PRODUCT FOCUS PAGE 34

















PRODUCT FOCUS PAGE 34







To actively listen may be the number one key to improved communication. This is a skill that needs to be honed, and we have to follow some rules to become good at it.
COVER STORY
Healthcare leaders are learning the value that biomedical engineers and imaging technologists bring to project management conversations related to imaging installations and site remodeling.

Rylie Pattison is a leader with growing responsibilities at University Hospitals Parma Medical Center.


Catch up on the latest news from around the diagnostic imaging world.
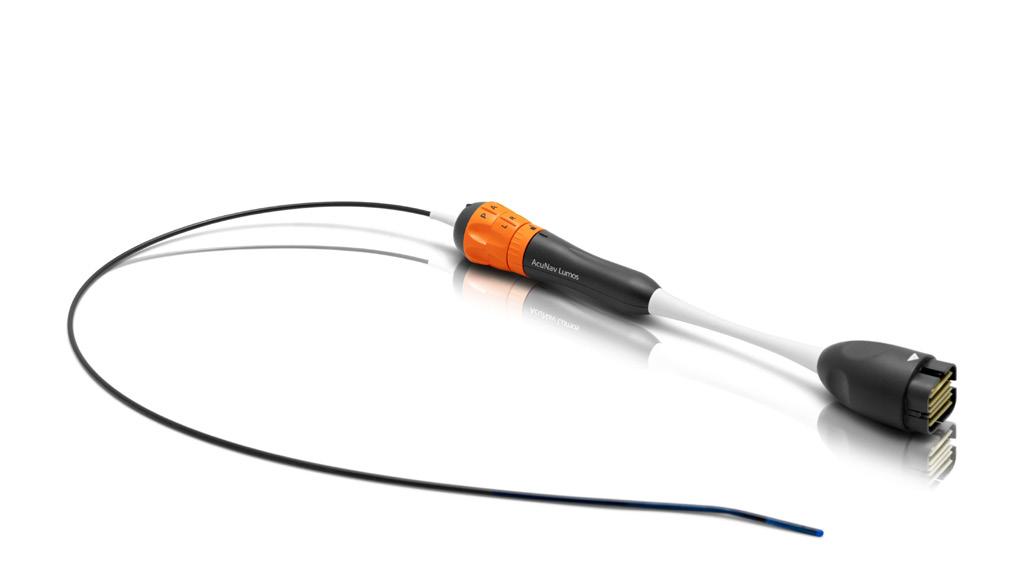
The newest technology and advances in ultrasound transducers are featured.

Connect wisdom from short sayings to personal experiences for value and added impact.
MD
President
John M. Krieg john@mdpublishing.com
Vice
Kristin
kristin@mdpublishing.com
Vice
Jayme
Senior
Megan
Editorial
Editorial
Beth
David
Kimberly
Megan
Jason
Art
Taylor
Alicia
Kristin
Cindy
Kennedy
Haley
Accounting Diane



Ry lie Pattison, CNMT, RT(N)(CT), earned a Master of Science in Radiologic Sciences and a Bachelor of Science at the University of Findlay before embarking on her imaging career. It is a career that already includes leadership responsibilities in her role as team lead nuclear medicine technologist with University Hospitals Parma Medical Center. ICE Magazine recently asked this rising star about her background and her plans for the future.
Q: WHERE DID YOU GROW UP? OR, WHERE ARE YOU FROM?
A: I grew up in Castle Rock, Colorado, located between Denver and Colorado Springs. I lived there until I was 18.
Q: WHERE DID YOU RECEIVE YOUR IMAGING TRAINING/EDUCATION? WHAT DEGREES/CERTIFICATIONS DO YOU HAVE?
A: I began my journey at the University of Findlay where I played collegiate volleyball and discovered my passion for nuclear medicine. There, I attended the Nuclear Medicine Institute, which included clinical training at The Toledo Hospital. After earning my bachelor’s degree and graduating from the Nuclear Medicine Institute, I went on to pursue a Master of Science in Radiologic Sciences at the University of Findlay. I hold certifications in nuclear medicine through
both the Nuclear Medicine Technologist Certification Board (NMTCB) and the American Registry of Radiologic Technologists (ARRT). Additionally, I earned certification in computed tomography (CT) through ARRT.
Q: HOW DID YOU FIRST DECIDE TO START WORKING IN IMAGING?
A: I always joke that I wanted to be a photographer when I was younger – I just found a more roundabout way of doing it. Now I get to take images of the body and its functions, which is even more fascinating. I have always been drawn to the medical field, and during student orientation at the University of Findlay I was introduced to nuclear medicine. All it took was one look through the program brochure for me to realize this was exactly what I was meant to do. As my education and experience grew, I knew without a doubt that I could not picture myself in any other career, which is ironic since I wanted to be a literal photographer.
Q: WHAT IS THE MOST REWARDING ASPECT OF YOUR JOB?
A: The most rewarding aspect of my job is knowing that the work I do has a direct and meaningful impact on patients. Many patients come feeling anxious or scared, and I find it deeply gratifying to provide comfort and compassionate care during that time. Helping them feel at ease while guiding them toward the
answers and care they need is what makes this work so important to me. The greatest compliment I can receive is when a patient says, “Thank you – you made this so much easier for me.” That simple expression of gratitude is what I strive for every day, and it’s what fuels my passion for this profession.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: As a team lead, I feel extremely fortunate to have the opportunity to cultivate a supportive and positive environment for not only my patients, but also for my colleagues. Being able to make a meaningful difference for patients while also using my leadership to empower my team to do the same is both rewarding and something I look forward to each day.
Q: WHAT INTERESTS YOU THE MOST ABOUT THE IMAGING FIELD?
A: What interests me the most about the imaging field is the way that it has transformed patient care. I am amazed each day how the discoveries within radiology allow us to answer complex questions about what is happening inside the body at a much deeper level. It is incredible to watch as technology advances, image quality improves, and new techniques emerge to give us clearer insights than ever before. I find it fascinating that I can inject a patient with a radiotracer and, within moments, map the function of their heart. The imaging field has driven remarkable advancements in medicine and will continue to evolve, offering endless opportunities for learning and growth.

Rylie Pattison discovered her passion for nuclear medicine when she was a student-athlete at the University of Findlay.
Q: WHAT HAS BEEN YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: My greatest accomplishment in my field thus far has been stepping into a leadership role where I can create a positive culture while maintaining the ability to make a meaningful difference in patients’ lives.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: My goals are to continue to learn and grow both as a technologist and as a leader. I have been fortunate to learn from excellent mentors, and I look forward to furthering my knowledge and experience. I aim to strengthen my skills and continue to be positive and compassionate for my patients and for my colleagues. •
FAVORITE HOBBY: Lifting
FAVORITE SHOW: “The 100”
FAVORITE FOOD: Steak
FAVORITE VACATION SPOT: The mountains
1 THING ON YOUR BUCKET LIST: To see the Northern Lights
SOMETHING YOUR CO-WORKERS DON’T KNOW ABOUT YOU: I am currently attempting to learn German.

AdventHealth Heartland Diagnostic Imaging Manager Casie Miller, MHA, CRA, RT(R) CT M ARRT, found her perfect career after first taking a nursing course. It was an injury, of all things, that pushed her toward diagnostic imaging.
“I was influenced to go into healthcare by my father who is a retired firefighter/paramedic. I always admired his desire to care for and help others and the joy he received from his profession,” Miller says. “I took a Certified Nursing Assistant course in high school and quickly realized that I had zero interest in nursing and that field was not for me. Shortly after, I had a sports injury and required X-rays of my ankle. This was my first real introduction to radiology, and I realized that imaging was what I had been looking for all along!”
She knows she made the correct choice.
“I love my career because it is a means to give back to my community and really take an interest in the needs of the people around me,” Miller explains. “Healthcare is comprised of such a vast array of opportunities to care for our consumers. Radiology allows me to meet people in the worst times of their lives and offer a small glimmer of
hope and kindness. As the imaging manager, I use my passion for our consumers to engage my team in growing their connections to the consumer and increase the positivity of their experiences with the team, the consumers and their peers.”
Looking ahead, the future of diagnostic imaging excites Miller.
“The imaging horizon is bright, especially right now! There are so many new ideas coming to light, I think those that most interest me are remote scanning opportunities and how sites are working to fine tuning their processes for safety, efficiency and patient satisfaction,” she says. “I also am excited about the new program being offered soon from ARRT, MR Technology Assistant. This certification will be a game changer for many facilities to have dedicated MR tech assistants who are certified in the field and really understand the needs and expectations of the modality.”
She is also excited about the future of the imaging professionals she works with at AdventHealth. Her leadership style includes an open-door policy with a desire to serve and empower her colleagues.
“My approach to leadership is simple, I lean towards being a democratic leader, and I truly appreciate having in-depth conversations with my team surrounding numerous important topics,” Miller explains. “I push for an autonomous sentiment on my team, with the understanding that learning and growing are never ending, and transformation and enthusiasm are keys to success. I’m also a firm believer in servant leadership; my team cannot perform if they do not have the tools they need or feel safe and cared for in their workplace. At AdventHealth we thrive on servant leadership, a team that is well cared for, will in turn make the same caring connection with their consumers.”
Miller is quick to point out that others have empowered her.
“I have had a few great mentors throughout my career, and I must give them all credit. Andrew Santos, CEO of AdventHealth North Pinellas; Justin Evans, executive director and administrator of AdventHealth Lake Placid; Zbigniew Nawrocki, assistant vice president of ancillary services of AdventHealth Heartland; and Victoria Selley, MD, CMO, of AdventHealth
MHA, CRA, RT(R) CT M ARRT
1. What is the last book you read? “Reset” by Dan Heath
2. What is your favorite movie? My favorite movie is such a hard pick! Anything with Johnny Depp like “The Pirates of the Caribbean.”
3. What is something most of your coworkers don’t know about you? Something that most of my coworkers do not know about me is that I am half Canadian and half American.
4. What is one thing you do every morning to start your day?
One thing I do every morning to start my day is read my daily devotion and say a prayer. Having a spiritual connection is very important to me and helps me to start my day on the right foot.
Heartland,” Miller says. “Over the past few years and time with my mentors, I have learned many lessons in operations, leadership, budget creation and production, and employee engagement. I think the most precious of these lessons were hospital operations and how they connect to employee engagement and patient satisfaction.”
“Most recently, Victoria has begun mentoring me and it is immensely refreshing to have a strong female leader who thrives in their environment, truly enjoys teaching, and is excited to help other female leaders learn and grow in their own careers,” she adds. “I cannot thank my mentors enough; I truly appreciate all they have taught and continue to teach me throughout my career; they are blazing a path for future leaders each day. Presently, I do not mentor an imaging professional, although I am open to the prospect. I do maintain an opendoor policy to ensure I am accessible to all that may need help or conversation, perhaps soon I will have the opportunity to pay it forward by mentoring a future imaging leader.”
Miller is a leader with many accomplishments, but one stands out.
“The greatest accomplishment of my career thus far is completing my CRA, Certified Radiology Administrator certification, through the AHRA. This was the point when I felt I had really ‘made it’ and was able to show everything I had learned and that I could apply all the knowledge I had learned throughout my career,” she says.
“I would like to share that for any imaging professionals who are interested in leadership or are currently in leadership, joining the AHRA and sitting for the CRA certification is a great opportunity to gain knowledge and connect with like-minded individuals in the field,” she adds. “It is important to stay connected and up to date on current events in imaging, attending conferences, listening to speakers in webinars or podcasts, and directed readings are all essential and offered through numerous organizations such as ICE and AHRA.”
It is hard to image that an injury could be a good thing, but the diagnostic imaging field continues to benefit from the time Casie Miller went in for X-rays to diagnose a sports injury. •
5. Who has had the biggest influence on your life? The biggest influence in my life has been on my parents. They have always been my cheerleaders, they are who I get my work ethic from –I grew up watching them work for everything they have in life, they taught me the importance of family and caring for others, and they are who taught me the necessary morals and life skills I needed to navigate adulthood, and corporate America.
6. What would your superpower be? Mind reading! My oh my that could be a blessing and a curse.
7. What are your hobbies? My hobbies are walking, swimming, especially at the beach, shopping, reading, traveling and spending time with my nieces and nephews.
8. What is your perfect meal? The perfect meal would be a Maine baked potato, roasted root vegetables and teriyaki tofu.

BY MATT SKOUFALOS
As a true Minnesotan, diagnostic imaging director Brianna Iverson couldn’t imagine a better professional setup than her work at RiverView Health in Crookston, Minnesota, which both fulfills her career interests and keeps her as close as possible to the land and people she so dearly loves.
Iverson traces her work to a lifelong academic interest in the sciences, and a feeling of being called to the career in healthcare that followed. When a friend of her mother’s suggested that she pursue radiology for the variety of options it offers, Iverson enrolled in a rad tech program at Northland Community & Technical College in her hometown of East Grand Forks, Minnesota.
“My career is always something I’ve been deeply passionate about,” she said; “I [also] knew I wanted to stay close to home and close to family.”
Iverson graduated in 2013, and spent about 12 years working as a rad tech. In the course of her employment, she also learned CT and Dual-Energy X-ray Absorptiometry (DXA) imaging, and began to pursue pathways to a leadership role.
“I had worked in healthcare long enough to see what kind of influence leadership can have on an organization and individuals, and I knew I wanted to be a part of that,” she said. “Leadership is something that’s natural for me, and I find a lot of joy in being a leader and a coach. ”
In pursuit of her career advancement, Iverson completed an undergraduate degree in healthcare management and leadership at the University of Minnesota-Crookston, and a master’s degree in organizational leadership from the University of
Mary. In 2023, it all paid off, as she became director of diagnostic imaging at RiverView Health of Crookston, Minnesota.
“Throughout my master’s, I learned a lot of different leadership styles,” Iverson said. “I believe strongly in servant and empathetic leadership. It can make a difference when staff feel heard and valued and supported. Seeing what can happen under the right leadership is one of the biggest rewards of my career.”
In addition to leading technologists through their day-today responsibilities, Iverson has worked to help train the next generation of imaging professionals as a teacher for an RT program in Detroit Lakes, Minnesota. She was able to apply practical and theoretical experience from her own career and academic expertise to the clinical instruction.
“Being a part of the education side of the profession has been super-rewarding,” Iverson said. “I love coming to work every single day. I hope I continue to feel this way throughout my career.”
Away from work, Iverson is deeply connected to her Minnesota roots, perhaps most directly in her love of the outdoors. Her family of four spends as much time as possible at its renowned lakes, whether ice fishing in the winter or swimming, camping, and boating in the summer. As a child, Iverson recalls camping at her grandparents’ cabin, then roughing it in tents, and finally, a 30-foot motor home.
“I loved every second of my childhood, and these camping weekends completely shaped who I am,” she said. “I knew that when I became a mom, I wanted to carry on those traditions with my family and my boys, Benson (12) and Dax (9). It’s super-special to see them making the same memories that I had growing up.”
When the lakes freeze over in the Minnesota winter, the
family takes its RV edition “Ice House” from the banks of the waterway out onto the frozen lake surface itself. With a full living space, including a kitchen, TV and bathroom, “we’re definitely not roughing it completely,” Iverson said, “but we absolutely love it.”
“Winters get long here, and then we have snow from October to May, so it gives us a hobby all winter long,” Iverson said. “We get to catch walleye, which is delicious; we’ll fillet it up and cook it, or fry it at home. We’ll play cards while we’re fishing, or the boys will make snowmen.”
At the lakes, “you’re completely immersed in the Minnesota outdoors,” she said. “The Duluth area up north is gorgeous, and not a lot of people know about it. We do Lake Bemidji in the summers, and Lake of the Woods or Stump Lake for the ice fishing.”
Brianna and her husband, Kevin, will celebrate their 10-year wedding anniversary in February 2026. As important to her life as motherhood is, she also spends lots of time with her parents, who live close by, and as an auntie to her siblings’ children.


“My family is full of love and laughter and support, and I love to have them around,” Iverson said. “I could never leave Minnesota, and I could never be far from my family.”
As important as her home life is, Iverson also dedicates time to outfitting it with a collection of houseplants and antiques. She said the 40-some individual plants in her home bring life and character into it, as she manages the unique needs of each.
The greenery is offset by Iverson’s curation of vintage home goods and antiques, which similarly add more stories to the space to complement her warmth and personality. Likewise, her love of animals extends beyond the present household roster of Pebbles, a German Shepherd, and farm cat, Oreo.
“If it were up to me, I would have 20 more,” Iverson said. “I have been known to bring home surprise pets. Animals bring such joy and energy, and I can’t imagine a life without them. Pretty much every animal I’ve ever brought home was a surprise – a lab, a German shepherd, a


cat, a guinea pig, hamster – and they just end up being a part of our family.”
Iverson is also “a self-proclaimed coffee addict,” happy to receive everything from a black cup of coffee to a fancy latte at any hour of the day. She nonetheless ranks the coffee she had in the Dominican Republic as “the most fabulous thing I’ve ever tasted, and that alone is going to make me want to go back.”
When she’s not at work, or filling her house with life in all its vibrant forms, Iverson enjoys catching a comedy show, or watching a funny movie. Recently, she’s also begun nurturing a fledgling interest in poetry writing and hopes to someday publish her growing collection.
“I started writing a year ago, and I have a collection saved on my desktop,” Iverson said. “I plan on getting a good stack of them and self-publishing. The poetry I write is exactly what I’m feeling at the time I’m writing, and it explains my feelings in depth. It’ll be really fun to publish.” •





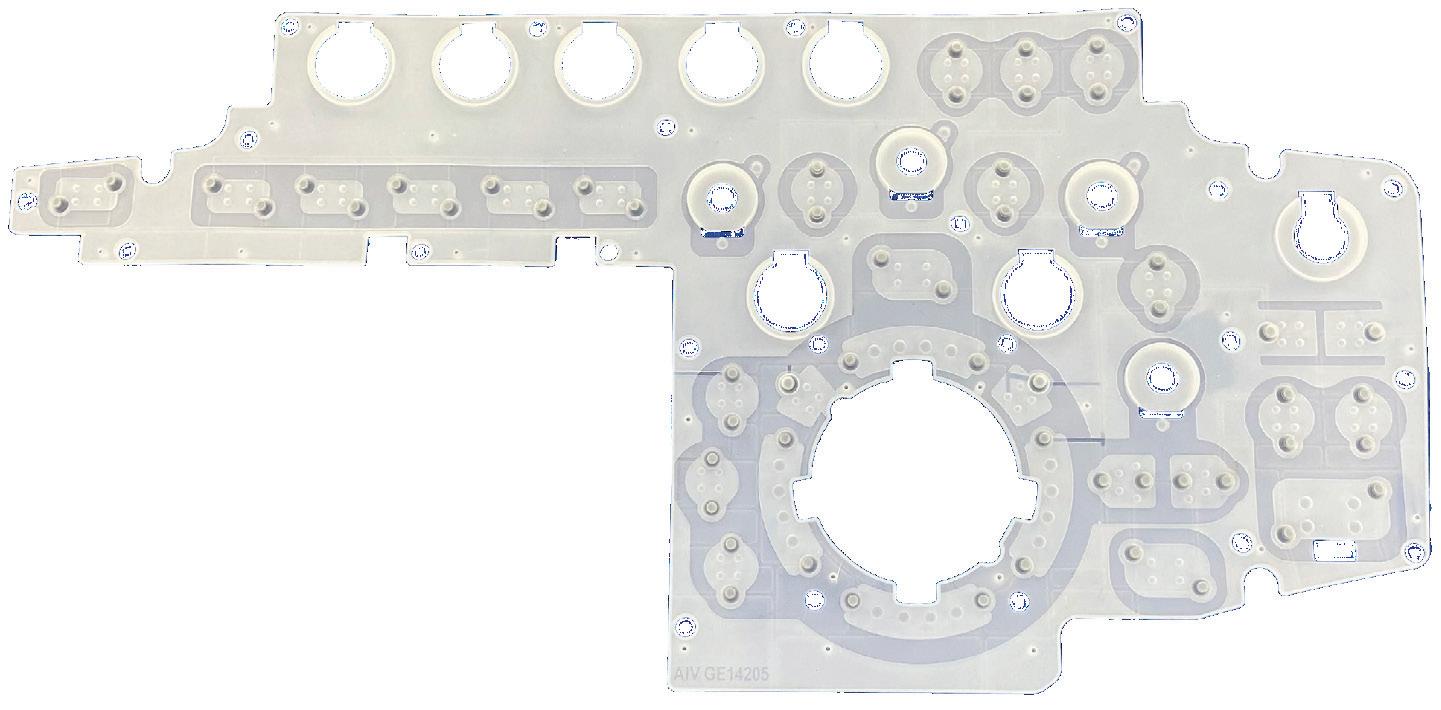
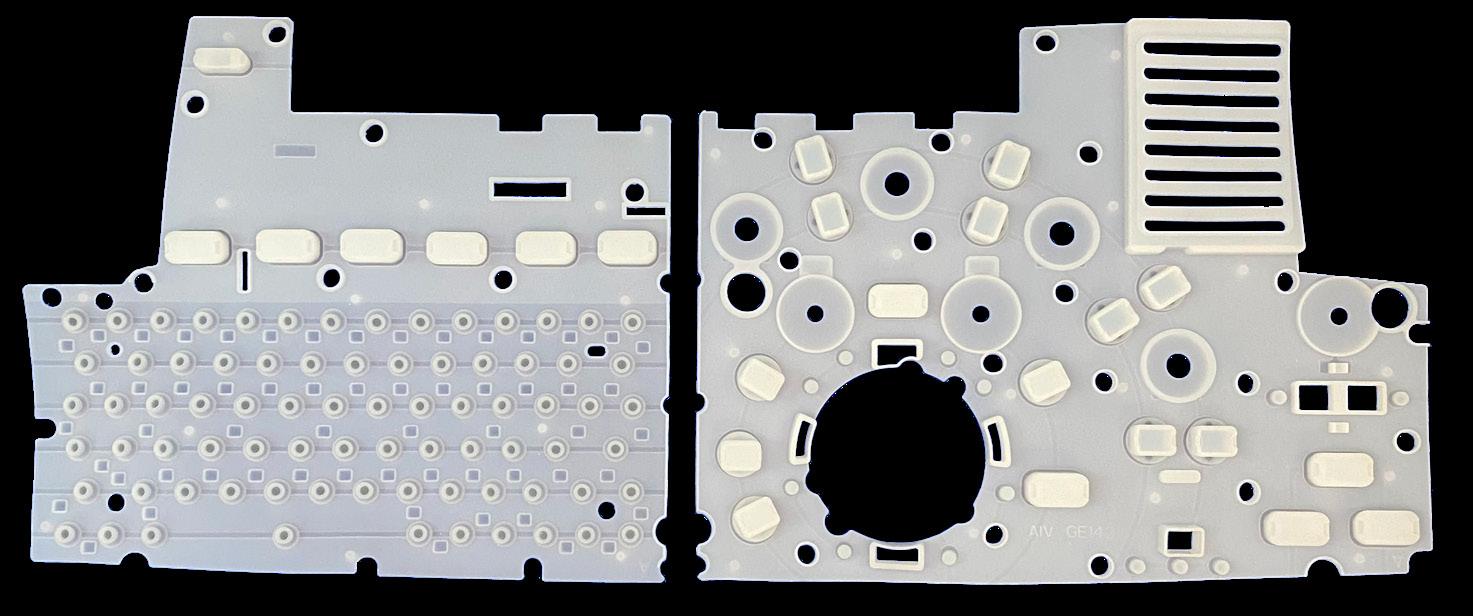
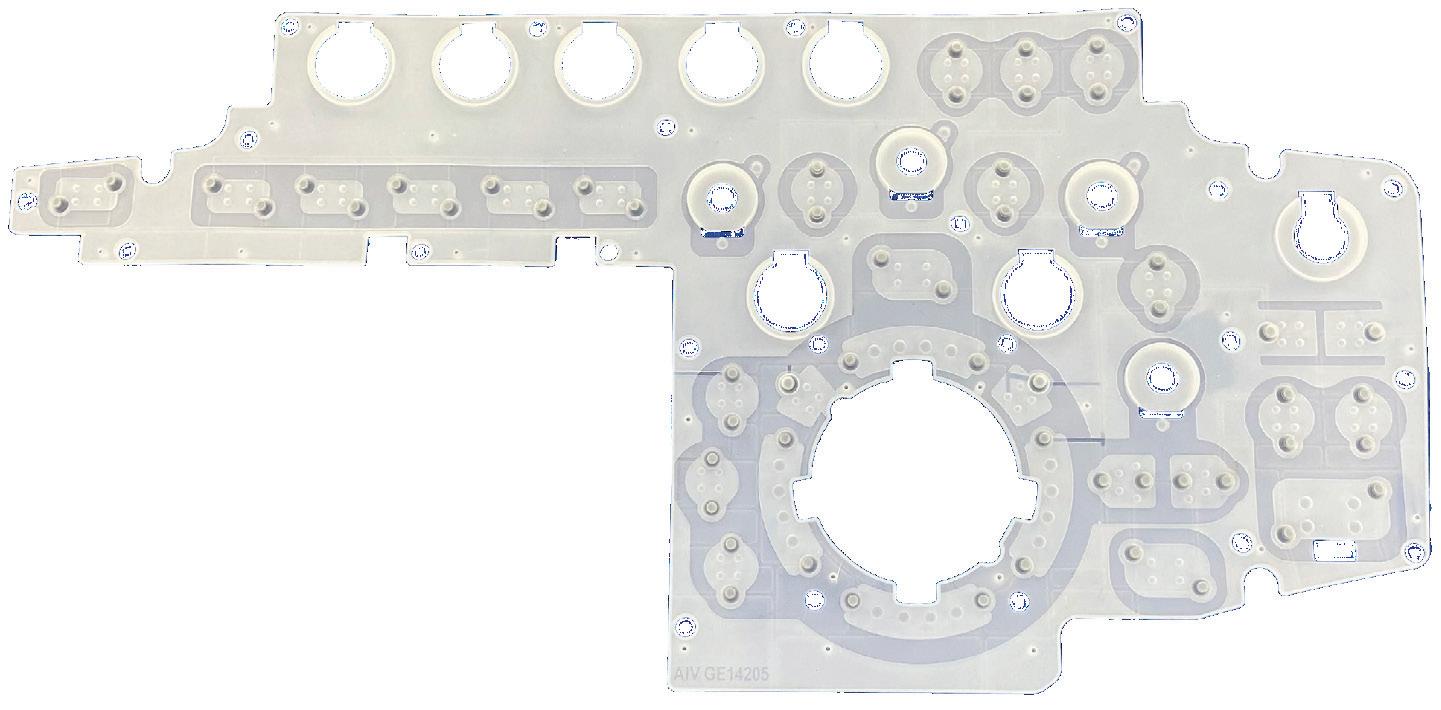
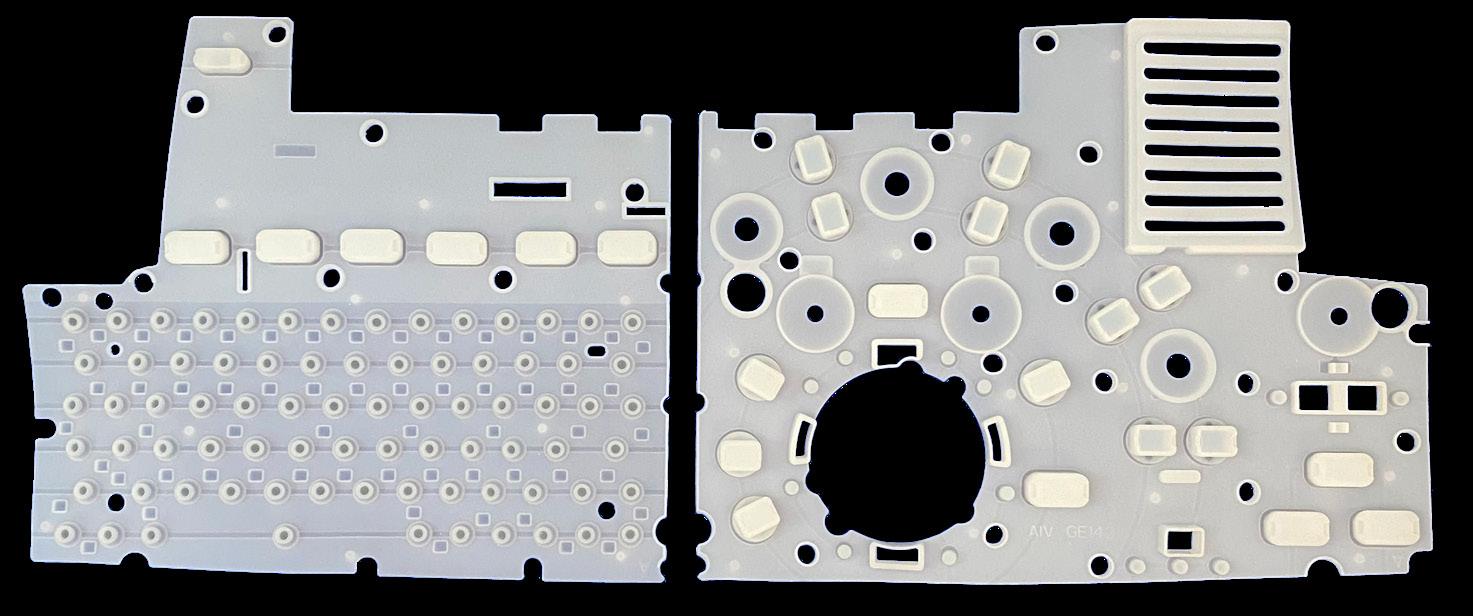
AI V Inc. is an ISO13485:2016 certified manufacturer of replacement parts and offers repair services on certain medical devices. They recently joined the imaging space, and the AIV team is excited to start offering replacement parts in this new arena. AIV has developed a replacement solution for the lower panel keyboard elastomer for the GE LOGIQ S7/ S8 OPIO4 and E9 series. Through relationships the company has developed over the years, the staff were able to identify a common failure piece. From there, the engineering team helped develop a replacement part that will save end users thousands of dollars in repair costs.
AIV Inc. Vice President of Sales & Product Development Jeff Taltavull shared more about the company and its goals.
Q: HOW DOES YOUR COMPANY STAND OUT IN THE IMAGING SPACE?
A: While we are new to the imaging space, we have over 40 years of being a solutions provider in the medical device field. We are looking forward to expanding our scope into the imaging space.
Q: WHAT IS ON THE HORIZON FOR YOUR COMPANY?
A: We are looking to expand our scope in the imaging space and are actively looking at additional models and brands that have similar lower control panel needs to expand our elastomer line.
Q: IS THERE ANYTHING ELSE YOU WOULD LIKE ICE MAGAZINE READERS TO KNOW?
A: AIV has built its business in being a repair and replacement parts solution provider for the last 40 years. We identify our opportunities based on the needs of our customer base. These opportunities don’t always fall in our historical infusion pump scope, and I would just like to reiterate that we have substantial capabilities. If you have a need that is not being met in the marketplace or by the OEM, please reach out to us. We have a streamlined evaluation process for repairs and replacement parts and are always looking forward to developing solutions for our customers. Let us know if we can help. •
For more information, visit aiv-inc.com.

•99%




At the annual Transcatheter Cardiovascular Therapeutics meeting, Royal Philips introduced an industry-first innovation that integrates pre-operative CT data directly into the cath lab workflow, according to a press release.
This new capability, available through the integration of Philips’ Advanced Visualization Workspace (AVW) with the Azurion image-guided therapy system, marks a first step towards CT-guided percutaneous coronary intervention (PCI), a minimally invasive procedure to open narrowed coronary arteries and restore blood flow to the heart.
The new capability, Follow C-arm, automatically synchronizes the 3D reconstruction of coronary arteries with the movement of the Azurion C-arm. As the C-arm angulation changes, the CT volume rotates in real time to match, giving interventionalists the 3D anatomical view without manual interaction. This seamless connection helps clinicians combine the detailed insights of CT imaging with the flexibility of live X-ray guidance inside the cath lab. The combined AVW–Azurion approach aims to provide enhanced anatomical insights to guide complex PCI procedures, publications have shown that leveraging
CCTA may lead to reduction in contrast medium use and radiation dose during interventions.
Coronary computed tomography angiography (CCTA) is increasingly used in global clinical guidelines as a firstline tool for the diagnosis and planning of coronary artery disease. With more patients now arriving at the cath lab with prior CT scans, physicians are seeking ways to incorporate this information into their interventional workflows. By integrating CT data directly into Azurion, Philips is helping interventionalists expand the use of CT beyond diagnosis and planning, supporting a future in which CT-guided PCI becomes standard practice.
“By bringing pre-operative CT into the cath lab and linking it directly to the movement of the C-arm, Philips is delivering an industry-first that helps interventionalists prepare for and execute PCI procedures with greater confidence,” said Mark Stoffels, business leader image-guided therapy systems at Philips. “This seamless integration is a significant step towards CT-guided PCI, aligning with our commitment to improving workflow efficiency and advancing patient care in interventional cardiology.”
FUJIFILM Sonosite Inc., a global leader in point-ofcare ultrasound (POCUS) solutions, has announced the launch of Sonosite MT, the latest evolution in its line of portable ultrasound systems, according to a press release.
“Continuing Sonosite’s commitment to creating the most durable, reliable, and easy-to-use ultrasound technology with an education-first approach, Sonosite MT joins the renowned Sonosite PX, Sonosite LX, and Sonosite ST systems to advance clinical imaging across healthcare environments,” the release adds.
Designed as a “Grab and Go” clamshell form factor, Sonosite MT is engineered for seamless use both on and off the stand, offering clinicians superb mobility without compromising functionality. Featuring an intuitive all-touch user interface, a clinical monitor and control panel, this system delivers a familiar user experience that minimizes workflow disruption and promotes clinician adoption.
“At FUJIFILM Sonosite, our mission is to empower clinicians with ultrasound systems that perform reliably in the most demanding clinical settings. Sonosite MT exemplifies this mission by integrating our core product pillars: durability, reliability and ease of use,” said Richard Fabian, president and chief executive officer of FUJIFILM Sonosite Inc. “This new system continues our journey of excellence, providing a portable ultrasound platform that supports both clinical confidence and operational efficiency.”
Key features of the Sonosite MT mentioned in the press release include:
• Durable Design: Engineered to withstand the rigors of the clinical environment, ensuring uptime and dependable performance
• Excellent Imaging: Delivers clear, high-resolution

images to support accurate diagnosis across diverse patient populations
• Enhanced Mobility: Lightweight and compact, enabling quick transport and use in various care settings
• Intuitive All-Touch User Interface: Seamless touchscreen control with a user experience harmonized with the FFSS portfolio, facilitating ease of training and adoption
• Risk Management and Infection Control: Featuring a buttonless monitor and control panel design that can be easily cleaned and disinfected.
• Medical Informatics Interoperability: Integrated with Synapse Synchronicity workflow manager to streamline clinical operations and data management
GE HealthCare and UC San Diego Health have announced a strategic enterprise collaboration focused on bringing advanced digital innovation and medical technologies to the San Diego health system to help deliver high-quality, timely and consistent care that can help meet individual patient’s health care needs. The collaboration is centered on integrating innovative imaging and technology throughout the UC San Diego Health system with the goals of improved outcomes and greater cross-functional connectivity.
“This Care Alliance was designed to standardize future-focused technology with the goal of measurable improvements in patient outcomes,” stated Catherine Estrampes, president and CEO, U.S. and Canada at GE HealthCare. “This value-based delivery framework is driven by system-wide efficiency that can help increase access to innovative technology for clinicians and individualized care for patients.”
The Care Alliance is anchored in key pillars including:
• Service line excellence leveraging innovative imaging solutions and novel therapies, such as theranostics, to advance the cancer care journey for early detection, effective treatment and enhanced monitoring.
• AI and digital solutions to drive innovation, efficiency and excellence in care delivery.
• Optimized technology program including a customized model and a technical services support program for advanced education to arm clinicians with the technological expertise they need to deliver exceptional care.
• An augmented service delivery model that includes service experts and field engineers to help support preventative maintenance for connected equipment to reduce downtime and complexity, as well as improve efficiency and issue resolution speed. Through the joint effort, innovative imaging systems including X-ray, CT, PET/CT, PET/MR, SPECT/CT, MRI, image guided systems, and nuclear medicine in combination with AI and digital tools to help optimize efficient processes will be leveraged. Advanced technologies will be integrated across facilities and clinical teams, including imaging technology that can help pioneer theranostics, which combines diagnostics and therapeutics to provide a more precise approach to treating diseases, particularly cancer. Some solutions that will be implemented include GE HealthCare’s StarGuide SPECT/CT, Smart Subscription for CT and SIGNA Continuum program for MR.
Sirona Medical has received U.S. Food and Drug Administration 510(k) clearance for its Sirona Advanced Imaging Suite, marking a significant regulatory milestone and the company’s first Class II medical device designation, according to a news release.
This clearance expands Sirona’s diagnostic imaging capabilities to include PET-CT support with quantitative SUV analysis, image fusion, maximum intensity projection (MIP) generation and multi-planar reconstruction (MPR).
“This milestone reflects our commitment to closing the most critical capability gaps that limit the flexibility and reach of modern radiology,” said Dr. Peter Sachs, radiologist, imaging informaticist, and Sirona Advisor. “By pioneering the field of 100% cloud-native PET viewing and PET-CT fusion, we’re enabling radiologists to interpret advanced imaging studies from anywhere – without compromise in diagnostic confidence, speed or quality.”
The clearance follows an extensive multi-disciplinary effort across Sirona’s product, engineering, quality and regulatory teams. The newly cleared functionality represents
a significant step in Sirona’s mission to unify the radiology workflow by bringing advanced visualization, reporting and collaboration into a single, cloud-native environment accessible through a browser.
“With PET-CT now cleared, Sirona has completed a four-year journey toward delivering the most complete, FDA-cleared, and cloud native diagnostic environment in the industry,” said Ken Kaufman, chief executive officer of Sirona Medical. “This is a foundational milestone for our customers.”
Sirona’s cloud-native architecture fundamentally changes how innovation reaches radiologists. With the FDA clearance of the Sirona Advanced Imaging Suite, new functionality no longer requires complex, site-by-site installations or lengthy upgrade cycles. Instead, capabilities can be deployed to every user instantly through the cloud.
Sirona’s Advanced Imaging Suite began rolling out to users in November 2025, with immediate availability for existing customers participating in early-access programs.
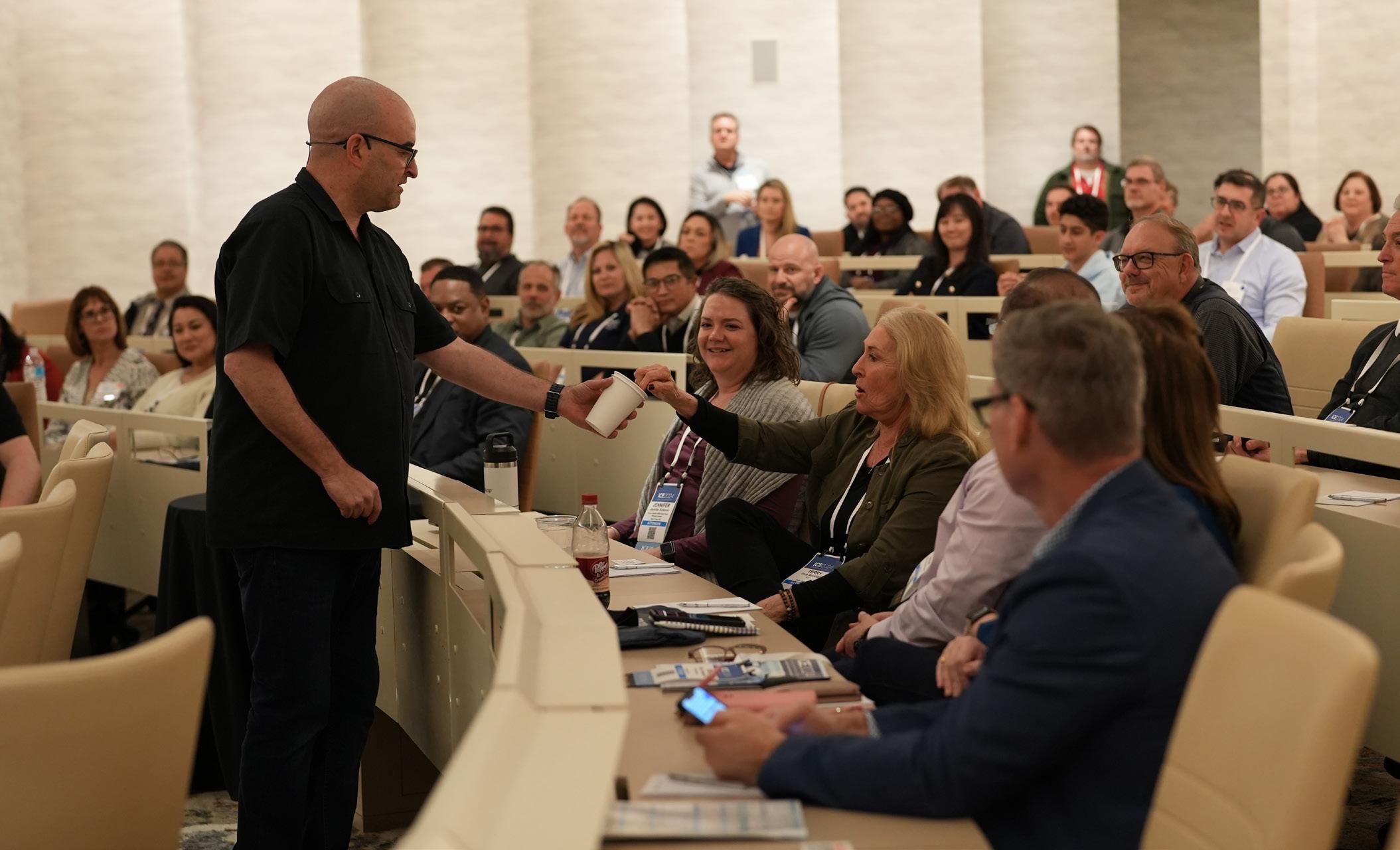
Registration is now open for the 2026 Imaging Conference & Expo (ICE) scheduled for February 20-22 in San Antonio, Texas! And registration is FREE for hospital and imaging center employees as well as active military and full-time students.
ICE is the only conference dedicated to imaging directors, radiology administrators and imaging engineers from hospital imaging departments, freestanding imaging centers and group practices. The conference delivers valuable CE credits from the ASRT and ACI (pending approval).
This is the imaging conference where all imaging professionals come together for conversations regarding capital projects, imaging practices, service solutions and more.
ICE 2026, like previous years, offers invaluable continuing education, productive networking and an exclusive exhibit hall. Attendees will have the perfect opportunity to enhance their careers and spend time with colleagues.
ICE is the perfect resource to grow and prosper, personally and professionally. Attendees and exhibitors continue to share positive feedback from previous ICE conferences and plan to return.
“I had many takeaways from the conference. The leadership summit was a great platform to share current challenges in healthcare. To me this was a new topic that I have never experienced before at an imaging conference,” Taylor/Chaplin Breast Health Center Associate Director
Kathryn Fields ARRT, ARDMS, MBA, said. “It was great to connect prior to the summit and meet the participants, and then later have an open discussion on topics of our choice that are currently affecting us in our work and healthcare system. It’s always great to see what other facilities are doing and how they handle certain challenges.”
“Overall, it was a great discussion and when I came back to work, I felt motivated and refreshed with new ideas to implement and try out with my team because of the discussion,” she added.
Daniel Adamas from Renovo praised ICE after attending in a previous year.
“My favorite part is the general structure of the event. I like the fact that technicians, service managers and clinical managers can share an event and trade stories of their concerns,” Adams said. “I think it helps service people understand what is important to clinicians as well as giving insight to clinicians regarding service challenges/issues.”
Ohio State University Wexner Medical Center MR Imaging Manager Annette Long agrees.
“The ICE conference is a fantastic event to attend, offering excellent lectures and highly relevant material,” she said. •
Check out the schedule and register today at AttendICE.com.

The recent ICE webinar presentation “SpectralDR Dual Energy X-ray: Clinical and operational impacts” sponsored by KA Imaging was a hit among imaging leaders with almost 100 attendees for the live presentation. The live presentation was eligible for 1.0 ARRT Category A CE credit by the AHRA.
Webinar presenter Dr. Karim S. Karim, Ph.D., PEng, MBA, FEIC, FCAE, is the co-founder and chief technology officer of KA Imaging. He discussed increased visualization of cardiothoracic abnormalities, lesions and calcifications with single exposure SpectralDR dual energy X-ray, and its clinical and operational impacts.
The webinar armed attendees with the ability to understand single exposure SpectralDR dual-energy subtraction (DES) X-ray, the limitations of the old dual exposure DES techniques and how SpectralDR technology overcomes these limitations.
Karim also discussed the clinical use cases where SpectralDR has an edge over digital X-ray and shared more about hospital implementations of SpectralDR through multiple clinical studies in North America. He also examined the operational and financial impacts of SpectralDR adoption in a clinical setting.
An informative question-and-answer session provided attendees with the opportunity to gain additional insights from Karim.
Sherry McDavid, RT, CV Senior Tech, CPC, at King’s Daughter’s Medical Center in Kentucky won an ICE gym bag during the webinar.
Attendees provided feedback regarding the webinar via a survey that included the question, “What do ICE webinars provide the industry?”
“The option to participate in webinars that cannot be attended in person,” said Irine Gordon, an interventional radio-
logic technologist with Baylor Scott & White All Saints.
“Sharing new and innovative ideas for radiology,” said Renee Howard, OP and NM manager, Atrium Navicent.
“CEUs and data relevant to our practices. Thank you!” said Jennifer Sturm, a certified nuclear medicine technologist with Novant Health.
“A great opportunity to learn about new technology or ideas. Healthcare is forever changing and can be difficult to manage. Any opportunity to learn more and connect with others is beneficial,” explained Jessica Chambers, regional director of imaging with SSM Health.
“Excellent opportunity for attendees to gain advanced knowledge in different technologies,” said Terry Ferguson, a retired education director.
“Current insights and best practices in credentialing, accreditation and assessment. Expert guidance from leaders in testing, certification and regulatory compliance. Professional development opportunities to enhance knowledge and maintain credentials,” shared Chikodinaka McCarty, an imaging education coordinator with Houston Methodist Hospital.
“Training without the expense of travel and tuition,” said Mitch Hoffman, CBET, with Parkview Health System.
“More than reading about the news in an article, participating in such webinars gives the opportunity to get more information and get some queries clarified from the presenter,” said Kumar Balasubramanian, manager medical equipment planning with Hamad Medical Corporation in Qatar. •
For more information, visit ICEwebinars.live.


Premium Quality
Exceptional Value
• Drop-in replacements for your system. Fit and function like the original.
• Premium inserts from I.A.E.
• X-ray tubes on the shelf, and ready to ship.
• New, with an extensive warranty

Impressive Warranty Contact us at:
Email: info@X-RayAmerica.com
Phone: 1.854.999.6888
Global: IAE.it US Headquarters: X-RayAmerica.com


The inaugural winners of the ICE Diamond Awards exemplify imaging leadership. These exceptional imaging directors and managers, representing eight regions across the United States, were nominated and selected by the ICE community in recognition of their outstanding leadership and contributions to the imaging field.
“We’re thrilled to announce that included in our December issue of ICE Magazine and at the 2026 ICE Conference we will shine a special spotlight on our Inaugural 2025 ICE Diamond Award winners!,” ICE Magazine’s Megan Cabot shared.
Keep reading to find out more about each winner and attend the 2026 ICE Conference as the ICE community celebrates their achievements and they are presented with their ICE Diamond Award trophy.
Register today at AttendICE.com.



Executive Director at Radiologic Associates of Middletown
I have been in the radiology field for over 25 years including a solid track record of operations management, practice development and growth strategy.
WHAT DO YOU LOVE ABOUT YOUR JOB?
As an executive director of a private radiology practice, I get to work in all phases of radiology. Running the practice allows me a daily variety and keeps the work fun and enjoyable.
FUN FACT ABOUT YOU:
I love home projects. I take great pleasure and pride in seeing a project from start to finish. If I could go back to any job I have had in my life … I would be a bartender. Ask me to make you a drink, you will see why!


Radiology Operations Manager at Children’s National Hospital
I have been in radiology and worked at Children’s National Hospital for my entire career, which has been just over 18 years. Starting my career as a radiologic technologist, then becoming a lead radiologic technologist and now an operations manager for several of our outpatient sites for the past 4 years.
WHAT DO YOU LOVE ABOUT YOUR JOB?
I love my job for so many different reasons. Working and helping children has always been so amazing and seeing their resilience and strength is truly incredible. I also love the people that I work with. We get the opportunity to work with such amazing and unique people every day. Working with other technologists, doctors, nurses and other practitioners to pursue great work, incredible advances and a great work environment.
FUN FACT ABOUT YOU:
Something that not many people know about me is that I played the tenor saxophone in my high school jazz band and I absolutely loved it. Unfortunately, I do not play anymore but it was definitely a highlight in high school.

Radiology Director at University Hospitals
I serve as the director of radiology for University Hospitals Academic Market and ambulatory locations, overseeing imaging operations across Cleveland Medical Center and multiple health centers. With over 20 years of experience in medical imaging, I specialize in operational leadership, capital planning and process.
I love that my role challenges me to think strategically while staying connected to patient care. Whether it’s driving process improvement, planning for new technology, or mentoring future leaders, every initiative helps move our imaging program forward. Building strong, connected teams that deliver excellent imaging care is both inspiring and fulfilling.
FUN FACT ABOUT YOU:
I serve as the secretary for my daughter’s gymnastics booster club, organizing fundraisers, community events and meets has become one of my favorite creative outlets outside of work. I love staying involved in my kids’ sports and community activities, and volunteering in these ways keeps me grounded, balanced and connected beyond the hospital.


Regional Service Line Director of Imaging at SSM Health
I serve as the regional service line director of imaging at SSM Health, where I lead strategic growth and operational excellence across seven hospitals, including an academic medical center and a dedicated children’s hospital. I began my imaging career in 2002 with the U.S. Air Force.
I love that I’m given the autonomy to find creative ways to remove barriers for my team. Whether that’s through introducing new technologies or implementing innovative ideas. Healthcare is constantly evolving and becoming more complex each year, and I thrive in that dynamic environment. This career continuously challenges me, and I truly appreciate that I’m always learning, growing and never stagnant.
FUN FACT ABOUT YOU:
We’re die-hard Dodgers fans – in fact, all three of my children are named after Dodgers! I also hold a brown belt in Brazilian Jiu Jitsu, which has taught me discipline and resilience both on and off the mat. I’m a huge travel buff, and cruising is our favorite way to explore the world. When I’m on PTO, you can usually find me


Vice
I have worked in radiology since the early 1990s and have served in enterprise-level leadership roles overseeing imaging services across several large health systems. My career has centered on advancing operational excellence, technology integration and clinical quality across diverse markets.
WHAT DO YOU LOVE ABOUT YOUR JOB?
What I value most about my role is the ability to influence both people and performance at scale. I find it deeply meaningful to align strategy, technology and culture in ways that elevate care quality, service and operational excellence. Seeing teams thrive, delivering outstanding results while growing professionally, is the most rewarding aspect of the work.
FUN FACT ABOUT YOU:
I spent many years umpiring high school and college baseball. The experience taught me valuable leadership lessons about composure, fairness and decision-making under pressure. Those are skills that have been translated directly into my daily work.

Imaging Operations Manager at UT Southwestern Medical Center at Moncrief Cancer Institute
I am an imaging operations manager for UT Southwestern at Moncrief Cancer Institute. I am multi-modality imaging technologist with 28 years of experience with more than half that time spent in leadership roles.
WHAT DO YOU LOVE ABOUT YOUR JOB?
I work for an academic organization that values education and research. UT Southwestern saved my own mother’s life through innovation, research and clinical trials. That is when I knew I wanted to be part of this organization too. I feel honored to work at such an amazing place. I love solving problems, putting out fires and helping people succeed. My current role is the perfect blend of holding people up while operating a fire extinguisher!
FUN FACT ABOUT YOU:
I love to travel, play board games and go to the movies. A fun fact about me is that about 14 years ago, my husband and I learned to ballroom dance specifically for an amateur competition that we won! We had zero dance experience at that time, but I fell in love with ballroom dance! I have been dancing in my kitchen ever since!


Director of Diagnostic Service at Madison Health
I started in the radiology field in 2000 and entered a director position in 2016 with Madisonhealth in Rexburg, Idaho as the director of radiology. Over the years, my leadership responsibilities have grown within Madisonhealth.
As a leader in the radiology profession, I enjoy being proactive to what the radiology market needs are. This allows my team to have equipment and supplies they need to help providers get answers for their patients in a timely manner. I also enjoy mentoring others to be the best version of themselves as a technologists and as a leader. I also love the challenges of healthcare and working towards solutions as well as preventing challenges from arising.
FUN FACT ABOUT YOU:
I love airplanes. I love the aviation industry. I love the business side of it and the challenges they encounter daily. All airplanes are amazing to me however, the larger the airplane, the more amazing it is. I will look to the

Executive Director of Imaging at Children’s Hospital of Los Angeles
I currently am privileged to lead the imaging department at Children’s Hospital Los Angeles, the top pediatric hospital in the Western U.S. I oversee all clinical modalities, imaging research and education. I have been in imaging for 34 years, starting first as a nuclear medicine technologist and slowly growing in responsibility to my current role.
I love that I can have big impacts on the care of so many patients not only the care they receive in imaging but every service in the hospital that relies on imaging. I love getting the gift to be part of a team of caring imaging technologists, nurses, doctors and essential support team members and watch them support each other and care for patients and families every day.
FUN FACT ABOUT YOU:
I am an addicted video gamer and have been since I got the very first PONG game as a kid. I wake up early on the weekends just to get some gaming in. I also love tabletop games and Dungeons & Dragons. I love to read anything and everything I can and typically read a couple books a week.


Ultrasound probes, also called transducers, are devices that emit and receive high-frequency sound waves to create images of internal body structures. They come in various shapes and sizes, with common types including linear for superficial structures like thyroids and breasts, curvilinear (or convex) for deeper imaging like abdominal organs, and phased array for applications requiring a narrow field of view, such as cardiac imaging. The specific shape and design of the probe are optimized for different parts of the body and imaging needs.
ICE Magazine asked imaging leaders to share their insights regarding ultrasound probes and transducers. Participants are:
• AdventHealth Imaging Centers Clinical Director Cory Whitehouse and subject matter expert Allison Fritzinger;
• Madison and Guilford Radiology Manager Sarah Pucillo, RDMS (AB,BR) (RVT);
• Madisonhealth Lead Sonographer Eric Belk, RT (R)(MR) (CT), RDMS; and
• UT Southwestern Medical Center Technical Manager Kim Pongsatianwong, MBA, RDMS, RVT.
Q: HOW WOULD YOU DESCRIBE THE CURRENT STATE OF ULTRASOUND PROBE AND TRANSDUCER TECHNOLOGY IN YOUR DEPARTMENT OR FACILITY? HAVE YOU NOTICED ANY MAJOR CHANGES IN RECENT YEARS?
W&F: We have purchased new machines and probes with the latest technology with Philips.
Pucillo: Guilford and Madison Radiology (owned by RAM radiology) are fortunate enough to have newer ultrasound machines in both offices. Newer machines bring better technology in ultrasound probes with better resolution and
image quality. In recent years image quality has of course improved, but probe weight and size have also improved. Probes on new machines are lighter and smaller than older versions, which also is better for ergonomics.
Belk: Our transducers are one generation behind due to limitations of our current ultrasound system. Some of the improvements are improved color Doppler, better penetration, improved near field resolution.
Pongsatianwong: Our facility is equipped with ultrasound systems from multiple vendors, and while we’re still a step behind, we’re actively working to close that gap. Over the past few years, we’ve committed to investing in upgrades and partnerships that keep our imaging capabilities aligned with evolving technology. This includes the integration of high-frequency linear transducers that provide improved resolution for superficial and small-parts imaging, as well as transducers that have microvascular imaging capabilities that enhance visualization of low-velocity blood flow in fine vascular structures. We have software updates that support 3D-like color renderings of blood flow to help in more complex vascular cases. We also purchased transvaginal probes with 3D capabilities that allow for automatic sweeps to decrease sonographer shoulder movements and increase image quality. Overall, the current state of our ultrasound probe and transducer technology is optimistically progressive. These recent upgrades, including lighter probes and better cable design coupled with better dynamic range and signal-noise performance, have significantly improved image quality, diagnostic capabilities and workflow efficiency.
Q: WHAT ARE THE MOST COMMON ISSUES OR CHALLENGES YOUR TEAM ENCOUNTERS RELATED TO PROBE MAINTENANCE, PERFORMANCE OR LONGEVITY?
W&F: If not properly maintained they can affect ultrasound image quality.
Pucillo: The most common issue we have seen is discolored probe cords – even with compatible cleaning solutions. Luckily this is only a cosmetic issue. We have also noticed that probes being smaller and more lightweight means when dropped they break. We have been lucky in that we have not had any major issues with probes for unexplained causes.
Belk: For proper cleaning techniques and supplies, we get different information from our application person than what the ultrasound system provides online.
Pongsatianwong: Our most common maintenance issue involves broken or damaged transducer crystals, typically as a result of regular wear and tear or occasional mishandling during daily use. Given that our department manages close to 200 ultrasound transducers – slightly more than half of which are located within the inpatient hospital – it can be challenging to maintain consistent quality control, timely repairs and accurate inventory tracking. We have implemented a structured quarterly QC program and enabled efficient processes between our clinical, physics and biomedical teams to ensure that all transducers are routinely tested for element integrity and image quality.
Q: HOW DOES YOUR FACILITY APPROACH PROBE AND TRANSDUCER PURCHASING DECISIONS, REPAIRS AND REPLACEMENT CYCLES? DO YOU WORK WITH OEMS, THIRD-PARTY PROVIDERS OR A MIX?
W&F: We work with third-party provider Intelas.
Pucillo: We use a mix. We are always looking for the best value for the best price.
Belk: We are a low-volume site which empowers the sonographers to look for wear on transducers or a decrease in transducer performance. When we see wear or loss of detail while scanning, we contact our ultrasound machine vendor to replace the transducer. We included in our service contract a provision for them to replace our transducers. As for new lines of service, we work with our providers and with our vendor to ensure we are getting the correct transducers to meet their needs. We only work with our ultrasound system manufacturer as we only have one machine and need it up and running quickly when it goes down.
Pongsatianwong: Our facility takes a structured and collaborative approach to ultrasound transducer purchasing, repair and replacement. Purchasing decisions are driven by clinical demand, image quality requirements and equipment compatibility across our existing ultrasound systems. We also consider factors such as transducer versatility, ergonomic design and cost efficiency. Input is gathered from sonographers and radiologists with considerations being given to referring clinicians and new emerging applications of ultrasound. For repairs and replacements, we primarily work with the original equipment manufacturers for warranty and specialized probes, particularly where proprietary technology is involved. A transducer is typically loaned for use while our original transducer is being repaired. Our replacement cycles are guided by both usage data and QC results. Probes are evaluated regularly for element dropout, cable damage and performance degradation. Devices that fail QC or are beyond economical repair are prioritized for replacement during the capital budget cycle. From a budgeting and approval standpoint, transducer purchases and major repairs are coordinated through our department’s operations committee and






reviewed as part of the annual capital planning process. Routine or minor replacements may be approved at the departmental level, while larger acquisitions are submitted for capital budget approval.
Q: WHAT STEPS DO YOU TAKE TO ENSURE PROPER HANDLING AND CARE OF PROBES TO MINIMIZE DAMAGE AND DOWNTIME? HOW IMPORTANT IS USER EDUCATION IN MAINTAINING PROBE HEALTH?
W&F: Probe handling is held to a high standard. Our technologists are aware of the cost and sensitivity of the probes. They are educated on how to properly clean and store them.
Pucillo: Proper staff training is key to making sure we are appropriately handling the probes and their care. User education allows us to make sure we are not damaging this important medical equipment. We utilize training and reading materials from our companies such as Civco, Philips and GE.
Belk: We are lucky enough to have employees that understand that the equipment is very fragile. All of our ultrasound sonographers have been shown and demonstrated how to clean, care for, use and proper storage of transducers before they are allowed to perform studies on their own. As far as education to protect and maintain transducer health, we see this as extremely important.
Pongsatianwong: Technologist education on proper handling and cleaning of transducers is emphasized during onboarding and initial competency training to ensure best practices are followed consistently. Proper disinfection procedures, including using the appropriate manufacturer-approved disinfecting wipes is also a key point that is stressed to reduce damage to the transducer housing and cable. Each exam room is equipped with probe racks and transvaginal probe holder attachments to allow secure, convenient access and storage between patients. Less frequently used probes are stored in cushion-lined cabinets to prevent impact damage and reduce cable strain. Additionally, technologists are encouraged to report any probe performance concerns immediately so that issues can be addressed before they lead to failure or extended downtime.
high-quality imaging equipment, and know that having such allows us to have better exams, more accurate reads and thus happier patients.
Belk: Look for equipment that is sustainable in the future. Will have software updates that bring the newer technology to the equipment currently available. Looking for all-inclusive maintenance contracts
Pongsatianwong: We evaluate systems based on total cost of ownership, including factors such as reliability, service contracts, interoperability and expected lifespan. At the same time, we also consider a manufacturer’s future roadmap for anticipated release of new features that can elevate our department. To manage budgets effectively while staying technologically current, we increasingly look to partnership models with vendors that emphasize flexibility and life cycle management. These may include subscription- or service-based cost structures, trade-in programs, or bundled agreements that provide access to ongoing software updates and periodic hardware refreshes. This approach allows us to maintain cutting-edge imaging capability without the financial strain of repeated large capital purchases.
Q: WHAT ELSE WOULD YOU LIKE TO SHARE WITH ICE MAGAZINE READERS REGARDING PROBES AND TRANSDUCERS?
W&F: Proper storage and upkeep are key. As well as technologist awareness of proper usage and maintenance.
Pucillo: We are excited to see what the future technology brings and are committed to continue to grow and advance our imaging equipment to provide the best care possible to our patients.
Belk: Most ultrasound sonographers understand how fragile the transducers face is. It is also important to teach that cable and pin systems are equally as fragile.
HOW DO YOU BALANCE BUDGET CONSTRAINTS WITH THE NEED FOR HIGH-QUALITY
W&F: Maintain constant communication with financial leadership on needs, repairs and replacements so we can budget accordingly.
Pucillo: We view probes and high-quality imaging equipment as an investment. It is important to us to have
Pongsatianwong: Looking ahead, I think the most exciting part of probe and transducer development is how rapidly the technology is expanding the reach of ultrasound. We’re seeing smaller, smarter and more connected devices that can bring the same level of high-quality imaging. The pace of innovation means that partnering closely with vendors, sonographers and radiologists is more important than ever. As ultrasound applications continue to move into new clinical and procedural territories, transducer technology must continue to advance to keep pace with the growing demands of modern healthcare. •

The global ultrasound transducer market size was valued at $3.65 billion in 2023 and is projected to grow at a CAGR of 3.2% from 2024 to 2030, according to a Grand View Research report. The market growth is driven by the increasing use of ultrasound transducers in diagnostic imaging and non-invasive procedures, alongside advancements in transducer technology and frequent product launches by key players, the report states.
Grand View Research adds that “in addition, the rise in ultrasound-assisted surgeries and diagnostics for soft-tissue injuries contributes to this expansion. For instance, in September 2023, GE HealthCare received over $44 million from the Bill & Melinda Gates Foundation to develop AI-assisted ultrasound tools. These tools are designed to aid healthcare professionals in improving obstetric and lung scans for maternal, fetal and pediatric care.”
The availability of advanced ultrasound transducers is expected to drive the ultrasound transducer market during the forecast period.
The Grand View Research report also states: “Technological advancements in ultrasound transducers have enhanced image quality and expanded clinical applications, such as detailed imaging for various medical specialties. These innovations enable more accurate diagnoses and treatments, contributing to the growth of the ultrasound transducer market. The ongoing development of portable and AI-assisted ultrasound devices further broadens their use and accessibility. For instance, in September 2023, Exo Imaging Inc. joined the handheld ultrasound market with the launch of its AI-powered Iris system, following over $300 million in funding. Pronounced “echo,” the company announced the Iris device, which aims to replace traditional cart-based ultrasound machines with a sleek, portable unit that connects to a smartphone for image display.”
Precedence Research has also released a report predicting continued growth of the ultrasound transducer market.
“The global ultrasound transducer market size was calculated at $3.80 billion in 2024, and is projected to hit around $3.92 billion by 2025, and is anticipated to reach around $5.23 billion by 2034, growing at a CAGR of 3.25% from 2025 to 2034,” the report states. “The demand for the ultrasound transducer market is growing due to their rising use in medical fields like diagnostics and surgeries. The increasing prevalence of medical conditions also contributes to market growth.”
“The U.S. ultrasound transducer market size was exhibited at $1.03 billion in 2024 and is projected to be worth around $1.45 billion by 2034, growing at a CAGR of 3.44% from 2025 to 2034,” the report adds.
“North America dominated the global ultrasound transducer market in 2024,” it continues. “The dominance of the region is attributed to the well-established healthcare infrastructure in countries like the United States, which focuses on the adoption of advanced technologies. Governments are also contributing heavily to the adoption of medical technologies. Additionally, the rising prevalence of chronic diseases is leading to the need for advanced technologies. The rising influence of social media is also increasing health awareness among the population, which is focused on adopting diagnosis at an early stage.”
Global Market Insights (GMI) forecasts growth for the ultrasound probe market.
“Ultrasound probes market size was valued at $3.7 billion in 2023 and is estimated to grow at 3.7% CAGR from 2024 to 2032. Ultrasound probes, also known as transducers, are handheld devices used in medical imaging to generate and receive ultrasound waves. These probes consist of piezoelectric crystals that convert electrical energy into mechanical vibrations (sound waves) and vice versa,” GMI reports.
The global ultrasound transducer market will witness a robust CAGR of 6.8%, valued at $3.7 billion in 2024 , expected to appreciate and reach $5.5 billion by 2030, according to Strategic Market Research. •
Exo Iris is the company’s high-performance handheld ultrasound device. With affordable, AI-powered medical imaging in a pocket-sized device, caregivers can get to answers immediately to accelerate diagnosis and create new care pathways for heart failure patients at the point of care. AI-powered handheld ultrasound can lower the threshold for answers at the point of care, enabling access to simple and affordable medical imaging. With the launch of Exo’s latest AI capabilities, health systems and caregivers – particularly those in rural and under-resourced settings – can leverage Exo Iris to simplify the process of obtaining and interpreting medical images specific to the heart and lungs. As a result, caregivers can accelerate their patients’ diagnosis and treatment no matter where they are located. In addition to cardiac and lung AI, Exo Iris features Pulsed-Wave Doppler capabilities to provide physicians with even more opportunities to look at blood velocity to support diagnosis and deeper findings in cardiac, abdominal and vascular applications.

*Disclaimer: Products are listed in no particular order.
FUJIFILM Sonosite recently introduced the UHF46-20 Transducer, the world’s first and only 46-MHz ultra-high frequency (UHF) transducer for point-of-care ultrasound (POCUS). With a minimum scan depth of 4mm, the UHF46-20 Transducer enables clinicians to clearly visualize the first one to two centimeters beneath the skin and identify structures smaller than 1mm, such as superficial nerves and vessels, with high-quality resolution. The UHF46-20 transducer, when paired with the Sonosite LX system, enables the largest frequency range of any point-of-care ultrasound system on the market today – addressing a longstanding challenge that current clinical ultrasound systems have been unable to overcome. The combination of the new transducer and the Sonosite LX offers clinicians a versatile solution for a wide spectrum of imaging needs, spanning from deep abdominal scans to ultra-high resolution superficial assessments. The UHF46-20 Transducer holds promise for improving outcomes across a range of sensitive applications including neonatal intensive care unit (NICU) and rheumatology.

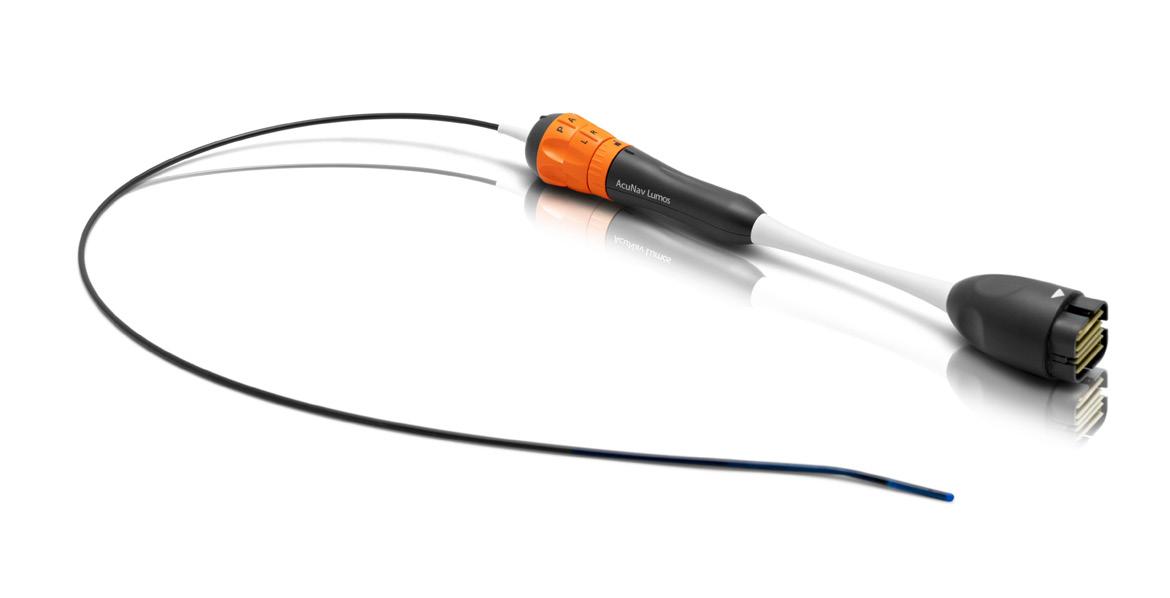
The AcuNav Lumos 4D intracardiac echocardiography (ICE) catheter, exclusively available on the ACUSON Origin ultrasound system, enables more treatment possibilities for more patients through the power of clinically relevant imaging. AcuNav Lumos’s improved biplane imaging and multiplanar reconstruction (MPR) delivers 4D imaging with or without ECG for diagnostic/clinically relevant volume rates. This provides excellence in anatomical assessment and device guidance. With real-time 4D color Doppler, this 4D ICE catheter allows for better leak detection, helping physicians identify complications during structural heart and electrophysiology procedures in real-time. AcuNav Lumos’s next-level tools enable device placement in even the frailest, most complex or contraindicated patients, and with conscious sedation, it supports optimal outcomes without compromising safety.
The new 6Sc-D probe introduced exclusively with GE HealthCare’s Vivid Pioneer, which launched in August 2025, is built on XDclear technology and is designed to enable clinicians to visualize fine anatomical structures and assess cardiac function with a new level of accuracy across a wide range of patients, from pediatrics to adults. Its elongated footprint and tip design improve intercostal access, making it ideal for adults with tight ribs or small body habitus.

• Register for free and apply to any of our listings
• Browse our 350+ open positions across the United States

• Get directly connected with industry hiring managers
• A talent network of 3600+ actively looking biomedical and imaging professionals
• A variety of listing and advertising options
• Social media, print, and eNews promotion
“HTMjobs.com is a remarkable website that can be used by any personnel looking for employment, internships, or just a good read from their Career Center . The site offers job postings from employers in the HTM industry, as well as resources for job seekers to help them prepare for their job search, including resume tips, interview advice, and more.”

BY MATT SKOUFALOS
At any healthcare facility, a capital project represents a sizeable budget, a business opportunity and a diversity of stakeholder interests. When that project involves the installation, relocation, or expansion of medical imaging equipment, it can become even more complex. So why don’t more facilities solicit the perspectives of the people who operate, maintain and repair those devices when they’re creating the spaces in which they’ll function?
Traditionally, biomedical engineers and imaging technologists have been absent from project management conversations related to imaging installations and site remodeling. But when they’re invited to become active participants in these discussions, healthcare decision-makers are discovering that their professional insights and the practical experiences gleaned from their work can add greatly to the conversations and improve the overall outcome of the project.
Glen McQuien, chief operating officer at Emeritus Clinical Solutions of Richardson, Texas, describes healthcare technology management (HTM) leaders as “break-fix kind of people” – capable, professional, but all too commonly siloed in their focus. That kind of specialized expertise doesn’t always lend itself to the lateral thinking from which facilities projects benefit.
“In today’s world, everything is integrated,” McQuien said. “Not only does an HTM professional need to know their trade, but knowing the clinical application of the technology is more and more critical. What is the patient experiencing? What monitoring is going on? What diagnostic systems are happening? To understand those, not at a physician or a nurse level, but a workflow level, becomes critical.”
If those questions aren’t asked until after a project is completed, “we’ve
missed an opportunity to add value to the process,” McQuien said. To his thinking, bringing imaging professionals in for project planning conversations is “the natural next evolution of IT and biomed joining together.” It reflects a commitment to comprehensively considering a project from its earliest stages, so that when a new imaging space is delivered, everyone understands not only how to best leverage the technology at its core, but the behind-thescenes workflow considerations that will dictate how that space optimally functions.
McQuien’s interest in learning to yoke the institutional memory of his imaging professionals arose from time spent as a biomedical director. He witnessed plenty of individual vendors advocating for priority on a job site, but no one coordinating their discrete technologies on the receiving side.
“That’s when I recognized that we had a huge gap,” McQuien said. “Many
biomedical groups or departments are never involved in the construction until it’s over. Large organizations get that perfectly right, but anyone who’s not a large corporate hospital with these resources needs someone to step into the gap.”
To McQuien, bringing imaging technologists and technicians into the conversation helps avoid cost overruns by tapping into a resource that already exists within the institution. Asking the people who work with the technology for their perspectives in designing the environment in which they’ll work can help improve their overall efficiency.
“From a construction perspective, if it isn’t done well, in comes the cables; in comes the power cords running across the floor,” McQuien said. “It presents itself not only as not the best design, but as a safety hazard.”
“Those things become critical,” he said. “When one piece is missing, healthcare is interrupted, and the patient pays the price. We can eliminate the sacrifice the patient is making because of poor planning.”
AS FAR AS PROJECTS GO, I’M A FIRM BELIEVER THAT FORM FOLLOWS FUNCTION. YOU HAVE TO BUILD SOMETHING ACCORDING TO THE FUNCTION YOU WANT IT TO SERVE. IF YOU DON’T HAVE THE RIGHT FOLKS AT THE TABLE, YOU’RE PRONE TO DOING IT COMPLETELY WRONG.
- MARIO PISTILLI, EXECUTIVE DIRECTOR FOR CHILDREN’S
HOSPITAL
OF LOS ANGELES
To that end, McQuien believes that the earlier imaging professionals are brought into the budgeting process, the more meaningful the impact can become, especially in helping to translate among different departments, or offering insights that come from an insider’s perspective.
“Technology is evolving rapidly, and sometimes we get ourselves into a corner where we only know one way to do it,” McQuien said. “‘This is the way we’ve always done it’ is a statement I absolutely despise. I’ve met with physicians; I’ve met with cardiothoracic surgeons. All of them gave me their perfect lab, and none of them was the same. You have to develop consensus.”
One of the most significant issues around which to build consensus, McQuien said, is that of patient and workplace safety. A hybrid operating room, for example, includes a variety of technologies, from medical imaging
systems to surgical robots to patient monitoring devices. Physical real estate is at a premium, and “there’s only so much geography” to manage competing interests, he said.
When they’re able to converse with each other fluently, however, “that’s where you start building capital.”
“I’ve never seen a control room big enough for what you want to do in it,” McQuien said.
“Everyone needs what they need, where they choose to stand, and it changes according to hospital workflow. The users will help you integrate it into that space.”
“[By adding in imaging professionals], you’re going to make it better –and other times, you’re going to make it excellent.”
Angelica Jaramillo, manager of pro-
gram operations at UT Southwestern Medical Center in Dallas, Texas, summed up the estimated savings that her project oversight work has preserved for her employer as “the argument for due diligence.” A radiologic technologist with a background in radiation safety, Jaramillo knew she could help eliminate over-spending on jobs by creating a more robust front-end vetting process and facilitating conversations among different departments within the institution.
“I’m the advocate for the tech and the facility,” Jaramillo said. “Healthcare professionals and facilities professionals speak different languages. I translate for both sides; I don’t pick sides. I try to break it down so they understand why we can’t do something or why we have to do this.”
“It’s all about letting everyone know that we’re a team,” she said. “We all have the same goal: to build this for patient care, and so a tech can work in there.”
going to cause artifacts in those images. You can’t have elevators too close, because any vibrations will distort image quality.”
“If we want to put a PET-CT somewhere, let’s make sure that space is strong enough to support that equipment,” she continued. “Some wholebody scanners can weigh 35,000 pounds, so you have to be sure that where you’re putting it can support it. You’re also looking at all the lead shielding that goes into the walls, the ceilings; and PET-CTs have to support all the other rooms required in the workflow.”
One of the most commonly overlooked considerations that Jaramillo said she has internalized is a commitment to charting the end-to-end path of travel a piece of imaging equipment will take as it’s moved throughout a facility.
UNDERSTANDING THAT THE PEOPLE AT THE TABLE ARE EXPERTS IN THEIR AREAS DOESN’T NECESSARILY MEAN THAT THEY’RE EXPERTS IN OUR DEPARTMENT OR OUR OPERATIONS.
THEY’RE SEEING IT FROM A MUCH MORE MACRO PERSPECTIVE, WHICH IS THEIR JOB, BUT SOMETIMES THAT [VIEWPOINT] NEEDS OUR PERSPECTIVE TO MAKE THAT WORK.
- RUTH RIZZO, RADIOLOGY PROJECT MANAGER
Jaramillo said, “I always make sure I get an end-user in the discussion because they know what kinds of procedures they’re doing, and how they’re doing it.”
“You have to include the end user,” she said.
Prior to the establishment of that deeper, multi-stakeholder planning process, Jaramillo said that new facilities installations often would begin as duplicates of an existing instance of the same technology elsewhere in the system – whether or not rolling out an identical site plan in a second location made sense, or was physically feasible. Sometimes that impulse, which might have begun as an attempt to save time and effort, led to oversights that resulted in costly setbacks and lost weeks.
“Two things you have to consider,” Jaramillo said: “one, what are you installing, and then, is that space even adequate to meet those requirements? MRI are the touchiest – very heavy, so you have to make sure you have the structure to support it, to get it there, and that there isn’t anything that’s
“Will you have to demolish rooms to do it?” she said. “What’s in those rooms? Once, we got to a good portion of our design, and discovered a tiny part of the hallway was a chokepoint where, for no reason at all, it became smaller for about 10 feet. The only way this equipment would have fit was cutting the walls down to the studs, and demolishing a corner of a room that turned out to hold the fire suppression system.”
Jaramillo works to incorporate a diversity of perspectives from multiple stakeholders in a project; those of everyone from medical equipment managers and facilities directors to technical supervisors, vendors and service specialists. When they’re all around the same table, she acknowledges that sometimes it can be intimidating for imaging technologists, in whom it is instilled to not shake up the chain of command, to advocate for what they believe is best for a project. That’s why Jaramillo works to create pathways for everyone to contribute their insight when it’s needed, regardless of their job title within the institution.
“I work with the smartest people in the world,” Jaramillo said. “A lot of my job is research to explain to them why
something isn’t a good idea. There are so many times that you’re in the ER, and if you don’t speak up, a problem could happen. If an expert is wrong, you’re worried that you’re going to get chewed out. In reality, you’re the one who works in the space; if anything, you’re the expert here.”
When those conversations arise, Jaramillo said she typically falls back on a shared value: that patient care is the highest and best priority of any healthcare system. A poorly designed imaging suite would be detrimental to that priority, and so that’s ultimately the common ground most stakeholders can find in working to advance the goals of any project.
“Working in a hospital setting, everyone knows that patient care is the utmost priority,” Jaramillo said. “Everything we do is for patients.”
Children’s Hospital of Los Angeles Executive Director for Imaging Mario Pistilli credits his radiology project manager, Ruth Rizzo, with supporting his role by helping to coordinate and facilitate high-level, necessary conversations around construction projects and process improvement.
Instead of multiple members of his team needing to walk other decision-makers through imaging operations, Rizzo can field their questions, debrief afterwards with other department heads, and determine when to bring them in as needed.
“Now, instead of teaching five people, I have one person in my operation who attends all our meetings, once a week, to talk about departmental issues,” Pistilli said. “She can go get that information, or might already know it at a high level.”
In the decade she spent with the radiology department, Rizzo’s talent and versatility was indispensable. When Pistilli asked how he could support her professional development, Rizzo said she had an interest in project management, but lacked the credentials to pursue it. Pistilli supported her efforts to get the schooling she needed, and created a role in which she could leverage
it to fill needs within the department.
“As far as projects go, I’m a firm believer that form follows function,” Pistilli said. “You have to build something according to the function you want it to serve. If you don’t have the right folks at the table, you’re prone to doing it completely wrong.”
“[Ruth] can attend meetings, escalate, sift through, and find the right people,” he said. “Prior to her dedicated position, I did everything myself. Now she’s involved from the very first submission for a project to even happen, all the way through completion.”
Rizzo helps select designers, contractors, and medical equipment; identify stakeholders before design begins; and negotiate among them all. When the success of a project hinges on the time, effort, and energy of its participants, realizing that everyone’s professional lives are intertwined is a key place from which to operate, Pistilli said.
“Everyone brings their experiences, so it just makes the chance for success greater the more heads you put into the equation,” he said.
Rizzo said that her professional self-confidence is strengthened by the support she receives from her boss. She said she’s leaned on Pistilli’s example for building cross-disciplinary consensus by welcoming a variety of perspectives to get to a better outcome.
“Understanding that the people at the table are experts in their areas doesn’t necessarily mean that they’re experts in our department or our operations,” Rizzo said. “They’re seeing it from a much more macro perspective, which is their job, but sometimes that [viewpoint] needs our perspective to make that work.”
“I’m no expert, but I can tell when somebody needs to be brought into a conversation,” she said. “You don’t have to be a subject-matter expert to be a successful project manager; you just have to be curious, ask a lot of questions, and find those areas where the subject-matter experts need to be brought in.” •





“Quality” and “Safety” – these words are used often in healthcare, but what do they really mean in practice?

BY DARLENE K. HUMPHREYS
At the Intersocietal Accreditation Commission (IAC), quality and safety aren’t just abstract ideals. They are the foundation upon which every accreditation program is built. Understanding their true meaning is essential for any facility striving to deliver top-tier patient care.
Quality is not merely about doing things well, it’s about doing them right, consistently, and in accordance with established standards.
Definition: The standard of something as measured against other things of a similar kind; the degree of excellence of something.
In healthcare, this means providing services that are:
• Evidence-based
Darlene K. Humphreys, AS, RT(R)(M)(MR) (CT), is the director of accreditation for the Intersocietal Accreditation Commission (IAC)-MRI. In 2009, Humphreys began working with IAC as an MRI/CT application reviewer. Her longstanding commitment to imaging excellence led her to join IAC full-time in June 2021. She has experience in a variety of clinical settings including hospitals, free standing imaging centers and teleradiology, giving her a unique perspective on the needs of many.
• Performed with technical accuracy
• Interpreted by qualified professionals
• Delivered with a patient-first mindset
While quality speaks to excellence, safety speaks to trust. Patients deserve to know they are well cared for – where risks are minimized and protocols are in place to protect them at every step.
Definition: The condition of being protected from or unlikely to cause danger, risk, or injury.
Safety in healthcare involves:
• Following best practices to avoid errors
• Maintaining equipment and environments to prevent harm
• Ensuring all staff are trained and competent
• Creating a culture where speaking up about concerns is encouraged
Quality and safety are not optional – they are expected. Through accreditation, the IAC
helps facilities demonstrate that they meet these expectations not only in principle, but in practice. Accreditation is both a benchmark and a motivator: it assures patients, payers, and providers that excellence and safety are at the forefront.
All patients who enter into the healthcare system in America deserve many things. Most healthcare facilities have developed their own list of quality points, often referred to as a Patient’s Bill of Rights. These rights vary from facility to facility, state to state, but they generally contain the same items:
• Right to Respectful Care: All patients have the right to receive considerate, respectful, and dignified care without discrimination based on race, religion, or any other factor.
• Informed Consent: Patients have the right to be fully informed about their diagnosis, treatment options, and the qualifications of their healthcare providers before consenting to or refusing procedures.
• Right to Refuse Treatment: Patients have the right to refuse medical treatment or to withdraw from experimental research after being fully informed of the consequences.
• Confidentiality and Privacy: Patients’ communications and health information must be treated confidentially and protected.
• Access to Emergency Services: Patients have the right to access necessary emergency health care without delay.
• Participation in Treatment Decisions: Patients have the right to participate in all decisions related to their own healthcare, including making an advanced directive.
• Cultural and Spiritual Values: Patients’ cultural, psychosocial, spiritual, and personal values and preferences must be respected during their care.
These demonstrate basic rights that are promised to each of us at the most vulnerable times in our lives. However, nowhere in this bill of rights is quality and safety ever mentioned.
Are those things just inherent? Do we just assume that facilities or healthcare workers have a calling to ensure that their work and caring is quality work? Or, that they are providing as much protection and safety as possible?
Benchmarking quality and safety can indeed be complex – these attributes can be moving targets without standardized, clearly defined guidelines. What one person considers a “quality” outcome may differ significantly from another’s perspective. To reduce ambiguity and ensure consistency, the best approach is to establish a formal quality and safety improvement program.
A quality and safety program provides a structured framework to assess, improve, and maintain processes. It outlines clear direction, timelines, activities, and evaluation metrics.
1. Form a Quality Improvement (QI) Team & Define Objectives
• Select key personnel who are committed to the program’s success.
• Clearly define what you are trying to accomplish – specific outcomes related to quality and safety.
• Identify measures that provide meaningful and actionable data.
• Focus on areas you can control and avoid overextending into variables outside your influence.
• Establish minimum thresholds or boundaries for each metric to reduce individual interpretation and ensure consistency.
2. Begin Gathering Data
• Collect data across multiple points in time to determine a reliable baseline average.
• Ensure data is objective, measurable, and repeatable.
• For each measure that falls below threshold, develop and document a corrective action plan.
3. Identify Opportunities for Improvement
• Use your data to pinpoint weaknesses or areas needing attention.
• Activate your corrective action plans and monitor for effectiveness.
• Consider how best to communicate your quality strategy to internal stakeholders for better alignment and support.
4. Set Specific, Realistic Goals
• Once you establish baseline performance, set attainable improvement goals.
• Goals should be SMART: Specific, Measurable, Achievable, Relevant, and Time-bound.
• Assign reasonable time frames for reaching each goal.
5. Monitor Progress & Evaluate Results
• Regularly monitor outcomes and evaluate trends.
• Share results – both positive and negative – with your entire organization.
• Highlight and celebrate successes.
• For underperformance, revisit and implement your corrective action plan promptly.
6. Sustain the Improvement
• Prevent regression by maintaining ongoing monitoring.
• If performance dips, early detection allows for quick intervention.
• Continually refine your processes to adapt to new challenges and maintain gains.
Implementing and managing a quality and safety program can be time-consuming and, at times, tedious. We won’t pretend otherwise. However, there are resources available to help streamline this process and make it more manageable.
The IAC offers a suite of QI tools designed to support facilities in their commitment to safety and excellence in medical imaging. Importantly, you do not need to be an IAC-accredited facility to access these tools. While setting up a free account is required, the tools themselves are available at no cost to all users and can be accessed at intersocietal.org.
The most comprehensive resource available is the IAC QI tool. It provides an easy-to-use, self-assessment platform that helps facilities evaluate performance across four key quality measures.
By participating in this initiative, your facility gains valuable insights into its quality and safety practices, empowering your team to make informed improvements and maintain high standards of care.
This platform is an easy to use, self-assessment for facilities to evaluate four key measures of quality, as defined in the IAC Standards:
• Test appropriateness
• Technical quality and safety of the imaging
• Interpretive quality review
• Report completeness and timeliness
For facilities pursuing accreditation or reaccreditation, use of the QI tool will ensure compliance with the requirements. Those not participating in the IAC process are welcome to access the QI tool as a method for developing their own QI program; again free of charge.
Other tools provided by the IAC include Accreditation Simplified live and on-demand webinars. These webinars also include a continuing education credit for attendees and are offered at no cost to everyone.
It depends on thoughtful planning, ongoing commitment, and the dedication of a few conscientious individuals to stay healthy and effective. Like any living thing, it needs care and attention. It thrives on the data you feed it – and in return, it grows stronger, providing valuable insights that support your patients, your staff, and your entire facility.
Nurture it. Invest in it. And it will reward you with better outcomes and a safer, higher-quality environment for all. •


DIRECTOR’S CUT
BY BETH ALLEN
Ihave heard that we retain only 25% of what we hear. Based on my own experience, I believe this to be an accurate statistic. To actively listen may be the number one key to improved communication. This is a skill that needs to be honed, and we have to follow some rules to become good at it.
The definition of active listening is beyond just hearing the words. I used my research partner, Professor Google, and this is what I found: “Active listening is a communication skill that involves actively processing and seeking to understand the meaning and intent behind the words spoken by another person. It requires being a mindful and focused participant in the communication process, paying attention to both
verbal and nonverbal cues.”
It is not listening to wait for a pause to interject a response.
Another way to phrase this would be attentive listening. I am being attentive while someone else is speaking. I am giving my full attention.
I can demonstrate my full attention by maintaining eye contact if we are speaking in person. It is easy to be distracted by things happening around us, but if we are having an important conversation then it is critical that we can ignore those distractions. Our body language, facial expressions and responses to what is being said give the speaker confirmation that we are completely engaged in the conversation. Nonverbal communication is just as important as a listener. A smile and nod can be a powerful message to the speaker and
give them confidence to continue. The opposite will happen when the listener is fidgeting, checking their watch or looking at anything other than the speaker.
The listener also needs to participate in the conversation. By asking clarifying questions or summarizing what was heard, we can make sure we are truly understanding the intent of the speaker. It will reinforce that the listener is interested in what is being said.
Although it may be difficult at times, it is beneficial to not judge the viewpoint of the speaker. If we try to understand what is being said, ask clarifying questions to make sure there is a clear understanding before letting any predetermined thoughts enter our minds. It is also important to listen for what the meaning is behind what is being said. What emotion is behind the point being made.
In order to be a good active listener, I believe there are some old habits that need to be broken. It takes a lot of concentration to be a good listener.
We need to be present, which may take some mindfulness work on the side.
We need to be consciously aware of what the perception is of how we are listening.
One tip is to repeat the speaker’s words in your head to block out wherever your mind may be wandering to.
We should also end with a recap of key points or sum-



mary of what was said at the end of the conversation. This skill is important when communicating with anyone but needs to be in practice with every patient that we speak with. They are in an unfamiliar environment, concerned about the test or maybe just the results of the test. They also may not have had a chance to really discuss their concerns with anyone before you. Healthcare has become so fast paced that those discussions do not always happen the way that they should. Patients may be desperate to feel like someone listened to them.
If we take a minute to actively listen, we may get to the bottom of what they are trying to communicate more efficiently. Hopefully, they will leave feeling heard, cared for and relieved.
To actively listen, there cannot be any multi-tasking. Multi-tasking is really a fantasy anyway. It is what makes us feel like we are accomplishing lots of things but is really getting in the way of accomplishing anything well. It clouds our mind, increases stress and is not efficient. This is my commitment for the New Year – no multitasking. Pick something and finish it. That is a whole different subject …
Thanks for all you do! •
Beth Allen, RT(R)(CT), CRA, is the director, clinical operations at Banner Imaging
- New Windows 10 Platform with Dynamic Digital DR Panel
- Eliminates the OEM Saturn Windows 95 Platform
- Dose Reduction
- HIPAA Compliant, 510k approved.
- Fluoroscopy digital recording loops for MBS studies
- Upgrade Provided to your Proven R/F System in 4 days.
- Complete Refurbished Systems Available



BY MEREDITH CHECK, M.P.P.
Now that most state legislative sessions have concluded and proposals are being submitted for the 2026 legislative sessions, this is the perfect time to reflect and plan. Here’s a look at what ASRT has done, what’s in store for 2026 and, most importantly, the ways the medical imaging and radiation therapy community can engage with advocacy.
As we move into the next legislative session and policy proposals are introduced, ASRT Government Relations continues to prepare for legislative and regulatory work. We are evaluating the political and policy landscape that will affect medical imaging and radiation therapy professionals across the country. ASRT will advocate for proposals that uphold nationally recognized education, training and credentialling standards while enhancing quality, safe patient care. We also expect the 2026 elections to affect our advocacy efforts. Local, state and federal government elections will be held in 2026, primary elections will begin this spring, and the November 2026 general election is a year from now.
You may wonder how these elections are relevant to the policy landscape. Politicians who are in tighter re-election campaigns may introduce more aggressive proposals to demonstrate that they are being productive. In states that typically support a smaller footprint for state government, this could mean efforts to deregulate and remove vital protections from the medical imaging and radiation therapy profession. If an elected official has strong support from other healthcare
workers, it could manifest as expanded scopes and encroachment. All this to say that election years bring a sense of urgency for elected officials. As advocates it’s our job to stay on track so that worrying policies do not make it through.
Along with tracking, monitoring and responding to proposed legislative and regulatory changes at the state level, ASRT continues to work with the federal government to elevate the medical imaging and radiation therapy profession and promote patient safety. Partnering with other organizations representing the profession, the ASRT has worked to improve reimbursements for diagnostic imaging and radiation oncology procedures. ASRT submitted comments on both the Medicare Physician Fee Schedule and Outpatient Prospective Payment System for calendar year 2026.
In collaboration with the American Society for Radiation Oncology, ASRT launched a grassroots campaign in support of the Radiation Oncology Case Rate (ROCR) Value Based Payment Program Act of 2025 (S.1031/H.R.2120). ASRT supports ROCR because:
• It is a viable payment reform proposal that would usher in a new era of stable payments after years of declines and consolidation.
• It would increase access to care, improve the quality of cancer treatment and reduce disparities for rural and underserved patients.
• It would encourage innovation and lower Medicare spending and patient costs.
Along with radiation therapy reimbursement, ASRT has also launched a grassroots campaign in support of S.1692,
the Radiology Outpatient Ordering Transmission (ROOT) Act. The bill addresses implementation concerns raised by the Centers for Medicare & Medicaid Services by simplifying the administration of the Appropriate Use Criteria program that was authorized by the Protecting Access to Medicare Act of 2014. If it passes, the bill will streamline the use of AUC so Medicare beneficiaries receive appropriate advanced diagnostic imaging services, and it will save money for Medicare beneficiaries and the Medicare system.
This legislation will reduce the ever-increasing volume of imaging studies that are ordered and ensure that only appropriate imaging tests are performed. It will do this by requiring clinicians to consult evidence-based, physician-developed clinical guidelines at the point of ordering.
The Society is also partnering with other organizations to ensure that the regulations protecting patients from ionizing radiation exposure remain in place. For example, an executive order was issued instructing the Nuclear Regulatory Commission to re-evaluate the principle of ALARA – as low as reasonably achievable – and its usage with power plants. However, ALARA is a critical radiation safety principle within healthcare. Therefore, ASRT is keeping a close eye on what impacts the changes to industrial radiation safety will have on medical radiation safety.
One of the questions ASRT staff have received from mem-
bers is the status of the Medicare Access to Radiology Care Act, or MARCA. This proposed legislation would amend the Medicare reimbursement policy for radiologist assistants to align with state radiologist assistant licensure laws.
Under MARCA, Medicare would fully reimburse facilities for procedures or services, regardless of the setting in which the service is performed – hospital, critical access hospital, ambulatory surgical center or any other facility setting. ASRT is steadfast in its support of RAs and its work to enact MARCA.
Rest assured, ASRT has continued and will continue to work with MARCA partners and champions in Congress to further this effort. For bills to move smoothly through the legislative process and become law, policy proposals require work behind the scenes. ASRT remains committed to this work.
A federal government shutdown continues as of October, the time of writing. Most of ASRT’s federal efforts will continue throughout 2026, which is the last year of the 119th Congress. ASRT and its allies will be sprinting to the finish line before newly elected officials move as a result of the November 2026 elections. •
Meredith Check, M.P.P., is the ASRT Director of Government Relations and Public Policy. She holds a master’s degree in public policy from American University’s School of Public Affairs and has nearly 10 years of advocacy and public policy experience. She joined the ASRT’s Government Relations and Public Policy Department in the fall of 2021.


BY MARK WATTS
One day in the not-so-distant future, a patient named Lisa leaves the hospital wearing a small adhesive device on her chest. The patch, a Medtronic BioButton, is no bigger than a coin, yet it continuously measures her heart rate, breathing and body temperature. It sends that data wirelessly to her doctor so they can make sure she’s recovering safely at home. Lisa hardly notices it; the device has become just another part of modern life – quietly working in the background to keep her healthy.
What Lisa and millions of other patients don’t see, however, is the invisible world her data travels through. Each of those wireless transmissions – carrying her most private health details – passes through networks, cloud systems and public WiFi before reaching the hospital’s servers. At any point along that invisible journey, someone could be listening.
This risk isn’t imaginary. Across the country, healthcare systems are experiencing a surge in what experts call the Internet of Medical Things, or IoMT. It includes everything from hospital monitors and insulin pumps to consumer smartwatches and home oxygen machines. These tools continuously collect and transmit sensitive health data, often through unprotected or weakly encrypted connections. For hospitals, the technology brings better patient care – but also opens the door to one of the least understood cybersecurity threats today: data
interception during transmission.
Think of it like sending an important letter. Your hospital protects its servers like a locked vault and guards its data centers like a fortress. But what about the moment that letter is carried through the air by a postal worker? That’s where it’s most vulnerable. For wireless patient data, interception during transmission is that unguarded moment. Hackers don’t need to break into servers or steal a password. They just need to position themselves between a device and the network, silently capturing sensitive data as it flows by.
A single vulnerable point in a patient’s data journey can cause major harm. Imagine if someone intercepted Lisa’s BioButton transmissions from her phone while she sat in a café with public WiFi. With simple, commercially available tools, an attacker could eavesdrop on Bluetooth signals, uncover her health patterns, or even clone her monitor’s communication link. Lisa wouldn’t know. Her doctor wouldn’t know. Her hospital wouldn’t know – until the damage was done.
The real tragedy is that most healthcare security systems aren’t built to stop this kind of threat. Firewalls, antivirus tools, and encrypted storage protect information that’s at rest, sitting safely in databases. But once that information starts moving through the wireless airwaves, those traditional tools fall silent. Many connected devices still rely on old communication protocols that offer little or no encryption, making the problem worse. Fortunately, new technology is stepping in to fill that gap – and it’s powered by artificial intelligence. Systems that use AI are redefining cybersecurity for connected medical envi-
ronments. Instead of waiting for a system breach or data theft to occur, AI empowered cybersecurity actively watches every transmission as it happens, identifying and neutralizing threats in real time – often within a fraction of a second.
Here’s what makes AI empowered cybersecurity different. It uses advanced learning algorithms that understand how each connected device normally behaves. Over time, it learns the baseline patterns for a hospital’s entire IoMT ecosystem – from BioButtons and pacemakers to infusion pumps and smartphones. If a single transmission seems even slightly off, the AI flags it instantly. That’s the power of sub-second detection. No human could monitor millions of wireless transactions that quickly or accurately.
When the system detects abnormal behavior, it acts automatically. It isolates the affected device, stops the suspicious transmission, and alerts healthcare security teams before data can be stolen or tampered with. This isn’t theoretical. GuardDog AI’s approach to behavioral analysis, end-to-end encryption monitoring, and device authentication closes the biggest blind spot in digital healthcare – the one between your devices and your servers.
Beyond security, AI also helps hospitals stay compliant with regulations like HIPAA. It automatically maintains detailed audit trails, proving that every wireless communication pathway is

continuously protected and documented. For hospital leadership, that means fewer headaches, faster compliance reporting, and more trust from patients and regulators alike.
But perhaps the most meaningful advantage is peace of mind. For patients like Lisa, it means her doctor isn’t just receiving accurate data – all that life-saving information is being transmitted in a protected digital space. For hospitals, it means their IoMT network can keep growing without exposing their patients or their reputations to unnecessary risk.
As healthcare continues to evolve, the line between medicine and technology will only blur further. Devices will grow smarter, data will move faster, and expectations will rise higher. The solution isn’t to slow progress; it’s to secure it. AI systems like GuardDog give healthcare organizations the confidence to innovate safely – protecting patients while ensuring the future of connected medicine stays both intelligent and secure.
In the digital age, every heartbeat, every breath, and every byte of patient data matters. AI is making sure they all stay safe. •
Mark Watts is an experienced imaging professional who founded an AI company called Zenlike.ai.
Image One Medical is the only Engineer-Owned medical equipment service group that is fully dedicated to Florida’s amazing base of Imaging Centers, Hospitals, and Cancer Treatment Centers.
We have a mission: Self perform on every aspect of our business. Specialize on specific modalities: Pet CT, CT & MRI, and Focus in a key geographic region. Fort Myers I Fort Lauderdale I Tampa I Orlando
FLORIDA BASED
Dealer and servicer of PET CT, CT and nuclear medicine
• Equipment service: full coverage plans
• Equipment sales: installation, relocation and project management
• Mobile coach construction, refurbishment, maintenance and management


BY DANIEL BOBINSKI
ncient wisdom packed into short, memorable phrases has guided humanity for millennia. These pithy statements carry profound truth that transcends time and culture. Consider Aesop, who around 600 BC observed, “Better to be wise by the misfortunes of others than by your own.”
Jump forward 250 years and Aristotle taught us, “We are what we repeatedly do. Excellence, then, is not an act, but a habit.” A couple of centuries later, Cicero advised, “Never go to excess, but let moderation be your guide.”
These insights aren’t even close to the oldest. Around 900 BC, King Solomon penned statements like, “A gentle answer turns away wrath, but a harsh word stirs up anger,” and “Plans fail for lack of counsel, but with many advisers they succeed.”
Want to go back even further? The “Instructions of Shuruppak” – also known as the Babylonian Counsels of Wisdom from 1500 BC – gave us gems like “Do not say evil things; speak well of people,” and “Reverence begets favor.”
Each of these brief statements contains enough wisdom to fill volumes. Although we could write books expounding on any single axiom, the beauty of these axioms lies in their brevity. That said, the challenge isn’t finding good axioms, it’s making them work in our lives.
It’s here where we often fall short. We nod in agreement when we hear a clever saying, and maybe we even share it on social media. But too often it stops there. We move on without letting the power of the words sink in.
Axioms work best when we connect them to our own experiences. Take the image of a turtle making progress. A common axiom states: “Turtles make progress only when they stick their necks out.” There’s rich symbolism there. By pushing ourselves past our comfort zones, we reach our destinations.
Ask yourself: “When have I done that?”
Other axioms carry the same idea. “No risk, no reward.” “Nothing ventured, nothing gained.” “A journey of a thousand miles begins with a single step.” These are all powerful statements, but don’t just acknowledge their wisdom. They’ll be more useful when you can connect specific events from your past to keep your future more balanced and productive.
Even better, tie a saying to multiple experiences. By doing that, your brain creates even stronger neural pathways connecting you to that wisdom. The connections are even stronger when you link an axiom to an event that carried strong emotional weight. In other words, identifying multiple situations or even one intense experience can cement an axiom’s value in your mind.
During decades of coaching and management training, I’ve selected or developed multiple workplace axioms that consistently help people succeed. Several of them are listed below. Hopefully these will resonate with your own experiences.
You’ll go where you’re focused. Any good driving instructor teaches this principle: Your vehicle travels in the direction you’re looking. Life works the same way. Focus dominates destination. If you’re constantly looking at trouble spots, you’re likely to stumble into them. But when you focus on potential solutions and paths that lead toward success, you’re far more likely to achieve success. Think about this principle in your own experiences. When has your focus helped you reach your desired destination?
Slower up front equals faster down the road. Type A personalities need to memorize this one. The quickest way to get from point A to point B isn’t always a straight line, especially when working with others. About 65% of the population processes decisions more slowly than the typical driver personality. Therefore, Type A personalities can

capitalize on a paradox. When they slow down to work with others, they often get faster results overall. Many “fast movers” doubt this at first, but they eventually find it to be true. If you’re a fast mover, give focused thought to this one.
Acknowledgement does not equal agreement. Effective communicators master this vital distinction, and it’s invaluable for conflict resolution. Unfortunately, too many people hold the mistaken belief that by acknowledging someone’s viewpoint they’re endorsing it as truth. This is not true! You can fully acknowledge another person’s perspective without accepting it as correct.
As a silly example, let’s say someone believes the moon is made of blue cheese. We can acknowledge someone holds that belief even though we completely disagree with it.
Think about when someone has respectfully acknowledged your position without agreeing with it. Chances are that action allowed the conversation to continue without any unneeded tension. Mastering the ability to acknowledge without agreeing transforms your communication effectiveness.
Value the differences. Our current culture makes it far too easy to criticize people who operate differently than we do. We find fault with coworkers whose approaches don’t match our own methods. But here’s the truth: diverse styles bring diverse strengths, and workplaces benefit from having diverse kinds of strengths. The driver personality excels at swift, bold decisions. The analytical mind catches critical errors others overlook. The relationship-builder creates essential team cohesion. The creative thinker sparks breakthrough innovations.
Rather than criticizing differences, we must actively and consciously choose to value what others bring to the table. Even better if we celebrate and leverage those distinctions. When has someone whose style completely differs from yours delivered exactly what the situation required?
Only make new mistakes. This principle partners well with a quote attributed to Theodore Roosevelt: “The man who never makes a mistake is the man who never does anything.” The truth is that everyone makes mistakes, but problems arise when people make the same mistakes repeatedly, never learning from them. When have you chosen to learn what to do or not do after a mistake has been made?
This principle of learning from mistakes connects with another favorite saying of mine: “Good judgment comes from experience; experience comes from bad judgment.”
Bottom line, remember that good axioms can influence your life’s direction. Therefore, knowing that you’ll go where you’re focused, I strongly suggest deliberately selecting memorable phrases to guide you in useful, productive and excellent ways. •
Daniel Bobinski, who has a doctorate in theology, is a best-selling author and a popular speaker at conferences and retreats. For more than 30 years he’s been working with teams and individuals (1:1 coaching) to help them achieve excellence. He was also teaching Emotional Intelligence since before it was a thing. Reach him by email at DanielBobinski@ protonmail.com or 208-649-6400.

BY NICOLE DHANRAJ
he headlines declared the end of DEI. The reality in radiology departments, however, was a quiet, creative pivot.
As 2025 draws to a close, radiology leaders across the country are taking a collective deep breath. It’s been a year of fatigue, tension, and hard questions about the future of diversity, equity, and inclusion in healthcare. We watched as DEI offices were restructured, training programs were paused, and the term “diversity” became politically charged. In many institutions, leaders had to choose between policy compliance and personal conviction.
Yet, radiology’s initiatives remain standing.
The mission hasn’t changed. The intent hasn’t disappeared. If anything, this year has reminded us that equity was never about slogans or mandates. It’s about people: the teams we build, the colleagues we nurture, and the patients who trust us with their care.
Here is how we kept the spirit of equity alive, and how we can hardwire it into quality for 2026.
1. The Tightrope Between Compliance and Conviction
For many department chairs and imaging directors, 2025 was a balancing act. The quiet creativity of our field, known for rapidly adjusting protocols and reimagining workflows, was on full display.
I heard from leaders that they had to pause their DEI committee, but instead, they created different committees and councils with different names. The mission didn’t change. They just changed the language.
Leaders successfully folded equity and inclusion into everyday operations. They embedded fairness in hiring, redesigned faculty development under “leadership growth,” and framed mentorship as “talent sustainability.”
When you create spaces where people feel seen and supported, that is equity in action, regardless of the label.
2. The Fatigue Was Real But So Was the Progress
By midyear, many teams admitted to feeling deep fatigue. The constant push and pull between enthusiasm, bureaucracy, and backlash left people drained.
And yet, beneath the fatigue, meaningful progress con-
tinued quietly. Departments started using dashboards not just to count representation, but to track retention, promotion equity, and sense of belonging. This progress was often driven by micro-movements such as culture/empathy focused lunch and learn Fridays where technologists and physicians share patient stories that taught them empathy, or celebrating cultural holidays to build connection.
3. Expanding Equity Beyond People Into Practice
This year also expanded our view of what equity really means in radiology. It’s not just about who’s in the room, it’s about who gets access to the scan, the technology, and the care. Equity showed up in unexpected places:
• AI researchers began auditing their models to ensure algorithmic fairness across patient populations.
• Community imaging centers partnered with mobile screening units to reach rural and underserved communities.
• Radiologists spoke up about the subtle ways bias can enter reporting language, building lexicons that are more neutral and patient-centered.
4. Belonging Became the New North Star
When the politics got loud, many departments refocused on something simpler and more universal: belonging. At its core, every professional from the reading room to the front desk wants to feel valued, respected, and safe to contribute.
Belonging is the emotional pulse of inclusion. Small efforts such as recognizing international medical graduates on their anniversaries or creating short “get to know me” profiles created connections that built resilience.
The question isn’t “Will DEI survive?” It’s “How will we carry its spirit forward?” Here are five ways to hardwire equity into your department’s muscle memory.
1. Reframing
Even if your institution has pulled back on DEI language, your core values, equity, respect, and fairness don’t need to change. Frame them as pillars of quality, safety, and team excellence. When teams are diverse, they diagnose more accurately. When leadership is fair, burnout decreases. You don’t need a DEI office to live those values, just consistency and courage.
Make inclusion invisible in the best way possible. It shouldn’t require a committee meeting to make fair hiring decisions or ensure every voice is heard in rounds.
One radiology department started requiring every hiring panel to include at least one member outside the subspecialty to minimize “like-me” bias. Another created a simple “decision debrief” after major staffing changes, where leaders explained the rationale transparently. That’s inclusion in motion not as an initiative, but as deeply ingrained practice.
3. Prioritize Sponsorship: Talent Protection for At-Risk Groups
If 2025 showed us anything, it’s that representation without support leads to attrition. Mentorship and sponsorship are still the most powerful tools we have.
Encourage experienced staff to actively advocate for others in leadership discussions (“Have we considered them for this role?”). That simple act of sponsorship often changes a career trajectory protecting diverse talent from burnout and ensuring we retain high-potential professionals.
Diagnostic
Keep connecting internal equity efforts to external outcomes. Radiology’s mission isn’t only about workforce composition it’s about diagnostic fairness and patient trust.
When an algorithm overfits to one population, or when a scheduling policy systematically limits access for rural patients, that’s an equity issue disguised as an operational one.
As leaders, we can use language that everyone sup-
ports: quality, safety, access, and trust. That’s equity translated into the language of healthcare excellence.
5. The Leadership Pulse: Small Actions, Big Culture Change Culture starts at the top, and leadership isn’t about grand gestures. It’s in how you respond when someone is interrupted in a meeting. It’s whether you rotate who presents cases in conference. It’s if you say, “Tell me more about your perspective,” instead of assuming. These are the small, daily decisions that either build or break inclusion.
As the year ends, it’s worth remembering: the spirit of equity doesn’t live or die based on whether it’s written in a strategic plan. It lives in how we treat each other. Radiology has always been a field defined by vision, by our ability to see clearly what others might miss.
So, maybe that’s our task for 2026: to keep seeing people fully, their talent, their stories, their potential even when the headlines say otherwise.
So, maybe that’s our task for 2026: to keep seeing people fully, their talent, their stories, their potential, even when the headlines say otherwise
Because the work isn’t gone.
It’s just grown quieter, deeper, and more human. And sometimes, that’s when real change finally begins. •
Nicole Dhanraj, Ph.D., SHRM-SCP, PMP, GPHR, CPSS, CRA, R.T(R)(CT)(MR), is an experienced imaging director.




Occasional stress is a normal part of life for the majority of people. We experience it from time-to-time, depending on what we have going on in our lives. It becomes a concerning issue, however, when it’s ongoing and taking up too much time in one’s life. Chronic stress can lead to people becoming unhealthier and less financially stable. Many people make poor health and financial decisions when stressed, making it crucial that they keep stress to a minimum and learn how to reduce it.
“Without a doubt, stress gets in the way of people reaching their health and wealth goals,” said Jeff Smith, a financial planner and owner of The Retirement Smith. “It weakens the body and often your bank account. Learning about what you can do to avoid and manage it should be a high priority for everyone.”
According to the National Institutes of Health, stress is a physical and emotional reaction that people experience as they encounter changes in life. When people are feeling stress their body goes into a “fight-or-flight” mode, due to hormones that are being released. While this happening occasionally is normal, when it becomes frequent or chronic it can contribute to worsening of health problems, including asthma, depression, anxiety and other mental illnesses. It can also contribute to worsening digestive issues, sleep disorders, headaches, etc.
Ongoing stress can take a toll on our daily lives in numerous ways. The Centers for Disease Control and Prevention (CDC) reports that stress can lead to changes
in appetite, energy, desires, and interests, as well as lead to trouble concentrating and making decisions. For some people, this may lead to things like overeating, emotional eating, using drugs or alcohol, retail therapy and making financial decisions that may be regretted later. Stress reduction and management should be a top priority for everyone. While most people realize this, they may not always know what steps to take to make it happen. Here are some tips to help keep stress under control:
• Get mentally healthy. Protecting mental health is a must for those who want to manage the stress in their lives. To do this, the CDC recommends taking breaks from the news, practice daily gratitude, connect with others, and do things that will help reduce stress, such as meditate, spend time outdoors or find other ways to relax.
• Get physically healthier. Taking care of your body is important to managing stress. This can be done by getting enough sleep, staying physically active, eating healthy, limiting alcohol and avoiding smoking. Being physically active helps to reduce stress and keep the body healthier, as well as improves one’s emotional well-being.
• Become financially secure. One of the top things that people stress over is finances. Having financial security helps to alleviate the stress risks from the issue. Focus on having an emergency fund and a plan for navigating the future financially.
• Get help when needed. There are times when people need to work with someone to achieve the goals they desire. Whether you need to team up with a financial planner to address money matters, a dietician to learn to eat healthier, or a personal trainer to improve health,
the return on investment will be solid.
• Have patience and self-compassion. Living a life with less stress and worry doesn’t happen overnight. It’s something we work at and practice, so it’s imperative that people be patient with the process and have self-compassion to help keep them going.
“We can do things to help address the stress, so it’s best to stay ahead of it,” said Jennifer Scherer, a registered dietitian nutritionist, medical exercise specialist, certified personal trainer, and owner of Fredericksburg Fitness Studio. “Now is the best time to make it a priority to address the stress in your life, which ends up impacting everything else.”
Financial stress is something that many people are familiar with, and according to a study published in the Journal of Family and Economic Issues, it leads to psychological distress. They report that a substantial number of U.S. families face financial strains, which negatively influences their finances, health behaviors and outcomes, and overall well-being. They report that it also plays a significant role in mental health.
Jeff Smith and his wife, Jennifer Scherer, have a podcast focusing on holistic wellness and financial planning for retirement. The Fitness & Finance Radio podcast offers a look at essential topics to know about keeping healthy and how it can impact their overall finances in retirement. The two bring passion and experience to the table.
The Fitness & Finance Radio podcast can be accessed on YouTube for free. •
1. National Institutes of Health. Stress. https://www.nccih. nih.gov/health/stress
2. Centers for Disease Control and Prevention. Managing Stress. https://www.cdc.gov/mental-health/living-with/ index.html
3. Journal of Family and Economic Issues. The Relationship Between Financial Worries and Psychological Distress Among U.S. Adults. February 2022. https://pmc.ncbi. nlm.nih.gov/articles/PMC8806009/





































































































































































































































































































































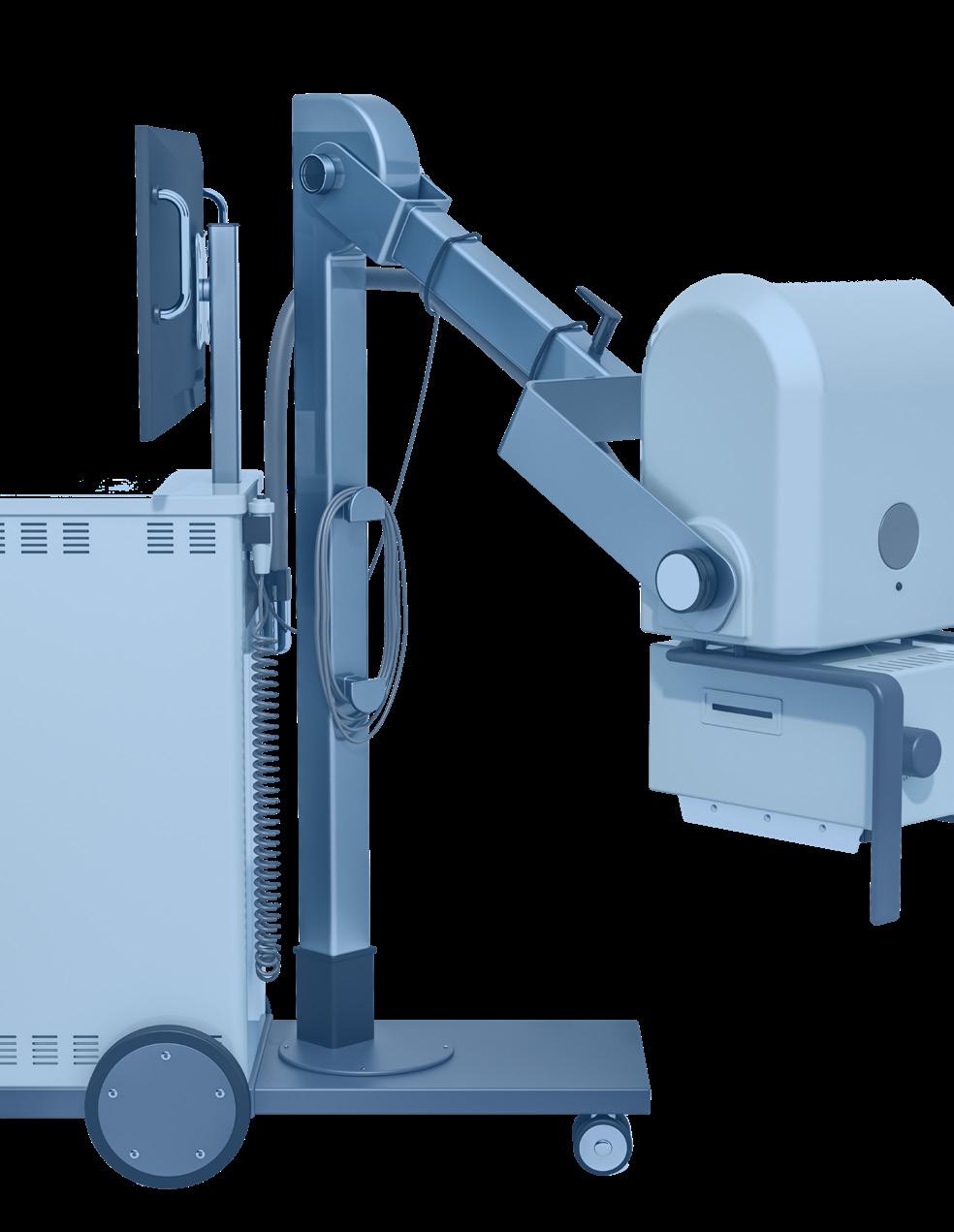


ACROSS
1 Problem for the imaging field due to skyrocketing demand for radiology services, 2 words
8 Type of MRI unit, 2 words
10 Emergency call for help
12 Stick to
13 Brought back to its original functioning condition
16 MR spectroscopy, abbr.
17 Abnormal growth in body tissue
19 Forearm bones
22 EEG, PET and MRI scans are often used to detect problems with this organ
23 Produced an image of an organ or area of the body
25 Latest technology affecting radiology and many other fields, abbr.
26 Safe medical imaging technique that’s now portable
29 Hospital care provider, abbr.
30 Groundbreaking system (for ultrasound) use in medical settings to aid in quick diagnosis and treatment at the patient’s bedside
31 ____tope
1 Devices used to destroy tissues as an alternative to conventional surgical removal
2 Taking tissue from a patient for diagnostic study
3 Aspect ____ in imaging
4 Premium cable network
5 _____-Sternberg cell- it reveals diseased tissue as Hodgkin lymphoma
6 The A in FAST
7 Made less difficult or painful
9 Unit of absorbed radiation, abbr.
“A person’s a person, no matter how small.”
– Dr. Seuss
11 Area used for surgeries, abbr.
14 Seldom seen
15 Belonging to us
16 Instruction books for radiology equipment
17 Software protocol enabling software applications to control and receive images from scanners
18 Odorless radioactive gas
20 West coast city, abbr.
21 Nickel symbol
22 Makes unclear or indistinct
24 Etiology, in relation to disease
27 Can material
28 Measure of image resolution, abbr.
29 Brazilian city
X-ray
Beekley
Beekley
Computed Tomography
Beekley
Beekley
Espin Medical www.espinmedical.com • (206) 755-1768
ImageOne Medical
image1group.com • 877-304-9000 49
KEI Medical Imaging Services keimedicalimaging.com • 512-477-1500 57
KEI Medical Imaging Services
keimedicalimaging.com • 512-477-1500 57
Metropolis International, LLC Metropolismedical.com • 718-371-6026
Metropolis International, LLC
Metropolismedical.com • 718-371-6026
PM Imaging Management pmimagingmgmt.com • 213-276-8209
PM Imaging Management pmimagingmgmt.com • 213-276-8209
Radon Medical radonmedicalimaging.com • 866-723-6698
Radon Medical radonmedicalimaging.com
843-767-8090
866-723-6698
RSTI rsti-training.com • 800-229-7784
843-767-8090
RSTI rsti-training.com
Breast Imaging
Beekley Medical beekley.com • 800-233-5539 63
Radon Medical radonmedicalimaging.com • 866-723-6698 45
RSTI
rsti-training.com • 800-229-7784 3, 56
C-Arm
Engineering Services
eng-services.com • 330-425-9279 2
Espin Medical
www.espinmedical.com • (206) 755-1768 17
Metropolis International, LLC
Metropolismedical.com • 718-371-6026 47
X-ray America, LLC
x-rayamerica.com • 854-999-6888 23
Cables
Engineering Services eng-services.com • 330-425-9279 2
Computed Tomography
Beekley Medical beekley.com • 800-233-5539 63
CM Parts Plus
cmpartsplus.com • 877-267-2784 58
Espin Medical
www.espinmedical.com • (206) 755-1768 17
FDM Enterprises fdmenterprises.com • 615-479-5572 53
ImageOne Medical image1group.com • 877-304-9000 49
KEI Medical Imaging Services keimedicalimaging.com • 512-477-1500 57
Metropolis International, LLC
Metropolismedical.com • 718-371-6026 47
PM Imaging Management pmimagingmgmt.com • 213-276-8209 57
Radon Medical radonmedicalimaging.com • 866-723-6698 45
Ray-Pac ray-pac.com • 843-767-8090 64
RSTI
rsti-training.com • 800-229-7784 3, 56
X-ray America, LLC
x-rayamerica.com • 854-999-6888 23
Contrast Imaging
Maull Biomedical
Brandywine Imaging


Register to view the webinars each month
Watch recorded webinars on-demand
3.EARN
ARRT Category A CE credits pending approval