The latest breakthrough in enzymatic pre-cleaning sprays, Prepzyme® Forever Wet’s unique humectant properties form a moist coating over the instruments that lasts for days.

•The humectant formulation creates a moisture retention barrier which keeps soiled instruments and scopes moist for a prolonged period of time – unlike a GEL which HAS NO MOISTURE RETENTION properties
•Operating room safe, non-aerosol, multi-tiered enzymatic spray helps prevent bio-burden from drying on the surface of soiled instruments and scopes
•Ideal for transporting soiled instruments that may sit for an extended period of time
•Reduces tray weight during transport compared to liquid presoaks
•Soiled sharps are visible through humectant
• Decreases spills and potential cross-contamination
A simple & effective way to protect personnel, patients and the environment from contaminated sharps
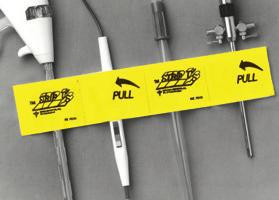
Cover biohazard symbols on SST Tray Systems with a 4”x 4” Removable Clean Label







TRANSPORTATION IDENTIFICATION TAG
2 in 1 removable label for effective communication


UltraSAFE is an innovative instrument for large biospecimens which allows Perioperative Nurses to handle Pathology specimens in complete safety, with no exposure to formalin fumes. Through the one-way valve lid, UltraSAFE automatically dispenses formalin into specimen buckets utilizing an automatic injection system. The buckets are filled in an enclosed and vented chamber that eliminates operator exposure to formalin fumes. Formalin is dispensed based on specimen weight and specific lab guidelines. Time to fixation, weight of specimen, and exact formalin quantity are recorded on a printed label to ensure standardized documentation.







Formalin has been proven to be carcinogenic and detrimental to human health. Yet, OR personnel are exposed to formalin fumes on a daily basis.

In the past year, Congress has been holding hearings and discussing various proposals purported to decrease the cost of health care; guarantee safe, high-quality care for patients and ensure patient access to care. States and other stakeholders have also been asking questions about current practices and considering alternatives to achieve those same goals.
As we consider what all that means for surgery centers and other health care providers, one overarching theme emerges: the devil is in the details. On the surface, many of these proposals sound like simple fixes to complex problems. In fact, many exacerbate the very problems they are intended to address, and others create new, seemingly unanticipated, problems.
Price transparency has been the hottest topic on Capitol Hill this past year impacting ASCs and provides a good example of how wellintended efforts can go sideways. It is easy to agree that patients should be able to determine the cost of an elective surgical procedure or preventive screening before deciding whether and where to obtain that
care. The difficulty is determining the simplest way to help them obtain all the information they need to make an informed choice.
Since being the lower cost site of service has been a defining element of the ASC model, surgery centers have always worked with their patients to help them understand the cost of their procedure. The No Surprises Act enacted in 2020 builds on this to prevent surprise medical bills by requiring all health care providers to give, upon request, a good faith estimate to patients for the care they are considering. However, regulations to fully implement these requirements have still not been finalized.
Even though the No Surprises law is still a work in progress, members of Congress now want to require providers to post prices for their services on their websites or face very substantial financial penalties. Leaving aside the practicality of patients going to various websites to price shop, it’s frustrating to see new requirements being proposed when the old ones haven’t yet been implemented or evaluated. Hopefully, cooler heads will prevail, and Congress will let the No Surprises law be fully executed before making providers waste time and money on additional solutions.
Site neutral payments are another topic that has gotten a lot of attention on Capitol Hill recently. This is another area where good intentions don’t automatically translate into good policy. At first glance, it seems sensible that health care procedures should cost the same no matter where provided. Unfortunately, that theory does not work well in practice and would create significant barriers to access to care. Both hospitals and surgery centers allocate significant resources to compliance with the regulatory requirements that apply in their facilities. Physicians’ offices, on the other hand, do not need to meet those same criteria and, therefore, can provide certain procedures at a lower cost but with trade-offs on safety that limit the types of patients that should receive care there.
Determining when the more highly regulated environment is the right setting for a patient is a clinical decision that must be made by the patient and their physician. Any site neutral policy that attempts to use an arbitrary mathematical formula – such as where patient volume is predominant or a plurality – to determine which site of service’s fee schedule should ap -

ply for all settings could cause the more highly regulated providers to discontinue offering those procedures and force patients into a less appropriate setting.
Quality measurement and reporting is another area where, despite many well-intended efforts, the goal of providing a single comprehensive set of meaningful data that improves the patient experience remains elusive. The ASC community has long supported quality reporting and continues to develop meaningful measures for surgery centers and their patients.
As measures continue to be added to the program, however, the specific contents and requirements associated with each measure need to be considered carefully to balance their value against the burden of reporting. Administratively burdensome measures can quickly drive up the overall cost of care. Reporting demands can also effect efficiency, one of the attributes of surgery centers physicians and patients say they value most.
As an example, the Centers for Medicare & Medicaid Services (CMS) currently requires ASCs to report data monthly on the COVID
vaccination status of their health care workers. Implementation has been confusing, with definitions constantly changing midstream. The COVID-19 Public Health Emergency ended on May 11, 2023. Facilities have never been required to collect the vaccination status of their patients and guests, and many health care facilities no longer require their patients and guests to wear masks. And yet, surgery centers and other health care facilities must continue to report on HCP vaccination status monthly to avoid penalties. It is difficult to claim it is a matter of epidemiology when we do not know the vaccination status for a sizable number of the individuals coming through the facility daily, including the patients undergoing surgery. ASCA continues to ask for this measure’s removal, or at least a reduction to reporting annually instead of monthly.
Anyone who works directly with patients in a surgery center would have a difficult time also tracking and responding to these critical policies as they arise. ASCA represents your interests in all these efforts and many more. If you work
in an ASC, please make sure your facility’s membership is current in 2024 and contact Maia Kunkel at mkunkel@ascassociation.org if you would like to explore some ways to get more involved with ASCA and its advocacy for surgery centers.
Before I sign off, I have one reminder for the ASC community. In 2025 Medicare-certified ASCs need to conduct the Outpatient and Ambulatory Surgery Consumer Assessment of Healthcare Providers and Systems (OAS CAHPS) Survey or face future cuts in their Medicare payment rates. Surgery centers must select an approved vendor to administer the survey to their patients.
Finding the right vendor and setting up the survey takes time, and with thousands of ASCs preparing to begin working with a limited number of approved survey providers simultaneously, ASCA is encouraging all ASCs to start now. To help, ASCA has posted a collection of OAS CAHPS resources on our website at www.ascassociation. org/oas-cahps We invite all ASCs to use the information available there.
he December 2023 issue featured an ethics-focused article addressing the role of credentialing organizations in upholding ethical standards and fostering accountability. This month’s follow-up article explores the ethical landscape within the nursing profession, including general expectations for conduct, national and state level resources, and information about reporting alleged violations.
TSpecialty nursing certifications not only enable nurses to expand their knowledge, skills, and expertise but also open doors to advance career opportunities. These certifications possess distinct characteristics, including additional training requirements, expiration after a specified duration, and renewable status upon meeting specific conditions. The United States boasts a robust and diverse representation of nursing specialty certifications.
The conversation about nursing certification, standards of practice, and accountability begins with an overview of the oversight structure.
Regulation practices vary widely, encompassing international, national, state and individual credentialing organizations.
On an international level, the American Board of Nursing Specialties (ABNS) plays a pivotal role in improving patient outcomes and consumer protection by promoting quality nursing certification. With a membership comprising 73 member organizations, ABNS represents almost 930,000 certified registered nurses worldwide (ABNS, 2020).
At the national level, the National Council of State Boards of Nursing (NCSBN) serves as the primary regulatory board for nursing. NCSBN’s mission revolves around ensuring safe and competent nursing care through effective regulation, practice and education. By empowering nursing regulators across the nation, NCSBN strives to protect the public’s health and welfare. Collaborating with Nursing Regulatory Bodies (NRBs), which issue licenses, outline standards, and monitor compliance, NCSBN oversees the safe practice of nursing. Currently, 59 NRBs operate in
the United States, all being members of NCSBN. Another important function of not only this regulatory board, but also of specialty certification boards, is a mechanism for verifying credentials (e.g. NURSYS; NCSBN, 2023).
While the NCSBN has a national purview, individual jurisdictions enact Nurse Practice Acts (NPA) enforced by their respective NRBs.1 These laws encompass qualifications for licensure, allowable nursing titles, scope of practice and consequences for non-adherence to the law (NCBSN, 2023). Compliance with these laws and regulations is required for the maintenance of nursing licenses. The Nurse Practice Act Toolkit links users to their State Boards of Nursing (BON), where they can then locate their NPA. BONs embed accountability mechanisms for regulation of practice within their states, and the processes for intake of complaints therefore varies by jurisdiction. Each state BON regulates and oversees nursing practice in their state by enforcing state nursing laws and disciplining nurses

who violate these state standards and laws.
In addition to national and state obligations, individual credentialing organizations often establish ethical codes of conduct for their certificants. As an example, the Competency & Credentialing Institute (CCI) maintains a Code of Ethics, which details ethical responsibilities of CCI certificants and addresses regulation of practice, misuse or misrepresentation, and potential sanctions. CCI also provides a mechanism to report an alleged ethics violation of CCI’s ethical policy and procedure requirements through self-reports or reports concerning another nurse.
Some general guidelines for possible reasons to report an alleged ethical violation may include:
• Falsification of information and/or documentation
• Failure to maintain required licensure
• Gross negligence
• Commission of a crime
• Misrepresenting the status of a credential
• Cheating on an exam
• Violating policies or procedures
• Engaging in conduct unbecoming of the profession.
While the specific expectations of licensing boards may differ, the underlying ethical principles of the nursing profession remain steadfast. The American Nurses Association Code of Ethics stipulates the values and ethical responsibilities of the nursing profession in general. These components are vital in sustaining the integrity, reliability, and trustworthiness of the profession, which in turn benefits patients, the public, and other stakeholders alike.
Sources:
• ABNS: https://www.nursingcertification.org/
• NCSBN: https://www.ncsbn.org/ boards.page
• CCI Ethics Webpage: https:// www.cc-institute.org/ethicspolicy/
• ShiftMed: https://www.shiftmed. com/blog/complete-list-of-specialty-nursing-certifications/
• ANA Code of Ethics: https:// www.nursingworld.org/practicepolicy/nursing-excellence/ethics/ code-of-ethics-for-nurses/

https://www.ncsbn. org/nursing-regulation/ about-nursing-regulatory-bodies.page
– Melissa R. Nosik, Ph.D., BCBA-D, ICE-CCP, SHRMSCP is the chief executive officer of the Competency & Credentialing Institute. Lisa Rosenfield, MA, serves as the accreditation and compliance manager at the Competency & Credentialing Institute.

- Mai-Linh King, MS, BCBA, CPTM is a consultant for Spark LLC working with the Competency & Credentialing Institute.

S everal surgical markets are expected to grow in coming years. The predicted growth of thee markets suggest that the surgical instrument storage market also has potential to increase over the years.
According to a Towards Healthcare report, the ambulatory surgical centers market was accounted for $87.32 billion in 2021 and is predicted to increase at $152.6 billion by 2030 and poised to grow at a compound annual growth rate (CAGR) of 6.4% from 2022 to 2030.
Transparency Market Research reports that the surgical kits market will exceed $40 billion by 2031.
Mkt Reach states that the closed surgical case carts market is expected to witness steady growth during the forecast period (ending on 2031), with a CAGR of 10%. The increasing number of surgical procedures, technological advancements, and the need for efficient instrument management are driving the market’s growth.
A Mordor Intelligence report states that the global surgical case carts market size is estimated at $415.36 million in 2024, and is expected to reach $590.5 million by 2029, growing at a CAGR of 7.29% during the forecast period (2024-2029).
“The COVID-19 pandemic and numerous advisories from the respec-
tive government regarding surgical procedures led to a significant decrease in surgical procedures around the world. For instance, according to the study published in PLOS One, in August 2022, the quaternary care facility successfully dealt with the COVID-19 pandemic’s pressures by significantly reducing the number of surgical procedures performed during the peak of the pandemic. However, despite uneven recovery rates across subspecialties and case classes, total surgical procedure volumes did not fully return to pre-COVID-19 levels until well into 2021. This has impacted the adoption of surgical case carts due to the reduced number of surgeries during the pandemic,” the report states. “However, the number of surgeries increased after the initial decline during the pandemic, and it is expected that the studied market will bounce back to its full potential in the coming years. For instance, according to the research study published in Frontiers in Surgery, in December 2021, there was a 48.0% decrease in total surgical procedure volume immediately after the March 2020 recommendation to cancel elective surgical procedures. However, after the reopening, the rate of surgical procedures rebounded to pre-pandemic levels, and the trend was maintained throughout the peak burden of patients with COVID-19 in the fall and winter in the United States. This shows that the
number of surgical procedures is expected to reach a pre-COVID level soon, and the studied market is expected to grow over the forecast period. Certain factors that are propelling the market growth are the increasing number of surgeries and rising health care infrastructure.”
A post on Medium.com says the future of the operating room cabinets market is “expected to be positive.”
“The increasing number of surgeries and the rising demand for efficient storage solutions in operating rooms are driving market growth. Additionally, advancements in technology have led to the development of innovative cabinet designs with features like automated inventory management systems, antimicrobial coatings, and RFID tracking, which further contribute to the market’s expansion,” the post states.
The Medium.com post also states, “Furthermore, the global market for operating room cabinets is projected to grow at a CAGR of 6% during the forecasted period. This growth can be attributed to factors such as the increasing number of surgical procedures, advancements in health care infrastructure, and the rising adoption of technology-driven storage solutions. The market is highly competitive, with key players focusing on product innovation and strategic partnerships to gain a competitive edge.”
Miltex Instrument Cassettes, distributed by Henry Schein Medical, are manufactured with passivated stainless steel and are available in a variety of sizes and configurations to meet all storage needs. The cassettes also feature a double-hinged, “Tuck-Away” lid that folds under for easy storage during use. This ensures that the lid is not misplaced during procedures, saves valuable space over single-hinge lids, and provides an incline for better instrument viewing and access during procedures. Silicone strips and mats are also available to assure instrument adhesion and retention when the lid is closed. These soft cushion options are customized to fit perfectly into Miltex Cassettes and protect your instrument investment long into the future. To learn more, please visit HenrySchein.com/ASC. To speak with a Henry Schein Medical Sales representative, call 800-772-4346.


The HEMCO Acid Storage Cabinet is specifically designed for the storage of corrosive chemicals and is available in 12”, 18”, 24”, 30”, 36”, 42”, and 48” widths. Standard size is 35” high and 22” deep. The molded one-piece fiberglass liner inserts directly in the cabinet and is sealed on all edges for ease of cleaning. Interior features a containment lip, on the front bottom edge to hold spills. The front access doors have air inlet vents, are lined, and the edges are sealed. No metal is exposed to corrosive vapors. Shelf is removable for smaller container storage.
Medline’s Steriset container is used to sterilize, store and transport surgical instruments to the operating room. It is the only sterilization container on the market that is 100% reusable. The Steriset has four premium features: double lid protection, stainless steel pressure-activated valve, tamper-evident heat-activated ThermoLoc, and an optional temperature-activated condensate drain for heavy loads. With its unique container technology, the Steriset eliminates human error and hygienic security risks that come with traditional filtered containers and sterilization wrap. Each Steriset container has an average lifespan of 10-12 years and has a lifetime warranty on the premium features, providing long-term, eco-friendly cost savings.


CIVCO’s Ultrasound Probe Storage Cabinet provides a safe and clean environment for disinfected ultrasound probes. A fan draws air through a replaceable HEPA filter for continuous clean air flow using positive pressure. The system’s specialty shelves protect delicate probes from damage and vertical suspension facilitates drying. A 2022 study uncovered a very low risk of pathogenic bacterium growth on ultrasound probes 30 days after high-level disinfection when stored in the CIVCO Storage Cabinet.
For more information, visit civco.com.
Introducing Aesculap’s newest sterilization powerhouse – the AESCULAP Aicon Sterile Container System. With features that help streamline processes and reduce the possibility of wet sets, Aesculap’s next generation rigid container is everything you’d expect from the market leader. The new AESCULAP Aicon Container delivers greater sterility confidence, 100% container and basket synchronization, up to a 47 percent less dry time with the Enhanced Drying System1 and up to a 200 percent increase in sterile aseptic area.2
1 Based on FDA Claims. Data on file.
2 Data on file.

KARL STORZ No-Wrap Sterilization
Containers help realize cost savings while protecting equipment investment and reducing the environmental impact of reprocessing. These custom designed containers are a trusted system for protection of endoscopic instrumentation during sterilization, transport and storage. KARL STORZ wrap-free containers provide effective sterilization while reducing waste and enhancing efficiency by eliminating the need for traditional medical blue wrap required for use with traditional sterilization systems.
For more information, visit karlstorznetwork1.com/cleaning-and-reprocessing.


The Pegasus Hygieia Rack System is an 100% aluminum sealed structure with no open holes, movable shelves without tools and standard rails and heavyweight telescopic slides. It features high-density, flexible storage for greater capacity without stacking, protecting packs. Optional add-ons include NoTouch system with built-in handles and silicone pads that virtually eliminate human handling during reprocessing. Stainless shelves/baskets resist contamination and go directly into the autoclave and CSPS container storage system that maintains sterility during SPD to OR transport with ergonomic shelves to access the heaviest containers and helps protect packs from tears. Salus Trolleys provide lightweight, durable transport.


Like
idea of light-based disinfection, but uncomfortable
UV? Indigo-Clean kills MRSA, C Diff and a range of other pathogens—even in shadowed and hard-to-reach areas—safely, with no room downtime.
Indigo-Clean is clinically proven to:
• Kill 88% of harmful bacteria, including MRSA & C. Diff
• Reduce SSIs by 73%
• Kill 94% of SARS-CoV-2 & Influenza A
• Certified safe: ‘Risk Exempt’ per IEC Standard 62471
* Murrell LJ, Hamilton EK, Johnson HB, Spencer M. Influence of a visible-light continuous environmental disinfection system on microbial contamination and surgical site infections in an orthopedic operating room. Am J Infect Control. 2019; 47(7):804-810. doi:10.1016/j.ajic.2018.12.002




•
•
•
•

• Keeps sterile tethered appliances on the surgical field from falling to the floor with 4 hook & loop closures
• Latex free self adhesive back for attachment to the surgical field
• Economical - Saves pre-op time
• Several sizes, configurations, colors
• Sterile shelf life 2 years
•











Electro Lube™ anti-stick solution is clinically demonstrated to keep tissue from sticking to electrosurgical instrumentation during use, leading to less tim e spent on handbacks to remove eschar buildup during the procedur e. Electro Lube is packaged sterile, and ready to use. To obtain samples and schedule a product trial at y our facility, visit www.steris.com/healthcare.


Periop ConneCT, a premier event for Perioperative RNs, CSTs, and SPD professionals in Connecticut and the Northeast, is seeking dynamic presenters and/or poster presentations for its upcoming conference. We invite you to share your expertise and insights with our attendees on the following engaging topics:
1. Patient Advocacy/ Patient Safety: Illuminate best practices, case studies, and strategies for enhancing patient advocacy and safety in perioperative care.
2. Clinical Innovations/ Adapting to New Technology: Explore the latest advancements in clinical practices, surgical technologies, and methods to seamlessly adapt to emerging innovations in the perioperative field.
3. Personal and Professional Development: Empower attendees with valuable insights on personal and professional growth, offering practical tips, mentorship stories, and effective strategies for career advancement.
4. Diversity, Equity, and Inclusion in the Workplace: Contribute to the dialogue on fostering a diverse, equitable, and inclusive perioperative environment. Share experiences, successful initiatives, and strategies to promote a more inclusive workplace.



 By don sadler
By don sadler
The hybrid operating room is an emerging trend in health care that is worth paying attention to. Hybrid ORs offer significant benefits to both patients and hospitals.
“Several factors are motivating hospitals to build or consider building hybrid ORs,” says Anthony Borrelli, executive director of endoscopy product and marketing with FUJIFILM Healthcare Americas Corporation. “This starts with return on investment as providers have started to recognize the cost savings and ROI that come with implementing a hybrid OR.”
A hybrid OR is a state-of-the-art space that combines a traditional operating room with an image guided interventional suite. Equipped with both surgical equipment and instrumentation, along with dedicated advanced imaging modalities, hybrid ORs are designed to accommodate traditional surgical, minimally invasive and interventional procedures in the same space.
David Lyons, MD, FASA, Member, American Society of Anesthesiologists Committee on Facilities and Equipment and Division Chief, vascular anesthesiology at the University of Rochester Medical Center, explains that hybrid ORs are designed around permanently installed imaging hardware.
“This provides superior capabilities to mobile equipment, but also significantly impacts the OR space in terms of flexibility of configuration and positioning of equipment and personnel,” says Lyons.
Renee Hildebrand, MSN, CSSM, CNOR, RNFA, the director of perioperative services for Texas Health, has been involved in the construction of two hybrid ORs.
“Hybrid rooms raise the bar when it comes to department advancement and technology,” she says. “If used correctly, they’re a one-stop shop for a patient who might have required several different procedures in different departments.”
Anecdotal evidence indicates that there are only about 100 hybrid ORs in the U.S. today. However, this number is expected to increase significantly over the next decade because of a surge in patient population and growing number of interventional imaging procedures and minimally invasive surgeries.
According to Transparency Market Research, the global hybrid operating room market is expected to grow at a CAGR of 7.7% between now and 2031, reaching $1.8 billion. The report attributes this growth to a rise in the number of surgical procedures that will be performed worldwide during the forecast period.
Vasant Jayasankar, MD, MS, FACS, assistant clinical professor of surgery at Medical University of South Carolina and medical director of cardiac and thoracic surgery at AnMed Medical Center, has utilized hybrid ORs for a variety of complex vascular and cardiac procedures.
“These include transcatheter aortic valve replacements (TAVRs), endovascular AAA repairs, and hybrid open/endovascular procedures,” says
Jayasankar. “The main benefit of a hybrid OR is the highresolution advanced imaging capabilities, which are far superior to the traditional C-arm technology utilized in traditional ORs.”
Another benefit, says Jayasankar, is the ability to perform complex open surgeries that can’t be performed in traditional catheterization labs.
“This gives the surgeon and staff the benefits of both environments without the downsides,” he says. “And patients benefit from their providers being able to perform more advanced and complex procedures.”
Renae Wright, DNP, RN, CNOR, perioperative practice specialist with the Association of periOperative Registered Nurses (AORN) and lead author of the AORN Guideline for Minimally Invasive Surgery, points to another key benefit of hybrid ORs: a potentially shorter time to treatment.
“For unstable trauma patients, hybrid ORs offer the opportunity for concurrent imaging and operative procedures,” says Wright. “This eliminates the need for patient transport between the imaging and procedural areas because the two areas are combined into one space. And patients undergoing minimally invasive procedures could experience a shorter hospital stay and recovery, as well as less discomfort.”
Hospitals benefit from improved patient throughput since hybrid ORs can reduce or eliminate time spent waiting or in transport between imaging and procedural areas.
“There are also likely some perceived benefits associated with being able to market that you have a hybrid OR, which could attract surgeons and community attention,” says Wright.
According to Rob Fabrizio, director of strategic marketing and diagnostic imaging with FUJIFILM Healthcare Americas Corporation, a key benefit of hybrid ORs is that they drive collaborative care.
“The hybrid OR is designed for multiple specialties to work together, with imaging equipment and surgical systems all in one space,” says Fabrizio. “So, a trauma patient might receive a CT scan of the head to rule out a brain bleed while a vascular surgeon addresses his abdominal hemorrhaging or a neurosurgeon addresses his spinal injury.”
“The clinical team can work in tandem,” Fabrizio adds, “which drives the best possible collaborative care. In trauma cases, this collaborative care can be lifesaving.”
Borrelli stresses the efficiency and cost saving benefits of hybrid ORs.
“For example, if surgeons begin a laparoscopic procedure but need to suddenly switch to open surgery or endoscopic/endoluminal exploration, they can do so
in a hybrid OR without moving the patient to another room,” he says. “This also improves patient safety.”
Health care providers also benefit from hybrid ORs since there’s less setup time and nurses and technologists can focus on the procedure and the patient, rather than the equipment.
Clinical teams can address more than one problem on the same patient in a hybrid OR, which leads to shorter recovery times.
“Studies have shown that patients undergoing procedures in a hybrid OR experience less risk of procedural complications and infections and reduced OR time because they don’t need to be transferred between procedures,” says Borrelli.
The biggest potential disadvantage of hybrid ORs, says Jayasankar, is that the imaging tables don’t allow for the full freedom of movement in three dimensions that a traditional operating table allows.
“This can make certain open procedures more challenging to perform in these environments,” he says.
Otherwise, the biggest drawback of hybrid ORs tends to be the initial cost of building them, along with the space requirements and staff and training expertise needed to operate them. A traditional OR is about 700 square feet but a hybrid OR requires 1,000 to 1,200 square feet to accommodate the imaging equipment, control room and separate clinical teams.
“Once these details are worked out, I don’t see any significant drawbacks to adding a hybrid OR,” says Fabrizio.
“Launching a hybrid OR is a big undertaking that requires a significant resource commitment on the part of the health care institution,” says Borrelli. “However, once the new suite is up and running, the benefits appear to be worth the investment.”
The cost of building and maintaining a hybrid OR may make them prohibitive for rural hospitals that might not have the resources.
“It also depends on the types of procedures that will be performed in the operating room,” says Wright. “Utilization of the hybrid OR could be low or it could very much be in high demand.”
“The last thing you want is an expensive hybrid OR sitting empty,” says Hildebrand.
Borrelli notes that hybrid ORs can get crowded because of the need for additional equipment and staff.
“So, it’s important to choose the right technology,” he says.
Fujifilm’s ELUXEO Surgical System allows physicians to swiftly adjust their endoscopic imaging tools, which eliminates the need for multiple equipment towers. “This makes the system a space saver and problem solver in the hybrid OR,” he says.
“Studies have shown that patients undergoing procedures in a hybrid OR experience less risk of procedural complications and infections and reduced OR time because they don’t need to be transferred between procedures.”
- borrelli

As you begin the hybrid OR planning process, identify your goals for the hybrid OR, your budget for the project and what types of procedures will be performed in the space.
There’s a growing list of procedures that can be performed in hybrid ORs, including many cardiac procedures that have previously been done in a cath lab. Newer procedures being performed in hybrid ORs include TAVRs, mitral valve clipping, endoscopic abdominal aortic aneurysms and aortic arch repairs.
“Hybrid ORs allow practitioners to perform a wide range of procedures in the same environment,” says Jayasankar. “Standalone catheter-based procedures, hybrid open and catheter-based procedures, and traditional open procedures can all be done in the same room.”
Most hybrid ORs include a single-plane angiographic X-ray imaging system along with surgical equipment for open cardiac surgery. Lights must have a longer arm reach and light and boom placement must allow anesthesia staff access to the head of the table. C-arms can be either ceiling- or floor-mounted, depending on what procedures will be performed in the room.
If most procedures will be interventional, the OR table should communicate with the imaging system, but this generally isn’t necessary if the room will serve primarily as an OR. Some tables feature two tabletops: one for imaging and one for surgical procedures.
The hybrid OR should include both a live and reference monitor, along with displays at the OR table for surgeons and surgical assistants and wall displays. Well-funded hospitals may have a dedicated wall just for imaging.
Based on her experience, Hildebrand offers a number of crucial factors to consider in the planning and construction of a hybrid OR, including the following:
• Room layout: The control room needs to have full visibility of the entire patient. “Many rooms have
built-in support columns that can’t be moved,” says Hildebrand.
• In-room storage: Hildebrand recommends including a storage room off one end of the hybrid OR for perfusion supplies in case you have to convert to a cardiopulmonary bypass case.
• Strategic placement of items: These include glove boxes, outlets, hand gel, clippers, white board, X-ray apron hanging posts and the surgical pause poster. “The exact placement of these items sometimes isn’t planned for until the end of the project, so they’re just put wherever there’s room, which often isn’t the best place for them,” says Hildebrand.
• Booms and lights: Make sure OR lights don’t interfere with the C-arm or booms. “And if booms are placed in the room, make sure they don’t conflict with the C-arm and monitors,” says Hildebrand.
• Bed selection: This is critical, says Hildebrand, “because some beds can interfere with the C-arm range of motion.”
• Floor color: Hildebrand recommends any floor color except blue, because “most hybrids are vascular in specialty and the primary suture used in vascular cases is blue.”
Wright stresses that developing a successful hybrid OR program involves more than just the design and construction of the room. It also requires developing and training perioperative team members who will work in the space.
“Team members must be comfortable with the needs of the patients receiving care in the space and know how to use the room’s technology and equipment,” says Wright. “It is the responsibility of the interdisciplinary team tasked with developing and
overseeing the program to make sure there is a plan in place for hybrid OR team training.”
Jayasankar believes that perioperative team members need to have a good understanding of both the open surgery world and the catheter world.
“It can be challenging to master all aspects of both types of procedures, but I think it’s important to make the effort to learn as much as you can,” he says.
According to Lyons, there are key differences between providing anesthesia in a hybrid OR compared to a traditional OR. These are related to patient access, patient positioning and equipment positioning.
“The C-arm must be free to move, which can substantially limit physical access to the patient during the procedure,” Lyons explains. “The anesthesiologist must take this into account and ensure that all the monitors and vascular access devices are in place and appropriate for the full range of possible procedures, including endovascular or open surgery.”
“Additionally, all anesthetic and monitoring equipment must be positioned to accommodate the motion of both the patient and imaging equipment,” adds Lyons.
Another anesthesiology consideration is the fact that an angiography table typically used in a hybrid OR is limited in its mobility compared to a regular OR table. “Specifically, they are unable to flex or raise the back into a ‘beach chair’ position,” says Lyons. “Appropriate patient positioning is an important part of inducing anesthesia safely – it has a significant impact on ventilation with a face mask and the placement of a breathing tube.”
Lyons points out that the advanced imaging systems in hybrid ORs allow many procedures to be performed under sedation rather than general anesthesia.
“However, conditions can change rapidly and there may be a medical need for general anesthesia after the procedure is underway,” he says. “Given the physical restrictions of the hybrid OR, it’s important to have a plan for how this will be executed.”
Hildebrand stresses the importance of teamwork when it comes to hybrid OR success. “There’s often a collaboration between different departments, such as the OR and cardiac cath or interventional radiology departments,” she says. “Simulations prior to a go-live date are critical with the entire team, including anesthesia and surgeons/proceduralists.”
Fabrizio stresses that a hybrid OR is only as good as the technology in the room.
“Choose a reputable technology vendor that offers next-generation imaging equipment and surgical systems with consistently proven dependability,” he says. “Look for high-performing, small-footprint compatible systems and technology that provides multiple uses, along with a vendor that delivers timely support and service.”
Wright believes more research on the outcomes of patients treated in hybrid ORs is needed to guide further development of these spaces, along with research into best practices for workflow.
“This will enable perioperative teams to maximize efficiency and productivity and optimize patient outcomes,” she says.







E
dith

What’s important, though, is not the birth and death years on one’s grave marker.
It’s that dash between the years.
It’s how a person lived during the dash – and Edith Dee Hall lived quite the dash. She might be the most accomplished Kimball native that Kimball doesn’t know much, if anything, about.
“It’s not every day that a little girl from Kimball, Nebraska, helps change the way surgery is done around the world,” said Brenda Ulmer, a renowned perioperative nurse and past board president of AORN, the Association of periOperative Registered Nurses.
Hall was born into a family with roots in Kimball’s pioneer era and graduated in 1915 from Kimball County High School. She moved to, and died in, New York City.
In between is the story of a noteworthy figure in nursing history.
This is Edith Dee Hall’s story.
The reason that Hall’s Kimball connection is being rediscovered is because she founded the Association of Operating Room Nurses, as it was first known, in 1949 and Ulmer – the devoted member of 45,000-member AORN that she is – felt that operating room nurses had much more to know about one of their matriarchs.
“I started searching for more in-depth information on Edith Hall earlier this year



while working on a book update for AORN,” Ulmer told the Observer. “I wanted to include more information about Edith as the founder of AORN. I just felt that we need to know more about her. I also wanted to learn how a woman from Kimball, Nebraska, made it from Kimball to New York City, by way of Washington in the 1920s – an amazing accomplishment.”
Ulmer learned of Hall’s burial in Kimball, and she contacted the Observer in search of an obituary that might have run in the paper.
The Observer did, in fact, run a brief notice about Hall’s graveside services in the April 15, 1971, edition, but it didn’t say much about her life. It mentioned that she was a registered nurse who was born in Kimball, died in New York City and belonged to the Episcopal Church.
Hall’s survivors were identified as half-sister Beatrice Sheahan of New York, brother Alfred Hall of California and Genevieve Dillon of Kimball. Sheahan, by the way, is buried next to Hall.
The report included no reference to Hall’s stature in the nursing profession.
Hall also is missing, at least as a featured subject, from the voluminous 1988 history book “Kimball County Nebraska 100 Years.”
Hall’s very existence is even new to Karen Bivens, a knowledgable student
of local history and board member with the Plains Historical Society.
“I never heard of the lady, but that doesn’t mean anything,” Bivens said. “If she was born and raised here, it shows that no matter where you’re from, even if you’re from a small town, you can achieve great things.”
For Ulmer, piecing together Hall’s journey is a mission.
“As is often the case,” Ulmer reflected, “we don’t know much about the folks who came before us. I was surprised at how little we know about Edith … and how she had the grit to make it from Kimball to New York and accomplish what she did.”
Bivens unearthed information in the Observer from 1915 to 1920 that meshes with some of Ulmer’s findings about Hall, who graduated from KCHS in 1915.
The paper kept up with Hall’s post-high school progression, reporting that she was attending the University of Nebraska at Lincoln in 1917, applied in 1918 to a military training school for nurses, went to work at a New York City area hospital in Newark, N.J., in 1919, and returned to visit her parents for a month in 1920.
Why did Hall became a nurse? Ulmer believes that she found out.
“In response to an outreach by the government during World War I, thousands of women applied to become nurses to support the war
effort,” Ulmer explained. “I found Edith’s brother’s draft card. He was drafted into the Army in 1917. I am still not sure of her path, but it seems like she answered the call to duty.”
Hall was trained and graduated from Walter Reed Hospital in Washington, D.C., and later was operating room supervisor at the New York Polyclinic Medical School and Hospital. She was AORN’s first executive secretary, serving from 1957-62, and in her later years was a consultant and writer for “Hospital Management” magazine.
Ulmer said it looks like Edith spent time at Fort Des Moines Army Hospital before going on to Walter Reed Hospital, which is consistent with an Observer report in 1919 that she was in Des Moines, Iowa.
Hall’s influence on AORN was immense. The year after she died, the organization dedicated its annual conference to her. Her sister, Beatrice, was invited and opened the association’s exhibition hall.
“AORN has been a strong organization almost from the beginning,” Ulmer said. “Our standards, recommended practices and guidelines form the bedrock on which patient care is formed in the United States and around the world.”
Much credit for that goes to Edith Dee Hall, that little girl from Kimball who founded AORN and lived quite the dash.