











































T. Reeves, MD, FAAP, DABOM
on the Line: Hepatocellular carcinoma in South Texas
Gabrielle Holliefield, MS, OMS-II; Thomas Althaus, OMS-II; and Ramaswamy Sharma, MS,
Reimagining Reconstruction: Developments in restorative surgery
Alyssa Francesca Ahorro, OMS-III; Bryanna Le, OMS-III; Camille Irene Hulipas, OMS-III; and Ramaswamy Sharma, MS, PhD................................................................................................................................26 When Peripheral Tolerance Brings Central Recognition: The
Kaeli Alpha, OMS-II; Blessina Babu, OMS-II; Karen Johns, OMS-II; and Ramaswamy Sharma, MS, PhD
Breakthrough Imaging Technology Debuts at UT Health San Antonio Center for Brain Health By Claire Kowalick
BCMS President’s Message By John Shepherd, MD, President, Bexar County Medical Society
Schutz,
PUBLISHED BY: Traveling Blender, LLC. 10036 Saxet Boerne, TX 78006
PUBLISHER: Louis Doucette louis@travelingblender.com
BUSINESS MANAGER: Vicki Schroder vicki@travelingblender.com
GRAPHIC DESIGNER: Jennifer Nelson jennifer@travelingblender.com
ADVERTISING SALES: AUSTIN: Sandy Weatherford sandy@travelingblender.com SAN ANTONIO: Gerry Lair gerrylair@yahoo.com
For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.
San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EDITORIAL CORRESPONDENCE:
Bexar County Medical Society 4334 N Loop 1604 W, Ste. 200 San Antonio, TX 78249
Email: editor@bcms.org
MAGAZINE ADDRESS CHANGES: Call (210) 301-4391 or Email: membership@bcms.org
SUBSCRIPTION RATES: $30 per year or $4 per individual issue
ADVERTISING CORRESPONDENCE: Louis Doucette, President Traveling Blender, LLC.
A Publication Management Firm 10036 Saxet, Boerne, TX 78006 www.travelingblender.com
For advertising rates and information Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national origin, or an intention to make such preference limitation or discrimination.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2025 SmithPrint, Inc. PRINTED IN THE USA

In This Season of Reflection, We Wish You Health and Peace in the New Year.

Insurance For Good reflects our ongoing commitment to physician well-being throughout the year, using surplus funds to provide Texas physicians and their families with meaningful resources beyond insurance coverage.
Anticipate Joy is one of the many benefits we’re honored to offer.
Through free, completely confidential, HIPAA-compliant online counseling, Anticipate Joy helps lighten life’s demands and makes mental health care simple to access. Every session with a licensed counselor is private, compassionate, and on your terms — whether by video, phone, or text, making it easier to find balance in everyday life.

We’d be glad to share more about the Anticipate Joy benefit and support your insurance needs. Our advisors are available at 1-800-880-8181, Monday through Friday, 8:00 AM to 5:00 PM CST, or learn more at tmait.org.









Clarity is the only nonprofit mental health treatment center for children (ages 3-17) in South Texas.
Our staff of children’s mental health professionals is the largest in the region thanks to an affiliation with the UT Health Science Center.
When a child is in crisis, we work with families to get them much needed treatment regardless of their ability to pay.
Our 8-acre campus in the South Texas Medical Center provides a full continuum of care. Additional partial hospitalization and outpatient services are available at our Southside High School location.
John Shepherd, MD, President
Lyssa Ochoa, MD, Vice President
Jennifer R. Rushton, MD, President-Elect
Lubna Naeem, MD, Treasurer
Lauren Tarbox, MD, Secretary
Ezequiel “Zeke” Silva, III, MD, Immediate Past President
Woodson “Scott” Jones, Member
John Lim, MD, Member
Sumeru “Sam” G. Mehta, MD, Member
M. “Hamed” Reza Mizani, MD, Member
Priti Mody-Bailey, MD, Member
Dan Powell, MD, Member
Saqib Z. Syed, MD, Member
Nancy Vacca, MD, Member
Luis O. Rohena, MD, Military Representative
Jayesh Shah, MD, TMA President
John Pham, DO, UIW Medical School Representative
Robert Leverence, MD, UT Health Medical School Representative
Cynthia Cantu, DO, UT Health Medical School Representative
Lori Kels, MD, UIW Medical School Representative
Ronald Rodriguez, MD, UT Health Medical School Representative
Alice Gong, MD, Board of Ethics Representative
Melody Newsom, BCMS CEO/Executive Director
George F. “Rick” Evans, Jr., General Counsel
Melody Newsom, CEO/Executive Director
Brissa Vela, Chief Membership & Development Officer
Yvonne Nino, Controller
Betty Fernandez, BCVI Director of Operations
Phil Hornbeak, Auto Program Director
Al Ortiz, Chief Information Officer
Jacob Hernandez, Advocacy and Public Health Specialist
Jennifer C. Seger MD, Chair
Timothy C. Hlavinka, MD, Member
John Robert Holcomb, MD, Member
Soma S. S. Jyothula, MD, Member
George-Thomas Martin Pugh, MD, Member
Adam Ratner, MD, Member
Rajam Ramamurthy, MD, Member
Patrick Reeves, MD, Member
John Joseph Seidenfeld, MD, Member
Amith Skandhan, MD, Member
Francis Vu Tran, MD, Member
Subhashini Valavalkar, MD, Member
Louis Doucette, Consultant
Brissa Vela, Staff Liaison
Gabriella Bradberry, Staff Liaison
Trisha Doucette, Editor
Ayomide Akinsooto, Student
Gabrielle Holliefield, Student
Rita Espinoza, DrPH, Volunteer
8535 Tom Slick San Antonio, TX 78229 claritycgc.org | 210-616-0300
Melissa Rosales, Volunteer
Ramaswamy Sharma, MS, PhD, Volunteer
Andrea Wazir, Volunteer












American Health Imaging offers up to 60% less than hospitals in-network with 99% of health with competitive rates to save your patients money – taking the guesswork out of what’s best for you and your patients.
for the medical insights you need, and
that matters for you and your patients, while giving patients
alternatives to
them time and money.

By John Shepherd, MD, President, Bexar County Medical Society
Sometimes the most meaningful seasons of life begin with a simple yes — the kind we offer before we fully understand what it will ask of us. My own “yes” came when I agreed to become the Bexar County Medical Society president. I didn’t know then how many doors it would open, how many lessons it would teach or how deeply it would connect me to this community. But I know now: this was my Year of Yes.
Saying yes to service strengthened our ties across San Antonio in ways that mattered. Yes to outreach meant deepening our connections with the broader community — partnering with organizations like San Antonio Medical Foundation, CASA, our military medical community and other local non-profits that share our mission to care, protect and uplift. Those relationships have built bridges between physicians and the people we serve, reminding us that medicine extends far beyond the clinic walls. When we show up in support of our community, our community shows up for us.
Saying yes to advocacy meant stepping forward, even when the issues were complex or the conversations uncomfortable. It meant calling legislators, attending hearings, and standing up for the values that define our profession. It meant collaborating with the Texas Medical Association and TEXPAC to move medicine forward — protecting patient access, preserving physician autonomy and ensuring that lawmakers truly understand what’s at stake.
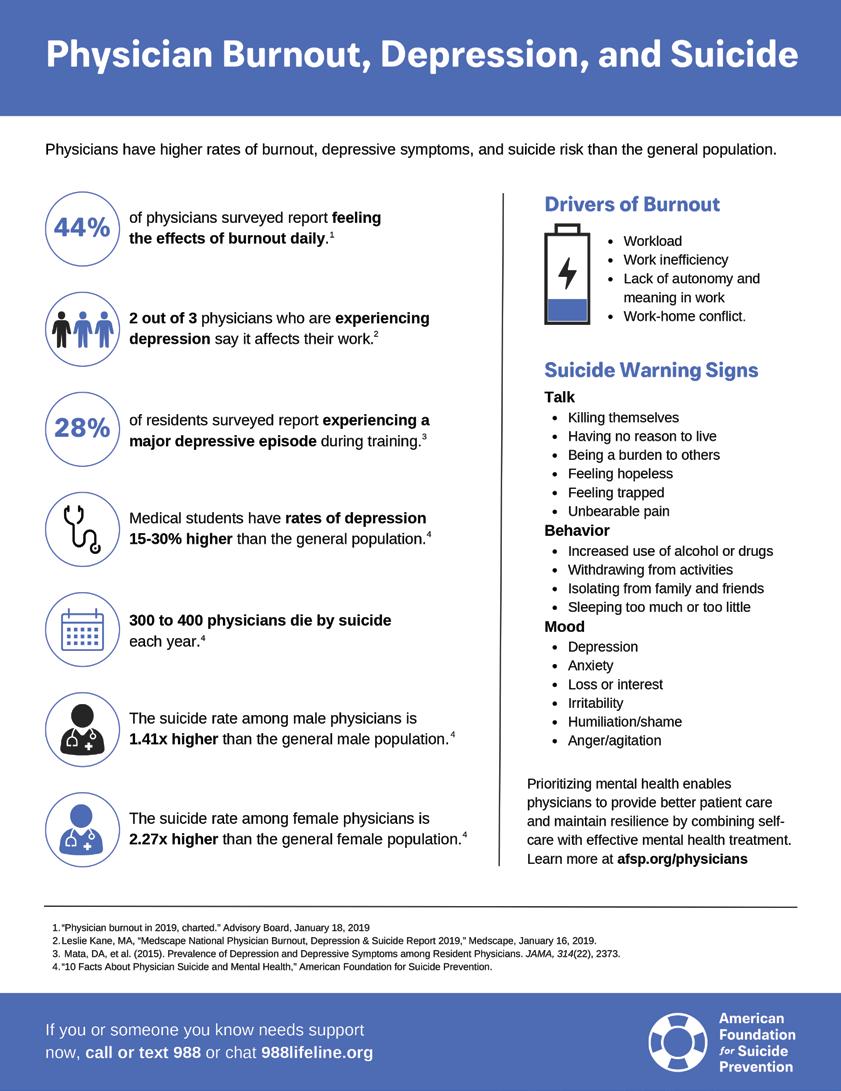
This year, advocacy looked like teamwork in motion. We worked tirelessly to address scope-of-practice issues, to champion physician wellness and to shine a light on the burdens that drive burnout. We reminded policymakers that protecting physicians and the practice of medicine means they are protecting patients. We said yes to being a steady, credible voice for science and compassion even when the headlines or hashtags attempted to tell a different story.
Advocacy didn’t always happen in the Capitol. Sometimes it was a conversation in a clinic hallway, a fundraiser, a text thread with colleagues or a thank you note to a legislator who listened. Each of those yeses, big or small, strengthened the foundation of organization medicine and built relationships that made progress possible.
Leadership isn’t about having all the answers. It’s about having the courage to say yes, and humble enough to learn from what happens next. " "

Saying yes also meant saying yes to growth. Leadership isn’t a comfortable place; it’s a classroom that never stops testing you. There were moments this year that challenged me — to see differently, to listen longer, to lead with both firmness and grace. But every challenge brought a lesson, and every lesson deepened my respect for the people who make BCMS what it is.
We said yes to innovation — to new ways of engaging members, to fresh ideas from early-career physicians to technology that helps us connect in smarter, more inclusive ways. We said yes to mentorship, to celebrating our students and residents, and to recognizing the voices that will carry medicine into its next era. Growth doesn’t happen by accident; it happens when people keep showing up and saying yes, even when they’re unsure of what comes next.
And we said yes to gratitude — to celebrating the countless volunteers, committee chairs and staff who keep the wheels turning behind the scenes. Their quiet dedication makes every visible success possible.
Of all the yeses this year, the most meaningful may be the ones shared with the family of medicine — the spouses, partners and loved ones who make it possible for us to do what we do. They are the steady voices of encouragement when the OR calls at 2 a.m., the hands that sometimes hold everything together during call weekends, the hearts that remind us that medicine is both a profession and a shared life.
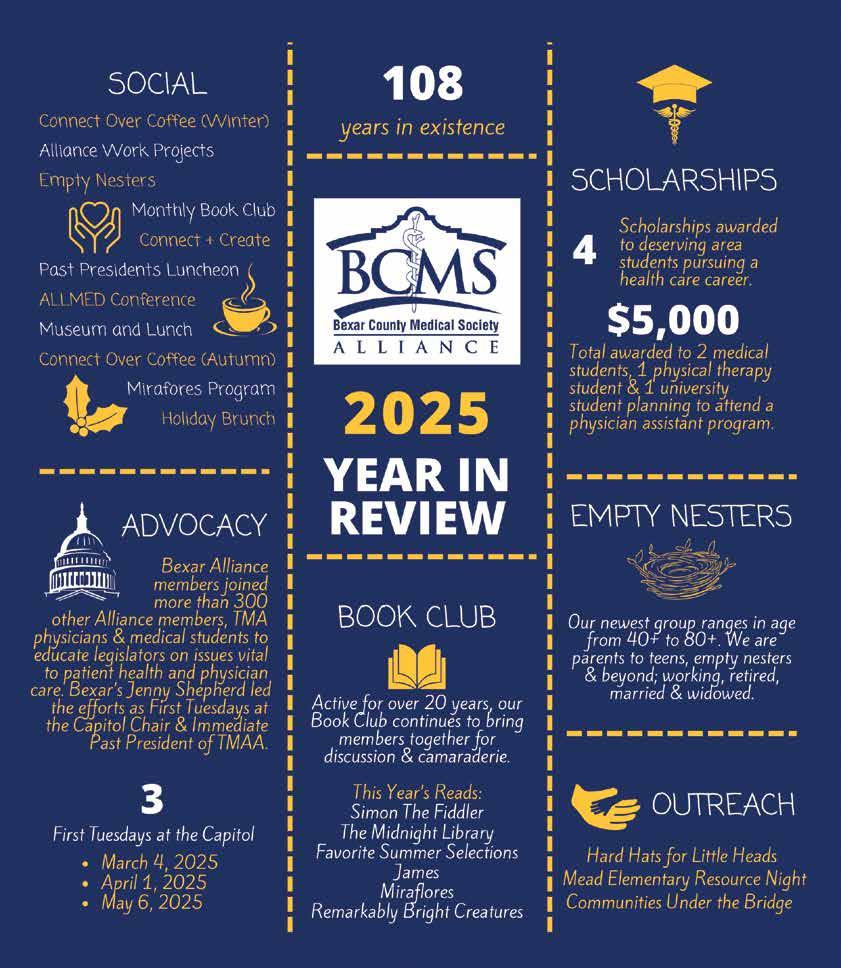
Our physician families, and the BCMS Alliance, have been powerful partners in outreach, advocacy and community service. They help to humanize the issues we fight for and are often the non-clinical face of medicine in our communities. Through their work in Bexar County, they bridge the space between medicine and the community it serves, extending the reach of medicine beyond the hospital corridors and clinic walls.
Looking back on this year as president, every step forward started with that single choice — to say yes. Yes to showing up. Yes to helping. Yes to believing that change is possible.
“The Year of Yes” wasn’t about overcommitting or saying yes to everything but it was about being open. Open to new connections, new collaborations and new ways of leading. It was about trusting that the right yes can result in positive growth that you can’t always predict.
Leadership has a way of revealing what you’re made of and, just as important, who stands beside you. What I’ve seen this year is a profession defined by generosity, courage and care. A community of physicians who continue to say yes to what matters most: their patients, their peers and the calling of medicine itself.
"Progress in medicine always starts with that simple word — yes — spoken by people who believe that we can do better.
As this chapter closes for me, I hope our Society continues to say yes — yes to service that strengthens our city, yes to advocacy that protects our profession, yes to mentorship that nurtures the next generation and yes to compassion that keeps us human.
Medicine will always face challenges. Some of those challenges will be new and some familiar, but this community has shown me that the power of yes can meet them all because saying yes isn’t just optimism — it’s about belief. Belief that our voices matter, our actions matter and the progress in medicine always begins with people willing to lean in instead of stepping back.
I began this year unsure if I was ready. I end it certain that every “yes” was worth it. So, here’s to the next chapter — to the leaders who will carry the torch forward, and to a community that continues to answer the call with vision, integrity and purpose. May we always have to courage to say yes: to each other, to our patients and to the future of medicine.
John Shepherd, MD, 2025 President of the Bexar County Medical Society and TEXPAC Chair, has been an active advocate for the Family of Medicine at the Texas State Capitol and has held several “Party of Medicine” events, introducing physicians on how to get involved with legislation that affects medical issues. He has been Chief of Surgery at Christus Santa Rosa Children’s Hospital and a past member of the Board of Directors of Tejas Anesthesia. Dr. Shepherd is currently a Pediatric Anesthesiologist with University Medical Associates, and serves on the BCMS Legislative Committee and the Bexar Delegation to TMA.



By The SAFARI Research Group

At the turn of the century and well into the early 2000s, headlines describing an “obesity epidemic” have reflected a growing concern among medical, public health and research communities, policy makers and the public. In San Antonio, meanwhile, three landmark research studies from some of our esteemed research institutions were busy cataloging health challenges, including obesity, within large local Mexican American families: the San Antonio Family Diabetes/Gallbladder Study, the San Antonio Family Heart Study and the Veteran Administration Genetic Epidemiology Study. Obesity and childhood obesity were/are major public health challenges, locally and globally. And as the headlines have accurately indicated, the prevalence rates of overweight and obesity in children have risen globally in recent decades. Behind the headlines, however, is an inconvenient truth about obesity: it often clusters with cardiometabolic risk traits like insulin resistance, hyperglycemia, dyslipidemia and hypertension to represent the metabolic syndrome, a strong predictor of cardiovascular disease and type 2 diabetes. Unfortunately, childhood obesity in the U.S. is marked by remarkable gender, population and ethnic differences, and it is associated with immediate and long-term adverse health outcomes and quite possibly a shortened lifespan. With this health specter looming in the background in the early 2000s, and to address the knowledge gap regarding the relationship between childhood obesity and the metabolic syndrome, a genetic epidemiological study called the San Antonio Family Assessment of Metabolic Risk Indicators in Youth (SAFARI) Study was conceived. To acknowledge the 20-year anniversary of our first study participant in late 2005, we will present some very eye-opening findings about the children of our community who visited the Texas Diabetes Institute for their SAFARI Study clinic appointments between 2005 and 2010.
Selected Demographic and Cardiometabolic Risk Profiles of 670 SAFARI Non-Diabetic Study Participants
*6 components of MS; MS was defined as presence of ≥3 of the 6 dichotomized cardiometabolic risk traits; #HDL-C: High-density lipoprotein cholesterol.
The 670 non-diabetic SAFARI Study participants are children or biological relatives, aged 6 to 17 years, of adult participants from the three aforementioned studies. Extensive family history, demographic, phenotypic, genotypic, behavioral and environmental data were obtained from SAFARI Study participants and their parents/ guardians. Disturbingly, the SAFARI Study confirmed that our community was not immune from the national and global trends of highrisk health outcomes. 52.7% of the youth in the SAFARI Study were overweight, 33.6% were obese and 18.7% of them exhibited metabolic syndrome (the SAFARI definition is based on six components). The prevalence rates of these six components ranged from 11.9% (high blood pressure) to 31.9% (low HDL-cholesterol).1 While the rate of pre-diabetes (measured as impaired fasting glucose or impaired glucose tolerance or both) in SAFARI children was 13.2%, it was about 31% in children who were considered having metabolic syndrome. Although only about 1% of normal-weight children had metabolic syndrome, its prevalence rose dramatically with increasing levels of obesity. For example, among the 65 children in the study who were severely obese, more than two-thirds had already developed metabolic syndrome. Although it would be convenient if one or two genes were responsible for prediabetes or obesity, or if there was one on/off switch, we know this is not a reality for these cardiometabolic risk traits. We do know that over the last 20 years, the “genetics” part of this study has become increasingly important in our discovery process and led to some impactful findings as well. For instance, several of the cardiometabolic risk traits were found to be under strong additive genetic influences (that is the cumulative effects of multiple genes) — the metabolic syndrome in this cohort had a genetic influence of 68%, and obesity had a genetic influence of 78%. In another example, the SAFARI Study found that acanthosis nigricans is a composite marker of childhood obesity and insulin resistance and their complex interactions with other cardiometabolic risk traits.2
In addition to genetic factors, numerous environmental factors have been found to influence variation in childhood obesity and the related cardiometabolic risk traits, including chemical (e.g., exposures to organic chemical pollutants and heavy metals) and nonchemical factors (e.g., socioeconomic status, lifestyle behaviors [diet and physical activity], family and social stressors, and community stressors) and their complex interactions. Some of these findings that have been published (and one soon-to-be published) include examining the influence of such environmental factors on childhood obesity risk:
• Gene-by-Environment Interaction Influences on Childhood Obesity and Cardiometabolic Risk (“Go outside and play!”): We looked at environmental or lifestyle behavioral factors of sedentary activity and physical fitness, and significant gene x sedentary activity interactions were found to negatively influence BMI (Body-mass-index), waist circumference, fasting insulin, the Homeostasis Model Assessment for Insulin Resistance (also known as HOMA-IR), the number of metabolic syndrome components and HDL-cholesterol. Significant gene x physical fitness interactions were found with BMI, waist circumference, fat mass
and HOMA-IR. These findings provide evidence of the interplay with genetic factors and the lifestyle factors of sedentary activity and physical fitness vs. variation in cardiometabolic risk traits.3
• Impact of Serum Carotenoids, Biomarkers of Fruit and Vegetable Intake, on Childhood Obesity and Cardiometabolic Risk (“Eat your fruits and vegetables — part 1!”): Selected carotenoids (e.g., α and β carotenoids — found in yellow, orange and red fruits and vegetables and leafy greens) were measured and their associations with cardiometabolic risk traits were assessed. Serum α-carotene and β-carotene were found to be inversely correlated with obesity measures and triglycerides, and positively correlated with HDL cholesterol. These data reveal that low intake of fruits and vegetables is associated with increased cardiometabolic risk in SAFARI children.4,5
• Impact of Neighborhood Income on BMI via Serum Carotenoids (“Eat your fruits and vegetables — part 2!”): When neighborhood income was estimated using 2010 Census data, it was found to be negatively associated with BMI and HOMAIR. Using a mediation analysis, the median household income per block group was found to be a direct determinant of BMI with an inverse relationship. The median income was positively associated with serum α- and β- carotenoid levels, but they were inversely associated with BMI. All associations examined were statistically significant. These findings imply that the fruit and vegetable intake of SAFARI children in poorer neighborhoods is insufficient, in turn increasing the risk of childhood obesity (soon to be published).
• Early-life Exposure to Organic Chemicals and Cardiometabolic Risk — A Pilot Study (“Be careful what you put in your body!”): A pilot study involving 25 SAFARI Study children was conducted to assess the extent to which exposure to organic chemicals influences childhood obesity or cardiometabolic risk traits, using deciduous teeth collected from these children as a source of biomarkers of early-life exposures. The chemical contents found in these “baby teeth” would serve as a proxy of exposures to low levels of organic chemicals during early life, including the critical periods of pre-, peri- and post-natal development. Significant positive correlations were found between certain phthalates (chemicals found in plastics in a variety of consumer products, from food storage containers to toys to personal care items) and fat mass, fasting insulin and HOMA-IR, and one phthalate exhibited a negative correlation with blood pressure measures. Further, acetaminophen (APAP) exhibited a significant negative association with HDL cholesterol and a significant positive association with the liver marker alanine transaminase.4
We initiated the SAFARI Study to assess the burden of childhood obesity and its associated cardiometabolic risk in the San Antonio Mexican American community to eventually identify potential opportunities to develop early childhood intervention strategies to prevent or reduce the disease risk later in life, contribute to lifelong well-being, and to identify and characterize specific genetic markers with relevance to targeted personalized treatments. One major benefit over the years with this study was realizing that there is no "one-size-fits-all" approach to address the burden of childhood obesity; with increasing advances
in technology and medical information, the use of multi-omics data and their integration are necessary to unravel the molecular basis of these complex relationships and are critical for the development of “precision” disease prevention, cure and reduction in childhood obesity and associated cardiometabolic risk.
To meet the study objectives, we continue to conduct studies/ analyses focused on genetic and environmental determinants of these health conditions over the years. Several ongoing studies are examining the role of additional risk factors associated with childhood obesity, and a few papers are in the pipeline for this year/early next year. For example, we are examining the impact of a mother’s lifestyle factors during pregnancy (e.g., soda intake) on a child’s disease risk as well as identification of novel biomarkers of childhood obesity such as leucine-rich alpha-2-glycoprotein 1 [LRG1].7,8 A major ongoing activity is to translate and disseminate our study findings into easily understandable ways for the public, including our SAFARI Study participants, to ensure that such knowledge can lead to disease prevention and improved health outcomes. A practical and comprehensive disease prevention approach can be achieved through community engagement by mobilizing community members, community-based organizations, healthcare professional institutes, governmental and other non-governmental organizations. Indeed, a recent funding award this year from the Texas Higher Education Coordinating Board’s Minority Health Research and Education Grant Program will enable the SAFARI investigators — here at Texas A&M University-San Antonio and with our collaborators across the state — to identify molecular mechanisms underlying the connection between early-life environmental exposures and childhood obesity as well as cardiometabolic risk. The funding will also support the implementation of effective evidence-based interventions for high-risk individuals through community engagement. It is hoped that with this recent award from the Texas Higher Education Coordinating Board and the proposed community engagement initiatives, it will bring the SAFARI Study full circle. Having already produced numerous high-impact scholarly manuscripts, significant scientific presentations and the training of many students and post-graduates, the SAFARI Study is now poised to directly give back to our community. Our research findings have provided, and will continue to provide, actionable health benefits to the families involved and community at-large and inform the healthcare providers. The SAFARI Study would not have been possible without the kind support from its participants and their parents/guardians, and we are deeply indebted to their enthusiasm and generosity.
References:
1. Fowler, S.P. et al., Hum Genet. 2013 Sep;132(9):1059-71. doi: 10.1007/s00439-013-1315-2
2. Lopez-Alvarenga, J.C. et al., PLoS One. 2020 Oct 15;15(10):e0240467. doi: 10.1371/ journal.pone.0240467
3. Arya, R. et al., Genet Epidemiol. 2018 Jun;42(4):378-393. doi: 10.1002/gepi.22114
4. Farook, V.S. et al., Am J Clin Nutr. 2017 Jul;106(1):52-58. doi: 10.3945/ajcn.116.144006
5. Mummidi, S. et al., Sci Rep. 2021 Jan 13;11(1):871. doi: 10.1038/ s41598-020-79387-8
6. Farook, V.S. et al., International Journal of Environmental Research and Public Health. 2025; 22(10):1494. https://doi.org/10.3390/ ijerph22101494
7. Reyna, A.R. Master's thesis, The University of Texas Rio Grande Valley, 2024]. ScholarWorks @ UTRGV. https://scholarworks.utrgv. edu/etd/1478
8. Reyna, A. et al., 2024 Obesity Week, 42nd Annual Meeting of The Obesity Society at Obesity week, San Antonio, Texas November 3-6, 2024 (Poster-400)
Texas A&M University-San Antonio, San Antonio, Texas: Roy Resendez, MA; Jennifer Schneider, PMP; Rector Arya, PhD; Srinivas Mummidi, DVM, PhD; Donna M. Lehman, PhD; Bryan Bayles, PhD; Hemant Kulkarni, MD; Ravindranath Duggirala, PhD (Principal Investigator, SAFARI Study); Texas A&M University Institute for Genome Sciences and Society, College Station, Texas: Jun Fan, PhD; Texas A&M School of Public Health, College Station, Texas: Vijay Golla, MBBS, PhD, MPH; University of Texas Health San Antonio and University Health System (Texas Diabetes Institute), San Antonio, Texas: Sharon P. Fowler, PhD; Suman Challa, BDS, MSPH; Lily Q. Dong, PhD; Jane L. Lynch, MD; Ralph A. DeFronzo, MD; Southwest Research Institute, San Antonio, Texas: David E. Camann, MS; The Health Collaborative, San Antonio, Texas: Elizabeth Lutz, MBA; University of Texas Rio Grande Valley, Brownsville and Harlingen, Texas: Juan Carlos Lopez-Alvarenga, MD, DSc, PhD; Doreen D. Garza, MPH; David Salazar, MS; Vincent Diego, PhD; Marcio Almeida, PhD; Joanne E. Curran, PhD; John Blangero, PhD; Pennsylvania State University, Hershey, Pennsylvania: Daniel E. Hale, MD; Pennsylvania State University, University Park, Pennsylvania: Jairam KP Vanamala, PhD; Purdue University, West Lafayette, Indiana: Lavanya Reddivari, PhD.
Funding Support: National Institutes of Health, Veterans Administration, USDA National Institute of Food and Agriculture, AT&T Foundation (Genomics Computing Center, Texas Biomedical Research Institute), Voelcker Foundation, Baptist Health Foundation, Texas Higher Education Coordinating Board’s Minority Health Research and Education Grant Program and Fraternal Order of Eagles San Antonio Aerie and Auxiliary.



The Bexar County Medical Society is committed to helping our members find personal balance and improve general well-being.

BCMS Physician Wellness Program
Resources and services provided to help BCMS members maintain a healthy and well-balanced lifestyle through confidential counseling, educational resources, local events, webinars and more.


A BCMS provided resource for physician members who seek counseling from Texas-licensed professionals, discretely and confidentially through BetterHelp. Free 30 days counseling.

Wellness Coaching Webinars & Events
Nora Vasquez, MD, an Internal Medicine Doctor and Advanced Certified Physician Coach, helps physicians and healthcare professionals overcome burnout so that they can lead with joy and confidence while creating a more harmonious work-life balance that is fulfilling!

Utilize our free Find a Doc service when looking for a new physician. Our members can be found by the specified tabs provided to narrow down your preferred physician.
Physician Support Line (888) 409-0141
Psychiatrists are available to help physicians and medical students navigate the balance of a personal and professional life. Free, confidential and anonymous. No appointment necessary. Call for any issue, not just a crisis.

Physician Coach Support

Free Confidential Physician-to-Physician support line. A group of volunteer physicians using their own personal development skills and life coaching certifications to support other physicians!

Physician Health & Rehabilitation Program
Confidential advocacy group of BCMS physicians that identify and facilitate recovery success for physicians with substance use disorder (Alcohol and/or Drugs) and depression, through support and monitoring.
Please scan QR code for more information and available resources for BCMS Members


By Sara Hamilton, PsyD
It is 11:37 p.m. Anna is in her favorite spot on the couch and isn’t loving this TV show. She wanders to the fridge, then the pantry. A bite of this, a bite of that, until she settles on making nachos … the sad, microwaved kind. On the counter are the bags that contained the burgers and fries her husband brought home for them all, the only meal she had today. A leftover grilled cheese crust, lots of coffee, half a warm protein shake, and some soggy cheerios from the sticky, insistent hands of her toddler were all that made it into her stomach today otherwise. She eats the nachos in front of the TV and stops when there are none left, leaving her mind quiet and her stomach uncomfortable.
How did she get here?
After waking up late (someone stayed up doomscrolling and watching too many Tiktoks!), chugging coffee, and rushing the crew out of the house this morning, Anna had missed her dose of her ADHD meds. At 3:00 p.m., when her older kids wanted their afterschool snack, she realized she hadn’t eaten. She had been in “the zone” on a home renovation project (definitely not her project for work that is due in two days. She’ll do that tomorrow!) and the time had flown by. Anna shrugged it off because she rarely eats a real lunch anyway — her meds make it so she isn’t hungry. As they settle in to do homework, she loses track of time.
When the kids complain that they are hungry (again??), she realizes she has no idea what to make for dinner, the produce she bought last week has gone bad and the idea of figuring this all out overwhelms her. She asks her husband to pick up food on his way home from work and to get “something bad” since she hasn’t eaten all day and “can get away with it.” He arrives, her favorite Whataburger order in hand, because he knows how she gets when she is hungry. After the bedtime routine, her husband goes to bed, and she stays up to have some quality time for herself.
Anna’s day is not an unusual one for people with Attention-Deficit Hyperactivity Disorder (ADHD). In ADHD (and other mental health conditions as well as various cognitive conditions), executive functioning is impaired, which can make it difficult to engage in heathy eating behaviors for a variety of reasons. Executive functions are top-down mental processes required when operating on automatic — instinctual or intuitive processes are impossible or unlikely to be successful.1 They include the following:
• Working Memory: Taking in new information, integrating it with existing knowledge and utilizing that information; planning, self-monitoring, problem-solving.
• Inhibitory Control: Focus, verbal and motor behaviors, prioritizing, emotional intensity/expression, task initiation, attention, concentration, screening out irrelevant stimuli.
• Cognitive Flexibility: Problem-solving, shifting between tasks, empathy, creativity.
These skills are very important in engaging in healthy eating behaviors, particularly in an environment where we have so many things competing for our attention. Those with ADHD and other conditions that impair executive functioning are more likely to consume ultra-processed foods (UPF) and less likely to consume
produce and other nutrient-dense foods.2,3 Western diets (defined generally as including ultra-processed animal products and overall containing high amounts of carbohydrates and fat) are associated with impairment in and faster declines of executive functioning, independent of weight gain and adiposity.4,5 Therefore, those who are most vulnerable to eating large amounts of processed foods are at risk of then further increasing their intake due to the impact of the foods themselves. This makes it increasingly difficult for people to reduce their intake once they have established a pattern of frequent UPF consumption.
• Budgeting for meals/groceries
• Meal planning
• Reading nutrition labels and applying the information
• Cooking multi-dish meals
• Remembering to bring the lunch you packed to work
• Eating a wide variety of foods
• Eating slowly
• Remembering what you ate earlier
• Completing food journals
• Calculating carbs for diabetes management
• Portion control
• Eating when hungry, due to poor ability to detect subtle levels of hunger
• Stopping when full when larger portion sizes are available
• Resisting available food when not hungry
• Resisting sales on food
• Saying no to “food pushers” who encourage them to eat
• Resisting cravings
• Eating for stimulation/dopamine
• Externally-prompted eating
• Consuming narrow variety of foods
• Fast food consumption
• Grazing/snacking
• Skipping meals
• Overeating
• Binge eating
• Purging
• Eating only when very hungry
• Eating until very full
• Buying fresh food that then goes bad due to forgetting to use it
• Emotional eating
• Binge drinking
• Fad diets
• All-or-nothing and black-and-white thinking about dieting (ex: “good” vs. “bad” foods)
• Frequency and intensity of cravings and difficulty resisting them
There are several factors to consider in the primary care setting where providers are often treating mental health concerns, including ADHD, and making recommendations for diet and nutrition. ADHD in adults has increased since the pandemic. Between 2019 and 2023, prescriptions for ADHD meds rose by 23.8%, primarily in young adults and women. Many practitioners are likely seeing and treating more people with ADHD than ever before as a result.6
Because many mental health issues can present with executive functioning deficits, it is important to make an accurate diagnosis. Screening for depression, anxiety and ADHD using the PHQ3, GAD7 and Adult ADHD Self-Report Scale, respectively, can be done quickly with these easily administered tools. If treating with medication, prioritizing treating ADHD first can address co-morbid depression and anxiety; when the patient can function better in their daily life, their overall mental health is likely to improve as their outlook about future functioning brightens and they have fewer daily negative consequences. However, ADHD medications have their own risks regarding eating behaviors. These medications often suppress appetite, which can contribute to undereating, grazing and compensatory overeating at meals. These medications can also negatively impact sleep, which may increase appetite and weight. Despite appetite suppression, these medications can improve executive functioning in a way that may reduce risk of aforementioned behaviors and increase ease of engaging in healthy behaviors.
To determine impact of any executive functioning impairments on eating habits, it can be helpful to ask patients to complete a 24-hour food recall and note any deficits in variety of foods consumed, cooking abilities, consistency of food intake and intake of fresh foods. Rather than directing patients to simply “diet and exercise,” encourage them to increase variety of food consumed, eat meals regularly, consume more fresh foods (if available to them), and work to improve cooking abilities with fresh ingredients (available through https://www.chefsa. org/ and https://safoodbank.org/communitywellness/). If deciding whether to remove a patient from an ADHD medication to start a weight loss medication, consider that removing their ADHD medication may make it more difficult for the patient to engage in necessary behaviors to support the results of a weight loss medication and may make a negative outcome (malnutrition, etc.) more likely.
Patients are also likely to benefit from referrals to dietitians who can help them to improve their nutrition and health even if the client’s weight does not change. Dietitians can help those who tend to think in very strict diet terms to engage in more sustainable behaviors to reduce risk of weight regain after fad dieting. Dietitians can also counsel patients on sustainable movement habits.
A reminder not to emphasize willpower or motivation, as these are not the issues contributing to any eating struggle. Those with ADHD are already likely to blame themselves and this message would further reinforce narratives that discourage effective action rather than enhance it. Encouragement of sustainable habits and specific recommendations will go a long way in helping clients with ADHD to make progress in engaging in healthier eating habits.
References:
1. Diamond, A. (2013). Executive functions. Annual Review of Psychology, 64, 135–168. https://doi.org/10.1146/annurevpsych-113011-143750 PubMedAnnual Reviews
2. Favieri, F., Tambelli, R., Chen, E., & Casagrande, M. (2024). Self-Regulation in Eating Behaviors: The Role of Executive Function in Response to Food Stimuli. Nutrients, 16(14), 2318. https://doi. org/10.3390/nu16142318
3. Wyckoff, E.P., Evans, B.C., Manasse, S. M., Butryn, M.L., & Forman, E.M. (2017). Executive functioning and dietary intake: Neurocognitive correlates of fruit, vegetable and saturated fat intake in adults with obesity. Appetite, 111, 79–85. https://doi.org/10.1016/j. appet.2016.12.039
4. Attuquayefio, T., Stevenson, R.J., Oaten, M.J., & Francis, H.M. (2017). A four-day Western-style dietary intervention causes reductions in hippocampal-dependent learning and memory and interoceptive sensitivity. PloS one, 12(2), e0172645. https://doi. org/10.1371/journal.pone.0172645
5. Gomes Gonçalves N, Vidal Ferreira N, Khandpur N, et al. (2023). Association Between Consumption of Ultraprocessed Foods and Cognitive Decline. JAMA Neurol. 80(2):142–150. doi:10.1001/ jamaneurol.2022.4397
6. Huskamp, H.A., Busch, A.B., & Frank, R.G. (2025). Recent Trends in Medication Treatment for Attention-Deficit Hyperactivity Disorder. Psychiatric services (Washington, D.C.), appips20240574. Advance online publication. https://doi.org/10.1176/appi. ps.20240574

Sara Hamilton, PsyD, is a licensed clinical psychologist and the clinical director of the Bariatric Counseling Center.

By Patrick T. Reeves, MD, FAAP, DABOM
Metabolic dysfunction associated steatohepatitis, or MASH (formerly nonalcoholic steatohepatitis), has emerged as one of the most pressing challenges in modern primary care. Once viewed as a benign finding of “fatty liver,” this disease is now recognized as a major cause of cirrhosis, hepatocellular carcinoma and the leading indication for liver transplantation in women in the United States. Its rise parallels the epidemic of obesity, insulin resistance and metabolic syndrome, conditions that frontline clinicians encounter daily. Fortunately, the past five years have transformed our therapeutic landscape. Two interventions, glucagon-like peptide 1 receptor agonists (GLP 1 RAs) and metabolic bariatric surgery, have demonstrated powerful potential not just to induce weight loss but also to reverse the inflammatory and fibrotic processes that define MASH.
The Weight - Liver Connection
The pathophysiology of MASH centers on insulin resistance, lipotoxicity and chronic inflammation. Excess adipose tissue, partic-
ularly visceral fat, drives hepatic fat accumulation through free fatty acid flux and altered adipokine signaling. Over time, this metabolic overload promotes oxidative stress, hepatocyte ballooning and fibrogenesis. Traditional approaches, including caloric restriction, exercise and control of diabetes and dyslipidemia, remain foundational, yet they often fall short in achieving the 10 to 15% sustained weight loss typically required for histologic remission. This gap has made pharmacologic and surgical weight loss strategies critical allies in managing MASH.
GLP 1 receptor agonists such as semaglutide, liraglutide and tirzepatide were initially designed to improve glycemic control in type 2 diabetes. Their benefits soon extended beyond the pancreas. By enhancing satiety, delaying gastric emptying, and improving insulin sensitivity, they promote consistent, clinically meaningful weight loss. More importantly, they exert direct anti-inflammatory and antifibrotic effects on hepatic tissue.
A pivotal phase 2 trial published in The New England Journal of Medicine evaluated semaglutide 0.4 mg daily in adults with biopsy confirmed NASH. The study found NASH resolution without worsening fibrosis in 59% of participants compared with 17% in the placebo group.1 Subsequent analyses have reinforced these findings: GLP 1 therapies consistently reduce hepatic steatosis on MRI PDFF, improve transaminases and, in some patients, regress fibrosis stage.
In 2025, the FDA extended the indication for semaglutide (Wegovy) to include adults with obesity and biopsy proven MASH with moderate to advanced fibrosis, making it the first approved pharmacotherapy for this condition. This approval underscores that treating obesity is not just cosmetic; it is hepatoprotective.
For the primary care physician, these drugs offer a realistic outpatient pathway for MASH management. Key counseling points include confirming that the patient’s GLP 1 is FDA approved rather than compounded, monitoring for gastrointestinal side effects, and maintaining follow-up labs for liver function and nutritional status. Providers should pair medication with a structured lifestyle plan and regular exercise to preserve lean muscle mass during rapid weight loss.
For clinicians: The American Association for the Study of Liver Diseases (AASLD) provides clinical and patient education resources at https://www.aasld.org/liver-fellow-network/core-series/nafld.
For patients: The American Liver Foundation offers accessible information on MASH at https://liverfoundation.org/.
When lifestyle and medication alone are insufficient, bariatric surgery remains the most effective intervention for sustained weight loss and metabolic improvement. The 2022 ASMBS/IFSO joint guidelines broadened eligibility to include patients with BMI ≥ 35 kg/m² regardless of comorbidities, and those with BMI ≥ 30 kg/m² if metabolic disease is present.4
In the context of MASH, the outcomes are remarkable. A multicenter French cohort study following patients up to 10 years post-surgery found histologic resolution of NASH in 84% and fibrosis regression in 70% of participants.2 Sleeve gastrectomy and Roux en Y gastric bypass remain the dominant procedures, each producing average total body weight loss of 25 to 35% and profound improvements in insulin resistance and hepatic inflammation.
Compared head-to-head with pharmacotherapy, surgery achieves deeper and more durable reductions in hepatic fat content and fibrosis. A systematic review comparing GLP 1 receptor agonists with bariatric surgery demonstrated that surgical patients lost an average of 22.7 kg more and achieved greater reductions in BMI and steatosis markers.3
The evolving evidence suggests that GLP 1 medications and bariatric surgery need not be viewed as competing options but rather as complementary. Preoperative GLP 1 therapy may optimize glycemic control and weight before surgery, reducing anesthesia risks and improving postoperative recovery. Postoperatively, GLP 1s can help sustain weight loss and prevent weight regain, a frequent concern several years after surgery. Early studies support this synergy, showing additive benefits for both metabolic health and liver histology.
For the primary care physician, the key lies in coordination: ensuring that obesity medicine specialists, gastroenterologists, endocrinologists and surgeons work as a team. Referral timing is critical. Patients with BMI ≥ 30 and evidence of hepatic steatosis on ultrasound or elevated ALT should undergo metabolic evaluation. Those with fibrosis scores above 1.3 on FIB 4 or abnormal elastography should be referred for hepatology assessment and considered for advanced therapies.
For clinicians: NIH LiverTox database offers drug-related liver guidance at https://www.ncbi.nlm.nih.gov/books/NBK547852/.
For patients: AASLD’s patient resource library is available at https://www.aasld.org/patient-resources.
MASH has long lacked an effective medical therapy, but we are entering an era where weight loss interventions, both medical and surgical, can reverse the disease’s trajectory. For primary care physicians, the message is clear: early detection, patient education and timely escalation of care save lives. Whether through GLP 1 medications, bariatric surgery or both, we now have tools that address the root causes of fatty liver disease rather than merely managing its consequences. The liver’s remarkable ability to heal itself, when given the right metabolic environment, is the foundation of this new therapeutic optimism.
References:
1. Newsome, P.N., Buchholtz, K., Cusi, K. et al. A Placebo Controlled Trial of Subcutaneous Semaglutide in Nonalcoholic Steatohepatitis. N Engl J Med. 2021;384(12):1113–1124. PMID: 33789008
2. Lassailly, G., Caiazzo, R., Buob, D. et al. Bariatric Surgery Provides Long Term Resolution of Nonalcoholic Steatohepatitis and Regression of Fibrosis. Gastroenterology. 2020;159(4):1290–1301. PMID: 32615288
3. Sarma, S., Palcu, P. Weight loss between glucagon like peptide 1 receptor agonists and bariatric surgery in adults with obesity: A systematic review and meta-analysis. Obesity (Silver Spring). 2022;30(11):2111–2121. PMID: 36321278
4. Eisenberg, D., Shikora, S.A., Aarts, E. et al. ASMBS and IFSO Indications for Metabolic and Bariatric Surgery. Obes Surg. 2023;33(1):3–14. PMID: 36336720

Patrick Reeves, MD, FAAP, DABOM, is a native Texan and graduate of Texas A&M University (class of 2012) who currently serves as a triple board-certified pediatric gastroenterologist, obesity medicine specialist and general pediatrician in San Antonio, Texas. He works on the liver transplant unit at University Hospital and is active in clinical research focused on clinical action plan implementation. Dr. Reeves is a member of the Bexar County Medical Society.

By Gabrielle Holliefield, MS, OMS-II; Thomas Althaus, OMS-II; and Ramaswamy Sharma, MS, PhD
Hepatocellular carcinoma (HCC) is among the most rapidly increasing causes of cancer-related mortality in the United States, with Texas reporting the highest incidence and death rates.1,2 This alarming statistic highlights the need to examine the risk factors driving this disparity and explore new approaches for earlier detection and treatment to address HCC more effectively within our communities and improve patient outcomes. A deeper investigation into race and ethnicity reveals that HCC incidence among Hispanics in Texas is 26 to 37% higher than the national average. Furthermore, a nationwide survey from 1988-1994 recorded Hispanic individuals as having a 5-fold greater risk of HCC mortality, indicating Hispanic ethnicity as an independent prognostic factor.1,2 Notably, there is also a disparity within the Hispanic population, with HCC being disproportionately higher among Hispanics in the South Texas region as compared to Hispanics in the rest of Texas. This disparity is thought to be driven by the high prevalence of diabetes mellitus and obesity in this community, both of which are major contributors to non-alcoholic fatty liver disease (NAFLD), a known risk factor for HCC. Other prominent risk factors for HCC that may also contribute to disproportionate rates of HCC in Hispanics in South Texas include hepatitis B, hepatitis C, metabolic syndrome and environmental exposures.1
The progression of NAFLD to cirrhosis and ultimately HCC is thought to result from excessive intracellular accumulation of fatty acids, leading to oxidative stress. Insulin resistance, dysregulated adipokine signaling and activation of the PI3K/AKT/mTOR and Wnt/β-catenin pathways contribute to this process by disrupting the oxidant-antioxidant balance, thereby promoting HCC development. Interestingly, the gut microbiota has been found to play a significant role in NAFLD-associated HCC, suggesting that gut microbiota dysbiosis is linked to HCC occurrence. A healthy gut microbiota helps prevent hepatic inflammation; thus, dysbiosis can induce liver inflammation and injury by increasing intestinal permeability, facilitating bacterial and toxin translocation to the liver, and impairing immune regulation. Furthermore, dysbiosis can also result in senescent hepatic stellate cells producing growth factors, chemokines and pro-inflamma-
tory cytokines, all of which contribute to HCC advancement.3 With this in mind, the gut microbiota represents a potentially promising modifiable factor that can be targeted to mitigate the progression of NAFLD to HCC. Strategies promoting a healthy gut microbiome, including dietary habits, prebiotic and probiotic supplementation, and other microbiome-targeted therapies, may be beneficial considerations in the management and prevention of NAFLD-related liver disease. While consideration of specific risk factors is key in addressing disparities among Hispanics in South Texas, early detection and screening remain a significant factor influencing treatment and outcomes. According to 2020 SEER data on outcomes, early-stage HCC has a 5-year survival rate of >70% which decreases to 20% in advanced stages, with a median survival of 1-1.5 years.4,5 Only very early-stage and early-stage HCC presenting with small, localized tumors are suitable for curative treatments, such as surgical resection, ablative therapy and even liver transplantation. The question then remains, how do local practices align with national guidelines for screening, especially when considering that Hispanic patients in South Texas have lower odds of receiving any treatment, and more specifically, curative treatment?6 According to the Texas Liver Institute, screening is suggested for high-risk patients every six months, which is consistent with the national AASLD guidelines.7,8 Emphasis for screening includes all adults with cirrhosis, selected chronic HBV patients and patients with NAFLD who have advanced fibrosis/cirrhosis. However, the effectiveness of screening remains dependent on accessibility for patients to see a primary care physician for regular screenings to take place. When addressing the concerning rate of HCC, it may be beneficial for physicians to take action even before the diagnosis of one of the HCC risk factors. Specifically, an article by El-Serag et al. points out that patients with cirrhosis are often unaware that they have it, therefore, not receiving proper care, and increasing the likelihood of HCC. With this in mind, the prevention of HCC can begin with physicians identifying patients early on who have primary risk factors. For example, it may be important for physicians to recognize the risk of NAFLD in patients with obesity and diabetes. To align with this, Clinical Care Pathways have been developed to provide healthcare providers with guidance on who to screen.9
While conducting an ultrasound every six months remains the gold standard for screening high-risk patients, a growing movement towards personalized risk-based surveillance, as well as new developments in liquid biopsy testing, are proving to be promising alternatives for earlier detection. With the evolving treatment landscape of HCC and heterogeneity in liver tumor aggressiveness and progression, it should not be surprising that the emerging data have shown that taking an individualized approach that incorporates a diverse care team can lead to improved outcomes for patients. Reviewing high-risk patient cases in a multidisciplinary tumor board could increase the chances of earlier detection and decrease time to treatment.10 Personalized diagnosis has only increased in the setting of HCC, with liquid biopsies showing promising evidence for early detection. Several cfDNA methylation panels (and other ctDNA approaches) have shown high sensitivity/specificity for HCC in research and early clinical validation. For example, this year, Mursla Bio’s newly developed EvoLiver was granted FDA Breakthrough Device designation for HCC surveillance. Using a novel platform for detecting biomarker signatures in hepatocyte extracellular vesicles, this noninvasive approach can provide high specificity for early cancer detection with quick turnaround and low sample burden.11 While this rapidly evolving space is a promising alternative in the future for high-risk communities, such technologies are still in early clinical validation and not yet a replacement for ultrasound/AASLD standard care.
Texas’s disproportionately high rates of HCC, particularly among the Hispanic population in South Texas, underscore the urgent need for heightened vigilance within practice. Studies outline the mechanism of how NAFLD leads to progression of HCC through oxidative stress, dysregulated metabolic signaling and gut microbiota dysbiosis, highlighting the gut-liver axis as a promising modifiable target for prevention. Despite the current screening practices aligning with national guidelines and the clear survival advantage of early detection, persistent barriers — such as limited access to care and delayed testing — continue to hinder early detection and treatment, leading to overall poorer outcomes for the South Texas community. Emerging tools, including personalized risk-based surveillance and liquid biopsy, offer the potential to improve early detection. Addressing HCC disparities will require improved identification of high-risk individuals as well as the integration of multidisciplinary, personalized approaches and expanded research into local disparities, which will enhance prevention, surveillance and treatment across the South Texas community.
References:
1. Ha, J., Chaudhri, A., Avirineni, A., & Pan, J.-J. (2017). Burden of hepatocellular carcinoma among Hispanics in South Texas: A systematic review. Biomarker Research, 5(1). https://doi. org/10.1186/s40364-017-0096-5
2. El-Serag, H.B., Sardell, R., Thrift, A.P., Kanwal, F., & Miller, P. (2020). Texas has the highest hepatocellular carcinoma incidence rates in the USA. Digestive Diseases and Sciences, 66(3), 912–916. https://doi.org/10.1007/s10620-020-06231-4
3. Shi, Y., Taherifard, E., Saeed, A., & Saeed, A. (2024). MASLD-related HCC: A comprehensive review of the trends, pathophysiology, tumor microenvironment, surveillance, and treatment options. Current Issues in Molecular Biology, 46(6), 5965–5983. https://doi.org/10.3390/cimb46060356
4. Llovet, J.M., Kelley, R.K., Villanueva, A., Singal, A.G., Pikarsky, E., Roayaie, S., Lencioni, R., Koike, K., Zucman-Rossi, J., & Finn, R.S. (2021). Hepatocellular carcinoma. Nature Reviews Disease Primers, 7(1). https://doi.org/10.1038/s41572-020-00240-3
5. Brar, G., Greten, T.F., Graubard, B I., McNeel, T S., Petrick, J L., McGlynn, K A., & Altekruse, S.F. (2020). Hepatocellular carcinoma survival by etiology: A seer‐medicare database analysis. Hepatology Communications, 4(10), 1541–1551. https://doi. org/10.1002/hep4.1564
6. Gutierrez, J.A., Bresnahan, L.Z., Rios, E., Wanchoo, P., San Valentin, A., & Fisher, M.E. (2022). Closing the disparity gap and optimizing advanced hepatocellular carcinoma care in the Hispanic community. Clinical Liver Disease, 19(6), 239–243. https://doi. org/10.1002/cld.1213
7. Liver cancer. Texas Liver Institute. (2014, August 3) https://txliver.com/patient-education/liver-cancer/
8. Singal, A.G., Llovet, J.M., Yarchoan, M., Mehta, N., Heimbach, J.K., Dawson, L.A., Jou, J.H., Kulik, L.M., Agopian, V.G., Marrero, J.A., Mendiratta-Lala, M., Brown, D.B., Rilling, W.S., Goyal, L., Wei, A.C., & Taddei, T.H. (2023). Aasld Practice guidance on prevention, diagnosis, and treatment of hepatocellular carcinoma. Hepatology, 78(6), 1922–1965. https://doi.org/10.1097/ hep.0000000000000466
9. El-Serag, H.B., Ward, J.W., Asrani, S.K., Singal, A.G., Rich, N., Thrift, A.P., Deshpande, S., Turner, B.J., Kaseb, A.O., Harrison, A.C., Fortune, B.E., & Kanwal, F. (2023). Prevention of hepatocellular carcinoma (HCC). White Paper of the Texas Collaborative Center for hepatocellular cancer (tech) multi-stakeholder conference. Clinical Gastroenterology and Hepatology, 21(9), 2183–2192. https://doi.org/10.1016/j.cgh.2023.03.029
10. Kinsey, E., & Lee, H.M. (2024). Management of hepatocellular carcinoma in 2024: The multidisciplinary paradigm in an evolving treatment landscape. Cancers, 16(3), 666. https://doi. org/10.3390/cancers16030666
11. Sava, J. (2025, November 17). FDA grants breakthrough designation for Evoliver in HCC. Targeted Oncology - Immunotherapy, Biomarkers, and Cancer Pathways. https://www.targetedonc.com/ view/fda-grants-breakthrough-designation-for-evoliver-in-hcc

Gabrielle Holliefield, MS, OMS-II, is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2028. She is interested in pursuing a career in hematology-oncology.

Thomas Althaus, OMS-II, is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2028. His interests include internal medicine and adult oncology.

Ramaswamy Sharma, MS, PhD, is a Professor of Histology and Pathology at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life. Dr. Sharma serves on the BCMS Publications Committee.

By Barbara S. Taylor, MD, MS; Thomas Patterson, MD; and Anna Taranova, MD
Why Should South Texans Care About Chronic Infectious Diseases?
Medea “Dee” Morris never expected that an infectious disease would turn her life upside down, until it did. While most people she knew improved after COVID-19, Dee did not, and she found herself unable to work, care for an ill parent, or complete even basic household tasks. After being dismissed by multiple physicians, Dr. Monica Verduzco Gutierrez at UT Health diagnosed Dee with Long COVID based on her fatigue, brain fog, headaches and Postural Orthostatic Tachycardia Syndrome (POTS), which makes it difficult for her to stand. Last year Dee joined thousands of others with Long COVID as a participant in treatment trials. Though her symptoms persist, she hopes that research will pave the way for effective medications and therapies for her and the millions of others with Long COVID.
Greg Casillas knew about HIV research because his eldest brother, Paul, participated in treatment studies after his diagnosis in 1982. Paul meticulously documented his response to each new treatment in journals for his physicians, but scientific research did not move quickly enough to save him. Greg himself was diagnosed with HIV in 2000, and he attributes his current excellent health on one daily pill to those like his brother, who were early participants in HIV clinical trials.
Dee and Greg both became advocates for the importance of research through different pathways, but they joined UT San Antonio’s Center for Chronic Infectious Diseases as advisors because of their common commitment to reducing the burden of these illnesses in South Texas and globally.
South Texas bears a disproportionate burden of chronic infectious diseases that cause lasting harm over months and years in both urban and rural communities, sometimes leading to disability and death if
not addressed. These infections can spread without warning and exist for years without causing symptoms, like Mycobacterium tuberculosis, which causes illness in 4.1 out of 100,000 Texans, an incidence 50% higher than the overall United States.1 The border counties of South Texas are particularly impacted, representing 21.2% of tuberculosis diagnoses in Texas in 2022, although only 9.5% of Texans live in a border county, and five of 10 counties with highest incidence of new tuberculosis cases were in South Texas.2 Our own work on tuberculosis screening found that 8% of individuals in primary care clinics in South Texas tested positive for latent tuberculosis infection, many with a high risk of progression to active disease due to comorbidities such as diabetes.3 In 2024, University Health, which serves Bexar County and the surrounding areas, admitted 73 individuals to the hospital with active tuberculosis disease.
Tuberculosis is only one of many chronic infectious diseases that are more common in South Texas. In 2022, Texas recorded one of the highest rates of new HIV diagnoses in the nation, with 11 of the most impacted counties in the U.S. located in the state.4 The federally funded Ryan White Act supports care for Texans living with HIV provided through the San Antonio Translational Grant Area grant award to University Health, providing services for 3,390 individuals across Bexar, Comal, Guadalupe and Wilson counties, including 95 youth and children under 12 years old. South Texas bore the brunt of the COVID-19 pandemic in both cases and deaths, leading to increased Long COVID in the region.5 Perhaps least well known is that South Texans are at higher risk for chronic endemic fungal infections. Valley Fever, caused by coccidioidomycosis, which occurs in South and West Texas, and incidence of other fungal infections such as cryptococcus and histoplasmosis are also high in the area.6 While Valley Fever causes
a transient illness in most patients, in some it can progress to debilitating neurologic disease with meningitis and transverse myelitis. Protecting the health of South Texas will require coordinated efforts across healthcare providers and systems to prevent, diagnose, and treat chronic infectious disease, as well as innovative research to develop new tools for this effort.
Improving our ability to diagnose, prevent, and treat chronic infectious diseases impacting Texans requires a clear understanding and recognition of the comorbidities and other factors that place our communities at risk for poor outcomes. All the chronic infections mentioned above are more challenging to address in the context of other chronic comorbidities, such as diabetes, cardiovascular disease, substance use disorder, community-wide stigma, cancer and dementia. For example, people with HIV face increased risk from cardiovascular disease and dementia,7 while those with diabetes are at increased risk for progression to tuberculosis disease.8 South Texans face higher burdens of diabetes and cardiovascular disease than many other places in the U.S., making the intersection of these conditions particularly important in our region.
As of 2023, 16.8% of Texans remain uninsured — the highest rate in the nation. In South Texas, however, the share of residents without health coverage is even greater, ranging from 18% in Bexar County to more than 30% in many counties along the U.S./Mexico Border.4 This lack of access to healthcare serves as an added barrier to health for those with chronic infectious diseases. This, combined with the increased level of stigma sometimes faced by people living with these infections,9 creates conditions that make engagement in care challenging for chronic infectious diseases.
A Center dedicated to innovative translational and clinical research, partnered with South Texas communities, will allow us to address the urgent threats of chronic infectious diseases at the source and disseminate new solutions nationally and globally. Our Center’s founding faculty already have an outstanding track record on the forefront of prevention and treatment research for chronic infections impacting our region. Since March 2020, we have been international leaders in COVID therapeutic trials, which led to success in Long COVID studies and COVID and HIV vaccine studies. Over the past four years, the Center’s research profile expanded to include inpatient and outpatient clinical trials, vaccine trials, behavioral interventions and longitudinal cohort studies. The Center’s core faculty have skills in translational research, epidemiology, diagnostics, clinical research and implementation science. We have the support of an outstanding Advisory Board of those with lived experience, like Dee and Greg, alongside key partners like University Health, Texas Biomedical Research Institute and the San Antonio Metropolitan Health District. Together, we will work to eradicate chronic infectious diseases in South Texas through groundbreaking prevention, diagnostics and treatment responsive to the needs of our community.
References:
1. Reported Tuberculosis in the United States, 2023. Report from the United States Centers for Disease Control and Prevention, Atlanta, 2023
2. The Impact of TB in Texas, 2022. Report from the Texas Department of Health and Human Services, Austin, 2022
3. Naqvi, S., Cantu, Y., Ong Uti, S. et al. Successes and challenges of latent TB screening and treatment in a high-prevalence US region. Int J Tuberc Lung Dis. Aug 1 2022;26(8):720–726. doi:10.5588/ ijtld.21.0454
4. Sullivan, P.S., Woodyatt, C., Koski, C. et al. A Data Visualization and Dissemination Resource to Support HIV Prevention and Care at the Local Level: Analysis and Uses of the AIDSVu Public Data Resource. Journal of Medical Internet Research. Oct 23 2020;22(10):e23173. doi:10.2196/23173
5. Khan, D., Park, M., Burkholder, J. et al. Tracking COVID-19 in the United States With Surveillance of Aggregate Cases and Deaths. Public Health Rep. May–Jun 2023;138(3):428–437. doi:10.1177/00333549231163531
6. Mayfield, H., Davila, V., Penedo, E. Coccidioidomycosis-Related Hospital Visits, Texas, USA, 2016-2021. Emerging Infectious Diseases. May 2024;30(5):882–889. doi:10.3201/eid3005.231624
7. Feinstein, M.J. HIV and Cardiovascular Disease: From Insights to Interventions. Top Antivir Med. Oct–Nov 2021;29(4):407–411
8. Yorke, E., Atiase, Y., Akpalu, J., Sarfo-Kantanka, O., Boima, V., Dey, I.D. The Bidirectional Relationship between Tuberculosis and Diabetes. Tuberc Res Treat. 2017;2017:1702578. doi:10.1155/2017/1702578
9. Baldwin, A., Sileo, K.M., Huynh, T.A. et al. Applying the Health Stigma and Discrimination Framework to Assess HIV Stigma among Health Care Professionals: A Mixed Methods, Community-Based Participatory Research Study. J Health Care Poor Underserved. 2022;33(2):950–972. doi:10.1353/hpu.2022.0074



Barbara S. Taylor, MD, MS, is the founding Director for the Center for Chronic Infectious Disease, and Professor of Medicine and Infectious Disease at the Joe R. and Teresa Lozano Long School of Medicine, UT San Antonio.
Thomas Patterson, MD, is the Co-Director of the Center for Chronic Infectious Disease, and Professor and Chair of the Department of Medicine at the Joe R. and Teresa Lozano Long School of Medicine, UT San Antonio.
Anna Taranova, MD, serves as the Vice President for Health Innovation at University Health in San Antonio.

Reconstructive surgery, a sub-specialty of plastic surgery, has become a vital cog of surgical oncology. What was once deemed an aesthetic pursuit has evolved into a field that addresses restoration of form and function after tumor resection, thereby enhancing patient survival, emotional well-being and quality of life.
The past several decades has witnessed advances in surgical techniques, microsurgery, imaging and perioperative care, enhancing the disciplines of surgical oncology and reconstructive surgery. For example, resection of primary sarcomas around the knee combined with joint-preserving endoprosthetic reconstruction has improved survival, function and patient satisfaction. A recent report evaluated clinical and functional outcomes of 165 patients following proximal humeral endoprosthetic reconstruction and found preservation of auxiliary nerve and reattachment of deltoid muscle in approximately 90% or more cases. Similarly, reconstructive surgery after radical resection for the treatment of pelvic cancer may help prevent permanent urinary and fecal incontinence or sexual dysfunction.
Reconstructive surgeons play an important role in the planning and holistic decision-making process of multidisciplinary tumor boards, ensuring that both functional and cosmetic outcomes of surgery are fully considered. With ongoing innovations each year, every small advancement continues to reshape patient care and redefine the borders of medicine through enhanced surgical prowess, ingenuity, collaboration and compassion.
Microsurgery allows surgeons to operate on and transplant small, vascularized tissues from one location in the body to another using specialized instruments; it has played a vital role in reconstructive surgery, particularly in head and neck-related cancer surgery. Historically, surgical resections such as radical laryngopharyngectomy for cancers involving the jaw, tongue or other areas were either avoided or limited to preserve swallowing and speech functions, resulting in increased risk of cancer recurrence. Today, microsurgery techniques such as free flap reconstruction involving fibula and radial forearm flaps, allow for immediate reconstruction of pharyngeal walls, tongues and mandibles; importantly, mandibular reconstruction procedures in oral cancer
patients such as “Jaw in a Day®” neither increase total operation time significantly nor post-operative recovery time when combined with retroauricular robot-assisted neck dissection. These improvements have led to increased patient willingness to undergo these procedures and have transformed patient quality of life after surgical resection. While the concept of microsurgery appears to have originated in 1921 with the use of microscopes by the Swedish otolaryngologist, Carl-Olof Siggesson Nylen, it has now evolved to “supermicrosurgery” that employs forceps with tip diameters of 100 μm as well as sutures that are ≤0.01 mm in diameter; such ultra-fine instruments are critical for nerve reconstruction, corneal transplants, cataract surgeries, retinal repairs and other procedures. The development of these tools, along with advancements in imaging techniques such as magnetic resonance lymphography and near-infrared fluorescence, has revolutionized lymphatic surgery and peripheral nerve surgery, particularly when integrated with robotic systems such as the MUSA platform and artificial intelligence (AI)-powered imaging to generate 3D anatomical images in real-time. Innovations in microsurgery have laid the groundwork for transformative applications in several areas such as breast reconstruction, limb salvage procedures and cutaneous malignancy treatments.
Breast reconstruction has advanced significantly over the years. The deep inferior epigastric perforator (DIEP) flap after mastectomy to prevent muscle dysfunction as well as disfigurement has remained the gold standard for autologous vascularized tissue reconstruction. More recently, the superficial branch of the superficial circumflex iliac artery perforator (SB-SCIP) flap is increasingly being used as it minimizes potential abdominal wall complications such as bulging and hernias, which can adversely affect clinical outcomes as well as patient self-image. Robotic-assisted flap harvest, combined with either indocyanine green angiography (ICG) to visualize vessels for real-time intraoperative guidance or 3D printing and modeling for flap perforator mapping and personalized flap design, has significantly reduced harvest time, flap failure risk and donor site complications.
Limb salvage procedures have also benefited from 3D-printed, patient-specific implants, leading to enhanced surgical precision, sta -
bility and fixation. Using data from CT and MRI imaging, implants that exactly match the patient’s anatomy can be created; these can be precisely placed with sub-millimeter accuracy using robotic systems, leading to better fit, stability and long-term use. Newer biocompatible alloys seeded with stem cells further add to regeneration and enhanced biomechanical integration, which, in turn, accelerates recovery time in terms of mobility and independence, thereby boosting patient morale and increasing satisfaction with the procedure.
Skin malignancy treatment using procedures such as Mohs micrographic surgery has shown better results when followed by immediate reconstruction, not only in terms of oncologic clearance but also with regard to aesthetics and functional rehabilitation. The use of refined layered excision methods has enabled reconstructive surgeons to completely dissect out cancerous tissue while preserving healthy tissue. Integrating AI with these procedures has further enhanced outcomes. Advances in AI have led to accurate 3D imaging and modeling, critical for preoperative surgical planning of flap design and placement. AI is increasingly being used intraoperatively to assess tumor margins in real time, enabling fast and more informed clinical decision making; AI-based detection of pathological features has reduced the risk of incomplete resections, cancer recurrence and future complications. AI-powered virtual guidance systems also help train surgeons through simulations.
Some of the key challenges that remain include achieving seamless data integration across platforms, addressing the variability in outcomes with different tumor types, adapting AI-based robotic systems in disciplines such as pediatric and neurosurgical oncology wherein anatomical variability presents unique problems, and the development of standardized clinical protocols that are also cost-effective. While augmented reality (AR) systems offer the hope of enhanced surgical planning, specifically in terms of intraoperative navigation for precise flap placement and better anatomical alignment, current models lack the accuracy of traditional CAD/CAM-guided approaches and need to be refined. Nevertheless, reconstructive surgery has emerged as a cornerstone of modern medicine by offering patients both functional and aesthetic outcomes that help restore dignity and hope.
References:
1. Ahorro, A.F., Huang, J., Weyer, C., & Moenster, J.M. (2025). Apocrine mixed tumor of the upper cutaneous lip: a case report. Cureus. https://doi.org/10.7759/cureus.78623
2. Allam, O., Foster, C., Knoedler, L., Knoedler, S., Oh, S.J., Pomahac, B., & Ayyala, H.S. (2024). Future of autologous breast reconstruction: a review of novel technological innovations. Plastic and Aesthetic Research. https://doi.org/10.20517/2347-9264.2024.21
3. Banegas, D.W., Cho, J.M., Gong, M., Kim, H., Nam, W., Kim, H.J., Koh, Y.W., & Kim, D. (2025). Is Jaw in a Day® reconstruction feasible in patients undergoing robotic neck dissection for oral cancer?: a case series with comparative analysis. Maxillofacial Plastic and Reconstructive Surgery, 47(1). https://doi.org/10.1186/s40902-025-00489-2
4. Civita, F., Rota, I., Rossi, D.S., Sinatra, A., Beltramini, G.A., & Bolzoni, A.R. (2025). Augmented reality vs CAD/CAM system in orthognathic surgery: development and accuracy evaluation. Maxillofacial Plastic and Reconstructive Surgery, 47(1). https://doi. org/10.1186/s40902-025-00471-y
5. Evenhuis, R., Bus, M.P.A., Sellevold, S., Dierselhuis, E.F., Trikoupis, I.G., Scorianz, M., Walter, S., Cabrolier, J., Fiocco, M., & Van De Sande, M.a.J. (2025). Proximal humeral endoprosthetic reconstruction for tumour defects. Bone & Joint Open, 6(6), 715–723. https:// doi.org/10.1302/2633-1462.66.bjo-2025-0018
6. Fatani, B., & Alshalawi, S.S. (2025). Advances in microvascular head and neck reconstruction using free fibula and radial forearm free flap to reconstruct various orofacial defects: a mini review. International Journal of Otorhinolaryngology and Head and Neck Surgery, 11(4), 465–468. https://doi.org/10.18203/issn.2454-5929.ijohns20252264
7. Kok Wah, J.N. (2025). AI-driven robotic surgery in oncology: advancing precision, personalization, and patient outcomes. Journal of Robotic Surgery, 19(1): 382. https://doi.org/10.1007/s11701-02502555-3
8. Li, Z., Liu, W., Niu, X., Jiang, C., & Zhang, Q. (2025). The clinical outcomes of joint-preserving endoprosthesis reconstruction for primary sarcomas about the knee. Journal of Orthopaedic Surgery and Research, 20(1). https://doi.org/10.1186/s13018-025-06252-7
9. Pson, I. (2025). Reconstructive surgery and surgical oncology: Integrating precision and restoration in modern cancer care. Case Reports in Surgery and Invasive Procedures, 9(1). https://www.alliedacademies.org/articles/reconstructive-surgery-and-surgical-oncology-integrating-precision-and-restoration-in-modern-cancer-care-32908.html
10. Scaglioni, M.F., Martini, F., & Meroni, M. (2025). Present and future of autologous breast reconstruction: advancing techniques to minimize morbidity and complications, enhancing quality of life and patient satisfaction. Journal of Clinical Medicine, 14(8), 2599. https://doi.org/10.3390/jcm14082599
11. Thamm, O.C., Eschborn, J., Schäfer, R.C., & Schmidt, J. (2024). Advances in modern microsurgery. Journal of Clinical Medicine, 13(17), 5284. https://doi.org/10.3390/jcm13175284




Alyssa Francesca Ahorro, OMS-III, is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027. She is currently pursuing her interests in surgery and oncology while also completing a Master of Public Health.
Bryanna Le, OMS-III, is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027. She is currently pursuing her interests in anesthesiology.
Camille Irene Hulipas, OMS-III, is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027. Camille is driven by a passion for equitable healthcare and is interested in pursuing emergency medicine.
Ramaswamy Sharma, MS, PhD, is a Professor of Histology and Pathology at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life. Dr. Sharma serves on the BCMS Publications Committee.

By Kaeli Alpha, OMS-II; Blessina Babu, OMS-II; Karen Johns, OMS-II; and Ramaswamy Sharma, MS, PhD
Our immune system is comprised of a multitude of defense mechanisms that fend off thousands to millions of pathogens on a daily basis. The first line of defense, called innate immunity, is non-specific in terms of its recognition of specific microbes. However, during persistent infection, it is followed by a much more powerful and destructive second response, called adaptive immunity, mediated by T and B lymphocytes. Given their memory and potency of response, T and B lymphocytes must be able to accurately distinguish and tolerate the presence of an individual’s own cells as well as the normal flora, the harmless and sometimes beneficial commensal microbes that colonize us, while specifically targeting pathogens. The role of central immune tolerance in getting rid of self-reactive lymphocytes was conceptualized by the Nobel laureates, Sir Frank Macfarlane Burnet and Peter Medawar, in the 1940s and 1950s. However, while central immune tolerance helps nip self-reactive immune cells in the bud by eliminating them during their maturation in the thymus or bone marrow, it is not 100% efficient. Dr. Mary Brunkow, a Senior Program Manager at the Institute for Systems Biology in Seattle, Dr. Fred Ramsdell, a Scientific Advisor at Sonoma Biotherapeutics in San Francisco, and Dr. Shimon Sakaguchi, a professor at the Immunology Frontier Research Center at Osaka University in Japan, revolutionized our understanding of the immune system by their discovery of regulatory T lymphocytes and the FoxP3 gene that function in peripheral immune tolerance; their groundbreaking discoveries of this second checkpoint were honored with the 2025 Nobel Prize in Physiology or Medicine.
Central immune tolerance occurs in the primary lymphoid organs, the bone marrow and the thymus. B lymphocytes that react to selfantigens in the bone marrow during development follow one of three pathways: they undergo clonal deletion and are destroyed, they change their antigen receptors to produce a new non-self-reactive antigen receptor through a process of receptor editing, or they become functionally inactive via anergy. Self-reactive T-lymphocytes, on the other hand, undergo apoptosis in the thymus. Thus, central immune tolerance stops self-reactive immune cells from reaching the circulatory
system. In the 1970s and early 1980s, a few researchers suggested the existence of suppressor T lymphocytes which could regulate autoreactive immune cells that escaped central tolerance. However, flawed research that included experimental inconsistencies, overinterpretation of results and lack of molecular markers led to loss of credibility of the hypothesis, and research on suppressor T lymphocytes was largely abandoned. The general notion was that central immune tolerance was sufficient to eliminate autoreactive lymphocytes.
In the early 1980s, Shimon Sakaguchi, who worked at the Aichi Cancer Center Research Institute in Nagoya, Japan, found to his surprise that newborn mice developed autoimmune diseases if their thymus was removed three days after birth. Interestingly, injection of mature T lymphocytes from mice that were genetically identical into these thymectomized mice prevented autoimmunity, suggesting the existence of a specialized subset of T cells. Further research over the next decade revealed that these cells expressed a surface protein, CD25, in addition to CD4. This new subset of CD4+, CD25+ cells were called regulatory T cells (Tregs). He published this discovery in the Journalof Immunology in 1995, but given the past history of suppressor T cells, the scientific community needed more evidence.
Meanwhile, Mary Brunkow and Fred Ramsdell, who were working at a Celltech Chiroscience in Bothell, Washington, a company that developed therapeutics for autoimmune disorders, set out to identify the gene responsible for the phenotype observed in scurfy mice. These shortlived mice had scaly, flaky skin, splenomegaly and lymphadenopathy. Presence of self-reactive T cells had been demonstrated in these mice, making it an ideal model for elucidating the molecular mechanisms underlying autoimmune diseases. Female mice were carriers while 50% of male mice present with the disease, suggesting that the mutation was located on the X chromosome. Mapping led to the identification of 20 potential genes that were painstakingly scrutinized over many years; finally, the researchers determined that the FoxP3 gene was responsible for the scurfy phenotype. In addition, they recognized that the phenotype of scurfy mice mirrored the symptoms seen in a rare, life-threatening, autoimmune disorder, IPEX syndrome (Immune
dysregulation, Polyendocrinopathy, Enteropathy, X-linked), and identified its human ortholog. They published their discoveries linking mutations in the FoxP3 gene to both IPEX and scurfy in Nature Genetics in 2001. A couple of years later, Shimon Sakaguchi and other researchers showed that FoxP3 was essential for the development of Tregs, now classified as CD4+ CD25+ FoxXP3+, and the concept of peripheral immune tolerance was recognized.
Peripheral immune tolerance encompasses multiple mechanisms that regulate 30 to 40% of low affinity self-reactive lymphocytes which escape recognition by central immune tolerance and circulate throughout the body. Tregs ensure that self-reactive lymphocytes fail to respond to self-antigens by (1) expressing CTLA-4 which competes for a required co-stimulatory signal by antigen presenting cells and thereby suppresses their activation, (2) secreting anti-inflammatory cytokines such as IL-10 which reduces antigen presentation, TGF-β which inhibits T cell proliferation and their differentiation into Th1 and Th17 cells, and IL-35 which suppresses effector T cell activity while also promoting Treg development, and (3) disrupting metabolism by consuming IL-2, a growth factor required for T cell proliferation, as well as by expressing the enzymes CD39 and CD73 that convert ATP to anti-inflammatory adenosine. All of these mechanisms ensure that Tregs downregulate the immune system when it is not needed.
Discovery of peripheral immune tolerance has profound implications in the development of new therapies for autoimmune disorders, allergies, cancers and in improving transplant outcomes. For example, increasing Treg activity can inhibit autoimmune attacks on pancreatic beta cells in type 1 diabetes; similarly, it can downregulate the hyperactive immune response in lupus. Modulating the Th17/ Treg axis using mesenchymal stem cells can also have beneficial effects in multiple sclerosis by decreasing neuroinflammation and slowing down the progression of the disease. Suppression of immune responses against transplants using Tregs can also reduce the need for lifelong use of immunosuppressive treatments in these patients. A phase II trial, iWITH (Immunosuppression Withdrawal for Stable Pediatric Liver Transplant Patients), evaluated whether transplant recipients could safely taper off immunosuppressants if their immune systems naturally developed tolerance to the transplanted organ. The trial identified biomarkers that can help predict which pediatric patients will tolerate reduced immunosuppression without rejection of the transplant. Tumors are known to exploit peripheral tolerance to evade immune detection; research on cancer immunotherapies based on blocking Treg recruitment, inhibiting FoxP3 signaling, or using checkpoint inhibitors such as anti-CTLA-4 and anti-PD-1 are ongoing for treating melanoma, lung cancer and other solid tumors. Oral immunotherapy for various allergies arising from pollen, dust or food-related proteins is based on re-training the immune system to recognize harmless antigens; modulating Treg expression is also the principle underlying treatment of asthma. Gene editing of mutated FoxP3 using CRISPR/Cas9 as well as supplementation with autologous CD4+ T cells that express FoxP3 using a lentiviral vector are approaches currently in clinical trials to restore Treg function in patients with IPEX syndrome.
In summary, the discovery of peripheral immune tolerance by these Nobel laureates has not only rewired our understanding of the immune system, but also has provided us with novel therapeutic targets to treat several disorders.
References:
1. Bennett, C.L., Brunkow, M.E., Ramsdell, F. et al. A rare polyadenylation signal mutation of the FoxP3 gene (AAUAAA-->AAUGAA) leads to the IPEX syndrome. Immunogenetics. 2001;53(6):435-439. doi:10.1007/s002510100358
2. Goswami, T.K., Singh, M., Dhawan, M. et al. Regulatory T cells (Tregs) and their therapeutic potential against autoimmune disorders - Advances and challenges. Hum Vaccin Immunother. 2022;18(1):2035117. doi:10.1080/21645515.2022.2035117
3. Meng, X., Layhadi, J.A., Keane, S.T., Cartwright, N.J.K., Durham, S.R., Shamji, M.H. Immunological mechanisms of tolerance: Central, peripheral and the role of T and B cells. Asia Pac Allergy. 2023 Dec;13(4):175-186. doi: 10.5415/apallergy.0000000000000128
4. Nobel Prize in Physiology or Medicine 2025. (2025). NobelPrize.org. https://www.nobelprize.org/prizes/medicine/2025/press-release/
5. Asano, M., Toda, M., Sakaguchi, N., Sakaguchi, S. (1996). Autoimmune disease as a consequence of developmental abnormality of a T cell subpopulation. The Journal of experimental medicine, 184(2), 387–396. doi: 10.1084/jem.184.2.387
6. Sakaguchi, S., Sakaguchi, N., Asano, M., Itoh, M., Toda, M. (1995). Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor alpha-chains (CD25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. Journal of immunology (Baltimore, Md.: 1950), 155(3), 1151–1164
7. Sakaguchi, S., Takahashi, T., Nishizuka, Y. (1982). Study on cellular events in postthymectomy autoimmune oophoritis in mice. I. Requirement of Lyt-1 effector cells for oocytes damage after adoptive transfer. J Exp Med. 1982 Dec 1;156(6):1565-76. doi: 10.1084/ jem.156.6.1565

Kaeli Alpha, OMS-II, is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2028. She is interested in pursuing a career in Child and Adolescent Psychiatry focused on patient-centered care. She is passionate about giving back to her local community and mentoring youth.

Blessina Babu, OMS-II, is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2028. She is passionate about providing care to underserved communities and believes that healthcare is a fundamental right, not a privilege.

Karen Johns, OMS-II, is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2028. She is interested in pursuing a career in oncology with a focus on cancer genetics. She is passionate about translating laboratory discoveries into clinical protocols that can measurably improve patient outcomes.

Ramaswamy Sharma, MS, PhD, is a Professor of Histology and Pathology at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life. Dr. Sharma serves on the BCMS Publications Committee.
By Claire Kowalick
Aleap forward in brain imaging has arrived in San Antonio. UT Health San Antonio’s Center for Brain Health, which opens in December 2025, is the first in Texas to house a Siemens MAGNETOM 7-Tesla Terra.X magnetic resonance imaging (MRI) system — one of the most advanced MRI technologies available. This scanner produces ultra-high-resolution brain images, offering a new tool for diagnosing and studying conditions like dementia, Alzheimer’s, Parkinson’s and other brain diseases.
Housed in the new Center for Brain Health, the 50,000-pound 7T Terra.X MRI system is an upgrade over conventional MRI scanners, which generally operate at 1.5 or 3 Tesla. MRI power is measured in Tesla units, with 7 Tesla representing a magnetic field strength more than 140,000 times that of Earth.
“This will improve detection of small metastases, multiple sclerosis lesions, and more. It does not replace the other MRIs in the Imaging Center and the Medical Arts & Research Center but rather expands what is possible,” said Ray Lee, PhD, radiologist with UT Health San Antonio and associate professor of radiology in the Joe R. and Teresa Lozano Long School of Medicine at The University of Texas at San Antonio.
Compared to standard MRI, the 7T offers dramatically improved resolution, especially in deep or complex regions such as the brainstem and temporal lobes. It can distinguish between small differences that may not be visible with lower-powered scans. For example, the 7T can more accurately distinguish between a benign blood vessel and an aneurysm.
“This MRI lets us see incredible detail, even without contrast, including deep structures like the brainstem where many diseases begin, and veins where amyloid is cleared,” said Sudha Seshadri, MD, DM, neurology professor at UT San Antonio and founding director of the Glenn Biggs Institute for Alzheimer’s and Neurodegenerative Diseases at UT Health San Antonio, which will move to its new home located in the Center for Brain Health building in December.
The scanner incorporates a dynamic parallel transmit architecture, which eliminates image distortion caused by magnetic field inhomogeneity — a common challenge in ultra-high-field MRI.
“With eight transmitters instead of two, we can dynamically adjust the magnetic field to create a more uniform image, allowing us to clearly see regions that used to be obscured,” Lee said. “This has become the new standard for 7T imaging.”
The system can also switch between research and Food and Drug Administrationapproved clinical modes in minutes.
“We’re right at the transition point where 7T MRI is becoming a clinical tool,” said Lee. “Currently, we are mostly research-focused, but we will eventually be able to scan patients with much greater accuracy.”
This flexibility is already enabling work on surgical planning for deep brain stimulation, substance use disorder research, and advanced diagnostics.
“This technology expands what is possible,” Lee said. “It will enhance research and discovery, right here in our community.”

Claire Kowalick is a science writer and senior public relations specialist at The University of Texas at San Antonio’s Health Science Center. She is a graduate of the University of North Texas. As a science writer, she combines her passion for writing with a deep appreciation of biomedical science to tell people about the groundbreaking research and novel discoveries happening at South Texas’ largest academic research institution.



On November 5, 2025, BCMS hosted its highly anticipated Annual Women Leaders in Medicine Awards Ceremony at the elegant UIW Skyroom, a venue befitting the occasion’s prestige. The event brought together a vibrant gathering of more than 400 physicians, healthcare professionals and community advocates from across Bexar County, all united in recognition of the honorees’ extraordinary contributions to patient care and medical leadership.
The event served as a powerful reminder of the vital role women continue to play in shaping the future of medicine — through innovation, mentorship and a steadfast devotion to service.
















WAYU Advanced Wound Clinic and Hyperbarics, Texas Indo-American Physicians Society, Southwest Chapter








The Colette M. Kohler, MD Awards stand as a tribute to the extraordinary dedication, leadership and vision that continue to shape the future of healthcare. Named in honor of Colette M. Kohler, MD, whose legacy embodies compassion, excellence and a steadfast commitment to advancing medicine, these awards celebrate women who exemplify the highest standards of service, innovation and patient care.


Steven Schenker Distinguished Professor in Medicine, Division Chief, Department of Gastroenterology & Nutrition

Associate Professor/Clinical Director, Pathology Residency Program, Department of Pathology & Laboratory Medicine

Professor, Vice Chair & Division Director for Education
Department of Obstetrics and Gynecology
Assistant Professor/Clinical & Associate Medical Director, Family Health Center Department of Family & Community Medicine

Crystal M. Manohar, MD, MBA, FASA
Professor/Clinical, Anesthesiology & Critical Care Vice Chair of Education & Residency, Program Director, Department of Anesthesiology

P.
Professor/Clinical Department of Ophthalmology
Associate Program Director, Assistant Professor/Clinical Division of Dermatology and Cutaneous Surgery

Associate Professor/Clinical & Director of Ultrasound, Department of Emergency Medicine

Associate Professor/Clinical Department of Radiology

Assistant Professor/Clinical Division of Nephrology, Department of Medicine

Associate Professor/Clinical, Director of Surgical Pathology Department of Pathology & Laboratory Medicine

Professor/Clinical Department of Radiology
We extend our deepest gratitude to the generous sponsors whose support made the 2025 Women Leaders in Medicine Awards possible. Their commitment to empowering women in healthcare ensures that the remarkable achievements of trailblazing physicians and medical professionals are recognized. By investing in this celebration, our sponsors are not only honoring today’s leaders but also helping to inspire the next generation of women who will shape the future of medicine.





























By Josh Andrews
As a physician, your time is your most valuable asset. Between patient care, charting, research and family, there are few hours left to actively manage investments. Yet, like many high-income professionals, you also face unique financial challenges: volatile stock markets, low yields from “safe” investments and inflation steadily eroding purchasing power. One investment approach gaining traction among physicians and other busy professionals is mortgage note investing. While not as widely known as real estate rentals or mutual funds, it offers compelling benefits — steady income, diversification and inflation protection — all without the headaches of being a landlord.
When someone buys a home or commercial property, they often take out a mortgage. That mortgage is a “note” — a legal promise to repay the loan with interest. Banks and other lenders frequently sell these notes to investors. As a mortgage note investor, you essentially step into the shoes of the bank. The borrower continues making payments, but instead of the bank collecting them, you do. The result: a steady stream of income backed by real estate collateral.
At Paper Profits, based in Austin, Texas, we specialize in purchasing and managing these notes for the benefit of our investors. The process allows busy professionals — like physicians — to participate in real estate in a completely passive way.
1. Steady, Predictable Income.
Unlike stock dividends or rental property cash flow that can fluctuate, mortgage notes are structured with clear payment schedules. Borrowers typically pay monthly, which provides a more consistent and reliable income stream. For physicians planning retirement, this predictability can be especially valuable.
2.
Most physicians are heavily concentrated in traditional assets — retirement accounts filled with mutual funds and perhaps some real estate. Mortgage notes represent a different asset class: debt secured by property. This
diversification helps reduce reliance on the stock market while still being rooted in the security of real estate.
3. Inflation Protection
With real inflation running higher than official numbers, preserving purchasing power is essential. Mortgage notes pay fixed interest rates, but unlike bonds, they are backed by tangible real estate. That security plus the ability to reinvest interest helps investors outpace inflation.
Safety: The first question most people ask is: Is this safe? No investment is without risk. But with notes, safety comes from the fact that they are backed by real estate. If a borrower defaults, the property serves as collateral. The key lies in proper underwriting and conservative loan-to-value ratios, so the investor has a margin of safety.
Liquidity: Unlike stocks, notes are not instantly liquid. A mortgage note is a contract with a defined term, and investors typically commit their money for a short period.
Defaults: Yes, borrowers sometimes stop paying. But in those cases, investors have options: restructuring the loan, selling the note, or foreclosing and taking control of the property. At Paper Profits, we carefully vet every loan we purchase, often buying at a discount, so there is built-in protection if a borrower runs into trouble. We also handle all day-to-day management; you don’t do anything but receive income each month.
The beauty of mortgage note investing — done through a managed fund — is that you don’t have to manage the details.
Consider this scenario: A borrower owes $200,000 on property worth $300,000. The borrower is paying 8% interest.
We purchase that mortgage note at $180,000.
The effective rate of return or yield is 12-15% or more depending on the details of the note and mortgage.
In this case, the investor earns steady income from the borrower’s payments and holds a loan well-secured by the property’s value. Even if the borrower defaults, the underlying collateral provides multiple exit strategies.
At Paper Profits, we’ve spent over a decade specializing in mortgage note investing. Based in Austin, Texas, we focus on purchasing and holding notes that generate reliable returns for our investors. Our process emphasizes risk management, careful loan selection and transparency.
Physicians and their families who invest with us often share similar goals:
• Reliable retirement income.
• Protection against inflation.
• A way to grow wealth without the stress of active management.
We understand that your time is best spent in your profession and with your family — not managing investments or monitoring the stock ticker. Mortgage note investing is designed to align with that reality.
If you’d like to learn more, I invite you to request a complimentary copy of the book Paper Profits: How to Buy and Profit from Notes –A Beginner’s Guide. This resource explains the basic strategies in detail and provides real-world examples of how mortgage note investing works. Request it here: www.PaperProfitsFund.com. I also welcome you to schedule a private consultation to see if this approach fits your financial goals.
Physicians dedicate their lives to caring for others. But your financial health deserves just as much attention as your physical health. Mortgage note investing is not a magic bullet — but it can be a powerful, steady and intelligent addition to your financial toolkit.
At Paper Profits, our mission is simple: help busy professionals like you protect and grow wealth with confidence.

Josh Andrews Founder, Paper Profits www.PaperProfitsFund.com
By Jacob Hernandez
On Saturday, November 1, Bexar County Medical Society’s Physician Wellness Committee joined the American Foundation for Suicide Prevention for the third year at the annual Out of the Darkness Community Walk for San Antonio and South Texas. At these events, teams of survivors, loved ones and groups such as BCMS walk to raise awareness and funding for suicide prevention efforts. This year, our team consisted of Dr. Mrudula Rao; Dr. Jennifer Rushton; Dr. Dan Deane; Dr. Gerardo Ortega and Mrs. Catherine Ortega; and BCMS CEO/Executive Director Melody Newsom.
The event begins with a ceremony and array of community resource tables at Nelson Wolff Municipal Stadium, followed by the walk itself, which follows a three-mile route from the Stadium past Levi Strauss Park, across Old Highway 90, abutting Rodriguez County Park, and around the Leon Creek Greenway South, before heading back to the Stadium. Our team greatly enjoyed the physical and community aspects of the walk, and were glad to continue this important tradition for yet another year. We will definitely be back for the fall 2026 walk!
A special thanks to WoodmenLife Chapter 4525 for a generous donation to cover the costs of Physician Wellness Committee T-shirts given to each attendee.





As a BCMS member, you can find exclusive discounts on premium products and services that you and your practice use every day.

Sol Schwartz & Associates P.C. (HHH Gold Sponsor)
Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Christopher Davis, CPA 210-384-8000, ext. 118 cbd@ssacpa.com www.ssacpa.com
“Dedicated to working with physicians and physician groups.”
CLA - CliftonLarsonAllen LLP (HH Silver Sponsor)
Transform complexity into opportunities. Work with professionals who understand the specific financial, operational, clinical, and strategic needs of physician practices and medical groups. Our team is made up of knowledgeable, accessible, and responsive individuals devoted to the health care industry.
Bryan Garcia
210-298-7924
Bryan.Garcia@CLAconnect.com CLAconnect.com
"We'll get you there."

Aspect Wealth Management (HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark President 210-268-1520
MClark@aspectwealth.com www.aspectwealth.com
“Your wealth. . .All aspects”

Atlas Retirement Strategies LLC (HHH Gold Sponsor)
Atlas Retirement Strategies LLC is a comprehensive financial planning firm dedicated to serving the unique needs of the medical community. We offer customized strategies in business planning, retirement planning, risk management, wealth preservation, estate planning, and wealth transfer – empowering healthcare professionals to achieve long-term financial security, clarity, and peace of mind.
David M. Webb, Ph.D., MSM, CLF, CLTC, LACP
Founder & Principal
210-281-4400
David@atlas-plans.com www.atlas-plans.com

Broadway Bank (HHH Gold Sponsor)
Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead 210-283-6640
TDuran@broadway.bank www.broadwaybank.com
“We’re here for good.”

Texas Partners Banks (HHH Gold Sponsor)
Our private banking team specializes in healthcare banking and will work with you to craft and seamlessly integrate financial solutions for you and your practice, including practice loans, lines of credit and custom local lockbox solutions headquartered in San Antonio.
Maria Breen 210-807-5562
Maria.Breen@texaspartners.bank www.texaspartners.bank

Lone Star National Bank (HHH Gold Sponsor)
Established in 1983, Lone Star National Bank has provided banking services to communities in South Texas for the past 41 years. LSNB is an independent and locally owned bank subsidiary of Lone Star National Bancshares-Texas, Inc with consolidated assets of $3 billion (12/31/23) and 36 full-service banking centers throughout Starr, Hidalgo, Cameron and Bexar counties. Aside from personal and business banking, LSNB offers investments, wealth management & trust along with property and casualty insurance, health insurance and supplemental coverage.
Ivan Corona Molina Assistant VP 210-479-4713
MolinaI@lonestarnationalbank.com www.lonestarnationalbank.com
“We do what the Little Banks can’t, and the Big Banks won’t!”
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Robert Lindley
SVP | Private Banking Team Lead 210-343-4526
Robert.Lindley@amegybank.com
Denise Smith
Vice President | Private Banking 210-343-4502
Denise.C.Smith@amegybank.com
Scott Gonzales
Assistant Vice President | Private Banking 210-343-4494
Scott.Gonzales@amegybank.com www.amegybank.com “Community banking partnership”
Synergy Federal Credit Union (HH Silver Sponsor)
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help physicians get the banking services they need.
Synergy FCU Member Services 210-750-8333 info@synergyfcu.org www.synergyfcu.org
“Once a member, always a member. Join today!”

Huffman Developments (HH Silver Sponsor)
Building spaces that inspire success. Huffman Developments specializes in custom commercial and medical projects from concept to completion. With over 40 years of experience, our team delivers high-quality, long-lasting facilities tailored to each client’s vision and business goals.
Steve Huffman
President 210-979-2500 x207 (direct) 210-213-2421 (cell)
SHuffman@huffmandev.com www.huffmandev.com
"Building Excellence One Project at a Time"

Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor)
Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for healthcare entities.
Betty Fernandez Director of Operations 210-582-6355
Betty.Fernandez@bexarcv.com www.bexarcv.com
“Proudly serving the medical community since 1998”

Avid Wealth Partners (HHH Gold Sponsor)
For over 15 years, Avid Wealth Partners has been the trusted financial partner for local physician specialists and practice owners. We specialize in physician-focused financial advising, offering proactive tax planning, customized investment strategies, and comprehensive risk management solutions. Our approach addresses every aspect of your
financial life, protecting your hardearned assets and building lasting wealth. With a team of credentialed specialists, we simplify complexity so you can focus on what you do best— caring for patients
MDWealth@avidwp.com
www.avidforphysicians.com
210-864-3333

Elizabeth Olney with Edward Jones (HHH Gold Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney
Financial Advisor
210-858-5880
Elizabeth.Olney@edwardjones.com www.edwardjones.com/elizabeth-olney

Aspect Wealth Management
(HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark President 210-268-1520
MClark@aspectwealth.com www.aspectwealth.com
“Your wealth. . .All aspects”
Hancock Whitney (HH Silver Sponsor)
Since the late 1800s, Hancock Whitney has embodied core values of Honor & Integrity, Strength & Stability, Commitment to Service, Teamwork and Personal Responsibility. Hancock Whitney offices and financial centers in Mississippi, Alabama, Florida, Louisiana and Texas offer comprehensive financial products and services, including traditional and online banking; commercial, treasury management, and small business banking; private banking; trust; healthcare banking; and mortgage services.
John Riquelme
San Antonio Market President 210-273-0989
John.Riquelme@hancockwhitney.com
Serina Perez
San Antonio Business Banking 210-507-9636
Serina.Perez@hancockwhitney.com

UT Health San Antonio
MD Anderson Cancer Center (HHH Gold Sponsor)
UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
UT Health San Antonio Physicians
Regina Delgado
Business Development Manager 210-450-3713
DelgadoR4@uthscsa.edu
UT Health San Antonio
MD Anderson Mays Cancer Center
Laura Kouba
Business Development Manager 210-265-7662
NorrisKouba@uthscsa.edu
Appointments: 210-450-1000
UT Health San Antonio 7979 Wurzbach Road San Antonio, TX 78229

Golden Billing & Benefits
(HHH Gold Sponsor)
Golden Billing is owned and operated for over 20 years in Houston, TX. The owner, Marcus Yi, is focused on creating a partnership with clients. We are dedicated to optimizing the small business doctor’s productivity and maximizing practice cash flow by accurate claims coding and timely processing. Call today for a free consultation. If you don’t want to use us at lease maybe we can help you fine tune your decision.
Marcus Yi
713-263-0054
MYi@goldenbilling.com www.goldenbilling.com

Genuine Health Group (HHH Gold Sponsor)
Genuine Health Group partners with primary care providers to help them successfully adopt value-based payment models and demonstrate better health outcomes. Providers choose us for our proven expertise and consistency both for their patients enrolled in Medicare Advantage plans
and for their patients with traditional Medicare who can align with one of ACOs. We have a track record of effectively reducing the cost of care while simultaneously improving care quality.
786-878-5500
info@genuinehealthgroup.com www.genuinehealthgroup.com
Equality Health
(HH Silver Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos
Network Development Manager 210-608-4205
CLeos@equalityhealth.com www.equalityhealth.com “Reimagining the New Frontier of Value-Based Care.”
SpeedEz’s (HH Silver Sponsor)
For over three decades, SpeedE’z has been Bexar County’s truly local partner for answering service, contact center and courier solutions. R.N. owned and family-led, we combine compassionate care with professional expertise. Our HIPAA Certification, SOC 2 Type II Compliance and Woman-Owned HUB status reflect our commitment to integrity and security. Ranked Top Ten nationally in the ATSI Award of Excellence, our team delivers results that stand out – rooted right here in San Antonio!
Lauren Garza President 210-615-0964 Lauren@speedez.com https://speedez.com
DialOPS
(H Bronze Sponsor)
Dialops is a trusted U.S.-based medical answering service and virtual receptionist solution designed specifically for healthcare practices. We provide 24/7 live call handling, HIPAA-compliant messaging, appointment scheduling, and reliable after-hours and overflow support. Our medically trained agents answer every call with professionalism and care— just like your in-office staff—ensuring your patients always feel heard and supported. From solo providers to busy clinics, Dialops helps reduce missed calls, ease front desk overload, and improve the patient experience—all at a fraction of the cost of hiring in-house. Rachel Caero Rachel@dialops.net 877-2-DIALOPS/210-699-7198 www.dialops.net

TMA Insurance Trust (HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service insurance agency offering a full line of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.
Wendell England Director of Member Benefits 512-370-1746
Wendell.England@tmait.org 800-880-8181 www.tmait.org
“We offer BCMS members a free insurance portfolio review.”

Texas Medical Liability Trust (HHHH 10K Platinum Sponsor)
With more than 20,000 healthcare professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of healthcare for patients by educating, protecting and defending physicians.
Patty Spann
Director of Sales and Business Development 512-425-5932
Patty-Spann@tmlt.org www.tmlt.org
“Recommended partner of the Bexar County Medical Society”
MedPro Group (HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze, RPLU, ARM
AVP Market Manager, SW Division 512-658-0262
Fax: 844-293-6355
Kirsten.Baze@medpro.com www.medpro.com
Continued on page 42
LASO Health Telemedicine and Rx App
(HH Silver Sponsor)
LASO Health is the industry’s only solution that makes healthcare services accessible, cost-transparent and convenient. Its mission is to reinvent “healthcare” in the United States by empowering every individual and employer, insured or uninsured to have easy, timely, predictable, cost-effective care.
LASO combines an intuitive, mobile superapp with a marketplace of virtual and in-person health services to give customers a one-touch, onestop-shop, comprehensive health solution.
Ruby Garza, MBA
210-212-2622
RGarza@texaskidneycare.com www.lasohealth.com

EnviroMerica
(HHHH 10K Platinum Sponsor)
Eliminate all liabilities caused by non-compliance with state and federal regulations and enjoy true peace of mind. Protect your practice by becoming audit proof as a subscriber to our compliance software that’s affordable and guaranteed. We have been protecting physicians for over 27 years and in 2013 were selected as the exclusive vendor of choice for compliance and medical waste by the 2nd largest Medical Association in the nation.
Work with certified experts who understand the specific compliance requirements imposed by OSHA, HHS/OCR (HIPAA), Boards, DOT, EPA, DTSC, CMS & many more. Everything we do, say, or develop for is guaranteed against fines and backed by our insurance policy that covers all our clients for up to $2 Million per occurrence. This is true peace of mind that is invaluable.
Julian Goduci
Founder/CEO
1-888-323-0583 or 650-655-2045
JulianG@enviromerica.com
Enviromerica.com
"Providing True Peace of Mind."
Henry Schein Medical (HH Silver Sponsor)
From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving officebased practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Kelly Emmon
Field Sales Consultant
210-279-6544
Kelly.Emmon@henryschein.com www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”
SpeedEz’s (HH Silver Sponsor)
For over three decades, SpeedE’z has been Bexar County’s truly local partner for answering service, contact center and courier solutions. R.N. owned and family-led, we combine compassionate care with professional expertise. Our HIPAA Certification, SOC 2 Type II Compliance and Woman-Owned HUB status reflect our commitment to integrity and security. Ranked Top Ten nationally in the ATSI Award of Excellence, our team delivers results that stand out – rooted right here in San Antonio!
Lauren Garza
President 210-615-0964
Lauren@speedez.com https://speedez.com
Methodist Physician Practices (HH Silver Sponsor)
Methodist Physician Practices is committed to providing exceptional care for patients in greater San Antonio and South Texas. As part of Methodist Healthcare, we are dedicated to raising the standards of performance excellence while advancing the health and well-being of the communities we serve. Our extensive network of highly-skilled primary care physicians, specialists and surgical care providers ensures patients receive comprehensive, coordinated and compassionate care.
As part of the Methodist Healthcare System, our physicians are
committed to delivering personalized, high-quality services that meet the diverse needs of our patients. At Methodist Physician Practices, we go beyond healthcare — providing hope, healing and unwavering support for each individual we serve.
Erin Fitzgerald
Methodist Healthcare I Methodist Physician Practices M:281-673-7350
methodistphysicianpractices.com
The Health Cell (HH Silver Sponsor)
“Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more!
Kevin Barber President 210-308-7907 (Direct) KBarber@bdo.com
Valerie Rogler Program Coordinator 210-904-5404
Valerie@thehealthcell.org www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA) (HH Silver Sponsor)
SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising.
Jeannine Ruffner President info4@samgma.org www.samgma.org

Favorite Healthcare Staffing
(HHHH 10K Platinum Sponsor)
Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle.
San Antonio Office 210-301-4362
www.favoritestaffing.com
“Favorite Healthcare Staffing offers preferred pricing for BCMS members.”


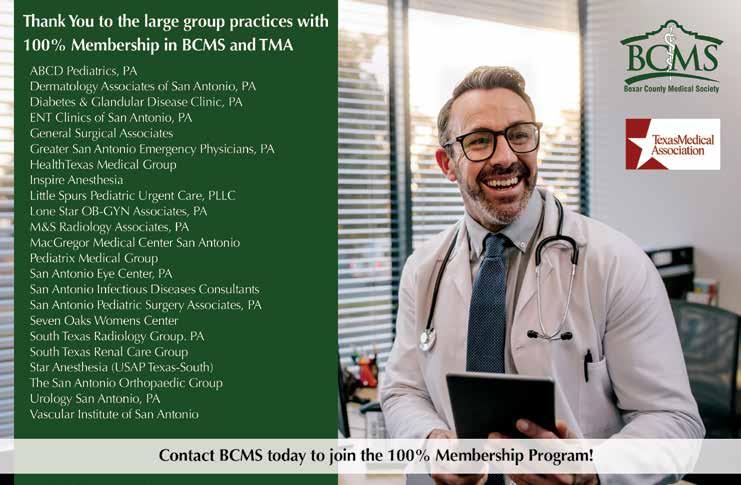

By Stephen Schutz, MD
The full-size luxury SUV is a mostly American creation, with the introduction of the Lincoln Navigator and Cadillac Escalade in the late 1990s. Almost 30 years later, the Navigator continues to deliver on the big SUV brief — towering road presence, palatial interior space and lots of luxury. But in a hyper-competitive (and lucrative) market where the Cadillac Escalade embraces extroversion and the Mercedes GLS leans into continental refinement, Lincoln is leading with comfort and understated elegance rather than cutting-edge technology or driver involvement.
Lincoln carries over its proven Ford F150-derived 3.5-liter twin-turbocharged EcoBoost V6, which produces 440HP and 510 lb-ft of torque. That betters the Escalade’s 420HP or the Mercedes GLS450’s 375HP, by the way, and the Navigator’s V6 synchs with a 10-speed automatic transmission and standard rear-wheel drive, with all-wheel drive optional. Acceleration is brisk for a vehicle tipping the scales at over 6,000 pounds. Expect a 0–60 mph run in the mid-five-second range, plenty for merging or passing with confidence. What impresses more than raw speed is how unobtrusive the drivetrain feels — power delivery is smooth, turbo lag minimal and the transmission fades into the background.
Fuel economy remains decent for the class but still pretty lousy: 16 MPG City and 22 Highway. Obvs, anyone considering this SUV isn’t cross shopping it with a Toyota Prius.
The Navigator rides on the F150’s body-on-frame architecture shared with the Expedition, but Lincoln dresses it up with an adaptive suspension system that includes road-previewing cameras. The result is a ride quality that’s surprisingly good for a vehicle with

such mass and height. Broken pavement is ironed flat, and highway cruising feels almost limousine-like. Handling is not the Navigator’s strong suit, as you’d expect. The steering is light and numb, body motions are controlled but obvious, and the Navigator cries “Uncle” quickly if you push it on a winding road. Buyers comparing it with a BMW X7 or Mercedes GLS will immediately notice the lack of sportiness, but Lincoln, understanding its customers, focused on comfort and silence rather than athleticism.
Oh, by the way, the Navigator, like all big American SUVs based on full-size pickup trucks, is difficult to park. I suspect 0% of readers will be surprised by that.
Visually, the 2025 Navigator received only minor updates compared with the last version. The front fascia carries a wide chrome grille flanked by adaptive LED headlights, and Lincoln has resisted the urge to exaggerate its proportions further. Where Cadillac’s Escalade is angular and aggressive, the Navigator strikes a softer, more understated stance. The Navigator is still a massive hunk of SUV, especially in the extended L variant, but the clean lines and restrained detailing minimize visual bloat. New wheel designs of up to 24 inches add some flash, and a few fresh paint colors broaden its appeal. The rear is dominated by a full-width LED light bar, a design element that continues to give the Navigator a modern but not overly trendy signature at night.
Step inside, and the Navigator reminds you why people buy these behemoths. The interior is gigantic, with three rows of seating that can actually accommodate real adults, even if you don’t choose the L. The second row can be outfitted with captain’s chairs or a bench, and the



third row remains one of the roomiest in the class. Cargo space in the standard-wheelbase model is excellent, while the long-wheelbase L is just huge.
Leather upholstery, genuine wood trim and soft-touch surfaces abound, and the color combinations feel warmer than in many German competitors.
Tech is a mixed bag. The 13.2-inch infotainment screen runs a slick version of Ford’s Sync 4 system, which integrates wireless Apple CarPlay and Android Auto. But the overall design of the interface feels more conservative than cutting-edge, and Lincoln doesn’t match Cadillac’s wow-factor OLED display setup.
On the safety front, Lincoln equips the Navigator with a robust suite of driver assists, including adaptive cruise with lane-centering, intersection assist and hands-free driving via Lincoln’s BlueCruise. BlueCruise is now an outstanding system, and no way would I buy a Navigator without it.
Pricing starts in the low $90,000s for the base model and climbs past $115,000 fully loaded. It’s reasonable to expect average transaction prices to be around $100,000.
The Navigator remains an excellent option for buyers who want a traditional full-size luxury SUV. It doesn’t scream for attention like the Escalade, nor does it chase European athleticism. Instead, it leans into calm refinement, a plush interior and a distinctively American sense of scale. If you want a big luxury SUV that whispers rather than shouts, the Navigator remains a solid choice.

Stephen Schutz, MD, is a board-certified Gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.




11911 IH 10 West San Antonio, TX 78230
Coby Allen 210.725.5447
Northside Honda 9100 San Pedro Ave. San Antonio, TX 78216
Daniel Garcia 210-988-9644
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Rick Cavender 888-901-8483
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Emilio Gonzalez 210-341-3311
Bluebonnet Chrysler
Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Don Bartholomew 830-606-3463
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX 78006
William Taylor 830-981-6000
14610 IH 10 West San Antonio, TX 78249
Mark Hennigan 210-941-4556
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX 78216
James Godkin 210-366-9600
North Park Lexus 611 Lockhill Selma San Antonio, TX 78216
Jose Contreras 210-308-8900
9455 IH 10 West San Antonio, TX 78230
Jordan Trevino 210-738-3499
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX 78257
James Cole 210-816-6000
Northside Ford 12300 San Pedro San Antonio, TX 78216
David Starnes 210-319-5684
North Park Lincoln 9207 San Pedro San Antonio, TX 78216
Sandy Small 210-341-8841
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Steven Markham 726-226-0028
Cavender Toyota 5730 NW Loop 410 San Antonio, TX 78238
Spencer Herrera 210-862-9769
North Park Toyota 10703 SW Loop 410 San Antonio, TX 78211
Justin Boone 833-669-2401
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson 888-718-9510


