
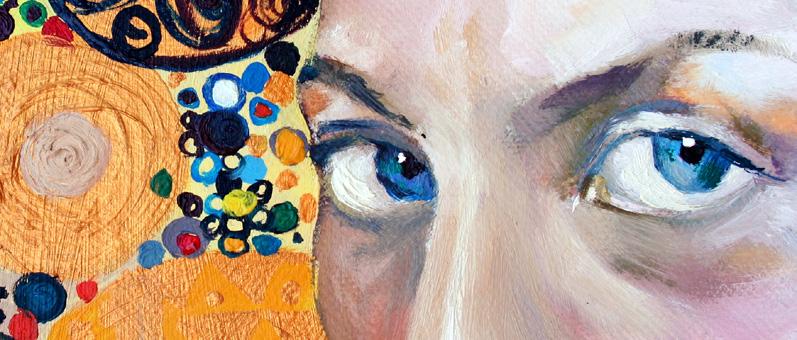
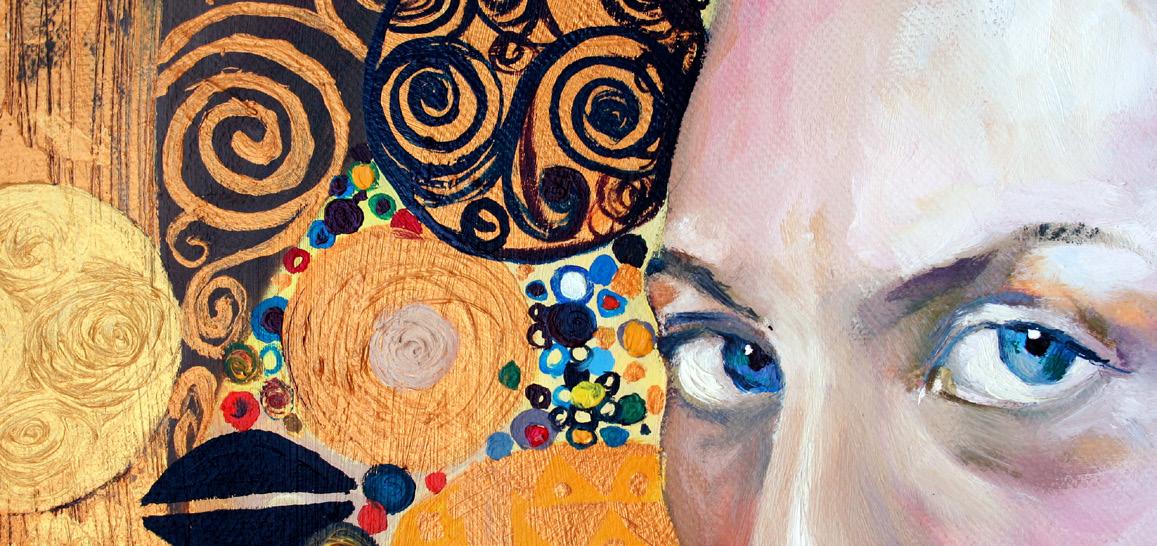
THE WORLD’S FIRST FUNKY OPHTHALMOLOGY MAGAZINE and the Art of Patient Counseling The Subjective Side of Surgery p18 THE ART ISSUE May 2020 piemagazine.org 13 13 Cover Story
nAMD DME RVO
EYLEA® is indicated for adults for the treatment of neovascular (wet) age-related macular degeneration (AMD), visual impairment due to macular edema secondary to retinal vein occlusion (branch RVO or central RVO), visual impairment due to diabetic macular edema (DME), and visual impairment due to myopic choroidal neovascularization (myopic CNV).



REFERENCES: 1 EYLEA® approved package insert Singapore March 2019, Bayer (South East Asia) Pte Ltd. 2. Wells JA, Glassman AR, Ayala AR, et al. Aflibercept, bevacizumab or ranibizumab for diabetic macular edema: two-year results from a comparative effectiveness randomized clinical trial. Ophthalmology. 2016;123:1351-1359 3 Korobelnik JF, Do DV, Schmidt-Erfurth U et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology 2014;121:2247-2254. 4 Eleftheriadou M, Gemenetzi M, Lukic M, et al. Three-year outcomes of aflibercept treatment for neovascular age-related macular degeneration: evidence from a clinical setting. Ophthalmol Ther. 2018;7:361-368. 5 Pielen A, Clark WL, Boyer DS, et al. Integrated results from the COPERNICUS and GALILEO studies. Clin Ophthalmol. 2017;11:1533-1540.
ABBREVIATED PRESCRIBING INFORMATION
EYLEA SOLUTION FOR INJECTION IN VIAL 2MG. Approved name(s) of the active ingredient(s) One ml solution for injection contains 40 mg aflibercept. Each vial provides a usable amount to deliver a single dose of 50 µl containing 2 mg aflibercept. Indication EYLEA is indicated for the treatment of neovascular (wet) age-related macular degeneration (AMD), macular edema secondary to retinal vein occlusion (branch RVO or central RVO), diabetic macular edema (DME) and myopic choroidal neovascularization (myopic CNV). Dosage Regimen wAMD: The recommended dose for EYLEA is 2 mg aflibercept, equivalent to 50 µl. EYLEA treatment is initiated with one injection per month for three consecutive doses, followed by one injection every two months. Based on the physician’s judgement of visual and/or anatomic outcomes, the treatment interval may be maintained at two months or further extended, such as with a treat-and-extend dosing regimen, where treatment intervals are increased in 2- or 4- weekly increments to maintain stable visual and/or anatomic outcomes. If visual and/or anatomic outcomes deteriorate, the treatment interval should be shortened accordingly to a minimum of two months during the first 12 months of treatment. There is no requirement for monitoring between injections. Based on the physician’s judgement the schedule of monitoring visits may be more frequent than the injection visits. Treatment interval greater than 4 months between injections have not been studied. Branch RVO or central RVO: The recommended dose for EYLEA is 2 mg aflibercept, equivalent to 50 microliters. After the initial injection, treatment is given monthly until visual and/or anatomic outcomes are stable. Three or more consecutive, monthly injections may be needed. The interval between two doses should not be shorter than one month. If there is no improvement in visual and anatomic outcomes over the course of the first three injections, continued treatment is not recommended. If necessary, treatment may be continued and the interval may be extended based on visual and/or anatomic outcomes (treat and extend regimen). Usually, monitoring should be done at the injection visits. During treatment interval extension through to completion of therapy, the monitoring schedule should be determined by the treating physician based on the individual patient’s response and may be more frequent than the schedule of injections. DME: The recommended dose for EYLEA is 2 mg aflibercept, equivalent to 50 microliters. EYLEA treatment is initiated with one injection per month for five consecutive doses followed by one injection every two months. There is no requirement for monitoring between injections. After the first 12 months of treatment with EYLEA, and based on visual and/or anatomic outcomes, the treatment interval may be extended, such as with a treat-and-extend dosing regimen, where the treatment intervals are gradually increased to maintain stable visual and/or anatomic outcomes; however there are insufficient data to conclude on the length of these intervals. If visual and/or anatomic outcomes deteriorate, the treatment interval should be shortened accordingly. The schedule for monitoring should therefore be determined by the treating physician and may be more frequent than the schedule of injections. If visual and anatomic outcomes indicate that the patient is not benefiting from continued treatment, EYLEA should be discontinued. Myopic CNV: The recommended dose for EYLEA is a single intravitreal injection of 2 mg aflibercept, equivalent to 50 microliters. Additional doses should be administered only if visual and anatomic outcomes indicate that the disease persists. Recurrences are treated like a new manifestation of the disease. The monitoring schedule should be determined by the treating physician based on the individual patient’s response. The interval between two doses should not be shorter than one month. Method of administration Intravitreal injections must be carried out according to medical standards and applicable guidelines by a qualified physician experienced in administering intravitreal injections. Following intravitreal injection patients should be instructed to report any symptoms suggestive of endophthalmitis (e.g., eye pain, redness of the eye, photophobia, blurring of vision) without delay. Each vial should only be used for the treatment of a single eye. Contraindications Hypersensitivity to the active substance aflibercept or to any of the excipients, active or suspected ocular or periocular infection, active severe intraocular inflammation. Special warnings and special precautions for use Endophthalmitis, increase in intraocular pressure, immunogenicity, systemic adverse events including non-ocular haemorrhages and arterial thromboembolic events. As with other intravitreal anti-VEGF treatments for AMD, the safety and efficacy of Eylea therapy administered to both eyes concurrently have not been systematically studied. When initiating Eylea therapy, caution should be used in patients with risk factors for retinal pigment epithelial tears. The dose should be withheld and treatment should not be resumed earlier than the next scheduled treatment in the event of: a decrease in best-corrected visual acuity (BCVA) of ≥30 letters compared with the last assessment of visual acuity; a subretinal haemorrhage involving the centre of the fovea, or, if the size of the haemorrhage is ≥50%, of the total lesion area. The dose should be withheld within the previous or next 28 days in the event of a performed or planned intraocular surgery. EYLEA should not be used in pregnancy unless the potential benefit outweighs the potential risk to the foetus. Women of childbearing potential have to use effective contraception during treatment and for at least 3 months after the last injection of aflibercept. Undesirable effects Very Common: Conjunctival hemorrhage, eye pain. Common: Retinal pigment epithelial tear, detachment of the retinal pigment epithelium, retinal degeneration, vitreous haemorrhage, cataract (cortical, nuclear, subcapsular), corneal erosion, corneal abrasion, intraocular pressure increased, vision blurred, vitreous floaters or detachment, injection site pain, foreign body sensation in eyes, lacrimation increased, eyelid edema, injection site hemorrhage, punctate keratitis, conjunctival hyperemia, ocular hyperemia. For a full listing of precautions and undesirable effects, please refer to the full product insert. For further prescribing information, please contact: Bayer (South East Asia)Pte Ltd. 2 Tanjong Katong Road #07-01 Paya Lebar Quarter 3 Singapore 437161. Date of revision of text March 2019.
Bayer (South East Asia) Pte Ltd
2, Tanjong Katong Road #07-01, Paya Lebar Quarter 3, Singapore 437161. Tel: +65 496 1888 Fax: +65 6496 1491 Website: www.bayer.com
PP-EYL-SG-0054-1(09/19)
ded dosing1–5
TRE A T W I T H Achieve uns










Matt Young CEO & Publisher Robert Anderson Media Director Hannah Nguyen Production & Circulation Manager Gloria D. Gamat Chief Editor Brooke Herron Editor Ruchi Mahajan Ranga Project Manager Writers Andrew Sweeney April Ingram Chow Ee-Tan Joanna Lee Hazlin Hassan Konstantin Yakimchuk Khor Hui-Min Olawale Salami Sam McCommon Tan Sher Lynn Graphic Designer Maricel Salvador Media MICE Pte. Ltd. 6001 Beach Road, #19-06 Golden Mile Tower, Singapore 199589 Tel: +65 8186 7677 Fax: +65 6298 6316 Email: enquiry@mediamice.com www.mediaMICE.com Asia-Pacific Vitreo-retina Society Vitreo-Retinal Society - India All India Ophthalmological Society IN THIS ISSUE... We are looking for eye doctors who can contribute articles to PIE magazine. Interested? Let's talk! Send us an email at enquiry@mediamice.com. To place an advertisement, advertorial, symposium highlight, video, email blast, or other promotion in PIE magazine contact CEO Matt Young at matt@mediamice.com. The Lowdown on Inherited Retinal Degenerative Diseases Finding Fulfillment as a Female Ophthalmologist Posterior Segment Enlightenment 28 Advances in the Treatment of Agerelated Macular Degeneration Drug Delivery to the Posterior Segment: What’s in the Pipeline? Diabetic Retinopathy: Treatment Management Updates Spotlight on Central Serous Chorioretinopathy Gazing into the Future of Retina Decoding the Challenges and Opportunities in Artificial Intelligence Shedding Light on the Latest Diagnostics and Treatment for Uveitis Impact of Systemic Medications on Retinal Function Retinal Imaging for Early Diagnosis and Patient Management Innovation Conference Highlights 07 26 30 12 10 14 16 23 26 36 38 40 Banana Man... PIE Man... Whatever you Call Me: I Have Coronavirus (COVID-19) 18 Cover Story The Subjective Side of Surgery and the Art of Patient Counseling m a g a z i n e p os terior s e gment nnovation en ightenment PUBLISHED BY SOCIETY FRIENDS
I’m Still Alive and Changed Forever






Infected with COVID-19, for Ophthalmology










































































































Iwas slow to pick up on the story, until I became the story.
Sitting in the hospital bed in Da Nang, infected with coronavirus (COVID-19), I was processing several events at once, any of which would be a full load to consider.




Due to my underlying history with asthma, there was a chance I’d become a severe case — possibly fatal. I had been experiencing breathlessness at night.
But once I came to terms with that, wherein I held neither a positive nor negative outlook, I simply tried to hold a neutral outlook. I was here in the moment . . . for a moment that seemed to have no length of time . . . and I could get to other things.

I thought about family, of course, and how they were doing. I had a huge outpouring of support from friends, especially in our industry, which brought me closer than ever to our field. The communication was ongoing and intensive . . . lots of video chatting and pacing in circles counterclockwise between four walls. Never clockwise.
The hospital didn’t allow chairs, so for 21 days I propped up my contaminated pillow against the bed wall, opened my laptop, and dove in. Keeping busy in hospital isolation while sick with a disease of global attention, and with the outcome unknown, was the same as keeping sane.
At first, my thoughts went to the incredible journey I had been on with my colleague Robert Anderson
throughout India, Africa and Europe as part of our worldwide media tour. I had always dreamed of doing a European road trip, and we did it really well — though upon landing back home in Vietnam I became the boy in a bubble. What a difference 24 hours makes.
My mind, essentially, was still in business mode. Matt the CEO was still here and was following up with friends and contacts from the road trip.
The truth was, business was at a sudden standstill — I just didn’t quite realize it yet. Given how much effort we put into our “tri-continental” media tour, I think I wasn’t ready to accept it.
It had been one month since we made the transition from quarterly magazines to a regular online presence at piemagazine.org and cakemagazine. org. Still in business mode, I hadn’t given much thought to editorial. We were still more than a month away from publishing our next ebook issues of PIE and CAKE magazines.
And yet, with business grinding to a halt — and in an isolated, quiet environment — Matt the CEO suddenly thought a little more deeply and became once again Matt the journalist.



















It dawned on me that the pandemic may well be the story of our lives. I’ve asked multiple people now: Bigger than 9/11? Oh yeah, without hesitation.
We’re also in the healthcare industry as media, and so that fact started hitting particularly hard. I was in hospital quarantine being looked after by heroic doctors and nurses in Vietnam who were


LETTER TO READERS
“My mind, essentially, was still in business mode. Matt the CEO was still here and was following up with friends and contacts from the road trip.”
| May 2020 4
putting themselves at risk. What could I possibly do at this time to help?
Well, although I’ve become a good salesman over the years as a necessity (being the founder and CEO of Media MICE, you have to be able to sell your ideas), journalism is much closer to my core. It is what I went to graduate school for at Northwestern. I majored in English (always funny to me, as that’s also my native language anyway). And, I’m a dramatic person, so I always love a good story.
As publisher of PIE and CAKE magazines, I always had a hand in the editorial. But with magazines, you are essentially filling out pages with solid content for print (and some online) distribution. Your distribution is essentially guaranteed through your print quantity and some blasts. Digital media is different because it’s all about eyeballs and how you can make a reader come to you digitally.
one digital story a week to begin with, on both piemagazine.org and cakemagazine.org. That was out the window. We would have to ramp up immediately with more intensive COVID-19 coverage. We were in a unique position to: report from Asia, where it all started; report globally on it as we are present in both East and West; explain what’s happening in our unique voice; do it all with really cool, funky multimedia (articles, videos, gifs, jpgs, animations — the best of online reporting technology, and we’re just getting started); and be really social and connected about it all on LinkedIn and Facebook. We also could understand and explain with more authority than most, as I was infected. Our industry and its patients would benefit from our critical information and voice at this time. And so we dug in and investigated quickly, finding stories from potentially coronavirus-infused corneas to the ocular side effects of a potential COVID-19 fighting drug: hydroxychloroquine.
Near the end of my hospital quarantine, I also realized that our new media journey would include considerable multimedia. So, while nurses were asking me to pack up and get ready to leave, I was still staying on the line with Dr. Ken Fong, president of the Malaysian Society of Ophthalmology, for a few more minutes of interviewing.
It was odd that after all the timelessness of quarantine where the clock never seemed to make a difference, I was suddenly out of time.

to print at conferences and engage delegates directly with our editorial. Our magazines remain unique in the industry — no question — and they will return. So for now, please help support by perusing our e-books.

Matt the reporter is back. The last time I was so fierce, I was the youngest American reporter on the trail of Lee Boyd Malvo, the Washington D.C. sniper in the early 2000s. I’ll never forget breaking a news story back then about Mr. Malvo, once caught, having an allergic reaction in prison from the vegetarian loaf he was fed. Served him right, I guess.
I do also remember breaking a few news stories within ophthalmology in the early 2000s, namely: 1) The drawbacks of the LADARVision system at the time (Sorry Alcon, had to do it, but you have better stuff now); 2) first reporting out TLSS (Transient Light Sensitivity Syndrome) related to femtosecond lasers, which some financially incentivized ophthalmologists were sitting on as “no big deal”. . . a lot was written on it after, though; and 3) my very first ophthalmology story ever was explaining why certain lot numbers of microkeratome blades were causing diffuse lamellar keratitis in 2003.





Do I still like breaking news? You bet I do.


I hope you’re ready for me, ophthalmology! I’m back . . . and also, new and improved!

A little after mid-March when I was diagnosed with coronavirus, I swung into action in my bed and started planning and executing the reporting.
First, I thought, I’m sure many in our industry would want to know what the coronavirus experience was like. I tried to explain my personal journey with the disease — both symptoms and how it made me feel emotionally — over a 3-part series. You can still read those at piemagazine.org
Secondly, we were planning on having




























































































































































































































Since then I’ve continued to do many, many interviews all over the world with executives and KOLs in ophthalmology from home quarantine, where I presently am. We call the video series “Q&A from Quarantine.” I hope it helps to aid in a worldwide sharing of information among some high-level thinkers both in industry and practice, so that we can come together and learn from our collective challenging experiences.
And of course, we still publish our PIE and CAKE magazine ebooks. We believe it’s important to keep the format going, as there will still be a time to return
CEO, Publisher & REPORTER, PIE and CAKE magazines Matt Young
| May 2020 5
And so the old gears of a reporter’s mind starting cranking. We are quite possibly in the most significant story of our lives. It is in the healthcare industry, which we cover. I am at one epicenter of the disease. Like everyone else doing their part in the crisis, I need to do what I was trained to do. I need to do my core job.
Dr. Cheung currently serves as deputy head and senior consultant of the medial retina service for Singapore National Eye Centre (SNEC), as well as senior clinician investigator for the Singapore Eye Research Institute (SERI). Her research interests include the study of risk factors and clinical features of macular diseases that may be unique in Asian populations.

Dr. Cheung has published more than 150 articles, mostly regarding age-related macular degeneration, including polypoidal choroidal vasculopathy, and conducted several clinical trials in anti-vascular endothelial growth factor therapies. Dr. Cheung has also been actively involved in training and education, and has served as an instructor on Asia-Pacific Academy
of Ophthalmology (APAO) and American Academy of Ophthalmology (AAO) courses and many other educational programmes. In addition, she is also a volunteer faculty member for the ORBIS Flying Eye Hospital Programme.
Dr. Cheung has received a number of prestigious awards, including the Macula Society Young Investigator Award (2017), APAO achievement award (2017), APAO Nakajima Award (2014), APAO Outstanding Service in Prevention of Blindness Award (2013), the Bayer Global Ophthalmology Research Award (2012), the Roper-Hall Medal (2005) and the Elizabeth Hunt Medal (Royal College of Ophthalmologists, UK).
gemmy.cheung.c.m@singhealth.com.sg
Prof. Gillies presently holds a number of positions including: director of research and director of the Macula Research Group for the Save Sight Institute; foundation fellow for the Sydney Medical School; professor in the Department of Clinical Ophthalmology at the University of Sydney; head of the Medical Retina Unit at the Sydney Eye Hospital; deputy chair for the Ophthalmic Research Institute of Australia; and director of Eye Associates in Sydney.
Prof. Gillies has served as a principal investigator or associate investigator in more than 70 clinical trials, and his research regarding macular degeneration and drug safety and efficacy has been published in 188 journals. He has also received a number of grants to study treatments for age-related macular degeneration, retinal disease and Muller cell dysfunction
– among other treatments and studies. Prof. Gillies has also appeared in national media on numerous occasions, including the evening news of all major networks, on ABC radio as a local expert, as well as in print media.

His dedication and research has resulted in multiple awards. Most recently, he received Gerard Crock trophies for the best papers at the Royal Australian and New Zealand College of Ophthalmologists (RANZCO) Annual Scientific Meeting (2013 and 2015), an achievement award from the Asia-Pacific Academy of Ophthalmology (APAO) in 2014, and an achievement award from the American Academy of Ophthalmology (AAO) in 2015.
mark.gillies@sydney.edu.au
Dr. Gupta currently serves as a professor of ophthalmology at Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh in India. Throughout her career, she has completed original work in the fields of intraocular tuberculosis, optical coherence tomography, diabetic retinopathy, and fungal endophthalmitis. In addition, she is actively studying vitreoretina and uveitis diseases.

She has been published in 65 per-reviewed journals, and has authored 17 book chapters and four complete books. Dr. Gupta also holds a US patent for the development of
multiplex PCR for uveitis. In addition, she is a sought after speaker, and has made more than 350 presentations in various national and international meetings.
Dr. Gupta has received several awards for her work, including the first JN Pahwa award from the Vitreo Retinal Society of India, the first NA Rao Award from the Uveitis Society of India, and the first NA Rao award from All India Ophthalmological Society (AIOS).
vishalisara@yahoo.co.in
| May 2020 6
Dr. Gemmy Cheung
Prof. Mark Gillies
ADVISORY BOARD MEMBERS
Dr. Vishali Gupta
The Lowdown on the Latest

in Inherited Retinal Degenerative Diseases

 by Konstantin Yakimchuk
by Konstantin Yakimchuk
Inherited retinal degenerative diseases (IRDD) are a spectrum of retinal pathologies which includes age-related macular degeneration (AMD), retinitis pigmentosa (RP), Leber congenital amaurosis (LCA), choroideremia, Stargardt disease (SD), Usher syndrome and achromatopsia.
Characterized by heterogeneous mutations, these pathologies can lead to progressive deterioration of photoreceptor cells accompanied by severe vision impairment. Among them — AMD, which manifests with severe vision failure in the central part of the retina — remains one of the main causes of visual dysfunction.1
According to Dr. Shalesh Kaushal, a highly experienced ophthalmologist practicing in Florida (USA), the most common retinal disease that any ophthalmologist observes is AMD.
There are genetic susceptibilities to AMD, said Dr. Kaushal: “In the USA, the incidence of AMD varies from 8 to 30% in people over 65 years old. Worldwide, AMD has a prevalence of about 8.7%.” As for other retinal diseases, Stargardt disease shows a prevalence of 1 in 8,000 to 1 in 10,000; retinitis pigmentosa 1 in 3,500 to 1 in 4,000; and choroideremia 1 in 50,000 to 1 in 100,000.
While breakthroughs in anti-VEGF dosing regimens are changing the landscape in AMD treatment, there are no specific drug therapies for the other inherited retinal degenerative diseases at this time. Dr. Kaushal emphasized that although that is the case, it is an exciting time for the development of treatment of these retinal diseases because of the confluence of molecular genetics and biochemistry in elucidating the triggering pathogenetic events leading to the various IRDDs. “Besides drugs, stem cell and gene therapy approaches are also being developed,” he shared.
Retinitis Pigmentosa
Retinitis pigmentosa (RP) represents a complex group of retinal dystrophies characterized by the degeneration of photoreceptor cells and the detachment of the retinal epithelium. Visual acuity declines during the late stages of RP. Nextgeneration sequencing has recently identified various mutations associated with RP. In particular, mutations of

RETINOPATHIES POSTERIOR SEGMENT
| May 2020 7
RPGR, EYS, PRPF31 and USH2A are present in almost half of RP patients.2 Several clinical trials are underway to test novel gene therapy approaches. In particular, a recent study aims to investigate the efficacy of AAV-based vector carrying the full-length RPGR protein.3
Leber Congenital Amaurosis (LCA)
The severe decline of vision and degeneration of retinal cells are the main characteristics of a number of inherited dystrophies called LCA. The subtypes of LCA are caused by mutations of different genes, such as RPE65. Several clinical trials for the treatment of LCA have been initiated by Spark Therapeutics (PA, USA) using voretigene neparvovec (AAV2-hRPE65v2), an AAV-based vector.4 The results of the study have demonstrated the positive effect of AAV2-hRPE65v2 on retinal function in RPE65-related LCA.
Choroideremia
Choroideremia, an X-linked retinal disease, is characterized by progressive deterioration of both the retina and choroid. The symptoms include pigmentary pattern, focal atrophy and vascular changes.5 With regard to diagnostic imaging, OCT may show decreased thickness of the outer nuclear layer and increased pigmentation in the later stages of the disease. With regard to the gene therapy of choroideremia, the AAV2REP1 vector, which includes enhancing WPRE sequence, has already been implemented in clinical trials.6
Stargardt Macular Dystrophy

Stargardt disease (SD) is an autosomal recessive degenerative disease. Several IRDDs, such as Stargardt macular dystrophy (or SD), autosomal recessive retinitis pigmentosa and fundus flavimaculatus are caused by mutations in the ABCA4 gene. The modifications of ABCA4 protein leads to the accumulation of lipofuscin, damaging retinal photoreceptor cells and the retinal pigment epithelium (RPE). A recent study has presented
a comprehensive analysis of ABCA4 polypeptides and concluded that mutations of the C-terminal domain of ABCA4 induce RDD.7 The main clinical features of SD include the decline of central vision and the appearance of foveal lesions. A recently initiated clinical trial aims to test the efficacy of SAR422459, lentivirus-based vector.8
Usher Syndrome and Achromatopsia
Both Usher syndrome and achromatopsia belong to the group of autosomal recessive IRDDs. Usher syndrome is characterized by sensory deterioration of both auditory and visual sensory systems. The genes affected in patients with Usher syndrome, are involved in the regulation cell motility and adhesion.9 Since some causative genes for this disease are very large, it might be difficult to guarantee their efficient delivery. However, animal studies have already shown promising results regarding gene delivery. In particular, the significant expression of USH2A proteins in retinal cells in a mouse model was achieved using AAVbased vector with inserted a rhodopsin kinase promoter.10
In contrast to Usher syndrome, achromatopsia affects the visual system only. Its symptoms include pronounced nystagmus, photophobia, declined visual acuity and diminished color vision. This disease is caused by mutations in several genes involved in the regulation of the cone phototransduction.11 The therapeutic approaches of gene replacement were tested in mouse models and demonstrated recovery of cone-related visual acuity.12
Other Therapies for IRDDs
In addition to gene therapy, tauroursodeoxycholic acid, which has previously been shown to improve the course of neurodegenerative disorders caused by oxidative stress, might potentially be effective for IRDDs.13 Subcutaneous injection of tauroursodeoxycholic acid protected cone loss and visual deterioration in a mouse model of retinal degeneration. Furthermore, recent research in animal
models has shown the efficacy of cell therapies to stimulate RPE or to supply viable nutrients to photoreceptor cells.14


Dietary Recommendations for Patients with IRDDs
According to Dr. Kaushal, since the retina is a sensitive barometer of health and nutrition there are some foundational dietary recommendations. In particular, he emphasized daily multi-vitamin supplements containing B-complex and at least 1,000 to 2,000mg of omega-3 is highly advised. Fish oil, such as krill oil and especially cod oil, is also beneficial. Furthermore, 5 to 7 servings per week of dark green vegetables (such as kale, broccoli, spinach, Brussel sprouts, collard greens, Swiss chard or asparagus) and 5 to 7 servings of dark fruits (like blueberries, blackberries, pomegranate, plums or cherries), are highly recommended for patients with IRDDs. In addition, beets, arugula and cilantro would help strengthen blood vessels and enhance blood flow.
However, there are also some foods that should be avoided. Dr. Kaushal suggested eliminating white flour, white sugar and fried and processed foods, and to minimize white rice. Moreover, artificial sweeteners should be avoided and replaced with stevia, cinnamon or xylitol. In addition, low-glycemic and gluten-free foods are preferred. In line with these recommendations, a recent study has reported that adherence to the Mediterranean diet is associated with a 41% reduced risk of AMD. 15
The Future of Treatment
Over the last few decades, significant progress has been achieved in deciphering the genetic basis of IRDDs. For example, dietary restrictions are highly recommended for patients with IRDDs. Although no adequate treatment for IRDDs exists, several gene therapy techniques have been developed and successfully tested in animal models and in a few clinical trials. The future clinical studies will focus on the development of effective systems of gene delivery without adverse side effects.
RETINOPATHIES POSTERIOR SEGMENT
| May 2020 8
References:
1 Handa JT, Bowes Rickman C, Dick AD, et al. A systems biology approach towards understanding and treating non-neovascular age-related macular degeneration. Nat Commun. 2019;10(1):3347.
2 Birtel J, Gliem M, Mangold E, et al. Next-generation sequencing identifies unexpected genotype-phenotype correlations in patients with retinitis pigmentosa. PLoS One. 2018;13(12):e0207958.
3 Martinez-Fernandez De La Camara C, Nanda A, Salvetti AP, et al. Gene therapy for the treatment of X-linked retinitis pigmentosa. Expert Opin Orphan Drugs. 2018; 6(3): 167–177.
4 Russell S, Bennett J, Wellman JA, et al. Efficacy and safety of voretigene neparvovec (AAV2-hRPE65v2) in patients with RPE65-mediated inherited retinal dystrophy: a randomised, controlled, open-label, phase 3 trial. Lancet. 2017; 390(10097): 849–860.
5 Aleman TS, Han G, Serrano LW, et al. Natural History of the Central Structural Abnormalities in Choroideremia: A Prospective Cross-Sectional Study. Ophthalmology. 2017;124(3):359-373.
Contributing Doctor
D r. Shalesh Kaushal obtained his B.S. from Yale University in Molecular Biophysics and Biochemistry. Subsequently, he completed his M.D. at Johns Hopkins and Ph.D. at MIT, with Nobel Laureate Dr. Har Gobind Khorana. Following his Ph.D., he completed his residency at the Doheny Eye Institute/USC Department of Ophthalmology and his surgical retina fellowship at the Washington University St. Louis/Barnes Retina Institute. While at the University of Florida, he was the Richardson II Chair and head of the retina division.

INDUSTRY UPDATE
6 Dimopoulos IS, Hoang SC, Radziwon A, et al. TwoYear Results After AAV2-Mediated Gene Therapy for Choroideremia: The Alberta Experience. Am J Ophthalmol. 2018 Sep;193:130-142.
7 Patel MJ, Biswas SB, Biswas-Fiss EE. Functional significance of the conserved C-Terminal VFVNFA motif in the retina-specific ABC transporter, ABCA4, and its role in inherited visual disease. Biochem Bioph Res Co. 2019;519(1):46-52.
8 Parker MA, Choi D, Erker LR, et al. Test-Retest Variability of Functional and Structural Parameters in Patients with Stargardt Disease Participating in the SAR422459 Gene Therapy Trial. Transl Vis Sci Technol. 2016;5(5):10.
9 Mathur P, Yang J. Usher syndrome: Hearing loss, retinal degeneration and associated abnormalities. Biochim Biophys Acta. 2015;1852(3):406-420.
10 Zou J, Luo L, Shen Z, et al. Whirlin replacement restores the formation of the USH2 protein complex in whirlin knockout photoreceptors. Invest Ophthalmol Vis Sci. 2011; 52(5): 2343–2351.
Dr. Kaushal established the clinical and surgical retina division; recruited physicians; trained residents and surgical fellows; and mentored undergraduates, medical students, graduate students and postdocs in his research lab. In 2009, he was recruited to the University of Massachusetts as the chairman to build a new eye center and the first new academic Department of Ophthalmology in the USA in over 25 years. Besides these academic pursuits, he is the founder of three biotech companies and has been a consultant for most of the leading ophthalmic pharmaceutical companies. In 2013, Dr. Kaushal transitioned back to
11 Pascual-Camps I, Barranco-Gonzalez H, Avino-Martinez J, Silva E, H arto-Castano M. Diagnosis and Treatment Options for Achromatopsia: A Review of the Literature. J Pediatr Ophthalmol Strabismus. 2018;55(2):85-92.
12 Pang JJ, Deng WT, Dai X, et al. AAV-mediated cone rescue in a naturally occurring mouse model of CNGA3achromatopsia. PLoS One. 2012;7(4):e35250.
13 Tao Y, Dong X, Lu X, et al. Subcutaneous delivery of tauroursodeoxycholic acid rescues the cone photoreceptors in degenerative retina: A promising therapeutic molecule for retinopathy. Biomed Pharmacother. 2019;117:109021.
14 Ben M’Barek K, Habeler W, Regent F, Monville C. Developing Cell-Based Therapies for RPE-Associated Degenerative Eye Diseases. Adv Exp Med Biol. 2019;1186:55-97.
15 Merle BMJ, Colijn JM, Cougnard-Gregoire A, et al. Mediterranean Diet and Incidence of Advanced Age-Related Macular Degeneration: The EYE-RISK Consortium. Ophthalmology. 2019;126(3):381-390.
Florida to pursue private practice. He has a currently funded research project studying the incidence of diabetic retinopathy in the general population using a novel telemedicine instrument. In 2015, Dr. Kaushal received the prestigious Seelig Research Award from the ACN. He is recognized in Marquis’s Who’s Who in Medicine and Science and nominated by Castel Connolly as a Top Doctor. He has been invited as a speaker throughout the U.S. and internationally.
skaushal@compretina.com
Heidelberg Engineering appoints Christopher Mody as Clinical Director
With more than 30 years of clinical ophthalmology experience in the public sector, ophthalmic scientist Christopher Mody has been appointed to clinical director at Heidelberg Engineering. For the last seven years, Mr. Mody worked for Heidelberg Engineering UK where he was one of the leading figures of the Heidelberg Engineering Academy, raising the standard of imaging education and coordinating numerous significant research projects.
In his new role, Mr. Mody is in charge of facilitating the exchange of scientific information between the global ophthalmic community and Heidelberg Engineering, which works closely with scientists and clinicians to develop ophthalmic solutions. And as clinical director, Mr. Mody will influence the clinical direction of the
entire Heidelberg Engineering product portfolio, as well as the integration of third-party solutions.
The appointment of Mr. Mody further strengthens its ties with the medical community, with the goal of identifying and translating clinical needs into the company’s product management and R&D functions. For example, Mr. Mody will be tasked with further developing and validating an enhanced diagnostic toolbox for early detection and management of glaucoma and employing state-of-theart imaging technologies and traditional parameters to deliver multifaceted clinical evaluation of the disease.
According to Ali Tafreshi, head of product management and clinical affairs at Heidelberg Engineering, Mr. Mody is
ideally suited to support the company’s translational science program, which is designed to deliver comprehensive, clinically relevant solutions to its customers. “His knowledge will continue to strengthen our research alliances, while his passion for education will enhance the company’s role in advancing patient care,” he said.
“When I joined the Heidelberg Engineering UK team, I witnessed daily how the dynamic diagnostic information that our customers obtain empowers them to deliver better care,” said Mr. Mody. “In my new global role, I will devote myself to the exchange of accurate intelligence between the ophthalmic community and our company for the development of innovative solutions that continue to fulfill clinical needs.”
| May 2020 9
Drug Delivery
to the Posterior Segment


What’s in the Pipeline?
 by Tan Sher Lynn
by Tan Sher Lynn
Today, a variety of approaches are available for drug delivery to the posterior segment, each with their own advantages and challenges. These methods include topical, periocular, transscleral, suprachoroidal and intravitreal; with implant, encapsulated cell technology (ECT), pump/port, nano- and microparticle, and composite delivery systems.

The latest information in ocular drug delivery was presented during the session “Update on Drug Delivery to the Posterior Segment of the Eye”, at the 13th Asia-Pacific Vitreo-retina Society Congress (APVRS 2019), held last November in Shanghai, China.
Challenges of Ocular Drug Delivery
Dr. Jennifer J. Kang-Mieler explained that since the MARINA and ANCHOR trials demonstrated monthly intravitreal ranibizumab injections resulted in significant vision gains in age-related macular degeneration (AMD) patients, the use of other anti-VEGF agents (such as bevacizumab and aflibercept) has increased for treating AMD, diabetic retinopathy and occlusive disease. Nevertheless, all anti-VEGF therapies share a common limitation — in order to be effective, a monthly or bimonthly injection is required for the duration of two years, and often longer.
“With the availability of anti-VEGF pharmacological treatments, we can administer monthly/bimonthly intravitreal injections with the knowledge that the great majority of our patients will maintain their current visual acuity and/or show improvement. However, the burden of monthly visits and frequent injections on patients, physicians and the health care system cannot be denied. We need a better way to deliver the treatment,” she said.
Dr. Kang-Mieler continued that a variety of polymeric systems are in development for posterior segment drug delivery, especially for anti-VEGF treatment. However, it remains a big
| May 2020 10
TREATMENT UPDATE POSTERIOR SEGMENT
challenge to achieve a sustained release of anti-VEGF medication. Therefore, she and her team have developed a composite drug delivery system (DDS) that combines aflibercept-loaded microspheres with a thermo-responsive hydrogel, which can release bioactive aflibercept for more than six months.
“In vivo choroidal neovascularization (CNV) rodent model data showed that aflibercept treatment (bolus or DDS) significantly reduced CNV lesion area. The intravitreal concentration of aflibercept was bioactive for six months in non-human primate eyes and there were no significant adverse effects. We concluded that the biodegradable microsphere-thermo-responsive hydrogel system may be a novel DDS to replace repeated anti-VEGF therapy,” she said.
Microneedle Drug Delivery and Suprachoroidal Cannulation

Dr. Wiliam F. Mieler explained that the suprachoroidal drug delivery system consists of the transscleral injection approach, direct catheterization and direct placement of implants.
“Clearside Biomedical developed a micrometer-sized needle and injector that can deliver drug into the suprachoroidal space. Yet, the variation in scleral thickness poses a challenge to safety because questions such as ‘how deep did we inject?’ and ‘in which plane did we inject?’ will arise,” he said.
As for microcatheter suprachoroidal drug delivery, Dr. Mieler noted that it possesses various potential indications, including the treatment of macular edema, AMD and certain forms of uveitis; targeted chemotherapy delivery; and delivery of stem cells. “The microcatheter suprachoroidal approach takes on the benefits of the slow release of corticosteroids (e. g., fluocinolone implant for diabetic macular edema) and avoids the long-term effect on intraocular pressure and the crystalline lens.
“Delivery of various drugs into the suprachoroidal space is certainly a potential delivery system. It is technically feasible with microneedles and/or cannulation . . . it may allow

for improved drug delivery to the posterior segment and avoid some of the current intravitreal complications,” he concluded.
Looking Down the Treatment Pipeline
Next, Dr. Pravin U. Dugel discussed newer anti-VEGFs, including abicipar pegol, brolucizumab and faricimab.
“Faricimab is a very elegantly designed, novel, bispecific antibody that simultaneously binds to and inhibits both vascular endothelial growth factor A (VEGF-A) and angiopoietin-2 (Ang-2) — and is the first bispecific antibody designed specifically for the treatment of retinal eye diseases. Plus, and it has an optimized Fc (fragment crystallizable) region that will increase the systemic clearance and decreases inflammation,” he said.
He noted that there has been a lot of advancement in the treatment of AMD and diabetic retinopathy with the current anti-VEGF drugs. “However, a lot of work remains to be done, and opportunities are present in drugs that are able to achieve better short-term efficacy, better long-term efficacy and better sustainability,” emphasized Dr. Dugel.
He also covered a few novel therapeutics in the pipeline, including GB-102 (Graybug Vision, CA, U.S.); OPT-302 (Opthea, Victoria, Australia); and PAN-01-102 (a topical eye drop that blocks VEGF-C, D and A; PanOptica, NJ, U.S.). Dr. Dugel also discussed gene therapy, which he says is one of the most exciting things happening, as it has the ability to achieve all three objectives of drug delivery (i.e. short-term efficacy, better long-term efficacy and better sustainability).
In summary, intravitreal injections and sustained-release solid implant intravitreal devices are the most common techniques employed at the present time. Advances will continue to occur via new and improved drug delivery techniques, along with development of new therapeutic agents.
Editor’s Note:
The 13th Asia-Pacific Vitreo-retina Society Congress (APVRS 2019) was held in Shanghai, China, on November 22-24, 2019. Media MICE Pte Ltd, PIE magazine’s parent company was the Official Media Partner at APVRS 2019. Reporting for this story also took place at APVRS 2019.
| May 2020 11
Incoming! Drugs to the posterior segment.
Advances in AMD Treatment
by Hazlin Hassan
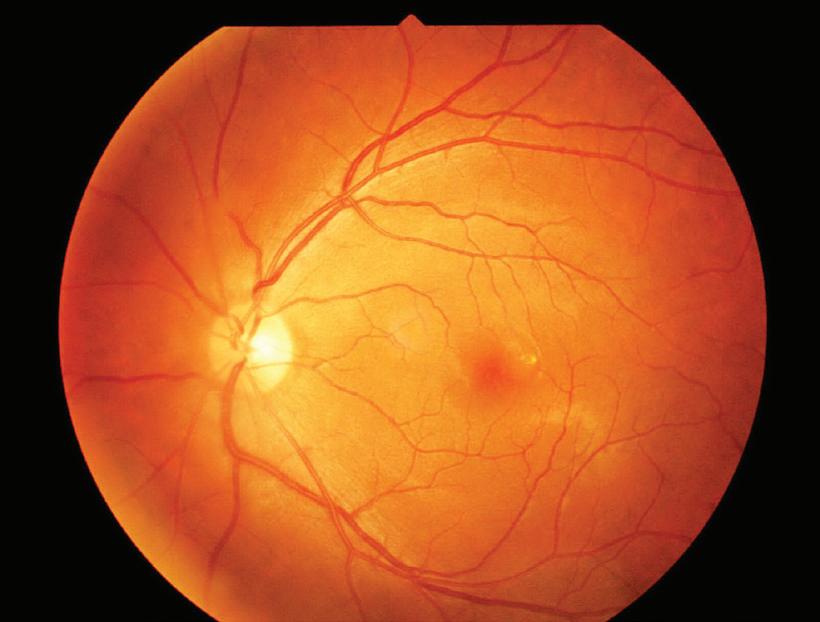
Age-related macular degeneration (AMD) is the leading cause of irreversible vision loss in patients over the age of 50, and can arise from environmental and genetic origins.


Its characteristics include drusen, hyperpigmentation, hypopigmentation of the retinal pigment epithelium (RPE), geographic atrophy and, in some patients, late-stage choroidal neovascularization (CNV).
During the 13th Asia-Pacific Vitreoretina Society Congress (APVRS 2019) last November, speakers from around the world presented on the latest developments in the pathogenesis and treatment of neovascular AMD, including pharmacologic agents, longterm results of the IVAN study, and a possible link to intestinal microbes.
Advances in AMD Imaging
“Exciting recent advances have resulted in changes to the way doctors look at drusen, pigmentary abnormalities, geographic atrophy and CNV,” said Dr. Danny Ng, clinical assistant professor from the Chinese University of Hong Kong.
The 5-year risk of progression from intermediate to advanced AMD is reported to range from 0.5 – 50%. “With such a great variability in this disease prognosis, we need to better define how we can use imaging biomarkers to predict the course of the disease,” he said.
Imaging, notably optical coherence tomography (OCT), can predict the risk of advancing disease; the response to intravitreal anti-VEGF treatment; and helps doctors to better understand the pathogenesis of AMD.
Regression of drusen can be a risk factor for the progression from intermediate to advanced AMD, warned Dr. Ng. A study showed that 82% of patients’ eyes that developed geographic atrophy had preceding drusen regression.
Another study also found that drusen regression preceded geographic atrophy and also preceded the development of CNV. “With structural OCT scans, we are discovering more and more precursors that can lead to the development of advanced AMD,” said Dr. Ng.
These include hyper-reflective foci, reticular pseudodrusen and nascent geographic atrophy.


Healthy Gut, Healthy Eyes?
Gut microbiome, or gut flora, may be linked to AMD, which could have an implication on treatments in the future.
“Each of us carries up to 100 trillion bacteria in our gut, comprising more than 10,000 different bacterial species,” said Dr. Sebastian Wolf, professor of ophthalmology, University Eye Hospital Bern, Switzerland. It plays a very important role for nutrition and in the digestion of food.
But what has AMD got to do with microbiome?
In a small pilot study, involving patients with exudative AMD, significant differences in the abundance in the microbiome constitution were seen in patients with AMD, noted Dr. Wolf.
This shows that there may be a link between the intestinal microbiome and the development of AMD.
| May 2020 12 AMD TREATMENT POSTERIOR SEGMENT
“Our research results have confirmed that the composition of the gut microbiome is altered in patients with neovascular AMD. We know that the composition of the gut flow can be influenced by genetics. There may be a way to modify your risks by modifying your gut microbiome,” he added.
Five-year Results of the IVAN Trial: A Study of Function and Morphology
“Five-year results of a study comparing bevacizumab and ranibizumab found no difference in the treatment efficacy between the two drugs investigated,” said Dr. Usha Chakravarthy, professor of ophthalmology at the Queen’s University of Belfast in Northern Ireland and chief investigator of the Inhibition of VEGF in Age-related choroidal Neovascularisation (IVAN) trial.
The IVAN study*, regarded by the National Institute for Health Research (NIHR) as one of the most important trials of the last decade, enrolled 610 participants with neovascular AMD (nAMD). It closed in October 2012 after all participants completed two full years of follow-up.
INDUSTRY UPDATE
“The two drugs were found to be very equivalent in terms of their visual outcomes and also the treatment regimens were likewise similar in terms of visual outcomes,” said Prof. Chakravarthy.
The study also compared two treatment regimens: continuous monthly treatment and intermittent treatment.
The aim of the IVAN follow-up study, after five years and 537 participants, was to look at macular function and morphology over an extended period of follow-up.
“People who exhibited good vision tended to maintain their good vision, but there was a gradual decline and similarly for all the other layers of visual acuity,” she said. The study also looked at whether changing to the other drug made any difference. All the patients involved in the study went on to ranibizumab at the end of the trial.
“Subsequently, a portion of them switched to aflibercept. So we looked to see whether switching from ranibizumab to aflibercept gave these people an extra edge in terms of outcome. And the
answer is no, those who did not switch, had 59 letters of vision and those who switched, had almost identical visual function. So switching did not make any difference,” explained Prof. Chakravarthy.
To summarize, she said that visual acuity declined slowly over time regardless of the level of best corrected vision at IVAN exit, and treatment switches did not result in better visual acuity outcomes.
* Chakravarthy U, Harding SP, Rogers CA, et al; IVAN study investigators. Alternative treatments to inhibit VEGF in age-related choroidal neovascularisation: 2-year findings of the IVAN randomised controlled trial. Lancet. 2013;382(9900):1258-1267.
Editor’s Note:
The 13th Asia-Pacific Vitreo-retina Society Congress (APVRS 2019) was held in Shanghai, China, on November 22-24, 2019. Media MICE Pte Ltd, PIE magazine’s parent company was the Official Media Partner at APVRS 2019. Reporting for this story also took place at APVRS 2019.
Vitra 2 Laser from Quantel Medical Receives FDA Approval
Quantel Medical’s Vitra 2® laser for retinal photocoagulation recently received approval from the U.S. Food and Drug Administration (FDA). The new laser retains all the benefits of the original Vitra – like reliability, compactness and versatility – and adds a range of improvements and additional functionalities.
“After a successful career spanning more than 13 years, and with more than 3,000 units sold worldwide, Quantel Medical is proud to announce the renewal of its 532nm flagship Vitra photocoagulator,” said Quantel Medical CEO Jean-Marc
Gendre. “We are very excited to bring our new 532nm laser to ophthalmologists and their patients.”
Vitra 2 has a new generation of optimized laser cavity and an increased max power level, as well as new clinically oriented software with an interface that simplifies treatment procedures and doctors’ workflow. It is also now compatible with SingleSpot and MultiSpot technologies.
“Thanks to its flexibility and its ease of use, we are sure that more and more surgeons will embrace the MultiSpot technology delivery mode and its
associated treatments benefits for retinal photocoagulation,” continued Mr. Gendre.
Additionally, the Vitra 2 is compatible with Haag Streit and Zeiss slit lamps and with Quantel Medical YAG and YAG/ SLT lasers. It can also be connected to a wide range of delivery systems, including operating microscopes, laser indirect ophthalmoscopes and laser probes.
The Vitra 2 was launched in Europe in 2018. According to Quantel Medical, the laser has already met its market in the countries where it’s been commercialized.
| May 2020 13
Diabetic Retinopathy
Treatment Management Updates
by Joanna Lee
Recent advances in the management of diabetic macular edema (DME) and proliferative diabetic retinopathy (PDR) were hot symposium topics at the 13th AsiaPacific Vitreo-retina Society Congress (APVRS 2019), held last November in Shanghai, China.
Singapore National Eye Centre (SNEC) Medical Director Dr. Tien-Yin Wong set the stage by presenting an overview of all the major studies for DME — such as RISE & RIDE, ETDRS, DRCR Protocol T, DRCR Protocol V — and how the results of these RCTs could be applied to clinical practices.
Overall, the studies showed that antiVEGFs improved vision with good longterm outcomes (5-year outcome with DRCR.net Protocol I; 3-year outcomes of RESTORE and VIVID/VISTA studies) as opposed to laser treatment. The visual acuity (VA) gain was about 10-12 letters.
For severe DME with poorer vision, aflibercept was shown to be superior; however, for milder DME with good vision, there appeared to be no difference among the agents. Additionally, there seems to be improvement in VA and macular thickness with the use of intravitreal triamcinolone (IVTA) and dexamethasone implant (Ozurdex, Allergan), but the VA gain is inferior to that of anti-VEGFs in clinical trials. “However, steroids are useful for pseudophakic eyes and second- or third-line therapies,” he said.
It may also be beneficial to look at the prognosis, as vision loss may not be only caused by DME — but also by macular atrophy or ischemic maculopathy.
On DME Treatment
Following that, Dr. Jun Kong looked treatment for eyes with center-involved DME and VA of 20/25. He noted the results of Protocol V1 showed no difference in rates of VA loss (one or more lines) at two years among eyes managed with aflibercept, laser or observation. Of those three management strategies (not monotherapies), they found that at two year, eyes with VA of 20/20 (and a proportion of eyes at 20/20 or better) was significantly greater with aflibercept (77%) than observation (66%). However, the proportion of eyes with 20/25 or better was similar in each group (about 85%).
Follow-up was carefully done, with aflibercept initiated in the laser and observation groups if vision decreased by one line at two consecutive visits or more than two lines at one visit; changes on OCT did not spark aflibercept initiation. The primary outcome was a loss of five or more letters, with the reason likely to be clinically relevant in eyes with good vision, and unlikely to be due to chance variations.
To sum up, among eyes with DME and good VA, there was no significant difference in VA loss at two years in eyes that were initially managed with aflibercept, laser photocoagulation or observation. The laser or observation groups were given aflibercept only if VA had worsened.
On Improved Surgical Outcomes for TRD
Surgical outcomes of for diabetic traction retinal detachment (TRD) have been improved, according to



Dr. Masahito Ohji, who talked about management of diabetic TRD. One reason for this is Alcon’s advanced ULTRAVIT Beveled High-Speed probe for microincision vitrectomy surgery (MIVS). This machine provides a closer port proximity to the retina, which allows more access to tissue planes. It also increases the cut speed up to 10,000 cuts-per-minute, while reducing vitreoretinal traction. Having this technology has also improved the understanding of DR’s pathogenesis.
In his meta-analysis of intraoperative and postoperative indices, with and without preoperative administration of anti-VEGF, Dr. Ohji said the results were very positive with very low intraoperative bleeding or frequencies of required endodiathermy. Postoperatively, the general incidence of early VH and VH clear-up time was also very low.
On Pregnancy and Diabetic Retinopathy
Dr. Mae-Lynn Bastion’s presentation, entitled “Diabetic Retinopathy in Pregnancy: A Clear and Present Danger” provides a glimpse of an ongoing investigation into this rarely discussed area of ophthalmic research. Dr. Bastion and her co-investigators embarked on a retrospective study of Malaysian cases of DR in pregnancy, believed to the first study of its kind in the country.
Practitioners often face a dilemma when encountering DR or centerinvolving DME in pregnant patients — risks of harm to the baby2 when administering anti-VEGF injections to
| May 2020 14 DR TREATMENT POSTERIOR SEGMENT
the mother, some of which result in spontaneous abortions.
“There is a lack of clear evidence for administering anti-VEGFs to pregnant women,” she said. From her observations of data thus far, it is vital to perform pre-pregnancy screening of diabetics as early as possible in DR progression. There should be pregnancy testing prior to giving anti-VEGF to young female diabetics; awareness of risk factors for progression in pregnancy; and the condition should be treated as conservatively as possible. “If anti-VEGF treatment is required, try to avoid it in the first trimester of pregnancy,” she said.
On Intraretinal Fluid in DME
As little is known about the significance of intraretinal fluid in DME, Dr. Hyung Chan Kim delved into the correlation of retinal fluid volume with visual and anatomical outcomes after treatment in DME. Following his study on observing
INDUSTRY UPDATE
3D morphologic changes in AMD3, Dr. Kim attempted to analyze the changes in DME as well.
In his presentation entitled, “3D Analysis of Morphologic Changes with Visual Outcome in DME,” he discussed his retrospective, cross-sectional study of 65 eyes of DME patients treated with intravitreal bevacizumab (IVB). The investigated parameters were the baseline fluid volumes and best corrected visual acuity (BCVA), and DRIL (disorganized retinal inner layers), a “robust biomarker for DME”.4 He also looked at other DME biomarkers like OCT patterns, deep capillary plexus (DCP) loss and hyperreflective foci. Treatment response during the study showed 58% of patients had a good response when the central macular thickness was reduced by more than 50 microns after anti-VEGF. The study showed how baseline inner IRF volume correlates with poor visual outcome after treatment, indicating that inner IRF volume could be a biomarker for DME.
References:
1 Baker CW, Glassman AR, Beaulieu WT, et al; DRCR Retina Network. Effect of Initial Management With Aflibercept vs Laser Photocoagulation vs Observation on Vision Loss Among Patients With Diabetic Macular Edema Involving the Center of the Macula and Good Visual Acuity: A Randomized Clinical Trial. JAMA. 2019;321(19):1880-1894.
2 Polizzi S, Mahajan VB. Intravitreal Anti-VEGF Injections in Pregnancy: Case Series and Review of Literature. J Ocul Pharmacol Ther. 2015; 31(10): 605–610.
3 Lee H, Jo A, Kim HC. Three-Dimensional Analysis of Morphologic Changes and Visual Outcomes in Neovascular Age-Related Macular Degeneration. Invest Ophthalmol Vis Sci. 2017;58(2):1337-1345.
4 Sun JK, Lin MM, Lammer J, et al. Disorganization of the retinal inner layers as a predictor of visual acuity in eyes with center-involved diabetic macular edema. JAMA Ophthalmol. 2014;132(11):1309-1316.
Editor’s Note:
The 13th Asia-Pacific Vitreo-retina Society Congress (APVRS 2019) was held in Shanghai, China, on November 22-24, 2019. Media MICE Pte Ltd, PIE magazine’s parent company was the Official Media Partner at APVRS 2019. Reporting for this story also took place at APVRS 2019.
Merger Discussions Begin for Quantel Medical and Ellex
Quantel Medical, a division of Lumibird Group, recently announced that merger discussions have commenced with Ellex. Both ophthalmic medical device companies share the same goal – fighting the major causes of blindness – as well as the same purpose, values and established reputation.
Quantel Medical CEO Jean-Marc Gendre said that “the future success of the both companies depend on the sharing of R&D capabilities and manufacturing structures, and on strengthening our approach to clinical research in order to meet the current and future needs of ophthalmologists”. The French company has a strong emphasis in R&D and a comprehensive portfolio of diagnostic ultrasound, surgical lasers and a range of
disposable products for ophthalmologists.
Meanwhile, Australia-based Ellex designs, manufactures and sells ophthalmic lasers and devices to treat glaucoma and retinal disease (primarily caused by diabetes, secondary cataract and vitreous opacities), as well as age-related macular degeneration.
Together, the complementary strengths of both companies – like strongly branded products and ophthalmic market knowhow – enables them to offer a broader range of products, at all price points, to better meet diverse client needs.
“We can offer clients a more holistic solution,” said Ellex Interim CEO Maria Maieli, adding that Ellex is particularly strong in laser treatment for glaucoma
therapy, while Quantel Medical has a greater influence in laser treatment in retinal disease and diagnosis solutions.
In addition, the strength of Ellex’s market locations is matched and supported by Quantel Medical’s successful distribution channels. The merger will allow both companies to combine their market presence to satisfy existing customer requirements while exploring new markets – making the most of their respective strengths.
“The vision is to become the world leader in ophthalmic ultrasound and laser technology, to diagnosis and treat eye disease,” concluded Marc Le Flohic, CEO for Lumibird Group, one of the world’s leading laser specialists.
| May 2020 15
Central Serous ChorioretinopathySpotlight on

 by Brooke Herron
by Brooke Herron
On the last day of the 13thAnnual Meeting of the Asia-Pacific Vitreoretina Society (APVRS 2019) held in Shanghai, China, delegates attended a symposium on ‘Central Serous Chorioretinopathy’ to explore the spectrum of the condition’s unsolved issues, including the role of the choroid, the relationship with polypoidal choroidal vasculopathy (PCV), as well as diagnostic challenges and treatment options.
Central serous chorioretinopathy (CSC) is the fourth most common ‘wet’ maculopathy, after agerelated macular degeneration (AMD), diabetic macular edema (DME) and retinal vein occlusion (RVO), and in its chronic form, can result in irreversible vision loss and decreased vision-related
quality of life. However, treatment options remain controversial, with photodynamic therapy (PDT) serving as the most promising therapy.

The PLACE Trial
According to Dr. Camiel Boon, professor of ophthalmology at Leiden University Medical Center in the Netherlands, there is a lot of controversy in regard to the classification and treatment of CSC: “That’s because there is a lack of prospective randomized controlled trials; and that is why we conducted the PLACE trial.”

The PLACE trial compared half-dose PDT with high-density micropulse laser (HSML) treatment in patients with
chronic CSC, with the primary outcome focused on anatomical success with the complete absence of subretinal fluid (SRF) on OCT. They found that PDT therapy is more effective than HSML in treatment of chronic CSC, with regard to anatomical success, as well as in functional parameters like BCVA and microperimetry. Dr. Boon noted that “a complete resolution of macular SRF appears necessary for significant BVCA increase”. In addition, the long-term follow-up concluded that recurrences of SRF are less likely in chronic CSC patients successfully treated with half-dose PDT compared to HSML.
“Current evidence strongly suggests that half-dose PDT should be the treatment of choice in chronic CSC:
| May 2020 16
MACULOPATHY POSTERIOR SEGMENT
it’s the most effective and it is safe,” shared Dr. Boon, adding that although observation may be the preferred approach in acute CSC, treatment should be considered in select cases.
The Relationship between CSC and PCV
Dr. Huijun Qi, from the Department of Ophthalmology at Peking University’s People Hospital, China, shared a case from 2008 of a 47-year-old male with impaired vision in the right eye for two weeks, who was diagnosed with CSC in both eyes. “The patient was treated with Chinese medicine and did not return for a second visit,” she said. “Eight years later, the patient came to us again with visual deformation in his left eye.”
At this visit in 2016, the patient was diagnosed with polypoidal choroidal vasculopathy (PCV): “His left eye changed from CSC to PCV,” she shared. The polyp was treated with three antiVEGF injections, plus rescue laser therapy, and then remained stable. Meanwhile, the patient’s right eye showed SRF and abnormal vascular networks – but as the patient had no complaints, his right eye was not treated . . . until 2019, when he returned with loss of vision for one week. “OCT and OCTA showed SRF and polyps in the right eye,” said Dr. Qi. “The right eye changed from CSC to PCV after 11 years.” The patient was treated with three injections of antiVEGF.
She stated that “the development of PCV may be secondary to chronic CSC caused by long-term exudation or non-specific RPE dysfunction.” Dr. Qi also said that CSC is associated with pachychoroid PCV and that patients with chronic CSC should follow-up for a very long time to watch out for progression to PCV.
Multimodal Imaging in CSC
Dr. Bhuvan Channa, vitreo-retina head at the Bharti Eye Hospital Foundation in India, discussed the important of multimodal imaging in CSC diagnosis, as well as how CSC appears in each modality.
For example, fundus fluorescein angiography (FFA) – which is the oldest imaging technique for CSC evaluation – typically shows a single leakage point, or less commonly, multifocal point leaks – which could be localized within or adjacent to the area of SRF in acute CSC. In chronic CSC, multifocal leakage can be seen, resulting in patches of granular or mottled hyperfluorescence in the mid and late phases.
Meanwhile, on SD-OCT, acute CSC is classically seen as a serous macular detachment, while in chronic CSC, RPE degeneration along with shallow SRF and cystoid or schitic retinal edema is seen. Degenerative RPE changes may also be seen all over the macula, which affects vision.
Now, as newer imaging modalities emerge, there could be more in understanding the disease’s pathophysiology. For example, enhanced depth imaging (EDI) and swept source OCT (SS-OCT) have allowed in vivo documentation of RPE-Bruch membrane complex and choroidal vasculature. In acute CSC, fundus autofluorescence (FAF) shows an area of hypoautofluorescence, precisely corresponding to the leakage point noted in FA, in more than 75% of patients.
Dr. Channa noted that the gold standard imaging tool for cases of chronic CSC is indocyanine green angiography (ICGA), showing transient hyperpermeability of choroidal vessels, visible as a multifocal hyperfluorescence, increasing midphase and fading in the late phase. And finally, OCT angiography (OCTA) allows for the detection of occult CNV, which was previously undiagnosed by conventional imaging modalities.
“Multimodal imaging techniques have revolutionized the understanding about the pathophysiology of CSC, the diagnosis, as well as management of this condition,” concluded Dr. Channa. “The role of the choroid in the pathogenesis has been increasingly emphasized by the newer imaging modalities.”
Editor’s Note:
The 13th Asia-Pacific Vitreo-retina Society Congress (APVRS 2019) was held in Shanghai, China, on November 22-24, 2019. Media MICE Pte Ltd, PIE magazine’s parent company was the Official Media Partner at APVRS 2019. Reporting for this story also took place at APVRS 2019.
| May 2020 17
The Subjective Side of Surgery
and the
by Brooke Herron
In art, determining value is largely subjective. Although art can possess objective characteristics such as age, condition or rarity —ultimately, it’s the viewer’s perception that counts.

A quote from famous French artist Edgar Degas says it nicely: “Art is not what you see, but what you make others see.”
Unfortunately for Degas, he suffered from (presumed) progressive retinal disease and eventually lost much of his vision; a study of his art reveals this deterioration. That historical tidbit aside, his quote resonated with us at PIE because ‘making others see’ is also what ophthalmologists do.
There’s also a very important subjective element in ophthalmology: the patient. Their satisfaction with a procedure can impact the overall results, even if objective measures like visual acuity say otherwise. Like in art, it’s the viewer’s perception that counts — and therefore, patient education and counseling are critical components for successful surgical outcomes.
To illustrate the role of patient satisfaction in ophthalmology, PIE spoke with esteemed vitreoretinal surgeons from Singapore and Brazil to paint a portrait of the subjective side of surgery and the art of patient counseling.

| May 2020 18 COVER STORY
Guan, medical director and
ophthalmologist
Broad Brush Strokes of Patient Counseling
“Where the spirit does not work with the hand, there is no art.” — Leonardo da Vinci
Like in art, to create a vitreoretinal masterpiece, all of the elements must come together — the objective (such as evidence of visual improvement or halted disease progression) as well as the subjective (like patient satisfaction).
“Retinal procedures are notoriously unforgiving . . . even a relatively routine procedure can lead to potentially sightthreatening complications,” explained Dr. Au Eong. He believes all retinal procedures require detailed preoperative counseling.

Before surgery, he tries to paint a clear picture of the prognosis: “I always educate patients on the potential benefits and risks of retinal procedures, as well as their success and failure rates, so that they fully understand the implications of undergoing surgery.”
He says this is especially important because of the unpredictability of surgical complications. “I always highlight the possibility that their ocular condition could worsen — including the risk of blindness — even if these risks are very small.”
This open communication builds trust and is the framework for resulting patient satisfaction. “Whatever the surgical outcome, the subjective result is affected by the patient’s expectation and whether the outcome meets this expectation,” shared Dr. Au Eong.
“For this reason, I do not want to unnecessarily heighten a patient’s expectation of a good outcome — this only makes it more difficult to meet or exceed it.”
Instead, he ensures that patients understand that a poor outcome is always a possibility. “In fact, it may be the expected outcome in patients whose conditions have very poor visual prognosis,” said Dr. Au Eong.
or even internal limiting membrane peeling (ILM),” explained Prof. Nakamura. “Even if a patient has good visual acuity and OCT looks okay, we select the better case for surgery and tell them it’s necessary to remove the traction.”
Surgical intervention and earlier traction release, as opposed to observation, was also recommended by Hikichi et al. After observing patients with VMT for five years (without surgery), they found: visual acuity (VA) declined by two or more lines (64%); cystoid changes persisted (67%); and new cystoid changes appeared (17%). In just 11% of cases, there was a spontaneous complete PVD and resolution of VMT.2
Nickname: The Vitreoretinal van Gogh
The Composition of Specific Cases
“The great artist is the simplifier. ” — Vincent van Gogh
Vitreoretinal procedures are complicated. Like a great artist, it’s the surgeon’s job to simplify the explanation to help the patient fully understand their surgery, risks and/or prognosis. Of the different vitreoretinal procedures performed by Prof. Nakamura, he says patients with surface retinal diseases always receive additional counseling.
Vitreomacular traction (VMT) syndrome occurs when there is an incomplete posterior vitreous detachment (PVD), which leaves the vitreous partially attached to the retina. This causes a tractional pull on the macula, resulting in anatomical changes and a decline in vision. VMT is believed to be associated with a broad spectrum of maculopathies, including cystoid macular edema (CME), epiretinal membrane (ERM), and macular hole (MH).1
“These patients might need surgery in both eyes, vitrectomies with epiretinal,
Plus, earlier surgical intervention can translate into better outcomes: “This is especially important in cases where traction is evident and distortions of the ellipsoid zone can be seen on OCT,” said Prof. Nakamura.

Macular holes (MH) are small breaks in the retina which cause blurred or distorted central vision. Additional counseling is recommended in these cases, especially in longstanding or chronic MHs, where the patient may be anxious for improvement. Prof. Nakamura advised that if there is a good indication for surgery, he tells patients that he will do whatever necessary — including considering other treatment options. He also informs patients with long-term MHs that even with surgery, the hole may not close.
Additionally, microperimetry adds value when counseling MH patients. “This is useful in cases where the patient has high expectations (both anatomically and functionally), even if you counseled in advance that the latter might not follow the first,” continued Prof. Nakamura. “Still, we encourage them to get the surgery soon after the diagnosis — it’s better when you diagnose with the early symptoms and act right away,” he said.
In cases of MH, a big part of patient counseling is explaining and evaluating the options. “The more you talk to your patient, the better he reacts . . . and that also gives him a sense of
| May 2020 19
Artist: Dr. Au Eong Kah
senior consultant
at International Eye Cataract Retina Centre, Mount Elizabeth Medical Centre and Farrer Park Medical Centre, Singapore
Nickname: The Renoir of Retina
Artist: Hudson Nakamura, professor at the Eye Bank Foundation of Goiás, Goiânia, Brazil
security,” shared Prof. Nakamura.
Diabetic tractional retinal detachment (TRD) is the most advanced form of diabetic retinal disease. Prof. Nakamura said that diabetic retinopathy (DR) patients — especially those with TRDs — require a gentle approach, but sometimes it has to be aggressive.
“When the macula is threatened by a TRD simulating vitreomacular traction syndrome . . . but also a vascularized one in a proliferative case, we know that the more difficult the traction, the more difficult it will be to split the fibrotic or epiretinal component from the retina itself,” he explained. “That might require retinotomies apart from the peeling itself. Plus, a double peel of ILM and ERM might be necessary to relieve traction.”
He continued: “Sometimes the detachment comes with too many vascular tufts — and though that makes the surgery demanding, it’s still possible to relieve the traction and spare the macula. Usually theses surgeries end up with silicone oil, and the vision won’t be great — so, this needs to be explained to the patient and their family.”
Do you see what I see?
“Art is meant to disturb, science reassures.” — Georges Braque
Occasionally, objective and subjective outcomes disagree: For example, in cases where anatomical results look good (sometimes even great), but the patient does not see improvement, or is unhappy with the procedure. This is exactly where patient satisfaction can impact overall results.
Prof. Nakamura has experienced this scenario in a patient with VMT. “[Postoperatively] the anatomic result was awesome . . . but the vision stayed the same — actually, it dropped a bit. So, at the beginning, the patient felt that the procedure didn’t help much, even though the surgery went well.”
So, what happened? After some followup appointments, the patient concluded that even though his vision slightly worsened, overall, he was glad he had the surgery. “The surgery prevented the condition from worsening in the shortor long-term,” said Prof. Nakamura. “Patients with previous tractions see that the traction is no longer there, and the floaters are gone . . . then they realize the procedure was successful.”
This clash of outcomes is one area where technology can help. “Microperimetry and OCT can objectively report pre- and postoperative results . . . and even help make decisions,” he explained. “When a patient isn’t satisfied, showing them the evolution from before to after surgery can help improve satisfaction . . . and
Discovering the ‘Art of Ophthalmology’
“Bring your humanity to your art. Bring your art to humanity.” — Maxime Lagacé
If the patient’s eye is the canvas, the art of ophthalmology begins long before the doctor picks up his instruments (or paintbrush) – and the aesthetic begins at that first appointment. Prof. Nakamura says this gradual relationship built from pre- to post-op is an ‘art of ophthalmology’.
“You see each patient . . . he’s your partner on the other side, even a part of your medical family,” he shared. “And when the results appear, you become a doctor for the referral of future patients — but you
it helps the patient know that they’re being taken care of.”
Sculpting Improved Outcomes
“An artist should never be a prisoner of himself, prisoner of style, prisoner of reputation, prisoner of success, etc.” —
Henri Matisse
How can an artist positively influence his audience’s feelings toward a particular piece? That’s a good question . . . and probably one to be debated with art scholars finer than us at PIE. Fortunately, doctors can help influence patients’ feelings toward surgery . . . and their satisfaction with the outcome.
In fact, a 2019 study ranked provider attitude, along with technical competence, accessibility and efficacy as the key attributes for patient satisfaction.3
Therefore, it’s key to establish a good doctor-patient relationship. A big part of this is trust: “It’s about offering the options and never hiding what could be done . . . this helps a lot,” said Prof. Nakamura, adding that he discusses recent statistics and scientific papers with patients, too.
It’s also important that patients understand the risks of surgery. “I usually explain the pros and cons for
may never achieve this if you don’t interact with the patient. It’s about building the relationship . . . it’s not merely work.”
There is also a certain art in capturing images and editing surgical videos — the visual representation of ophthalmology that speaks the artist’s language of lines, shapes, values (or contrast), colors and space.
“From taking the first OCT picture, to the footage from the operating room, and turning that into a visual case study, I really like doing that myself,” said Prof. Nakamura.
| May 2020 20
COVER STORY
Contributing Doctors
undergoing the procedure and the chances for a desired outcome . . . but I emphasize that there could be a long wait, and in some cases, the outcome could be worse,” he shared. “Many times, the patient and their family will decide the best option. Once they understand, we go ahead and do what’s best and necessary.”
Subjective Impressions are Valuable
“I put my heart and my soul into my work and have lost my mind in the process.” — Vincent van
Gogh
Of course, all doctors want their patients to be satisfied — or beyond that, happy — with surgical results. Not only do patients’ subjective feelings impact clinical outcomes and compliance, they can also affect loyalty and referrals.3
Direct referrals from previous patients (or word-of-mouth) can be hugely beneficial to the bottom-line. “For us, it’s the main driver for the growth of our patient load . . . it’s the best advertisement and it’s free!” said Dr. Au Eong.
Prof. Nakamura agreed: “Patients listen to other patients who have similar diseases and they do a great job spreading the news,” he said, adding that it’s even better when other doctors and specialists compliment your work via the patient. “When that comes back to you, you’re happier and convinced that you’ve done the right procedure.”
To encourage positive reviews, Prof. Nakamura explained that a good attitude, communication and trust with the patient is vital. “Talk positively with your patient and go see them. I see patients from different places (teaching institutions, private practice) and in the postoperative period, they want to see you, they want to personally ask you questions,” he said. “This is why I accompany my residents and fellows to see private clinic patients, they don’t do it alone. The answers we provide during these appointment helps erase their doubts.”
Dr. Au Eong said that to help ensure referrals, they strive to give patients the most pleasant experience possible. “We make sure our staff pays extra attention to the needs of every patient. Our goal is to take the patient on a comfortable and hassle-free journey from the moment they step through our doors, to when they leave our clinic,” he shared. “All of the staff plays his or her part, from the receptionist to the optometrist and, of course, the ophthalmologist.”
References:
1 Bottós J, Elizalde J, Arevalo F, Rodrigues EB, Maia M. Vitreomacular Traction Syndrome. J Ophthalmic Vis Res. 2012; 7(2): 148–161.

2 Hikichi T, Yoshida A, Trempe CL. Course of vitreomacular traction syndrome. Am. J. Ophthalmol. 1995;119(1):55–61.
3 Ng JHY, Luk BHK. Patient satisfaction: Concept analysis in the healthcare context. Patient Educ Couns. 2019;102(4):790-796.
Dr. Au Eong Kah Guan is medical director and senior consultant ophthalmologist at International Eye Cataract Retina Centre in Mount Elizabeth Medical Centre and Farrer Park Medical Centre, Singapore. He was previously head and senior consultant in the Department of Ophthalmology & Visual Sciences in Alexandra Hospital and Jurong Medical Centre; deputy director and head of research in The Eye Institute, National Healthcare Group; and adjunct associate professor in the Department of Ophthalmology, Yong Loo Lin School of Medicine, National University of Singapore. Dr. Au Eong graduated from the National University of Singapore with a Bachelor of Medicine and Bachelor of Surgery in 1989 and a Master of Medicine (Ophthalmology) in 1995. He is a fellow of the Royal College of Surgeons of Edinburgh, the Royal College of Physicians and Surgeons of Glasgow, and the Academy of Medicine in Singapore. He is also a diplomat and member of the Royal College of Ophthalmologists in London. His current areas of practice include vitreo-retina, cataract and comprehensive ophthalmology.
aekg@eyecataractretina.com
Prof. Hudson Nakamura is an ophthalmologist specializing in retina and vitreous. He did his vitreoretinal disease fellowship at the University of Toronto, Canada, and another retinal fellowship in his hometown city, Goiânia, Brazil at the CBCO – Brazilian Center for Eye Surgery.
Prof. Nakamura completed his study from the School of Medicine at the Federal University of Goiás and residency from the Base Hospital of the Federal District, Brasília, Brazil. He has been a member of industry organizations including the American Academy of Ophthalmology, Brazilian Council of Ophthalmology, Canadian Society of Ophthalmology and the Association for Research in Vision and Ophthalmology. He is currently working as a professor in the Department of Retina and Vitreous Course of Medical Residency in Ophthalmology and Fellowship in Vitreoretinal Diseases.
hudson.nakamura@gmail.com
| May 2020 21
Can art training improve ophthalmologic observational skills?
Although observation and description are critical to practicing ophthalmology, medical education does not provide explicit training in these areas. As a result, students are often criticized for deficiencies in both skills. Therefore, Gurwin et al. evaluated the effects of formal visual art observation training on general and ophthalmologic observational skills of medical students.
Participants & Methods:
Control
No observation sessions were attended
Art Training
Attended 6 custom-designed, 1.5-hour art observation sessions over a 3-month period.
Both groups underwent pre-and post-testing on works of art, retinal pathology images and external photographs of eye disease.
Observational skills significantly improved in the Art Group:
Conclusion
These results led the authors to conclude that art observation training for first-year medical students can improve clinical ophthalmology observational skills: “Principles from the field of visual arts, which is reputed to excel in teaching observation and descriptive abilities, can be successfully applied to medical training.”
| May 2020 22
Retinal & External Eye Images (combined) 36.4 PRE TEST 30.4 POST TEST −5.9 MEAN CHANGE PRE TEST POST TEST +12.8 MEAN CHANGE 35.1 47.9 * Gurwin J, Revere KE, Niepold S, et al. A Randomized Controlled Study of Art Observation Training to Improve Medical Student Ophthalmology Skills. Ophthalmology. 2018;125(1):8-14. +19.1 MEAN CHANGE −13.5 MEAN CHANGE PRE TEST 70.9 POST TEST 90.0 PRE TEST 65.8 POST TEST 52.3
Gazing into the Future of Retina
by Joanna Lee
What does the future hold for retina treatments?
Ophthalmologists discussed this, and other exciting developments in retina, during the 78th Annual Meeting of the All India Ophthalmological Society (AIOC 2020) in Gurugram, India, held earlier this year.
On C-test Scores
To clinically standardize an ordinal measure of monocular tritan discrimination, Dr. Ross Littlewood has developed the C-test1 for blue and yellow contrast. The test consists of 10 novel pseudoisochromatic plates, each displaying a target with two blue/ yellow contrast borders and difficulty increasing from plates 1 to 10. The score is based on the last correctlyidentified plate.
The C-test is based on his observations of the koniocellular subsystem, which has several clinical benefits: It’s helpful in diagnosing amblyopia where only parvocellular signals are blocked, however, C-tests would show up as normal because koniocellular signals remain normal.
“This is useful where loss of vision occurs in someone without a welldocumented history,” said Dr. Littlewood. Another application is ascertaining retinal ischemia and edema. Ischemic situations (like advanced diabetic retinopathy) have
a worse prognosis if tritan contrast is low.
“A very low C-test score is predictive measure of someone who has got both ischemia and edema, like in central retinal vein occlusion (CRVO).” Last, it is helpful in determining optic neuritis. The C-test is currently available for purchase.
On Optic Nerve Regeneration Transplants
Will optic nerve regeneration (or transplants) become a reality in the next ten years, or remain as science fiction? Prof. Rajvardhan Azad, president of the India ROP Society, had a chance to find out.
Prof. Azad participated in an eyeball transplantation project headed by Zhongshan Ophthalmic Center’s Director Dr. Yizhi Liu and his team from Zhongshan University (Guangzhou, China). During his presentation, he provided a glimpse of this preliminary study, which reconnected the optic nerve after transection in an animal model.
From the transplant, they identified two barriers to optic nerve regeneration: the BDNF (or brain derived neurotrophic growth factor) that prevents ganglion cells from going into apoptosis; and the CSPG (chondroition sulphate proteoglyutein) in the glial scar, which is an antibody to inhibit
oligodentrocytes.
Other than barriers, they have also identified promoters of optic nerve regeneration such as beta-tubulin m-RNA in ganglion cells; bcl-2 (B-Cell Lymphoma 2) proto oncogene for ganglion cells regeneration in vitro; and matrix metalloproteinase, identified as a molecule essential for regeneration to foster a receptive transplant environment in eye and CNS tissue. Further investigation is ongoing and Prof. Azad expects this to become a reality within 10 to 15 years.
On Surgical Robotics
Surgical robotics have been increasingly used in orthopedics, gastroenterology and neurology. But what about vitreoretinal surgery (VR)?
“The driving force behind the development of robotics in VR surgery has been AI, deep learning and OCT-imaging,” said Dr. Rajiv Raman, during his presentation titled “Robotic Vitreous Surgery Possibilities and Expectations.” In June 2019, the Preceyes Surgical System (PSS) R1.1 to assist surgeons in vitreoretinal procedures received its CE approval. A month before that, the first ever robotic VR surgery was performed in the United Kingdom.
Robotic approaches in ophthalmology have been broadly seen in three areas. 2 First, as an assistive hand held device; the robot works as a smart surgical tool and is manually operated by the surgeon to augment surgical capabilities, such as with tremor filtering or to improve static tasks like drug delivery. It works as a co-manipulator in surgical tasks, such as retinal vein cannulation. Separate robotic manipulators (to which instruments can be attached), are used in motion-controlling by surgeons. Cataract surgeries can even be done remotely through telemanipulation.
“The sensors in the instruments will also increase our safety in surgical performance. The future of VR surgery is actually robotic surgery . . . and it will find applications within the many steps of our routine vitreoretinal procedures,” he concluded.
| May 2020 23
AI TOOLS IN RETINA INNOVATION
On Retinal Plugs
Dr. Ajay Aurora presented his innovative investigation into “Retinal Plug for Retinal Hole in Retinal Detachment.” He shared the fibrin glue used in VR surgery 3 could be a promising technique for the treatment of uncomplicated rhegmatogenous retinal detachment (RD), leading to early visual recovery and requiring no postoperative positioning, while avoiding the usual problems of gas or oil tamponade.
He also foresaw an exciting future for retina plugs made with glue that can be “locked” to rivet a hole, gluing the retina to the RPE. His vision of future retinal plugs involves RD surgeries using the “glue plug.”
On OCTRAR
In another exciting development, Dr. Anand Rajendran presented on “Augmented Reality — GenNext in Retinal Imaging (OCTRAR),” in collaboration with a team from the Indian Institute of Technology (IIT), Madras.
OCTRAR stands for Optical Coherence
Tomography Reconstruction and visualization in Augmented Reality (AR). It provides a novel way to reconstruct a 3D model from OCT images and OCT angiograms. The reconstructed model is then visualized in augmented reality with the help of an AR headset.
This AR can be experienced by the user
either by placing the AR headset on the head or by using smartphones.

They proposed to display the model on a Heads-Up Display (HUD), powered by a smartphone for easy accessibility. This will provide the physician with an easily accessible mode of the eye, specifically the macula. The doctor will be able to control and interact with the model under examination using a Bluetooth connected joystick.
He said: “To our knowledge, this is the first time such a unique system is being developed for visualization of ocular scans.” His team demonstrated the AR headsets and handphone application during the presentation.
The application of this technology might be relevant to on-field diagnostics, telemedicine and medical AI.
On Vitrectomy for CRAO
Lastly, Dr. Nishikant Borse shared on “Vitrectomy for Central Retinal Artery Occlusion (CRAO) — Future Options.”
There are very limited treatment options non-dissolution of CRAOs. Medical thrombolysis has not worked well because thrombolysis is caused by cholesterol. Surgical vitrectomy gives the advantage of hypotony, directly massaging the CRA and dislodging the embolus with good results.
There are a few limitations to this intervention — for instance, deep embolus. Furthermore, there hasn’t been a consensus of when to intervene within the duration of the CRAO. This is because the survival of retinal cells almost always relies on the amount of residual blood flow and the length of time between onset and treatment.
“Residual blood flow might have been present in eyes where visual improvement was seen after reperfusion,” he said, adding that it was difficult to detect. So, how can the blood flow be quantified more accurately?
Enter a new platform that combines the non-invasive measurement of the
retina or choroid structure and ocular blood flow based on OCT; and widefield semi-quantitative global flow visualization, using line-scanning Doppler flowmetry (LSDF). This imaging platform enables comprehensive assessment of blood flow in retina and choroid.
“It will enable us to know the amount of ocular and residual flow without injecting a dye. In the future, that will help us to know when to intervene and when not to intervene,” he said.
Another CRAO advance to watch is in endovascular surgery4, using a 47-gauge microneedle to directly inject TPA into the central retinal artery. As a result, there were no vitreous hemorrhages after cannulation. “This surgical procedure is very challenging and demands high precision. Thus, the development of robotic technology, such as the robotic armrest, will help in the cannulization — and it will be a very important step achieved in the management of CRAO,” concluded Dr. Borse.
References:
1 Franzco RL, Doba FH. The “C test” for tritan discrimination. Color Res Appl. 2017;43(1):5864.
2 de Smet MD, Naus GJL, Faridpooya K, Mura M. Robotic-assisted surgery in ophthalmology. Curr Opin Ophthalmol. 2018; 29:248-253.
3 Tyagi M, Basu S. Glue-assisted retinopexy for rhegmatogenous retinal detachments (GuARD): A novel surgical technique for closing retinal breaks. Indian J Ophthalmol. 2019;67(5):677680.
4 Kadonosono K, Yamane S., Inoue M, et al. Intraretinal Arterial Cannulation using a Microneedle for Central Retinal Artery Occlusion. Sci Rep. 2018; 8: 1360.
Editor’s Note:
The 78 th Annual Meeting of the All India Ophthalmological Society (AIOC 2020) took place from 13 to 16 February in Gurugram, India. Reporting for this story also took place at the AIOC 2020. Media MICE Pte Ltd, CAKE magazine’s parent company, was the media partner at AIOC 2020.
| May 2020 24 AI TOOLS IN RETINA INNOVATION
Researchers are always thinking of new innovations to help patients


https://2020 apvrs org/
Decoding the Challenges and Opportunities in
Artificial Intelligence
by Brooke Herron
Recent developments in machine learning and artificial intelligence (AI) have created a buzz throughout the ophthalmic industry. Most notably, is the use of deep learning to screen and detect diseases like diabetic retinopathy (DR), diabetic macular edema (DME), glaucoma and others. For busy surgeons, this extra hand in patient diagnosis can not only save valuable time, it could also potentially increase access to eye care for millions of patients.
Now, as the technology grows closer to fruition, health care providers must learn and decide how to implement and integrate AI into their practice. At the recent 78th Annual Conference of the All India Ophthalmological Society (AIOC 2020), industry experts dove into this topic, revealing their experience and vital input into this critically important technology.
AI in Ophthalmology

So, what exactly do all these buzzwords mean? In her presentation, Dr. Naama Hammel, a clinical research scientist at Google Health, succinctly defined the three main terms: (1) artificial
intelligence (AI) is a grand project [for machines] to build non-human intelligence; (2) machine learning (ML) occurs when machines learn to be smarter [by analyzing data]; and (3) deep learning (DL) is a particular kind of machine learning [often associated with human-like artificial intelligence].
According to Dr. Hammel, there are several reasons to apply DL to medicine. “Deep learning is very useful in situations where we have a lot of data to look through and we don’t have enough expertise to do it – and this is exactly the situation in diabetic retinopathy,” she explained. “Worldwide, there are 415 million people with diabetes. That’s a lot of data to look through, plus expertise in grading can be limited — this is where an algorithm can scale and enhance.”
This is important because all of diabetic patients need an annual screening for DR — and there aren’t enough doctors to check, or even screen, all of these people. And even in teleophthalmology DR screening programs, there aren’t enough doctors to grade all the acquired photos. This is precisely where AI can fill the gap by reading fundus images to detect DR.
So, how accurate is AI in screening DR? Dr. Hammel discussed a study published in 2016 where Google collaborated with two big hospitals in India. Together, they trained a model that can read a new fundus photo and determine whether the patient has DR. “The algorithm turned out to be very accurate… on par with ophthalmologists,” she stated. “Additional work on the same data improved the algorithm and it’s now on par with retina specialists, who are the gold standard.”

She continued that the algorithm will only be as good as we teach it; so, if we train it to detect DR, that’s what it will do. If it sees something else, it will simply say ‘no DR’. “This is something that’s very important, because it’s different from what humans think. They [algorithms] are trained to do a specific task and that’s what they know how to do.”
She concluded that as ophthalmologists, it’s important to
| May 2020 26 AI TOOLS INNOVATION
AI algorithms can be as good as ophthalmologists and retinal specialists in detecting DR.
Editor’s Note:

understand machine learning: “We need to be ready for the prime time when it comes,” said Dr. Hammel.
Screening and Detection
By the year 2040, the global burden of patients will diabetes is expected to rise to 642 million. For ophthalmologists, that mean that of those, an estimated 224 million will have some form of DR; while 70 million will have sight-threatening DR. India alone has 77 million cases of diabetes, with approximately 15 million patients affected with DR. With the rising incidence of diabetes and its comorbidities, more effective screening and diagnosis will certainly be needed.
Unfortunately, in India and across the developing world, there is often a delay in detecting DR – and this is precisely where AI can step in. Traditionally, access to appropriate specialists or imaging devices could cause a delay in DR detection. However today, there is an opportunity to treat more patients using teleophthalmology (especially in rural areas) and AI.
In her presentation discussing AI in DR detection, Dr. R. Rajalakshmi, from Dr. Mohan’s Diabetes Specialities Centre, explained that machines are taught to recognize specific patterns in high-resolution images — in fact, the system uses thousands of retinal images of varying grades of DR, which allow it to make an accurate diagnosis.
Additionally, using AI for DR detection has been proven to be fast, consistent, scalable and accurate. According to Dr. Rajalakshmi, there are several advantages to this approach: Physicians are less burdened and can screen large numbers of patients, leading to earlier detection and enabling specialists to focus on treatment. Plus, many AI systems have an accuracy of more than 90%, making them a reliable diagnostic.
However, as with anything, AI does have limitations. “A machine may miss things that a human reader would notice, unless it is trained to identify the lesion, giving patients a false sense of security,” shared Dr. Rajalaksmhi.
Current Challenges in AI
Of course, when incorporating any new technology into an existing practice, there are challenges to overcome — and adding AI into the diagnostic mix is no different. Dr. Rajalakshmi said that currently, the challenge is deploying these models into clinical practice, and it must happen with care and caution. Governmental and regulatory approval for the use of AI in medicine is in various stages worldwide.
She concluded that ophthalmologists should not feel threatened by AI: “AI is not the ‘AlphaGo’ that will eventually replace the ophthalmologist,” she said. “It is a tool — not a threat.”
| May 2020 27
Not to fret, AI will aid — not replace— doctors.
AIOC 2020 was held in Gurugram, India, from February 13 to 16, 2020. Reporting for this story also took place at AIOC 2020. Media MICE Pte Ltd, PIE Magazine’s parent company, was the media partner at AIOC 2020.
by Tan Sher Lynn
as a Female Ophthalmologist Finding Fulfillment

Dr. Soundari Sivagnanam was born in New Delhi, and brought up in Tirunelveli, a small town in South India. After completing her MBBS, she got married and moved to Chennai, where she enrolled at the Regional Institute of Ophthalmology, and subsequently, Stanley Medical College.
She said her husband influenced her decision to choose ophthalmology. “He is a biomedical engineer (in the same field) and he thinks very highly of ophthalmology,” explained Dr. Sivagnanam.
“When I first started my studies in ophthalmology, I thought, ‘what is there to read about such a small structure?’. Boy, I was wrong. After going through the course, my entire ideology changed. Although the eye is a seemingly small area compared to the rest of the body, there are so many things to learn and do at each of its structures, such as the cornea.
“It dawned on me that ophthalmology is actually a very challenging field, where there’s a lot to understand and apply into clinical practice. And I wondered if I made the right decision,” she recalled.
Nevertheless, the more Dr. Sivagnanam studied the eye, the more she fell in love with the discipline: “Performing eye surgery gives me an adrenaline rush and it has become addictive. Today, if any medical graduates asked me to suggest a discipline, without a second thought, I would definitely tell them to choose ophthalmology.”
Work is Passion
Because of her love for her work, Dr. Sivagnanam has never taken a break throughout her career — even when she had a high-risk pregnancy with her second child, she worked until the last day of her pregnancy.
“My work gives me a lot of pleasure. Especially when patients give me so much
WOMEN IN OPHTHALMOLOGY ENLIGHTENMENT
| May 2020 28
trust by coming back to me, I don’t feel like leaving them alone by taking days off,” shared Dr. Sivagnanam. “So, I worked until the last day of my pregnancy and the next day I went to the hospital and delivered my baby.
“My work is my passion and I enjoy it — and I would say that this is the most important thing,” she said.
Dr. Sivagnanam learned her passion for ophthalmology from Dr. Amar Agarwal, the chairman of Dr. Agarwal’s Eye Hospital. “Dr. Agarwal is the one who shaped me into being a very good doctor. Other than ophthalmology, he doesn’t seem to think about anything else. He has been my mentor from the very beginning,” she said.
As a Female in the Field
Dr. Sivagnanam said that ophthalmology is a good field for female doctors because it allows for a better work-life balance: “The number of emergency cases is much less than other specialties, and you will have more time to spend with your family.”
Perhaps, because of this, ophthalmology is increasingly becoming a female-dominated industry. Dr. Sivagnanam observed: “Even in our institution alone, there are many female eye doctors, but just a handful of males. These female doctors are very good at what they do.”
In terms of family, Dr. Sivagnanam is very grateful for her supportive husband, parents and in-laws. “Having a small, few-months-old child and going back to work was difficult . . . having to juggle feedings and all that. My family members have helped me a lot, especially when my kids were little. Even now that my kids are older, I still have their support. And because of them, I can continue my work without taking a break,” she shared.
Keep Learning
Dr. Sivagnanam is a firm believer of lifelong learning. “Whatever you do, do it with passion and keep learning throughout life. Learning is a process that never ends, there are so many
new things coming out every day. And whatever you’ve done in your life, things will keep changing.
“For example, during my post-graduate days, I thought that laser was the only treatment option for cataract, but now it is the last option.
“Nowadays, people are trying to figure out the age and sex of a patient by looking at a fundus photograph. Is the patient a smoker or not, and can he or she develop a certain condition within a few months? Coupled with the advancement of technology, we really need to keep updating ourselves every day, because what we have now will not be good enough in a few years’ time.
“Moreover, patients are very wellinformed today. They search Google, research online and then come back to you,” she explained. “Would you be in the position to answer all their questions? Would they have trust in you? That’s why continuous learning and updating is the most important thing.”
Saving Sight, Saving Lives
To Dr. Sivagnanam, ophthalmology is a very gratifying field because it gives patients the gift of sight. According to her, the human eye, as the ‘window of health’ can often reveal clues that signal issues elsewhere in the body, thus enabling early detection and treatment.
“An ophthalmologist’s recommendations can often help physicians (of other specialties) treat systematic conditions before the manifestation of the related disease,” she said.
“In certain cases, neuro-ophthalmology is a field that saves lives. In my clinical experience, there have been lots of circumstances during which I was able to diagnose the associated neurological problem when the patient came in for a general eye check-up.
“For example, a 10-year-old patient came for an eye check for some visual disturbances. One examination report indicated that he had normal vision, but when a perimetry test was done,
it confirmed the suspicion that he had a visual field defect. It was a case of pituitary adenoma. The patient was referred to the neurologist and was cured, ultimately,” she said.
In another case, Dr. Sivagnanam described an old man who came into the hospital complaining of dizziness; upon examination, he was found to have a visual field defect. “He was given an urgent referral for an MRI scan and was diagnosed as having a stroke. Because of the timely diagnosis, the patient’s life was saved.”
The field of ophthalmology is advancing, and as a result, saving more sight. However, eye donation is one area where Dr. Sivagnanam thinks industry awareness could be increased.
“The awareness regarding eye donation is lacking. We see young people in their 20s, passing away without pledging to be a donor,” she said. “We, as ophthalmologists, should take up the responsibility to promote organ donation so that more people will know this needs to be done. I feel that the reach will be better when organ donation is explained by a doctor.”
Contributing Doctor
Dr. Soundari Sivagnanam is a senior consultant at Dr. Agarwal’s Eye Hospital in Chennai, India, specializing in general ophthalmology and neuroophthalmology. She has been on the teaching faculty for DNB students at Dr. Agarwal’s Eye Hospital since 2007, and the program coordinator for “Kalpavriksha,” a postgraduate update program since its induction (2007). She has presented in national conferences and participated in international conferences. She has also co-authored a few peer-reviewed articles. During her free time, Dr. Sivagnanam loves to spend time with her kids, listen to music and read.
soundari404@gmail.com

| May 2020 29
by Matt Young
Banana Man... PIE Guy… Whatever you Call Me: I Have Coronavirus (COVID-19)

March 20, 2020
Since the news broke that an American in Da Nang has contracted coronavirus — number 68 in the country — I have been silent on social media about my condition for a few days. It was awkward. I was content being in a local hospital quarantine (as strange as that sounds), because I had planned to be here, and was actively posting about my containment in a positive manner.
But it was altogether different being infected, suddenly at a ground-zero of the global pandemic. I would have to notify many people of my contact, first and foremost. I would have to move from one hospital quarantine to another more serious quarantine facility for treatment. I’d be subjected to a litany of tests.
And I might have to die.
Grocery Shopping for Quarantine
Thirty minutes before COOP closed, I was hoofing it into this glorious Amsterdam supermarket, although for more ominous reasons this time.
Typically, I like international grocery shopping. I once bought a Yeti (an industrial-strength cooler) to zipup and check-in cold groceries as luggage, only to unzip them 24 hours later still frozen or chilled. It’s a weird little hobby, but one that I enjoy given that I have to travel to global conferences multiple times a month for work, and sometimes there’s only time to work under
“I was prepared for a local hospital quarantine in Vietnam; I wasn’t prepared for coronavirus (COVID-19).”
COVID-19 SPECIAL REPORT ENLIGHTENMENT
| May 2020 30
an exhibition roof (they often look the same). For me, I enjoy grocery shopping somewhere new, bringing tasty food back to share with my family. This time was different though. I wasn’t there for enjoyment. I was building a really minimalist bug-out bag.
Packaged waffles, boxed teas, sausages… good foodstuffs from Europe, essentially, went into my bag and luggage. Things were changing by the hour, but I highly suspected due to my recent travel to Germany, I would be quarantined as soon as I got to the airport in Da Nang, Vietnam, my home. I would be precisely correct.

Recent news about my coronavirus status reported that I was a tourist coming to Da Nang. Not so. It has been my wonderful home for five years, along with my wife and children. That said, I still need reminders of the West, and hence, while I enjoy local food, I need my sausage and waffles.
Also, contrary to some online suggestions surrounding those reports, I wasn’t out gallivanting as a rich American tourist at a time of crisis. As a CEO and company founder, I was trying to save the medical publishing business I started 11 years prior in Singapore. My family and dozen employees depend on it, not to mention our future as pioneers in medical communication, which is my life’s vocation.
Testing Positive
On Wednesday, March 18, I tested positive for coronavirus (COVID-19) back in a local hospital quarantine in Da Nang, Vietnam. The news was devastating… and embarrassing.


Having been on a media tour, I would now have to notify so many people — including many customers — that I put them at risk for coronavirus by virtue of our simple contact. Contrary to the advice of my friends, family and colleagues, who advised total rest, I stayed up late Tuesday night on my laptop sending email after email to notify those at risk. These same people just days before had been extremely supportive of my quarantine at a local hospital due to my travel to Germany. But would they be supportive now, knowing that I may have infected them?
To their credit, every single person in my network was. I’m not saying I deserved this outpouring of support. I’m saying it happened.
Some may be reading this who was unaware of my coronavirus status until now. Coronavirus (COVID-19) symptoms appear 2-14 days after exposure, according to the Centers for Disease Control and Prevention (CDC). As I started displaying symptoms late at night on Monday, March 16 — including minor headache, minor
backache, phlegm and shortness of breath — I tracked back 14 days to essentially the beginning of March and notified many of those I had come into contact with (if I didn’t notify you for some reason and you feel I should have, I’m sorry. It is not an easy task to remember and notify potential contacts, especially when sick. The timeframe of notification also is not set in stone, I realize).
After that, I waited to live or die.
I suppose I will live, given that I am not elderly, but my shortness of breath was a concern. I have experience with exercise-induced asthma and coughvariant asthma. Were those underlying conditions that would put me a graver risk of death? Would my shortness of breath eventually require intubation? Little information was forthcoming.
Rewind to 2019
For Media MICE, 2019 was a banner year. I remember November 24, 2019, very fondly. I was still wearing my banana shirt, black fedora and dark shades from the conference and dancing to a Shanghai salsa band (they do exist), having just finished a successful media partnership with the Asia-Pacific Vitreo-retina Society (APVRS). The whole team was there. My colleague Rob and I were dressed akin to “The Blues Brothers” — that is, the 1980s stars John Belushi and Dan Aykroyd in the movie of the same name — except we called ourselves “The Banana Brothers.”

I keep going back, but so much of the weirdness of what we do requires context.
In 2017, a couple days before the European Society of Cataract and Refractive Surgeons (ESCRS) meeting in Lisbon, Portugal, I spotted some banana short sleeve shirts in Hoi An, Vietnam. Right around then, local Da Nang expats may remember fruit fashion started becoming popular in our city. However, for whatever reason, I asked a tailor to make me a full fruit suit. The first one — turned around within a day — was a banana suit. I asked for three more (watermelon, strawberry/flower and orange). I asked

| May 2020 31
Matt in happier times wearing his banana suit at an ophthalmology conference.
An chest x-ray machine is taken away after used on Matt.
The vitals are less concerning than Matt looks at the moment.
The hospital “minibar” that Matt created, supplied courtesy of COOP supermarket in Amsterdam.
for matching flat caps as well. They were finished just in time before my flight.
This would continue my trend of wearing outrageous “fashions” for inbound marketing purposes at conferences we attended. I figured we were in media — though in a very dry medical field of ophthalmology. Still, I thought, we should stand out and shine a light on issues — whether with flower or banana power. Looking ravishing also had the effect of starting conversations.
But this time was different. While I had worn different shades of Google Glass in the past; carried a Double Robot around the world with my Indian colleague as robotic telepresence; donned gangster outfits, pirate outfits, and committed various forms of skullcap-duggery in ophthalmology — I was not ready for the response in Lisbon.

It was ginormous. Committing my zaniness in ophthalmology to the form of a suit was incredibly powerful. At the time, we published 3,000 hardcopies of PIE magazine (Posterior segment – Innovation – Enlightenment) and were out by noon on the first day. And this was for an anterior segment conference! No sin to any layman, but in the ophthalmic industry, you just don’t typically mix anterior and posterior . . . well, until we did. “Like Ice Cream on a Cone, Dumbbells and Biceps, Burgers and Fries, Fish on Hooks, Wine and Cheese, and Milk and Cookies, the Anterior and Posterior Segments are Better Together” we proclaimed. That is, until we published CAKE (Cataract – Anterior segment – Kudos – Enlightenment) magazine two years later, and we happily divided the segments of the eye once again to provide specialized knowledge about each one.
Essentially, by the outlandishness of our outfits in a sophisticated and sane medical industry, and the thematic angles of our content, we proclaimed ourselves to be ophthalmology’s

first funky magazines. We thought of ourselves as MAD magazine in style, but serious ophthalmic journalists in substance. We believed our contribution, over time, meant more doctors reading our content, spreading knowledge, and making the world of vision better overall.
Hence, we were PIE and CAKE, and on November 24, 2019, we were the opposite of bluesy. We were red hot and on top of the world at Bar Rouge, one of Shanghai’s top nightspots. We were slated to post the company’s best full-year performance to date — and that more importantly, our hypothesis was right: We were making a difference in spreading more knowledge of surgery and therapies supporting sight.

Seven days earlier, the first case of coronavirus (COVID-19) was detected in another part of China: Wuhan. Little did we know it would change all of our lives in 2020.

The Real-Life Disaster Movie Begins
Asleep, I felt my phone vibrate just after midnight on January 31, 2020. Instinctively, I woke up to find that the Asia-Pacific Academy of Ophthalmology (APAO) annual conference had been postponed due to the outbreak of coronavirus. For us, the APAO had become a major media push each year.
The year earlier for the APAO in Bangkok, we created wildly customized chef outfits (courtesy of our great Hoi An tailors); created the “best recipes of ophthalmology surgery” editions; published both of our magazines and a daily congress newspaper; filmed video interviews from our media stall on-site; and celebrated our Media MICE 10-year anniversary. I gave a speech in which I changed outfits several times, ending up in a tank top that said: “I’m not perfect, but I am one of a kind.” My muscles clearly lacked perfection.
There was a silver lining. We had been invited to be the media partner for the Annual Meeting of the All India Ophthalmological Society (AIOC 2020), just outside of Delhi, India. Quickly, we decided to shift all our first-quarter efforts into supporting the AIOC with our magazines and a daily congress newspaper. It turned out to be our largest publication experience to date, with all 12,500 hardcopies pushed out over four days. Moreover, we decided to make India the first stop on a worldwide media tour, promoting our media business — but also listening to our customers at a time of impending crisis. We knew 2020 would be a time of disruptive change due to coronavirus. We didn’t know at the time it would eventually clear out the streets of Paris, London and New York like in a disaster movie.
Showing Up
Off to Morocco we went, on the second leg of our journey, where the ESCRS Winter Meeting took place. There, we met with a handful of customers to kickstart our media tour. Then it was on to Switzerland and Germany, where we noticed the lion’s share of our European customers were based. Hungary and The Netherlands rounded out our tour, providing the opportunity to meet new customers, understand where the industry was going in a tumultuous 2020 and solidify our cooperation with
Matt’s encampment at the second hospital quarantine facility.
ENLIGHTENMENT COVID-19 SPECIAL REPORT | May 2020 32
Matt delivering a speech in the Media MICE booth at APAO 2019 Bangkok.
“But this year, APAO was postponed. My mind went into overdrive.”
World Ophthalmology Congress (WOC) representatives, who are based in Amsterdam.
We felt that we were making incredible progress. After a 12-hour drive through a German snowstorm in near-whiteout conditions, we made it to Jena, Germany. We had multiple meetings with our associates at Zeiss, who have been a partner for nearly a decade. Meetings with many other companies were making things clear: We would immediately pivot to much more digital offerings in 2020. With conference cancellation after cancellation, it was apparent that social media, website content, webinars, and the like, would be needed in 2020 like never before — and with conferences rattled, companies were looking to invest in our unique approach, so long as we moved fast enough to fill out the digital space.
We were moving fast — on the autobahn from Berlin at 210kph on a Sunday to make a meeting the following day in Basel, and on a flight the following day to Budapest to round out a connection we made in Marrakesh. On another day, we reached Berlin at 2 a.m. after driving all night from Frankfurt, only to find our morning meeting was canceled. But we showed up, and that’s an important part of business life — or so we thought.
Today
It is now Friday, March 20, at 8:35 a.m. Today begins day 7 of my hospital quarantine. It is day 4 of being coronavirus positive.
I feel that in relaying my story in Vietnam, context is critical. I’m one of the first Americans to test positive for coronavirus in Vietnam, a concerning distinction.
“What do I feel? How do I evaluate what happened? What do I see looking forward?”
Well, on days 1 and 2 of being coronavirus positive, I felt the symptoms described above, plus a bit of coughing. The last two days, fortunately, I have been almost completely symptom-free.
During this ordeal, I experienced a mixture of guilt, as well as fear of death.
I replayed the tape of recent events in my mind, and here’s what I remember…
When I embarked on the initial leg of my journey to India on February 11, it really was a requirement to continue business as normally as possible. At that time, coronavirus in India was not a major concern. Nearly 10,000 delegates showed up, and almost all without masks. Coronavirus was still — from what I can remember — thought to be a Far East problem, with a possibility of global impact.
Even so, all 16 people in Vietnam initially infected with coronavirus were cured. As of February 25, no new cases had been recorded since February 13. It seemed safe to continue my journey to Africa and Europe without the concern of impacting others.
The ESCRS in Morocco was from February 21-23, which spanned a weekend, and went on without a hitch. It seemed fairly well attended, and flights both going and coming were packed.

The following work week, the Swiss Academy of Ophthalmology meeting also was well attended, and I met with many customers there. Coronavirus was not a major topic of discussion. We met with many other Swiss clients that week — in Bern and Heerbrugg.

Our week of German meetings began the last few days in February, continuing into the first week of March. One German client stayed home and teleconferenced with us, having just gotten back from the Middle East with a cold. I thought it was noble . . . but would I have done the same? Other clients began tapping our feet with their feet, instead of shaking our hands. Still others were forbidden to shake hands at all in the company facilities, a new policy.
I noticed other conferences we were due to attend begin to cancel (Frankfurt Retina and EPOMEC in Dubai).
By the afternoon of March 12, allvirtual meetings (which previously were scheduled as in-person meetings) were happening. The rest were cancelled. On this date, I realized that questions about Germany and coronavirus had been circling, and that it may be challenging to get back home. Quarantine was likely. I went to the supermarket at 8:30 p.m. and built my bug-out bag.
On the morning of Friday the 13th, I ominously flew home to Vietnam — and I haven’t set foot into my actual house since then, as I was quarantined immediately at the airport and taken to local hospital quarantine.
 Matt in Jena.
Matt and Robert in Morocco.
Matt begins experiencing symptoms of coronavirus (COVID - 19) the night before he tests positive. They include mild headache, mild backache, shortness of breath, and phlegm. There was no fever in his case.
Matt in Jena.
Matt and Robert in Morocco.
Matt begins experiencing symptoms of coronavirus (COVID - 19) the night before he tests positive. They include mild headache, mild backache, shortness of breath, and phlegm. There was no fever in his case.
| May 2020 33
I don’t recall hearing the phrase “social distancing” one time while I was in Europe. So much happened in the near blink of an eye.
The U.K.’s Daily Mail ran photos of the Causeway from Singapore to Johor Bahru (which I used to cross three times a week) full of traffic on March 17, and completely empty on March 18. It showed crowds gathered at Buckingham Palace in the U.K. on March 13, and nearly empty on March 18. In a handful of days, the world changed forever. And other than the drive in the ambulance, I have seen little of its current state since I was quarantined on March 14 at the Da Nang airport upon entry.
At the same time, I did do some things wrong in the context of the world we live in today. I was still aggressively traveling and meeting at a time when others began videoconferencing. I went to some bars. I pushed the limits of globalization, at the end of that era. It seems we are at the end — at least of the Golden Age.
I also honestly declared where I had been internationally at Da Nang Airport. I had no symptoms upon arrival and everyone else on my flight seemed to make it through customs without an issue. But I declared and was immediately taken into quarantine at a local hospital. A local news site later said I had exceedingly little concerning contact with the local populace as I exited the plane — mostly with health care workers, which by my recollection were in full hazmat suits.
While some guilt remains over possible contact, I know that I did not bring coronavirus to Europe from Asia (as my symptoms appeared way after my February 11 departure date). And I know by immediately declaring I had been in Germany, that I limited my contact with Vietnamese people based on an immediate quarantine. Had customs not flagged me, my wife had prepared a home quarantine for me in Da Nang in a room I call “the bunker.”
Vietnam: Developed Nation
But Vietnam did quarantine me, and this last part of my story I would like to devote to the people of Da Nang.
While they are in hazmat suits, their bedside manner is impeccable. I can tell by the friendliness to which they respond to my overtures such as “xin chào” (hello) or “cảm on” (thank you). I see through the masks and plastic… and I see smiles.
While the facilities are modest, what I love about Vietnam is that it impresses upon you how simple living — even within a hospital quarantine — is good living. The shower can be made hot, although a cool shower is sometimes just as nice or better. While there is no air conditioning in my current room, there are plenty of fans (and I don’t think air conditioning would be good for my health anyway at this time).
They clearly know what they are doing, because as of today, no deaths have been reported related to coronavirus in Vietnam.


I haven’t always been a fan of Vietnamese food — even after 5 years, but I am now. Every meal has been delicious in the local hospitals. That’s incredibly ironic, as hospital food in the West is known to be appalling. And my bug-out bag, though nice, wasn’t really required after all. It’s just for creature comforts now.
The entire healthcare system is quite communicative, from the deputy director of the local CDC — who speaks to my wife — all the way to the local English-speaking nurse, that has me on WhatsApp and even asks me what I would like for lunch.
Even though initially I wondered about a camera in the corner of the room, I realized that they were vigilantly keeping an eye on my vital signs. I once tried to turn a machine to see my oxygenation levels, and my wife called and said to turn it back toward the camera. She was translating for the hospital, which wanted to keep my vitals in view of
their human monitors. That’s a keen eye on my treatment!
And so, I dedicate this last paragraph to a particular idea about Vietnam, whose time has come to rise in the world. Although I am but a small part of the world’s healthcare industry, I would like to say this: Vietnam has reached developed nation status when it comes to preventing and treating coronavirus, which is something even my own country of the U.S. cannot say. For some time, many people thought it was such an odd choice for an American to live in Vietnam. Now, not so much, huh? I say that knowing I’m not out of the woods — or quarantine — yet. But I am happy to be here, or as happy as can be expected.
Editor’s Note:

This article first appeared on PIE magazine’s website on March 20, 2020.
piemagazine.org/banana-man-pieguy-whatever-you-call-me-i-havecoronavirus-covid-19/
Matt Young recovered from COVID-19 and has been sent home to his family in Da Nang when this issue went to press.
| May 2020 34
Healthcare workers outside Matt’s isolated room in the second hospital quarantine facility
“Your health care workers have devoted tireless hours to my cause.”
ENLIGHTENMENT COVID-19 SPECIAL REPORT
Guided by a local health care worker during the first hospital quarantine
Providing Solutions for Subretinal Injection



jections are challenging. Let make it easier with our wide etinal injection cannulas so the one that is best for each t that with our MicroDose give you precision and total the injection process. Having ls can make the job easier.

nstellation®, Bausch & Lomb Stellaris® and DORC Eva® with David M. Brown, MD, Houston, TX Kit includes preassembled adapter and syringe 3275 MicroDose™ Injection Kit
Control + Precision with our MicroDose™ Injection Kit and Subretinal Cannulas M ed On e Surg i cal, I n c. ● TEL : 9 41 .3 59 3 1 2 9 6 7 0 T a ll e v a st Ro ad, S a r a s o t a, F L 34 24 3 U S A ww w M e d On e com ● M ed O n e@ M e d O ne. c o m
Shedding Light on the Latest Diagnostics and Treatment for Uveitis

 by Brooke Herron
by Brooke Herron
During a symposium on ‘Uveitis and Ocular Inflammation Treatment’ on the last day of the Asia-Pacific Vitreoretina Society (APVRS) 2019 annual meeting in Shanghai, China, renowned speakers discussed the importance of early diagnosis, as well as proper treatment for refractory uveitis.
Although uveitis is a common cause of blindness – accounting for 10 to 15 percent of vision loss – diagnosis and treatment remains a challenge. There are various reasons for this, including the lack of a clinical database and sample bank; the fact that its disease mechanisms are not fully understood; and the lack of ideal therapeutic treatment regimens.
Uveitis also has multiple etiologies: non-infectious uveitis usually has systemic involvement, infectious uveitis shows acute or chronic inflammation, while others causes of inflammation result from malignant cells.
Combining Tools for a Better Diagnosis
“As we know, it’s now an image-based diagnosis . . . and often types of infectious and non-infectious uveitis have similar designs and that can be confusing,” said Dr. Yong Tao from the Department of Ophthalmology at Beijing Chaoyang Hospital.
He then presented the case of a young female suffering from blurred vision in the right eye for two weeks. One week later, her intraocular pressure (IOP) increased to 40mmHg and she was diagnosed with presumed PosnerSchlossman syndrome. The patient was treated with steroid eye drops and IOP decreased.
“There were no signs of inflammation in the anterior chamber . . . which means we couldn’t make a diagnosis of acute retinal necrosis (ARN), according to the 1994 guidelines,” said. Dr. Tao. However, after a sample of the aqueous humor was collected, the varicella zoster virus was found, and ARN was diagnosed.
| May 2020 36 APVRS 2019 COVERAGE CONFERENCE HIGHLIGHTS
The findings from this case, among others, led Dr. Tao to conclude that “if we only use images for diagnosis, it may lead us to diagnosis the patient in the middle or late stage, but if we can combine the tools, we can make an early diagnosis which means a better prognosis”.
Updates in CMV Treatment
Dr. Ian Wong from the University of Hong Kong presented an update on CMV (cytomegalovirus-associated uveitis) treatment. He says that in addition to HIV-infected/AIDS patients, CMV retinitis (CMVR) is also seen in other patients, mainly those on immunosuppression – and that there’s more evidence that the clinical features may not be entirely the same compared with HIV patients.
This could be a concern for patients under immunosuppression, or in those about to receive immunosuppression. Therefore, he asked the question: Are the clinical features in these patients similar to those with HIV/AIDS?
“In Asia, the CMV seroprevalence is quite high, most people aged 50 and above have some CMV in their body,” stated Dr. Wong, adding that in Hong Kong while the AIDS prevalence is quite low, the CMVR prevalence remains higher. As this is a notable concern, he then presented results from two studies of CMVR patients without HIV/AIDS.
Overall, it was found that in non-HIV/ AIDS patients with CMVR, aqueous tapping for PCR is highly sensitive –and more so than a blood test, and that a negative blood test does not rule of CMVR. Overall, the visual prognosis is generally poor, including patients with poor presenting visual acuity and in those with macular involvement. In addition, he reiterated the importance of screening for at-risk patients.
Alternative Therapies for Autoimmune Uveitis

Dr. Xiaomin Zhang from Tianjin Medical University Eye Hospital and Eye Institute discussed using Mesenchymal Stem Cell (MSC) therapy as an alternative therapy for autoimmune
uveitis, explaining that MSCs have both an immunosuppressive and neurotrophic effect.
“They have been successfully used to treat systemic autoimmune diseases and are a good candidate for treating retina-involved uveitis,” Dr. Zhang told delegates.
She presented two cases, one of which concerned a 56-year-old male with recurrent uveitis in both eyes for two years. The patient was diagnosed with Vogt-Koyanagi-Harada (VKH) syndrome. The patient refused systemic corticosteroids treatment and received an intravenous infusion of allogenic MSCs from a human umbilical cord. A low dose of corticosteroid combined with immunosuppressant was administered for inflammation after 6 days of follow-up and was discontinued after 12 months. There was no recurrence of inflammation found in subsequent follow-up over three years.
The second case was a 65-year-old female with uveitis in the right eye for six years and a presenting BCVA of 20/80. The patient was diagnosed with idiopathic panuveitis and had accepted steroid and immunosuppressant therapy for three years – however, inflammation reoccurred each time the prednisone was tapered. The patient then received intravenous MSCs. Systemic medicine was tapered and discontinued after 14 months without relapse, and the BVCA stabilized at 20/40.
The results from these cases led Dr. Zhang to conclude that “MSC therapy is effective in maintaining remission in uveitis patients refractory to previous immunosuppressive therapy”.
Looking at VKH in Chinese Patients
During his presentation, Dr. Peizeng Yang from the Chongqing Eye Institute, detailed the efforts undertaken to address these challenges in diagnosis and treatment of uveitis, specifically as it applies to VKH syndrome in Chinese patients, which is a common uveitis entity in China.
“We collected 20,000 samples from uveitis patients to establish the world’s largest uveitis biological sample bank,” he told delegates. From there, a large data set of Chinese VKH patients was used to develop diagnostic criteria, as detailed in a recent study published in JAMA (Sept. 2019).
Once diagnosis is confirmed, treatment follows – and Dr. Yang says novel treatment regimens have been developed for VKH and have shown good results. In a study published in 2018, he says that a reduced dose of corticosteroids, combined with immune-suppressive agents, resulted in controlled uveitis in 97% of patients, with 80% of eyes achieving ≥20/40, with no side effects. He also noted various published research on other uveitis entities in Chinese patients and discussed genetic studies on uveitis.
Editor’s Note:
The 13 th Asia-Pacific Vitreo-retina Society Congress (APVRS 2019) was held in Shanghai, China, on November 22-24, 2019. Media MICE Pte Ltd, PIE magazine’s parent company was the Official Media Partner at APVRS 2019. Reporting for this story also took place at APVRS 2019.
The latest updates on treating ocular inflammation have arrived!
| May 2020 37
Impact of Systemic Medications on Retinal Function



 by Khor Hui-Min
by Khor Hui-Min
Ocular side effects of systemic drugs include abnormal and/ or blurred vision, poor focusing ability, dry or irritated eyes, color perception changes and altered pupil size. The reaction, and its severity, depends on the amount of drug administered, the nature of the drug and the route of administration, as well as pathophysiologic variables, age and gender, drug interactions in multiple drug therapy, and allergies to drugs.
The retinal pigment epithelium (RPE) is a likely target for systemically administered compounds, since the underlying choroid is highly vascularized. The specialized pigment epithelium has numerous functions that all maintain the integrity and function of photoreceptors. Consequently, said the experts, toxic effects on the pigment epithelium will eventually affect the neural retina.
During a symposium on the “Impact of Systemic Medications on Retinal Function” at the 13th Asia-Pacific Vitreo-retina Society Congress (APVRS 2019) held last November in Shanghai, China, various esteemed researchers presented their latest findings and techniques.
Dr. Elliott Sohn, associate professor and director of surgical and medical retina fellowships at the University of Iowa, U.S., spoke on the disruption of the pigment epithelium from drugs like thioridazine (an antipsychotic drug), dideoxyinosine (an HIV treatment) and deferoxamine (a commonly used ironchelating agent to treat transfusionrelated hemosiderosis).
On the retinal toxicity of systemic and topical medications, delegates heard that thioridazine, a piperidine antipsychotic drug that previously was

widely used to treat schizophrenia and psychosis, can cause acute toxicity in high doses, producing symptoms such as blurred vision, dyschromatopsia (reddish or brownish discoloration of vision) and nyctalopia. On the other hand, retinal changes (including retinal depigmentation) have been reported in patients receiving dideoxyinosine; related systemic toxicities of deferoxamine include sight-threatening ocular toxicity involving the RPE.
Dr. William F. Mieler from the University of Illinois, U.S., discussed chloroquine and hydroxychloroquine. Chloroquine is used for the prevention and treatment of malaria and amoebiasis; while hydroxychloroquine, a less toxic metabolite of chloroquine, is used as treatment for rheumatic diseases such as systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), juvenile idiopathic arthritis (JIA) and
| May 2020 38
APVRS 2019 COVERAGE CONFERENCE HIGHLIGHTS
Systemic medications can cause a ripple effect of unwanted retinal toxicity.
Sjogren’s syndrome. Both can cause retinopathy, but the effects are seen in hydroxychloroquine much less frequently, and without crossing the blood-retinal barrier. High dose and long duration of treatment are the greatest risk factors for toxicity, and the primary screening tools are automated perimetry and SD-OCT. Toxicity is not reversible, thus prevention is the key.
Dr. Mieler also talked about pentosan polysulfate sodium (PPS), a semisynthetic polysulfated xylan used in the prevention and treatment of thrombi, as a novel therapy in the treatment and management of mucopolysaccharidoses, as well as treatment of interstitial cystitis or nephritis.
The long-term effects are not yet fully known, although progressive atrophy has been documented,” said Dr. Mieler.
Further, Dr. Mieler also presented on chemotherapeutics, mitogen-activated protein kinases (MEK) and checkpoint inhibitors. For checkpoint inhibitors, side effects typically occur within a few weeks to a few months after initiating treatment and can usually be managed with topical or systemic corticosteroids.
Dr. Shibo Tang, vice president of the Aier Eye Hospital Group, China, discussed cystoid macular edema (CME), which affects the central retina or macula. Although painless, this condition leads to the formation of multiple cyst-like (cystoid) areas of fluid in the macula and causes retinal swelling (edema).
Dr. Joo Yong Lee from the Asan Medical Center, University of Ulsan College of Medicine in Seoul, Korea, spoke on vascular occlusion caused by quinine sulfate, cisplatin/BCNU (carmustine), interferon, oral contraceptives, ergot alkaloids, gemcitabine and antibiotics (vancomycin, aminoglycosine). He also spoke on retinal adverse events caused by anti-cancer agents.
“Retinal specialists should always consider the possibility that retinal problems are associated with systemic medications. Since there is no consensus on routine ophthalmologic monitoring after systemic medication,


prompt consultation with a retinal specialist can lead to early detection, proper diagnosis and appropriate treatment,” explained Dr. Lee.
Prof. Dr. Young Hee Yoon, also from the Asan Medical Center, discussed crystalline deposition: “In addition to morphological changes of tamoxifen retinopathy on SD-OCT, its vascular changes on OCT, such as telangiectatic vascular change at the deep capillary plexus and right-angled vessels, are similar to those observed in the early stages of MacTel2.”
“These findings suggest that the target Müller cell dysfunction could be a potential therapeutic strategy in the management of tamoxifen retinopathy,” said Prof. Dr. Yoon.
In conclusion, Dr. Mieler advised delegates that there are thousands of therapeutic medications available on the market, but relatively few cause retinal complications. “Therefore it is important to recognize the usual patterns of toxicity, and be alert for possible new associations in the future,” he said.
Editor’s Note:

The 13th Asia-Pacific Vitreo-retina Society Congress (APVRS 2019) was held in Shanghai, China, on November 22-24, 2019. Media MICE Pte Ltd, PIE magazine’s parent company was the Official Media Partner at APVRS 2019. Reporting for this story also took place at APVRS 2019.
“The potential side effects of using PPS are visual impairment, as well as macular pigment mottling and excrescences on Bruch’s membrane. Watch out for retinal toxicity . . .
| May 2020 39
Retinal Imaging for Early Diagnosis and Patient Management

 by Tan Sher Lynn
by Tan Sher Lynn
Retinal imaging involves the creation of a two-dimensional image of the three-dimensional retinal tissue. Such techniques are indispensable for diagnosis and management of the disease, allowing practitioners to view the condition directly and plan treatment accordingly.
During the 13th Asia-Pacific Vitreoretina Society Congress (APVRS 2019) in Shanghai, China, last November, Dr. Srinivas Sadda presented the topic of “Wide Field Fundus Photography –Montage, Wide, Ultrawide, Which Is Better?”
According to Dr. Sadda, there has been recent innovation in the technology, instruments and modalities of widefield imaging. For example, the Monaco
(Optos, Dunfermline, Scotland) integrates OCT with ultra-widefield retinal imaging to feature color, autofluorescence and OCT scans for both eyes, in as little as two minutes. Meanwhile, confocal 4-color widefield imaging is a multimodal scanning laser ophthalmoscopy (cSLO), providing widefield color (red, green, blue and infrared), with retromode and OCT/OCTA imaging. He added that the rapid pace of advances in widefield imaging has necessitated the consideration of a new nomenclature for describing these images.
APVRS 2019 COVERAGE CONFERENCE HIGHLIGHTS | May 2020 40
Each day, AI takes one step closer as a tool for disease diagnosis and management.
In his presentation “Autofluorescence Imaging: An Adjunct or a MustHave”, Dr. Frank G. Holz discussed the growing spectrum of applications for fundus autofluorescence (FAF), a relatively new imaging modality that focuses on the fluorescent properties of pigments in the retina to generate images; these images help doctors view various disease processes from a different perspective, aiding in the understanding of the pathophysiology of different retinal disorders.
“Autofluorescence imaging refines phenotyping and differential diagnosis of retinal diseases,” shared Dr. Holz.
“It helps in the identification of early disease stages to allow for earlier intervention and better outcomes, monitoring disease progression in the context of natural history and interventional studies, and the identification of prognostic biomarkers, as well as novel clinical endpoints closely linked to visual function. I think that it is a must-have adjunct to other screening modalities,” he explained.
It is a definite ‘yes’ for Dr. Min Wang, who presented “Multicolor Imaging — Better than Conventional Color Fundus Photo?” According to Dr. Wang, multicolor images are taken with the cSLO to capture three simultaneous reflection images with three individual laser wavelengths: blue, green and infrared. These different wavelengths of monochromatic light penetrate the retinal surface at different depths to show details at the various layers of the retina, generating a single multispectral, color-like high resolution and high contrast image by merging the information of these images.
“Multicolor scanning laser imaging is an innovative technology for fundus imaging, offering detail and clarity not available from traditional color fundus photographs (CFP). It has many clinical applications and in some cases may be used to replace conventional CFP. Further studies will need to validate the retinal details seen on multicolor imaging with conventional CFP and other imaging modalities,” he said.
Progress Continues in AI
In his presentation, “Artificial Intelligence Applications on Color Images – Uncovering New Information”, Dr. Adnan Tufail noted that artificial intelligence (AI) and machine learning are already with us and will enhance our understanding of the retina by allowing quantification of humanidentifiable factors for association testing. Using sparse labels, we will also gain insight into novel anatomical associations that may enhance understanding of retinal disease or development.
Presenting on the topic “Predicting Cardiovascular Risk and Anemia from Fundus Photos Using AI”, Dr. Akinori Mitani explained that AI is the science of making things smart; machine learning refers to machines that learn from examples; and deep learning is a particular kind of machine learning.
“The deep learning system consists of layers of simple trainable mathematical units. It is highly accurate and learns features from raw data. Deep learning can help us find novel signals in medical images, such as cardiovascular risk factors and hemoglobin concentration in anemia,
giving us a better understanding of what appears in retinal images and providing additional value to retinal image screening,” he said, adding that deep neural networks can be adapted for diabetic screening as well.

As advancements continue to develop in the field of retinal imaging, so will our understanding of ocular diseases. These exciting imaging modalities have transformed our knowledge in the molecular pathogenesis of retinal diseases and are playing an increasing role in the early diagnosis and management of patients. And now, with the growing incorporation of AI technology in imaging modalities, AI integration will eventually transform from a luxury into a necessity.
Editor’s Note:
The 13th Asia-Pacific Vitreo-retina Society Congress (APVRS 2019) was held in Shanghai, China, on November 22-24, 2019. Media MICE Pte Ltd, PIE magazine’s parent company was the Official Media Partner at APVRS 2019. Reporting for this story also took place at APVRS 2019.
Say ‘cheese!’ New imaging modalities focus on retinal disease.
| May 2020 41

| May 2020 42



| May 2020 43 6001 Beach Road, #19-06 Golden Mile Tower, Singapore 199589 Phone: +65 8186 7677 | U.S.: +1 302 261 5379 E-mail: enquiry@mediamice.com Web: www.mediamice.com www.piemagazine.org www.cakemagazine.org magazine posterior segment innovation enlightenment CONTENT MARKETING + ADVERTISING + MEDICAL WRITING













2 18 November 2022 | Issue #1 SHOW DAILY by DIGITAL MARKETING + ADVERTISING + VIDEO PRODUCTION + MEDICAL WRITING + EVENTS Request our 2023 Media Kit Now! Write enquiry@mediamice.com for a copy HQ Office: 6001 Beach Road, #09-09 Golden Mile Tower, Singapore 199589 Phone: +65 8186 7677 Satellite Office: 2 Nuoc Man 2 Street, Da Nang City, Vietnam 50506 Phone: +84 868 063 773 E-mail: enquiry@mediamice.com Web: www.mediamice.com

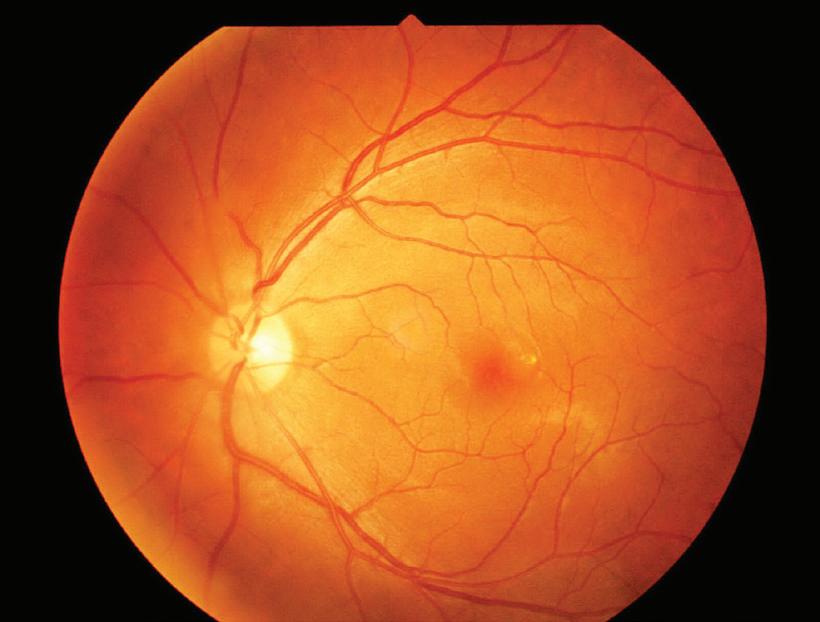
































































































































































































































































 by Tan Sher Lynn
by Tan Sher Lynn






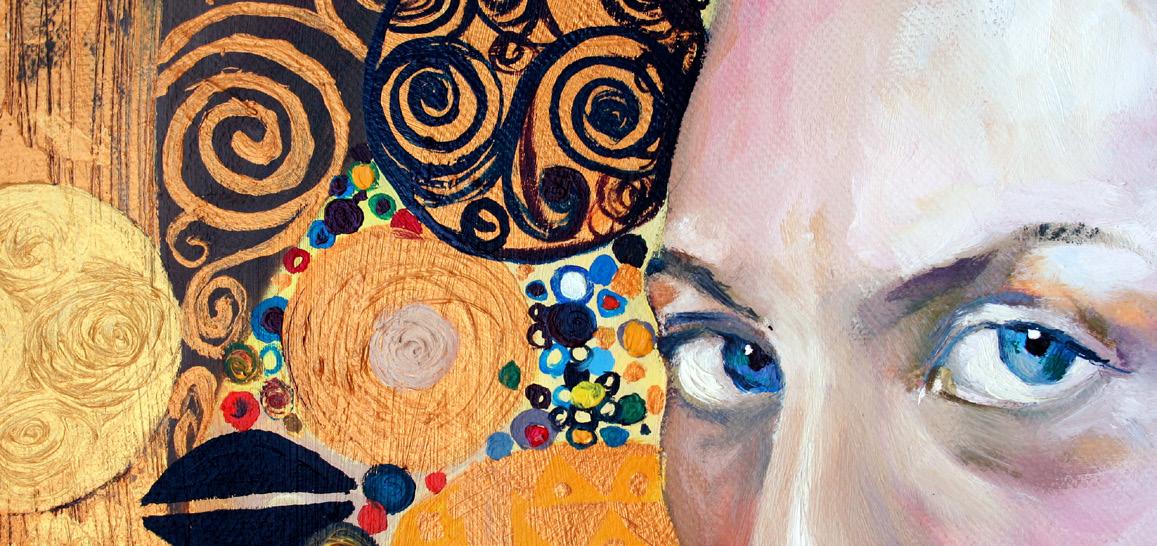









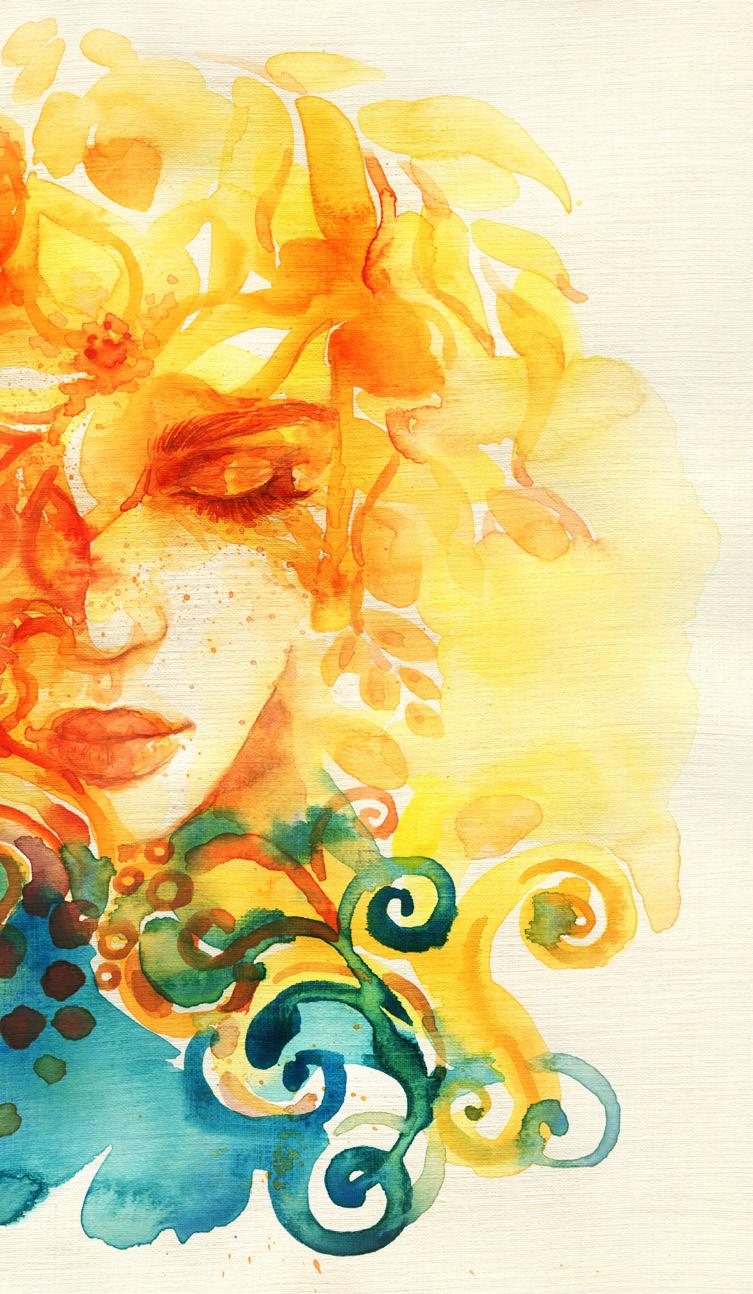


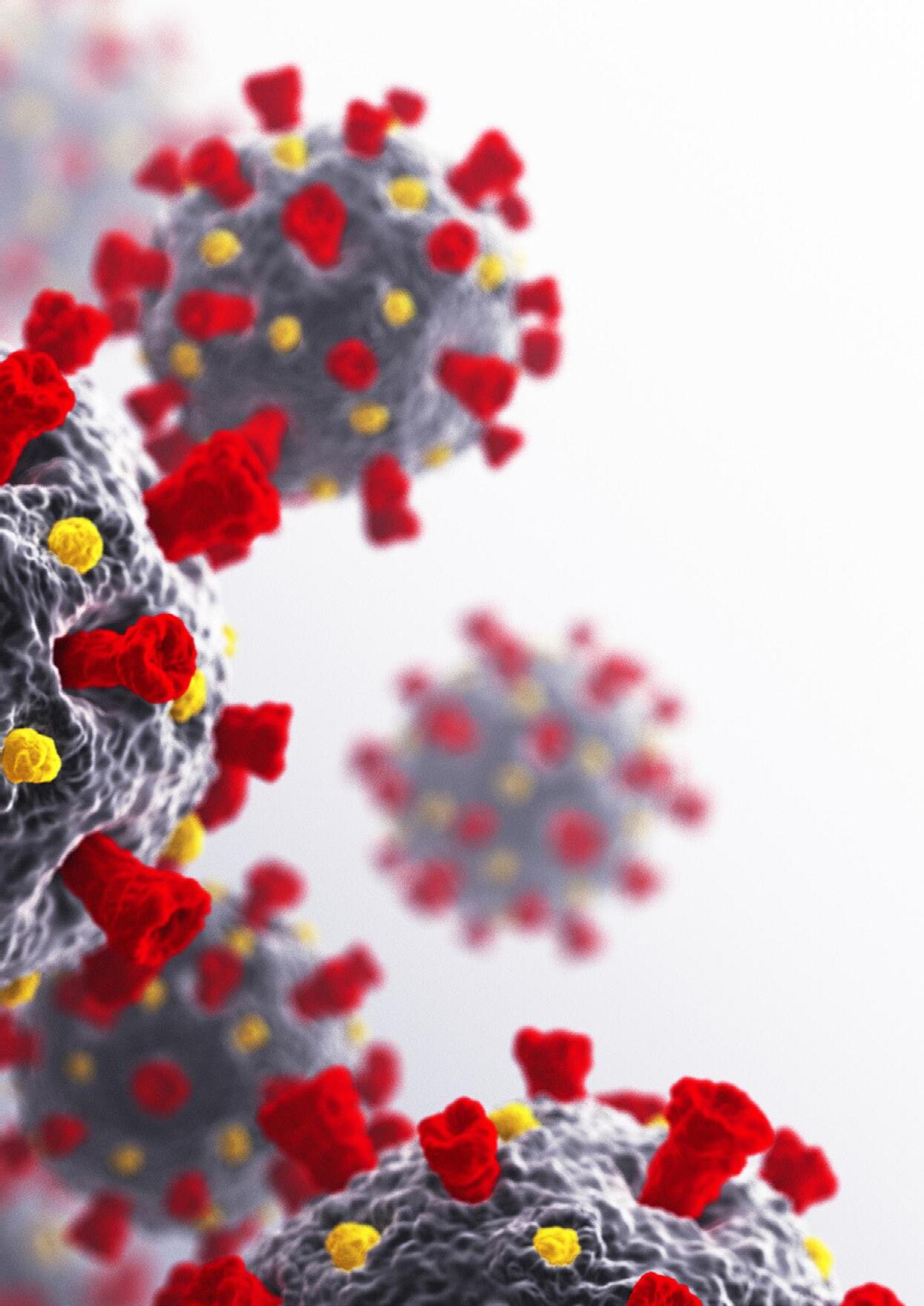










 Matt in Jena.
Matt and Robert in Morocco.
Matt begins experiencing symptoms of coronavirus (COVID - 19) the night before he tests positive. They include mild headache, mild backache, shortness of breath, and phlegm. There was no fever in his case.
Matt in Jena.
Matt and Robert in Morocco.
Matt begins experiencing symptoms of coronavirus (COVID - 19) the night before he tests positive. They include mild headache, mild backache, shortness of breath, and phlegm. There was no fever in his case.







 by Brooke Herron
by Brooke Herron



 by Khor Hui-Min
by Khor Hui-Min




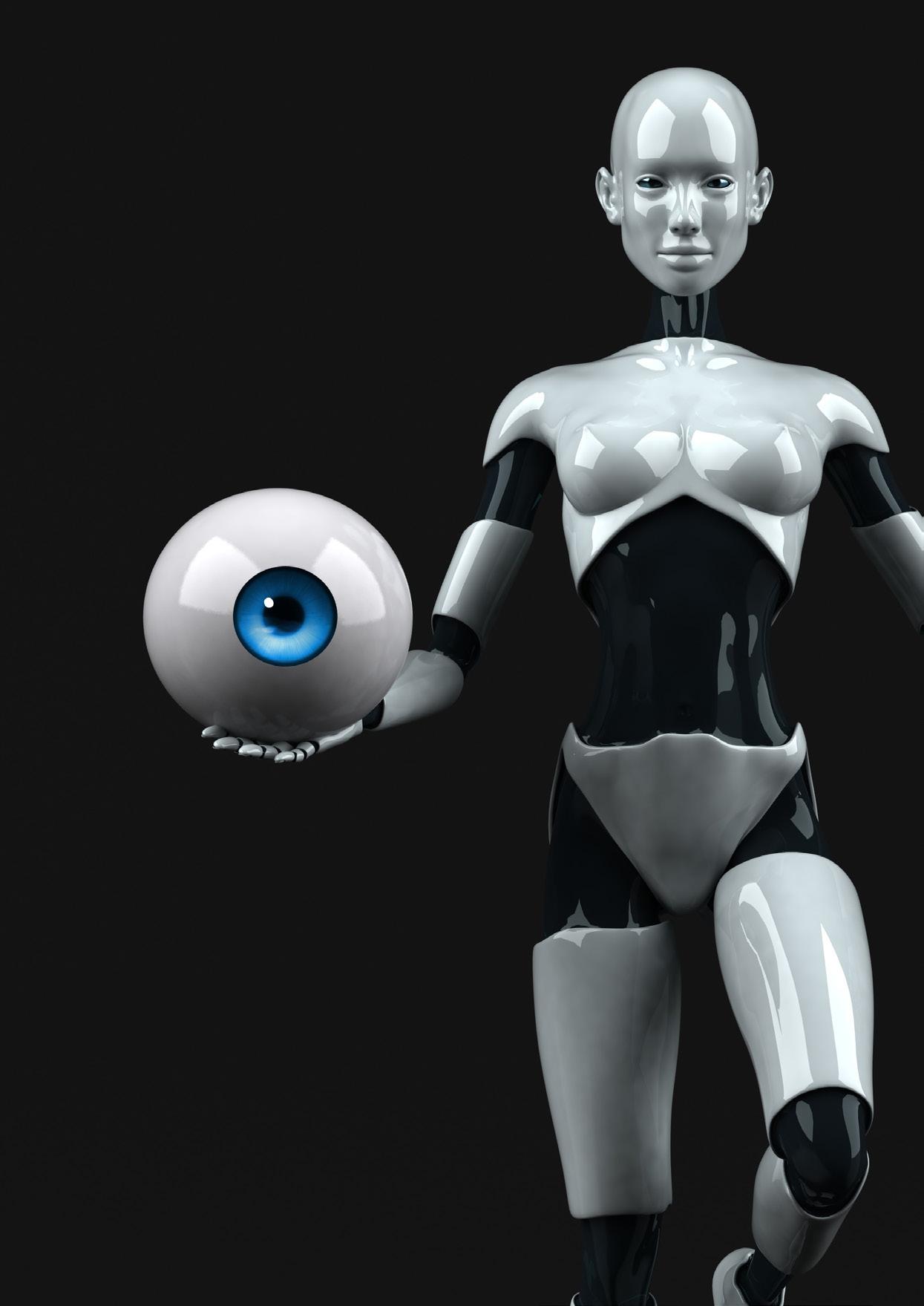 by Tan Sher Lynn
by Tan Sher Lynn