
















































Sunstar Oral Health, part of Sunstar, in partnership with the International Federation of Dental Hygienists (IFDH), presented the winners of the sixth edition of the World Dental Hygienist Awards at the International Symposium on Dental Hygiene (ISDH), in Seoul, South Korea.
Mayumi Kaneda, Director of the Sunstar Foundation and Wanda Fedora, President, International Federation of Dental Hygienists welcomed the global winners to the World Dental Hygienist Awards ceremony. The awards, supported by the Sunstar Foundation, celebrate and recognize the achievements of dental hygienists worldwide and were originally established in 2007.
Each of the winners received their all-expenses trip to the ceremony at ISDH Seoul, a trophy and a USD 1,500 prize, presented by Mayumi Kaneda, Director of the Sunstar Foundation.
The winners were:
• Public Health: Federica D’Anteo, Italy, Dental Hygienist at II Centro Dentale s.a.s, in Cavaria con Premezzo and author
• Research: Thérèse Elkerbout, Netherlands, Dental Hygienist and Clinical Epidemiologist at the Academic Center for Dentistry, Amsterdam
• Entrepreneur: Juhwa Lee, South Korea, Master,

Hiroshima University, Graduate School
• Full Time Clinician: Lorella Mengarelli, Italy, Dental Hygienist at Studio Tiozzi Ferroni in Cesenatico
• New RDH: Brittany Glauz, United States, Dental Hygienist, Creator of Brush with Britt Podcast, Speaker and Writer
• Academia: Gianna Maria Nardi, Italy, Dental Hygienist and Associate Professor at Sapienza University.
Mayumi Kaneda, Director of the Sunstar Foundation, commented: “It was wonderful to meet all the winners and congratulate them in person. We are so proud of all their work and incredible contributions to the profession.” n
Anetwork of Community Dental Services CIC (CDS) Support Practices has been established in the East Midlands to relieve the pressure on waiting times for paediatric patients in the aftermath of the Covid-19 pandemic. They are being operated by leading community dental provider CDS and general dental practices in the East Midlands. The aim of the Support Practices is to deliver a high-quality service for children requiring level one care.
Covid-19 caused significant interruptions to dental care and many children have not seen a dentist leading to increased dental need among this group. Teams in the practices have been supported to treat patients that may otherwise only have been able to access care through the community dental service. Paediatric patients referred to CDS are triaged and assessed for suitability for care in a Support Practice, enabling them to be seen and treated more quickly. It has increased capacity for the teams in CDS to treat more complex paediatric and special care patients, also reducing the time they are waiting for appointments.
Prior to starting to treat CDS referral patients, the dentists from the Support Practices receive online training with the Midlands Paediatric Team and a hands-on study day. Dentists take part in regular peer review sessions and are invited to attend the paediatric MCN meetings.
Milan Chande, Principal Dentist at The Dental Wellness Centre in Leicester, said, “Being a CDS support practice has been really rewarding and
The GDC has welcomed the legislative change, that came into effect on 26 June 2024, that aims to improve direct access for patients to dental hygienists and therapists, while promoting better use of the skill mix in the dental team.
The new legislation enables dental hygienists and therapists across the UK to legally supply and administer specific prescription-only medicines under an exemptions mechanism, without the need for a dentist’s prescription, a patient-specific direction or a patient group direction.
While specified medicines can legally be supplied and administered under exemptions, the GDC expects dental hygienists and dental therapists to undertake the appropriate training to ensure they are competent to use this new mechanism. There is no obligation for dental hygienists and therapists to administer and supply these medicines under exemptions, and many of them may wish to continue to rely on existing mechanisms in their work instead.
The regulator states that dental hygienists and dental therapists, regardless of previous training, experience, and qualifications, should ensure that they are appropriately trained, competent and indemnified to supply and administer specific medicines under the exemptions mechanism. This means that they should ensure they have undertaken appropriate training before supplying and administering these medicines under the new mechanism.
has upskilled the team. We usually see patients who require multiple restorations, silver Diamine Fluoride, Hall crowns or extractions. It is fantastic to know we have done something to improve the oral health of the child and have given them a positive dental experience.”
Nicola Milner, Chief Operating Officer for CDS in the East Midlands, said, “During the Covid-19 pandemic, we were used as an Urgent Care Site for Covid positive patients. This led to a significant backlog of patients waiting for an assessment appointment. Transferring level 1 patients to the Support Practices allows us to focus on treating the more complex paediatric patients who really need our specialist care and reduces the waiting time for appointments. We are incredibly grateful to all our partner Support Practices in Leicestershire, Derbyshire, and Nottinghamshire and we have really appreciated working with them to treat these paediatric patients.”
CDS carefully selects the referrals being sent to the Support Practices to ensure they need Level 1 care. The practices carry out a course of treatment, then discharge the children back to their GDP. The Support Practices help children to build up an acceptance and tolerance of treatment, making it easier to care for them in the future in general practice.
376* patients have been transferred over to the Support Practices, who treat children who are referred from CDS or 111, or Looked After Children who have been identified as needing a review of their oral health needs.
*Data up to the end of April 2024 n
To this end, the GDC ‘strongly encourages’ hygienists and therapists to select a course that follows the training curriculum developed by the British Association of Dental Therapists (BADT) and the British Society of Dental Hygiene & Therapy (BSDHT).
NHS England and Health Education and Improvement Wales (HEIW) are developing training courses. Further details on the timescale and how to access the training will follow shortly from each of the four nations.
Ross Scales, GDC Head of Upstream Regulation, said: “We welcome this legislative change, because it will bring improvements for dental patients across a number of settings. We thank colleagues at the professional associations and at NHS England for developing a curriculum outlining the knowledge and skills needed for dental hygienists and dental therapists to work to this mechanism. This curriculum also provides a basis for undergraduate training providers to build relevant training into their courses, so future generations of dental professionals can benefit too.”
Debbie Hemington, BADT President, said: “This is a change that will bring lasting benefits to not only the dental team, but the patients who they provide care to. It will make better use of the skills UK-based dental therapists hold, and will improve the efficiency of dental practices day-to-day.”
Miranda Steeples, BSDHT President, commented:
“We are pleased to be working with BADT to make sure we encourage dental hygienists and therapists to take up the right training course, so that those who want to make use of this mechanism can do so confidently and competently.” n
he British Society of Dental Hygiene and Therapy’s (BSDHT) ‘First Smiles’ 2024 initiative was a huge success, transforming children's perceptions of oral health through fun-filled, educational school visits and providing a positive basis for lifelong smiles.
During National Smile Month, the 'First Smiles' programme, supported by Oral-B for the ninth
consecutive year, empowered BSDHT volunteers to deliver engaging school visits.
Across the UK, dedicated dental hygienists and dental therapists conducted interactive sessions on brushing techniques, healthy eating and distributed toothbrushes, making learning about oral health both fun and impactful. Their collective efforts were
met with enthusiasm from children and appreciation from parents and teachers.
‘First Smiles' is crucial for the future health of the nation, spreading awareness about preventive care and promoting healthy habits from a young age, as well as exemplifying the BSDHT’s commitment to public health advocacy.
For further information, visit www.bsdht.org.uk n



Follow
The curse of the dental professional, particularly when it comes to preventative care, is that you can only do so much. In large part, you rely upon each patient to do as they’re told, adopt new habits, and ditch bad ones.
It’s not necessarily that the patients are ignoring you or feel that they know better. Habits can be difficult to adjust. I know, as I’m just as guilty. I brush twice a day for the full two minutes with an electric toothbrush. That’s easy – it’s a habit that’s been ingrained since my first tooth came through – since before I can remember. But when it comes to flossing or using an interdental brush, I struggle.
Rates: UK £39.95 per year; Overseas £83 - all cheques in sterling drawn on a UK bank made payable to ‘Smile’. 8 issues including 16 hrs CPD £39.95

Published by Purple Media Solutions
The Old School House, St Stephen’s Street Tonbridge, Kent TN9 2AD Tel: 01732 371 570
Managing Editor James Cooke james cooke @purplems.com Tel: 01732 371 581
Commercial Director Gary Henson gary.henson@purplems.com Tel: 07803 505208
Production and Designer 1 Lorna Reekie lorna reekie @purplems.com Tel: 01732 371 584
Production and Designer 2 Rob Tremain rob.tremain@purplems.com

I’m reminded each time I visit my local dental practice by both the dentist and dental hygienist, but soon slip back into my old ways. I know I need to work on this.

Divisional Administrator Francesca Smith francesca.smith@purplems.com Tel: 01732 371 570






With that confession out of the way, I found the feature on pages 12-14 of this issue particularly insightful. Dr Hafeez Ahmed details a survey he carried out amongst patients that explores how different types of language can have differing effects when it comes to trying to steer a patient s behaviour. While you flick through the mag to look into the findings, I’m off to find the floss at the back of the cupboard.

the information in this publication is correct and accurate, the publisher cannot accept liability for any consequential loss or damage, however caused, arising as a result of using information printed in this magazine. The views expressed in Smile OHM Magazine are not necessarily the views of the magazine, nor of Purple Media Solutions Editorial Advisory Board: Dr Barry Oulton, B.Ch.D. DPDS MNLP; Dr Graham Barnby, BDS, DGDP RCS; Dr Ewa Rozwadowska, BDS; Dr Yogi Savania BChD, MFGDP; Dr Ashok Sethi, BDS, DGDP (UK), MGDS RCS; Dr Paroo Mistry BDS MFDS MSc MOrth FDS (orth); Dr Tim Sunnucks, BDS DRDP; Dr Jason Burns, BDS, LDS, DGDP (UK), DFO, MSc; Prof Phillip Dowell, BDS, MScD, DGDP RCS, FICD; Dr Nigel Taylor MDSc, BDS, FDS RCS(Eng), M’Orth RCS(Eng), D’Orth RCS(Eng); Mark Wright BDS(Lon), DGDP RCS(UK), Dip Imp Dent.RCS (Eng) Adv. Cert, FICD; Dr Yasminder Virdee, BDS.


in association with:

Other titles include:
Circulation Manager Andy Kirk
Managing Director Ed Hunt ed.hunt@purplems.com Tel: 01732 371 577



Buy 2 get 1 free (while stocks last)
Directa’s ProphyCare, is one of the most well-known brands of prophylaxis paste worldwide, offering reliable results ranging from regular cleaning of the teeth to more complicated implant maintenance procedures.ProphyCare pastes are available in different grits from coarse to extra-fine and are colour coded for easy identification. All ProphyCare pastes have a mild minty taste and do not splatter, it stays in the polishing cup during the treatment.


Climate change and caring for our planet are rarely out of the news, so how can dentistry take more responsibility and become more sustainable?

According to the FDI, the healthcare sector is responsible for around 5% of global greenhouse gas emissions. The latest statistics show that the world generates around 53.85 billion tonnes of Greenhouse gas emissions.1
The least sustainable part of dentistry is our patients and staff travelling to the dental practice. We can help to reduce this by booking families for appointments at the same time and possible staff car share arrangements. However, without the patients and staff, there is no dental practice, so it is inherently difficult to offset these.
Some of the other less environmentally friendly factors of dental treatment are the single-use items and plastics that, again, are unavoidable.
What is being done to help?
The Sustainability in Dentistry Task Team provides guidance and scientific expertise to ensure effective execution of the Sustainability in Dentistry project. The project aims to map out strategies and implement solutions to help reduce the environmental impact of dentistry and the dental industry.
Its current goals are to:
• Increase awareness of the need to implement sustainable actions in the dental community
• To develop a guide for oral health professionals to identify actions that can lead to environmentally sustainable outcomes
• To conduct a review of the current literature and identify the current research and guidelines and to identify any gaps in the literature regarding sustainability in dentistry
This will only be successful if many dental professionals decide they care enough to put the work in to make this feasible by acting in their own dental practices.
There is so much that can be done including recycling, energy usage, and other sustainable changes to the working environment.
How can I get involved?
You can get involved in several ways, including taking part in their sustainability toolkit and registering your practice to help increase interest and provide support.
Focus on the prevention of oral diseases is the best way to help not only patients but also improve carbon emissions.
If, as a practice, patients need less work done on their mouths, they will have less need to travel to see you. In today’s world, most people must travel by car or bus unless they live very near the practice. Walking or biking would be a great alternative if possible. However, in this busy world, it is not always a practical solution depending on circumstances.
Cutting down on the need to travel will reduce emissions from this type of transport, leading to a healthier world.
The FDI Sustainability Award promotes sustainability in dental practice by providing the opportunity for individuals or dental practices to receive global recognition. Each year, four awards will be granted: two for dental practice and two for individuals.
Not only is it good for the environment but you can be globally recognised as trying your best for both dentistry and the planet. Although the deadline for entry this year has now closed, the winners will be announced during the FDI World Dental Congress, held in Istanbul in September 2024.
If you are interested in taking part in this next year, you can go to https://www.fdiworlddental. org/sustainability-dentistry to find out more information.
References 1. https://ourworldindata.org/greenhouse-gasemissions Accessed 19th July 2024 09.44 n
KAREN COATES


In an exclusive post-event discussion, Miranda Steeples and Sharon Broom sat down to reflect on the success and impact of the BSDHT’s ‘First Smiles’ initiative during National Smile Month

Miranda: Let’s get the excitement out there from the outset, Sharon – the BSDHT’s First Smiles initiative for 2024 was a huge success! It was clear to me that it brought fun-filled, educational school visits that transformed children’s perceptions of oral health. How do you think it went this year?
Sharon: I couldn’t agree more! During National Smile Month, with the wonderful support of Oral-B, our volunteers were equipped with everything they needed to make these visits engaging and educational. It was incredible to see how these visits created such a lively and dynamic learning environment for the children.
Miranda: Absolutely. It was a fantastic way to help them feel at ease with the idea that their friendly dental hygienist or dental therapist is their go-to person for great oral healthcare. ‘First Smiles’ is so important for us at the BSDHT and our members to promote oral health from a young age. It really helps us spread awareness about preventive care and encourage healthy habits.
Sharon: Exactly. Plus, the initiative boosts the profession’s role in public health advocacy and community engagement. With Oral-B’s support for the ninth year in a row, ‘First Smiles’ shows our strong partnership aimed at improving oral health.
Miranda: Totally agree. The activities included fun sessions on brushing techniques, educational games about healthy eating, and handing out toothbrushes. Informative talks and Q&A sessions addressed concerns from children, parents, carers, and teachers. These sessions were designed to be both fun and educational, making learning about oral health enjoyable.
Sharon: And the efforts across the UK were phenomenal. From Taunton to Fordingbridge, Stowmarket to York, our dedicated dental
professionals made a huge impact. Their collective efforts were met with enthusiasm from children and appreciation from parents and teachers.
Miranda: I saw the same. The response was overwhelmingly positive. Children were enthusiastic and engaged, often excited to learn new ways to take care of their teeth. Parents and teachers valued the practical advice and resources, reinforcing the importance of oral health in daily routines.
Sharon: We also tackled some common misconceptions, like the idea that baby teeth don’t need much care because they’re temporary, and that sugary snacks aren’t harmful if not followed by brushing. Addressing these misconceptions was key to helping both children and adults understand the importance of good oral hygiene early on.
Miranda: There’s no doubt that role of dental hygienists and dental therapists in public health initiatives is growing and ‘First Smiles’ ties in perfectly with that ethos. Our involvement in events like National Smile Month highlights our ability to lead community outreach, support public health policies, and collaborate with other professionals to improve overall health outcomes.
Sharon: Yes, creating an engaging and supportive environment through ‘First Smiles’ effectively taught and inspired better oral health practices. Our message to parents, carers and children is clear: oral health is a vital part of overall health. Starting good oral hygiene habits early can prevent many dental problems and lead to a healthier, happier life.
Miranda: And then, beyond First Smiles, the BSDHT is committed to various initiatives aimed at improving oral health education and access to care. So, we encourage our members to stay active in community outreach, keep up with the latest best
practices, and support policies that promote better oral health for everyone.
Sharon: With ‘First Smiles’ representing a movement towards better oral health for future generations, I think we are in a good place. With continued support and dedication, we can make a lasting difference in the lives of children and their families. After all, we’ve made great strides, thanks to everyone who participated, and we’re excited to keep building on this success.
For further information, visit bsdht.org.uk. n
THE AUTHORS


The most effective and body-friendly way of healing soft tissue and oral wounds.















Patient Case Study – Before

Patient presented with Stage 4 Grade B Generalised Periodontitis.
Treatment: RSD Q&Q. blue®m TOOTh protocol.










Patient Case Study – After

Recall at 12 months
Case study and photographs courtesy 0f Pat Popat BSc(Hons), PTLLS, RDH, RDT
With it's unique, oxygen enriched formula, blue®m ghts perio disease and reduces pocket depth.
Anna Middleton explores the successful integration and profitability of Guided Biofilm Therapy at London Hygienist, highlighting its impact on patient care and practice growth
In the practical and aspirational world of dental hygiene and therapy, finding effective and patient-friendly approaches is key to success in terms of ensuring better patient outcomes and fostering growth within practices.
Realising this, I established London Hygienist with a mission to transform the delivery of oral health care and improve access to dental services. The belief that everyone should love their smile underpins the practice, emphasising the profound impact a healthy mouth can have on one’s appearance, confidence, happiness and overall health.
Recognising that fear and pain are significant barriers to dental care, the focus has been on preventive measures, raising awareness within my patient base and further afield through social media and consumer print that dental decay and gum disease are entirely preventable and even reversible in their early stages.
Embracing Guided Biofilm Therapy
My commitment to patient-centred care led to the incorporation of Guided Biofilm Therapy (GBT) into the practice.
Traditional methods of professional teeth cleaning often resulted in discomfort, deterring patients from regular visits. Understanding the long-lasting impact of a negative dental experience meant that I sought a method that would address both the clinical and emotional needs of my patients.
GBT emerged as a game-changer, offering minimally invasive, highly effective care with an emphasis on patient comfort. It is a modern approach that uses a combination of warm water, air and soft powder to clean teeth gently.
I describe it as a ‘spa for your teeth’, and it is suitable for all patients, including children, adults with gum disease, and those with orthodontic appliances or dental restorations. This gentle yet effective treatment has become the driving unique selling point (USP) of my direct access business, ensuring every appointment is guided not only by clinical dental needs but also by emotional well-being.
A transformative experience
Patients have responded overwhelmingly positively to GBT, as evidenced by high retention rates and a steady stream of new referrals. The frequency of visits has increased, with many patients now attending every three months, appreciating both the comfort of the treatment and the importance of preventive and supportive prophylaxis. This focus on patient satisfaction has allowed London Hygienist to expand across three London sites, further cementing the practice’s reputation for excellence.
Clinically, GBT has proven to be gentle and precise, facilitating the effortless removal of biofilm and hard deposits. This precision reduces the risk of over-instrumentation and iatrogenic damage to both hard and soft tissues, preserving the integrity of the patient’s oral structures.
Enhancing the delivery of oral health care to meet patient expectations has always been central to London Hygienist’s business ethos. With the advancements in technology and innovative approaches in dentistry, it is an exciting time to be in the field.
This forward-thinking outlook has been crucial in building a strong reputation and fostering growth over the years. Positive patient experiences have undoubtedly contributed to the loyalty they continue to show to the practice.


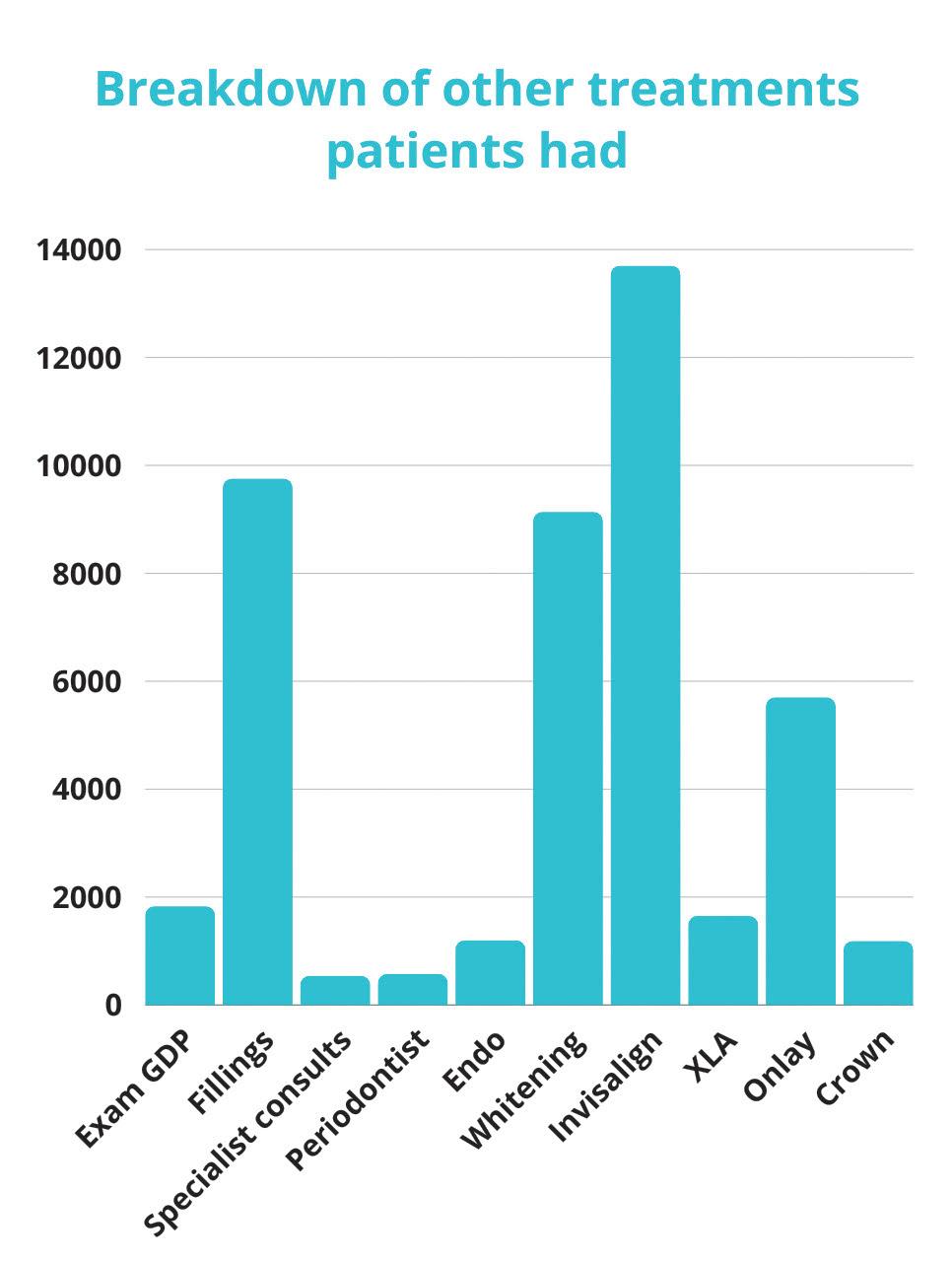
In fact, the integration of GBT into London Hygienist has significantly impacted profitability. To offer one example, since May 2021, at one clinic alone, 71 days of work across two days a month have resulted in 210 unique direct access patient leads.
These are the figures from that period for that one clinic:
• Total first-time spend of these patients: £32,278
• Return spends from the same group of patients: £23,949
• Total hygiene-related revenue: £56,227
• Additional revenue from other treatments by these patients: £52,610 (see Figure 1 for breakdown)
• Overall total revenue from hygiene leads: £108,837
All patients across the three London Hygienist sites receive GBT as the standard of care, ensuring consistent, high-quality treatment. This uniform approach eliminates confusion that can arise from offering multiple treatment options with different price points. The consistency of GBT, along with increased patient retention and frequent visits, highlights its success and efficiency within the practice.
This means that the future of GBT within the practice and the broader field of dental hygiene in the UK is promising, and there is hope for improved patient access to GBT, enhancing overall health in a gentle, timely and progressive manner.
The potential for dental hygienists and dental therapists to work even more to their full scope of practice and continue to open direct access clinics is an exciting prospect, signalling a new era of patient-focused care. Indeed, for London Hygienist, developing with GBT as its USP has proven to be a tremendous success, benefiting not only the business but also the other clinicians and clinics involved.
The journey with GBT has shown that innovation and patient-centred care can go hand in hand, driving both profitability and excellence in dental hygiene.
For further information, please visit ems-dental.com n
ABOUT THE AUTHOR

Anna is a multi-award-winning dental hygienist and the founder of London Hygienist, which has a mission to change the way oral health care is delivered to patients. Anna is an official provider and Swiss Dental Academy trainer of EMS’s Guided Biofilm Therapy and a member of the British Society of Dental Hygiene and Therapy. Anna lectures and writes regularly for both industry and consumer press.
















































Not only does the patient interview need to be empathetic but the discussion content needs to be topic specific.1
In recent years, clinicians have been encouraged by the General Dental Council to move towards patient-centred care. 2 In addition to this, it has been described that simply ‘being nice’ and maintaining a good relationship with the patient are not sufficient for patient-centred care. Patient-centred care requires detailed topicbased discussions. 3 However, there appear to be no studies reporting on topic-specific words and their influence on patient understanding.
Beyond that, it is accepted that ‘effective communication’ is essential to behaviour change, as comprehensively discussed in a series of articles by Ruth Freeman in 1999.4 The importance of effective communication and behaviour change is further underlined by the fact that the majority of dental care requires patients to adhere to advice, otherwise the care is undermined. 5
It is intriguing that, despite the dental profession believing they are actively engaging in effective patient communication, the prevalence of periodontal diseases remains largely unchanged. Chronic periodontitis occurs in 45% of the UK population6 and in 11.2% of the global population.7
Experience suggests that, when patients find it difficult to make the necessary behavioural changes, it is generally for a variety of reasons, including: they do not fully understand periodontal diseases; they do not appreciate the long-term implications and legacy of the disease; they do not entirely recognise the pivotal role of homecare; or they are individuals who understand all the advice but do not want to change.
A possible solution
In my practice, I created a table with a list of 20 topic-specific words and phrases (table 1). The words and phrases were selected from those I heard being used most commonly by patients and dental professionals. On the right-hand side of the list, I placed a Likert-type scale, numbered from one to five. My plan was to ask potential participants to rate the words/phrases by circling one number on the scale for each of them, to indicate the degree of perceived encouragement or motivation each word/phrase offered them.
Starting in June 2022, every new patient referred was invited to take part with the aim of compiling 100 lists. By virtue of the referral, all patients had received at least one course of periodontal therapy from the referring dentist. Potential participants were recruited by discussing the purpose of the study with them in the waiting room, following the completion of their initial consultation. The following statements were made as an invitation to take part:
“I am conducting a small study in an attempt to identify if some of the words we use when we discuss gum disease with our patients affect their enthusiasm more than others. Essentially, I want to see if some words create more of a feeling of seriousness and if some words create a greater feeling of enthusiasm or motivation to act on the advice.”
‘Motivation’ was defined as: “It makes you feel like taking the matter seriously,” and “It makes you want to do your part in resolving the matter.” Potential participants were also advised: “What I really want to see is if any of the words or phrases make you feel more like sitting down for eight to 10 minutes
each evening to use floss, inter-dental brushes or wood sticks to clean in-between your teeth and the margins of your gums.”
During the discussion, and before the patients agreed to participate, they were given the list so they could see what was being described. They were also given the guidance for the Likert-type scale (table 2). To maintain anonymity, patients were
advised that they were not required to put their name on the list – only their age and gender.
Those patients who agreed to take part were then shown to a seat and asked to read the list and rating scale carefully, and to confirm their understanding. Reassuringly, a few of them smiled and said: “It’s pretty straightforward.” Others laughed and said: “It’s not rocket science.”
100 lists were rated between June 2022 and January 2023; a record was kept of the participants, although at no point were their names written on the list. 15 patients declined the invitation to take part in the study. Of the reasons given, the two main ones were: “It’s not something that I’m
in,” and, “I don’t have time.”
On the 100 lists that were completed, responses were received for all 20 words/phrases.
demographic was split, 61 females and 39 males. The average age was 57 years; the youngest patient was 18 and the oldest was 77.
A mean score for each word/phrase was calculated. The maximum score was five – the word/phrase was most likely to encourage/motivate the patient; the lowest score was one – the word/phrase was least likely to encourage/motivate the patient. Although it was not the original intention, the Mean Score became known as the ‘Encouragement Value’.
Discussion
The findings suggest that, in the opinion of susceptible patients with experience of periodontal diseases, certain words when used to describe the disease can, somehow, generate different feelings, with some being more motivational than others. This indicates that patients form different meanings from different words. It also suggests that words can change the way a patient thinks. These points align well with research carried out by Andrew Newberg and Mark Waldman, in their book Words Can Change Your Brain.8 The authors also propose that the mechanism behind how we process a communication is directly related to the number of words that are used. They claim that 30 seconds of language is all the brain can understand and, accordingly, they encourage fewer words for greater impact.
The findings also revealed a trend: the more severe sounding words scored higher Mean Values. This finding aligns with the consensus that the more immediate and severe the threat, the greater the chance of positive behaviour changes. 9 DeMatteo and DiNicola also found that patients with mildly threatening problems tend not to comply with their therapists’ advice. Worryingly, this suggests that some of our patients, irrespective of how we communicate with them, will fail to comply until a stage when tooth loss is inevitable.
In a more recent study, which investigated the collaboration between medicine and dentistry in relation to diabetes management, 10 patients reported inconsistency in the information and advice they were given by different healthcare providers. It was suggested that consistency would be beneficial to communication. Diabetes and periodontitis are inextricably linked as chronic inflammatory diseases that adversely influence one another. The creation and
use of universal statements as scripts, using the topic-specific words reported by patients as more encouraging, makes sense. The scripts would increase consistency in information sharing and, thus, increase the potential for a positive impact on a patient’s periodontal health.
The short- and long-term aim of periodontal therapy is to keep the inflammatory response below the threshold of bone loss or further bone loss. This is entirely dependent upon us, as clinicians, persuading our patients to take our advice and follow it.
Compliance is defined as: “The extent to which a person’s behaviour coincides with medical




and dental advice.”11 Compliance requires that a patient is more than just a passive receiver of information. The estimates of compliance range from 20% to over 80%.12 Generally, the rates of compliance for long-term therapy tend to converge at 50%, regardless of setting or illness.13 Although we know that patients do not follow oral hygiene recommendations consistently, we do not know specifically why they do not. One reason it is not understood could be that compliance research has been dominated by the perspective of the healthcare professional. These findings offer an insight into these patients’ perspectives.





























































The degree to which a patient complies with oral hygiene instruction is of more importance than the choice of any particular treatment method.14 The literature shows that compliance in general decreases as treatment time or the complexity of the required behavioural change increases.14 It is often the case that by the time some susceptible patients appreciate what their type of periodontal disease is and what self-care is necessary to treat, stabilise and maintain it, insufficient bone remains to retain some of their teeth. Therefore, if we are to succeed with a preventative approach, we need to empower patients and achieve compliance at early stages of bone loss.
Around 2006, I had carefully devised the following statements to explain gum disease to my patients in a way I thought would be most effective:
1. Gum disease is an infection that irreversibly destroys the bone that holds your teeth in place.
2. When a significant amount of bone has been destroyed, your teeth will feel loose or wobbly.
3. When insufficient bone remains to support your teeth, they will start to drift or fall out.
A few of the words and phrases I put in the list in this study closely resemble some of the ones in these statements. In fact, it is my use of the above statements with my patients that inspired me to conduct this study. To avoid bias, I deliberately avoided using the above statements in the initial consultations during the period of this study.
The above statements might not be to everyone’s liking but they are simple, short, topic-specific, and to the point. They accurately reflect the seriousness of the condition. I devised them to increase the likelihood of patients fully understanding what is being said, as, amongst other things, understanding helps allay anxiety.15 I appreciate that the statements have a negative tone. However, once patients appreciate the seriousness of their condition, positive tones can be introduced by discussing the benefits of resolving the condition. Since using these statements, I have found my patients clearly understand the seriousness of their condition and, almost always, express their gratitude for the unambiguous nature of my communication. The message contains bad news, but I deliver it gently with a measured, polite firmness aimed at ensuring patients understand the potential seriousness of periodontal infection.16, 17, 18
Conclusion
In respect to the patient discussion, these findings suggest that the information which is conveyed by a single word or phrase, does have the potential to affect the communication. Each word has a meaning but, more importantly, each word creates a mood.
Context
I am a clinician operating a private referral practice restricted to periodontal care, some minor oral surgery and implant dentistry. On a day-to-day basis, most treatments involve helping patients resolve their periodontal problems. I am not a research and have no experience of statistical analysis. This opinion paper was prompted by the fact that a poor understanding of ‘gum disease’ was relatively common amongst patients, even though they had regularly seen a dentist and/or a dental hygienist. Some of them had received multiple courses of periodontal therapy but still could not demonstrate a good understanding of gum disease. It is hoped that this article stimulates wide-spread debate as to how we communicate with our patients. It is also hoped that researchers will be inspired to utilise their resources to produce a more robust and in-depth study so that we can all learn from best practice.
This article was first published in Dental Health 2024;63(2):34-37 – doi.org/10.59489/bsdht141
Table 3: The results present the actual number of patients who circled each score. The mean is represented on the right-hand side and the words/phrases have been listed in descending order of Encouragement Value. For example, the Mean Score for ‘Will result in tooth loss’ was calculated as follows: 13x4 + 87x5 divided by 100 (52+435 divided by 100 = 4.87)
References
1. Suchman AL, Markakis K, Beckman HB, Frankel R. A model of empathetic communication in the medical interview. JAMA. 1997: 277(8):678-682.
2. General Dental Council. Standards for the dental team. 2013.
3. Asimakopoulou K. A good relationship and good communication are not sufficient for patientcentred care; Brit Dent J. 2015; 219(3):105-106. Published online: 14 August 2015 | doi:10.1038/ sj.bdj.2015.589.
4. Freeman R. The psychology of dental patient care: The common-sense approach, Brit Dent J. 1999; 186(9):450-452.
5. Brown JC. Patient non-compliance - a neglected topic in dentistry. JAmDent Assoc. 1981; 103(4):567-569.
6. Adult dental health survey 2009- summary report and thematic series 2011.
7. Kassebaum N J, Bernabe E, Dahiya M, Bhandari B, Murray C J L, Marcenes W. Global burden of severe periodontitis in 1990–2010: A systematic review and metaregression. J Dent Res. 2014; 93(11):1045–1053.
8. Newberg, A., Waldman, M. R Words can change your brain. Hudson Street Press (2012).
9. DeMatteo, M.R., DiNicola, D.d. Achieving patient compliance. New York: Pergamon Press Inc.(1982).
10. Bissett SM, Stone KM, Rapley T, PreshawPM. An exploratory qualitative interview study about collaboration between medicine and dentistry in relation to diabetes management. BMJ Open 2013; 3(2):e002192 doi:10.1136/ bmjopen-2012-002192.
11. Haynes RB. Introduction. In: Compliance in health care. Baltimore: John Hopkins Univ. Pr. (1979).
12. Buckalew LW, Sallis RE. Patient compliance and medication perception. J Clin Psychol. 1986: 42(1):49-53.
13. Morris LS, Schulz RM. Patient compliance- an overview. JClinPharmTher. 1992:17(5):283-295.
14. Ramjford SP, Morrison EC, Burgett FG, Nissle RR, Shick RA, Zann GJ et al. Oral hygiene and maintenance of periodontal support. JPeriodontol. 1982; 53(1):26-30.
15. Freeman R. Communication, body language and dental anxiety. Dental Update 1992; 19(7):307-309.
16. Ptacek JT, Eberhardt TL. Breaking bad news. A review of the literature. JAMA 1996;276(6):296-502.
17. Davis, K. Power words in periodontal communication. Reg Dent Hyg.2011;31(9):74.
18. Davis K. The Art & Science of Effective Communication for Non-surgical Periodontal Treatment. Contin Educ.2007: 58-68. n


These are exciting times for dental hygienists and dental therapists. The Chief Dental Officer (CDO) for Ireland, Dr Dympna Kavanagh, recently said of the profession: “We are the right people in the right place at the right time.” This positive affirmation from the CDO should be music to our ears, as support from this quarter will help ensure that oral health starts to be recognised as a key element of a wider general health strategy, which, if actioned, should improve overall health outcomes for all.

There are five noncommunicable diseases (NCDs): cardiovascular disease, cancer, chronic respiratory disease, mental health disorders and diabetes . According to the World Health Organisation (WHO), NCDs kill 41 million people each year, equivalent to 74% of all deaths globally , and are a result of a combination of genetic, physiological, environmental and behavioural factors. The WHO Global Health Status 2022 highlighted the world’s oral health crisis and calls for it to be added as the 6th non-communicable disease.
NCDs encompass a broad range of conditions that lead to high treatment costs, imposing a direct economic burden on health services and society as a whole. This is problematic for two reasons: firstly, governments do not have sufficient funds to increase public health spending, and secondly, but importantly, there are not enough healthcare professionals to meet the needs of the general population.
WHO has clearly outlined the economic argument for governments to invest in preventing and controlling NCDs and promoting, protecting, and caring for mental health. We dental professionals are well placed to speak to our patients about oral health prevention and non-communicable diseases.
What matters here is much closer to home; we need to recognise and then utilise the skills dental hygienists and therapists offer to make a real difference in improving the overall health of our local communities.
When considering NCDs, there is evidence for prevention using the six pillars of lifestyle medicine - plant-based nutrition, physical activity, avoidance of risky substances, stress management, restorative sleep and social connections.
Lifestyle medicine (LM) primarily promotes lifestyle change as a method of treating chronic disease, which can also have a significant positive impact on mental health. Research shows that simple interventions in the six pillars of LM might prevent, delay and improve neurocognitive impairment. This includes preventing and managing risk factors such as diabetes mellitus type 2, hypertension, sleep disorders, illicit drugs and psychiatric factors .
The mouth’s health is linked to various other conditions, including increasing evidence of the link between periodontal and systemic disease. Dental pain has a huge impact on people’s lives, both physically and mentally.
Nearly half of all adults in the UK have some form of periodontal disease and present at dental practices every day. By increasing public awareness of the connection between oral and systemic health and providing treatments using proven preventive products and equipment, hygienists and therapists are well-placed to treat patients in all stages of preventive care.
The challenges
The perception of dental hygienists and therapists as simply there to provide a scale and polish is outdated. The new model for practices of the future relies heavily on the skills of this group of dental care professionals, who are highly qualified in their own right, able to diagnose, perform oral cancer screening, promote health, and, of course, prevent disease.
There is no doubt in my mind that dental hygienists and therapists are valuable (and often underrated) dental team members, ideally placed to help individuals and families implement and maintain healthier lifestyles as they see many patients at regular intervals. However, this additional support takes time and cannot be done effectively under the current model of 30-minute appointments.
The learners on the Postgraduate Diploma in Oral and Positive Health ( level 7) have already changed their practice and look at treatments and their patients differently.
Whether working independently, under a Direct Access arrangement, or under the prescription of a dentist, hygienists and therapists remain at the forefront of dental care for patients and are fundamental to the future success of dental practices.
The NSK Ikigai Oral Health Community is a dedicated dental hygienist and therapist support network. It is an active community and professional hub that underscores the crucial role dental professionals play in oral health and the wider healthcare arena.
With the services of dental hygienists and therapists in high demand and patients
having increasingly complex needs, there is an understanding that as clinicians, hygienists and therapists can be overwhelmed by responsibility and often feel isolated in the practice environment. A support network of like-minded professionals is one pivotal way to change that. NSK Ikigai provides this platform and allows fellow professionals to reach out and gain new clinical skills, follow thought leaders and develop new professional relationships.
The NSK Ikigai Oral Health Community is focused on connecting people through a whole programme of Ikigai live events and webinars and our thriving online Facebook and Instagram groups.
Members can interact and join in with hands-on workshops with Ikigai clinical educators from all areas of dentistry at upcoming events, including:
• IDHA Conference (11th – 12th Oct 2024 )
• BSDHT Oral Health Conference 2024 (22nd –23rd November 2024) - the biggest event of the year for dental hygienists and therapists with two days of clinical education and CPD, featuring presentations from leading speakers and updates from the profession.
The 2024 programme of Ikigai Oral Health Community webinars covers a range of health, wellbeing, and clinical subjects from leading educators. It also includes Ikigai Enhance, a new series of face-to-face clinical skills training courses for hygienists and therapists to fully embrace their vocation.
The NSK Ikigai community connects people, empowers them with learning, and gives them the confidence to tackle professional challenges and understand better ways to manage health and wellness to enhance career satisfaction. Come and join us!
If you want to discuss an idea you are passionate about, let us know.
To find out more about the NSK Ikigai Oral Hygiene Community and to get details of the Autumn ‘24 oral health webinars and face-toface hands-on events visit https://mynsk.co.uk/ ikigai/. For all the latest news and chat join us on Facebook at facebook.com/groups/NSKIKIGAI or on Instagram @ikigaioralhygiene n
SIOBHAN KELLEHER

Siobhan is a multi-award-winning dental hygienist who combines her master’s degree in personal and management coaching with a postgraduate diploma in positive health to provide postgraduate education to the profession. The Postgraduate Diploma in Oral and Positive Health (Level 7) is the first of its kind globally. Siobhan is the clinical and project lead of the NSK Ikigai Community.
Award-winning TRIOS technology distilled down to its most essential and affordable form. That’s TRIOS Core. Accurate, fast and easy, for a great send-to-lab experience.
“Dentists wouldn’t dream of working without a nurse, so why do they think it’s ok for a hygienist or therapist to work without one”
Dental therapists and dental hygienists deserve greater acknowledgement and respect for their skills, according to Sarah Murray, and should be given a wider patient treatment remit
Sarah Murray, a registered dental therapist, and qualified dental hygienist with a Master’s degree in Reflective Practice, says despite recent moves to allow therapists and hygienists to supply and administer certain medicines without a prescription or the patient needing to see a dentist under new Direct Access proposals, they still operate in the shadow of dentists.
As a practitioner at the forefront of the Direct Access campaign, Sarah is determined to “Keep pushing forwards. I’m trying to push our profession forwards in the right way and make us more recognised because we’ve got a huge number of skills and attributes, but dentists still see themselves as the leaders of the dental team, despite the skill set that we offer.”
She also points out that it’s not only from a treatment perspective that dental therapists and dental hygienists are sometimes treated with little respect by dentists. “We’ve got a very active hygienist and therapist network on Facebook and when you hear about how some of my dental colleagues are treated by dentists, it’s absolute madness,” she says, adding: “BSDHT collected data during Covid on whether dental hygienists and therapists worked with a dental nurse or not, and what would the advantages and disadvantages be? Some of the stories we have heard were absolutely horrendous…things like not drinking enough water throughout the day because they don’t have time to go to the toilet. Absolutely basic things because of not having a dental nurse. Or being subjected to verbal or physical abuse from patients. Dentists wouldn’t dream of working without a nurse, so why do they think it’s okay for a hygienist or therapist to work without one?”
Sarah is now working with colleagues on publishing their findings for a paper later this year. She’s also working on a project to explore how many student dental hygienists and/or therapists there are in the UK, as this data is not on file. “The government has said it’s going to increase student numbers, whether that’s therapists, hygienists or dentists, but there hasn’t been a huge amount of consideration for increasing numbers of dental nurses once these dental professionals have graduated from dental school. We’re trying, as a profession, to push to be working with a dental nurse, and yet this aspect hasn’t been considered.”
Evolving appointment charging
Alongside the challenges that dental therapists and dental hygienists face from within the profession, they also face the challenge of ensuring consistently high patient communication and treatment standards against a backdrop of personnel shortages.
Says Sarah: “We know a lot of our patients aren’t managing to be seen every three months because there’s so much demand. At dental school, the students see a patient in the morning and one in the afternoon – and we’re seeing patients for two hours. I’m not sure how you suddenly switch from a two-hour appointment, where you’re doing everything correctly, to 30 or 45-minute appointments when starting to work as

a graduate in practice. I think is a real challenge. There needs to be greater consideration for mandatory Dental Foundation Training for dental therapists in particular.”
Sarah stresses that students are taught best practice, “But then, in practice, some of those things just aren’t applied because you simply don’t have time to do it,” she says, adding that many patients also don’t understand the value of taking time to have those conversations. “They have an expectation that we’re going to be doing something in their mouth, but they don’t understand having to pay for us spending half an hour talking to them about their lifestyle, oral hygiene and their behaviours when working in general practice.” She says the answer could be to change the way dental services are charged for, moving towards a package of care price, rather than a price based on timed appointment slots. “When you charge an amount for 30 minutes the patient expectation is that they will be in the chair for 30 minutes. We don’t have that expectation when we go to the hairdressers.”
And as a Philips KOL Sarah is keen for dental therapists and dental hygienists to have time to speak to patients about how they can improve their oral hygiene, including the value of using powered toothbrushes such as Philips’ Sonicare.
“I believe there’s a place for manual toothbrushes, but I do think powered brushes are superior and having a timer can help some patients to extend their brushing time. I tell students that dental health surveys state that patients only brush their teeth for about 47 or 48 seconds, So, just by extending that brushing time – doubling it – could assist our patients to improve their oral health, so the timer on a powered brush is really important.”
She also points out that Philips brushes require
less dexterity from patients than rival brands because of their sonic technology. She says: “It’s important that students understand the difference between Philips Sonicare and other brush brands and the different brush heads, so we can recommend the right products to the right patients…that’s really important too. And that supports ethical selling.”
Looking to the immediate future, Sarah has just completed work with the University of Suffolk in developing its new BSc in Dental Hygiene and Dental Therapy and she is exploring ways to improve the future for academic dental hygienists and dental therapists. “The career pathways for academics who are dentists is really well thought out and planned. Conversely, the academic career path for dental therapists and hygienists is currently inadequate, so I plan to explore how we can develop a pathway and encourage colleagues to be part of the future of dental education.” n




By updating the Ecosite Elements shade palette, we have made our established range even better. The clever shade combination is made up of three modules, which now include the two Pure shades A1 and BL1, providing a simple, aesthetic solution.
Fundamental composites - perfect results, amazing simplicity


With an innovative NC1 material structure



Exceptional handling for maximum safety and precision thanks to the push-and-flow effect
Advanced, intuitive and quick shade slection


Available Pure shades: BL1, B1, A1, A2, A3, A3.5
Available Pure shades: BL1, B1, A1, A2, A3, A3.5
For more information visit uk.dmg-dental.com




Coates






Caring for patients with additional needs requires understanding and adaptability
Students in England will soon be able to take British Sign Language as a GCSE.i It will be taught in schools from September 2025 and will be open to all pupils. As we move towards an ever more inclusive society, dental professionals must ensure that patients with additional needs have access to the same level of oral health services and expertise as others. Understanding their unique challenges, adapting techniques, and creating a welcoming environment can help create a positive dental experience for these patients.
Dental patients with additional needs can encompass a wide range of disabling conditions including intellectual disability, dementia, physical limitations, movement disorders, behavioural disorders, and chronic medical conditions. Many of these individuals can be treated in routine dental settings with minimal special accommodations or with interventions that are well within the scope of most dental professionals.ii
Some patients with additional needs do, however, require interventions that go beyond the scope of routine behaviour management techniques. These techniques can include desensitisation, anti-anxiety medications, therapeutic immobilisation, sedation and general anaesthesia.ii
Unmet needs
Under the Equality Act 2010, public sector organisations have to make changes in their approach or provisions to ensure that services are accessible to disabled people as well as everybody else. People with learning disabilities might have difficulty with reading or writing, explaining symptoms and understanding new information. They have higher levels of gum disease, greater gingival inflammation, higher numbers of missing teeth, increased rates of edentulism, higher plaque levels, greater unmet oral health needs, poorer access to dental services and less preventative dentistry. They are often unaware of dental problems and may be reliant on their carers.iii
Similarly, under the Accessible Information Standardiv dental surgeries that provide NHS services must ensure that people who are deaf are provided with information in a format that makes sense to them. This also applies to hearing parents that have deaf children or deaf parents with hearing children. Indeed, effective communication is crucial.v It’s important to take the time to establish a rapport and build trust with patients with additional needs and their carers. The dental team should use simple and clear language, visual aids, and alternative communication methods if necessary. They should be encouraged to express their concerns or queries, ensuring their participation in the decision-making process.vi
Sensory considerations
Many patients with additional needs may have heightened sensory sensitivities,vii making dental visits overwhelming. It is important therefore to be

mindful of the clinic environment by minimising noise levels, using natural lighting, and providing comfortable seating. Practices should consider allowing extra time for patient appointments to help alleviate any stress or anxiety.
Visual supports can help to aid understanding and reduce anxiety. Using stories or creating illustrated step-by-step guides to explain dental procedures and routines may help some patients. These tools can provide reassurance and a sense of familiarity, making the experience more predictable and less intimidating for patients with additional needs.iii
Dental professionals can implement techniques to make the dental experience more sensoryfriendly. For example, using desensitisation techniques, gradually introducing patients to the dental environment, and involving them in play therapy to familiarise them with dental tools and equipment.iii
Collaboration with carers
Collaboration with carers is vital to providing comprehensive care.viii Dental professionals should encourage open communication and provide carers with educational resources, such as instructional videos or printed materials, to help them maintain optimal oral hygiene practices at home.
Positive reinforcementix can also significantly impact a patient’s experience. Dental teams can offer praise and rewards for cooperation and positive behaviour during dental visits. This reinforcement can help to build a trusting relationship and reduce anxiety in subsequent visits.
Oral hygiene can present a challenge for many patients with additional needs, including those with sensory or motor dysfunction.


Recommending the right oral hygiene products for our patients is essential for their oral health. The FLEXI range of interdental brushes from TANDEX can help some patients with additional needs as they are easier to grip and less tricky to use than string floss. Each product’s handle is flexible, and the brush can be bent into the perfect shape to clean in between the teeth. Available in 11 different sizes, the line presents a solution for each individual patient, for a comfortable and effective clean. Given that patients with additional needs are more prone to tooth decay,iii the brushes can be used to apply PREVENT GEL too, a product which contains 0.12% chlorhexidine and 900ppm fluoride which offers antibacterial and enamel strengthening properties. Caring for patients with additional needs in the dental setting requires understanding, empathy, and adaptability. By implementing effective communication strategies, creating a sensoryfriendly environment, collaborating with carers, and tailoring treatment plans, dental professionals can provide optimal dental care to this vulnerable population. With this knowledge and approach, patients with additional needs will receive the treatment they deserve, contributing to their overall well-being and quality of life.
For more information on Tandex’s range of products, visit https://tandex.dk/
Our products are also available from CTS Dental Supplies https://www.cts-dental.com/ n
References available upon request.
ABOUT THE AUTHOR

Anna Middleton, Dental Therapist and Founder of London Hygienist
• A dentolegal advice line, with out-of-hours advice available for emergencies 24/7, 365 days of the year
• A huge range of CPD, including live webinars, online modules, and more
• Help responding to and resolving patient complaints
• Access to our confidential counselling service to support you through stressful situations.








Artificial Intelligence (AI) is increasingly being used across various industries, including dentistry. In order to implement it safely and without unintentional consequences, it is necessary for dentists to understand the technology they have in practice, developing an awareness of the potential risks and how to mitigate against them.
Narrow and Generative Artificial Intelligence Machine Learning (ML) and AI have long been used for data analysis, diagnosis, prediction and recommendation across industries, including healthcare. This well-established branch of AI starts with a clear scope or target application, develops models with well-defined datasets, and results in models which excel at the specific tasks for which they are designed. This is “Narrow AI” – niche, expert systems with clear and measurable deliverables to assess performance and steer continuous model development and improvement.
Since the public release of ChatGPT, “Generative AI” using Large Language Models (LLMs) have been rapidly and enthusiastically deployed across nearly every area of our lives. An LLM can be conceptualised as a compressed digital representation of meaning and context between words, predicting which word would best follow a current dialogue. LLMs are non-deterministic – results will differ when provided the same input and it is not possible to deduce how an LLM gets to the results it generates. Benchmarks and defined datasets are used to measure the capabilities of LLMs and rank competing models as they race to evolve. Their generic nature, wide applicability and variability of output makes it challenging to evaluate and quantify the performance of generative LLMs for specific applications.
AI in dentistry
In dentistry, AI-assisted technologies are already demonstrating early potential to support clinicians, streamline professional workflows and improve patient care and communication.
Narrow AI is being used to analyse radiographs supporting diagnosis and treatment presentation. Web chatbots provide automated and personalised initial contact, signposting and qualifying new patient inquiries. LLMs can be used to generate letters and written reports. Different AI models, technologies and implementations are required for the wide range of tasks, applications and automations within the operation of the dental practice.
In the clinical setting, it is crucial to make sure that AI technologies are created, deployed and adopted safely without compromising clinical standards or introducing risk and unintended consequences.
Risk, a measure of impact and likelihood of an undesirable outcome, exists in every technology, process, system and action. Sources of risk introduced by AI particularly relevant to dentistry include accuracy, reliability, repeatability, accountability, privacy and medico-legal considerations. The acceptable tolerance of risk factors will vary based on the specific use case.
For example, a chatbot designed to automatically qualify, categorise and signpost patient enquiries using an LLM – finetuned with information you provide – should process little personally sensitive data and present a low clinical impact if incorrect or inaccurate information is presented. In contrast, if asked to advise patients on treatment decisions or medical factors, it must prove that it will reliably present correct and accurate information, or always advise the patient to speak to a dentist.
AI technologies used to support clinicians with assessment or treatment planning need

to demonstrate high and quantifiable levels of accuracy, reliability and repeatability to ensure clinical safety of the patient. This requires a highly focussed, narrow AI specialising in the discipline and task. The experience of the clinician will affect the ability to interpret and confidence to challenge presented information – an AI system may not have the capability to consider the nuances of a particularly complex or unique case.
One of the hopes for Generative AI is the potential to free dentists from the administrative burdens of clinical record keeping, reports and letters. LLMs impressively create, summarise and reword text, mimicking comprehension and expertise. LLMs are not clinical or precise. They are prone to hallucination, confidently and coherently introducing incorrect or inaccurate information, introducing risk for patients and clinicians. The dentist is fully responsible and accountable, and a thorough and immediate critical review for accuracy and correctness is essential. The written record must be a true and accurate representation of what really happens in an appointment, not a report of what should have happened in an ideal world. If used in a medicolegal claim, you as a clinician will need to prove beyond all doubt that the record is indeed fully valid and reliable to provide any protection.
Making the vision real
Delivering the visions presented by AI evangelists is possible, and we must do so in a sensible and level-headed way, taking a conscientious approach to risk management in order to ensure the safety and interests of patients. AI systems will need to be backed up by solid, reliable data to prove accuracy and integrity.
For dentists looking for an effortless, highly accurate, complete and contemporaneous way to ensure this data exists, Dental Audio Notes (DAN) offers a solution. It provides robust evidence of the communication between patient and practitioner during the appointment via clinical audio recording and transcription for both the patients’ and dentists’ protection. Even more, DAN manages the consent, security, accessibility, privacy and storage of the data for the full lifetime of the record, so dentists can be confident that when they need it, they have the most reliable data and one less thing to worry about.
For more information about Dental Audio Notes (DAN), or to arrange a free demo, please visit dentalaudionotes.com n
ALEKSANDRA ROZWADOWSKA

Aleksandra (Ala) is a dentist and the co-founder of Dental Audio Notes alongside her husband, Adam. Dental Audio Notes was created in response to the challenges of trying to master every aspect of clinical dentistry. Together, they love helping dentists to master their clinical records, and to finally get credit for the good work they do with their patients, instead of relying just on what they had time to write down.

















•
• Carry out
•












• Continue to monitor and support

































Careful handling of the waste products from your dental practice is essential to ensure the safety of clinicians, patients, and the wider environment. Numerous guidelines are in place to ensure waste items are appropriately managed – with dedicated pathways for those that can be recycled, treated, incinerated, or sent to landfill.
Given the broad range of waste generated in the dental practice, effective segregation is important for the safe and efficient treatment of this waste. This requires consistency among staff, as it only works when everyone contributes.
However, it can be difficult to remember which waste items should be separated for which treatment method, which is where the colour code comes in. This provides a simple way to identify waste items according to the level of risk they present, as well as the appropriate disposal methods for those items. Dental professionals should take the time to refresh their knowledge of the colour code waste system to optimise clinical waste management within the practice.
Current guidelines
One of the most important sources of information regarding the colour code waste system is the Health Technical Memorandum 07-01 (HTM 07-01),1 which offers comprehensive advice for the safe and sustainable management of healthcare waste. The guidance is not mandatory but provides best practice recommendations for practices striving to ensure the highest standards for their patients, staff and business.
HTM 07-01 allocates 13 different colours to each component of healthcare and infectious waste. It provides a clear and concise way for professionals to implement safe and effective waste segregation onsite. A decision-tree is available within the document that clearly defines which waste items go where.
Colour breakdown
Three of the most commonly used waste streams in dentistry are for infectious, highly infectious and offensive waste, represented by orange, yellow and tiger colouring (yellow with a black stripe), respectively. To judge which colour waste stream is most appropriate in any given moment, you must establish whether an item is infectious, and if so, the risks it poses.
If a waste item has been in contact with a patient who is either being treated for infection; is carrying a transmissible disease; has a known history of infection, such as a bloodborne virus; or if the item is/ has been in contact with a culture, stock, or sample of infectious agents from laboratory work, allocate it into the appropriate orange or yellow waste stream.1 Where the waste is infectious and contaminated with Category A Pathogens, medicines or chemicals, it is allocated yellow – otherwise, place it into the orange stream. Separating these accurately is essential, as highly infectious waste (yellow stream) will most often be sent for incineration, whereas known infectious items (orange stream) may be suitable for alternative (and less energy-intensive) treatment.

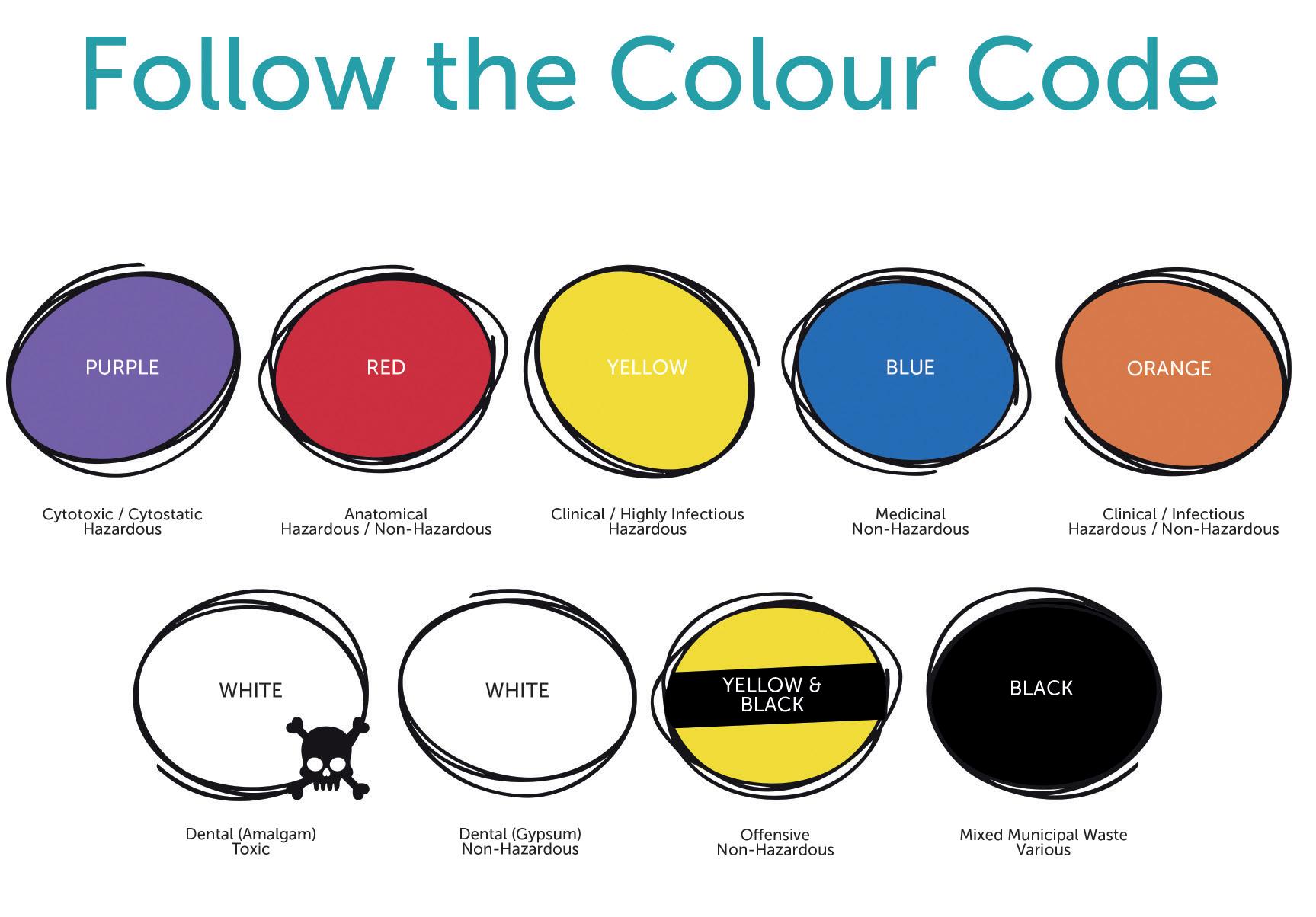
Be aware, not all clinical waste is infectious. When an item doesn’t meet this criteria, it must be placed in the offensive stream (tiger colouring). You may find this makes up a majority of your disposal needs. This includes products that have been in contact with bodily fluids – if they are not hazardous or infectious, opt for a tiger container.1 Aside from non-infectious clinical waste such as single-use PPE, other products that can’t be mixed with municipal items, such as nappies, inconvenience pads, and feminine sanitary items, should be placed in here too.
Dental waste is signified by white in the colour code – with a skull and crossbones (hazardous) for amalgam and without (non-hazardous) for gypsum. This protects people and the environment from potential mercury vapour that can be released from waste amalgam, keeps waste gypsum away from general landfill, and prevents it from creating dangerous sulphide gas. Mixed municipal waste, which is black in the colour code, encompasses waste that can be disposed of in landfill and usually includes food packaging, plastics that can’t be recycled, and tissues.
The remaining colours in the code are unlikely to be managed in the dental practice, but are still worth professionals being aware of. These are purple cytotoxic and cytostatic waste (used if you provide cosmetic procedures such as botulinum toxin injections in your practice); red anatomical waste; blue pharmaceutical waste (which includes used or partially used anaesthetic cartridges); and clear lateral flow testing waste.
In addition to educating staff and giving them access to resources that refresh their knowledge and understanding about safe waste segregation, it can be helpful to provide reminders. For example, signposting staff to useful resources online can help to refresh their understanding of how the best practice colour code applies to their everyday work. Physical reminders located around the premises can also be beneficial, such as placing posters outlining appropriate waste streams and their allocated colour at relevant points in the practice. Experts in the field, Initial Medical, offer
an array of posters that are free to download from their website, which can be utilised in the dental practice to facilitate safe and efficient waste segregation by all colleagues.
However you support your team in implementing safe management of clinical waste, it’s important they can do this confidently. Much waste is generated in the dental practice and effectively segregating it means that businesses can minimise its environmental impact, by ensuring waste is treated in the most sustainable and least energy-intensive way possible. As you move further towards best practice standards, be sure to review your waste protocols.
To find out more, get in touch at 0808 304 7411 or visit the website today www.initial.co.uk/medical
Reference 1. NHS England, (2022). Health Technical Memorandum 07:01 Safe and sustainable management of healthcare waste. (Online) Available at: https://www.england.nhs. uk/wp-content/uploads/2021/05/B2159iiihealth-technical-memorandum-07-01.pdf [Accessed April 2024] n
REBECCA WATERS

Rebecca has worked in the healthcare sector for the past 20 years and earned a BSc Chemistry (Hons) prior to joining Rentokil Initial in 2003. She works within the Research and Development team and keeps up to date on all changes within the clinical waste management industry, as well as the specialist hygiene and infection control industries, and is an active member of the CIWM and HWMA.
Many dental manufacturers claim their products make Dentists’ lives easier, but not every manufacturer makes it their mission. That’s unless it’s Centrix, the 50-years old dental innovator which launched the first direct-to-prep delivery system back in 1970.
Centrix continues to produce single-patient-use products designed to make dentistry easier. This includes the ubiquitous Benda Brush and Benda Micro brush; Tempit temporary filling materials; FluoroDose sodium fluoride varnish, which is available in five patient-pleasing flavours and can be applied in less than a minute via its innovative LolliTray dispenser; NoMix moisture-activated temporary cement, which is designed for use in the surgery and at home in emergencies; Exposé disposable caries indicators which eliminate the need for measuring and mixing, and the risk of spillages; and many others.
FluoroDose
Think there’s nothing new in the world of fluoride varnish? Think again.
To make your life easier, Centrix has redesigned its FluoroDose packaging with new patented features to enhance its handling, comfort and patient safety. In addition to a single dose of varnish, each LolliTray contains a Benda Brush applicator and has been designed so that the Benda Brush can be “popped up” with one hand, making removal simple and safe.
Centrix’s FluoroDose is the award winning 5% sodium fluoride varnish that’s easy to apply in less than a minute. It has a smooth consistency, fast application and choice of five patient-pleasing flavours – caramel, bubble gum, mint, cherry and melon. It is supplied in an Introductory Pack containing all five flavours and refills of individual flavours.


Because the varnish is freshly mixed prior to application it is always in the optimum fluoride distribution, unlike syringes which frequently separate out leaving inconsistent mixes of ineffectively low and dangerously high fluoride concentrations. Each LolliTray contains enough varnish to protect a full adult dentition. Non-gritty and easy to apply in an undetectable very thin film, it is not coloured so that it does not affect the appearance after bleaching etc.
Quick-drying and long-lasting, FluoroDose is suitable for adults with caries risk factors as well as children. It can be applied as often as needed – every three months for high-risk patients or every six months for medium risk ones – and it’s FDAapproved for treating dentinal sensitivity.
With its new LolliTray delivery system award winning FluoroDose, the Dental Advisor’s Top Award Fluoride Varnish six years running, just got better!
With today’s emphasis on minimally invasive dentistry, Clinicians want to ensure that their direct restorations remove as little healthy tooth tissue as possible. One thing that can help ensure this is a caries detection dye.
Exposé caries indicators make the use and application of a caries detection dye simple, messfree and precise. Its well-known Benda Micro brush applicator, available in either fine or extrafine, is prefilled with a dry blue dye, which is simply touched onto a wet tooth to activate. The dye, which acts by staining caries by-products, stains active caries lesions thereby enabling the Clinician to identify precisely the tooth material to be removed. Plus, because it does not become liquid until it has touched the wet tooth there are no drips to stain clothing or soft tissue.
Benda Brush and Benda Micro brushes
While a brush is a seemingly simple tool, it’s important to have the right one for the job.
When applying a precise amount of material to a broad surface, the one-piece Benda Brush with its bendable brush head is ideal. The Benda Brush smoothly places and spreads fissure sealants,
bonding and etching agents, whitening agents and other materials. Benda Micro brushes are perfect for applying smaller amounts of materials or when precise placement is required, such as with selective etching or single point placement. Both brush heads can be angled with ease and remain in position without bouncing back. Their chemical-resistant, non-absorbent fibres are suitable for harsh substances. Disposable for easy clean-up, Benda Brush and Benda Micro brushes are available in two sizes and assorted colours, so they can be colour-coded to avoid cross-contamination.

All of these exciting innovations are now available from Trycare, the UK’s fastest growing dental dealer, who have been appointed sole UK Distributors for the complete range of Centrix problemsolvers. This expands further the comprehensive range of products available from Trycare, which includes everything you need from all the major manufacturers. Yet another reason to contact Trycare and “Discover the magic” for yourself!
For further information about the complete Centrix range contact your local Trycare representative, call 01274 885544 or visit www.trycare.co.uk/centrix. n
We speak to Fiona Sloss, Dental Therapist at Clyde Munro Dental Group, about what the role means to her and how dental therapy skills can be better utilised within the practice


Please could you outline your career so far?
I started working as a Dental Nurse when I was 19 years old, but I wanted to be more hands-on and involved with patient care. I took the online access to higher education diploma and was later accepted by the University of Sheffield to study hygiene and therapy when I was about 21. It was a fantastic course and I couldn’t recommend it enough – there was a practical approach with a lot of emphasis on therapy and we were trained alongside dentists.
I studied during Covid, which brought its own challenges. We could only see a limited number of patients each week, which delayed graduation. I was therefore pleased to find a job in a great practice, which later joined the Clyde Munro group. It meant moving to a small Scottish town, which might not have been the easiest relocation, but my
practice colleagues helped me find an Airbnb until I could purchase my own place which was amazing. My family is Scottish so I have spent much time here, and I can’t speak highly enough of the country and the people.
What do you enjoy most about the dental therapist role?
Definitely the patient interaction! I enjoy getting to prevent problems, while also being able to help people out of problems that have already occurred. Seeing patients leave the practice happier than when they arrived is the best.
I also really enjoy the restorative work and in future would like to focus more on the cosmetic side. Between Direct Access and potential incoming changes to the dental hygienist/ therapist’s prescribing rights, there are many
things we can do – and even more we will be able to do – in these areas.
How important is the role of dental therapist in practice?
For patients, the dental therapist can help shorten wait times for treatment. My scope of practice is smaller than a dentist’s, but that means I focus specifically on the procedures I do offer. I also usually have more time in appointments to dedicate to prevention and patient education, which is essential for their current and future oral health. Especially when it comes to children, I find I am able to spend more time with them than a dentist feasibly could. From the practice’s perspective, my role as a dental therapist allows the dentists to focus on more advanced treatments. One of the dentists I work with likes to concentrate on implants, for
example, so I take on more of the restorative work that his patients need to allow him time for this. That’s where I think the dental therapist can be best utilised in practice – working alongside dentists with a special interest in a specific area. However, the ability to share the workload is useful for many practices, especially given that most are fit to bursting with patients right now!
Why do you think the dental therapist may be under-utilised in practice and across dentistry as a whole?
In many cases, I think dentists aren’t fully aware of what a dental therapist can do. The sooner that dentists understand the dental therapist’s scope, the better. That’s why I believe my university training alongside dentists was so beneficial. Those dentists could see the value of dental therapy for them and their patients from the beginning of their careers.
What is one thing that every practice team can implement to enhance the benefits of a dental therapist?
Communication is essential. I know that I can speak to a dentist whenever I have a query or want to confirm a course of treatment. This ensures continuity of care for the patient and also shows the dentist which areas I am most confident in. This is important for building their trust in my skills – which is the second most important aspect of utilising the skill mix in the practice.
What is it like working with Clyde Munro?
On a day-to-day basis, the practice hasn’t changed since joining Clyde Munro. It’s good to know that high standards are maintained in order to meet expectations across the group, but our clinic was already in a good place. Clyde Munro has helped me introduce the GBT kit into my work, funding and supporting the change of process this required, which I really appreciated. I have been using this now for over a year and patient feedback is incredible!
What are your thoughts on the Dental Therapist Support Programme Clyde Munro offers?
I’m a big believer in this programme. If it had been available when I started at the practice, I would have raced to get involved. It’s providing a level of support that is just not available elsewhere. To have the support of the dentists in your practice echoed by
the group on a wider level means a lot. It also provides a great opportunity to meet other dental therapists and hygienists – we’re often the only dental therapist/hygienist in the practice so being able to connect with more professionals in our position is amazing. In addition, Clyde Munro’s Dental Therapist Programme covers useful clinical topics which enhance the skills of newly qualified professionals or offer a valuable refresher for those who have not had a chance to utilise their therapy skills for some time. It’s all about building competence and confidence.
Any final thoughts?
The more we get used to working as a team, and the sooner all professionals become comfortable working together in this way, the better dentistry will be further down the line. For dentists beginning to work with a dental therapist, there is going to be a learning curve, but if you don’t start you won’t ever see the benefits.
Find out more about Clyde Munro’s innovative Therapist Support Programme at careers. clydemunrodental.com/therapist-supportprogramme/











We are always talking about the importance of quality over quantity, substance over form, but what does that really mean? In dentistry, this can apply to everything from the care delivered to your patients to the benefits you offer your practice team and the training courses you attend to further your clinical skills. In every situation, it’s important to consider whether the perceived value of an activity or event is accurately reflected in reality.
Though it’s difficult to define exactly what quality care is, Donabedian’s 1980s suggestion was “care which is expected to maximise an inclusive measure of patient welfare, after one has taken account of the balance of expected gains and losses that attend the process of care in all its parts”.i The World Health Organization offered its own description in 2018, stating the three key components for quality patient care to be effective, evidence-based services; safe; and people-centred.ii
Both of these can be applied to modern dentistry, where it is more important than ever that expectations of both healthcare professionals and patients are met.iii A survey from 2015iv found that the patient experience was often focused on access, value, health, trust, safety, technology, environment and patientcentred care. Confidence in their dentist’s skills was another major contributor to patients’ satisfaction.v
From a professional perspective, treatment success rates will indicate both clinical skill and quality of care provided. Though not easy to achieve, this is much simpler to monitor compared to patientdriven factors. A clinical audit of treatment delivered can be used to demonstrate how often procedures end in the desired/expected outcome.
Most businesses talk about supporting their staff, but it is important to ensure that there is substance in what is delivered.
A benefits scheme, for example, may be considered to offer a tangible list of advantages for team members. Reports from both 2020vi and 2022vii suggested that employee benefits were the main reason that those surveyed would change job, other than for higher pay. The favourite benefits among UK workersviii are thought to include health insurance, flexible working, pension contribution matching, paid sick leave, mental health and wellbeing support, extra holiday allowance and support for parents, among others.
Supporting dental professionals with tangible education and career development opportunities is also important. This means providing access to training courses, and being flexible in allowing for time out of the practice to attend programmes. Skill advancement should also be actively discussed during annual appraisals in order to ensure that individuals feel supported in making the right career decisions for them. This is critical in dentistry right now given the challenges being faced in recruitment across the country.
An education of substance
Complementing education for all members of the dental team, and providing a platform to find the right programmes, are dental exhibitions and conferences. These make sourcing information and professional recommendations easy, with training providers on hand to offer bespoke advice and guidance. Added advantages of attending such events include being able to take the whole team, networking with the wider dental community and discovering state-of-the-art innovations that will help to drive the future success of your business.


However, not all events are made equal. As with all the other areas discussed, it is important to ensure that you select an event that will truly deliver all that you need it to.
What does this look like? A broad range of industry organisations should be in attendance ensuring you can engage with everyone necessary to make intelligent business decisions. There should be an opportunity to try products and materials for yourself, on stands and perhaps also in a practical workshop situation for an enriched learning experience. With regards to the educational programme, make sure there are appropriate lectures for all members of your team that are covering genuinely relevant topics. It is just as useful to check the speaker line-up – you need more than one main headline speaker to make your team’s visit productive and valuable.
If you’re looking for an event you can rely on in 2025, take your team to BDIA Dental Showcase. This is the largest gathering of practice owners, team members and product experts in the UK, designed specifically to deliver tangible benefits that positively affect your business development and staff retention. Several brands attend BDIA Dental Showcase as their only UK event, making this an exclusive opportunity to see them and their cutting-edge solutions. Plus, the conference programme includes a substantial range of leading speakers and relevant topics, with dedicated theatres for fast-growing disciplines such as dental implantology and cosmetic dentistry, and unique hands-on workshops for a truly comprehensive experience.
Whether looking to deliver exceptional patient care, improve staff retention with better support or find an event that facilitates business growth, make sure you do your homework. It’s important to look beyond the headlines to make sure you are getting quality over quantity and substance over form!
BDIA Dental Showcase 2025, 14th-15th March ExCeL London, dentalshowcase.com
References i. Donabedian A. The Definition of Quality and Approaches to Its Assessment. Vol 1. Explorations in Quality Assessment and Monitoring. Ann Arbor, Michigan, USA: Health Administration Press; 1980.
ii. WHO. Handbook for national quality policy and strategy – A practical approach for developing policy and strategy to improve quality of care. Geneva: World Health Organization; 2018. iii. Busse R, Panteli D, Quentin W. An introduction to healthcare quality: defining and explaining its role in health systems. In: Busse R, Klazinga N, Panteli D, et al., editors. Improving healthcare quality in Europe: Characteristics, effectiveness and implementation of different strategies [Internet]. Copenhagen (Denmark): European Observatory on Health Systems and Policies; 2019. (Health Policy Series, No. 53.) 1. Available from: https:// www.ncbi.nlm.nih.gov/books/NBK549277/
iv. Tickle, M., O' Malley, L., Brocklehurst, P. et al. A national survey of the public's views on quality in dental care. Br Dent J 219, E1 (2015). https://doi. org/10.1038/sj.bdj.2015.595
v. Dopeykar N, Bahadori M, Mehdizadeh P, Ravangard R, Salesi M, Hosseini SM. Assessing the quality of dental services using SERVQUAL model. Dent Res J (Isfahan). 2018 Nov-Dec;15(6):430-436. PMID: 30534171; PMCID: PMC6243813.
vi. LinkedIn Talent Solutions. Global Talent Trends 2020 report. https://business.linkedin.com/ talent-solutions/recruiting-tips/global-talenttrends-2020-report/3qc [Accessed May 2024]
vii. CIPD. Executive Report June 2022. CIPD Good work Index 2022/ UK Working Lives Survey. chromeextension://efaidnbmnnnibpcajpcglclefindmkaj/ https://www.cipd.org/globalassets/media/knowledge/ knowledge-hub/reports/good-work-iindex-executivereport-2022_tcm18-109897.pdf [Accessed May 2024]
viii. Globacare. Creating an effective employee benefits package. https://www.globacare. co.uk/guides/what-are-the-ten-best-employeebenefits-to-offer-staff [Accessed May 2024] n
DAVID HUSSEY

David is Event Director, at MA Exhibitions.








As we know, excellent oral hygiene is crucial for maintaining oral health, and ensuring a good quality of life. However, for some patients, keeping the teeth and gingiva clean is physically challenging. Certain medical conditions can mean that it is hard to take care of personal hygiene. For example, patients with impaired motor skills or memory can find this particularly difficult.
Conditions which pose challenges
There are a number of conditions which might impact a patient’s ability to carry out effective oral hygiene. These might mean that patients are unable to move normally, or have problems with memory. Some of the most common of these conditions include multiple sclerosis (MS), cerebral palsy, epilepsy, rheumatoid arthritis, Parkinson’s disease and Alzheimer’s disease or having had a stroke.i
Reduced mobility can make it difficult for some patients to open their mouth, or to hold and move a toothbrush properly. This can mean that it’s difficult to remove plaque from all tooth surfaces leading to an increased risk of gingival irritation and inflammation, and oral diseases such as caries, gingivitis, and periodontitis. These conditions can be painful, and can lead to infections and tooth loss in the long-term.
When the memory is affected, this might mean that patients forget to brush their teeth, or make and attend dental appointments. It can be helpful to discuss strategies to help manage this with a patient’s family or carers, as this will help them to maintain a good quality of life, and help to keep their mouth healthy. Additionally, some medications or conditions can cause dry mouth – making the mouth feel sore. Because of this, some patients can find toothbrushing painful, and the lack of saliva can make them more prone to caries. It’s important to help patients manage this to maintain a healthy mouth.
To help maintain a healthy mouth, there are a number of adjustments both to lifestyle and oral hygiene that could be made. It’s important for patients (and/or their family or carers) to understand how best to take care of the mouth, and the effects that certain factors can have on oral health.
Firstly, brushing the teeth properly – either independently or with assistance – is important for preventing the development of oral diseases. This means brushing twice a day using a toothpaste which contains sufficient fluoride (1350-1500ppm). Further to this, interdental cleaning once per day is important for removing plaque in areas regular brushing cannot reach – demonstrating how to do this effectively is crucial for solidifying patient understanding. i Making lifestyle adjustments can also be key for prevention. This might mean increasing the amount of fruit and vegetables they eat, cutting down on sugary food and drink, and opting for sugar-free versions where appropriate. Limiting the amount of alcohol patients consume can also be helpful for protecting oral health, as well as quitting smoking – this is because both of these can increase the risk of mouth cancer.i
Regular dental appointments are essential. Where dental professionals are able to monitor patients’ oral health status regularly, they will be able to more easily intervene and prevent the development of oral diseases. Clinicians should also recommend solutions for dry mouth, where applicable, to help make brushing easier, and more comfortable.

The implications of poor oral hygiene on soft tissue health can be substantial. If the gingiva becomes consistently inflamed, red, and sore, the patient may develop periodontitis. The disease is characterised by bleeding, swelling, pain, and bad breath and, in severe cases, it can cause the gingiva to pull away from the tooth and bone. Eventually, if left untreated, tooth loss is a possibility. Periodontal disease is estimated to affect around 19% of adults, globally.ii
In some cases, particularly for patients who find toothbrushing difficult, a mouthwash can be a helpful tool. This should be used at a different time to toothbrushing and, with the right ingredients, may help patients to keep plaque levels under control. Perio plus Balance Mouthwash from Curaprox reduces the risk of tooth decay and is ideal for long-term use. This makes it a great solution for patients who have impaired motor skills, with a chlorhexidine concentration of 0.05% giving patients the benefits of its antibacterial properties, and its unique formula offering longterm protection against harmful bacteria.
If patients are struggling to carry out oral hygiene effectively, due to a health condition or a motor issue, it is important to work with them to help find solutions which work for their unique situation. In particular, establishing a routine which is simple to follow and uses tools which are accessible for them will offer the best results. Regular check-ups will help you to monitor their
progress, and make adjustments to their routine and offer treatments where needed. For more information, please visit www.curaprox. co.uk and www.curaden.co.uk
References
i. NHS King’s College Hospital. Mouth care for people with impaired motor skills or neurological conditions. Accessed April 24. https://www.kch. nhs.uk/wp-content/uploads/2023/01/pl-1028.1mouth-care-for-people-with-impaired-motorskills-or-neurological-conditions.pdf ii. World Health Organization. Oral Health. Accessed April 24. https://www.who.int/newsroom/fact-sheets/detail/oral-health n
TOM ALCRAFT

Tom is Curaden UK Commercial Director for UK & Ireland.














Guests join us from all areas of the industry to provide their own unique perspectives on a wide range of topics, from manufacturers and figureheads of various dental organisations, to those in the trenches working in practice, and more.
















Nothing is off limits in The Probe Dental Podcast, so be sure to tune in wherever you get your podcasts! The Probe Dental Podcast features discussions that explore all areas of the British dental sector.










For more information, sponsorship opportunities or to book a podcast please contact








Recently, headlines have reported a “very concerning” increase in the number of younger patients in the UK with mouth cancer, despite the lack of an obvious reason for a spike in cases.i Traditionally, mouth cancer has been considered by many to be an “old man’s disease” – something that young people and women should be less concerned about – with research suggesting that only 20% of women think that they are at risk. Because of this, some patients in these demographics might be flying under the radar.ii It has been suggested that women, therefore, often miss out on an early diagnosis, in a similar way to other supposedly “male” conditions such as cardiac diseases or heart attacks.iii Some research suggests that, as tobacco use is decreasing, human papillomavirus (HPV) might be to blame for the increasing rates in mouth cancer in younger people.
the risks the virus presents, and whether they are at increased risk of mouth cancer. By making patients aware of the signs and symptoms of the early stages of mouth cancer, they will feel more confident about reporting any concerns to you quickly. Because early signs can resemble benign issues, like mouth ulcers, some patients might feel that they are wasting your time by flagging the unusual lesion. As such, it’s important to reassure patients that if they notice anything out of the ordinary, and it lasts for 3 weeks or more, they should book an appointment.
In addition to lingering mouth ulcers, other early signs of mouth cancer might include a red or white patch, a lump, pain, difficulty swallowing, croaky voice, or weight loss.vii Dental professionals should be checking their patient’s mouth and tongue for these signs at every appointment, and it’s helpful

HPV: what are the risks?
HPV is a virus and, like other viruses such as the flu, there are many different types.iv It can infect the mouth and throat, with some types (most often HPV 16) leading to mouth and oropharyngeal cancer. In the UK, HPV is thought to be responsible for around 25% of cancers of this kind.iv Whilst HPV can be contracted by anyone, with most adults having some form of the virus during their lives, and 10% of men and 5% of women having it at any given moment, it is generally associated with cervical cancer in women.v
This is problematic as it may mean that patients are completely unaware of their level of risk for both HPV and oral cancer, together and separately. Because HPV increases the risk of some types of cancer, including mouth cancer, and causes almost all cases of cervical cancer, the HPV vaccination was developed to help prevent cancer caused by the virus. It is offered to all children in the UK who are between the ages of 11-13.vi A study from 2021 found that rates of cervical cancer were reduced by almost 90% in women in their 20s in England who were offered the vaccine at ages 12-13.vi
everybody’s oral health
The HPV vaccine has been instrumental in reducing the rates of the virus in the UK population. However, it’s important that patients understand
to make patients aware of what you’re checking for so that they can monitor their own health at home when brushing their teeth.
Detecting mouth cancer early
While clinicians will carry out examinations for oral cancer at every appointment, it is important to know what to do if they find something suspicious. Because the early symptoms can be difficult to spot, some dental professionals may doubt themselves about what they’ve seen. As such, it’s important to establish a patient’s level of risk, and carry out the right tests before referring the patient for a biopsy or further testing. Additionally, carrying out effective tests will help to ensure that dental professionals do not miss anything. Biopsies are invasive procedures, so it’s important to undertake all necessary prediagnostic tests prior to referring patients.
The BeVigilant™ OraFusion™ System, available from Total TMJ, is the ideal solution here. The prediagnostic test is designed to be used at point of care to establish the likelihood of a cancerous lesion in 15 minutes or less. The device analyses saliva to produce a result of high, moderate, or low level of risk, by detecting biomarkers associated with oral cancer. This is a fantastic system for clinicians who would like to feel more confident about their decision making when

they spot an unusual lesion, offering improved certainty and allowing oral cancer to be detected in stages I and II.
HPV can affect anybody, so it’s important to keep patients informed about the signs and symptoms of oral cancer to help ensure any early signs of the disease are detected as early as possible.
For more details about the BeVigilant™ OraFusion™ System, visit the Total TMJ website www.totaltmj. co.uk/products/bevigilant-orafusion/, or email info@ totaltmj.co.uk
References
i. BBC News. Concerns voiced over rise in mouth cancer in younger patients. Accessed Mar 24. https://www.bbc.co.uk/news/uk-englandnorfolk-67895314
ii. Oral Health Foundation. Women and mouth cancer: What you need to know about this increasingly common illness. Accessed Mar 24. https://www.dentalhealth.org/news/womenand-mouth-cancer-what-you-need-to-knowabout-this-increasingly-common-illness
iii. RACGP. Tongue cancer diagnoses on the rise. Accessed Mar 24. https://www1.racgp.org.au/ newsgp/clinical/tongue-cancer-diagnoseson-the-rise
iv. Cancer Research UK. Risks and causes. Accessed Mar 24. https://www.cancerresearchuk.org/ about-cancer/mouth-cancer/risks-causes
v. Vitality. EVERYTHING YOU NEED TO KNOW ABOUT ORAL HPV. Accessed Mar 24. https:// vitality-dental.co.uk/everything-you-need-toknow-about-oral-hpv/
vi. Cancer Research UK. The HPV vaccine. Mar 24. https://www.cancerresearchuk.org/about-cancer/ causes-of-cancer/infections-eg-hpv-and-cancer/ the-hpv-vaccine
vii. NHS. Symptoms of mouth cancer. Accessed Mar 24. https://www.nhs.uk/conditions/mouthcancer/symptoms/ n
PHIL SILVER

Phil is Founder of Total TMJ, which distributes innovative technologies from innovative healthcare manufacturers to dentists and clinicians around the world.
High Quality doesn’t have to mean high price and for ease available from your current Interdental brush supplier.





marketing materials available to all


practices and a loyalty scheme to claim free brushes. For more information or to request a sample, visit www.optim-idb.uk
Summer is finally here, and with it comes the long anticipated warm, bright weather. Your patients will have been eagerly awaiting hot afternoons in their gardens, but may not realise the impact this new wave of weather will have on their oral health.
Providing effective support can help patients recognise the good habits they need to reinforce or pick up when the summer sun makes its appearance. Whether this is through face-to-face appointments, or reminders on social media, spreading the simple messages that can have the greatest impact is key to protecting their oral health.
Beating the heat
In the warmer months, it’s easy for patients to forget to keep on top of hydration. However, considering the impact on salivary production, it’s an important aspect of oral health care. Salivary flow rates decrease in the summer when compared to the winter months, caused by hypofunction of the salivary glands.i Whilst this can be caused by anything from anxiety to acute infections, dehydration is the more likely cause at this time of year.
Studies have shown that once exposed to higher temperatures, a decrease in salivary flow rates is almost immediate. In one, patients that were subject to 37ºC temperatures for just 10 minutes – too short a period for dehydration – quickly saw decreased salivary flow.ii Whilst the UK is unlikely to see consistent weeks upon end of 37ºC highs, we can recognise that with longer exposures to hotter temperatures, patients are more likely to experience dry mouth.
The nutrient supply within saliva serves to maintain the presence of certain bacteria and exclude others.iii Saliva itself performs bacterial clearance, buffering capacities, direct antibacterial activity and remineralisation – when reduced, as seen in the heat, dental caries and infections can develop.iv
Patients should be remined to keep hydrated in the summer months, emphasising the effect dehydration can have on their oral health. The Eatwell Guide encourages water, lower-fat milks, and lower-sugar or sugar-free drinks (including tea and coffee) to make up daily fluid intake.v Avoiding excessive intake of high-sugar fluids, such as juices or some sodas, is key for maintaining the dentition.

Despite the increased risk of dehydration, summer is by no means doom and gloom for the dentition. A lack of sunlight has been connected with gum disease, and with approximately one billion people around the world being vitamin D deficient, the summer sun is an opportunity to improve the battle against oral infections.vi
Through sunlight exposure, 7-dehydrocholesterol in the skin absorbs UV B radiation, and is converted to previtamin D3, which in turn isomerises into

vitamin D3. The effects on oral health can be profound. Vitamin D impacts bone and tooth mineralisation, and with unregulated levels patients may develop a rachitic tooth, which is highly susceptible to fracture and decay.vii
Many studies have also found that the presence of periodontitis is associated with lower levels of vitamin D when compared with patients without the disease.vii Those with the deficiency have also been observed to experience high levels inflammation, as well as increased bleeding on probing, compared to those with high levels of the vitamin.vii
Treatments for vitamin D deficient individuals come in the form of supplements, which can often be bought over the counter, and prescription vitamin D. Changes to a patient’s diet may be beneficial, with more fatty fish, egg yolks, and yoghurt being recommended solutions.viii In the summer, taking advantage of the sun will also be of use, but should be done responsibly with sunscreen and adequate hydration.
Why stop at summer?
Summer will not last forever, but patients must be informed on how best to protect their oral health in the warm weather. Hydration is essential, and safely getting enough sun should be recommended whilst the season lasts, but nothing will beat an effective year-round oral hygiene routine.
Brushing twice daily, with interdental cleaning and the use of an effective toothpaste is essential, no matter the weather. Consider recommending patients use either of the specialised 100% Natural Baking Soda Toothpaste solutions from Arm & Hammer™, available to strengthen either Whitening Protection or Gum Protection. Each solution utilises baking soda, which is alkaline in nature, to help return the oral pH to neutral levels within the mouth. Containing 1450ppm of fluoride, their formulas effectively remineralise and strengthen enamel, and remove more plaque around the gumline to prevent infection, when compared to non-baking soda toothpastes.
With the warm weather incoming, patients should be aware of the ways the environment can affect them in the short term, and in turn pick up habits that will protect their oral health long into the future. For more information about the carefully formulated Arm & Hammer™ toothpaste range, please visit https://www.armandhammer.co.uk/ or email: ukenquiries@churchdwight.com
Arm & Hammer™ oral healthcare products can now be purchased from Boots, Amazon, Superdrug, ASDA, Sainsbury’s, Tesco, Morrison’s, Waitrose & Partners and Ocado.
References
i. Dodds, M., Roland, S., Edgar, M., & Thornhill, M. (2015). Saliva A review of its role in maintaining oral health and preventing dental disease. Bdj Team, 2, 15123.
ii. Ligtenberg, A. J. M., Meuffels, M., & Veerman, E. C. I. (2020). Effects of environmental temperature on saliva flow rate and secretion of protein, amylase and mucin 5B. Archives of oral biology, 109, 104593.
iii. Carpenter, G. H. (2020). Salivary factors that maintain the normal oral commensal microflora. Journal of Dental Research, 99(6), 644-649.
iv. Mallya, P. S., & Mallya, S. (2020). Microbiology and clinical implications of dental caries-a review. J Evol Med Dent Sci, 9, 3670-3675.
v. NHS, (2022). The Eatwell Guide, (Online). Available at: https://www.nhs.uk/live-well/eat-well/foodguidelines-and-food-labels/the-eatwell-guide/ [Accessed May 2024]
vi. Oral Health Foundation, (2015). Smile it’s summer! Sunbathing to healthier gums. (Online) Available at: https://www.dentalhealth.org/news/ smile-its-summer-sunbathing-to-healthier-gums [Accessed May 2024]
vii. Botelho, J., Machado, V., Proença, L., Delgado, A. S., & Mendes, J. J. (2020). Vitamin D deficiency and oral health: a comprehensive review. Nutrients, 12(5), 1471.
viii. Armstrong, M., Wartenberg, L., Spritzler, F., (2024) Common Symptoms of Vitamin D Deficiency and How to Treat Them. Healthline, (Online). Available at: https://www.healthline.com/nutrition/vitamind-deficiency-symptoms [Accessed May 2024] n
ANNE SYMONS

Anne is a Dental Hygienist currently working in a Specialist Periodontal/Implant practice and also a busy NHS surgery. She has previously worked in a Max Fax unit, and taught Oral Health care to staff in nursing and residential homes. Anne is also a Professional Educator for Waterpik.
Experience exceptionally lightweight loupes with crystal clear optics, designed and optimised for you.
• Custom Measurements
• Custom Fitting
• Custom Fabrication
For a t as unique as you are.


Alzheimer’s Disease (AD) is thought to contribute to between 60-70% of dementia cases. It is characterised by memory loss, behavioural changes, and a lack of ability to perform daily tasks. Patients with late-stage dementia will eventually need full-time care and face lower life expectancy. The pathological hallmarks of AD include AmyloidBeta protein (Aß) in the brain, and intracellular Tau protein aggregation (forming neurofibrillary tangles), leading to neuroinflammation and eventually neuronal death. Currently, over 55 million people have dementia worldwide, with nearly 10 million new cases every year. Globally, cases are expected to reach 78 million by 2030, and 139 million by 2050.
Both periodontal disease and endodontic disease have a high global prevalence, of more than 50%. Similar oral bacteria have been implicated in both periodontal and endodontic diseases, such as the keystone pathogen, Porphyromonas gingivalis. As a major cause of tooth loss, these oral diseases compromise mastication, aesthetics, self-confidence and quality of life. Over the past several decades, significant associations between oral health status and systemic diseases have been established, including cardiovascular disease, diabetes and AD (Figure 1).
My PhD supervisor at University of Central Lancashire (UCLan), Dr Sim Singhrao, was the one of the first researchers to link periodontitis and AD, after detecting a known virulence factor of P. gingivalis in post-mortem brains of AD patients more than a decade ago. Since then, mounting evidence have pointed consistently to the infectious and inflammatory aetiology of AD.
The importance of research
Currently, the Alzheimer’s Society and the World Health Organization (WHO) do not include oral disease as a modifiable risk factor. Whilst AD causation due to infection is difficult to prove, recent discoveries have reignited interest into the links to oral health. Epidemiological studies have reported lower odds of developing AD when procedures which removed oral infection were carried out such as endodontic treatment and limited extractions of grossly carious teeth. Patients who had frequent periodontal emergencies and those with more than four teeth extracted increased their odds of AD. Clinical studies have shown a correlation between periodontal disease with serum levels of Aß. It is important to acknowledge the potential bi-directional relationship in discussions with patients to encourage preventive measures.
Research techniques and key findings
My research comprised of a number of laboratory studies using a variety of methods. These included: scanning electron microscopy (SEM), immunohistochemistry, transmission electron microscopy (TEM), antimicrobial assays, and cell culture studies.
The detection of Aß protein in endodonticperiodontal infected teeth
This study on extracted teeth found that microbes associated with endodontic and periodontal disease produced insoluble Aß. Like prions, insoluble Aß can have the potential for cross-seeding to the brain and aggregating to form plaques, potentially increasing the risk of development of AD later in life. In the UK, endodontic instruments are single use to minimise the risk of cross-seeding prions, which
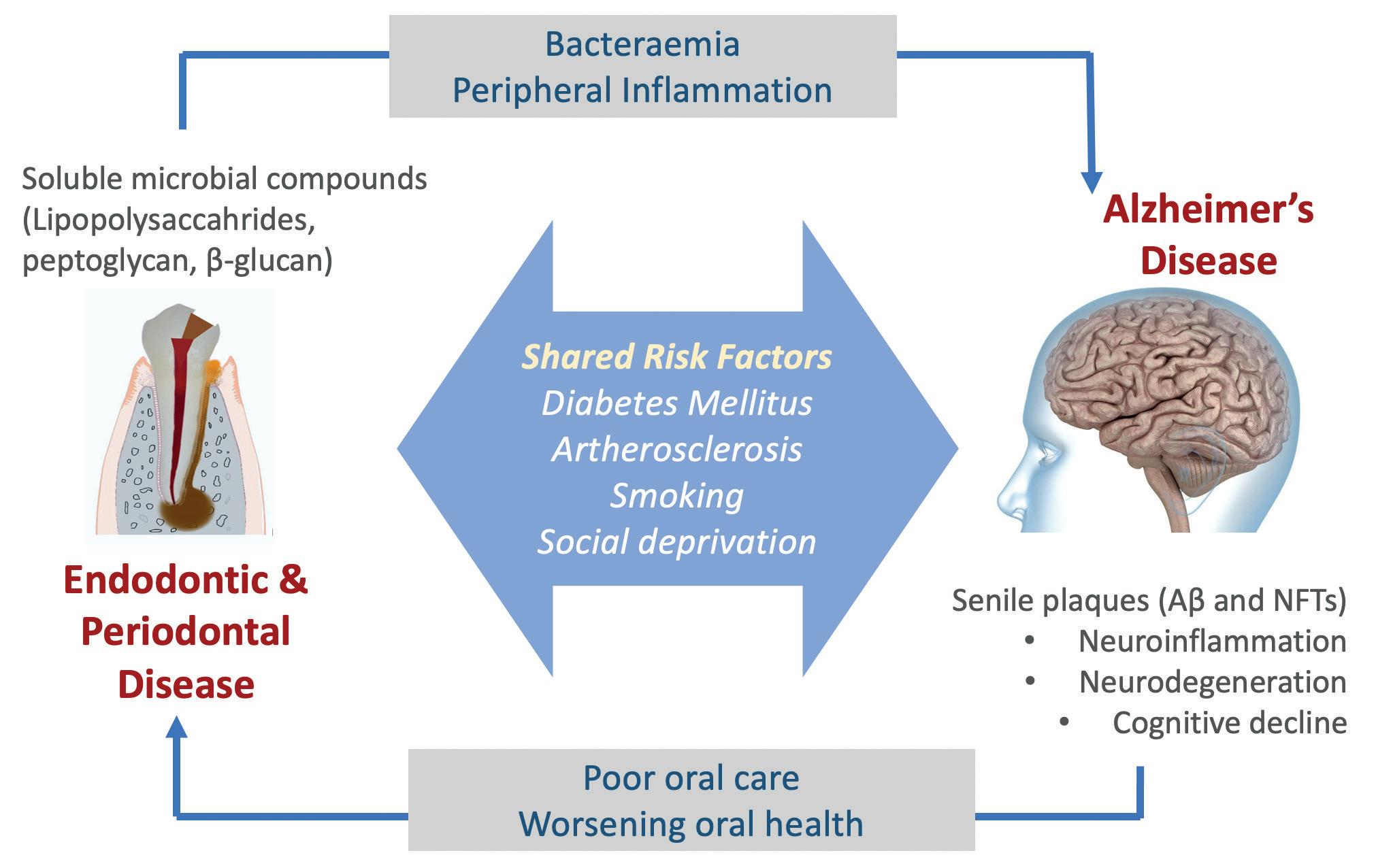
theoretically confers protection from the cross contamination of the Aß protein as well.
The Tau peptide and gingipains study
The gingipains enzyme from P. gingivalis can release the Tau protein from nerve cells. Once released, Tau changes its form to filaments and re-attaches to nerve cells, causing severe damage, becoming incorporated into the lesion known as neurofibrillary tangles. This kills nerve cells, leaking more Tau peptides into the brain and the process is repeated leading to further cognitive impairment as AD progresses.
The P. gingivalis - human neuroblastoma cell culture study
This cell culture study showed that P. gingivalis and its virulence factors, in the presence of inflammatory mediators, can increase the production of Aß proteins. This suggests that P. gingivalis virulence factors can act as antigens of the immune system. The Aß proteins may be harmless when they exist in low quantities, but when they are at consistently high levels, along with inflammation, the risk of developing AD is likely to be higher.
Impact on the profession
At the recent British Endodontic Society’s (BES) Spring Scientific Meeting, I was honoured to win the Poster Prize. This was a unique opportunity to share my research findings with a diverse range of dental professionals including specialists, private practitioners, NHS dentists, and consultants in attendance. I would encourage more colleagues who are conducting endodontic research to engage with the BES as a platform to showcase their scientific findings, as it is a great way to raise awareness about your research. The BES also provides many opportunities for young researchers via the Undergraduate Research Prize and Aspiring Endodontic Researcher Prize, as well as the BES Research Grant.
I hope that my research will facilitate further conversations around oral diseases and systemic health, particularly Alzheimer’s Disease, and increase awareness of this link amongst the profession. Longitudinal clinical studies will be able to produce
stronger correlations but will likely require tracking larger patient cohorts over a long period of time, thus requiring sufficient funding.
With stronger evidence, organisations like the Alzheimer’s Society and the WHO may consider acknowledging oral diseases as a modifiable risk factor. This is crucial for increased public awareness and contributes to AD prevention.
Going forward, awareness of the bi-directional relationship between oral health and general health amongst patients is crucial. Clinicians must have conversations with patients about the benefits of good oral hygiene practices as well as the importance of retaining as many natural teeth as possible as they age. Many infected teeth need not be extracted with early endodontic intervention. Attending regular dental appointments is crucial for both dental and overall health – and the whole dental team must remind patients of this. In the context of AD and many other systemic diseases, interdisciplinary research collaboration between the specialties of endodontology, periodontology, together with our medical colleagues could pave the way for improved patient outcomes.
For more information about the BES, or to join, please visit the website www.britishendodonticsociety.org. uk or call 07762945847 n
References available upon request
DR SHALINI KANAGASINGAM

Dr Kanagasingam is Senior Clinical Lecturer, University of Central Lancashire and Consultant in Endodontics, King’s College Hospital Trust.





























Kenvue is delighted to bring you this article, with the aim of supporting the ongoing Enhanced CPD needs of dental healthcare professionals in improving and maintaining the oral health of their patients.
The aim of this article is to explore the interrelationship between periodontal disease and diabetes mellitus, and the role of dental teams in their early detection and management
On completing this Enhanced CPD session, the reader will:
• Understand the significant impact of oral diseases, particularly periodontitis and caries, on global health as leading contributors to years lost due to disability (YLD)
• Understand the prevalence and severity of periodontitis globally and its link to type 2 diabetes mellitus (T2DM)
• Understand the influence of glycaemic control on oral health and the potential consequences of poor glycaemic management
• Understand the role of dental teams in detecting non-diabetic hyperglycaemia (NDH) and undiagnosed T2DM in patients
• Understand the specific challenges and statistics related to diabetes in the UK, including the number of people diagnosed and the significance of early detection and management for improved health outcomes.
Learning Outcomes: A,C
This article considers the bi-directional link between periodontal disease and diabetes, as well as offering evidencebased tips on preventive strategies for patients.
The Global Burden of Diseases, Injuries, and Risk Factors Study 2017 indicated that between 1990 and 2017, oral diseases — primarily periodontitis and caries — were the leading contributors to years lost due to disability (YLD) in agestandardised rates among 354 diseases and injuries across 195 countries. 1
It was found that severe periodontitis impacts 11.2% of the global adult population, while milder forms affect 50% of adults and 60% of those aged over 65. Notably, severe periodontitis is strongly and independently linked to type 2 diabetes mellitus (T2DM). 1
Additionally, the glycaemic status is known to affect oral health directly; poor glycaemic control can worsen periodontal health, which, if not managed, could result in tooth loss and related psychosocial issues.1
Due to the established bidirectional relationship between periodontitis and T2DM, enhancements in periodontal health may improve diabetes management. This was supported by a recent randomised control trial that showed a 0.6% decrease in HbA1c (glycated haemoglobin) after 12 months following intensive periodontal treatment.1
It has also been suggested that many individuals with T2DM may go undiagnosed for years because the condition often shows no symptoms in its early stages. This situation presents challenges for secondary prevention and management of the disease. Consequently, it is beneficial to investigate non-traditional methods for early detection of individuals with non-diabetic hyperglycaemia (NDH) and undiagnosed T2DM.1
Commenting on this state of affairs, Yonel and colleagues (2020) wrote: ‘It is in the interests of dental teams to know whether their patients have NDH or undiagnosed T2DM, due to the impact of both upon periodontal stability and treatment outcomes. Given the inter-relationship between
these two chronic, noncommunicable diseases, raising awareness of the NDH/ T2DM status of patients in the dental environment will enable dental teams to better target their prevention and management strategies to improve oral health.’1
They continued: ‘Moreover, earlier detection of both conditions will facilitate improved systemic health outcomes for these individuals by facilitating appropriate prevention and interventions, further demonstrating the role that dental teams can play in assisting with management of the growing health and economic burden of T2DM.’1
The situation in the UK
In the UK, almost half of all adults have some form of periodontal disease.2 Adding to the data base, Midwood and colleagues’ (2019) study revealed that over three-quarters (76%) of dental attenders in a cohort of 814 aged between 18 and 92 had bleeding on probing.3
Commenting on these figures, Rana and colleagues (2023) stated: ‘These high rates of gingivitis highlight a need for better communication to patients/the public about how they should be caring for their teeth and gums to achieve
Diabetes and periodontitis: EFOP and WONCA guidance10
In 2023, Herrera and colleagues reported back from the Joint Workshop by the European Federation of Periodontology (EFP) and the European arm of the World Organization of Family Doctors (WONCA Europe) on the association between periodontal diseases and diabetes.10 They offered guidance for oral health professionals (OHPs) in relation to diabetes and periodontitis, including:10
1. The OHP should inform patients with pre-diabetes (NDH)/diabetes about their increased risk of periodontitis and its impact on glycaemic control and its complications. They should then conduct a thorough periodontal examination, including a full periodontal chart and radiographs, and record signs of inflammation (bleeding on probing).
2. Periodontal treatment in pre-diabetes/NDH and diabetes should ideally be performed to a defined endpoint of no periodontal pockets of >4 mm with bleeding on probing or deep pockets (≥6 mm), and if this endpoint is not achieved in general dental practice, such patients should be referred to a periodontal specialist. Stable patients should be enrolled in a regular supportive periodontal care programme, with a frequency of visits appropriate to their needs.
3. Undiagnosed pre-diabetes/NDH and diabetes may significantly impact an individual’s health. The oral healthcare team should be aware that multiple periodontal abscesses in untreated patients, and/or a poor response to optimal periodontal treatment, can indicate an undiagnosed metabolic condition and such individuals’ risk for diabetes should be assessed according to national guidelines for the management of such patients.

periodontal health/stability, and the risks associated with not following this guidance.’4
As for the prevalence of diabetes, in 2023, Diabetes UK reported that the number of individuals diagnosed with diabetes had surpassed five million for the first time. This total includes 4.3 million people who have been diagnosed with diabetes in the UK, along with an estimated additional 850,000 individuals who have diabetes but have not yet been diagnosed.5
According to the European Federation of Periodontology’s (EFP) ‘Recommendations for the oral-healthcare team’ (2020), there are a number of key messages for the oral health care team to bear in mind.6
For instance, patients with diabetes often struggle to maintain stable blood-glucose levels and face a heightened risk of complications. It is crucial to provide oral health education and personalised advice tailored to the needs of patients with diabetes, including specific risk factors and a customised oral care regimen. Annual oral screenings are recommended for children and adolescents.6
Additionally, individuals at risk for type 2 diabetes, although not currently diabetic, should be made aware of their risk and referred to a doctor for further evaluation. Risk assessment should involve a questionnaire and follow screening guidelines based on recommendations from both the American Diabetes Association and the EFP. Both diabetic patients and those with periodontitis require lifelong professional oral care.6
‘Delivering better oral health: an evidence-based toolkit for prevention’ (2021) adds to this picture, stating: ‘Glycaemia in those without a diagnosis of diabetes, and hyperglycaemia in those with diabetes are both risk factors for poor periodontal health and also impair the response to its treatment. While well-controlled diabetes is not a risk factor, many people oscillate between different levels of control. Therefore, it is best to assume an increased risk of periodontal diseases for anyone who has diabetes.’7
Diabetes control recommendations in the Toolkit for those with diabetes – in addition to the usual good practice for periodontal disease prevention – include: 7
• Discuss how controlling diabetes impacts periodontal health, and inquire about the patient's level of glycaemic control (HbA1c)
• Levels consistently below 7.0% (8.6 mmol/L) indicate good control. The target HbA1c value for most people with diabetes is 6.5% or below 48 mmol/mol
1. According to the Global Burden of Diseases, Injuries, and Risk Factors Study 2017, which diseases were the leading contributors to years lost due to disability (YLD) from 1990 to 2017?
a) Cardiovascular diseases
b) Respiratory diseases
c) Oral diseases (mainly periodontitis and caries)
d) Infectious diseases
2. What percentage of the global adult population is impacted by severe periodontitis?
a) 5.2%
b) 11.2%
c) 20.4%
d) 15.3%
3. What proportion of adults in the UK have been diagnosed with diabetes, according to Diabetes UK in 2023?
a) About 10% of the population
b) About 6.5% of the population
c) About 8.6% of the population
d) Less than 5% of the population
4. How does poor glycaemic control affect oral health according to the study?
a) It improves periodontal health
b) It has no significant impact on oral health
c) It worsens periodontal health
d) It reduces the incidence of caries
5. What is the target HbA1c value for most people with diabetes?
a) 7.0% or below
b) 7.5% or below
• Note that individual threshold units may vary as set by healthcare teams, so dental teams should discuss specific targets with each patient
• Encourage patients to maintain good diabetes control through diet, medication, exercise, and regular follow-ups with their diabetes doctor
• Write to the diabetes doctor to request guidance on a patient’s diabetes status and health, particularly HbA1c levels
• Inform the doctor about the patient’s periodontitis status, which can assist in tailoring diabetes care and advice, thereby helping the patient achieve more effective diabetes control.
Pursuing good clinical outcomes
As stated by Turner and Bouloux (2023), ‘DM and periodontal disease are bi-directionally linked, the one affecting the other and vice versa, although the mechanism is not fully understood. Periodontal disease has an adverse effect on glycaemic control. That improves when periodontitis is successfully treated.’8
Indeed, periodontal disease has been described as the sixth complication of DM (after retinopathy, neuropathy, nephropathy, macrovascular and microvascular disease including cerebrovascular disease and altered wound healing).9
However, ‘Fortunately, periodontitis is both a treatable and preventable disease, with good clinical outcomes when detected at an early stage. Prevention depends on daily efficient and effective control of plaque by patients.’8
c) 8.0% or below
d) 6.5% or below
Although patients may struggle to achieve a good level of oral health following oral health advice, Rana and colleagues (2023) suggested that education focused on ‘gingivitis-associated risks’ may help to improve compliance.4
Concluding their survey of patient-reported understanding and dentist-reported management of periodontal diseases, they added: ‘More than 50% of patients knew gingivitis causes poor oral health but <20% knew it elevated risks of other systemic conditions. Patients thought education on risks associated with poor oral health and product recommendations were most likely, and daily reminders least likely, to improve compliance with oral health advice (OHA).
‘Also, 40% of dentists thought their patients were relatively unaware of the importance of gingival health, 76.9% of their patient-base had gingivitis, and 96% give OHA to these patients but only 30% thought this effected improvement. The most useful tools for improving oral health were better patient knowledge of the consequences and one-to-one instruction.’ 4 n
References available upon request.
UK-LI-2400150

The Probe proudly presents The 2024 Dental Awards
The 2024 Dental Awards marks the 26th edition of this prestigious event that, for more than quarter of a century, has sought to recognise the outstanding individuals and teams whose dedication and drive continues to raise standards throughout the UK dentistry profession.
Winning or becoming a finalist in the Dental Awards is a tremendous accolade that provides a significant boost to the profile of a practice. Not only is the event an opportunity to share in the
happiness and success of those who win an award, but it offers the chance to see what fellow dental professionals are doing across the United Kingdom.
The Dental Awards presentation, which streamed on the-probe.co.uk, as well as on The Probe’s Youtube channel, is available to watch on-demand now. Scan the QR code (below) to see the winners of The Dental Awards 2024 react to their victories, as well as to discover who was named a finalist in each of the 12 hotly contested categories.
Winner: Trudy Horne, Dorset Dental Clinic, Poole
Trudy truly embodies what it means to be the face of the practice. Her calm, authoritative yet kind manner enables her to support nervous patients, negotiate with difficult customers, and develop a positive team environment. This has led to Trudy being well-liked by patients and highly respected by colleagues.
Highly Commended: Shauna Church, Inspired Dental Care, Exeter
Finalists: Mary Holroyd, Shiraz Endo, Solihull
Kelly Bird, All Saints Dental Clinic, Kings Heath
Winner: Amanda Reast, The Dental Architect, Leeds
Amanda regularly goes above and beyond for her practice. With more than 30 years’ experience of the profession, she spends her time across multiple sites and consequently no one day is alike.
Highly Commended: Alex McWhirter, North Cardiff Dental, Cardiff
Finalists: Fiona McHugh, Dorset Dental Clinic, Poole
Simona Pacuraru, All Saints Dental Clinic, Kings Heath
Brittany Pittham, Inspired Dental Care, Exeter
Winner: Community Dental Services CIC - Oral Health Improvement Team
With a team of 13 covering five counties, Colworth House’ ‘Brush for Better Health’ National Smile Month campaign was inspired. Promoting National Smile Month at 21 different events. By linking in with Library Rhyme Time session, Baby groups and various pop-up events, the team managed to train over 5,200 people directly and impact a further 13,500 people indirectly.
The Dental Awards 2024 is brought to you by B.A. International, Colosseum Dental, Dental Elite, and Waterpik, in association with The Association of Dental Administrators and Practice Managers, British Association of Dental Nurses, British Association of Dental Therapists, British Society of Dental Hygiene and Therapy, and The Oral Health Foundation. For more, visit https://the-probe.co.uk/ awards/the-dental-awards-2024/



To see the full list of our winners, highly commended, and finalists, and to watch the 2024 Dental Awards Presentation, scan the QR code or visit: https://the-probe.co.uk/awards/the-dental-awards-2024/
Winner: Glenhaven Dental, Cardiff
The team at this family run, multi-generational practice are an inspiration. The judges said that their entry was beautifully presented and that the team focus was clearly apparent, as was a holistic approach to care for patients as well as the wider community.
Highly Commended: Smile Stories, Bournemouth
Finalists: Dorset Dental Clinic, Poole
Cheadle Hulme Dental and Cosmetics, Manchester
Stradbrook Dental, Tonbridge
Winner: Smile Together Dental CIC, Bodmin
The judges were extremely impressed by the unique way in which Smile Together CIC works, its ethos and its team dynamic. Being one of the South West’s largest NHS referral and emergency dental care providers, it partners with NHS Cornwall and the Isles of Scilly Integrated Care Board to provide emergency dental treatment for people who don’t have their own dentist. This numbered over 32,000 appointments last year alone. The practice is run as an employee-owned community interest company that reinvests profits into improving patient facilities. Reinvesting over £7 million since 2016, Smile Together was also the first UK dental practice to achieve B corporation certification in 2022.
Highly Commended: Dorset Dental Clinic, Poole
Finalists: Glenhaven Dental, Cardiff
North Cardiff Dental, Cardiff
DRMR Clinic, London
Website / Digital Campaign
Winner: Cheadle Hulme Dental and Cosmetics, Manchester
The judges described the look and feel of the Cheadle Hulme website as extremely animated. Not only does it contain all the essential information that a dental website needs to present, it also guides potential patients around the practice premises so they can be familiar with the environment when they visit helping to allay any concerns.
HighlyCommended: {my}dentist, Kearsley
Finalists: Inspired Dental Care, Exeter
Meliora Dental, Leeds
DRMR Clinic, London
Winner: KeepStokeSmiling
The judges described the KeepStokeSmiling outreach campaign as a breath of fresh air. Originally conceived in 2018, they not only target an audience in need, but reach an entire community in all its diversities, whether vulnerable or otherwise. Continually promoting the importance of good oral health, a real benefit has been achieved in both changing habits and increased awareness.
HighlyCommended: Avan Mohammed, Queen’s Gate Orthodontics – Teddy Dentists
Finalists: Liz Matthews, Langmans Dental Health Centre
Smile Together Dental CIC
Community Dental Services CIC









Predicta® Bioactive Desensitizer by Parkell swiftly alleviates dentin hypersensitivity using natural tooth elements, calcium and phosphate. Upon application, it forms hydroxyapatite plugs in the dentinal tubules and adds a mineralization layer that broadens the seal, protecting pain-sensing A-delta nerve fibers. Ideal to treat sensitivity from exposed roots after perio-surgery, bleaching, scaling, root planing, and gingival recession.
Patients report immediate relief from sensitivity lasting up to six months.
Get your heavily discounted Predicta® Bioactive Desensitizer kit here:

https://europe.parkell.com/predicta-bioactivedesensitizer-uk-probe
europe.parkell.com/predicta-bioactive-desensitizer-uk-probe
If it’s not written down, it’s not done
Dr Jaswinder Jandu shares his experience of note taking with Kiroku and the difference it has made in his practice:
“I’ve been a dentist for over 25 years. I’ve seen the transition for paper notes, into computer notes. I have experience of different types of software and I can honestly say that using Kiroku for four years now has given me the confidence to know that my notes are recorded accurately and professionally.
“Kiroku has made me more efficient in my note taking. Any software updates that need doing are automatically done. I don’t have to stay at work until seven or eight o’clock at night writing up my notes to make sure that they are done in an accurate fashion. The
notes are bespoke, to suit you – I think that’s great!

“We’ve had CQC inspections and they were also impressed with the note taking and the amount of detail that’s in there. I was very grateful for that. As we all know, if it’s not written down, it’s not done.
“So, a big thank you to Kiroku. A big thank you for the support, and we’ll keep on using it.”
Visit the Kiroku website to find out more about how you can level up your clinical notes, 60% faster.
www.trykiroku.com
Working with the best in a supportive network of peers
Whether you’re just starting out in your professional practice, or looking for a fantastic new opportunity with a supportive team dedicated to clinical excellence, Rodericks Dental Partners can help.
Rodericks Dental Partners is committed to the provision of excellent patient care, and offers comprehensive NHS and private dental services through over 200 practices across England and Wales. Benefitting from a large network of like-minded peers, and run by dental professionals for dental professionals, Rodericks Dental Partners understands the importance of valuing and trusting the expertise of each and every team member.
Natasha, an International Dental Graduate
at Victoria House Dental Practice in Loughborough, says:
“I took part in a specialised programme run by the clinical team to help prepare me for my time in practice. Right from the start, I established a close relationship with my fantastic clinical advisor, who offered invaluable guidance and unwavering support as I transitioned into my role.”

Visit the website to find a wealth of new opportunities, and to find out more! visit www.rodericksdentalpartners.co.uk/careers
Professional throughout the entire process
At Dental Elite, we know that finding a new role in dentistry can be stressful, and the last thing you want is to be left in the dark. Our team is always on hand for support and guidance throughout the job searching process, and it reflects in the thoughts of the professionals that use our service.
Tiphanie Jackson said: “Toni (Dental Elite’s Recruitment Consultant) was very professional throughout the entire recruitment process. She was great at communication, through both messages and calls.”
My Sonder felt the same way, saying: “Toni is amazing. She was quick with her responses, and really efficient with the communication between me and the new employer.”
If you’re looking for a new role in dentistry, or looking to hire at your practice, Dental Elite can support you at every step of the process.
To learn more about specialist recruitment that keeps you in the loop, contact the Dental Elite team today!
For more information contact the Dental Elite team on 01788 545900 https://dentalelite.co.uk/ www.dentalelite.co.uk
BioMin F - continuous 12 hour fluoride protection!
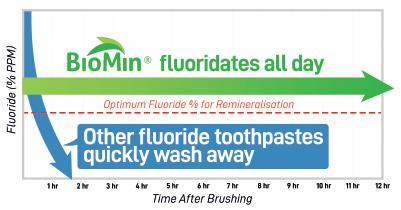
Conventional 1450ppm and above fluoride toothpastes only deliver fluoride for a maximum of 90 minutes, whatever their fluoride content and provided the patient does not rinse. Despite its lower 530ppm fluoride content, Biomin F remains active for up to 12 hours, continuously releasing fluoride to strengthen teeth and protect against decay, even if the patient’s toothbrushing is erratic and inefficient.
Available from Trycare, BioMin F contains tiny bioglass particles made up of fluoro calcium phosphosilicate bioactive glass which bonds to teeth and enters the dentinal tubules, where they gradually dissolve for up to 12 hours, slowly releasing calcium, fluoride and phosphate ions. These combine with saliva to form fluorapatite which strengthens teeth, aids effective remineralisation of enamel and provides effective treatment for hypersensitivity.
Patients also report that teeth feel smoother and cleaner, there is a noticeable absence of background oral sensitivity and that gums are healthier and less prone to bleeding.
A genuine Practice Builder, BioMin F enables patients to enhance their smile and improve their oral health and comfort. It is the only toothpaste approved by the Oral Health Foundation for sensitivity relief and remineralisation.
Tel: 01274 885544.
www.trycare.co.uk/biomin
FluoroDose - the top fluoride dose just got better!
Centrix’s FluoroDose is the award winning 5% sodium fluoride varnish that’s easy to apply in less than a minute.

To make your life easier, Centrix has redesigned its FluoroDose packaging with new patented features to enhance its handling, comfort and patient safety. In addition to a single dose of varnish, each LolliTray contains a Benda Brush applicator and has been designed so that the Benda Brush can be “popped up” with one hand, making removal simple and safe.
Centrix’s FluoroDose has a smooth consistency, fast application and five patient-pleasing flavours – caramel, bubble gum, mint, cherry and melon. It is supplied in an Introductory Pack containing all five flavours and refills of individual flavours.
Because the varnish is freshly mixed prior to application it is always in the optimum fluoride distribution, unlike syringes which frequently separate out leaving inconsistent mixes of ineffectively low and dangerously high fluoride concentrations. Each LolliTray contains enough varnish to protect a full adult dentition. Non-gritty and easy to apply in an undetectable very thin film, it is not coloured so that it does not affect the appearance after bleaching etc.
Quick-drying and long-lasting, suitable for adults with caries risk factors as well as children. It can be applied as often as needed – every three months for high-risk patients or every six months for medium risk ones – and it’s FDA-approved for treating dentinal sensitivity.
Tel: 01274 885544
www.trycare.co.uk





The couple that helps you to achieve even better oral hygiene

FLEXI
• The special FLEXIBLE HANDLE makes it possible to angle the handle to achieve better and easier access to all interdental spaces.
• The non-slip handle ensures good grip even when fingers are wet.
• All brushes have plastic coated wire. This ensures no metal is in direct contact with teeth and gums, thus making them much more comfortable to use and preventing dental injuries.
• 11 sizes ensure that all needs are covered.



TANDEX PREVENT Gel
• Strengthens the enamel and has an anti-bacterial effect.
• 0.12% chlorhexidine and 900 ppm fluoride.
• The consistency combined with the needle shaped tube end make it easy to apply directly on the FLEXI brush and use wherever needed.
• Pleasant taste of peppermint.
• No alcohol or abrasives.
BROUGHT TO YOU BY
A day to support you with everything you need to effortlessly increase implant numbers and associated profits, regardless of your current implant numbers or your chosen implant system.
For GDP’s who:
O er implants and want to do more Are just starting their implant journey
Dental Hygienists & Therapists who: Are identifying potential implant patients
Supporting the long term maintenance of implants
Teams:
Looking at how implants can support practice growth.
Helping delegates with sales, systems and processes to streamline workflow.




Warden
Identifying an Implant Patient.
Pinder
The Importance of Implant Maintenance.
Dr Emanuele Clozza
A Paradigm Shift Using Photogrammetry to Record the Position of a Complete Arch of Implants in a Digital Workflow.
Dr Aly Virani







