socials



I hope you had a wonderful festive season and that your year ahead is a success!
What is exciting about 2023?
As you may know, we have elected a Vice President – a big congratulations to Matt Cooper who is now the first Vice President of Osteopathy Australia. This change to our constitution and our Board operation is a really exciting step in ensuring great succession as we forge ahead delivering our strategy to help our members, the profession and consumers.
2023 is my last year as President and also fellow director Georgia Ellis’s last year on the Board. This creates a very exciting opportunity for two new osteopathic Board members to be elected later in 2023. I strongly encourage anyone considering applying for the Board to complete our governance eLearning training that will be available in early 2023, and also attend our webinar early in 2023.
Strategically, we have a lot of our projects being executed throughout 2023. Our endeavours to make an impact on the poor geographic workforce distribution of osteopaths in Australia are being driven by our New Course Committee, which is working with consultants on a business case to present to universities outside of Victoria to explore opportunities. This is something that will be part of our ongoing strategy going forward until we gain greater distribution of osteopaths throughout Australia. Our consumer branding marketing strategy will be executed throughout 2023. This is a very exciting project to help consumers easily understand what an osteopath is and how we can help them. This is a great opportunity for osteopathic advocacy and will help attract people to seek osteopathic help.
In late 2022 I attended the AHPA (Allied Health Practitioners Association) Health Symposium where Anne-Marie Boxall, the Chief Allied Health Officer for the Australian Government, spoke about how the Government sees allied health as one service, and that a multidisciplinary approach to health is best for patient outcomes. Antony is the current chair of AHPA and should be commended for his role there; having osteopathy represented so well in this forum is indicative of how well we are regarded in the allied health space. Antony is also the sole allied health representative on the Government’s Strengthening Medicare Taskforce. His role is to advocate for greater Medicare benefits for Australians to access allied health. This is an incredible table for him to be sitting at. We hope to see you all in a faceto-face environment throughout 2023 with greater Professional Development seminars and consultation meetings with you, our members. Wishing you all the best for a great 2023.
Michelle Funder, President Osteopathy Australia mfunder.director@osteopathy.org.au

Osteopathy Australia
T (02) 9410 0099 E info@osteopathy.org.au
W www.osteopathy.org.au
osteopathyaustralia osteoaust
osteopathyaustralia osteopathyau
OSTEO LIFE is the quarterly magazine for Osteopathy Australia members. For enquiries, feedback, or to contribute, contact Communications on 02 9410 0099 or comms@osteopathy.org.au. For advertising enquires, email info@osteopathy.org.au.
Editorial and Education Advisory Group
Toby Barker, Casey Beaumont, Amy Lawton, Melissa McDougall, Adam Nicholson, Jade Scott, Sally Tran, Heath Williams
Chief Executive Antony Nicholas
Sub Editor Adam Scroggy Designer Stephanie Goh
Advertising info@osteopathy.org.au
Printed by Megacolour
Book review
26 Massage Yourself: Self-massage of muscles, tendons and ligaments by Rowland Benjamin Practice Management
30 Upcoming workplace relations changes
32 Everything you need to know about your employment contract Advertorials
28 A transcript from the launch of DrRest
34 Heat Wraps are recommended in Australia’s new Clinical Care Standard for Low Back Pain
“I strongly encourage anyone considering applying for the Board to complete our governance eLearning training that will be available in early 2023”
Natasha Owens has joined the Osteopathy Australia team as our new Senior Policy and Advocacy Officer.
Natasha has a background in health and environmental policy and science having completed a Bachelor of Arts in Development Studies and Master of Science in Environment Health. This study has given her a comprehensive understanding of a wide range of areas including local and international health policy and legislation, anthropology, and the social determinants of health.
Towards the end of her studies, she started working as a medical receptionist, which ultimately confirmed that she wished to progress her career within the health industry more specifically. From there she progressed into national management and operational roles within a corporate medical practice group before settling in a clinical governance and policy role, where she further progressed her skills completing a Graduate Cert in Health Service Management, Safety and Quality.
This led Natasha to believe that policy is an area that can have some of the most powerful impacts on health. Whether it’s minor policies that ensure safety, quality and best practice is upheld, or larger, industry-changing policies, each will have immediate and flow-on effects for practitioners and patients alike.

On starting, Natasha noted, “My first few weeks have been met with warm welcomes and a sense of community from all in the team and the wider osteopathic and allied health community. It has been great to
learn about osteopathy from the team and see that there is plenty of room for me to be able to use my skills to promote osteopathy and to provide support and resources to our members.”
Having worked in and managed in the primary healthcare sector, Natasha understands the realities of running a practice and working with practitioners and patients alike, using this understanding
to produce policies and resources that are practical and relevant to the needs of osteopaths. She will also be working with the rest of the Osteopathy Australia team to actively advocate for the rights, recognition, and entitlements of osteopaths.
Natasha is excited to get started and said, “I look forward to working with the wider osteopathic community and positively impacting the profession.”
“I look forward to working with the wider osteopathic community and positively impacting the profession”
ANTONY NICHOLAS, CHIEF EXECUTIVE, OSTEOPATHY AUSTRALIA

Welcome 2023 and (everything crossed) the year where we can get back to normality and forging ahead. Regardless of what happens, we have shown we are prepared to show up and do what needs to be done to support you and the osteopathy industry through any challenge.
Osteopathy Australia, as always, is maintaining all our core work, but also has some exciting projects in development and over 2023 we will be focusing on them a lot more. These include:
The ‘new course committee’, using the economic and financial data collected by expert consultants will start targeting identified universities to lobby for new osteopathy courses (see page 7 for more);
Building, expanding and developing more eLearning, podcasts and webinars as your essential affordable CPD hub;
Launching our osteopathy branding and marketing campaign to target all the Australians who have not used an osteopath;
Building on support offerings such as the counselling service launched in August 2022;
Launching the clinical supervision modules and templates to help osteopaths be better clinical supervisors or clinical mentors (see page 16 for more);
Patient reported outcomes trial to gather better data to demonstrate the efficacy of osteopathy;
Continually improving, updating and tweaking the usability of our new member website, dashboard and interaction;
Continually improving and expanding our consumer-focused website; Educating our members on what the intensive consumer sentiment research we completed over the past year tells us about how you and how we should be advertising;
Continuing to build better links between Osteo Life clinical articles, continuing professional development; Continuing to lobby for expanding the role of osteopaths in occupational rehabilitation management, expanded aged or disability care or working with general practice, plus developing resources to help you do it.
Naturally, we are adding all these new components of our work while maintaining all our existing projects and making sure we continue to support you and advance osteopathy.
At the October 2022 annual general meeting, amendments proposed for the Constitution of Osteopathy Australia were passed.
As it has been five years since the last constitutional amendments, these changes helped keep the Constitution current, and for better succession planning of the Board, the role of the Vice President was created. Thank you to the members who attended, and those who submitted proxies to assist in passing these changes.
After the annual general meeting and the passing of these changes, the
Board of directors voted on nominations for the role and Matthew Cooper, osteopath, was elected to be the first Vice President.
Matthew stated, “A seamless handover to and succession is vital for the continuation of a productive board and an effective association. I feel compelled to drive the future strategic direction of the association and think this step of adding a Vice President will help with this.”

“Regardless of what happens we have shown that we are prepared to show up and do what needs to be done to support you and the osteopathy industry”
If you’re a final year student or graduate member, you have free access to the Osteopathy Australia Graduate Guide to help you transition into practice. It has a step-by-step guide on what you need to do and where to get more information, support and help.
It also has everything you need to know from the scope of practice to the business of osteopathy to working as a locum vs an employee, understanding private health funds and your CPD obligations.

Osteopathy Australia has a strategic aim of developing more undergraduate and postgraduate osteopathy courses around Australia.
Universities are currently experiencing incredibly difficult times and health courses are expensive to run. However, over the last few years, we have been investing in developing better resources to demonstrate why universities should offer osteopathy courses. It is our longterm strategy to have osteopathy courses available to potential students in every state. This will not be easy to achieve. The Board of Osteopathy Australia has previously committed, and continues with its commitment of hundreds of thousands of dollars to achieve this.
It goes without saying that the strategic targets will be for courses outside of Victoria and initially targeting capital and some major regional cities, as access to osteopaths and osteopathy clinics will be vital. We also don’t care if a university wants to offer undergraduate or postgraduate course options.
To further this strategic aim for 2023 we have contracted PhillipsKPA, who are educational expert consultants, to develop a business and economic case to present to selected universities to build interest in developing sustainable osteopathy programs. An important consideration for universities is the extent to which there is opportunity and demand for an increased supply of osteopathy graduates, plus access to potential staff, clinical supervisors and clinical placements. Hopefully most of you participated in our December survey. This work will be the backbone of our educated, financially savvy, and professional approach to universities.
On a slightly depressing but realistic note – timelines for this are long. Even if a new university said yes tomorrow, it would be 2-3 years before the course would commence enrolments and, depending on course structure, another 3-5 years before the first graduates.
Over the past five years Osteopathy Australia has engaged with several universities – mainly in Sydney but also


in other states – on new courses, but two promising options were obliterated with the impact of COVID.
It was clear to us the money argument and the need for profession participation will be core to future interest. We will be targeting select universities in the first half of 2023, particularly those close to a range of osteopath businesses and who already offer a range of allied health or health sciences degrees.
PLEASE DO if you have close contacts or regular patients who are senior university staff, such as VC, Deans or Executives, contact us as key contacts are essential.
PLEASE DON’T make course pitches or directly contact universities yourself as this never ends well, is often perceived as unprofessional and often undermines our work to build momentum or interest.
PLEASE DO speak to us first.
Fellow osteopaths often approach Osteohustle because they want to market on social media, but they don’t know how to without feeling sales-y, unprofessional or worrying about AHPRA guidelines. If you’re an osteopath who enjoys social media, this two-part article will show you exactly how to help more people outside of your treatment room, share your version of osteopathy, and ultimately get more patients through social media. In this article, part one, we’ll be exploring some important foundations of understanding about social media, and walk through steps one to three of my eight steps to success on social media.
Before we dive into my eight steps to success on social media, it’s essential that we shift our collective approach to social media as osteopaths.
I often see osteopaths using social media as an advertising platform, and this is where many of us stumble, stopping us from seeing the results from social media that we’re looking for.
Social media is about being social, it’s not a platform to sell. For osteopaths, selling on social media means always or often posting things such as, “We have appointments available on Saturday.”
Posting ‘sales’ content will likely only get you patients if you have already invested time and effort to build a value-based community. The more you give to your followers, the more you’ll get back from them.
For osteopaths, building a community on social media is more than a group of people who sometimes ‘like’ your content. It’s about bringing local people together who follow, engage and share your content because they believe in what you do and why you do it.
Gary Vee’s book Jab, Jab, Jab, Right Hook outlines the importance of providing genuine value (aka your knowledge) to people (jab) and continuing to give and give (jab, jab) before asking for anything in return (right hook).
Being known as an osteopath who looks to share what they know will lead to people connecting the dots for themselves in the shape of visiting your website, calling the clinic or booking online.
Step 1: Set clear goals. You need to have two specific goals for social media.
Your first goal should be based on what you define as success on social media. I’ll lay out what I believe are some excellent ‘success markers’ for osteopaths on social media, however, ultimately this first goal is up to you. No matter what you set as your first goal, your second goal needs to be to get people off social media. Let’s explore both these goals and how you should define them.
Goal 1: Success on social media
“Success” is a loose term, giving us the scope to define what this means to us personally.
When I ask my coaching clients what they would define as success on social media they’ll often reply with either “I don’t know” or “more followers”. I always reply with the same advice. You’re better off having 500 followers that consistently engage in your content
Alan Zaia is an award-winning British osteopath, a finalist in The Institute of Osteopathy Practice of the Year 2019 awards and the founder and CEO of Osteohustle (osteohustle.com). Osteohustle is an international network of osteopaths who provide easy, ethical and effective business and marketing tools through coaching, courses and community.
and love what you do, as opposed to 5,000 followers who don’t pay attention to your content.
When osteopaths say they define success as getting more new patients or followers on social media, in my experience, what they actually mean is, “I want to help more people, and I want to see my clinic benefit financially from the money, time and effort I put into social media.”

To help more people through social media you need to know you’re sharing content that people want to engage in. Therefore, a great measure of success for osteopaths is positive comments on content. These positive comments show you how many people you’ve helped through that piece of content.
The best way to demonstrate this point is to give you a comparison
ALAN ZAIAbetween unhelpful definitions of success for osteopaths, and specific, ethics-first definitions.
Instead of social media success meaning: New patients; Followers; and Views.
Aim for social media success meaning:
X number of positive comments on each piece of content;
X number of DMs from potential patients per month;
X number of patients who say they heard about you from your social media per month;
Collaborating with X number of local businesses every year.
Choose your definition of success to start with, and make that your first social media goal. Your second social media goal will be the same for every osteopath.
Goal 2: Get people off social media. Getting people off social media and into places like your website, mailing list, on the phone or onto your treatment couch is essential for osteopaths.
Getting people onto your website, or subscribed to your clinic newsletter is important because we can’t control social media organisations. If Facebook changes a feature or is shut down tomorrow, you need to have a way to continue to help people and remind them of the fantastic work you do.
For 99% of osteopaths, we need to get patients off social media and into the clinic in order to benefit financially from the time, effort and money we put into social media. However, asking for someone to book an appointment is quite a big ask.
Remember Jab, Jab, Jab, Right Hook? You must lay the foundations of sharing excellent, informative and helpful content before you go for the right hook of asking people to book an appointment in a social media post. We’ll cover exactly how to provide patients and potential patients with ethics-first, helpful content in Step 3.
Step 2: Choose one platform. By choosing one platform to focus on you can double down on learning how
to interact in that one social media space. You can also experiment until you find the perfect systems that work for you to move you toward your two social media goals.
There are many reasons why you should choose one platform over the other. You should consider your goals, which platform the types of patients you love to treat may be on, and which platforms you’re already familiar with.
You’re going to be spending a lot of time on the platform you choose – more than you think – so make it easy on yourself and choose the one you already know and enjoy the most.
I’ve generalised here to give you an idea of which platform to choose, however, this is by no means a definitive guide; Use Facebook if you’re comfortable using text and video to talk with lots of people on their own and in different Pages and Groups; Use Instagram if you enjoy showing your work through images and videos – whether with animals, exercise, nutrition, opinions or life behind the scenes;
“For 99% of osteopaths, we need to get patients off social media and into the clinic in order to benefit financially from the time, effort and money we put into social media”
Use YouTube if you want to educate and share exercise and rehabilitation information on camera; Use TikTok if you’re comfortable on camera and enjoy sharing snippets of information in easily digestible ways. Resist the temptation to copy content across different platforms because it still takes time and energy to do. Once you’ve chosen one platform to master, spend at least 6-12 months focusing on that one space.
Step 3: Understand your content
Content is a huge topic when speaking about social media. Your content will be the key to giving value and helping more people outside of your treatment room.
For simplicity, this article will cover three core concepts of content creation: Content type, Medium and Design. The best thing to do when you’re deciding how to create content is to find a social media profile that you aspire to be like, which shares your values and beliefs, and then get inspiration from that.
Content type
Here are three types of content you should aim to publish:
1. Educational (your expert opinion, advice, daily tips);
2. Entertainment (humour, jokes, funny stories);
3. Selling (promo of your products and services).
A good rule of thumb when creating engaging content is to post 3-5 educational and entertaining pieces to every selling-based piece of content.
You can see from the above list that not everything is about osteopathy; it can be about what you’re doing that day, general health and fitness advice, healthy recipes and even what you’re up to on the weekend.
As long as you share your personality and don’t go against clear AHPRA guidelines (sharing patient reviews, and using words like “best” or “now” when describing your treatments), you’ll be able to know you’re staying out of the AHPRA grey area.
How should you deliver this type of content? The answer is video.
Video will always get you further, quicker. YouTube and TikTok are clearly video-based platforms, but Facebook and Instagram are now prioritising video as well.
Facebook is pushing video-based content to more people. Sprout Social summarised their 2021 study on social media, and concluded “Facebook has been pretty transparent about how video is among the top-performing content on the platform.”
In July 2022, Adam Mosseri, CEO of Instagram, said, “If you look at what people like and consume and view on Instagram, that’s also shifting more and more to video over time.”
Your brand should colour everything you do on your social media. Branding will give you the visual and audible consistency required to make content creation appealing, easy and attractive for potential patients.
Canva! My number one secret weapon I tell all osteopaths about is Canva.com. If you haven’t already discovered Canva, go and have a look. I love Canva because it allows you to create professional, branded products and content for free.
There are plenty of amazing YouTube channels filled with Canva creation tutorials, so grab a coffee, start learning and create some templates.
I highly recommend paying the small subscription for Canva Pro. Still, it’s a hugely powerful tool even if you choose to stay with the free version.
Social media can be used as a powerful tool to help more people outside your treatment room, share your version of osteopathy and create engaged local communities. These work together to bring in new patients from social media over time.
Keep an eye out for part two where we’ll be continuing our deep dive into everything an osteopath needs to find success on social media.
We know that managing your insurance isn’t always at the top of your to-do list. That’s why we’ve redeveloped PolicyHub, our online self-service portal that you can access anytime, designed with you in mind.
We’ve made it simpler to see all your policy documents within the one easy-to-use platform:

• View your payment history
• Download an invoice, payment summary or Certificate of Currency
• Finalise your renewal, and much more!
knowing your data is protected with multi-factor authentication.
for PolicyHub today
Being a clinician can be a bit of a rollercoaster ride. One minute you are up to your eyeballs in work, wondering how you are going to get it all done, and the next you are scrambling around for patients, worrying about how you will pay the bills. These seasonal ups and downs are a natural part of the business, and although quiet days may be occurring more regularly for some, they should be inevitably embraced just as much as the busy days. This article explores ways osteopaths can utilise their quiet time to better themselves in practice and in life.
Sailing into a socioeconomic headwind of inflationary pressure, the rapid and unexpected dampening of economical demand has created a precarious short-term outlook on the future for small business and sole traders. This pressure is evidently creeping its way through osteopathy clinics, with an increasing number of patients unable to afford the out-of-pocket costs for treatment (Duckett et al. 2022).
Coupled with an unprecedented number of graduating osteopaths entering the clinical landscape in 2022, a highly saturated supply market will resultantly see more osteopaths struggle to fill their patient books. This pressure may bring some practitioners to breaking point, at which their passion for the profession will be challenged. This is where the motive must shift away from an immediate financial incentive to one of self-belief and an unrelenting desire to grow. Here are a few tips to help be mentally resilient and remain productive during the quiet days.
Quiet days can create a psychological spiral of overthinking. The issue with this is that when you look at what might happen, you are blinded from thinking past those possibilities. They often say too much analysis leads to paralysis. The key is to recognise and acknowledge the presence of these negative thoughts, allow yourself a few minutes to think about them and then move on. If you
are having trouble recognising these thoughts, start by answering the following questions:
1) Is this thought helpful?
2) What purpose does this thought serve you?
3) How does this thought make you feel?
4) Is this thought realistic?
5) What would you tell a friend who is having the same thought?
This is a simple technique used to help promote mindfulness, whereby you skilfully disengage from your negative thoughts and emotions and view them as a separate body. Practising these simple steps can help identify what you can control rather than worrying about what you can’t.
Face your weaknesses head on. This may require a long, hard look in the mirror, but by doing so you are helping to improve your skill diversity, which can open up a door for treating new types of patients. Read a book, complete a course, update yourself on the latest research, listen to a podcast or reach out to peers in the industry.
Using your quiet time to build your skills can help manage your stress, improve your productivity and enhance your creativity. Eventually, you’ll see this reflect on the outcomes of your patients, which will help improve your retention and overall demand.
It may take time, but in a profession that is rapidly growing, it’s important to grow with it.
Jason Izydorczyk graduated from Victoria University with a BSC (Clinical Sciences) and a Master’s in Health Sciences (Osteopathy) in 2018. During his studies he competed nationally and internationally as a rower and undertook internships at both the British School of Osteopathy, London and SMRC Hospital, India. During his years of practice he broadened his osteopathic skills by undertaking seminars in dry needling, tendon rehabilitation, strength and conditioning, and mental health. He currently practises out of a private practice in Bayside, Melbourne and mentors elite junior rowers.

There are days when work just finds you and productivity happens naturally, but this doesn’t neglect that there are other days that will still feel rotten. In a situation where you are feeling down, an effective way to combat this is to practise gratitude. Start by writing down three things that you are grateful for. This could be the people around you, your skills or your environment. Nurture these feelings. Let them sink in and soak them up. It’s amazing what you notice when you focus on being grateful.
Next, express some gratitude to someone who did something nice. You can do this in a number of ways, but certainly one of the most relevant
Spend your quiet time creating and executing a simple networking strategy:

1) Choose your target audience: This may be the local gym, cafe or community organisation.
2) Plan your approach: Approach each opportunity with a goal. It might be to connect with three new people in your industry or learn something new about a different career path.
3) Follow up: Send a LinkedIn connection request or an email to your new connection.
4) Engage regularly: Send some useful tips or ask for their feedback or opinion. This makes your presence felt by those around you.
and effective ways if by offering to treat them. Not only does this help improve on your own self-gratitude, but it also helps to create a positive relationship with your co-workers. This cycle of positivity will help improve your workplace culture and refine your skills in the process. They always say a little positivity goes a long way.
4. MAKE YOURSELF KNOWN
Network internally and externally. This can help open an avenue of long-term business relationships. You might offer your services to colleagues and receptionists or network with local traders. Engaging with those around you and finding opportunities to assist them helps to improve your visibility and enhances your personal brand.
Don’t be afraid to put yourself out there. The biggest mistake you can make is being too afraid to make one.
5. PLAN YOUR WEEK
Planning is crucial. Spend some time at the start of your week anticipating and planning your quiet days. Start by writing a list of goals and organise them by priority. These can be workrelated or personal.
Next, break these goals down into daily tasks and organise them by priority. For example, your goal might be to be better at treating lower back pain. Your task might be to spend 30 minutes watching videos about acute lower back injuries. This will help improve your focus and accountability. In fact, just 10 minutes of planning can save up to two hours of wasted time and diffused effort (Tracy, 2017).
1. Write out your plan at the start of the week. Plan to do this at the same time every week.
2. Break up your plan into a goal list and corresponding task list.
3. Divide your goal list between work and life.
4. Refer back to this plan at the start and end of your day.
5. Mark each task when completed.
“Please put on your own oxygen mask first before helping others!” I’m sure many of you are familiar with this inflight safety message, but it’s also a useful phrase to remind us about the importance of self-care. If you don’t look after yourself first, you won’t be able to help yourself or others (Importance of self-care planning: COVID-19 mental health and well-being resources, 2020)
Implementing self-care can be as simple as spending some time outside of your clinic for some fresh air and exercise. Taking time to focus on yourself during a quiet day may seem counterproductive, but when gaining more work is always on your mind, the
Positive thoughts can empower us, while negative thoughts can paralyse us.mental strain can be just as exhausting as the physical work.
Furthermore, I’m sure many of you have endorsed the importance of selfcare to your patients. Perhaps it’s worth practising what you preach.
7. DON’T BE AFRAID TO TALK ABOUT THE ‘F-WORD’
Finances can feel uncomfortable to discuss, but they shouldn’t be avoided. According to a 2022 employee financial wellness survey conducted by PWC, 34% of employees say that financial stress/money worries in the past year have had a severe or major impact on their mental health (PWC, 2022).
If you are struggling to meet your financial goals, use your time to plan and budget. If you are still struggling to meet critical costs, let someone know. Get it off your chest.
8. BE PATIENT
During quiet days it’s still important to be productive and not fall into a habit of waiting for the work to come to you. But it’s important to be patient. Even though some of your work may not pay
off for months, being patient can help aid your foresight.
Never lose sight of your long-term goals. If it helps, put your goals in writing and hang them where you can see them everyday. This helps to build motivation and momentum.
Osteopathy is an exciting industry that is clearly growing. But what makes it even more exciting is not how far it has come, but how far it can go. Though the short-term may be riddled with hurdles, controlling your quiet days will help you to stay on course. If you’re passionate about this profession, endeavouring with this passion can ignite possibilities. It may take time, but in a world that values quick and dynamic action, sometimes it’s those who are patient that prosper when the fruit starts to fall.
The information provided in this article is obtained from personal experience and perspective and not intended as formal mental health advice. If you or the person you are concerned about are struggling with mental health, please seek professional assistance.
1. Identify key socioeconomic issues that are affecting the patient intake of osteopaths.
2. Recognise the presence of negative thoughts and how they affect productivity.
3. Apply simple mindset techniques to help combat negative thoughts.
4. Apply planning techniques to construct a quiet day to enhance productivity and motivation.

5. Adopt a simple networking strategy to grow visibility and business.
Blackdoginstitute.org.au. 2020. Importance of self-care planning: COVID-19 mental health and wellbeing resources. [online]: https:// www.blackdoginstitute.org.au/wp-content/ uploads/2020/04/COVID-19_Self-Care-Planning_ Black-Dog-Institute.pdf
Duckett, S., Stobart, A. and Lin, L., 2022. Not so universal - How to reduce out-of-pocket healthcare payments. https://grattan.edu.au/wp-content/ uploads/2022/03/Not-so-universal-how-toreduce-out-of-pocket-healthcare-paymentsGrattan-Report.pdf.
Tracy, B., 2017. Eat That Frog!. Berrett-Koehler Publishers.
2022 PWC Employee Financial Wellness Survey. 2022. [online]: https://www.pwc.com/us/en/ services/consulting/business-transformation/ library/assets/pwc-2022-employee-financialwellness-survey-results.pdf.



• Herring roe is a natural source of specialised pro-resolving mediators, with minimal processing required.
• Relieves inflammation.
• Specialised pro-resolving mediators are used in the body’s natural inflammation resolution process.
• Supports cardiovascular system health.
UC PROMEGA DIFFERENCE
A low-excipient, bioefficient phospholipid form of broad spectrum omega-3 SPMs, including 18-HEPE, 14-HDHA, 17-HDHA and RvE2
What are SPMs?
Specialised pro-resolving mediators (SPMs) are lipid mediators synthesised from omega-3 fatty acids EPA and DHA, that are imperative in the resolution phase of inflammation.
INFLAMMATION RESOLUTION
SPMs actively promote the resolution of inflammation and restoration of homoeostasis. Endogenous SPM production may be impaired by inflammation and ageing
NATURAL SOURCE
Sustainably supplied Norwegian herring roe is a natural source of SPMs, with minimal processing required


ACTIVE INGREDIENTS
DOSE:
Adults: Take 1 capsule one to four times a day, or as professionally prescribed.
Have you wanted to get involved in the supervision of osteopathy students at your practice but didn’t know where to begin? Our Clinical Supervision eLearning modules provide a how-to guide for osteopaths who are excited about mentoring their future colleagues. Upon completion of these modules, clinicians will be recognised as Osteopathy Australia-endorsed clinical supervisors with the skills and capabilities required to facilitate external placement of osteopathy students in their final years of study.
• Unconditional AHPRA registration
• Greater than or equal to five years of clinical experience
• Current First Aid Level 2, Working with Children Check, police check, and professional indemnity insurance
• No conflicts of interest with the student (family, friend, partner, employee)
• Operate from a workplace that has been established for greater than or equal to three years
Clinical placements provide a fantastic opportunity for students and supervising clinicians to grow in knowledge and skills and contribute meaningfully to the profession. Engaging in the supervision of student practitioners can add significant value to you and your workplace by: Providing an opportunity to actively participate in educating and shaping your future colleagues;
Setting an example for students, which makes you an attractive business to work for;
Furthering your own knowledge and gaining transferable skills in supervision and mentoring; and Opening doors for networking and collaboration with universities, educators, and clinicians from other professions.
A clinical supervisor oversees the practise of a student and provides them with opportunities to learn in the workplace. The role of the supervisor is to mentor students in their interactions with patients, record relevant information about their progress, and report back to the relevant university as required.
Step 1: you will work with students to create a list of learning goals to work towards, identify an appropriate method of supervision to be undertaken, and set a meeting and feedback schedule.
Step 2: you will endeavour to assist students in achieving their learning goals and take steps to ensure the student in practicing safely and competently via direct observation and case review.
Step 3: you will provide constructive feedback to students, help to fill gaps in their skills and knowledge, and evaluate their progress (and your own performance) regularly.
Clinical placement provides a practical opportunity to reinforce knowledge and skills learned at university. You should report back to the relevant university at regular intervals during placement to discuss the student’s learning goals, progress, and any issues arising. Students undertaking accredited clinical placements are covered under the university insurance policy. As such, universities are there to support and advise you in the event of an accident, injury, or complaint involving a student.
There are several avenues for students to connect with prospective supervisors. On completion of the Clinical Supervision eLearning Modules, Osteopathy Australia-endorsed clinical supervisors will appear in a database accessible to all final-year students. Students will then contact prospective supervisors with an expression of interest. If willing and able to supervise the student, the supervisor will then meet with the student to discuss the details of supervision and sign a Supervision Agreement to be provided to the relevant university for approval in approximately 6-8 weeks from lodgement. Placement can commence upon approval.
In October 2020, Osteopathy Australia embarked on a mission to produce an online resource for supervisors that would cover everything from the basics to advanced supervision strategies, and most importantly align with the standards and requirements of osteopathy courses across Australia. An Education Committee, comprised of representatives from each university, began meeting monthly to brainstorm ideas for these modules and engage relevant stakeholders with expertise in the fields of healthcare education, mentorship, occupational health and safety, and psychology.
The Committee worked together to determine a list of standardised eligibility
requirements for supervisors and their workplaces across all universities. They also sought expertise from representatives of AHPRA, Guild Insurance, and WorkSafe to ensure eligible workplaces are fully equipped to take on students in a safe and supported manner.
Module 2
The Committee liaised with key experts to identify a list of evidence-based and endorsed methods of supervision based upon student learning goals and capabilities.
Module 3
The Committee consulted literature on various models of clinical reasoning to equip supervisors to deliver constructive feedback and perform effective selfevaluation, both in person and remotely.
Module 4
The Committee worked with specialists in psychology and student mental health to help supervisors identify mental health warning signs and navigate challenges associated with inclusivity, equity and diversity.
Module 5
The Committee referenced the most recent Osteopathy Board ‘Code of conduct for registered health practitioners’ to create guidelines for professionalism in teaching, supervising, and assessing students.
These modules aim to provide clinicians with the tools to become well-rounded, safe, and effective supervisors with vested interests in the advancement of their future colleagues and the profession as a whole. They also provide supervisors with transferable skills that can help them to thrive in their role and mutually benefit from the placement experience.
‘After all, the clinical placement journey should be just as enriching and invaluable for supervisors as it is for students’
The benefits of supervision
‘The transition to treating real-life patients was challenging and overwhelming at times. But through my experience in clinical placement, and with the help of a really supportive supervisor, I was able to overcome a lot of my insecurities and improve my skills in a safe and supported way. My supervisor played a meaningful role in my journey to practice, and I found clinical placement to be an invaluable experience overall.’
– Chanelle Mastronardo (Osteopath – RMIT 2017)

1: Clinical supervision in practice
2: Fundamentals of clinical supervision
Eligibility requirements
Roles and responsibilities
Application process
Insurance and legalities
Initiating and structuring supervision
SMART learning goals
Methods of supervision
Supervision relationships
3: Clinical supervision in practice
Models of clinical reasoning
Self-evaluation
Conflict resolution
Remote supervision
Are you OK?
For more information about getting involved in student clinical placement please contact:
Kylie Spencer RMIT University
kylie.spencer@rmit.edu.au
Sarah McPherson
Southern Cross University
sarah.mcpherson@scu.edu.au
Breanna Wright
Victoria University
Student mental health and wellbeing
Mental health first aid
Inclusivity, equity, diversity
Setting healthy boundaries
Professionalism
5: Code of conduct
Safe and respectful practice
Health and wellbeing
– KylieSpencer, Program Manager, Osteopathy RMIT University
breanna.wright@vu.edu.au
Teaching, supervising and assessing
“After all, the clinical placement journey should be just as enriching and invaluable for supervisors as it is for students”
While acupuncture has been practised for thousands of years, dry needling began gaining traction in the 20th century and now offers an additional technique in the osteopath’s toolbox for treating musculoskeletal conditions. Here, Wael Mahmoud briefly outlines the history of dry needling and some of the conditions it has been used to treat.

The first description in the medical literature of dry needling using an acupuncture needle dates from 1979 when Czech physician Karel Lewit published a paper titled ‘The needle effect in the relief of myofascial pain’ (Lewit, 1979).
Lewit needled several anatomical locations and described how immediate analgesia without hypesthesia was observed in 86.8% of cases when the needle touched the most painful spot. He termed this the ‘needle effect’. He also reported that, of 288 pain sites followed up, permanent relief of tenderness was achieved in 92 needled structures, while relief lasted for several months in 58 structures, several weeks in 63 and several days in 32 (Lewit, 1979). The effectiveness of treatment was related to the intensity of pain produced at the trigger zone and to the precision with which the site of maximal tenderness was located by the needle.
Lewit concluded that dry needling was highly effective for treating chronic myofascial pain. Importantly, he also recognised that it was the acupuncture needle that caused the analgesic effect.
The American Physical Therapy Association (APTA) defines dry needling as ‘a skilled intervention that uses a thin filiform needle to penetrate the skin and stimulate underlying myofascial trigger points, muscular, and connective tissues for the management of neuromusculoskeletal pain and movement impairments’ (APTA, 2013).
The APTA goes on to describe dry needling as a technique that can be
used ‘to treat dysfunctions in skeletal muscle, fascia, and connective tissue, and diminish persistent peripheral nociceptive input, and reduce or restore impairments of body structure and function leading to improved activity and participation’ (APTA, 2013).
Interestingly, APTA’s definition includes needling to connective tissues, not just myofascial trigger points (MTrPs). This makes sense because although the target tissue may be taut bands within muscle tissue, a needle cannot avoid contacting – and therefore affecting – the surrounding extracellular matrix and collagenous, elastic and reticular fibres en route to its target. Indeed, dry needling has been used to treat dense collagen structures such as tendons and ligaments (Krey et al, 2015).
It has been argued that the definition of dry needling should also include the stimulation of neural tissues (Dunning et al, 2014). This is supported by the logical inference that, just as a needle cannot bypass connective tissue en route to an MTrP, it also cannot avoid contact with free nerve endings.
As defined above, dry needling targets MTrPs, taut bands or muscle knots. MTrPs are not new – as far back as 370 BC physicians and scholars were aware of these tender points and their associated referred pain patterns. New theories about, and insights into, MTrPs now enable a better understanding of the role of dry needling and its probable mechanisms (see box, page 20).
The modern definition of an MTrP describes an entity with characteristics
Wael Mahmoud is an osteopath and acupuncturist. He graduated from the British School of Osteopathy in London before migrating to Australia. He has worked in senior academic roles at both RMIT and Victoria University, Melbourne. He is now in private practice at Black Rock Osteopathy, Victoria and runs CPD Health Courses, which provides dry needling education to manual therapists in Australia and the UK. He is the author of Two Hands: The Gamechanger Guide for Manual Therapists, which aims to bridge the gap between undergraduate training and real-world practice as a manual therapist.
not dissimilar from those postulated almost 2,500 years ago, having a relationship with pain, sensitivity and palpable hardening or nodules. An MTrP is now described as a discrete, hyperirritable nodule in a taut band of skeletal muscle, which is palpable and tender during physical examination (Shah et al, 2015).
MTrPs may be active or latent. Active MTrPs are clinically associated with spontaneous pain in specific referred pain patterns. Strong digital pressure over an active MTrP exacerbates the patient’s spontaneous pain and reproduces familiar symptoms (Shah et al, 2015). In contrast, strong digital pressure over a latent MTrP elicits local but not referred pain.
Both latent and active MTrPs can be associated with muscle dysfunction, muscle weakness and a limited range of motion.
It is still not known how MTrPs develop – a number of pathophysiological mechanisms have been proposed, but, as yet, none has been proven. However, their existence is not in question; experienced therapists can palpate them, and the biochemical environment around them differs from adjacent nontrigger point locations (Shah et al, 2008).

Pistoning, fast in-out, dynamic, deep and pistoning with rotation are all synonyms for essentially the same technique developed by Chang-Zern Hong (Hong, 1999). Hong describes the technique as fast-in, fast-out, meaning the needle is inserted quickly into the required location and depth. The eponym ‘Hong fast in-out’ is used to describe both a syringe-based technique, which often carries an injectate of 0.5% lidocaine, and a needling technique using acupuncture needles.
Both techniques use multiple insertions into an MTrP, predetermined by careful palpation, to elicit a local twitch response (LTR) (see box, page 21). Hong suggested that if an LTR and referred pain are elicited before the needling technique is applied, these should be the signs and symptoms elicited during the procedure.
Once needling has been completed and an LTR elicited, the taut band should be less prominent on manual palpation or may have disappeared entirely.
Peter Baldry was perhaps the bestknown advocate of superficial dry needling (SDN). Baldry began his career using the deep dry needling techniques of Karel Lewit but, in a paper published in 2002, he described a patient who presented to his clinic complaining of referred arm pain due to an MTrP in the anterior scalene. The patient’s exquisite tenderness and referred pain disappeared immediately after an acupuncture needle was placed
“The modern definition of an MTrP describes an entity with characteristics not dissimilar from those postulated almost 2,500 years ago, having a relationship with pain, sensitivity and palpable hardening or nodules”
into the muscle very superficially and retained there for no longer than 30 seconds (Baldry, 2002).
Baldry reported similar results using SDN on other muscles, some deeper than the anterior scalene.
The recommended procedure for SDN, as described by Baldry, is to place a 0.3 x 30mm needle to a depth of 5–10mm at an MTrP site and to leave it in situ for approximately 30 seconds. The needle is then withdrawn and pressure applied, equal to that applied when initially palpating and evoking a withdrawal and painful reaction. If pain is still present, the needle is reinserted to the same depth and left for two to three minutes. In weak responders the needle should be rotated in situ for at least three minutes.
Affected muscles should be stretched after treatment but immediate strengthening or loading of the same muscles should be avoided.
The needle winding technique can be an alternative to the fast in-out technique in patients who cannot tolerate the high intensity of needle pistoning.
Evidence suggests that manually inserting and rotating needles every five minutes for a total of 30 minutes leads to intracellular calcium wave propagation and increases in extracellular adenosine triphosphate and adenosine for up to 60 minutes (Perreault et al, 2017).
The accumulation of adenosine activates A1 adenosine receptors and provides a strong antinociceptive effect via inhibition of adenylate cyclase (Bowsher, 1998). The intracellular calcium wave propagation also helps initiate rho kinase-mediated tissue remodelling and blocks pain at the level of the spine by stimulating glycinergic and GABAergic interneurons (Langevin et al, 2001, 2011; Langevin, 2014).
Zhang and colleagues (2012) reported greater activation of C-fibres, distal
The terms ‘myofascial pain’ and ‘trigger point’ were introduced to the medical literature in 1940 when Arthur Steindler published a paper on biomechanical studies and low back pain (Steindler, 1940). At around the same time, Thomas Lewis and Jon Kellgren were investigating referred pain from noxious stimuli in healthy muscle, fascia and tendon tissue. They observed that pain resulting from a hypertonic saline injection was felt distant from the puncture site and could chart zones of referred pain in neighbouring and distant tissue (Kellgren, 1939, 2001).
Kellgren’s work inspired Janet Travell and Seymour Rinzler to further investigate myofascial pain. In a paper published in 1952 they first coined the term ‘myofascial trigger area’ (Travell and Rinzler, 1952), describing it as a small, hypersensitive region from which impulses bombard the central nervous system and give rise to referred pain. They also described the referral patterns emanating from these trigger areas.
Thirty years later, Travell co-authored The Trigger Point Manual: Myofascial Pain and Dysfunction with David Simons (Travell and Simons, 1982). The twovolume text provides a muscle-by-muscle description of how trigger points refer pain to other parts of the body.
superficial and deep mechanoreceptors and stretch receptors with needle rotation compared to other needle movements.
Western medical acupuncture (WMA) works via local, segmental and autonomic pathways.
The local effects of WMA – those that occur around and beneath the needle site – are perhaps the easiest to understand because they are visible when a needle is inserted into the skin. These local effects are the result of a predictable and ordered set of events that occur in the superficial tissues under the skin and involve small myelinated and unmyelinated nerve fibres in the skin (A-Delta fibres) and muscle (C-fibres).
Erythema often occurs around the acupuncture needle during or after the treatment, particularly on the trunk. The erythema reflects the release of vasoactive neuropeptides, including calcitonin gene-related peptide and
histamine. Raised skin may be seen because of fluid extravasation, along with itchiness and a wheal formation as a result of histamine release. Pain may also be experienced on needle insertion due to stimulation of A-Delta fibres.
The local effect mechanism of WMA is based on increasing blood flow and invoking the body’s natural response to injury then subsequent healing.
The segmental effects of dry needling occur at the dorsal horn of the corresponding spinal segment. These can be explained using the example of a degenerative hip joint presentation.
In this presentation, the synovium, capsule and subchondral bone show degenerative changes and inflammation. Noxious stimuli travel via C-fibres from the tissues to the dorsal horn of spinal segments L2/3 and L3/4. Segmental inhibition occurs when a needle is inserted into the hip joint as A-Delta fibres inhibit C-fibre transmission from the damaged tissues. The result is less pain from the hip joint structures. This is known as segmental analgesia.
WMA may also have autonomic effects that are centrally mediated in the spinal cord and brain. Evidence suggests that WMA can be efficacious in treating nausea and vomiting and in providing analgesia. The latter may be linked to
“The needle winding technique can be an alternative to the fast in-out technique in patients who cannot tolerate the high intensity of needle pistoning”
Beta-endorphin and other endogenous opioids (Sun et al, 1993; Kotani et al, 2001).
Dry needling – adverse events
Brady et al (2013) quantified the risk of adverse events (AEs) related to dry needling. In their study, 1,463 mild AEs
were reported from 7,629 treatments with trigger point dry needling. No significant AEs were reported.
Common mild AEs included bruising (7.55%), bleeding (4.65%) and pain during (3.01%) and after (2.19%) treatment. Uncommon AEs were aggravation of symptoms (0.88%), drowsiness (0.26%), headache (0.14%) and nausea (0.13%) while fatigue (0.04%),
altered emotions (0.04%), shaking, itching, claustrophobia and numbness (all 0.01%) were rare.
Another paper supports the low level of AEs reported by the Brady et al paper by Boyce et al (2020). Using a prospective questionnaire study design, data were collected about the incidence of minor and major adverse events during 20,464 Trigger Point Dry Needling (TDN) treatment sessions delivered by 420 physical therapists. The paper concluded that expected minor AEs such as mild bleeding, bruising, and pain during TDN were common, and major AEs were rare.
According to Uzar et al (2018), deep dry needling is an evidence-based treatment technique that is accepted and used by physical therapists for the treatment of musculoskeletal pain. Pneumothorax is a very rare but serious complication associated with acupuncture and dry needling around the thoracic region.

The LTR is characterised by a visible contraction of part of the taut band in the involved muscle on mechanical stimulation with needling or palpation to a sensitive site in the region of an MTrP (Simons and Dexter, 1995).
Hong (1994) was the first to report significant pain reduction immediately after treatment only when an LTR was elicited, with no difference between the use of a lidocaine injection or dry needling in 41 of 58 patients with myofascial pain syndrome (MPS). Long-term outcomes were not measured.
In a study of 39 patients with MPS, dry needling of MTrPs resulted in significant reductions in pain and medication intake versus non-penetrating sham needling, and patients who experienced a LTR had better pain scores at four weeks (Simons and Dexter, 1995).
Rha and colleagues (2011) reported that pain reduction was more significant immediately after the needling procedure in patients who were LTR positive than in those who were LTR negative, regardless of the muscle being treated. Likewise, Bubnov and Wang (2013) found a significant correlation between LTR elicitation and pain relief in 133 subjects with MTrPs, immediately and at 24 hours after needling.
Although there is good evidence for piston-type needling being able to elicit an LTR, there are some possible drawbacks. A higher dosage of needling to MTrPs has been shown to result in overexpression of tumour necrosis factor along the needle pathway and in the serum, increased levels of substance P in the treated muscle and dorsal root ganglion, and reductions in endogenous opioid levels (Rha et al, 2011), all of which are evidence of skeletal muscle damage that may be counterproductive for pain management.
Valdes (2021) states that knowledge and practice in the correct needling direction, needle depth, and palpation of these areas are essential when trained in DN techniques. Lack of training, practitioner negligence, and poor knowledge of surface and underlying anatomy can put a patient at risk of an AE.
It must be noted that an iatrogenic DN induced pneumothorax may take several hours to develop and may not be evident initially. The signs and symptoms can vary as a result of a person’s overall health but include pleuritic chest pain initially, which may be followed by dyspnoea and cough. A chest x-ray is required to diagnose a pneumothorax.
One of the most commonly needled points by acupuncturists and dry needling therapists is LI4, located midway along the second metacarpal, on its radial border. Acupuncturists use LI4 to treat many conditions, including pain in the upper arm, axilla, head and neck, as well as nausea, chest pain, insomnia and febrile disease. Dry needling therapists may needle around LI4 when treating MTrPs in the adductor pollicis and the first dorsal interossei.
According to some Traditional Chinese Medicine practitioners, LI4 is contraindicated during pregnancy, particularly in the first trimester, because of concerns that stimulating it may lead to premature labour. Deadman et al (1998) state that acupuncture has a strong action on promoting labour.
However, White et al (2008) note that acupuncture is often used in China to treat many conditions during the first trimester of pregnancy, without any special precautions. In a trial by Smith et al (2002) involving 593 women with nausea of pregnancy, neither pregnancy outcomes nor the child’s health were affected by acupuncture.

In the absence of clear scientific data to show why acupuncture or dry needling are contraindicated during pregnancy, I personally use both techniques for pregnant women. However, I carefully evaluate the risk/benefit balance for every patient’s specific presenting symptom and circumstance. I avoid strong stimulatory techniques in the first trimester because of the general effects that needling has on the body rather than any consequences related to pregnancy termination. Dry needling therapists should however make their own clinical reasoning decisions based on the available scientific literature.
Many therapists who practise dry needling will sterilise a patient’s skin to reduce the risk of infection. However, in healthy individuals with a normally functioning immune system this precaution is unsupported by the literature.
Hoffman (2001) describes an experiment in which volunteers were injected with Staphylococcus aureus, a bacterium usually present naturally on and under human skin and in the upper respiratory tract. The study found that approximately 7.5 million organisms were required to produce infection at an injection site.
The maximum bacterial population on human skin is about 1,000,000 cm2. Hoffman estimated that inserting an acupuncture needle could push approximately 660 organisms into the skin. If these mixed with a colony of subdermal organisms, the estimate might reach 10,000 organisms – 0.13%
of the estimated number required to cause an infection (Hoffman, 2001).
However, dry needling therapists often use resheathing when practising the fast in-out technique. Once an LTR is achieved, the therapist may wish to elicit further twitches in a different location and will use the same needle again. Using Hoffman’s results it is possible to calculate that the same needle would have to be reinserted 750 times to potentially compromise a patient’s otherwise healthy immune system. That said, resheathing should only be used two or three times in a given treatment region and resheathing is not recommended in patients with a compromised immune system.
In dry needling the acupuncture needle replaces an osteopath’s hands, thumbs and fingers and offers them another tool for treating the musculoskeletal issues they encounter in practice.
Listed below are conditions in which dry needling has been beneficial and the findings from a relevant study that support its use. It is important to remember that dry needling will not work for everyone and that patients rarely present to a therapist in the same way they do in a clinical trial or study.
Wry neck. Dry needling was effective in achieving pain-free neck movements in patients with acute facet joint lock wry neck (Shanmugam and Mathias, 2017). Lumbar radiculopathy. Standard physical therapy and standard physical therapy plus dry needling (experimental group) strategies were evaluated. Pain and disability improvement were more significant in the experimental group, both in post intervention and follow-up (Mahmoudzadeh et al, 2016).
“Using Hoffman’s results it is possible to calculate that the same needle would have to be reinserted 750 times to potentially compromise a patient’s otherwise healthy immune system”In a trial by Smith et al (2002) involving 593 women with nausea of pregnancy, neither pregnancy outcomes nor the child’s health were affected by acupuncture.
Chronic neck pain. Results suggested that trigger point acupuncture may be more effective than standard acupuncture for chronic neck pain in aged patients. This may relate to the effect of the needle on sensitised nociceptors near a trigger point. In contrast, non-trigger point regions, including acupoints, may not have sensitised nociceptors in the same location (Itoh et al, 2007).
Knee pain after arthroplasty. Dry needling was found to be superior to placebo in controlling myofascial pain after knee arthroplasty (Mayoral et al, 2013). This study introduced a novel placebo methodology for dry needling that could be utilised in similar studies to avoid the possible interference of the surgical treatment with the intervention on the MTrPs.
Spasticity after stroke (wrist flexors). A single two-minute session of dry needling reduced wrist flexor spasticity and improved alpha motor neuron excitability in patients with chronic stroke (Fakhari et al, 2017).
Spasticity after stroke (shoulder range of motion). Incorporating deep dry needling into a multimodal
rehabilitation program effectively decreased localised pressure sensitivity and improved shoulder range of motion in individuals who had experienced a stroke (Mendigutia-Gómez et al, 2016). Lateral epicondylitis. Both visual analogue scale measurements and grip strength improved significantly compared to baseline at three, six and 12 months after treatment, despite no significant improvement at one month. Nirschl tennis elbow scores were also significantly improved at six and 12 months. Complete remission was achieved in 14% of patients. Interestingly, 97% of patients complained of increased pain after the procedure, which resolved after two to 14 days (Suzuki et al, 2020). MTrPs in the upper trapezius. Combining dry needling with the muscle energy technique led to the most significant improvement for this presentation (Lari et al, 2016). Ankle instability. The combination of MTrP dry needling within the lateral peroneus muscle and a proprioceptive strengthening exercise program resulted in better pain and function outcomes one
month after therapy for ankle instability (Salom-Moreno et al, 2015). Shoulder injuries. The use of dry needling in elite athletes during a competitive phase provided shortterm pain relief and improved function in shoulder injuries. It may also help to maintain rotator cuff balance and strength, reducing further pain and injury (Osborne and Gatt, 2010).
Fibromyalgia. The first randomised controlled study to evaluate dry needling as an associated treatment for fibromyalgia found that severely affected patients obtained shortterm improvement following weekly dry needling for six weeks (Casanueva et al, 2014).
Greater trochanteric pain syndrome. Brennan et al (2017) found that dry needling was ‘noninferior’ to (i.e. no less beneficial than) cortisone injections. However, dry needling does not have the same AE and risk profile as cortisone. Plantar heel pain. Dry needling resulted in an improvement in pain severity levels and may be an alternative to more invasive treatments (Eftekharsadat et al, 2016).

Subacromial pain syndrome. The pain pressure threshold and range of motion increased significantly at three to four days (but not immediately) after dry needling in the symptomatic shoulder only. There were no significant changes in muscle thickness, resting or contracted, in symptomatic or non-symptomatic shoulders (Koppenhaver et al, 2016).
Thigh muscle strength. In elite soccer players, dry needling showed a significant effect (compared to placebo) on hip flexion that persisted four weeks after treatment. Compared to a non-intervention control, it also showed a significant effect on the maximum force of knee extensors at four weeks (Haser et al, 2017).
Postoperative shoulder pain. Adding a single dry needling treatment to a management protocol designed to assist patients with postoperative shoulder pain may result in faster gains in function (Arias-Buría et al, 2015).

Multifidus activity. A slight increase in the percentage of muscle activity after (versus before) a dry needling procedure was observed in the treated group compared to a control group (Dar and Hicks, 2016).
The best way to incorporate dry needling into osteopathic practice is to do it slowly and deliberately. The first goal is to practise safely, then build confidence and, finally, over time, become more effective.
My advice to an osteopath who has just completed training in dry needling would be to pick three muscles they are confident needling and frequently use in their practice and to only apply dry needling to those muscles in the first month after training. Having gained greater confidence and achieved positive results, they can then add another three muscles. This allows them to control which skills they use and to get better at
them rather than allowing serendipity to determine their success or otherwise.
In my practice, dry needling takes very little of my total treatment time, on average, about seven minutes. I assess patients in precisely the same way I always do, using observation and palpation. I apply dry needling first, then re-assess; that way, I can reduce the hands-on load but more importantly it saves me time, which I spend doing other maintenance treatment that I may not have otherwise had time to perform.
American Physical Therapy Association. (2013) Description of dry needling in clinical practice: an educational resource paper. https://www.mptalliance. com/wp-content/uploads/2015/12/APTA-DN_ ClinicalPracticeEducationalResourcePaper.pdf, last accessed 10 June 2022.
Arias-Buría, J.L., Valero-Alcaide, R., Cleland, J.A., Salom-Moreno, J., Ortega-Santiago, R., Atín-Arratibel, M.A., Fernández-de-las-Peñas, C. (2015) Inclusion of trigger point dry needling in a multimodal physical therapy program for postoperative shoulder pain: a randomized clinical trial. Journal of Manipulative and Physiological Therapeutics 38(3), 179–187. DOI: 10.1016/j.jmpt.2014.11.007
Baldry, P. (2002) Superficial versus deep dry needling. Acupuncture in Medicine 20(2–3), 78–81. DOI: 10.1136/ aim.20.2-3.78
Bowsher, D. (1998) Mechanisms of acupuncture. In: Medical Acupuncture, a Western Scientific Approach Eds: J. Filshie, A. R. White. Elsevier
Boyce, D. et al. (2020) ‘Adverse Events Associated with Therapeutic Dry Needling’, International Journal of Sports Physical Therapy, 15(1), pp. 103–113. Available at: https://discovery.ebsco.com/linkprocessor/ plink?id=efa26adb-b128-3513-9fe3-83065c4e7c5b
Brady, S., McEvoy, J., Dommerholt, J., Doody, C. (2013) Adverse events following trigger point dry needling: a prospective survey of chartered physiotherapists. Journal of Manual Manipulative Therapy 22(3), 134–140. DOI: 0.1179/2042618613Y.0000000044
Brennan, K.L., Allen, B.C., Maldonado, Y.M. (2017) Dry needling versus cortisone injection in the treatment of greater trochanteric pain syndrome: a noninferiority randomized clinical trial. Journal of Orthopaedic and Sports Physical Therapy 47(4), 232–239. DOI: 10.2519/ jospt.2017.6994
Bubnov, R.V., Wang, J. (2013) Clinical comparative study for ultrasound-guided trigger-point needling for myofascial pain. Medical Acupuncture 25(6), 437–443. DOI: 10.1089/acu.2013.0973
Casanueva, B., Rivas, P., Rodero, B., Quintial, C., Llorca, J., González-Gay, M.A. (2014) Short-term improvement following dry needle stimulation of tender points in fibromyalgia. Rheumatology International 34(6), 861–866. DOI: 10.1007/s00296-013-2759-3
Dar, G., Hicks, G.E. (2016) The immediate effect of dry needling on multifidus muscles’ function in healthy individuals. Journal of Back and Musculoskeletal Rehabilitation 29(2), 273–278. DOI: 10.3233/BMR150624
Deadman, P., Al-Khafaji, M., Baker, K. (1998) A Manual of Acupuncture. Journal of Chinese Medicine
Dunning, J., Butts, R., Mourad, F., Young, I., Flannagan, S., Perreault, T. (2014) Dry needling: a literature review with implications for clinical practice guidelines. Physical Therapy Reviews 19(4), 252–265. DOI: 10.1179 /108331913X13844245102034
Eftekharsadat, B., Babaei-Ghazani, A., Zeinolabedinzadeh, V. (2016) Dry needling in patients with chronic heel pain due to plantar fasciitis: a singleblinded randomized clinical trial. Medical Journal of the Islamic Republic of Iran 30, 401.
Fakhari, Z., Ansari, N.N., Naghdi, S., Mansouri, K., Radinmehr, H. (2017) A single group, pretest-posttest clinical trial for the effects of dry needling on wrist flexors spasticity after stroke. NeuroRehabilitation 40(3), 325–336. DOI: 10.3233/NRE-161420
Haser, C., Stöggl, T., Kriner, M., Mikoleit, J., Wolfahrt, B., Scherr, J., Halle, M., Pfab, F. (2017) Effect of dry needling on thigh muscle strength and hip flexion in elite soccer players. Medicine and Science in Sports and Exercise 49(2), 378–383. DOI: 10.1249/ MSS.0000000000001111
Hoffman, P. (2001) Skin disinfection and acupuncture. Acupuncture in Medicine 19(2), 112–116. DOI: 10.1136/ aim.19.2.112
Hong, C-Z. (1994) Lidocaine injection versus dry needling to myofascial trigger point. American Journal of Physical Medicine & Rehabilitation 73(4), 256–263. DOI: 10.1097/00002060-199407000-00006
Hong, C-Z. (1999) Current research on myofascial trigger points–pathophysiological studies. Journal of Musculoskeletal Pain 7(1–2), 121–129. DOI: 10.1300/ J094v07n01_12
Itoh, K., Katsumi, Y., Hirota, S., Kitakoji, H. (2007) Randomised trial of trigger point acupuncture compared with other acupuncture for treatment of chronic neck pain. Complementary Therapies in Medicine 15(3), 172–179. DOI: 10.1016/j.ctim.2006.05.003
Kellgren, J. (1939) On the distribution of pain arising from deep somatic structures with charts of segmental pain areas. Clinical Science 4, 35 Kellgren, J.H. (2001) Observations on referred pain arising from muscle. In: Classic Papers in Rheumatology Eds: P. Dieppe, F.A. Wollheim, R. Schumacher. CRC Press. pp 352–353
Koppenhaver, S., Embry, R., Ciccarello, J., Waltrip, J., Pike, R., Walker, M., Fernández-de-Las-Peñas, C. et al. (2016) Effects of dry needling to the symptomatic versus control shoulder in patients with unilateral subacromial pain syndrome. Manual Therapy 26, 62–69. DOI: 10.1016/j.math.2016.07.009
Kotani, N., Hashimoto, H., Sato, Y., Sessler, D.I., Yoshioka, H., Kitayama, M., Yasuda, T. and Matsuki, A. (2001). Preoperative intradermal acupuncture reduces postoperative pain, nausea and vomiting, analgesic requirement, and sympathoadrenal responses. Anesthesiology, [online] 95(2), pp.349–356. doi:10.1097/00000542-200108000-00015.
Krey, D., Borchers, J., McCamey, K. (2015) Tendon needling for treatment of tendinopathy: a systematic review. The Physician and Sportsmedicine 43(1), 80–86. DOI: 10.1080/00913847.2015.1004296
Langevin, H.M. (2014) Acupuncture, connective tissue, and peripheral sensory modulation. Critical Reviews in Eukaryotic Gene Expression 24(3), 249–253. DOI: 10.1615/critreveukaryotgeneexpr.2014008284
Langevin, H.M., Bouffard, N.A., Fox, J.R., Palmer, B.M., Wu, J., Iatridis, J.C., Barnes, W.D. et al. (2011) Fibroblast cytoskeletal remodeling contributes to connective tissue tension. Journal of Cellular Physiology 226(5), 1166–1175. DOI: 10.1002/jcp.22442
Langevin, H.M., Churchill, D.L., Cipolla, M.J. (2001) Mechanical signaling through connective tissue: a mechanism for the therapeutic effect of acupuncture. FASEB Journal 15(12), 2275–2282. DOI: 10.1096/fj.010015hyp
Lari, A.Y., Okhovatian, F., Naimi, S.S., Baghban, A.A. (2016) The effect of the combination of dry needling and MET on latent trigger point upper trapezius in females. Manual Therapy 21, 204–209. DOI: 10.1016/j. math.2015.08.004
Lewit, K. (1979) The needle effect in the relief of myofascial pain. Pain 6(1), 83-90. DOI: 10.1016/03043959(79)90142-8
Mahmoudzadeh, A., Rezaeian, Z.S., Karimi, A., Dommerholt, J. (2016) The effect of dry needling on the radiating pain in subjects with discogenic low-back pain: a randomized control trial. Journal of Research in Medical Sciences 21, 86. DOI: 10.4103/17351995.192502
Mayoral, O., Salvat, I., Martín, M.T., Martín, S., Santiago, J., Cotarelo, J., Rodríguez, C. (2013) Efficacy of myofascial trigger point dry needling in the prevention of pain after total knee arthroplasty: a randomized, double-blinded, placebo-controlled trial. EvidenceBased Complementary and Alternative Medicine 2013, 694941. DOI: 10.1155/2013/694941
Mendigutia-Gómez, A., Martín-Hernández, C., Salom-Moreno, J., Fernández-de-Las-Peñas, C. (2016) Effect of dry needling on spasticity, shoulder range of motion, and pressure pain sensitivity in patients with stroke: a crossover study. Journal of Manipulative and Physiological Therapeutics 39(5), 348–358. DOI: 10.1016/j.jmpt.2016.04.006
Osborne, N.J., Gatt, I.T. (2010) Management of shoulder injuries using dry needling in elite volleyball players. Acupuncture in Medicine 28(1), 42–45. DOI: 10.1136/aim.2009.001560
Perreault, T., Dunning, J., Butts, R. (2017) The local twitch response during trigger point dry needling: is it necessary for successful outcomes? Journal of Bodywork and Movement Therapies 21(4), 940–947. DOI: 10.1016/j.jbmt.2017.03.008
Rha, D-W., Shin, J.C., Kim, Y-K., Jung, J.H., Kim, Y.U., Lee, C.C. (2011) Detecting local twitch responses of myofascial trigger points in the lower-back muscles using ultrasonography. Archives of Physical Medicine and Rehabilitation 92(10), 1576–1580. DOI: 10.1016/j. apmr.2011.05.005
Salom-Moreno, J., Ayuso-Casado, B., Tamaral-Costa, B., Sánchez-Milá, Z., Fernández-de-Las-Peñas, C., Alburquerque-Sendín, F. (2015) Trigger point dry needling and proprioceptive exercises for the management of chronic ankle instability: a randomized clinical trial. Evidence-Based Complementary and Alternative Medicine 2015, 790209. DOI: 10.1155/2015/790209
Shah, J.P., Danoff, J.V., Desai, M.J., Parikh, S., Nakamura, L.Y., Phillips, T.M., Gerber, L.H. (2008) Biochemicals associated with pain and inflammation are elevated in sites near to and remote from active myofascial trigger points. Archives of Physical Medicine and Rehabilitation 89(1), 16–23. DOI: 10.1016/j. apmr.2007.10.018
Shah, J.P., Thaker, N., Heimur, J., Aredo, J.V., Sikdar, S., Gerber, L. (2015) Myofascial trigger points then and now: a historical and scientific perspective. PM & R 7(7), 746–761. DOI: 10.1016/j. pmrj.2015.01.024
Shanmugam, S., Mathias, L. (2017) Immediate effects of paraspinal dry needling in patients with acute facet joint lock induced wry neck. Journal of Clinical and Diagnostic Research 11(6), YM01–YM03. DOI: 10.7860/ JCDR/2017/26407.10079
Simons, D.G., Dexter, J.R. (1995) Comparison of local twitch responses elicited by palpitation and needling of myofascial trigger points. Journal of Musculoskeletal Pain 3(1), 49–61. DOI: 10.1300/ J094v03n01_05
Smith, C., Crowther, C. and Beilby, J. (2002). Acupuncture To Treat Nausea and Vomiting in Early Pregnancy: A Randomized Controlled Trial. Birth, 29(1), pp.1–9. doi:10.1046/j.1523-536x.2002.00149.x.
Steindler, A. (1940) The interpretation of sciatic radiation and the syndrome of low back pain.
Journal of Bone and Joint Surgery 22, 28–34
Sun, B. and Luo, M., (1993) Shandong science and technology press. Jinan, China, pp.284-293
Suzuki, T., Iwamoto, T., Matsumura, N., Nakamura, M., Matsumoto, M., Sato, K. (2020) Percutaneous tendon needling without ultrasonography for lateral epicondylitis. Keio Journal of Medicine 69(2), 37–42. DOI: 10.2302/kjm.2019-0004-OA
Travell, J., Rinzler, S.H. (1952) The myofascial genesis of pain. Postgraduate Medicine 11(5), 425–434. DOI: 10.1080/00325481.1952.11694280
Travell, J., Simons, D. (1982) Myofascial Pain and Dysfunction. The Trigger Point Manual, 1st edn. Williams & Wilkins
Uzar, T., Turkmen, I., Menekse, E.B., Dirican, A., Ekaterina, P. and Ozkaya, S. (2018). A case with iatrogenic pneumothorax due to deep dry needling. Radiology Case Reports, 13(6), pp.1246–1248. doi:10.1016/j.radcr.2018.08.019.
Valdes, V.R. (2021) ‘Dry Needling in Physical Therapy Practice: Adverse Events Part 2: Serious Adverse Events’, Orthopaedic Physical Therapy Practice, 33(2), pp. 96–100. Available at: https://discovery.ebsco.com/ linkprocessor/plink?id=0a2957d8-d93f-3fe4-b5012c57656a0e09
White, A., Cummings, M., Filshie, J. (2008) An Introduction to Western Medical Acupuncture. Churchill Livingstone
Zhang, Z-J., Wang, X-M., McAlonan, G.M. (2012) Neural acupuncture unit: a new concept for interpreting effects and mechanisms of acupuncture. Evidence-Based Complementary and Alternative Medicine 2012, 1–23. DOI: 10.1155/2012/429412
 Author Rowland Benjamin Reviewer Toby Barker
Author Rowland Benjamin Reviewer Toby Barker
A shift towards an emphasis on selfmanagement strategies has been driven by both evidence and the COVID-19 pandemic, which hindered our ability as osteopaths to use manual therapy as our primary treatment modality. In Rowland Benjamin’s recent publication Massage Yourself: Self-massage of muscles, tendons and ligaments he provides a comprehensive overview of how a broad variety of soft tissue techniques can be performed on oneself at home.
My first impressions of this book were that it explores the treatment of an extensive range of soft tissues and a considerable effort has been made by the author to put this together. I felt that although this book is designed for use by patients/the general public, at times this could become somewhat challenging; the use of very specific, often ‘not common knowledge’, muscle groups or tissues without extensive detail on how the reader might determine which to self-massage may make this book more difficult for some to use without the guidance of a practitioner. Likewise, some information provided in the section
regarding spinal curves and posture may not be diagnostically useful or easily contextualised for the general public without guidance. I therefore felt that this could in fact be a more useful tool for clinicians to refer to when providing self-management strategies to patients, for which the author has created a useful resource. Benjamin does however acknowledge this in his ‘Theory and Practice’ chapter.
Benjamin provides a good level of anatomical knowledge, detailed diagrams and clear instruction throughout the book. He begins with an introduction to the theory and practice of massage techniques, which although detailed, I felt could have benefited from referencing in order to produce a more academic text.
Overall, this book provides the reader with a thorough guide through self-massage techniques; although lacking some depth of academic rigour and presented in a somewhat ‘home-made’ style, I feel this serves its purpose as a reference resource for practitioners and patients.
Rowland Benjamin has worked as an osteopath for 37 years and in the health and massage field for over 40 years. He established yoga schools in Australia and the UK and worked with yoga and massage for several years before training as an osteopath. He set up his first osteopathic practice in Sydney, Australia before moving to Liverpool, UK for work and further studies in osteopathy.
Title: Massage Yourself: Self-massage of muscles, tendons and ligaments
Author: Rowland Benjamin
Editor: Rowland Benjamin
Illustrated by: Rowland Benjamin
Publisher: Rowland Benjamin, 2022
ISBN: 0958111928, 9780958111928
“My first impressions of this book were that it explores the treatment of an extensive range of soft tissues and a considerable effort has been made by the author to put this together”
Following five years of research and development and a further two years of real-time trials in an osteopathic clinical setting, our DrRest experts have created a mattress that health professionals can confidently recommend to patients. A sleep system that complements and supports the care that osteopathic practitioners provide.


Learn more about becoming a DrRest referrer or partner at drrest.com.au/join
ENDORSED BY*
Introducing DrRest, the most innovative sleep system designed by health experts for spinal alignment and quality rest.
At the recent event launch of DrRest, acclaimed journalist Jacqui Felgate hosted a panel of the leading health experts behind this innovative new sleep system. Through their conversation, they share their understanding of sleep in supporting clinical outcomes for your patients.

JF: The first thing that struck me when looking at what you created with DrRest were the before-and-after case studies of patients lying on your mattress compared to another and your ‘aha’ moment as a team. Tell me about that.
GM: It really was an ‘aha’ moment. Our expectations were, ‘Okay, this is what we’re hoping to achieve,’ but seeing spinal alignment in real-time and on various patients that had different ailments was a wow moment. It was an emotional moment because we had uncovered a design with this unique shoulder zone and Technogel© technology to have such a positive impact on patients’ health.
GQ: When George showed us the results from his 150 trials, I was thinking, ‘Well, this is not photoshopped, this is the real deal.’ We often see these types of spinal alignment images with mattresses but they’re not real.
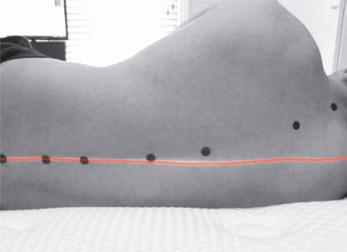
NA: Seeing the spinal alignment, comfort and results of the DrRest trials was an impressive outcome that I could immediately see would benefit my patient cohort of sleep disorders.
JF: Gerald, as a surgeon, how significant are sleep difficulties for your patients preand post-surgery?
GQ: One of the key differentiators of whether someone needs surgery or has pain severe enough for surgery is whether they have pain at night keeping them awake and unable to sleep. With that clinical understanding, we were really interested in whether a mattress itself can promote sleep comfort such that patients don’t have that all-encompassing 24/7 pain impacting their quality of life.
JF: That’s what you want! And George, your patients, what do you see?
GM: So I have a similar cohort, nonsurgically based, but they’re musculoskeletal, lower back, neck pain and hip and shoulder pain. Often they’re waking up with back pain even after treatment. I began to realise their mattress was contributing to the problem.
I think this is why we found DrRest so special. It’s one thing to have prescriptive mattresses made for an individual and another thing to have a mattress that actually customises to each individual to support pain reduction and functionality.

GM: We use the term spinal alignment to take the pressure off your lumbar, thoracic, and cervical spine. We’ve tested out creating this pressure relief by looking at interface pressure, which is the pressure that the mattress exerts on you when you lay on it. So, laying on a mattress it feels plush, firm or medium – that’s the interface pressure.

So, to have spinal alignment with really low interface pressure, that’s a unique attribute of DrRest.
JF: Nick, what considerations did you take into account as part of the design process to create this adaptable sleep surface?
NA: The main consideration was something that was going to be comfortable. I see a lot of patients with neck pain, shoulder pain and hip pain and that results in fragmented sleep, with less of the important sleep such as slow-wave sleep. The other part to take into consideration was my cohort of patients with sleep apnoea and snoring. A comfortable mattress that allows people to sleep on their side while using a positional aid for supine sleep disorder breathing was important.
GQ: We also considered allergies and ensured all materials and components in the mattress are hypoallergenic along with thermal properties and how they might influence sleep. For example, if you sleep on a non-breathable mattress or cover and the body gets too hot, it will stimulate the nervous system to wake you up during the night. The Technogel© component is actually an inherent cooling material that may decrease body temperature by up to three degrees. Where the Technogel© is located in the DrRest mattress, this is where the core part of your body lies.
NA: The University of Basel and the University of Torino actually did a study with Technogel©. They looked at changes in mattress, body surface and core body temperature versus a foam mattress and
showed there was a significant decrease in core body and back surface temperature during sleep with the Technogel© mattress, resulting in a significant increase in slow wave sleep.
GQ: For me, one of the key points of difference of the mattress itself is where the Technogel© is used – in the shoulder zone, which really is a unique part of DrRest. Technogel© is the gel we use in operative surgery for pressure care to not cause nerve damage or pressure sores after prolonged periods of undergoing surgery that can last anywhere between 2-3 hours. It’s what protects the bony prominences and pressure areas. Not only that but Technogel© keeps things stable and firm and provides support as we’re operating. Thanks to its 3D conformity, it moulds itself to each individual patient’s physical structure and evenly distributes and reduces pressure over the entire contact surface, improving blood circulation.
The specifically designed Technogel© for the DrRest mattress allows the shoulders to sink in and the spine to align, and responds in that the more weight or pressure you apply to it, the liquid (which acts as a solid) generates this unique hydraulic response.

JF: When people do sleep in the wrong position or with pain, what impact does
that have on their quality of sleep and their quality of life?
NA: Sleep helps us to restore and rejuvenate. We secrete important hormones such as growth hormone. Our cells repair. We have muscle growth and protein synthesis, and it’s important for our immune function. So, getting the right amount and type of sleep is incredibly important.
GM: It’s interesting hearing Nick say that, because when I see patients with torn muscles or ligaments from trauma who don’t require surgery but are on the cusp and they’re not sleeping, it means they’re not healing correctly because they’re not producing the appropriate restorative hormones.
JF: What did you each notice when you slept on a DrRest mattress the first time?
GM: It was unusual but enlightening at the same time because I genuinely felt my spine was relaxing. It was interesting and I couldn’t feel any pressure nor that reaction force; the sensation of the springs pushing up. It was amazing as it was what we set out to achieve, but it was nice to actually experience it.
GQ: It was an aha moment for me. I came quite late to side sleeping and sleeping on my side on a firm mattress in the past. I would wake up with aches and pains. I am biased, but sleeping on a DrRest mattress, I just thought this is ticking all the boxes in giving me the optimal rest and recovery.
NA: I’m a side sleeper, so when I slept on the mattress I thought it was fantastic. On my current mattress I often wake up with a sore shoulder or a sore neck. My pillow isn’t right – I keep on adjusting it. So, when I slept on a DrRest, I said, ‘When are they available!’ as I think it will definitely help improve my sleep.
DrRest is endorsed by Osteopathy Australia and is available to allied health professionals now. Visit info@drrest.com.au to learn more.
“I think this is why we found DrRest so special – it’s one thing to have prescriptive mattresses made for an individual and another thing to have a mattress that actually customises to each individual to support pain reduction and functionality”OPTIMAL PRESSURE RELIEF To neck, shoulders, spine, lower back and hips. SUPPORT FOR ALL BODY TYPES Unique support system with a self-levelling design that adapts to each body to minimise hammocking or side bending of the spine. LOWER BODY ZONE Comfort construction-quilted bottom zones. SHOULDER ZONE The DrRest shoulder zone has been expertly designed with Technogel©, the world’s only three-dimensional biocompatible comfort layer. HEAD ZONE Comfort construction – quilted top.
2022 has been a big year for industrial relations in Australia, with a number of significant changes (and proposed changes) on the horizon. The most extensive potential changes originate from the recent introduction of the Fair Work Legislation Amendment (Secure Job Better Pay) Bill 2022 into parliament, which if passed will affect the enterprise bargaining process, job security, and pay equity in the workplace.
Paid Family and Domestic Violence leave will also be introduced into the National Employment Standards (NES), and there will be an increase to Services Australia’s Parental Leave Pay entitlement to 26 weeks announced in the most recent Federal Budget.
This can be a lot to take in, so the HR Advisory Service has prepared an article to flag and discuss these coming changes.
Note: This bill has only been introduced into Parliament at this stage, so we will note that the following changes are not final just yet, but they have the most far-reaching effects if passed. These include:
Contracts and industrial instruments that prevent employees from discussing their remuneration with others will no longer be permitted. The aim is to promote gender equity within the workplace, and it will now be a workplace right for employees to ask their colleagues about their rates of pay (who are also entitled to refuse to answer).
Employees already have an ability to make a request for flexible working arrangements under certain circumstances. New provisions include requiring employers to genuinely try and reach agreement, including suggesting alternative options, and allow employees to contest a refusal with the Fair Work Commission – who will have powers that include require an employer to grant the request.
There will be a limitation to fixed term contracts (where they end
at a pre-determined time period). Unless they meet certain criteria, the terms will not be valid if they extend for a period of more than two years, or it may be renewed so they’re employed for more than two years, or it is a new contract following on from a previous fixedterm contract that means together they extend for more than two years.
Currently the cap on small claims for underpayment is $20,000. This bill will look to increase the cap up to $100,000.
One of the more substantial changes, it promises to shake up multi-employer bargaining, and among other changes, now also permit employees (through employee bargaining representatives) to require multiple employers to enter bargaining process, so long as there are clearly identifiable common interests between the employers, and also add new employers to existing agreements.
It will now be an offence to advertise a role at a pay rate that is less than what is proscribed in the Fair Work Act 2009 or an industrial instrument – an EBA or modern award.
Protections against sexual harassment will be expanded. Instead of just covering sexual harassment between two employees, it will also extend to cover sexual harassment that occurs in connection with a worker, a prospective worker, or a person conducting a business or undertaking. This means it will include third parties like a customer or client, or any member of the general public. Three forms of discrimination will be added to existing general protections provisions. These will cover breastfeeding, gender identity, and intersex status.
Currently, the NES provides for five days of unpaid family and domestic violence leave.
The recently passed Fair Work Amendment (Paid Family and Domestic Violence Leave) Bill 2022 will now provide employees with 10 days of paid family and domestic violence leave. This will be paid at the ordinary rate of pay they would have otherwise received had they worked, and casual employees will also be entitled to this paid leave. This leave entitlement will reset each year, rather than accruing progressively.
The same evidence requirements for the unpaid leave will apply, and employers should take reasonable steps to ensure information is kept confidential.
It will take effect from 1 February 2023 for most businesses, but small businesses (with 14 employees or less) will be given a grace period of six months.

The recent budget announced an intention to increase the length of the Parental Leave Scheme through Services Australia (Centrelink) to 26 weeks.
The current entitlement is 20 weeks (18 weeks parental leave PLP and two weeks Dad and Partner Pay).
From 1 July 2023, this will be combined into a single 20-week payment, and starting from 1 July 2024, PLP will then increase by two weeks per year until it reaches 26 weeks on 1 July 2026.
Other changes include allowing for gender neutral claiming so either parent may access to claim the PLP. Both parents will also be allowed to access it at the same time, and it may be taken in smaller blocks (as little as one day) while working in between.
There are many different changes coming to our industrial relations landscape, and it is important for employers to remain informed so they can be prepared as best as possible. The HR Advisory Service will keep members informed about the status of these new IR reforms and reach out as they begin to each take effect. If at any
time you are unsure of your obligations towards your employees, please feel free to contact the HR Advisory Service for more information.
This document does not constitute human resource or legal advice and should not be relied upon as such. It is intended only to provide a summary and general overview on matters of interest and it is not intended to be comprehensive. You should contact the Osteopathy Australia HR Service or seek professional advice before acting or relying on any of the content.
© Wentworth Advantage Pty Ltd 2022
So, you’ve just accepted a new job. Congratulations! Now it’s time to sign the employment contract that was emailed to you a few days ago. This part is easy, right? Not always!
Understanding the terms of an employment contract can be difficult, with many employment contracts containing terminology and wording that is legalistic and highly formal. Further, while an employment contract should contain terms and conditions that suit employer and employee, many employees struggle when it comes to negotiating a favourable employment contract and this can lead to the employment relationship getting off on the wrong foot.
This resource has been designed to explain everything you need to know about your employment contract, including tips about how to get terms and conditions built into your employment contract that suit you.
An employment contract is an agreement that establishes the terms and conditions of an employment relationship between employer and employee. It’s important to note that a contract can be either written or verbal. Despite this, it is always strongly recommended that the contract is in writing. If you commence a new job and your employer does not provide you with a written contract, ask for one.
Every employment contract must be compliant with the National Employment Standards, and any applicable modern award or other industrial instrument.
Unincorporated businesses in Western Australia must ensure their employment contracts are compliant with the Minimum Conditions of Employment Act 1993, and any applicable State Award.

Yes. An employment contract can be permanent (full time/part time), casual or for a fixed or maximum term.
While an employment contract needs to be comprehensive (to ensure the best interests of both employer and employee are protected), it shouldn’t be overwhelming.
This is a fine line that, if crossed, can leave employees feeling confused, apprehensive, or even intimidated. Some of the more critical terms included in an employment contract include: Commencement date (and finish date if contract is for a fixed duration); Employment status (i.e. full-time, part-time, casual, etc.);
Hours of work (e.g., 38 hours per week); Remuneration structure (e.g., hourly rate, salary, etc.).
While the above terms are obvious, there are other common terms and conditions that aren’t as familiar to many employees entering into an employment contract. These include:
It is becoming increasingly common for organisations to provide a “restraint clause” in the employment contract. In essence, a restraint clause is designed to prevent former employees from working for and potentially sharing confidential and critical information with a direct competitor. While every business has a right to protect its interests, restraint clauses are not automatically enforceable. To be enforced, a business would essentially need to take legal action against the former employee.
A probationary period is designed to allow both employer and employee to assess whether the employment relationship is right for them. Typically a probationary period will be between
three to six months, and during that time the employer should be providing regular training and assistance to ensure you are performing at the level required.
The notice provisions in an employment contract dictate how much notice either party must provide in the event of the employment relationship being terminated (either by the employee or employer). Note, the notice period for both parties should be the same. For example, if an employee is expected to provide a month’s notice, the employer should also be expected to provide the same. If there is inconsistency in the notice periods for employer and employee, the clause could be considered unfair. At the same time, the notice period should not be excessive (e.g. six months for a junior employee) or too short (e.g. inconsistent with the minimum notice periods provided in the relevant industrial legislation).
Generally, an intellectual property clause will stipulate that any ideas, strategies, treatments, etc. that are created by an employee while employed are the property of the employer. This clause is now standard in most employment contracts and shouldn’t be feared.
No. An employment contract can’t contain terms that are illegal – either from a criminal or employment law perspective. For example, and as mentioned previously, the notice period in an employment contract can’t be less than the minimum notice periods provided for in the relevant legislation. Similarly, an employment contract can’t provide remuneration that is less than the minimum wage set by the Fair Work Commission (or Western Australian Industrial Relations Commission for unincorporated businesses in WA) each year.
Only by agreement between employee and employer. This agreement should also be in writing.
Employment contracts can sometimes be mistaken with independent contractor agreements. These types of agreements are essentially business-to-business and therefore outside the scope of employment legislation. These agreements are between “principal” and “contractor”, and their terms are highly negotiable.
If you are an inexperienced worker (such as a new graduate), you should not be engaged as an independent contractor for a variety of reasons. Namely, an independent contractor is running their own business and therefore is responsible for managing taxation, insurance and other business matters. Further, a contractor is responsible for their work and should not receive any coaching or training from the principal (as this is indicative of employment), and this is hugely problematic for inexperienced workers who require a higher level of support.
If you have been approached as a new graduate about becoming an independent contractor, contact the HR Service for advice.
Too often, employees (particularly new graduates) will sign the first employment contract that comes their way just to get a foot in the door. While this approach is very much understandable, it is also risky for several reasons.
First, they may not know what they are signing up for, and there could be requirements of the contract that are inconsistent with what was promised during the recruitment process.
Second, they may be selling themselves short or preventing themselves from enjoying the flexibility that so many workplaces offer in the 21st century.
So how does one successfully negotiate a desirable employment contract, particularly without the “leverage” of being a more seasoned or experienced employee?
The best place to start is to know exactly where you stand. Find out whether an award applies to your employment and familiarise yourself with the terms of that award. Given an employment contract cannot provide terms that are less favourable than those contained in a
relevant award, you can use the award as a base for your negotiations.
Knowing what’s happening in the market is vital to ensure you get the best possible outcome in your employment contract. This may be easier said than done, but try speaking to others you know in the industry (e.g. other new grads you met at university) about their employment situation and the terms and conditions they receive. Another good way to research the market is to check job boards for similar positions. It is becoming more common for organisations to advertise specific elements of a role in the job ad as a means of attracting applicants, so information is becoming more accessible in this regard.
Don’t be afraid to seek professional advice if you are unsure about any of the terms of the contract. We can conduct a full review of your contract to answer any questions or concerns you might have.
You wouldn’t have applied for the job if you didn’t think you could do it, so carry that same confidence into discussions with your new employer about the employment contract. Provided you have already been formally offered the job, and you have accepted that offer, your employer cannot rescind the offer because you are trying to negotiate better terms and conditions. This would be the same as terminating your employment and carries risks for the employer.
For more information and support, please contact the friendly team at Osteopathy Australia HR Service. Email hrhotline@osteopathy.org.au, or phone 1300 143 602.
This document does not constitute human resource or legal advice and should not be relied upon as such. It is intended only to provide a summary and general overview on matters of interest and it is not intended to be comprehensive. You should contact the Osteopathy Australia HR Service or seek professional advice before acting or relying on any of the content.
© Wentworth Advantage Pty Ltd 2022

Australia has a new Clinical Care Standard for low back pain (LBP). This condition affects one in six Australians and is a leading cause of disability, lost work productivity, and early retirement. Developed by the Australian Commission on Safety and Quality in Health Care, the Low Back Pain Clinical Care Standard guides health professionals in best practice for managing LBP and recommends a non-pharmacological approach as the first-line treatment with less reliance on pain medications and imaging.
The purpose of easing pain is to restore functionality through movement to promote recovery. Heat Wraps encourage this by keeping patients moving and reducing the pain barrier to activity with continuous low-level heat.



A heat wrap is a specific form of continuous low-level heat applied within a lightweight elasticised wrap that is flexible to facilitate movement and activity and promote recovery from low back pain.

Heat wraps differ from other heat products, such as wheat bags, heat creams, heat packs, and hot water bottles, as they are designed to produce a continuous low-level heat above 40 degrees Celsius for extended periods of up to 12 hours. Continuous levellow heat wraps are the most researched and evidence-based form of heat delivery.


Heat wraps contain eco-friendly ingredients, iron powder, salt, charcoal, and mineral vermiculite. When exposed to air, these contents oxidise the iron powder to release heat, known as an exothermic reaction. This activity is a “rusting process” accelerated by salt and evenly dispersed by mineral vermiculite.


The main advantage of a heat wrap is that it enables you to stay active due to


its lightweight and flexible design. This assists in promoting and facilitating low back pain recovery. The convenience of repositioning when required without disrupting heat production is a further advantage of heat wraps.
Heat wraps deliver a continuous low level of heat for up to 12 hours which differentiates them from other heat applications such as wheat bags, which reach high temperatures for a shorter duration and require constant reheating. Wheat bags and heat packs are
not as practical, requiring patients to sit or be immobilised, contrary to the evidence recommending staying active in Australia’s low back pain clinical care standard.
Heat wraps combine evidence-based continuous low-level heat and movement to promote recovery from low back pain as recommended in Low back pain clinical care standard 2022.
Free clinic sample packs for osteopaths: flexeze.com.au/pages/professional-hub



Hit the snooze button in the morning because the admin is already sorted. Grab a coffee between patients because your notes are done. Leave the practice in time to make your dinner plans. This is what life looks like when you use Cliniko.
Start saving time with your 90-day free trial cliniko.com/oa-member