














routine prophylaxis in patients 12 years and older with hemophilia A or B without inhibitors
















routine prophylaxis in patients 12 years and older with hemophilia A or B without inhibitors





Introducing HYMPAVZI—a once-weekly subcutaneous prophylactic treatment that comes in a fixed-dose,* prefilled pen
*Your first dose (loading dose) of HYMPAVZI is 300 mg (two 150 mg injections). Then you will inject a weekly (maintenance) dose consisting of 1 or 2 injections as prescribed by your healthcare provider. If more than one injection is required to deliver a complete dose, administer each injection at a di erent injection site.
What is HYMPAVZI?

















It is not known if HYMPAVZI is safe and e ective in children younger than 12 years old.
IMPORTANT SAFETY INFORMATION
Important: Before you start using HYMPAVZI, it is very important to talk to your healthcare provider about using factor VIII and factor IX products (products that help blood clot but work in a di erent way than HYMPAVZI). You may need to use factor VIII or factor IX medicines to treat episodes of breakthrough bleeding during treatment with HYMPAVZI. Carefully follow your healthcare provider’s instructions regarding when to use factor VIII or factor IX medicines and the prescribed dose during your treatment with HYMPAVZI.
Before using HYMPAVZI, tell your healthcare provider about all of your medical conditions, including if you:
• have a planned surgery. Your healthcare provider may stop treatment with HYMPAVZI before your surgery. Talk to your healthcare provider about when to stop using HYMPAVZI and when to start it again if you have a planned surgery.
• have a severe short-term (acute) illness such as an infection or injury.
• are pregnant or plan to become pregnant. HYMPAVZI may harm your unborn baby.
Females who are able to become pregnant:
- Your healthcare provider will do a pregnancy test before you start your treatment with HYMPAVZI.
- You should use e ective birth control (contraception) during treatment with HYMPAVZI and for at least 2 months after the last dose of HYMPAVZI.
- Tell your healthcare provider right away if you become pregnant or think that you may be pregnant during treatment with HYMPAVZI.
• are breastfeeding or plan to breastfeed. It is not known if HYMPAVZI passes into your breast milk.



HYMPAVZI is a prescription medicine used to prevent or reduce the frequency of bleeding episodes in adults and children 12 years of age and older with hemophilia A without factor VIII inhibitors or hemophilia B without factor IX inhibitors.





Tell your healthcare provider about all the medicines you take, including prescription medicines, over-the-counter medicines, vitamins, and herbal supplements.
What are the possible side e ects of HYMPAVZI?
HYMPAVZI may cause serious side e ects, including:
• blood clots (thromboembolic events). HYMPAVZI may increase the risk for your blood to clot. Blood clots may form in blood vessels in your arm, leg, lung, or head and can be life-threatening. Get medical help right away if you develop any of these signs or symptoms of blood clots: swelling or pain in arms or legs; redness or discoloration in your arms or legs; shortness of breath; pain in chest or upper back; fast heart rate; cough up blood; feel faint; headache; numbness in your face; eye pain or swelling; trouble seeing
• allergic reactions. Allergic reactions, including rash and itching have happened in people treated with HYMPAVZI. Stop using HYMPAVZI and get medical help right away if you develop any of the following symptoms of a severe allergic reaction: swelling of your face, lips, mouth, or tongue; trouble breathing; wheezing; dizziness or fainting; fast heartbeat or pounding in your chest; sweating
The most common side e ects of HYMPAVZI are injection site reactions, headache, and itching.
These are not all the possible side e ects of HYMPAVZI. Call your doctor for medical advice about side e ects. You may report side e ects to the FDA at 1-800-FDA-1088.
Please see Important Facts about HYMPAVZI on the next page or at www.HYMPAVZI.com
Important information: Before you start using HYMPAVZI, it is very important to talk to your healthcare provider about using factor VIII and factor IX products (products that help blood clot but work in a different way than HYMPAVZI). You may need to use factor VIII or factor IX medicines to treat episodes of breakthrough bleeding during treatment with HYMPAVZI. Carefully follow your healthcare provider’s instructions regarding when to use factor VIII or factor IX medicines and the prescribed dose during your treatment with HYMPAVZI.
What is HYMPAVZI used for?
HYMPAVZI is a prescription medicine used to prevent or reduce the frequency of bleeding episodes in adults and children 12 years of age and older with hemophilia A without factor VIII inhibitors or hemophilia B without factor IX inhibitors. It is not known if HYMPAVZI is safe and effective in children younger than 12 years old.
What should I tell my healthcare provider before using HYMPAVZI?
Tell your healthcare provider about all your medical conditions, including if you:
• have a planned surgery. Talk to your healthcare provider about when to stop using HYMPAVZI and when to start it again if you have a planned surgery.
• have a severe short-term (acute) illness such as an infection or injury.
• are pregnant or plan to become pregnant. HYMPAVZI may harm your unborn baby.
Females who are able to become pregnant:
̓ Your healthcare provider will do a pregnancy test before you start your treatment with HYMPAVZI.
̓ You should use effective birth control (contraception) during treatment with HYMPAVZI and for 2 months after the last dose of HYMPAVZI.
̓ Tell your healthcare provider right away if you become pregnant or think that you may be pregnant during treatment with HYMPAVZI.
• are breastfeeding or plan to breastfeed. It is not known if HYMPAVZI passes into your breast milk.
Tell your healthcare provider about all the medicines you take, including prescription medicines, over-the-counter medicines, vitamins, and herbal supplements.
How should I use HYMPAVZI?
See the detailed “Instructions for Use” that comes with your HYMPAVZI for information on how to inject a dose of HYMPAVZI, and how to properly throw away (dispose of) used HYMPAVZI prefilled syringe or HYMPAVZI prefilled pen.
• Use HYMPAVZI exactly as prescribed by your healthcare provider.
• Your healthcare provider will provide information on the treatment of breakthrough bleeding during your treatment with HYMPAVZI. Do not use HYMPAVZI to treat breakthrough bleeding.





What warnings should I know about HYMPAVZI?
HYMPAVZI may cause serious side effects, including:
• blood clots (thromboembolic events). HYMPAVZI may increase the risk for your blood to clot in blood vessels in your arm, leg, lung, or head and can be life-threatening. Get medical help right away if you develop any of these signs or symptoms of blood clots:
̓ swelling or pain in arms or legs
̓ redness or discoloration in your arms or legs
̓ shortness of breath
̓ pain in chest or upper back
̓ fast heart rate
̓ cough up blood
̓ feel faint
̓ headache
̓ numbness in your face
̓ eye pain or swelling
̓ trouble seeing
• allergic reactions. Allergic reactions, including rash and itching have happened in people treated with HYMPAVZI. Stop using HYMPAVZI and get medical help right away if you develop any of the following symptoms of a severe allergic reaction:
̓ swelling of your face, lips, mouth, or tongue
̓ trouble breathing
̓ wheezing
̓ dizziness or fainting
̓ fast heartbeat or pounding in your chest
̓ sweating
The most common side effects of HYMPAVZI are injection site reactions, including:
• itching
• swelling
• hardening
• redness
• bruising
• pain
Headache and itching were also common side effects. A serious side effect of swelling in the legs happened in one patient in the clinical trial.
These are not all of the possible side effects of HYMPAVZI. Call your doctor for medical advice about side effects. For more information, ask your doctor.
This information is not comprehensive. How to get more information:
• Talk to your health care provider or pharmacist
• Visit www.HYMPAVZI.com to obtain the FDA-approved product labeling
• Call 1-888-HYMPAV-Z
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
Pfizer Inc., 66 Hudson Blvd East, New York, NY 10001 © 2024 Pfizer Inc. HYMPAVZI is a trademark of Pfizer Inc. All rights reserved. October 2024 PP-HYM-USA-0057


From Capitol Hill to the Rockies:

WASHINGTON DAYS
MARCH 5-7, 2025
Raise your voice on Capitol Hill in Washington, D.C.! Advocate for the bleeding disorders community and shape healthcare policy.
AUGUST 21-23, 2025
Connect, learn, and grow at the largest bleeding disorders conference in the U.S. Experience cutting-edge education and networking opportunities in Aurora-Denver, CO.


Stay up to date on all things NBDF! Visit bleeding.org/events and follow us on social.









We have a thirty-year legacy of translating science to medicine for serious diseases. We’re now applying our cutting-edge science to advance research in hemophilia B. Through our clinical research programs, we hope to answer more questions, develop more potential treatments, and discover more possibilities for patients and their families.









LEARN MORE ABOUT HOW WE MOVE SCIENCE TO MEDICINE









President and CEO
Philip M. Gattone, M.Ed.
Chair of the Board
Ryan Griffith
Vice Chair of the Board
Susan Hartmann
Treasurer Joseph Alioto, M.D.
Nikki Angeles; Cindy Bailey, PT, DPT; Maureen Baldwin, M.D., MPH; Diane Bartlett, MSSW, LCSW; Angela Brown; Tyler Buckner, M.D.; Kara Burge, LCSW; Nancy Durben; Maureen Grace; Donovan Guerrero; Brandon Hardesty, M.D.; Shanthi Hegde; Patrick James Lynch; Delores Johnson-Huber; Matthew Kivel, Psy.D.; Kim Martin; Scott Martin; Jacob Murdock; Lakeisha Parker; John Palmatier; Phillip Smith; Eliza VanZweden; Patti Williford; Nandi Yeakle
Executive Editor
Kyla Clark, kclark@bleeding.org
Senior Editor Neil Frick, M.S., nfrick@bleeding.org
Advertising Sales
Tom Corcoran, thomasWcorcoran@proton.me, 215.275.6420
Contributing Staff Associate
Angelina Wang
MANIFEST.COM
EDITORIAL, DESIGN & PRODUCTION MANAGEMENT
Managing Editor
Donna Behen, donna.behen@manifest.com
Creative Director
John Lanuza
Senior Editor
Matt Morgan
Art Director
Angela Koch
Production Director
Laura Marlowe
HemAware
engage in the practice of medicine. NBDF under no circumstances recommends particular treatments for specific individuals and in all cases recommends that you consult your physician or local treatment center before pursuing any course of treatment. All manuscript submissions should be typed double space, between 500 and 1,000 words in length











“We’re not just a community; we’re a family with a common purpose.”
Thank you for joining us at the Foundation’s recent Bleeding Disorders Conference (BDC) in Atlanta. With nearly 1,800 attendees, we powerfully demonstrated our community’s strength and unity. Our theme, “The Power of One Voice,” reminded us that while our journeys are unique, our collective voice drives meaningful change.
Connecting with you at the BDC and in chapter visits across the country has been incredibly inspiring. Your resilience, knowledge, and compassion de ne our community and motivate our mission. Each chapter contributes uniquely to our national organization, addressing local needs while supporting our broader goals. This diversity strengthens our collective impact.
In this issue, we’re highlighting an important feature story on chronic pain, which
sheds light on the challenges faced by many in our community. It underscores the vital role of hemophilia treatment center (HTC) physical therapists, whose expertise brings meaningful support and relief to patients’ lives.
As we move forward, remember that our strength lies in unity. By sharing experiences, supporting one another, and advocating together, we advance research, treatment, and quality of life for all a ected by bleeding disorders. We’re not just a community; we’re a family with a common purpose.
I’m honored to be part of this remarkable community. Together, let’s continue raising awareness, pushing for advancements, and supporting each other through challenges. We’re building a brighter future for all living with bleeding disorders. We are truly stronger together.

National Bleeding Disorders Foundation: bleeding.org
Facebook: @NationalBleedingDisordersFoundation
X: @nbd_foundation and @NBDFespanol
Instagram: @nbd_foundation
TikTok: @natlbdfoundation
YouTube: youtube.com/@NBDFvideo Advocacy: bleeding.org/advocacy
Steps for Living: stepsforliving.bleeding.org
Victory For Women: victoryforwomen.org
Better You Know: betteryouknow.org
STATS, FACTS, AND NEWS YOU CAN USE
We asked community members this question, and here are some of your answers:
















I give to NBDF because they give to all of us.
@PMILLSRVA











I support NBDF so they can provide vital programs and services to our community and so they can continue to move the needle on research!
@JUSTBETHANNLIVING



I give back to NBDF for my son.
@CATHERINESKI123













Because we cannot be more grateful with all the information that we’ve received from NBDF.
@CARRILLOPAT






My Grandson has hemophilia A severe.


There are several scholarship opportunities available to people with bleeding disorders. Both the National Bleeding Disorders Foundation (NBDF) and the Hemophilia Federation of America (HFA) have online listings of these scholarships:
NBDF: https://www.bleeding.org/ community-resources/financial-assistance/ scholarships
HFA: https://www.hemophiliafed.org/ scholarships
In addition, I encourage you to reach out to your local chapter as well as manufacturer website and specialty pharmacy if you use medications. Some hemophilia treatment centers have an educator/career counselor who can provide additional resources.
— Diane Bartlett, MSSW, LCSW Bartlett is a clinical social worker and program manager at St. Luke’s Hemophilia Center in Boise, Idaho, and a member of the Social Work Working Group.
WHAT DO YOU LOVE ABOUT YOUR JOB?
I think the heart and soul of this job is the community. It truly is a family. I have watched kids grow up, I’ve seen teens turn into mentors, and I’ve become so enmeshed in these people’s lives that it fuels me. I love being able to find wins for our families, encourage them to use their voice to speak up for themselves and for others, watch as kids learn how to self-infuse, and getting running hugs that knock me over from little kids at our Unite for Bleeding Disorders Walk.
WHAT DO YOU THINK IS THE BIGGEST CHALLENGE THAT PATIENTS AND FAMILIES FACE TODAY?
It’s no surprise that our biggest challenge is still access to treatment and care. The rules are constantly changing between insurance companies, Medicaid, med carveouts, formulary restrictions, you name it, that there’s always someone experiencing a challenge with accessing their factor or their care. We also realize that bleeding disorders are lifelong and truly affect the whole family. Education, connection, and support are the most important thing the chapter provides to those living with inheritable bleeding disorders.
HOW CAN SOMEONE WHO IS NEW TO THE BLEEDING DISORDERS COMMUNITY GET MORE INVOLVED IN THEIR CHAPTER?
I know it is super overwhelming to step into a new community when you’ve never met anyone in the room. However, I think all it takes is one community program to realize that you are not alone, the community is incredibly supportive, and that life gets a lot easier when you have a village behind you. Some of the most impactful things you can do are to attend education events and support the local Walks.
The start of a new year is a great time to make a change for the better in your lifestyle habits. These tips can help you ensure that your New Year’s resolution will have true staying power.
USE AN APP TO TRACK YOUR PROGRESS
Whether you’re looking to quit smoking, lose weight, get more active, or improve your sleep schedule, there’s a smartphone app that can help you stay motivated.
Working toward a goal is easier if you share the experience with an accountability partner.
It’s normal to have setbacks from time to time, but aim to keep a positive attitude and remain focused on your end goal

KEEP YOUR GOAL REALISTIC
Rather than aim for a drastic change, break your goal down into small, more manageable steps.
Planning to buy yourself some new workout gear or some other treat after you’ve reached a particular mile can be a powerful incentive.
The National Bleeding Disorders Foundation invites ALL community members to attend Washington Days 2025! The first Washington Days after a national election is always extra exciting. Scheduled for March 5-7, 2025, Washington Days will give us an opportunity to educate all of the new policymakers — there will be dozens of new representatives and senators, a new president, and lots of new congressional staff — about bleeding disorders and what matters most to our community.

Besides the day attending meetings on Capitol Hill in state teams, there will also







be lots of time to meet and network with hundreds of other advocates from across the country, and trainings and policy updates to equip you to continue advocating when you get home. We will re ne the precise issues we’ll be advocating for as we get closer to March, but it’s safe to assume that we’ll be talking about important federal programs affecting our community and bills to address access to care challenges.
Wouldn’t it be amazing if we had advocates from every state? What



if we had participants from every district where a new representative has been elected? Imagine what we could accomplish with broad representation from the entire community — people living with hemophilia, von Willebrand disease, rare bleeding disorders, caregivers, chapter executives and volunteers, people who work at hemophilia treatment centers, and more. We hope to see you there!

















STEPS FOR LIVING BY THE NUMBERS
NBDF’s Steps for Living website was recently redesigned to include more expanded content and make it easier for people to fi nd what they need. Here’s a look at how popular the new site has become.
Active Users
24,778 (420% Increase)
Engaged Sessions
15,516 (360% Increase)
File Downloads
1,900 (760% Increase)
Now through December 3, if you pledge to donate $20 or more per month, you will receive 1 pair of custom NBDF Converse sneakers OR 1 pair of custom NBDF Nike sneakers. The choice is yours!




At the National Bleeding Disorders Foundation (NBDF), Giving Tuesday is Giving Shoesday — a remarkable opportunity to lace up our shoes and unite as we work toward a world without inheritable blood and bleeding disorders .
• Your donation ensures that no family faces their diagnosis alone.
• Your donation helps families connect with their local chapters and hemophilia treatment centers.
• Your donation assists patients and families in navigating insurance to access comprehensive care.
• Your donation contributes to reshaping the future of our community, medicine, and hope.
Thank you for being a part of our compassionate community and for helping us make Giving Tuesday a day of hope, healing, and positive change.



To learn more and donate, visit bleeding.org/givingshoesday
Take these steps for stronger bones, no matter your age
Bone health isn’t necessarily top of mind — especially at younger ages — but it should be.
People with hemophilia are four times more likely than those without the bleeding disorder to develop osteoporosis-related fractures due to low bone mineral density (BMD), according to one study.
The reasons are complex, says Brandon Hardesty, MD, an adult hematologist at the Indiana Hemophilia and Thrombosis Center in Indianapolis.
“Many hemophilia treaters are not thinking about this issue, except in their elderly individuals,” he says. “The fact that we see lower BMD in pediatrics is one of the more concerning things that we’ve observed. It really makes an argument for doing something earlier.”

IT DOWN
Stopping the trend of low bone mineral density requires earlier intervention.
Before prophylaxis was available, people with bleeding disorders generally avoided physical activity. As kids, therefore, they missed out on play that is crucial for bone health, says Cindy Bailey, PT, DPT, OCS, SCS, ATC, director of physical and occupational therapy for the Orthopaedic Hemophilia Treatment Center at the Luskin Orthopaedic Institute for Children in Los Angeles.
“Our bones retain calcium when we do weightbearing exercise, like when you land from a jump,” she says. “Because people with bleeding disorders weren’t as active as children, they didn’t develop as much BMD early on.”
Lower BMD leads to osteoporosis, which weakens bones and contributes to fragility fractures. But this isn’t just a concern for older generations.
“Unfortunately, there is still an increased prevalence of low BMD among younger individuals who have been on prophylaxis their entire life,” Hardesty says. He points to deficiencies in factors VIII and IX, proteins that help bone formation.
Here, Bailey and Hardesty share three steps to have healthier bones.
“We never know when a person may have a bleed that prevents them from being active,” Bailey says.
“If we can work on cardiovascular fitness, joint strength, and balance now, that will help a person have a better outcome later on.”
iBailey recommends starting with cardiovascular exercise, such as walking. Then, add in strength and balance exercises. Finally, jump into weight-bearing exercises for the most bone-density benefits. Just don’t forget to wear safety equipment — Bailey says most pediatric fractures happen during play and home activities.
A few key lifestyle changes can help you build stronger bones. Prioritize a healthy diet with foods rich in protein, calcium, and vitamin D, such as meat, beans, dairy, leafy greens, tofu, fatty fish, and fortified milk, cereal, and juice. Vitamin D, which you can also get from supplements and sun exposure, helps your body absorb calcium. Additionally, avoid smoking and drinking excessive alcohol, which prohibit bone growth.
Hardesty says to talk to your health care provider about testing your vitamin D levels and bone density, so you can correct deficiencies before a fracture occurs. He is helping to write a new guideline on bone health that includes regular screenings at earlier ages for the National Bleeding Disorders Foundation’s Medical and Scientific Advisory Council. “My hope is that by recommending testing earlier,” he says, “we can pick up on low BMD earlier.”
—By Celeste Sepessy
IMPROVE YOUR HEALTH WITH PHYSICAL ACTIVITY: Regular physical activity is good for building healthy bones and other benefits. Discover more at Steps for Living: bleeding.org/physical-activity-adults
Try these tips to be confident in this important decision
Choosing a day care provider can be difficult for any parent. But Lakeisha Parker of Bryant, Arkansas, had more considerations than most because her son, Treston, has hemophilia.
“My first concern was would they have nurses? And if he has a bleed, how would they respond?” Parker says. “A lot of people don’t know what hemophilia is.”
When Treston was 1, Parker did her research to find the right day care. You can take a similar approach to calm your fears and make the best decision for your situation.
Day care staff need to understand your child’s bleeding disorder, says Kara Burge, LCSW, a social worker at the Arkansas Center for Bleeding Disorders at Arkansas Children’s Hospital in Little Rock.
“Families might need to educate their day care providers on what happens if their child gets hit in the head with a toy,” she says. “Does the provider know when that could be life-threatening?”
Start by asking providers whether they have ever had a child with a bleeding disorder under their care. Burge also recommends giving your chosen day care a fact sheet about your child’s bleeding disorder to help staff understand the condition as well as when to worry, when to administer treatment, and when to call you. The National Bleeding Disorders Foundation has resources on its Steps for Living website (stepsforliving.bleeding.org), and your medical provider or hemophilia treatment center may be able to assist with materials to share.
Parents commonly worry about how they’ll know if an accident happens during the day if their children can’t speak for themselves, Burge says.
That’s why communication is essential. Parker, for example, was clear that she wanted to be informed about any bites or bumps.
“I’m always reaching out to the administrator and Treston’s teacher: How is he? Keep me informed of everything,” she says. “I haven’t had any problems.”
As a result, Parker has been able to focus on her job and completing her doctorate. And Treston, now 2, is thriving.
“When I first got him in day care, I was stressed out constantly,” she says. “As time has progressed, I don’t worry. It’s been beneficial for him and for me.”
—By Stephanie Conner
“My first concern was would they have nurses? And if he has a bleed, how would they respond?”
The National Bleeding Disorders Foundation recommends focusing on these factors as you research your options for day care:
Well-trained staff. Ask about the qualifications and training of the center’s employees.
Group size.
With a smaller child-toteacher ratio and overall program size, teachers can more closely watch for accidents and injuries.
Low staff turnover. This can signal that the program values good teachers and staff and works to keep them.
Safe and healthy environment. Make sure the program is licensed and clean, and that children are supervised at all times.
Enriching activities. Understand how much movement is involved and make sure you’re comfortable with your child participating in those activities. DO YOUR RESEARCH Make sure your potential day care providers know what to do about bleeding disorders.



CHANGE AGENT
“Young adults are the next generation that are going to be change makers.”
couldn’t tolerate any antifibrinolytics (they caused nausea and vomiting). And her bleeding continued.
She attended conferences on bleeding disorders. There, she met doctors who guided her to demand tests, question her physicians, and keep at it until she had answers. Soon afterward, she learned that she also has factor VII deficiency. Successful treatments followed.
will replicate.
After being diagnosed with von Willebrand disease, Shanthi Hegde became an advocate for herself and others
Shanthi Hegde doesn’t like to be uninformed. A biology major at Northeastern University in Boston who plans to be a doctor, she loves medical research. But when she was diagnosed with von Willebrand disease (VWD) at age 19, after menstruating for almost nine months straight, she walked out of the health care provider’s o ce feeling very uninformed.
“When I first saw a hematologist, I had never heard of von Willebrand disease, and they didn’t give me much information about it. I ended up just doing a Google search,” says Hegde, a native of Cumming, Georgia.
She learned that VWD affects 1% of the population. As she dug further, she discovered the National Bleeding Disorders Foundation (NBDF) website, where she learned more about her condition and found a community that offered guidance and understanding.
“It was really nice to have a community to go to as a newly diagnosed patient,” says Hegde, who is now 21 and a college senior.
Hegde felt grateful to the organization. But her disease was not easily remedied. She developed anaphylaxis while taking desmopressin, and then
Around this time, Hegde “stumbled upon” NBDF’s National Youth Leadership Institute, applied, and was accepted into the 2023 NYLI cohort. “I am so thankful for the opportunity,” she says. “I have gotten to meet some amazing friends from all across the United States who have VWD, who have platelet disorders, who have hemophilia.”
Today, Hegde is an NYLI representative on the NBDF Board of Directors and has started Husky Hemophilia Group at Northeastern, which provides education about bleeding disorders and support to people who have one. Husky Hemophilia Group brings in speakers, advocates for bleeding disorders with elected officials, and helps educate the university community. Finding the confidence to start the group began with her involvement in NYLI.
“The benefit of connecting with this community is just learning from everyone and feeling that you’re part of a family,” Hegde says. “Young adults are the next generation that are going to be change makers in the bleeding disorders community, and it’s super important to stay involved so that we can be the voice and the power of the mission.”
—By Andrea Atkins
MORE ON NYLI: Discover how NBDF’s National Youth Leadership Institute assists youths in becoming leaders: bleeding.org/nyli

For generations, menstruation has been a hushed and secretive matter. Thankfully, that’s beginning to change.
Nikki Angeles, 32, of Coram, New York, was 16 when she was finally diagnosed with von Willebrand disease. That was five years after she started having abnormally heavy periods, which caused her to miss almost two weeks of school every month.
“I didn’t understand what was happening, and neither did my mother. I didn’t know what it meant or that it was abnormal,” Angeles says. She never knew to talk to her doctors about it, and none ever brought it up with her.
Up to 30% of women report heavy menstrual bleeding at some point in
their reproductive lives, and studies show that they frequently delay seeking help. As Angeles discovered, heavy menstrual bleeding is often not recognized as abnormal, partly because of the stigma surrounding menstrual periods, leaving women with bleeding disorders to struggle unnecessarily on their own.
Progress is being made, says Maureen Baldwin, M.D., MPH, an associate professor of obstetrics and gynecology at Oregon Health & Science University.
“In some states, schools are required to have menstrual products in the bathrooms for free. There is also some legislation being pushed through in some states.” (The website period.org has a catalog of these advocacy efforts.)
Patti Williford, a chapter advancement specialist with the National Bleeding Disorders Foundation (NBDF), agrees that the conversation about periods, which was hush-hush for so long, is finally opening up.
“Over the past 10 years, I’ve seen it become an important topic of conversation in the bleeding disorders
community and in society as a whole,” Williford says. “Women, girls, and people with the potential to menstruate [WGPPM] are more openly having these conversations, as are people who don’t have the potential to menstruate.”
To that end, NBDF has held period parties, where WGPPM can get support and information.
“It’s a great place for people to come and share their personal experiences, gain a better understanding of the issues faced by WGPPM, and learn how they can get involved to help solve these problems. It’s a very open and nonjudgmental space,” Williford says.
To continue the progress, Angeles has established an Instagram account (@nikki.marie_xo) to spread the word about period stigma and bleeding disorders awareness. She urges other WGPPM who’ve been diagnosed with a bleeding disorder to:
Talk about periods openly and without shame.
Don’t be afraid to seek out other opinions. “I have noticed that the first conversations for heavy periods are around either birth control or hysterectomy, which takes away your right to consider other options,” she says. If your hematologist or OB/GYN won’t listen to you, find another one who will.
Join a community of other WGPPM with bleeding disorders who can support and validate your experiences. Most important, Angeles says: “Educate yourself so you can advocate for yourself. No one knows what is going on but you. It makes you successful in your own diagnosis and your own life.”
—By Beth Levine
Visit VICTORYFORWOMEN.ORG, which celebrates the voices of women in the bleeding disorders community. Visit BETTERYOUKNOW.ORG, a bilingual initiative created to improve the awareness of signs and symptoms of bleeding disorders in women, girls, and people who have the potential to menstruate, and steps to seek out a diagnosis.
Can you imagine crossing the prairie in a covered wagon while having to deal with your period? Or better yet, being a cavewoman? Here’s what some of our ancestors used to catch the flow before we had tampons, pads, and cups.
Menstrual products have come a long way.
(nonabsorbent!)
Made of (nonbreathing, nonporous) rubber, the bloomers only added a layer of protection from leaks.
Use this guide to decide what’s important to you and what care you need
The end of life is something everyone faces but few people want to discuss. Advances in medicine have extended the lives of many people with inheritable blood and bleeding disorders.
“We frequently now have patients with bleeding disorders living otherwise normal life expectancies, so we’re not as well prepared for what end-of-life


When deciding on end-of-life care, consider what matters most to you and your loved ones.
care will look like for them,” says David Hedrick, M.D., an adult hematologistoncologist at the Indiana Hemophilia & Thrombosis Center. He urges people to prepare for end-of-life care with their families and doctors as early as possible.
If you don’t know where to start, your hemophilia treatment center (HTC) can help. “HTC social workers are trained in medical decision-making processes, including end-of-life care,” says Bryn Dunham, LCSW, a social worker at the Hemophilia and Thrombosis Center at the University of Colorado Anschutz Medical Campus.
Breaking down end-of-life care planning can also help. Here’s how.




“It’s really about taking control of the dying process rather than the dying process taking control over you.”
ENVISION YOUR IDEAL END OF LIFE
Take a holistic approach that goes beyond medical planning. “Sometimes that includes planning funeral services, making amends with family members, or dividing certain possessions,” Dunham says. “It’s really about taking control of the dying process rather than the dying process taking control over you or the caregiver.”
CREATE A PLAN FOR MEDICAL DECISION-MAKING
Get the proper legal documents in place to help doctors and caregivers manage your care as you wish. These include a durable medical power of attorney and a living will.
With a durable medical power of attorney, also called a health care proxy, you appoint someone to make medical decisions for you if you can’t make them yourself.
A living will, which is different from an inheritance will, outlines the medical treatments you would and wouldn’t want at the end of your life. Some hospitals and HTCs have their own living will documents you can ll out and keep on le.
DECIDE BETWEEN PALLIATIVE AND HOSPICE CARE
Palliative care manages symptoms related to a serious illness, such as cancer or heart failure, at any stage, not just the end of someone’s life. You can receive palliative care (also called comfort care) along with treatment to cure your illness, such as chemotherapy for cancer.
Hospice care is for people who are dying. It’s also a Medicare Part A and
medical insurance benefit administered by a hospice care provider.
To enroll in hospice care, a health care provider must certify that you have a terminal illness and have six months or less to live. Also, you must agree to stop any curative treatment for your terminal illness, though you can still receive palliative care to manage physical and mental health symptoms or other chronic health conditions.
A hospice physician will manage your primary care. Depending on what your insurance allows, the physician can coordinate palliative care, including the use of prophylaxis, with your HTC team, Hedrick says.
Medicare policies usually provide good coverage for palliative and hospice care for people with bleeding disorders, Dunham says. “But if you have a medigap policy or private insurance, you want to call them to nd out about bene ts.”
People with blood and bleeding disorders can run into problems that other people on hospice care don’t face. In general, treatments such as blood transfusions are not covered or allowed under hospice care because they are seen as curative or life-extending, Hedrick explains. So, you need to find out ahead of time what palliative care rules your insurance or hospice provider has for bleeding disorders.
“Occasionally, we have had issues with clotting factor being covered,” Hedrick says.
Your local HTC can advocate on your behalf and help explain the special
circumstances for people with bleeding disorders. “Our HTC will work with a hospice physician to ensure that there’s access to factor products and anything else that would keep the person comfortable and would help them maintain their quality of life,” Dunham says.
Know the resources and support services that are available in your community. Your HTC is the best place to start. You can also contact your local Area Agency on Aging ( eldercare.acl.gov ); these are public or private nonprofit, statedesignated groups that provide resources and support services for older people and their caregivers.
Different hospice providers offer different services. Before you choose one, compare them. Focus on what’s important to you and your loved ones and which services can add to your quality of life.
Some hospice programs offer special services such as art therapy and music therapy. Some have respite care, where trained volunteers sit with the person for a few hours so caregivers can take a break.
HTC social workers often know which local hospice agencies or nursing facilities can handle the complexities of people with bleeding disorders. “Some of it is dictated by insurance,” Hedrick says. “But we build relationships with the facilities and organizations in the area to know the best places for bleeding disorders patients.”
—By Rita Colorito



he’d be today
but he knows pain would be a much bigger problem in his life.
The 23-year-old college student who lives in New Hampshire has had chronic pain for as long as he can remember, stemming from his severe hemophilia A.
“I think I was 5,” he says. “I’ve always had a hard time with my ankles, but I’ve had muscle pains and even oral pain.”
As a child, bleeds, injuries, and chronic pain kept him from playing sports like he wanted to.
“I was on recreational basketball teams in middle school and high school, but I had to sit out probably three-quarters of the games because of bleeds,” Guerrero says.
One thing he has stuck with over the years is physical therapy, or PT.
“I’ve been doing physical therapy off and on since I was a kid,” Guerrero says. “I tend to go in seasons. Summer is always tough for me with injuries and bleeds, so I go a lot in the summer months.”
Guerrero stretches and does exercises that build strength and stability, which are key to recovery and injury prevention.
“It helps alleviate pain just by keeping me active, which is the best thing you can do for your body when you’re not under an acute injury or bleed,” he says. “I appreciate the fact that PT provides accountability. I wouldn’t be able to do this on my own because I don’t have the education and the training.”
Guerrero is far from alone. Up to 58% of people with hemophilia report having chronic pain compared with 20% of the general population, according to research gathered by the National Bleeding Disorders Foundation’s Medical and Scientific Advisory Council (MASAC). And people with hemophilia say their chronic pain affects their general activity (74%), their work (71%), their mobility (70%), and their ability to maintain relationships (56%).
“Chronic pain is a big problem among the hemophilia population,” says Tyler



When managing chronic pain in people with bleeding disorders, physical therapists should consider each person’s specific impairment and participation goals, according to new recommendations from the National Bleeding Disorders Foundation’s Medical and Scientific Advisory Council. The treatment recommendations are divided into five categories:
EDUCATION. Everyone with a bleeding disorder should receive education on pain, musculoskeletal anatomy, biomechanics, joint health, exercise safety, and the prevention and treatment of bleeding episodes.
AQUATIC THERAPY. Aquatic interventions should be offered as part of the physical therapy plan of care, leveraging the properties of water to reduce pain and improve function.
THERAPEUTIC EXERCISE. Programs that include strengthening, stretching, and aerobic exercising should be tailored to people’s needs. It’s also recommended that pain management programs include mental health services to reduce the effect of pain and complement therapeutic exercise.
MANUAL THERAPY. Manual interventions, including joint mobilizations and soft-tissue work, should be part of an individualized treatment program.
OTHER THERAPEUTIC METHODS. Transcutaneous electrical nerve stimulation, cryotherapy, and heat therapy should be offered, although there is limited evidence of their efficacy, so careful monitoring is recommended. Other methods, such as dry needling, acupressure, cupping, blood-flow restriction, and instrumentassisted soft-tissue mobilization, should be used only in coordination with a hematologist because of the potential risk of bleeding. 5 ELEMENTS OF PHYSICAL THERAPY FOR CHRONIC PAIN

Chronic pain and mental health are intimately connected, says Matthew Kivel, Psy.D., a psychologist at Oregon Health & Science University.
“Pain is a physical sensation, and we know chronic pain is especially prevalent among people with bleeding disorders,” he says. “The mental health component — it’s sort of like the volume gauge on pain. Your pain can feel more intense or less intense based on the psychological and emotional factors you are having with the pain.”
Kivel says anxiety and depression are two common mental health conditions that can increase the experience of pain. They can also worsen pain by making it more difficult to take steps to alleviate it.
“It’s cyclical. The more psychological distress, the more that your pain can be intensifi ed,” he says. “And when you’re depressed, when you’re anxious, it’s harder to do the things that a physical therapist might recommend for pain.”
That’s why the recently published physical therapy recommendations from the National Bleeding Disorders Foundation’s Medical and Scientifi c Advisory Council suggest psychosocial support. Kivel says working with a health psychologist or a mental health provider with experience treating chronic pain can help people learn coping strategies. Two such strategies are:
Activity pacing. This involves working closely with your physical
therapist to determine a safe range of activity and, within that, pushing yourself a bit further than you thought you could go. For instance, if your physical therapist says it’s safe to walk for 10 to 15 minutes and your goal is 10, push yourself to walk one extra minute.
Sensory distraction. With this technique, you’ll focus on something other than your pain.
“Your brain can only hold so much sensory information at a time,” Kivel says. “If you focus on something outside of the pain, it can make it easier to not be as impacted by it.” If you have pain when walking, for example, focus on the sights and sounds around you or try chewing gum and focusing on its fl avor and texture.
WE RECOGNIZED THAT CHRONIC PAIN IS A PERVASIVE ISSUE IN THE BLEEDING DISORDERS COMMUNITY, AND WE NEEDED TO EQUIP PHYSICAL THERAPISTS WITH THE KNOWLEDGE TO MANAGE IT WELL.
TYLER BUCKNER,
M.D.
Buckner, M.D., chair of the NBDF Pain Initiative Task Force. “We’re seeing a significant impact on patients’ quality of life, from limiting their physical activities to affecting their mental health and social interactions.”
Buckner, a hematologist at the Hemophilia and Thrombosis Center at the University of Colorado Anschutz Medical Campus, emphasizes that chronic pain is often tied to joint damage caused by repeated bleeds, especially for people who lacked access to adequate treatments earlier in life.
Managing chronic pain in people with bleeding disorders is complex. Many traditional pain relief methods, such as nonsteroidal anti-inflammatory drugs, or NSAIDs, are often not advised because of bleeding risks. Opioids sometimes are reserved for treating chronic pain, but their use is limited by potential side effects, including tolerance, dependence, and addiction.
Physical therapy, however, has emerged as a cornerstone in treating chronic pain, offering a safer, more effective approach that goes beyond medication.
Physical therapy has become an indispensable tool in managing chronic pain for people like Guerrero. By focusing on movement, physical therapy helps reduce pain, improve mobility, and prevent future injuries, though access to specialized care remains a challenge. Not everyone lives near a hemophilia treatment center or has a physical therapist trained to understand the intricacies of bleeding disorders.
That’s why MASAC published physical therapy recommendations for chronic pain management earlier this year.
“We recognized that chronic pain is a pervasive issue in the bleeding disorders community, and we needed to equip physical therapists with the knowledge to manage it well,” Buckner says. “This document provides a framework for PTs to safely and effectively treat patients, regardless of their prior experience with bleeding disorders.”
The MASAC recommendations offer details for physical therapists managing chronic pain in people with bleeding disorders, recognizing that patients will have unique needs.
“There is no one-size-fits-all approach to pain management. The document really reflects that,” says Nancy Durben, a physical therapist at the Oregon Health & Science University’s Hemostasis and Thrombosis Center, and lead author of the MASAC communication. “It’s meant to be flexible, customizable. We wrote it in a way that hopefully provides physical therapists with more options for treating patients who have bleeding disorders.”
The document begins with recommendations for conducting a proper assessment, suggesting that physical therapists use a combination of patient- and clinicianreported measures of health-related quality of life and functional assessment tools to develop a personalized care plan.
The document goes on to stress that while physical therapy plays a critical role, it’s not the only component of chronic pain management. An interdisciplinary approach involving medical providers, physical therapists, psychologists, social workers, and pharmacists is essential.
“Chronic pain is multifaceted and requires a team e ort,” Durben says. “People benet most when we combine physical therapy with medical management, psychological support, and patient education.”
Psychological support, for example, addresses the mental health concerns of chronic pain, such as depression and anxiety, which are common among people with bleeding disorders. Although medical providers are the ones who prescribe medications for pain, pharmacists can also partner with the health care team to o er guidance so that people receive the safest and most e ective treatments while minimizing risks.
“Our goal is to create a holistic treatment plan that addresses every aspect of the patient’s pain experience,” Buckner says. “It’s about providing comprehensive care that adapts to patients’ needs over time, ensuring they have the support and resources to manage their pain.”
For Guerrero, the combination of physical therapy and caring providers has been crucial.
“Pain, for me, is lifelong,” he says. “But my team has really helped me live better with it so I can have a high quality of life.”
The MASAC recommendations are a significant step toward improving chronic pain management for all people with bleeding disorders. As the community continues to advocate for better pain management practices, there is hope that people like Guerrero will have the resources and care they need to live active, fulfilling lives.
34-58% of people with hemophilia have chronic pain compared with 20% of the general population
SOURCE: Research gathered by NBDF’s Medical and Scientific Advisory Council





































NBDF’S NEW PRESIDENT AND CEO SHARES HIS THOUGHTS ABOUT THE IMPORTANCE OF COLLABORATION, HEALTH EQUITY, AND COMPASSION
was initially drawn to the chronic disease nonprofit space after his son was diagnosed with epilepsy in 1991 at age 4. Seeking support and wanting to help others in the same situation, he and his wife started to become active in the epilepsy community.
After receiving a master’s degree in education, Gattone spent some time doing community education at an epilepsy center in Chicago, eventually becoming CEO of the Epilepsy Foundation of Chicago and ultimately CEO of the Epilepsy Foundation of America (EFA). Thanks to Gattone’s leadership and vision, the EFA experienced record growth in community engagement, strategic partnerships, marketing, programming, and fundraising during his tenure.
In February 2024, Gattone took over as president and CEO of the National Bleeding Disorders Foundation. He shared his insights with HemAware , highlighting the pressing challenges facing the bleeding disorders community today and emphasizing how collaboration is essential to overcoming them and driving meaningful change.
Q WHAT LESSONS DID YOU LEARN ABOUT RUNNING A NONPROFIT DURING YOUR TENURE AS CEO OF THE EPILEPSY FOUNDATION, AND HOW WILL THOSE LESSONS INFORM YOUR NEW ROLE AT NBDF?
One thing I learned is to involve as many people as possible when you’re working to make an impact on behalf of people who live with a health condition. In my role at NBDF, I’m working with our chapter leadership, our board, local and regional boards, staff, volunteers, families, providers, advocates, and other advocacy partners to build a strategy to make the biggest impact possible. The old saying is true: “If you want to go fast, go it alone. If you want to go far, go together.”
Q WHAT DO YOU BELIEVE ARE THE BIGGEST CHALLENGES FACING THE NONPROFIT SECTOR TODAY, AND HOW DO YOU PLAN TO ADDRESS THEM?
The challenges for us right now include sustaining ourselves as an organization and making sure that our chapters have the resources they need to serve the families in their communities. I think the vast majority of our chapters would say that they do not have enough resources.
And the same is true nationally. We have investment opportunities in research and in awareness and advocacy. We have amazing opportunities to make a greater impact. And in order to grow, we really have to understand that and
sustain our efforts. This means fundraising both at a local level and at a national level. We also need to get more people and more partnerships to attach to our mission.
Understanding the challenges that families go through is a common link across different conditions that people understand and can quickly identify with. If we can send the message to the broader public about the impact of blood and bleeding disorders and the hope that exists and how NBDF is uniquely positioned to meet the needs of our community, I think we’re going to find many more people, many more friends and partners, who want to help us achieve our mission.
Q HOW DO YOU ENVISION WORKING WITH OTHER NATIONAL NONPROFIT ORGANIZATIONS DEVOTED TO BLEEDING DISORDERS?
What I’ve seen and what I’ve understood is that sometimes there can be a duplication of efforts. And I know that the people I’ve spoken with across our community broadly have expressed that same sentiment. We would all like to work together more effectively.
I was really impacted by the willingness of community partners in my previous role to work together. I would like to extend that invitation to work together more closely with our community partners because I see exponentially greater impact by doing so. We can leverage our resources, our talent, our energy, and our efforts to solve challenges together much more effectively than we can each doing it on our own. So, to me, the power of collaboration doesn’t just exist within NBDF. My vision extends beyond NBDF to collaborate and work together with the Hemophilia Alliance, the Hemophilia Federation of America, the World Federation of Hemophilia, and other groups that are dedicated to helping people with inheritable blood and bleeding disorders improve their lives.
Q TREATMENTS FOR BLEEDING DISORDERS HAVE COME A LONG WAY. HOW WILL NBDF CONTINUE TO ADVANCE NEW THERAPIES?
My predecessor, Dr. Len Valentino, really left a legacy of advancing new therapies and research and investing in new therapies that can make a difference in a time frame that matters. With all of the work that was done under



“HIS WARMTH AND KINDNESS WERE AS IMPRESSIVE AS HIS IDEAS AND EXPERIENCE.” @bauman07
“HE HAS BROUGHT NEW LIFE TO THE CHAPTER AND THE BLEEDING DISORDERS COMMUNITY”

@samantha_nazaario 718_10_321
his leadership, NBDF is now positioned very well to make advancements in those areas.
There are wonderful therapies that have come forward to help people with specific bleeding disorders. Unfortunately, there are also inheritable blood and bleeding disorders for which there still are no therapies.
Q WHAT ARE YOUR THOUGHTS ON ADDRESSING THE ISSUE OF HEALTH CARE INEQUITIES AND PROVIDING ACCESS TO ANYONE WHO NEEDS TREATMENT FOR A BLEEDING DISORDER?
Hearing so many diverse opinions and views has really opened my eyes to understand the gap that exists within our communities for some individuals. At NBDF, we are committed to ensuring that everybody who has a need is getting fair and equitable access to the very best care. And we have invested in that effort in terms of material resources, financial resources, and human resources.
Q WHAT ADVICE WOULD YOU GIVE TO ASPIRING LEADERS WHO HOPE TO MAKE A SIGNIFICANT IMPACT IN THE NONPROFIT SECTOR?
I would encourage anybody who is an aspiring leader and wants to make an impact to realize that there is power in your voice; there is power when you speak out. Tell your story and be proud of who you are. Keep your eyes open for opportunities to serve as a volunteer, as an advocate, because service leads to additional opportunities to get involved.
Q IS THERE ANYTHING ELSE THAT YOU WOULD LIKE TO SHARE WITH THE BLEEDING DISORDERS COMMUNITY?
I just want to say to families who may have just heard the words “you have hemophilia” or “you have von Willebrand disease” or “you have a rare bleeding disorder:” When you hear those words, it can rock your world, and it can knock you down.
I want everybody to know that from the CEO to every employee on our team, our board of directors, and our volunteers, we are with you. When you first get diagnosed, NBDF is with you. When you are struggling and you’re down and you’re not sure where to turn, you can lean on NBDF. And when you find the care that you need and you find success in your therapy, we’re with you to celebrate. But in the meantime, while we work for that, we will continue to advocate, educate, and innovate, and we will continue to be there with you every step of the way.








The 2024 Bleeding Disorders Conference was a celebration of community. From the opening session — which recognized the members unite their voices, stories, and passions — to the fes together in Atlanta to share insights, learn about the latest

My BDC 2024 highlight was looking over at Jeanne White-Ginder as soon as the teaser trailer for the documentary ended during opening session. It was the first time I ever shared edited footage from the film with Jeanne, and the look in her eyes was extremely satisfying. This film needs to exist for numerous reasons — one of them is for Jeanne.





the history, hope, and unity of the bleeding disorders strength that emerges when our community tive final night event, nearly 1,800 people came advancements in care, and support one another.



ahighlight of this year’s opening session was a sneak preview of an upcoming documentary about the life of Ryan White followed by a moving talk by Ryan’s mother, Jeanne White-Ginder.
Ryan White, of Kokomo, Indiana, has long been an iconic figure in the history of bleeding disorders advocacy. Born with severe hemophilia A, Ryan was diagnosed with AIDS at age 13 after contracting HIV through contaminated factor. This was in the early days of HIV/AIDS when the disease was little understood. Ryan was banned from attending school, and he and his family fought to overturn that ban.
In the process, Ryan became a national figure for HIV/AIDS awareness and helped to educate the public about the myths and realities of the disease. He passed away of AIDS in 1990 at the age of 18.
“Ryan’s story is an example of the impact that one person, a teenager from rural Indiana no less, can have on the entire world,” says Patrick James Lynch, the documentary’s producer. “The legislation that bears his name and still serves more than half of all Americans with HIV/AIDS [the Ryan White Comprehensive AIDS Resources Emergency Act] is an excellent example of bipartisan policy that truly makes a difference for all Americans.”
“I’m a mom just like all of you moms and Ryan was a very ordinary kid, just like your kids, but because of a misunderstood disease called AIDS, my life changed overnight,” White-Ginder told the audience. She went on to share personal reflections on Ryan’s journey, including his friendship with Elton John.
White-Ginder told the story of when she and Ryan were invited to attend an AIDS benefit in New York City and he was interviewed beforehand by Good Morning America . “David Hartman asked Ryan, ‘Who are you looking forward to meeting at this AIDS benefit?’ and Ryan said, ‘Oh, boy, meeting Elton John, definitely!’ And I thought, ‘I’ve always loved his music, but I always thought Elton was a little different and kind of weird.’ Well, Elton ended up being my best friend in the whole world, and he still is today.”
Lynch says the documentary is a work in progress because more funding is needed to license all of the archival footage in the film. “We are a few hundred thousand dollars away from the finished film being TV-ready, but screening the teaser trailer at BDC was a tremendous way of making the wider community aware of the project, and our needs,” he says.


The highlight has got to be seeing my friends from all over the country with bleeding disorders. It’s really cool to go from not having seen each other for a year to then jump right back into the conversation.

What really caught my interest were all of the companies in the exhibit hall that are working on new gene therapies for hemophilia. I’m looking forward to the ensuing generations of gene therapies that are to come.

RYAN WHITE
YOUTH AWARD
Gabi Flores
St. Louis, Missouri
Diagnosed with platelet dysfunction at 14, Gabi Flores was inspired to become deeply involved in the bleeding disorders community and pursue a degree in political science to focus on health care policy. They are now active in state and federal legislation, having helped pass laws on copay accumulators and step therapy. They reflect on their journey with gratitude for the strengths it has revealed.
ADVOCATE OF THE YEAR
Kate Bazinsky Wellesley, Massachusetts
Kate Reinhalter Bazinsky has over two decades of experience in health policy and advocacy, and became a passionate advocate for the bleeding disorders community after her son was diagnosed with severe hemophilia A. She co-founded and chairs the Bleeding Disorders Substance Use & Mental Health Access Coalition (BD SUMHAC), working to ensure equitable access to treatment for individuals with bleeding disorders.
LIFETIME ACHIEVEMENT AWARD
Michael Tarantino, M.D.* Peoria, Illinois
Tarantino is a board-certifi ed pediatric hematologist/ oncologist with over 30 years of experience and serves as a professor of pediatrics and medicine at the University of Illinois College of Medicine in Peoria. A national and international leader in bleeding and clotting disorders, he has authored over 150 peer-reviewed publications and has been recognized for his advocacy and contributions to the fi eld, including awards from the National Bleeding Disorders Foundation.

Mark Reding, M.D. Minneapolis, Minnesota
Reding is the director of the Center for Bleeding and Clotting Disorders and a professor of medicine at the University of Minnesota, where he has been a faculty member since 1999. He has received multiple awards for his clinical excellence and mentorship, and is also involved in research on immune responses to factor VIII.
In Memory of Joey Smiles* Scranton, Pennsylvania
Joey's warmth, resilience, and dedication made him a beloved presence at every advocacy event and a cherished member of the Eastern Pennsylvania Bleeding Disorders Foundation. As a devoted board member and natural teacher, he shared his experiences to uplift others, inspiring the community with his courage and compassion. Joey passed away unexpectedly on April 22, 2024, but his legacy of strength, advocacy, and kindness will continue to resonate within our hearts.

Congratulations go to these people who were recognized at impact on the inheritable blood and
Sammie Valadez Peru, Illinois
Valadez, a respected expert in inheritable bleeding disorders, has von Willebrand disease (VWD) and is a devoted mother to children with bleeding disorders. She co-chairs the Lived Experience Experts Working Group for the National Research Blueprint and is vice president of the Bleeding Disorders Alliance of Illinois, reflecting her deep commitment to improving lives within the bleeding disorders community.


PHYSICAL
North Carolina
Newman, a physical therapist with a master’s from Ithaca College, has been with the UNC Hemophilia and Thrombosis Center since 2011, expanding her role from part time to full time. She is involved in research, advocacy, and various projects at the center and actively participates in multiple professional organizations and committees related to bleeding disorders.

the 2024 Bleeding Disorders Conference for making a lasting and bleeding disorders community.

Kathaleen Schnur, MSW, LCSW Pittsburgh, Pennsylvania
Schnur has a decade of experience from the Hemophilia Center of Western PA, where she addresses social work issues at multiple levels and collaborates with national groups to develop educational initiatives. As the NBDF Social Work Working Group chair and a recent member of the World Federation of Hemophilia Psychosocial Committee, she is dedicated to empowering individuals and advocating for change in the fi eld of bleeding disorders.
MARY M. GOOLEY
HUMANITARIAN OF THE YEAR
Craig Hooper, Ph.D.* Atlanta, Georgia
After completing a postdoctoral fellowship at Mayo Clinic, Hooper joined the Centers for Disease Control and Prevention’s Division of Host Factors, now known as the Division of Blood Disorders, where he directed the laboratories and later served as division director from 2015 to 2023.

Scott and Kim Martin* Houston, Texas
Private investors
Scott and Kim Martin have dedicated their efforts to improving the lives of those with bleeding disorders, inspired by their son with severe hemophilia. Scott, who is a former chair of the NBDF board and cofounded Inspiration Biopharmaceuticals and Martin Midstream Partners, serves on multiple nonprofit and corporate boards.
(Read more about Scott and Kim on Page 42.)
Donna Cardi, RN, BSN* New York City
Cardi began her nursing career in 1975 at the New York Hospital’s neonatal ICU, where she spent 19 years and earned distinctions including senior staff nurse and head nurse. In 1993, she transitioned to the hemophilia treatment center at the New York-Presbyterian Hospital/Weill Cornell Medical College, where she spent 31 years as a clinical nurse coordinator, making signifi cant contributions to patient care, education, and research in pediatric hematology and oncology.


Paul Monahan, M.D. Chapel Hill, North Carolina
Monahan, executive director of hematology research and development at CSL Behring, has led gene therapy clinical development for hemophilia A&B across several companies, culminating in the global approval of the first licensed gene therapy for hemophilia in 2022-2023. Prior to his industry work, Monahan was a professor of pediatrics at the University of North Carolina at Chapel Hill School of Medicine, where he treated children with bleeding disorders for over 20 years.
GENETIC COUNSELOR OF THE YEAR
Hannah Helber, MS, CGC Houston, Texas
Helber is a certified genetic counselor at Texas Children's Hospital and Baylor College of Medicine, where she specializes in hereditary hematologic disorders. A graduate of The Ohio State University and Baylor's Genetic Counseling Program, she is dedicated to counseling and educating families affected by bleeding disorders through her work with the multidisciplinary HTC clinic.
Jeremy Griffin New York, New York
Griffin is the executive director of the New York City Hemophilia Chapter (NYCHC), where he has been working since 2016. He is known for his work in building engaged patient communities and is particularly proud of co-developing the TORCH (Teen Opportunities and Resources for Community Health) Teen Retreat.

NANDI YEAKLE PHILADELPHIA, PENNSYLVANIA
For me, the most enlightening session of the entire conference was “Finding Our Way Back to Each Other,” which was led by a married couple who are both reverends. It was so welcoming and supportive and I loved being able to share my story with others and to feel like we’re all going through this together.

My favorite thing this year has been the emphasis on women, girls, and people with the potential to menstruate. It’s so exciting to see how every chapter and every community is talking about women and recognizing that women can bleed, too, and that this is an area where we need to focus more research on.
BDC’s closing night event was a fun-filled fi nale. “Tonight, we celebrate not just what we’ve learned, but who we are — a family united by challenges but defi ned by our strength and joy,” said Phil Gattone, NBDF’s president and CEO.














A valued and beloved member of the National Bleeding Disorders Foundation for more than 25 years, Neil Frick passed away unexpectedly in July 2024. He has left a profound void in the hearts of countless members of the bleeding disorders community, who mourn the loss of a compassionate leader who made a significant impact in the lives of people with bleeding disorders. Here, colleagues and friends share their remembrances of Neil.

“Neil was incredibly passionate about the work that he and all of us did together at NBDF. He was proud of his role as the senior vice president for medical programs and information and he was fiercely protective and caring about his team, many of whom he had worked with for the majority of his 25+ years at NHF/NBDF. They were dear friends . . . a family to Neil.
He had friends all across the globe. After his passing, we received so many emails, texts, WhatsApp messages, and notes of condolences and there was a common thread throughout: Neil’s smile, wit, dry sense of humor, and how caring he was of everyone. Each of them felt truly seen and heard by Neil.”
DAWN ROTELLINI , CHIEF OPERATING OFFICER, NATIONAL BLEEDING DISORDERS FOUNDATION



Neil was a thoughtful and e ective supporter of nurses in the bleeding disorders community.




If you didn’t have a chance to work with Neil, you missed an amazing opportunity to learn and interact with one of the best advisers in our profession.





“Neil was part of the team that raised me up in the community and was always kind to me. I will miss his face and his smile, because every time he saw me he greeted me with a smile and a big hug. That’s who he is to me . . . a smile and a warm hug.”
CATHY TIGGS , MSSA, LISW, UNIVERSITY HOSPITALS CLEVELAND HEMOSTASIS & THROMBOSIS CENTER

“I
had the honor of working with Neil for many years on di erent NHF/NBDF projects, and when we started traveling together internationally, we became very tight. His acerbic humor was often punctuated with an “Oh, please,” complete with a look of disdain. I miss him terribly.”
RANDY

Neil was a true leader — he greatly contributed to improved treatment, care, and education of people with bleeding disorders and their families.
SHARON CARIS, FORMER EXECUTIVE DIRECTOR OF HAEMOPHILIA FOUNDATION AUSTRALIA

“I’ve known Neil for about 25 years. At first, I knew him as a member of NBDF, as someone who was always there. But when I became chair of MASAC, I really got to know him. He was my right-hand man. He had a wicked sense of humor, and he cared so deeply about this community. We’re really going to miss him.”
AMY DUNN , M.D., CHAIR, NBDF MEDICAL AND SCIENTIFIC ADVISORY COUNCIL (MASAC)




This summer, kids with bleeding disorders and their family members participated in activities inspired by the Olympics, The Amazing Race, and STEM during camps hosted by three NBDF chapters
In early June, 45 children and teens with bleeding disorders and their siblings spent a week at Kings Lake Camp in Wasilla, Alaska.
Campers hiked, canoed, competed in races inspired by the Olympics, and slept in rustic cabins. Some activities were distinctly Alaskan: Everyone helped the Alaska Department of Fish and Game stock Kings Lake with buckets full of rainbow trout. During a polar bear plunge, brave participants jumped into the frigid lake. Campers also learned how to self-infuse and how to gauge health risks associated with different behaviors.
“This independent lifestyle is crucial in Alaskan villages with limited access to care,” AHA Executive Director John Palmatier says. “Camp provides valuable tools that campers use for the rest of their lives.”
Learn more about the Alaska Hemophilia Association: alaskableedingdisorders.org





Beginning in late July, 40 campers with bleeding disorders spent five days at Camp Wilderness at the Lake Doniphan Conference & Retreat Center near Kansas City, Missouri.
In addition to swimming, fishing, and archery, campers did STEM activities, including racing robots and launching rockets that they built themselves.
The campers, ages 7 to 17, connected with peers and counselors, many of whom were Camp Wilderness alumni. Campers participated in daily infusion clinics, where they were paired with nurses or peers to build their skills and confidence.
“My favorite part of camp is watching experienced youth encourage, teach, and challenge the newer infusers,” MHA Executive Director Angela Brown says. “When they bang that gong and receive their Big Stick award, it’s a proud moment.”
Learn more about the Midwest Hemophilia Association: midwesthemophilia.org

NATIONAL BLEEDING DISORDERS FOUNDATION’S NEVADA CHAPTER: FAMILY CAMP
More than 60 children and adults, ranging in age from 1 to 80, attended Family Camp in June at Camp de Benneville Pines in Southern California. Families participated in hiking and other outdoor activities, artistic endeavors such as tiedyeing, and team-building exercises including an Amazing Race event. Children and families also attended infusion clinics, where everyone received ageappropriate medical support and information.
“Our program offers a break where families can bond, relax, and enjoy shared experiences free from the constant pressures associated with bleeding disorders,” says Jacob Murdock, executive director of NBDF’s Nevada Chapter. “It’s crucial to provide opportunities for these families to escape their daily worries and create new, positive memories together.”
Learn more about the Nevada Chapter of NBDF: hfnv.org
—By Lisa Fields

The event will bring together medical and musculoskeletal (MSK) professionals, bleeding disorders patients, and community advocates
Next year, the World Federation of Hemophilia (WFH) will host the WFH 2025 Comprehensive Care Summit: New Developments in Bleeding Disorders and MSK, or musculoskeletal disorders. The global event will take place in person from April 23 to 25 in Dubai, United Arab Emirates, at Le Meridien Dubai Hotel & Conference Centre. The 2025 summit builds on the success of the first Comprehensive Care Summit, held in 2023 in Buenos Aires, Argentina. The summit will bring together medical and musculoskeletal (MSK) professionals, bleeding disorders patients,
and community advocates to discuss the latest medical research and assess current issues in managing bleeding disorders. Over three days, participants will enjoy more than 40 hours of continuing educational sessions across three tracks: musculoskeletal, medical, and people with bleeding disorders (PWBD).
Speakers from around the world will cover a variety of topics, including advances in arthropathies, therapeutic and technological advancements in hemophilia, and women and bleeding disorders. Participants will have the opportunity to take part in interactive
sessions, panel discussions, and innovative industry symposia.
The medical track will feature cuttingedge research and the latest developments in the treatment of hemophilia and other bleeding disorders. PWBD sessions will provide educational content from a multidisciplinary perspective, including the psychosocial specialist, dentist, nurse, physician, physiotherapist, community member, and patient points of view. Musculoskeletal tracks will be devoted to the latest musculoskeletal trends and emerging techniques and will appeal to MSK specialists, health care professionals, PWBDs, and their families.
Researchers from around the world will have the opportunity to submit abstracts covering solutions and interventions related to the summit tracks. Allied health professionals in an academic or community setting, community organization members, health care providers, and students who are doing new and innovative research will all have a chance to showcase their work to a global audience of experts.
Dubai’s commitment to innovation and excellence is the perfect fit for the summit. The city is an ideal location for the summit because of its geographic position as a global hub connecting the world, making it easily accessible for international attendees. Dubai boasts world-class infrastructure and a wide range of accommodations. The city offers visitors a rich cultural experience and a wide range of leisure activities, ensuring that attendees can enjoy a balanced mix of professional development and personal relaxation.
“The WFH 2025 Comprehensive Care Summit: New Developments in Bleeding Disorders and MSK will highlight the importance of different aspects of care in the comprehensive care framework, and the importance of exploring innovative approaches to care,” says Cesar Garrido, president of WFH. “Our field is changing every day, and I encourage you to attend and be part of the conversation.”
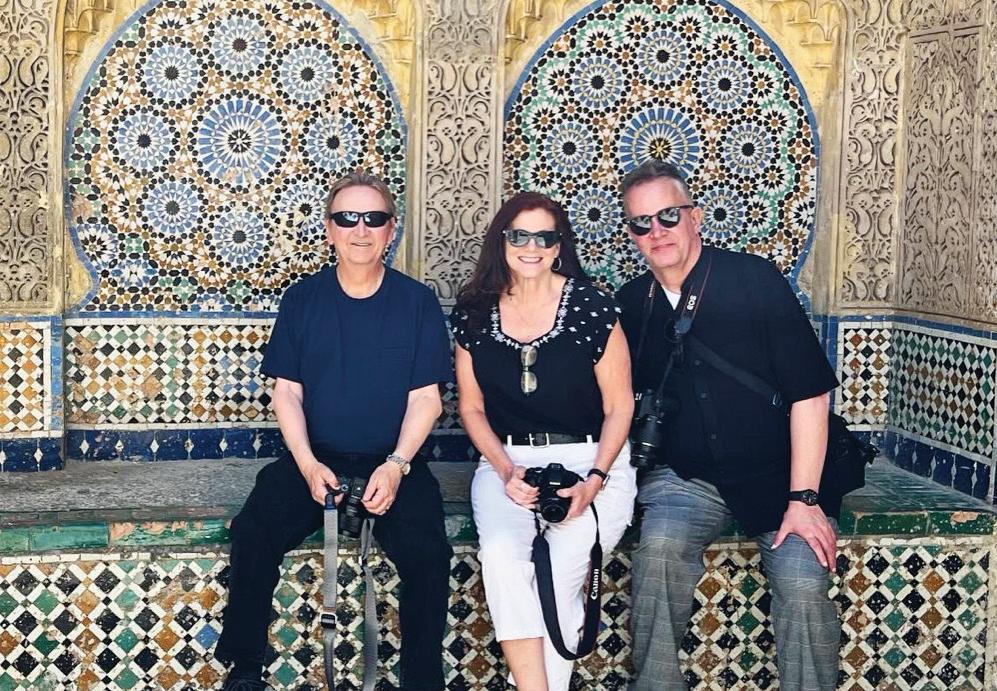
Kim and Scott Martin strengthened their 20-plus-year relationship with NBDF by becoming founding donors to the foundation’s venture philanthropy fund
When Kim and Scott Martin’s son, Scott Jr., was born with severe hemophilia B in 2003, the treatment landscape was extremely limited.
“Back then, we only had one recombinant option,” says Scott, a Houstonbased private investor. “Today, so much has changed. We now have five or six recombinant options for hemophilia B,
as well as gene therapy. Hemophilia A patients also have a gene therapy option, as well as many other choices.”
Helping to fund research into better treatments has been near and dear to the Martins ever since they first got involved with their local Lone Star Chapter

COUPLE GOALS
Scott and Kim Martin have given their time and treasure to NBDF for more than 20 years.
of the National Bleeding Disorders Foundation (NBDF, then called the National Hemophilia Foundation), soon after their son was born.
The Martins were the founding chairs of the first bleeding disorders walk in Houston and were instrumental in organizing a family camp for their chapter.
After attending the Bleeding Disorders Conference in 2004, the couple were inspired to get involved on a national level.
Scott joined the board of NBDF in 2014 and went on to serve as chair in 2021–23. During his time on the board, “there was a big push within the organization to focus more on research for our patient population,” he says. Then, “an anonymous donor passed away and left his almost $3 million estate to NBDF,” Scott says. “His stipulation was that 100% of the money go to research.”
In 2022, NBDF used that donation to launch Pathway to Cures (P2C), a venture philanthropy fund focused on investing in emerging biotech companies developing cures, therapies, and technologies to support the inheritable blood and bleeding disorders community. Though NBDF is the parent organization, P2C operates independently with a volunteer board of directors, a team of investors, scientific researchers, and health care professionals.
The Martins became founding donors to P2C, and Scott currently serves as the board chair. The couple say their involvement with P2C is especially meaningful when they think about how much their child’s life has improved thanks to better treatments. “Today, our son is in college, he infuses himself once a week, and he’s able to play basketball, golf, and tennis,” Kim says.
Adds Scott: “We are so grateful for the improvements in care and the sacrifices of so many others over the past few decades, which have benefited our son and all current patients.”
—By Christina Frank






























































The first large study in more than 30 years reveals that boys and young men develop and function normally
It has been several decades since a large U.S. study of neurodevelopment and other cognitive functions in children and young adults with hemophilia was published. Results of this earlier research evaluating hemophilia and neurocognitive development suggested that the disease was associated with poorer outcomes in areas such as academic achievement, attention, behaviors, and emotional and adaptive functioning compared with the general U.S. population.
However, these studies reflected a very different time — when HIV infections placed a significant burden on patients, and before today’s enhanced standards of care were available. Investigators of a
recently published observational study set out to capture new data that accounts for advances in care and other factors. Findings from the Evolving Treatment of Hemophilia’s Impact on Neurodevelopment, Intelligence, and Other Cognitive Functions (eTHINK) study were published in May in The Journal of Pediatrics
The only previous large study examining neurodevelopment in hemophilia, the Hemophilia Growth and Development Study (HGDS), was published in 1994. “Since then, many disease and treatment-related factors have evolved, making the current study an important update of the existing literature,” the authors explain.
Males with hemophilia performed within or above expectations on standardized tests.
The new study assessed the effects of hemophilia type and severity, intracerebral hemorrhage, hemophilia treatment type, socioeconomic status, and neurodevelopmental disorders or symptoms (e.g., ADHD, attention problems) on cognitive, adaptive, and social-emotional functioning compared with the general population. Between September 2018 and October 2019, eTHINK investigators at hemophilia treatment centers enrolled 551 male patients ages 1 to 21 with hemophilia A or B of any severity, with or without inhibitors.
Investigators found that male children and young adults with hemophilia performed within or above age expectations on standardized tests of “higherorder” intellectual ability. This stands in contrast with the HGDS results showing decreased intellectual functioning associated with the presence of HIV. As HIV is no longer a significant issue for people with hemophilia in developed countries, the authors suggest that this is a contributing factor in higher intellectual performance.
Overall, the results of eTHINK suggest that boys and young men with hemophilia develop and function within the normal range for their age in several cognitive and behavioral areas.

Delores Johnson-Huber says raising sons with hemophilia has taught her the importance of having a voice
After my newborn son Ethan’s circumcision, he wouldn’t stop bleeding. The doctor said it was normal and sent us home with Silvadene cream, despite my protests.
The first time I changed Ethan’s diaper at home, it was full of blood. I called the hospital and was told again that this was normal. I knew it wasn’t. Bleeding disorders run in my family: My mom was a carrier, and I was diagnosed with von Willebrand disease at age 5. So finally,
after more back-and-forth, the hospital relented and allowed me to bring him back in. It came as no surprise when doctors diagnosed Ethan with hemophilia A. He ended up with a blood transfusion and was in the NICU for 46 days. Things felt very heavy back then. I wasn’t allowed to hold my new baby, and I grieved for the time we lost together. If doctors had listened to me in the first place, things might not have escalated to that point.
As Ethan grew, my voice grew stronger as well. Frequent nosebleeds plagued him, and because he needed factor so often, doctors implanted a port when he was about 18 months old. He spent many weeks, sometimes months, in the hospital with infections, which I blamed on the port. Yet once again, my beliefs were ignored. When he was about 4, I stopped taking no for an answer. They removed the port, and sure enough, the infections stopped.
I knew I couldn’t keep fighting alone, so I found my local chapter of the National Hemophilia Foundation (now called the National Bleeding Disorders Foundation) in Western Pennsylvania. Suddenly, I had an entire group of moms supporting me. They walked me through things, answered my questions, and formed a strong bond with me and my son.
Before my second child, Kyrie, was born, testing revealed that he also had hemophilia A. By that time, I knew I had to demand every single thing that my kids needed. At one point in elementary school, Ethan was restricted from gym. I marched into that school and told them: “He has rights, and you have to let him participate. You’re going to treat him fairly and with respect.”
Today, I’m so proud of my boys. From the beginning, I took them to advocacy events, like Washington Days, so they could see how important it is to take on issues that really matter. They’ve also learned to speak up for themselves. Ethan’s 18 now, and if he gets a bleed, he knows exactly what to do. Kyrie’s 9. He’s still a little needle-shy, so he doesn’t do his own infusions quite yet, but he does mix his own medicine.
I know what it felt like to be brushed off, and I didn’t want my kids to grow up like that. The more that I do, the more I realize how important it is to have a voice. I want to continue to do that for myself, my boys, and for people who can’t yet do it for themselves.
—By Delores Johnson-Huber, as told to Leslie Pepper











— Julian Person


