




FREE freight on all online orders


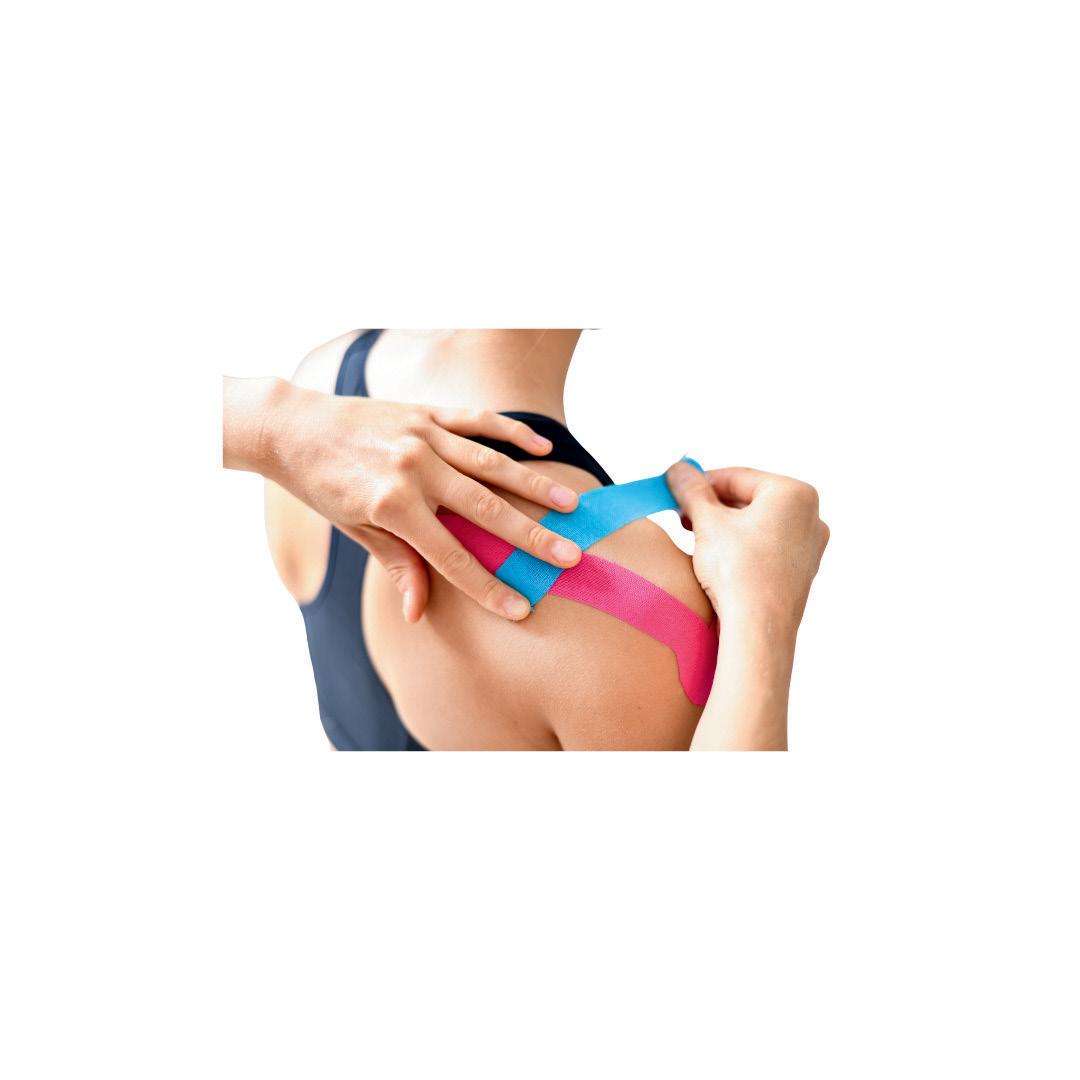
We offer a full range of products for your practice, from treatment tables and assessment tools to rehabilitation aids, pain management products, braces, orthotics, and massage essentials.
Whether you're setting up a new clinic or stocking up on essentials, we've got you covered!









s 2025 draws to a close, it’s the perfect time to reflect on the year that’s been and to look ahead to what lies ahead for our profession.
One of our major projects of the year has been the launch of our brand-new member database and website, which is now live. We know how important it is for members to have a system that’s easy to use and genuinely helpful. The new platform is a huge step forward, more intuitive, more efficient, and designed to give you a smoother experience. While we are confident it represents a major upgrade, as with any new system there may be some initial teething issues. We’ll continue refining and improving based on your feedback. Beyond this, the platform creates opportunities for us to enhance membership offerings as the profession continues to evolve.
It was wonderful to be able to catch up with so many members over the last few months, starting at our conference with our friends from Osteopathy NZ held in Auckland from 5–7 September. It was fantastic to see so many of our members presenting on their areas of expertise, research and special interests. Well done to everyone involved.



direction of the Association, and I appreciate the time and effort you took out of your week to be part of the discussion. There have also been some changes to the Board in recent months. We extend a heartfelt thank-you to Brett Wiener who finishes his time on the Board at the end of December. Brett has been a tireless advocate for our members and has played a pivotal role in securing fantastic outcomes for the Association. With his term concluding, Brett also steps down as Vice President, and I’m pleased to share that Tink Gee will take on the role of Vice President from 2026.
Our AGM was held in Melbourne on 24 October alongside the Melbourne community forum. We also held similar connect sessions across every state and territory, as well as online. These meetings have been invaluable in allowing us to connect with you directly, hear your feedback and share updates on the work being done behind the scenes. The conversations in these sessions have been both constructive and energising, and I want to extend my sincere thanks to everyone who attended. Your contributions are instrumental in shaping the future
We also extend a fond farewell and so much appreciation to Joey Calandra who stepped down from the Board at the end of November after four years of service as an external director. Joey’s wealth of knowledge in the allied health and digital health space has been immense and invaluable, and his commitment has left a lasting imprint on our Association. We welcomed two new directors in the second half of 2025, Osteopathy Australia member Mollie McCarthy started as the new Early Careers Director (replacing Julia Biernacki) and a soon-to-start Stefanie Johnstone who will be replacing Joey as an External Director. Stefanie plays a pivotal role in enabling impactful research at Deakin University. By integrating her strategic planning, operational insights, and collaborative leadership, Stefanie will help ensure that our research initiatives are both innovative and aligned with Osteopathy Australia’s ambitions. Her multidisciplinary background, from medical science to creative writing, supports a well-rounded and holistic approach to her strategic responsibilities at the Association. Both will bring incredible insight and expertise as our Board continues to evolve.
Thank you once again for your ongoing support and engagement throughout 2025. Together, we’ve achieved a lot this year, and I’m excited for what lies ahead as we continue building a stronger, more connected future for osteopathy in Australia.
Yours in health, MATT COOPER
President mcooper.director@osteopathy.org.au
Osteopathy Australia acknowledges the Traditional Custodians and Elders of Country throughout Australia, and their connection to land, sea and community. We pay our respects to Aboriginal and Torres Strait Islander Elders, past, present and emerging.

Osteopathy Australia T (02) 9410 0099 E info@osteopathy.org.au W www.osteopathy.org.au osteopathyaustralia osteopathyau osteopathyaustralia
OSTEO LIFE is a magazine for Osteopathy Australia members.
For enquiries, feedback, or to contribute, contact Communications on 02 9410 0099 or comms@osteopathy.org.au
For advertising enquires, email info@osteopathy.org.au
Communications and Marketing
Working Group Tara Bain, Toby Barker, Adam Nicholson, Rebekka Thompson-Jones
Chief Executive Antony Nicholas Editor Rebekka Thompson-Jones
Designer Stephanie Goh
Advertising
www.citrusmedia.com.au

When Guild Insurance was first established, our mission was to protect and serve the health professionals that our community depended on. And now, over 60 years later, our dedication and commitment remain unwavering. We’ve widened the network of professionals we support, ensuring
your safety and that of your profession, so you can continue looking after your patients.
Through our partnership with Osteopathy Australia, you can trust that you’re supported by a policy tailored specifically for your profession. You also gain access to valuable risk management
resources to help minimise the risk of claims, all while being backed by the industry body that advocates for Australian Osteopaths.
We’re here to support you at every step of your professional journey. Visit guildinsurance.com.au/osteopaths or call 1800 810 213 and be part of something bigger.
Osteopathy Australia aims to support, enhance and promote the profession. Here’s a quick recap of everything osteo from the past few months.
As the osteopathy profession continues to diversify across demographics, cultures, practice areas, scopes, qualifications and emerging career paths it brings added complexity and challenges for Osteopathy Australia. Like all associations, we are a member-focused organisation and must remain customer-centric to meet your evolving needs. We also face a unique challenge: we help shape what you may need, want, or be required to become in the future.
To achieve this with a small team, we must leverage technology and human-centred design (HCD) to better serve you. As we transition to the new member portal, website, CPD and eLearning platform, our goal is to deliver more relevant, streamlined and effective experiences.
As a small organisation, we must optimise how we connect with and support members across Australia. Human-centred design (HCD) begins with empathy, understanding your needs, motivations and challenges. This insight helps us focus on services and programs that solve real problems, driving engagement and satisfaction.

HCD also guides the design of intuitive, enjoyable, and meaningful experiences, whether through services or technology like our member portal and encourages co-creation with you at the centre.
Last year, through member forums, we heard you. The searchability of our website, ease of use of the member portal, and access to CPD weren’t
We want members to see that we listen and that your input directly shapes our offerings. That’s why we’ve transitioned to an entirely new IT platform to address these concerns.
And yes, like anyone who’s ever switched practice software knows, it’s
“We want members to see that we listen and that your input directly shapes our offerings.”
not always smooth sailing. But it’s a necessary step toward building a better, more responsive experience for you.
Over the past several months, we’ve partnered with technology experts to ensure our website, member portal, CPD and eLearning systems are open, user-friendly and member focused. At the same time, we’ve worked with a customer engagement specialist using human-centred design to help shape our future direction.
Rather than assuming we have all the answers, those who’ve participated know we come with questions and ideas -because the real answers come from you, our members. Thank you to everyone who contributed through interviews, surveys, focus groups and more recently the community forums across the country. Your input has been invaluable and helped us develop our focus over the coming years.
We’re excited to share the changes coming over the next year. Our goal is to make it easier for you to connect with us for support, help or advice, improve website searchability and streamline processes such as automated CPD record-keeping. We’re enhancing how your information is displayed and accessed, so you stay informed and up to date.
You’ll also see a broader range of CPD options – micro, short and long-form – alongside growing community forums and more structured mentoring, training and induction programs.
We hope you’ll enjoy the journey with us.
ANTONY NICHOLAS Chief Executive ceo@osteopathy.org.au


by Angie Bruce
ast week I had a call from one of my best friends from university. We graduated in 2003, and we both still practise close to full-time – give or take a few hours. She was very sad after a patient had passed away from cancer and was rocked by the loss. We discussed her feelings both as friends and colleagues, and it has been one of the many discussions over the years, offering support to one another.
In addition to making my own phone calls to friends and colleagues to discuss difficult cases, I’m also married to an osteopath who is open to debriefing on difficult days. We have a difficult and rewarding job, and I think it’s made easier with support. As I’ve got older, I’ve become more conscious of leaning on friends and my husband, aware they have limited resources.
A few years ago, while wondering how to put formal support in place, I was fortunate enough to have a GP speak about her own burnout and how she had joined a BALINT group, which she would recommend to all of us. You can find out more information here: www.balintanz.org. With over 21 years of practice, it’s no surprise that I’ve experienced various forms of burnout and compassion fatigue. In fact, I have found patients to be more complex post-COVID. I applied to join a BALINT group and started my online group within a few months.
BALINT groups emerged following WWI and, since the 1950s, have been used in medical schools, residency programs and
among practising clinicians worldwide.1–3 The Australia and New Zealand BALINT Society is open to all health professionals and has the tag line: ‘Improved care and wellbeing through clinical reflective practice for doctors and other health professionals’. I thought, ‘How wonderful, that comment includes the wellbeing of the practitioner.’ So much of our CPD is focused on improving the care of our patients, and the COVID years highlighted that practitioners of all kinds need to be cared for if they are going to succeed in caring for others.
The idea of reflective practice is more than debriefing about a difficult day. It’s a formal case presentation model facilitated by experienced facilitators with varying specialities – GPs, psychiatrists, psychologists or psychotherapists can all be facilitators. Participants are invited to explore the clinicianpatient relationship using facilitated discussion.
The Australia and New Zealand BALINT Society outlines these foundation principles:
• recognise they are not alone in having challenging interactions with patients or clients;
• develop an increased understanding and empathy for patients or clients;
• explore how feelings and thoughts affect the clinicianpatient and other therapeutic relationships;
• expand their capacity and repertoire for handling difficult situations.
My group is multidisciplinary. There are two GPs with over 20 years of experience in practice, and three novice
“So much of our CPD is focused on improving the care of our patients, and the COVID years highlighted that practitioners of all kinds need to be cared for if they are going to succeed in caring for others.”
GPs, an obstetrician-gynaecologist, a psychiatrist and me. There are occasions when a case is brought forward and solutions are offered. However, mostly it’s about provoking insight, personal growth or satisfaction in practice while reflecting on cases and the interactions between patient and practitioner.
A single clinician presents a case, and the group can ask any clarifying questions. The presenter is then asked to sit back while the group offers perspectives on different aspects of the case. The presenter is then invited back into the group discussion, often with a new perspective on the case and the practitioner-client interaction. For all participants, there are learnings and there is a change in approach, often with more compassion for the client.
WELCOME
THE
We’re delighted to welcome Amanda Sayan to the Osteopathy Australia team as our Research and Grants Project Officer.
Amanda brings over 20 years of experience in international education, most recently serving as Director of Global Engagement at the University of Sydney. She’s passionate about fostering global cooperation and understanding through research – a focus that has seen her develop and manage international partnerships with leading universities around
It takes time to feel safe in a group experience. There are rules of engagement, and facilitators are trained well to build support and trust among participants. There are a variety of cases, the mundane, or more ‘risky’ cases that leave us questioning our knowledge, and may expose our difficulty setting limits, or negative feelings towards patients. These feelings are normalised and, in doing so, help us better understand ourselves and our interactions. By participating in this format, I have experienced improved compassion for myself and, in turn, helped support my patients and improve their care.
In late 2024, I attended the Pelvic Pain Victoria Symposium with 100 clinicians of all varieties, physiotherapists, psychologists, obstetricians and gynaecologists, GPs, pain physicians, occupational therapists, nurses and naturopaths. One session was a presentation on running an in-house supervision run by a psychologist in a large pelvic health physiotherapy clinic. There were so many questions from the audience that it ran overtime, and I noticed a real thirst for all practitioners to be supported in their vocation to care for others.
I’ve been fortunate to work as a supervising clinician at both Melbourne universities over the last eight years, and novice clinicians often have questions and need to discuss interactions with patients. And yet, for most of us, this was the last time we had a formal experience of reflecting on our interactions. I would encourage any osteopath at any point in their career to seek formal support/supervision, and BALINT is one group that offers a facilitated group approach.
1 Turner AL, Malm RL. A preliminary investigation of Balint and nonBalint behavioral medicine training. Fam Med. 2004 Feb;36(2):114–22.
2 Johnson AH. The Balint movement in America. Fam Med. 2001 Mar;33(3):174–7.
3 Adler HM. The sociophysiology of caring in the doctor-patient relationship. J Gen Intern Med. 2002 Nov;17(11):883–90. DOI: 10.1046/j.1525-1497.2002.10640.x.
the world. Her work has centred on facilitating multidisciplinary research collaborations aligned with the United Nations Sustainable Development Goals (SDGs).
Amanda joins Osteopathy Australia part-time, working Monday, Tuesday, and Thursday, and is already bringing her strategic eye and collaborative spirit to our research and grants initiatives.
Please join us in giving Amanda a warm welcome to the team!
Amanda can be contacted via research@osteopathy.org.au

At Osteopathy Australia, our Board is at the heart of shaping the future of the profession, driving advocacy and ensuring strong governance. Like the profession itself, our Board continues to evolve. In recent months, we have farewelled dedicated leaders, welcomed new directors and prepared for fresh perspectives that will guide us into 2026 and beyond.
FAREWELL
We extend a heartfelt thank you to Brett Wiener, who concludes his time on the Board at the end of December. Brett has been a tireless advocate for our members and played a pivotal role in securing outstanding outcomes for the Association. His leadership and vision have strengthened our profession in countless ways. With his term ending, Brett also steps down as Vice President. We are pleased to share that Tink Gee will take on the Vice President role from 2026, ensuring continuity of leadership as the Board looks ahead.
We also extend a fond farewell and deep appreciation to Joey Calandra, who steps down from the Board this month after more than four years of service as an external director. Joey has been a driving force in strengthening governance, expanding strategy and embedding sustainability across our work. His expertise in allied health and digital health has been immense, and

“In recent months, we have farewelled dedicated leaders, welcomed new directors, and prepared for fresh perspectives that will guide us into 2026 and beyond.”
Change also brings new energy. We are delighted to welcome Mollie McCarthy as our Early Career Director, replacing Julia Biernacki. Mollie is an early career osteopath who graduated from RMIT University in 2022 and is now completing a Master of Science in Medicine (Pain Management) at the University of Sydney. Passionate about advocating for the next generation, Mollie is committed to sustainable practice models that support clinician wellbeing and longevity in the profession. She champions both hands-on and hands-off approaches to care, ensuring osteopaths can thrive throughout their careers.

Welcoming Tink Gee and Mollie McCarthy (L-R)
It has been a privilege to contribute to an organisation and a profession I care deeply about, alongside colleagues who share a selfless commitment to protecting and advancing osteopathy in Australia.
When I joined the Board in January 2020, none of us could have predicted the global and national challenges that were about to unfold. From the uncertainty of the pandemic to seismic shifts in healthcare funding, digital transformation and workforce sustainability, the past six years have tested the resilience and adaptability of our profession. They have also highlighted the importance of strong governance, forward thinking and collaboration.
During my tenure, I’ve had the honour of chairing multiple committees, including Finance, the Early Career Advisory Group and Rebuild Better. These roles gave me the opportunity to work closely with colleagues to ensure that our strategic direction aligned with both immediate challenges and long-term opportunities.
• In finance, we strengthened oversight and embedded practices that improved transparency, accountability and sustainability. Today, the organisation is better positioned to weather disruption while continuing to deliver value for members.
• Through the Early Career Advisory Group, we amplified the voices of students and graduates, ensuring that their unique challenges were not only heard but actively shaped our policies, resources, and advocacy.
• Rebuild Better was developed in response to COVID-19, acting as a central hub to provide resources that helped members manage, adapt to, and recover from a rapidly changing environment. Through Rebuild Better, we supported the membership in rebuilding stronger systems and processes – ensuring everyone was equipped to navigate challenges and thrive in a post-COVID landscape.
• Perhaps one of the pieces of work I am most proud of is creating and leading the development of the Caring for the Clinician Framework. This initiative incorporated digital learning to enhance clinician wellbeing and professional development, supporting members through what has been a particularly volatile and challenging time. By focusing on the wellbeing of osteopaths themselves, we strengthened member satisfaction and retention, and set a benchmark for future innovation in member services.
The quality of governance at Osteopathy Australia has improved exponentially since I joined the Board. That growth is a direct reflection of the calibre and commitment of the people I’ve had the privilege to work with. The Board and its committees have been filled with incredible human beings who are selfless, intrinsically motivated and unwavering in their pursuit of excellence. What has struck me most is that the work has always been about more than policies, budgets, and frameworks. It has been about shared purpose – ensuring that Osteopathy in Australia is not only recognised and respected within the broader health
system, but continues to grow, adapt, and deliver value for patients and communities. I also want to thank the staff. The sheer volume of work this outstanding team delivers is nothing short of miraculous. For such a small group tasked with such a huge job, they constantly wear multiple hats and do so with professionalism, creativity and commitment. It has been a true privilege to meet and get to know each of them over the years.
Finally, I want to acknowledge Antony. Many will know his unwavering dedication, but I think it’s worth stating plainly: osteopathy in Australia would not be the same without him. In fact, I would go so far as to say it may not exist in its current form without his leadership, perseverance and integrity. There is a phrase Antony often embodies: “The best work is done when nobody is watching.” It speaks to the importance of integrity, intrinsic motivation and commitment to excellence. It reminds us that true quality is achieved not because of recognition, but because of personal standards and an unshakable belief in the cause. Antony has lived that philosophy every day, and osteopathy is stronger because of it. We all owe him an immense amount of gratitude.
As I conclude my six-year term, I do so with optimism. The profession has challenges ahead – workforce distribution, digital transformation, funding pressures but it also has enormous opportunities. Osteopathy is uniquely positioned to play a greater role in preventative health, multidisciplinary care, and community wellbeing. With the right advocacy, leadership, and continued investment in member value, the profession can not only navigate disruption but thrive within it.
I am grateful for the trust members have placed in me as part of the Board, and for the opportunity to contribute to shaping the future of Osteopathy in Australia. The journey has been rewarding, challenging, and deeply meaningful. And while I may be stepping away from the Board table, I will always remain a passionate advocate for our profession and the people who dedicate their lives to it.

She is also deeply engaged in fostering connections across the osteopathic community and promoting interdisciplinary collaboration, advancing recognition of osteopathy within integrated, team-based models of care. Mollie’s voice will be pivotal in ensuring early career practitioners are heard and represented at the Board level.
We also warmly welcome Stefanie Johnstone, who will replace Joey as an External Director. Stefanie plays a pivotal role at Deakin University in enabling impactful research. By integrating strategic planning, operational insights and collaborative leadership, Stefanie ensures research initiatives are both innovative and aligned with long-term ambitions.
Her multidisciplinary background –from medical science to creative writing – provides a wellrounded perspective. With her expertise in the aged care sector, Stefanie will be a critical voice as new legislation reshapes the landscape. We are excited for the insight and expertise she will bring to the association.
Farewelling
Julia Biernacki

Reflecting on his time, Joey shared:
“With this evolving leadership, Osteopathy Australia is well positioned to continue advancing our advocacy, strengthening research and ensuring the profession thrives in the years ahead.”
As we farewell Brett and Joey, and welcome Mollie and Stefanie, we are reminded that the strength of our Board lies in its ability to blend experience with fresh perspectives. With this evolving leadership, Osteopathy Australia is well positioned to continue advancing our advocacy, strengthening research and ensuring the profession thrives in the years ahead.
I was appointed as an Independent Director to strengthen governance and advise on profession-wide growth. Over four and a half years, it has been a privilege to advocate for osteopathy’s role in healthcare, shaped by my own experience of its profound impact on my health and wellbeing.
I’ve helped co-design a multi-faceted strategy – expanding university programs, building research partnerships, growing the workforce, and supporting the creation of the Osteopathy Australia Research Institute. Serving on the Finance Committee and Early Career Advisory Committee has been rewarding, as has co-designing the association’s Strategic Plan.
I’m grateful for the opportunity to work on strengthening our value proposition and branding, broadening our reach, and improving the member experience. Most of all, I’m thankful to have governed alongside such insightful and committed colleagues – including Presidents Michelle and Matthew, fellow directors Brett, Julia, Tink, Deanne, Andrew, Georgia, Cris and Kathryn, as well as CEO Antony and the Osteopathy Australia team. While it is sad to leave, I know this is the right time. With the new aged care legislation having come into effect on 1 November, Stefanie’s expertise in this area will be invaluable. It has been an honour to contribute.

Osteopathy Australia is pleased to announce two funding opportunities aimed at fostering innovation, building research capacity, and strengthening the evidence base for osteopathy.
Fuel bold ideas that can shape the future of osteopathy.
Funding: Up to $20,000 per project
Open to: All academic levels – including PhD students
Duration: Up to 24 months
The Spark Grant supports high-quality, independent research aligned with Osteopathy Australia’s research priorities. In this round, two grants will be awarded, providing the momentum to launch innovative projects with potential for real-world and societal impact.
Priority research areas:
• Ageing and disability – promoting healthy ageing, reducing falls, and improving functional outcomes;
• Primary and community care – advancing prevention, continuity of care and cost-effective health delivery;
• Musculoskeletal and pain conditions – improving outcomes in musculoskeletal pain, pelvic pain and endometriosis;
• Women’s health – supporting health across the lifespan and capacity building for women’s wellbeing.
Support for emerging researchers taking the first step.
Funding: Up to $5,000 per project
Open to: Early Career Researchers and PhD students
Duration: 12 months
The Seeding Grant provides catalyst funding for early-stage or pilot research. In this round, two grants will be awarded. It’s the ideal platform to gather preliminary data, build research confidence, and prepare for future, larger-scale projects.
Focus areas:
• Contemporary osteopathic practice;
• Clinical safety and treatment effectiveness;
• Measurable outcomes in health and wellbeing;
• Osteopathy’s role in the Australian healthcare system;
• Consumer use and access to osteopathic care.
“The
Osteopathy Australia grants program has been instrumental in fostering high-quality research. It allowed me to build research skills, engage with collaborators, and generate findings that have direct relevance to clinical practice.”
Dr Nicholas Tripodi, PhD
These grants provide funding opportunities for researchers and practitioners to initiate innovative projects that can evolve into larger-scale, externally funded studies with the potential to deliver meaningful societal impact.
They offer a unique opportunity to:
• Advance osteopathic research and practice
• Build your research profile and capacity
• Generate pilot data for future competitive funding (e.g. NHMRC, ARC)
• Contribute to the evidence base and impact of osteopathy in Australia
Applications close 16 January 2026
For more information, contact our Research and Grant Officer at research@osteopathy.org.au.
Applications open: 27 October 2025
Applications close: 16 January 2026
Applications review: February – March 2026
Notification of outcomes: April 2026

Reviewers appreciate proposals that are clear, focused, and thoughtfully designed. Show that your research question is important, your approach is rigorous, and your outcomes will make a genuine contribution to osteopathic practice. Strong, collaborative teams that balance experience with fresh perspectives stand out. Above all, make sure the significance and potential impact of your work are clear and compelling.
Kathryn Refshauge Co-Director Brain and Mind Centre Professor Emeritus Faculty of Medicine and Health, The University
of Sydney
Australians spend nearly 2,000 hours a year at work.
It’s no surprise, then, that workplace health and rehabilitation are becoming increasingly important in helping people recover from injury and stay safe at work.
While it’s a multifaceted sector, osteopaths who work in occupational health may work across the private sector, as well as in the Workers’ Compensation and Rehabilitation schemes. Osteopaths can work across all state and territory workers compensation schemes. From Osteopathy Australia’s advocacy work, osteopaths are now recognised to work in Victoria, New South Wales, Queensland, Tasmania and nationally through Comcare, as occupational rehabilitation consultants. Osteopathy Australia continues to advocate for osteopaths increasingly working in this sector, and they are now formally recognised as part of this picture – a milestone for the profession and a sign of just how far osteopathy has come in broadening its scope.
Our Advanced Practice Occupational Health osteopaths demonstrate the value of this pathway, showing how osteopathy can play a leading role in creating healthier, safer workplaces.
“Occupational health has opened many doors throughout my career, and I see it as a great way for showcasing the diverse skills we bring as osteopaths. It’s great to see Osteopathy Australia supporting opportunities beyond private practice, and exciting to witness more osteopaths making the transition into the occupational health field.”
– Shaun Coghlan
“There are so many opportunities for osteopaths outside of private practice. Recognition as an Advanced Practitioner has added credibility to our services and helped shine a light on how osteopaths can contribute to safer, healthier workplaces.”
– Heath Williams
Occupational health work takes osteopathy beyond the clinic walls. Instead of treating patients in the traditional sense, practitioners step into workplaces, boardrooms and rehabilitation settings to:
• Identify barriers that might slow recovery;
• Assess work capacity and design meaningful duties plans;
• Conduct ergonomic and job assessments;
• Build and monitor return-to-work programs;
• Advise employers on modifications that reduce risk and improve wellbeing.
It’s about applying osteopathic principles to the bigger picture – the worker, the workplace and the systems that shape recovery.
The Occupational Health Advanced and Extended Practice Recognition Program formalises this scope of practice. Practitioners can demonstrate their advanced scope either through tertiary qualifications in occupational health, ergonomics, or work health and safety, or through a vocational pathway built on extensive experience and case-based assessment.
For those still developing in the field, the Extended Practice pathway offers recognition through professional development or supervised practice. Both levels of recognition last three years and require re-credentialling, ensuring practitioners remain current and accountable in a rapidly evolving sector.
Heath has been at the forefront of occupational health osteopathy for almost two decades. He graduated from Victoria University with a Bachelor of Clinical Science and Master’s in Health Science (Osteopathy). Since then, he has had a varied work career in the health sector, including teaching postgraduate training to health professionals in office and vehicle ergonomics, manual handling training, and strength and conditioning. Heath has worked extensively in the occupational health and safety industry, firstly with Health
Shaun’s journey into occupational health integrates clinical leadership, education, and consultancy. Practising at both The Osteopaths of Blackburn and Principle Four Osteopathy in Melbourne, he balances private practice with academic and corporate work. His diverse professional portfolio reflects a commitment to advancing health and wellbeing in both clinical and workplace settings.

Recognition is more than a title. It brings professional credibility, stronger referral networks and career opportunities across occupational health, rehabilitation, education and consultancy. Most importantly, it reassures employers and workers alike that osteopaths in this field meet rigorous, nationally recognised standards.
Recognition in occupational health is more than professional development; it’s about positioning osteopathy where it can have the greatest impact. By working alongside employers, insurers and allied health teams, Advanced Occupational Health osteopaths help reduce injury risk, shorten recovery
Advanced Practice Recognition can be gained in the following areas:
• Paediatrics
• Sports Management
• Exercise-based Rehabilitation
• Occupational Health
• Pain Management
In 2020, Shaun completed a Diploma in Work Health and Safety, strengthening his expertise in risk management and workplace wellness. He currently lectures at Victoria University, helping to shape the next generation of osteopaths, and consults for Corporate Work Health Australia, where he delivers ergonomics training and conducts risk assessments for organisations across Melbourne.
Shaun’s unique combination of clinical knowledge and occupational health expertise demonstrates the valuable role osteopaths can play in addressing the evolving demands of modern workplaces.

times, and improve both physical and mental health outcomes for workers. For the profession, this recognition cements osteopathy’s place in occupational health and opens up meaningful career pathways that extend far beyond the clinic.
If you’re an osteopath with an interest in ergonomics, workplace rehabilitation or injury prevention, the recognition program provides a structured way to expand your scope and gain credibility in the sector. Whether through tertiary study, vocational experience, or extended practice routes, the program ensures osteopaths are well equipped to meet the demands of occupational health today and into the future.
Learn more about the Occupational Health Advanced and Extended Practice Recognition Program at: https://osteopathy.org.au/Web/Web/careers/ advanced-practice/advanced-practice. aspx?hkey=eb44395b-20d5-4fea-b2b104099c8d2cbd

Where did you study and when did you graduate? I graduated from RMIT University in December 2021.
Where did you land your first job after university? Where are you now (if not still at your first job)? While in university, I decided moving away from Melbourne would give me the best opportunity to focus on building my skills. After graduating, and with the end of lockdown, I moved to the Surf Coast and worked in Barwon Heads and Ocean Grove. I worked on the coast for roughly one year, then moved back to Melbourne. Now, I work four days in Seddon, and one day a week in St Albans. These clinics have mainly been employee-based jobs, except that I now have an employee/subcontractor split.
What’s something you learned in university you still remember and/or use now? Since I wasn’t able to learn many extra hands-on techniques during my last two years of clinic due to COVID, we became experts in taking case histories. So, all the extra helpful questions and prompts we learned in university, I still use today.
What’s something you learned/developed since being in private practice? I’ve learned so much since being in private practice. One of these lessons is true active listening. Listening to patients’ stories, goals, expectations and what this all means to them. Reading between the lines and looking beyond their injury or complaint. A true whole-body approach enables me to build rapport with patients and achieve better patient outcomes. Another skill I’ve developed is my hands-on assessment. My assessment now looks quite different from when I graduated from university. I’m so much more holistic, and I listen to my hands more, all thanks to weekly mentoring and support.

What’s your favourite part of the job? Definitely listening to people’s stories, being part of their journey to feeling and moving better, and helping them problem-solve. I love hearing about people’s lives, their families, what they like to cook and what they do for work, among other things. I love being a small part of their health journey and using my hands to assess and validate what that person has been experiencing. I enjoy problem-solving and doing what osteopaths do best – treating the whole person and looking outside the box. I also love working with the team at my workplace. I’ve learned so much from them, and we have the opportunity to bounce ideas off each other, and create a great environment for everyone to be in.
What’s something you’d change about working in private practice? There are a few aspects of private practice that I would want to change. Private practice can sometimes feel corporate, when it comes to patient numbers, visit averages and cancellation rates, etc. Sometimes it’s easy to let these statistics define you. So having a well-balanced view on practitioner statistics as well as nurturing what else they bring to the table I think is really important.
I also wish that more patients could access great quality of care in private practice. Having worked in a suburb with low socio-economic status, I’ve witnessed people miss out on continuity of care due to financial reasons, lack of communication, or mismatched expectations. I firmly believe that practitioners need to be paid appropriately for their time and expertise; however, I wish that osteopathy could be more accessible for people of all demographics.
The final change to private practice I’d make is the focus that we put on building great team culture. Having worked in a few clinics now, there can be real variation in what the ‘vibes’ are in your workplace. From clinics that you struggle to flourish in, to clinics where you have limited support, it can feel like a lottery win to find a place that you actually fit into.
What’s something you’d tell current osteopathy students and/or new graduates? I would tell new career osteopaths and students to gather as much work and life experience as possible. Work experience includes meeting and networking with senior osteopaths, observing osteopaths in clinics, working as a receptionist and working as a trainer in a sports club. Immerse yourself in the industry and build connections with other allied health practitioners around you. Take any opportunity to do something related to your future career. By life experience, I mean taking a break, travelling, trying something new, meeting new people, volunteering and learning a skill. When you work as an osteopath, you meet new people every day, so it’s imperative to build your social skills and learn how to get out of your comfort zone. I really believe this will help you connect with people. I thought that when I reached my fifth year out as an osteopath, I’d know all the answers, but really, you are a blank canvas. So broaden your experience as much as you can, because as an osteopath, the learning never stops.
What’s something you’ve found helpful from your Osteopathy Australia membership? To be honest, I love scrolling through the Facebook Member’s Forum and reading posts and comments about what fellow osteopaths are up to. From a practical perspective, I really enjoy the webinars that are offered – from pelvic health to headache management, to AI, there’s a wealth of information available which is what I find helpful from my membership.

If you’re finishing your osteopathy studies between June and December , you can access a special membership offer exclusive to Osteopathy Australia final-year Student Members.
Your active 2025 Student Membership (valid until 31 December 2025) gives you VIP access to upgrade to Early Career Member, for just $250 — a huge saving as you begin your professional journey! Offer ends 31 December 2025.
1. Log in at www.osteopathy.org.au
2. Go to Membership > Early Career osteopaths to upgrade and claim your offer.
Once your payment has been processed, you’ll unlock:
• Discounted Guild professional indemnity insurance – call 1800 810 213 and mention the Early Career Member, Year 1 rate.
• Important: your free student liability insurance doesn’t cover osteopathic practice. Contact Guild to arrange professional cover before you start treating patients.
• Savings for years to come – enjoy reduced membership fees for your first five years in practice.
• Free Osteopath Career Guide and access to member-only resources, tools and advice.
Dr Paul Orrock has recently retired from his academic position at Southern Cross University after a long career, having lectured in osteopathy at the Royal Melbourne Institute of Technology University, Victoria University and most recently Southern Cross University, where he founded the programme. Many Australian osteopaths have been taught and mentored by Paul across the 32 years of academic life, and at one stage Paul estimates he had taught over half the registered osteopaths in Australia. “The time was right for me to step back, as the programme and team at SCU are well-established, although I miss the students and being involved in their discovery of the noble profession of osteopathy,” Paul said recently. He is now an Adjunct Associate Professor at SCU and is continuing his engagement and contributing to the profession as a practitioner in Byron Bay and by serving as the current Chair of the Osteopathy Board of
Australia. “I love the dynamic and challenge of continual learning, both at the Board and private practice – which constantly keeps you in your problem-solving mode.”
Paul would also like to let the profession know more about his current research project: A History of Osteopathy in Australia, which aims to establish an online archive to be hosted on the Osteopathy Australia website. The first stage in 2025 involves interviewing 12 elders and leaders of the profession who can cover the history and evolution of the practice, education, regulation and administration of the profession. Paul is the Principal Investigator, and the project received funding from Osteopathy Australia for an experienced Oral Historian, Dr Jo Kijas, to assist with methodology and the interviews. More interviews will be completed in 2026, and a callout for documentation and archival material will be made, all to be digitised and organised on the website for public access in perpetuity. Paul wishes to state that, “there are many more people that we plan to interview beyond the initial twelve interviewees, so if you haven’t heard from me yet – stay tuned!”

In late October, Osteopathy Australia launched the new website and member portal, giving you a cleaner, more intuitive way to manage your professional development and member profile.
Access to Continuing Professional Development (CPD) has always been at your fingertips, but the new portal makes the experience smoother and more efficient:
• Search by category – quickly find courses and webinars relevant to your needs;
• Automatic CPD logging – when you complete a webinar, your record updates instantly;
• Streamlined functionality – less clutter, clearer design, faster navigation.
These changes are the result of listening to your feedback , and we hope the improvements make it easier to focus on learning while the portal takes care of the admin.
• Go to osteopathy.org.au/Web/Web/Sign-in.aspx
• Use the Forgot password? link to set a new password. (Your password must be at least 12 characters long and include at least one letter, one number and one special character; accounts are locked after five invalid login attempts).
• Enter the email address linked to your membership.
If you are having trouble logging in, please call us during business hours (9AM – 5PM) on 1800 467 836 or email info@osteopathy.org.au; we’re happy to help.
Your profile powers our communication including Find an Osteo tool and ensures you receive important updates and opportunities. Yet 30 per cent of members still have out-of-date details – meaning missed chances to now receive emails directly from patients via your Find an Osteo profile, promote your practice, connect with peers and stay informed.
If you haven’t already, please log in and confirm that your:
• Clinic address is correct;
• Mobile number, email and home address are current. It takes just a few minutes and ensures you get the full benefit of your membership.


BY CONOR MCLAREN, JUSTPROTECT
The Privacy Act 1988 is a critical piece of Australian legislation designed to promote and protect the privacy of individuals and regulate how certain Australian organisations (such as health service providers) handle personal information.
The Act was recently amended via The Privacy and Other Legislation Amendment Bill 2024, which ultimately endeavoured to further strengthen these privacy protections by implementing a first tranche of recommendations from the Privacy Act Review. However, these changes also have numerous potential implications for osteopaths.
This article therefore follows on from the recent webinar that JustProtect presented with Osteopathy Australia and focuses on the key changes to the Privacy Act paired with some of the core operational and cybersecurity measures that can be adopted to take deliberate steps towards compliance.

• Clarifying the reasonable steps organisations must take to secure personal information, including both technical cybersecurity measures and organisational measures such as processes and procedures.
• The establishment of a statutory tort for serious invasions of privacy, providing individuals with a legal avenue to seek redress for privacy violations.
• The enhancement of the Office of the Australian Information Commissioner’s (OAIC) enforcement and investigation capabilities, including new levels of civil penalties and the authority to issue infringement notices.
• A directive for the OAIC to create a Children’s Online Privacy Code, applicable not only to social media platforms but also to any online services likely to be accessed by children.
• The introduction of a system to designate a list of countries and binding schemes with adequate privacy protections to facilitate cross-border data transfers.
• A requirement for privacy policies to include information about substantially automated decisions that significantly impact individuals’ rights or interests, detailing the types of decisions and the personal information used.
One of the more material impacts stemming from these changes is the fact that the OAIC will gain a wider array of enforcement options along with new functions and capabilities. Among these are two new provisions that allow civil penalties to be adjusted according to the severity of the privacy breach.
According to the Bill’s explanatory memorandum, the Bill’s new civil penalty provisions for breaches of certain privacy obligations of the APPs (e.g. incorrect Privacy Policy) and non-compliant eligible data breach statements would be subject to infringement notices. The memorandum explains that the maximum associated penalty for bodies corporate equates to approximately $330,000, which is a significant sum of money for small-medium businesses.
As evident from the above, these amendments increase the scope of the OAIC’s investigative and enforcement powers and broaden the applicability of various lower levels of penalties. This ultimately places an increased emphasis on the need for health service providers such as osteopaths to take more deliberate steps towards compliance.
Now is the time to take action to embed privacy and cybersecurity into your daily operations. However, doing so requires a deliberate set of actions as outlined below:
1. Understanding your obligations
Understanding your compliance obligations is the first step. While reading legislation might not be everyone’s idea of fun, the OAIC offers a wealth of guides and information on their website to help health service providers understand their specific obligations. Health service providers must take the time to fully understand what exactly these obligations entail and put a plan together to put these into practice.
2) Creating and updating a privacy policy
Create a privacy policy that clearly outlines how your organisation handles personal information. It’s not enough to set and forget; consistently update the policy to ensure it reflects current practices and legislative requirements.
3) Developing an organisational privacy management plan
Next, develop a privacy management plan. This plan should outline specific, measurable goals and targets to implement your requirements under the Privacy Act and embed privacy into your operations. This plan is ultimately your road map towards protecting your patient’s data and privacy.
4) Establishing accountability and communication
Clear and documented lines of accountability and communication are essential. Define who is responsible for privacy within your organisation and who can be contacted regarding privacy questions or concerns. In smaller organisations, this may be a single person wearing multiple hats. However, in larger organisations this might involve multiple different individuals and departments
5) Conducting a data inventory and analysis
Once the abovementioned key foundations for your privacy program are established, conduct an inventory and analysis
of how your organisation handles personal information. As part of this, it is important to identify the types of data stored, accessed, and transmitted as part of your operations.
6) Developing a data breach response plan
All health service providers should develop a data breach response plan. This plan, which you hope never to use, is critical in the event of a data breach. It should set out key actions, procedures, and lines of authority in the unfortunate event of a data breach.
7) Privacy and cybersecurity training
In addition to these steps, it’s vital to provide ongoing privacy and cybersecurity training for your staff. Regular training sessions can help employees understand the importance of privacy and cybersecurity, recognise potential threats, and know how to respond appropriately.
8) Implementing key technical cybersecurity controls
Further to the above organisational steps, it is critically important to implement a multi-layered set of cybersecurity controls including but not limited to encryption, anti-virus software, strong passwords, multi-factor authentication, regularly updates and backups, email security and user account management.
9) If in doubt, seek legal advice
Please note that this blog post does not constitute legal advice. The information provided is for general informational purposes only and should not be relied upon as legal advice. Always consult with a qualified legal professional for specific legal guidance.
JustProtect is a multi-disciplinary team of experts dedicated to enhancing cybersecurity and privacy for healthcare organisations across Australia. If you have any further questions related to this article, please do not hesitate to get in touch for a no-obligation chat.
We are giving away a free Privacy Management Plan template to all readers. Simply scan the QR code below and you will be prompted to download your own customisable copy!


BY NICHOLAS LUCAS
Transcranial direct current stimulation (tDCS) represents a significant advancement in non-invasive brain stimulation technology. In June 2025, the Australian Therapeutic Goods Administration (TGA) approved medical-grade tDCS devices for clinical use, marking a pivotal moment for healthcare practitioners seeking evidence-based neuromodulation therapies.1
tDCS may offer a fundamentally different approach to managing complex neurological conditions by modulating neural activity to restore or modulate effective brain function rather than focus on symptom suppression. For osteopaths, this represents an opportunity to integrate cutting-edge neuroscience with the profession’s core philosophy of supporting the body’s inherent capacity for self-regulation and healing. However, the clinical applications of tDCS may extend beyond its regulatory approval; with the technology’s ability to influence the brain’s complex networks in ways that align with osteopathy’s whole-person approach.
Fibromyalgia provides an exemplary case for understanding how tDCS can be integrated into osteopathic practice. This chronic pain condition affects approximately 3-5 per cent of the Australian population, with significantly higher prevalence in women.2 Many cases remain undiagnosed or misdiagnosed due to the complexity of symptoms and lack of definitive biomarkers and the condition imposes a substantial
economic burden on both individuals and the healthcare system.3 Daily life for those living with fibromyalgia is characterised by widespread musculoskeletal pain, profound fatigue, sleep disturbances, and cognitive dysfunction. Simple activities that healthy individuals take for granted, such as grocery shopping, household chores, or social activities, become significant challenges. Many patients are unable to participate fully in work, family life, or recreational activities, with unpredictability of symptoms and concurrent feelings of isolation and depression adding further challenges.
For osteopathic practitioners, fibromyalgia represents both a challenge and an opportunity. Traditional osteopathic approaches are valuable for addressing musculoskeletal dysfunction, and now tDCS offers a unique advantage, providing a means to directly address the neurological dysfunction underlying the condition, while complementing osteopathic interventions.
The view that tDCS merely increases and decreases neuronal excitability is oversimplified; the true mechanism of action involves far more sophisticated neurobiological processes. The contemporary understanding of tDCS mechanism relies on several key principles. First, neural degeneracy, referring to the ability of multiple neural pathways to produce similar functional outcomes , is fundamental to understanding why tDCS can be effective across diverse patient populations despite individual variations in brain structure and function.4
Second, the brain operates as a polycomputing system, where multiple computational processes occur simultaneously across different neural networks;5 tDCS doesn’t simply turn brain regions “on” or “off” but rather modulates the complex interactions between these parallel processing systems. This framework helps explain why tDCS effects often extend beyond the primary stimulation site to influence distributed neural networks. Third, predictive processing; the brain continuously generates predictions about sensory input and updates these predictions based on prediction errors.6 tDCS appears to influence this predictive processing by modulating the precision of neural signals, thereby affecting how the brain processes and responds to both internal and external stimuli. Neuroplasticity mechanisms underlie the lasting effects of tDCS. Stimulation promotes long-term potentiation (LTP) and long-term depression (LTD) at synaptic connections, leading to structural and functional changes that persist beyond the stimulation period.7,8 These neuroplastic changes are activitydependent, meaning that the brain’s state during stimulation significantly influences the therapeutic outcome.
tDCS should be understood as a complex neuromodulation technique that simultaneously engages multiple levels of brain organisation. This sophisticated mechanism of action aligns well with osteopathic principles of addressing root causes.
The integration of tDCS into osteopathic practice presents a fundamental shift in the patho-anatomical approach to clinical reasoning. We are not “treating fibromyalgia”, instead, we are stimulating the brain to activate the body’s own self-regulatory systems to restore normal function to pain and emotional processing networks. This approach aligns perfectly with osteopathic philosophy, the principle being that the body possesses inherent mechanisms for maintaining health and recovering from dysfunction. In fibromyalgia, these self-regulatory systems have become dysregulated, leading to central sensitisation, altered pain processing and disrupted emotional regulation. In simplistic terms, tDCS provides a means of “resetting” these systems by modulating the neural networks responsible for pain perception, emotional processing and cognitive function.
The osteopathic clinical reasoning process for tDCS begins with a comprehensive assessment of the patient’s neurological presentation. This involves evaluating not just pain symptoms but also neurologic and cognitive function, emotional regulation, sleep patterns and autonomic nervous system activity. The goal is to identify which neural networks are dysregulated and how tDCS might be used to restore normal function. For example, a patient presenting with widespread pain, fatigue and cognitive dysfunction might show evidence of dysregulation in the default mode network, central executive network and pain processing pathways. An osteopathic approach would consider how these networks interact and how tDCS stimulation might be tailored to address the specific pattern of dysfunction present in that individual. This reasoning framework emphasises the importance of individualised treatment protocols, which should be adapted based on the individual’s specific neurological findings and clinical presentation. The integration of manual therapy with tDCS further exemplifies the osteopathic approach; the combination addresses both peripheral and central components of the pain experience, providing a more comprehensive therapeutic intervention than either modality alone.
“tDCS may offer a fundamentally different approach to managing complex neurological conditions by modulating neural activity to restore or modulate effective brain function rather than focus on symptom suppression.”

“The safety profile of tDCS has been consistently excellent across all meta-analyses.”
The evidence base for tDCS in fibromyalgia has grown substantially over the past decade, with several high-quality meta-analyses providing insights into its therapeutic potential.
Winterholler et al. (2025) conducted a systematic review and meta-analysis evaluating the clinical, neurophysiological and neurochemical effects of tDCS in fibromyalgia, synthesising data from studies published between 2013 and 2023.9 Their findings revealed that anodal tDCS applied over the primary motor cortex (M1) and dorsolateral prefrontal cortex (DLPFC) produced short- to mid-term reductions in pain and mood disturbances.
Yang et al. (2024) conducted a systematic review and meta-analysis, examining 20 studies with 851 participants.10 Their analysis revealed a significant moderate effect size for pain reduction. Importantly, the authors assessed whether these effects reached the minimal clinically important difference, finding that only stimulation of the primary motor cortex (M1) and dorsolateral prefrontal cortex (DLPFC) achieved clinically meaningful pain reduction.
A meta-analysis by Moshfeghinia et al. (2023) focused on 20 studies with 664 patients and found an even larger effect size for pain reduction.11 This analysis confirmed the dose-response relationship, with protocols lasting four weeks or longer showing superior outcomes compared to shorter treatment courses.
The analgesic mechanisms of tDCS have been further elucidated by Teixeira et al. (2023), who conducted a metaregression analysis examining potential influencers of clinical effect.12 Their analysis of 16 randomised controlled trials revealed that treatment duration was the strongest predictor of therapeutic response, with longer protocols producing more substantial and sustained pain relief.
The safety profile of tDCS has been consistently excellent across all meta-analyses. Yang et al. reported only mild and transient adverse effects, including headache, neck pain and tingling sensations, with no significant difference in withdrawal rates between active and sham groups.10 This safety profile is particularly important given the limited tolerability of many pharmacological treatments for fibromyalgia.
Home-based tDCS has emerged as a particularly promising approach. Antonioni et al. (2024) analysed 12 studies with 446 participants receiving supervised home-based treatment and found large effect sizes for pain reduction with excellent safety and adherence rates.13 The convenience and accessibility of home-based treatment may enhance longterm compliance and therapeutic outcomes.
However, these meta-analyses also reveal important limitations in the current evidence base. Study durations have generally been short, with most trials lasting 2–4 weeks. Long-term follow-up data are limited, making it difficult to assess the durability of treatment effects. Additionally, there has been limited investigation of optimal stimulation parameters, with most studies using standard protocols rather
than individualised approaches. The heterogeneity observed across studies suggests that treatment response may depend on factors not adequately captured in current research. Patient characteristics, stimulation parameters, concurrent treatments, and individual differences in brain structure and function all likely influence outcomes. This variability points to the need for more personalised approaches to tDCS treatment.
The real impact of tDCS becomes apparent when examining the clinical outcomes reported in randomised controlled trials. The landmark study by Fregni et al. (2006) provided the first randomised controlled evidence for tDCS in fibromyalgia.14 In this proof-of-principle study, patients receiving anodal tDCS over the primary motor cortex showed significantly greater pain improvement compared to both sham stimulation and stimulation of the dorsolateral prefrontal cortex. The effects were sustained for three weeks after treatment completion, suggesting lasting neuroplastic changes rather than temporary symptom relief. More recent studies have demonstrated the potential for functional recovery alongside pain reduction. Patients in tDCS trials have reported improvements in sleep quality, cognitive function, and overall quality of life that persisted beyond the treatment period. The combination of tDCS with other interventions appears particularly promising. Several studies, including a recent study by Caumo et al (2025), have shown enhanced effects when tDCS is combined with exercise, cognitive behavioral therapy and pain education.15 This finding aligns with osteopathic principles of multimodal treatment and suggests that tDCS may be most effective when integrated into comprehensive care plans rather than used as a standalone intervention. However, not all patients respond equally well to tDCS. Clinical trials consistently show variability in treatment response, with some participants experiencing substantial improvements while others show minimal change despite receiving identical treatment protocols. This variability underscores the importance of patient selection and individualised treatment approaches, and highlights the need for better predictors of treatment response to guide clinical decision-making. The sustained nature of improvements observed in many studies is particularly encouraging. Unlike pharmacological treatments that require ongoing administration, tDCS appears to produce lasting changes in brain function that can persist for weeks to months after treatment completion. This suggests that tDCS works by facilitating neuroplastic changes that restore normal pain processing rather than simply masking symptoms.
While the evidence for tDCS in fibromyalgia is encouraging, it is necessary to acknowledge significant limitations in the current research base. These limitations have important implications for clinical practice and highlight areas where further research is needed. The most significant limitation is the short duration of most studies. The majority of randomised controlled trials have followed patients for only 2–4 weeks, with few extending beyond three months. This is problematic because fibromyalgia is a chronic condition requiring long-term management. We simply don’t know whether the benefits of tDCS are sustained over months or years, or whether maintenance treatments are necessary to preserve therapeutic gains.
Study sample sizes have generally been small, with most trials including fewer than 50 participants. Small sample sizes limit statistical power and make it difficult to detect important subgroup differences or rare adverse effects. They also reduce the generalisability of findings to the broader fibromyalgia population.
The heterogeneity of treatment protocols across studies presents another challenge. Studies have used different electrode placements, current intensities, session durations, and treatment schedules. This variability makes it difficult to determine optimal treatment parameters and contributes to the heterogeneity observed in meta-analyses.
Patient selection criteria have varied considerably between studies. This variability affects the interpretation of results and makes it difficult to determine which patients are most likely to benefit from tDCS.
The lack of active control conditions in many studies is also problematic. While sham-controlled trials are important for establishing efficacy, they don’t provide information about how tDCS compares to other active treatments. Few studies have directly compared tDCS to established fibromyalgia treatments such as pregabalin, duloxetine or cognitive behavioral therapy.
Outcome measures have focused primarily on pain intensity, with less attention to other important domains such as function, quality of life and patient-reported improvement.This narrow focus may underestimate the full therapeutic potential of tDCS and doesn’t capture outcomes that matter most to patients.
For these reasons, the current evidence base, while promising, should be interpreted with appropriate caution. The moderate effect sizes observed in meta-analyses represent average treatment effects across heterogeneous populations and protocols. Individual patient responses may vary considerably from these averages. Anecdotally, what we have seen in practice mirrors what the evidence suggests, with some patients reporting significant improvements and others being non-responders.
The limitations of standardised tDCS protocols become particularly apparent when considered in light of recent advances in human connectome research revealing that individual differences in brain structure and function are far more extensive and unique than previously recognised.16,17,18 This individual variability has profound implications for brain stimulation approaches. The assumption underlying most tDCS research has been that standardised electrode placements will produce similar effects across different individuals, however each person’s unique pattern of white matter tracts and functional networks means that identical stimulation protocols may engage different neural circuits and produce different therapeutic effects. For example, the primary motor cortex (M1), the most common target for tDCS in fibromyalgia studies, is located in a similar anatomical position across individuals, however, the specific neural circuits connected to this region vary considerably between people; identical stimulation protocols applied to these different individuals would be expected to produce different therapeutic effects. The concept of neural degeneracy adds another layer of complexity. Multiple neural pathways can produce similar functional outcomes, meaning that different individuals may achieve pain relief through different mechanisms. This degeneracy suggests that effective tDCS protocols should be tailored to each person’s unique
functional neural performance and neural architecture rather than applying standardised approaches.
Despite these individual differences, standardised tDCS protocols have still produced moderate to large effect sizes in fibromyalgia research. This apparent paradox can be understood in several ways. First, fibromyalgia may involve dysfunction in neural networks that are relatively consistent across individuals, such as the default mode network or pain processing pathways. Second, tDCS may work through multiple mechanisms simultaneously, increasing the likelihood that at least some therapeutic pathways will be engaged in each individual. The robustness of tDCS effects despite individual variability actually supports its therapeutic potential. If standardised protocols can produce meaningful benefits across diverse populations, individualised approaches based on each person’s unique connectome might achieve even greater therapeutic effects.
The integration of individualised tDCS protocols into osteopathic practice requires a systematic approach to neurological assessment and treatment planning. This process begins with a comprehensive evaluation that goes beyond traditional pain assessment to examine the full spectrum of neural function. The neurological examination for tDCS planning should include assessment of the following domains to provide information about the functional status of different neural networks and can guide electrode placement and stimulation parameters.
1. Cognitive assessment might include evaluation of attention, working memory, executive function, and processing speed. Deficits in these areas suggest dysfunction in the central executive network or default mode network, which could be targeted with dorsolateral prefrontal cortex stimulation. The Montreal Cognitive Assessment (MoCA) may provide a standardised tool for this evaluation.
2. Emotional regulation assessment should examine mood symptoms, anxiety levels, and emotional reactivity. The presence of significant depression or anxiety suggests involvement of limbic networks that might benefit from targeted stimulation. The Beck Depression Inventory and Generalised Anxiety Disorder-7 scale provide standardised measures for this assessment.
3. Sensory processing evaluation should go beyond simple pain assessment to examine tactile sensitivity, temperature perception and proprioception. Abnormalities in these areas may indicate dysfunction in somatosensory networks that could influence electrode placement. Simple bedside tests such as two-point discrimination, vibration threshold and joint position sense can provide valuable information.
“The robustness of tDCS effects despite individual variability actually supports its therapeutic potential.”
“The integration of tDCS with other osteopathic interventions provides additional opportunities for individualisation.”
4. Motor control assessment should include evaluation of strength, coordination, balance, and movement quality. While fibromyalgia is not primarily a motor disorder, many patients experience motor symptoms that may reflect dysfunction in motor networks. Simple tests such as finger-to-nose coordination, heel-to-shin testing, and single-leg stance can reveal subtle motor abnormalities.
5. Autonomic nervous system assessment might include evaluation of heart rate variability, blood pressure responses to position changes, and pupillary responses. Autonomic dysfunction is common in fibromyalgia and may influence treatment response. While detailed autonomic testing requires specialised equipment, simple bedside assessments can provide useful clinical information. Based on this comprehensive assessment, individualised tDCS protocols can be developed. For example, a patient with prominent cognitive symptoms and executive dysfunction might benefit from anodal stimulation of the dorsolateral prefrontal cortex. A patient with significant emotional dysregulation might benefit from stimulation targeting limbic networks. A patient with predominant sensory symptoms might benefit from somatosensory cortex stimulation.
The individualised electrode placement requires knowledge of functional neuroanatomy and an understanding of how different electrode placements influence neural activity.
Dr Nicholas Lucas qualified as an osteopath in 1999 from Victoria University. He was a lecturer in neuromusculoskeletal assessment and diagnosis at Western Sydney University from 2000 to 2009. He was a founding executive editor of the International Journal of Osteopathic Medicine serving in that role for 15 years. He has degrees in both Pain Medicine and Clinical Epidemiology and a PhD (Medicine) from the University of Sydney. Most recently, he has been involved in clinical research and education in non-invasive neuromodulation for people with chronic pain, post-stroke rehabilitation, depression and related neurological conditions.
High-definition tDCS systems, which use multiple electrodes, may allow for more precise targeting of specific brain regions. Stimulation parameters should also be individualised based on patient characteristics and treatment goals. Current intensity, session duration, and treatment frequency may all need to be adjusted based on individual response and tolerance. Some patients may require higher intensities to achieve therapeutic effects, while others may be more sensitive to stimulation.
The integration of tDCS with other osteopathic interventions provides additional opportunities for individualisation. Manual therapy techniques can be selected based on the patient’s specific somatic dysfunction patterns and can be timed to complement tDCS effects. Exercise prescriptions can be tailored to address specific motor or cognitive deficits identified during assessment. This individualised approach represents a significant departure from the standardised protocols used in most research studies. However, it aligns with both osteopathic principles and emerging understanding of brain network individuality. While more research is needed to validate individualised approaches, the theoretical foundation is strong and the potential for improved outcomes is substantial. By targeting the specific neural networks that are most dysfunctional in each patient, treatment can be more precisely directed toward the underlying pathophysiology. This precision medicine approach to tDCS represents the future of neuromodulation therapy and positions osteopathic practitioners at the forefront of this emerging field.
The recent TGA approval of medical-grade tDCS specifically for chronic pain represents a significant opportunity for the osteopathic profession. For the first time, we have access to a neuromodulation technology that genuinely aligns with osteopathic principles. In principle, tDCS works through sophisticated neurobiological mechanisms that restore or enhance brain function, rather than mask dysfunction. The evidence is compelling, with numerous meta-analyses reporting consistent moderate to large effect sizes for pain reduction in fibromyalgia. Importantly, the safety profile is favourable, with no serious adverse events across 33,000 treatment sessions. This is particularly relevant for patients who have often exhausted conventional treatments or experienced intolerable side effects from medications However, the real opportunity lies in individualisation; Human Connectome research showing the uniqueness of neural networks suggests potential for personalised approaches. The challenge, of course, is developing the clinical expertise to implement this effectively, with sophisticated clinical reasoning being required to integrate neurological assessment with treatment planning. By thoughtfully integrating evidencebased technologies like tDCS with traditional osteopathic approaches, we can position ourselves at the forefront of precision medicine while remaining true to foundational principles. For these reasons, tDCS deserves serious consideration by any osteopath treating patients with complex pain conditions.
To find the full list of references for this article, scan the QR code here.
Osteopaths invited to join national PACE-RURAL project

OBY ALISON SIM
steopaths across Victoria, New South Wales, Queensland and Western Australia are invited to participate in an exciting new research initiative aimed at improving musculoskeletal (MSK) care for people living in regional, rural and remote Australia.
The PACE-RURAL trial (PAthway of CarE for people with chronic musculoskeletal conditions living in RURAL, regional and remote Australia using allied telehealth) is a $2.5 million project funded by the Medical Research Future Fund led by Prof Trudy Rebbeck at University of Sydney. The project seeks to address the inequities in care faced by people living outside major cities who experience chronic pain from MSK conditions like back, neck, hip and knee pain.
These conditions are among the leading causes of disability in Australia, yet people living in regional, rural and remote areas regularly face significant barriers to accessing care that people in urban areas may take for granted. This includes longer wait times for GP appointments, limited availability of imaging and specialist services and the need to travel long distances to access appropriate care. These challenges can
“Osteopaths, along with physiotherapists, chiropractors and exercise physiologists are vital to the success of this project.”
delay early intervention and contribute to poorer outcomes for people with musculoskeletal conditions.
PACE-RURAL offers an innovative, structured model of care that begins with early risk screening. People identified as low risk are guided to co-designed self-management resources through mypainhub.com while those at higher risk are offered early telehealth consultations with specialist allied health practitioners. This model aims to provide timely, evidenceinformed care closer to home, reduce unnecessary escalation of healthcare and improve patient outcomes.
Osteopaths, along with physiotherapists, chiropractors and exercise physiologists are vital to the success of this project. The PACE-RURAL project is currently recruiting clinicians in NSW, VIC, QLD and WA to:
• Use a simple digital screening tool to identify and refer suitable patients;
• Collaborate with a network of allied health specialists delivering care via telehealth;
• Access training in pain science communication, digital health tools and risk-informed care planning.
Participating osteopaths will contribute to the implementation of a new care model that reflects core osteopathic principles – emphasising whole-person care, supporting self-management, and addressing biopsychosocial factors early to prevent chronicity.
This is a valuable opportunity to be involved in a collaborative research project that supports regional, rural and remote communities. It offers participating clinicians the chance to strengthen their digital health capabilities, access professional development (provided at no cost), and be part of a broader effort to improve access to timely, evidenceinformed musculoskeletal care.
If you are an osteopath working in a regional, rural or remote settings in QLD, NSW, VIC or WA and are interested in learning more or getting involved, please contact Dr Alison Sim at a.sim@latrobe.edu.au

BY PETER MCCANN, REBECCA PRENC, PETER MCGLYNN AND CARL THISTLETHWAYTE

Sarcopenia is a progressive skeletal muscle disorder characterised by a decline in muscle strength, mass and physical performance, formally recognised as a chronic disease with its own ICD-10 code in 2016 (M62.84).1 While traditionally viewed through a geriatric lens, sarcopenia has become increasingly relevant to the profession of osteopathy due to its strong association with musculoskeletal dysfunction, frailty, and chronic disease.1
This condition now demands attention as both a lifestyledriven and lifestyle-responsive disorder, positioning osteopaths at the forefront of its prevention and management. Sarcopenia’s systemic consequences extend beyond muscle loss; it reflects a multisystem syndrome of metabolic dysregulation, mitochondrial dysfunction, hormonal decline, inflammation, and physical inactivity.2 The following discussion will outline the latest understanding of sarcopenia’s pathophysiology, diagnostic advances and evidence-based interventions, framed within a lifestyle medicine approach to support interdisciplinary, proactive musculoskeletal care.
Skeletal muscle is not only essential for movement and function but also for systemic metabolic homeostasis. Muscle mass is the primary site of postprandial glucose disposal and a key regulator of lipid metabolism. Loss of muscle mass and function, as seen in sarcopenia, is therefore closely linked with metabolic syndrome, insulin resistance, type 2 diabetes and cardiovascular disease.3 Given the similar risk factors for sarcopenia and osteoporosis, this may increase the likelihood of these conditions co-existing and potentially contribute to a vicious cycle of physical decline and loss of independence.
Importantly, skeletal muscle acts as an endocrine organ through the release of myokines such as irisin and interleukin-6, which mediate anti-inflammatory and insulin-sensitising effects.4 Regular contraction-induced myokine secretion plays a crucial role in maintaining wholebody homeostasis. Conversely, sedentary behaviour and sarcopenia lead to myokine deficiency, chronic low-grade systemic inflammation and functional decline.
Given these complex bidirectional relationships, sarcopenia serves as both a consequence and amplifier of broader chronic disease processes, a concept especially relevant to osteopaths engaged in physical rehabilitation and chronic disease prevention.
Globally, sarcopenia affects 10–30 per cent of older adults, with higher rates in those who are hospitalised or institutionalised.5 Recent meta-analyses suggest the prevalence of severe sarcopenia in community-dwelling populations ranges from 2.2–10 per cent, depending on the criteria used.6 In Australia, the growing ageing population means sarcopenia is increasingly encountered in primary care and rehabilitation settings. Concerningly, it often goes under recognised due to poor screening uptake and a lack of standardised assessments in clinical practice.
Sarcopenia is independently associated with falls, fractures, functional dependency, cognitive decline and increased mortality risk.7 Its clinical trajectory also overlaps with common musculoskeletal complaints such as chronic back pain, joint arthritis and reduced mobility, complicating the diagnosis unless actively screened.
“This condition now demands attention as both a lifestyledriven and lifestyleresponsive disorder, positioning osteopaths at the forefront of its prevention and management.”
The strength, assistance with walking, rising from a chair, climbing stairs and falls (SARC-F) questionnaire is a validated, rapid self-reported tool that can be used as part of the clinical history to assist with sarcopenia screening in clinical settings.8
The European Working Group on Sarcopenia in Older People (EWGSOP2) updated their diagnostic framework in 2019, emphasising low muscle strength as the primary indicator of sarcopenia, confirmed by reduced muscle quantity or quality and categorised by impaired physical performance.1 This stepwise approach remains the gold standard internationally and is applicable in Australian allied healthcare settings. Key measures include:
• Grip strength: <27 kg (men) or <16 kg (women) indicates probable sarcopenia.1
• Chair stand test: >15 seconds for 5 rises is associated with low strength.9
• Gait speed: <0.8 m/s reflects poor functional performance and increased fall risk.10
• Muscle mass: ideally measured using Dual-energy X-ray Absorptiometry (DXA), though validated alternatives such as Bioelectrical Impedance Analysis (BIA) are accessible in clinical settings.
Recent research has added nuance to diagnosis, recommending inclusion of muscle-specific force (strength per unit mass) to identify functional sarcopenia that may be missed by mass- based assessments alone.11
The biological underpinnings of sarcopenia are complex and multifactorial. Key contributors include:
• Anabolic resistance: reduced muscle protein synthesis in response to dietary protein or exercise in older adults.12
• Mitochondrial dysfunction: impaired ATP production and increased oxidative stress compromise muscle energetics.2
• Endocrine dysregulation: decreased testosterone, oestrogen, growth hormone, and insulin-like growth factor-1 (IGF-1) contribute to catabolism.13
• Inflammaging: chronic low-grade systemic inflammation, marked by elevated TNF-α and IL-6, promotes muscle breakdown and insulin resistance.14
• Neuromuscular degeneration: denervation and motor unit loss further reduce muscle recruitment and function.15 Understanding these mechanisms provides a rationale for multidimensional interventions targeting strength, nutrition, inflammation and lifestyle behaviours.
LIFESTYLE MEDICINE AND MSK STRATEGIES FOR SARCOPENIA MANAGEMENT
“Osteopaths are encouraged to actively engage in interdisciplinary networks to address sarcopenia holistically.”
training.20 Whey protein isolate remains an effective adjunct due to its high leucine content and rapid digestibility.
Vitamin D repletion is important, as deficiency is common in older adults and is associated with muscle weakness and impaired balance.21 Simple screening tools such as a 3-day food diary, 24-hour dietary recall, and the Mini Nutritional Assessment (MNA) can help identify individuals at risk due to unmanaged caloric restriction or excess, which is known to increase the risk of sarcopenia.23 These tools can also guide appropriate referrals to dietitians.
Figure 1 Lifestyle factors that influence muscle protein synthesis
SARCOPENIA INTERVENTION
Progressive resistance training (PRT) is one of the most effective strategies to prevent and reverse sarcopenia.16 PRT has been consistently shown to positively impact strength, power, gait speed, functional capacity, balance and skeletal muscle index across diverse settings in older adults with sarcopenia.16,17 PRT has also been shown to significantly improve mobility and reduce falls in sarcopenic adults across diverse settings.17
Key principles include:
• Moderate-to-high intensity resistance (70–85% 1RM);
• Two to three sessions per week;
• Focus on large muscle groups (e.g. hips, thighs, trunk);
• Progressive overload.
Aerobic training may have a minimal direct effect on muscle mass or strength; however, it appears to have utility in preserving pre-existing muscle and improving mitochondrial function, and therefore should be considered in exercise prescription.16,18 Osteopaths, in conjunction with other musculoskeletal allied health practitioners, are well placed to prescribe and supervise such programs, tailoring them to individual capabilities and health goals.
AND NUTRITIONAL SUPPORT
Dietary protein is essential to support muscle protein synthesis. Older adults exhibit anabolic resistance, requiring higher protein intakes than younger individuals. Current consensus recommends 1.0–1.2 g/kg/day of protein, ideally distributed across meals to maximise muscle stimulation16,20. Specifically, leucine-enriched protein supplementation may enhance the anabolic response, particularly when combined with resistance
Emerging research is exploring the role of the gut-muscle axis, where microbiome composition and gut permeability influence systemic chronic inflammation and muscle mass regulation. Exercise and prebiotic/probiotic strategies may support muscle function indirectly through microbial modulation.22 Sleep quality is another overlooked but important factor. Short sleep duration and poor sleep efficiency are linked with sarcopenia, likely through hormonal and inflammatory immune pathways.24 Interventions targeting sleep hygiene, stress reduction, and circadian rhythm support can improve recovery and reduce the risk of sarcopenia.
Chronic musculoskeletal pain is often a barrier to active rehabilitation in older patients.25 While manual therapies may not play a direct role in the management of primary sarcopenia, osteopathic techniques may support sarcopenia management by reducing pain and facilitating movement.19 Furthermore, as there is a relationship between osteoporosis and sarcopenia (osteosarcopenia), it is important to acknowledge that manual therapy may, in some instances, lead to adverse reactions, due to potential fractures.19
Lifestyle medicine emphasises behaviour change and selfefficacy. Motivational interviewing, goal setting and readiness for change are evidence-based strategies that support engagement and adherence.26 Incorporating the general lifestyle screening tool (LM 25) questionnaire enables osteopaths to assess a patient’s lifestyle behaviours, to explore and codesign behavioural change strategies and health priorities.27
Sarcopenia and frailty are also influenced by social isolation and depression, which may reduce physical activity and nutritional intake.28 Osteopaths can screen for psychosocial barriers using appropriate outcome measures and coordinate with GPs or mental health professionals when necessary.
Osteopaths are encouraged to actively engage in interdisciplinary networks to address sarcopenia holistically. Coordinated care and case conferencing involving musculoskeletal health professionals, dietitians, general practitioners and geriatricians ensures continuity and collaboration of person-centred management for chronic, complex conditions.
Australia’s National Preventive Health Strategy 2021–2030 emphasises healthy ageing, functional independence, and the role of non-pharmacological interventions, making sarcopenia an ideal target for allied health-led initiatives.29
Osteopaths, as musculoskeletal allied health practitioners, are strongly positioned to assist in the detection and management of sarcopenia in the community. A summary of recommendations at each stage of a typical consultation is presented in Fig. 2.19
Embedding sarcopenia screening and exercise programs in primary and allied health care, aged care, and hospital discharge planning represents a systems-level opportunity to reduce disability and healthcare costs.
Peter McCann Dr Peter McCann MRes
MASc BASc DASc, FASLM, FAICE Peter has 30 years clinical experience in the field of musculoskeletal and LBP management. He is a casual academic at the School of Health, Medicine and Applied Sciences – Murdoch University.He is certified by the International Board of Lifestyle Medicine and a Fellow of the Australasian Society of Lifestyle Medicine and co-founder of the ASLM Musculoskeletal CoP.
Rebecca Prenc Rebecca holds a Master of Health Science and a Bachelor of Clinical Science (Osteopathy) from Victoria University, as well as a Bachelor of Health Science (Food Science and Nutrition) from Deakin University and a Graduate Certificate in Tertiary Education. She worked in several clinics before establishing her own within a multidisciplinary GP setting in 2018. Rebecca also teaches in the osteopathy programme at Victoria University, where she focuses on first-year education. Rebecca is volunteers her time and knowledge by participating in the CPD Working Group.
HISTORY
EXAMINATION
Identify key risk factors, signs and symptoms
• Age >60
• Loss of weight
• Reported weakness
• Falls
REFERRAL
EXERCISE PRESCRIPTION
MONITORING
• Chronic disease
• Chronic physical inactivity
• Smoking
Routinely evaluate patients at risk:
• Gait speed: < 0.8m/s
• Chair stand test: >12 seconds for 5 rises
• Grip strength: <25.5kg (males), <20kg (females)
Any positive finding should trigger management and investigation
Refer patients with, or at risk of sarcopenia for:
• Body composition assessment
• Bone densitometry
• Clinical nutrition
• Falls risk assessment and management
Exercise prescription should focus on:
• Safety: Seated, supervised and gradually progressed
• Resistance training: > 3 sessions per week
• Gait and balance training: >3 sessions per week
• Aerobic training: 150 mins per week
• Monitor at-risk patients annually
• Monitor patients with sarcopenia more regularly for improvement/decline
Sarcopenia is a prevalent and under-recognised condition that intersects directly with the core goals of osteopathic and lifestyle medicine. As Australia’s population ages, the role of osteopaths in screening, preventing and managing sarcopenia will become increasingly important.
Through evidence-based exercise prescription, nutritional guidance, education, behavioural support and interdisciplinary collaboration, osteopaths can make a significant impact on individual and public health outcomes. Sarcopenia should no longer be considered a passive consequence of ageing; it is a modifiable, preventable and reversible condition when addressed early through lifestyle medicine and rehabilitative care.
To find the full list of references for this article, scan the QR code here.

END OF CPD CYCLE RECOMMENDED MANDATORY TOPICS
AI tools for clinical administration in allied health
This on-demand webinar is tailored for members of Osteopathy Australia seeking to enhance their clinical practice through technology. Osteopaths will learn how AI can streamline operations, improve patient outcomes and enrich the quality of healthcare delivery.
Building trust with patients
On-demand webinar which will show you how to leverage your website to showcase your authority, build trust with your patients, increase bookings and stay Ahpra compliant.
Cybersecurity essentials and Privacy Act compliance for osteopaths
Find out about the cybersecurity threats facing Australian healthcare workers in this on-demand webinar, highlighting the increasing risk of data breaches within the healthcare sector. The webinar will also cover the recent changes to the Privacy Act introduced by the Privacy and Other Legislation Amendment Bill 2024.
Everything HICAPS: updates, answers to your questions and support
Hear how HICAPS can help your practice get the most from electronic claiming in this on-demand webinar. This webinar
will give you the latest on the HICAPS terminal, portal and website and how to find guides, item numbers and utilise the HICAPS Helpdesk.
Non-invasive brain stimulation for the chronic pain and post-stroke rehab. An opportunity for the profession
Non-invasive brain stimulation has recently gained regulatory approval in Australia for the treatment of chronic pain and post-stroke rehabilitation, marking a significant advancement in neurological care.
Join Dr Nic Lucas for this insightful webinar as this breakthrough opens new doors for osteopaths, whether you’re looking to refer patients or become trained in this cutting-edge modality. Osteo Talk podcast coming soon.
OAIC guide to health policy
Based on the Office of the Australian Information Commissioner’s (OAIC) Guide to health privacy (updated 9 May 2025), this elearning module explains how an osteopath can help keep a patient’s personal information safe.
Effective communication with problematic patients
This elearning module is designed to help osteopaths learn how to communicate in difficult situations and make sure bias, stereotypes and culture don’t negatively affect treatments.
Record keeping guidelines
Guild Insurance’s vast experience in managing osteopathic claims suggests many don’t fully understand what’s required in a detailed clinical record. This elearning module will help you avoid being part of the cohort whose records aren’t up to scratch.
Why insurers care about your communication
This elearning module has been created using the experience of Guild Insurance, managing and analysing osteopathy claims for many years with a focus on the relationship between communication and patient complaints.
LISTEN NOW
Inside sports osteopathy pathways, frameworks and the future
In this episode of Advanced Sports Management osteopath Louise Bibby is joined by two highly respected colleaguesBruce Duncan (Director, North Carlton Osteopathy) and Jason Stone (Director, Wantirna Osteopathy).
Together, they share stories from their involvement in sport, reflect on the origins of the Advanced Practice Groups, and unpack their pathways into sports osteopathy.
Link: omny.fm/shows/osteo-talk/inside-sports-osteopathypathways-frameworks-and-the-future?in_playlist=podcast
Vascular consideration in osteopathic practice
In this episode, osteopaths Prue Eddie and Michael Solano, faculty of the Australian Research College of Osteopathic
Medicine’s Rule of the Artery Program, join host Sonia Wainberg to unpack Dr Andrew Taylor Still’s enduring principle that “the rule of the artery is supreme.” Together, they explore how osteopathic principles support the body’s innate ability to self-regulate through unobstructed blood and lymphatic flow and optimal cellular vitality.
Link: omny.fm/shows/osteo-talk/vascular-considerations-inosteopathic-practice?in_playlist=podcast
Women’s Health Week forum
In this episode, we dive into the theme of Women’s Health Week: Our respected podcast panellists reflect on years of clinical practice and lived experiences as they highlight how education and access to information can transform patient outcomes, especially for women navigating chronic pain. Listen to the conversation between Osteopathy Australia members Beth Yule, Daniela Aiello and guests.
Link: omny.fm/shows/osteo-talk/womens-health-weekforum?in_playlist=podcast
From physiology to performance: the evolution of female athlete care with Hannah Moore

Join Australia’s first Advanced Sports Osteopath, Louise Bibby, as she sits down to chat with Hannah Moore, PhD candidate, researcher, and Strength & Conditioning Coach for the Western Bulldogs AFLW team in this extended episode.
Link: omny.fm/shows/osteo-talk/from-physiology-toperformance-the-evolution-of-female-athlete-care-withhannah-moore?in_playlist=podcast


FlexEze Heat Wraps deliver evidence-based, continuous low-level heat - supporting mobility in line with the Australian Low Back Pain Clinical Care Standard.
FlexEze Heat Wraps offer your patients a drug-free way to relieve back pain and complement hands-on osteopathic carehelping them stay active and Moving with Eze












Following five years of research and development and a further two years of real-time trials in an osteopathic clinical setting, our DrRest experts have created a mattress that health professionals can confidently recommend to patients. A sleep system that complements and supports the care that osteopathic practitioners provide.
Learn more about becoming a DrRest referrer or partner at drrest.com.au/join
ENDORSED BY*
