through stressful situations.






EDUCATION: CURADEN
Show and tell
Dentistry has consistently fostered a strong need for technological advancements. The incorporation of more sophisticated technology has had many benefits: improved clinical accuracy, patient comfort, treatment success. In the Continuing Professional Development (CPD) of a dentist or dental hygienist/ therapist, technology has also enriched teaching and learning experiences.
Lifelong learning is crucial for every dental professional because knowledge, skills and technology are always evolving.i Whether studying the theory, obtaining the practical skills or attending seminars, there are many ways to advance your professional career in oral health. Staying up to date with the changes and developments of the industry will allow exceptional patient care to be delivered.i
Curaden leads the way
Over many decades, Curaden has been dedicated to ensuring lifelong oral health for all. They have trained over 60,000 dental professionals across the globe on preventative thinking and decisive action, supporting dental teams in giving firstclass treatments. Through exceptional dentistry, patient education and professional support, Curaden promotes health and happiness among the general population.ii
At Curaden, the mission to empower dental professionals is being achieved with specialised training and quality products. Their worldwide distribution net reflects the excellence of their service.

Checking the catalogue
Innovative products are important for treatment success and the continual growth of a dental practice. The Curaprox product range from Curaden is filled with effective products to meet every need. These include:
• Fresh breath
• Teeth whitening
• Sensitive teeth
• Braces and aligner care
• Gingival issues
• Denture and implant care
Curaprox products can revolutionise the daily oral hygiene routine for patients. The toothbrush choice is vast: the CS manual toothbrushes have unique Curen® filaments for a gentle but powerful cleaning effect, and a deliberately angled head for maximum coverage. There is also a variety in hydrosonic toothbrushes and specialised toothbrushes for implants, orthodontic appliances and sensitive gums.
For interdental cleaning, the range of CPS interdental brushes are effective and sustainable,

with refill packaging meaning only the brush tip needs replacing, reducing plastic waste. With numerous sizes available, there is an appropriate interdental brush for every interdental space.
For orthodontic patients, the Curaprox Ortho Travel Set features a unique Ortho travel toothbrush, a Be you whitening toothpaste, three CPS Ortho interdental brushes and a colourful case for the easy maintenance of oral hygiene on the go. Curaprox Aligner Foam is also ideal for safeguarding teeth when wearing plastic aligners, retainers and mouth guards, using natural minerals to shield and enrich each tooth.
The convenience of the Curaprox Implant Care Kit, which contains everything from a CS surgical toothbrush to Perio Plus Regenerate mouth rinse, means that patients can maintain post-surgery care wherever, whenever, ensuring the success of the implant treatment.
Curaprox also houses a reliable product range for babies and kids – toothpastes and toothbrushes designed to make brushing fun and enjoyable for


little ones. The variety in soothers and teething rings can provide relief for parent and toddler alike. With bright colours and fruity flavours, the children’s range can increase adherence with the daily oral hygiene routine, improving their health.iii
Becoming familiar with the extensive options available for these wants and needs can help you point patients towards the right solutions. Curaden representatives are available for lunchtime sessions at your practice to demonstrate all such products and more.
Getting ahead
These Curaden educational sessions provide a fantastic opportunity to prevent oral health problems before they emerge, all from the comfort of your practice. As Curaprox conveniently comes to you, the relaxed atmosphere of the sessions will make them a positive environment for the whole team. Not only will products be available to try and sample, but Curaden representatives will also explore the science behind each one, and how best to use them clinically. By providing a greater understanding of each product, you can effectively communicate with patients on the benefits of using them and the problems they can prevent.
Curaden seeks a healthier, smiling world. Join them in fulfilling this. To arrange a Practice Educational Meeting with your Curaden Development Manager please email us on sales@curaden.co.uk
For more information, please visit www.curaprox. co.uk and www.curaden.co.uk
References
i. Lee, J. il (2023). Dental education now and in the future. Journal of Periodontal & Implant Science, [online] 53(3), pp.171–172. doi:https://doi. org/10.5051/jpis.235303edi01.
ii. Curaden. (n.d.). Story. [online] Available at: https:// curaden.com/story/ [Accessed 23 Jul. 2024].
iii. www.colgateprofessional.com. (n.d.). Toothpaste Flavors: Influencing Oral Health Behavior. [online] Available at: https://www.colgateprofessional. com/dentist-resources/patient-care/toothpasteflavors-influencing-oral-health-behavior. n







































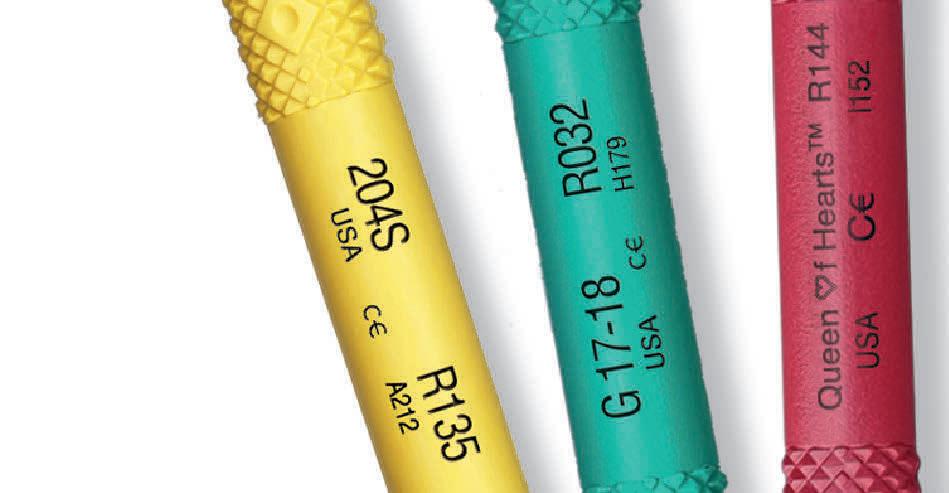




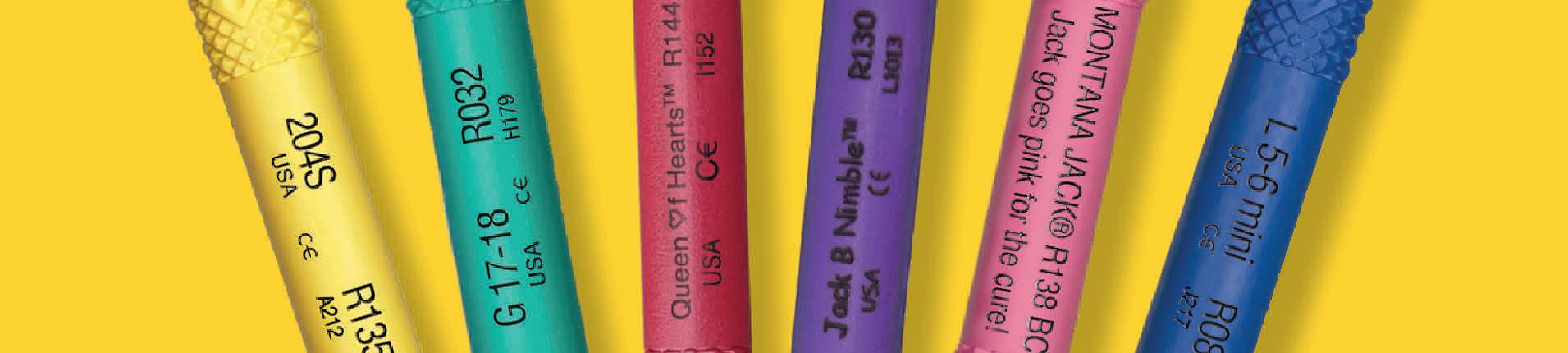






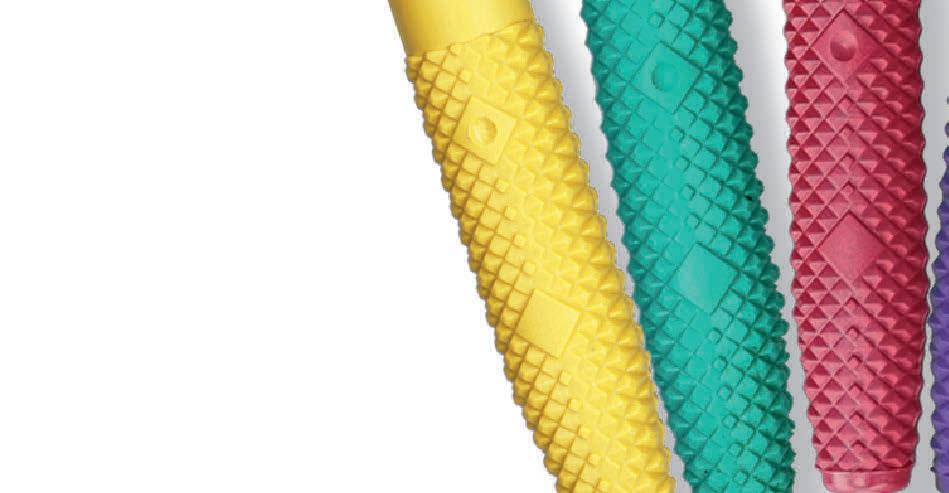





















Expertly















FINER • SHARPER • STRONGER

Evil energy
Learning objectives
• To understand the impact of energy drinks on oral health
• To identify patients who may be more likely to consume energy drinks
• To find hygienic solutions for patients who drink energy drinks
Across the UK, 1.7 million people consume energy drinks 2-3 times a day. i Alarmingly, one third of the children in the UK have them every week. ii Designed to improve physical and mental performance, the popularity of this type of beverage is led by athletes, students, adolescents, and night-shift workers, iii with 26% of Brits needing an energy drink to wake up in the morning and 23% needing one to get through the rest of the day. iv
However, the consistent consumption of energy drinks is damaging to oral health, and also overall health. One of the reasons why young adults are attracted to energy drinks may be because of a lack of knowledge of their potentially harmful effects. v As the industry is showing no signs in slowing down – its projected growth by 2031 is £83.88 billion – it is imperative that patients are made aware of the damage that energy drinks can cause to their oral health and beyond. vi

The double threat
Energy drinks are acidic, with an average pH of 2.5-3.5. iii The citric acid in energy drinks is highly erosive, and the demineralising effect of citric acid continues even after the pH has been neutralised. v They are also high in sugar; 63% of consumers misjudged how much sugar is in an energy drink, with some brands containing more than six spoons of sugar in one can – that is the total recommended daily allowance for an adult. iv Cariogenic bacteria such as streptococcus mutans metabolise sugar into acids that demineralise or break down tooth enamel. vii The acidity and the sugar content make energy drinks an erosive threat to teeth.
In addition to oral health complications, frequently drinking sugary beverages alters the microbiome composition of the gut, impacting function and contributing to the risk of obesity, cardiovascular diseases and increased mortality. viii Educating at-risk patients about the threat of energy drinks is vital for their health.
Energising athletes
Among the consumers of energy drinks, athletes are prone to oral health risks. Peak sporting performance can be attained through the frequent consumption of foods, drinks, energy bars and gels that are rich in carbohydrates. 66.7% of elite athletes consume sports and energy drinks, with the former
GDC Development Outcome: C

replenishing electrolytes and the latter using caffeine to improve endurance. viii
Of the athletes who consume energy drinks, 63.5% have dental caries and 46.1% have gingivitis. viii As athletes tend to focus on physical health rather than their dental health, the risk of oral diseases is higher. ix Furthermore, intense exercise can lead to immunosuppression, which alters saliva composition. viii Saliva may then fail to neutralise the erosive acids, further increasing the risk of dental erosion. Promoting an effective oral hygiene routine can offset the oral health risks in energy drink-consuming athletes.
Helping youth
Boys and older adolescents are far more likely to drink energy drinks. The pleasant taste and the promise of a stimulating effect that keeps them awake is why they are so regularly drunk. x But all young people are vulnerable. As well as physical health implications, energy drinks have been shown to have an impact on mental health. As dopamine, serotonin and adrenaline are secreted when consuming an energy drink, they are highly addicted and are associated with poor lifestyle choices and self-destructive behaviour.xi
Other effects of energy drink consumption include:
• Poor sleep quality/insomnia
• Low academic performance
• Psychological distress
• Panic and anxiety disorders xii
• ADHD symptoms (hyperactive energy can cause teeth grinding and tooth loss) xiii
The consumption of energy drinks may be only one factor in the aetiology of oral health diseases. For those that regularly have these beverages, there are strong correlations with smoking, binge drinking (with energy drinks often used as a mixer), skipping meals, an unhealthy diet, and substance abuse.vi All of these can heighten the risk of oral health complications, so promoting the regulation or prohibition of these habits is a key task for practitioners. A growing number of young children consume energy drinks, particularly those from socio-economically disadvantaged backgrounds. ii 18% of children aged 3-10 have consumed an energy drink, despite the recommendation that you must be over 16 to have one. vi As 4% of people say that they feel addicted to energy drinks, it is crucial that young patients are deterred from frequently drinking them. xiv
What we can do
The adverse effects of drinking energy drinks can have implications across oral health, physical health, and mental health. As a practitioner, developing your relationship with patients can help educate them on risks to their oral health. Communication over lifestyle habits, such as frequently consuming energy drinks, and the impacts they can have on their health may deter patients from these habits. Using posters in your practice can help educate children and young adults on the effects of energy drinks too. Encouraging a consistent oral hygiene routine is essential to prevent oral diseases. As the fermentation of dietary carbohydrates releases the acid that causes caries, effectively removing the particles from the oral cavity can promote a healthier mouth. iii Whilst toothbrushing twice a day and drinking water after consuming sugary products can help, interdental cleaning is recommended to disrupt the particles that a toothbrush cannot reach.
For a superb interdental brush, the FLEXI from TANDEX can access the areas that were previously missed. There are 11 different colour-coded sizes to meet

the demands of the patient. Between the flexible handle and the malleable brush, FLEXI is designed for ergonomic satisfaction, helping to comfortably reach all the interdental spaces. PREVENT Gel from TANDEX can be easily applied using a FLEXI brush, introducing enamel strengthening properties and 0.12% chlorhexidine for the gold standard of oral disinfection. Pleasant tasting and non-abrasive, PREVENT Gel ensures an enjoyable experience to increase adherence to an effective oral hygiene
routine. With TANDEX products, your patients can optimise their health.
As energy drinks continue to grow in popularity, the risk of caries or gingival diseases will increase. Identifying patients who regularly consume them is important in order to educate them on the health implications, whilst preventing young children from developing this habit is essential for their long-term oral and overall health.
For more information on Tandex’s range of products, visit https://tandex.dk/ or visit the Facebook page: https://www.
To answer the questions below, visit cpd.the-probe.co.uk and register/log in. Click on ‘Courses’. Search for the course with the same headline as the corresponding article.
facebook.com/TandexUK
Our products are also available from DHB Oral Healthcare https://dhb.co.uk/ n
References available upon request
About the author
Jacob Watwood on behalf of Tandex.

1. What is the average pH for an energy drink?
a. 1.5-2.5
b. 2.5-3.5
c. 3.5-4.5
d. 4.5-5.5
2. Which of the following demographics is not associated with regular energy drink consumption?
a. Athletes
b. Students
c. Night-time workers
d. The elderly
3. Which of these is a risk of high sugar consumption?
a. Cardiovascular disease
b. Obesity
c. Increased mortality
d. All of the above
CPD questions – Evil energy
4. Which of these is not a health effect of drinking energy drinks?
a. Insomnia
b. Panic / anxiety
c. Common cold
d. Low academic performance
5. Which of the following has a strong correlation with energy drink consumption?
a. Binge drinking
b. High grades
c. A wealthy background
d. Excelling at sports
6. What is the percentage of children aged 3-10 who have had an energy drink?
a. 4%
b. 8%
c. 15%
d. 18%
How can steroid use impact oral health?
Learning objectives
• Understand what steroids may be used for in dental and medical settings
• Consider the impact of steroid use on general and oral health
• Recognise how tailored oral hygiene advice can support patient care
GDC Development Outcome: C

Steroids are anti-inflammatory medicines used to treat a wide range of conditions. People may be prescribed steroids to treat issues such as allergies, asthma, inflammatory bowel disease, Addison’s disease, and arthritis. i
Over the years, various researchers have estimated the number of people in the UK being prescribed steroids. One study, from 2000, estimated that 0.9% of the population were using oral corticosteroids at any point in time, most commonly people aged 70-79.
ii Another study, from 2020, examined the
potential over-prescription of steroids, finding that more than 35,500 people were prescribed a high dose of prednisolone, with over one million taking the drug in that year alone.iii
With the use of steroids widespread in this country, it’s important that primary care providers are aware of its potential risks and side-effects to help patients more effectively manage their oral health.
What are steroids prescribed for in dentistry?
In dentistry, steroids are most commonly used in the treatment of post-surgery
discomfort, as well as oral lichen planus, pemphigus, recurrent aphthous stomatitis, and temporomandibular disorders. In the short-term, steroids are helpful for easing patients’ recovery. However, in the longterm, over prescription or over use of steroids can have the potential to effect systemic and oral health. iv
Using systemic steroids to treat oral lesions over a long period of time may result in weight gain, delayed healing, increased likelihood of infections, osteoporosis, fractures, high blood pressure, peptic ulcers, and steroid-
Up on CPD

induced diabetes. iv As such, it’s important to carefully consider the use of steroids in dentistry, and be mindful of patients who are using steroids long-term as this may have an impact on their health.
The impact of steroid use on oral health
Research also suggests that the long-term use of steroids can increase the risk of gingivitis and periodontitis. When injected into the gingivae or applied topically, steroids may disrupt the blood supply and collagen formation.
The specific effects of inhalation steroid therapy include candidiasis (a fungal infection causing white patches), xerostomia (dry mouth), altered saliva and saliva flow, mouth ulcers, irritation inside and around the corners of the mouth, caries, gingivitis, periodontitis, sore throat, hoarse voice, and cough. Research suggests that these side-effects in particular are estimated to effect between 10% and 30% of individuals.
iv Because steroid use can have a specific impact on patients’ oral health, and therefore their quality of life, it’s important that dental practitioners understand that steroids may be the underlying cause, and how to help patients manage their oral health.
Managing oral health in patients taking steroids
Periodontitis is the leading cause of tooth loss in adults – with the disease affecting the periodontal tissue structures and bone which support the teeth. Research suggests that patients with asthma and COPD who are treated with corticosteroids had a higher incidence of periodontal disease than those who were not. As such, it is important that dental professionals are aware of this risk, whether patients inhale steroids or receive them orally. v Special considerations must be made for patients who are undergoing steroid inhalation therapy. This should include educating patients about the possible adverse effects, and recommend the use of a spacer device to reduce the amount of medication deposited in the mouth. Regular oral health examinations are essential to monitor patients’ health – the frequency of these examinations should be based upon the oral disease risk of each individual. Further, encouraging proper oral hygiene practices is essential for maintaining oral health – including brushing the teeth twice per day and interdental cleaning once per day. It is also recommended that patients
undergoing inhalation therapy rinse the mouth after use, especially before bed to counteract the medicine’s potential sideeffects. vi
The use of chlorhexidine is recommended for its antimicrobial effects, as is a diet of reduced sugary foods or drinks and increased fluid intake. The addition of fluoride is also important for these patients, to help maintain the strength of the teeth. vi
Oral health solutions for targeted care
In order to provide targeted care to patients who need it, ensure you’re recommending products which benefit their unique needs. Interdental cleaning is essential for all patients, particularly those who are experiencing gingivitis or periodontitis. Removing plaque and debris will help to reduce the risk of these conditions, and protect the gingivae and dentition. Further, for those who require enhanced protection, recommend oral hygiene supplements which include ingredients for strengthening the teeth and offering an antibacterial effect.
TANDEX, the premium oral health brand from Denmark, offers a wide range of oral hygiene solutions to help your patients keep
their teeth and gingivae healthy. Recommend the range of FLEXI interdental brushes to help patients clean in between their teeth far more easily than using dental floss. The FLEXI’s flexible handle and range of 11 different sizes make it easy to clean every interdental space. Additionally, recommend that patients apply PREVENT GEL using the FLEXI for an oral health boost. PREVENT GEL contains 0.12% chlorhexidine and 900ppm fluoride for an antibacterial effect and enamel strengthening properties. Long-term steroid use can have an effect on patients’ general and dental health. Whilst they are suitable for treating a number of conditions, both relating to oral health
and systemic health, over prescription or over use may lead to problems down the line. These can affect patients’ overall and dental health, with caries, gingivitis, and periodontitis particular concerns. Knowing this, dental practitioners should ensure a full medical history is taken, to give them a proper understanding of factors which may impact dental care. Special care must be taken when treating patients who are taking steroids to improve their oral health in order to reduce the risk of complications.
For more information on Tandex’s range of products, visit https://tandex.dk/ or visit the Facebook page: https://www.facebook.com/ TandexUK
To answer the questions below, visit cpd.the-probe.co.uk and register/log in. Click on ‘Courses’.
Search for the course with the same headline as the corresponding article.
Our products are also available from CTS
Dental Supplies https://www.cts-dental.com/ and DHB Oral Healthcare https://dhb.co.uk/ n
References available upon request
About the author
Jacob Watwood on behalf of Tandex.

CPD questions – How can steroid use impact oral health?
1. What medical issues might steroids be used to treat?
a. Asthma
b. Inflammatory bowel disease
c. Arthritis
d. All of the above
2. How many people were prescribed a high dose of prednisolone in 2020?
a. 25,500
b. 35,500
c. 45,500
d. 55,500
3. What oral health conditions might steroids be used to treat?
a. Post-surgery discomfort
b. Oral lichen planus
c. Recurrent aphthous stomatitis
d. All of the above
4. Which of these is NOT a side-effect of long-term use of systemic steroids to treat oral lesions?
a. Weight loss
b. Delayed healing
c. Increased likelihood of infections
d. High-blood pressure
5. Inhalation steroid therapy impacts oral health in what percentage of cases?
a. 0-20%
b. 10-30%
c. 20-40%
d. 30-50%
6. What special considerations should be made for patients who are undergoing steroid inhalation therapy?
a. Encouraging proper oral hygiene practices
b. Use of a spacer device
c. Regular dental check ups
d. All of the above
An introduction to the S3 Treatment Guidelines for Periodontitis
Kenvue is delighted to bring you this article, with the aim of supporting the ongoing Enhanced CPD needs of dental healthcare professionals in improving and maintaining the oral health of their patients.
The aim of this article is to introduce and offer context for the European Federation of Periodontology’s (EFP) S3 Treatment Guidelines for Periodontitis, as well as the British Society of Periodontology’s (BSP) adolopment of them.
On completing this Enhanced CPD session, the reader will:
• Understand the need for the creation of the EFP’s S3 Treatment Guidelines for Periodontitis
• Understand the intricacies of the adolopment process and its role in tailoring the EFP S3 Treatment Guidelines for Periodontitis for the UK
• Understand the clinical impact and patient outcomes associated with the stepwise approach recommended by the BSP S3 Treatment Guidelines for Periodontitis for periodontitis management
• Understand how guidelines support clinicians in making evidence-based treatment decisions and prioritising personalised patient education in periodontitis management.
• Understand the potential for systemic health benefits associated with managing periodontitis, particularly concerning related diseases like diabetes and cardiovascular conditions.
Learning Outcomes: A,C,D
This article introduces and provides context for the European Federation of Periodontology’s S3 Treatment Guidelines for Periodontitis, along with the British Society of Periodontology’s adaptation of these guidelines.
The UK’s S3 Treatment Guidelines for Periodontitis are derived from the European Federation of Periodontology (EFP) guideline. 1 This original guideline was created using an S3-level methodology, which involved the evaluation of evidence from 15 systematic reviews combined with a consensus process among diverse stakeholders. It addresses health equity, environmental factors, and clinical effectiveness. The guideline offers 62 clinical recommendations for managing stage I–III periodontitis, organised in a step-by-step (stepwise) approach according to the 2017 classification system.2
A global challenge
Periodontitis is a chronic, multifactorial inflammatory disease linked to dysbiotic dental plaque biofilms. It involves the progressive breakdown of the structures supporting the teeth.2
Key indicators of this condition include clinical attachment loss (CAL) and alveolar bone loss observed through radiographic examination, along with periodontal pocketing and gingival bleeding. Without treatment, periodontitis can result in tooth loss. However, it is largely preventable and treatable in most instances.2
Despite being largely preventable, oral diseases present a significant health burden globally, as reported by the World Health Organization (WHO). They affect individuals across their lifespan, leading to pain, discomfort, disfigurement, and even death. Severe periodontal diseases are estimated to impact approximately 19% of the global adult population, accounting for over 1 billion cases worldwide. 3

As stated by West and colleagues (2021): ‘Periodontitis is a major public health problem due to its high prevalence, and since it may lead to tooth loss and disability, it negatively affects chewing function and aesthetics, is a source of social inequality, and significantly impairs quality of life. Periodontitis accounts for a substantial proportion of edentulism and masticatory dysfunction, has a negative impact on general health and results in significant dental care costs.’2
In addition to the direct consequences of periodontitis outlined earlier, periodontal infections are associated with various systemic diseases that can contribute to premature mortality. These include diabetes, cardiovascular diseases, and adverse pregnancy outcomes.2
Addressing UK need
Following the release of the EFP’s clinical practice guideline for treating stages I-III periodontitis in July 2020, the next phase involved implementing the recommendations of this international document at the national level.1,4
The BSP was one of just three national periodontal associations that opted to undergo the official ‘adolopment’ process, to ensure the guideline’s proper implementation in the UK (alongside Germany and Spain).4
This entailed making some adjustments to the original guideline to align seamlessly with the national healthcare system or adhere to national regulations, involving close collaboration with numerous
stakeholders. For instance, in the UK, one of the 62 recommendations was omitted,* whereas in Germany, another recommendation was revised and rephrased to prevent potential legal issues.4
As stated by the EFP, ‘Adolopment is a new word made up of three familiar words: adoption, adaptation, and development. It is used to describe an intricate process in which clinical practice guidelines that have been drawn up to the highest regulated standard – the S3 level – can be implemented in specific countries with the highest level of flexibility to ensure a perfect “fit”.’4
In essence, it involves adaptation through the GRADE Adolopment process, leveraging a highquality guideline like the EFP’s as a foundational blueprint for national adoption. Instead of reinventing the wheel, this approach streamlines the adaptation process. For each of the 62 recommendations in the EFP guideline, decisions had to be made whether to adopt them unchanged, modify them, or introduce additional recommendations.4
Ultimately, ‘The S3-level guideline development is a combination of a systematic appraisal of the available evidence and the combined clinical “common sense” of a guideline group representative for the addressees of the guideline.’4
Guideline overview
The BSP states: ‘The guidelines are there to support clinicians when treating periodontal disease, helping them make up to date evidence-based treatment decisions and focus on personalised patient education. This in turn should empower patients to take more responsibility for their health, ultimately improving outcomes.’5
Regarding their application, the guidance follows a ‘stepwise’ treatment approach, addressing Stages I, II and III of the disease.5 Guidance for Stage IV is under evaluation and will be published separately, as it poses distinct challenges due to its complex restorative rehabilitation needs, requiring a multidisciplinary approach to management.5,6
Looking at the available guidance in further detail, Roberts, Winning and Harrison (2021) wrote: ‘The guideline recommends four steps of periodontal therapy, to be undertaken sequentially, alongside 62 individual recommendations that are rated according to the strength of consensus and grade of recommendation of each working group.’6
In practical terms, each of the four treatment steps, ‘…includes different interventions and builds incrementally on previous steps; the disease stage and response to treatment will impact on the interventions required.’6
Furthermore, ‘Clinicians should discuss the periodontal diagnosis, risk factors, treatment alternatives, and the risks and benefits of treatment with each patient, and then agree a personalised care plan for each patient.’6
In summary, the four steps for Stages I to III of periodontitis are as follows:6
• Step 1: ‘Guiding behaviour change by motivating the patient to undertake successful removal of supragingival dental biofilm and risk factor control.’
• ‘Step 2: Cause-related therapy, aimed at controlling (reducing/eliminating) the subgingival biofilm and calculus (subgingival instrumentation).’
• ‘Step 3: Treating areas that do not respond adequately to the second step of therapy, to gain
CPD Questions
1. What is the primary purpose of the UK’s S3 Treatment Guidelines for Periodontitis derived from the EFP guideline?
a) To standardise dental practices globally
b) To promote environmental sustainability
c) To provide evidence-based guidance for clinicians
d) To regulate dental education standards
2. Which term best describes the process of adapting the EFP guideline for national implementation in the UK healthcare system?
a) Adaptation
b) Adoption
c) Adolopment
d) Development
3. How many clinical recommendations are offered by the EFP guideline for managing Stages I, II and III periodontitis?
a) 15
b) 30
c) 45
d) 62
4. According to the BSP, what does the guideline aim to emphasise to clinicians?
a) Surgical intervention techniques
b) Patient-centred education
c) Cosmetic dental procedures
d) Holistic dental care
5. What is the specific focus of Step 2 in the treatment of Stages I, II and III periodontitis?
a) Management of systemic health conditions
b) Prevention of periodontal pocketing
c) Treatment of intra-bony and furcation lesions
d) Cause-related therapy
further access to subgingival instrumentation or aiming at regenerating or resecting lesions that add complexity to the management of periodontitis (intra-bony and furcation lesions).’
• ‘Step 4: Supportive periodontal care (SPC), aimed at maintaining periodontal stability in all treated periodontitis patients, combining preventive and therapeutic interventions defined in the first and second steps of therapy, depending on the gingival and periodontal status of the patient’s dentition.’
Overcoming everyday challenges
As stated succinctly by Roberts, Winning and Harrison (2021): ‘From the practitioner’s perspective, it is important to note that the S3-level treatment guidelines are indeed just that: ‘guidelines’. Individual judgement and adaptation can of course be applied at the practitioner’s discretion.’6
They continue: ‘However, the fact that these guidelines now exist and are currently being adopted by national societies and stakeholders across multiple European jurisdictions allows for standardisation and transparency in our approach to the management of periodontitis. This will be of benefit to both patients and practitioners alike.’6
* In the UK, the issue revolved around the recommendation concerning the inclusion of antiseptics in toothpaste, where consensus could not be achieved. Therefore, recommendation 4.12 regarding dentifrice and antiseptics was not adopted.4
References
1. Sanz M et al. Treatment of stage I-III periodontitisThe EFP S3 level clinical practice guideline. J Clin Periodontol 2020; 47(Suppl. 22): 4-60
2. West N et al. BSP implementation of European S3-level evidence-based treatment guidelines for stage I-III periodontitis in UK clinical practice. Journal of Dentistry 2021; 106: 103562
3. Oral health. WHO 2023. Available at: https://www. who.int/news-room/fact-sheets/detail/oral-health. Accessed 19 June 2024
4. Perio Insight 15. EFP 2021. Available at: https:// www.efp.org/fileadmin/uploads/efp/Documents/ Perio_Insight/Perioinsight15.pdf. Accessed 18 June 2024
5. Vithlani V, Dunn I. S3 Treatment Guidelines for Periodontitis. BSP Available at: https://www. bsperio.org.uk/news/s3-treatment-guidelines-forperiodontitis. Accessed 18 June 2024
6. Roberts A, Winning L, Harrison P. Periodontitis: all change please? Introduction to the new S3-level treatment guidelines. Journal of the Irish Dental Association 2021; 67(5): 262-266 n
This article is equivalent to one hour of Enhanced CPD. To provide feedback on this article, please contact dentalcpd@its.jnj.com
UK-LI-2400215
How intraoral scanners can be used to inform digital workflows, create optimal care journeys and enhance practice growth opportunities
Align Technology is delighted to bring you this article, with the aim of supporting the ongoing Enhanced CPD needs of dental healthcare professionals in improving and maintaining the oral health of their patients.
On completing this Enhanced CPD session, the reader will:
• Communicate effectively to educate patients on ways to improve their oral health
• Aid discussions in the dental chair, helping to prevent, diagnose, and treat oral health conditions
• Maximise skillsets, technology, treatment acceptance, and practice revenue
• Streamline dental practice processes, improve the patient and staff experience
Learning Outcomes: A,B,C,D
Dynamics in the oral health space
Recruitment and retention of dentists and other practice team members is a major issue impacting capacity, access and delivery of care. The macroeconomic environment continues to create financial pressure on dental practices. We need to continuously look for ways to adapt operational models, streamline staff training, and improve patient communication for long term practice stability.
During the first 10 years of my career as a Dental Therapist (DT), I experienced a significant increase in frustration levels due to these challenges. A typical day involved seeing up to 20 patients in 30-minute appointment slots, with no supporting dental nurse. This meant minimal time to communicate effectively, including educating patients on how to improve their oral health. A truly disheartening situation - I knew these patients would likely return in six months with the same issues. And I knew that improved collaboration with other clinical team members could help, particularly while the patient was still at the practice. But it felt like we were in a vicious circle.
Driving change – moments of wisdom in the dental chair
Dental Therapists play a unique role at the heart of dental teams, a role that is often misunderstood and under-utilised. In fact, guidance from NHS England on potential business models for NHS General Dental Practices referred to research and practice-based evidence about the clinical effectiveness, safety, and acceptability of using Dental Therapists and Dental Hygienists to provide preventative and diagnostic care to patients, alongside performing a range of treatments to both adults and children. They were told by practice owners that working with DTs is economical, increases patient access, and promotes efficient division of labour across the dental team.
With that understanding, I had the opportunity to attend an Align Technology practice training event that changed my perspective even further.
During the session I was impressed by the iTero™ scanner and its patient education capabilities. Using these digital features meant that I could show my patients the issues I could personally see inside their mouth. At that point, the iTero scanner was not being used by DTs. I identified an opportunity to try using the iTero scanner to understand the impact on a few patients.
The first time I used an iTero scanner was with a gentleman who had a broken amalgam on the upper right second molar, something recorded on his treatment plan for several years but which he had chosen not to address. It was asymptomatic; however, when I showed it to him on the scan, his reaction was: "Get that out of my mouth." This was a pivotal moment for me. I understood the benefit
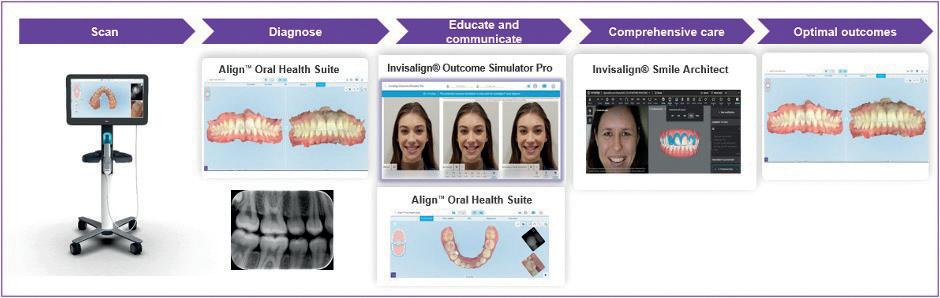
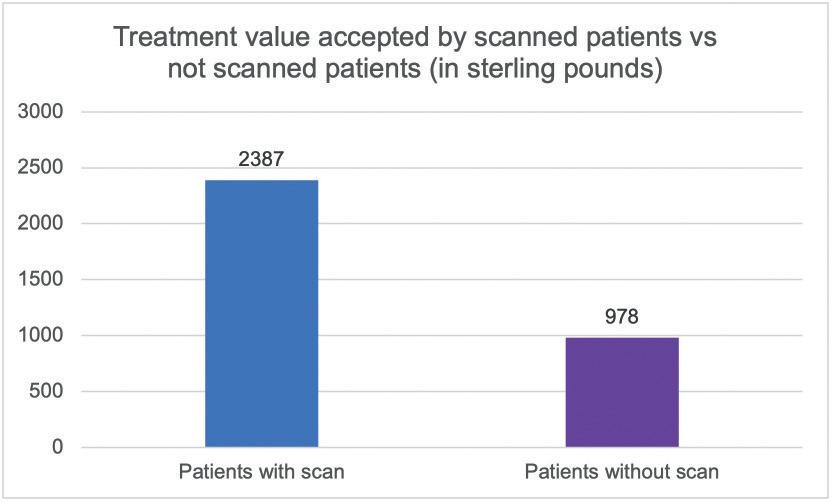
of scanning for everyone who would come into our practice, including patients who had never been scanned before, but who I had treated for many years.
Bringing digital dentistry to a new practice – maximising skillsets, technology, treatment acceptance, and practice revenue
Since then, I have moved to a Dental Therapist role in London's financial district where I have introduced a therapist-led model that has significantly improved patient care. I introduced a protocol which involves scanning every patient at every appointment. I now see up to eight patients daily, a mix of both new and existing. The iTero scanner is in constant use, helping to empower our patients to visualise and understand potential issues and to make informed decisions about their oral health. In turn, this has driven treatment acceptance and enhanced the quality of care we provide.
This therapist-led model is highly collaborative and involves multiple team members. My responsibility is to stabilise patients and refer them to the hygienist to address their periodontal needs. Dentists are responsible for treatments such as occlusion, tooth movement, and indirect restorative procedures. I ensure treatments are completed as planned (figure 1).
Results: We increased the number of scans by 167% within six months: Scanning every patient led to significant changes. Using the iTero intraoral
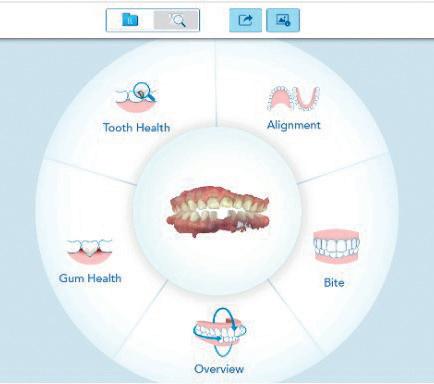
scanner has improved patient communications, and being able to visualise their oral health at the chair side, means that patients are more likely to embrace our recommended treatment plans, including orthodontic care.
Our analysis reveals that patients who have not been scanned have an average treatment value of £978, while scanned patients have a treatment value of £2,387 - a 145% increase in revenue (figure 2). This increase is a testament to the improved quality of care and outcomes achieved when utilising the right tools to communicate treatment plans. In turn this has led to the prevention of discomfort, fewer emergency visits and enhanced quality of life for our patients.
Optimising the iTero scanner tools during consults
During a patient consultation, I discuss their dental needs and concerns. This is followed with an iTero scan, to help better understand their oral health, including diagnosing any issues or identifying changes they would like to make. I encourage my patients to watch the screen during the scan. They are often amazed by the quality of the images, and this helps to prompt wider discussion.
Figure 1. Enhanced workflow shows the scan as an essential tool for aiding diagnosis, communication and education
Figure 3. The Align™ Oral Health Suite showing the patient’s scan in the centre and the oral health conditions displayed in the circumference
Figure 2. Revenue from scanned patients vs. patients who were not scanned during their consultation examination
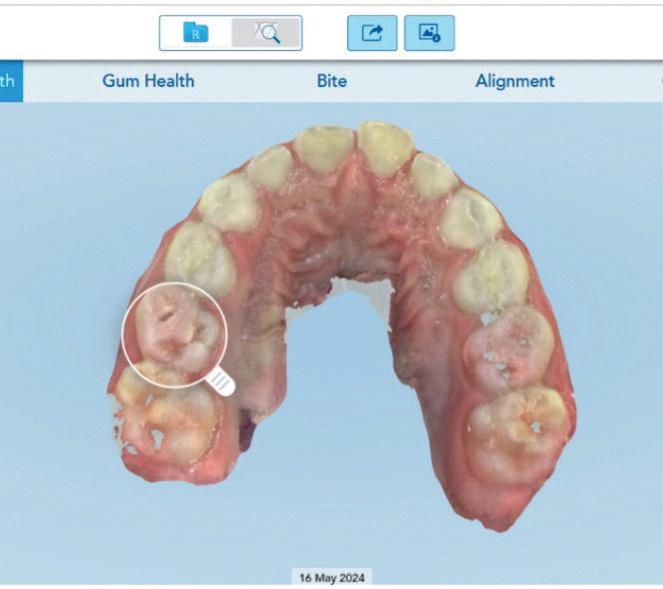
After also capturing extraoral photographs, we review the scan together using the Align™ Oral Health Suite (figure 3).
The Align Oral Health Suite has a selection of tools available to highlight findings, while the iTero™ Near Infra-Red imaging (NIRI) technology (figure 4) helps us identify potential interproximal carious lesions, which we then confirm with bitewing radiographs. We also closely examine stone model views of the scan (rather than full colour) to assess tooth wear, erosion, and recession areas – and the implications of not going ahead with treatment. I analyse the results to create a treatment plan while the nurse uses the Invisalign® Outcome Simulator Pro for in-face visualisation. Throughout, we avoid using technical dental language and take advantage of the scanner's visualisations to explain each finding.
My favourite ways to use the iTero scanner NIRI is my favourite feature. It supports me when assessing interproximal lesions and is especially helpful when treating young children or those that cannot tolerate bite wing radiographs. NIRI’s non-ionizing radiation also allows us to scan patients more often, based on their risk of dental caries. Being able to view scans from multiple angles helps us to determine if lesions are present when you have bitewings with overlapping surfaces. This is not possible with radiographs.
In addition, for patients presenting interproximal carious lesions, I can effectively treat them with resin infiltrations. We scan the patient post-treatment to determine the success of the restoration, which is impossible to determine with radiographs. Generally, I treat these lesions per quadrant, and then rescan and show the before-and-after with the Align Oral Health Suite. I can justify this less invasive treatment because it is costeffective for the clinic and less invasive for the patients.
Conclusion
In my opinion, iTero scanners can completely transform workflows, streamline processes and improve practice performance. By empowering staff, it creates stronger loyalty and offers career development opportunities to Dental Therapists and Hygienists. By creating personalised visualisations to aid discussions in the dental chair, helping to prevent, diagnose, and treat oral health conditions, scanners provide patients with valuable information to make informed decisions about accepting comprehensive dental care.

CPD Questions
What percentage of patients does the author scan at every appointment?
A 50 per cent
B 100 per cent, but only at the first appointment
C 100 per cent
D 25 per cent
2. Which feature of the iTero scanner is used to identify interproximal caries lesions?
A. NiTi
B. NIRI
C. NaNa
D. NoNo
3. What does the writer’s Nurse use the Invisalign® Outcome Simulator Pro for?
A. In-face visualisation
B. In face care
C. In face assessment
D. In face analysis
4. What is the average treatment value of the writer’s scanned patients?
A. £5000
B. £1,000
C. £2,000
D. £2,387
5. What was the age of the young patient featured in the case study who was able to engage with his own scan on screen?
A. Ten years’ old
B. Thirteen years’ old

Clinical Case Study
A six-year-old male patient presented to my clinic. His mother requested a second opinion after noticing dark areas on his teeth, something for which his previous dentist had only applied fluoride.
Before scanning, I explained what a scan was and handed him a wand tip so that he could feel its soft texture and flexibility. I showed him a scan and invited him to touch the screen and spin the 3D model around. I promised he could do the same with his own scan.
Clinical findings
I detected carious lesions in all lower deciduous molars and the upper second deciduous molars. I recommended sealants in the upper and lower primary permanent molars to prevent future decay. The upper left central incisor and lower right central incisor were loose, and the lower left deciduous central incisor had recently exfoliated. This patient also presented an anterior open bite due to thumb sucking which will be closely monitored to prevent further issues.
The mother accepted all recommended
C. Six years’ old
D. Eighteen years’ old
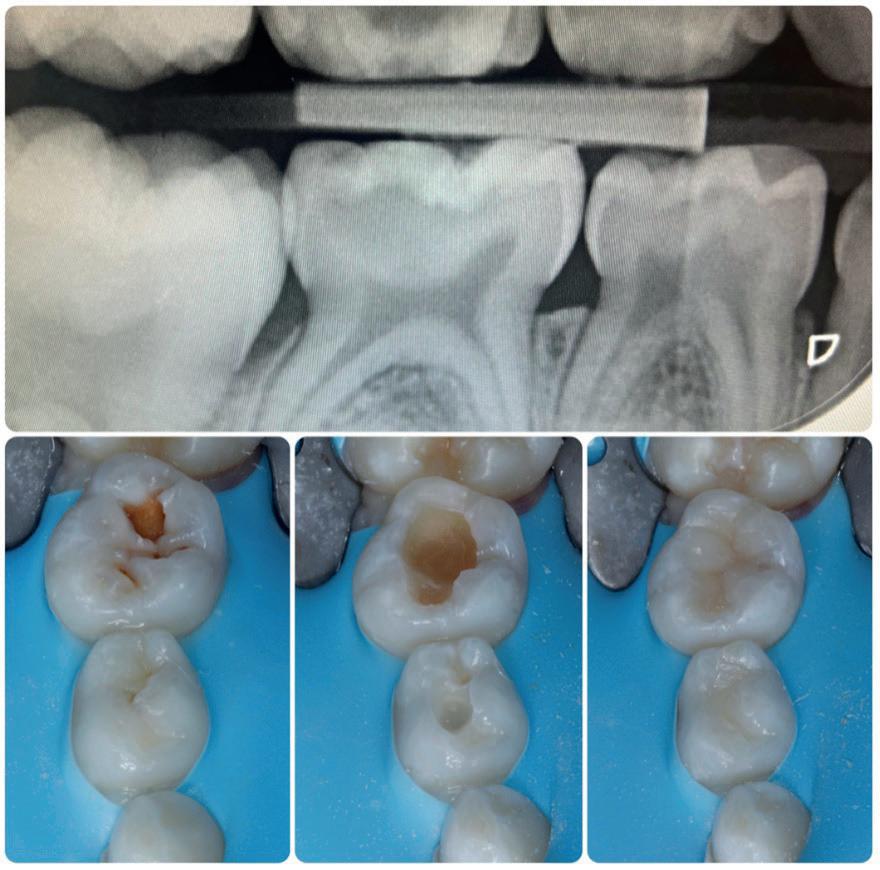
treatments, stating: “Bringing my son to have this examination was a world away from the dentistry we have experienced in the past. He was included in every discussion, and it was clear that he learned a lot on the day. Every child (and every adult!) should have an experience like that.” n
This article is an adaptation of a white paper by Cat Edney published in October 2024
ABOUT THE AUTHOR
CAT EDNEY DH DT PGDIP (DIST)
Multi-award winning Dental Therapist Cat Edney has over 15 years’ experience working in specialist and private practice..

Figure 4. The Align™ Oral Health interface for Tooth Health condition shows the 3D model, the iTero Near Infra-Red imaging (NIRI) technology view, and the integrated intraoral camera view
Figure 5. New patient exam with a young child using the iTero™ scanner and the Align™ Oral Health Suite to help diagnose, communicate, and educate the patient and his mother, and build a treatment plan.
Figure 7. Images from a bitewing radiograph and preparations and final restorations on deciduous molars during the restorative phase
The Dental Awards 2025 is now open for entries
An early bird discount is in effect until 13th January 2025

The countdown to The Probe’s Dental Awards 2025 is on, as entries are set to open at the-probe.co.uk/awards in November.
Register before 13th January 2025 to qualify for an early bird discount of £35 per entry.
2025 marks the 27th year for The Dental Awards, presented by The Probe, which celebrates the very best of British dentistry.
As the original and most respected awards programme in UK dentistry, The Probe’s Dental Awards are judged by a panel of leading practitioners and KOLs, providing an unrivalled opportunity for practices and DCPs to shine a spotlight on the vast skill and talent that exist within their teams.
The 12 categories forming The Dental Awards 2025 are:
• National Smile Month Award
• Dentist of the Year
• Young Dentist of the Year
• Dental Therapist of the Year



• Dental Hygienist of the Year
• Practice Manager of the Year
• Dental Nurse of the Year
• Front of House/Receptionist Award
• Practice of the Year
• Team of the Year
• Best Outreach or Charity Initiative
• Best Website or Digital Campaign
For more information on each category, including entry criteria, visit https://the-probe. co.uk/awards/categories/
“We at The Probe are so excited to announce the 27th edition of The Dental Awards for 2025 – the longest-running awards event in British dentistry,” said James Cooke, Editor of The Probe. “And, for the fourth year in a row, we’re going to follow what has proven to be a popular and successful new format for The Dental Awards ceremony. Finalists, Highly Commended, and Winners will all be announced via a streamed video presentation




in the spring. The winners will then have the opportunity to join members of the judging panel and our sponsors for a free, intimate meal, where they will be presented with their certificates and trophies in person. So, there’s no need to pay extortionate ticket costs!”
The Dental Awards 2025 is presented by B.A. International, Colosseum Dental, Dental Elite, and Waterpik, in association with The Association of Dental Administrators and Practice Managers, British Association of Dental Nurses, British Association of Dental Therapists, British Society of Dental Hygienists and Therapists, and the Oral Health Foundation.
For more i nformation on our sponsors and partners, visit https://the-probe.co.uk/awards/sponsors/ Entry closes 24th February 2025. Those who enter before 13th January 2025 qualify for an early bird rate of £35 per entry. All entries on or after 13th January 2025 will be priced at £60 each. n











Thrilled to welcome a new professional the team!
Dental Elite offers bespoke recruitment services, to help talented professionals find the best opportunities, as well as to meet the requirements of all its valued clients.
The company is thrilled to welcome Mark Rushton to the Dental Elite recruitment team. As an experienced recruitment resourcer, he identifies and attracts top talent, connecting them with dental practices, to meet their specific needs.
As part of Dental Elite’s excellent recruitment team, Mark will work tirelessly to ensure the right practices are matched with the right candidates. Whether you are a dental practice looking
to secure a great colleague, or a professional looking for a great place to work, Dental Elite has a solution for you.
To find out more, contact the team today.

For more information contact the Dental Elite team on 01788 545900 https://dentalelite.co.uk/
dentalelite.co.uk
How confident are you in your service contracts?
If you have been left wanting from your current decontamination equipment service provider, consider making a switch.
Eschmann – the expert in infection control – is proud to offer the truly comprehensive Care & Cover service and maintenance package. With no hidden fees, this guarantees access to unlimited breakdown cover and Eschmann original parts and labour, as well as Annual Validation & Pressure Vessel Certification, annual servicing and software upgrades, and enhanced CPD user training. We also offer a UK-based technical support telephone line and a network of 50+ Eschmann-trained engineers nationwide, who fix 91% of issues in their first visit.

Don’t wait for an equipment malfunction or a failed CQC inspection to discover that your equipment is not sufficiently covered or validated by your current service provider. Check your service contract today and make a change for complete confidence that you’ll be protected in the future.
For more information on leading Eschmann decontamination products, please visit the website or call 01903 753322
eschmann.co.uk
Accurate notes, perfectly transcribed in real time
Kiroku is already superpowered, saving clinicians literally hours of time making notes and producing essential documentation. The new advanced AI assistant features in Kiroku are designed by dentists to be a total game-changer.
New voice transcription features allow you to create consultation notes from your discussions with patients in real time. This ensures an accurate record every time, safeguarding clinicians, and facilitating more effective communication with patients.
Once the information is input, you have everything you need for documentation, including summaries, advice and information for patients, professional referral letters and consent forms, all converted from consultation notes at the touch of a button.
Filling in the gap
For patients with a diastema or spaces, using a toothbrush may fail to clean between the teeth. An interdental brush is the solution, and the FLEXI range from TANDEX will tackle the hidden plaque effectively. Recommended by dentists and dental hygienists, the FLEXI series has 11 different sizes, with larger ones ideal for cleaning around braces and diastemas. Reaching all the places a toothbrush cannot, the FLEXI reduces plaque and massages the gums to create a comfortable and clean experience, especially when used with the easily applied PREVENT Gel from TANDEX.
Featuring a flexible handle and a malleable brush, the FLEXI is a simple yet effective addition to the daily dental hygiene routine. By getting to the places that
With the amazing AI features from Kiroku, you can audit all your notes instantly, never missing a key detail again. The system learns from your style, and provides relevant input prompts and suggestions for edits to templates to make your life easier.
Find out more by contacting the team today!
To find out more about Kiroku, or to start your free trial, please visit trykiroku.com.
trykiroku.com

toothbrushes cannot, the FLEXI is a key ally in fighting off oral health complications.
For more information on Tandex’s range of products, visit https://tandex.dk/
Our products are also available from DHB Oral Healthcare https://dhb.co.uk/
tandex.dk
A fast response and excellent support

Amanda Dillaway is the Practice Manager at Brampton Dental Practice in Cambridgeshire. She comments on the team’s experience of working with Eschmann:
“Our engineer, Gary Conway, recommended the Enbio autoclave as the best fit for us when our old machine couldn’t be repaired any more. The Eschmann team took away our old equipment and installed the new machine while providing training for the team – it was also kindly made clear that we could arrange any further training if needed.
“Since the new equipment was installed, we have received a fast and efficient response from Eschmann regarding any information or clarification we needed.
“The team think the Enbio is brilliant, especially because it is big enough to fit the implant kits – our implant dentist brings kits from other practices, so we need to sterilise them before use. The fast cycle time makes a huge difference to the turn-around of instruments.
“We would recommend Eschmann to other practices – our team has worked with them for years now. Whenever we contact the Eschmann team, whether by phone or text, we always get a quick answer and all the help and information that we need. They’re excellent.”
For more information on the highly effective and affordable range of infection control products from Eschmann, visit the website or call: 01903 753322
eschmann.co.uk
Add AI to the team
A busy practice can put a strain on workloads, with a risk of miscommunication.
Note-taking is a crucial part of communicating, and using Kiroku can make it fast and easy.

An AI-driven platform, Kiroku makes note taking 60% faster, incorporating clickable templates and customised options to get the important details down in a flash. This will make handovers for emergency appointments, dental hygienists and receptionists quicker, with minimal waiting time.
The industry leader in dental AI, Kiroku can help avoid team burnout, with dental nurses never having to struggle spelling complex terminology again. For non-native English and neurodivergent staff, Kiroku can empower workers by providing confidence and speed with communication.
To keep on top of your practice workload, having Kiroku’s extra pair of invisible hands will streamline your note taking to ensure that every detail is recorded accurately and quickly. Get ahead of the curve by incorporating Kiroku.
To find out more about Kiroku, or to start your free trial, please visit trykiroku.com
trykiroku.com

















Ultimate moisture control
Far outlasts co on rolls and other absorbent pads, and doesn’t lose moisture when handled.
DryTips® advantage over traditional co on rolls:
• Effective coverage of parotid orifice and buccal mucosa
• Polyethylene film for cu ing protection
• Enables easier access to molar region
• Flexible, accomodates cheek movement
• Stays comfortably in place, yet is easily removed with water spray
• Reflective coating for increased visibility and to aid in retraction

Do you have any questions? We are happy to help!
Jaeson Duckworth | +44 (0) 7590033844 jduckworth@younginnovations.com
Scan and learn more about DryTips.

Reflective coating now available.
IDEAL FOR: NEW!
• Impressions
• Occlusal adjustments
• Orthodontics
• Fluoride applications
• Composites
• Cementation
• Fissure sealing
• Paint-on techniques



FULL-DAY
GBT WORKSHOP

Claire Berry 11/01 Manchester
FULL-DAY
GBT WORKSHOP

Benjamin Tighe 01/02 Oxford
FULL-DAY
GBT WORKSHOP

Louise Warden 01/03 Glasgow
FULL-DAY
GBT WORKSHOP

Christina Chatfield 05/04 Brighton

FULL-DAY
GBT WORKSHOP
Kayley McCauley 18/01 Cardiff
FULL-DAY
GBT WORKSHOP

Amanda Gallie 15/02 Cambridge
FULL-DAY
GBT WORKSHOP

Anna Middleton 15/03 Exeter

FULL-DAY
GBT WORKSHOP
Faye Donald 12/04 Newcastle

FULL-DAY
GBT WORKSHOP
Laura Bailey 24/01 London

FULL-DAY
GBT WORKSHOP
Claire Berry 22/02 Liverpool

FULL-DAY
GBT WORKSHOP
Benjamin Tighe 29/03 London

FULL-DAY
GBT WORKSHOP
Benjamin Tighe 26/04 Jersey

Scan the code or visit www.swissdentalacademy.com to
