


































MultiMedical Systems has been trusted for nearly 30 years for skilled BMET staffing – but we can also deliver:
• Cybersecurity solutions for medical devices
• Compliance and regulatory support
• Tailor-Made Field Service Staffing designed for your needs
From the frontlines of patient care to the backend of compliance, MultiMedical Systems delivers the expertise you need, exactly when you need it.
Finally, the features you love most about your favorite ride share app, food delivery app, Angi, UpWork, or TaskRabbit are available for medical imaging equipment maintenance and repair.
Enter a Trace Ticket with one tap to broadcast your repair needs to a network of qualified technicians.
Review Bids to find the best service option for improved repair outcomes with less equipment down time, resulting in a lower overall cost.
Track progress, issue payments and rate services all in a single dashboard.


Speed
Instantly blast your service request to every qualified and vetted service provider

From response times to uptime, you no longer have to rely on service companies to track their own activities and performance


Like your favorite personal apps, get in-app alerts when a service technician is on their way, arrived, waiting for a part, completed a job, etc.
Pay
Competitive bidding among service technicians allows you to get the best price and only pay and track one entity





P.12 SPOTLIGHT
p.12 Department of the Month: TRIMEDX Clinical Engineering at UPMC Children’s Hospital of Pittsburgh
p.14 Professional of the Month: Erika Colombe
p.16 Next Gen: Kyle Koscinski
p.18 Shifting Gears: Andrew Gutierrez, Cool Cars for the Boys
P.20 INDUSTRY UPDATES
p.20 News & Notes
p.26 TechNation Pulse
p.28 Welcome to TechNation
p.29 Ribbon Cutting: MedService Repair
p.30 AAMI Update
p.31 ECRI Update
P.32 THE BENCH
p.32 Biomed 101
p.36 Tools of the Trade
p.69 Webinar Wednesday
P.38 FEATURE ARTICLES
p.38 Roundtable: Education, Training and Apprenticeships
p.46 Cover Story: Why & How to Develop an HTM Strategic Plan: Align and Achieve

P.50 EXPERT ADVICE
p.50 Cybersecurity
p.52 The Future
p.54 Right to Repair
p.56 SPONSORED CONTENT: Renew Biomedical
p.58 The Massey Method
p.60 Networking Notes
p.62 Health-ISAC
PUBLISHER John M. Krieg
VICE PRESIDENT Kristin Leavoy
VICE PRESIDENT Jayme McKelvey BUSINESS DEVELOPMENT
EDITORIAL John Wallace
CONTRIBUTORS
K. Richard Douglas
Joie Marhefka
Steven J. Yelton
Garrett Seeley
Phil Englert
Nathan Proctor
Nadia ElKaissi
ACCOUNT Megan Cabot
EXECUTIVE
ART DEPARTMENT Karlee Gower
Taylor Hayes
Alicia Brown
DIGITAL SERVICES Cindy Galindo
Kennedy Krieg
Haley Harris
EVENTS Kristin Leavoy Sydney Krieg
WEBINARS Linda Hasluem
HTMJOBS.COM Sydney Krieg
ACCOUNTING Diane Costea
CIRCULATION Joanna Manjarrez

p.66 Biomed Brainbuster
p.67 Word Search
p.67 [Contest] What’s on Your Bench?
p.68 NESCE Scrapbook
p.72 Preferred Vendors
p.76 Service Index
p.79 Alphabetical Index
p.80 Time Capsule
Rob Bundick, Director HTM & Biomedical Engineering, ProHealth Care
Carol Davis-Smith, CCE, FACCE, AAMIF, Owner/ President of Carol Davis-Smith & Associates, LLC
Nadia ElKaissi, CHTM, Biomedical Engineer, HTM, VA Central Office (19HTM)
Bryant Hawkins Sr., Site Manager, Children’s Hospital of New Orleans
Earl Morris Jr., BMET, Director of Clinical Engineering, Harrison County Hospital
Leticia Reynolds, Clinical Engineering Operations Manager at UCHealth Parkview Medical Center


Our nationally recognized programs include Biomedical Equipment Technology (BMET), Biomedical Equipment Support Specialist (BESS), and the Dental Repair Technician (DRT) Certificate. Each is designed to equip you with the advanced skills needed to thrive in today’s evolving healthcare and dental technology landscape.



CBET’s Virtual Reality (VR) labs offer a flexible and immersive learning experience that adapts to your busy schedule. our VR labs allow you to practice and perfect your skills in a controlled, risk-free environment.








BY K. RICHARD DOUGLAS
The University of Pittsburgh Medical Center (UPMC) is a large nonprofit with approximately 100,000 employees and 40 affiliated hospitals. One of those hospitals is UPMC Children’s Hospital of Pittsburgh. It provides 1.5 million square feet of space to provide treatment of childhood conditions and diseases and accommodate the families of patients.
The state-of-the-art facility has won national recognition and includes a 10-story, 300,000-square foot research facility.
M anaging medical equipment for the Children’s Hospital is the TRIMEDX Clinical Engineering Department at UPMC Children’s Hospital of Pittsburgh. The department is comprised of 10 members. They include Site Manager Ross Scalise, Clinical Engineering Supervisor Alan Knupp, six
BMETs and two imaging technicians.
Knupp says that the group’s technicians have areas of specialty.
“ We have technicians who are specifically trained and assigned to various specialty areas within our department. These include anesthesia, ventilators, dialysis, EEG, imaging modalities and ECMO. Whenever possible, we also ensure there is a backup technician available to provide coverage and maintain continuity of expertise in each area,” he says.
Knupp says that the team supports a children’s hospital with 330 licensed beds, along with three main offsite facilities. These offsite locations vary in function but typically include office spaces, imaging services and, in some cases, operating rooms.
H e says that service contracts are managed through a thoughtful, data-driven process that typically takes place during budget planning.
“ The team reviews the previous years’ service history and associated costs to determine whether it makes
financial and operational sense to continue, modify or initiate new service contracts,” Knupp says.
The team also collaborates closely with its IT counterparts.
The TRIMEDX Clinical Engineering team took on a largescale project that benefited patients and clinicians.
“One of the most impactful special projects the team has taken on was the replacement of approximately 500 patient monitors across the hospital. This initiative required nearly a year of detailed planning, coordination and execution. The team was responsible for configuring each monitor with new IP and MAC addresses, integrating them into the hospital’s system, and managing live swaps in critical care units – often while patients were actively being treated. This meant working closely with clinical staff to ensure seamless transitions,” Knupp says.
H e adds that the project also introduced a new capability to allow real-time monitor viewing from any workstation, significantly enhancing clinical accessibility.
“ This project demanded collaboration across multiple hospital departments, IT, GE and hospital administration. It demonstrated the team’s ability to manage large-scale, high-impact technology upgrades without disrupting patient care,” Knupp adds.
In tackling the large patient monitor project, the group proved that they were up to meeting the many challenges that can be encountered with so many touchpoints and variables.
“ The patient monitor replacement project also serves
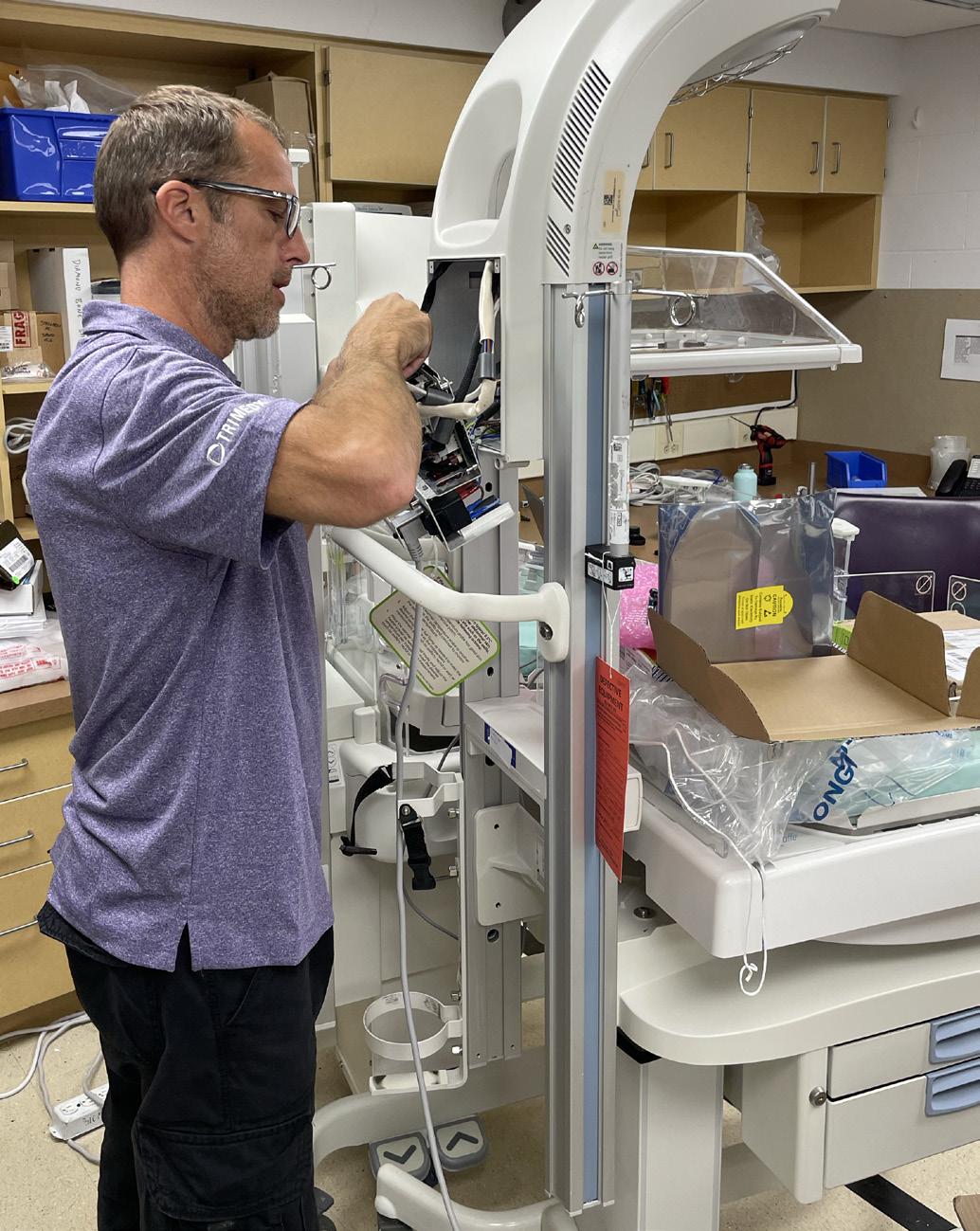
as a prime example of the department’s problem-solving capabilities. The team had to navigate a wide range of logistical and technical challenges, from coordinating live equipment swaps to customizing installations for different units. For instance, some ICUs required remote monitors outside patient rooms, which involved sourcing and installing specialized cabling, adapters and power supplies,” Knupp says.
H e adds that in operating rooms and cath labs, the team had to pre-plan for multiple displays and ensure that vital signs could be viewed from various locations within the room. All of this had to be done without interrupting patient care, requiring precise scheduling and strong communication with clinical staff.
“ The success of this project laid the groundwork for another major initiative: the replacement of approximately 2,500 infusion devices, including 770 syringe pumps,” Knupp says.
H e says that this project, which is currently underway, involves tagging, inventorying and coordinating floor-byfloor device swaps.
“ The team has applied lessons learned from the monitor project to streamline this rollout, once again demonstrating their ability to solve complex problems through collaboration, planning and a patient-centered approach,” Knupp adds.
The TRIMEDX Clinical Engineering Department at UPMC Children’s Hospital of Pittsburgh proves that a midsized specialized team can accomplish a lot. For the health of pediatric patients, that value cannot be overstated.

BY K. RICHARD DOUGLAS
Windsor, Ontario sits across the Detroit River from Detroit on the Canadian side. The city features a waterfront park that stretches three miles and is known as the “Automotive Capital of Canada.”
The city also has two campuses of St. Clair College. The college is known for it’s excellent biomedical engineering technology program. One of the program’s graduates is Erika Colombe, biomedical engineer technologist for TRH services in Cambridge, Ontario. Colombe works as a field service technologist with the company.
While Colombe’s interest in the biomed field began in high school, it was piqued while attending St. Clair.
“I learned and got into the HTM field through my professors at St. Clair College. These professors are James Linton and Jim Durocher. They introduced this to my class and encouraged us to integrate any management into any of our assignments with emphasis on our project management course,” she says.

Colombe says that the program she took was biomedical engineering technology, a three-year advanced diploma in Canada.
The biomed job opportunities are not that great in Windsor, but Colombe was prepared for that reality before entering the job market.
“I was pretty lucky to have professors that were pretty straight forward about this topic.
I would’ve never found a job in Windsor, my hometown. I had to move away. Currently, right now, the jobs in Ontario itself are very limited; most of them are located out of province but definitely not as bad as if in the U.S. I see jobs all the time for the U.S. as compared to Canada,” she says.
She says that working for an independent company, her training looked a little bit different.
“I had one-on-one training with the other technicians on job sites for about a month then I was on my own. Since then, I have helped develop a more standardized training program for my company. After that I have received a variety of manufacturing training on various equipment,” Colombe says.
Today, as a senior technologist, she offers support to new members of her team, including job preparations, what questions to ask, etcetera.
“I am not only working with management I directly report to, but management at the sites I work at. St. Clairs’ Project Management course encouraged us and taught us that every single person you work for/with is management and always a customer – whether it is a nurse, physiotherapist, dentist, etcetera,” Columbe says.
Since entering the field, Colombe has worked as a biomedical technologist, senior technologist and team trainer.
With a few years under her belt, the field-tested biomed is used to challenges and knows she is on the job to get the repair completed.
“One of the biggest challenges I have faced in itself comes from working for an independent company. When describing what we do, I call us a ‘fix it company.’ We fix everything. For our customers, we do not send anything back to the manufacturer unless it is our only option. With this, it means a lot of learning and troubleshooting,” Colombe says.
That often requires troubleshooting older equipment. She says that this means understanding the issue and repairing it on the first try.
“In addition, because we work on so much equipment, it has been a challenge simply learning it all. We work anywhere from surgical sites, dental offices, physiotherapy clinics, hospitals;
My favorite part of being a biomed is the challenge. As much as it drives me crazy, I love working on broken equipment and trying to figure out what is wrong with them. The reward when you figure it out is blissful.
basically, anything medical we work on. This went way beyond the scope I was taught in school and three years into my career, I am still learning,” Colombe says.
She says that on a more interpersonal level, time management is one of the hardest challenges and she tells every new member of her team that.
“If I am only given five hours on site to complete a job, I have to finish it and I am not leaving until it’s done. This is because of costs from our end as well as [the] customer’s end. Customers do not want to pay for us to come onsite another day if we don’t need to. They are given a time a frame and we are expected to complete it in that time frame. So, time management is an absolute key part of my job,” Colombe says.
Colombe describes herself as “just a young woman passionate about what she does.”
“I try my best to make light of everything; my job is tough. And it’s not only tough for me but for all the other techs as well. I want to keep the team in a good mood constantly and I try my best to do that – my boss would describe me as a ‘yapper’ when I’m around everyone,” Colombe says.
Family includes a twin sister who is a nurse.
“She’s two minutes older and never lets me forget. I also have an older brother who is a biomedical engineering technologist, although he followed in my footsteps,” Colombe says.
When not working, she enjoys painting, drawing and occasionally even playing video games.
“I was an avid soccer player for most of my life and even to this day, I still love the sport,” she says.
“I do have memberships with MedWrench and I also follow TechNation as a whole. Here in Ontario, I am working towards my OACETT, certified engineer technologist certifications,” she adds.
Biomed customers in Ontario can rest assured that when this biomed is on the job, the goal will be to get things fixed. A passion for the field can only mean good things.

FAVORITE BOOK:
I am currently reading a Court of Thornes and Roses series and loving it!
FAVORITE MOVIE:
I’m not much of a movie watcher but my favorite television show is “Vanderpump Rules.” I’m a sucker for good reality TV.
FAVORITE FOOD:
It’s cliché, but I could eat pizza every day. Specifically, pizza from Windsor, Ontario, my hometown; it’s what Windsor is known for.
HIDDEN TALENT:
I’m not sure yet but I did teach myself to play the guitar.
FAVORITE PART OF BEING A BIOMED?
My favorite part of being a biomed is the challenge. As much as it drives me crazy, I love working on broken equipment and trying to figure out what is wrong with them. The reward when you figure it out is blissful.
WHY DO YOU READ TECHNATION?
I read TechNation because there is so much to learn from everyone in all parts of society. I love reading about people who do the same job I do and see what their days look like compared to mine. I like to read about the new skills that people mention and how I can apply them to my everyday life.
Kaleida Health Imaging Specialist I Kyle Koscinski believes in continuing education. He holds associate and bachelor’s degrees in engineering as well as the following certifications: CBET, A+, Drager Apollo & M300 certification, Siemens Basic & Advanced Service Essentials, and Zoll R-series certification.
TechNation interviewed this New York native to find out more about his path to HTM and his goals for the future.
Q: WHERE DID YOU GROW UP?
A: Depew, NY (Buffalo Metropolitan Area)
Q: HOW DID YOU FIRST DISCOVER HTM?
A: Recommended field from a relative.
Q: WHY (OR HOW) DID YOU CHOOSE TO GET INTO THIS FIELD?
A: It was the first job field that responded to my application to work. After gaining experience, I decided to stay and invest in a future in the field. The main appeal at the time; healthcare was considered one of the more reliable jobs to have for life.
Q: WHAT DO YOU LIKE MOST ABOUT YOUR POSITION?
A: The complexity of the equipment being worked on makes it engaging; more fulfilling.
Q: WHAT INTERESTS YOU THE MOST ABOUT HTM?
A: The direction the field can go in 10, 20, and 50 years from now. How fast technology evolves; it’s exciting to think about what new equipment/techniques will be used and worked on in the future.
Q: WHAT HAS BEEN YOUR GREATEST ACCOMPLISHMENT IN YOUR FIELD THUS FAR?
A: Getting to the position I am in currently (imaging) after starting from the lowest entry position.
Q: WHAT GOALS DO YOU HAVE FOR YOURSELF IN THE NEXT 5 YEARS?
A: The main goal is expanding my knowledge in as many areas of imaging as I can through various means and OEM training.

FAVORITE HOBBY: Cooking
FAVORITE MEAL: Braised beef ribs with asparagus
WHAT WOULD YOUR SUPERPOWER BE? Getting somewhere quickly/teleporting
SOMETHING YOUR CO-WORKERS DON’T KNOW ABOUT YOU: I have an autoimmune disease.











K. RICHARD DOUGLAS
Turning a wrench is a lifestyle choice. It can mean many things, but it always involves hand or power tools, a knowledge of using tools and repair, maintenance or modification techniques and the foresight to complete a project.
Wrenching on a project car or on a medical device both mean that knowledge and tools collide in the hands of a skilled technician or mechanic. Something of value will result because of the effort.
In the world of car enthusiasts, there are projects meant to restore, modify, upgrade or enhance the vehicle. Whether the project is restoring a salvage car to pristine condition, increasing the horsepower of a daily driver or building a car for the track, there are skills, parts, tools and experience that all come into play.
Andrew Gutierrez, MBA, CBET, a clinical engineering technician in Stockton, California, understands the enthusiasm and wrenching skills needed to achieve a transformed and unique project vehicle. He also has the hands-on experience.
Gutierrez has been working recently on two project vehicles, a 1971 Chevelle and a 1951 Chevy classic truck. He has very specific future plans for the two project vehicles.
“My two vehicles are for my two boys, Andrew Jr., who is six and Nikolai, who is five. I have them help me do little things to get their problem-solving gears turning and ask questions,” he explains.
Since the boys will not be able to slide behind the steering wheels for at least nine years, are they excited about their future rides? What if they turn 16 and decide they want a Hellcat instead?
“My sons absolutely love the time we spend on these builds. For them, it’s not just about the car – it’s the bonding, the learning and the lessons about patience and hard work. Even if someday, they want a Hellcat, the
foundation we’ve built together won’t change. They’re learning that these projects are more than machines; they’re quality time and life lessons,” Gutierrez says.
He says that the old truck brings back some childhood memories.
“This truck was chosen because when I was little, my dad had an old one similar to that. I could see through the floorboards, and I remember cruising with him as a kid,” he says.
The Chevelle is a vehicle that Gutierrez wanted since he was young.
“This car was a dream project as a kid. I’ve always loved the aesthetic and performance of muscle cars, and I wanted to create something that embodies speed, power and nostalgia,” he says.
The two project vehicles have already received nicknames from their future owners.
Andrew Jr. named the Chevelle “oralleys” because Gutierrez would take him all the time to the store for parts. Niko named the 1951 Chevy truck “Bubba G.”
Gutierrez embraced the hobby of working on cars many years ago.
“I really got into cars when I was little. My dad worked with me in the garage, and those early moments of wrenching together really stuck with me. That foundation shaped everything that came later,” he says.
These two projects have not been Gutierrez’s first.
“My very first big project was an LS swap into a 1957 Chevy pickup, just like my dad had. That build was special because it connected me back to him,” he says.
Interestingly, it was not working on cars that led to the biomed profession for Gutierrez. It was the other way around; his ability to work on fabricating frames, working on engines and transmissions and brakes all came out of his healthcare career.
“Honestly, I credit my career in biomed for that. Working in healthcare technology management taught me how to diagnose, repair, and fabricate – just in a different setting. Those skills translated directly into cars,” he says.
The vehicles have had a chance to dazzle local car-lovers. Gutierrez says that he took the Chevelle out to participate in the Modesto, California Graffiti Night Parade. He says it was a highlight of owning the car so far.
The vintage pickup truck is a mix of restoration and customization.
“The plan is to maintain the exterior’s classic lines but upgrade the engine to Gen 3 LM7. The suspension is Mustang II in front and rear four-link and the interior is from Range Rover,” Gutierrez says.
With the addition of the more modern engines, Gutierrez used engine-mount kits as well as reinforcing the older frames, not designed for modern torque.
In addition to his ability to wrench and restore classic vehicles, Gutierrez also has created a biomed crossword puzzle book and sells biomed/HTM T-shirts.
HTM field and give professionals something fun, meaningful and stylish.
“Some proceeds from select designs support related causes – i.e., cancer charities when tied to oncology-related themes,” Gutierrez says.
He said inspiration for the design of a new T-shirt comes directly from his day-to-day experiences as a biomed.
“Every work order, every repair, every perspective I see in the hospital sparks ideas. And I think about how it would connect with all healthcare workers; not just biomeds. That’s how I build designs that really resonate,” Gutierrez adds.
His design themes include slogans such as: “Biomed: The Backbone of Healthcare,” “HTM: We Keep It Running So They Can Save Lives,” and “Built for Techs. Powered by Purpose.”
“Each piece is carefully themed – from maternity tech to ESUs, pumps and lab departments – to ensure it resonates with professionals in that area,” Gutierrez says.
While the T-shirts, biomed puzzle book and car projects are


Asahi Kasei has advanced its suite of critical care products through premarket approval by the U.S. Food and Drug Administration (FDA) for ZOLL’s Zenix monitor/ defibrillator. The Zenix device is the culmination of years of user feedback and is ZOLL’s most clinically advanced, user-friendly professional monitor/ defibrillator, according to a press release.
The Zenix monitor/defibrillator is designed for use in EMS and hospital settings. It features a large, durable touchscreen and functionality to automate workflows. Users can dynamically customize the device with real-time adjustments that make it easy to use in critical moments. The device also features ZOLL’s Real BVM Help and exclusive Real CPR Help technology.
“The approval of Zenix reflects our strategic, longterm focus on growth through high-value, solutionbased technologies. This device has been designed with an understanding of customer needs, and we expect it will be well-received by customers and healthcare professionals,” commented Ken Shinomiya, leader of the healthcare sector at Asahi Kasei. “This innovation expands our critical care portfolio and offers healthcare providers an excellent tool to tackle their key challenges. We will stay competitive and reinforce our commitment to long-term profitable growth through these innovations.”
The Zenix monitor/defibrillator is available in the U.S. and Canada.
Renovo Solutions has announced a strategic partnership with Surgical Solutions, a leader in on-site surgical support services. The collaboration is designed to help hospitals and health systems reduce costs, improve efficiency and strengthen outcomes for patients, staff and providers across the United States.
By bringing together Surgical Solutions’ ISO 9001-certified sterile processing and perioperative services with Renovo’s comprehensive HTM programs, biomedical and imaging expertise, and surgical equipment repair capabilities, this partnership creates a more integrated and effective approach to supporting operating rooms (ORs) and sterile processing departments (SPDs), a press release states. Renovo Solutions is ISO 13485 certified, underscoring its commitment to the highest quality management standards for medical devices, patient safety, and compliance.
“This partnership allows us to deliver even more value to our clients by uniting Renovo’s technology-driven HTM programs with Surgical Solutions’ deep expertise in the surgical ecosystem,” said Matt Forrest, vice president of business development at Renovo Solutions. “It’s about ensuring efficiency, compliance and cost savings – while improving care.”
The Hawaii Society for Healthcare Engineering has announced its 7th annual Hawaii Healthcare Technology & Facilities Engineering Expo. The 2026 Expo is set for Thursday, May 14 at Prince Waikiki. The all-day event begins at 7 a.m.
HISHE is a personal membership organization devoted to professionals who design, build, maintain, and operate hospitals and other healthcare facilities. HISHE members include healthcare facility managers, engineers, architects, designers, constructors and others.
HISHE’s objective is to encourage and assist the membership in the development of their professional knowledge and competence in the field of healthcare engineering through pertinent educational seminars,

Through this partnership, Renovo clients will have access to expanded support including enhanced staffing, sterile processing services and procedural expertise. Together, the two companies will help hospitals and health systems:
• Prevent case delays and streamline OR workflows to ensure on-time starts
• Enhance compliance and readiness for Joint Commission and DNV surveys
• Reduce infection risks through improved instrument reprocessing
• Keep equipment reliable and eliminate costly downtime
• Address staffing gaps with CRCST-certified SPD and OR support staff
• Ease financial pressure with cost-efficient, guaranteed savings solutions
“This collaboration represents a powerful opportunity to solve some of the toughest challenges hospitals face today,” said Ben Schraeder, senior vice president of strategy at Surgical Solutions. “By combining our strengths, we are able to support both the clinical and technical sides of the OR and SPD, ultimately improving efficiency, compliance and patient outcomes.”

conferences and to provide a medium for the exchange of personal experience as well as the distribution of relevant reference documents and codes relative to the facilities management field.
Early bird registration at a reduced rate is available through April 10 at HISHEHawaii.org.
Sponsorships remain available. For information about how to support the organization via a sponsorship contact Jessica Onaga at 808-783-6594 or via email at jessica.onaga@palimomi.org.
The HISHE’s 8th annual golf tournament will be held Friday, May 15 at Kapolei Golf Course. For details about the golf tournament visit, hishehawaii.org/ event-6360582.

AdvaMed has submitted formal comments responding to the U.S. Department of Commerce investigation into whether the U.S.’s current level of medtech imports has national security implications. The comments outlined medtech as an American success story and the United States as the global leader in innovating and making the highest quality medtech for the United States and world, an export powerhouse, and much less reliant on medtech imports than sometimes perceived.
“We look forward to working with the Administration to recognize and to reward the unique strength of the U.S. medtech industry and to pursue targeted, America First policies that further bolster our domestic base and export platform,” Scott Whitaker, AdvaMed president and CEO, wrote. “These policies include seeking fair and reciprocal tariff-free trade with our most important allies, aggressively addressing unfair market access barriers in specific countries, and advancing domestic regulatory reforms and procurement incentives to enhance U.S. competitiveness at home and abroad. Appropriately tailored policies can ensure that this critical American industry continues to thrive, innovate, protect and strengthen the economic and healthcare systems of our great nation.”
The extensive comments, submitted by AdvaMed on behalf of its more than 600 member companies, describes the flourishing U.S. medtech industry: Supporting three million well-paying jobs, U.S. medtech manufacturing jobs having grown three times faster than overall U.S.
manufacturing jobs; 70 percent of the medtech sold in the United States is made here, as demonstrated by U.S. Census data on U.S. manufacturing output; by far, the United States is the world leader in medtech exports, enjoying trade surpluses with virtually all trade partners, especially those with large economies.
Tax relief and other pro-growth policies enacted under both Trump administrations have contributed to significant medtech investments in the United States, with billions of dollars in new investments announced this year alone.
The comments outline a series of recommended policies to further support U.S. dominance in medtech production, innovation, exports, and the source of jobs and investment in every state. The response also describes the extensive value of U.S.-dominated medtech to patients, doctors, and hospitals, providing safe, effective medtech for every medical condition at costs that are consistently low relative to other health care spending and often deflationary because of industry competition.
“The American medtech industry is the backbone of our country’s health care system,” Whitaker said.
Through the Commerce Department investigation and tariff deliberations, AdvaMed urges the Administration to consider how lower tariffs combined with supportive policies will promote more medtech manufacturing and job growth in the United States, which means greater access to lifesaving technologies and lower costs to American hospitals and patients and more investment in the United States.
D’Juan James, MBA, CHTM, senior director of clinical engineering for Kaleida Health, recently received Kaleida Health’s Leadership and Influence Award for his ability to influence others, inspire a collective commitment to organizational goals and serve as a role model in promoting the organization’s values.
As voted on by Kaleida Health Employee Resource Groups (ERGs), the Leadership and Influence Award highlights employees’ meaningful impact, visionary leadership, innovative practices, trusted support, cross-functional collaboration and continuous personal and professional growth.

WILLIAMSBURG, Va. | Navy Medicine commands and partners responded to an urgent requirement request from U.S. Naval Hospital, Guantanamo Bay, Cuba, Sept. 19, delivering critical surgical equipment and expertise that bolstered medical readiness across the Fleet and Joint Force.
When GTMO reported a shortage of sterilization equipment and trained personnel, Naval Medical Readiness Logistics Command (NMRLC), Naval Medical Forces Atlantic, Naval Medical Center Portsmouth, Naval Hospital Jacksonville, Defense Health Headquarters, U.S. Naval Hospital Guantanamo Bay, and Defense Logistics Agency, coordinated under a tight 48-hour timeline.
The mission required locating and preparing
Automated Field Steam Sterilizers and Ultrasonic Portable Washers without drawing down prepositioned war reserve materiel already set aside for other operational commitments. Once the equipment was identified, biomedical technicians at NMRLC conducted immediate maintenance and calibration to ensure the systems were fully mission ready.
“An automated field steam sterilizer is a device used to kill or remove all forms of microbial life, including bacteria, viruses, fungi, and spores, to render objects or surfaces completely free of viable microorganisms,” said Jerhmain Jordan, NMRLC’s electronic technician (biomedical) supervisor.
“Sterilization is the highest level of microbial killing, going beyond simply cleaning or disinfecting.”
An ultrasonic portable washer is a military biomedical portable ultrasonic cleaner used for sterilizing surgical instruments and other medical equipment in field hospitals and other austere combat environments.

Transporting the gear posed additional challenges since commercial carriers do not service GTMO. The team secured military airlift, ensuring delivery by the deadline. When one sterilizer malfunctioned after arrival, technicians at NMRLC provided remote troubleshooting to restore full capability within 24 hours.
This rapid, coordinated response ensured GTMO remained fully equipped to deliver surgical care in support of deployed Sailors, Marines, and joint partners. The effort demonstrated Navy Medicine’s ability to move quickly, solve complex logistics challenges and sustain readiness in austere environments.
“This was a perfect example of multiple commands coming together to maintain mission capability,” said Capt. Jared McKendall, chief of staff, Defense Health Network Atlantic. “The teamwork ensured uninterrupted support for
the Fleet and our operational mission overseas.”
Naval Medical Readiness Logistics Command (NMRLC), headquartered in Williamsburg, Va., provides centralized program management and logistics support to ensure Navy Medicine is manned, trained and equipped to support the operational forces. NMRLC delivers expeditionary medical systems, optical fabrication, medical logistics and materiel readiness to sustain Sailors and Marines worldwide. The command plays a vital role in supporting the Navy Surgeon General’s priority of medical force readiness and the Navy’s overall warfighting mission.
Navy Medicine – represented by more than 44,000 highly trained military and civilian healthcare professionals – provides enduring expeditionary medical support to the warfighter on, below, and above the sea, and ashore.









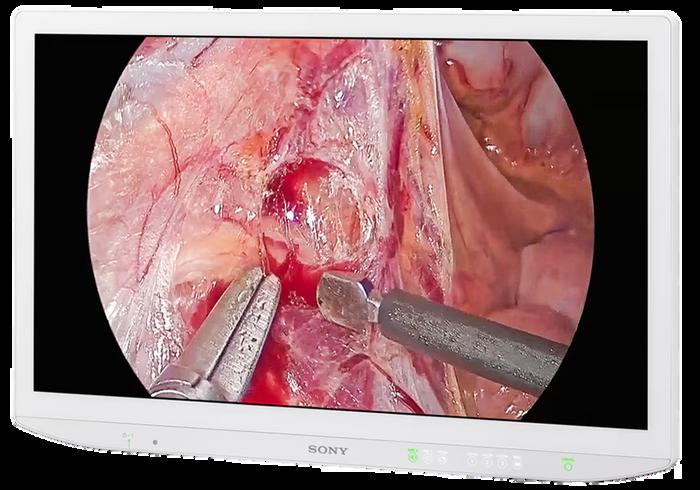
Registration is now open for the 2026 Imaging Conference & Expo (ICE) scheduled for February 20-22 in San Antonio, Texas! Registration is FREE for hospital and imaging center employees as well as active military and students.
ICE is the only conference dedicated to imaging directors, radiology administrators and imaging engineers from hospital imaging departments, freestanding imaging centers and group practices. The conference also delivers valuable CE credits from the ASRT and ACI (pending approval).
This is the imaging conference where all imaging professionals come together for conversations regarding capital projects, imaging practices, service solutions and more.
ICE 2026, like previous years, offers invaluable continuing education, productive networking and an exclusive exhibit hall. Attendees will have the perfect opportunity to enhance their careers and spend time with colleagues. It is the perfect resource to grow and prosper, personally and professionally. Previous attendees and exhibitors have applauded ICE conferences and expect to return.
“I had many takeaways from the conference. The leadership summit was a great platform to share current challenges in healthcare. To me this was a new topic that I have never experienced before at an imaging conference,” Taylor/Chaplin Breast Health Center Associate Director Kathryn Fields ARRT, ARDMS, MBA, said. “It was great to connect prior to the Summit and meet the participants, and then later have an
MD Expo Baltimore invites HTM professionals and thought leaders to submit presentations for the April 2026 conference. MD Expo provides healthcare technology management professionals with a unique and rewarding conference. Clinical engineers, biomedical technicians, directors, managers, procurement/asset managers and others responsible for medical devices and technology will gather in a one-of-a-kind environment to network with peers and learn the latest technologies and advances in HTM.
Benefits of presenting at MD Expo include sharing knowledge and experience with current and future leaders.

open discussion on topics of our choice that are currently affecting us in our work and health care system. It’s always great to see what other facilities are doing and how they handle certain challenges.”
“Overall, it was a great discussion and when I came back to work, I felt motivated and refreshed with new ideas to implement and try out with my team because of the discussion,” she added.
Daniel Adams from Renovo praised ICE after attending in a previous year.
“My favorite part is the general structure of the event. I like the fact that technicians, service managers and clinical managers can share an event and trade stories of their concerns,” Adams said. “I think it helps service people understand what is important to clinicians as well as giving insight to clinicians regarding service challenges/issues.”
MR Imaging Manager Annette Long, R.T.(R), MR, MRSO, from the Ohio State University Wexner Medical Center always enjoys the conference.
“The ICE conference is a fantastic event to attend, offering excellent lectures and highly relevant material,” she said. “While it is a smaller conference, great attention to detail is given to ensuring a top-notch experience, from perfectly curated catering to enjoyable and engaging happy hours.”
Check out the schedule and register today at AttendICE.com.
Speakers are recognized as leaders in the HTM community who take time to enhance the professional development of others. Presenters may also add speaking engagements to their list of achievements on LinkedIn and their resume.
Presenters also benefit from networking with HTM colleagues from across the nation and gaining awareness of available resources.
For more information, visit mdexposhow.com/call-for-presenters.
HTM professionals are encouraged to vote for the 2026 Tech Choice Awards! Five finalists for each of the 14 categories were determined by nominations. Voting is open until January 9, 2026. The 14 award categories are:
• Association of the Year sponsored by MMS
• ISO Professional of the Year sponsored by MedWrench
• Director/Manager of the Year sponsored by MW Imaging
• Professional of the Year sponsored by Innovative Radiology
• Young Professional of the Year sponsored by Prescott’s
• Military BMET of the Year sponsored by College of Biomedical Equipment Technology (CBET)
• Outstanding Vendor of the Year
• Industry Influencer of the Year sponsored by SOMA Tech Intl
• Icon Award sponsored by Renovo Solutions
• Women in Leadership Award sponsored by Avante Health Solutions
• Humanitarian of the Year Award sponsored by Pronk Technologies
• Educator of the Year sponsored by Maull Biomedical
• Large Department of the Year sponsored by USOC BioMedical Services
• Small/Midsize Department of the Year sponsored by USOC BioMedical Services
The Tech Choice Awards (also known as the Wrenchies) are the people’s choice award for the HTM community. The winners are based 100 percent on the number of votes each finalist receives during the voting period. A special thank you goes out to the sponsors who help make the Tech Choice Awards possible. The sponsors do not have any input when it comes to selecting winners.
Wrenchie winners will be announced in an upcoming issue of TechNation with an award ceremony planned for the MD Expo Baltimore in April 2026.
Visit 1technation.com/techchoiceawards to vote for your favorites.
Enter the contest and help TechNation celebrate. Fill out the short form at 1technation.com/contest for a chance to win one of 12 prizes, each valued at $150 or more!
Additional entries to win can be acquired by sharing on LinkedIn or submitting a photo. Each month, a winner will be selected and featured in TechNation magazine! October winner is Corey Weeden.
Find out more information on Page 80.









Q: WHAT PRODUCT, SERVICE OR SOLUTIONS DOES YOUR COMPANY PROVIDE TO THE INDUSTRY?
Rytex Industries is your trusted source for replacement parts for X-ray, CT, MRI, Cath Lab, and RF systems. We proudly support trusted brands including GE, Philips, Siemens, Toshiba, Carestream, Del Medical, Canon, and Shimadzu.
With over 20,000+ OEM imaging parts in stock, we supply boards, DR panels, X-ray tubes, CT tubes, collimators, transformers, MRI coils, and more, all backed by a 90-day warranty and worldwide shipping.
In addition to our extensive parts inventory, Rytex offers complete installation and de-installation services for imaging systems and now provides X-ray equipment rentals, giving facilities flexible options to stay up and running without interruption.
Our mission is to keep imaging departments operating efficiently through dependable parts, expert support, and professional service, every time.
Q: TELL US WHAT DIFFERENTIATES YOUR COMPANY FROM THE COMPETITION?
What sets Rytex Industries apart is our commitment to reliability, transparency, and personal service. We’re not just a parts provider, we’re a partner to our customers.
Our team understands the urgency of medical imaging service needs, so we maintain a large in-stock inventory for same-day shipping and back every sale with a 90-day warranty.
At Rytex, we take a hands-on approach, offering tech support, testing all of our parts before shipment and responsive communication. Every order (large or small) receives the same level of care and attention that has built long-term trust with our clients across the U.S. and around the world.
Q: WHY DID YOU CHOOSE TECHNATION FOR ADVERTISING?
We chose TechNation because it connects us directly with the professionals we serve; biomedical engineers, imaging specialists, and healthcare technology management (HTM) leaders who rely on trusted partners to keep their systems performing at their best. TechNation’s readership reflects the same values we hold at Rytex: integrity, quality, and collaboration. Advertising through this platform helps us share our message with a community that values dependable service, proven solutions, and lasting relationships.
For more information, visit rytexindustries.com


or 30 years, MedService Repair has been a trusted and independent service partner to endoscopy practices across North America. TechNation recently interviewed MedService Repair President Michael Goy to find out more about the company.
Goy: MedService Repair offers full-service repair and maintenance capabilities, parts and PM kits, and certified refurbished Medivators’ reprocessors. We also provide service and support for acquiring a broad range of necessary equipment and consumables including Scope Buddy flushing pumps, leak testers, flexible and rigid endoscopes, power tools, light sources, pigtails, filters and more. If it is used in endoscopy, we have a solution!
We are very excited about our enhanced ability to provide preventative maintenance kits used by biomedical engineers across the U.S.! When we started selling kits and break/fix parts, our customers asked us about enhanced training for their teams. We listened and developed two unique programs under the umbrella of MedService Repair University.
• Biomed training: At our corporate location, we have a program to provide hands-on training to certify biomedical engineers to perform preventative maintenance service and troubleshoot and address break/fix service needs on all Medivators Reprocessor models.
• Clinical training: At a customer location, a MedService repair clinical trainer will work with facility personnel to review scope handling procedures and offer an unbiased review of processes to enhance patient safety.
Goy: Facilities choose MedService Repair for our commitment to exceptional customer service and unmatched expertise in providing service and support on Medivators reprocessors. MedService Repair is led by multiple award-winning, Medivators-trained field service engineers who drive successful service outcomes and a team of account managers who anticipate customer needs and provide consultative solutions to support facilities. The quality of scope
reprocessing and handling practices leads directly to the quality of patient outcomes. Good health for your patients.
In addition to providing all of the above, we also offer significant cost savings compared to working with the OEMs. It is our goal to use our knowledge and experience to provide customers with the right advice in choosing the highest quality and most economical products. We believe in long-term relationships and will never pressure a customer to purchase new equipment when current equipment is operational and meets the needs of their practice. Good health for your practice.
Goy: MedService Repair is very excited to offer two enhanced enzymatic detergents to customers! Endocept and Medizyme represent the future of data driven enzymatic detergents for precleaning endoscopes prior to reprocessing. Our new products are developed for endoscopy while also being more cost efficient compared to current products in the marketplace. We offer free trials of these enzymatics to show customers the value in their own facility! We have another new product line launching in the start of 2026. This will be a very powerful solution to our market! More info to come …
Goy: When you work with MedService Repair, you can expect to receive exceptional service that meets the highest industry standards, using parts sourced exclusively from OEM-caliber providers – delivering top-quality performance at a fraction of the cost. MedService Repair is focused on providing the service a facility needs at the highest level possible. We are focused on being a partner to your facility and keeping your current equipment running at OEM specifications. Our focus is not on selling you replacement equipment that you do not need.
We are focused on listening to customers to design service programs that best meet their needs. The secret sauce is our ability to support a customer. The extra benefit is that they save significant spend working with us compared to the OEM. We are committed to our core values: Good health for your patients. Good health for your practice.

Dental equipment is healthcare equipment, but until now, the professionals who repair these devices are often unaware of the resources and support available to the healthcare technology management (HTM) field. Taking a crucial step to change this, the Association for the Advancement of Medical Instrumentation (AAMI) is bringing the popular “Dental Fix Summit” to the annual AAMI eXchange HTM conference.
“For a long time, dental equipment repair technicians have operated in a silo, similar to how our healthcare model has mentally separated dental care from medical care. UptimeHealth and AAMI wanted to change this narrative,” announced Jinesh Patel, CEO and co-founder of UptimeHealth after meeting with AAMI CEO Pamela Arora and AAMI HTM leadership.
UptimeHealth, a software and services company for outpatient healthcare, has built a strong presence in dental equipment management through its annual Dental Fix Summit. In a bid to bring that resource to the wider HTM community, AAMI has acquired the annual summit, with plans to make it a key feature of the association’s next annual HTM conference in Denver
Colorado, May 29 to June 1, 2026.
“We say dental care is part of healthcare. That means dental equipment is part of HTM,” added Danielle McGeary, vice president of HTM, AAMI. “Much like with hospitalbased HTM, dental instrument servicing is having pipeline issues, but the situation is made worse because folks aren’t as aware of the field or its challenges. By welcoming this community, we’re raising awareness, broadening personnel pipelines, and helping to ensure patients everywhere benefit from safe and effectively serviced devices.”
AAMI’s initial five-year plan for the acquisition includes continued collaboration between AAMI and UptimeHealth, with the co-creation of a dental pavilion on the expansive AAMI eXchange expo hall floor. There, HTM professionals will be able to meet with dental equipment vendors and specialized service providers. The pavilion, sponsored by UptimeHealth, will host 30 vendors and service providers supporting the dental industry.
Additionally, the 2026 eXchange will host hands-on demonstrations and educational presentations intended for dental equipment technicians. A plan to create a dental track of educational sessions at future eXchange conferences is in progress. According to AAMI, the track will see overlap into the conference’s popular sterilization track for device reprocessing – another significant area of interest for dental device service technicians.
“This is going to be a natural, wonderful synergy,” said Patel. “We’ll bring dental vendors and service technicians right to the center of the expo floor, making them feel included in the HTM world.”


The FDA’s Center for Devices and Radiological Health announced a pilot program last year called the Communications Pilot to Enhance the Medical Device Recall Program, designed to shorten the delay between FDA’s initial awareness of a potentially high-risk medical device issue and public communication to health care providers, patients and the public.
The “Early Alert” is distinct from a formal recall announcement. The FDA can issue an early alert when they deem the risk to be significant, even if they haven’t yet completed the full evaluation or determined if the issue warrants a recall.
Initially, the pilot was limited to devices in five categories (cardiovascular, gastrorenal, general hospital, obstetrics & gynecology, and urology) but on September 29, 2025, FDA announced the program has expanded to cover all medical devices for potentially high-risk removals or corrections.
“ECRI strongly supports the FDA Early Alert Pilot Program as an important step toward improving responsiveness and speed in our nation’s medical device safety infrastructure. It’s good for the industry and good for patient safety,” said Scott Lucas, vice president of device safety at ECRI. “By sharing alerts faster, the FDA can better equip healthcare professionals and patients to make informed decisions faster, helping to prevent harm and support timely corrective action.”
“At ECRI, we have long advocated for the need to improve the timeliness of communication surrounding unsafe medical devices. The problematic gaps in our nation’s recall process for at-home medical devices made the #1 spot in our annual research report in 2023, the Top Ten Health Technology Hazards,” Lucas added. “We commend the FDA for its commitment to continuous improvement. Initiatives like this strengthen public trust and demonstrate how clear, rapid communication can protect patients.”
“The quicker that FDA and manufacturers can notify healthcare providers of safety issues, we’re fully supportive of that,” agreed Tom Toczylowski, associate director of ECRI Alerts. “We’ve engaged with the FDA on this topic numerous times over the last several years, including before they launched this pilot program. The program’s expansion is a positive step forward.”
Now, when a device manufacturer initiates corrective actions for a potentially serious issue, the FDA may issue an Early Alert even before confirming whether a full recall is required. The FDA still retains its usual recall processes, but Early Alerts are an additional layer of more proactive communication that’s faster than the FDA’s previous process.
ECRI publishes exclusive hazard alerts which sound the alarm about potential threats in devices and pharmaceuticals long before they turn into potential recalls. ECRI remains the fastest and most comprehensive source for coverage of medical device safety issues, often sharing hazard alerts weeks or months before the FDA. Learn more about ECRI.org.

BY BOYD S. CAMPBELL CBET, CRES, CHTM
s biomedical professionals, we often work behind the scenes – ensuring equipment is safe, calibrated, and reliable before it ever reaches a patient. It’s easy to think of what we do as purely technical work, but every now and then, something happens that reminds us of the human side of our profession.
While in biomedical school, there was one lesson that always stood out: “Never walk away from a device unless you would be comfortable having it used on a loved one.”
That principle really hit home for me about a month ago. My fiancée was diagnosed with a rare form of breast cancer that accounts for only about 1% of all breast cancer cases. It was discovered in one of the most unlikely places – the dermatologist’s office.
Fortunately, the dermatologist had seen one similar case before in his career and immediately performed a biopsy. Unfortunately, the results came back positive for Paget’s Disease of the breast.
As our journey continued, the next stop was the surgeon’s office to prepare for surgery – only the third such case he had ever treated. The surgery went well, requiring a partial mastectomy. From there, we visited the oncologist and then the radiation oncologist. It’s a path many others have walked before, but for me, the biomed side of my brain couldn’t help but pay attention to something else along the way.
At every stop, I found myself checking the inspection stickers on the medical equipment being used. At the dermatologist’s office – where the biopsy was performed – the equipment had been inspected by Southeastern Biomedical. At the surgeon’s office, the same. The oncologist’s office? Once again, Southeastern Biomedical.
But the story doesn’t end there. As my fiancée continues her journey, she is now preparing for radiation
therapy. Knowing the facility where she will receive treatment, I have the utmost confidence in the care she will get. Why? Because I know that the devices the radiation physicist will use are of the highest quality. How do I know this? I’ve supplied that facility with Fluke Biomedical and Raysafe products for many years. And there’s one more reason for my confidence — Southeastern Biomedical provides the on-site calibration services for all their biomedical test equipment.
As a biomedical technician and co-owner of Southeastern Biomedical, that realization struck me deeply. What we were taught in school wasn’t just a professional standard or a safety protocol – it was a life lesson. It reminded me that the work we do every day truly touches people’s lives, sometimes in the most personal way imaginable.
Every inspection, every calibration, and every record we document represents a promise – that someone’s loved one can trust the device being used to diagnose or treat them. That’s why we can never forget that early lesson: “Never walk away from a device unless you’d want it used on someone you love.”

Boyd Campbell, CBET, CRES, CHTM is the co-owner of Southeastern Biomedical Association.
TechNation’s recent Webinar Wednesday presentation “Bridging the Gaps in Healthcare Operations: How Digital Procurement Drives Standardization, Savings & Uptime” was popular among HTM professionals. Sponsored by PartsSource, the webinar is eligible for 1 CE credit from the ACI.
In today’s complex healthcare environment, health systems are under increasing pressure to reduce costs, maintain equipment uptime, and overcome staffing shortages – all while advancing digital transformation goals. Yet many organizations still rely on outdated, manual processes to manage critical parts and service procurement.
In the webinar, PartsSource Chief Commercial Officer Jeff Evans shared how leading health systems are modernizing their operations by leveraging data-driven, tech-enabled solutions that deliver immediate ROI, drive standardization and unlock clinical capacity.
Evans discussed how automation and digital procurement platforms are transforming healthcare technology management and supply chain workflows. He shared the operational impact of shifting from transactional sourcing to strategic vendor management. He also discussed ways to reduce clinical equipment downtime through predictive analytics and network optimization. In addition, Evans talked about how to identify and eliminate hidden cost variability across a system.
Attendees were also able to ask questions during the session.
Martin O’Brien, a biomedical technician instructor with RTS Medical in Wisconsin won a Swiss Force Meister Multi-Tool during the webinar.
Attendees shared feedback via a post-webinar survey that included the question, “What does Webinar Wednesday provide the industry?”
“Insight into what is trending,” said Chad Rivers, BMET II, Children’s Health.
“Webinar Wednesday provides free, high-quality educational sessions that help healthcare professionals stay informed about innovations, best practices and operational strategies in the industry,” said Hia Al Saleh, a biomedical engineer with St. Clair College.
“An opportunity to gain insight and knowledge of current industry status, changes and the future of HTM,” Franciscan Health East BMET III Brian Snyder, CBET, said.
Watch these webinars on-demand
TechNation’s Webinar Wednesday series featured “Reactive Mode to Leader Mode” by Eric Massey on October 1. The webinar, which is available for on-demand viewing at WebinarWednesday.live, is eligible for 1 credit from the ACI.
This webinar shared the ongoing shift from Reactive Mode – a state of constant firefighting and reactivity – to Leader Mode – where leaders intentionally focus on high-impact priorities.
Participants were able to join Massey as he explored the Core Day framework and the 60/40 Rule as practical tools for structuring time and energy more effectively. Through guided reflection and a practical exercise, attendees were able to identify one leadership habit to implement immediately and receive a sample Core Day planner page to reinforce learning.
Massey delivered several takeaways for attendees including how to:
• Identify where you’re stuck in Reactive Mode and discover why it keeps even the best leaders from performing at their peak.
• Learn the Core Day Framework – a proven structure to protect your time, focus and energy for what truly matters.
• Experience the 60/40 Rule in action and see how elite leaders prioritize their day for maximum impact.
• Create one immediate leadership shift by replacing a reactive habit with an intentional one.
Massey also emphasized the message, “Your job should support your life, not be your life.”
This was a popular webinar with 83 tuned in for the live presentation. The on-demand recording has been accessed by several people. A video link to watch the webinar is 1technation. com/reactive-mode-to-leader-mode-massey/
Gerald McNeil, a BMET III, GE HealthCare in Maine won a Swiss Force Meister Multi-Tool during the session. McNeil and other attendees provided insightful feedback regarding the webinar via a survey that included the question: “What does Webinar Wednesday provide the industry?”
“Continued growth and educational opportunities especially when training dollars are scarce,” said Paul Neher, a supervisor of biomedical service at Parkview Health.
“An excellent way to get CE credits and useful information,” said Dan Harper, CE manager, with Intermountain Health-St. Mary’s Regional Hospital.
“A variety of topics that are pertinent to the biomed world,” said David Taylor, a Senior BMET III with Baylor Scott & White.
“Practical tools/helps for the HTM community,” said David Banister with Clinical Engineering Services.
“Learning and professional development opportunities,” said Samantha Edmonds, an imaging service engineer with Intelas.
The recent Webinar Wednesday Tools of the Trade presentation “Downtime Trace+SkillNet: The Future of HTM Workforce Readiness” explored a new frontier in healthcare technology management (HTM). The trio of presenters shared a new high-tech way for HTM professionals to add gig work and track their skills and capabilities.
SkillNet Founder and CEO Mike Kritzman provided detailed insights regarding the SkillNet app and how its many features provide a quick and easy avenue to record repair work, education, training and more.
Downtime Trace Chief Products Officer and Co-Founder Jason Mobley along with advisor Dave Francoeur discussed how the Downtime Trace app delivers an on-demand marketplace that connects hospitals with skilled technicians in moments of urgent downtime. Health systems can immediately locate skilled professionals to keep equipment online without patient care being interrupted.
Together, Downtime Trace and SkillNet solve one of the industry’s biggest challenges: matching the right talent to the right need, at the right time.
SkillNet provides the Downtime Trace marketplace with accurate, validated and standardized transcripts that capture a service technician’s training, certifications and on-the-job experience in one portable record. By creating a common language of skills, SkillNet ensures hospitals know exactly what work each technician is capable of performing.
The combined value includes:
• Speed: Hospitals engage qualified service companies and technicians within minutes
• Trust: Skills are transparent, validated and consistent across the industry
• Efficiency: Less time spent on paperwork, more time solving other downtime challenges
• Opportunity: Professionals gain visibility and recognition for their expertise
The presenters also fielded questions during the webinar.
The webinar is eligible for 1 CE credit from the ACI and a recording of the presentation is available for on-demand viewing at WebinarWednesday.live. HTM professionals everywhere can join the 42 attendees present for the live webinar in expanding their knowledge while also earning CE credit.
Michael Lucas, an imaging biomedical technician with Columbus Regional Health in Indiana, won a Swiss Force Meister Multi-Tool during the webinar. He and others participated in a post-webinar survey that included the question, “What was your single biggest takeaway from today’s product demo?”
“Using tools to track time,” said Dat Ha, a biomedical technician with Children’s Health.
“Just seeing how technology is evolving in our field,” said Todd Walker, a biomed with Oregon Health & Science University.
“No more spreadsheets to track techs’ abilities and training,” said Casey Celver, a biomed with Legacy Emanuel.
“Importance of training tracking,” said Joseph Manning, BESS, ICVAHCS.


DEMO: DECEMBER 10 at 2PM ET
Registration on WebinarWebnesday.live
Eligible for 1 CE credit from the ACI.

This educational webinar highlights the importance of training and certifying biomedical engineers to serve as Medical Laser Safety Officers (MLSO) in a healthcare facility. Biomedical engineers should be Laser Safety Officers (LSOs) because their technical expertise with medical devices, understanding of safety protocols and familiarity with equipment maintenance and calibration make them ideal for managing complex laser systems and ensuring patient, staff and public safety in healthcare environments. Their technical background directly aligns with the need for precise risk assessment, implementation of control measures and adherence to strict ANSI standards.
The course objectives include the duties of the MLSO, a specially trained professional responsible for ensuring the safe use of lasers in medical settings such as hospitals, surgical centers, vision clinics and dermatology offices. This webinar will review the MLSO role as defined and guided by ANSI Z136.3, the American National Standards Institute (ANSI) standard for the Safe Use of Lasers in Healthcare. In addition, the webinar will discuss the benefits of having biomedical engineers assume this regulatory role within the facility-based laser program.
For more information, visit medicallasersafety.com









TechNation invited HTM experts to participate in this roundtable article focused on education, training, and apprenticeships in order to share their opinions with readers. The goal is to highlight challenges, successes and insights related to workforce development – how technicians are trained, how programs are evolving, and what the future holds for education in this vital profession.
Participants in the 2025 Roundtable article on education, training, and apprenticeships are:
• BC Group International Director of Business Development Justin Barbour;
• College of Biomedical Equipment Technology President Richard L. “Monty” Gonzales;
• Innovatus Imaging Director of Commercial Operations and instructor in Penn State’s Biomedical Engineering Technology Program Ted Lucidi;
• Maull Biomedical Training LLC Owner Stephen Maull;
• Radiological Service Training Institute (RSTI) CEO Todd
Boyland, CRES, CPSM;
• Renovo Solutions Technical Training Manager Donald Armstrong, CBET, CHTM, CABT, CRES; and
• Webinar Wednesday Marketing Manager Linda Hasluem.
Q: WHAT DO YOU BELIEVE ARE THE MOST CRITICAL SKILLS OR AREAS OF KNOWLEDGE THAT TODAY’S HTM PROFESSIONALS NEED?
BARBOUR: The most powerful skill we possess is also the one we often overlook: communication. It’s the foundation of every successful technician. Technical mastery means little if you can’t clearly connect with people. Each day, we engage with medical staff, administrators, vendors, contractors, patients and, yes, even the machines themselves.
GONZALES: In the rapidly transforming field of healthcare, the most critical skills for today’s professionals revolve around a fusion of technical mastery and adaptive expertise to address megatrends like AI proliferation, cybersecurity imperatives, and the demands of an increasingly varied field of necessary expertise. Foremost are proficiencies in emerging technologies – such as AI supporting predictive
equipment maintenance, secure HIoT architectures for connected medical devices, and a nuanced understanding of advanced data analytics for life cycle optimization –which are indispensable for safeguarding patient safety. Complementing these are essential soft skills, including problem-solving, cross-disciplinary communication to align technical and clinical teams, and ethical acumen to empower HTM professionals. To cultivate a truly future-proof HTM workforce, three paramount training requirements must take center stage. First, blending curricula across biomedical, dental and veterinary device maintenance to foster versatile professionals who seamlessly service interconnected ecosystems, thereby reducing silos and enhancing crosssector efficiencies. Second, expanding technicians’ roles via advanced certifications in diagnostic imaging, linear accelerator operations and other domains to enable proactive interventions beyond conventional pathways. Third, conditioning and equipping technicians for on-demand, justin-time training through digital platforms, AR/VR and other innovative methods – prioritizing adaptive upskilling to align with fiscal realities and emergent demands, empowering lean teams to achieve more while transforming constraints into catalysts for innovation.
LUCIDI: As an instructor in Penn State’s biomedical engineering technology program, I believe that some of the most important skills for someone entering HTM are related to soft skills and customer service. We can educate most individuals on the how-to’s of troubleshooting, servicing and performing preventive maintenance. It’s more challenging to develop excellent customer service skills. Oftentimes in HTM, we have to fix the people, not the device. Many of today’s, and more of tomorrow’s, medical devices are and will be integrated into PC architecture. From a content perspective, students will benefit from programs that include content on PCs, networking and cybersecurity.
MAULL: The most important skill a BMET needs to have is ‘people’ skills. That is a skill that you kind of either have it or you don’t. Anybody can be taught how to maintain medical equipment, but it’s more difficult to make someone more of a people person than they currently are. You want the department to be glad to see you when you arrive, not be like, “Oh man, they sent Steve! I can’t stand Steve.”
BOYLAND: Today’s HTM professionals need a balance of technical proficiency, critical thinking and communication skills. As equipment becomes more integrated with networks and data systems, understanding connectivity, cybersecurity and interoperability is just as important as understanding the imaging hardware itself. At RSTI, we emphasize hands-on experience and root-cause troubleshooting because the ability to think through complex problems – not just follow a service manual – is what sets great engineers apart.
ARMSTRONG: While our field is highly technical, I believe the most critical skills for today’s HTM professionals are life skills – often called soft skills. Throughout my career, these have not received enough focus in training. If we can prioritize and empower our teams to develop and use skills such
as communication, ethics, teamwork, openness, humility, willingness and a positive attitude, then technical training becomes much easier by comparison. Strong life skills create stronger, more adaptable technicians.
HASLUEM: Definitely communication – it should be the number 1 critical skill! Strong communication is vital for teamwork with hospital/clinical colleagues and vendors. Being a good problem solver is a good skill to have too. With the rapid advancements in healthcare technology, HTM professionals definitely need a varied blend of technical expertise. The HTM field has expanded far beyond traditional equipment repair to cybersecurity, data analytics, etc. so they need to stay current with the latest technologies transforming the industry. Here at TechNation, our Webinar Wednesday series has seen a big shift in webinar subjects over the past couple of years. Our traditional equipment webinars are still popular, especially our Tools of the Trade live demos, but the interest in our technical and IT skills webinars, especially cybersecurity, have generated a lot of interest and are always well received and attended.
Q: HOW EFFECTIVE DO YOU THINK CURRENT HTM EDUCATION AND TRAINING PROGRAMS ARE IN PREPARING NEW TECHNICIANS FOR THE FIELD? ARE THERE SPECIFIC GAPS OR STRENGTHS YOU’VE OBSERVED?
BARBOUR: In many ways, modern technician training has become more effective than ever before. Students and instructors now have access to an incredible range of resources that deliver the latest information in highly engaging and accessible formats (videos, whitepapers, safety recalls, social media and even AI-driven tools). Training materials and supplies are also more readily available than in the past. A thriving market for used medical equipment, along with affordable electronics components from platforms like Amazon and AliExpress, allows technicians to practice and refine their skills.
GONZALES: Key gaps include insufficient emphasis on core skills for emerging technologies, such as AI-driven predictive maintenance and HIoT integration, which hinders technicians’ proactive innovation; a lack of foundational training in ethics within healthcare technology management; underdeveloped skills in effective communication and customer service, essential for clinical collaboration and the adoption of a patient-centered approach; inadequate coverage of compliance and the evolving regulatory environment; pronounced deficiencies in cybersecurity and medical device integration, exposing graduates to risks in networked, datavulnerable systems; and other shortfalls, such as limited focus on developing the next generation of HTM leaders. Bridging these gaps through industry-informed education and training programs is essential to equip technicians for resilient, forward-thinking contributions.
LUCIDI: I believe that the current content provided by most HTM programs is meeting the needs of the field. Today’s technology moves at an outstanding pace. It’s challenging for today’s institutions to “show” the latest technology. It’s
important to focus on fundamentals, not the latest tech. Whether techs are testing the latest, flashy, new physiological monitor, or one that’s 10-15 years old, the same parameters need to be verified. Simulators change and monitors change, but the parameters being verified are the same. If an institution focuses on the fundamentals, it’s preparing students for any level of technology.
MAULL: I know that there is more help than ever before. Several companies are making training more accessible by doing the training remotely or bringing the training on-site, which is getting more and more common.
BOYLAND: HTM programs are doing a commendable job introducing the fundamentals, but there’s a noticeable gap between classroom theory and field-ready confidence –especially in advanced imaging. Many new technicians have the desire and baseline knowledge but need applied, real-equipment exposure to transition effectively into a service role. That’s where RSTI’s model excels – our training center houses more than 70 fully functional imaging systems and offers a 4:1 student-to-equipment ratio so every learner develops real-world proficiency.
ARMSTRONG: We believe that current HTM education and training programs are strong in developing technical knowledge, but there is a significant gap when it comes to preparing new technicians with essential personal and professional skills. Our Renovo internal training courses do an excellent job of covering the technical aspects of the role, which are both important and necessary. However, once new technicians enter the field, they often face challenges communicating effectively with clinical staff and hospital leadership – skills that require deliberate development. In addition, a strong understanding of safety and regulatory requirements is critical. We place great emphasis on ensuring our new technicians are well-rounded, combining both the technical competence and interpersonal skills needed to succeed in any environment.
HASLUEM: Here at TechNation, I hope that our Webinar Wednesday series helps prepare new technicians by providing more than foundational knowledge. Our webinars offer a wide range of topics which cater to all levels of abilities. I have noticed an increase in student attendees over the past couple of years, especially for our Tools of the Trade live demos, which have grown in popularity, so I hope that we are doing our bit to help prepare a new generation of biomeds for the field!
Q: DOES YOUR ORGANIZATION PARTICIPATE IN OR SUPPORT APPRENTICESHIP OR INTERNSHIP PROGRAMS?
BARBOUR: While BC Group International does not offer a formal internship program due to the sensitivity of our laboratory and manufacturing environments, we have a long-standing tradition of identifying exceptional individuals and developing them into outstanding professionals. Our company maintains strong relationships with many of the leading industry schools, and we actively support internships
through training, mentorship and placement assistance.
GONZALES: Yes, the College of Biomedical Equipment Technology is deeply committed to apprenticeship, internship, and on-the-job (OJT) training programs, viewing them as vital bridges between students and our employer partners. Apprenticeships have ebbed and flowed in popularity over recent decades – once a cornerstone of skilled trades that declined with the rise of formal academia – they are now resurging as an attractive option for healthcare organizations seeking to build pipelines of trained technicians while managing budgets, with apprenticeships, pre-apprenticeships and hybrid OJT initiatives providing an effective means to achieve both. We have long championed the Association for the Advancement of Medical Instrumentation (AAMI) Apprenticeship Program. Our recent collaboration with American Healthcare Apprenticeships (AHA) has further enabled the college to expand its national reach, introducing students to HTM education and career pathways. Last year, we formed a partnership comprising AAMI, AHA, the college and HOSA-Future Health Professionals. This year, HOSA-Future Health Professionals formally introduced and launched a biomedical equipment technician competitive track for talented high school STEM students nationwide. We take great pride in this partnership and the opportunity to engage with the talented students participating at state and national levels and feel strongly that this initiative will fuel interest in apprenticeship opportunities.
LUCIDI: Innovatus, because of our specialized focus, is rather limited on the content that could be shared during a full apprenticeship or internship program. We are open to students shadowing our techs, but apprenticeship programs are best hosted by healthcare facilities and independent service providers with a wide scope of support. Students are best served by selecting an internship or apprentice program (or site) which offers exposure across the widest variety of devices and environments.
BOYLAND: Yes. RSTI proudly supports both DoD SkillBridge and GI Bill approved programs that provide pathways for service members and veterans transitioning into civilian HTM careers. These programs are structured around career-ready, hands-on imaging service training followed by industry placement partnerships with hospitals, ISOs and OEM-alternative service organizations. The impact has been tremendous – graduates leave with technical competency, industry certifications and a clear path to employment in an essential healthcare field.
ARMSTRONG: At Renovo, we run our own internal apprenticeship program while also engaging with AAMI’s national initiative. Our apprentices are typically recent graduates or second-career professionals new to HTM. They complete a six-month blended training program combining remote learning and on-site experience. After progressing through three phases and demonstrating readiness, apprentices are typically promoted to BMET I, with oversight from both the on-site and training managers.







Q: HOW CAN PARTNERSHIPS BETWEEN SCHOOLS, HOSPITALS AND INDUSTRY LEADERS IMPROVE HTM EDUCATION AND WORKFORCE READINESS?
BARBOUR: We are a community. Although we each play distinct roles within this skilled trade, our success depends on mutual support and collaboration. Through a robust digital network, we can instantly share information, ensuring trainees have access to the most current knowledge and the best opportunities as they enter the workforce. This bidirectional exchange benefits everyone. Companies gain access to highly qualified candidates, while schools receive real time feedback to strengthen their programs. Across the country, many schools, hospitals, and organizations proudly champion their local HTMA chapters, further reinforcing our professional network. Like any skilled trade, well-rounded technicians must cultivate a broad range of experiences to remain efficient and adaptable. Our community makes this possible by providing hands-on exposure that maximizes every technician’s potential.
GONZALES: One of my favorite quotes from Arthur Levine and Scott Van Pelt’s “The Great Upheaval” is that “some organizations will survive, and some will thrive” amid the complexities of our technology-driven society. The current transformation in higher education – fueled by industry, demographic, economic and technological shifts – is profoundly reshaping our approach to supporting the healthcare industry. To navigate such radical change, strong industry partnerships are not merely advisable but essential to achieving our mission. Strong relationships between the college and our industry partners amplify workforce readiness by fostering innovation, research and the iteration of training development to target gaps in workforce development and training aligned with the career pathways
of today and tomorrow. Ultimately, such partnerships not only close skill gaps but elevate HTM as a profession responsive to changing expectations, producing adaptable professionals who enhance patient outcomes and operational resilience across the healthcare continuum.
LUCIDI: Partnerships between industry and education are vital to the success of HTM. As an educator, I only have a short, very limited time to expose students to a wide variety of medical devices. In fact, the content that students are exposed to in the classroom is most likely less than 10% of the devices they will encounter in the field. Many HTM programs include some type of internship within a healthcare facility. It’s my belief that HTM students would be best served by participating in clinical rotations throughout their education, similar to nursing and radiation technology students. Students would learn at an accelerated rate, and the healthcare facility would benefit from having additional HTM personnel.
MAULL: I have long thought the biggest hurdle to the growth of our career field was the lack of knowledge of the existence of our career field. The day I became a BMET (military trained) was the first time I had ever heard of a BMET. I was a college graduate and didn’t even know this was a job. Bryant Hawkins is a BMET who is doing a great job leading the charge in developing awareness of the HTM career field in middle schools and high schools. The associate degree for clinical engineering also appears to be making a bit of a comeback as well after many schools dropped the degree program over the last 15 years or so.
BOYLAND: Collaboration is the key to bridging the workforce gap. When schools provide foundational knowledge, hospitals offer clinical exposure, and industry partners like
RSTI deliver specialized technical training, we create a comprehensive training pipeline that builds competent and confident professionals. These partnerships also ensure that training stays aligned with real-time industry needs from technology updates to regulatory compliance – so graduates are workforce-ready on day one.
ARMSTRONG: I serve on the EQ-WG05 HTM Educational Programs Standards Committee, where we work to standardize and strengthen HTM education to ensure students are well-prepared for success. Collaboration between schools, AAMI and industry leaders is essential to aligning training with real-world needs. Regular roundtables at conferences help us share challenges and successes, fostering a strong community dedicated to developing and sustaining high-quality HTM programs and graduates.
HASLUEM: Just continue to work closely together to ensure that future and seasoned techs get exposure to experts in the field. Webinar Wednesday will certainly continue to provide up-to-date education and information on products and services to the HTM industry.
BARBOUR: Every training program, certificate, degree and certification provides technicians with a way to demonstrate their proficiency and mark their professional achievements. While certifications alone do not define a technician’s worth or overall qualification, they do serve as a reliable indicator of a certain level of skill and competence.
GONZALES: Certification programs such as the Certified Biomedical Equipment Technician (CBET) and Certified Healthcare Technology Manager (CHTM) serve as pivotal accelerators for HTM careers, validating specialized expertise and signaling a commitment to excellence and lifelong professional growth. For emerging technicians navigating changing demographics and evolving workforce expectations, earning an AAMI certification offers a tangible pathway to credibility, enhancing employability as employers increasingly prioritize certified talent to manage complex, patient-centric environments. Certifications are widely respected professional credentials that underscore an individual’s dedication to continuous development and service to the industry. As an educational institution, the College of Biomedical Equipment Technology prioritizes equipping students with a thorough understanding of the credentialing process and its profound relevance to their career trajectories; to this end, we integrate AAMI certification preparation directly into our curricula through targeted content and discussions aligned with AAMI credentialing requirements. All graduates are strongly encouraged to pursue the appropriate AAMI credential, ensuring they enter the field not only skilled but also strategically positioned for advancement.
LUCIDI: I believe that certifications can help in advancing a career. Today, only a small portion of employers require certification as a condition for employment, and even fewer offer increased pay for achieving it. Seeing
as there are no state or national-level requirements for licensure or certification (yet) and little to no salary incentive, I view certification as an activity pursued by those desiring to improve themselves. Certifications help elevate the individual. I value certification but would not commit to limiting employment offers to only those who are certified. When considering choosing between two individuals with similar experience, interpersonal skills and personal recommendations, the certified individual would be my choice.
BOYLAND: Certifications validate expertise and demonstrate a commitment to professional growth, but they’re most meaningful when paired with hands-on, practical experience. Earning a CBET or CHTM can open doors and provide recognition, but the real advancement happens when technicians continue to learn, adapt and apply new skills. We often encourage our students to pursue certifications after completing core training, so they have both the knowledge and the confidence to succeed.
ARMSTRONG: I’m a strong supporter of certification and its role in advancing HTM careers. Certifications like CABT, CBET, CRES and CHTM not only validate technical knowledge but also build confidence and professional pride. The CABT, introduced by AAMI as an entry point for students and newcomers, is a great way to start. As someone who has taught the CBET review course for several years, I’ve seen firsthand how certification transforms technicians – it shifts their mindset from having a job to building a career and a true profession.
HASLUEM: Every certification is important, as it encourages people to have a higher standard of competence and professionalism. Certifications validate skills, so we are proud that we can offer CE credits for our webinars, live and ondemand, to help biomeds advance in their careers. Added bonus – our webinars are free!
Q: LOOKING AHEAD, HOW DO YOU SEE HTM TRAINING AND PROFESSIONAL DEVELOPMENT EVOLVING IN THE NEXT 5-10 YEARS?
BARBOUR: I’m optimistic about the future of our field and the growing effectiveness of technicians, regardless of their initial level of training. With instant access to resources, technicians can now solve problems more efficiently and make datadriven decisions that reduce unnecessary contracts and parts purchases (ultimately lowering costs and improving outcomes). Advancements in tools, intelligent and intuitive test equipment, AI driven knowledge bases, and augmented reality technologies are transforming the learning curve, enabling even junior technicians to perform with exceptional effectiveness.
GONZALES: Over the next 5-10 years, HTM training and professional development will likely shift toward hyperpersonalized, technology-infused models that harness virtual reality (VR) and augmented reality (AR) for immersive simulations of AI-driven device troubleshooting and Healthcare Internet of Things (HIoT) deployments – rendering education more accessible and scalable amid hospital

financial constraints. This evolution will prioritize shortduration programs, micro-credentials and curated learning paths, enabling technicians to upskill in real time and ensuring a diverse workforce remains equipped to match the rapid pace of technological and healthcare advancements. Professional development will increasingly emphasize holistic competencies, seamlessly blending technical expertise with essential soft skills such as ethics, communication and customer service – areas often undervalued yet vital for success. As evolving expectations demand greater agility, hybrid apprenticeships incorporating remote mentorship will proliferate, lowering barriers to entry and retention. Ultimately, this trajectory will position HTM as a forward-thinking profession: resilient to disruptions and indispensable to the sustainability and efficacy of the U.S. healthcare system.
LUCIDI: As mentioned earlier, I believe that we’ll see HTM programs increase the amount of time spent in the clinical environment via internships and apprenticeship programs. No doubt, many in-person programs will transition to hybrid or to fully virtual training in combination with clinical rotations. With the huge vacancies in HTM, I believe it’s the most effective means of reaching the greatest number of potential students.
MAULL: There will be a lot of remote training via VR (virtual reality). With a headset, the student(s) can be in one city and the instructor(s) can be in another city but they can meet in a virtual classroom and perform operation and maintenance training on a virtual piece of medical equipment. The technology to do so is already here and is constantly improving; this method of delivering training will become more and more common in the coming years.
BOYLAND: The future of HTM training will blend immersive, technology-driven learning with experiential education. Virtual simulations and online theory modules will complement – but never replace the need for hands-on practice. We’ll also see greater emphasis on networking, cybersecurity, AI integration and multimodality service skills as imaging systems become more interconnected. At RSTI, we’re committed to evolving right alongside the industry, ensuring that every technician – whether new to the field or advancing their career — has access to training that’s relevant, rigorous and impactful.
ARMSTRONG: I see technologies like virtual reality (VR), augmented reality (AR) and artificial intelligence (AI) playing a major role in the future of HTM training. I hope colleges and training programs adapt quickly to integrate these tools so our field stays ahead of the curve. HTM professionals have always been adaptable, and this will be another exciting evolution. I welcome these advancements – they’ll attract new talent and enhance how we learn and grow in this profession.
HASLUEM: I’m sure AI and VR will no doubt play a central role at some stage, but until that time Webinar Wednesday we will continue to provide continuous education for the HTM field as long as we are needed. 2026 will be exciting for us as we are adding two new ideas to our series – a Roundtable spotlight and Unlock and Learn series. I’m sure they will help our attendees with their HTM training and professional development. Find out more at webinarwednesday.live.
• Register for free and apply to any of our listings
• Browse our 350+ open positions across the United States

• Get directly connected to industry hiring managers





• A talent network of 3600+ actively looking biomedical and imaging professionals
• A variety of listing and advertising options
• Social media, print, and eNews promotion Featured Employers: Agiliti,
“HTMjobs.com is a remarkable website that can be used by any personnel looking for employment, internships, or just a good read from their Career Center . The site offers job postings from employers in the HTM industry, as well as resources for job seekers to help them prepare for their job search, including resume tips, interview advice, and more.”

By K. Richard Douglas

trategic planning is a structured process for organizations to outline their future direction, set clear goals and allocate resources effectively. The process is important for navigating dynamic environments, fostering internal alignment and enhancing competitiveness.
It is a comprehensive framework that serves as a roadmap for an organization, outlining its vision, mission and long-term goals and detailing the actionable steps required to achieve them. It involves a structured process of defining strategy and making plans for the future.
Strategic planning typically encompasses stages like building awareness, goal formulation, environmental analysis (including SWOT – strengths, weaknesses, opportunities and threats), strategy creation, implementation, continuous monitoring and evaluation.
Key aspects of a strategic plan include: mission, vision and values. These foundational elements define the organization’s core purpose, what the future would look like if its goals were achieved along with the guiding principles for behavior and decision-making.
It is important to differentiate strategic plans from operational business plans and emphasize the necessity of flexibility and
stakeholder involvement for successful execution, noting that effective strategic planning is an ongoing and adaptive process crucial for long-term growth and resilience.
Developing a comprehensive strategic plan is vital for any healthcare technology management (HTM) department, serving as a long-term roadmap that aligns departmental goals with the overarching mission of the health system.
Strategic planning looks three to five years out, focusing on a long-term vision and a broad scope. It involves higher levels of leadership within the department (such as directors) in its generation. The strategic plan requires specific, long-term budget dollars targeted toward future initiatives, potentially including capital expenses like the construction of new facilities or the establishment of a central depot for repairing low-acuity devices.
Adjustments to the strategic plan are occasional, necessitated by significant circumstantial changes, such as merging from a 25-hospital system to a 33-hospital system. Strategic progress is typically reported to the executive team.
Operational planning, conversely, addresses short-term objectives, often focusing on annual goals. These goals are narrow and detailed, involving day-in and day-out activities.
Operational plans involve managers, supervisors and frontline staff in their creation and they are subject to frequent, even daily, adjustments (e.g., during morning huddles).
The operational plan relies on the operating budget, covering expenses like parts, service contracts and labor. Operational

reports, such as monthly PM compliance and incident reports, are shared throughout the organization. Crucially, the operational plan should incorporate milestones and objectives necessary to achieve the goals set forth in the strategic plan.
Mike Busdicker, MBA, CHTM, AAMIF, FACHE, an HTM professional with 43 years of experience, including senior leadership, presented on the topic of “Why and How to Develop an HTM Strategic Plan” at last year’s MD Expo in Las Vegas.
“The healthcare industry continues to change and the HTM department needs to ensure they are positioned for the future. A strategic plan will provide the HTM department with clear direction, improved decision-making, enhance operational efficiency and will help establish performance metrics to achieve department and organizational goals,” Busdicker says.
He says that it can also generate innovation, improve resource allocation and allow the department to be proactive in managing risks and adapting to a rapidly changing healthcare environment.
In order to formulate a successful strategic plan, HTM leadership needs to rely on the right sources of information to make accurate forecasts.
“Good leaders will rely on a variety of information that can be gathered through internal and external analysis. This data will allow leaders to understand the department’s current state, define its future vision and set measurable goals,”
Busdicker says.
He says that internal information focuses on the department itself and will identify strengths and weaknesses. This should include things like key performance indicators (KPIs) and metrics, operational information, financial data, staffing, core competencies and stakeholder feedback.
“External information should focus on the larger environment to identify opportunities and threats that may be outside the department’s control. Information can come from things like industry research, competitor analysis, customer analysis and economic trends,” Busdicker adds.
He says that once this information is captured, leaders should integrate internal and external data.
“This can be done by using a SWOT analysis to combine internal data (strengths and weaknesses) with external data (opportunities and threats) to get a complete picture of where the department stands. This will provide leadership with strategic themes, goals and objectives and provide the framework for development of action plans,” Busdicker says.
Creating a strategic plan is necessary to avoid falling behind the industry curve, as evidenced by major corporations like Blockbuster, Circuit City, and Toys-R-Us that either failed to plan strategically or failed to routinely review their plans. For HTM, a strategic plan serves several critical functions:
• Sets Direction and Goal Alignment: It clearly defines the
department’s path, getting all caregivers working toward a shared objective. It ensures the HTM department’s goals are aligned with, or mirror, the organization’s goals.
• Resource Allocation and Risk Management: The plan determines how to allocate financial, manpower and technology resources effectively to accomplish strategic goals. It also identifies potential risks and outlines mitigation strategies.
• Performance Measurement and Communication: The plan establishes a year-by-year road map with key indicators for routine assessment. Communicating this plan to frontline staff helps them understand the department’s future and identify opportunities for career development.

How do you get all stakeholders on board with a strategic plan as it relates to HTM? Where does the consensus come from in creating and adapting the plan? Some major retailers have failed, so why did their strategic plans go wrong?
“In order to develop a sense of ownership, leaders must be sure to involve key stakeholders early and often. This can be done through empowering individuals in the development of the plan and creating cross-functional teams to drive alignment,” Busdicker says.
He says that the strategic plan must be communicated to staff with a clear vision and benefits.
“Leaders must be able to explain the ‘why’ and the vision for success. This communication needs to occur often and can be done through various channels. The plan should be accessible and easy to understand by all employees,” Busdicker says.
He says that the strategic plan should be part of the daily, or weekly, work plan and integrated into things like team meetings and huddles. This will help drive home the importance and provide employees with a general sense of status and their individual contributions.
“Leaders should be sure to celebrate achievements related to the strategic plan. One avenue is to develop ‘quick wins’ that take no more than 90 days to complete. Also, good leaders will acknowledge specific employees or teams and reward desired behaviors that contribute to moving the strategy forward,”
Busdicker adds.
He says that consensus in relation to strategic planning for HTM comes from a collaborative, inclusive process where input from all stakeholders has been considered and valued.
“This should lead to a shared understanding of goals, direction and the path forward. Some of the key elements include active listening, open discussion, respect of ideas, incorporating diverse perspectives, establishing clear objectives and empowering employees and stakeholders to contribute. All of these items will help build trust, provide new ideas and strengthen commitment to the plan,” Busdicker says.
He says that organizations like Toys-R-Us and Circuit City did not position themselves for the future. They ignored things like online retail, mail order, newer integrated technology, smaller and more powerful widgets. They stayed in their lane and did not look or adjust to the future.
Busdicker says that HTM departments must be aligned with the strategies of the organization. This includes alignment with the overarching goals to ensure effective resource allocation, patient safety and operational success.
“When the HTM department is on the same page as the organization it can lead to enhanced life cycle management, equipment standardization, meaningful metrics and continuous improvement. A misalignment can lead to fragmented technology management, inefficient spending and compromised patient care,” he says.
This will ensure that the HTM department’s work will directly contribute to the larger organizational strategy and provide a single direction. These measurable and actionable items will provide effective resource allocation, improved collaboration with other departments, and a focused approach to achieving the overall strategic success.
The HTM mission statement should be identical to the health system’s mission. The HTM vision, while not identical, must be aligned with the organization’s vision. Leaders must ensure staff understand how their contributions — such as equipment availability, compliance and cost avoidance — fulfill the mission.
With the building blocks in place, what can impede a strategic plan?
“There are a number of things that can impede a strategic plan with the most prevalent being poor planning – unclear objectives, unrealistic goals, insufficient data – and poor execution. An HTM department that rushes to complete a strategic plan could end up with a document that has unclear objectives, unrealistic goals and insufficient data. This typically results in lack of buy-in from employees, no stakeholder involvement and misalignment with the organization,” Busdicker says.
He says that poor execution of the strategic plan can lead to failure of reaching goals and objectives. This topic includes the lack of communication to employees and stakeholders, limited resources, no buy-in, a resistance to change and an inability to adapt.

Resources that can guide best practices in establishing a successful strategic plan can come from internal and external sources.
“There are a number of internal and external resources for developing a strategic plan. Some have been covered like the SWOT analysis, competitor analysis, industry reports, and market analysis. Each healthcare institution should have a department, personnel, or a potential management firm, dedicated to development of an organizational strategy. These are internal resources that can be utilized by the HTM department,” Busdicker says.
He says that external resources for development of a strategic plan include management firms, consultants, education classes and books.
“One of my favorite books is ‘If Disney Ran Your Hospital: 9 ½ Things You Would Do Differently,’ by Fred Lee. This book outlines the difference, but same, ‘service experience’ provided by Disney and healthcare institutions. It can provide a framework for data collection and development of a strategic plan,” Busdicker adds.
their level of interest and influence. The focus should be on engaging those with high interest and high influence, as they are most helpful in overcoming obstacles and barriers.
A communication plan detailing how often and with what level of detail different stakeholder groups receive updates must be developed. Finally, the plan requires continuous evaluation, monitoring progress against the established road map and strategic priorities, learning from items that were not successful, and reporting HTM contributions to overall organizational success to higher leadership.
Key components include defining clear objectives and setting SMART (specific, measurable, achievable, relevant and timely) goals. A situation analysis, which includes a SWOT analysis should be conducted. Leadership should focus predominantly on strengths and opportunities, as strengths set the team apart, and opportunities can be developed into strengths. Strategic priorities must then be captured and aligned with broader organizational objectives like stewardship, quality and safety.
Busdicker says to provide more details of the plan to the high-interest, high-influence stakeholders. As far as some of the barriers mentioned earlier, some of the high-influence stakeholders may be able to help overcome those.
Communication is paramount to a successful strategic plan. Stakeholders should be identified and categorized based on

With a plan in place and barriers out of the way; a strategic plan can lead to HTM success.

The Cybersecurity Working Group (CWG) of the Health Sector Coordinating Council (HSCC) is providing healthcare organizations with templates and a methodology to visualize, identify and measure systemic risk posed by third-party technology, software and communications services essential to clinical, administrative and manufacturing workflows.
The Health Industry Cybersecurity Sector Mapping and Risk Toolkit (SMART) culminates 16 months of cross-sector collaboration among 80 organizations in patient care; health insurance; labs, pharmaceutical and blood services; medical technology, public health and health IT.
“Critical functions in the health sector form a complex ecosystem of interdependent organizations of all sizes, including patient care, payment and data management systems, pharmaceutical, manufacturing, technology research, and public health administration,” said Samantha Jacques, vice chair of the HSCC CWG and co-lead of the SMART Task Group. “A cybersecurity event affecting a single supplier or third-party support for critical functions across healthcare workflows poses one-to-many impact. A disruption to one payment clearinghouse, for example, can shut down a significant portion of the nation’s healthcare delivery.” Jacques is vice president of clinical engineering for McLaren Health in Michigan.
The SMART Toolkit is intended for cybersecurity, supply
chain, risk, operational and administrative executives across health industry organizations of all sizes and subsectors, including healthcare providers, insurance, plans and manufacturers. Its recommended practices directly address imperatives for third-party risk management in the Health Industry Cybersecurity Strategic Plan 2024-2029 released by the CWG last year.
Premera BlueCross Chief Information Security Officer Dr. Adrian Mayers, a co-lead of the SMART Task Group, observed that, “The impact of a cyber disruption on critical functions can include loss of patient data and payment information, theft of intellectual property, or exploitation of medical device vulnerabilities that lead to disruption of functionality or patient harm. The growth of ransomware threatens the availability of critical functions and systems, leaving organizations unable to provide services or products relied upon by patients and health professionals.”
Larger organizations have dedicated resources to improve the resiliency of their critical functions, but many small- to medium-sized organizations lack similar scale and need support with tools appropriate to their size, capability and resource constraints. The SMART Toolkit provides them actionable guidance and methods for managing systemic risks related to their critical functions and dependencies within the health system. It empowers these organizations to demand secure products and high availability of services from their suppliers, thereby driving improved standards for critical functions across the entire healthcare ecosystem. In situations where customer leverage is insufficient to influence third-party security, the SMART tool can help organizations anticipate potential incidents and develop backup and resiliency plans.


BY JOIE N. MARHEFKA
s 2025 comes to an end, I am taking an opportunity to reflect on the year that was and look ahead to 2026. From my perspective as an educator, I am thinking of ways to ensure that we continue to prepare students for careers in 2026 and beyond. The following are a few things that are on my mind.
In my 2023 year-end column, I wrote “One topic that it seems no one in education can stop talking about is artificial intelligence (AI), especially the use of ChatGPT.” This is true today more than ever. The majority of my students say they use AI on a regular basis. A couple of them are working on a project related to generative AI. Alumni have recently been telling me that they are using AI at work. Employers are asking for us to teach AI, as they are looking to hire graduates who are AI literate. I’ve been wrestling with how to include AI in my curriculum. While I have more questions than answers at this point, I am working on it. While I don’t think AI can replace humans, especially in fields like HTM, I think it can
help us to work more efficiently, as long as we understand how and when to use it. Of course, ethical and regulatory questions need to be considered as well. My goal is to teach students how to use AI as a tool, while still making sure their fundamental skills are strong and that they can think critically.
While AI is a “hot topic” and has been mentioned by some employers as a skill they’d like prospective employees to have, by far the most common feedback from employers is that they want graduates to have strong communication and customer service skills. In the AI era, soft skills (also known as durable skills) including critical thinking, communication, collaboration, creativity, fortitude, growth mindset, and leadership remain as important as ever. This has been on my mind as I strive to prepare my students for their future careers.
In addition to making sure my students have fundamental skills, AI skills, and durable skills by the time they graduate, I encourage them to take advantage of opportunities that could help them with their future careers. I am happy to report that this year’s students seem to be embracing this. In
the fall semester, we visited Bayer Radiology and toured several local hospitals. We hosted a well-attended networking event with alumni and invited several guest speakers from various aspects of the industry. Next semester, a group of students is planning to attend a local HTM conference, and several students are participating in research projects. I’m glad to see that these students are taking advantage of opportunities to explore the HTM field beyond the classroom, build their networks and make their resumes shine.









BY NATHAN PROCTOR
The campaign to win the Right to Repair – reforms that ensure manufacturers can’t constrain repair of modern equipment – has often felt contentious. Right now, the battlefield for those rights is the literal battlefield.
Congress is on the verge of giving the U.S. Military the Right to Repair.
Both the U.S. House and Senate have passed their versions of the National Defense Authorization Act (NDAA) with provisions that ensure every branch of the military can access all the parts, tools and information they need to make repairs on their own.
Next, the legislation heads to a conference committee, where leadership of the House and Senate can iron out differences and make any final changes. Pressure is mounting from defense contractors and others to soften
or remove Right to Repair provisions, and conference committees tend to be the least transparent part of the process. The White House signaled support for the policy as well.
In other words, while we are close to passing a Right to Repair measure all the way through the U.S. Congress, we aren’t there yet.
Medical device repair is a critical part of the equation.
While the military is the sole buyer of some of the equipment they purchase – such as specialty weapons systems – they also purchase a lot of equipment which is otherwise generally available. That’s why a wide range of manufacturers and trade groups have come out against Right to Repair, including AdvaMed, which represents medical device manufacturers.
The Associated Equipment Distributors (AED), which represents dealerships for farm, construction and other heavy equipment, has claimed that granting the military a Right to Repair would “set a terrible precedent,” which
the group fears could be expanded to other markets.
But failures of non-weapons systems can be a huge problem for military operations. Navy Secretary John Phelan told Congress this story in June: “I went on the [USS Gerald R. Ford] carrier; they had eight ovens – this is a ship that serves 15,300 meals a day. Only two were working. Six were out [for repair].”
“I am a huge supporter of ‘Right to Repair,’ ” said Phelan.
My organization, PIRG, has collected a range of stories, including from medical device repair technicians about being denied access to critical materials and service access that directly impacted troops’ healthcare.
“I was fixing that equipment with one hand tied behind my back,” Retired Master Sgt. Wesley Reid told me, regarding challenges around keeping a CT scan working without needed microcontrollers the manufacturer refused to provide.
I am hopeful that soon, biomeds helping to save the lives of wounded service members won’t have their hands tied behind their backs. If you agree, you should reach out to your senators and let them know you want Congress to put military Right to Repair over the finish line.

Nathan Proctor is senior director of the U.S. PIRG Campaign for the Right to Repair.









BY STEVEN LUTZ
Biomedical technology is at the heart of healthcare, where every diagnostic unit, monitor, or life-saving device depends on precision and reliability. Behind the smooth operation of lifesaving technologies are skilled biomedical equipment technicians, the unsung heroes making medical equipment function when it’s needed most.
As demand for healthcare technology management (HTM) continues to grow, the need for trained professionals is more pressing than ever.
ReNew Biomedical has been a leading force in providing education, certification and apprenticeship programs for aspiring biomeds. With the launch of the ReNew Biomedical Training Academy, ReNew has opened new pathways to enter and thrive in the HTM field.
ReNew Biomedical began its mission to service and maintain life-saving medical equipment in 2014. What started as one small workbench has evolved into a service depot, full-time traveling techs, multiple remote service depots and a nationwide leader in healthcare technology management. Along the way, they focused not only on service and repair operations but also on creating opportunities and career pipelines for the next generation of technicians.
From the ReNew Biomedical Apprenticeship Program to in-person and online courses, ReNew is training and educating students, newcomers to the field and seasoned technicians alike.
Whether you’re just starting a career or looking to advance your skills, there are several pathways you can take to enter the biomedical technology field. We’ll break down the most common places to start your journey.

What began as one small workbench has evolved into a nationwide leader in biomedical service and education.
For those who thrive in a hands-on learning environment, in-person courses are a fantastic option. In-person classes provide students with direct access to state-of-the-art biomedical equipment benches and instruction from experienced, certified professionals. Students are immersed in real-world scenarios and learn by doing.
In 2021, ReNew launched its training academy, providing education through in-person classes and hands-on experience for technicians looking to complete their CABT and CBET certifications. Since then, ReNew has graduated 10 classes of biomedical students, totaling 51 CABT certifications and 12 CBET certifications.
Courses cover essential topics in healthcare technology management, including:
• Biomedical equipment functions
• Clinical application of devices in healthcare settings
• Preventative maintenance
• Safety standards
• Diagnostics and troubleshooting
For those who need more flexibility, there are online learning resources, such as ReNew’s Fundamentals of HTM course. Self-paced digital courses allow students to learn the basics of healthcare technology management from the comfort of their own home. The online format covers foundational knowledge that will prepare you for certification exams like the Certified Associate in Biomedical Technology (CABT).
The Fundamentals of HTM course includes:
• Occupational safety
• Patient safety
• Anatomy and physiology
• Electrical systems and IT
• Medical equipment fundamentals
• Problem solving/troubleshooting
Best for: Individuals balancing work, school, or other commitments who want to pursue certification without attending a traditional classroom setting.
For those who learn best by doing, partnered apprenticeship programs offer the most immersive pathway into the HTM field. In 2021, ReNew launched its apprenticeship program, combining in-person classes, mentorship and hands-on experience to aspiring biomedical technicians.
Apprentices partner with experienced technicians, and are trained on real-world equipment, learning to troubleshoot, repair and maintain biomedical devices in a supervised setting.
Apprenticeship programs include:
• Paid, on-the-job training
• Industry-recognized certifications
• Mentorship from seasoned professionals
ReNew’s Apprenticeship Program has received national recognition for producing industry firsts like Josh Weatherford, the first AAMI/Federal Department of Laborregistered biomedical apprentice to receive a CABT and CBET, and JL Morgan, the first graduate of the Tennessee Biomedical Technician Apprenticeship Program. Apprenticeships create pathways for long-term careers in the biomedical field, setting technicians up for success as certified professionals.
The demand for certified biomedical technicians continues to rise, with more hospitals, clinics, and healthcare organizations relying on skilled professionals to keep their medical equipment ready and functioning at all times.
Whether you’re looking to get started in the field, train your team on new devices, or advance your career, there have never been more opportunities to grow in and advance in the HTM field.

Steven Lutz is the general manager with ReNew Biomedical.

BY ERIC MASSEY
It’s 2 a.m., and your phone buzzes again. Another critical equipment failure. Another sleepless night.
You entered this field to make a difference but lately, it feels like the difference is costing you everything.
If you’ve ever felt that way, you’re not alone. According to the CDC’s VitalSigns report, 46% of healthcare workers reported feeling burned out “often” or “very often” in 2022. In healthcare technology management (HTM), where uptime and patient safety are the mission, burnout doesn’t just drain leaders, it threatens the very systems they protect.
Early in my leadership career, I believed being
“always on” was what great leaders did. I was the first to respond, the last to log off, and I wore exhaustion like a badge of honor. On paper, I was performing. But behind the scenes, I was running on fumes – mentally, emotionally and physically.
The turning point came when I realized that burnout doesn’t make you stronger it makes you replaceable. Balance, on the other hand, makes you sustainable. Here are five shifts that helped me move from burnout to balance. They can help you do the same.
Early in my career, I worked 70-hour weeks convinced that effort equaled effectiveness. But at the end of those weeks, I was exhausted and still behind. What I lacked wasn’t effort it was focus.
Start each week with one question: “What are the three outcomes that would make this week a win?”
This is what I call the Core Week mindset: clarity before activity. Protect time for deep work the same way you protect uptime in your facilities. When everything is urgent, nothing is truly important.
Our industry runs on preventative maintenance schedules. Why should your energy be any different?
Researching Brendon Burchard’s “High Performance Habits” shows that top performers take short breaks about every 52 minutes to maintain focus and stamina. Yet most leaders run through their days like they’re racing a 24-hour shift with no pit stops.
A few years ago, I started blocking short recovery breaks into my calendar even just a 10-minute walk between calls. That simple shift increased my clarity and patience with my team more than any leadership course ever did.
Treat recovery as part of the system:
• Schedule 15-minute resets every few hours
• Protect one night a week with no work messages
• Prioritize hydration, movement, and sleep as seriously as uptime metrics
You wouldn’t skip PMs on a ventilator and expect reliability. Don’t skip them on yourself and expect clarity.
Your team mirrors what you model. If they see you responding to messages at midnight, they’ll assume that’s what leadership requires.
I learned this the hard way. When I began setting a visible boundary “I don’t check messages after 7 p.m. unless it’s urgent” something shifted. My team followed suit. Stress levels dropped, and our responsiveness during the day improved.
Leaders create culture through consistency. I use what I call the 60/40 Rule – 60% drive, 40% recovery. When we honor both – we perform longer, think clearer and serve better.
Burnout thrives where purpose fades. Every HTM professional contributes to patient safety, but that truth can get buried under work orders, budgets and system alerts.
Each morning, take two minutes to reconnect to your “why.”
“Who will be safer because I do my job well today?” I started doing this before reviewing my first report or email. It re-centers me on impact, not inboxes. Purpose turns exhaustion into endurance, it reminds us that our work isn’t just technical, it’s deeply human.
The best leaders aren’t those who fix every issue; they’re those who model sustainable success.
That may mean delegating more, saying no to one extra project, or taking a real vacation without checking your phone. When you manage your energy with the same discipline you manage your team’s workload, you build longevity – for yourself and for everyone watching.
Leadership isn’t about being available 24/7. It’s about being effective when it counts.
Ask yourself: “Am I leading from exhaustion or from energy?”
Because the leaders who thrive in 2026 and beyond won’t be the ones who grind the hardest, they’ll be the ones who protect their energy, lead with purpose and inspire their teams to do the same.
If you’re tired of running on fumes and ready to lead with balance, clarity and purpose, let’s connect. What’s one shift you’ll make this week to protect your energy? Share it with me on LinkedIn, I’d love to hear your story and help you thrive.
The choice is yours – lead with energy or lose it. Let’s choose energy.

Eric Massey is a regional director of operations with Intelas and founder of The Massey Method. Find him on LinkedIn at linkedin. com/in/eric-masseyhts.
“Leaders create culture through consistency. Model rest, and your team will mirror balance.”
BY GARRETT SEELEY AND RICHARD THAI
As we write this, the Microsoft Windows 10 Home Operating System (OS) is officially transitioning to end of life (EOL). It will be out of support as of October 14, 2025. Security updates, virus patches, fixes, or additions from Microsoft for the Windows 10 Home user will no longer be available. As of now, the Windows 10 Enterprise (for businesses) and the Windows 10 IoT (Internet of Things) versions are considered Long-Term Service Channel (LTSC). LTSC is scheduled for end of service on January 12, 2027, with options to extend to 2032. Fortunately, Enterprise and IoT are common operating systems for medical devices, but the end of support for the Home OS may still affect some devices. As a result, some medical devices will require updating to the newer Windows 11 OS. This will depend on what the original equipment manufacturer (OEM) has verified will work for each medical device.
An update is a minor incremental change to software or hardware for security patches and bug fixes. We use updates to make small adjustments to an existing OS, allowing it to function better or adapt to newer hardware. Updates support device stability and security. The problem with updates is the labor cost. Older software is expensive to continually update, and hardware changes eventually force full OS rewrites. An upgrade, by contrast, is a major operating system replacement. It would include more features and improvements as well as changes to the look and feel of the system. It is a full replacement of software. This is a great option to reinvigorate the operations of an older device. There is only so much that can be done to adapt a new OS to an older medical device. Eventually, all operating systems go out of support and require replacement.
It’s a familiar scene: The hospital gets a unit that runs faithfully for eight years only to have its end of life occur. This progress is driven by several factors: advancements in hardware, new techniques for old medical processes, or loss of parts support. The field often pushes for new equipment. An OS used in medical devices follows the same pattern. It must be repaired and maintained as a component of the overall medical device. This is done with updates. The medical device lifespan is around 10 years. A standard OS life cycle is five years. It is anticipated that the OS would be upgraded once during the medical device life cycle.
Remember that with LTSC, this is not always true. We can sometimes extend the lifespan of certain devices beyond the 10-year range. This will depend on device upgradability and network security. Additionally, we also must do update maintenance for medical-purpose workstations. As a rule, life expectancy for workstations is five years with no upgrade to the OS. This is due to the expected workstation life cycle of a typical five-year replacement. Older medical devices with out-of-support operating systems can continue to run; however, doing so is labor intensive. Monthly security scans are recommended on an outdated OS. This motivates us to replace units that cannot be upgraded. OEMs will check the compatibility of OS upgrades with their equipment and certify any upgrades. A lack of upgrades authorized by the OEM can determine when equipment needs to be replaced. If there are no alternatives to updating or upgrading OS, the equipment itself may be deemed end of life.
When there is an upgrade for legacy biomedical equipment that does not require system replacement, the upgrade may have to be purchased. Once procured, a kickoff meeting will be held with the vendor and the service provider to find the best time to schedule downtime and the upgrade. The manufacturer upgrade must have been tested to be compatible with their systems. FDA requirements stipulate that the upgrade must not make a substantive change to the device.

VHA facilities have internal checks to perform when upgrading an OS. We must check if there is an Environmental Risk Assessment (ERA) approved of the new OS and, if not, we must submit an ERA update request. This is reviewed to ensure it complies with the network security policy. If physical media like a USB drive is used, it needs to go through media scanning before it can be used on any upgrade. Any backups must be made and saved before performing upgrades, and once the upgrade is complete, tests need to be done to ensure the device is in operational order as well as communicating correctly with the network. This all takes labor and must be documented as devices work in the greater hospital system. It may seem exhaustive, but these are best practices to make sure that the OS upgrade doesn’t affect the hospital overall.
It is important to note that this whole process would only breathe new life into a legacy system rather than replace it. This is the last point I’d like to focus on, mainly because there is a new phenomenon: retiring devices due to their embedded operating systems. Some operating systems are built into devices and are not upgradable due to the design of the device. This is especially true for Internet of Medical Things (IoMT) devices, such as home-use patient monitors. Consider a device that is only seven years old; however, when purchased, it was with the Windows 7 operating system. Let’s assume the device is functional; in fact, it’s the physician’s preferred device. The only issue is that the operating system is out of support and the OEM has no upgrade options. In these cases, the only course of action is to fall back on routine security scans. Additionally, previous
articles covered how to isolate the unit through VLAN and ISE settings if applicable.
The bottom line is that an out-of-support OS is a death knell to a medical device. The unit needs to be replaced as soon as fiscally possible. If networked, the device is vulnerable to attacks and poses a security risk.
The bottom line is that Windows 10 is going away and that will cause us to update or replace existing devices. The process involves significant planning and compliance checks to ensure continued device operation and network security. There will be some devices that we can easily upgrade. Some devices, especially those with an embedded or non-upgradable OS, may have to be retired, particularly if they pose security risks. Proper network maintenance and security scans will help to extend the usage, but only temporarily. Ultimately, coordinating with OEMs is an essential step for managing the life cycle of these devices efficiently.


Garrett Seeley is a Biomedical Equipment Support SpecialistImaging with VISN 17: VA North Texas Health Care System, U.S. Department of Veterans Affairs.
Richard Thai is a Biomedical Engineer with VISN 17: VA North Texas Health Care System, U.S. Department of Veterans Affairs.

BY PHIL ENGLERT
In today’s interconnected healthcare environment, the cyber resilience of medical devices is inseparable from patient safety. As cyber threats increasingly target embedded systems and clinical networks, HTM professionals are on the front lines of safeguarding device integrity.
One of the most promising tools in this effort is the Software Bill of Materials (SBOM). Much like a parts list for software, an SBOM provides visibility into the components that make up a medical device’s software stack. For HTM teams, SBOMs offer a practical, actionable way to assess risk, streamline procurement, and respond to vulnerabilities ultimately supporting safer, more resilient care delivery.
An SBOM is a formal record of the software components, libraries, and dependencies that are included in a software product. For medical devices, this means knowing what open-source and proprietary code is embedded in the firmware, operating system, or application layer. SBOMs are machine-readable and standardized, enabling automated analysis and integration into cybersecurity workflows.
Two key use cases for SBOMs in HTM are procurement and vulnerability management. HTM teams can use SBOMs to evaluate the security posture of devices before purchase, identifying known vulnerabilities or unsupported components. Once devices are in the environment and new threats emerge (e.g., Log4j or OpenSSL flaws), SBOMs help quickly determine which devices are affected and prioritize mitigation.
The Manufacturer Disclosure Statement for Medical Device Security (MDS2) has long been a staple in HTM risk assessments. While the MDS2 outlines a device’s security
capabilities and configurations, it often lacks the granularity needed for software-level analysis. SBOMs complement the MDS2 by providing a detailed inventory of software components, enabling cross-referencing to known vulnerabilities via NIST’s National Vulnerability Database, assessing patching feasibility and vendor responsiveness, and informing compensating controls when direct remediation isn’t possible. Together, the MDS2 and SBOM form a more comprehensive picture of device risk, supporting informed decisions across the device life cycle.
To many in HTM, the concept of an SBOM may feel familiar. In fact, SBOMs are often compared to Material Safety Data Sheets (MSDS), which list the chemical contents and handling precautions for physical products. Just as an MSDS helps facilities manage chemical risks, SBOMs help manage software risks. Both documents promote transparency from manufacturers, enable informed handling and response, and support compliance with safety regulations. I like this analogy for bridging understanding across clinical engineering, IT and procurement teams.
For medical device manufacturers, SBOMs are no longer optional. In the U.S., Section 524B of the Federal Food, Drug, and Cosmetic Act, enacted under the 2023 Consolidated Appropriations Act, requires manufacturers to provide SBOMs as part of premarket submissions for cyber devices. The FDA’s final guidance (October 2023) mandates that SBOMs be included in submissions starting October 2024, with enforcement ramping up in 2025.
In the European Union, the Medical Device Regulation (EU MDR) also emphasizes cybersecurity and postmarket surveillance. While not SBOM-specific, the MDR’s focus on software life cycle management and risk mitigation aligns with SBOM principles.
These regulations underscore the need for HTM teams to understand and utilize SBOMs as part of their compliance and risk management strategies. During procurement, SBOMs can be used to screen for high-risk components like outdated libraries, compare vendors’ software hygiene and patching practices, and inform contract language around cybersecurity support. For example, a hospital evaluating two infusion pumps might find that one includes a deprecated Java library with known CVEs, while the other uses a more secure alternative. This insight can influence purchasing decisions and long-term support planning.
When a new vulnerability is disclosed, time is critical. SBOMs allow HTM teams to rapidly identify affected devices, coordinate with vendors for patches or mitigations, and document risk decisions for auditors and regulators. When the 2021 Log4j vulnerability crisis, organizations with SBOMs were able to quickly identify which devices used the affected library and take action. Those without SBOMs faced delays, uncertainty, and increased risk exposure.
Managing cyber risks through Software Bill of Materials (SBOMs) requires specialized tools for data quality evaluation and vulnerability correlation/prioritization because SBOMs are only as useful as the accuracy, completeness, and actionable insights they provide. SBOMs list software components, versions, and dependencies but not all SBOMs
are created equal. Tools are needed because SBOMs can contain hundreds or thousands of components and vulnerability databases are vast and constantly changing. Issues like incorrect metadata, ambiguous entries, or missing components undermine risk analysis and vulnerability tracking. Reliable SBOMs enable shared understanding of software risks across clinical, HTM and IT teams. Automated SBOM analysis is a cornerstone of scalable medical device cybersecurity.
For HTM professionals, SBOMs represent far more than a compliance checkbox, they’re a strategic lever for advancing patient safety and operational resilience. When embedded into procurement workflows, risk assessments, and vulnerability management, SBOMs empower HTM teams to proactively identify software risks, streamline coordination with IT and clinical stakeholders, and uphold the integrity of care environments. As cyber threats grow more sophisticated, pairing SBOMs with tools like the MDS2 becomes essential for sustaining secure, transparent, and trustworthy medical device ecosystems.

Phil Englert is the director of medical device security for Health-ISAC.


















Every vaporizer serviced by G.A.S. is fully refurbished, calibrated, and certified to meet stringent ISO 13485 standards — extending the life of your equipment without the cost of replacement.


6 Movement and body of laws
Process of facilitating operations without human intervention
Risk scoring ____(visual tools used in risk assessment and enterprise risk management) 12 Sequences of medical processes
Historical period
Medical title abbreviation
Testing environment in a computer system in which new or untested software can be run securely.
The words can appear horizontally, vertically, diagonally, and may be spelled forwards or backwards. 1. Inventory
Calibration
Compliance
Budgeting
Scheduling
Preventive
Reports 8. Audits
Upgrades
Training
Procurement
Goals
Maintenance
Mayra Becerra
CBET, Manager Clinical Engineering-Imaging at University of Miami
• Water
• Screwdrivers
• Pens
• Sticky Notes
• A mirror
Submit your bench to be featured in TechNation at 1technation.com/my-bench/. You could win a $25 Amazon gift card via the “What’s On Your Bench” Contest!

The New England Society of Clinical Engineering (NESCE) recently held its 2025 Northeastern Healthcare Technology Symposium, a premier event bringing together innovators, industry leaders, and healthcare professionals to explore the latest advancements in healthcare technology. The symposium featured expert speakers, interactive workshops and engaging panel discussions focused on transformative solutions that improve patient care, streamline operations and enhance health outcomes. Attendees networked with peers, explored the exhibit hall, shared insights and discovered cutting-edge tools that are shaping the future of healthcare.


1 3 4 2



5 6

DECEMBER 10
SPONSORED BY TOOLS OF THE TRADE

Save the date for this live webinar. Participation is eligible for 1 CE credit from the ACI.

SPONSORED BY Building a Cybersecurity Program Around Clinical Zero Trust: Strategies for Healthcare Resilience

CHECK OUT OUR ON-DEMAND PODCASTS AT 1TECHNATION.COM/ CATEGORY/PODCASTS

SPONSORED BY Standardize Your Testing

SPONSORED BY TOOLS OF THE TRADE FlowAnalyser PRO
All webinars, podcast, and product demos are eligible for 1 CE credit from the ACI.





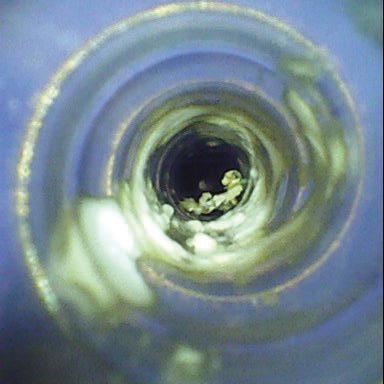



Ready for a borescope that offers partnership in every pixel?
Scan to get started.
From capturing detailed lumen images to building complete inspection workflows, Healthmark stands with you every step of the way. The Flexible Inspection Scope pairs precision optics with a full network of support—including a team that customizes implementation and training to ensure your success. Because when it comes to borescopes, it’s more than pixels that matter—it’s partnership.
Admar Neuro admarneuro.com • 728-900-3969
AMX Solutions amxsolutionsinc.com • 866-630-2697
BC Group bcgroupstore.com.com • 314-638-3800
FiberTech fibertechmedical.com • 866-628-6888
Interlight interlightus.com • 800-743-0005
Jet Medical jetmedical.com • 714-937-0809
Metropolis International metropolismedical.com • 718-371-6026
Nuclear Camera Services nuclearcameraservices.com • (630) 780-6363
Ozark Biomedical ozarkbiomedical.com • 800-457-7576
PM Biomedical pmbiomedical.com • 800-777-6474
Pronk Technologies, Inc. pronktech.com • 800-609-9802
Rytex Industries rytexindustries.com • 727-557-7450
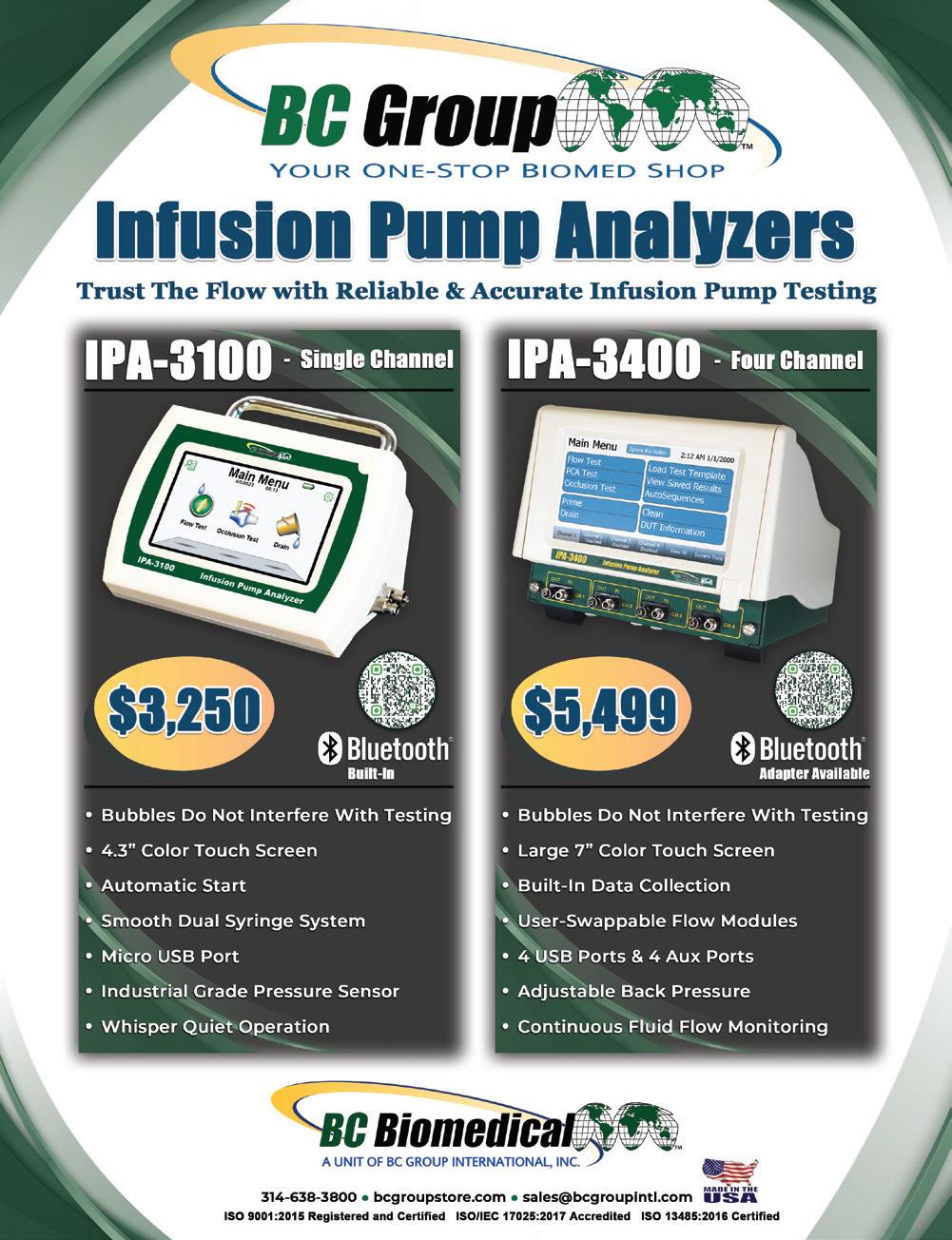
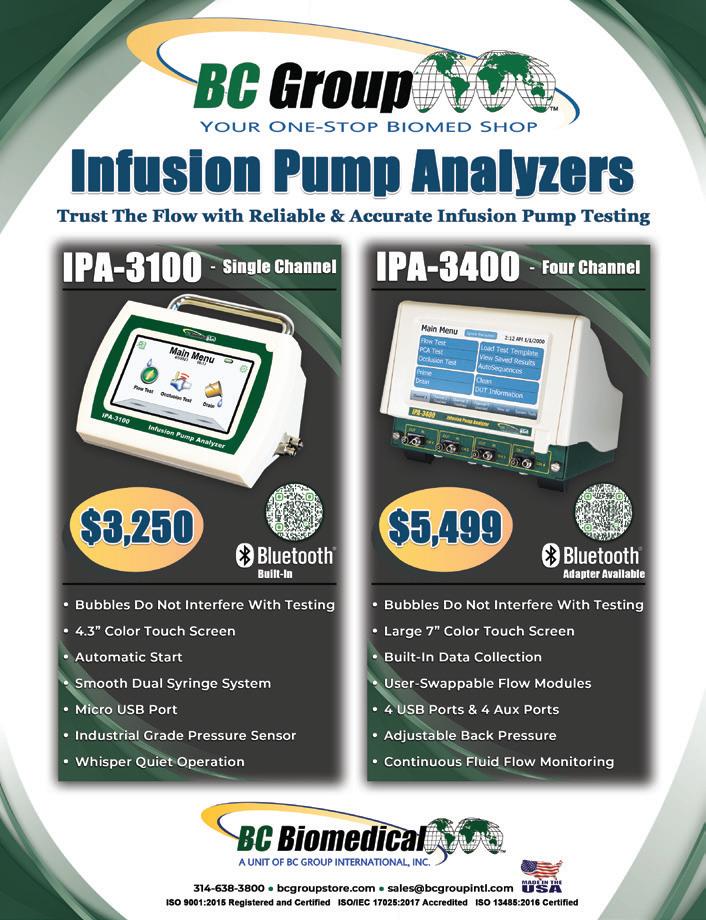
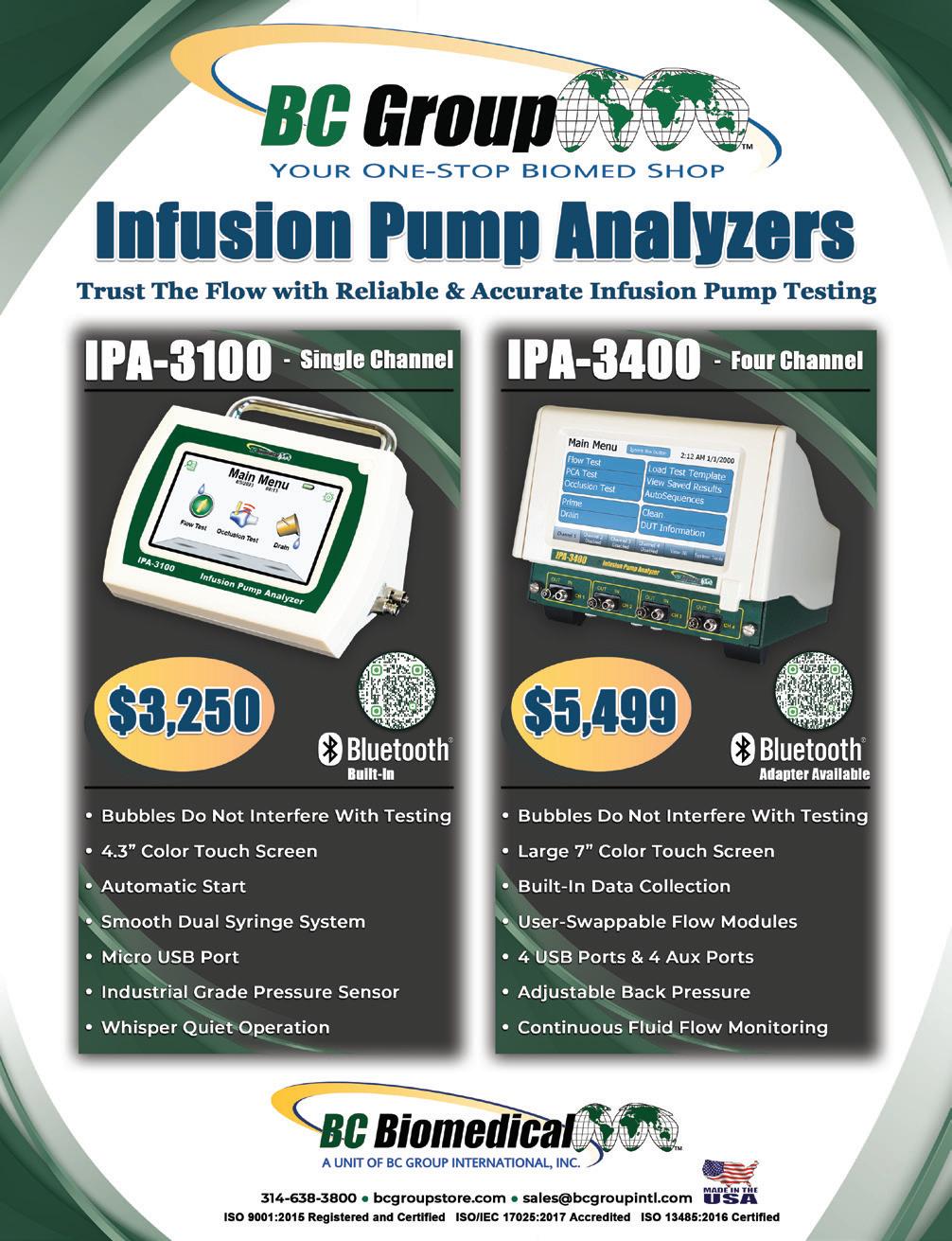










...Since you are still flipping through this magazine, it simply means you still have not found an honest, reliable, pre-owned imaging company that sells working systems. Well, Look No Further!




























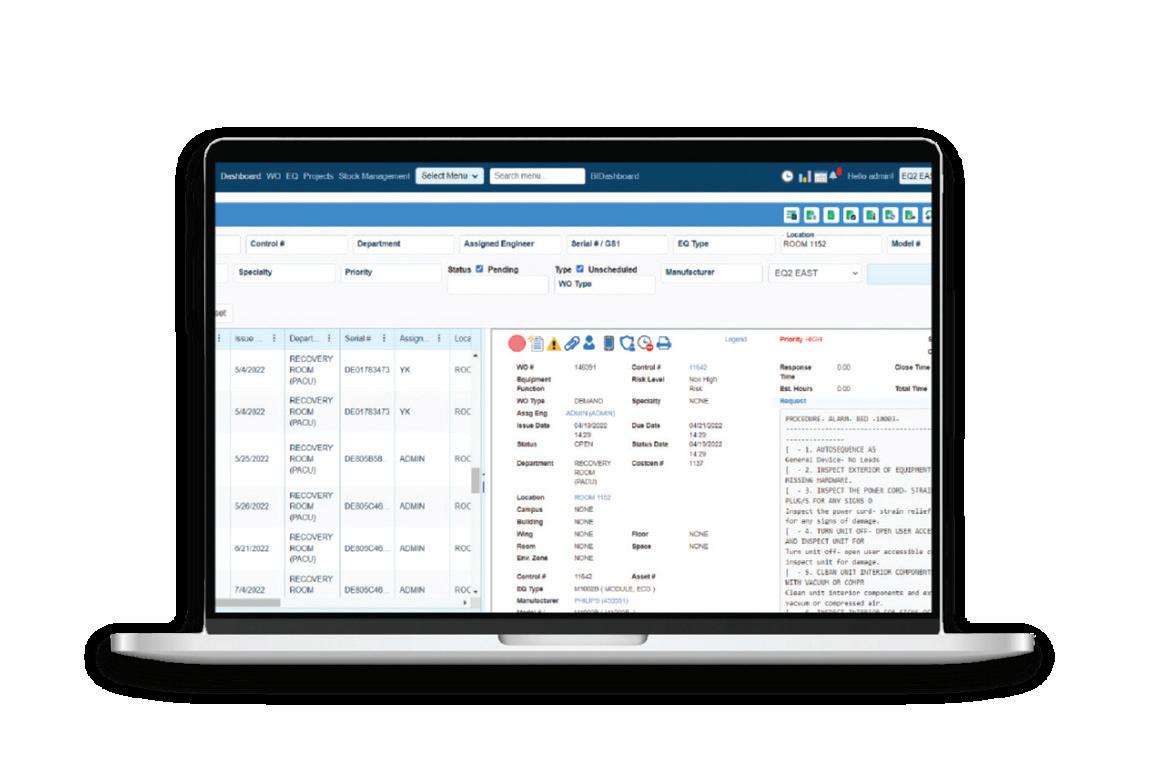
“EQ2 HEMS by TMA Systems is designed specifically for healthcare and the unique needs of HTM....(with) specialized workflows for managing medical equipment and advanced compliance tools and reports, including AEM program management and everything needed to be ready for the next survey.ˮ
Rich Sable,
Manager of Client Success

Innovatus Imaging innovatusimaging.com • 844-687-5100
International X-Ray Brokers internationalxraybrokers.com • 508-559-9441
Metropolis International, LLC Metropolismedical.com
Blender
Patient Monitors
AIV
BC Group International, Inc BCGroupStore.com • 314-638-3800
PM Biomedical pmbiomedical.com • 800-777-6474
Pronk Technologies, Inc. pronktech.com • 800-609-9802
Southeastern Biomedical, Inc sebiomedical.com/ • 828-396-6010
Tenacore LLC tenacore.com • 800-297-2241
USOC Medical usocmedical.com • 855-888-8762
Admar Neuro admarneuro.com • 728-900-3969 74
AMX Solutions
www.amxsolutionsinc.com • 866-630-2697 74
General Anesthetic Services generalanestheticservices.com • 800-717-5955 65
Innovatus Imaging innovatusimaging.com • 844-687-5100 8
Nuclear Camera Services nuclearcameraservices.co • (630) 780-6363 73
Rental/Leasing
General Anesthetic Services generalanestheticservices.com • 800-717-5955 65
Admar Neuro admarneuro.com • 728-900-3969 74
• 888-587-6759
AMX Solutions
www.amxsolutionsinc.com • 866-630-2697 74
BC Group International, Inc BCGroupStore.com • 314-638-3800 72,84
CM Parts Plus cmpartsplus.com • 877-267-2784
General Anesthetic Services generalanestheticservices.com • 800-717-5955 65
Innovatus Imaging innovatusimaging.com • 844-687-5100 8
International X-Ray Brokers internationalxraybrokers.com • 508-559-9441 64 Nuclear Camera Services nuclearcameraservices.co • (630) 780-6363 73 PM Biomedical pmbiomedical.com
Surgical
Test Equipment
BC Group International, Inc BCGroupStore.com • 314-638-3800
Tubes/Bulbs
X-Ray
AllParts Medical allpartsmedical.com
Solutions www.amxsolutionsinc.com
866-630-2697
service based parts provider that specializes in all imaging modalities and manufacturers. Created to offer hospitals and ISO’s a cost effective and time saving solution for ordering imaging replacement parts, equipment moves, ultrasound probe repair and on-site service.




TechNation cover articles addressed important topics in 2025

in just three easy steps!
1. Scan this QR code to visit 1technation.com/contest
2. Fill out our contest form and get bonus entries by uploading a photo from the past 15 years of
3. Enter to win a prize! Winners
page 26.







Popular TechNation features include the annual 40 under 40 and teh Top Tools Techs Want.



Brat a.k.a Bratwurst couldn’t miss the fun and excitement at the HTM Mixer Milwaukee.











Choose the right capital equipment, supplies, and health IT for your facility with guidance from ECRI Instituteʼs team of biomedical and cybersecurity engineers, clinicians, and human factors experts.



ECRI is a trusted authority on healthcare technologies that improve the quality and cost-effectiveness of patient care.
Get test results and ratings, free of vendor bias


Stay on top of risks with hazard and recall notifications
Compare technology with overviews and specifications
Learn more at www.ecri.org/solutions/device-evaluations or contact us today at 610-825-6000, x5891.