LasersMedSci
DOI10.1007/s10103-013-1469-0
ComparativestudyofCO2-andEr:YAGlaserablation ofmultiplecutaneousneurofibromasinvonRecklinghausen's disease
LukasK.Kriechbaumer & MartinSusani & SusanneG.Kircher & KlausDistelmaier & WolfgangHappak
Received:15July2013/Accepted:13October2013 # Springer-VerlagLondon2013
Abstract Withaprevalenceof1in3,000births, neurofibromatosistype1(NF1)isoneofthemostcommon geneticdisordersandischaracterizedbyanuninhibited expansionofneuraltissue.Occasionally,severedeformities occur,butfrequentlyconsiderablecosmeticdisfigurementis causedbythedevelopmentofhundredsofbenigncutaneous neurofibromas.Theobjectiveofthisstudywastoevaluatethe erbium:yttrium – aluminium – garnet(Er:YAG)laserasa therapeuticoptionfortheremovalofmultiplecutaneous neurofibromas.Inthisprospective,comparative,invivostudy, 15,580neurofibromas(44operationson21patients)were removedviaelectrosurgery,CO2-orEr:YAGlaserablation.In 12adjacenttestareas,wecomparedthezoneofthermalnecrosis, thepostoperativepain,thetimetoreepithelialization,theduration ofpostoperativeerythemaandthecosmeticoutcomeofthese surgicalmethods.WhencomparedtoelectrosurgeryandCO2
Electronicsupplementarymaterial Theonlineversionofthisarticle (doi:10.1007/s10103-013-1469-0)containssupplementarymaterial, whichisavailabletoauthorizedusers.
L.K.Kriechbaumer(*) UniversityClinicofTraumaSurgery,MedicalUniversityofVienna, WähringerGürtel18-20,1090Vienna,Austria e-mail:lukas.kriechbaumer@meduniwien.ac.at
M.Susani
ClinicalInstituteofPathology,MedicalUniversityofVienna, Vienna,Austria
S.G.Kircher
DepartmentofMedicalChemistry,MedicalUniversityofVienna, Vienna,Austria
K.Distelmaier
DivisionofCardiology,DepartmentofInternalMedicineII,Medical UniversityofVienna,Vienna,Austria
W.Happak
DivisionofPlasticandReconstructiveSurgery,Departmentof Surgery,MedicalUniversityofVienna,Vienna,Austria
laserablation,theEr:YAGlaserablationoutperformedtheother methodsoftumorremoval.Rapidhealingbysecondintentionas wellastheminimaldiscomfortandscarformationfollowing Er:YAGlaserablationwerenoted.After36monthsoffollow-up, permanentdyspigmentationwasrareandhypertrophicscarring wasnotobserved.Er:YAGlaservaporizationofmultiple cutaneousneurofibromasisasimpleandrapidprocedurethat resultsinsignificantlybettercosmeticresultsthanCO2 laser treatmentorelectrosurgery.
Keywords Er:YAGlaserablation . Neurofibromas . NeurofibromatosistypeI(NF1)
Introduction
Neurofibromatosistype1(NF1,vonRecklinghausen'sdisease [1])isoneofthemostcommoninheriteddisorderswithan incidenceofapproximately1in3,000births[2].Mutationsin thetumorsuppressorgeneneurofibrominareresponsiblefor thealterationsthatoccurpredominantlyinthenervousand cutaneoustissue.Possible complicationsofNF1include disfigurement,cognitiveimp airment,vasculopathy, angiomas,hypertension,skeletalsystemdefects, macrocephaly,andopticgliomas.Additionalcomplications includemalignanciessuchascentralnervoussystemand peripheralnervesheathtumors[3–9].
Thecosmeticdisfigurementfromhundredsofcutaneous neurofibromasisperceivedasthemajorclinicalproblemby mostpatients[10–13].Thesetumorsdevelopbeforepuberty andincreaseinnumberandsizeuntiladvancedage,butthey donotundergomalignanttransformation.Although histologicallybenign,cutaneousneurofibromasareoften painfulduetopressureasaresultoftheirlocation,are irritatingandpruritic,andhavesevereadverseeffectson psychologicalandsocialdistress[4, 10, 11, 13–18].
Largetumorscanbeexcisedformedicalorcosmeticreasons. Removinglargenumbersofcutaneousneurofibromasby excisionisexceedinglytimeconsuming,costlyanddisfiguring. CO2 laserablationisanalternativetoexcisionthathasbecome thestandardtreatmentforremovinghundredsofneurofibromas withminimalbloodloss.Additionally,thewoundshealby secondintention.Thisprocedureresultsinflatanddepigmented scars.Despitethesideeffectofhypopigmentation,marked patientsatisfactionhasbeennoted[11–15, 17, 19].Nevertheless, thepotentialforundesirablewoundhealing,prolongederythema, delayedreepithelialization,andtheformationofdepigmentedor evenhypertrophicscarsandkeloids[17]canmaketheuseof CO2 lasersahazardousprocess[14, 17, 20, 21].Thelikelihood ofsimilaradverseeffectsseemstobeevenhigherwhenusing electrosurgery[22].
Thewavelengthofanotherablativelaser,theerbium: yttrium–aluminum–garnetlaser(Er:YAGlaser,2,940nm), correspondstothepeakabsorptioncoefficientofwaterand isthereforeabsorbed12–18timesmoreefficientlybywater containingcellsthantheCO2 laser[23].Thecombinationofa smallpenetrationdepthduetothehighabsorptioncoefficient andashortpulselengthleadstotheplasmaformationandan explosiveliketissue"vaporization"[ 24].Therefore,heat conductionintothesurroundingtissueisminimal,andthe thermalnecrosiszoneisuptotentimessmallerwhen comparedtotheCO2 laser[21, 25–28].
Duetotheminorthermaldamage,theEr:YAGlasercauses minimalcollagentighteningorhemostaticeffects;however,it doeshaveadvantagesoflesspain,lessriskofseriousscarringor keloiddevelopment,fasterhealing,andfasterresolutionof erythemawhencomparedtotheCO2 laserorelectrosurgery [24, 27, 29, 30].Additionalfavorableresultshavebeennoted whentheEr:YAGlaserisusedin tissueswithhighwatercontent andalowtendencyforbleeding.Cutaneousneurofibromasmeet thesecriteriabecausetheyarecomposedofSchwanncells, fibroblasts,perineuralcells,axonalprocesses,andmastcellsthat areembeddedinanabundantcollagenousextracellularmatrix withahighwatercontent(~86%)[1, 26, 31–33].
Inthisprospectivestudy,weassessedtheeffectivenessof theEr:YAGlaserfortheremovalofmultiplecutaneous neurofibromas.Aspostoperativehealingisstrongly dependentontheamountofresidualthermaldamage,we expectedafasterpostoperativerecovery,anoverall improvementinthecosmeticresult,andsideeffectprofile whencomparedtootherestablishedtreatmentmodalities.
Methods
Patients
Between2004and2012,21patients(fourmenand17 women,FitzpatrickskinphototypesII–IV)withameanage
of46.4(range21 – 73)yearssufferingfromhundredsof cutaneousneurofibromasweretreatedby44Er:YAGlaser ablationoperations(Table 1).Inareasofthebodywhere aestheticsareoflessconcern,someneurofibromaswerealso removedwithaCO2 laserorelectrosurgicaldevices.The prospectivestudywasapprovedbytheEthicsCommitteeof theMedicalUniversityofVienna.Followinganexplanation ofthetrial,itsaims,andthefactthattheywillhavescarsafter treatment,allpatientsgavewritteninformedconsent.Noneof ourpatientssufferedfromseveresystemicdiseasesorknown woundhealingdisturbances.
Procedure
Inthisstudy,onlyneurofibromassmallerthan1cmindiameter weretreatedwithlaserablation.Largeneurofibromasandsome indelicateanatomicregions(e.g.,theeyelid)wereexcisedwith ascalpel,andthewoundsweresutured.Inthemajorityof operations,onesideofthebody(fromtheheadtotheankles) wastreatedwiththeEr:YAGlaser.
Thethreevarietiesofneurofibromas(pedunculated, sessile,subcutaneous)requiredifferentsurgicalprocedures asdescribedbyAlgermissenetal.[14].Theuseofthe Er:YAGlaserissimilartotheapproachusedwiththeCO2 laserwiththeexceptionthat,duetominorthermaldamage, thereisnocoagulationofthewound.However,theoccasional bleedingdoesnotimpedethesurgicalprogressasthe vaporizationofthesmallneurofibromasiscompletedwithin afewseconds.Whenremovingdeeperneurofibromas,digital pressureisnecessary,andthispressurepreventsbleeding duringtheapplicationofthelaserbeam.Anybleedingthat didnotstopspontaneouslyafterdigitalpressurewas cauterizedbyashortsubcutaneouselectricpulsewitha "ColoradoNeedle"inthespraymode.Thesurgeontookthe appropriateprecautiontoavoidcontactbetweenthe electrocauteryandskinlayers.Inrarecases,skinsuturewas usedtoachievehaemostasis.Incontrasttoresurfacing procedureswipingbetweenlaserpassesisnotnecessary.
WeusedaBuraneEr:YAGLaser(WaveLight,Germany) withanablationandcoagulationmodeandaWaveguide smokeevacuationsystem(LaserSystemsGmbH,Austria). Thislaserhasamaximumenergyof2,000mJandamaximum powerof20Wandislicensedforthedebulkingofbenign tumorsandtheexcisionofexternaltumors.Thelaserbeam wasusedintheslightlydefocusedmode(spotsize2–5mm diameter),applyingapproximately1,200 – 2,000mJata frequencyrangeof6–15Hz.Thefluenceoftheablativepulses wasabout12J/cm2.Withthehelpofsurgicaleyeloupes,we supervisedthevaporizationofthegelatinousmassesduring theoperation.
Indirectlyadjacenttestareasontheabdominalwall,the chestorthebackwecomparedtheEr:YAGlaserwithtwo establishedablativetools.Therefore,318neurofibromaswere
Table1 Patients'characteristics
PatientSexAgeSkin type OpsResected neurofibromas
PigmentationReappearance (%) Pain (VAS)
Daysin hospital Cosmetic result
1w39361,400Hyperpigmentation(legs)4241.4 2m67372,620Pigmented324.51.2 3m4832630Pigmented3141.8 4w4741360Pigmented4251.6 5w49241,750Depigmentation(trunk)2353.4 6w51331,030Hyperpigmentation(arms)3241.8 7w52321,170Hypopigmentation(trunk)234.52.8 8w4021430Pigmented3241.4 9w213170Pigmented2452 10w4633640Hyperpigmentation(arms)4143 11w4121480Pigmented3142 12m5731330Pigmented2141.2 13w2031250Pigmented5341.6 14w3331400Pigmented4242.2 15w7332500Pigmented224.51.2 16w6631450Hypopigmentation(trunk)4142.8 17w43221,150Pigmented225.52.4 18w4642900Hypopigmentation(trunk)5142.6 19w4641320Pigmented2151.6 20m4821150Hypopigmentation(trunk)3252.4 21w4221550Pigmented3161.6
Mean46.42.92.1741.93.11.94.52.0 SD±13.60.61.8625.31.00.90.50.7
Skintype Fitzpatrickskintype, Ops numberofoperations, SD± standarddeviation, Reappearance after1year, VAS painmeasuredatday1afterthe operationwithavisualanaloguescale(range1–10), Cosmeticresult meanvaluesofpanelassessment(scores1=excellentto6=unacceptable)
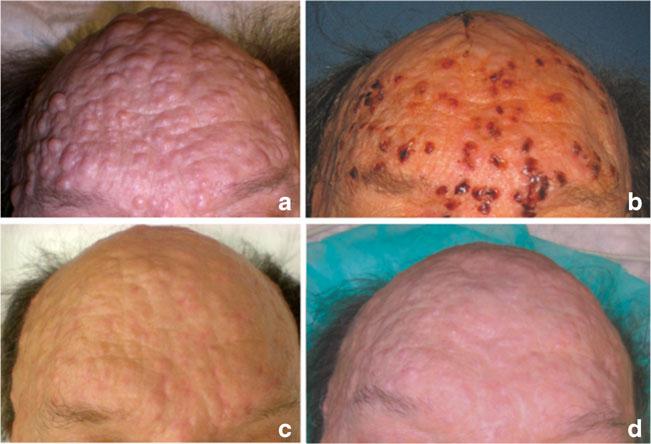
removedbyaCO 2 laseroranelectrosurgicaldevice, respectively(Fig. 1a–d).WeusedanIllumina740CO2 laser (HeraeusLaserSonics,USA)inthecontinuouswave(cw) modeorsuperpulsed.Thespotsize(2–5mm)oftheCO2 laser wasadaptedtothesizeoftheneurofibromas,andweapplieda
powerofapproximately15–25Winthecwmode.Inthe superpulsedmode,thislaseremitsacontrolledtrainofshort duration(1ms),high-power(300Wpeakpower)pulses.Ata repetitionrateof30Hztheappliedfluencewasabout10.6J/ cm2.TheexcessresidualheatproducedbytheCO2 laser
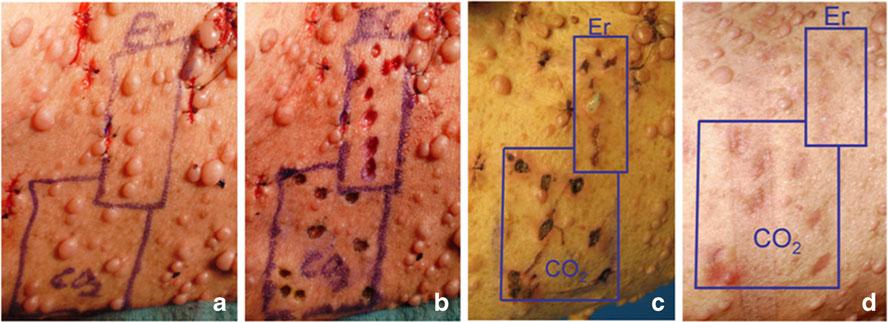
Fig.1 Intestareas,theeffectsoftheEr:YAGandtheCO2 laserwere compared.Neurofibromasofequalsize(a )werevaporizedinthesame anatomicregion(b ). c Onthefourthpostoperativeday,thewounds causedbytheCO2 laserweremarkedlywiderandcoveredwithathicker
scabwhencomparedtothosetreatedbytheEr:YAGlaser.After6weeks, theCO2 laserwoundswerestillerythematous,whiletheEr:YAGlaser woundshadalmostcompletelyreturnedtotheirnormalskincolor(d )
causedimmediatecoagulationofthesmallvesselsintheskin. However,theresultingeschardidnotallowthefull observationofthetumorremoval.Apossibleconsequence ofthisescharistheapplicationoftoolittleortoomuchenergy whichmayleadtoincompletetumorremovalortoexcessive scarringasthetemperatureinthecarbonizedzonemayreach upto500°C[34].
TheVIO300Delectrosurgicalsystem(ERBE ElektromedizinGmbH,Germany)wasusedinthecutting mode(effect4,180W)whenusingeitherawirelooporthe "ColoradoNeedle"fortumorremovalorinthespray coagulationmode(effect1,40W)whenbleedingoccurred afterEr:YAGlaservaporization.Theelectrosurgical procedureswereonlyimplementedonpedunculated neurofibromasthatcouldbeablatedatthebaseoftheskin stalk.Duetosuspectedinferiorcosmeticresults,theCO2 laser andtheelectrosurgicaldeviceswerenotusedontheface.
Inordertohistologicallycomparethethermalnecrosisin humanskinmadebyelectrosurgery,CO2-orEr:YAGlaser,78 specimens(12patients)wereharvestedfromtestareasafter tumorremoval.Allspecimenswereimmediatelyfixedin 4.5%formaldehyde,embeddedinparaffin,sectionedand stainedwithhematoxylinandeosin(H&E).
Postoperativelyanantibioticointment(©Flamazine)was appliedandtheentireareawascoveredwithsterilegauze.To avoidinfectionsduringhealing,allpatientsweretreated precautionarywithValacyclovir(©Valtrex)andMoxifloxacin (©Avelox)for7days.Ultravioletlightprotectionwas recommendedfor3monthstoavoiddyspigmentation.
Datacollection
Histopathology
Thestudypathologistremainedblindedtotheablativemethod throughoutthehistologicevaluationprocessandusedlight microscopyanda μmscalebarforthemeasurementofthe thermalnecrosiszoneintheH&Estrains(Fig. 2).These examinationsweredonebyhand.
Totalbodyexamination
TheoverallcosmeticimprovementofwholebodyEr:YAG lasertherapywasassessedusingdigitalphotographsfrom eachpatientpreoperativelyand4monthspostoperativelyby threephysiciansandtwonurseswhowerenotinvolvedinthe study.Theaestheticresultsweregradedsubjectivelybythe observersonascaleasfollows:1=excellent,2=good, 3=acceptable,4=poor,5=bad,6=unacceptable(Table 1).
Fortheevaluationofthe12testareas,theobserverswere blindedastowhichlaserwasusedforeachside(Fig. 1a–d). Theappearanceofthescarswasgradedaccordingtoascale proposedbyBeausangetal.[35]thatincludescolor,contour,
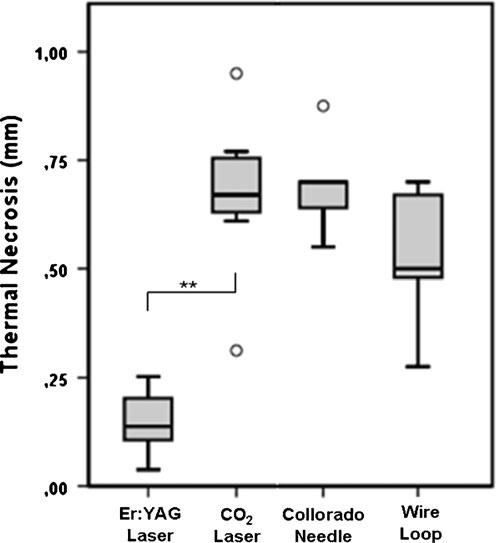
Fig.2 Comparisonofthermalskinnecrosisfollowingelectrosurgery, Er:YAGlaserandCO2 laserablation(78specimen,12patients). I 95% confidenceinterval;[statisticalsignificance;**p <0.001.CO2 laser: continuouswaveandsuperpulsedmodearecombined,sincethethermal damagewasidentical
matte,distortionandanoverallscarassessmentindicatedona visualanaloguescale(VAS).Thisscalecorrelateswellwith histologicscarfindings,andthepossiblescorerangeisfrom4 to24withlowerscoresindic atinginconspicuousscars (Fig. 3).
Clinicalfactors
Timetoreepithelialization(=timewhen95%ofthewounds wereclosed)andthedurationofpostoperativeerythemaafter electrosurgery,CO2 laser-andEr:YAGlaserablationwere documented(Fig. 4 ).Complicationsthatoccurred perioperativelyorduringthehealingprocessandpatient reportednociception1daypostoperativelyweredocumented onaVAS(0=nopain,10=intolerablepain)(Table 1).
Statisticalanalysis
One-wayanalysisofvariance(ANOVA)followedbyposthocBonferronitestswasusedtocomparetheextentof thermalnecrosisusingdifferentablativetechniques.Ina subpopulationof12patients,treatedwithalldifferent ablativetechniquesondifferentareasoftheirbody,a one-waywithin-subjectsANOVAwasconducted. Greenhouse–Geissercorrectionwasappliedconsidering thelowsamplesize.Fortheanalysisofthescarassessment
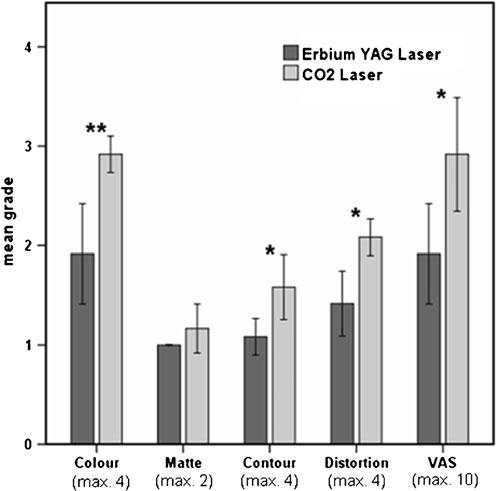
Fig.3 Scarassessmentofthetestareas4monthspostoperativelyusinga gradingscaleproposedbyBeausangetal.a. Τ standarddeviation; max maximalreachablepoints.*p <0.05(Wilcoxonsignedranktest);**p < 0.01(Wilcoxonsignedranktest)
scalein12testareasWilcoxonsignedranktestswere appliedforpairwisecomparisonofcolour,matte,contour, distortionandtheVAS.A p value ≤0.05wasconsidered statisticallysignificant.StatisticalanalysesofFig. 4 were performedusingtheMann–Whitney U -test.Variablesare expressedasmedianswithinter-quartileranges(25th–75th percentiles).Statisticalanalyseswereperformedwith version13.0SPSSforWindows(SPSSInc.,Chicago,IL, USA).
Fig.4 Timetill reepithelializationanddurationof erythema. I 95%confidence interval;[statisticalsignificance measuredwiththeMann–Whitney U -test;**p <0.001
Statementofinstitutionalreviewboardapproval
ThestudywasapprovedbytheEthicsCommitteeofthe MedicalUniversityofViennainMay23,2006(EKNr.: 128/2006).
Results
Histologicfindings
Duetoaclearlydiscernibleboundaryofthermallydenatured dermalcollagenatthedeepermarginofthewoundsduetoa changeofhuefromredtopurple,themeasurementofresidual thermalnecrosiswaseasilydeterminedwithH&Estains.In thegivensetting,theamountofcollateralthermaldamage aftercwandsuperpulsedCO2 laserirradiationwasidentical andthereforethepresentedresultsarenotdivided.The differencesinthermaldamagebetweenEr:YAGlaserand CO2 laserorelectrosurgicaldeviceswerehighlysignificant (p <0.001,ANOVA)andshowedaclearvantageforthe Er:YAGlaser(Fig. 2).Awithin-subjectsANOVAconfirmed theseresultsinasubpopulationof12patients(F =52.40, df = 1.45, p <0.001).
Clinicalimprovement
Medianfollow-upforthe21patients(44operations)was 3(±1.9)years.WiththeEr:YAGlaser,wewereableto removeonaverage354neurofibromas(maximum620)in oneoperation(mean2.8h).Postoperativediscomfortwas minimal(VAS1.9),andcompletereepithelialization occurredwithinanaverageof9.8daysforEr:YAGlaser
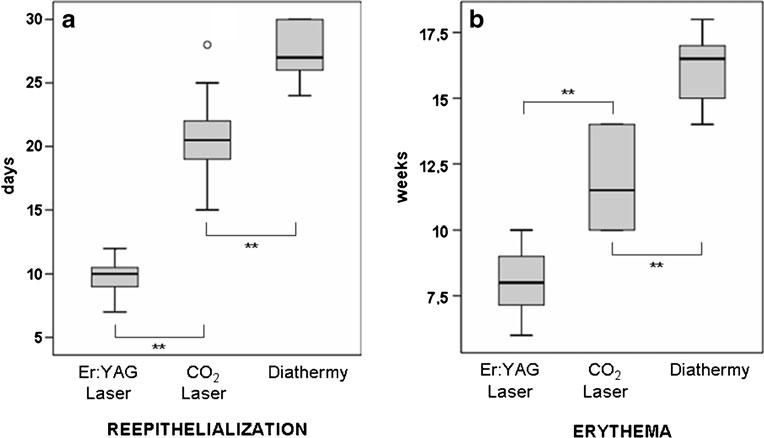
Fig.5a Thepatientatinitial presentation. b Patientswere dismissedonpostoperativeday4 or5. c Thesamepatientduring follow-upat5months. d Longtermresultafter5years.The recurrencerateoftreated neurofibromasseemstobevery low
treatedskin,comparedwith20.8daysforCO2 lasertreatedneurofibromas(p <0.001,Fig. 4).Patientswere discharged4–5dayspostoperative(mean4.5)andwere instructedtoshowereveryday.Thefirstoutpatientvisit wasarranged4dayslater,andtheconsecutivevisitswere arrangedweeklyandthe reaftermonthly(Fig. 5a – d ). Postoperativeerythemapersistedfor8.2weeksafter Er:YAGlaservaporizationandfor11.9weeksafterCO2 lasertreatment.Themajorityoferythemafadedwithin 14 – 17weekswhenelectrosurgicaldeviceswereused (Fig. 4).

Fig.6 EvenseveralyearsafterCO2 laservaporizationthescarsare usuallycompletelydepigmentedandcauseaspottedappearanceofthe skinsurface
TheuseoftheCO2 laserorthediathermyconsistentlyled todepigmentedscars(Fig. 6).Incontrast,afterEr:YAGlaser vaporization,theprimarilypinkscarsgraduallyreturnedto theirnormalskintexture(Fig. 7a,b).Depigmentationor persistenthyperpigmentationwererareexceptions.Basedon theconsensusofthepatientsandsurgeonsalltreatedareas benefitedconsiderablyfromEr:YAGlaservaporization.The resultsdifferedfromregiontoregion,andthebestoutcome wasobservedontheface.Despitethesebenefits,"normal" skincouldnotbeachieved.
Thefrequencyofreappearanceoftreatedneurofibromas after1yearrangedfrom2%to5%(median3.1%).These percentagesaresimilartothedatafrompreviousresearch conductedwiththeCO2 laser[13, 36].Anaccelerationof tumorgrowththroughthelasertreatmentwasnotobserved.
ThemeanscoreforoverallaestheticoutcomeafterEr:YAG laservaporizationobtainedfromphotographicpanel assessmentatfourmonthspostoperativelywas2(±0.7). Overall,indicatinggoodresults.Ofthe21patientsassessed, 11(52.4%)scoredexcellenttogood,nine(42.9%)scored goodtoacceptableandonescoredacceptabletopoor (Table 1).
In12patients,photographicanalysisoftestareasalloweda side-by-sidecomparisonof310scarsdevelopingafterCO2 andEr:YAGlaserablation.Thescargradingsystemusedby theblindedpanelshowedaclearpreferenceforthenew techniqueofEr:YAGlasertreatment.IntheEr:YAGlaser treatedregionswemeasuredamedianscoreof9(interquartile range,5.5–10)comparedtoamedianscoreof13(interquartile range,9.5–13)intheCO2 laser-treatedregions(p =0.012, Fig. 3).
Itwasnotedthatallpatientsinthisstudywouldagreetothe useoftheEr:YAGlaserinsubsequentsurgicalprocedures.
Fig.7 Intraoperativeview(a ) andcontrolafter6months(b ). Thescarshavegraduallyreturned totheirnormaltexture. Empty circle excisionofalarge neurofibroma

SideeffectsofEr:YAGlasertreatment
Ararecomplicationofthelaserablationwasthelacerationof asubcutaneousveinthatrequireddeepsuturinginorderto achievehemostasis.Postoperativehyperpigmentationwas observedontheextremitiesoftwopatientsandlastedfor 4months.Persistenthyperpigmentationcouldbedetectedon thelowerextremitiesofanotherpatient.Fourpatientsshowed hypopigmentationandoneshoweddepigmentationofthe trunk(Table 1 ).Therewerenocasesoffacial dyspigmentation,hypertrophicscarringorkeloidformation.
Discussion
Duetothedisfigurementcausedbythemultitudeof neurofibromaspatientsfrequentlyexperiencesocietal animosity.Awithdrawalfr ompubliclifeisacommon consequence.Theearlyremovalofthesetumorsnotonly tendstoresultinanoptimalcosmeticoutcome,butmayalso restrictsocialwithdrawal.
Skininjuryleadstotheinitiationofalongcascadeof healingevents[27, 37].Theconsequenceisrepairwithan inferiortissue.However,typicallythistissueissmoothand hasanormalappearance.Lesscosmeticscarsarisewhenthe healingprocessdeviatesfromthenormalorderlypattern[37, 38].Thedegreeofthisdeviationisstronglydependentonthe extentofwoundmeasurements.Apartfromthecwmodeof theCO2 laser,thelasersettingsusedinthisstudyallowedfor theapplicationofenergyabovetheablationthresholdofthe skin(approximately1J/cm2 forEr:YAGand5J/cm2 forCO2 lasersinthemilliseconddomain)andshorterthanthethermal relaxationtimeoftheepidermis(1–10ms)[25, 39–42].Thus, thisstudywasconductedinwhathasbeentermedthe"cold ablationregime,"whichkeepsthethermaldamageata minimum[42–44].Contrarytoourexpectations,theuseof thesuperpulsedmodedidnotdemonstrateanadvantageover thecwmode.Areasonfortheequalzoneofthermalnecrosis usingbothmodescouldbetheknownfactofheat accumulationaftermanypulses,whichcancounteractthe benefitofarapidpulseemission[39].
Theexplosiveablationoftissueduetothephotothermal selectivityoftheEr:YAGlaserpulsepreventsunwantedheat diffusionfromthetarget,whichdecreasesthechanceof scarring,persistentpigmentary,vascular,andtextural alterationsorotherunwantedsideeffectsassociatedwiththe useofaCO2 laseroramonopolardiathermy.Thus,theoverall recoveryperiodafterEr:YAGlaservaporizationis considerablyshorter,andthecosmeticresultsaresuperiorto alternativetreatments.Theuseofelectrosurgicaldevicesin thetreatmentofcutaneousneurofibromasislimitedand resultsinwidezonesofthermaldamagewhichrendersthese toolslessideal.
Facialhealingtimeisrapidcomparedtootherareasofthe bodyduetogoodperfusionandthehighdensityofcutaneous appendages(hairfollicles,dermalglands)fromwhichthe reepithelializationderives[38, 45].Reepithelializationafter usingtheEr:YAGlasertookanaverageof9.8dayswhichwas slightlyprolongedcomparedtothe7daystocompletehealing notedinacasereportbyKardorff[18].Anexplanationforthis differenceisthattheKardorffpaperfocusedonfacialhealing only.Intheseareaswealsoobservedcompletehealingwithin 5to8days.InourstudyneithertheCO 2 lasernorthe electrosurgicaldeviceswereusedontheface.However,faster facialhealingwouldalsobeexpectedwiththesemodalities. ReepithelializationafterEr:YAGlaservaporizationwas notablyshorterthanpreviousreportsoftheCO 2 laser treatment(3–6weeks)[11–13, 17, 36].Thehealingtimefor CO2 laserwoundsnotedinthisstudywasconsistentwith otherpublicationsandrequired3weeks.[ 11 , 12 , 14 ]. Electrosurgicallyresectedtumorsrequiredmoreprolonged medicalcareatupto3.9weeks.Thesedataareessentialsince rapidwoundclosureisakeyfactorinthepreventionof infections,woundhealingdisturbancesandscarring[46].
PostoperativeerythemaresultingfromEr:YAGlaser vaporizationpersistedfor8.2weeksandwassignificantly shorterwhencomparedtotheCO2 laserwith11.9weeks(p <0.001).Thesetimesaresimilartowhatwasfoundby Algermissenetal.afterCO2 laserablation(12weeks)[14]. Thissignificantlyshorterrecoveryperiodisimportantnot onlyforcosmeticreasonsbutalsobecausepersistenterythema isoftenthefirstsignofevolvinghypertrophicscars[46, 47].
EventhoughtheformationofhypertrophicscarsafterCO2 laservaporizationofcutaneousneurofibromasisarare complication[14, 15, 17],itcanoftentimesonlybeprevented bythepostoperativeapplicationofsteroids.AsEr:YAGlaser treatmentdoesnotresultinhypertrophicscarringandtherisk forhyper-orhypopigmentationisgreatlyreduced,thewounds donotrequireextensivepostoperativecare(e.g.,steroids, compressiondressingsorsiliconesheets).
TheCO 2 laservaporizationconsistentlyleadsto depigmentationandthereforetoaspottedappearanceofthe skinsurfacesimilartothoseassociatedwithsmallpoxscars. Conversely,theEr:YAGlaserinducesminimumscartissue formationandtypicallyallowsrepigmentationwiththebenefit ofafairlyhomogenousskintexture.Asaresult,wefoundthat apartfromtheparameter"matte"allotherparametersofthe scarassessmentscaleshowedasignificantdifferencebetween bothlasers(Fig. 3).
Thelimitationsofthisstudyarethesmallsamplesize,which mustbetakenintoconsiderationwheninterpretingtheresults andthefactthatonlytheassessmentoftestareaswasblinded whereasthepanelevaluationoftheoverallcosmeticresultswas unblindedandrathersubjective.Ontheotherhandthestudy designallowedforadirectcomparisonbetweendifferent surgicalmethodsinthesameregiononthesameindividual.
Conclusion
WeproposetheclinicaluseoftheEr:YAGlaserforthe removalofmultiplecutaneousneurofibromas.This recommendationisbasedontheshorterpatientrecoverytime, fasterreepithelialization,reduceddurationofpostoperative erythema,lowerriskofscarringandbettercosmeticresults whencomparedtootherestablishedtreatmentmodalities.
Acknowledgments TheauthorsthankDr.KatharinaKlien (DepartmentofOccupationalMedicine,MedicalUniversityofVienna, Austria),Dr.GerhildThalhammer(UniversityClinicofTraumaSurgery, MedicalUniversityofVienna,Austria),Mag.EdithKriechbaumerand Dr.KarenEiler(VCAWestLosAngelesAnimalHospital)forhelpful commentsonanearlyversionandforthefinalreviewofthisarticle.
Conflictofinterest Wecertifythatwehavenoaffiliationwithor financialinvolvementinanyorganizationorentitywithadirectfinancial interestinthesubjectmatterormaterialsdiscussedinthemanuscript (e.g.,employment,consultancies,stockownership,honoraria).
Authorscontribution LukasK.Kriechbaumer:Experimentaldesign, contributiontotheindicatedsurgeries,dataacquisition,analysisand interpretation,statisticalanalysis,writing,anddraftingandrevisingthe manuscript.
MartinSusani:Experimentaldesign,histologicalexaminationsand measurements,andfinalapprovaloftheversiontobepublished.
SusanneG.Kircher:Measurementsofwatercontent,acquisition, analysisandinterpretationofdata,andfinalapprovaloftheversionto bepublished.
KlausDistelmaier:Experimentaldesign,dataacquisition,analysis andinterpretation,statisticalanalysis,andfinalapprovaloftheversion tobepublished.
WolfgangHappak:Experiment aldesign,developmentofthe indicatedsurgeries,acquisition,analysisandinterpretationofdata,final approvaloftheversiontobepublished,andsupervisorysupport.
References
1.vonRecklinghausenFD(1882)In:HirschwaldA(ed)Überdie multiplenFibromederHautundihreBeziehungzudenmultiplen Neuromen.FestschriftfürRudolphVirchow,Berlin
2.RiccardiVM(1981)VonRecklinghausenneurofibromatosis.NEngl JMed305(27):1617–1627
3.OrfanosCE,GarbeC(2002)TherapiederHautkrankheiten,2. Auflage.SpringerVerlag,Berlin,pp973–974
4.WieneckeR(2005)FehlbildungenundGenodermatosen.In:BraunFalcoO,PlewigG,WolffHH,BurgdorfWHC,LandthalerM(eds) DermatologieundVenerologie,5thedn.SpringerVerlag,Heidelberg, pp724–727
5.Ruiz-MaldonadoR,TamayoL(1996)Neurocutaneoussyndromes. In:HarperJ,PembreyM(eds)Inheritedskindisorders:The genodermatoses.Butterworth-Heinemann,Oxford,pp145–148
6.KleihuesP,KisslingM,WiestlerOD(2001)Tumorendes Nervensystems.In:BöckerW,DenkH,HeizPU(eds)Pathologie, 2Auflage.Urban&Fischer-Verlag,München,pp313–325
7.AltmeyerP,Bacharach-BuhlesM(2002)SpringerEnzyklopädie DermatologieAllergologieUm weltmedizin.SpringerVerlag, Berlin,pp1137–1141
8.KorfBR(2000)Malignancyinneurofibromatosistype1.Oncologist 5(6):477–485
9.BährM(2003)ZerebraleMissbildungenundneurokutane Syndrome.In:BrandtT,DichgansJ,DienerH(eds)Therapieund VerlaufneurologischerErk rankungen.KohlhammerGmbH, Stuttgart,pp906–909
10.LinAN,CarterDM(1975)Hereditarycutaneousdisorders.In: MoschellaSL,HurleyH(eds)Dermatology,3rdedn.Saunders, Edinburgh,pp1344–1349
11.MorenoJC,MathoretC,LantieriL,ZellerJ,RevuzJ,WolkensteinP (2001)Carbondioxidelaserforremovalofmultiplecutaneous neurofibromas.BrJDermatol144(5):1096–1098
12.BeckerDWJr(1991)Useofthecarbondioxidelaserintreating multiplecutaneousneurofibromas.AnnPlastSurg26(6):582–586
13.RoenigkRK,RatzJL(1987)CO2lasertreatmentofcutaneous neurofibromas.JDermatolSurgOncol13(2):187–190
14.AlgermissenB,MüllerU,KatalinicD,BerlinHP(2001) LaserbehandlungvonkutanenNeurofibromen.JournalMED:12/01 http://www.journalmed.de/aktuellview.php?id=53 .Accessed20 June2007
15.QueringsK,FuchsD,KungEE,HafnerJ(2000)CO2-lasertherapy ofstigmatizingcutaneouslesionsintuberoussclerosis(BournevillePringle)andinneurofibromatosis1(vonRecklinghausen).Schweiz MedWochenschr130(45):1738–1743
16.HankeCW,ConnerAC,ReedJC(1987)Treatmentofmultiplefacial neurofibromaswithdermabrasion.JDermatolSurgOncol13(6): 631–637
17.OstertagJU,TheunissenCC,NeumannHA(2002)Hypertrophic scarsaftertherapywithCO2 laserfortreatmentofmultiplecutaneous neurofibromas.DermatolSurg28(3):296–298
18.KardorffB(1998)NeurofibromatoseTypI(MorbusRecklinghausen): kombinierteErbium.YAG-Laser-undExzisionstherapievonkutanen NeurofibromenDerm4:404–406
19.AchauerBM,KamVMV,BernsMW(1992)Laserinplasticsurgery anddermatology.ThiemeMedicalPublishers,Inc,NewYork,pp 113–130
20.GrossmanAR,MajidianAM,GrossmanPH(1998)Thermalinjuriesas aresultofCO2 laserresurfacing.PlastReconstrSurg102(4):1247–1252
21.AlsterTS,LuptonJR(2002)Preventionandtreatmentofsideeffects andcomplicationsofcutaneouslaserresurfacing.PlastReconstrSurg 109(1):308–316,discussion317–308
22.LohSA,CarlsonGA,ChangEI,HuangE,PalankerD,GurtnerGC (2009)Comparativehealingofsurgicalincisionscreatedbythe PEAKPlasmaBlade,conventionalelectrosurgery,andascalpel. PlastReconstrSurg124(6):1849–1859
23.AlsterTS(1999)CutaneousresurfacingwithCO2anderbium:YAG lasers:preoperative,intraoperative,andpostoperativeconsiderations. PlastReconstrSurg103(2):619–632,discussion633–614
24.MajaronB,PlestenjakP,Lukač M(1999)Thermo-mechanicallaser ablationofsoftbiologicaltissue:modelingthemicroexplosions. ApplPhysB69:71–80
25.HohenleutnerU,HohenleutnerS,BaumlerW,LandthalerM(1997) FastandeffectiveskinablationwithanEr:YAGlaser:determination ofablationratesandthermaldamagezones.LasersSurgMed20(3): 242–247
26.KriechbaumerLK,SusaniM,KircherSG,HappakW(2012) Vaporizationofcutaneousneurofibromaswithanerbium:yttrium–aluminum–garnetlaser:acomparativehistologicevaluation.Plast ReconstrSurg129(3):602e–604e
27.LePillouerPA,CasanovaD(2002)Scarringprocessafterinduced dermabrasion.WoundRepairRegen10(2):113–115
28.MerigoE,CliniF,FornainiC,OppiciA,PatiesC,ZangrandiA, FontanaM,RoccaJP,MeletiM,ManfrediM,CellaL,VescoviP (2013)Laser-assistedsurgerywithdifferentwavelengths:a preliminaryexvivostudyonthermalincreaseandhistological evaluation.LasersMedSci28(2):497–504
29.Drnovsek-OlupB,VedlinB(1997)UseofEr:YAGlaserforbenign skindisorders.LasersSurgMed21:13–19
30.TanziEL,AlsterTS(2003)Single-passcarbondioxideversus multiple-passEr:YAGlaserskinresurfacing:acomparisonof postoperativewoundhealingandside-effectrates.DermatolSurg 29(1):80–84
31.KimuraM,KamataY,MatsumotoK,TakayaH(1974)Electron microscopicalstudyonthetumorofvonRecklinghausen's neurofibromatosis.ActaPatholJpn24(1):79–91
32.LassmannH,JureckaW,LassmannG,GebhartW,MatrasH,Watzek G(1977)Differenttypesofbenignnervesheathtumors.Light
microscopy,electronmicroscopyandautoradiography.Virchows ArchAPatholAnatHistol375(3):197–210
33.PeltonenJ,JaakkolaS,LebwohlM,RenvallS,RisteliL,VirtanenI, UittoJ(1988)Cellulardifferentiationandexpressionofmatrixgenes intype1neurofibromatosis.LabInvest59(6):760–771
34.ZhangJZ,ShenYG,ZhangXX(2009)Adynamicphoto-thermal modelofcarbondioxidelasertissueablation.LasersMedSci24(3): 329–338
35.BeausangE,FloydH,DunnKW,OrtonCI,FergusonMW(1998)A newquantitativescaleforclinicalscarassessment.PlastReconstr Surg102(6):1954–1961
36.AlgermissenB,MüllerU,KatalinicD,BerlienH-P(2001)CO2 laser treatmentofneurofibromasofpatientswithneurofibromatosistype1: fiveyearsexperience.MedLaserAppl16:265–274
37.SingerAJ,ClarkRA(1999)Cutaneouswoundhealing.NEnglJ Med341(10):738–746
38.ScheithauerM,RiechelmannH(2003)Review:PartI.Basic mechanismsofcutaneouswoundhealing.Laryngorhinootologie 82(1):31–35
39.WalshJTJr,FlotteTJ,AndersonRR,DeutschTF(1988)PulsedCO2 lasertissueablation:effectoftissuetypeandpulsedurationon thermaldamage.LasersSurgMed8(2):108–118
40.Lukač M,SultT,SultR(2007)Newoptionstreatmentstrategieswith theVSPerbium:YAGaestheticslaser.JLaserHealthAcad1:1–9
41.TrellesMA,VelezM,MordonS(2008)Correlationofhistological findingsofsinglesessionEr:YAGskinfractionalresurfacingwith variouspassesandenergiesandthepossibleclinicalimplications. LasersSurgMed40(3):171–177
42.RossEV,BarnetteDJ,GlatterRD,GrevelinkJM(1999)Effectsof overlapandpassnumberinCO2 laserskinresurfacing:astudyof residualthermaldamage,celldeath,andwoundhealing.LasersSurg Med24(2):103–112
43.KhatriKA,RossV,GrevelinkJM,MagroCM,AndersonRR(1999) Comparisonoferbium:YAGandcarbondioxidelasersinresurfacing offacialrhytides.ArchDermatol135(4):391–397
44.VenugopalanV,NishiokaNS,MikicBB(1991)TheeffectofCO2 laserpulserepetitionrateontissueablationrateandthermaldamage. IEEETransBiomedEng38(10):1049–1052
45.PatelGK,WilsonCH,HardingKG,FinlayAY,BowdenPE(2006) Numerouskeratinocytesubtypesinvolvedinwoundreepithelialization.JInvestDermatol126(2):497–502
46.MustoeTA(2004)Scarsandkeloids.Bmj328(7452):1329–1330
47.TeotL(2002)Clinicalevaluationofscars.WoundRepairRegen 10(2):93–97
