



*Individual
What is BEQVEZ?
• Have an active infection







































IMPORTANT SAFETY INFORMATION

















































































































FOR ELIGIBLE ADULTS WITH MODERATE TO SEVERE HEMOPHILIA B







*Individual
• Have an active infection


























































































































































In hemophilia B, the factor IX (FIX) gene is changed or mutated. As a result, the body doesn’t make enough clotting FIX protein. BEQVEZ aims to deliver a working gene to help your body make its own FIX. BEQVEZ o ers a chance at bleed protection without the need for FIX prophylaxis after just one infusion*








BEQVEZ is a one-time gene therapy used for the treatment of adults with moderate to severe hemophilia B who are receiving routine prophylaxis, or have a current life-threatening bleed or a history of life-threatening bleeds, or have repeated serious spontaneous bleeds.
Before treatment with BEQVEZ, your healthcare professional will conduct a blood test to check for neutralizing antibodies to the AAVRh74var virus. The results of this testing will help determine if you may receive BEQVEZ.
Before receiving BEQVEZ, tell your healthcare professional about all your medical conditions, including if you:
• Have kidney or liver problems, including hepatitis
• Have factor IX inhibitors or a history of factor IX inhibitors
BEQVEZ may cause serious side e ects, including:
Increased Liver Enzymes. Most patients treated with BEQVEZ developed elevated liver enzyme levels and most did not experience any symptoms.
Your healthcare professional will monitor liver enzymes and factor IX activity levels before administration of BEQVEZ and frequently following the administration to detect and identify possible elevations in liver enzymes and to monitor your response to BEQVEZ. Your doctor may prescribe a corticosteroid for the treatment of elevated liver enzymes.
Limit alcohol consumption during the first year following BEQVEZ infusion, as alcohol may reduce the e ect of BEQVEZ and may increase liver enzyme levels.
Infusion reactions, including hypersensitivity and severe allergic reactions (anaphylaxis) may occur. Alert your healthcare professional right away if you get any symptoms of hypersensitivity, which may include but are not limited to low blood pressure, fever, heart palpitation, nausea, vomiting, chills, or headache.




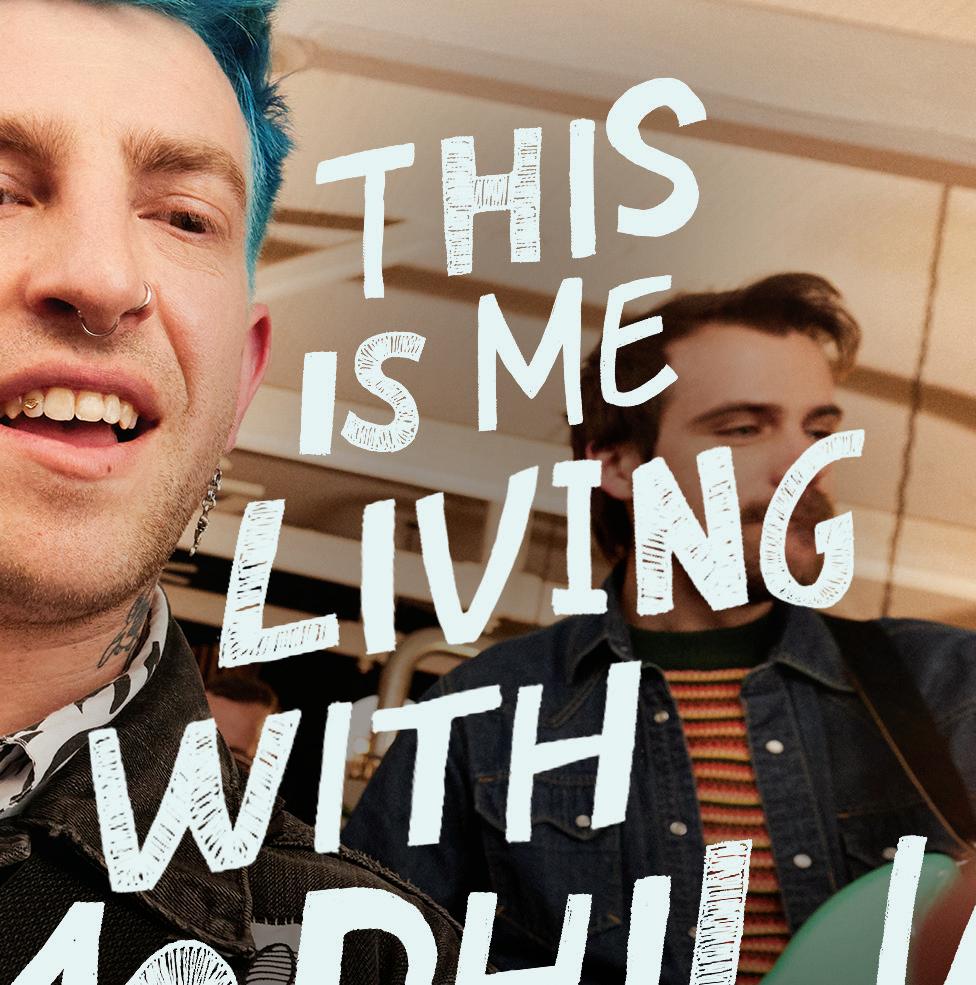




*Tim
Tim, who received the BEQVEZ infusion in 2021*
Scan the QR code to sign up now at BEQVEZ.com


Get emails with educational tools and materials to help support you on your BEQVEZ treatment journey
BEQVEZ can insert itself into the DNA of cells in the human body. The e ect that insertion may have on those cells is unknown but may contribute to a theoretical risk of cancer. There have been no reported cases of cancer caused by treatment with BEQVEZ.
The most common side e ect of BEQVEZ is increased liver enzymes. These are not all the possible side e ects of BEQVEZ. For more information, ask your healthcare professional.
Talk to your healthcare professional before receiving any vaccinations if you are taking a corticosteroid.
Talk to your doctor about any medications you plan to take including over the counter medications, herbal supplements, and vitamins as certain substances can a ect the liver and may reduce the e ectiveness of BEQVEZ.
Your healthcare professional will test your factor IX activity levels and for factor IX inhibitors.
After receiving BEQVEZ, your doctor will discuss whether and when you are able to stop prophylaxis, if you need to resume prophylaxis, and actions you may need to take for surgeries, procedures, injuries, and bleeding events.
Do not donate blood, organs, tissues, or cells for transplantation following administration of BEQVEZ. BEQVEZ is not intended for administration to women. Males should not donate sperm and should use a male condom or not have sexual intercourse for up to 6 months after receiving BEQVEZ.
Patients and caregivers should ensure proper handling of any materials that have come into contact with the patient’s urine, feces, saliva, mucus, or semen in the first 6 months after BEQVEZ infusion.
You are encouraged to report negative side e ects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
Please see Important Facts on page 2.
What is BEQVEZ used for?
BEQVEZ is a one-time gene therapy used for the treatment of adults with moderate to severe hemophilia B who are receiving routine prophylaxis, or have a current lifethreatening bleed or a history of life-threatening bleeds, or have repeated serious spontaneous bleeds.
Before treatment with BEQVEZ, your doctor will conduct a blood test to check for neutralizing antibodies to the AAVRh74var virus. The results of this testing will help determine if you may receive BEQVEZ.
Women, patients under the age of 18 years, patients with hypersensitivity to factor IX replacement product, and patients with a history of or active factor IX inhibitors should not take BEQVEZ.
What should I tell my healthcare provider before my BEQVEZ infusion?
Tell your doctor about all your medical conditions, including if you:
• Have kidney or liver problems, including hepatitis
• Have factor IX inhibitors or a history of factor IX inhibitors
• Have an active HIV infection
• Have hypersensitivity to factor IX replacement product
What warnings should I know about BEQVEZ?
BEQVEZ may cause increased liver enzymes. Most patients treated with BEQVEZ developed elevated liver enzyme levels and most did not experience any symptoms. Your doctor will monitor liver enzymes and factor IX activity levels before administration of BEQVEZ and frequently following the administration to detect and identify possible elevations in liver enzymes, to monitor your response to BEQVEZ, and to test for the development of inhibitors. Your doctor may prescribe a corticosteroid for the treatment of elevated liver enzymes.
Infusion reactions, including hypersensitivity and severe allergic reactions (anaphylaxis) may occur. Alert your doctor right away if you get any symptoms of hypersensitivity, which may include but are not limited to low blood pressure, fever, heart palpitation, nausea, vomiting, chills, or headache.
BEQVEZ can insert itself into the DNA of cells in the human body. The effect that insertion may have on those cells is unknown but may contribute to a theoretical risk of cancer.
What are the side effects of BEQVEZ?
The most common side effect of BEQVEZ is increased liver enzymes. This is not the only possible side effect of BEQVEZ. For more information, ask your doctor.
What should I avoid after my BEQVEZ infusion?
Limit alcohol consumption during the first year following BEQVEZ infusion, as alcohol may reduce the effect of BEQVEZ and may increase liver enzyme levels.
Do not donate blood, organs, tissues, or cells for transplantation following administration of BEQVEZ.
Males should not donate sperm and should use a male condom or not have sexual intercourse for up to 6 months after receiving BEQVEZ.
What else do I need to know after I receive my BEQVEZ infusion?
Your doctor will test your factor IX activity levels and for factor IX inhibitors.
Your doctor will discuss whether and when you are able to stop prophylaxis, if you need to resume prophylaxis, and actions you may need to take for surgeries, procedures, injuries, and bleeding events.
Patients and caregivers should ensure proper handling of any materials that have come into contact with the patient’s urine, feces, saliva, mucus, or semen in the first 6 months after BEQVEZ infusion.
Talk to your doctor about any medications you plan to take including over-the-counter medications, herbal supplements, and vitamins as certain substances can affect the liver and may reduce the effectiveness of BEQVEZ and may increase the risk of serious liver reactions.
Talk to your doctor before receiving any vaccinations if you are taking a corticosteroid.
Ask your doctor or pharmacist. This is only a brief summary of important information. For full Prescribing Information, go to BEQVEZ.com.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.

hemaware.org
manifest.com

pfizer.com
President and CEO
Philip M. Gattone, M.Ed.
Chair of the Board
Ryan Griffith
Vice Chair of the Board
Susan Hartmann
Treasurer Joseph Alioto, M.D.
Executive Editor
Kyla Clark, kclark@bleeding.org
Senior Editor
Neil Frick, M.S., nfrick@bleeding.org
Advertising Sales Tom Corcoran, thomasWcorcoran@proton.me, 215.275.6420
Contributing Staff Associate Angelina Wang
EDITORIAL, DESIGN & PRODUCTION MANAGEMENT
Managing Editor Donna Behen, donna.behen@manifest.com
Creative Director John Lanuza
Senior Editor Kellie Escoto
Art Director Angela Koch
Production Director Laura Marlowe
Photo Editor Sara Elder The National Bleeding Disorders Foundation is grateful to Pfizer for sponsoring this special issue. HemAware (ISSN 1088-7008) is published by the National Bleeding Disorders Foundation (NBDF), 1230 Avenue of the Americas, 16th Floor, New York, NY 10020, 212.328.3700, toll free 800.42.HANDI, fax 212.328.3777. The opinions expressed are those of the authors alone and do not represent the opinions, policies, or position of NBDF, the Board of Directors, or editorial staff This material is provided for your general information only. NBDF does not give medical advice or engage in the practice of medicine. NBDF under no circumstances recommends particular treatments for specific individuals and in all cases recommends that you consult your physician or local treatment center before pursuing any course of treatment. Acceptance of advertising for products and services in HemAware in no way constitutes endorsement by the National Bleeding Disorders Foundation. ©2024 National Bleeding Disorders Foundation.

At the National Bleeding Disorders Foundation (NBDF), our mission is rooted in the core beliefs of innovation, sustainability, and access, and Pfizer’s unwavering support and partnership have been instrumental in advancing these pillars, making a tangible di erence in the lives of those we serve in the bleeding disorders community.
Innovation lies at the heart of progress. P zer’s dedication to groundbreaking research and the development of cutting-edge therapies has signi cantly improved treatment options for people with bleeding disorders. By pushing the boundaries of medical science, P zer not only enhances the quality of life for patients but also inspires hope for a future where bleeding disorders can be managed e ectively, or even cured.
Sustainability ensures that these advancements endure, providing long-term benefits to the bleeding disorders community. P zer’s commitment to sustainable health care solutions means that people with bleeding disorders can count on consistent and reliable care. This focus on longevity and stability fosters a sense of security and optimism, allowing community members and their families to plan for brighter futures.
Access is a fundamental right yet remains a significant challenge for many affected by
“Together, we are breaking barriers, setting new standards in care, and creating a more inclusive and supportive community.”
bleeding disorders. P zer’s e orts to broaden the availability and affordability of lifechanging treatments are commendable. Its initiatives to overcome barriers to care resonate deeply with NBDF’s mission to ensure that all people, regardless of their circumstances, can access the therapies and support they need to lead healthy, fulfilling lives.
Our partnership with Pfizer exemplifies a shared vision of a world where those affected by bleeding disorders can thrive without the constraints of their condition. Together, we are breaking barriers, setting new standards in care, and creating a more inclusive and supportive community.
I extend my deepest thanks to Pfizer and all of our partners for their remarkable partnership and steadfast dedication to the bleeding disorders community. As we continue this journey together, I am confident that our combined efforts will lead to even greater advancements and a brighter future for all.
With heartfelt appreciation,
Philip M. Gattone, M.Ed., President and CEO National Bleeding Disorders Foundation
In this special issue of HemAware, you’ll meet two men with hemophilia B who underwent gene therapy — a groundbreaking advance that addresses the disease at its genetic root and has the potential to help people produce their own stable and protective levels of clotting factor for years. However, the therapy comes with risks, which is why experts say pursuing this treatment must involve careful deliberation and collaboration among patients, their loved ones, and their healthcare teams. Learn how these two men navigated this complex journey.
















“When you don’t have to think about treating all the time, it really takes a big load off of you mentally.”
Maurits
As a longtime car enthusiast, one of Bill Maurits’ favorite activities is attending antique and classic car shows. But living with severe hemophilia B, he knew that spending all day at a show would mean suffering the consequences later, even though he would treat prophylactically the night before.
“I’d typically go to car shows on Fridays because I’d have to have my ankles in ice Friday night, all day Saturday, and all day Sunday just to be able to ‘half gimp’ into work on Monday morning,” says Bill, 54, a structural engineering designer in Conowingo, Maryland.
Now, eight years after taking part in a clinical trial for gene therapy for hemophilia B, Bill says that recovering from a day at a car show looks extremely di erent. “I don’t treat the night before a show. I’m a little sore when I get home and a little less sore the next day, and after that I’m good to go,” he says. “Just having that higher level of factor all the time makes a big di erence in my recovery.”
Dave Robinson, 61, who received gene therapy for severe hemophilia B in 2016 as part of a clinical trial, says he’s been able to significantly increase his daily walking routine since undergoing the treatment. “After I began using extended half-life factor, I started doing more walking for exercise, but I could only walk about 3,000 or 4,000 steps a day because my ankles were in pretty bad shape and there was a lot of pain involved,” says Dave, an IT consultant in Falls Church, Virginia. “Since having gene therapy, I’ve been able to up my walking game considerably. I’m usually able to walk anywhere from 7,500 to 10,000 steps in a day, and even though I still feel some pain, I’ve learned over time that the pain is not a bleed. I haven’t experienced any ankle bleeds, even with the increase in the amount of walking I do.”
Bill and Dave are among the more than 400 men worldwide (to date) who have undergone gene therapy for hemophilia, a breakthrough and potentially life-changing treatment that addresses the disease at its genetic source. While both men say that gene therapy didn’t cure them of their
In 2023, when Bill Maurits and Dave Robinson were invited to participate in a patient panel, they discovered a touching connection: As children in the 1970s, they were patients of the same hemophilia treatment center and their mothers knew each other. Both women were actively involved in the Maryland chapter of what is now called the National Bleeding Disorders Foundation. Fifty years ago, their mothers probably never could have imagined that their sons would be the beneficiaries of this amazing medical breakthrough.







CHALLENGES
Growing up, both Dave and Bill say they experienced a range of treatment approaches to hemophilia care.

hemophilia, it did improve their disease classi cation from severe to mild. Since hemophilia A and B are caused by genetic mutations, the goal of gene therapy is to deliver healthy copies of those genes to the cells in the liver that produce clotting factor. The desired result is better clotting factor activity to protect against bleeding. Now that some gene therapies for hemophilia have been approved by the Food and Drug Administration (there is one approved for hemophilia A and two for hemophilia B, with another hemophilia A gene therapy in development), more and more men like Bill and Dave are contemplating gene therapy.




“If you’re having difficulty with infusions or problems with breakthrough bleeding, it’s a natural segue to talking about gene therapy.”
Nicoletta Machin, D.O


Choosing to undergo gene therapy is no small decision, and experts and patients say it’s a highly personal choice. It should include conversations with your healthcare team about treatment goals as well as considerations such as disease severity, time commitment, and lifestyle impacts.
Nicoletta Machin, D.O., a hematologist at the Hemophilia Center of Western Pennsylvania in Pittsburgh, says she starts the conversation with patients by talking about what is and isn’t working for them right now. “We evaluate how well someone is doing on current therapy,” she says. “If you’re having difficulty with infusions or problems with breakthrough bleeding, it’s a natural segue to talking about gene therapy.”
A conversation like this is what led Dave down the road to gene therapy. “Part of my motivation for getting gene therapy was that I’ve always hated infusing myself, and I’ve never been great at it,” he says. “Plus, I saw my uncle dealing with the increased difficulty of administering prophylactic treatments well into his 80s. I didn’t want to go through that.”
For people who are interested in gene therapy, the process can take months or even years. First, patients must undergo several steps of medical and psychosocial evaluation to determine whether they are qualified. Physicians examine the person’s overall health and coexisting conditions, while social workers assess patients to ensure they have a strong support network. Preparing for gene therapy may require some lifestyle changes, too, such as abstaining from alcohol and committing to the use of contraception for at least six months after infusion.
The run-up to therapy is a good time to ask questions and parse the information you receive. “Gene therapy could be a lifelong change,” says Denise Lowery, LCSW, a social worker at the UC Davis Hemostasis and Thrombosis Center in Sacramento, California. “I sit down with patients and take them through every stage one step at a time.”
Gene therapy for hemophilia is delivered as a one-time infusion, administered
at a hemophilia treatment center in an hourlong procedure. A delivery vehicle, called an adeno-associated virus (AAV) vector, brings a working copy of the defective gene to the patient’s liver. This gene tells the body to produce the missing clotting factor protein. After gene therapy, the recipient still has hemophilia, but this treatment can significantly reduce or end the need for prophylactic factor replacement. “From the evidence we have, many people have sustained factor levels for years after gene therapy,” Machin says. “Hemophilia can become a very small part of your life. It’s a really incredible thing.”
On the other hand, there’s no guarantee that the therapy will eliminate the need for prophylaxis, says Steven Pipe, M.D., medical director of the Pediatric Hemophilia and Coagulation Disorders Program at the University of Michigan in Ann Arbor. “There is a pretty wide range of outcomes that different people can experience, so it’s important that patients are aware of the possibility that they may not get good gene expression or lose expression for various reasons and have to return to prophylaxis,” he says. Some people who undergo gene therapy will still require factor before major surgeries and after injuries.
Bill considers the treatment to have been worthwhile no matter what the future holds. “If the e ects of gene therapy went away tomorrow, well, at least I had a pretty good run of eight years,” he says. Bill was one of the first clinical trial patients to undergo gene therapy in 2016. “I was kind of doing it for science, letting them learn about it. I gured it sounds like they are anticipating good success, so I’ll give it a shot.”
If you’re considering gene therapy, the best decision-maker is you, says Kat Molitor, MSN, R.N., a clinical nurse specialist at the Indiana Hemophilia & Thrombosis Center in Indianapolis. “The landscape of healthcare is changing for the better toward patients being considered the experts on their life,” she explains. “They know what is right for them and their lifestyle. It’s important to involve the individual as the expert on their own lived experience.”


Gene therapy is currently available only to men age 18 or older who have moderately severe or severe hemophilia and who are receiving routine prophylaxis; have a history of lifethreatening bleeds; or have repeated serious spontaneous bleeds.
In addition, patients need to undergo tests to confirm their eligibility. One test involves checking for preexisting immunity or neutralizing antibodies to the AAV vector that delivers the working copy of the gene to the liver. “We’re using recombinant vectors as the delivery vehicle, but they share similarities with naturally occurring AAV viruses. Although they don’t typically cause any human disease, we get exposed to these viruses from early childhood all the way through adulthood,” Pipe says. “And depending on how these antibodies can cross-react against these vectors, it could have some implications for whether someone is eligible for the therapy or whether it might have some sort of adverse impact on their outcome.”
Liver health is another consideration. “Because the treatment targets the liver, we need to make sure that a patient’s liver

“We need to make sure that a patient’s liver is in good enough health to receive the therapy.”
Steven Pipe, M.D.



is in good enough health to receive the therapy,” Pipe says. Since roughly a third of adults with hemophilia are dealing with legacy issues related to HIV and hepatitis C, which can damage the liver, patients must undergo blood tests and liver scans to evaluate their liver health.
“Having a history of liver problems or chronic infections doesn’t mean you are automatically excluded,” Machin says. “There is a process for evaluating your health to determine if it is a barrier or not.”
In Dave’s case, before the gene therapy trial, he took part in a clinical trial that successfully cleared his hepatitis C infection, making him eligible for gene therapy.
Once a person has cleared the eligibility requirements, the actual infusion day is somewhat anticlimactic. The gene therapy is given as a one-time infusion into a vein
with a needle, which takes about an hour. Patients stay at the center for at least three hours afterward to monitor vital signs and watch for possible reactions.
“Some people have a mild reaction, like itching around the IV site or just a sensation that something isn’t quite right,” Machin says. “We can provide medication to support patients through those kinds of reactions.”
Bill and Dave say their infusion days were relatively uneventful, without any reactions that patients sometimes have.
“For me, gene therapy has been kind of like the Seinfeld drug, because it’s a drug about nothing,” Dave jokes. “After you get it, it’s not like some big spectacular thing happens. Nothing happens. You just don’t bleed. But in the end, that’s pretty spectacular.”
Gene therapy is expensive, with a price tag of about $3 million. So, people often ask, “How can I pay for it?” Here’s what you need to know :
1.
Given that the lifetime cost of treating hemophilia can often exceed $20 million, gene therapy could ultimately save insurance companies money. “My record was $768,000 of product in one year, and there’s got to be guys out there who can beat that,” says gene therapy recipient Bill Maurits. “So it’s easy to see why gene therapy can save money.”
2.
Ryan Faden, director of patient access at the National Bleeding Disorders Foundation, says the big unknown is how long the effects of gene therapy will last. “The longer the durability, the more cost-effective the gene therapy treatment would be for payers,” he says. Some manufacturers and insurers are making “ad hoc arrangements,” Faden says, so that if someone doesn’t have a lasting response, the health insurance plan would receive a rebate.
3.
Your provider or social worker can help you navigate the payment process. In addition, manufacturers have set up departments called hubs to guide patients through the process of obtaining coverage.
The hard work begins in the days immediately after the infusion, Pipe says, “because we have to make sure that patients keep up with regular monitoring so they have the best chance of ending up with a good outcome.”
Patients in the clinical trials underwent a vigorous monitoring process. Dave recalls that the first 12 weeks after the infusion were particularly intense. “You’re getting blood drawn at least twice a week, and it can be a lot of blood,” he says. However, now that the therapy is approved, blood draws occur less frequently — typically once a week for the rst three months.
In addition to checking factor levels and looking for signs that the body is having a reaction to the treatment, regular bloodwork is also needed to monitor liver function. In some patients, gene therapy can cause elevated liver enzymes, Pipe says.
“In all of the clinical trials, this hasn’t resulted in any dysfunction of the liver, and if we weren’t doing the monitoring, patients wouldn’t have any idea that these biomarkers were going up in their blood,” he says. But it’s important to monitor patients, he says, because early gene therapy research showed that when patients had elevated liver enzymes, it sometimes caused a decline in, or even a complete loss of, expression of the gene.
“These elevated liver enzymes occur fairly early after receiving the therapy, usually between week four and week 12, and sometimes up to week 20,” Pipe
says. “So, it’s in that first six months after receiving the treatment that we’re doing the most intensive monitoring.” (Neither Bill nor Dave developed this complication.)
If liver enzymes are found to be above a critical threshold, the patient must take oral corticosteroids (such as prednisone) for anywhere from six weeks to several months. “Being on prednisone daily for several weeks has some consequences, including mood swings, stomach irritation, increased blood pressure, weight gain, and a redistribution of body fat, all of which will resolve after you come off the steroids. But patients have to at least be prepared for all of that,” Pipe says.
Because alcohol can have a toxic effect on the liver and potentially interfere with the therapy’s long-term effectiveness, people who undergo gene therapy for hemophilia are usually advised to limit or avoid drinking alcohol for at least six months after treatment, and ideally longer.
Another precaution involves sexual activity. Because the gene therapy vector can stay in semen for some time a fter the infusion, men are advised to use an effective form of contraception with their partners for at least six months.
Over the long term, gene therapy patients are encouraged to continue to visit their HTC, Pipe says. “Even though you might be liberated from the need for regular prophylaxis, you may still have legacy issues related to your hemophilia, such as joint disease and possibly residuals from HIV and hepatitis C,” he says. “And the HTC is there to care for you holistically.”
“Since having gene therapy, I’ve calculated that I’ve been able to avoid more than 270 treatments, so I’m pretty happy with it.””
Dave Robinson
















From regular visits to the treatment center for infusions to sharing lifestyle tips on forums, people with hemophilia have built a community that knows what it’s like to live with a bleeding disorder and can support others.
“This community understands the importance of being there for each other,” says Lucy Ramirez, LCSW, a social worker at Rush Hemophilia and Thrombophilia Center in Chicago. So, if you undergo gene therapy and no longer have bleeding symptoms, do you still belong in the bleeding disorders community?
Yes, Ramirez says. “A person still has a bleeding disorder even if their factor levels change because of treatment,” she explains. “You have lived through it and made lasting relationships, and if you want to continue to be a part of the community, you can.”
People who’ve had gene therapy can be a vital resource for others who are weighing their options. “Someone who has lived with severe hemophilia and undergone gene therapy can contribute their experiences,” Ramirez says.
“Along with a social worker, a person who knows the ups and downs of managing their disease and undergoing treatment is probably one of the best resources to help other people make the decision to undergo gene therapy, walk them through the process, and manage that transition.”
Bill Maurits says he isn’t worried about fitting in. “Hemophilia may have shaped me, but it doesn’t define me,” he says.

Tim participated in the BEQVEZ clinical study. He was compensated for sharing his story. His words and opinions are his own. BEQVEZ is not approved for use in females.

Discuss BEQVEZ with your doctor







Please see Important Facts on page C3.











































































































































Receive BEQVEZ infusion STEP 3: Confirm your eligibility


































Below you will see an overview of the BEQVEZ treatment journey and post-infusion monitoring
BEQVEZ is a one-time gene therapy used for the treatment of adults with moderate to severe hemophilia B who are receiving routine prophylaxis, or have a current life-threatening bleed or a history of life-threatening bleeds, or have repeated serious spontaneous bleeds.
Before treatment with BEQVEZ, your healthcare professional will conduct a blood test to check for neutralizing antibodies to the AAVRh74var virus. The results of this testing will help determine if you may receive BEQVEZ.
Before receiving BEQVEZ, tell your healthcare professional about all your medical conditions, including if you: Have kidney or liver problems, including hepatitis; have factor IX inhibitors or a history of factor IX inhibitors; have an active infection.
For eligible adults with moderate to severe hemophilia B

If you are an adult male with moderate to severe hemophilia B, you may be wondering if BEQVEZ is an option for you. To find out, the first step is to discuss BEQVEZ with your doctor. Together, you can decide if BEQVEZ is a good choice for you and your treatment goals.
You may want to discuss:
What goals are most important to you when choosing a treatment?
What are your short- and long-term plans after treatment?
Are you able to commit to potential temporary lifestyle changes?
To find out if BEQVEZ is right for you, you and your doctor will talk about considerations like potential lifestyle changes. You will also need lab testing to see if you’re eligible for BEQVEZ and confirmation of your insurance coverage.
Your doctor will check your eligibility with various tests to confirm if BEQVEZ may be a treatment option for you. These tests include, but are not limited to, checking your liver health, checking for factor IX (FIX) inhibitors, and seeing if you have any neutralizing antibodies (NAbs) to BEQVEZ. Your care team will talk to you about your results and whether BEQVEZ is right for you.
Your doctor will get the results from your NAb test after about 7 to 10 days.
IMPORTANT SAFETY INFORMATION (cont’d)
BEQVEZ may cause serious side effects, including: Increased Liver Enzymes. Most patients treated with BEQVEZ developed elevated liver enzyme levels and most did not experience any symptoms. Your healthcare professional will monitor liver enzymes and factor IX activity levels before administration of BEQVEZ and frequently following the administration to detect and identify possible elevations in liver enzymes and to monitor your response to BEQVEZ. Your doctor may prescribe a corticosteroid for the treatment of elevated liver enzymes.
On the day of your infusion, you should plan to spend all day at the gene therapy infusion center. This includes preparation time for your infusion. You may need to fill out some paperwork. The process before, during, and after the infusion may vary across centers.
The infusion takes about 1 hour
After the infusion, you’ll stay at the infusion center for at least 3 hours for monitoring
• Your care team will check your vital signs, like your heart rate and temperature
• They will also check if you have an infusion-related reaction
• When your care team is sure you are ready to leave the infusion center, you can go home
Your care team will give you a follow-up plan to routinely monitor your liver and factor IX (FIX) activity levels.
It will be important to see your care team routinely for post-infusion monitoring.
You will have blood tests to assess your liver health and FIX activity levels, which are done 1 or 2 times a week in the first 4 months after receiving BEQVEZ and lessen over time.
In the clinical trial for BEQVEZ, some participants had raised liver enzyme levels and/or a decrease in FIX activity levels. Depending on their levels, these participants were prescribed corticosteroids.
Your care team will also remind you about:
• Limiting alcohol during the first year after the BEQVEZ infusion
• Not donating sperm, being abstinent, or using a male condom for the first 6 months after your infusion
Your doctor may talk with you about enrolling in a registry to assess the long-term efficacy and safety of treatments for hemophilia.
Limit alcohol consumption during the first year following BEQVEZ infusion, as alcohol may reduce the effect of BEQVEZ and may increase liver enzyme levels.
Infusion reactions, including hypersensitivity and severe allergic reactions (anaphylaxis) may occur. Alert your healthcare professional right away if you get any symptoms of hypersensitivity, which may include but are not limited to low blood pressure, fever, heart palpitation, nausea, vomiting, chills, or headache.

After the infusion, when do you need to have scheduled follow-ups?
Your care team may suggest that you visit the same lab for all your tests. This may help minimize any potential variability in results. You can also speak to your doctor and nurse who may be able to help guide you to resources and tools after your BEQVEZ infusion.
YEAR 1
WEEKS 1-16
WEEKS 17-18
WEEKS 19-52
YEAR 2 TO END OF YEAR 3
YEAR 4 TO END OF YEAR 6
Once or twice every week Once every week
At Weeks 24, 32, 42, and 52
Once every 3 months
Once every 6 months
Once every year AFTER YEAR 6
Tim, who received the BEQVEZ infusion in 2021

” Since BEQVeZ, I’Ve had ZEro rEgrE ts and ZEro BlEeds”*
About Tim:
• Diagnosed with severe hemophilia B as a baby
• Lives an active life traveling with his band
• Before BEQVEZ, needed FIX prophy infusions 2 times per week and sometimes needed on-demand treatment for breakthrough bleeds
• Now, he’s living life prophy free
*60% of participants (27 out of 45) had zero bleeds during the efficacy evaluation period. While on routine FIX prophy, 29% of the same participants (13 out of 45) had zero bleeds in the lead-in period.
Individual results and duration of effect may vary. It is not possible to predict who will respond and how long the treatment response will continue.

Pfizer GeneTogether is here to help provide personalized support throughout your BEQVEZ journey. If you and your doctor decide BEQVEZ is the right treatment choice for you, your care team will work with you to enroll you in Pfizer GeneTogether.
The program includes:
• Information and resources to support you before, during, and after treatment
• Dedicated Patient Case Managers ready to answer questions you may have about the planning needed to receive BEQVEZ
Your Pfizer GeneTogether care team will help you get ready for your infusion by:
• Assisting you with any travel logistics required for your treatment
• Confirming the date of the infusion and any preparation or planning needed beforehand
• Checking with your care team to make sure you’re all set for your infusion
One-on-one patient support and information is here for you Call 1-855-4BEQVEZ (1-855-423-7839) 9:00 AM to 7:00 PM ET Monday to Friday
(cont’d)
BEQVEZ can insert itself into the DNA of cells in the human body. The effect that insertion may have on those cells is unknown but may contribute to a theoretical risk of cancer. There have been no reported cases of cancer caused by treatment with BEQVEZ.
The most common side effect of BEQVEZ is increased liver enzymes. These are not all the possible side effects of BEQVEZ. For more information, ask your healthcare professional.
Talk to your healthcare professional before receiving any vaccinations if you are taking a corticosteroid.
Talk to your doctor about any medications you plan to take including over the counter medications, herbal supplements, and vitamins as certain substances can affect the liver and may reduce the effectiveness of BEQVEZ.
Your healthcare professional will test your factor IX activity levels and for factor IX inhibitors.
After receiving BEQVEZ, your doctor will discuss whether and when you are able to stop prophylaxis, if you need to resume prophylaxis, and actions you may need to take for surgeries, procedures, injuries, and bleeding events.

What is BEQVEZ used for?
BEQVEZ is a one-time gene therapy used for the treatment of adults with moderate to severe hemophilia B who are receiving routine prophylaxis, or have a current lifethreatening bleed or a history of life-threatening bleeds, or have repeated serious spontaneous bleeds.
Before treatment with BEQVEZ, your doctor will conduct a blood test to check for neutralizing antibodies to the AAVRh74var virus. The results of this testing will help determine if you may receive BEQVEZ.
Women, patients under the age of 18 years, patients with hypersensitivity to factor IX replacement product, and patients with a history of or active factor IX inhibitors should not take BEQVEZ.
What should I tell my healthcare provider before my BEQVEZ infusion?
Tell your doctor about all your medical conditions, including if you:
• Have kidney or liver problems, including hepatitis
• Have factor IX inhibitors or a history of factor IX inhibitors
• Have an active HIV infection
• Have hypersensitivity to factor IX replacement product
What warnings should I know about BEQVEZ?
BEQVEZ may cause increased liver enzymes. Most patients treated with BEQVEZ developed elevated liver enzyme levels and most did not experience any symptoms. Your doctor will monitor liver enzymes and factor IX activity levels before administration of BEQVEZ and frequently following the administration to detect and identify possible elevations in liver enzymes, to monitor your response to BEQVEZ, and to test for the development of inhibitors. Your doctor may prescribe a corticosteroid for the treatment of elevated liver enzymes.
Infusion reactions, including hypersensitivity and severe allergic reactions (anaphylaxis) may occur. Alert your doctor right away if you get any symptoms of hypersensitivity, which may include but are not limited to low blood pressure, fever, heart palpitation, nausea, vomiting, chills, or headache.
BEQVEZ can insert itself into the DNA of cells in the human body. The effect that insertion may have on those cells is unknown but may contribute to a theoretical risk of cancer.
What are the side effects of BEQVEZ?
The most common side effect of BEQVEZ is increased liver enzymes. This is not the only possible side effect of BEQVEZ. For more information, ask your doctor.
What should I avoid after my BEQVEZ infusion?
Limit alcohol consumption during the first year following BEQVEZ infusion, as alcohol may reduce the effect of BEQVEZ and may increase liver enzyme levels.
Do not donate blood, organs, tissues, or cells for transplantation following administration of BEQVEZ.
Males should not donate sperm and should use a male condom or not have sexual intercourse for up to 6 months after receiving BEQVEZ.
What else do I need to know after I receive my BEQVEZ infusion?
Your doctor will test your factor IX activity levels and for factor IX inhibitors.
Your doctor will discuss whether and when you are able to stop prophylaxis, if you need to resume prophylaxis, and actions you may need to take for surgeries, procedures, injuries, and bleeding events.
Patients and caregivers should ensure proper handling of any materials that have come into contact with the patient’s urine, feces, saliva, mucus, or semen in the first 6 months after BEQVEZ infusion.
Talk to your doctor about any medications you plan to take including over-the-counter medications, herbal supplements, and vitamins as certain substances can affect the liver and may reduce the effectiveness of BEQVEZ and may increase the risk of serious liver reactions.
Talk to your doctor before receiving any vaccinations if you are taking a corticosteroid.
Ask your doctor or pharmacist. This is only a brief summary of important information. For full Prescribing Information, go to BEQVEZ.com.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.







Tim participated in the BEQVEZ clinical study. He was compensated for sharing his story. BEQVEZ is not approved for use in females.



























Known safety profile, studied since 2017
* Individual results and duration of e ect may vary. The main BEQVEZ study is ongoing to assess the long-term e icacy and safety of BEQVEZ. On-demand FIX may still be required.
Scan the QR code to sign up now at BEQVEZ.com Get emails with educational tools and materials to help support you on your BEQVEZ treatment journey
Please see Important Facts on page C3.

You are encouraged to report negative side e ects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.






































































































































































A one-time infusion may help your body make its own factor IX (FIX)
O ers a chance of bleed protection without the need for FIX prophylaxis*

































BEQVEZ is FDA approved as a one-time gene therapy infusion for eligible adults with moderate to severe hemophilia B
BEQVEZ is a one-time gene therapy used for the treatment of adults with moderate to severe hemophilia B who are receiving routine prophylaxis, or have a current life-threatening bleed or a history of life-threatening bleeds, or have repeated serious spontaneous bleeds.
Before treatment with BEQVEZ, your healthcare professional will conduct a blood test to check for neutralizing antibodies to the AAVRh74var virus. The results of this testing will help determine if you may receive BEQVEZ.
Do not donate blood, organs, tissues, or cells for transplantation following administration of BEQVEZ. BEQVEZ is not intended for administration to women. Males should not donate sperm and should use a male condom or not have sexual intercourse for up to 6 months after receiving BEQVEZ.
Patients and caregivers should ensure proper handling of any materials that have come into contact with the patient’s urine, feces, saliva, mucus, or semen in the first 6 months after BEQVEZ infusion.