













PUBLISHED
Traveling Blender, LLC. 10036 Saxet Boerne, TX 78006
PUBLISHER: Louis Doucette louis@travelingblender.com
BUSINESS MANAGER: Vicki Schroder vicki@travelingblender.com
GRAPHIC DESIGNER: Jennifer Nelson jennifer@travelingblender.com
Sandy Weatherford sandy@travelingblender.com SAN ANTONIO: Gerry Lair gerrylair@yahoo.com
For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.
San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EDITORIAL CORRESPONDENCE:
Bexar County Medical Society 4334 N Loop 1604 W, Ste. 200 San Antonio, TX 78249
Email: editor@bcms.org
MAGAZINE ADDRESS CHANGES: Call (210) 301-4391 or Email: membership@bcms.org
SUBSCRIPTION RATES: $30 per year or $4 per individual issue
ADVERTISING CORRESPONDENCE: Louis Doucette, President Traveling Blender, LLC.
A Publication Management Firm 10036 Saxet, Boerne, TX 78006 www.travelingblender.com
For advertising rates and information Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national origin, or an intention to make such preference limitation or discrimination.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2025 SmithPrint, Inc. PRINTED IN THE USA


John Shepherd, MD, President
Lyssa Ochoa, MD, Vice President
Jennifer R. Rushton, MD, President-Elect
Lubna Naeem, MD, Treasurer
Lauren Tarbox, MD, Secretary
Ezequiel “Zeke” Silva, III, MD, Immediate Past President
Woodson “Scott” Jones, Member
John Lim, MD, Member
Sumeru “Sam” G. Mehta, MD, Member
M. “Hamed” Reza Mizani, MD, Member
Priti Mody-Bailey, MD, Member
Dan Powell, MD, Member
Saqib Z. Syed, MD, Member
Nancy Vacca, MD, Member
Col Joseph J. Hudak, MD, MMAS, Military Representative
Jayesh Shah, MD, TMA Board of Trustees Representative
John Pham, DO, UIW Medical School Representative
Robert Leverence, MD, UT Health Medical School Representative
Cynthia Cantu, DO, UT Health Medical School Representative
Lori Kels, MD, UIW Medical School Representative
Ronald Rodriguez, MD, UT Health Medical School Representative
Alice Gong, MD, Board of Ethics Representative
Melody Newsom, BCMS CEO/Executive Director
George F. “Rick” Evans, Jr., General Counsel
Melody Newsom, CEO/Executive Director
Brissa Vela, Chief Membership & Development Officer
Yvonne Nino, Controller
Betty Fernandez, BCVI Director of Operations
Phil Hornbeak, Auto Program Director
Al Ortiz, Chief Information Officer
Jacob Hernandez, Advocacy and Public Health Specialist
Jennifer C. Seger MD, Chair
Timothy C. Hlavinka, MD, Member
John Robert Holcomb, MD, Member
Soma S. S. Jyothula, MD, Member
George-Thomas Martin Pugh, MD, Member
Adam Ratner, MD, Member
Rajam Ramamurthy, MD, Member
Patrick Reeves, MD, Member
John Joseph Seidenfeld, MD, Member
Amith Skandhan, MD, Member
Francis Vu Tran, MD, Member
Subhashini Valavalkar, MD, Member
Louis Doucette, Consultant
Brissa Vela, Staff Liaison
Gabriella Bradberry, Staff Liaison
Trisha Doucette, Editor
Ayomide Akinsooto, Student
Elizabeth Allen, Volunteer
Rita Espinoza, DrPH, Volunteer
Ramaswamy Sharma, MS, PhD, Volunteer

from your good work instead of investors?
We’re rewarding eligible Texas members with a 5% dividend. Does your malpractice liability insurer do that?
At The Doctors Company we answer only to physicians like you. Not Wall Street. That’s why we’re able to award a 5% earned dividend to our eligible Texas members this year. Altogether, we’re returning $15.1 million to doctors in 2025, which brings the total dividend payments we’ve shared with physicians to $485 million.



By John Shepherd, MD, President, Bexar County Medical Society
People are more than their titles. I’ve sat in enough rooms to know that what makes someone a strong leader — or a great teammate — often has little to do with their job description. It’s the stories behind the roles — the life experiences, values and relationships that shape how they show up.
That’s why I wanted to share our board with you in a way that goes beyond the usual list of accolades. Yes, this is a group of incredibly accomplished people — but more importantly, they’re thoughtful, curious, grounded and human. They’ve built careers, yes, but also families, communities and lives filled with growth, challenge and meaning.

Their leadership is informed by all of it — the pivots and reinventions, the personal wins, the hard lessons, the people they love and the causes they care deeply about. That kind of richness doesn’t always make it onto a resume, but it’s what gives our board depth and heart.
So, as you read through these stories, I hope you’ll get more than just a snapshot of what each person has accomplished. I hope you’ll get a sense of who they are. And if something sparks a connection — reach out. These aren’t just bios. They’re an open door.
If you had told me 30 years ago that I’d one day trade my jump boots for a tractor and bee hives, I probably would’ve laughed. But life has a way of surprising you. After 18 years in the U.S. Army — some of that time as an Airborne paratrooper and later as the senior Flight Surgeon with the 160th Special Operations Aviation Regiment — I’ve found myself living a very different kind of adventure with my wife, Jenny.
My time in the Army was intense, humbling and full of purpose. The 160th — better known as the Night Stalkers — is a unit that flies missions in some of the toughest conditions imaginable. Working with the world’s most elite aviators taught me lessons I carry with me to this day. But after nearly two decades in uniform, I knew it was time for a new chapter.
I left special operations to pursue a residency in anesthesia, followed by a fellowship in pediatric anesthesia. That path led me to the U.S. Army Burn Unit in San Antonio, where I served as Chief of Anesthesia. Working with critically burned patients and their families — witnessing their courage and resilience — was an experience that shaped me deeply, both professionally and personally.
These days, life looks a little different — but just as full. Jenny and I have backpacked nearly half the Colorado Trail, explored the raw beauty of Antarctica, and even crawled through the narrow, winding Cu Chi tunnels in Vietnam — a sobering reminder of history and human endurance. Whether it’s watching the silliness of penguins on

ice or navigating a claustrophobic maze underground, travel reminds us how big the world is — and how much there is to learn from it.
At home, we love our weekends of biking or hiking the local trails around San Antonio or unwinding at our ranchette just outside the city. I still play indoor box lacrosse, a longtime passion that keeps me on my toes and connected to a sport I’ve loved since I played in college.
But the real heart of my life is our family. Time with our daughter Anna and her husband Zach, our son Adam and his wife Allie, and our sweet granddaughter Lucia brings a joy that no title or career could match. Our ranchette just outside the city is our gathering place, where we share slow evenings, board games and good bourbon on the porch while watching the sunset.
From Army greens to OR scrubs to beekeeping suits, my journey has taken some unexpected turns. But through it all, it’s the moments with the people I love — at home, on a trail or around a table — that have truly made it all worthwhile.


I’m Dr. Lyssa Ochoa, a board-certified vascular surgeon and the founder of the San Antonio Vascular and Endovascular Clinic (The SAVE Clinic), which I established in 2018 to serve the communities of South San Antonio. My mission is simple but urgent: to reduce the devastating number of diabetes-related amputations that occur in our city’s most underserved zip codes — rates that are up to three times the already-high state average.
I was born and raised in the Rio Grande Valley along the Texas-Mexico border, where I learned early on about the resilience of communities facing systemic inequities. After completing medical school, general surgery residency and vascular surgery fellowship at Baylor College of Medicine in Houston, I began practicing in San Antonio in 2011. Six years later, I made the decision to leave a large private group and open my own clinic — one that would be mission-driven and embedded in the communities most in need.
One of my proudest achievements has been building the only ambulatory surgery center on the Southside of San Antonio. It’s more than just a facility — it’s a platform for a community-based approach to addressing the root causes of health disparities. It represents a model of care where patients are seen, heard and treated with dignity.

My work extends beyond the clinic walls. I partner with schools, universities and nonprofits to mentor students, lead health equity research, and support programs like Healthy Corner Stores, Siclovia, Fit Family Challenge, Health Confianza and SA Ready to Work.
During the pandemic, I was honored to help lead the effort to bring a mass vaccination site to the Southside.
In 2024, I became the founding Chair of the Center for Health Equity in South Texas (CHEST), a nonprofit that unites cross-sector partners to tackle the social and structural barriers to health. Through CHEST, we are building lasting, collaborative solutions for our region.
What keeps me going is the resilience and compassion I witness every day — from my patients, other professionals and friends, as well the many students who walk this journey with me.
On weekends, I love taking long walks with my three dogs — Conan, Didi and Suzy — and riding bikes with my husband along the Salado Creek Trail. It’s where I reconnect, reflect and recharge.
My vision is to create a healthcare system grounded in equity, powered by community, and led with heart.


I chose medicine as a profession when I was around 12 years old, after my grandfather lived with us as he suffered from advanced prostate cancer. I made visits to the hospital with him and was in awe of the environment. I admired the physicians that cared for him, and I was fascinated by the technology around me. All these years later, as a pathologist, I love being a hospital-based physician, consulting with colleagues in virtually all other specialties regarding laboratory testing and differential diagnoses. The advances in diagnostic technology are one of reasons I chose to specialize in hematopathology and molecular genetic pathology. Pathology is a challenging and rapidly changing field that keeps me learning new things every day.
Serving as the System Medical Director for Pathology and Laboratory Medicine for Baptist Health System is the part of my career that I am most proud of. It is my responsibility to ensure that the medical staff across all our hospitals have the laboratory testing they need to take care of our patients. This requires bringing in new tests when needed, which is a difficult undertaking that requires many resources. In the end, providing valuable results in a timely manner makes it completely worthwhile.
I became involved with BCMS because I am passionate about service and representation. When I first started working in San Antonio, I was usually the youngest person in the room, and often the only woman and Mexican American. I quickly realized that my perspective was unique and important to these groups. Through BCMS, I realized the power of advocacy and how one person can truly impact our patients’ lives and our ability to practice medicine.
When I’m not working, I enjoy relaxing at home with my husband and our five cats, reading, listening to music, and taking walks around the neighborhood. I also like trying to learn new languages; I’m currently working on Portuguese and German. I love to travel in my free time. I cherish taking trips with my parents and girls’ trips with my dearest friends. My husband and I enjoy taking trips inspired by musicians we want to see in concert. We’ve seen the Rolling Stones in four different U.S. cities, Radiohead in Barcelona and heard Mozart performed in the Vienna concert hall. I’m also passionate about philanthropy, especially animal welfare and environmental causes, as well as the Fiesta Commission. I am an active member of Impact SA, a nonprofit women’s collective-giving grant-making organization helping to improve our San Antonio community.



I am an Internal Medicine physician, experienced leader and tireless healthcare advocate, dedicated to advancing a health system that is equitable, patient-centered and physician-led. Currently serving as Treasurer of the Bexar County Medical Society (BMCS) — following an impactful term as Secretary — I combine frontline clinical experience with statewide and national advocacy to turn member voices into meaningful action and measurable change.
I serve on the Texas Medical Association’s Council on Legislation, where I help shape health policy across the state. I am a regular presence at First Tuesdays at the Capitol, meeting with lawmakers to promote pro-medicine legislation, and have represented BCMS at the AMA National Advocacy Conference. Recently, I testified at a Texas Senate hearing to oppose SB 3055, which would have expanded independent practice for nurse practitioners — strongly defending the value of team-based, physician-led care.
My advocacy also extends nationally to visa reform for international medical graduates (IMGs), ensuring that young physicians can enter residency programs on time, and serve in communities that need them the most. During the COVID-19 pandemic, I served as Communications Chair for the BCMS COVID-19 Task Force, leading vital public health outreach.
I’ve proudly led public health initiatives around childhood obesity prevention, breast cancer awareness and youth education, and I am deeply committed to mentoring medical students — inspiring and guiding future physicians with compassion and integrity. For my leadership and commitment to advocacy, I was honored with the Women in Medicine Leadership Award by BCMS.
As an IMG myself, with hands-on experience in rural health collaboratives, I understand the need to bridge healthcare gaps. I advocate for legislation that supports physician-led teams and equitable care in rural communities, drawing inspiration from the visionary leadership of my fellow BCMS members, Executive Committee and Board, as well as TMA President Dr. Jayesh Shah.
Beyond my professional roles, I am the wife of Dr. Muhammad Naeem, a gastroenterologist, and mother to our two children, Hamza and Soni. I find joy in traveling, connecting with others, and building strong vibrant communities.



I grew up in Corpus Christi, Texas and still love to visit the beach with my family. I am married to Dr. Jake Mancuso (interventional cardiologist with CCSA) and we have three beautiful children — James 11, Claire 9, and Charlotte 7. I attended Southern Methodist University as a President’s Scholar and graduated with a Bachelor of Science in Chemistry with a minor in Psychology.
After college, I moved to San Antonio and was a ‘lifer’ at UT Health Science Center at San Antonio, finishing medical school, internship, residency, chief residency and nephrology fellowship at this esteemed institution.
I now practice Adult Nephrology with South Texas Renal Care Group, focusing in the Northeast area of San Antonio. I chose nephrology to be able to walk with my patients down a hardship-filled road to provide support and compassion along the way, celebrating the transplants and victories, as well as heartbreaking times with the love I share with my patients. Nephrology is a specialty of family and relationships, of complicated diseases, and the importance of maintaining dignity while navigating difficult choices, and I love every aspect of this career I am building.
In my free time, I enjoy traveling, cooking large holiday meals, watching movies with popcorn, driving to the Hill Country to see the fireflies, and being with my family, but I love the balance between being the mother of three — sprinting to ballet and lacrosse while checking boxes for camps in the summer or upcoming recitals — to the physician of many — being a female physician means always wearing several different hats, or shoes!
Every year is a new challenge with a growing family but I hope to be an example to my kids, showing balance, grit and what love can do for everyone around you. Truly listening and showing empathy along with expertise with experience builds a strong practice as well as solid relationships and this is what I hope to embody for my family and patients.
I love San Antonio and what the city has given me, and I’m excited to continue to share the bond of the physicians and healthcare teams to see what can be accomplished in the future.
With my family at my side, I will watch Pooch Parade every year and enjoy the Christmas lights on the River Walk as carols ring along the stones. I’m excited to serve on the Board of Bexar County Medical Society as Secretary and work along with the physicians of BCMS to enhance the medical community of San Antonio.






My path to medicine was relatively traditional, shaped by a deep love of science and early admiration for my hometown family physician. Growing up in a small Texas town, I saw firsthand how one dedicated doctor could make an enormous difference in the lives of others. That example left a lasting impression on me and made “Pre-Med” a natural choice when I enrolled at the University of Texas. From there, my journey into medicine took root and never wavered. I found an outstanding practice in the South Texas Radiology Group, which I joined in 2002. I have always believed that physicians must have a strong and visible presence in the institutions and conversations that shape our work. That belief is what drives my service to the Bexar County Medical Society and other professional organizations. Medicine is an incredible profession, and we as physicians have a responsibility to advocate for our patients, our colleagues and our ability to practice with integrity. Too often, decisions that affect clinical care are made without meaningful physician input. Whether in the legislature, in regulatory agencies or within hospital systems, physicians must provide the expertise and perspective that only we can offer.

From a personal standpoint, one of my proudest accomplishments was completing an Ironman triathlon in 2012. The months of preparation and discipline required to cross that finish line taught me lessons that still resonate in my daily life.
From an advocacy perspective, I’m especially proud to have led the effort to pass the Life of the Mother Act earlier this year — a piece of legislation that protects physicians’ ability to provide medically necessary care during pregnancy complications. It was a meaningful, hardwon victory.
Outside of medicine, I’m fortunate to have a wonderful family. My wife and I recently celebrated our 25th wedding anniversary, and we are proud parents to two remarkable young adult children who continue to inspire us.
In my spare time, I enjoy playing golf and spending time outdoors. My favorite book is Love in the Time of Cholera by Gabriel García Márquez, and my favorite movie — fittingly Texan — is Urban Cowboy. I’ve always dreamed of visiting Asia, and hope to make that trip in the next couple of years.


Leaders of the Bexar County Medical Society Alliance (BCMSA) have long been recognized for their dynamic influence. Locally, our BCMSA leaders are instrumental in advancing public health initiatives, supporting medical families, and fostering community partnerships that promote wellness and education.
Through TMAA, they help shape health policy, advocate for legislative priorities, and mentor emerging leaders across Texas.
1. Hometown: Kingwood, Texas
2. As a child, what did you want to be when you grew up? In business, like my dad, (or alternatively, a dolphin trainer at SeaWorld!)
3. Academics/Training: Proud Aggie Bachelor of Business Administration and Masters Marketing & Statistics
4. Family: Dr. Benjamin Webb and son Luke (16) as well as parents Hans and Constance Kohler — Minana and Opa Extraordinaire!
5. Pets: Too many dogs to mention (just like Jenny!)
6. Places I've lived: Houston, College Station, Austin, LA, San Antonio
7. Year I moved to San Antonio: 2007
8. Favorite Places to Travel: South Coast of England, Germany, Bermuda, California
9. Hobbies: Running, English Equestrian, Barre Class, Walking Dogs, Cooking
10. BCMSA Leadership: Secretary (2022) President (2024), Steering Committee (2025)
11. TMAA/AMAA Leadership: TMAA Board Secretary, TMAA Resource Liaison
12. Fun Fact others may be surprised to learn about you: I'm also a British Citizen!

On the national stage, they contribute to the AMAA, where they bring Texas perspectives to broader conversations about healthcare advocacy, physician family support and national health campaigns. Two of our 2025 BCMSA leaders are Victoria Kohler-Webb and Jenny Shepherd, and while their influence is well-known, we thought we would share a few Fun Facts about these hard-working, dedicated women!
1. I’m a midwestern girl born in Illinois surrounded by cornfields and soybeans, and educated in Indiana — I love my Hoosiers!
2. I wanted to be a “pet-inarian” when I was younger, which didn’t happen but I seem to be a collector of large, needy dogs. We’ve had 11 dogs and 10 other species — everything from cats to snakes and rats.
3. I started my professional career as an audiologist for the DOD in El Paso where John (another midwesterner) and I met.
4. My number one “want to travel to” is India. My daughter Anna spent a summer there and said the Taj Mahal was overrated compared to the rest of India. I’ll see for myself.
5. I read over 100 books a year across all genres. While my favorite book is probably The Talisman by Stephen King or Enchanted by Orson Scott Card, I’m currently reading a bio of Eleanor Roosevelt.
6. I loved the 14 years I spent as an army wife and am really proud of the work John and I both did to serve soldiers and their families.
7. My favorite movie is It’s a Wonderful Life. I watch it at least once, if not more each year, always reminding myself you don’t always easily see the differences you make in the world.
8. Leadership in medicine? I’ve done a little bit of everything across TMA, Alliance, TEXPAC and Foundation but what I love best is teaching others about the power of legislative relationships and advocacy.
9. I’m an incredibly competitive board game player and take our family’s March Madness tournament betting bracket seriously.
10. John and I have climbed six of Colorado’s 14k peaks together.



By Robert Horn, MD
New cancer diagnoses are expected to rise globally through the 21st century to an estimated 35 million cases per year in 2050 — a 77% increase from 2022.1 Additionally, trends over the last decade have shown that cancer diagnoses in younger populations, specifically in breast and gastrointestinal cancers,2 are changing the ways in which healthcare providers have approached everything from screening to treatment. The healthcare sector is rising to meet this challenge through a variety of modalities, including new therapeutics and refinement of established paradigms. However, at the forefront of the effort are changes with regards to cancer screening. In 2021, The United States Preventive Service Task Force decreased the recommended age for colon cancer screening to 45 and recently in April of this year, recommended biennial mammography for breast cancer screening to start at age 40, lowered from age 50 in 2016.14
The causes of these trends are thought to likely be multifactorial, with diet, obesity and environmental exposures all playing a role. Healthcare providers are striving to not only discover these cancers early but also provide their patients with information to decrease and understand their individual risk. As it is summertime, there is a certain utility in exploring some of these environmental factors that patients may come across during these warm months. The first thing that comes to mind are back yard cookouts and brews poolside with friends and loved ones.
The health detriments of excessive alcohol consumption are reasonably well known, specifically with regards to liver disease, heart disease, stroke and injuries from alcohol-related accidents. However, even modest consumption of alcohol conveys increased risk for a variety of different cancers. In January of 2023, The Canadian Centre on Substance Use and Addiction published a report stating that even drinking between three and six standard drinks per week raised an individual’s risk of developing cancer.3 This amount of alcohol is significantly lower than
what is considered a moderation level of consumption in the Dietary Guidelines for Americans produced by the U.S. Department of Agriculture and U.S. Department of Health and Human Services, at seven drinks per week for non-pregnant woman and 14 drinks for men.4 The carcinogenic effect is thought to not be directly from ethanol but rather acetaldehyde, one of the metabolic by-products from its oxidation.
Several studies have established the increased risk for cancer with moderate to heavy alcohol consumption, but the risk does vary somewhat across tumor types. One such meta-analysis published in 2015 showed a strong correlation with a relative risk (RR) for oral cavity and pharyngeal cancer of 1.83 (95% CI: 1.62 – 2.07) in moderate alcohol consumption and 5.13 (95% CI: 4.31 – 6.10) with heavy consumption — a similar pattern in Laryngeal cancer with a RR of 1.44 (95% CI: 1.25 – 1.66) in moderate drinkers and 2.65 (95% CI: 2.19 – 3.19) in heavy drinkers. Additionally, alcohol was also found to convey an increased RR for breast cancer with a relative risk of 1.23 (95% CI: 1.19 – 1.28) in moderate drinkers and 1.61 (95% CI: 1.33 – 1.94) with heavy alcohol consumption.6 While the risk from alcohol consumption has been observed independent from several confounders, including tobacco use, there has been a documented compounding effect where individuals who smoke and drink have an increased cancer risk compared to those who only smoke or only consume alcohol.7
Colon cancer, currently being the third most frequent in terms of incidence and second overall in mortality, has been on somewhat of a decline in high-incidence countries, such as the United States. This is thought to be largely due to changes towards a healthier lifestyle and improvements in screening.1 However, it is still important to identify those who may be at higher risk, either from inherited, familial or genetic factors, or because of lifestyle — factors such as obesity, alcohol, tobacco use, low physical activity, consumption of high amounts of processed foods, red meat and a diet low in fiber.
The first meta-analysis looking specifically at red meat (beef, pork, lamb) consumption and risk for colorectal cancer (CRC) was published in 2001 by a research group at the University of Cambridge. Their findings suggested that a daily increase in red meat consumption of one portion (100g) increased an individual’s CRC risk by a modest 12 to 17%, RR of 1.17 (95% CI: 1.05 – 1.31).8,9 A more contemporary review article, which included data from an additional 9 meta-analysis published between 2001 and 2015, found the RR to vary between 1.06 to 1.35 for red meat and between 1.09 and 1.49 for processed meats.9 While the specific mechanism behind the relationship is somewhat unclear, there are several that have been proposed, from N-nitroso compounds, polycyclic aromatic hydrocarbons (similar to the mechanism from tobacco smoke), to the heme molecules and alteration of GI bacterial flora.9,10 The American Cancer Society, American Society for Clinical Oncology and European Society for Medical Oncology all have different recommendations regarding what quantity could be considered a safe amount of red meat. However, all three societies agree on some form of limitation. In addition to dietary modification and appropriate screening, encouraging an active lifestyle can be beneficial. With added outdoor hours that come with summertime, also encourage your patients to practice adequate sun protection. Skin cancers, while not a leading cause of cancer-related deaths, are by far the most commonly occurring group of cancers in the United States. The frequency is highest for basal and squamous cell carcinoma followed by melanoma11 and then less frequent types such as Merkel cell carcinoma. The overwhelming majority of these cancers are believed to be because of modifiable risk factors.12 Cumulative lifetime exposure to ultraviolet (UV) radiation (via outdoor activity or indoor tanning), herbicide exposure and immunosuppression (from HIV/AIDS or organ transplantation) all can increase the risk for skin cancer. Protection in the form of topical, water-resistant sunscreen (with appropriate application frequency depending on SPF) as well as the use of physical barriers, such as UV resistant clothing and natural shade can all help reduce UV exposure.13 Additionally, having both a heightened surveillance for suspicious lesions and prompt evaluation with individuals who have significant, cumulative lifetime sun exposure, can help catch skin cancers earlier, at a point where they can be successfully excised. While it is not practical to expect our patients to be able to avoid every environmental or lifestyle-related risk factor, being aware of these modifiable risk factors holds value. Being cognizant of these risk factors certainly enables both early identification of patients who may be at higher risk as well as appropriate counseling. As exciting as new advances in the field of Oncology may be, it will never be more important than both early detection and prevention.
References:
1. Bray, F., Laversanne, M., Sung, H., Ferlay, J., Siegel, R.L., Soerjomataram, I., Jemal, A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024 MayJun;74(3):229-263. doi: 10.3322/caac.21834. Epub 2024 Apr 4. PMID: 38572751
2. Koh, B., Tan, D.J.H., Ng, C.H., et al. Patterns in Cancer Incidence Among People Younger Than 50 Years in the US, 2010 to 2019. JAMA Netw Open. 2023;6(8):e2328171. doi:10.1001/ jamanetworkopen.2023.28171
3. Paradis, C., Butt, P., Shield, K., Poole, N., Wells, S., Naimi, T., Sherk, A., the Low-Risk Alcohol Drinking Guidelines Scientific Expert Panels. (2023). Canada’s Guidance on Alcohol and Health: Final Report. Ottawa, Ont.: Canadian Centre on Substance Use and Addiction
4. U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 20202025. 9th Edition. December 2020
5. Pöschl, G., Seitz, H.K.: Alcohol and cancer. Alcohol 39:155-165, 2004
6. Bagnardi, V., Rota, M., Botteri, E., et al. Alcohol consumption and site-specific cancer risk: A comprehensive dose-response meta-analysis. British Journal of Cancer 2015; 112(3):580–593
7. LoConte, N.K., Brewster, A.M., Kaur, J.S., Merrill, J.K., Alberg, A.J. Alcohol and cancer: A statement of the American Society of Clinical Oncology. Journal of Clinical Oncology 2018; 36(1):83–93
8. Sandhu, M.S., White, I.R., McPherson, K. Systematic review of the prospective cohort studies on meat consumption and colorectal cancer risk: a meta-analytical approach. Cancer Epidemiol Biomarkers Prev 2001;5:439-46
9. Aykan, N.F. Red Meat and Colorectal Cancer. Oncol Rev. 2015 Dec 28;9(1):288. doi: 10.4081/oncol.2015.288. PMID: 26779313; PMCID: PMC4698595
10. Diakité, M.T., Diakité, B., Koné, A., Balam, S., Fofana, D., Diallo, D., Kassogué, Y., Traoré, C.B., Kamaté, B., Ba, D., Ly, M., Ba, M., Koné, B., Maiga, A.I., Achenbach, C., Holl, J., Murphy, R., Hou, L., Maiga, M. Relationships between gut microbiota, red meat consumption and colorectal cancer. J Carcinog Mutagen. 2022;13(3):1000385. Epub 2022 May 12. PMID: 37206892; PMCID: PMC10194058
11. Aggarwal, P., Knabel, P., Fleischer, A.B. Jr. United States burden of melanoma and non-melanoma skin cancer from 1990 to 2019. J Am Acad Dermatol. 2021;85(2):388-395
12. Islami, F., Goding Sauer, A., Miller, K.D. et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States. CA Cancer J Clin. 2018;68(1):31-54
13. Perez, M., Abisaad, J.A., Rojas, K.D., Marchetti, M.A., Jaimes, N. Skin cancer: Primary, secondary, and tertiary prevention. Part I. J Am Acad Dermatol. 2022 Aug;87(2):255-268. doi: 10.1016/j. jaad.2021.12.066. Epub 2022 Feb 14. PMID: 35176397
14. US Preventive Services Task Force. Screening for Breast Cancer: US Preventive Services Task Force Recommendation Statement. JAMA. 2024;331(22):1918–1930. doi:10.1001/jama.2024.5534

Robert Horn, MD, is a board-certified physician specializing in Hematology and Medical Oncology at Texas Oncology-San Antonio Medical Center. He completed a Fellowship in Medical Oncology and Hematology at Texas Tech University Health Sciences Center and a Residency in Internal Medicine at The University of Texas Health Science Center. Dr. Horn is dedicated to providing exceptional care and is a member of the American College of Physicians, the American Society of Clinical Oncology, and the American Society of Hematology. He also served as Chief Fellow at Texas Tech in 2023, and is a member of the Bexar County Medical Society.

By Ghanshyam Mudigonda, MDac; Ashika Chacko, MDac; Lara Jones, DOab; and Holly Keyt, MDab
Affiliations:
a University of Texas Health Science Center at San Antonio, Department of Pulmonology, San Antonio, TX, USA
b University Health Transplant Institute, San Antonio, TX, USA
c University Health, San Antonio, TX, USA
Each year in the United States, approximately 2,500–3,300 lung transplants are performed. As of 2024, an estimated 30,000–35,000 individuals are living with a lung transplant. With advances in survival and long-term outcomes, post-transplant care now places greater emphasis on chronic health maintenance — including skin care. Immunosuppressive therapy, while vital to preventing rejection, increases the risk of skin cancer and other dermatologic complications, particularly during the summer months. This article highlights essential strategies for sun protection and skin care, equipping lung transplant recipients with practical tools to enjoy the season while minimizing dermatologic risk.
Cutaneous malignancy is the most common cancer following lung transplantation. Lung transplant recipients face a markedly higher risk of squamous cell carcinoma (SCC), basal cell carcinoma (BCC) and melanoma compared to the general population. SCC is not only more common but also more aggressive, with increased rates of recurrence, metastasis and mortality. BCC is the second most common skin cancer. Although less aggressive than SCC, transplant recipients experience a 10-fold increased incidence. Melanoma, though less frequent, remains a critical concern due to its potential lethality. Melanoma may arise de novo or, rarely, be donor derived. Other malignancies in this population include Kaposi Sarcoma, which is linked to HHV-8 and occurs more frequently in immunocompromised hosts, and Merkel Cell Carcinoma, a rare and aggressive neuroendocrine tumor associated with polyomavirus. Several risk factors contribute to this distribution of risk, as outlined below.
Agent or Factor
Chronic Immunosuppression
Calcineurin Inhibitors (Cyclosporin, Tacrolimus)
Azathioprine (AZA)
Mycophenolate Mofetil (MMF)
mTOR Inhibitors (Sirolimus, Everolimus)
• Immunosuppressive Regimen: Lung transplant recipients often require the highest levels of immunosuppression among solid organ recipients. This prolonged immunosuppression compromises tumor immune surveillance, elevating cancer risk.
• Photosensitizing Medications: Voriconazole, commonly used to prevent fungal infections, is associated with increased SCC risk, likely due to photosensitizing metabolites. Prolonged Voriconazole therapy (>30 days) is associated with a 2.4 to 3.5- fold increased risk of SCC.
• Chronic Infections: Oncogenic viruses, particularly HPV, may contribute to cutaneous neoplasia.
• Demographics: Older age, male sex and fair skin (Fitzpatrick types I–III) increased risk.
• Personal History: Individuals with prior skin cancer have higher rates of recurrence post-transplant.
• UV Exposure: A modifiable but significant factor contributing to risk.
Although the U.S. Preventive Services Task Force (USPSTF) does not recommend routine screening for the general population, transplant recipients represent a high-risk group warranting regular evaluation. A visual skin examination is one way to screen for skin cancers in at-risk populations. It should be noted that visual skin examination is subjective, and most methods of screening were developed for use by medical professionals. One commonly taught screening tool that can be used is the ABCDE criteria for melanoma:
• Asymmetry
• Border irregularity
• Color variation
Mechanism
Impaired tumor surveillance
Promote TGF-β, impair DNA repair
UV-sensitizing, mutagenic
Lacks photosensitizing effects
Anti-proliferative
T-cell depleting Induction Agents (Anti-Thymocyte Globulin) Early profound immunosuppression
• Diameter >6 mm
• Evolution over time
Impact on Skin Cancer Risk
High (SCC)
Lower (vs. AZA)
Lower incidence of skin cancers, especially SCC
Increased (early post-transplant)
To reduce the risk of skin damage and complications following transplant, USPSTF recommends patients should adopt comprehensive sun protection practices. This includes applying a broad-spectrum sunscreen with an SPF of 50 or higher every two hours, wearing sun-protective clothing such as long sleeves, wide-brimmed hats and sunglasses, and avoiding direct sun exposure between 10 a.m. and 4 p.m. when UV radiation is most intense. Seeking shade and avoiding indoor tanning are also essential. Additionally, patients should be aware of medications that may increase photosensitivity, including Voriconazole and Azathioprine. It is important to discuss any potential drug adjustments with a healthcare provider, as discontinuation of certain medications must be approached with caution. Corticosteroids, commonly used in transplant regimens, can lead to acne, skin thinning, striae, hypertrichosis and purpura. These changes can concern patients and should be differentiated from skin cancer by clinicians.
Summer heat increases the risk of dehydration, especially in transplant recipients on diuretics or fluid-restrictive regimens. Increased insensible losses through sweat and respiration can quickly destabilize fluid balance.
Signs of Dehydration:
• Dizziness, dry mouth, fatigue, dark or decreased urine output.
Clinical Concerns:
• Dehydration may impair renal function and alter drug pharmacokinetics.
• Tailored fluid management plans are essential, especially during heat waves or illness.
Conclusion
Skin and summer care is an essential yet underemphasized aspect of post-lung transplant management. Integrating sun protection, medication awareness, dermatologic surveillance and hydration strategies into routine care can significantly impact long-term outcomes.

Ghanshyam Mudigonda, MD, is a Pulmonary and Critical Care fellow at the University of Texas Health Science Center at San Antonio (UTHSCSA), where he was also a hospitalist from 2023-2024. His interests include lung transplant, transplant disparities and clinical education. He completed the Clinical Educator Track during his Internal Medicine residency at LSU Health Shreveport from July 2020 to June 2023, honing both his clinical and teaching skills in Shreveport, Louisiana.

Ashika Ann Chacko, MD, is a Pulmonary and Critical Care Medicine fellow at University of Texas Health Science Center at San Antonio. She earned her medical degree from Kasturba Medical College, Mangalore, India and completed her Internal Medicine residency in McAllen, Texas. Her academic interests include Acute Respiratory Distress Syndrome (ARDS), pulmonary hypertension, medical education and advancing health equity.
Here are some examples of skin cancers: Squamous Cell Carcinoma




By Jeremiah Brown, Jr., MS, MD
Ultraviolet (UV) radiation, a component of sunlight, is a wellknown environmental hazard. Dermatologists have long warned of its damaging effects on skin, and eye care professionals are equally aware of the dangers UV rays pose to the ocular system. Anterior segment complications such as pterygium and photokeratitis are commonly associated with UV exposure. However, the potential retinal consequences as less well known to the public.
UV radiation is divided into three bands:
• UVA (320–400 nm): Least energetic, penetrates the eye most deeply.
• UVB (280–320 nm): More energetic and mostly absorbed by the cornea and lens.
• UVC (100–280 nm): Completely absorbed by the Earth’s atmosphere.
Although the eye has natural defenses — eyelids, eyebrows and intraocular structures that filter shorter wavelengths — these mechanisms are not impenetrable. Prolonged or intense UV exposure can overwhelm these barriers, particularly in individuals with certain risk factors such as aphakia, pseudophakia or lesser degrees of ocular pigmentation.
Anterior segment conditions linked to UV exposure include:
• Photokeratitis: A painful, acute condition, essentially a sunburn of the cornea, often resulting from high-altitude or highly reflective environments.
• Pinguecula and Pterygium: Degenerative changes in the conjunctiva, strongly associated with chronic UV exposure.
• Cataract: Numerous epidemiological studies, including the WHO’s Global Burden of Disease, have linked UVB exposure to increased rates of cortical cataracts.
These conditions are visible, often symptomatic, and easier for patients to connect with sun exposure. However, the damage can extend further into the eye.
Despite the eye’s natural UV filtration, a small amount — especially UVA — can reach the retina. This is of particular concern in individuals with compromised lens integrity, such as those who have undergone cataract surgery without UV-blocking intraocular lenses (IOLs), or in children, whose lenses are more transmissive.
Oxidative stress is the primary mechanism by which UV radiation exerts its effects on the retina. UV-induced reactive oxygen species (ROS) can damage retinal pigment epithelium (RPE) cells, photoreceptors and Bruch’s membrane. Chronic oxidative damage plays a well-documented role in the pathogenesis of age-related macular degeneration (AMD).
The relationship between UV exposure and AMD has been studied extensively, but findings remain somewhat controversial due to confounding variables like genetics, smoking and diet. However, there is mounting evidence that long-term exposure to sunlight, particularly in outdoor workers and populations near the equator, correlates with higher AMD prevalence.
Some histological studies have shown that lipofuscin accumulation in RPE cells — a hallmark of AMD — is exacerbated by UV light. The phototoxic properties of A2E, a key component of lipofuscin, are enhanced under UV and blue light, suggesting that cumulative exposure may accelerate retinal aging and degeneration.
Solar retinopathy is a photochemical retinal injury resulting from direct or prolonged exposure to solar radiation, most commonly due to sun gazing, eclipse viewing without proper eye protection or exposure to high-intensity sunlight. The condition primarily affects the foveal region of the retina, leading to damage of the photoreceptors and retinal pigment epithelium. Clinically, patients may present with central scotoma, blurred vision, metamorphopsia or chromatopsia, often in both eyes, though symptoms can vary in severity. Fundus examination may reveal subtle foveal changes such as a yellow-white spot or pigmentary disturbance, while optical coherence tomography (OCT) typically shows disruption of the ellipsoid zone and retinal thinning. Although some visual recovery is possible over weeks to months, persistent deficits can occur. Prevention through public education and proper use of solar filters is essential.
Solar retinopathy is primarily caused by short-wavelength visible light, particularly in the blue light spectrum (400–500 nm), as well as some contribution from ultraviolet-A (UV-A, 315–400 nm) radiation. Although much of the UV radiation is absorbed by the cornea and lens, blue and near-UV light can penetrate the ocular media and reach the retina. These wavelengths are especially damaging due to their higher energy, which induces photochemical injury to the retinal pigment epithelium (RPE) and photoreceptor cells, particularly in the fovea where light is most intensely focused.
Children’s eyes absorb more UV radiation due to larger pupils and clearer lenses. Studies suggest that by the age of 18, a person has already received approximately 80% of their lifetime UV exposure. Yet, few children wear sunglasses or brimmed hats, and UV protection is often not prioritized in pediatric care.
This early exposure may not manifest in symptoms for decades but predispose one to age-related macular changes. Preventive steps in this age group are critical.
• Cataract Surgery: When selecting intraocular lenses, especially for younger patients, UV-blocking and blue-light filtering lenses may offer long-term protective benefits. While the debate continues over the impact of blue-light filtering IOLs on contrast sensitivity and circadian rhythms, the potential for retinal protection should not be dismissed. Patients receiving light adjustable lenses must wear filtering lenses in the postoperative period to prevent premature crosslinking of the photoactive lens molecules.
• Photodynamic Therapy and Laser Treatments: Patients undergoing treatments that involve light activation (i.e., photodynamic therapy with verteporfin) must be carefully counseled on post-treatment light exposure, as residual photosensitization can exacerbate retinal damage.
• Patient Education: Routine eye examinations offer an opportunity to reinforce UV protection, especially in patients with early AMD, retinal dystrophies or high cumulative sun exposure.
While total UV avoidance is neither practical nor advisable, especially given the benefits of sunlight for mood and vitamin D synthesis, effective protective strategies can reduce risk significantly:
• Sunglasses: Look for lenses that block 100% UVA and UVB. Sunglasses that do not have labeling confirming this filtering is present are only tinted and do not provide UV protection. Wraparound styles offer enhanced protection by minimizing peripheral light exposure.
• Wide-Brimmed Hats: These can reduce UV exposure to the eyes by up to 50%.
• UV-blocking Contact Lenses: These offer supplementary protection, particularly for those not wearing sunglasses.
• Patient Education: Incorporating sun safety into routine eye exams — especially for children, outdoor workers and post-cataract patients — is essential.
Several promising areas of research are underway:
• Retinal biomarkers of UV exposure: Imaging modalities such as autofluorescence and high-resolution OCT may help detect early changes attributable to UV-related oxidative stress.
• Gene-environment interactions: Understanding how UV exposure interacts with genetic susceptibility loci for AMD could offer more personalized prevention strategies.
• Advanced materials: The development of more effective, comfortable and fashionable UV-blocking lenses could improve compliance, particularly in younger populations.
While the full scope of UV radiation’s impact on the retina continues to be elucidated, the evidence supports a cautious and proactive approach. Encouraging UV protection from an early age, particularly in high-risk individuals, may reduce the burden of retinal disease over a lifetime.
Let us raise awareness of what we can prevent.
Figure 1.
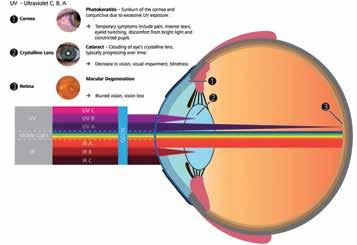
Source: Modified from https://i.sstatic.net/i00Oe.jpg
1. Taylor, H.R. Ultraviolet radiation and the eye: an epidemiologic study. Trans Am Ophthalmol Soc. 1989;87:802–853
2. Sliney, D.H. How light reaches the eye and its components. Int J Toxicol. 2002;21(6):501–509. doi:10.1080/10915810290096523
3. Schick, T., Ersoy, L., Lechanteur, Y.T., et al. History of sunlight exposure is a risk factor for age-related macular degeneration. Retina. 2016;36(4):787–790. doi:10.1097/ IAE.0000000000000816
4. Roberts, J.E. Ultraviolet radiation as a risk factor for cataract and macular degeneration. Eye Contact Lens. 2011;37(4):246–249. doi:10.1097/ICL.0b013e31821c8e57
5. Youssef, P.N., Sheibani, N., Albert, D.M. Retinal light toxicity. Eye (Lond). 2011;25(1):1–14. doi:10.1038/eye.2010.149
6. Margrain, T.H., Boulton, M., Marshall, J., Sliney, D.H. Do blue light filters confer protection against age-related macular degeneration? Prog Retin Eye Res. 2004;23(5):523–531. doi:10.1016/j.preteyeres.2004.05.001
7. Delcourt, C., Carrière, I., Ponton-Sanchez, A., Fourrey, N., Lacroux, A., Papoz, L.; POLA Study Group. Light exposure and the risk of age-related macular degeneration: the Pathologies Oculaires Liées à l’Age (POLA) study. Arch Ophthalmol. 2001;119(10):1463–1468. doi:10.1001/archopht.119.10.1463
8. Zhang, Z., Shan, X., Li, S., et al. Retinal light damage: from mechanisms to protective strategies. Survey of Ophthalmology 69 (2024) 905-915

Jeremiah Brown, MS, MD, is a graduate of Harvard University. A U.S. Army veteran, Dr. Brown served as director of ophthalmology research at the U.S. Army’s Laser Research Laboratory at Brooks Air Force Base, a division of the Walter Reed Army Institute of Research. He has co-authored more than 25 peerreviewed articles in ophthalmology research as well as textbook chapters. He is a frequent lecturer to ophthalmology residents as well as practicing ophthalmologists. Dr. Brown practices vitreoretinal diseases in San Antonio and Schertz, and is a member of Retina Consultants of Texas and the Bexar County Medical Society.

By Craig Ainsworth, MD
The San Antonio area has a treasure trove of beautiful parks, hiking trails, rivers, lakes and access to several state parks. At these locations, city dwellers can train for races, exercise, connect with family or just relax and spend time together. If you are going to beat the summer heat and safely enjoy the many outdoor activities that the city has to offer, you need to plan, prepare and take measures to avoid heat injuries.
Exertional heat injuries can range from mild conditions like heat cramps (muscle cramps that occur during exercise) to more serious conditions like heat syncope, exercise associated collapse, heat exhaustion and heat injury. Heat injury is a progressive, multi-organ system condition with elevated temperature after vigorous activity and is associated with end organ damage-usually to the muscle, liver or kidneys. Heat stroke occurs when the heat injury involves elevated temperatures and neurologic symptoms such as encephalopathy and/or seizures.
Knowing the factors that can predispose to exertional heat illness can help us to plan, prepare and prevent it. These factors include low physical fitness, lack of acclimatization, use of alcohol prior to exercise or outdoor activities, use of stimulant medications and inadequate hydration.
Individual athletes can plan and prepare to prevent heat illness by first acclimatizing to heat and humidity over a 10-to-14-day period. Significant exertion in the heat should be limited to short time intervals that are slowly and gradually increased. The CDC and sports medicine societies have guidelines regarding when outdoor activities should be limited or cancelled based on heat and humidity. Additionally, individual athletes can prevent injury by adequately hydrating with cold drinks. If an athlete is unsure if hydration is adequate, they should establish a pattern of weighing in before and after an activity during their acclimatization period. Athletes should consume sodium-containing fluids and not just water alone as this can drop sodium levels and cause muscle cramping. Athletes who plan on running in longer races or endurance events in the summertime should be encouraged to pre-cool by drinking frozen drinks, covering the neck with an iced towel, and immersing the hands or arms in ice-containing coolers. Athletes should wear clothing that breathes or ventilates well and allows for evaporative cooling. It is important to note that clothing that is completely saturated with sweat limits evaporative cooling and should be changed if possible.
Coaches, trainers and those responsible for athletes can prevent and treat heat illness by ensuring that appropriate medical care equipment is available in the event that athletes develop heat injuries. This equipment can include cold water immersion tubs, spray bottles, fans and cold drinks. Coaches and athletic directors should regularly review their emergency plans for treating patients with severe heat injury prior to EMS arrival. Athletic training sessions should include
periods of rest that can be used for hydration and cooling. Athletes should be trained to stop exercising if they experience severe exhaustion or lightheadedness.
The severity of heat illness may not be apparent during a patient’s initial presentation. The severity of morbidity and mortality from heat injury are related to the duration of core temperature elevation. Once a heat injury is recognized, every effort needs to be made to get the patient to water, ice and shade. Heat injury should be conceptualized as a “heat attack” and rapid cooling initiated to mitigate its effects. Evaporative cooling is the most effective, but humid conditions can limit its use. Heat stroke is diagnosed when a patient has a temperature greater than 104.9 and altered mental status. These patients should be placed in an ice water immersion bath as soon as possible after removing clothing and athletic equipment.
Apart from athletes, children and animals are at risk for heat-related illness. Both children and animals should never be left in a parked car. This can rapidly result in death for both due to extreme temperature elevation, which occurs when cars are parked in the summer. Walking animals should occur in the cooler early morning or late evening hours. If an animal demonstrates excessive panting or salivating, it should be brought into a shady area after being cooled by being hosed down with water. Similarly, children who are flushed or reporting severe fatigue with outside activities should be treated with similar measures.
Heat can kill, but this shouldn’t keep us from enjoying the incredible natural beauty and outdoor activities that our city has to offer. With thought and planning, almost all heat injuries can be avoided and if they occur, treated. Coaches, trainers and parents need to watch the weather, heat index and take the appropriate measures to keep their athletes and others safe. Be mindful of the signs of heat injuries in others and don’t be afraid to ask someone how they are and if needed help get them to water, ice and shade.

Craig Ainsworth, MD, is a four-time Ironman and loves to get outside to hunt, fish, swim, bike and run. He earned his bachelor’s degree in microbiology at Brigham Young University. He attended USUHS, the military’s medical school, and graduated in 2007. He did a residency in Internal Medicine and a Critical Care Medicine Fellowship at Walter Reed National Military Medical Center. After completing his military obligation, he joined Texas IPS and has been in private practice since 2019. He and his wife are the parents of eight children and just welcomed their first grandchild. They have called San Antonio home since 2016. Dr. Ainsworth is a member of the Bexar County Medical Society.

By Ruba Krichati, OMS-II; Nishita Maknojia, OMS-I; Laila Barkoudeh, OMS-I; and Ramaswamy Sharma, MS, PhD
Melanoma is a cancer in which melanocytes, the cells that produce the pigment melanin responsible for skin and eye color, undergo dysregulated proliferation. The incidence of melanoma has been rising steadily over the past three decades. According to the American Cancer Society, an estimated 212,200 new cases of melanoma will be diagnosed in 2025 in the United States; 107,240 of these cases will be invasive and occur in 60,550 men and 44,410 women, resulting in 8,430 melanoma-related deaths (5,470 men and 2,960 women). Texas ranks third in the nation in melanoma incidence, with an estimated 5,700 new cases and 490 deaths in 2025. Although melanoma accounts for only about 1% of all skin cancers, it is responsible for more than 65% of skin cancer-related deaths as it is highly invasive and can metastasize to other organs rapidly as compared to other skin cancers. In addition to skin cancer, non-cutaneous primary melanomas also occur, such as uveal melanoma arising from the iris, ciliary body or choroid, melanomas of mucus membranes in the nasal, nasopharyngeal, gastrointestinal and genital tracts, and melanomas with unknown primary (MUP) origin.
Overexposure to UV radiation from the sun or tanning beds, having fair skin, blonde or red hair, blue eyes, atypical moles (dysplastic or large congenital nevi), and a personal history of skin cancer or a family history of melanoma increase the risk for developing melanoma. Mutations in several genes such as CDKN2A, MC1R, MDM2, are all associated with increased risk; germline mutations in CDKN2A are associated with familial atypical multiple mole melanoma syndrome (FAMMM syndrome). Mutations in BRAF, RAS, NF-1 and fusion of kinases are thought to initiate cutaneous melanomas.
Traditionally, four subtypes of melanoma have been recognized based on their histopathological characteristics and their rate of growth. Around 90% of melanomas are slow-growing, appearing as pigmented macules that originate either from melanocytes located in the basal layer of the epidermis or in the hair follicle, proliferate radially within the epidermis at a rate of 0.1 mm per month, and form papules or nodules as they infiltrate further into the dermis after a few months to years; these include superficial spreading melanoma (SSM; 70%), lentigo maligna melanoma (LM; 10%), which mostly occurs in continuously sun-exposed areas such as the face and neck, especially in elderly females, and acral lentiginous melanoma (ALM; 10%), which presents either as red, orange or dark pigmentation with irregular borders in palmoplantar regions or with a longitudinal dark
streak beneath the nail bed (melanonychia) in individuals with darker skin tones and predisposed genetic factors. In contrast, nodular melanoma (NM) is thought to arise from dermal melanocytes, exhibits a growth rate of 0.5 mm per month, and infiltrates rapidly to initiate early vertical growth; its similarity with other benign lesions makes it difficult to diagnose, resulting in more than 40% of melanoma-related deaths. Other variant clinical presentations of melanoma such as desmoplastic melanoma (1-4%), which are characterized by the presence of spindle cells, amelanotic melanoma that lacks melanin and is, therefore, difficult to detect, spitzoid melanoma, which resembles a benign spitz nevus, and nevoid melanoma that appears as a benign skin mole, further complicate the diagnosis of melanoma.
The ABCDE criteria formulated by Dr. Darell Rigel and colleagues can be used for identifying most early melanoma lesions and includes Asymmetry (one half of a lesion is different from the other half), Border (lesion border is irregular), Color (lesion has uneven, variegated colors such as pink, grey, blue, black, tan, red), Diameter (lesion is usually >6 mm in diameter although some may be smaller), and Evolving (lesion changes in size, shape or color over time). However, nodular melanoma does not conform to these criteria and is detected based on EFG criteria: Elevated above the skin surface, Firm to touch and Growing.
Wide local excision surgery has been the standard-of-care therapy for several decades; Mohs micrographic surgery that involves precise resection of cancerous tissue while conserving normal tissue has also shown considerable promise. In recent years, significant strides have been made in the immunotherapeutic treatment of melanoma. Since melanoma is associated with activating mutations in kinases such as BRAF, targeted therapy with immune checkpoint inhibitors has radically enhanced outcomes. Bristol-Myers Squibb’s Opdualag, a combination therapy consisting of nicoluman and relatlimab that target PD-1 and LAG-3 receptors, was approved by the FDA in March 2022 and has improved median progression-free survival (PFS) in advanced melanoma cases from 4.6 months to 10.2 months. Opdualag specifically helps to restore and enhance T cell activity against melanoma cells.
In February 2024, the FDA approved lifileucel (Amtagvi), the first adoptive T-cell therapy using tumor-infiltrating lymphocytes (TIL) for patients with metastatic melanoma. This innovative form of personalized immunotherapy involves isolating the patient’s own T cells that have naturally infiltrated the tumor to target the cancer cells, allowing them to proliferate ex vivo using IL-2, depleting other
lymphocytes in the patient via chemotherapy, and then re-infusing these expanded TIL intravenously. The patient continues to receive IL-2 to stimulate TIL. Since TIL recognize multiple tumor antigens, they provide a broad immune response as compared to Chimeric Antigen Receptor (CAR) T cells. However, this treatment is restricted to specialized centers as it requires growth of the isolated T-cells in a quality-controlled environment; careful monitoring of the patient for immune-related toxicities is also important.
In May 2024, Innovent Biologics reported results from a phase I study of IBI363, a PD-1/IL-2Rα bispecific antibody fusion protein, in patients with prior immunotherapy and cold tumors; they observed “encouraging” efficacy and an acceptable safety profile; a phase II trial in patients with mucosal and acral melanoma was reported as ongoing in May 2025.
In June 2024, follow-up of phase 2b study of a combination of Moderna’s mRNA-4157 (V940) vaccine along with Merck’s anti-PD1, pembrolizumab, as an adjuvant showed a 49% decrease in the risk of recurrence or death in patients with resected stage III or IV melanoma and a 62% reduction in the risk of distant metastasis or death as compared to treatment with pembrolizumab alone. Phase 3 trials in patients with resected high-risk (Stage IIB-IV) melanoma were initiated in October 2024. These advancements underscore the importance of continued research and personalized treatment in improving melanoma outcomes.
References:
1. Chen, Y., Lin, J., Wang, H., Zhang, W., Liang, X., Cui, J., Sun, Y., Fang, M., Pan, Y., Chu, Q., Bai, X., Zhang, J., Li, N., Zhang, X., Zhao, L., Chen, H., Wang, H., Chen, Y., Sun, X., Zhou, H. (2024). First-in-class PD-1/IL-2 bispecific antibody fusion protein IBI363 in patients with advanced melanoma: Safety and efficacy results from a phase I study. Journal of Clinical Oncology, 42(16_suppl), 9562. https://doi.org/10.1200/jco.2024.42.16_suppl.9562
2. Chick, R.C., Beane, J.D., Contreras, C.M. (2025). Adoptive T-Cell therapy in melanoma. In Surg Oncol Clin N Am (Vol. 34, pp. 423–436).
3. Janes, L.A., Haykal, T., Angeles, C.V. (2025). Vaccines in melanoma. Surgical Oncology Clinics of North America, 34(3), 411–421. https://doi.org/10.1016/j.soc.2025.01.004
4. Long, G.V., Hodi, F.S., Lipson, E.J., Schadendorf, D., Ascierto, P.A., Matamala, L., Salman, P., Gutiérrez, E.C., Rutkowski, P., Gogas, H.J., Lao, C.D., De Menezes, J.J., Dalle, S., Arance, A., Grob, J., Keidel, S., Shaikh, A., Sobiesk, A.M., Dolfi, S., Tawbi, H.A. (2023). Overall Survival and Response with Nivolumab and Relatlimab in Advanced Melanoma. NEJM Evidence, 2(4). https://doi.org/10.1056/evidoa2200239
5. Lian, B., Chen, Y., Luo, Z., Zhang, X., Wu, D., Li, K., Zou, Z., Fang, M., Jing, C., Feng, H., Jiang, Y., Zhang, W., Li, X., Jiang, R., Wang, E., Yi, C., Zhang, Y., Zhang, X., Ren, X., Guo, J. (2025). A multicenter, randomized, controlled, open-label, phase 2 study of the PD-1/IL-2 α-bias bispecific antibody fusion protein IBI363 in mucosal and acral melanoma. Journal of Clinical Oncology, 43(16_suppl). https://doi.org/10.1200/ jco.2025.43.16_suppl.tps9594
6. Merck (2025, June 2). Merck and Moderna Initiate Phase 3 Trial Evaluating Adjuvant V940 (mRNA-4157) in Combination with KEYTRUDA® (pembrolizumab) After Neoadjuvant KEYTRU-
DA and Chemotherapy in Patients with Certain Types of NonSmall Cell Lung Cancer (NSCLC). https://www.merck.com/ news/merck-and-moderna-initiate-phase-3-trial-evaluating-adjuvant-v940-mrna-4157-in-combination-with-keytruda-pembrolizumab-after-neoadjuvant-keytruda-and-chemotherapy-in-patients-with-certain-ty/
7. Moderna (2025, June 2). Moderna & Merck Announce 3-Year Data For mRNA-4157 (V940) in Combination With KEYTRUDA(R) (pembrolizumab) Demonstrated Sustained Improvement in Recurrence-Free Survival & Distant Metastasis-Free Survival Versus KEYTRUDA in Patients With High-Risk Stage III/IV Melanoma Following Complete Resection. https://investors.modernatx.com/news/news-details/2024/Moderna--Merck-Announce-3-Year-Data-For-mRNA-4157-V940-in-Combination-With-KEYTRUDAR-pembrolizumab-Demonstrated-Sustained-Improvement-in-Recurrence-Free-Survival--Distant-Metastasis-Free-Survival-Versus-KEYTRUDA-in-Patients-With-High-Risk-Stage-IIIIV/default.aspx
8. Targeted Oncology. (2024). Novel combinations highlight treatment advances in melanoma. https://www.targetedonc.com/view/ novel-combinations-highlight-treatment-advances-in-melanoma
9. Tawbi, H.A., Schadendorf, D., Lipson, E.J., Ascierto, P.A., Matamala, L., Gutiérrez, E.C., Rutkowski, P., Gogas, H.J., Lao, C.D., De Menezes, J.J., Dalle, S., Arance, A., Grob, J., Srivastava, S., Abaskharoun, M., Hamilton, M., Keidel, S., Simonsen, K.L., Sobiesk, A.M., . . . Long, G.V. (2022). Relatlimab and Nivolumab versus Nivolumab in Untreated Advanced Melanoma. New England Journal of Medicine, 386(1), 24–34. https://doi. org/10.1056/nejmoa2109970

Ruba Krichati, OMS-II, is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027. Her interests include internal medicine, health advocacy and healthcare policy. She is dedicated to improving health equity, addressing systemic disparities in underserved communities, and advancing patient-centered care through leadership, community engagement and evidence-based practice.

Nishita Maknojia, OMS-I, is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2028. She is interested in the impact of journalism on healthcare and how health education can play a pivotal role in improving health outcomes. She is also dedicated to learning about various health disparities that underserved communities face.

Laila Barkoudeh, OMS-I, is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2028. Her interests include internal medicine, academic medicine, medical education, international medicine and community outreach.

Ramaswamy Sharma, MS, PhD, is a Professor of Histology and Pathology at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life. Dr. Sharma is a member of the BCMS Publications Committee.

By Esther Shin, OMS-III, and Gabriel Bietz, MD
Sunlight is our primary natural source of vitamin D synthesis. Vitamin D, also known as the “sunshine vitamin,” plays a crucial role in musculoskeletal health, immune regulation and energy levels.1 However, excess sun exposure has been known to be a major contributor to the development of skin cancer — one of the most common types of malignancy worldwide. This presents a concern in South Texas, where we experience a high UV index score for prolonged periods of time. Public health guidelines have therefore long since advocated for reduction of sun exposure and implementation of protective measures such as sunscreen to minimize ultraviolet (UV) exposure and thereby skin cancer risk. However, with the increasing rates of vitamin D deficiency seen in different patient populations, questions are starting to be raised about our current sun safety guidelines potentially having a negative impact on our health.
Vitamin D is synthesized in the skin upon exposure to UVB light (wavelengths of 290-315 nanometers). This process is influenced by latitude, time of day, season, skin pigmentation, local pollution, reflective surfaces and use of protective measures.2 The initial inactive vitamin D compound is metabolized by 25-hydroxylase into 25-hydroxyvitamin D (25(OH)D) in the liver. 25-hydroxyvitamin D is then converted into its biologically active form 1,25-dihydroxyvitamin D (1,25 (OH)) by 24-hydroxyvitamin D-1 alpha-hydroxylase in the kidneys.1 The vitamin D receptor is present throughout the body and facilitates a wide range of functions that include stimulation of insulin production, T and B lymphocyte function modulation, inhibition of cellular proliferation, and inducing terminal differentiation.1 However, the dominant function of activated vitamin D is to regulate plasma calcium and phosphate levels, both of which are required
for bone mineralization. The hormonal form of vitamin D stimulates and enhances intestinal calcium and phosphorus absorption.3 Calcium levels also play a crucial role in neuromuscular junction function, nerve transmission, vasodilatation and hormone secretion.4
Deficiency of vitamin D is therefore associated with rickets, osteomalacia, osteopenia, osteoporosis, obesity, type 2 diabetes mellitus, hypertension, depression, fibromyalgia, chronic fatigue syndrome and Alzheimer’s disease.5
Vitamin D sufficiency is generally defined as a serum level of 25(OH)D above 30 ng/mL. Levels below 20 ng/mL indicate deficiency and between 20 and 30 ng/ml suggest insufficiency. Risk factors for vitamin D deficiency include working indoors full time, older adults, dark skin tone and malabsorption syndromes like celiac disease. Approximately 20 minutes of daily sunshine with over 40% of skin exposure is required to prevent vitamin D deficiency.5 With over 1 billion people worldwide being either vitamin D deficient or insufficient, there is rising public health concern.5
On the other hand, UV radiation is classified as a Group 1 carcinogen by the World Health Organization (WHO).6 The resulting oxidative stress and direct DNA damage lead to mutations in tumor suppressor genes and proto-oncogenes, precipitating skin cancers. The three most common types of skin cancers are basal cell carcinoma, squamous cell carcinoma and melanoma. Furthermore, sunburns during childhood significantly increase risk of developing skin cancer later in life.7 In the United States, over 5 million cases are being treated every year. To that end, public health campaigns teach effective ways of blocking UVB radiation such as using sunscreen with a sun protection factor at least 30, limiting sunburn incidences, and discouraging indoor tanning bed use.
The interplay of different risk factors may require a personalized approach in risk stratification. For example, those with Fitzpatrick skin types I to III produce vitamin D more efficiently but may need to take more caution due to higher risk for skin damage. Types IV through VI have stronger natural protection but will need longer sun exposure to synthesize adequate amounts of vitamin D.8 Residents of high latitude regions or long winters will also have an increased risk of vitamin D deficiency. Patients may also have medical conditions that impair vitamin D metabolism such as malabsorption syndromes, chronic kidney disease, obesity and aging.9 To such patients with higher risk, the NIH recommends dietary supplementation of 600-800 IU/day.10
In conclusion, balancing skin cancer prevention and vitamin D insufficiency is a nuanced public health challenge. The risk of skin cancer from excess UV exposure is real and preventable, while vitamin D deficiency remains a frequently overlooked but manageable public health concern. The relationship between two competing health priorities can be managed with several guidelines. United guidance should emphasize measured sun exposure, vitamin D diet supplementation and education on how to meet vitamin D needs safely, especially in high-risk populations. Clinicians, public health authorities, researchers and patients themselves will need to continue refining and communicating nuanced strategies that will support both objectives.
References:
1. Krati Chauhan, Huecker, M.R. (2019, October 21). Vitamin D. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/ books/NBK441912/
2. Wacker, M., Holick, M.F. (2013). Sunlight and Vitamin D. Dermato-Endocrinology, 5(1), 51–108. https://doi.org/10.4161/ derm.24494
3. Nair, R., Maseeh, A. (2012). Vitamin D: The “sunshine” vitamin. Journal of Pharmacology & Pharmacotherapeutics, 3(2), 118–126. https://doi.org/10.4103/0976-500X.95506
4. Ross, A.C., Taylor, C.L., Yaktine, A.L., B, H. (2011). Overview of Vitamin D. Nih.gov; National Academies Press (US). https:// www.ncbi.nlm.nih.gov/books/NBK56061/
5. Naeem, D.Z. (2010). Vitamin D Deficiency- An Ignored Epidemic. International Journal of Health Sciences, 4(1), V. https:// pmc.ncbi.nlm.nih.gov/articles/PMC3068797/#b1-ijhs-4-1-005a
6. Mogensen, M., Jemec, G.B. (2010). The potential carcinogenic risk of tanning beds: clinical guidelines and patient safety advice. Cancer management and research, 2, 277–282. https://doi. org/10.2147/CMR.S7403
7. Hufford, D., Rehfuess, E., World Health Organization. (2003). Sun protection and schools: how to make a difference. World Health Organization
8. Raymond-Lezman, J.R., Riskin, S.I. (2023). Benefits and Risks of Sun Exposure to Maintain Adequate Vitamin D Levels. Cureus, 15(5). https://doi.org/10.7759/cureus.38578
9. Sizar, O., Khare, S., Goyal, A., Bansal, P., Givler, A. (2023). Vitamin D Deficiency. PubMed; StatPearls Publishing. https://www. ncbi.nlm.nih.gov/books/NBK532266/
10. Mf, H., & Tc, C. (2008, April 1). Vitamin D Deficiency: A Worldwide Problem with Health Consequences. The American Journal of Clinical Nutrition. https://pubmed.ncbi.nlm.nih. gov/18400738/


Esther Shin, OMS-III, is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, with an interest in public health.
Gabriel Bietz, MD, is a board-certified vascular surgeon and Chairman of the Board for San Antonio Surgical Center of Excellence. He is a partner at Texas Cardiac and Vascular Institute, serving patients across San Antonio, Seguin and Corpus Christi. He is recognized for his expertise in both open and endovascular procedures, along with his leadership in advancing patient-centered vascular care. In addition to his medical career, Dr. Bietz is a serial entrepreneur with ventures spanning healthcare and private investments, and is a member of the Bexar County Medical Society.

By Camille Irene Hulipas, OMS-II; Elizabeth Ou, OMS-II; and Ramaswamy Sharma, MS, PhD
While sunlight is considered to be essential for vitamin D production and overall well-being, excessive exposure to the sun’s electromagnetic radiation such as ultraviolet (UV) rays can lead to skin damage. UV radiation from the sun is composed of three types of wavelengths: UVA (320-400 nm), UVB (280320 nm), and UVC (100-280 nm). Of these, UVC and most of UVB radiation is absorbed by the Earth’s ozone layer in the atmosphere and is not thought to pose a major health risk. Therefore, wavelengths from approximately 300 to 400 nm, consisting of approximately 95% UVA and 5% UVB rays, play a significant role in our health. UVA penetrates deep into the dermis and can generate reactive oxygen species (ROS) that break down collagen and elastic fibers, resulting in premature aging (photoaging) of the skin, manifested as wrinkles or sagging skin and pigmentation or dark spots; long-term exposure to UVA has been traditionally associated with skin cancer such as melanoma. UVB rays, on the other hand, affect the superficial layer of skin, the epidermis; shorter exposures to UVB can lead to sunburns while longer exposures can damage DNA of epidermal cells called keratinocytes via formation of cyclobutene pyrimidine dimers or pyrimidine (6-4) pyrimidone photoproducts, leading to basal and squamous cell carcinoma. UVB rays, and to a lesser extent, UVA rays can also oxidize and damage DNA bases by forming 8-oxo-7,8 dihydro-2’-deoxyguanosine (8-oxo-dG). The differential effects of UVA and UVB on the skin, however, are not entirely clear and more studies are needed to establish a causal link. Nevertheless, the association between UV rays and skin damage has been confirmed by epidemiological studies over the years; it is, therefore, not surprising that one in five Americans will develop skin cancer in their lifetime.
Proactive measures to minimize UV-related damage include the use of sunscreens in addition to protective clothing and staying in the shade. Although sunscreens cannot block 100% of UV rays, they can play an essential role in protecting your skin. Sunscreens can be
primarily classified into two primary categories: physical or mineral sunscreens and chemical sunscreens. Physical sunscreens prevent penetration of both UVA and UVB rays into the skin by scattering and reflecting them away from the skin. These sunscreens usually contain finely ground zinc oxide or titanium dioxide and function as physical barriers. Physical sunscreens can be greasy and zinc oxide leaves a white cast, but they are generally less irritating to the skin as compared to chemical sunscreens. Chemical sunscreens contain organic compounds such as oxybenzone, avobenzone, octinoxate and homosalate, which absorb and convert UV radiation into heat that is released from the skin. These sunscreens do not have a thick consistency as do physical sunscreens, making them less visible as compared to physical sunscreens. However, chemical sunscreens need to be applied at least 15- 30 minutes before sun exposure to ensure their absorption by the skin whereas physical sunscreens tend to provide immediate protection. Absorption by the skin can lead to irritation or trigger allergic reactions in certain individuals; oxybenzone and octinoxate may also affect the endocrine system. Hybrid formulations incorporating UV-absorbing and UV-reflecting properties of physical and chemical sunscreens can be more beneficial. Addition of iron oxide to prevent high energy visible light that damages collagen and causes hyperpigmentation can also be helpful. Overall, it is best to select a broad-spectrum sunscreen that protects against both UVA and UVB rays.
Sun protection factor (SPF) indicates the level of protection afforded by a sunscreen and is based on the time taken by sunscreen-treated skin to become red or burn when exposed to ultraviolet light as compared to unprotected skin. SPFs of 15, 30, 50 and 100 block 93%, 97%, 98% and 99% of UVB rays, respectively; thus, higher the number, higher the protection. Typically, a lower SPF in the range of 15-30 may suffice to prevent photoaging in individuals who spend most of their time indoors in temperate climates, while a higher SPF of 30 or above would be recommended for those individuals located
in countries with intense UVB radiation at lower or higher altitudes and spending the day outdoors. Since UV rays are stronger at high altitudes and can penetrate windows, sunscreens with higher SPFs are important during airplane travel, irrespective of duration of the flight or proximity to a window seat. SPF50 or higher is recommended for individuals with inherited or acquired photosensitivity disorders, transplant patients, patients at risk for skin cancer, and those who suffer from malabsorption. While SPF measures protection against UV rays, a relatively newer UVA-Protection Factor, measured by a PA++++ rating, indicates protection against UVA rays. PA+ is least protective while PA++++ offers the most protection against UV rays. A high UVA-PF is recommended in all cases
Sunscreen should be applied in a uniform layer every two hours. SPF lip balms provide protection for the lips. It is recommended to use approximately two milligrams of sunscreen per square centimeter of skin, equivalent to a dollop the size of a quarter for the head, face and neck. Most users apply less, which may not offer sufficient protection. Lotions or creams tend to provide better coverage as compared to sprays or powdered formulations. Water-resistant sunscreens, which contain film-forming polymers of acrylates, oils, waxes, resins or other emollients, maintain their SPF protection during swimming or sweating for 40 or 80 minutes, as noted on their labels.
Since vitamin D is synthesized when the skin is exposed to the sun and is essential for bone health, immune function and overall well-being, it is important to note that there has been no conclusive evidence to link sunscreen and vitamin D deficiency. Increasing the UVA‐PF for a given SPF is associated with improved vitamin D3 production. Brief periods of “safe” sun exposure can help maintain vitamin D levels without excessive UV damage; the shadow rule — less UV exposure during early morning and late afternoon when an individual’s shadow is taller than the actual height, and more UV exposure when the shadow is shorter as compared to the height, can be used to gauge when it is relatively safe to go outdoors. Most weather apps also list UV index, created by the Environmental Protection Agency in conformation with recommendations from the World Health Organization; the UV index ranges from 0 to 11+ in concordance with the movement of the sun. Lower the UV index, safer the exposure to sunlight.
Protecting the skin from UV radiation is essential for long-term skin health and the prevention of sun-related conditions, including premature aging and skin cancer. Understanding the differences between physical and chemical sunscreens, following proper application techniques, and incorporating protective measures can effectively minimize UV damage.
References:
1. American Academy of Dermatology Association. (2025, January 31). How to Apply Sunscreen. https://www.aad.org/public/ everyday-care/sun-protection/shade-clothing-sunscreen/how-toapply-sunscreen
2. American Cancer Society. (2024, June 26). How to Use Sunscreen. https://www.cancer.org/content/dam/CRC/PDF/Public/9651.00.pdf
3. Bennett, S.L., & Khachemoune, A. (2022). Dispelling myths about sunscreen. The Journal of dermatological treatment, 33(2), 666–670. https://doi.org/10.1080/09546634.2020.1789047
4. Berry, E.G., Bezecny, J., Acton, M., Sulmonetti, T.P., Anderson, D.M., Beckham, H.W., Durr, R.A., Chiba, T., Beem, J., Brash, D.E., Kulkarni, R., Cassidy, P.B., Leachman, S.A. (2022). Slip versus Slop: A Head-to-Head Comparison of UV-Protective Clothing to Sunscreen. Cancers, 14(3), 542. https://doi-org.uiwtx.idm. oclc.org/10.3390/cancers14030542
5. Dara, J. (2025, March 3). Should you wear sunscreen on a plane? Dermatologists weigh in. Condé Nast Traveler. https://www. cntraveler.com/articles/why-you-should-wear-sunscreen-on-aplane
6. Flores, T. (2022, March 25). What is hybrid sunscreen? Chemical and mineral blends may be best for sun protection. HuffPost. https://www.huffpost.com/entry/chemical-mineral-hybrid-sunscreen-spfs_l_623b7184e4b046c938e488e6
7. Gabros, S., Patel, P., Zito, P.M. (2025). Sunscreens and Photoprotection. In StatPearls. StatPearls Publishing
8. EWG’s Guide to Sunscreens. (n.d.). The trouble with sunscreen ingredients | EWG’s Guide to Sunscreens. EWG’s Guide to Sunscreens ©2025. https://www.ewg.org/sunscreen/report/the-trouble-with-sunscreen-chemicals/
9. Passeron, T., Bouillon, R., Callender, V., Cestari, T., Diepgen, T., Green, A., Van Der Pols, J., Bernard, B., Ly, F., Bernerd, F., Marrot, L., Nielsen, M., Verschoore, M., Jablonski, N., Young, A. (2019). Sunscreen photoprotection and vitamin D status. British Journal of Dermatology, 181(5), 916–931. https://doi. org/10.1111/bjd.17992
10. Pfeifer, G.P. (2020). Mechanisms of UV-induced mutations and skin cancer. Genome Instability & Disease, 1(3), 99–113. https://doi.org/10.1007/s42764-020-00009-8
11. Taylor, S. (2002). Simple dosage guide for suncreams will help users. BMJ, 324(7352), 1526a–11526. https://doi.org/10.1136/ bmj.324.7352.1526/a
12. The Skin Cancer Foundation. (2025, January 27). Skin cancer Facts & Statistics - The Skin Cancer Foundation. https://www. skincancer.org/skin-cancer-information/skin-cancer-facts/
13. United States Environmental Protection Agency. (2025, March 20). Ultraviolet (UV) Radiation and Sun Exposure. https:// www.epa.gov/radtown/ultraviolet-uv-radiation-and-sun-exposure



Camille Irene Hulipas, OMS-II, is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027.
Elizabeth Ou, OMS-II, is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027. She is a Registered Nurse and a cancer survivor. Her interests include reproductive endocrinology, women’s health and dermatology.
Ramaswamy Sharma, MS, PhD, is a Professor of Histology and Pathology at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life. Dr. Sharma is a member of the BCMS Publications Committee.

By Ivana Tieu, OMS-III and Rachelle Hamblin MD, MPH
Every day, firefighters put their lives on the line — responding to emergencies, navigating hazardous environments, and facing unpredictable physical demands. Yet, beyond the emergencies they respond to, these frontline heroes face an invisible risk: occupational carcinogens. In 2022, the International Agency for Research on Cancer (IARC) officially classified firefighter occupational exposure as a Group 1 Known Human Carcinogen, directly linking the job to an increased cancer risk.
To help address these risks, the San Antonio Fire Department (SAFD), in collaboration with the SAFD Occupational Cancer Committee (OCC), organized the 3rd Annual SAFD Wellness and Cancer Prevention Fair. The event was coordinated by Rachelle Hamblin MD, MPH, a member of the SAFD OCC, who worked closely with SAFD, Local 624, the Fire Training Academy, Mays Cancer Center, UT Health San Antonio, the University of the Incarnate Word and over 40 health partners to bring this initiative to life over the past three years.
The fair was founded not only as a proactive health initiative, but also in response to the numerous losses of our brothers and sisters in the fire service. Cancer has now become the leading cause of line of duty deaths (LODDs) among firefighters, accounting for an alarming 75% of all cases. Through targeted cancer education, early detection screenings and community-wide collaboration, the event seeks to raise awareness of occupational cancer risks and ultimately reduce preventable cancer-related deaths among firefighters and their families.
The event aligned with January's Firefighter Cancer Awareness Month and focused on prevention, education and screening. More than 510 firefighters, retirees and family members attended and were supported by over 300 volunteers and 61 vendors. Booths offered services such as skin and pre-esophageal cancer screenings, HbA1c testing, osteopathic manipulative medicine, blood donations, nutritional counseling and educational materials focused on firefighterspecific health risks.
One of the main highlights was the free skin cancer screenings, conducted as part of the American Academy of Dermatology (AAD) SPOT Skin Cancer™ Check Program. The screenings were coordinated by Dr. Sandra Osswald of UT Health through the AAD SPOT Skin Cancer™ Check Program, with skin exams performed by dermatology and family medicine faculty and residents from UT Health San Antonio, the SAUSHEC military program and private practices.
Medical student volunteers from the University of the Incarnate Word School of Osteopathic Medicine (UIWSOM) and the Long School of Medicine supported the effort through outreach, assistance with skin exams and patient education. Together, the team performed 431 total skin exams. In addition to screening, medical students provided firefighters with educational handouts and one-on-one guidance tailored to their occupational risks. These materials included practical instructions on how to prevent skin cancer on the job — such as choosing appropriate UV-protective gear, incorporating sunscreen into daily routines, performing monthly self-screening exams, and
scheduling routine skin checks. Local community partners also contributed generously, donating sunscreen and protective hats to support firefighter health. Multiple confirmed diagnoses of melanoma, squamous cell carcinoma, basal cell carcinoma and precancerous lesions have resulted from this initiative over the past two years, empowering our firefighters to take action to prevent, treat, and survive occupational skin cancer.
Key services included 201 EsoGuard esophageal cancer screenings, with around 8% showing abnormal esophageal cell changes; 220 A1C screenings for blood sugar control; 80 osteopathic manipulative treatments (OMT); and 38 blood donations for local banks.
Since the fair’s start in 2023, more than 1,700 firefighters have participated and over 1,100 total skin exams have been completed. In some cases, screenings revealed lesions of concern, prompting further follow-up and, at times, life-saving treatment. These efforts are guided by the SAFD Occupational Cancer Committee, Local 624, SAFD and supported by local dermatologists, academic institutions, healthcare partners and volunteers.
The fair has grown each year and has served as a model across the nation, inspiring fire departments and the Firefighter Cancer Support Network to create their own health, wellness and cancer prevention programs. It continues to highlight the importance of proactive healthcare and has become part of a broader initiative — the San Antonio Firefighters Cancer Prevention Program — a historical partnership with SAFD, Mays Cancer Center, UT Health, Sylvester Cancer Center and the University of Miami to help lower cancer risks among firefighters and EMS personnel. As part of this expanded effort, the Mays Cancer Center contributes by helping connect firefighters diagnosed with cancer to comprehensive care, as well as screening, diagnosis and survivorship resources.
It's more than a wellness event — it's a community effort to protect those who protect us.

References:
1. International Agency for Research on Cancer. IARC Monographs on the Identification of Carcinogenic Hazards to Humans. Volume 132: Occupational Exposure as a Firefighter. Lyon, France: IARC; June 7–14, 2022. In press
2. Demers, P.A., DeMarini, D.M., Fent, K.W., et al. Carcinogenicity of occupational exposure as a firefighter. Lancet Oncol. 2022;23(8):985–986. doi:10.1016/S1470-2045(22)00390-4
3. American Academy of Dermatology. SPOT Skin Cancer™ Screening Program. https://www.aad.org/public/public-health/ spot-skin-cancer. Accessed June 5, 2025
4. National Institute for Occupational Safety and Health (NIOSH). Firefighter Cancer Awareness and Prevention. Centers for Disease Control and Prevention. https://www.cdc.gov/ niosh/firefighters/. Accessed June 5, 2025
Primary Author: Ivana Tieu
Contributing Author: Rachelle Hamblin MD, MPH

Ivana Tieu is a third-year medical student at the University of the Incarnate Word School of Osteopathic Medicine. She helped lead the planning and execution of the San Antonio Fire Department Wellness and Cancer Prevention Fair alongside UIWSOM students. Passionate about community health and dermatologic outreach, her article highlights the fair’s collaborative efforts to promote firefighter cancer prevention and expand access to early detection resources.
Acknowledgments: Elizabeth Hang, Suraiya Kerai, Fatma Zeynep Deligonul, Kayley Yates, Alicia Cortez, James Mayberry, MD, and Sandra Osswald, MD

By Rajam Ramamurthy, MD
John, in his early 70s, was having fun in the swimming pool of their spacious home with his 4-year-old grandson. Suddenly, he felt weakness in his left leg, and then his left arm. He called for help and said to his wife, “I'm having a stroke, call EMS,” pulled himself out of the pool, and lost consciousness. He was taken to the nearest hospital. That was 10 years ago. I visited John about a year later. He was in a wheelchair, and the left side of his body was paralyzed. His speech was unaffected, and his mind was as clear as it had been. He was working on a book. John and his wife were both physicians and served in academia all their lives.
John came to my mind when we were discussing editorial for San Antonio Medicine magazine. The discussion centered on stroke care in San Antonio. None of the people present knew any details. If the patient gets to the hospital alive, who will take charge? Is it an emergency room physician, a neurologist, a neurosurgeon or an interventional radiologist? My brain was racing; I must find the answer — at my age, stroke care matters. I volunteered to check. I started with a friend at University Hospital in the department of radiology. He introduced me to Dr. Sujani Bandela, a neurologist who is very involved with the stroke care program at University Hospital. The following is a summary of the interview.
Question: How prevalent is stroke in the U.S.? Please discuss the Texas scenario, and are there any differences between the populations?
Answer: The ‘Stroke Belt’ or ‘Stroke Alley’ is a geographic area in the eastern United States that has been recognized for having a high incidence of stroke compared to other places. It is debated if Texas belongs in the stroke belt. East Texas is included in the stroke belt. Eleven states, including Alabama, Arkansas, Georgia, Indiana, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee and Virginia, are in the stroke belt. In 2016, the stroke mortality rate was 126/100,000 in the belt compared to 99/100,000 nationally. Overall, this is a phenomenal decline in stroke mortality in the U.S. from 1968, when it was 582/100,000 in the stroke belt and 433/100,000 in the rest of the U.S.
More strokes are seen at a younger age in the East Texas and South Texas areas. There are differences in these areas due to socioeconomic disparities and more aggressive risk factors. Annually, in the U.S., about 800,000 people suffer from strokes.
Question: In a restaurant, mall or a gathering, a person is suddenly acting differently. What will make me think of a stroke?
Answer: The word that should come to mind is an acronym, BEFAST.
Balance: The person is stumbling, falling to the floor, or feels dizzy.
Eyes: Eyes deviated to a side, loss of vision or double vision.
Face: Deviation of the mouth, twitching.
Arm Weakness: Limp arm or leg, tingling sensation at fingertips.
Speech: Slurring of speech, no speech,
Time: Time is of the essence. The earlier the person receives care, the better the outcome.
EMT technicians, firefighters, ambulance technicians and hospital personnel are all trained to use BEFAST. There are designated stroke centers in San Antonio. University Hospital is one of them and the only one that has a Neuro-Intensive Care Unit and the only JCAHO-approved (The Joint Commission and the American Heart Association/American Stroke Association) comprehensive stroke center in San Antonio. Emergency responders may go to one of the stroke centers if they recognize BEFAST signs in a patient. Sophisticated communication systems are in place, allowing the expert team to provide constant guidance to the transportation team. Comprehensive stroke centers, such as University Hospital, conduct weekly reviews of patients seen and maintain extensive data on management and outcomes. The weekly meetings comprise physicians (stroke, neurosurgery, emergency medicine, radiology), nursing, case managers, stroke coordinators and stroke navigators. The South Texas Regional Advisory Council also tracks progress and serves as a valuable resource for stroke centers, hosting annual meetings with first responders, physicians, nurses, and all patient care providers and staff.
Question: What are the risk factors for stroke?
Answer: Those conditions that are a risk factor for heart disease are also the factors for stroke. These are people with diabetes who have a three times higher risk of stroke, high blood pressure, high cholesterol, smoking and alcohol. These are the significant risk factors, but there are other, rarer causes of strokes, including autoimmune, trauma-related artery tears known as dissections, and substance use (methamphetamine and cocaine).
Question: I hear people who enjoy alcohol say that they take one alcoholic drink every day, and it is protective against heart disease. Can that apply to stroke?
Answer: No. Two or three drinks a week may be acceptable, but no relationship to stroke prevention. Substance use is one of the significant factors for stroke in the younger age group.
Question: What happens after a patient is brought to the stroke center?
Answer: After they reach our stroke center, a stroke alert is paged out to the ER, stroke doctors and rapid response teams. Then, a quick assessment is completed within minutes; CT scan imaging is done quickly to make a decision on timely interventions such as administering clot-busting medications or procedures to remove a clot (if seen on the CT scan). At that point, a neurointerventionalist is called who performs the procedure. The patient is watched closely in our neuro-ICU. There begins the start of the hospitalization, including the rest of the stroke workup of why it happened, so we can prevent another. Simultaneously, early therapies are started of physical, occupational and speech therapy to improve patient outcomes. Also, case management teams and coordinators are present and active in helping with discharge planning and further rehab plans.
The person is stumbling, falling to the floor, or feels dizzy.
Eyes deviated to a side, loss of vision or double vision.
Deviation of the mouth, twitching.
Limp arm or leg, tingling sensation at fingertips.
Slurring of speech, no speech. Time is of the essence. The earlier the person receives care, the better the outcome.
It is a whole team of experts from various fields working together to impact stroke care. From the witness and patient at the scene, to the first responders, ER personnel, stroke and neurosurgery teams, therapists, coordinators and case managers, it takes a comprehensive team to improve care and outcomes for the complex patients of stroke.
I thank Dr. Bandela for providing succinct information on stroke management. It is comforting to know that excellent stroke care is available for stroke victims in our city. The Baptist Hospital System has a network of facilities in different parts of the city that are Certified Stroke Care Centers. So are the Regional Hospitals and others. What could be improved is public awareness. It is my impression that BEFAST is not at the tongue tip of the common people as CPR is. I desire that those who have accidentally come across this article will copy the BEFAST table and put it on the refrigerator.
The use of recombinant tissue plasminogen activator (rTPA) administered within 4.5 hours of the patient's arrival at the stroke care center is the gold standard treatment for ischemic stroke. Surgical interventions for removing the clot are also frequently considered. It was a miracle that my friend was a physician and recognized his symptoms, or I wouldn’t be thumbing through his latest book today. More frightening is the thought of the child he was with, had he not been so quick.


Sujani Bandela, MD, is a Vascular Neurologist at University Hospital; an Assistant Professor, Vascular Neurology; Associate Program Director, Neurology Residency; and Associate Program Director, Vascular Neurology Fellowship at UT Health San Antonio.
Rajam Ramamurthy, MD, is a Professor Emeritus, Department of Pediatrics, UT Health San Antonio; BCMS Past President; Past Chair, BCMS Publications Committee, and currently serves on the BCMS Publications Committee.
By Parker Burch and Jairo Melo, MD
One of the primary benefits of employee wellness programs is the improvement in physical health. Regular health screenings, fitness challenges and nutritional guidance can help employees maintain a healthy lifestyle, reducing the risk of chronic diseases and absenteeism. But company resources can extend beyond physical wellness.
Work-Life balance is a crucial aspect of employee wellness, emphasizing the importance of maintaining a healthy equilibrium.
Introduction
Asthma is a chronic condition that impacts the lungs, in which the airway is hyperreactive and causes bronchospasm. It is thought to have a higher incidence in swimmers due to their continuous exposure to inhaling chlorine (which sits on the water’s surface) and cold water (which constricts the airway). Exercise-induced asthma (EIA) occurs several minutes after exercise begins. The prevalence of asthma in the general population is 5-20% and even higher in elite athletes.4
Hypothesis
Swimmers with cold and chlorine exposure have a higher prevalence of exercise-induced asthma compared to non-swimmer athletes.
Methods
1. Among high school students, 25 random athletes were selected from the swim, cross country and basketball teams. All were collectively non-smokers or vapers and had a BMI of less than 30. Those who had pre-existing lung conditions were taken into consideration during data analysis.
2. Athletes underwent baseline pulmonary function tests (PFTS) before their athletic sport and again after 15 minutes of exercise. Due to the nature of different athletics practices, cross-country athletes were tested outside, basketball athletes were tested inside, and swimmers were tested with a mix of indoors and outdoors. Each athlete performed pre- and post-exercise PFTs. PFTs include mea-
surements of FEV1, FEF 25%-75% (L/s), and FEV1/FVC (%).
The tests were repeated three times to reduce error.
3. Exercise-induced asthma is defined as airflow obstruction manifested either as an FEV1/FVC (%) of less than 70%, an FEV1 drop greater than 12%, and/or an FEF 25%-75% drop greater than 20%.
After testing, athletes were separated into three categories: Group 1, normal athletes, were those who began with normal PFTs and remained normal after exercise. Group 2, asthma athletes, began with abnormal PFTs. Group 3, exercise-induced asthma, were those athletes who started with normal PFTs and developed evidence of airflow obstruction after exercise.
Out of the 25 athletes, seven had PFTS with airflow obstruction suggestive of asthma (28%), and nine out of 25 (36%) had exercise-induced airflow obstruction suggestive of EIA. Only two athletes were aware of the airflow obstruction/asthma (8%).
Three out of 10 swimmers had exercise-induced asthma (EIA). They were all females and had been participating in swimming for more years than the other swimmers. Only one had pre-existing lung conditions. All swimmers were tested in cold weather (34º to 45º F). When testing the cross-country athletes (10 athletes), six out of 10 athletes had abnormal test results. Three were abnormal at baseline, and only one was aware of their asthma. The other three had normal baselines and worsened after exercise. The athletes with EIA were a mix of males and females, all with no pre-existing lung conditions and varying years of involvement in their sport, and they were all tested outside in cold temperatures (45º F). Lastly, when testing the basketball athletes, none had pre-existing lung conditions. However, five out of five had abnormal PFTs. Three of them were triggered by exercise, and none were aware. The athletes were all male and had spent many years doing their sport. They were all tested indoors in a climate-controlled environment (72º F).
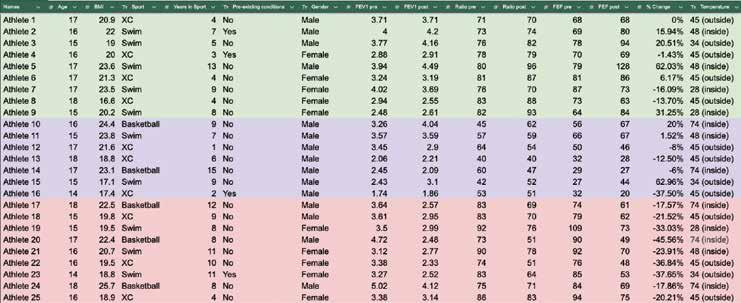

Based on the data collected in this study, there was no causal association between exposure to chlorine chemicals and the development of EIA in swimmers. The temperature of the air/water suggests significant risk factors for EIA. The cross-country athletes, who were all practicing in the cold, all had drops in their PFTs, but not all were significant enough to diagnose EIA. The same effect occurred for the swimmers with EIA, as they demonstrated substantial decreases in their lung function when swimming in cold weather. In contrast, the basketball athletes were in a climate-controlled environment; therefore, the temperature could not have been the cause of their diagnosis. This suggests that cold weather conditions could increase the risk of exercise-induced asthma.
In general, 15% to 25% of athletes have symptoms of asthma/ EIA.2 24% of athletes showed signs of asthma, and 36% of athletes showed signs of EIA. This demonstrates how the athletes with EIA in this study exceed the predicted amount. All of the athletes tested who showed results of EIA or asthma were not previously aware that they had this condition (except two athletes). Overall, 60% of athletes tested had EIA/asthma, and only two knew about it.
So few of these athletes were aware of their breathing conditions, which suggests the need for further research to spread awareness surrounding asthma and EIA. The typical stigma in athletes is that EIA and asthma are minor setbacks when, in reality, it can negatively impact an athlete’s performance.1 Spreading awareness of the significant prevalence of these conditions will assist athletes in recognizing these symptoms and seeking the proper treatment for themselves. However, one of the limitations of my study is that I had a small sample size, and this study was performed at one institution. For studies produced in the future, I will replicate with a larger sample size and more variety.
Percentage of Athletes’ Diagnosis
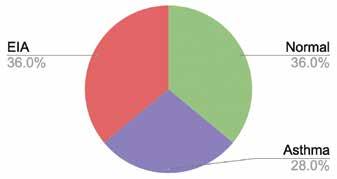
References:
1. Couto, M., et al. “Diagnosis and Treatment of Asthma in Athletes.” Breathe, vol. 8, no. 4, 1 June 2012, pp. 286–296, breathe.ersjournals.com/content/8/4/286, https://doi. org/10.1183/20734735.009612
2. Miller, Michael G., et al. National Athletic Trainers’ Association Position Statement: Management of Asthma in Athletes. 2005
3. Mountjoy, M., Fitch, K., Boulet, L.P., Bougault, V., van Mechelen, W., & Verhagen, E. (2015). Prevalence and characteristics of asthma in the aquatic disciplines. Journal of Allergy and Clinical Immunology, 136(3), 588–594. https://doi.org/10.1016/j. jaci.2015.01.041
4. O’Byrne, P. (2019). UpToDate. Retrieved from Uptodate.com website: https://www.uptodate.com/contents/exercise-induced-bronchoconstriction
5. Päivinen, M., Keskinen, K., Putus, T., Kujala, U. M., Kalliokoski, P., & Tikkanen, H. O. (2021). Asthma, allergies and respiratory symptoms in different activity groups of swimmers exercising in swimming halls. BMC Sports Science, Medicine and Rehabilitation, 13(1). https://doi.org/10.1186/s13102-021-00349-2


Parker Burch is a student at Brandeis High School, class of 2026, on the varsity swim and water polo teams. She is interested in potentially pursuing a career in the medical field.
Jairo Melo, MD, is a full-time practicing Pulmonary and Critical Care Physician, co-founder and Medical Director of TexasIPS, the largest Pulmonary group in Texas, and the Medical Director for the Critical Care and Thoracic service line for the Methodist Healthcare System in San Antonio. He has a passion for clinical integration among all different specialties involved in patient care, and his mission is to help people around him to achieve professional growth. Dr. Melo is a member of the Bexar County Medical Society.
Awareness of EIA & Asthma Diagnosis



January-March 2025
December 2024
ALLMED Planning Begins. BCMSA leaders Jenny Shepherd, Victoria Kohler-Webb and Danielle Henkes serve on the ALLMED Planning Committee.

Monthly Planning Continues. BCMSA is responsible for creating the theme, making decorations, organizing the Kick-Off Luncheon, obtaining sponsors and preparing participant goodie bags.
April 2025
BCMSA Empty Nester members
Mary Jo Dotson and Katrina Theis host Connect & Create to assemble ALLMED decorations and goodie bags.



Mary Jo Dotson
Katrina Theis
Louise Chumley
Virginia Profenna
Michelle Richardson
Rebecca Waller
Victoria Kohler-Webb
Danielle Henkes
Jenny Shepherd
May 8-10, 2025


The ALLMED Kick-Off Luncheon starts the conference at JW Marriott’s Cibolo Moon.

Check-In & Registration



TMAA President Jenny Shepherd welcomes attendees to the Day 1 afternoon session. Speakers included BCMS physician Nora Vasquez, MD, who shared insights on “High-Performance Leadership.”

The Poster Session Reception featured nine programs from local Texas Alliances. “Empty Nesters: Still Soaring” was the BCMSA poster entry, created by Danielle Henkes.
THANK YOU ALLMED ATTENDEES & VOLUNTEERS
Jenny Shepherd
John Shepherd, MD
Victoria Kohler-Webb
Katrina Theis
Neha Shah
Martha Vijjeswarapu
Danielle Henkes
Our Day 2 Session began with the TMAA Annual Business Meeting, led by President Jenny Shepherd. Adoption of updated state bylaws was one key business item, with Bexar well-represented by seven voting delegates: Jenny Shepherd, John Shepherd, Victoria Kohler-Webb, Katrina Theis, Neha Shah, Martha Vijjeswarapu and Danielle Henkes. The 2026 TMAA Board was voted upon and recognized.


OUR BCMSA LEADERS
Jenny Shepherd Council of Past Presidents & Advisory Committee
Victoria Kohler-Webb
Resource Liaison
2025-6 TMAA BOARD
Six rotating Roundtable Discussions filled out the morning, with BCMSA’s offering — “SOS (Struggles and How to Deal with Them)” — moderated by Victoria Kohler-Webb and Danielle Henkes. The exercise gave productive ideas to both participants and moderators to implement with their local alliances.


CONGRATULATIONS
Jenny Shepherd
John Shepherd, MD Dena Frolichstein
PLUS 1 MEMBER RECOGNITION
The Celebration Luncheon recognized Alliance accomplishments throughout the state. BCMSA received several membership awards: Silver Medal for TEXPAC Membership, Silver for Auto-Renewal, Bronze for 1st Time member increase.


“Adventure!” was the theme of the 32nd TMA Foundation Gala. Power couple TMAA President Jenny Shepherd and BCMS President John Shepherd co-hosted the event.

Day 3: ALLMED concluded Saturday morning at the TMA House of Delegates Business Session as Jenny Shepherd gave her farewell speech and installed her successor, Joi Smith, of the Smith CMS, as incoming TMAA president.

JENNY SHEPHERD 2024-5 TMAA PRESIDENT FAREWELL REMARKS
“As this year ends, my heart is full of gratitude. There have been challenges and victories. More than anything, there have been countless moments that reminded me just how special the Texas Medical community is. Thank you all for showing up in meaningful ways, for lifting each other up, and for the countless ways you’ve made a difference in your communities. It has been an honor to lead — but even more so, a privilege to serve alongside passionate, committed leaders. I know you have a choice in where you dedicate your time, energy and heart, and I’m incredibly grateful that you chose to spend it with me, in the service of Texas medicine and its families this year.”
By Melody Newsom, BCMS CEO/Executive Director
The Bexar County Medical Society (BCMS) had a banner weekend at the 2025 TexMed conference, held May 9–10 at the JW Marriott in San Antonio, which brought statewide attention to what I can only describe — fittingly — as a Superfecta of BCMS leadership. For those who know me, you know I spent many years in the horse racing business, so it’s no stretch for me to say that seeing five of our own cross the finish line with such impact and recognition was truly a winning ticket for organized medicine in Texas.
Jayesh “Jay” Shah, MD (BCMS President 2016) , was officially installed as the President of the Texas Medical Association (TMA). A respected physician and longtime leader in the medical community, Dr. Shah brings deep experience, vision and passion to this role. His presidency marks a significant milestone for BCMS and the broader Texas medical community, as he continues to advocate for physicians and patients statewide.
David N. Henkes, MD (BCMS President 2005) , received the prestigious TMA Distinguished Service Award in honor of his years of dedicated leadership of the Texas Delegation to the American Medical Association (AMA). Dr. Henkes has long been a guiding force at the intersection of state and national medical policy, and this award is a fitting tribute to his steadfast service.


Ezequel “Zeke” Silva, MD (BCMS President 2024) , has been making an indelible impact as Chair of the TMA Council on Legislation. In a legislative session marked by complex healthcare issues, Dr. Silva is a near-constant presence at the Texas Capitol — testifying multiple times per week on behalf of physicians and patients. His knowledge, poise and persistence have made him a trusted advocate under the dome.

John M. Shepherd, MD , the current President of BCMS , has stepped into a key leadership role as the new Chair of TEXPAC , the Texas Medical Association’s Political Action Committee. With a sharp focus on physician advocacy and policy influence, Dr. Shepherd is poised to help shape the future of healthcare in Texas through strategic political engagement.

Rounding out this impressive group is Jenny Shepherd , who continues to serve the medical community with heart and grace. She is the Immediate Past President of the TMA Alliance, Chair of First Tuesdays at the Capitol and is now stepping in as the acting President of the BCMS Alliance , continuing her legacy of support for physicians, their families and the broader health of the community.

In my 25+ years with BCMS, I have been blessed to work with these and so many other incredible physician leaders. Their dedication and service are not only admirable — they’re inspiring.
But this moment isn’t just about recognition — it’s a call to action. Please join these outstanding physicians who are making a real difference in the practice of medicine and our community’s health and safety. We need you to get involved. Whether you’re new to organized medicine or a longtime member, your engagement is crucial as we shape the future of healthcare in Texas.
Let’s keep this momentum going — and turn our Superfecta into a winning tradition.
As a BCMS member, you can find exclusive discounts on premium products and services that you and your practice use every day.

Sol Schwartz & Associates P.C. (HHH Gold Sponsor)
Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Christopher Davis, CPA 210-384-8000, ext. 118 cbd@ssacpa.com www.ssacpa.com
“Dedicated to working with physicians and physician groups.”

Atlas Retirement Strategies LLC (HHH Gold Sponsor)
Atlas Retirement Strategies LLC is a comprehensive financial planning firm dedicated to serving the unique needs of the medical community. We offer customized strategies in business planning, retirement planning, risk management, wealth preservation, estate planning, and wealth transfer – empowering healthcare professionals to achieve long-term financial security, clarity, and peace of mind.
Amanda Webb, LACP Founder & Principal 210-281-4400
Amanda@atlas-plans.com www.atlas-plans.com
MANAGEMENT

Aspect Wealth Management (HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark President 210-268-1520
MClark@aspectwealth.com www.aspectwealth.com
“Your wealth. . .All aspects”

Broadway Bank (HHH Gold Sponsor)
Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead 210-283-6640
TDuran@broadway.bank
www.broadwaybank.com
“We’re here for good.”

Texas Partners Banks (HHH Gold Sponsor)
Our private banking team specializes in healthcare banking and will work with you to craft and seamlessly integrate financial solutions for you and your practice, including practice loans, lines of credit and custom local lockbox solutions headquartered in San Antonio.
Maria Breen 210-807-5562
Maria.Breen@texaspartners.bank www.texaspartners.bank

Lone Star National Bank (HHH Gold Sponsor)
Established in 1983, Lone Star National Bank has provided banking services to communities in South Texas for the past 41 years. LSNB is an independent and locally owned bank subsidiary of Lone Star National Bancshares-Texas, Inc with consolidated assets of $3 billion (12/31/23) and 36 full-service banking centers throughout Starr, Hidalgo, Cameron and Bexar counties.
Aside from personal and business banking, LSNB offers investments, wealth management & trust along with property and casualty insurance, health insurance and supplemental coverage.
Ivan Corona Molina Assistant VP 210-479-4713
MolinaI@lonestarnationalbank.com www.lonestarnationalbank.com
“We do what the Little Banks can’t, and the Big Banks won’t!”
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Robert Lindley
SVP | Private Banking Team Lead 210-343-4526
Robert.Lindley@amegybank.com
Denise Smith
Vice President | Private Banking 210-343-4502
Denise.C.Smith@amegybank.com
Scott Gonzales
Assistant Vice President | Private Banking 210-343-4494
Scott.Gonzales@amegybank.com www.amegybank.com
“Community banking partnership”
Synergy Federal Credit Union (HH Silver Sponsor)
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help physicians get the banking services they need. Synergy FCU Member Services 210-750-8333 info@synergyfcu.org www.synergyfcu.org
“Once a member, always a member. Join today!”

American Health Imaging (HHH Gold Sponsor)
American Health Imaging (AHI) has 5 state-of-the-art imaging centers in San Antonio, TX with industry- boardcertified subspecialized radiologists delivering precise, reliable results. Easy scheduling and prompt report turnaround times, serving both physicians and their patients. Imaging at AHI is priced up to 60% less than hospitals and in-network with 99% of health plans with competitive rates to save patients money. AHI has an additional 37 best-in-class diagnostic imaging facilities in Alabama, Florida, Georgia, Texas and South Carolina. US Radiology Physician Number 210-572-1211
Casey Allen
Regional Sales Director | San Antonio US Radiology Specialists 210-846-0606
Casey.Allen@usradiology.com
Jasmine Mendoza
Jasmine.Mendoza@usradiology.com
Jaime Zamora Jaime.Zamora@usradiology.com

Sydnie Caradec
Sydnie.Caradec@usradiology.com
Sarah McMindes
Sarah.Mcmindes@usradiology.com
Scott Roberson
Scott.Roberson@usradiology.com
Ryan Denman
Ryan.Denman@usradiology.com
www.americanhealthimaging.com (main site)
www.americanhealthimaging.com/ physician-resources/ (Physician Resources to refer to American Health Imaging)

Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor)
Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for healthcare entities.
Betty Fernandez Director of Operations 210-582-6355
Betty.Fernandez@bexarcv.com www.bexarcv.com
“Proudly serving the medical community since 1998”

Avid Wealth Partners (*** Gold Sponsor)
For over 15 years, Avid Wealth Partners has been the trusted financial partner for local physician specialists and practice owners. We specialize in physician-focused financial advising, offering proactive tax planning, customized investment strategies, and comprehensive risk management solutions. Our approach addresses every aspect of your financial life, protecting your hardearned assets and building lasting wealth. With a team of credentialed specialists, we simplify complexity so you can focus on what you do best— caring for patients
MDWealth@avidwp.com www.avidforphysicians.com 210-864-3333

Elizabeth Olney with Edward Jones (HHH Gold Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney
Financial Advisor 210-858-5880
Elizabeth.Olney@edwardjones.com www.edwardjones.com/elizabeth-olney "Making Sense of Investing"

Aspect Wealth Management (HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark President 210-268-1520
MClark@aspectwealth.com www.aspectwealth.com
“Your wealth. . .All aspects”
Hancock Whitney (HH Silver Sponsor)
Since the late 1800s, Hancock Whitney has embodied core values of Honor & Integrity, Strength & Stability, Commitment to Service, Teamwork and Personal Responsibility. Hancock Whitney offices and financial centers in Mississippi, Alabama, Florida, Louisiana and Texas offer comprehensive financial products and services, including traditional and online banking; commercial, treasury management, and small business banking; private banking; trust; healthcare banking; and mortgage services.
John Riquelme
San Antonio Market President 210-273-0989
John.Riquelme@hancockwhitney.com
Serina Perez San Antonio Business Banking 210-507-9636
Serina.Perez@hancockwhitney.com

UT Health San Antonio
MD Anderson Cancer Center (HHH Gold Sponsor)
UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
UT Health San Antonio Physicians
Regina Delgado
Business Development Manager 210-450-3713
DelgadoR4@uthscsa.edu
UT Health San Antonio
MD Anderson Mays Cancer Center
Laura Kouba
Business Development Manager 210-265-7662
NorrisKouba@uthscsa.edu
Appointments: 210-450-1000
UT Health San Antonio 7979 Wurzbach Road San Antonio, TX 78229

Golden Billing & Benefits
(HHH Gold Sponsor)
Golden Billing is owned and operated for over 20 years in Houston, TX. The owner, Marcus Yi, is focused on creating a partnership with clients. We are dedicated to optimizing the small business doctor’s productivity and maximizing practice cash flow by accurate claims coding and timely processing. Call today for a free consultation. If you don’t want to use us at lease maybe we can help you fine tune your decision.
Marcus Yi 713-263-0054
MYi@goldenbilling.com www.goldenbilling.com

Genuine Health Group (HHH Gold Sponsor)
Genuine Health Group partners with primary care providers to help them successfully adopt value-based payment models and demonstrate better health outcomes. Providers choose us for our proven expertise and consistency both for their patients enrolled in Medicare Advantage plans and for their patients with traditional Medicare who can align with one
of ACOs. We have a track record of effectively reducing the cost of care while simultaneously improving care quality.
786-878-5500
info@genuinehealthgroup.com www.genuinehealthgroup.com
Equality Health (HH Silver Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos Network Development Manager 210-608-4205
CLeos@equalityhealth.com www.equalityhealth.com “Reimagining the New Frontier of Value-Based Care.”
DialOPS
(H Bronze Sponsor)
Dialops is a trusted U.S.-based medical answering service and virtual receptionist solution designed specifically for healthcare practices. We provide 24/7 live call handling, HIPAA-compliant messaging, appointment scheduling, and reliable after-hours and overflow support. Our medically trained agents answer every call with professionalism and care—just like your in-office staff— ensuring your patients always feel heard and supported. From solo providers to busy clinics, Dialops helps reduce missed calls, ease front desk overload, and improve the patient experience—all at a fraction of the cost of hiring in-house.
Rachel Caero Rachel@dialops.net
Call 877-2-DIALOPS/ 210-699-7198 or visit www.dialops.net to get started today.

TMA Insurance Trust
(HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service insurance agency offering a full line of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.
Wendell England Director of Member Benefits
512-370-1746
Wendell.England@tmait.org
800-880-8181
www.tmait.org
“We offer BCMS members a free insurance portfolio review.”

Texas Medical Liability Trust (HHHH 10K Platinum Sponsor)
With more than 20,000 healthcare professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of healthcare for patients by educating, protecting and defending physicians.
Patty Spann Director of Sales and Business Development 512-425-5932
Patty-Spann@tmlt.org www.tmlt.org
“Recommended partner of the Bexar County Medical Society”

The Bank of San Antonio Insurance Group, Inc. (HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Katy Brooks, CIC 210-807-5593
Katy.Brooks@bosainsurance.com www.thebankofsa.com
“Serving the medical community.”
MedPro Group (HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze, RPLU, ARM
AVP Market Manager, SW Division 512-658-0262
Fax: 844-293-6355
Kirsten.Baze@medpro.com www.medpro.com
LASO Health Telemedicine and Rx App (HH Silver Sponsor)
LASO Health is the industry’s only solution that makes healthcare services accessible, cost-transparent and convenient. Its mission is to reinvent “healthcare” in the United States by empowering every individual and employer, insured or uninsured to have easy, timely, predictable, cost-effective care. LASO combines an intuitive, mobile superapp with a marketplace of virtual and in-person health services to give customers a one-touch, onestop-shop, comprehensive health solution.
Ruby Garza, MBA 210-212-2622
RGarza@texaskidneycare.com www.lasohealth.com

Parvus Medical Suites (HHHH 10K Platinum Sponsor)
Parvus Medical Suites offers a new way to start your own private clinical practice, either full-time or part-time, at a much lower cost than a traditional clinic. We take care of providing well-qualified employees, so that you can focus solely on delivering high-quality patient care. Our turn-key practice spaces in San Antonio and New Braunfels are available for short- and long-term lease options, and come complete with all amenities. Micropractice medicine is revolutionizing independent clinical care.
John Rodriguez, MD Chief Medical Officer 210-632-3411
DrJohn@parvussuites.com www.parvussuites.com
Henry Schein Medical (HH Silver Sponsor)
From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Kelly Emmon
Field Sales Consultant
210-279-6544
Kelly.Emmon@henryschein.com www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”
Eleos Virtual Healthcare Solutions (HH Silver Sponsor)
Empowering physicians for a Balanced Future. Our virtual health associates alleviate administrative burdens in the evolving healthcare landscape, combatting burnout. Join us in transforming healthcare delivery, prioritizing your wellbeing and patient care.
Darby Rodriguez Regional Client Executive 281-753-3565
D.Rodriguez@eleosvhs.com www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care”
Methodist Physician Practices (**Silver Sponsor)
Methodist Physician Practices is committed to providing exceptional care for patients in greater San Antonio and South Texas. As part of Methodist Healthcare, we are dedicated to raising the standards of performance excellence while advancing the health and well-being of the communities we serve. Our extensive network of highly-skilled primary care physicians, specialists and surgical care providers ensures patients receive comprehensive, coordinated and compassionate care.
As part of the Methodist Healthcare System, our physicians are committed to delivering personalized, high-quality services that meet the
diverse needs of our patients. At Methodist Physician Practices, we go beyond healthcare — providing hope, healing and unwavering support for each individual we serve.
Erin Fitzgerald
Methodist Healthcare I Methodist Physician Practices M:281-673-7350
methodistphysicianpractices.com
Healthcare Leaders of San Antonio (HH Silver Sponsor)
We are dedicated to nurturing business connections and professional relationships, exchanging knowledge to enhance leadership, and creating career opportunities for healthcare and other industry leaders in a supportive community.
David Neathery President 210-797-8412
HealthcareLeadersSA@gmail.com
Gary Meyn, LFACHE Vice President 210-912-0120
GMeyn@vestedbb.com https://healthcareleaderssa.com/ “Come, Learn, Connect!”
The Health Cell (HH Silver Sponsor)
“Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more! Kevin Barber President 210-308-7907 (Direct) KBarber@bdo.com
Valerie Rogler Program Coordinator 210-904-5404
Valerie@thehealthcell.org www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA)
(HH Silver Sponsor)
SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising. Jeannine Ruffner President info4@samgma.org www.samgma.org

Favorite Healthcare Staffing
(HHHH 10K Platinum Sponsor)
Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle.
San Antonio Office 210-301-4362
www.favoritestaffing.com
“Favorite Healthcare Staffing offers preferred pricing for BCMS members.”



By Stephen Schutz, MD
The 2025 Mercedes Maybach GLS600 luxury SUV is not for the shy or understated. Its towering stance, relentless opulence and sixfigure price tag serve not only as a vehicle but as a mobile monument to success — or at least the appearance of it. In a world drunk on SUVs, the Maybach GLS is a black truffle sitting atop a table of cheeseburgers. But is it realistic to own, or just the perfect vehicle to take to a Diddy party?
Design-wise, the GLS600 wears a garish oversized grille, gleaming like a Bond villain’s grin. Gone are the meek pretensions of being just an S-Class on stilts. This is now an extroverted luxury monolith, an unspoken deal struck between Mercedes’ wealthiest customers and a company that’s obviously trying to keep up with Rolls Royce and Bentley.
For the record, the Maybach GLS600 starts at $178,450, but with options and option packages expect to pay over $200,000 even if you configure yours while sober (my press car stickered for just over $240,000). Fuel economy is a disappointing 18MPG Highway and 13MPG City, and I would imagine not a single owner cares.
Beneath the long hood lies the ubiquitous (and delicious) Mercedes 4.0-liter twin-turbocharged V8, massaged to deliver 550HP and 538 lb-ft of torque. Thanks to the EQ Boost 48-volt mild hybrid

system, there’s a mild jolt of electricity on takeoff — more refinement enhancer than performance tool. Zero to sixty takes just 4.7 seconds, though this is a machine built not for speed but for effortless thrust. Nevertheless, it feels as quick as its numbers indicate.
For many buyers, the Maybach GLS is not really about driving, it’s about being driven. Slip into the rear cabin and you’re greeted with a twin-throne layout that would shame most business-class seats. Reclining captain’s chairs with calf support, cooled cupholders and individual climate zones provide an exceptionally opulent experience in the second row (a normal second row seat that can accommodate three passengers is available if you’d prefer).
Naturally, sumptuous materials abound: porcelain white Nappa leather, dark walnut trim inlaid with Maybach crests, and even a “Moonlight Edition” interior theme that bathes the cabin in ambient light designed to mimic lunar radiance. It’s theatrical, almost absurd, and completely OTT. I fully expect to see one featured soon on, Your Friends and Neighbors
Yet the Maybach GLS600 rides on the same platform as the more pedestrian GLS450, and occasionally its humble origins peek through




the silk curtains. Yes, the E-Active Body Control suspension scans the road and counteracts roll, but there’s no hiding 6,000 pounds of rolling indulgence. On tight switchbacks, the Maybach feels as out of place as a tuxedo in a dive bar.
Where the Maybach excels — and perhaps overdelivers — is in its silencing of the outside world. At 75 mph, the cabin is tomb-quiet with engine, road and wind noise that have been almost completely banished. The only sound you’re likely to hear is your own sigh of satisfaction.
Technology is predictably everywhere. The updated MBUX infotainment system recognizes gestures, whispers and even mood. The rear tablets now integrate AI-assisted concierge functions, capable of booking restaurant reservations or suggesting playlist changes depending on cabin “emotional tone.” It’s as if Mercedes wants to replace not just the chauffeur, but your therapist and personal assistant, too.
There’s also the small matter of image. For those who find the RollsRoyce Cullinan and Bentley Bentayga insufficiently extroverted, the Maybach GLS offers a uniquely Teutonic form of automotive jewelry. It is less aristocratic than the Rolls, less sporty than the Bentley, and more visually ostentatious than either. And that’s precisely the point. This is not old money discretion but rather nouveau riche projection. The Maybach GLS says you’ve made it, and you’d like everyone to know.
Of course, there are flaws. The cargo space is laughable unless you select the standard rear seats, the footprint is mansion-like, and the design — particularly if you choose the two-tone paint and 23-inch turbine wheels — is a lot more Miami than Boerne. Those seeking subtlety should look elsewhere, but to critique the Maybach GLS600 for its excess is to miss the point. This is a statement vehicle, a rolling reflection of affluence, engineered for those whose egos are too large for a mere sedan.
And yet, beneath the spectacle, there is genuine substance. The engineering, craftsmanship and refinement present here are not marketing tricks. The Maybach GLS600 delivers a uniquely indulgent experience that combines German precision with unapologetic theater.
In the end, the 2025 Maybach GLS600 is the automotive equivalent of wearing a silk smoking jacket to breakfast. Completely unnecessary, utterly excessive, and yet strangely irresistible. And it’s definitely not for everyone, not even everyone who can afford it.

Stephen Schutz, MD, is a board-certified Gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.




11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Northside Honda 9100 San Pedro Ave. San Antonio, TX 78216
Jaime Anteola 210-744-6198
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Anthony Garcia 210-681-3399
14610 IH 10 West San Antonio, TX 78249
Tim Rivers 832-428-9507
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Domingo Saenz 210-341-3311
Auto Group
North Park Lexus 611 Lockhill Selma San Antonio, TX 78216
Jose Contreras 320-308-8900
Bluebonnet Chrysler
Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX 78006
James Godkin 830-981-6000
Cavender Toyota 5730 NW Loop 410 San Antonio, TX 78238
Spencer Herrera 210-581-0474
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX 78216
Chris Martinez 210-366-9600
North Park Toyota 10703 SW Loop 410 San Antonio, TX 78211
Justin Boone 210-635-5000
9455 IH 10 West San Antonio, TX 78230
Jordan Trevino 210-764-6945
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX 78257
James Cole 210-816-6000
Northside Ford 12300 San Pedro San Antonio, TX 78216
Marty Martinez 210-477-3472
North Park Lincoln 9207 San Pedro San Antonio, TX 78216
Sandy Small 210-341-8841
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200

North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson 877-356-0476


