INSIDE:
DOMESTIC AND FAMILY VIOLENCE
How osteopaths can support patients
RESEARCH
Association update
EMPLOYEE RETENTION
Your checklist to maintain a stable and engaged workforce


DOMESTIC AND FAMILY VIOLENCE
How osteopaths can support patients
RESEARCH
Association update
EMPLOYEE RETENTION
Your checklist to maintain a stable and engaged workforce

EXPLORING A COMPREHENSIVE TREATMENT APPROACH



As we near the end of 2024, it’s a perfect time to reflect on some of this year’s standout moments for Osteopathy Australia and our community. From packed events to new partnerships and advancements in education, this year has underscored our profession’s growth, resilience, and commitment to excellence.
Our sold-out national conference in October was undoubtedly a highlight. It was incredible to see so many of you in Sydney, connecting, sharing and learning. The conference celebrated the best of our profession – from innovative keynote speakers to handson workshops that explored new approaches in patientcentred care. Thank you to everyone who attended and the many hands behind the scenes, as well as the Osteopathic International Alliance (OIA) and Osteopaths New Zealand for their collaborative efforts. Together, we

Meeting (AGM) continues to be a valuable platform for shaping the future of osteopathy in Australia.
With a focus on professional development and strengthening our advocacy efforts, the AGM affirmed our commitment to progress and unity as a profession.
In August, Osteopathy Australia was proud to be part of the Western Bulldogs’ Athletic Performance Summit at Melbourne’s Western Oval, attended by over 30 osteopaths among 110 participants. Seeing the Osteopathy Australia emblem prominently displayed underscored our growing influence in sports medicine. Congratulations to the first osteopaths who completed the Strength and Conditioning Course through Victoria University and the Western Bulldogs. Your achievements highlight osteopathy’s expanding role in highperformance training and sports health.
One of our most exciting initiatives this year has been the partnership with Edith Cowan University (ECU) in Western Australia, aimed at launching a new osteopathy program in 2026. This collaboration marks a significant milestone in osteopathic education, and we are dedicated to helping ECU develop a curriculum that aligns with the evolving scope and core values of our profession. We look forward to sharing more on this project as it progresses.
instrumental in refining our strategic direction.
As we wrap up a productive and inspiring 2024, I’d like to extend my sincere thanks to each of you. Your commitment, whether in private practice, research, education, or advocacy, is what fuels the vibrancy and impact of osteopathy across Australia. Here’s to building on this year’s achievements and advancing our profession further in the year to come.
Yours in health, MATT COOPER President, Osteopathy Australia mcooper.director@osteopathy.org.au
Osteopathy Australia acknowledges the Traditional Custodians and Elders of Country throughout Australia, and their connection to land, sea and community. We pay our respects to Aboriginal and Torres Strait Islander Elders, past, present and emerging.

Osteopathy Australia
T (02) 9410 0099
E info@osteopathy.org.au
W www.osteopathy.org.au osteopathyaustralia osteopathyau osteopathyaustralia
OSTEO LIFE is a magazine for Osteopathy Australia members.
For enquiries, feedback, or to contribute, contact Communications on 02 9410 0099 or comms@osteopathy.org.au
For advertising enquires, email info@osteopathy.org.au.
Communications and Marketing Working Group Tara Bain, Toby Barker, Adam Nicholson, Rebekka Thompson-Jones
Chief Executive Antony Nicholas Editor Rebekka Thompson-Jones
Designer Stephanie Goh Advertising info@osteopathy.org.au
Printed by Megacolour Printed on 100% recycled paper: one of our commitments to a sustainable future.
Osteopathy Australia aims to support, enhance and promote the profession. Here’s a quick recap of everything osteo from the past few months.
After five long years, Osteopathy Australia successfully held its national conference – our first since the pandemic forced a cancellation in 2020. Further delayed in 2023 to accommodate the International Congress on Back Pain in Melbourne, the event finally took place over 25-26 October, with the added bonus of co-hosting the Osteopathic International Alliance conference. This collaboration brought a diverse roster of participants and speakers from across the globe, with around 25 countries represented. Thank you to everyone who registered, and an extra warm thank you to the dozens of osteopaths who delivered lectures, workshops and panel discussions. Early feedback suggests attendees had a great time and enjoyed the variety of speakers and perspectives, the historical insights, and the invaluable networking opportunities. A big thank you to Dominic, Leng and Rebekka, who worked over the preceding months to pull a logistical nightmare together, and to our entire team for helping us before or during the conference.
Thank you also to Stuart Hammond, who interviewed a range of speakers for our revitalised Osteo Talk podcasts – more

Mark your calendars! Next year’s conference heads to Auckland, New Zealand | Tāmaki Makaurau from 5-7 September 2025.
During the conference, we also held our annual general meeting, which I can safely say had the largest attendance of any AGM in the past decade.
One of the future constitutional changes the Board is suggesting is including two new membership categories. First, a five-year ‘early career’ membership would replace the current two-and-a-half-year ‘graduate’ membership. This is to support recent graduates as they transition into practice, focusing on financial sustainability. The second category aims to support osteopaths in corporate health or non-hands-on occupational rehabilitation roles to stay connected with the profession, as many of these roles find employer benefits cover much of what we offer, such as insurance, CPD or training and HR support. The Board’s intention is to hold a special general meeting soon, so that members can discuss and vote on these proposed changes.
As we wrap up 2024, Osteopathy Australia is already mapping out core projects for 2025. These include expanding our career hub including jobs guides, salary expectations and insights from osteopaths working in diverse roles; expanding our mentoring network; advancing efforts for a new university course in NSW; and launching a new member interface/database to streamline access to resources.
All this while continuing to deliver our ongoing projects, and striving to enhance and broaden our advocacy, education and communication efforts for osteopathy on your behalf.
ANTONY NICHOLAS Chief Executive, Osteopathy Australia ceo@osteopathy.org.au
OSTEOPATHY AUSTRALIA OFFICE CLOSURE OVER CHRISTMAS HOLIDAYS
We can hardly believe it’s that time of year again!
As we head into the holiday season, please note our office will be closed from Saturday, 21 December 2024, until Friday, 3 January 2025. Our last working day will be Friday, 20 December 2024, and we’ll be back, refreshed and ready to assist, on Monday, 6 January 2025.
We wish you a joyful festive season and a wonderful New Year ahead.


The 2024 Osteopathy Conference, held in Sydney from 25-26 October, was a landmark gathering, marking the first Australia-based event since COVID-19. Co-hosted by the Osteopath International Alliance, Osteopathy Australia and Osteopaths New Zealand, the conference was a global celebration aligning with the 150th anniversary of osteopathy’s founding by Andrew Taylor Still. The event brought together a diverse international community, with attendees from Australia, New Zealand, Italy, Korea and beyond. The conference offered a vibrant platform for knowledge exchange and a spotlight on cutting-edge research and clinical innovations.
We extend our sincere gratitude to all the speakers who presented over the two days. We are incredibly grateful for their time, expertise, and thought-provoking presentations, which made the event a true success.
The program was rich with high-calibre presentations on critical topics. Key sessions included:
• Neurotrauma and CTE: A powerful keynote by Professor Buckland, Associate Professor Alan Pearce and Andrea Miles on chronic traumatic encephalopathy (CTE) provided invaluable insights into the condition’s neuropathology and symptoms. Andrea’s deeply personal account reminded practitioners of their essential role in supporting patients through complex health challenges.
• Global regulation panel: This informative and self-reflective session brought together speakers from Osteopathy Australia and the Osteopathic International Alliance. The panel fostered an open discussion on regulatory challenges and the future of osteopathy, blending essential insights with humour and self-awareness.
• Professional identity panel: Following Professor Gary Fryer’s inspiring talk on Australian osteopathic

professional identity, the identity panel attracted a full house of enthusiastic delegates. This session delved into the profession’s unique role and adaptability within modern healthcare, sparking lively discussions on osteopathy’s contributions and its evolving identity.
• Clinical workshops: Interactive workshops were a cornerstone of the conference, offering practical training on techniques like muscle energy for shoulder impingement. Attendees had the chance to sharpen their diagnostic and therapeutic skills through sessions on biomechanics, rehabilitation, and pain science.
• Post-breast cancer rehabilitation: Amanda Hannaford’s presentation highlighted the crucial role osteopaths can play in helping breast cancer survivors manage musculoskeletal effects, from scar tissue to lymphatic cording.
• Pre-conference anatomy workshop: Frank Willard’s workshop on lateral cranial nerve anatomy provided in-depth clinical insights for practitioners. For those unable to attend, this valuable session will soon be available on-demand.
(Conference highlight by Deanne Mitchell, Director, Osteopathy Australia)

By Deanne Mitchell, Director, Osteopathy Australia
Emerging research on chronic traumatic encephalopathy (CTE) provides invaluable insights that enhance our understanding of this complex condition and offer osteopaths practical guidance for integrating these findings into clinical practice. Recent studies from the Concussion Legacy Foundation have identified a strong link between repetitive head impacts and the risk of tau protein misfolding, a hallmark of CTE. Notably, this risk stems from repeated head impacts or brain deceleration rather than from single concussive events –even with helmet protection.
A presentation on this topic was recorded at the Osteopathy Conference. If you’d like to view that, it’s available online at osteopathy.org.au/ events/the-science-and-lived-experience-ofcte-and-post-concussion-syndrome. One of the presenters is Andrea Miles, whose personal journey with CTE is a powerful reminder of the need for awareness and proactive measures, particularly in modifying contact sport practices for young and developing brains. We extend our gratitude to Professor Michael Buckland, Professor Alan Pearce and Andrea for sharing their expertise and research, which underscore the importance of preventive strategies in promoting long-term brain health. For further details on CTE, visit concussionfoundation.org
A special thank you to our gold sponsors: Cliniko, DrRest and Guild Insurance, as well as our silver sponsors, Aerobe, OPC Health and Scolicare. Their support was instrumental in ensuring the success of the conference, facilitating an environment where clinical excellence and continuing professional development could thrive. The sponsors’ commitment to the osteopathic community was evident through their engagement and presence at the event, showcasing innovative solutions that align with contemporary osteopathic practice.
We extend our appreciation to the Osteopathy Australia team for organising the event and to Stuart Hammond who volunteered his time to help us. Their efforts played a crucial role in making this conference a success, providing a seamless experience for attendees and creating a valuable opportunity for the global osteopathic community to connect and learn.
The 2024 Osteopathy Conference reinforced the profession’s commitment to clinical excellence, collaborative learning, and the integration of new therapeutic modalities. It not only celebrated osteopathy’s rich history but also looked forward to its future, equipping practitioners with the skills and knowledge to navigate the evolving landscape of healthcare. Here’s to the 2025 conference in Auckland, New Zealand / Tāmaki Makaurau – Aotearoa.
The 2024 Annual General Meeting (AGM) for Osteopathy Australia took place on Friday 25 October at the end of day one of the national conference, allowing Osteopathy Australia member delegates present the opportunity to participate in the governance process. We extend our appreciation to all attendees and those members who submitted proxy votes in advance, ensuring any member can participate in voting.
1. CHAIR’S REPORT
The AGM opened with the Chair’s Report, where Matthew Cooper, National President provided an overview of Osteopathy Australia’s key activities over the past year. The report highlighted significant achievements and demands in our advocacy work, the excitement about a proposed new course by Edith Cowan University and initiatives aimed at better member support and engagement. Matthew also touched on our strategic planning, town halls across the country and strategic priorities for the year ahead.
APPROVAL OF 2023 AGM MINUTES
The minutes from the 2023 AGM were presented and approved, ensuring accurate documentation.
3. PRESENTATION OF AUDITED FINANCIAL STATEMENTS
Don Hunter, Director and member of the Finance Committee presented the audited financial statements for the 2023-2024 fiscal year. Osteopathy Australia had an increase in income and membership growth, however, recorded a small deficit of around $20,000.
The Osteopathy Australia Research Foundation also showed growth and a distribution of funds for research projects. The auditor noted that the association had demonstrated sound financial management and processes, commending management by our external accountants and Operations Manager Leng Warwar.
The AGM notified members of the reappointment of the auditor, Bishop Collins Group for the upcoming year.
Osteopathy Australia is dedicated to upholding transparency in its operations. Financial reports, including the most recent audited statements, are available on the Osteopathy Australia website here: osteopathy.org.au/about-us/osteopathy-australia/ annual-general-meeting
To further enhance transparency, the association will now provide access to all past financial reports for members, rather than limiting access to the most recent report. This initiative aims to offer a comprehensive view of the association’s financial history and reinforce its dedication to open governance.
At the recent Allied Health Awards on the Gold Coast, Louise Bibby was awarded the prestigious title of 2024 Osteopath of the Year. This recognition honours her exceptional commitment to osteopathy, rural health, and her pioneering work in sports osteopathy. Louise’s dedication has made a tangible difference to communities, colleagues and the broader field of osteopathy.
For those who may not yet know Louise, her contributions to osteopathy are remarkable:
• AFLW and elite sport. As a key figure in sports osteopathy, Louise works with the Bulldogs in the AFLW, promoting osteopathic care at the elite level and highlighting its importance in athlete health and performance.
• Founder of the Osteo Sports Network. Louise established the Osteo Sports Network to enhance the role of osteopaths within the sports medicine landscape, fostering greater representation and integration of osteopathic practice in athletics.
• Victorian SMA Board Member. Serving on the Victorian Sports Medicine Australia (SMA) board, Louise champions professional development opportunities, particularly for rural practitioners, ensuring that osteopaths across the state have access to critical resources and support.
• Rural outreach programs. Through Central Mallee Health, Louise and her team cover a vast 40,000-square-kilometre area, bringing essential allied healthcare services to some of Australia’s most remote communities in the Mallee.
• Community health builder. In a commitment to fostering health at every level, Louise founded a gym in a rural town, not only addressing the community’s need for fitness resources but also strengthening local health infrastructure.
• Rural private practice leader. Louise’s rural private practice provides vital healthcare services and creates jobs for her community, showcasing the impact osteopathy can have in supporting the wellbeing and resilience of rural populations.

• Dedicated to professional development. Known for her commitment to learning and support for her colleagues, Louise actively participates in professional development, embodying a spirit of continuous improvement.
We’d also like to recognise the other distinguished nominees –Michelle Funder, Beth Yule and Elizabeth Johns – whose dedication and contributions continue to shape the future of osteopathy in meaningful ways. Each of these practitioners exemplifies the qualities that make our profession strong, resilient, and impactful. Congratulations to Louise Bibby on this well-deserved recognition.
Osteopathy Australia is proud to support practitioners like Louise, Michelle, Beth and Elizabeth who inspire excellence and uphold the values of our profession.
IN BRIEF
After much anticipation, the Osteo Talk podcast is back and ready to inspire. Rated the ninth best professional development podcast of 2024, Osteo Talk returns to bring education, engagement and a fresh injection of positivity and pride into the osteopathic profession. We’re thrilled to revive this series!
And we want to hear from you. What topics are on your mind? Be it clinical advancements, practice challenges or emerging trends, we’ll look to build episodes around the issues that matter most to our members. Stay tuned for the latest episodes and join us in celebrating the strength and spirit of osteopathy.

by Sophie Smibert and Corey Dyer

In August, we travelled to Bali to join Jorge Aranda and nine other osteopaths from around the world – including Corey Dyer, on his third mission with the Hands with Heart Foundation. Together, we volunteered our osteopathic skills to provide hands-on care for local children with disabilities who otherwise have little or no access to healthcare. It was a truly inspiring opportunity to put our skills to work for those who need them the most.
We stayed in Canggu, a comfortable base close to Bali’s main amenities. Each morning, we split into groups and headed off to different therapy centres or schools for children with disabilities around Denpasar. We rotated between a few locations; including a centre supporting children with cerebral palsy and brain injuries, a school for blind and intellectually disabled children (which also housed an orphanage), and we even conducted home visits for children who couldn’t travel to the centres. Our typical day involved treating children from 9am until early afternoon, then met for lunch to debrief, share our experiences and reflect. Some afternoons were free, though we often returned to families needing home-based care.
The children and families we worked with faced some extraordinary challenges, managing complex conditions with almost no support. Many parents would travel for hours across Bali, often on public transport, just to bring their children to us. We treated children with cerebral palsy, meningitis, hydrocephalus, epilepsy, Down syndrome, blindness and global developmental delays – conditions we rarely encounter back home without a full team of healthcare support. At first, it was hard to feel that our short time with each child could make a lasting difference. But within days, families started reporting positive changes: improved sleep, increased movement and flexibility, better digestion, and reduced pain. Seeing the relief and gratitude in the families’ faces was incredibly rewarding.
We also quickly learned that reducing the stigma around disability was just as impactful as the handson therapy itself. When stigma fades, families, communities and society can step in and support these children in powerful ways. Our presence, treating and engaging with these children with kindness and
care, helped reduce the stigma and remove fear. Part of Hands with Heart’s mission is to change the way the world sees disability, to treat not just the condition (as “any darn fool can find”) but the whole person, which is the essence of osteopathy.
The whole experience with Hands with Heart was at times confronting and challenging, both professionally and personally, but it was a hugely rewarding experience. The smiling, resilient children and their families reminded us why we were there, and the connections with other osteopaths from around the world sparked intense friendships. It was a journey that renewed our passion for osteopathy and deepened our commitment to helping kids reach their potential.
A BIT ABOUT HANDS WITH HEART
Hands with Heart Foundation is the initiative of Spanish osteopath Dr Jorge Aranda, and is dedicated to improving the lives of children with disabilities in developing countries. Through clinical missions with osteopaths, physiotherapists, and other allied health professionals, the foundation provides vital healthcare where it’s often inaccessible. By integrating therapeutic modalities into daily routines, Hands with Heart empowers children and families, promoting self-reliance and social sustainability to help children reach their full potential.
Hands with Heart (HwH) currently runs clinical missions in Bali, Costa Rica, Argentina and Romania, and is preparing to help war victims in Ukraine. HwH also supports the Parasurfing athletes at competitions in Australia and California.
HwH’s next clinical mission takes place in Bali in February 2025 and Australian osteopaths are warmly welcome to join the team. This provides participants with approximately 50 hours of direct clinical experience and is an invaluable opportunity to build on learning and experience in the paediatric field. Tutorial learning sessions, case conferences and team reflection sessions are also held to support volunteers. Places are open to experienced and recent graduates, and senior students are also invited to participate. handswithheartfoundation.org
Delivered by the Western Bulldogs in partnership with Victoria University, the Graduate Certificate in Strength & Conditioning offers a truly unique, career-advancing experience. The course has been recognised by Osteopathy Australia to provide an industry-first pathway for osteopaths to engage in postgraduate study and meet the tertiary qualification requirements for the Advanced Practice recognition in Sports Management.
This six-month program combines leading academic coursework in areas such as return to play, developing strength and power, and improving speed and agility with the opportunity to embed yourself within the high-performance department at the Western Bulldogs.
GAIN OVER 40HRS OF INDUSTRY IMMERSION AND IMPROVE YOUR ABILITY TO DELIVER END STAGE ATHLETIC REHABILITATION
Experience hands-on learning inside the Western Bulldogs Physical Performance Department and gain an unparalleled understanding of the high-performance protocols utilised across all four football programs.
Students will be exposed to a range of athletes and disciplines within the Physical Performance team, including strength and conditioning, medical, rehabilitation and sports nutrition.
Theoretical learning is also complemented by a series of Masterclasses delivered by senior Western Bulldogs high-performance staff. These are in-depth sessions on a series of topics that are unique to elite sport and explore principles of strength and conditioning and sports rehabilitation drawing on the experience of senior staff members.
COURSE
AND
Scan QR opposite for more information. The course is delivered full-time over one semester, consisting of four units designed specifically to give graduates the skills and knowledge required to work in high-performance sport. Each unit is taught across a four-week period, aligned with Victoria University’s award-winning VU block model. Hours are estimated to be between 10-15 hours a week, split between online and face-to-face modalities.
“This course and experience with VU and the Western Bulldogs is one of the greatest (if not the greatest) experiences I have been a part of. I have enjoyed everything regardless of the challenge and really would recommend this course to anyone, particularly osteopaths/health professionals who want to experience the elite environment and learn so much more about S&C and rehab.”
– Dr Timothy McCormick (Osteopath), 2024 Graduate
“The combination of studying with a top university for Sport Science and the chance to gain experience and insight at an AFL club – where I want to work after I finish studying – is what led me to choosing this course. I have thoroughly enjoyed the course and have found the experience with the Western Bulldogs to be invaluable. I would recommend the course to anyone interested in working in elite sport, particularly AFL.”
– Ash, 2023 Graduate

“The Western Bulldogs Graduate Certificate in Strength & Conditioning provided me with invaluable insight into the rehabilitation of elite athletes and as well as the general population. It has truly furthered my understanding of exercise prescription and improved my confidence when prescribing programs for injury prevention and athletic performance.”
– Dr Will Fleming (Osteopath), 2024 Graduate
Applications are open now for our semester one intake beginning Monday, 24 February 2025.

Register for our next information session by scanning the QR code or enquire today by emailing education@westernbulldogs.com.au
Learn more at education.westernbulldogs.com.au/sandc

In any workplace setting, maintaining a stable and engaged workforce is essential for sustaining productivity and fostering a positive organisational culture. Effective employee retention strategies play a pivotal role in achieving these objectives by ensuring that skilled and experienced employees remain committed to their roles within the organisation. Beyond simply reducing recruitment costs, they show a commitment to employee satisfaction and wellbeing, which in turn contributes to the long-term success and competitiveness of the organisation.
This article will focus on our Employee Retention Checklist, offering employers a practice resource. This checklist serves as a valuable guide, providing essential insights and frameworks for employers to evaluate, enact, and enhance their strategies for retaining staff.
Our Employee Retention Checklist is developed to provide employers with a comprehensive tool to optimise retention measures. It addresses key retention strategies and serves as a guide for creating a supportive work environment that foster long-term relationships with employees, driving organisational success and competitiveness in the market. Some of the key areas that will be addressed in the checklist include:
Legislative requirements and compliance
Compliance with legislative requirements, particularly in areas like pay, is essential. This ensures fairness, builds trust and reduces turnover by demonstrating a commitment to ethical practices and legal obligations. Upholding these standards fosters a positive work environment and reinforces employee loyalty, contributing to long-term organisational success.
Work/life balance is pivotal, as it directly impacts job satisfaction and overall wellbeing. Employees who feel they have a healthy balance between work and personal life are more likely to be engaged and committed. Conversely, imbalance can lead to burnout
and increased turnover. By prioritising work/life balance initiatives, employers foster a positive culture that values the holistic wellbeing of their workforce, enhancing retention and organisational success.
Alignment with organisational values is vital for employee retention. When employees share the company’s core values and mission, they feel a stronger sense of purpose and belonging, fostering commitment and loyalty. Conversely, a misalignment can lead to disengagement and increased turnover. Prioritising alignment to organisational values cultivates a unified workforce and motivates employees to contribute their best, ultimately enhancing retention and driving organisational success.
Employee retention is a critical focus for employers seeking to build sustainable and successful organisations. By fostering a loyal and engaged workforce, employers not only ensure continuity in operations but also reap numerous benefits. In this section, we delve into a few key reasons why retention holds such importance for employers in today’s dynamic business landscape.
Continuity and stability within an organisation are essential for its smooth functioning and sustained success. When businesses experience high turnover rates, they risk disruptions in operations and loss of institutional knowledge. Retaining experienced
employees ensures continuity in processes, workflows and relationships, thereby minimising disruptions and maintaining stability. Employees who are familiar with their roles and the organisation’s culture can contribute more effectively, leading to increased efficiency and productivity.
Cost savings
High turnover entails significant expenses associated with recruitment, training, and onboarding. By retaining talent, businesses minimise these costs and maximise the return on investment in human capital. Additionally, low turnover rates reduce the need for frequent recruitment efforts and decrease the likelihood of productivity dips during these transition periods.
Employee morale and engagement
When employees feel valued, supported and recognised for their contributions, morale improves, leading to higher levels of job satisfaction and commitment. Additionally, a positive work environment fosters strong relationships among colleagues and promotes a sense of belonging within the organisation. By prioritising retention, employers create a culture where employees feel appreciated and motivated to excel, which can help promote higher levels of performance and success.
Inadequate retention measures can have profound consequences for businesses, both financially and non-financially. High turnover rates not only incur significant recruitment costs and legal liabilities but also impact employee morale, organisational culture, and long-term success.
Firstly, neglecting employment retention measures can have significant financial implications for business. The most obvious consequence is that high turnover rates lead to substantial recruitment expenses, including advertising costs and hiring fees as positions are reopened and filled and reopened again. However, it is just as important to acknowledge the lesser considered consequence which is associated with non-compliance with legislation, such as failing to meet remuneration standards or breaching WHS standards, as these can incur fines and legal penalties. In addition to this, poor retention may also result in non-financial consequences. High turnover rates can erode employee morale and engagement, leading to a negative work environment characterised by low motivation and increased stress. This can result in decreased collaboration, communication breakdowns and a decline in team cohesion. Additionally, the loss of experienced employees can lead to a loss of institutional knowledge, hindering innovation and growth.
Employers must continue to prioritise employee retention efforts since there is a strong link with organisational success. As such, it is highly recommended that employers utilise our Employee Retention Checklist to ensure they address key retention concerns to prevent high turnover and other related complications.
If you have any questions about this article, please contact the Osteopathy Australia HR Service on 1300 143 602, or via email at HRHotline@osteopathy.org.au

“When employees feel valued, supported and recognised for their contributions, morale improves, leading to higher levels of job satisfaction and commitment”

FIRST PUBLISHED IN OSTEO LIFE WINTER 2022 UPDATED BY AUSTRALIAN WOMEN’S HEALTH ALLIANCE

Whether or not they decide to disclose it to you, as osteopaths, there is a high chance some of your patients are victims of domestic, family and sexual violence (DFSV), and some of them may be perpetrators. When you suspect or become aware of such situations it can be challenging on a number of levels. Knowing how to appropriately support your patient, and about the support services available, can make a huge difference for you as a practitioner and for your patients.
Domestic, family and sexual violence (DFSV) is a pervasive social and health issue that can impact a person’s physical, mental and emotional wellbeing. In Australia, 27% or one in four women and 7.3% or one in 14 men have been subject to physical violence from a current or former partner since the age of 15 years.¹ One in four women and one in six men have been subject to emotional abuse. Most frighteningly, one woman is killed on average every two weeks by a current or former partner in Australia.² Intimate partner homicide is the most prevalent type in Australia.3
DFSV is often mistaken to include only physical and sexual abuse, but this is only the tip of the iceberg. DFSV includes psychological, emotional, financial and other controlling behaviours.
‘Violence is a broad term, often used to encompass a wide range of behaviours and definitions that vary according to different legislation and practices. Harm from violence can be wide-ranging, including physical, sexual and psychological, with serious and long-term impacts on individuals, families and communities.4
Further, ‘Coercive control is often a significant part of a person’s experience of family and domestic violence. It is commonly used to describe a pattern of controlling behaviour, used by a perpetrator to establish and maintain control over another person.’ Note that legislation criminalising coercive control came into effect in New South Wales on July 1 2024, and in South Australia in August 2024.5
DFSV can have a significant impact on a person’s physical and psychological wellbeing. ‘Partner violence was ranked as the third leading risk factor contributing to total disease burden for women aged 25 to 44 years’.6
It can lead to serious acute and chronic health issues, complex trauma, depression, anxiety and substance abuse.
How common is domestic, family and sexual violence?
• One in four women (27% or 2.7 million) and one in eight men (12% or 1.1 million) experienced intimate partner or family member violence since the age of 15.
• One in four women (27% or 2.7 million) and one in six men (15% or 1.5 million) have experienced violence or emotional/economic abuse by a cohabiting partner since the age of 15.
• One in five women (22% or 2.2 million) and one in 17 men (6.1% or 582,400) experienced sexual violence since the age of 15.
Table 1 outlines various indicators a patient experiencing DFSV may present with and which you are likely to come across in your practice. Note these signs may be indicative of other social or health issues.
• Delay in seeking treatment
• Multiple presentations
• Non-compliance with treatment and attendances
• Accompanying partner who is over-attentive
• Identifiable social isolation
• Recent separation or divorce
• Past history of child abuse
• Aged less than 40 years old
• Abuse of a child in the family
• Obvious injuries, especially to the head/neck or multiple areas
• Bruises in various stages of healing
• Sexual assault
• Sexually transmissible infections
• Chronic pelvic pain
• Chronic abdominal pain
• Chronic headaches
• Chronic back pain
• Numbness and tingling from injuries
• Lethargy
PSYCHOLOGICAL PREGNANCY INDICATORS
• Insomnia
• Depression
• Suicidal ideation
• Anxiety symptoms and panic disorder
• Somatoform disorder
• Post-traumatic stress disorder
• Eating disorders
• Drug and alcohol abuse
• Miscarriages
• Unwanted pregnancy
• Antepartum haemorrhage
• Lack of prenatal care
• Low birth weight of an infant
Figure 1 Prevalence of sexual violence since the age of 15(a), 2021-22
a) Refers to the number of men/women who have experienced sexual violence since the age of 15, expressed as a percentage of all men/women aged 18 years and over.
b) Estimate for men has a relative standard error of 25% to 50% and should be used with caution.
c) Includes sexual assault and sexual threat. Where a person has experienced both sexual assault and sexual threat, they are counted separately for each but are counted only once in the aggregated sexual violence total.
Source: Australian Bureau of Statistics, Personal Safety, Australia 2021-22 financial year
“An osteopath is in a unique position to recognise the signs of abuse and make referrals if the patient requires support”
Along with the health impacts, DFSV is one of the biggest causes of homelessness in Australia. The economic and non-economic impact of pain and suffering, and the impacts of violence on the health system, production and consumption, children, the justice and service system costs Australia an estimated $26 billion a year, $5.7 billion of which is borne directly by victims.7
WHY DON’T THEY JUST LEAVE?
There are many barriers preventing a person experiencing DFSV from leaving an abusive relationship. For example, it can be very dangerous to leave as violence often escalates following separation. The victim/survivor may be isolated, they may have financial concerns, they may be worried about their children, abuse against pets, and/or they may feel shame. The abuse may have caused them to lose their confidence, their sense of self, and make them doubt themselves.
LISTEN Listen to the patient closely, with empathy and without judgement
INQUIRE
Inquire about needs and concerns, including emotional, physical, social and practical VALIDATE
Show that you understand and believe the patient and assure them they are not to blame
ENHANCE SAFETY
Discuss a plan to protect the patient and their children from further harm
Help them connect to information, services and social support
There are also structural barriers for those who face intersecting forms of disadvantage, which can impact seeking help for, reporting or leaving an abusive relationship. For instance, some women with disabilities may be at risk of their assistance devices being damaged or assistance animals being harmed. Many migrant and refugee women on temporary visas and their dependents are excluded from accessing migration system protections from violence.
As an osteopath, you may be the first (or only) point of contact for people experiencing DFSV. The whole person approach used by osteopaths, and the subsequent trust that is often built between osteopaths and their patients, means osteopaths are well placed to support patients in such cases. The role of osteopaths in supporting patients experiencing DFSV is sometimes described as a ‘canary in the coal mine’. While it is not the osteopath’s role to counsel the patient, an osteopath is in a unique position to recognise the signs of abuse and make referrals if the patient requires support. Osteopaths tend to have longer consultation times with patients compared with many other health professionals. The longer time allows for more in-depth conversations. Standard osteopathy treatment involves touch and visualising the affected part of the body or region, so it is often possible to see the physical signs of abuse.
Figure 2 What is domestic and family violence?8
PHYSICAL VIOLENCE
PSYCHOLOGICAL AND EMOTIONAL ABUSE
SEXUAL ABUSE
OTHER COERCIVE CONTROL TACTICS
• Slapping, hitting
• Kicking, beating
• Knives/guns
• Threats of physical violence
• Intimidation, humiliation
• Constant belittling
• Harassment
• Forced intercourse
• Sexual coercion
• Reproductive coercion
• Isolation from family/friends
• Monitoring movements
• Deprivation of basic necessities
• Mental health/substance use coercion
• Financial control and/or visa abuse
A victim survivor’s first experience of disclosure may influence whether they ever seek help in future. If they don’t feel believed, if they are blamed or if they are made to feel uncomfortable, they may never reach out to others about their experience in future.
The World Health Organization has developed a helpful framework for health practitioners to support patients experiencing DFSV called LIVES. It asks health professionals to listen to patients with empathy, inquire about their needs and concerns, validate their story, enhance their safety and support them by connecting them to information and services (see Table 2).
When supporting a patient experiencing DFSV, it’s very important to let them lead their own journey and respect their decisions, even if you don’t agree with them.
Where you have concerns for the safety of a child, you must report this to the relevant authority in your state or territory.
As an osteopath, you don’t need to be a social worker or a counsellor, but you can make a positive impact in the lives of your patients affected by DFSV.
Using economic abuse
Using coercion and threats
Making and/or carrying out threats to do something to hurt her/him • Threatening to leave her/him, to commit suicide, to report her/him to welfare • Making her/him drop charges • Making her/him do illegal things
Preventing her/him from getting or keeping a job • Making her/him ask for money • Giving her/him an allowance • Taking her/his money
• Not letting her/him know about or have access to family income
Using male privilege
Treating her/him like a servant
• Making all the big decisions
• Acting like the ‘master of the castle’ • Being the one to define men’s and women’s roles
There are a number of services available to assist you and your patients, including counselling, accommodation support, financial support and legal support.
• Statistically, it is quite likely that some of your patients are perpetrators and some of them are victims.
• Look out for ‘patterns of injuries’ as these might be an indication of DFSV.
• Listen to your patients. If the information doesn’t match, then listen more carefully because quite often they’ll tell you without telling you.
IN PERSON OR THROUGH THE USE OF TECHNOLOGY FACILITATED ABUSE
Using intimidation
Making her/him afraid by using looks, actions, gestures • Smashing things
• Destroying her/his property • Abusing pets
• Displaying weapons
Using children
Making her/ him feel guilty about the children
• Using the children to relay messages • Using visitation to harass her/him
• Threatening to take the children away
Using emotional abuse
Putting her/him down
• Making her/him feel bad about herself/himself • Calling her/him names, making her/him think she’s/he’s crazy, playing mind games • Humiliating her/him, making her/him feel guilty
Using isolation
Controlling what she/he does, who she/he sees and talks to, what she/he reads, where she/ he goes •limiting her/his outside involvement
Minimising, denying and blaming
Making light of the abuse and not taking her/his concerns about it seriously • Saying the abuse didn’t happen • Shifting responsibility for abusive behaviour • Saying she/he caused it
• Using jealousy to justify actions
To find the full list of references for this article, scan the QR code here.

1800Respect
Call 1800 737 732 Text 0458 737 732 www.1800respect.org.au
Chat online or video call via the website. National domestic, family and sexual violence counselling, information and support service. 24 hour, 7 days a week, free service
NSW DV Line
Call 1800 656 463
Telephone counselling and referrals to women experiencing domestic and family violence. 24 hours, 7 days a week, free service
Lifeline
Call 13 11 14 Text 0477 13 11 14 Chat online
Crisis support and suicide prevention service providing support for people experiencing emotional distress. 24 hours, 7 days a week, free service
13Yarn
Call 139 276
National crisis support line for Aboriginal and Torres Strait Islanders people. 24 hours, 7 days a week, free service
Men’s Referral Service
Call 1300 766 491
National counselling, information and referral service for men who use violence and abuse, to change their behaviour. 24 hour, 7 days a week, free service
QLife Call 1800 184 527 qlife.org.au
Telephone and web based counselling, referrals and support for LGBTI people and their families. Every day, 3pm-midnight, free service
ACON Call (02) 9206 2000 www.acon.org.au
LGBTI health organisation offering information, referrals, counselling, advocacy and practical support for LGBTI people in NSW experiencing DFSV.
DVNSW Good Practice guidelines 2022 www.dvnsw.org.au/categories/good-practiceguidelines
Professionals | 1800RESPECT www.1800respect.org.au/professionals
Work-induced stress and vicarious trauma | 1800RESPECT 1800respect.org.au/resources-and-tools/workinduced-stress-and-trauma
The Blue Knot Foundation professionals.blueknot.org.au/professionaldevelopment-training/
We all want to access, and offer, healthcare that treats people holistically for their healing and wellbeing.
Historically, however, important differences in the health, illness and experiences of people of different genders have been overlooked. This can lead to reduced health outcomes, such as women experiencing more pain and disabling chronic conditions, or women impacted by violence not having their health needs met.1
That’s why it’s important to understand and integrate gender-responsive approaches to healthcare.
Australian Women’s Health Alliance is the national voice on women’s health. The Alliance works closely with members, partners and government to progress its aim of achieving gender and health equity.
The Alliance articulates the policies and actions necessary to strengthen gender-responsive approaches to health and prevention, recognising
that women’s health is determined by social, cultural, environmental and political factors.
As a national peak body, the Alliance provides independent, evidence-based advice to promote a gendered approach to women’s healthcare.
The Women’s Health Hub is an up-to-date online repository of information for people working in health and social policy, advocacy, research, and practice. It contains open access Prevention in Practice resources, including free online training on gender-responsive health.
Whether it’s addressing the gendered nature of violence and its health impacts or enabling agency in healthcare, the Australian Women’s Health Alliance is vehicle for women’s health organisations, consumers and advocates to connect and collaborate.
Find out more by visiting the Women’s Health Hub: AustralianWomensHealth.org
1 Australian Women’s Health Alliance (2022) Policy Brief –Why women’s health matters
Osteopathy Australia has made significant strides in advancing research initiatives, enhancing funding and fostering collaboration within the osteopathic community.
Over the past few years, Osteopathy Australia’s Research Committee, alongside our dedicated team, has hit major research milestones. By creating new initiatives, increasing funding and expanding support, we’ve strengthened research capacity and leadership for both osteopaths and researchers. Here are some of the achievements so far:
✔ Research Foundation: We established the Osteopathy Australia Research Foundation to fund high-quality osteopathy research.
✔ Streamlined the grant process: Our research grants process is now faster and more userfriendly for applicants, reviewers and staff.
✔ Increased funding: We boosted our annual research grant budget allowing us to offer both project and seeding grants.
✔ Increased project support: Over the past few years, we’ve funded 15 research projects worth nearly $100,000.
✔ ORION study: Round two of the ORION study, conducted by the Australian Research Centre in Complementary and Integrative Medicine (ARCCIM), received funding from Osteopathy Australia. Complete the survey via: utsau.au1. qualtrics.com/jfe/form/SV_8BKu3KEJBHn5kTs
✔ National mentorship program: We launched a mentorship program to increase research engagement within osteopathy. The first round was a success, with the second currently in progress. Check out the program testimonials on our website at osteopathy.org.au/research/ research-mentorship-program
✔ Research webinar series: Now in its second year, our research webinar series continues to educate members. Six webinars have been launched to date and can be viewed here: osteopathy.org.au/osteo-brain-cpd-hub
✔ University engagement: We presented an “Introduction to Research” talk for first-year university students at RMIT University, delivered by Don Hunter, Chair of the Research Committee. Plans are in place to expand this to all osteopathy universities.
✔ Research guides: We developed guides covering essential research topics such as grant writing, data analysis, preparing manuscripts and journal selection, available to all members on our website
here: osteopathy.org.au/research/researcharticles-and-resources
✔ Career pathways in research: We added a dedicated research chapter to our career guide, detailing alternative career paths in Research and Academia for osteopaths.
✔ Targeted call for research (TCR): The Board allocated $100,000 for a new TCR. Details are expected by late 2024/early 2025.
✔ PROMs accessibility: We created a comprehensive list of standardised PROMs relevant to osteopathy, complete with instructions, scoring details and more. Access them here: osteopathy.org.au/research/ patient-reported-outcome-measures
✔ Digital PROMs study: We piloted a digital PROMs study using Physitrack, assessing the feasibility of collecting PROMs digitally in osteopathic practice.
Explore more research opportunities, including external grant opportunities and a research promotion page where researchers can promote their studies to boost recruitment (and where osteopaths can take part in relevant studies).
With exciting new ventures planned for 2025, you can stay updated on all our research activities via our website. Visit our research page for the latest!
(osteopathy.org.au/research)

BY DR BETH YULE, SENIOR OSTEOPATH

Migraine is a prevalent and debilitating neurological disorder that affects approximately 14% of the global population. This article explores a comprehensive treatment approach that integrates manual therapy with other therapeutic modalities. By addressing the multifactorial nature of migraines – including physical, psychological, and nutritional factors – this method aims to not only alleviate symptoms but also enhance overall wellbeing. Understanding individual triggers and employing personalised strategies can lead to more effective management of this complex condition.

Migraine is a complex neurological disorder that affects approximately 14% of the global population, contributing to an immense public health burden. Headache disorders, including tension-type headaches, cluster headaches, and medication overuse headaches, impact around 40% of people worldwide. Despite its prevalence and debilitating nature, migraine is often poorly diagnosed, treated, and managed. It is the third leading cause of disability-adjusted life years (DALYs), trailing only behind stroke and dementia.1
The disproportionate impact on women, with a 3:1 ratio compared to men, underscores the critical need for increased awareness and tailored care. Migraine diagnosis is complicated by the lack of a definitive test and the condition’s multifactorial nature. Migraine is influenced by a range of factors, including physical issues such as neck and jaw problems, hormonal imbalances, sleep disturbances, mental health challenges, and nutritional deficiencies. Additionally, chronic pain is shaped by past experiences, personal attitudes and beliefs, support networks,
“The goal of treatment is to reduce TCC sensitisation, which, in turn, makes it harder to trigger a migraine attack”
coping strategies and more. Due to these diverse contributing elements and the complex nature of migraine, treatment approaches often focus primarily on managing the symptoms rather than addressing the individual’s comprehensive needs. However, because it is a complex condition with diverse contributing elements, we need a personalised approach rather than symptomatic treatment.
In this context, manual therapy and complementary strategies offer a promising avenue, not only in alleviating symptoms but also in addressing the unique factors that contribute to each person’s experience of migraine.
Migraine is a complex neurological disorder involving a cascade of events in the brain, leading
to symptoms such as throbbing head pain, nausea, sensitivity to light and sound, and visual disturbances. Although the exact cause of migraine is still under investigation, research highlights the central role of trigeminocervical complex (TCC) attacks.2,3
The TCC, a crucial relay centre, processes sensory and visceral information, especially nociceptive facial and head signals. When the TCC becomes sensitised, it can trigger intense headaches and neurological symptoms characteristic of migraine.
Understanding the TCC and its broader neurological context is key to appreciating why migraine management must be comprehensive. It’s about addressing the headache and the underlying neurobiological framework contributing to the condition. The goal of treatment is to reduce TCC sensitisation, which, in turn, makes it harder to trigger a migraine attack. This approach requires identifying and addressing each individual’s unique contributing factors, thus treating neurological and holistic aspects of the condition.
To simplify this understanding, consider the “bucket theory,” which illustrates how migraine is a threshold condition. Imagine a bucket representing your capacity to handle various migraine triggers and stressors. When this bucket overflows, a migraine is triggered. The factors that contribute to this overflow vary for each person. For instance, chronic poor sleep might fill part of the bucket, ongoing stress may add to it, and neck problems could bring it closer to the edge. When these triggers accumulate without intervention, even a minor additional factor, like a restless night, might overflow the bucket, leading to a migraine. By addressing these contributing factors, you create more space in the bucket. Improving sleep, reducing stress, addressing neck and jaw problems, and focusing on diet and hormonal balance gradually lowers the level of triggers within the bucket. Consequently, everyday challenges that might have previously triggered a migraine are now less likely to do so.
Thus, the goal of treatment is to keep the bucket as empty as possible. By addressing the root causes of what fills the bucket, individuals can raise their threshold for migraine triggers and gain better control over their condition. This article will explore key factors contributing to the migraine bucket, including the neck, jaw, stress, sleep, and essential vitamins and minerals. Understanding how these elements impact the individual and their migraine attacks allows osteopaths to provide comprehensive and personalised care, enhancing patient outcomes.
The relationship between the neck and migraine is deeply connected through the trigeminocervical complex (TCC), located at the C1-3 levels of the cervical spine. Joint restrictions in the upper cervical spine, particularly from C1 to C3, are commonly found in patients with headaches and migraine. Neck pain and dysfunction can exacerbate TCC sensitisation via peripheral
sensitisation, serving as both a trigger and a consequence of migraine attacks.2 In the context of the “Bucket Theory,” neck issues contribute to filling the migraine “bucket,” adding to the overall load of factors that can trigger an attack.
Neck pain is a frequent yet often overlooked feature of migraine, affecting up to 80% of migraine sufferers – more common than nausea, a symptom widely recognised as part of the migraine experience. 3 This prevalence highlights the critical role of neck dysfunction in migraine diagnosis and management. Research shows that those with migraines exhibit a higher incidence of neck pain compared to the general population, often accompanied by reduced cervical spine range of motion.2 A study revealed that 100% of tension-type headache sufferers and 94% of migraine patients experienced their familiar head pain reproduced and alleviated through examination of specific areas in the upper cervical spine.5 Additionally, migraine sufferers often present with forward head posture, reduced cervical muscle strength and decreased muscle endurance.6 Compared to individuals without migraines, their cervical muscles take longer to reach peak force and exhibit higher levels of antagonistic muscle coactivation.4 This dysfunction in the neck’s muscular and postural systems not only contributes to TCC sensitisation but also adds to the overall stress in the “bucket,” potentially increasing the frequency and severity of migraine attacks.
There is a significant relationship between temporomandibular disorders (TMD) and migraine, with migraine patients showing a higher prevalence of TMD and bruxism (teeth grinding). Nociceptive inputs from the temporomandibular joint (TMJ) can lead to increased sensitisation of the trigeminocervical complex (TCC), heightening migraine symptoms.9 The TMJ also influences the neck, further contributing to the development and perpetuation of migraines.
In the context of the Bucket Theory, TMD and bruxism can be seen as additional factors that fill the migraine “bucket.” When the TMJ is dysfunctional, it adds to the overall stress on the TCC and contributes to the accumulation of triggers. This means that in individuals with existing migraine triggers like stress or poor sleep, TMD-related discomfort or bruxism can push the “bucket” closer to overflow, making it more likely for a migraine attack to occur. Individuals with migraine are more likely to have tenderness at the TMJ and masticatory muscles.7 The pain threshold in the temporalis muscle is often reduced in migraine patients, making this region more susceptible to pain during an attack. Research also identifies TMD as a risk factor for chronic migraine, as nociceptive afferents from the TMJ feed into the same pathways responsible for migraine activation.3 By contributing to the overall burden on the TCC, TMJ dysfunction plays a significant role in both the frequency and intensity of migraine attacks, emphasising the importance of addressing these factors to keep the “bucket” from overflowing.
A range of treatment techniques can significantly reduce the frequency, duration and intensity of headaches and migraine attacks. Trigger Point Therapy targets myofascial trigger points (TrPs) in key muscle groups such as the upper trapezius, temporalis, suboccipital and sternocleidomastoid muscles. Attacks are often linked to increased active TrPs, contributing to TCC sensitisation and perpetuating symptoms.3 By relieving these trigger points, patients can experience a reduced frequency and duration of attacks.
Effective treatment of the neck and orofacial region combined has been shown to decrease migraine-related pain and disability greater than cervical treatment alone, leading to greater overall improvements in migraine management. Addressing night teeth clenching in those with chronic migraine has also been shown to help reduce attacks.8
Furthermore, one study found that 100% of tensiontype headache sufferers and 94% of migraine patients had their familiar head pain reproduced and reduced through examination and palpation of specific areas in the upper cervical spine. This finding underscores the importance of addressing the cervical spine through targeted manual therapy and exercises, as this region plays a pivotal role in the onset and perpetuation of headaches and migraine.5
Craniocervical exercises and manual therapy are particularly beneficial for individuals with headaches and migraine who often have weakened cervical muscles and reduced neck mobility. Strengthening exercises and manual therapy improve cervical spine alignment, posture and mobility, which can help decrease TCC sensitisation.4 These techniques have been found effective in reducing the frequency, duration and intensity of attacks, with improvements observed up to six months after treatment.3 Each technique plays a role in migraine management, targeting different aspects of the condition and contributing to overall symptom relief.
While manual therapy is a crucial component of migraine treatment, effective management requires a holistic approach. Research shows that combining manual therapy with other therapeutic modalities – such as rehabilitation exercises, and pain education – yields the best results.3 Integrating psychological approaches, like relaxation techniques or cognitive behavioural therapy (CBT), further enhances treatment outcomes. These combined strategies address both the physical dysfunctions and emotional stressors that contribute to chronic pain, significantly reducing the overall burden of migraine. By managing both the physical and emotional factors contributing to the “bucket,” practitioners can help patients more effectively decrease the likelihood of migraine attacks being triggered. As Dr. William Osler wisely noted, “It is much more important to know what sort of a patient has a disease than what sort of a disease a patient has.” This perspective underscores the importance of understanding the individual’s overall health and
“By addressing the root causes of what fills the bucket, individuals can raise their threshold for migraine triggers and gain better control over their condition”
lifestyle in addition to treating their symptoms, aiming to keep the “bucket” as empty as possible for better control of their condition.
Stress is a prevalent trigger for migraine attacks, affecting approximately 70% of individuals with the condition.11 The relationship between stress and migraine is complex, with stress both initiating and intensifying attacks. In patients with chronic daily headaches, high stress levels are commonly observed, further worsening the frequency and severity of migraines. Additionally, the stress of living with migraines – such as the unpredictability of attacks, missed obligations, and work concerns – creates a vicious cycle that perpetuates the condition.
“Just relax” or “decrease your stress” is common advice for migraine sufferers, but it often fails to address the physiological impact of stress. While many know they should manage stress, fewer understand how it directly contributes to migraine attacks. Stress triggers hormonal and physiological responses, increasing inflammation, disrupting sleep, and heightening pain sensitivity –each of which fills the migraine “bucket” further. Educating patients on this connection can empower them to take meaningful steps in managing stress, helping prevent it from pushing them closer to a migraine threshold.
Addressing stress is essential in comprehensive migraine management. While common stress-relief techniques include relaxation exercises, breathing practices, mindfulness, and cognitive-behavioural therapy, stress-relieving activities can vary greatly between individuals. Effective stress management tools may include activities such as reading, watching TV mindfully, taking a bath, walking, painting, listening to music, yoga, pilates, talking to a friend, boxing, journalling, baking, or gardening. In the context of the “Bucket Theory,” reducing stress is crucial as it lowers the overall level in the “bucket,” making it less

likely to overflow and trigger a migraine. By employing personalised stress management strategies, patients can often experience fewer and less intense migraine attacks, ultimately improving their overall wellbeing.
Sleep and migraine have a complex, bidirectional relationship. Migraine can negatively impact sleep, while poor sleep quality or sleep disorders can exacerbate migraine.13 Understanding and addressing this interplay is crucial for effective migraine management.
Sleep is a basic necessity for life, yet many people struggle to prioritise it despite knowing
“Sleep is a basic necessity for life, yet many people struggle to prioritise it despite knowing its importance”
its importance. This disconnect often results in inadequate sleep, which contributes to a range of health issues, including migraine. By understanding how sleep impacts the body and contributes to migraine attacks, patients can be better educated on the necessity of proper sleep and motivated to make necessary changes.
From the “Bucket Theory” perspective, inadequate sleep is a significant factor in filling the migraine “bucket”. Poor sleep quality or sleep disorders, such as insomnia, restless leg syndrome, snoring, and sleep apnea, contribute to the overflow of the bucket.13 This results in a lower threshold for triggering a migraine attack. When the bucket fills up due to sleep issues, even small additional stressors or triggers can push it over the edge, leading to an attack.
Conversely, improving sleep quality and ensuring a consistent 7-9 hours of sleep per night can help to decrease the level of triggers in the bucket. Many patients find that a good night’s sleep or a nap can ease an ongoing migraine attack and potentially prevent future ones.13 By addressing sleep issues effectively, individuals can reduce the amount of stress placed on their migraine threshold, thereby alleviating the frequency and severity of their attacks.
Addressing sleep is not just about advising patients to “get more rest” but also understanding how poor sleep contributes to migraine through physiological mechanisms. This insight empowers patients to take actionable steps to improve their sleep quality, thereby lowering the overall burden on their migraine bucket and improving their quality of life.
Improving sleep quality and establishing regular sleep patterns are important for reducing migraine frequency and severity. Strategies to enhance sleep include maintaining a consistent sleep schedule, creating a restful sleep environment, and addressing any underlying sleep disorders. By prioritising good sleep hygiene, patients can better manage their migraine bucket, reducing the overall burden and decreasing the impact of migraine attacks.

Stress induces the release of cortisol and adrenaline, hormones that prepare the body for a “fight or flight” response. Elevated cortisol levels can disrupt the balance of other hormones, leading to a range of physiological issues.
Increased heart rate and blood pressure:
Stress hormones cause an increase in heart rate and blood pressure, which can contribute to the physical strain of migraine attacks.
Altered brain function:
Stress dampens the activity of the prefrontal cortex , affecting attention, inhibition, and complex learning while enhancing the activity of the amygdala, which heightens emotional responses. This change in brain activity can contribute to symptoms such as brain fog, difficulty concentrating, lower mood and motivation during a migraine attack.
Digestive and reproductive system impact:
Stress diverts blood flow from the gastrointestinal tract, leading to poor nutrient absorption and potential overgrowth of harmful bacteria, further increasing cortisol production. Similarly, reduced blood flow to reproductive organs can contribute to hormonal imbalances. A decrease in certain nutrients, increased cortisol and sex hormonal imbalances can all contribute to an increase in migraine attacks.
Metabolic and immune system disruption:
Increased cortisol levels can lead to insulin resistance, decreased liver function (affecting hormone metabolism), a weakened immune response, and heightened inflammation. Insulin resistance impacts the sex and thyroid hormones as well, contributing to an increase in headaches and migraine, in particular hormonal headaches and migraine.
Impaired sleep:
Cortisol plays a crucial role in regulating sleep patterns. Elevated stress levels can disrupt normal cortisol production, leading to difficulties falling and staying asleep, which in turn can exacerbate migraine. Normally, cortisol levels spike in the morning to help wake you up, while they decrease as bedtime approaches to facilitate sleep. Disruptions in this cycle can lead to poorer sleep quality and more frequent migraine attacks.
(American Psychological Association., 2024), (Maleki, N. et al., 2012).
Supplements can play a significant role in managing migraines, complementing other therapeutic approaches such as manual therapy and lifestyle modifications. Integrating the concept of Bucket Theory, supplements can help lower the level of migraine triggers and thus prevent the migraine bucket from overflowing. Here’s a detailed look at key supplements and their impacts:
Supplement: Magnesium
Dosage: 600 mg or more daily.
Magnesium is a crucial supplement for migraine management. It is recommended at a dosage of 600 mg daily, and it serves several important functions. It is vital for the production of serotonin, a neurotransmitter involved in mood regulation and pain perception. Magnesium also acts as a natural muscle relaxant, helping to alleviate muscle tension that can contribute to migraine attacks. Additionally, it plays a role in hormonal regulation, including the thyroid and sex hormones, and supports healthy sleep patterns and overall mental well-being. Magnesium deficiency has
been linked to cortical spreading depression, a phenomenon associated with migraines and can impair serotonin function and neurotransmitter synthesis. By addressing magnesium deficiency, you help reduce one of the key factors contributing to the migraine bucket, thereby potentially lowering the frequency and severity of attacks.14,15
Supplement: B vitamins
Dosage:
B1: 300 mg daily.
B2: 400 mg daily.
B6: 80 mg daily.
B12: 500 µg daily.
Folic Acid: 2 mg daily.16
B vitamins also play a crucial role in migraine management. Specifically, vitamins B1, B2, B6, B12, and folic acid are involved in serotonin synthesis and regulation, which is vital for pain modulation. Vitamin B6 is beneficial for hormone regulation and can help manage menstrual migraine by balancing hormonal fluctuations. B vitamins contribute to reducing inflammation and lowering homocysteine levels, which, when elevated, can lead to neuronal overstimulation and increased migraine risk.16
Sleep plays a vital role in regulating various hormones crucial for overall health and wellbeing, which in turn can significantly impact migraine management.
It’s important to recognise how disruptions in sleep not only directly contribute to filling the migraine bucket but also affect hormonal regulation, further influencing migraine triggers. Here’s how key hormones are affected by sleep and their relevance to migraine:
Cortisol: Cortisol is crucial for regulating the body’s stress response and maintaining alertness upon waking. Disruptions in sleep can lead to abnormal cortisol production, with potential consequences for migraine sufferers. Elevated cortisol levels can contribute to increased sensitivity to pain and heightened migraine symptoms. Proper sleep helps maintain balanced cortisol levels, supporting overall stress management and reducing migraine triggers.
Leptin and ghrelin: These hormones regulate hunger, fullness, fat storage, and blood sugar levels. Poor sleep can disrupt leptin, leading to increased hunger and cravings. Elevated ghrelin levels, which promote appetite, can also contribute to weight gain and metabolic disturbances. Insulin
resistance, often exacerbated by poor sleep, can further interfere with leptin receptors, disrupting appetite regulation, as well as impacting the sex and thyroid hormones, and increasing migraine frequency.
Oestrogen and progesterone: These hormones are regulated by cortisol levels and play a role in migraine patterns, especially in women. Disrupted sleep and cortisol imbalances can lead to fluctuations in oestrogen and progesterone, potentially exacerbating migraine. Oestrogen is known to influence migraine susceptibility, and imbalances can trigger or worsen migraine attacks, particularly hormonal migraine attacks. Proper sleep helps regulate these hormones, helping to reducing migraine frequency and intensity.
Human Growth Hormone (HGH): HGH is essential for metabolism, immune function, muscle development, and protein synthesis. Poor sleep impairs HGH production, which can affect overall health and increase susceptibility to migraine. Balanced sleep supports optimal HGH levels, promoting better metabolic function and helping reduce migraine risk.
(Sleep Centers of Middle Tennessee., 2022), (Waliszewska-Prosół, M. et al., 2021).
Vitamin B2 (riboflavin) is frequently recommended for migraine due to its role in cellular energy production and its ability to reduce the frequency of migraine attacks. By optimising B vitamin levels, you effectively manage one of the factors filling the migraine bucket, contributing to a reduction in migraine symptoms.
Supplement: Vitamin E
Dosage: 400 IU daily for 5 days, starting 2 days before menstruation and continuing 3 days into menstruation.
Vitamin E is known for its anti-prostaglandin effects, which can be beneficial in reducing menstrual migraine. At a dosage of 400 IU daily for five days, starting two days before menstruation and continuing three days into menstruation, vitamin E inhibits the release and conversion of arachidonic acid, thereby reducing prostaglandin levels that are involved in migraine pathology. Additionally, vitamin E acts as a progesterone antagonist, which is relevant for menstrual migraine due to progesterone fluctuations during the menstrual cycle.18
Supplement: Vitamin D
Dosage: 1000-4000 IU per day.
Vitamin D is vital for helping to absorb magnesium, regulating of various bodily functions and brain function. Low vitamin D levels can lead to inflammation, increased neuronal sensitivity, altered brain chemical levels, and decreased magnesium absorption, all of which can contribute to headaches and migraines.19
Supplement: Melatonin
Dosage: Optimal dosage is still being researched.
Melatonin is a hormone the pineal gland releases at night and helps regulate sleep. While the optimal dosage is still being researched, melatonin supplementation may assist in preventing migraine attacks by protecting the brain from oxidative stress, regulating neurotransmitters, improving sleep and relieving pain.20
While each of these supplements has the potential to help ease migraine attacks, recommendations should be tailored to each patient’s specific symptoms and needs. It is not necessary for every patient to take all these supplements at once. Instead, a personalised approach based on individual assessments will help ensure the most effective management of migraine. Integrating these supplements into a broader treatment plan that addresses various aspects such as physical therapy, stress management and sleep quality will contribute to a more comprehensive strategy for reducing migraine frequency and intensity. By addressing the unique combination of factors contributing to each patient’s migraine “bucket,” practitioners can help optimise outcomes and support overall wellbeing.
Migraine is a multifaceted condition that requires a comprehensive approach to manage and mitigate its impact effectively. By understanding the central role of the trigeminocervical complex (TCC) and the concept of Bucket Theory, practitioners can appreciate how various factors contribute to the onset and persistence of migraine attacks.
The TCC, as a crucial relay centre for nociceptive information, underscores the importance of addressing both physical and neurobiological components in migraine management. The Bucket Theory provides a useful framework for conceptualising how different stressors and triggers fill up an individual’s “bucket” of migraine susceptibility. Each factor – be it musculoskeletal issues in the neck and jaw, stress, sleep disturbances, or nutritional deficiencies – can add to this cumulative load, increasing the likelihood of a migraine attack.
Effective treatment involves a holistic approach that integrates various modalities. Manual therapy techniques, such as trigger point therapy, jaw/ TMJ treatment, and craniocervical exercises, target physical dysfunctions and help reduce TCC sensitisation. Stress management strategies and improving sleep quality are equally critical, as they address the psychological and physiological stressors contributing to migraine frequency and severity. Additionally, supplements like magnesium, B vitamins, vitamin E, vitamin D, and melatonin offer potential benefits but should be recommended based on individual patient needs and symptoms.
By focusing on these diverse yet interconnected aspects, practitioners can develop tailored treatment plans address immediate migraine symptoms and raise the threshold for future attacks. Understanding and addressing the myriad factors contributing to a patient’s migraine “bucket” empowers practitioners to provide more comprehensive, effective care.
Ultimately, successful migraine management requires a balance of treating physical symptoms, managing stress, improving sleep and optimising nutritional intake. As Dr. William Osler wisely observed, understanding the whole person –beyond just their disease – is key to achieving the best outcomes. Through a thorough, individualised approach, practitioners can help patients gain better control over their migraine attacks and improve their overall quality of life.
Scan for references
To find the full list of references for this article, scan the QR code here.


BY PETER M C CANN
Musculoskeletal conditions are the leading global cause of disability and the third greatest burden of disease,1 with low back pain (LBP) being the largest contributor. Since first reported in 2012, LBP has remained the top cause of years lived with disability (YLDs) globally, accounting for 69 million YLDs in 2020.2 LBP ranks as the leading cause of disability in 126 out of 195 countries.1 The associated disability burden, measured in disability-adjusted life years (DALYs), has significant socioeconomic consequences, including lower educational attainment, poor health outcomes, reduced employment and increased poverty.
In Australia, musculoskeletal conditions are the second leading cause of disease burden after cardiovascular disease, with LBP contributing 20.1% of all YLDs or approximately 298,624 YLDs.3 The economic impact of LBP is significant, with annual costs estimated at AUD 4.8 billion.4 As the leading cause of lost productivity, particularly during individuals’ prime working years, there is a need to address the growing burden of LBP, particularly in resource-constrained regions of Australia.
Superficial heat is defined as the application of heat to elevate tissue temperature, primarily affecting tissues within 0.5 cm of the skin’s surface.5, 6 It is often recommended as a first-line treatment for acute LBP. Research indicates that at skin surface temperatures between 44 and 51 degrees Celsius, the risk of burns increases, with a one-degree rise in this range doubling the burn risk. Below 44 degrees Celsius, the risk decreases significantly, likely due to more effective cellular repair processes. Skin perfusion increases at temperatures near 40 degrees Celsius, with blood flow increasing 15 to 20-fold at 43 degrees
Celsius. Temperatures below 43 degrees Celsius are generally considered safe for prolonged exposure without causing skin damage.
Heat wraps are a non-pharmacological intervention commonly used for the management of LBP. They differ from wheat bags, heat packs, and hot water bottles by delivering continuous low-level heat, typically above 40°C, for extended periods. Heat wraps are the most researched and evidence-based method of superficial heat application in LBP management.7-9
The heat produced by heat wraps comes from a chemical reaction involving iron powder, salt, charcoal and mineral vermiculite, which when exposed to air, oxidise to release heat. This eco-friendly mechanism provides a convenient, long-lasting, low-level heat that does not require reheating. Unlike other heat sources, such as wheat bags, which provide high temperatures for a shorter duration and limit movement, heat wraps are lightweight, flexible and reusable, providing pain relief while enabling patients to remain active, aligned with clinical care guidelines that emphasise active treatment strategies over passive strategies to promote movement for LBP recovery.
A 2006 Cochrane review by French et al.6 provided moderate-level evidence supporting heat wraps as effective in reducing pain and disability. More recently, a 2021 narrative review by Freiwald et al.10 reinforced these findings, highlighting heat wraps as an effective, safe, non-pharmacological and cost-efficient intervention for pain relief in LBP.
Clinical care standards for low back pain were recently released by the Australian Commission on Safety and Quality in Health Care,11 guiding practitioners in the best

“The benefits of heat wraps for LBP have been documented in multiple clinical trials and systematic reviews”
practices for low back pain management. The clinical care standard recommends a non-pharmacological approach as the first-line treatment for low back pain with less reliance on pain medications and imaging. Within the clinical care standard, it is recommended to prioritise active strategies over passive strategies for low back pain, such as staying active and easing low back pain with heat wraps.
Heat wraps may be applied as a standalone intervention or in combination with other treatments, such as manual therapy and exercise, to improve LBP patient outcomes. Healthcare practitioners, including osteopaths, physiotherapists and chiropractors, commonly use superficial heat as an adjunct to manual therapy. Applications include conduction and convection methods, such as heat wraps and heat packs, which differ from conversion-based methods such as ultrasound, low-level laser therapy, or diathermy.
Heat wraps have been successfully used in major hospitals nationwide for over a decade, assisting in the management of LBP and other pain conditions. There are a growing number of virtual hospitals incorporating heat wraps into their model of care as they fit well into telehealth consultation settings. Multiple hospitalbased clinical implementation studies and trials have been conducted using heat wraps as a component of new models of care in emergency department management of low back pain presentations.
The benefits of heat wraps for LBP have been documented in multiple clinical trials and systematic reviews.7-9, 12, 13 In the short term, heat wraps have been shown to significantly reduce pain and improve functional outcomes. A study by Gianola et al.14 demonstrated that patients who received heat wrap therapy experienced a marked reduction in pain intensity and disability scores compared to those receiving standard care. Another study by Oliveira et al.15 highlighted the effectiveness of heat wraps as an alternative to pharmacological interventions, particularly opioids, which carry risks of dependency and adverse side effects.
While the short-term benefits of heat wraps have some supporting evidence,13 clinical trials exploring its longterm efficacy remain limited. Most studies have focused on the immediate or short-term outcomes following heat wrap application, typically lasting from a few hours to several days. However, some research suggests
that combining heat wraps with other interventions,16 such as exercise or manual therapy, may offer more sustained improvements in pain and function.
Heat wraps offer both physiological and psychological benefits in the management of LBP. Physiologically, heat application reduces musculoskeletal tension, increases tissue flexibility, and enhances blood flow, accelerating tissue healing.8 These effects reduce muscle stiffness, improve range of motion, and restore normal movement patterns, supporting overall functional recovery.
The increased circulation and relaxation of muscles further contribute to pain relief and improved mobility.
Psychologically, the warmth provided by heat wraps can reduce stress and elevate mood, offering comfort that helps ease the psychological burden often associated with chronic pain. This stress-relieving effect aligns with the biopsychosocial (BPS) model of pain management, recognising that psychological wellbeing can influence pain perception. The comforting sensation of heat reduces physical symptoms, assists in reducing anxiety and improving coping strategies and supports a holistic approach to managing LBP.
Heat wraps may be integrated into a comprehensive treatment plan that addresses LBP’s physical and psychological components. Osteopaths often use a multimodal approach to LBP management, combining manual therapies, exercise, and patient education with adjunct therapies, including massage, dry needling and superficial heat. A key treatment objective is to relieve pain, restore normal function and promote long-term recovery from injury.
Manual therapies, such as soft tissue manipulation, joint mobilisation, and myofascial release, can be enhanced by superficial heat. By reducing muscle tension and improving tissue flexibility, superficial heat may assist osteopaths in performing manual techniques, allowing for more effective treatment of musculoskeletal conditions. For example, heat application before soft tissue manipulation may relax tight muscles, making it easier to release trigger points and improve joint range of motion.
In chronic LBP cases, where psychological factors play a significant role, heat wraps may be valuable as part of a biopsychosocial approach to management. The BPS model of pain management recognises that pain is influenced by a combination of biological, psychological, and social factors and that effective treatment should address all of these components. Heat wraps provide physical and psychological relief, aligning with a holistic BPS approach to LBP management.
Effective LBP management requires appropriate management, of which a key component is patient education. Educating patients about the nature of their condition and the benefits of different treatment modalities is important to encourage treatment adherence and promote self-management while fostering self-efficacy. In the case of heat wraps, patients should be instructed on the correct and safe use of the heat wrap, including the low-level temperature, duration, and frequency of application.
Research has shown that when well-informed about their condition and treatment options, patients are more likely to experience better outcomes. A study by Oliveira et al.17 found that patient education, combined with heat wrap therapy, significantly improved patient satisfaction and adherence to treatment protocols. Guidance and information about applying heat wraps safely and effectively enable osteopaths to empower patients to manage their own LBP actively.
While heat wraps are generally safe, some considerations and potential risks should be addressed to ensure safe and effective application. The primary concerns with heat include superficial burns, excessive tissue heating, and improper use. Patients should be advised to avoid applying heat directly to damaged or inflamed skin and not use it in combination with topical creams or other heat sources, which could lead to superficial burns or skin irritation.
The duration of heat application and the temperature of the heat source is important. Heat wraps are designed to be warm but not excessively hot. Heat wraps are designed to maintain a consistent temperature of between 40 – 45 degrees to reduce risk of overheating. Osteopaths should provide clear instructions to patients on how to safely use a heat wrap to manage LBP. It is also important to consider relative contraindications to superficial heat application. Patients with medical conditions, such as peripheral neuropathy, advanced diabetes, or circulatory disorders, may have reduced sensitivity to heat and hence may not feel excessive heat. These patients should use heat wraps cautiously. Heat wraps should not be applied to areas with acute inflammatory signs such as infection, swelling or redness. Direct application over open wounds is also to be avoided, as it may exacerbate these conditions.
While heat wraps alone provide relief from LBP, they are most effective when used as part of a comprehensive treatment plan that includes other modalities. In osteopathic practice, heat wraps are often combined with manual therapy, exercise and ergonomic interventions to address the underlying causes of LBP and promote long-term recovery.
Applying a heat wrap before or after manual therapy, osteopaths may enhance treatment efficacy and patient comfort. For example, superficial heat application before joint mobilisation relaxes surrounding muscles, making it easier to achieve joint movement and improve range of motion.
Exercise prescription is frequently incorporated as a component of LBP management plans, particularly for patients with chronic or recurrent pain. Strengthening the muscles that support the spine, improving posture, and enhancing flexibility are all thought to contribute to reducing the risk of future episodes of LBP. Heat wraps may be combined with movement prescriptions to assist patients in warming their muscles before activity, reducing the risk of injury and improving overall exercise performance. Post-exercise or activity
heat wrap application may also help alleviate muscle soreness and promote recovery.
Although heat wraps are becoming established as an effective treatment option for LBP management, there are several areas where further research is needed. One of the primary gaps in the literature is the long-term efficacy of heat therapy in managing chronic LBP. While short-term benefits are well-documented, more research is needed to determine whether heat wraps can provide sustained pain relief over extended periods. Future research should explore the comparative effectiveness of heat wraps versus other heat methods, such as hot water bottles or electric heating pads.
There is a need for more studies examining the psychological benefits of heat wraps, particularly in patients with chronic pain conditions. While there is moderate level evidence to suggest that heat wraps can reduce anxiety and improve mood, more research is needed to fully understand the mechanisms underlying these effects and how they can be leveraged to improve patient outcomes.
Heat wraps offer a safe, effective and nonpharmacological option for managing LBP, with benefits that extend beyond simple pain relief. By modulating pain signals, improving tissue healing and promoting relaxation, heat wraps can play a role in reducing disability and enhancing the quality of life for patients with LBP. Heat wraps can complement manual therapies and other interventions, when integrated into osteopathic practice, contributing to a whole body and patientcentred approach to LBP management and recovery.
The application of heat wraps aligns with the osteopathic philosophy of treating the person, addressing both the physical and psychological components of pain. By educating patients on the correct use of heat wraps and incorporating them into a broader treatment plan, osteopaths can empower patients to manage their condition and promote longterm LBP recovery. While more research is needed understand heat wraps’ long-term benefits and optimal application fully, their role in LBP management is supported by current evidence and clinical practice.
Osteopaths continue to seek effective, safe, nonpharmacological, evidence-based interventions to address the growing burden of LBP. Heat wraps provide a valuable addition as a clinical tool to the osteopathic toolkit, improving LBP patient outcomes and promoting recovery from LBP by mitigating a barrier to movement.
Scan for references
To find the full list of references for this article, scan the QR code here.


THE OSTEOPATHY AUSTRALIA CONFERENCE, OCTOBER 2024
DR. GEORGE MICHAEL, DR. DAVID BIRLEY

Research suggests that pain, inflammation, stress and anxiety are strongly linked to poor sleep. Sleep modulates pain perception and inflammatory responses, and more restful sleep improves pain tolerance. While we know that diet, exercise, and healthy lifestyle choices are well-known contributors to good sleep, the sleep environment, including the mattress, is equally important. The right mattress can help relieve pressure points, align the spine and regulate body temperature. Optimising sleep has potential clinical implications in the management of musculoskeletal health.
The DrRest Sleep System aligns with osteopaths as clinicians and is endorsed by Osteopathy Australia. It was created by health professionals specifically for health professionals to use as a valuable adjunct to treatment.
“For over 12 years, I could not lie on my left side for more than a couple of minutes, as not only had I broken and dislocated my left shoulder, but I’d also prolapsed an L5 disc on the left. As a simple anecdotal test, on the very first night, I purposely laid on my left side to see how long I could do it. The end result is that for the first time in 12 years, I woke on my left side. After that, I was sold.”
– David Birley

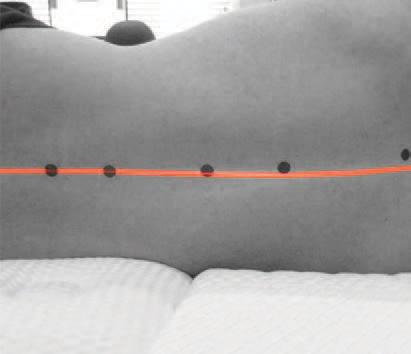
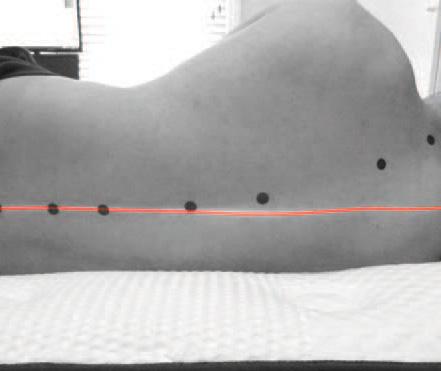
Through extensive patient trials and the expertise of sleep, respiratory and orthopaedic specialists, DrRest’s manufacturing journey saw 58 different mattresses over 10 years before the final patented design. It’s a significant investment into research and development to produce a unique product that works for every body type. The mattress is designed around optimal alignment and balanced interface pressure with a unique shoulder zone. The shoulder “sinks” into this adaptable zone to allow better sidelying alignment. Consider patients who have a right or left-side shoulder issue, or right or left-side neck degeneration, or a right or left-side disc prolapse or trochanteric bursitis... the DrRest mattress responds to the mass that is on it, in a way to help reduce the pain these patients experience, making it easier for them to find comfort and improve their sleep quality. DrRest is locally made and is achieving patient outcomes alongside business growth for practitioners. Become a DrRest partner or referrer to support patients’ sleep and musculoskeletal health easily within your practice.
The integration of a Technogel® shoulder zone is unmatched in supporting spinal balance and alignment, and is the cornerstone of quality sleep and recovery with the DrRest sleep system. Visit drrest.com.au or email info@drrest.com.au to learn more.

Artificial Intelligence (AI) has emerged as a powerful tool across industries, but its application in healthcare requires careful consideration. Generative AI, such as ChatGPT, offers potential benefits like streamlined documentation and enhanced efficiency but also presents risks such as inaccuracies, omissions, and privacy concerns.
Generative AI, specifically Large Language Models (LLMs) like ChatGPT, creates content by analysing vast amounts of training data and predicting the most probable sequence of words in response to a prompt. While the results can be impressive, LLMs lack true reasoning or understanding, making them prone to errors that are particularly critical in healthcare contexts.
1. Hallucinations: LLMs can fabricate information confidently, creating fictional patient histories, examination results, or treatment recommendations. For example, a referral letter generated by Chat a might include detailed but completely invented clinical observations.
2. Omissions: AI often struggles to summarise information accurately. Key details can be missed, especially in the middle of content. In healthcare, such omissions could result in incomplete patient records or miscommunication among practitioners.
3. Biases and data limitations: AI models are only as good as their training data, which may not always reflect diverse or specific healthcare needs, further limiting their reliability.
4. Privacy and compliance: Free tools like ChatGPT cannot guarantee compliance with local privacy standards such as the Australian Privacy Principles (APPs). Sensitive patient data sent to such platforms could be at risk. More secure options, like hosting AI on platforms such as Microsoft Azure, offer better compliance with regulations such as APPs, GDPR (General Data Protection Regulation), and HIPAA.
Cliniko is actively exploring AI applications but adopts a cautious, ethical stance to ensure tools meet healthcare’s rigorous standards:
• Reliability first: AI features for tasks like notetaking or report generation are being tested rigorously. Cliniko will only release tools that meet strict accuracy and safety benchmarks.
• Human oversight: Practitioners remain responsible for reviewing and verifying AI outputs. Automation is viewed as a support tool, not a replacement for professional judgement.
• Balanced innovation: Cliniko continues to focus on traditional development alongside AI, ensuring its solutions are reliable and effective with or without AI.
Cliniko integrates with third-party AI tools like Patient Notes, Heidi, and CliniScripts for note-taking, report writing, and summarising. These tools are purposebuilt for healthcare settings and can help practitioners save time. However, it is critical to review outputs carefully to address hallucinations or omissions, as no AI is currently 100% accurate.
AI is rapidly evolving and offers exciting opportunities for healthcare. However, its limitations mean that organisations like Cliniko must proceed thoughtfully. Cliniko’s guiding principles for AI are:
• Only implementing AI where its strengths outweigh its drawbacks.
• Ensuring AI-powered features are safe, effective, and beneficial to users and patients.
• Emphasising transparency and trust, rejecting AI as a gimmick and focusing on solutions that enhance practitioner workflows without compromising care quality.
AI will become increasingly embedded in healthcare practices, but its current flaws necessitate cautious adoption. Practitioners must remain vigilant, balancing the potential efficiency AI offers with the risks of misinformation, omissions, or data breaches. Cliniko is committed to leveraging AI responsibly, ensuring that any AI-powered features enhance your practice while maintaining safety, trust, and accuracy.
For a more in-depth feature visit: www.cliniko.com/ blog/news/our-current-stance-on-ai-at-cliniko/
Start your free 90-day trial today at cliniko.com/oa-member.
Key dates for your diary throughout the coming months.

5 FEB 2025 — 7:30PM AEST
Fascial connections: How old injuries contribute to pain and dysfunction
Presenter: Jack Williams
Register: Via CPD Hub
Link: osteopathy.org.au/events/fascial-connections-how-old-injuries-contribute-to-pain-and-dysfunction-
22 FEB 2025 9:00AM – 3:00PM
Fascial manipulation one day introductory workshop
Presenter: Jack Williams
Location: Melbourne Athletic Development
Physiotherapy
Register: Via CPD Hub
Link: osteopathy.org.au/events/fascial-manipulationworkshop--a-guide-to-the-human-fascial-system
SEMINAR VIDEO ON DEMAND
The lateral cranial nerves seminar
Presenter: Frank Willard
CONFERENCE VIDEO ON DEMAND
Systemic inflammation, depression and exercise in health and disease
Presenter: Frank Willard
Link: osteopathy.org.au/events/systemic-inflammation-depression-and-exercise-in-health-and-disease
ON DEMAND
The science and lived experience of CTE and post-concussion syndrome
Presenters: Michael Buckland, Alan Pearce, Andrea Miles & Rudi Gerhardt
Link: osteopathy.org.au/events/the-science-and-livedexperience-of-cte-and-post-concussion-syndrome
ON DEMAND
Conference 2024 clinical practice collection
Presenters: Amanda Hannaford, Andrew Timos & Donald Hunter
Link: osteopathy.org.au/events/conference-2024clinical-practice-collection
ON DEMAND
Perspectives on risk, compliance and practitioner distress
Presenters: Martin Fletcher & Susan Biggar
Link: osteopathy.org.au/events/perspectives-on-risk-compliance-and-practitioner-distress
ON DEMAND
Non-compliant practitioners, health data and AI insights
Presenters: Christie Boucher & Joel Friedlaender
Link: osteopathy.org.au/events/non-compliantpractitioners--health-data-and-ai-insights




Individually, we can achieve great things. But when you belong to a community swarming towards a common goal, that’s when we form our strongest line of defence, and the sky’s the limit.
Guild Insurance and Osteopathy Australia have partnered for over 20 years now
to protect the future of your profession. With us, you’ll be shielded by a policy created from unmatched insight into your profession, access to risk management materials to help you reduce the risk of a claim, backing from the industry body that stands up for Australian osteopaths, and so much more.
Together, we form the network that ensures Australian osteopaths don’t have to fly solo. Get the full picture of how you can be part of something bigger by visiting guildinsurance.com.au/osteopaths or calling 1800 810 213 today.
Don’t go it alone