Managing the pregnant patient
How to treat safely throughout pregnancy: an introduction
Endo for osteos
Endometriosis and allostatic load
Reasons to renew
Are you making the most of your membership?
Building connections
Osteopathy Australia heads to university Orientation Week
OSTEOPATHY AUSTRALIA MAGAZINE AUTUMN 2024
Always here, for 60 years.

Over 60 years ago, the Pharmacy Guild of Australia launched Guild Insurance – designed to protect and safeguard the pharmacy profession. Since then Guild has expanded the network of professionals we protect by forming partnerships with associations who represent a wide range of industries and the professionals who work within these fields.
Proudly partnering with Osteopathy Australia for over 22 years means we understand the importance of protecting you with more than just a policy.
With us, you’ll be shielded by a policy created from unmatched insight into your profession, access to risk management materials to help you reduce the risk of a claim, backing
from the industry body that stands up for Australian osteopaths, and so much more.
Find out how you can be part of something bigger by visiting: guildne.ws/OsteoLife or calling 1800 810 213 today.
Insurance issued by Guild Insurance Limited ABN 55 004 538 863, AFS Licence No. 233791 and subject to terms, conditions and exclusions. This information is of a general nature. Guild Insurance supports Osteopathy Australia through the payment of referral fees. Please refer to the policy wording and policy schedule for details. OST346694 Osteo Life Mag Ad 01/2024 Don’t go it alone

A promising start to 2024

I extend warm greetings to each of you in my capacity as the newly appointed President of Osteopathy Australia. It is with great pleasure that I reflect upon a promising start to 2024.
In the initial months of my presidency, a focus has been on re-establishing connections within our vibrant osteopathic community. Strengthening ties with critical stakeholders, including universities, the Australian Osteopathic Accreditation Council (AOAC), and the Osteopathy Board of Australia (OBA), has been of continued priority. Collaborative partnerships with these entities are indispensable for propelling the profession forward, ensuring alignment with industry standards, and enriching the overall landscape of osteopathic practice in Australia.
In February and March, the team at Osteopathy Australia greatly enjoyed being welcomed back into the universities to participate in Orientation Week celebrations across all four campuses. I sincerely thank the dedicated staff and senior students (as part of SOMA) who warmly welcomed Board members and the Osteopathy
“In my capacity as President, I hope that engagement and understanding of Osteopathy Australia’s initiatives reach new heights among our members”
Australia team. It was fantastic to meet the new students as they embark on their first steps in training to become the osteopaths of the future.
Equally exciting is the enrolment of the inaugural cohort of osteopaths in the recently established Graduate Certificate in Strength and Conditioning, offered in collaboration with Victoria University and the Western Bulldogs Football Club. This opportunity, a first of its kind for osteopaths in Australia, aligns with Osteopathy Australia’s quality practice framework and upon completion will allow participants to apply for advanced sports osteopath titling. Excitingly, 35% of the initial cohort are osteopaths. May this be the first of many new postgraduate opportunities moving forward.
The Board and I have convened multiple times, dedicating time to deliberating and strategising Osteopathy Australia’s plans in 2024 and beyond. Our most recent Board meeting is in Melbourne, and is happening as you are reading this issue of Osteo Life. This Board session is vital in providing a road map for enhancing the profession and guiding our CEO, Antony, and his team in pivotal projects contributing to the sustainability and growth of osteopathy in Australia for the next two years. As we progress into the year, the anticipation is building for the upcoming town halls scheduled
(continued on page 4)
16 Good hygiene, best practice guidelines
WELCOME 3
In this issue... 5 Osteopathy Australia News Careers 12 Exploring the vast horizon: career options for osteopaths beyond clinical practice Practice Management 13 Balancing clinical excellence and business success in osteopathy: a long-term perspective SHANE BUNTMAN 14 Can a patient under 18 provide informed consent? NEVENA BROWN & JAMES PAPWORTH Osteopathy Australia T (02) 9410 0099 E info@osteopathy.org.au W www.osteopathy.org.au osteopathyaustralia osteopathyau osteopathyaustralia osteoaust OSTEO LIFE is the quarterly magazine for Osteopathy Australia members. For enquiries, feedback, or to contribute, contact Communications on 02 9410 0099 or comms@osteopathy.org.au. For advertising enquires, email info@osteopathy.org.au. Editorial and Education Advisory Group Toby Barker, Amy Lawton, Adam Nicholson, Heath Williams Chief Executive Antony Nicholas Editor Rebekka Thompson-Jones Designer Stephanie Goh Sub Editor Adam Scroggy Advertising info@osteopathy.org.au Printed by Megacolour Printed on 100% recycled paper: one of our commitments to a sustainable future. OSTEO LIFE is published by Citrus Media www.citrusmedia.com.au
IBRAHIM SAMAAN Clinical
Endometriosis and allostatic overload: assisting with endo management
an osteopath’s perspective SARAH DRYBURGH
Osteopathic approach to managing the pregnant patient ASH BOLTON & DANIELA AIELLO
CPD Calendar Osteopathy Australia does not accept responsibility for any loss, damage, cost or expense incurred by reason of any person using or relying on the information contained in this magazine. The opinions expressed are those of the author and not Osteopathy Australia. All advertisements in this issue are paid advertisements. By registering with any company or affiliation mentioned in advertisements you will be sharing your personal information with the advertiser – please check their privacy policy. Osteopathy Australia takes no responsibility for the way personal information is used.
18
from
26
34
PRESIDENT’S MESSAGE
across the country. These gatherings provide a unique opportunity for members to engage directly with the Board and our CEO, Antony. During these interactions, we share insights into our ongoing initiatives and future plans on behalf of our members, fostering transparency and collaboration. I encourage all members to attend these meetings and remember; if you cannot attend in person, an online Zoom meeting will also be held.
Looking forward, I am delighted to announce the return of our Osteopathy Australia Conference, scheduled to take place in Sydney on 25-26 October. This conference, in collaboration with Osteopaths New Zealand and the Osteopathic International Alliance, promises to be a significant event. As our first major
In my capacity as President, I hope that engagement and understanding of Osteopathy Australia’s initiatives reach new heights among our members. Please explore our various social media pages on Instagram, Facebook, and LinkedIn to stay informed about the exciting and important tasks the association is working on daily to ensure osteopathy thrives within the Australian health landscape. We aspire for our members to take pride in belonging to the association and to advocate for the profession.
I am committed to promoting the professional development of our members and ensuring that Osteopathy Australia continues to be a leading force in advancing the standards and recognition of osteopathic practice. We are actively exploring opportunities for collaborations and partnerships to further enrich our members’ learning

members, stakeholders, and the entire
Osteopathy Australia community for welcoming me into the role and for your support. Together, we will continue to elevate the practice of osteopathy, advocate for its importance in healthcare, and empower our members to thrive in their professional journeys.
If you have any suggestions, feedback, or concerns, please feel free to contact me or any Osteopathy Australia team member. Your input is invaluable as we work together to shape the future of osteopathy in Australia.
mcooper.director@osteopathy.org.au
Osteopathy Australia acknowledges the Traditional Custodians and Elders of Country throughout Australia, and their connection to land, sea and community. We pay our respects to Aboriginal and Torres Strait Islander Elders, past, present and emerging.



4 WELCOME
Active Pain Relief TM Joint Stiffness Joint Stiffness Choose FlexEze Evidence-Based Heat Wraps Choose FlexEze Evidence-Based Heat Wraps Partner of: Partner of:
Osteopathy Australia news
OSTEOPATHY AUSTRALIA AIMS TO SUPPORT, ENHANCE AND PROMOTE THE PROFESSION. HERE’S A QUICK RECAP OF EVERYTHING OSTEO FROM THE PAST FEW MONTHS.

Notes from the Association
ANTONY NICHOLAS, CHIEF EXECUTIVE, OSTEOPATHY AUSTRALIA
Are you eager to have a greater influence on Osteopathy Australia’s direction, projects, and priorities? Your insights and contributions are invaluable as we embark on a strategic journey to shape the association’s future. Let’s be open, engaged and collaborative to ensure our direction aligns perfectly with the profession and your needs or aspirations. We want to craft a future Osteopathy Australia that truly serves osteopathy and you!
Member engagement and input play a pivotal role in the development of strategic plans by Osteopathy Australia and our role within the Australian healthcare environment. This importance stems from the unique perspective and insights you, as members, bring to the table. Your experiences on the front line enable us to craft strategies that are not only ambitious, but also grounded in the practical realities of osteopathic healthcare delivery.
In Australia’s complex healthcare landscape, characterised by its mix of public and private sectors, various state and federal health departments or schemes,
and a strong regulatory framework overseen by agencies like the Australian Health Practitioner Regulation Agency (Ahpra), understanding the nuances of regulatory compliance, patient care standards and industry innovation is essential. Through their engagement, members provide a rich source of knowledge and feedback on these topics, enabling us to align our strategic objectives with your current needs and consider the future challenges for osteopathy.
Moreover, we like to have strong member engagement as it helps facilitate a sense of ownership and commitment among osteopaths, enhancing our ability to mobilise members in promotion or advocacy efforts, professional development initiatives, and health campaigns. Plus, we exist to help members with the services they need to make practice easier. This active participation is crucial in a field as dynamic as osteopathy and healthcare, where advancements, policy shifts, and societal health needs evolve rapidly. That’s why we provide many platforms to post, chat and ask questions.
That strong engagement is why hundreds of osteopaths continually contribute to the association’s work. They are on the Board, on existing committees or
working groups, developing articles, podcasts or CPD, and more recently, our call for volunteers on working groups such as CPD, communications and marketing, aged care, or the academic research committee. The team at Osteopathy Australia is dedicated to turning the visions and aspirations of osteopathic leaders into reality, paving the way for a vibrant future in osteopathy.
Engaging members in the strategic planning process also ensures the process hears the diverse voices within Australia’s multifaceted osteopathy sector. This diversity of thought and experience enriches strategic planning, leading to more innovative and inclusive outcomes. By prioritising member engagement, we can foster a more collaborative and resilient community better equipped to meet the challenges of tomorrow.
Osteopath involvement with planning and decision-making is integral to how we operate. Our committees, our Board, discussion forums, town halls and online consultations regarding day-to-day and strategic planning are critical components in ensuring our projects, services and plans are relevant, responsive and reflective of the collective wisdom and ambitions of the osteopathic healthcare community.

NEWS 5
Disability Royal Commission –what I need to know as an osteopath
The Disability Royal Commission (DRC) made 222 recommendations to improve policies and practices. These recommendations aim to foster a more inclusive and just society that supports the independence of people with disability and is free from violence, abuse, neglect and exploitation. Osteopaths and all allied health professionals can make a big difference by implementing these recommendations. By doing so, the changes will make accessibility, inclusivity, and quality of life better for people with disability. Focusing on independence and safeguarding aligns with the broader goal of allied health of promoting wellbeing and quality of life for everyone.
A Royal Commission is an independent public inquiry and is the highest form of inquiry on matters of public importance. The DRC conducted a thorough investigation from April 2019 to September 2023, resulting in the final report, which includes 12 volumes with key findings and recommendations.
Osteopathy Australia is committed to ensuring our members can work with their clients to create a place where people with disability can enjoy all human rights and freedoms just like everyone else.
In this brief overview, we highlight some of the key volumes, findings and recommendations that are most important to our members.
EXECUTIVE SUMMARY
The DRC highlights collaboration among service providers and makes key recommendations in training, personcentred care and customised care plans.
VOLUMES OVERVIEW
Volumes 1 and 2 are the personal stories of people with disabilities. Volumes 3 to 12 focus on key issues and recommendations, highlighting healthcare access (Volume 6) and disability services (Volume 10).
Volume 1 – Voices of People with Disability: It shares the stories of 9,000 individuals living with disability and their
supporters, aims to raise awareness, offers insights into the daily challenges faced and advocates for creating safer and more inclusive communities.
Volume 3 – Nature and Extent of Violence, Abuse, Neglect and Exploitation: It highlights the need for better protection and support, especially for women and those living with psychological and intellectual disability, as well as those known to perpetrators.
Volume 4 – Realising the Human Rights of People with Disability: It focuses on Australia’s commitment to promoting the human rights of people living with disability. It recommends a more robust legal framework and the enactment of an Australian Disability Rights Act (DRA).
Volume 5 – Governing for Inclusion: It sheds light on the importance of national strategies, policies and leadership for equality and inclusion, advocating for the creation of a National Disability Commission (NDC) and the review of disability strategies.
Volume 6 – Enabling Autonomy and Access: It explores breaking barriers to independence, addressing concerns including access to information, decision-making and healthcare.
Key recommendations: Suggests changes to guardianship laws, improved healthcare coordination and opposes unnecessary procedures; Recognises the important role of accessible information and communication for people living with disability; Calls for updated guardianship and administration laws, focusing on supported decision-making; Addresses issues in the healthcare system, focusing on training for health professionals and the need for better coordination in providing accessible and inclusive healthcare services;
Expresses concerns about the overuse and misuse of restrictive practices, emphasising the need for training and awareness; Advocates for changes to ban unnecessary procedures like involuntary sterilisation.
Key recommendations for improving independence and access for osteopaths: Develop a national plan for promoting accessible information and communications in collaboration with people living with disability and their representative organisations; Increase the number and quality of Auslan interpreters and train interpreters in disability awareness; Improve transparency, collection of data, and advocacy for supported decision-making.
Volume 9 – First Nations People with Disability: It addresses systemic barriers faced by First Nations individuals with disability, while recommending the implementation of culturally sensitive support services, collaboration and awareness initiatives.
Volume 10 – Disability Services: It explores evidence of maltreatment in disability services and suggests steps for integrating human rights, support coordination and independent advocacy. Emphasises the integration of human rights into disability services, focusing on the responsibility of service providers. It recommends that support coordination providers should not provide other funded supports, advocating for separation of roles.
It highlights the value of independent advocacy for those at risk, promoting collaboration with NDIS participants and advocacy organisations.
Key recommendations for improving disability services:
Implement a capacity-building program to help disability service providers integrate human rights into their services;
6 NEWS
“Osteopathy Australia is committed to including these recommendations in our ongoing policy and advocacy efforts, ensuring members are educated and remain at the forefront of disability care”
Ensure separation of roles for support coordination providers, avoiding conflicts of interest; Include funding for support coordination in the NDIS plans of participants at risk of violence, abuse, neglect or exploitation; Examine the quality and consistency of support coordination, focusing on specific groups of people living with disability; Promote the value of independent advocacy for NDIS participants at risk when reviewing complaints and reportable incidents.
Volume 11 – Independent Oversight and Complaint Mechanisms:
It highlights the need for independent reporting of violence and abuse and suggests nationally consistent legislation, safeguards and complaint reporting.
Volume 12 – Beyond the Royal Commission:
It suggests practical ways to implement its recommendations into action, calling for high-quality data, research and a consistent approach to disability information nationwide.
ALLIED HEALTH’S ROLE
Allied health professionals, especially those in healthcare and disability services are pivotal in implementing the DRC’s recommendations. They significantly contribute an important role in preventative health by increasing an
individual’s functional capacity to prevent deconditioning and falls.
KEY RECOMMENDATIONS FOR ALLIED HEALTH PROFESSIONALS
Volume 6 – Enabling Autonomy and Access: Emphasise accessible information and communication; Advocate for reforms in guardianship and administration laws; Collaborate to address the overuse of restrictive practices and involuntary sterilisation.
Volume 10 – Disability Services: Support the NDIS Quality and Safeguards Commission’s capacity-building program; Advocate for separating support coordination providers from other funded supports; Promote independent advocacy for those at risk, connecting NDIS participants with suitable organisations.
CONCLUSION
Osteopathy Australia is committed to including these recommendations in our ongoing policy and advocacy efforts, ensuring members are educated and remain at the forefront of disability care. Collaboration with other peak bodies, the NDIS and the National Disability Insurance Agency (NDIA) is essential for continuous improvement in
the quality of care and support available to the disability community of Australia.
Osteopathy Australia would like to thank the commissioners who worked extremely hard to assemble this report, and the individuals, families, supporters and providers who shared their stories. We look forward to implementing the recommendations in our policy and advocacy work as a peak allied health body. The comprehensive approach outlined in these volumes emphasises the importance of accessible information, person-centred care, and systemic change required to create a more inclusive and supportive environment for individuals living with disability. Advocacy, collaboration and a commitment to human rights are key elements in making positive changes in disability services and healthcare access.
Osteopathy Australia acknowledges Australia’s First Nations peoples as the Traditional Custodians of the lands, seas and waters of Australia and pays respect to all First Nations Elders past, present and emerging. We pay our respects to all First Nations people with disability and recognise the distinct contributions they made to the outcome of the inquiry.
We acknowledge people with disability who fought and campaigned long and hard for the establishment of the Royal Commission. We recognise the courage and generosity of people with lived experience of disability who share their knowledge and experiences of violence, abuse, neglect and exploitation with the Royal Commission.
NEWS 7
CELEBRATING EXCELLENCE IN OSTEOPATHY:
Dr Benjamin James Field (Osteopath) receives prestigious honour
Dr Benjamin James (BJ) Field (Osteopath) has been honoured with the Order of Australia for his contributions to osteopathy and his work to strengthen the regulation of the profession.
As the founder of Canberra City Health Network, a former President of Osteopathy Australia and a board member of the Australian and New Zealand Osteopathic Council, his service underscores his commitment to advancing our profession.
BJ’s dedication extends to educating future osteopaths, highlighting his commitment to professional excellence and mentorship in the osteopathic community. Osteopathy Australia welcomes this recognition of industry leaders.
Medal of the Order of Australia (OAM) in the General Division for service to osteopathy:
Health Sector
Founder, Canberra City Health Network, since 2004, and Director, 2004-2022;
Member, Osteopathic Programme Advisory Committee (OPAC), Southern Cross University, 2016-2017; Board Member, Australian and New Zealand Osteopathic Council, 2008-2010; Advisory Member, National Registration and Accreditation Scheme, Council of Australian Governments, 2008-2010; Member, Australasian Conference of Osteopaths Registration Boards, 2008-2010; Accreditation Team Member, University of Western Sydney, 2007-2009.
Osteopathy
President, Osteopathy Australia ACT, 2005-2008, and Member, 2003-2008; Deputy Chair, Osteopaths and Chiropractors Registration Board of the Australian Capital Territory, 2007-2010;

National President, Osteopathy
Australia, 2008-2010, and Immediate Past President, 2010-2011; Board Member, Osteopathy Board of Australia, 2012-2013; Canberra Institute of Technology; Industry Advisory Board Member, Australian Capital Territory Massage Skills and Training Group,2016-2018; Clinical Supervisor, Massage Therapy Clinic, 2003-2004; Former Lecturer, Massage Therapy course, 2000s.
Sport
Consultant, Canberra Raiders, since 2005;
Junior Soccer Coach, Radford College, 2017-2020; Majura Football Club, 2019; North Canberra Futsal, 2014-2016; Awards and Recognition including Outstanding Contribution Award, Australian Osteopathic Association, 2010.
Celebrating Osteopathy Awareness Month in April
April was a special month for Osteopathy Australia: Osteopathy Awareness Month, where we shine a spotlight on osteopathy and its benefits to whole body health and wellbeing. With a suite of activities and resources, the month is an invitation for members to highlight how osteopathy can enhance wellbeing.
Osteopathy, with its unique whole body approach, offers more than just pain relief; it’s a path to understanding the intricate connections within our body and harnessing its natural ability to heal. In April, Osteopathy Australia demystifies the practice of osteopathy, showcasing its benefits in managing and preventing pain, enhancing mobility, and promoting overall health.
The campaign is rich with opportunities for members and the public alike. For professionals, it’s a chance to engage with communities, share knowledge, and highlight the importance of osteopathic care. The suite of marketing materials and suggested activities aims to empower you and provide
you with content to promote both yourself and the profession to your local community.
For the public, Osteopathy Awareness Month is an educational journey. Through insights and first-hand accounts, individuals discover the transformative impact osteopathy can have. The campaign encourages people to reconsider their relationship with pain and mobility, advocating for a life where discomfort is not the norm but an exception.
As part of the broader initiative, Osteopathy Australia has curated a collection of digital assets, from social media graphics to patient email banners, aimed at fostering a deeper understanding and appreciation of osteopathy. This effort not only amplifies the reach of osteopathic messages, but also strengthens the community of practitioners and patients alike.
Osteopathy Awareness Month is an extension of World Osteopathic Healthcare Week which took place on 15-21 April. Dedicated to celebrating and promoting osteopathy, this month is about sharing your knowledge with a wider audience.
5 reasons to get involved
1 Amplify osteopathy awareness as a profession to generate new business
2 Easy, ready-to-use content for your social media – saving you time
3 Fresh blogs and resources to share, aimed at educating patients on the value of osteopathy –we want to make your busy life easier
4 Unite the profession for a cause while showcasing the important work we do
5 Connect with other osteopaths and encourage community engagement
Let’s embrace this opportunity to learn, share, and celebrate the wonders of osteopathy.
8 NEWS
OSTEOPATHY AUSTRALIA MAKE THE MOST OF YOUR MEMBERSHIP

ADVOCACY AND POLITICAL LOBBYING
Osteopathy Australia works hard to gain professional rights and recognition for osteopaths in Australia through advocacy and political lobbying.

We promote osteopathy in the media, social media and throughout the community to generate positive publicity and raise the public’s awareness and understanding of the profession. PROMOTION

ADVANCED AND EXTENDED PRACTICE RECOGNITION PROGRAMS
Formal recognition program for osteopaths with additional qualifications and advanced skills and experience or osteopaths who have demonstrated extended knowledge and skill.

HR PORTAL
The 1300 143 602 hotline is a dedicated service for you, whether an associate, employee or business owner, to seek direct advice. A comprehensive online library of technical resources is available exclusively for members; including manuals, policies and template contracts and letters.
FIND AN OSTEO
Your clinic is listed in our online directory, helping patients find you. Membership to Osteopathy Australia signifies a standard of professionalism and ethics beyond registration requirements.

OSTEO LIFE
An exclusive quarterly publication that covers the latest news, trends, policies and events for industry professionals. The magazine is available only to Osteopathy Australia members.

PROFESSIONAL ADVICE, INFORMATION AND GUIDANCE
The 1800 467 836 number provides phone guidance and information to our members. We also communicate with hundreds of potential patients every week across Australia.

CPD HUB
Members can access online, print and face-to-face resources including webinars, eLearning, workshops and events, podcasts, the National Conference and Osteo Life magazine. You get to learn your way.

GUILD PROFESSIONAL INDEMNITY INSURANCE
Take advantage of enhanced professional indemnity insurance at a reduced rate. The enhanced policies include the added benefit of legal advice, public liability and “run off” cover.

MEMBER REWARDS PROGRAM
You and your family can save all year on lifestyle, leisure, and financial services with offers from Coles, Woolworths, The Good Guys, JB Hi-Fi, Specsavers, and more. Access discounts on movie tickets, eGift cards, sports, hotels worldwide, and travel.

PARTNERSHIPS
Save hundreds on our member exclusive partnerships that cover a range of courses and products essential to your clinical and professional needs.

ADVERTISING
This simple step can open doors to more patients and growth for your practice. Adopting these tips not only enhances your professional standing, but also
Take advantage of free or discounted advertising options among our wide network. Be featured or browse opportunities on our classifieds web page, Osteo Life publication or regular eFlyers that are distributed among thousands of contacts.
strengthens the osteopathy community as a whole. Let’s continue to uplift each other and promote the invaluable work we do in the health sector.
For more information about membership renewals: www.osteopathy.org.au
NEWS 9
| 02 9410 0099 | membership@osteopathy.org.au
Building connections and shaping futures through uni orientation weeks

In February and March, Osteopathy
Australia had the privilege of participating in student orientation weeks across several prestigious universities. Our journey began on 12 February at Victoria University’s vibrant campus, followed by visits to Southern Cross University (SCU) Lismore on 27 February and SCU Gold Coast Campus on 28 February, culminating in a visit to RMIT University on 6 March. These engagements provided us with a fantastic opportunity to meet face-to-face with the next generation of osteopaths, along with the dedicated university staff who play such a pivotal role in their education. A big shout-out to all the new students we met! Your enthusiasm and passion for embarking on a career in osteopathy were truly inspiring. To the university staff, we extend our heartfelt thanks for your warm welcome and the incredible work you do in shaping the future of healthcare education. Your commitment to excellence is evident and greatly appreciated.


We would also like to acknowledge our sponsors, who played a crucial role in making our participation in these events possible. A special thanks to Guild Insurance, FlexEze Heat Wrap Therapy, DrRest, and OPC Health. Your support not only contributes to the success of these orientation weeks, but also demonstrates your commitment to the osteopathy profession and the broader healthcare community.
Osteopathy Australia’s presence at these universities underscores our commitment to supporting the education and development of future osteopaths. Engaging with students and staff in person, after the challenges posed by COVID, has reinforced the value of community and connection within our profession. These face-to-face interactions are invaluable, offering a unique opportunity for students to learn, connect and be inspired by the possibilities that a career in osteopathy offers.
We look forward to continuing our support for osteopathy students and


the educational institutions that are nurturing the next generation of healthcare professionals. Together, we are not just building careers; we are shaping the future of health and wellbeing.

10 NEWS

Understanding Chronic Pain Management

The benefits of saffron and PEA and their influence on the endocannabinoid system
Chronic pain is on the rise and sufferers are more likely to experience psychological concerns such as depression, anxiety and sleep disturbances. PEA and saffron have the unique ability to influence the endocannabinoid system and in turn, manage chronic pain and its associated symptoms.
Chronic pain is persistent pain lasting more than 3-6 months. Over the past 10 years, general practitioners have seen a 67% rise in patients experiencing chronic pain.1
Chronic pain is complex and it is often reported that chronic pain sufferers concurrently experience psychological distress and symptoms such as poor mood and sleep.1 The body is equipped with a variety of mechanisms and systems to alleviate and resolve pain, including the endocannabinoid system. Compounds, such as palmitoylethanolamide (PEA) and Crocus sativus (saffron), have the unique ability to influence the endocannabinoid system and in turn, manage chronic pain and its associated symptoms. The endocannabinoid system is involved in the modulation of pain and inflammation. Cannabinoid 1 (CB1) receptors are located within the brain and central nervous system whilst cannabinoid 2 (CB2) receptors are found primarily in peripheral tissue and cells of the immune system.5 Endocannabinoids are produced endogenously or can be supplied exogenously to manage pain. Whilst PEA is not a cannabinoid itself, it is a naturally occurring endogenous fatty acid that is produced in response to inflammation or injury. In conditions such as chronic pain, it has been noted levels have been altered, highlighting the benefit of PEA supplementation.3
PEA works through:
• Enhancing tissue levels of anandamide, a cannabinoid that acts upon CB1 and CB2 receptors, providing analgesic properties.6
• An affinity to PPAR-α receptors, which reduces inflammation and the secretion of pro-inflammatory signalling molecules.6

• An affinity to receptors GPR55 and acts to desensitise TRPV1 which is involved in the sensation of pain and heat.7
• Inhibition of mast cell degranulation and subsequent histamine release whilst controlling glial cell behaviours.3
Ultimately, PEA provides analgesic, anti-inflammatory and neuroprotective benefits Due to its fatty nature, PEA has poor absorption. Levagen+ is considered a superior form of PEA which utilises LipiSperse® technology to increase bioavailability.6
Saffron is a notable adjunct therapy to PEA as chronic pain sufferers are more likely to experience psychological concerns such as depression, anxiety and sleep disturbances.1 Saffron has been shown to provide anti-inflammatory, antinociceptive, immunomodulatory, analgesic, antidepressant and anxiolytic effects.8
Saffron works through the following mechanisms:
• Attenuates pro-inflammatory mediators such as TNF-α and IL-6.8
• Reduces eosinophils, neutrophils and lymphocytes, leading to a down-regulation of leukotrienes, prostaglandins, cytokines, ROS and NO.8,9
• Partial agonism and selective desensitisation of the TRPA1 channel.10
• Antioxidant activity reduces oxidative damage by attenuating endogenous ROS.11
• Reuptake inhibitor of dopamine, serotonin, and norepinephrine.11
For optimal patient results, choose a standardised form of Saffron such as affron®. affron® is standardised by HPLC (high performance liquid chromatography) to Lepticrosalides® and has been shown to support mood, relaxation and sleep,12 critical for chronic pain sufferers.







REFERENCES UPON REQUEST. FOR PROFESSIONAL REFERENCE ONLY www.bioceuticals.com.au ©BioCeuticals 2023 ACN 062 851 683 For more information on managing chronic conditions, visit fxmedicine.com.au Your gateway to the latest research and information in functional and evidence-based complementary medicine.
Proud Partner of: opchealth.com.au Contact Us
Exploring the vast horizon: career options for osteopaths beyond clinical practice
Osteopathy, with its whole person approach to health and wellbeing, provides a solid foundation for practitioners to venture into a range of professional avenues. Shortly, Osteopathy Australia will be releasing more detailed information and guides on the career pathways. However, below provides you with an overview of the diverse career pathways.
While we know most osteopaths enjoy working in the conventional clinical setting, osteopaths possess the unique ability to apply their knowledge and skills in multiple fields, offering a range of opportunities for you to consider:
1 PRIVATE PRACTICE/ BUSINESS OWNER
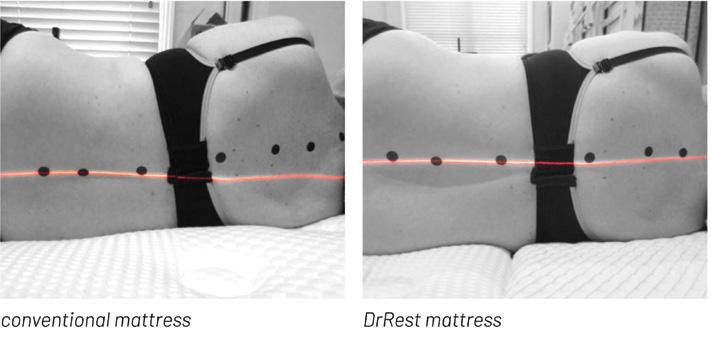
Osteopaths seeking autonomy and innovation can blend private practice with entrepreneurship. This approach allows for specialisation in fields such as women’s health, paediatrics or sports osteopathy while also exploring business ventures like wellness centres or health product development – see the DrRest article on page 32. This career path combines osteopathic care with business acumen, enabling practitioners to innovate in both patient care and health-focused entrepreneurship.
2 AGED CARE
Osteopaths can play a crucial role in supporting the health and mobility of the elderly. Working in aged care facilities or through home visits, osteopaths can significantly improve the quality of life for older adults, focusing on pain management, mobility, and functional independence.
3 DISABILITY SUPPORT
Osteopaths can offer a person-centred approach to the multidisciplinary support provided to individuals living with disability, including NDIS participants. Osteopaths working within this space can offer reasonable and necessary capacity-building supports
to help improve participants’ functional capacity that aligns with their individual goals. An osteopath’s role is pivotal in enhancing the day-to-day functioning and overall life experience of people living with disability. The Osteopathy Australia team is on hand to help you navigate the NDIS – just give us a call.
4 OCCUPATIONAL REHABILITATION
Osteopaths can work as a workplace/ occupational health rehabilitation consultant in certain states (VIC, NSW, QLD, TAS and Commcare – national scheme) where they will employ their clinical knowledge to assess and address the physical, psychological, social, environment and organisational risk factors that might affect a worker’s ability to recover and return to duties.
5 RESEARCH AND ACADEMIA
Passionate about developing evidence or nurturing the next generation? Osteopaths can pursue careers as educators or lecturers in universities and colleges, sharing their knowledge and experience with aspiring osteopathy students. This role involves not only teaching, but also contributing to curriculum development. For those with a keen interest in contributing to and building the evidence base for osteopathy, opportunities in research allow osteopaths to investigate new treatment methods, contribute to scientific knowledge and develop innovative healthcare solutions. Research opportunities aren’t limited to universities, with industry partners often looking for health researchers to be involved in the development of health-informed products or services.
6 SPORTS AND ATHLETICS
With an in-depth understanding of musculoskeletal health, osteopaths can become invaluable assets to sports teams and athletes. Working as sports trainers and therapists, they can help optimise
performance, provide injury prevention strategies, and facilitate recovery processes, ensuring athletes remain at the top of their game.
7 OCCUPATIONAL HEALTH
This field merges the principles of osteopathy with those of the workplace where you will aim to enhance employee wellbeing, reduce workplace injuries and risks, and foster a safe and healthy workplace.
8 CORPORATE WELLNESS
The corporate world is increasingly recognising the importance of employee wellbeing. Osteopaths can lead or contribute to workplace health programs, offering ergonomic assessments, stress management strategies and wellness workshops to improve the overall health and productivity of the workforce.
9 HEALTH JOURNALISM, SOCIAL MEDIA INFLUENCING
Alongside private practice, and for those with a talent for writing, opportunities in health journalism, blogging, or authoring books on osteopathy and whole-person health can be a fulfilling way to share knowledge and insights with a wider audience, influencing public understanding and appreciation of osteopathic medicine.
10 DIGITAL HEALTH INNOVATION
The growing field of digital health presents opportunities for osteopaths to contribute to the development of health apps, online therapy platforms, and telehealth services, applying their expertise to enhance digital healthcare solutions.
Each of these career paths gives a top line overview of the versatility of osteopathy, highlighting opportunities to inspire change, foster wellbeing and make a meaningful impact beyond traditional practices.
12 CAREERS
Balancing clinical excellence and business success in osteopathy: a long-term perspective
In this edition of Osteo Life, Shane Buntman discusses why he believe our industry has leaned too far towards celebrating practitioners with busy patient lists (business outcomes) rather than those excelling in their craft (clinical outcomes).
I want to emphasise that a busy list should result from excelling in your craft, not just a successful marketing strategy. True celebration should stem from clinical outcomes that contribute to our patients’ long-term health.
Understanding the importance of business success, it’s essential not to overlook the development of exceptional practitioners who deliver the highest quality of osteopathy.
In osteopathy, balancing clinical excellence and business success is crucial. Osteopaths, dedicated to their craft, may find themselves torn between developing superior clinical skills and maintaining a busy practice. This article explores the benefits of prioritising clinical expertise over focusing solely on business outcomes.
THE DILEMMA
Osteopaths face the challenge of managing the demands of a thriving practice while honing their clinical skills. The temptation to prioritise quantity over quality in patient care can be strong, particularly in an era where the business side of healthcare is becoming increasingly competitive. However, the long-term consequences of such an approach can impact both the practitioner and the patients.
DEVELOPING CLINICAL EXCELLENCE
Clinical excellence in osteopathy involves a commitment to continuous learning and refinement of skills. Osteopaths who invest time and effort in staying abreast of the latest research, attending relevant workshops, and seeking mentorship from experienced practitioners position themselves for long-term success. Building a foundation of clinical
excellence not only enhances the quality of patient care, but also fosters trust and loyalty among patients.
PATIENT-CENTRIC CARE
Prioritising clinical outcomes involves placing the patient at the centre of the treatment process. Osteopaths can cultivate an environment where patients feel valued and understood by focusing on thorough assessments, accurate diagnoses and personalised treatment plans. Patients who experience positive clinical outcomes are more likely to return and recommend the practice to others, fostering a sustainable and growth-oriented business model.
WORD OF MOUTH AND REPUTATION
In the healthcare industry, reputation is paramount. Osteopaths prioritising clinical excellence contribute to the positive wordof-mouth marketing that can significantly impact their practice. Satisfied patients are more likely to share their success stories with friends and family, creating a steady stream of referrals. A reputation for clinical excellence can set a practice apart in a crowded market and serve as a foundation for long-term success.
ETHICAL CONSIDERATIONS
Prioritising clinical outcomes over business outcomes aligns with healthcare providers’ ethical responsibilities. Osteopaths are entrusted with the wellbeing of their patients, and a commitment to clinical excellence demonstrates a dedication to upholding the highest standards of care. Ethical practices contribute not only to positive patient outcomes, but also to the overall professional integrity of the osteopath and the industry.

EMPLOYEE SATISFACTION AND RETENTION
For osteopathic practices with multiple staff members, the emphasis on clinical excellence extends beyond the practitioner to the entire team. Staff working in an environment prioritising patient care are more likely to experience job satisfaction and remain committed to the practice. The positive work culture that emerges from focussing on clinical excellence can lead to lower turnover rates and a stable, cohesive team.
ADAPTABILITY IN A CHANGING LANDSCAPE
The healthcare landscape is dynamic, with advancements and changes occurring regularly. Osteopaths prioritising clinical excellence position themselves as adaptable practitioners capable of evolving with the industry. This adaptability is crucial for long-term success, as it allows the practice to integrate new techniques, technologies, and approaches that enhance patient care and outcomes.
CONCLUSION
While a bustling practice may seem successful, the true marker is clinical excellence, leading to a sustainable and reputable practice. Committing to education, patient-centric care, and ethical practices allows osteopaths to balance clinical and business success, ensuring a fulfilling career.
PRACTICE MANAGEMENT 13
DR SHANE BUNTMAN
Dr Shane Buntman works at Melbourne Osteopathy Sports Injury Centre.
Can a patient under 18 provide informed consent?

There is no clear yes or no answer. As we explain, consent will depend on the individual. In any case, understanding your rights and the rights of your patient is imperative.
DEFINING INFORMED CONSENT
Put simply, informed consent is a patient’s voluntary decision to agree to treatment after being informed by a practitioner of all material risks associated with that treatment (as well as alternative options). The patient provides such consent by expressly indicating that they have adequate understanding of the benefits and material risks attached to the proposed treatment.
This of course imputes that the patient has the cognitive capacity to understand risks and benefits and can enter into such an agreement.
Generally, a patient will not have the mental capacity and cognition to consent if the following occurs:
The patient is too young;
The patient has a mental illness or intellectual disability that detrimentally affects their ability to make decisions;
The patient has dementia;
The patient is impaired by alcohol or substance;
The patient is unconscious.
At first instance, children under the age of 18 (minors) do not have such capacity. Generally, such consent must be given by a parent (as long as the family court has not restricted their access to the minor) or authorised guardian.
However, there are special considerations for minors, which entail determining when a minor is able to give informed consent on their own account.
RELEVANT LEGISLATION
Turning to legislation, in all Australian states and territories, except for South Australia, there is no legislation specifying when a child may consent to medical treatment on their own behalf. In South Australia, section 6 of the Consent to Medical Treatment and Palliative Care Act 1995 (SA) relevantly provides:
“A person of or over 16-years-of-age may make decisions about his or her own medical treatment as validly and effectively as an adult.”
Under that Act, a child under 16 can validly consent to treatment if:
“The medical practitioner is of the opinion that the child is capable of understanding the nature, consequences and risks of the treatment and that the treatment is in the best interest of the child’s health and wellbeing, and that opinion is supported by the written opinion of at least one other medical practitioner who personally examines the child before the treatment is commenced.” (Section 12, Consent to Medical Treatment and Palliative Care Act 1995 (SA))
In other states, such as NSW, the answer is not so clear-cut. Section 33 (2) of the Guardianship Act 1987 (NSW) provides: “...a person is incapable of giving consent to the carrying out of medical or dental treatment if the person: (a) is incapable of understanding the general nature and effect of the proposed treatment,
“However, there are special considerations for minors, which entail determining when a minor is able to give informed consent on their own account”
Nevena Brown is a Principal, and James Papworth a Senior Associate, at Meridian Lawyers.
(b) is incapable of indicating whether or not he or she consents or does not consent to the treatment being carried out.”
CONSENT AND PRIVACY
The Privacy Act 1988 Cth, which sets out the principles dealing with sensitive information and exemptions, does not provide an age at which children are considered capable of providing consent in relation to their personal information. According to the Australian Privacy Principle (APP) Guidelines:
1. Individuals under the age of 18 generally have capacity to consent if they have sufficient understanding and maturity to understand what is being proposed;
2. If it is impractical or unreasonable to assess an individual’s capacity to consent: Individuals aged 15 or over are presumed to have capacity to consent, unless there is some reason to suggest otherwise; Individuals aged under 15 are presumed not to have capacity to consent.
WHAT DOES THAT MEAN?
At common law, a child under 18 may legally consent to most types of medical treatment on their own behalf if they are competent to do so. If they are not competent, consent by a parent or authorised guardian must be obtained. In the absence of any legislation to guide practitioners, health practitioners must look to the common law for guidance on how to make an assessment
14 PRACTICE MANAGEMENT
of competency to consent for all patients under the age of 18.
Naturally, this will depend on considerations including that young person’s particular age, intelligence, maturity and independence, as well as the seriousness of the proposed treatment or procedure.
In Marion’s Case (Secretary, Department of Health and Community Services v JWB and SMB (1992)175 CLR 218), the High Court of Australia, in adopting a decision by the House of Lords in Gillick v West Norfolk and Wisbech Area Health Authority [1986] AC 112, held that a child with the maturity to understand the nature and consequences of the treatment has the legal capacity to consent on their own behalf, without the necessity for parental consent or knowledge.
Sufficiency of capacity is seen as a spectrum and the more serious the consequences of the decision, the higher the level of capacity that must be demonstrated.
ASSESSING THE MATURITY OF A MINOR
With the ‘mature minor’ principle in mind, a practitioner must assess each child’s mental state and cognition on a caseby-case basis to determine whether that particular child has sufficient intelligence and understanding to enable them to understand the proposed treatment.
This assessment necessarily involves determining the following issues:
What is the treatment for and what does it involve?
Can the patient communicate their consent?
Is the treatment necessary?
Are there any alternative options?
What are the likely effects and possible risks attached?
Are there any consequences of not treating?
What are the consequences of discovery of treatment by the child’s parent or guardian?
Other checks that are relevant to all consent should be assessed too, such as if the consent is freely given and if it is current (a practitioner cannot rely on consent obtained a time ago when the circumstances have materially altered).
The assessment and the health practitioner’s determination should always be documented.
“With the ‘mature minor’ principle in mind, a practitioner must assess each child’s mental state and cognition on a caseby-case basis to determine whether that particular child has sufficient intelligence and understanding to enable them to understand the proposed treatment”
IF UNCERTAIN, BE CAUTIOUS
Where there is any uncertainty, a practitioner should always err on the side of caution and either seek a second opinion, or seek the consent of the child’s parent or guardian. That said, practitioners should remain aware of the patient’s right to privacy and confidentiality, particularly if the young person does not consent to the release of information. This can often be a difficult circumstance to navigate where there are difficult family situations (or the particular issue is sensitive, such as pregnancy or STD).
When considering whether it is appropriate to release information to a third party, practitioners need to consider:
1. Does the patient consent to releasing information?
2. If not, you need to assess competency.
This may include assessing:
Does the patient understand about the request for information?
Why it is requested?
Who requested it?
The consequences of release, i.e. are there any safety issues in releasing the information?
Overall, it is important to remember your role and paramount duty to the patient. With that in mind, it is wise to ensure you know your and the patient’s rights so you can express and justify your position calmly and confidently, while not being dismissive of the emotional concerns of those involved.
PRACTICE MANAGEMENT 15
Disclaimer This information is current as of May 2023. This article does not constitute legal advice and does not give rise to any solicitor/ client relationship between Meridian Lawyers and the reader. Professional legal advice should be sought before acting or relying upon the content of this article.
Good hygiene, best practice guidelines
Good hygiene practice is a crucial part of an osteopath’s duty of care and has never been more important, particularly given heightened hygiene awareness among consumers. Ibrahim Samaan, practising physiotherapist and founder of hygiene company Purifas, outlines his hygiene practice guidelines for private osteopaths.
What are the go-to hygiene regulations practitioners should follow in order to minimise the risk of infection in their clinics and therapy environments? The astonishing answer is that there are none.
To date, many allied health professionals have been left to their own devices in an attempt to determine the areas of risk and how to manage them effectively in a clinical setting.
It was this distinct lack of any clear and direct instruction that prompted Ibrahim to develop a set of best practice guidelines (based on current research and evidence) specifically for therapy professionals.
These essential guidelines are laid out below in five easy-to-follow steps.
1
CLIENTS WITH SYMPTOMS OF ILLNESS SHOULD BE STRONGLY ADVISED NOT TO ATTEND THE CONSULTATION
It is well established (Sartwell 1966, Brookmeyer 2015, Backer et al 2020) by virologists and medical experts that the infectious period after contraction of an infectious pathogen begins before the carrier becomes symptomatic (if at all). While the overlap may vary between diseases, the incubation period is usually between 7-10 days, with a carrier typically becoming infectious within the latter five days.
While it is near impossible to monitor infection without symptoms, it should be made explicitly clear that a client with any symptoms, no matter how mild, should not attend therapy as they have the potential to be a carrier of an infectious pathogen. Extra caution may also be established by asking clients who have

“What are the go-to hygiene regulations practitioners should follow in order to minimise the risk of infection in their clinics and therapy environments?
The astonishing answer is that there are none”
been exposed to people who are ill to also reconsider their attendance.
You can communicate this to your clients by:
Displaying signs in high-traffic areas of your clinic;
Including a hygiene requirement section on your website;
Promoting your policies on social media; Explicitly asking your clients at the time of booking or when confirming their appointment.
2 CLIENTS AND PRACTITIONERS SHOULD WASH THEIR HANDS BEFORE AND AFTER THERAPY
The primary focus of hygiene research has largely been on hand hygiene and
IBRAHIM SAMAAN
Ahpra-registered physiotherapist
Ibrahim Samaan is the founder of Purifas, a healthcare company committed to reducing the risk of infection and improving comfort during therapy treatments. Ibrahim is the winner of two Gold 2021 Asia-Pacific Stevie Awards and was a 2020–2021 Physiotherapist of the Year Finalist in the Allied Health Awards for his efforts to improve hygiene standards in the physiotherapy sector.
its effectiveness in diminishing the transmission of disease via contact (Johnson et al 2005, CDC 2002). Hand washing is accepted as essential, especially in healthcare. However, the issue is compliance by healthcare personnel and attendants. Studies show the compliance rate to be as low as 10% (Grayson et al 2011, Azim & McLaws 2014).
Practitioners must observe frequent and stringent hand washing at three critical points:
1. Upon entry to the clinic;
2. Prior to treatment;
3. Immediately following contact with a client.
Clients should be given access to facilities to wash their hands upon entry to the clinic and at the completion of their treatment.
While thoroughly washing their hands, they must also limit the use of reusable towels, which have been shown
16 PRACTICE MANAGEMENT

to harbour bacteria despite repeated washing (Sifuentes et al 2013).
Healthcare-associated infections (HAIs) are a substantial contributor to the healthcare burden and preventable disease figures. With more than 12% of MRSA (methicillin-resistant Staphylococcus aureus) infections being contracted in a community setting, it is imperative that the increased hygiene practices implemented to mitigate the COVID-19 viral pandemic remain in place and become the new norm.
3 WITHIN THE CONSULTATION ROOM, ONLY APPLY SINGLE-USE, FIT-FOR-PURPOSE HYGIENE PRODUCTS TO ALL SHARED SURFACES AND ITEMS
Single-use protective materials are known to be more hygienic, quickly eliminating the trace of contact of the previous patient or potential infectious pathogens.
The main points of entry and exit of a pathogen are through the nasomucosal openings (Alberts et al 2002). Prone therapies use a shared face hole, which can significantly increase a client’s risk of cross transmission via contact, droplet and potentially airborne microbes shed from the nose, mouth and even eyes. Through single-use solutions, the risk of cross contamination of any bacteria/flora/ microbes is dramatically reduced.
Research (Sifuentes et al 2013) has shown that reusable materials – such as towels, pillowcases and bed linen –can harbour bacteria despite hospitalgrade washing. In particular, it was shown that Staphylococcus aureus can
“Research has shown that reusable materials – such as towels, pillowcases and bed linen – can harbour bacteria despite hospital-grade washing”
survive up to three weeks in cotton towels, which are commonly used in therapy clinics and hospitals, despite regular laundering (Sifuentes et al 2013). It was concluded that normal washing or laundering of towels, whether done in-house or externally, was not enough to remove all viable microorganisms (Sifuentes et al 2013).
4 SANITISE ALL SHARED SURFACES AFTER EACH CONSULTATION
All shared surfaces should be sanitised between each client to ensure the risk of cross transmission is minimised. To effectively sanitise a surface, research indicates it must first be cleaned with a detergent and then disinfected with an appropriate TGA-approved antibacterial or sanitising agent (CDC n.d., Hota 2004). (Remember to ensure that these agents are safe for use in a clinical setting.)
5 ALL HIGH-TRAFFIC AREAS AND CONTACT POINTS SHOULD BE CLEANED REGULARLY
High-traffic contact points, such as door handles, arm chairs, waiting room areas and reception desks,
are cross-transmission risks, especially in facilities with a high turnover of clients. All areas that customers come into contact with upon entry and exit of the clinic, such as bathroom areas, should be cleaned and sanitised regularly. There is evidence to show a significant reduction in HAIs when an employee is hired specifically to clean and sanitise hightraffic and common areas (Doll et al 2018). Depending on the size of your clinic, this may not be feasible. In which case, you should have these hygiene and safety tasks clearly assigned to the appropriate personnel, including clear outlines on what is needed to be done and the frequency. The Australian Commission on Safety and Quality in Health Care has provided some resources to assist business owners and health-related professionals develop an environmental cleaning program.
Making these five steps standard practice in your clinic or consultation setting will help maintain a safe and hygienic environment for your clients and contribute to a reduction in community transmission of illness.
These guidelines and the associated research have been fully evaluated by an expert review panel and subsequently endorsed by the Australian Physiotherapy Association.
PRACTICE MANAGEMENT 17

Endometriosis and allostatic overload: assisting with endo management from an osteopath’s perspective
Many of us have seen individuals with endometriosis, whether they sought treatment specifically for the condition or mentioned it in passing during a consultation. In this article, we’ll explore what endometriosis is, what causes it, why there is a mismatch between standard treatment and aetiology and, finally, a model that osteopaths could use to frame their treatments.
Osteopaths are well suited to be part of a management team for someone with endometriosis. By better understanding our role, we have an opportunity to help our patients understand and reconnect with their body and shape their journey through endometriosis.
WHAT IS ENDOMETRIOSIS?
Endometriosis is when tissue similar to the lining of the uterus (endometrium) is found in places outside of the uterus.1 The tissue can form nodules or plaques, which may be visualised at surgery. Endometriosis is commonly seen in the pelvic region on the peritoneum, the ovaries, and within the rectovaginal septum (aka pouch of Douglas).1 Still, it can be found anywhere in the body, including scar tissue, on the diaphragm or in the lungs.1
Endometriosis is a chronic inflammatory condition that is driven by oestrogen, although oestrogen does not cause endometriosis. The main symptoms are pain, particularly chronic pelvic pain (CPP), menorrhagia (heavy periods) and infertility.1
Endometriosis affects approximately 10% of people assigned female at birth,2 although the numbers may be higher as not all people are symptomatic and not all people are diagnosed.3 It predominantly affects females, but in very rare instances, it has been found in males.4 There is a diagnostic delay of approximately seven years, although
this will hopefully change as awareness increases. There is no known cure for endometriosis, and treatment is usually aimed at managing symptoms.2
Endometriosis is commonly classified using the revised American Society of Reproductive Medicine (rASRM) criteria based on surgically viewing the number of lesions. In Stage I and II, disease features include superficial peritoneal lesions and minimal adhesions. In contrast, Stage III and IV describe more extensive disease, including cystic ovarian endometriosis (endometrioma) and extensive scarring, fibrosis and adhesions.7 Note that the severity of symptoms a person experiences is not reflected by the stage of disease.8
Adenomyosis: a common cousin of endometriosis
Adenomyosis is a condition often found with endometriosis, although it can occur separately. It is when endometrial tissue infiltrates the myometrium (the muscular outer layer of the uterus). Its symptoms also include pain, infertility and longer and heavier menstrual cycles.8
SYMPTOMS OF ENDOMETRIOSIS
Symptoms of endometriosis vary between individuals, which can make diagnosis difficult. Some people experience no symptoms, 2 while others experience many. 2 See Table 1 (opposite page) for a summary list of symptoms.
SARAH DRYBURGH
Sarah qualified as an osteopath in New Zealand and has long held a fascination for chronic pelvic pain and endometriosis. In 2017 she founded her own clinic, Pivot Osteopathy, to focus more on pelvic and women’s health, later merging her clinic with pelvic health osteopath Liz Johns to further pursue her passion in this area. In 2022 she co-wrote the one day course ‘The Endo Enigma’ with osteopath/nutritionist Rebecca Malon to promote education and hands-on skills in the management of endometriosis.
Symptoms that affect the gastrointestinal system are common, although they can be misdiagnosed as irritable bowel syndrome.9
While the symptoms listed in Table 1 are commonly associated with endometriosis, the condition has been associated with a wide range of other symptoms including back pain, migraines, headaches, asthma and autoimmune conditions such as lupus and rheumatoid arthritis.7
Quality of life is commonly affected, with people experiencing higher levels of anxiety and depression, difficulties with personal relationships and impacts on mood, self-esteem, and feelings of guilt, shame, grief and loss.8,10
18 CLINICAL
PAIN IS THE MOST COMMON SYMPTOM OF ENDOMETRIOSIS
What is notable about pain in endometriosis is that the amount of pain and symptom severity does not correlate to the amount or severity of the disease.11 People can have severe disease (Stage III or IV) but may be asymptomatic, or they can have a minimal number of lesions (Stage I) and be in severe pain.8 These differences are important facts and something to remember throughout this article but also when working with patients with endometriosis.
Why does this happen? As will be expanded upon later in this article, the endometrial lesions do not cause pain. The pain from the endometrial lesions is caused through the interaction and dysregulation of hormonal, immune, neural and lymphatic factors.7,12,13 The interaction of these factors can lead to inflammation, peripheral and central sensitisation, adhesions and various co-morbidities due to cross-organ sensitisation.8 Co-morbidities due to cross-organ sensitisation are a common cause of
pain in endometriosis. Cross-organ sensitisation is where the spreading of noxious inputs from an affected visceral organ (such as the uterus) to an unaffected organ (such as the bladder) occurs due to shared nerve pathways.12 Co-morbidities such as irritable bowel syndrome (IBS), painful bladder syndrome (PBS) and ovarian cysts are common in endometriosis.8
Biomechanically, repeated cycles of inflammation can create changes at the tissue level.8 These changes can lead to the formation of adhesions and fibrous scar tissue bands that affect the normal anatomical movement of organs such as the bowel and bladder9 , affecting the local neural, immune, endocrine and lymphatic systems. These changes in anatomical movement can also contribute to infertility9 through the creation of an inflammatory microenvironment that affects fertilisation, distortions of the uterus that may disrupt implantation and painful sex.14
Not every person with endometriosis will get fibrosis and adhesions, and whether a person has fibrosis is not
“Endometriosis affects approximately 10% of people assigned female at birth, although the numbers may be higher as not all people are symptomatic and not all people are diagnosed”
TABLE 1: SYMPTOMS OF ENDOMETRIOSIS9
Menorrhagia (heavy periods)
Chronic pelvic pain
Cyclical pain
Ovulation pain
Dysmenorrhea (painful periods)
Dyspareunia (painful sex)
Dysuria (painful urination)
Dyschezia (painful defecation)
Gastrointestinal symptoms including IBS, bloating, constipation and food intolerances
Myofascial pain
Pelvic floor dysfunction
CLINICAL 19
linked to the stage of the disease (i.e. a person with stage IV endometriosis may never develop fibrosis, while someone with Stage II may have quite severe fibrosis around their lesions).8
WHAT CAUSES ENDOMETRIOSIS?
There are many theories, but the most well-accepted hypothesis is that of retrograde menstruation.8 In this theory, fragments of the endometrial tissue that lines the uterus leave the womb via the uterine (fallopian) tubes and create deposits within the peritoneal cavity. While this theory is regarded as important because it mainly explains how the endometrial deposits may have got to their positions, it does not explain why most women have retrograde menstruation, but only about 10% have endometriosis.2 Nor does it explain how the cells that leave the womb as cells of the endometrial lining transform into endometrial lesions, which are cells that are similar to that of the endometrial lining. Something else is going on. Several other theories have emerged, such as coelomic metaplasia and lymphatic and vascular metastasis, which all explain aspects of endometriosis. However, no single theory explains all the different ways endometriosis presents.4
It has been proposed that endometriosis likely results from a combination of these theories.4,8,9,14 For endometriosis to develop, we need factors including a favourable endocrine and metabolic environment, altered immunity and inflammatory responses, plus a genetic susceptibility to come together to promote the development of endometriosis.4 Other factors, such as childhood trauma6 and having a first degree relative with endometriosis,7 may predispose people to developing it, but we still don’t know why some people develop it and others do not. Once a pro-inflammatory state has started and the endometrial lesions have been established, it is thought that they drive more immune dysfunction and inflammation. This dysregulation of the local environment around the lesions can contribute to angiogenesis (growth of blood vessels), neurogenesis (growth of nerves), inflammation and alterations in the local lymphatic environment that can all potentially contribute to pain.13,15

“Hormone treatments are used to suppress the normal menstrual cycle, which in turn stops or slows the growth of endometrial lesions and can be effective in reducing endometriosis-related pain in some people”
Alterations in the gut microbiome, peritoneal fluid and female reproductive tract have also been identified. While it is not yet clear whether these changes are a result of endometriosis or whether they are the cause of endometriosis, the relationship may be bidirectional. Endometriosis may contribute to early changes in the microbiome.15 The cervical microbiome may be of particular importance as reduced diversity has been linked with more pain severity and infertility, although this research is still emerging.15
As oestrogen is a driver of the growth of endometriotic lesions, each menstrual cycle can potentially make things worse. Oestrogen stimulates the endometriotic lesions, which creates changes in the micro-environment surrounding the lesions, leading to local inflammation,
angiogenesis, neurogenesis12 and changes in the local lymphatic system.13 This is why shutting oestrogen down is a target for many medical treatments offered to patients. Although the role of oestrogen has been extensively studied,2 it is only one hormone in a very complex system. It can be helpful for some people, but it does not provide a cure or control symptoms in everyone.2
Now that we have a basic understanding of what causes endometriosis let’s look at the standard treatments offered.
STANDARD TREATMENTS
Current standard treatments are dictated by the primary issue (usually infertility or pelvic pain). The standard treatments offered to most patients are surgery, hormonal treatments and analgesics.4
20 CLINICAL

Surgery aims to remove or destroy endometriotic tissue and adhesions, and the surgeon’s skill and timing of the surgery can affect the outcome.2 Surgery has been shown to decrease pain in some, but not all, people. There is growing discussion surrounding when surgery should be used as there is a high rate of recurrence of symptoms after surgery, and repeat surgeries have been shown to be a cause of pain in endometriosis.8,9
Hormone treatments are used to suppress the normal menstrual cycle, which in turn stops or slows the growth of endometrial lesions and can be effective in reducing endometriosis-related pain in some people.8 Hormonal treatments include the combined oral contraceptive pill, devices such as the Mirena and
progestins and gonadotropin-releasing hormone analogues (GnRHa).8
Non-hormonal treatments are used to target pain and inflammation. NSAIDs and analgesics such as acetaminophen are used with varying degrees of success.2
While these treatments can be helpful, their targets are limited. There is growing awareness that a multidisciplinary approach is needed, the standard treatments offered are aimed at controlling oestrogen, cutting out lesions and trying to suppress pain and inflammation chemically.
The failure of standard treatments to fully control the symptoms of endometriosis has led to a growing call for modern management of endometriosis to be more patientfocused rather than focused on the
endometriotic lesions.8,9 Other treatment avenues that are being explored include nonpharmaceutical options, such as acupuncture and the use of botulinum toxin to reduce the musculoskeletal component of pelvic pain. Diet changes that reduce inflammation and improving the gut microbiome are also being suggested. The overlap of pain, trauma and other mental health conditions is now being seen as part of a more wholeperson treatment plan.2
Osteopaths are well suited to be part of a patient’s management team.
MATCHING THE TREATMENT TO THE CAUSE: PROPOSING A NEW MODEL
Current explanations for the cause of endometriosis are inadequately treated with the standard treatments offered.8,14 It is a complex, chronic condition, and many factors are at play.
Perhaps this partly concerns how endometriosis and chronic diseases are generally viewed. Too often, we forget that chronic disease happens within a system. The symptoms are often wide-ranging and seldom stem from a single cause.16
Rather than focusing on treating symptoms, we could view chronic disease states as a disruption of homeostasis and an increase in allostatic load.17 The concept of allostasis and allostatic load will be familiar to most osteopaths. It could give us a better framework to explain how osteopaths may assist with the management of endometriosis.
ALLOSTATIC LOAD AND ENDOMETRIOSIS
Allostasis is the hormonal, neural, immune and behavioural adaptations the body uses to adapt to or protect itself from stressors to maintain its internal state.16,18 In simple terms, the body uses its resources to maintain homeostasis as it reacts to constantly changing conditions.17 As the demands on a person’s system increase, they have an increasing allostatic load.19 When the demands on the system exceed the body’s resources to adapt to changing conditions, the result is allostatic overload.18
Not all people with a genetic predisposition develop endometriosis, and when they do, not all are symptomatic.4 Therefore, we must ask, “why?”
CLINICAL 21
A possible road to endometriosis
Endometrial lining cells transform into ‘endometrial-like cells’ causing inflammation = pain, and other symptoms
5
Multiple cycles with the inflammatory effect of oestrogen
3
Genetic/ epigenetic vulnerability
1
7
Worsening symptoms with increasing load from other lifestyle stressors: poor sleep, pain, anxiety/ depression, withdrawal from social activities 2
Retrograde menstruation with endometrial lining deposits in peritoneal cavity
Allostasis may provide an answer as it gives us a model to consider the cumulative load of various stressors. These stressors can activate various neuro-endocrine-immune pathways that interact and affect multiple systems.22 We can then consider how these pathways can produce pro-inflammatory and pronociceptive states that can contribute to the development of a chronic disease process such as endometriosis.
Figure 1: ‘A possible road to endometriosis’ above provides a visual application of increasing allostatic load and explores a possible route to endometriosis. If we apply the roadmap seen in Figure 1 to endometriosis, using a retrograde menstruation model, we have tissue from the lining of the uterus that ends up where it shouldn’t be. The immune system would usually clear it, but there may be neuro-immuneendocrine disruption due to factors such as gut dysbiosis, repeat menstrual
4
Stress/altered microbiome/toxin exposure, etc.
6
Delayed diagnosis. Increased inflammation and nervous system sensitisation. Progressive worsening of symptoms
cycles, childhood trauma, increasing social isolation and increasing pain. Delayed diagnosis and inadequate treatment lead to progressive worsening of symptoms, with the result being allostatic overload and difficulties with everyday life functioning. This road is theoretical but it shows how endometriosis is an evolving process.
An allostatic model of thinking about endometriosis is useful because if we think of the development and management of endometriosis as an issue of allostatic load rather than an issue of endometriotic lesions, pain and hormonal imbalances, we have a lot more treatment avenues to explore.
How do you apply this theory to osteopathic practice?
ALLOSTATIC LOAD – A MODEL FOR OSTEOPATHS?
Allostatic load allows us to view our patient’s symptoms within the context
of their whole story rather than as a list of symptoms.16 It allows us to explore aspects of our patient’s individual journey to endometriosis that may help us create a more meaningful treatment plan. Sharing the concept with our patients also allows them to appreciate the multi-dimensionality of their personal endometriosis journey.16
An allostatic model allows osteopaths to participate in endometriosis management by using our skills to remove layers of the allostatic load that could be contributing to a person’s inability to manage their symptoms. Osteopaths have a wide range of skills to use as they view the body as a unity of systems (neurologic-mechanical-circulatoryrespiratory-metabolic processes) that are associated with a variety of psychological responses that allow a person to manage social and environmental demands.20
While some aspects of a person’s allostatic load may be irreversible,16
22 CLINICAL
Figure 1: A possible road to endometriosis. Describing one possible journey for someone with a genetic vulnerability to progressive effects on all areas of life.
“Allostatic load allows us to view our patient’s symptoms within the context of their whole story rather than as a list of symptoms”
others may respond well to osteopathic treatment. Treatment could include hands-on techniques, education, exercises and taking the time to listen and support our patient, all aiming to lighten their allostatic load.
It’s easiest to explore the idea of allostatic load, osteopathy and endometriosis with a case study.
Anna (name changed for privacy reasons) was a 36-year-old female diagnosed with Stage III endometriosis via laparoscopy using the rASRM criteria. She had moderate endometriosis although she wasn’t sure where the lesions were found. Notes from her case history can be seen in Table 2. Using an allostatic load model to understand her symptoms, a few factors stand out. Anna has a high-stress job and a history of anxiety, depression and abuse, she feels fatigued, she isn’t sleeping well because she is in pain, and she would like to be in a relationship. She also has endometriosis and has tried surgery and hormone medications, which haven’t successfully managed her symptoms. All of these factors could place additional pressure on her neuro-endocrine-immune systems. She also has contributing factors in her physical body, which can be seen in Table 3: Notes from Examination.
A visual representation of Anna’s allostatic load is shown using a bubble diagram in Figure 2. This image combines information from her case history and examination. While it is beyond the osteopathic scope of practice to attempt to address all factors, there are many aspects of her presentation where osteopathic treatment could possibly lead to a reduction in her allostatic load.
TABLE 2: NOTES FROM CASE HISTORY
Hoping for support with pain from endometriosis
Fatigued and wants to exercise. She described her body as ‘sore and stiff’
High stress job, wants to date, fatigue/body image limiting
Poor sleep d/t pain. Worse at ovulation and menses
She has a history of depression/anxiety, although she is hoping to come off her medication
She has a history of childhood abuse and history of emotional abuse in her previous relationship
She suffered a fall on her coccyx as a teenager that is still occasionally painful with prolonged sitting and at times of stress
She had stopped OCP as felt it didn’t improve her symptoms.
She does not want another surgery
TABLE 3: NOTES FROM EXAMINATION
Kyphotic posture
Poor mobility through her thoracic region and an upper rib breathing pattern
Weak abdominals and lumbar tension
Diaphragm, neck and shoulder and TMJ tension
Bubble diagram showing Anna’s allostatic load
Endometriosis
Stress and emotions
High-stress job
Hx of abuse
Wants relationship
Depression/anxiety
Physical factors
Thoracic tension
Kyphotic posture
Upper rib breathing pattern
Weak abdominals
Lumbar tension
Anna’s Load
Poor sleep
Fatigue
Chronic pain
Neuroendocrineimmunelympatic
CLINICAL 23
Figure 2: Bubble diagram showing Anna’s allostatic load. Larger bubbles represent a greater contribution to an individual’s presentation. Bubble size can be changed through discussion with patient and over time as symptoms evolve.
An important part of Anna’s treatment was helping her understand her own ‘pain story’ and explaining how endometriosis was only one part of a much bigger picture. Although the bubble diagram wasn’t used as part of treatment in Anna’s case, bubble diagrams can be used to communicate the idea of allostatic load to patients. They may assist in developing dialogue between patients and their practitioner.
Osteopathically, some aspects of Anna’s musculoskeletal load that were considered in this case were her upper rib breathing pattern and it could potentially affect her body’s biochemistry. Her upper rib breathing pattern could be a cause or an effect of her diaphragm tension and contribute to her weak abdominals,21 lumbar tension, neck and shoulder and TMJ tension. The upper rib breathing pattern could also affect the neck and shoulder muscle tension due to the demands of lifting the ribcage, using additional energy to breathe. Poor diaphragm mobility could affect her lymphatic movement, which could contribute to the altered neuroimmune micro-environment around the endometrial lesions.12,13
WHY IS ALLOSTATIC LOAD IMPORTANT FOR US TO REFLECT ON AS OSTEOPATHS?
Understanding pain and dysfunction within a broader model can help us understand our role in endometriosis management and how we communicate with our patients. If a person believes that all their pain is due to an endometrial lesion, then the options are quite limited: cut the lesions out, suppress the hormone driving the development lesions (oestrogen suppression) and control the pain with medication.
If we can assist our patients (and ourselves) in taking a broader view of why a person may present to us with pain then the tools that are available to us expand. If the endometrial lesions are an aspect of pain, but not the only driver, we can assist our patients by removing layers of their allostatic load within our osteopathic scope of practice. This may give our patients the resources to address other layers of their allostatic load.
Let’s return to Anna for how managing physical factors and understanding allostatic load helped one patient.
“Understanding pain and dysfunction within a broader model can help us understand our role in endometriosis management and how we communicate with our patients”
In Anna’s case, it was possible to address her kyphotic posture, thoracic mobility, upper rib breathing pattern, coccyx issue, diaphragm, neck, shoulder and TMJ tension through a combination of hands-on therapy, education and exercise.
Reducing tension in her musculoskeletal system and thinking about lymphatic drainage during treatment led to her finding that she could sleep better as her pain had reduced.
The improved sleep reduced some of her fatigue, allowing her to use a range of mobility, breathing and strengthening exercises to address her upper rib breathing pattern, diaphragm tension and abdominal weakness and further improve her thoracic mobility.
As she moved more, she felt increased confidence in her body, and her body image began to change. These factors led her to return to working with her
psychologist, and she was ultimately able to come off her medication as she felt that her depression and anxiety had reduced to the point where she was able to manage without pharmaceutical assistance.
Anna was a success story for including osteopathy as part of endometriosis management. However, the success did not come from addressing an oestrogen imbalance and endometrial lesions. Instead, treatment success came from applying osteopathic skills to address factors that were contributing to her allostatic load. In addition to hands-on therapy and exercise, there were many discussions regarding the interaction between her physical body and other psychosocial factors that allowed her to understand endometriosis as an aspect of her presentation rather than the sole cause of her pain.


24 CLINICAL
Osteopaths can’t solve all the problems associated with allostatic load endometriosis, nor should we attempt to. Our patients need a whole-person approach to treatment, which may include medication, surgery, hormone suppression, diet changes, stress reduction, acupuncture, psychological support, pelvic floor osteopathy or physiotherapy, and a range of therapies may be appropriate for our patients at different times. Osteopaths can use the broad range of skills we have at our disposal to help our patients understand the role of endometriosis and other factors in their pain story and assist them in lightening their load.
In Table 4, you’ll find a list of possible targets that could be useful depending on your particular skill set. While this is an incomplete list, it is designed to act as a starting point for practitioners to think about how we can assist people with their management of endometriosis.
FINAL THOUGHTS
Managing endometriosis in an osteopathic context is not about specific techniques (although some may be more helpful than others), nor is it necessarily about treating endometriosis directly. Instead, it’s about helping our patients manage an incredibly complex, chronic condition by using our skills to reduce their allostatic load.
References
1. Burney RO, Giudice LC. Pathogenesis and pathophysiology of endometriosis. Fertility and Sterility. 2012 Sep 1;98(3):511–9.
2. Zondervan KT, Becker CM, Missmer SA. Endometriosis. Longo DL, editor. N Engl J Med. 2020 Mar 26;382(13):1244–56.
3. Leyendecker G, Wildt L, Mall G. The pathophysiology of endometriosis and adenomyosis: tissue injury and repair. Arch Gynecol Obstet. 2009 Oct 1;280(4):529–38.
4. Zondervan KT, Becker CM, Koga K, Missmer SA, Taylor RN, Viganò P. Endometriosis. Nat Rev Dis Primers. 2018 Jul 19;4(1):1–25.
5. Parazzini F, Esposito G, Tozzi L, Noli S, Bianchi S. Epidemiology of endometriosis and its comorbidities. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2017 Feb 1;209:3–7.
6. Harris HR, Wieser F, Vitonis AF, Rich-Edwards J, Boynton-Jarrett R, Bertone-Johnson ER, et al. Early life abuse and risk of endometriosis. Hum Reprod. 2018 Sep;33(9):1657–68.
7. Rahmioglu N, Mortlock S, Ghiasi M, Møller PL, Stefansdottir L, Galarneau G, et al. The genetic basis of endometriosis and comorbidity with other pain and inflammatory conditions. Nat Genet. 2023 Mar;55(3):423–36.
8. Chapron C, Marcellin L, Borghese B, Santulli P. Rethinking mechanisms, diagnosis and management of endometriosis. Nat Rev Endocrinol. 2019 Nov;15(11):666–82.
9. Ellis K, Munro D, Clarke J. Endometriosis Is Undervalued: A Call to Action. Frontiers in Global Women’s Health [Internet]. 2022 [cited 2023 Jan 29];3. Available from: https://www.frontiersin.org/ articles/10.3389/fgwh.2022.902371
10. Grogan S, Turley E, Cole J. ‘So many women suffer in silence’: a thematic analysis of women’s written accounts of coping with endometriosis. Psychology & Health. 2018 Nov 2;33(11):1364–78.
11. Coxon L, Horne AW, Vincent K. Pathophysiology of endometriosis-associated pain: A review of pelvic and central nervous system mechanisms. Best Practice & Research Clinical Obstetrics & Gynaecology. 2018 Aug 1;51:53–67.
12. Maddern J, Grundy L, Castro J, Brierley SM. Pain in Endometriosis. Frontiers in Cellular Neuroscience [Internet]. 2020 [cited 2023 Sep 11];14. Available from: https://www.frontiersin.org/articles/10.3389/ fncel.2020.590823
13. Tuckey B, Srbely J, Rigney G, Vythilingam M, Shah J. Impaired Lymphatic Drainage and Interstitial Inflammatory Stasis in Chronic Musculoskeletal and Idiopathic Pain Syndromes: Exploring a Novel Mechanism. Frontiers in Pain Research [Internet]. 2021 [cited 2023 Sep 17];2. Available from: https://www.frontiersin.org/ articles/10.3389/fpain.2021.691740
14. Borghese B, Santulli P, Marcellin L, Chapron C. [Definition, description, clinicopathological features, pathogenesis and natural history of endometriosis: CNGOF-HAS Endometriosis Guidelines]. Gynecol Obstet Fertil Senol. 2018 Mar;46(3):156–67.
15. Uzuner C, Mak J, El-Assaad F, Condous G. The bidirectional relationship between endometriosis and microbiome. Front Endocrinol (Lausanne). 2023 Mar 7;14:1110824.
16. Rabey M, Moloney N. “I Don’t Know Why I’ve Got this Pain!” Allostasis as a Possible Explanatory Model. Physical Therapy. 2022 May 1;102(5):pzac017.
17. McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Hormones and Behavior. 2003 Jan 1;43(1):2–15.
18. Borsook D, Maleki N, Becerra L, McEwen B. Understanding Migraine through the Lens of Maladaptive Stress Responses: A Model Disease of Allostatic Load. Neuron. 2012 Jan 26;73(2):219–34.
19. Lunghi C, Consorti G, Tramontano M, Esteves JE, Cerritelli F. Perspectives on tissue adaptation related to allostatic load: Scoping review and integrative hypothesis with a focus on osteopathic palpation. Journal of Bodywork and Movement Therapies. 2020 Jul 1;24(3):212–20.
20. Castagna C, Consorti G, Turinetto M, Lunghi C. Osteopathic Models Integration Radar Plot: A Proposed Framework for Osteopathic Diagnostic Clinical Reasoning. J Chiropr Humanit. 2021 Dec 22;28:49–59.
21. Boyle KL, Olinick J, Lewis C. The value of blowing up a balloon. N Am J Sports Phys Ther. 2010 Sep;5(3):179–88.
TABLE 4: TARGETS TO REDUCE ALLOSTATIC LOAD (AN INCOMPLETE LIST)
NB: THESE WILL VARY DEPENDING ON AN INDIVIDUAL’S SKILL-SET AND TREATMENT PREFERENCES
Myofascial tension
Altered biomechanics
Diaphragm/pelvic floor/core function
Breathing mechanics
Lymphatic drainage
Somatic nervous system
Autonomic nervous system
Discussion/education regarding fear avoidance behaviours
Education on pain or allostatic load
Visceral mobility
The role of adhesions
Exploration of social factors
Discussion around contributing environmental factors
Discussion around the contribution of trauma history (being particularly mindful of our scope of practice)
Identification of other stressors
CLINICAL 25

Osteopathic approach to managing the pregnant patient
We understand that treating a pregnant patient does not exist in a vacuum. Careful consideration must be made to previous pregnancies, birth experiences and postpartum health. For the purposes of this article, we have collated the most current research, combined with our many years of clinical experience, to provide you with an introduction on how to treat pregnant patients safely throughout pregnancy. For an extensive overview on osteopathic considerations in pregnancy, birth, and postpartum, please refer to the online course Bump into Osteo (bumpintoosteo.com.au).
THE ROLE OF THE OSTEOPATH
Pregnancy is an incredibly transformative journey, one that shows our body’s remarkable capacity to change and adapt. The physiological, hormonal, and biomechanical changes impacting all body systems are essential to facilitate the growing baby and in preparation for birth.
These changes can lead to an increased load on joints and connective tissue which, for some, can lead to various musculoskeletal conditions,1 with some reports suggesting up to 50% of pregnant women experience pelvic and back pain.2
Pregnant women have limited options when it comes to pain relief, therefore manual therapy may be the only option available. Some may also seek osteopathic care to be proactive in maintaining health before strain presents or they may be seeking advice in preparation for birth.
Osteopaths can play a key role in the care of pregnant patients. Osteopaths appreciate the systemic interconnections required during pregnancy, labour and birth. With that in mind, osteopaths can influence the structure and function of the musculoskeletal, respiratory, circulatory, digestive and autonomic nervous system.
BIOMECHANICAL AND HORMONAL CHANGES IN PREGNANCY
Understanding the hormonal and biomechanical changes that occur in pregnancy is necessary to appreciate how these changes can lead to neuromusculoskeletal conditions, and how we can then apply osteopathic
principles in the treatment and management of our patients.
Hormones
Primarily, altered levels of oestrogen, progesterone and relaxin will impact cartilage, ligaments and bone in pregnancy.
During pregnancy, oestrogen acts to decrease collagen synthesis and fibroblast proliferation. Changes to collagen can reduce ligament integrity and the ability of the ligament to withstand load, therefore increase risk of sprain and injury.
Relaxin acts to reduce the density and organisation of collagen bundles and leads to a marked local decrease in total collagen content. Relaxin reduces myotendinous stiffness by increasing tendon laxity through activation of collagenase.
These hormones result in a breakdown of collagen in targeted tissues, especially tissues around the pelvis, which is then replaced by modified collagen containing higher amounts of water to make the tissues more elastic.1
This modification results in ligament laxity and cartilage softening. This hormone shift is necessary to prepare the body for birth, but in some pregnant patients can lead to sources of pain and strain due to decreased joint stability and increased dependence on muscles around the pelvis.3
Biomechanical changes
The increasing size of breasts and growth of the baby results in anterior tilt of the pelvis.4 The centre of gravity is displaced anteriorly, resulting in an increased

ABOUT THE AUTHORS
Dr Daniela Aiello (Osteopath) and Dr Ash Bolton (Osteopath) have extensive experience in the osteopathic treatment of pregnant and postpartum patients. In 2022 they launched their online course Bump into Osteo and will be presenting an upcoming practical hands-on course in Melbourne and Sydney in 2024. Together in 2023, they designed and created a range of compression support wear for pregnant and postpartum patients: “continuall”. Their postpartum tights are listed on the TGA register as a class 1 medical device. They have presented webinars for Osteopathy Australia in the treatment and management of pregnant patients and been featured on Osteo Talk podcast.
moment arm of pelvic stabilisers and anterior torque at the hip (as large as eightfold). A compensatory increase in the lumbar lordosis shifts the centre of mass back to restore postural balance, which increases shear force at the lumbar facet joints by approximately 60%.5 Stretching of the abdominal muscles combined with the increased torque at the hip are counteracted by a compensatory shortening of the paraspinal muscles to maintain an upright posture.1 This predominately impacts the sacroiliac joint, pubic symphysis and lumbar spine in preparation for birth.1
26 CLINICAL
It is important to note that abdominal separation is a normal physiological change in pregnancy with studies showing 100% of women experiencing a degree of separation in the third trimester, as the linea alba will stretch to accommodate the enlarged uterus.6 Diastasis recti (DRAM) is diagnosed when separation of more than two finger widths is palpated at the middle of linea alba either 4.5cm above or below the umbilicus or a midline bulge with visible exertion.7
As the uterus grows the diaphragm is displaced superiorly approximately 5cm. The negative pleural pressure increases, leading to an earlier closure of the small airways. The chest height becomes shorter, but the other thoracic dimensions increase in order to maintain constant total lung capacity.
In order to compensate for the decreased lung capacity, the rib cage is forced to expand by 10-15cm. This can lead to rib dysfunction and pain as well as strain in the surrounding muscles and connective tissues. The average subcostal angle of the ribs at the xiphoid level increases.
FURTHER BIOMECHANICAL CHANGES OF THE DIAPHRAGM AND PELVIC FLOOR DURING PREGNANCY
The diaphragm muscle has more than one function. Not only does it provide the network necessary for breathing, but it also has other functions including balancing pressures in thoracic and abdominal cavities by working in synchronicity with
the pelvic floor. It also assists with venous drainage and lymphatic flow.
The diaphragm contracts eccentrically during inspiration and contracts concentrically together with the abdominal muscles during forced manoeuvres such as coughing thereby increasing intraabdominal pressure. The pelvic floor muscles work in synchronous cranio-caudal movements with the diaphragm – the pelvic floor and Transverse abdominus (TA) muscles should respond to the pressure of every inhale by relaxing, or eccentrically lengthening. On exhale, the pelvic floor and TA muscles should contract, or concentrically shorten.
This synergy helps to control and respond to changes in intra-abdominal pressure, provide trunk stability and contribute to continence while breathing and coughing.
As mentioned previously, there are hormonal and biomechanical changes during pregnancy that can impact the diaphragm. An enlarging uterus increases abdominal pressure, growing upwards and restricting the diaphragm, and downwards onto the pelvic floor.
COMMON PRESENTING MUSCULOSKELETAL CONDITIONS IN PREGNANCY
Pregnancy related pelvic girdle pain (PPGP)
Pregnancy related low back (PLBP) PPGP and PLBP will likely be the most common complaint osteopaths will see in practice. It affects greater than 50% of pregnant patients.
Other common conditions
Round ligament pain
Pelvic floor myofascial pain
and dysfunction
Wrist pain (carpal tunnel syndrome, DeQuervains tenosynovitis )
Foot pain (plantar fasciitis)
Hip dysfunction (greater trochanter pain syndrome, lateral femoral cutaneous neuropathy)
Headaches
Thoracic joint pain
Cervical joint pain
DIFFERENTIAL DIAGNOSIS OF LOW BACK AND PELVIC PAIN IN PREGNANCY
Pregnancy related pelvic girdle pain (PPGP) is an umbrella term encompassing several specific musculoskeletal conditions involving the sacroiliac joints, pubic symphysis and neighbouring connective tissue.
Pregnancy related low back pain (PLBP) refers to pain arising from the joints of the lumbar spine and surrounding soft tissues. Both PPGP and PLBP can occur simultaneously in the same patient.1
Having a sound understanding of common symptoms and presentations of PPGP and PLBP and how patients describe their pain can greatly improve history taking, evaluation and determining the specific etiology of pain for each patient. The onset of PPGP can happen at any point during a pregnancy, but most often will occur between 18 and 36 weeks gestation.8
PELVIS LUMBAR HIP
Sacroiliac joint dysfunction
Sacro-coccygeal joint dysfunction
Pubic symphysis dysfunction
Pelvic floor dysfunction
Pelvic floor prolapse
Osteitis Pubis
Piriformis syndrome
Lumbar facet joint sprain
Lumbar disc pathology
Lumbar radiculopathy
Lumbar muscle strain
Neuropathies
Cauda equina syndrome
Extra articular hip pathology
• Trochanteric bursitis
• Muscle tendonopathies/tears
• Round ligament pain
• Transient osteoporosis of pregnancy
Intra articular hip pathology
• Femoral acetabular impingement
• Developmental dysplasia of the hip (congenital dislocation of the hip, hip subluxation, acetabular dysplasia, and malformation of the femoral head)
• Inflammatory arthritides
• Labral tear
• Osteoarthritis
• Osteonecrosis
CLINICAL 27
TABLE 1: POTENTIAL MUSCULOSKELETAL DIFFERENTIAL
Sacroiliac joint dysfunction is one of the most common causes of PPGP. Research suggests that the long dorsal sacroiliac ligament is believed to be a source of posterior pelvic pain due to the forces transmitted from the SIJ and hip joint to the nociceptors and proprioceptors within the ligament.1
Typical clinical presentation: Pain arising from the sacroiliac joint will typically be described as:
Dull ache around the sacrum and buttocks (may be unilateral or bilateral);
Pain in their “hip,” referring to pain in the lateral thigh and/or groin area;
Leg pain as well as numbness and tingling, often radiating down the back of the leg, which can mimic lumbar radiculopathy or sciatica;
Describe a feeling of giving way on the side of pain.
Aggravating factors:
Pain with transitional movements, i.e. from sitting to standing;
Pain increasing with speed of walking; Stair climbing;
Turning over in bed;
Standing on one leg, i.e. putting underwear and pants on.
Patients often describe a feeling of giving way on the side of pain, making a complete neurologic exam essential to exclude a true neurologic deficit. It is important to note that lumbar disc herniations occur in approximately one in 10,000 pregnancies, which is not significantly different from the rate in nonpregnant people of childbearing age.9
TABLE 2: RED FLAGS TO REVIEW ON EVERY CONSULTATION
RED FLAG
PATHOLOGY
Decreased foetal movement * Placental abruption, pre-term labour
Vaginal bleeding
High blood pressure
Fever
Sudden abdominal pain
Unilateral leg swelling
Placental abruption, placenta previa, pre-term labour
Preeclampsia
Cholecystitis, UTI, infection
Pre-term labour, cholecystitis, preeclampsia
DVT
* Typically, foetal movement is felt between 16 to 24 weeks gestation. Primigravida patients will often not feel foetal movements until after 20 weeks gestation.1
Pubic Symphysis Dysfunction or SPD is also a likely cause of PPGP. Important to note that both SPD and SI joint dysfunction may occur simultaneously in the same patient. Patients with pubic symphysis dysfunction will describe pain: In their lower abdomen and pubic bone, perineum, groin or adductor region; Aggravated with weight bearing and walking and as a result they develop a more prominent waddling gait pattern; Pain and weakness when lifting legs and pain rolling over in bed that’s not always relieved with cessation of movement; Palpation over the joint may elicit exquisite pain.
Note: pubic symphysis issues and groin hernias can have similar presentations. The pubic symphysis capsule inserts within millimetres of the superficial inguinal ring. This anatomic proximity helps explain why they can mimic each other on clinical presentations. Patients who suffer from a true diastasis of the pubic symphysis will usually
describe click during delivery, usually accompanied with swelling in the area.1
See Table 1 on page 27, a table of potential musculoskeletal differential diagnosis that need to be considered.
Red flags not to be missed in case history
Specific attention to red flags must be made during initial history taking and must be reviewed in every consultation during pregnancy (see Table 2).
Signs and symptoms in combination
Patients may describe symptoms that can be the result of normal physiological changes in pregnancy. In isolation these symptoms may be considered innocuous, but in combination may indicate serious pathology. Understanding the serious pathologies that can occur in pregnancy will assist in differentiating between normal physiological changes or the need for immediate referral (see Table 3 on page 28).
TABLE 3: SYMPTOMS RELATING TO PHYSIOLOGICAL CHANGES VERSUS SERIOUS PATHOLOGY
SYMPTOMS PHYSIOLOGICAL CHANGES IN PREGNANCY SERIOUS PATHOLOGY
Nausea/vomiting HCG hormone cause nausea and vomiting
Urinary increase Pressure on bladder
Shortness of breath
Abdominal pain
Pressure from growing uterus on thoracic cavity
PGP or constipation
Vaginal discharge Increase is common in pregnancy
Vaginal fluid May be urinary loss due to pelvic floor dysfunction
Swelling in legs
Pelvic pressure
Increased fluid retention of pregnancy
PPGP
Cholestasis, hyperemisis gravidam
UTI
Pulmonary embolism
Placental abruption, cholecystitis, ectopic, incompetent cervix
STI or chorioamnionitis
Ruptured membranes, incompetent cervix
Unilateral may suggest DVT, bilateral preeclampsia
Incompetent cervix, cervical prolapse
28 CLINICAL
There are serious conditions not to be missed, the most common being preeclampsia which is characterised by maternal hypertension, proteinuria, oedema, foetal intrauterine growth restriction and premature birth.10 The condition can be life-threatening for the mother and the foetus, therefore it is essential to ask about symptoms of preeclampsia as part of every patient review during their pregnancy.
Symptoms include:
Headache (typically severe and frontal);
Swelling of the hands, feet and face (oedema);
Pain in the upper part of the abdomen (epigastric tenderness);
Visual disturbance (blurring of vision or flashing lights);
Reduced foetal movements. For other serious conditions not to be missed please refer to Table 4.
Medical conditions that are particularly important to be aware of during pregnancy include diabetes, hyper/hypotension, epilepsy, transient osteoporosis in pregnancy (TOP), hyper/hypothyroidism, previous thromboembolism, autoimmune diseases, and blood borne viruses.11
It is important to note that pathologies that can occur in the non-pregnant state can occur in pregnancy, including cancer or fractures.1 We must be diligent in reviewing patients that do not respond to treatment (or worsen) and not rely on the other medical professionals involved, as in most cases we may be the only practitioner concerned with the patient’s musculoskeletal health.
EXAMINATION
Simple considerations can have a significant impact on the overall patient comfort and safety within your treatment room. We must not overheat patients, therefore ensure air is circulating, offer water and do not over-drape your patients.12
There is no gold standard test for PPGP. Diagnosis is based on clinical presentation, the site of pain and the ability to reproduce the pain using specific provocation tests. The posterior pain pelvic provocation test, Patrick’s flexion, abduction, and external rotation (FABER) test and Menell’s test are of highest relevance for SIJ pain. The palpation of the symphysis test and modified Trendelenburg’s test are the
TABLE 4: SERIOUS CONDITIONS TO LOOK OUT FOR DURING CONSULTATION
SERIOUS CONDITION SIGNS AND SYMPTOMS
Cholecystitis
Pre-term labour
Shingles
Placental abruption
Urinary tract infection
Pruritis (usually hands and feet), fever, abdominal pain, nausea/vomiting
Vaginal discharge, abdominal pain, decreased foetal movements
Hypersensitivity over skin, unilateral thoraco/ lumbar pain, fatigue, vesicles
Vaginal bleeding, reduced foetal movement, abdominal pain
Fever, dysuria, suprapubic pain, increased urinary frequency
most sensitive and specific for symphysis pubis pain.13
Try not to move patients too often, as having to roll over multiple times may be uncomfortable and pain-inducing. Side lying (on their left side) with wedge pillow under their abdomen and pillow between knees is a safe, comfortable position.
Pregnancy pillows with belly cut-outs are available, however, careful consideration must be made when choosing to have a patient lying prone. Pregnant patients often favour this position, as they would not otherwise have the opportunity to lie prone, however, in the case of acute lower back pain or pelvic pain it can be extremely difficult to manoeuvre out of.
TREATMENT
Formulating a treatment plan requires the consideration and application of key osteopathic principles. Structure and function are interrelated. Aiming to improve both focal and global tissue mobility will help to improve function. The impact of these changes can extend beyond the neuromusculoskeletal system, with improvements to the respiratory, lymphatic, digestive and urinary systems, which can all lead to more positive birth outcomes. Osteopaths may feel the need to address all the areas of dysfunction, however, in our clinical experience we have seen the benefit of not overly bombarding pregnant patients with many techniques.
Osteopaths who choose to apply highvelocity low-amplitude manipulation as part of their treatment plan for pregnant patients must consider the prothrombotic and joint laxity risk factors to minimise the
risks of potentially dangerous neurological complications.14 Mild and transient adverse events have been reported after lumbar spinal manipulations whereas the serious adverse events reported in the literature all occurred following cervical spinal manipulation either during pregnancy15 or postpartum.16 Joint laxity should also be considered when applying end range techniques, especially in the third trimester of pregnancy.
External Cephalic Version (ECV) is a medical procedure performed by experienced doctors where they apply hands-on pressure to turn the baby from a breech position to a cephalic presentation (head down), while the foetus’ heart rate is monitored closely throughout.17 ECV has a fairly low success rate,18 with approximately 40% successful in nulliparous and 60% in multiparous patients.19
You may hear patients’ account of being told by other allied health professionals that we can ‘turn a baby’. It is important to stay within our scope of practice and acknowledge we cannot perform an ECV. Osteopaths do have an important role, however, in assessing areas of tension or restriction in our patients’ ribcage, pelvis, hip and lower abdominal/ lower uterine tissues that may be preventing the baby moving into position, which can be helpful before an ECV.
ADVICE MANAGEMENT
There are simple modifications that patients can make to help improve mobility and function and avoid aggravating musculoskeletal conditions. Movements such as getting in and out of cars and rolling over in bed should be
CLINICAL 29
“The onset of PPGP can happen at any point during a pregnancy, but most often will occur between 18 and 36 weeks gestation”
encouraged to do so with knees together. Other simple tips such as satin pyjamas and sheets to assist with ease of rolling over in bed can also be beneficial. Studies have shown a reduction in pelvic pain with the use of pregnancy belts and pillows.20,21
Swelling is also a common ailment experienced in pregnancy. Compression garments have been shown to help reduce swelling and improve circulation.22
Constipation in pregnancy is common.23 Therefore, educating patients on hydration, increasing fibre intake, keeping mobile and the use of a stool to place under their feet while on the toilet can reduce straining effort and thereby reduce pressure on their pelvic floor.
EXERCISE IN PREGNANCY
The importance of exercise during pregnancy and the postpartum period has gained support in recent years. For uncomplicated, low-risk pregnancies, moderate activity is now deemed very low risk and has been shown to assist in reducing pain in pregnancy and improve overall maternal and foetal health.24,25
Patients with medical or obstetric complications must be carefully evaluated by their treating physician throughout their pregnancy before exercises are recommended and routinely throughout.
The current recommendation for uncomplicated pregnancies is to meet the Australian Physical Activity guidelines:26
Be active on most, preferably all, days every week;
Accumulate 150 to 300 minutes (2½ to 5 hours) of moderate intensity physical activity or 75 to 150 minutes (1¼ to 2½ hours) of vigorous physical activity, or an equivalent combination of both moderate and vigorous activities, each week, with an activity reduction in second and third trimester for women at risk or pre-term labour or baby growth restriction;
Do muscle strengthening activities on at least two days each week;
Minimise the amount of time spent in prolonged sitting;
Break up long periods of sitting as often as possible;
These guidelines have slightly changed in the last few years. Previously inactive women are now encouraged to participate in physical activity during pregnancy that they were previously told to be cautious or avoid. They are advised to start slowly and gradually progress towards meeting the Australian Physical Activity guidelines.
Exercises to avoid during pregnancy are as follows:25
Contact sports; High altitude;
Laying on back after 20 weeks; Activities that carry a risk of falling; Diastasis Recti patients should avoid abdominal exercises that require high levels of force generation (such as aggressive sit-ups or lifting heavy objects).
When recommending exercises to your patient it is imperative that you confer with their personal trainer/Pilates instructor to ensure your patient is not engaging in activities that may be contraindicated or known to directly aggravate a specific musculoskeletal condition.
BIOPSYCHOSOCIAL ISSUES IN PREGNANCY
Embracing a biopsychosocial model of health requires seeing the psychological, biological and social factors for your patient as inextricable from one another. One factor can impact the other and vice versa. For example, hormonal changes (biological) can lead to mood changes (psychological). These mood changes can affect relationships with their partner and friends, and can sometimes lead to loss of income (social).
Pregnancy can be an incredibly transformative time in a person’s life and these changes can impact their biological, social and psychological wellbeing. Pregnancy may be the first time in their life they need to seek support to cope with these changes. As osteopaths, we need to be aware of the impact these changes can have on our patients and refer to appropriate health professionals in order to provide the best level of care for your patients.
Biological factors in the ‘biopsychosocial model’ capture the physical elements of the body that affect and determine maternal health. The hormones that are altered during and post pregnancy can lead to mood changes that influence psychological health. These mood changes can be influenced by social support too.
Many studies have shown there to be a significant association between physical symptoms and compromised psychological/emotional health.27 Women with PPGP in pregnancy are three times more likely to experience postpartum depression.1 Stress, depression and anxiety have not only been linked to preterm birth but also low birth weight and increased risk of complicated deliveries.28
Physical conditions patients may experience throughout pregnancy not only include the common musculoskeletal conditions, but also encompass many other physical issues postpartum including hemorrhoids, fatigue, dyspareunia and faecal or urinary incontinence.29 These issues can prevent people from working at times, which can lead to loss of income and further stress. Income can also impact stress with partners and families so the flow-on effect continues.
Poor nutrition is another biological factor that can affect mood and psychological wellbeing. The depletion of nutrients throughout pregnancy and a lack of recovery postpartum has been linked to increased risk of depression as well as postpartum depletion.30,31 Postnatal depletion is a condition impacted by nutrient depletion, sleep loss, and emotional shifts that occur postpartum. Patients can suffer the effects of depletion for many years, unaware of the support and treatments that are available.32
Referral to a dietitian can therefore enhance nutritional uptake and improve maternal mental health outcomes.
Social factors have been shown to play a protective role and moderate the impact of stress on physical and psychological health.33 Evidence suggests that a lack of social support increases the risk of postnatal depression.34
Of particular significance is the need for practitioners to employ clinically sensitive language, as it profoundly impacts patients’ experiences and outcomes. Research indicates that positive and empowering language not only aids in
30 CLINICAL
pain management, but also contributes to better birth outcomes.35 By recognising the potential effects of our words, osteopaths can create a supportive and empowering environment for pregnant individuals. Empowering pregnant patients through education, suggesting counselling if needed, or personalised birth planning can further enhance their confidence and reduce anxiety levels surrounding any fear of birth.
As health practitioners we need to be aware of the risk factors that are linked to antenatal, perinatal and postnatal depression.
Risk factors include:
Low self-esteem; History of anxiety or depression; Low social support;
Low income; History of abuse; Previous traumatic labour and birth; Cultural misinterpretations and beliefs.
Symptoms of perinatal anxiety or depression include:
Panic attacks (palpitations, shortness of breath, shaking);
Persistent, generalised worry, often focused on fears for the health, wellbeing or safety of the baby; Development of obsessive or compulsive thoughts and/or behaviours; Abrupt mood swings; Feeling constantly sad and/or crying for no obvious reason.
Early detection of maternal anxiety and depression is vital for treatment interventions to be implemented, therefore referral to a mental health practitioner as early as possible is necessary.
TAKE HOME MESSAGE
Osteopaths may be the first health professional that patients will see in pregnancy and can play a key role in their journey. We can play an important role in all stages of preconception, pregnancy and postpartum, by helping to improve structural mobility in order to restore function and help to prepare our patients for the upcoming physiological changes. We are privileged to play our role in providing patients with education, reassurance, pain relief, support and continuity of osteopathic care throughout their pregnancy and beyond.
References
1. Fitzgerald, C., & Segal, N. (2015). Musculoskeletal health in pregnancy and postpartum. Switzerland: SPRINGER INTERNATIONAL PU.
2. Kanakaris NK, Roberts CS, Giannoudis PV. Pregnancyrelated pelvic girdle pain: an update. BMC Med. 2011;9:15. Published 2011 Feb 15. doi:10.1186/1741-7015-9-15
3. Parker JM, Bhattacharjee M. Images in clinical medicine. Peripartum diastasis of the symphysis pubis. N Engl J Med. 2009;361(19):1886.”
4. Enders LA, Berger K, Chambers AJ, Redfern R, McCrory JL. Biomechanical evidence of wadling during pregnancy. In: Proceedings of the BMES 2009 Annual Fall Scientific Meeting; 2009 October 7–10; Pittsburgh, PA.”
5. Whitcombe KK, Shapiro LJ, Lieberman DE. Fetal load and the evolution of lumbar lordosis in bipedal hominins. Nature. 2007;450(7172):1075–8.”
6. Mota, P., Gil Pascoal, A., & Bo, K. (2015). Diastasis Recti Abdominis in Pregnancy and Postpartum Period. Risk Factors, Functional Implications and Resolution. Current Women s Health Reviews, 11(1). doi:10.2174/1573404811011 50914201735
7. Thabet, A. A., & Alshehri, M. A. (2019). Efficacy of deep core stability exercise program in postpartum women with diastasis recti abdominis: a randomised controlled trial. Journal of musculoskeletal & neuronal interactions, 19(1), 62–68.
8. Ostgaard HC, Andersson GB, Karlsson K. Prevalence of back pain in pregnancy. Spine (Phila Pa 1976). 1991 May;16(5):549-52. doi: 10.1097/00007632-199105000-00011. PMID: 1828912.
9. Weinreb JC, Wolbarsht LB, Cohen JM, Brown CE, Maravilla KR. Prevalence of lumbosacral intervertebral disk abnormalities on MR images in pregnant and asymptomatic nonpregnant women. Radiology. 1989 Jan;170(1 Pt 1):125-8. doi: 10.1148/radiology.170.1.2521192. PMID: 2521192.
10. Mayrink J, Costa ML, Cecatti JG. Preeclampsia in 2018: Revisiting Concepts, Physiopathology, and Prediction. ScientificWorldJournal. 2018;2018:6268276. Published 2018 Dec 6. doi:10.1155/2018/6268276
11. Weiniger, C.F., Einav, S., Elchalal, U. et al. Concurrent medical conditions among pregnant women - ignore at their peril: report from an antenatal anesthesia clinic. Isr J Health Policy Res 7, 16 (2018). https://doi.org/10.1186/s13584-0180210-7
12. Thurston RC, Luther JF, Wisniewski SR, Eng H, Wisner KL. Prospective evaluation of nighttime hot flashes during pregnancy and postpartum. Fertil Steril. 2013;100(6):1667-1672. doi:10.1016/j.fertnstert.2013.08.020
13. Carlson HL, Carlson NL, Pasternak BA, Balderston KD. Understanding and managing the back pain of pregnancy. Curr Womens Health Rep. 2003 Feb;3(1):65-71. PMID: 12521555.
14. Stuber JK, Wynd S, and Carol Ann Weis CA. “Adverse effects from spinal manipulation in the pregnant and post partum period”, a critical review of the literature Chiropractic & Manual Therapies, 2012, 20:8.
15. Schmitz A, Lutterbey G, von Engelhardt L, von Falkenhausen M, Stoffel M. Pathological cervical fracture after spinal manipulation in a pregnant patient. J Manipulative Physiol Ther. 2005 Oct;28(8):633-6. doi: 10.1016/j. jmpt.2005.08.017. PMID: 16226634.
16. Ng KP, Doube A. Stroke after neck manipulation in the post partum period. N Z Med J. 2001 Nov 9;114(1143):498. PMID: 11797875.
17. Bin, Y.S., Roberts, C.L., Nicholl, M.C. et al. Uptake of external cephalic version for term breech presentation: an Australian population study, 2002–2012. BMC Pregnancy Childbirth 17, 244 (2017). https://doi.org/10.1186/s12884-0171430-5
18. Hutton, E.K. Hofmeyr, G.J. Dowswell, T. (2015) External cephalic version for breech presentation before term. Cochrane Database of Systematic Reviews, Issue 7. Art. No.: CD000084. DOI: 10.1002/14651858.CD000084.pub3. [Accessed 12 May 2021]
19. RCOG (2010). GuidelineNo. 20a. Available at: https:// www.rcog.org.uk/globalassets/documents/guidelines/ gt20aexternalcephalicversion.pdf [Accessed 12 May 2021].
20. Mens, J.M.; Damen, L.; Snijders, C.J.; Stam, H.J. The mechanical effect of a pelvic belt in patients with pregnancyrelated pelvic pain. Clin. Biomech. 2006, 21, 122–127.
21. Vermani E, Mittal R, Weeks A. Pelvic girdle pain and low back pain in pregnancy: a review. Pain Pract. 2010;10(1):60–71.
22. Saliba-Júnior OA, Rollo HA, Saliba O, Sobreira ML. Positive perception and efficacy of compression stockings for prevention of lower limb edema in pregnant women. J Vasc Bras. 2022 Jan 31;21:e20210101. doi: 10.1590/16775449.210101. PMID: 35399341; PMCID: PMC8958436.
23. Gomes, C. F., Sousa, M., Lourenço, I., Martins, D., & Torres, J. (2018). Gastrointestinal diseases during pregnancy: what does the gastroenterologist need to know?. Annals of gastroenterology, 31(4), 385–394. https://doi.org/10.20524/aog.2018.0264
24. Davenport, Margie H. Ph.D. EXERCISE DURING PREGNANCY, ACSM’s Health & Fitness Journal: 9/10 2020Volume 24 - Issue 5 - p 10-17 doi:10.1289/EHP6221
25. Ing, P Exercise after pregnancy, (2022), Australian journal of General Practice, Volume 51, Issue 3, March 2022
26. Brown WJ, Hayman M, Haakstad LAH, Lamerton T, Mena GP, Green A, Keating SE, Gomes GAO, Coombes JS, Mielke GI. Australian guidelines for physical activity in pregnancy and postpartum. J Sci Med Sport. 2022 Jun;25(6):511-519. doi: 10.1016/j.jsams.2022.03.008. Epub 2022 Mar 16. PMID: 35418334
27. Craig PL, Knight J, Webster V, Harris E. Initiation and Duration of Breastfeeding in an Aboriginal Community in South Western Sydney. J Hum Lact. 2011 Aug; 27(3):250-61. PMid:21788654 http://dx.doi.org/10.1177/0890334411402998
28. Sandman C, Davis E, Buss C, Glynn L. Exposure to Prenatal Psychobiological Stress Exerts Programming Influences on the Mother and Her Fetus. Neuroendocrinology. 2012; 95(1): 8-21. PMid:21494029 http://dx.doi.org/10.1159/000327017
29. Borders N. After the Afterbirth: A Critical Review of Postpartum Health Relative to Method of Delivery. J Midwifery Womens Health. 2006 Jul-Aug;51(4): 242-8. PMid:16814217. http://dx.doi.org/10.1016/j.jmwh.2005.10.014
30. Alpert JE, Mischoulon D, Nierenberg AA, Fava M. Nutrition and depression (Focus on folate). Nutrition. 2000 JulAug;16(7-8):544-6. http://dx.doi.org/10.1016/S0899-9007(00)00327-0
31. Beard JL, Hendricks MK, Perez EM, Murray-Kolb LE, Berg A, Vernon-Feagans L, et al. Maternal Iron Deficiency Anemia. Affects Postpartum Emotions and Cognition. J Nutr. 2005 February 1; 135(2): 267-72. PMid:15671224
32. Serrallach, O., & Englhardt, M. (2018). The postnatal depletion cure : a complete guide to rebuilding your health & reclaiming your energy for mothers of newborns, toddlers, and young children. UK: Hachette
33. Razurel C, Bruchon-Schweitzer M, Dupanloup A, Irion O, Epiney M. Stressful events, social support and coping strategies of primparous women during the postpartum period: a qalitative study. Midwifery. 2011; 27(2): 237-42. PMid:19783333 http://dx.doi.org/10.1016/j.midw.2009.06.005
34. Webster J, Linnane JW, Dibley LM, Hinson JK, Starrenburg SE, Roberts JA. Measuring Social Support in Pregnancy: Can it be Simple and Meaningful? BIRTH. 2000 Jun; 27(2):97-101. PMid:11251486 http://dx.doi.org/10.1046/j.1523536x.2000.00097.x
35. Nieuwenhuijze M, Leahy-Warren P. Women's empowerment in pregnancy and childbirth: A concept analysis. Midwifery. 2019 Nov;78:1-7. doi:10.1016/j.midw.2019.07.015. Epub 2019 Jul 15. PMID: 31325736.
36. Buultjens, M., Murphy, G., Robinson, P., & Milgrom, J. (2013). The perinatal period: A literature review from the biopsychosocial perspective. Clinical Nursing Studies, 1(3). doi:10.5430/cns.v1n3p19
37. Conder, R.; Zamani, R.; Akrami, M. The Biomechanics of Pregnancy: A Systematic Review. J. Funct. Morphol. Kinesiol. 2019, 4, 72. https://doi.org/10.3390/jfmk4040072
38. Hofmeyr, G.J. Sadan, O. Myer, I.G. Galal, K.C. Simko, G. (1986) External cephalic version and spontaneous version rates: ethnic and other determinants. Br J Obstet Gynaecol, 93:13–16.
39. Lau, T.K. Lo, K.W.K. Wan, D. Rogers, M. (1997). Predictors of successful external cephalic version at term: a prospective study. Br J Obstet Gynaecol, 104:798–802.
40. Ostgaard S, Noren L, Johansson G, Ostgaard HC. Lumbar back and posterior pelvic pain during pregnancy: a 3-year follow-up. Eur Spine J. 2002;11(3):267–71.
41. Parry BL, Sorenson D, Meliska CJ, Basavaraj N, Zirpoli GG, Gamst A, et al. Hormonal basis of mood and postpartum disorders. Curr Womens Health Rep. 2003 Jun; 3(3):230-5. PMid:12734034
42. Ressler KJ, Nemeroff CB. Role of serotonergic and noradrenergic systems in the pathophysiology of depression and anxiety disorders. Depress Anxiety. 2000; 12 Suppl 1:2-19. http://dx.doi.org/10.1002/1520-6394(2000)12:1+<2::AIDDA2>3.0.CO;2-4
43. Williams A, Herron-Marx S, Knibb R. The prevalence of enduring postnatal perineal morbidity and its relationship to type of birth and birth risk factors. J Clin Nurs. 2007 Mar; 16(3):549-61. PMid:17335531 http://dx.doi.org/10.1111/j.13652702.2006.01593.x
CLINICAL 31
How can you earn more as an osteopath this year?
On average, osteopaths earn between $80k and $90k, according to the most recent data from Osteopathy Australia. With cost of living pressures, have you thought about how you can add additional income?
Whilst income potential is likely not the reason you became an osteopath, your health, wellbeing and business success are influenced by it. The good news is that in addition to consultations or during them, there are ways to earn more money.
Putting your osteo business hat on
Your primary focus is applying your skills to patients through consultations and care. You also have the opportunity to build your business revenue stream with complimentary services to existing patients, particularly those who ask you about sleep or beds.
The common assumption is that many clinics will establish themselves in areas of high visibility or demand. Often businesses build up their clientele with varied treatment areas or with a range of practitioners with additional qualifications or services. While all are valid, these strategies may take time to implement, with the rewards not immediately coming to your bottom line.
What if you could supplement your income with products and services that align with your business and practitioner values? A passive income stream you can implement that isn’t reliant on extra time, or additional investment whilst also supporting patient health outcomes and complementing your existing services and practice?
Passive income for osteopaths
Passive income is an opportunity for health practitioners and clinics to earn more in revenue with less time and input than an individual consultation. It’s an opportunity that more osteopaths are looking at closely, partnering with products, services or platforms that provide this.
One such avenue is the DrRest sleep
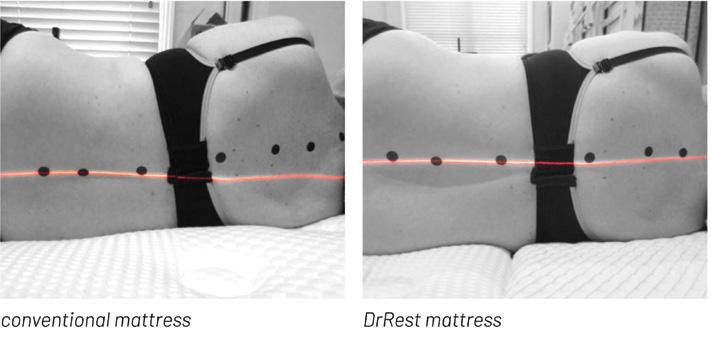
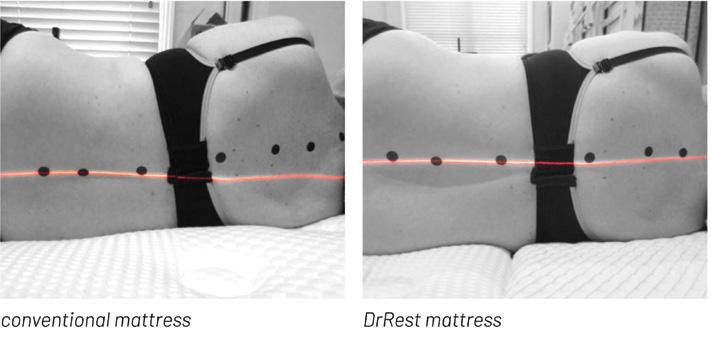
system, which was developed in Melbourne. Endorsed by Osteopathy Australia, DrRest offers achievable passive earning potential and increases how much you earn. Paired with improving your patient’s sleep quality and treatment outcomes, it’s worthy of every osteopath’s consideration.
What osteopaths like about this passive earning avenue
When DrRest launched to the market in 2022, it presented a quite distinct business model from what many osteopaths were accustomed to. Many clinics already sell vitamins, supplements or treatment aids designed for placement on the reception shelf for patients to purchase. The concept of recommending and transacting an actual mattress with a substantial dollar value in return was either new and exciting or daunting and overwhelming.
“Would I need to put a mattress in my clinic taking up space?” was a common question. The answer is adaptable - no, by simply being a referral partner, or yes if you have the space for maximum return. DrRest’s Dr George Michael notes, “It was important to us that there were options for all osteopaths. We want to ensure that this mattress is right where it should be for patients to benefit and for those treating them holistically to benefit as well. We’ve given practitioners the level of involvement they would like in providing their professional recommendation and
the return that comes from that.”
For the osteopaths who have joined DrRest, the benefits are flowing through. One DrRest partner in Melbourne has already seen a 15% increase in earnings this financial year without a substantial shift in the number of consultations conducted. Their DrRest partnership has provided them a profit of just under $16k from eight DrRest mattresses sold to patients with poor sleep quality and unresolved pain.
A business shift found through sleep
As we all know, sleep plays a crucial role in health, however, its importance can be easily overlooked by patients and practitioners. Maybe a new pillow, going to bed early, less screentime, adjusting sleep position will help? Critically, it’s the sleep surface that is fundamental to any real, lasting results. Whilst an osteopath isn’t a mattress salesperson, likewise, a mattress salesperson isn’t a health practitioner with
32 INDUSTRY ADVERTORIALUPDATE 3 2
ADVERTORIAL
Conventional (non DrRest) mattress
DrRest mattress
Super King $3,265 $5,999 $2,734 King $2,985 $5,499 $2,514 Queen $2,450 $4,499 $2,049 Double $2,200 $3,999 $1,799 King Single $2,065 $3,799 $1,734 Single X-Long $1,905 $3,499 $1,594 Single $1,795 $3,299 $1,504
DrRest OA DrRest OAMember Mattress Member RRP Margin
knowledge of anatomy, physiology, pain management, or individual patient needs.
For the DrRest sleep system, the focus is not about selling a mattress but instead supporting a health outcome - providing quality, restful sleep designed by health professionals. When our partners realise that it’s not about an uncomfortable conversation on the complicated options of springs or toppers, but instead just the one mattress designed for every body type, it becomes a natural professional recommendation that puts a mattress conversation right where it should be - in a clinic, not a retail store.
How to earn more as an osteopath this year
If caring about your patients beyond the consultation room is a key aspect of your business offering, consider increasing your passive income as a DrRest partner or referral partner.
To demonstrate what’s possible, as a full partner maximising the opportunity, one queen size DrRest mattress sale is equivalent in earnings to approximately 18 osteopathic consultations, delivering just over $2,000 straight onto your bottom line. The mattress sale is yours, once the wholesale order is processed online through your portal login. When the mattress is dispatched directly to your patient under full warranty of care by DrRest, the profit will already be there in your account.
However, if being a DrRest partner isn’t for you, then consider becoming a DrRest referrer. By referring a queen size mattress to one of your patients that results in a sale, you will earn $400 +GST, the equivalent earnings to approximately four consultations. Dr Michael says “Right now, it's about expanding the options for patients to get the best sleep surface for them. We want those conversations to happen with their health professional. Being a referrer facilitates that conversation and we value your expertise and time highly in return.”
Where can patients see the DrRest mattress?
DrRest has a dedicated showroom in Knoxfield, Victoria, and there are also DrRest partners in clinics around metropolitan Melbourne, regional Victoria & New South Wales. These locations allow patients to see, feel and learn how the DrRest sleep system supports their health.
*Assuming consult valued at $100, 18 consultations equals 1 queen size mattress sale as a Dr Rest Partner. YOUR profit is the RRP less OA member price = $2,049 1 queen size mattress sale as a Dr Rest Referrer equals 4 consultations = $440. 2K
Considering that over 80,000 Australians* visit an osteopath weekly, with the osteopathy industry contributing over $500 million per year to the Australian economy, maximising your business within that environment means standing out and offering patient support in diverse ways that are valuable to them. Where and how they sleep is a place to start.
So rest assured that it is possible to increase what you earn this year without changing the hours you consult or increasing fees. A mattress that changes a patient’s sleep quality, treatment outcomes and enhances their wellbeing may also support yours.
*https://osteopathy.org.au/article/working-as-an-oste opath-in-australia

For more information on the DrRest research and sleep system mentioned above visit www.drrest.com.au Osteopathic partners and referrers are invited to learn about wholesale business opportunities for your clinic by emailing info@drrest.com.au Find out
INDUSTRY UPDATE 33 ADVERTORIAL 3 3
LOWER BODY ZONE SUPPORT FOR ALL BODY TYPES OPTIMAL PRESSURE RELIEF SHOULDER ZONE HEAD ZONE Comfort construction - quilted bottom zones. Unique support system with a self-levelling design that adapts to each body to minimise hammocking or side bending of the spine. To neck, shoulders, spine, lower back and hips. The DrRest shoulder zone has been expertly designed with Technogel©, the world’s only three dimensional biocompatible comfort layer. Comfort constructionquilted top.
more
* PROFIT DR REST PARTNER DR REST REFERRAL PER MATTRESS SOLD CONSULTATIONS 18 400 * PROFIT PER MATTRESS REFERRAL = CONSULTATIONS 4 $ $ =
CPD calendar
Key dates for your diary throughout the coming months.
UPCOMING WEBINARS
8 MAY 2024 — 7:30PM
Osteopathy for birth preparation, supporting pregnant patients
Presenter: Kathryn Johns, Elizabeth Johns and Simone Keddy
Register: Via CPD Hub
15 MAY 2024 — 7:30PM – 8:30PM
Beneath the surface – exploring fascia’s role in pain
Presenter: Jack Williams
Register: Via CPD Hub
AVAILABLE NOW
Informed consent in under 20 minutes
Presenter: Christie Boucher
Register: Via CPD Hub
ENDORSED COURSE
26-27 JULY 2024
BioBasics – A didactic & laboratory exploration into the principles and practice of The Biodynamic Model – Victoria
WORKSHOPS
19 MAY 2024 — 8:30AM – 4PM
Shoulder impingement: A postural model – Melbourne
Presenter: Don Hunter
Location: High Street Holistic, 60 High Street, Preston Register: Via CPD Hub
25 MAY 2024 — 9AM – 4PM
Pregnancy and osteopathy a complete introduction
Presenter: Daniela Aiello and Ash Bolton
Location: Victoria University City Tower, Level 16 Room 10, 370 Little Lonsdale Street, Melbourne.
Register: Via CPD Hub
TBA JUNE
Shoulders rehabilitation essentials
Presenter: Wayne Rodgers
Location: Brisbane TBA
E-LEARNING
AVAILABLE NOW
Introduction to the National Disability Insurance Scheme (NDIS Module 1 of 3)
Register: Via CPD Hub
AVAILABLE NOW
8-9 years social and emotional development
Register: Via CPD Hub
AVAILABLE NOW
8–9-year old common conditions
Register: Via CPD Hub
AVAILABLE NOW
Working with people with disability (NDIS Module 2 of 3)
Register: Via CPD Hub
COMING SOON
Understanding osteopathic NDIS




34 CPD CALENDAR
SAVE THE DATE 25 – 26 OCTOBER 2024 OSTEOPATHY CONFERENCE – SYDNEY Sydney Central Hotel 169/179 Thomas St, Haymarket NSW
Of cial partner of Osteopathy Australia
Cliniko is an all-in-one practice management platform that helps you manage and grow your business, so you have more time to focus on patients.
Quick and easy to set up, Cliniko lets you work from any location, on any device to keep your practice running smoothly. Coordinate your appointment scheduling, offer convenient online bookings, create customised treatment notes and body charts that meet your needs, and so much more!
Special offer for Osteopathy Australia members

Cliniko is now professionally approved by Osteopathy Australia. To celebrate, we’re tripling our trial period for OA members. Sign up today to get 90 days of Cliniko, totally free.
Start your 90-day free trial at cliniko.com/oa-member
$




Done For You Practice Management NEW STARTER PLAN FROM JUST $9.50* PER MONTH! START A FREE TRIAL TODAY! $ The Most L ved and Most Secure Practice Management Software Scheduling & payments Client waitlist & reminders Online forms & bookings Get your evenings back with intuitive, award-winning EHR Progress notes, letters & reports Practice operations manual In-Platform telehealth