




Reflections from a TMA Insurance Trust advisor:
“When a physician reached out for help with health insurance. I immediately recognized the name. Because we’d worked together before, I remembered how committed they were to getting the right coverage—for themselves, their employees, and their families.
We moved right into reviewing plans, discussing options, and choosing what fit. I followed up with the practice manager, answered every question, and made sure no detail was overlooked. They told me how much the clear communication and care throughout the process meant to them— something I won’t forget.
That’s what I do for every physician I work with. Listen carefully, follow through, and stay involved long after coverage begins.”
Whether you work independently, with a partner, or manage a team, you may qualify for group coverage—even just for yourself and your family. With or without employees, we’ll help you find a plan that fits how you practice and who you care for.


Start your conversation at tmait.org, scan the QR code, or call 800-880-8181, Monday through Friday, 8:00 AM to 5:00 PM CST.


SCAN TO CALL




San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EDITORIAL CORRESPONDENCE:
Bexar County Medical Society 4334 N Loop 1604 W, Ste. 200 San Antonio, TX 78249
Email: editor@bcms.org
MAGAZINE ADDRESS CHANGES: Call (210) 301-4391 or Email: membership@bcms.org
SUBSCRIPTION RATES: $30 per year or $4 per individual issue
ADVERTISING CORRESPONDENCE: Louis Doucette, President Traveling Blender, LLC.
A Publication Management Firm 10036 Saxet, Boerne, TX 78006 www.travelingblender.com
For advertising rates and information Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national origin, or an intention to make such preference limitation or discrimination.
PUBLISHED
Traveling Blender, LLC. 10036 Saxet Boerne, TX 78006
PUBLISHER: Louis Doucette louis@travelingblender.com
BUSINESS MANAGER: Vicki Schroder vicki@travelingblender.com
GRAPHIC DESIGNER: Jennifer Nelson jennifer@travelingblender.com ADVERTISING SALES:
Sandy Weatherford sandy@travelingblender.com SAN ANTONIO: Gerry Lair gerrylair@yahoo.com
For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2025 SmithPrint, Inc. PRINTED IN THE USA



John Shepherd, MD, President
Lyssa Ochoa, MD, Vice President
Jennifer R. Rushton, MD, President-Elect
Lubna Naeem, MD, Treasurer
Lauren Tarbox, MD, Secretary
Ezequiel “Zeke” Silva, III, MD, Immediate Past President
Woodson “Scott” Jones, Member
John Lim, MD, Member
Sumeru “Sam” G. Mehta, MD, Member
M. “Hamed” Reza Mizani, MD, Member
Priti Mody-Bailey, MD, Member
Dan Powell, MD, Member
Saqib Z. Syed, MD, Member
Nancy Vacca, MD, Member
Col Joseph J. Hudak, MD, MMAS, Military Representative
Jayesh Shah, MD, TMA Board of Trustees Representative
John Pham, DO, UIW Medical School Representative
Robert Leverence, MD, UT Health Medical School Representative
Cynthia Cantu, DO, UT Health Medical School Representative
Lori Kels, MD, UIW Medical School Representative
Ronald Rodriguez, MD, UT Health Medical School Representative
Alice Gong, MD, Board of Ethics Representative
Melody Newsom, BCMS CEO/Executive Director
George F. “Rick” Evans, Jr., General Counsel
Melody Newsom, CEO/Executive Director
Brissa Vela, Chief Membership & Development Officer
Yvonne Nino, Controller
Betty Fernandez, BCVI Director of Operations
Phil Hornbeak, Auto Program Director
Al Ortiz, Chief Information Officer
Jacob Hernandez, Advocacy and Public Health Specialist
Jennifer C. Seger MD, Chair
Timothy C. Hlavinka, MD, Member
John Robert Holcomb, MD, Member
Soma S. S. Jyothula, MD, Member
George-Thomas Martin Pugh, MD, Member
Adam Ratner, MD, Member
Rajam Ramamurthy, MD, Member
Patrick Reeves, MD, Member
John Joseph Seidenfeld, MD, Member
Amith Skandhan, MD, Member
Francis Vu Tran, MD, Member
Subhashini Valavalkar, MD, Member
Louis Doucette, Consultant
Brissa Vela, Staff Liaison
Gabriella Bradberry, Staff Liaison
Trisha Doucette, Editor
Ayomide Akinsooto, Student
Elizabeth Allen, Volunteer
Rita Espinoza, DrPH, Volunteer
Ramaswamy Sharma, MS, PhD, Volunteer
45.2% 28%
of physicians surveyed report feeling the effects of burnout daily1
2 out of 3 physicians who are experiencing depression say it affects their work2 of residents surveyed report experiencing a major depressive episode during training3
• Workload
• Work inefficiency
• Lack of autonomy and meaning in work
• Work-home conflict
Medical students have rates of depression 15-30% higher than the general population4
300 to 400 physicians die by suicide each year4
Talk
• Killing themselves
• Having no reason to live
• Being a burden to others
• Feeling hopeless
• Feeling trapped
• Unbearable pain
Behavior
• Increased use of alcohol or drugs
• Withdrawing from activities
• Isolating from family and friends
• Sleeping too much or too little
The suicide rate among male physicians is 1.41x higher than the general male population4
The suicide rate among female physicians is 2.27x higher than the general female population4
1. “Measuring and addressing physician burnout,” May 15, 2025, https://www.ama-assn.org/practicemanagement/physician-health/measuring-and-addressing-physician-burnout.
2. Leslie Kane, MA, “Medscape National Physician Burnout, Depression & Suicide Report 2019,” Medscape, January 16, 2019.
3. Mata, DA, et al. (2015). Prevalence of Depression and Depressive Symptoms among Resident Physicians. JAMA, 314(22), 2373.
4. “10 Facts About Physician Suicide and Mental Health,” American Foundation for Suicide Prevention.
Mood
• Depression
• Anxiety
• Loss or interest
• Irritability
• Humiliation/shame
• Anger/agitation
Prioritizing mental health enables physicians to provide better patient care and maintain resilience by combining self-care with effective mental health treatment. Learn more at afsp.org/physicians
If you or someone you know needs support now, call or text 988 or chat 988lifeline.org
By John Shepherd, MD, President, Bexar County Medical Society
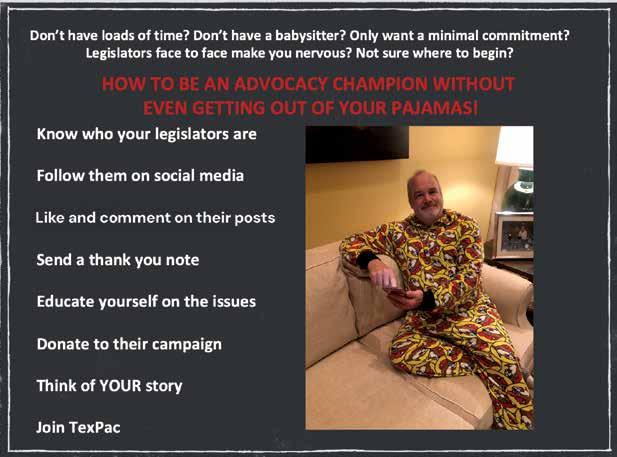
For many Texas physicians, TEXPAC can seem like a political mystery — or something best left to others. Maybe you’ve heard it’s too partisan, too expensive or too time-consuming. Maybe you think you’re already covered by your specialty society. I get it — I’ve heard all of these concerns firsthand. In fact, I didn’t used to believe in the power of TEXPAC either. I thought it didn’t represent my needs or reflect my values as a physician. Now that I know more, I see things differently.
As the Chair of TEXPAC and now longtime supporter, I want to set the record straight. These myths are not only keeping us from being heard — they’re putting our profession at risk. So, let’s talk about the facts surrounding a few of the biggest misconceptions about TEXPAC, and talk about why your voice really does matter.
Reality: TEXPAC is strictly nonpartisan. We don’t follow party lines — we follow medicine. Candidates from both sides of the aisle earn support when they demonstrate a commitment to physician-led care, patient safety and sound health policy. The TEXPAC Committee engages in long, thoughtful conversations when evaluating endorsements, considering not only voting records but also input from physicians across the state. We look at relationships, accessibility, past support for medical issues and the willingness of a candidate to listen and work with our community. These are nuanced decisions, made carefully by our colleagues who understand what’s at stake. Your voice helps shape these decisions and ensures that support goes to those who truly champion medicine — not just a party.
Reality: TEXPAC is physician-led and physician-accountable. Decisions about which candidates to support are made by doctors across Texas based on thorough interviews and voting records. It’s not a black box. As a member, you can see exactly how decisions are made, and even get involved if you want a voice in the process. Locally, BCMS has a Legislative Committee that works on advocacy issues and builds relationships with our county legislators. At the state level, the TMA TEXPAC Committee is composed of physicians and appointed Alliance members from around Texas who guide endorsements and strategy on behalf of all physicians.

Reality: TEXPAC has multiple membership levels, and any amount helps. Basic physician membership is just $99, and Alliance members can join for $59. For those who want to deepen their engagement, higher tiers like the Capital Club and the Patron Club include couples memberships and offer additional opportunities to interact directly with legislators. This isn’t about writing a big check — it’s about strength in numbers. The more physicians who join, the stronger our message. You don’t have to give at the highest level to make a difference — just joining sends a signal that physicians are united and paying attention.
Reality: Specialty societies are important — but they don’t replace TEXPAC. The Texas Medical Association (TMA) is the only organization that represents all Texas physicians across all specialties. TEXPAC is the advocacy arm that ensures we have a unified voice at the Capitol. When a legislative issue arises — whether it’s related to insurance, scope of practice, tort reform or telemedicine — it rarely affects just one specialty in isolation. For example, scope expansion battles may start in one field but often set precedent for others. When we stand together through TEXPAC, we amplify our influence and protect the profession as a whole. Relying solely on your specialty society without participating in TEXPAC is like covering only one corner of the playing field — you miss the broader defense we all need.
Reality: You can be a “checkbook member” and still make an impact. You don’t need to attend meetings or events — though we’d love to have you. Supporting TEXPAC financially helps us elect medicine-friendly candidates. The fight for better policy begins with a legislator who has open ears and an open mind to the needs of medicine. Beyond financial support, there are simple, low time-commitment ways to help — like sending a quick email, thanking your representative, or attending a one-time event such as a fundraiser. Every action, no matter how small, helps build meaningful relationships and strengthens the voice of medicine.
Myth #6: “TEXPAC Doesn’t Make a Real Difference”
Reality: TEXPAC and TMA have helped pass critical reforms and stop dangerous legislation that threatened our ability to care for patients. From preserving scope of practice protections to shaping telemedicine policy and reimbursement, TEXPAC is in the room when it matters. These victories aren’t accidental — they’re the result of sustained advocacy and trusted relationships with lawmakers built over time. When legislators hear directly from physicians, they better understand how their decisions impact real-world care. Whether it’s defeating harmful scope expansion bills or advancing legislation that supports physician wellness, every success is rooted in organized, proactive engagement. Without our collective voice, others — many with no medical background — will define the future of healthcare. TEXPAC ensures that the people shaping that future are informed, responsive and willing to listen to medicine.
We are at a crossroads. Legislative and regulatory threats to physician autonomy are growing. The only way to protect our profession — and our patients — is to get engaged and stay engaged.
Joining TEXPAC doesn’t mean you have to get political. It means you care about your ability to practice medicine, and you believe physicians — not outside interests — should be leading the conversation on healthcare in Texas. It means being part of something larger than yourself — an organized, respected voice that can open doors, shape legislation, and protect the values we all share. Our collective strength ensures we’re not just reacting to policy, but helping to write it. Whether you give, speak or simply stay informed, your involvement matters.
The future of medicine in Texas depends on what we do now — together.
By Brianna Menard, Director of TEXPAC and Political Education
When I joined TEXPAC last year, I brought a decade of experience in the Texas Legislature and a deep respect for the Texas Medical Association’s advocacy. But stepping into this role made one thing clear: the urgency of our political work cannot be overstated.
This past legislative session, the attacks on medicine were real, coordinated, and dangerously close to succeeding. Long-respected lawmakers used their political capital to advance harmful legislation, and we were forced to fight harder than ever with fewer resources than we needed.
That’s where TEXPAC comes in. As the bipartisan political arm of TMA, TEXPAC is the only vehicle we have to organize physicians and amplify their voices at the ballot box. Yet today, only 5% of eligible members are part of the PAC.
In the 2024 election cycle, we raised $1.6 million to support pro-medicine candidates. That sounds strong, until you see what we’re up against: $2.3 million raised by trial lawyers; $9 million raised by realtors; $24 million from tort reformers. Millions more from national nursing groups and big insurance interests. The truth is, we’re fighting forces with deep pockets and powerful friends. The competition is outspending us, and outorganizing us.
The good news? We have the numbers. If just 10% of eligible physicians joined today, we could close the funding gap overnight. If every current member upgraded their giving by just one level, we’d raise hundreds of thousands more to invest in candidates who have our backs. We already have the numbers. We just need the will.
To every physician who supports TEXPAC in any form — thank you. Your engagement strengthens the entire Family of Medicine. But this year, I’m asking you to do a little more. Recruit a colleague. Step up. Help us build the political muscle to protect medicine in Texas.
TEXPAC is how we organize. How we fight back. And how we win.
John Shepherd, MD, 2025 President of the Bexar County Medical Society and TEXPAC Chair, has been an active advocate for the Family of Medicine at the Texas State Capitol and has held several “Party of Medicine” events, introducing physicians on how to get involved with legislation that affects medical issues. He has been Chief of Surgery at Christus Santa Rosa Children’s Hospital and a past member of the Board of Directors of Tejas Anesthesia. Dr. Shepherd is currently a Pediatric Anesthesiologist with University Medical Associates, and serves on the BCMS Legislative Committee and the Bexar Delegation to TMA.

Brianna Menard is the Director of TEXPAC and Political Education at the Texas Medical Association. With nearly a decade of experience in the Texas Legislature, she most recently served as Executive Director of the Early Childhood Caucus of the Texas House of Representatives, leading a bipartisan coalition to make Texas the best place to raise a child.
During her legislative tenure, Brianna spearheaded key legislation on insulin copay caps, early learning funding, expanding access to highquality childcare, and strengthening the Texas workforce through apprenticeships. In the legislative off-seasons, she supported pragmatic candidates through door knocking and fundraising.


A first-time observer’s experience of the Texas legislative process.
By Sue Bernstein
On Tuesday, April 1, the Texas Medical Association (TMA) held its third First Tuesdays during the 89 th Texas Legislative Session. Bexar County Medical Society Alliance (BCMSA) member Sue Bernstein and her daughter Cassidy, a pre-med student at UT Austin, drove to the Austin TMA headquarters and met with other BCMSA members, medical students and physicians from across the state of Texas. Following briefings, Sue and Cassidy joined a sea of white coats walking side by side to the Texas Capitol to advocate together for our physicians and their patients.
This was a new experience for Cassidy and me! As part of the Bexar County and Texas medical communities, we were invited to join in a Texas Medical Association First Tuesdays at the Capitol event where doctors and other medical community members are updated on key legislative agenda items. We visited the Texas Capitol legislators to tell our stories from the front lines and represent patients in fighting for better care and a better healthcare system.



Lately, I’ve felt more compelled than ever to stand up and help. Given current laws and systems, my family members and I have experienced issues both as patients and as leaders in our medical practice. As a pre-med student, Cassidy was motivated to contribute as well.
As we learned from this experience, we all have a voice and it is empowering to do something proactive. More than 300 doctors took time off to participate and advocate for the family of medicine.
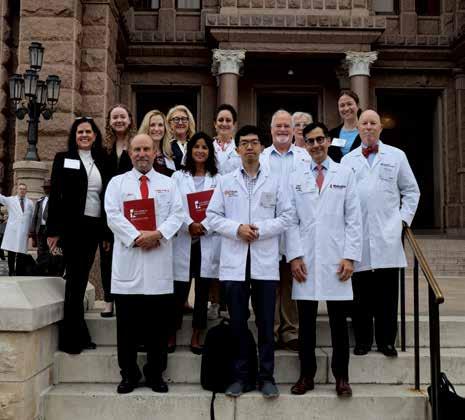
Here’s a photo of Cassidy and me along with other members of the Bexar County Medical Society delegation to the First Tuesdays at the Capitol on April 1, 2025.

Sue Bernstein, MS, served as BCMSA Co-chair and speaker for the recent Bexar County Medical Society Recharge & Reconnect Retreat. She is a Healthy Lifestyle Transformation Coach and Director of Business Development for her husband Eric’s practice, San Antonio Family Physicians.
By Jacob Hernandez

Each biennial session of the Texas Legislature brings victories, struggles and compromises for organized medicine, but the 89th Legislature, which met in Austin this spring, was perhaps the most hectic session ever for the advocacy team at the Texas Medical Association (TMA). Of the 8,719 bills filed for the 89th Regular Session, TMA tracked 2,795 (32%) of those bills, judging the legislation to be related in some fashion to the practice of medicine in Texas.
These included 34 discrete scope expansion bills that sought to threaten the team-based care framework that protects our patients. Not to be outdone, those acting in the interests of the insurance industry introduced legislation that would undermine state-mandated protections for patients and physicians, while opponents of our world-class medical liability landscape sought to erode the non-economic damages cap that has made Texas such a great place to practice medicine for over two decades.
But TMA’s tireless Division of Public Affairs, led by Vice President Clayton Stewart, and physicians and their allies across Texas rallied to not only defend the practice of medicine in our state, but to advance it as well. All major scope-of-practice bills were defeated, as were attempts to weaken tort reform, and not only were major pieces of pro-health plan legislation defeated, but Texas’ “gold-card” prior authorization law was strengthened, and a long-awaited solution to the question of physician non-compete reform was achieved. (For more on the non-competes, see pages 18-21.)
Vital to these outcomes was the aid of Bexar County physicians, medical students and allies, especially heavy hitters such as Dr. Ezequiel "Zeke" Silva III, TMA Council on Legislation Chair and Bexar County Medical Society (BCMS) Immediate Past President; Dr. Jayesh “Jay” Shah, TMA President; Dr. John Shepherd, BCMS President and TEXPAC Board Chair; and Mrs. Jenny Shepherd, TMA Alliance Immediate Past President. These hard-working advocates
were often at Austin, working with the Division of Public Affairs to advance the cause of organized medicine — particularly Dr. Silva, who testified multiple times at House and Senate hearings and, some weeks, was more often to be found in Austin than here in San Antonio. But they were joined in their efforts by the dozens who attended the First Tuesdays at the Capitol events in February, March, April and May — who came on short notice to testify against harmful legislation before the House Public Health Committee and Senate State Affairs Committee, and who contacted their legislators via TMA’s Grassroots Action Alerts. Here is some of what we achieved this spring:
The 89th Session started off with a bang as SB 911 was introduced in the Senate, with similar legislation filed in the House. This legislation sought to give APRNs full independent practice authority, and its advocates immediately began a full-court press to convince legislators that endangering team-based care was the only solution to the very real problem of rural healthcare access. From the beginning, TMA lobbyists, and physicians from across Bexar County and Texas, worked to provide the facts about what expanding APRN scope does and doesn’t do, and not without effect — SB 911 and accompanying House legislation died in Committee. But that wasn’t the end of the battle. HB 3794, filed at the beginning of March, had much the same aim, and this bill received a hearing in the House Public Health Committee on Monday, April 14.
We had less than a week’s notice to enlist as many physicians and medical students as possible to attend the hearing and testify on behalf of patient safety. Despite this last-minute addition of HB 3794 to the agenda, over 30 TMA members showed up at the Capitol (with many staying into the night) to make their voices, and the voice of organized medicine, heard. Our advocates made clear that promises made by bill supporters of increased access to care weren’t borne out in data on where APRNs end up practicing in states that expand scope, while
Dr. Silva presented study data showing that independently practicing nurse practitioners “had higher rates of preventable hospitalizations, increased the overall length of hospital stays, and raised the cost of care in the emergency department” when compared to physicians. Testifying physicians provided anecdotal and statistical data showing the importance of physician-led team care, and offered other solutions to the rural healthcare problem. Many members of the Committee were visibly impressed by our testimony, which was validated when HB 3794 failed to advance out of Committee.
A big victory, but again, not the end of the fight. With barely a month left in session, SB 3055 was snuck into the Senate and onto the docket for the Senate State Affairs Committee, with a hearing scheduled for Thursday, May 1 — this time, with barely a week’s notice. SB 3055 was narrower in scope than the prior bills, but no less dangerous — it would’ve applied to rural counties (defined as those with fewer than 68,750 residents), and given independent practice authority to those who have practiced for at least 10 years and practiced with a physician for four years. But the underlying issues remained the same. As Senator Donna Campbell (R–New Braunfels), herself a physician and former nurse who is one of medicine’s strongest advocates in the Legislature, said, APRNs have “a fraction of the training medical doctors do.” The two professions’ respective training produces a fundamentally different clinical approach that simply can’t be equated. Like in April, the hearing stretched past dusk, but physicians such as Dr. Lubna Naeem, BCMS Legislative & Socioeconomics Committee Vice Chair, stayed until they were called up to testify. This commitment was rewarded when SB 3055, like its predecessors, died in Committee.
The final major scope fight took us all the way to the Governor’s desk, and dragged all the way to the end of the Governor’s veto period. SB 268 would have limited the Texas Medical Board’s ability to issue cease-and-desist orders for the unauthorized practice of medicine; despite strong efforts by TMA and physician legislators, the back-andforth between acceptable and unacceptable forms of the legislation ended with a form unfriendly to medicine’s interests being sent to the Governor’s desk. Fortunately, after considerable grassroots outcry, it was ultimately vetoed. (For more on this, see Dr. Amith Skandhan’s article on the fight over SB 268 and the role grassroots advocacy played in its defeat, page 16.)
These hearings were some of the most dramatic moments of grassroots advocacy by TMA and BCMS members throughout the session, but they were far from the only ones. Members testified against legislation such as HB 139, a bill authorizing the creation of bare-bones, insurer-friendly “Employer Choice Plans” that do not include the necessary elements of a responsible or realistic health plan; HB 5402, a bill to require the Legislative Budget Board to provide impact statements on behalf of the health insurance industry; SB 407, which sought to require healthcare facilities’ vaccine-preventable disease policies to accept any and all immunization exemption requests made on the grounds of reasons of conscience; and HB 3219, which directed the Texas Department of State Health Services (DSHS) to authorize pharmacists to dispense ivermectin without a prescription, thus removing clinical involvement and putting patients in danger. All of these pieces of concerning legislation did not become law.
TMA member testimony was involved in bringing about additive accomplishments as well. Testimony was crucial to the passage of HB 3812, the “gold card” law cleanup bill that, in the words
of Dr. Silva, “streamlines eligibility, improves transparency, and enhances state oversight” by extending the evaluation period from six months to a year, codifies a minimum threshold of five services to qualify, and allows physicians to aggregate approvals across affiliated insurance plans. SB 922 will ensure that patients must receive serious and sensitive test results and diagnoses directly from a physician, instead of via an electronic patient portal, a method that often provides more anxiety than context. And legislation such as SB 2024 and SB 1313 places common-sense limits on the manner in which e-cigarette products can be marketed, with particular attention to methods that are too often used to target children.
No account of the accomplishments of the 89th Legislature would be complete without detailing the passage of two very important bills: SB 31, or the “Life of the Mother Act,” and HB 3749, or “Jenifer’s Law.” SB 31, in support of which many TMA physicians testified in both chambers, clarifies the language of Texas’ abortion ban to ensure that physicians do not face unnecessary obstacles in providing a pregnancy termination to a patient in a state of medical emergency that, in the reasonable medical judgment of the physician, necessitates doing so. The bill had buy-in across party and ideological lines, with hospitals, religious groups and anti-abortion groups all working together to “reach a sort of pathway of unifying language,” per Dr. Silva. The final product provides breathing room for physicians to, in the words of San Antonio OB-GYN Nichole Van de Putte, MD, “promptly treat obstetrical emergencies that pose a threat to maternal life.” SB 31 was effective immediately upon being signed by Governor Abbott in June, and is currently the law of the land.
Jenifer’s Law is another piece of legislation inspired by the wish to avoid tragic and unnecessary loss of life. It is named for central Texas radio personality Jenifer Cleveland, who died in July 2023 after receiving an IV infusion at a med spa in Wortham. The infusion contained a toxic mixture of chemicals that the unqualified employee administrating it did not have the training to understand were dangerous, and the physician who was ostensibly providing oversight was not fulfilling their role. Cleveland’s legislator, Rep. Angelia Orr (R–Hillsboro), introduced legislation to intensify and codify a robust system of oversight for elective intravenous therapy conducted outside of a traditional healthcare setting, requiring that only physician assistants and nurse practitioners can be delegated to administer these procedures. Dr. Silva testified on behalf of the legislation at a Senate Health and Human Services Committee hearing, joined by the husband of the late Ms. Cleveland, whose emotional testimony Dr. Silva described as one of the most impactful moments of the session.
Ultimately, the passage of Jenifer’s Law is an excellent example of the kind of work that staff and member advocates work so hard for during our legislative sessions: the fight to not just maintain but increase standards of care and patient safety across our state, so that every Texan can have access to the opportunity to lead a healthy life.

Jacob Hernandez is the Advocacy and Public Health Specialist for the Bexar County Medical Society.


By Amith Skandhan, MD, SFHM, FACP, and Jacob Hernandez
In the final days of the 2025 legislative session, an extraordinary thing happened in Texas: physicians of every background — students, residents, practicing clinicians and organized medicine leaders — mobilized with fierce urgency to stop a bill that threatened the safety of patients and the authority of the medical profession. Senate Bill 268 (SB 268) was poised to become law. It had already passed both legislative chambers and sat on Governor Greg Abbott’s desk.
But medicine fought back — and won.
This is the story of how that happened, what was at stake and why physician advocacy is not just important, but essential.
SB 268 would have gutted the Texas Medical Board’s (TMB) ability to issue cease-and-desist orders against individuals practicing medicine without a license. Instead, the bill proposed that only the individual’s “home” licensing board could investigate and take disciplinary action — even when someone was clearly performing acts that fall under the legal definition of “practicing medicine.”
In practical terms, that meant if a nurse began diagnosing or prescribing independently, only the Texas Board of Nursing could intervene. But it didn’t stop there. The same would apply to a chiropractor ordering imaging and making medical diagnoses outside their scope. Or a dentist performing cosmetic injections for non-dental indications. Or even a podiatrist managing conditions far beyond the lower extremity. Each would be shielded from immediate TMB oversight — even if their actions placed patients at direct risk.
The message was clear: as long as you had any license, you could potentially practice medicine — until your “home board” decided to act.
This bill blurred the line between distinct health professions and threatened to redefine who could provide care under the guise of regulation. Even more concerning, most licensing boards are not structured — or qualified — to evaluate or discipline based on the standards of medical practice.
Had SB 268 become law, the consequences could have been devastating. The TMB would have been legally handcuffed — unable to act swiftly against individuals providing unsafe, unlicensed care — simply because they happened to hold a license from another board.
This wasn’t just a turf war. This was about protecting patients from real harm.
As Dr. Jayesh “Jay” Shah, President of the Texas Medical Association (TMA) and a respected San Antonio physician, stated, “Only the Texas Medical Board is equipped to oversee the practice of medicine in our state. Patient safety depends on it.”

In every session, a version of this bill resurfaces — and in every session, medicine pushes back. But in 2025, SB 268 gained unexpected momentum. The Timeline:
• March, 2025 Physicians testified passionately against SB 268 in Senate hearings.
• April, 2025 Despite strong opposition, SB 268 passed the Senate.
• May 12, 2025: A House hearing featured further testimony, including Dr. Ezequiel "Zeke" Silva III of Bexar County Medical Society.
• May 15 & 22, 2025: The bill stalled in committee — twice. It looked like it might die.
• May 27, 2025: A last-minute push placed it on the House calendar. With an amendment negotiated by Rep. Tom Oliverson, MD, which preserved the TMB’s disciplinary power, the bill passed the House. At that point, TMA could cautiously support the modified bill.
• May 30 (Friday): A late-night conference committee meeting removed the critical amendment — effectively resurrecting the original threat.
• May 31–June 2 (Weekend): With barely any time left, the unmodified version passed both chambers. Medicine was stunned — and rallied.
The timing couldn’t have been worse — or more revealing of the strength of our medical community. Dr. Silva, Chair of the TMA Council on Legislation and Immediate Past President of BCMS, helped set the table for that weekend’s sprint. He had testified in opposition to SB 268 at the May 12 House Public Health hearing, and his early work with TMA and BCMS leaders was critical in stalling the bill in committee — twice — before it was ultimately forced to the floor.

It was Saturday, May 31. Many organizations were already wrapping up their session recaps. But when word spread that the protective amendment had been removed from SB 268 and the bill was moving forward in its most dangerous form, TMA and the Bexar County Medical Society (BCMS) sprang back into action.
What followed was nothing short of extraordinary:
Over 2,000 TMA members took action over a weekend, calling, emailing, and texting their legislators and the Governor’s Office. This wasn’t a pre-planned push. It was an emergency grassroots surge — fueled by urgency, professionalism and passion.

Physicians took time between patient rounds and family commitments. Others skipped weekend plans to get involved. “We knew what was at stake, and we couldn't afford to stay silent,” said Dr. Silva. “It took everyone — from students to senior physicians — to hold the line.” Medical students, like BCMS Legislative & Socioeconomics Committee member Rishi Goswamy, OMS-III, University of the Incarnate Word School of Osteopathic Medicine, personally called their representatives — repeatedly — until they got through. “We knew we had hours, not days. I kept calling until I got my representative on the line,” Rishi said. “He voted no. And I knew that call made a difference.”
This wasn’t just a bureaucratic campaign — it was a weekend-long sprint powered by grassroots perseverance. TMA’s inside-outside strategy was in full force: leaders working the Capitol channels, and everyday physicians flooding inboxes and phone lines. The sheer determination displayed by Texas physicians during those final days of session sent a clear message:
We are watching. We care. And we will not allow dangerous legislation to pass quietly.
On June 22, Governor Abbott issued his veto of SB 268. In his proclamation, he echoed the very concerns voiced by TMA and BCMS members:
“The Medical Board should not be prohibited from issuing a cease-and-desist order for unlicensed medical practice simply because the specific practice at issue is also regulated by another board.”
That statement validated the efforts of everyone involved. The system had worked — but only because physicians made it work.
Imagine a Texas where unlicensed individuals can legally provide medical services without the Medical Board's ability to intervene. Imagine the confusion among patients, the loss of accountability, the erosion of trust in our profession.
That was the future we nearly faced.
SB 268 is a case study in what happens when medicine is not at the table — or worse, when it’s ignored. And it is also a shining example of what organized medicine can achieve when we unite.
This victory was possible because of long-standing advocacy infrastructure. “What turned the tide wasn’t just the surge of weekend calls alone — it was the groundwork laid over months, and sometimes years, of relationship-building with our elected officials. When legislators picked up the phone, they didn’t just hear from random physicians; they heard from someone they knew and trusted, and that credibility counted when it mattered most,” noted John Shepherd, MD, Chair of TEXPAC and President of the Bexar County Medical Society. BCMS, through its Legislative and Socioeconomics Committee, monitors bills like SB 268 year-round. TMA, with its expert Governmental Affairs team and network of physician leaders, has the influence and agility to act quickly. But neither organization can do it alone. We need members. We need voices. We need every physician to engage.

If you’ve ever thought your voice doesn’t matter, let this be your answer: it does. It saved Texas medicine.
If you're not yet a member of BCMS or TMA, join today. These organizations are fighting for your license, your patients, your practice — and they need your help. Because when the next bill threatens the safety of our patients, you’ll want to know someone is fighting for you — and that you’re part of that fight.

The SB 268 story isn’t just about a bill. It’s about our collective power. It’s about what happens when physicians lead, organize, and speak with one voice. From student to seasoned specialist, from testifying in Austin to making weekend phone calls — this was a team effort. We didn’t just defeat a bill. We defended our profession. We protected our patients. We reminded Texas who medicine belongs to. Let’s keep that energy. We’ll need it.
https://www.bcms.org/LegCom.html


Amith Skandhan, MD, SFHM, FACP, is an associate professor in the Division of Hospital Medicine at UT Health San Antonio. He serves on multiple committees within the Bexar County Medical Society, including Legislative & Socioeconomics, Emergency Preparedness and Publications. He is a consultant to the Texas Medical Association’s Health IT and AI Committee. With a background in healthcare operations and quality improvement, Dr. Skandhan advocates for digital innovation and physician leadership to advance patient-centered care and professional advocacy across Texas.

Jacob Hernandez is the Advocacy and Public Health Specialist for the Bexar County Medical Society.












































How a physician-led proposal at the Bexar County Medical Society, adopted by the Texas Medical Association, culminated in Senate Bill 1318 and statewide non-compete reform.

By Lubna Naeem, MD
In the ever-evolving landscape of healthcare, the voices of physicians must do more than echo within hospital walls — they must rise into the chambers where policy is shaped. This past year, I had the privilege of witnessing firsthand how a resolution I authored — beginning at the county level — transformed into meaningful statewide reform.
What began as a local resolution submitted through the Bexar County Medical Society (BCMS) has now become SB 1318, which has become law, effective September 1, 2025 — a landmark piece of legislation that redefines how non-compete agreements affect our healthcare workforce.
The resolution was born out of conversations with fellow physicians who had experienced firsthand the harm caused by overly restrictive non-compete clauses. These provisions, originally meant to protect business interests, were increasingly disrupting continuity of care and limiting physician autonomy — particularly in areas already suffering from workforce shortages.
As a practicing internist and physician advocate, I felt a responsibility to act. I authored a resolution aimed at restoring fairness to these agreements — protecting the physician’s right to serve patients while ensuring that contracts remained reasonable and just.
In early 2024, I formally submitted the resolution to the BCMS Delegation to the Texas Medical Association (TMA). It was reviewed and unanimously approved by the TMA Reference Committee during the TMA Annual Meeting, reflecting widespread agreement that this was an issue of statewide importance. That approval placed the resolution into TMA’s official policy platform, giving it the momentum needed to draw the attention of lawmakers.
With strong leadership from Senator Charles Schwertner, a physician and legislator, the TMA-backed resolution was drafted into legislation as SB 1318. It passed both chambers of the Texas Legislature and was signed into law. It goes into effect on September 1, 2025.
SB 1318 introduces major protections for healthcare professionals by:
• Limiting non-compete clauses to one year
• Restricting the geographic limit to five miles from the primary practice site
• Voiding any non-compete if a provider is terminated without cause
• Capping contract buyouts at the provider’s annual salary





This is a major win — not just for physicians, but for all healthcare providers and, most importantly, for patients. It restores professional dignity, supports continuity of care, and ensures that physicians are not punished for wanting to remain in the communities they serve.
It also demonstrates the tangible impact that physician advocacy can have — when it is persistent, collaborative and grounded in realworld needs.
Although I authored the resolution, I want to emphasize that this success was only possible through collective action. From the early support of BCMS leadership, to the TMA House of Delegates, to Senator Schwertner and his legislative team — it truly took a village to bring this law to life. This reform is a testament to what we can achieve when we speak up, stand together, and support each other in advancing the medical profession.
This journey — from resolution to law — should remind all physicians that we have a role to play in shaping healthcare policy. Change doesn’t always begin in the Capitol. Sometimes, it starts with a conversation at a county medical society meeting and a single resolution written by a concerned colleague. If we want to protect our profession and advocate for better care for our patients, we must stay engaged at every level — county, state and beyond.
Special thanks to the BCMS leadership for their immense support throughout this journey — with heartfelt appreciation for Dr. Lyssa Ochoa, who strongly supported the resolution during the Reference Committee discussion, and Dr. Jayesh “Jay” Shah, TMA President, whose encouragement was instrumental in motivating me to write and submit the resolution in the first place

Lubna Naeem, MD, is a practicing internist in San Antonio with more than 25 years of experience in clinical medicine, advocacy and leadership. Dr. Naeem served on the Board of Directors of the Bexar County Medical Society as Secretary in 2024, and currently as Treasurer, Vice-Chair of the BCMS Legislative & Socioeconomics Committee, and Member Council on Legislation for TMA. She is a dedicated advocate for physician rights, international medical graduates and equitable healthcare access across Texas.


The Bexar County Medical Society is committed to helping our members find personal balance and improve general well-being.

BCMS Physician Wellness Program
Resources and services provided to help BCMS members maintain a healthy and well-balanced lifestyle through confidential counseling, educational resources, local events, webinars and more.


A BCMS provided resource for physician members who seek counseling from Texas-licensed professionals, discretely and confidentially through BetterHelp. Free 30 days counseling.

Free CME Wellness Coaching Webinars & Events
Nora Vasquez, MD, an Internal Medicine Doctor and Advanced Certified Physician Coach, helps physicians and healthcare professionals overcome burnout so that they can lead with joy and confidence while creating a more harmonious work-life balance that is fulfilling!

Utilize our free Find a Doc service when looking for a new physician. Our members can be found by the specified tabs provided to narrow down your preferred physician.
Physician Support Line (888) 409-0141
Psychiatrists are available to help physicians and medical students navigate the balance of a personal and professional life. Free, confidential and anonymous. No appointment necessary. Call for any issue, not just a crisis.

Physician Coach Support

Free Confidential Physician-to-Physician support line. A group of volunteer physicians using their own personal development skills and life coaching certifications to support other physicians!

Physician Health & Rehabilitation Program
Confidential advocacy group of BCMS physicians that identify and facilitate recovery success for physicians with substance use disorder (Alcohol and/or Drugs) and depression, through support and monitoring.
Please scan QR code for more information and available resources for BCMS Members

By Mike Kreager
Employers around the country celebrated last year’s court decision setting aside the FTC’s rule banning nearly all non-competes. But on September 1, new changes curtailing physician non-competes take effect in Texas. On that date, new non-competes must:
1. End within one year.
2. Not exceed five miles.
3. Allow a buyout of not more than one year’s salary and wages.
4. Be clearly and conspicuously stated.
5. Disappear if the physician is fired without good cause.
Reason for the
The legislature enacted these reforms to enhance competition and promote greater patient access to their physicians by curtailing perceived abuses of non-competes by employers who imposed terms lasting more than one year, extended the restricted radius long distances, and asked for exorbitant buyout amounts.
Discussion
The new law does not disturb the long-standing requirement that non-competes must contain only reasonable restraints. But the changes add guardrails that eliminate uncertainty over the duration and geographic reach of a physician non-compete. Previously, employers dictated those terms as a condition of employment. Yet, as discussed below, some ambiguity remains in applying the new law’s wording and new controversies will likely arise.
Non-competes now must have a hard stop of one year, or in the words of the statute, “the one-year anniversary of the date the contract or employment has terminated.” A multi-year non-compete is off limits. The statute’s reference to “contract or employment” captures both employment and independent contractor relationships.
Non-competes most often prohibit competition within a circle measured by a radius from a central location. For example, academic medical centers tend to favor 25- and 30-mile radii.5 In addition, employers with multiple practice sites tie the radius to each practice site, without regard to the physician seeing patients at a site. As a result,
the non-compete encompasses the entire city, forcing the employed physician to relocate to another city at the end of employment even though the radius might only be 10 miles from each site.
Under the new law, the radius cannot exceed five miles from “the location at which the physician primarilypracticed before the contract or employment terminated.” The word “primarily” strongly implies one site as the center point of the radius, excluding other possible sites. Nevertheless, could primarily be interpreted to count more than one site? In other words, does the word primarily mean also a substantial amount of time, not just more than half. For example, surgeons, anesthesiologists, radiologists and pathologists could be working at multiple facilities. One wonders also how to apply the five-mile radius to providers using telemedicine.
Texas is the one state in which the physician must be able to buy out the non-compete. The legislature added the buyout in 1999 so the physician could continue to see his or her patients. But departing physicians only very pay the buyout. The new cap will not spur greater use of the buyout. Future non-competes will undoubtedly adopt one year’s salary as the buyout amount, which is more than a physician can realistically afford to pay. Instead, the five-mile limit will prove far more beneficial to the departing physician.
The new cap tracks the existing rule of thumb for non-compete buyouts — one year’s compensation. Yet the law doesn’t envision the productivity models widely used for physician compensation, such wRVUs or a percentage of collections. These models often defer the payment of the bonus portion until the end of the year. When productivity is the basis of compensation, the determination of the buyout amount may vary year to year.
The new law deleted two clauses from the prior buyout law. First, the prior law required the buyout to be a “reasonable price.” The use of the word price emboldened employers to set an exorbitant price it considered to be reasonable. Disputes abounded over what was a reasonable buyout price. The new law requires only that the buyout be capped at one year’s salary. A physician who objects to the amount in the future may still argue the buyout isn’t reasonable. Just because the statute sets a maximum amount doesn’t mean that the maximum amount is a reasonable amount. It could be argued that the buyout amount should not exceed the value of a five-mile, one-year restriction against competition.
Second, the 1999 statute allowed the physician to ask an arbitrator to independently set the buyout. Arbitration has proven to be impractical due to the expense and delay in arriving at a decision from the arbitrator. Thus, removing arbitration from the non-compete law is inconsequential.
Future non-competes must be clearly and conspicuously written. These are new, separate concepts for non-competes. Non-competes historically are convoluted, intended to forestall the physician finding any loophole for post-employment competition. Clarity, or lack thereof, will become a new challenge to non-competes. Will the non-compete need to be worded like insurance policies, using easily understood, plain-meaning wording? The word “conspicuous” harkens to consumer protection rules, which in other contexts requires the wording to be in bold print and sufficiently large to read. To be conspicuous, the first page of the contract may need a warning that it contains a non-compete. Thus, future contracts must, under the new law, spotlight the non-compete.
Virtually all non-competes restrict the physician from competing after the end of employment regardless of the reason. Thus, the physician would be restricted from competing even if the employer changed its mind and terminated the physician’s employment shortly after starting work. The new law eliminates this possibility and gives a “free pass” to the physician who is fired without cause. On the other hand, the physician who quits is still bound by the non-compete.
The new law uses the phrase “without good cause.” That phrase is defined as being a “reasonable basis for discharge … directly related to the physician’s conduct.” The new law includes as examples of good cause, “the physician’s conduct on the job or otherwise, job performance, and contract or employment record.” The examples are regrettable. Job performance is ripe for an employer’s subjective evaluation. What the phrase “contract or employment record” means is anyone’s guess. The usual reasons to fire a physician for cause are the loss of medical license, loss of hospital staff privileges, loss of controlled substance registration and the like, which are objective reasons meeting the “good cause” standard of the new law.
New non-competes must comply with the changes beginning September 1, 2025. Prior non-competes are not subject to the new law, unless they are renewed after the effective date.
The new law exempts physician activities that are “managing or directing medical services in an administrative capacity for a medical practice or other health care provider.” There has been commentary
suggesting employers consider bifurcated non-competes: one that complies with the new law for medical services and another one without the new law’s conditions for administrative services.
All new physician employment agreements with non-competes must now comply with the new law’s limitations on duration, geographic reach, buyout, conspicuous and free pass reforms. Employers will want to update old employment agreements that renew after the effective date to conform to the new safeguards in the new law. Failure to include these updates could nullify the non-compete altogether. For new hires and renewals of existing hires, ask your lawyer to update your contract to comply with the new law.
The new law added a completely new non-compete section that extends its reforms to non-competes for dentists, nurses and physician assistants.
1. Non-Compete Clause Rule, 90 CFR 910.2 (2024), which was set aside nationwide by Ryan LLC v. FTC (N.D. Tex. 2025). The FTC appealed the decision, but the change in the administration and in the composition of the Commission makes it unlikely the ban will be resurrected. Instead, the Commission has signaled that it intends to enforce anticompetitive non-competes where needed.
2. SB 1318, amending Section 15.50 of the Texas Business & Commerce Code, signed into law on June 20, 2025.
3. Bill Analysis, Senate Research Center, March 24, 2025, “S.B. 1318 would establish guardrails for physician non-competes that protect patient access to care, reduce the legal ambiguity and burdens of litigation, safeguard the integrity and mobility of the healthcare workforce, and promote competition.”
4. The non-compete law requires the restrictions to be reasonably necessary to protect the employer’s business interests in its goodwill and confidential information. Tex. Bus. & Comm. Code §15.50.
5. A 25-mile radius will result in a non-compete restricting over 2,000 square miles (A = nr2).
6. Tex. Bus. & Comm. Code §§ 15.501.

Mike Kreager is the founder of the business law firm Kreager Mitchell PLLC. He has written and spoken extensively on physician non-competes.
By Jacob Hernandez

Much has been written about the legislative and partisan politics surrounding the passage of the recently enacted omnibus budget reconciliation bill — H.R. 1, or the “One Big Beautiful Bill Act.” As a general rule, these political considerations are beyond the scope of this publication and the Bexar County Medical Society (BCMS) — instead, I wish to focus on the likely and possible policy ramifications for healthcare in America of the bill’s provisions, and to begin to sketch out how they could affect your patients, your practices and your profession over the years to come.
First, there are good developments in the bill. Most directly germane to organized medicine, the version of H.R. 1 signed by President Trump does include a one-year increase to Medicare physician payment rates of 2.5% for 2026. This is less substantive than the version originally passed by the House of Representatives, which would have tied rates to 75% of the Medicare Economic Index (MEI), which measures physician practice cost adjusted for inflation. The House bill’s Section 44304 followed the suggestions of the Medicare Payment Advisory Commission (MedPAC) in creating this new adjustment, which, “because the increase becomes part of the baseline rather than a temporary patch,” would have, per the AMA, seen cumulative payment rate growth of 4.3% by 2035. However, the Senate Finance Committee stripped this provision from the bill, leaving physicians vulnerable to a payment cliff in 2027; we hope that steps are taken later in the 119th Congress to address this via standalone Medicare payment reform legislation, and we are glad that physicians will see some relief in 2026.
Perhaps the highest-profile healthcare-related aspect of H.R. 1 is the major transformation of Medicaid funding that will result. Nationwide, federal Medicaid spending will be reduced by about $1 trillion through 2034 (per the Congressional Budget Office). This will largely be achieved through community engagement requirements (more colloquially known as work reporting requirements), limits on states’ ability to fund Medicaid through provider taxes, increased cost-sharing provisions, making eligibility redeterminations more frequent and less
streamlined, shorter retroactive coverage periods, and a lower cap on state-directed payments from HHS. This will have a profound effect on healthcare for not only the roughly 4 million Texans who were enrolled in Medicaid as of October 2024, but on the whole landscape of Texas healthcare, especially in Bexar County. As our own TMA President Jayesh Shah, MD, has said, “States like Texas already face immense fiscal challenges in meeting the needs of Medicaid patients. Deep federal cuts and restrictions on provider-tax flexibility could trigger unintended consequences, straining hospitals, clinics, and — most critically — patients who rely on these services.”
Some of these changes are isolated to states that have expanded Medicaid (for instance, the community engagement requirements, which only apply to the ACA Medicaid expansion group), while others are geared to have a steeper impact on states that have expanded Medicaid, but will still impact states such as Texas that have not expanded Medicaid: for one example, the cap on state-directed payments. SDPs are used to ensure that managed care organizations pay providers such as hospitals and nursing facilities more than the Medicare payment ceiling (of course, as we all know, this does not apply to physicians), and perhaps as much as the average commercial rate. H.R. 1 caps SDP rates at 100% of Medicare rates for expansion states, and 110% for non-expansion states like Texas.
Many of the Medicaid changes are not slated to come into effect until 2027 or 2028, such as eligibility redeterminations (December 31, 2026), mandatory cost-sharing for those with incomes at 100% or more of the federal poverty level (October 1, 2028), limiting retroactive coverage to two months for traditional Medicaid enrollees (January 1, 2027), prohibitions on establishing any new provider taxes or raising current rates (July 4, 2028), community engagement requirements (December 31, 2026, or earlier with a CMS waiver), and the restrictions on state-directed payments (for non-expansion states, January 1, 2028). However, organized medicine has already been sounding the alarm about the ramifications that H.R. 1 may have on
patient care. A June letter from a coalition of state medical associations to which TMA was a signatory states the following:
“ThenewSenateMedicarepaymentcapsforStateDirected Payments at a percent of Medicare penalizes public hospital systems and physician specialists caring for some of the sickest patients across the nation.
The Moratorium on new provider taxes and a freeze on provider tax levels amounts to a long-term funding cut, as the funding will not keep pace with increased health care costs over time brought on by inflation, economic downturns, publichealthcrisesandnaturaldisasters.Italsoinequitablyfreezes rates in states with lower taxes.
TheUniformityRequirementforallprovidertaxesonhospitals, nursing homes, and managed care organizations to be equal in each provider category is essentially an elimination of numerousprovidertaxesacrossthenationbecausestateswould experienceextremedifficultymeetingtherulesandwouldneed more time to try to restructure or unwind existing programs and services.”
Similarly profound changes in federal healthcare spending may result from an action that was not taken by Congress in passing H.R. 1 — the reauthorization of enhanced premium tax credits for ACA marketplace health insurance coverage, which are stated to expire after December 31 of this year. These tax credits (which date in their current form to 2021 and the Covid era) lower the costs of premiums for many of the four million Texans who have insurance through a mar-
ketplace plan, and unless Congress passes a standalone reauthorization of the current levels by the end of the year, the Urban Institute estimates that around one million people could become uninsured, out of the nearly two million fewer people who would be covered by a subsidized marketplace plan. Unlike the changes included in H.R. 1, this is not yet a given, and I encourage you to contact your member of Congress throughout this year and support the reauthorization of the enhanced premium tax credits. Especially in a non-expansion state like Texas, these provisions are important in ensuring that patients have access to the quality care provided by Texas’ world-class physicians.
Finally, a lesser-known provision in H.R. 1 will affect the future of the medical profession in Texas and across the nation: changes to the awarding and administration of federal student loans, including loans taken out by medical students. Beginning in July 2026, there will be a $150,000 cap on professional program loans; this figure is well below the average amount of medical school debt that the average medical student takes out in order to attend a MD or DO program. This change could lead to a serious crisis in the student-to-physician pipeline, at a time when Texas and much of the country faces existing physician shortages. Further, medical students will no longer be able to receive Federal Direct Stafford loans and Federal Direct PLUS loans. The stated pretext of these changes is to spur colleges and universities to lower costs, but it is hard to see how the necessary adjustments can be made within one year to avoid a major disruption in the careers of today’s future physicians.

Jacob Hernandez is the Advocacy and Public Health Specialist for the Bexar County Medical Society.
The fight for medicine-friendly policy continues — one relationship at a time.
By Jenny Shepherd
John and I eloped before I had a chance to meet his mother — which, frankly, was a wise call on my husband’s part. In my mind, my new mother-in-law would be a Barbara Bush type — gracious, warm, ready to build a delightful relationship over shared interests and holiday casseroles. But reality had other plans. What I got instead was a one-way street paved with expectations: fix my computer, take me to dinner, do this, explain that. Relationship? Not so much.
It reminds me of how, if we’re not mindful, we sometimes approach our legislators. We show up on First Tuesdays after months away, armed with a list of needs, expecting a receptive smile and immediate action — without investing in the relationship that earns real influence. Just like with family, mutual respect takes time, effort and a little give and take.
So, what does relationship-building actually look like? It doesn’t require grand gestures or a packed calendar — just thoughtful effort showing consistency over complexity. Advocacy between sessions isn’t about talking points and pushing policy; it’s about building relationshipsandearningtrust. The months after session are when real connections take root, and even small actions can carry lasting effects. These moments are what pave the way for meaningful partnerships down the line. So, how do you put that into practice especially when time is short and your calendar is full? Here are a few straightforward, high-impact ways to build and sustain connections.
Don’t wait until the next session to reach out. Legislators are far more receptive when they hear from physicians between deadlines and votes. Send a quick email to check in, share a relevant article, or comment on a health policy issue they’ve been involved in. These small touch points keep you on their radar — and show that you’re invested beyond the urgent ask.
It sounds simple, but gratitude is powerful — and too often overlooked. A brief thank you note or email to your legislator after session can set you apart. Whether they supported a key bill or just took the time to meet with physicians, acknowledging their effort shows respect and opens the door to future dialogue. One quick scroll through social media makes it clear: criticism is loud and praise is rare. Be the exception. Praise in public, criticize in private. And remember that every legislator has something worth appreciating, even if it’s something outside of medicine. That thoughtful gesture of thanks, especially when no one is asking for anything, can go a long way in building goodwill.

A simple way to stay connected is by following your legislators online. It gives you a window into what matters to them, what’s happening in their district and how they’re communicating with constituents. It’s also a chance to show your support — like, share, or comment when they’re doing something positive for your community or for medicine.
And when appropriate, be a champion for them. Publicly recognizing their efforts or offering a thoughtful defense when they face unfair criticism helps reinforce the relationship. Engagement doesn’t always have to be in person — sometimes a thoughtful, well-timed tweet speaks volumes.
Campaign season doesn’t wait until November; for many legislators it begins as soon as they return to their districts and turn their attention to re-election. Supporting a campaign isn’t just about politics — it’s a signal that you value their leadership and want to keep medicine-friendly voices at the table.
That support doesn’t have to come in the form of a major time commitment or a large check (although that’s nice, too). Making a modest donation, attending a fundraiser, hosting a meet-and-greet, or even offering to place a sign in your yard sends a clear message: I’m invested — and medicine is invested.
You don’t have to be a political insider to show up. Fundraisers, town halls and local gatherings are opportunities to connect in a relaxed setting. Our Bexar County legislators are busy in the community with a host of activities, often partnering with other local organizations. Representative Josey Garcia launched “Team Josey,” a grassroots volunteer force of over 600 community members during the recent floods. Senator Jose Menendez hosted an elder abuse forum, and Representative Liz Campos plans an annual Independence Day event for the community and hosts back-to-school health and resource fairs. And that’s just a small sample — the list goes on.
When legislators see physicians outside the Capitol — at pancake breakfasts, blood drives or park cleanups — they remember. Presence matters.
Advocacy is a team sport. One physician or spouse showing up matters — but many from the family of medicine showing up consistently makes an impact that can’t be ignored. It’s important that multiple voices from the medical community build relationships with legislators. When a lawmaker hears from a variety of us in the
medical community — across specialties, generations, practice settings — they gain a fuller picture of medicine’s needs. It also ensures we’re not relying on the same few individuals to carry the entire weight of advocacy. We’re stronger when the effort is shared and we’re most effective when we make that effort before we need something.
While things under the dome are about to be a little quieter, our voices shouldn’t be. Relationships don’t grow overnight — they grow through presence, trust and a little persistence. Whether it’s a thank you note, a handshake at a town hall, or simply being the familiar face who shows up again and again, your engagement matters. So, pick one thing — just one — and do it this month. Send an email. Follow a legislator. Show up at a community event. Small steps, taken often, build the kind of influence that lasts longer than any legislative session.

Jenny Shepherd is the Immediate Past President of the TMA Alliance, Chair of First Tuesdays at the Capitol and acting BCMSA President with a legacy of supporting physicians, their families and the broader health of the community.

By Ethan McGonagle, UTHSCSA MS-II
My first experience with First Tuesdays at the Capitol came about quite by accident. In February of this year, I joined a student delegation from The University of Texas Health Science Center at San Antonio (UTHSCSA) traveling to the state Capitol. At the time, our medical school was undergoing a significant transition: a planned merger with the University of Texas at San Antonio (UTSA). While this may seem like a minor administrative change, it has far-reaching implications from an academic perspective. Curious but uninformed, I attended a virtual town hall in January to learn more. There, I discovered that a group of students, both from UTSA and UTHSCSA would be visiting Austin on the first Tuesday in February, a monthly event organized by the Texas Medical Association (TMA) to promote physician-led advocacy. Each First Tuesday brings together physicians, students and county medical societies from across Texas to meet with legislators and advocate for TMA’s legislative priorities.
That first trip was eye-opening. I found myself not only engaging with representatives from my own district, but also connecting with some of the most influential physicians in Bexar County and across the state. After my first day at the Capitol, leadership of the merger delegation told me they appreciated how I spoke and the points I raised. For my part, I enjoyed stepping outside the routine of medical school to learn firsthand how policy shapes our profession.
Encouraged by that experience, I began driving to Austin on the first Tuesday of every month, leaving before dawn to join the Bexar County Medical Society (BCMS) delegation. I read up on TMA’s priorities, joined meetings with representatives when possible and, above all, listened and learned. I gained insight into the ongoing tensions between healthcare providers and insurance companies, which this year have been highlighted by disputes over prior authorization requirements. I also became more informed of the persistent debates among physicians and other healthcare professionals regarding scope
of practice. Additionally, I learned more about the significant shortage of accessible healthcare in rural Texas and a wide array of other pressing challenges. This involvement has given me a much broader perspective on how medicine operates as an industry in Texas. It exposed me to the complex chess game the leadership of our trade must engage in to protect not just the interests of its physician constituents, but also the interest of the patients they care for. Furthermore, it presented me to community outreach and social programs both at the state and local levels — areas I had previously known little about. The social aspects were a pleasant bonus, too — mixers, networking events and galas providing opportunities to build lasting professional connections.
I am often asked why I chose to willingly devote so much time to TMA, First Tuesdays and BCMS. Is it driven by a passion for public policy, political ambitions or a personal agenda for professional growth? My honest answer echoes the words of Dr. Sheldon Gross, a past TMA President, who told me over lunch that the reason he engaged so deeply in healthcare advocacy was simple: “It was fun.”
Medical students have precious little free time, and we tend to guard it closely. So, it’s only natural that we look for activities that offer a meaningful return on time invested. When I was asked to help promote the First Tuesday in April, which focused on student participation, I quickly realized that appealing to ideals like “improving public health” or “influencing the future of medicine” rarely resonates with students who are years away from practicing independently. Those goals feel distant and abstract. Instead, I found more success by highlighting immediate tangible benefits: First Tuesday is an excused absence, a chance to network with industry professionals, a chance to discuss interesting issues with physicians and legislators alike and, most importantly, a genuinely enjoyable break from the classroom.
My journey with the TMA actually began months earlier in the fall of 2024 when I got involved with the student branch of the TMA at UTHSCSA. Our school’s branch combined student representation for the TMA, AMA and BCMS (TAB). Initially, I explored submitting student-led resolutions to shape organizational platforms. While this is a valuable component of student involvement, the slow process and layers of separation from real legislative change left me wanting more direct involvement. So, when the chance to participate in First Tuesday presented itself, I seized it. After being elected as our school’s TAB BCMS liaison, I made a point to never miss a BCMS board meeting or legislative committee session. I kept showing up, listening, learning, and building relationships. Through this, I become close with remarkable mentors like Dr. Jayesh “Jay” Shah, now TMA’s President, Dr. Ezequiel “Zeke” Silva III, TMA’s Chair of Legislation and the BCMS Immediate Past President, Melody Newsom, BCMS’s CEO/Executive Director, and Dr. John Shepherd, 2025 BCMS President and Chair of TEXPAC. These relationships weren’t formed through emails alone, but through genuine, consistent engagement in pursuit of shared goals.
My parting message to fellow and future medical students is simple: in healthcare advocacy, your voice matters. Legislators and sea -
soned physicians want to hear what the next generation has to say; they appreciate seeing us care about the future of our profession. While the biggest policy impacts often feel far away, the benefits of getting involved are immediate and real. It strengthens your network, broadens your perspective, and gives you a front-row seat to the real-time evolution of our trade.
And perhaps just as importantly … it’s fun.

Ethan McGonagle is a medical student at the Long School of Medicine-UT Health San Antonio, class of 2029, with a passion for public policy and social outreach. While active in academic research, he also wishes to expand his interests in social outreach and public policy, especially in San Antonio.

By Esther Shin, OMS-III, and Gabriel Bietz, MD
Texas House Bill 5294 (HB 5294) was introduced earlier this year to propose several changes to the medical education, admissions processes and employment practices within Texas. This article describes the proposed changes but, more importantly, the role that medical students played in advocacy regarding the various provisions of the bill.
Representative Greg Bonnen first filed House Bill 5294, which initially described three essential provisions. First, the bill prohibited the use of the pass/fail grading system in all Texas medical schools, requiring instead the assignment of letter grades (A to F) or an equivalent tiered system to all core coursework. The new grading system was to be used for both preclinical and clinical curriculum. The second provision was that medical schools must include standardized test scores (e.g., MCAT) as part of their admissions process. However, it should simultaneously not be the sole criterion. The third provision prohibits medical schools from granting preferential treatment in admissions or employment based on race, sex, color, ethnicity or national origin. There was a narrow exception made for bona fide qualifications based on sex. Furthermore, medical schools were to submit any proposed changes to academic standards to the Texas Legislature and the Texas Higher Education Coordinating Board. If a vote of two-thirds of all members of House is received, the last sections of the bill asserted that all would take effect immediately or with the admissions for the 2026 spring semester.1
However, the proposed changes became a source of concern for many current and aspiring medical students. They used various approaches to voice those concerns about the potential negative effects the bill could have on the wellbeing of students as well as the diversity in the medical workforce. They organized petitions, sending emails and letters to lawmakers that expressed their opposition to certain provisions of the bill. In particular, the grading system mandate was argued against due to its implications on mental health. They cited the rising rates of burnout seen in medical students and resident physicians. To this end, students utilized social media platforms and traditional media outlets to gain public support. Several medical students even directly testified in Austin, Texas at the State Capitol, presenting their personal testimonies to lawmakers.
With the collective advocacy efforts of these medical students, the bill was mended with several modifications:
• Different Grading Requirements: The amendment wrote that at least 50% of coursework was to be graded by the A-F system, instead of 100%. This allowed up to 50% of the curriculum to be graded as pass or fail.
• Delayed Implementation: The effective date of the grading system mandate was postponed to the admissions of 2026 fall semester. Current students will not be affected, medical schools would have additional time to adapt and future medical students would have a clearer influence on their decision on whether or not they want to pursue a medical education in Texas.

Texas House Bill 5294 did pass both the Texas House and Senate. However, it failed to become law at the regular session due to procedural issues on June 2, 2025. These outcomes demonstrate the impact that organized advocacy can have on legislative processes. It is important to involve not only medical professionals, but also medical trainees in the discussions about the future of medical education.
The involvement of medical students in the legislative process of HB 5294 highlights several key ideas. Medical students possess a unique perspective that can provide valuable insight on policies concerning medical education and their potential consequences. Furthermore, their efforts to voice their opinions show that there are advocacy strategies that can be effective. If mobilized, medical students can influence policy decisions. Finally, there is a need for ongoing discussion between policymakers and healthcare students and workers to ensure that current and new medical education policies align to meet the needs and realities of the community. By demonstrating the importance of student involvement in shaping policies that shape their education and professional development, the case of HB 5294 serves as a model for medical students in future advocacy efforts.
Reference:
1. TX - HB5294. (2025). BillTrack50. https://www.billtrack50. com/billdetail/1869633


Esther Shin, OMS-III, is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, with an interest in public health.
Gabriel Bietz, MD, is a board-certified vascular surgeon and Chairman of the Board for San Antonio Surgical Center of Excellence. He is a partner at Texas Cardiac and Vascular Institute, serving patients across San Antonio, Seguin and Corpus Christi. He is recognized for his expertise in both open and endovascular procedures, along with his leadership in advancing patientcentered vascular care. In addition to his medical career, Dr. Bietz is a serial entrepreneur with ventures spanning healthcare and private investments, and is a member of the Bexar County Medical Society.
By Patrick Reeves, MD, FAAP, DABOM
In the aftermath of the devastating flooding that swept through the Texas Hill Country this Independence Day, communities are grappling not only with physical losses but also with the emotional and psychological toll of the disaster.
As medical professionals in Bexar County and across Texas, we are called to respond not only to physical injuries but also to the mental health crises that often follow in a disaster’s wake. Many of our patients — whether they are directly impacted or connected to the region through family and friends — are experiencing trauma, grief, anxiety and, in some cases, overwhelming survival guilt. In these moments, timely and compassionate behavioral health support becomes as critical as any medical intervention.
Survival guilt is a complex and deeply personal reaction common among those who lived through a life-threatening event or lost loved ones while surviving themselves. Patients may feel undeserving of their survival, obsess over what more they could have done, or feel emotionally paralyzed in the aftermath. As clinicians, it is vital we acknowledge these feelings as valid and help patients understand that survival guilt is a normal response to trauma — not a sign of weakness or failure. Encourage patients to reframe their survival as a path to healing and purpose, and connect them with support systems that can guide them through that journey.
Texas is fortunate to have a range of behavioral health resources that can aid individuals and families coping with post-disaster mental health needs. One such organization is the Children’s Bereavement Center of South Texas (https://cbcst.org/), located in Bexar County, which offers counseling and grief support not only for children, but also for parents, families and caregivers impacted by loss. While the center's core mission is child-focused, its programs are designed to serve the entire family system, recognizing that recovery is most successful when it is community-based and holistic. Their services include trauma-informed counseling, peer support groups and school-based interventions, which are especially valuable now as displaced families seek stability and normalcy.
In addition, the Texas Health and Human Services Commission (HHSC) (https://www.hhs.texas.gov/services/mental-healthsubstance-use/mental-health-crisis-services/disaster-behavioralhealth-services) operates a disaster behavioral health services program that offers free and confidential support via the Texas Disaster Behavioral Health Services hotline. This service can connect
individuals to crisis counseling, stress management and referrals to local mental health providers.
Medical professionals should also be aware of resources provided by local Mental Health Authorities (LMHAs), who are often equipped with mobile crisis outreach teams ready to respond to acute needs in flood-affected areas. In addition, the HHSC webpage provides links and PDFs for Practical Tips for youth, the public and first responders in addition to a compendium of its own behavioral health resources.
It’s important for clinicians, especially those practicing in family medicine, pediatrics and emergency care, to proactively screen for signs of emotional distress. Symptoms may not be immediately evident, as patients might downplay their emotional needs while prioritizing logistical or physical concerns. Use trauma-informed language and ask open-ended questions like, “How are you coping with everything that’s happened?” or “What’s been the hardest part for you or your family since the flood?”
We must also remember that caregivers — first responders, teachers, medical staff — are themselves at risk of burnout, vicarious trauma and compassion fatigue in this prolonged recovery period. Encourage your colleagues to take advantage of employee assistance programs and mental health check-ins, and cultivate a culture of mutual support within your practice or institution.
As healthcare providers, we are uniquely positioned to normalize help-seeking behavior and reduce the stigma surrounding mental healthcare. By actively guiding patients toward resources like the Children’s Bereavement Center of South Texas, LMHAs and statewide crisis services, we can help bridge the gap between trauma and healing. The floodwaters may have receded, but the emotional aftershocks linger. Let’s ensure our response includes the full scope of care — physical, emotional and psychological — for every patient we serve.
Thank you for all that you do for patients and for Texas.

Patrick Reeves, MD, FAAP, DABOM, is a native Texan and graduate of Texas A&M University (class of 2012) who currently serves as a triple board-certified pediatric gastroenterologist, obesity medicine specialist and general pediatrician in San Antonio, Texas. He works on the liver transplant unit at University Hospital and is active in clinical research focused on clinical action plan implementation.
Courtesy of Broadway Bank
Dr. Amit Mehta is an entrepreneur-turned-investor focused on our healthcare investment practice. Dr. Mehta combines practical knowledge across the value-chain with entrepreneurial experience to lead the health-IT investment practice as Partner at Builders VC. Additionally, he has led Intrinsic Imaging to operate clinical trials in 64 countries globally for both pharma and biotech sponsors as Founder and Chief Medical Officer. Dr. Mehta completed his residency at Harvard Medical School where he also completed a fellowship in Minimally Invasive Image Guided Surgery. He has co-authored three textbooks in medicine, has widely published in peer-reviewed journals and currently is appointed as an SBIR/STTR reviewer for the National Institutes of Health. His passion for leadership excellence has led to his service to various start-up boards and non-profits. Amit is the previous recipient of the George Brown Radiological Society of North America award, the Joseph E Whitley award, and was named on the “40 under 40” list by the San Antonio Business Journal
For Dr. Amit Mehta, the road to becoming an interventional radiologist was guided by his passion for cutting-edge medicine and a desire to make a difference in people’s lives. Now, as a member of the South Texas Radiology Group and South Texas Radiology Imaging Centers, Dr. Mehta is at the forefront of minimally invasive, image-guided surgery in San Antonio.
“Our practice is thriving,” Dr. Mehta explains. “We have nearly 70 radiologists serving 4,000 to 5,000 patients daily across the San Antonio area and beyond, into South Texas and Mexico. I’m proud to be part of a group that’s so dedicated to advancing technology and providing the highest quality care to our community.”
Dr. Mehta’s journey to San Antonio was fueled by his admiration for the city’s unique combination of small-town charm and big-city opportunities. “San Antonio offers a hometown feel while allowing me to practice medicine at a level of quality that’s unparalleled in the country,” he says.
As a leader in imaging technology, Dr. Mehta and his team are committed to excellence. “What I’m most proud of is our dedication to quality and our ability to deliver care to patients — not just in San Antonio, but across the region.”
For over 20 years, Broadway Bank has been a vital partner in Dr. Mehta’s professional and personal endeavors. From financing imaging centers to providing resources for new equipment, the bank has been instrumental in helping South Texas Radiology Group achieve its mission of delivering exceptional care.
“The team at Broadway Bank has provided guidance and support for both medical and non-medical pursuits,” Dr. Mehta shares. “They’ve been there every step of the way, offering terms that make our projects successful. Their commitment to getting deals done, even when the macroeconomic environment was challenging, has been unmatched.”
Beyond his medical practice, Dr. Mehta has leaned on Broadway Bank for real estate and wealth management services. “One of the things that sets Broadway Bank apart is their ability to service my entire portfolio,” he says. “Whether it’s my medical practice, real estate investments, or other opportunities, they’ve consistently delivered personalized and concierge-level service.”
Dr. Mehta emphasizes that Broadway Bank’s local presence is key to its unparalleled service. “I’ve worked with many banking partners over the years, and Broadway Bank has always provided a level of service that stands out,” he explains. “Their local feel, combined with a commitment to technology and responsiveness, ensures that my needs are always met, no matter the project.”
For Dr. Mehta, banking with Broadway Bank is about more than transactions; it’s about trust, reliability and relationships. “Broadway Bank has shown me what it means to be a true partner. Their team is always first to provide solutions, and they’ve been a constant source of support for over two decades. I’m proud to bank with Broadway.”
Broadway Bank’s Private Banking team provides concierge financial services curated specifically for your business and personal needs. Our Private Bankers get to know you personally and professionally to tailor precise financial strategies. With a single point of contact available to you 7-days a week, you will get prompt personal service from a team of experts, each working together to accomplish your financial goals.
Visit Broadway.Bank/private to learn how you can benefit from modern banking that’s locally sourced and personally delivered.
Broadway Bank is a Gold Member of the BCMS Circle of Friends Program. BroadwayBank.com

The July 8th 1853 Club Luncheon welcomed Eva Y. Prieto, PhD, RN, Director of Health Promotion at Community First Health Plans, as its featured speaker. Dr. Prieto offered thoughtful insights on “Keeping a Healthy Mind,” highlighting practical ways to nurture mental wellness.
These quarterly gatherings are designed to foster connection among retired BCMS member physicians, offering a warm space to catch up with colleagues and hear engaging presentations on timely topics.
Mark your calendar: The next 1853 Club Luncheon is scheduled for October 7, 2025.
Interested in joining the 1853 Club? If you’re a retired or life member of BCMS, reach out to membership@bcms.org or call 210-301-4391 to learn more.





As a BCMS member, you can find exclusive discounts on premium products and services that you and your practice use every day.

Sol Schwartz & Associates P.C. (HHH Gold Sponsor)
Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Christopher Davis, CPA 210-384-8000, ext. 118 cbd@ssacpa.com www.ssacpa.com
“Dedicated to working with physicians and physician groups.”

Atlas Retirement Strategies LLC (HHH Gold Sponsor)
Atlas Retirement Strategies LLC is a comprehensive financial planning firm dedicated to serving the unique needs of the medical community. We offer customized strategies in business planning, retirement planning, risk management, wealth preservation, estate planning, and wealth transfer – empowering healthcare professionals to achieve long-term financial security, clarity, and peace of mind.
Amanda Webb, LACP Founder & Principal 210-281-4400
Amanda@atlas-plans.com www.atlas-plans.com
MANAGEMENT

Aspect Wealth Management (HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark President 210-268-1520
MClark@aspectwealth.com www.aspectwealth.com
“Your wealth. . .All aspects”

Broadway Bank (HHH Gold Sponsor)
Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead 210-283-6640
TDuran@broadway.bank
www.broadwaybank.com
“We’re here for good.”

Texas Partners Banks (HHH Gold Sponsor)
Our private banking team specializes in healthcare banking and will work with you to craft and seamlessly integrate financial solutions for you and your practice, including practice loans, lines of credit and custom local lockbox solutions headquartered in San Antonio.
Maria Breen 210-807-5562
Maria.Breen@texaspartners.bank www.texaspartners.bank

Lone Star National Bank (HHH Gold Sponsor)
Established in 1983, Lone Star National Bank has provided banking services to communities in South Texas for the past 41 years. LSNB is an independent and locally owned bank subsidiary of Lone Star National Bancshares-Texas, Inc with consolidated assets of $3 billion (12/31/23) and 36 full-service banking centers throughout Starr, Hidalgo, Cameron and Bexar counties.
Aside from personal and business banking, LSNB offers investments, wealth management & trust along with property and casualty insurance, health insurance and supplemental coverage.
Ivan Corona Molina Assistant VP 210-479-4713
MolinaI@lonestarnationalbank.com www.lonestarnationalbank.com
“We do what the Little Banks can’t, and the Big Banks won’t!”
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Robert Lindley
SVP | Private Banking Team Lead 210-343-4526
Robert.Lindley@amegybank.com
Denise Smith
Vice President | Private Banking 210-343-4502
Denise.C.Smith@amegybank.com
Scott Gonzales
Assistant Vice President | Private Banking 210-343-4494
Scott.Gonzales@amegybank.com www.amegybank.com
“Community banking partnership”
Synergy Federal Credit Union (HH Silver Sponsor)
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help physicians get the banking services they need. Synergy FCU Member Services 210-750-8333 info@synergyfcu.org www.synergyfcu.org
“Once a member, always a member. Join today!”

American Health Imaging (HHH Gold Sponsor)
American Health Imaging (AHI) has 5 state-of-the-art imaging centers in San Antonio, TX with industry- boardcertified subspecialized radiologists delivering precise, reliable results. Easy scheduling and prompt report turnaround times, serving both physicians and their patients. Imaging at AHI is priced up to 60% less than hospitals and in-network with 99% of health plans with competitive rates to save patients money. AHI has an additional 37 best-in-class diagnostic imaging facilities in Alabama, Florida, Georgia, Texas and South Carolina. US Radiology Physician Number 210-572-1211
Casey Allen
Regional Sales Director | San Antonio US Radiology Specialists 210-846-0606
Casey.Allen@usradiology.com
Jasmine Mendoza
Jasmine.Mendoza@usradiology.com
Jaime Zamora Jaime.Zamora@usradiology.com

Sydnie Caradec
Sydnie.Caradec@usradiology.com
Sarah McMindes
Sarah.Mcmindes@usradiology.com
Scott Roberson
Scott.Roberson@usradiology.com
Ryan Denman
Ryan.Denman@usradiology.com
www.americanhealthimaging.com (main site)
www.americanhealthimaging.com/ physician-resources/ (Physician Resources to refer to American Health Imaging)

Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor)
Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for healthcare entities.
Betty Fernandez Director of Operations 210-582-6355
Betty.Fernandez@bexarcv.com www.bexarcv.com
“Proudly serving the medical community since 1998”

Avid Wealth Partners (*** Gold Sponsor)
For over 15 years, Avid Wealth Partners has been the trusted financial partner for local physician specialists and practice owners. We specialize in physician-focused financial advising, offering proactive tax planning, customized investment strategies, and comprehensive risk management solutions. Our approach addresses every aspect of your financial life, protecting your hardearned assets and building lasting wealth. With a team of credentialed specialists, we simplify complexity so you can focus on what you do best— caring for patients
MDWealth@avidwp.com www.avidforphysicians.com 210-864-3333

Elizabeth Olney with Edward Jones (HHH Gold Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney
Financial Advisor 210-858-5880
Elizabeth.Olney@edwardjones.com www.edwardjones.com/elizabeth-olney "Making Sense of Investing"

Aspect Wealth Management (HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark President 210-268-1520
MClark@aspectwealth.com www.aspectwealth.com
“Your wealth. . .All aspects”
Hancock Whitney (HH Silver Sponsor)
Since the late 1800s, Hancock Whitney has embodied core values of Honor & Integrity, Strength & Stability, Commitment to Service, Teamwork and Personal Responsibility. Hancock Whitney offices and financial centers in Mississippi, Alabama, Florida, Louisiana and Texas offer comprehensive financial products and services, including traditional and online banking; commercial, treasury management, and small business banking; private banking; trust; healthcare banking; and mortgage services.
John Riquelme
San Antonio Market President 210-273-0989
John.Riquelme@hancockwhitney.com
Serina Perez San Antonio Business Banking 210-507-9636
Serina.Perez@hancockwhitney.com

UT Health San Antonio
MD Anderson Cancer Center (HHH Gold Sponsor)
UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
UT Health San Antonio Physicians
Regina Delgado
Business Development Manager 210-450-3713
DelgadoR4@uthscsa.edu
UT Health San Antonio
MD Anderson Mays Cancer Center
Laura Kouba
Business Development Manager 210-265-7662
NorrisKouba@uthscsa.edu
Appointments: 210-450-1000
UT Health San Antonio 7979 Wurzbach Road San Antonio, TX 78229

Golden Billing & Benefits
(HHH Gold Sponsor)
Golden Billing is owned and operated for over 20 years in Houston, TX. The owner, Marcus Yi, is focused on creating a partnership with clients. We are dedicated to optimizing the small business doctor’s productivity and maximizing practice cash flow by accurate claims coding and timely processing. Call today for a free consultation. If you don’t want to use us at lease maybe we can help you fine tune your decision.
Marcus Yi 713-263-0054
MYi@goldenbilling.com www.goldenbilling.com

Genuine Health Group (HHH Gold Sponsor)
Genuine Health Group partners with primary care providers to help them successfully adopt value-based payment models and demonstrate better health outcomes. Providers choose us for our proven expertise and consistency both for their patients enrolled in Medicare Advantage plans and for their patients with traditional Medicare who can align with one
of ACOs. We have a track record of effectively reducing the cost of care while simultaneously improving care quality.
786-878-5500
info@genuinehealthgroup.com www.genuinehealthgroup.com
Equality Health (HH Silver Sponsor)
Equality Health deploys a wholeperson care model that helps independent practices adopt and deliver value-based care for diverse communities. Our model offers technology, care coordination and hands-on support to optimize practice performance for Medicaid patients in Texas.
Cristian Leos Network Development Manager 210-608-4205
CLeos@equalityhealth.com www.equalityhealth.com “Reimagining the New Frontier of Value-Based Care.”
DialOPS
(H Bronze Sponsor)
Dialops is a trusted U.S.-based medical answering service and virtual receptionist solution designed specifically for healthcare practices. We provide 24/7 live call handling, HIPAA-compliant messaging, appointment scheduling, and reliable after-hours and overflow support. Our medically trained agents answer every call with professionalism and care—just like your in-office staff— ensuring your patients always feel heard and supported. From solo providers to busy clinics, Dialops helps reduce missed calls, ease front desk overload, and improve the patient experience—all at a fraction of the cost of hiring in-house.
Rachel Caero Rachel@dialops.net
Call 877-2-DIALOPS/ 210-699-7198 or visit www.dialops.net to get started today.

TMA Insurance Trust
(HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service insurance agency offering a full line of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.
Wendell England Director of Member Benefits
512-370-1746
Wendell.England@tmait.org
800-880-8181
www.tmait.org
“We offer BCMS members a free insurance portfolio review.”

Texas Medical Liability Trust (HHHH 10K Platinum Sponsor)
With more than 20,000 healthcare professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of healthcare for patients by educating, protecting and defending physicians.
Patty Spann Director of Sales and Business Development 512-425-5932
Patty-Spann@tmlt.org www.tmlt.org
“Recommended partner of the Bexar County Medical Society”

The Bank of San Antonio Insurance Group, Inc. (HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Katy Brooks, CIC 210-807-5593
Katy.Brooks@bosainsurance.com www.thebankofsa.com
“Serving the medical community.”
MedPro Group (HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze, RPLU, ARM
AVP Market Manager, SW Division 512-658-0262
Fax: 844-293-6355
Kirsten.Baze@medpro.com www.medpro.com
LASO Health Telemedicine and Rx App (HH Silver Sponsor)
LASO Health is the industry’s only solution that makes healthcare services accessible, cost-transparent and convenient. Its mission is to reinvent “healthcare” in the United States by empowering every individual and employer, insured or uninsured to have easy, timely, predictable, cost-effective care. LASO combines an intuitive, mobile superapp with a marketplace of virtual and in-person health services to give customers a one-touch, onestop-shop, comprehensive health solution.
Ruby Garza, MBA 210-212-2622
RGarza@texaskidneycare.com www.lasohealth.com

Parvus Medical Suites (HHHH 10K Platinum Sponsor)
Parvus Medical Suites offers a new way to start your own private clinical practice, either full-time or part-time, at a much lower cost than a traditional clinic. We take care of providing well-qualified employees, so that you can focus solely on delivering high-quality patient care. Our turn-key practice spaces in San Antonio and New Braunfels are available for short- and long-term lease options, and come complete with all amenities. Micropractice medicine is revolutionizing independent clinical care.
John Rodriguez, MD Chief Medical Officer 210-632-3411
DrJohn@parvussuites.com www.parvussuites.com
Henry Schein Medical (HH Silver Sponsor)
From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Kelly Emmon
Field Sales Consultant
210-279-6544
Kelly.Emmon@henryschein.com www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”
Eleos Virtual Healthcare Solutions (HH Silver Sponsor)
Empowering physicians for a Balanced Future. Our virtual health associates alleviate administrative burdens in the evolving healthcare landscape, combatting burnout. Join us in transforming healthcare delivery, prioritizing your wellbeing and patient care.
Darby Rodriguez Regional Client Executive 281-753-3565
D.Rodriguez@eleosvhs.com www.equalityhealth.com
“Reimagining the New Frontier of Value-Based Care”
Methodist Physician Practices (**Silver Sponsor)
Methodist Physician Practices is committed to providing exceptional care for patients in greater San Antonio and South Texas. As part of Methodist Healthcare, we are dedicated to raising the standards of performance excellence while advancing the health and well-being of the communities we serve. Our extensive network of highly-skilled primary care physicians, specialists and surgical care providers ensures patients receive comprehensive, coordinated and compassionate care.
As part of the Methodist Healthcare System, our physicians are committed to delivering personalized, high-quality services that meet the
diverse needs of our patients. At Methodist Physician Practices, we go beyond healthcare — providing hope, healing and unwavering support for each individual we serve.
Erin Fitzgerald
Methodist Healthcare I Methodist Physician Practices M:281-673-7350
methodistphysicianpractices.com
Healthcare Leaders of San Antonio (HH Silver Sponsor)
We are dedicated to nurturing business connections and professional relationships, exchanging knowledge to enhance leadership, and creating career opportunities for healthcare and other industry leaders in a supportive community.
David Neathery President 210-797-8412
HealthcareLeadersSA@gmail.com
Gary Meyn, LFACHE Vice President 210-912-0120
GMeyn@vestedbb.com https://healthcareleaderssa.com/ “Come, Learn, Connect!”
The Health Cell (HH Silver Sponsor)
“Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more! Kevin Barber President 210-308-7907 (Direct) KBarber@bdo.com
Valerie Rogler Program Coordinator 210-904-5404
Valerie@thehealthcell.org www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA)
(HH Silver Sponsor)
SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising. Jeannine Ruffner President info4@samgma.org www.samgma.org

Favorite Healthcare Staffing
(HHHH 10K Platinum Sponsor)
Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle.
San Antonio Office 210-301-4362
www.favoritestaffing.com
“Favorite Healthcare Staffing offers preferred pricing for BCMS members.”


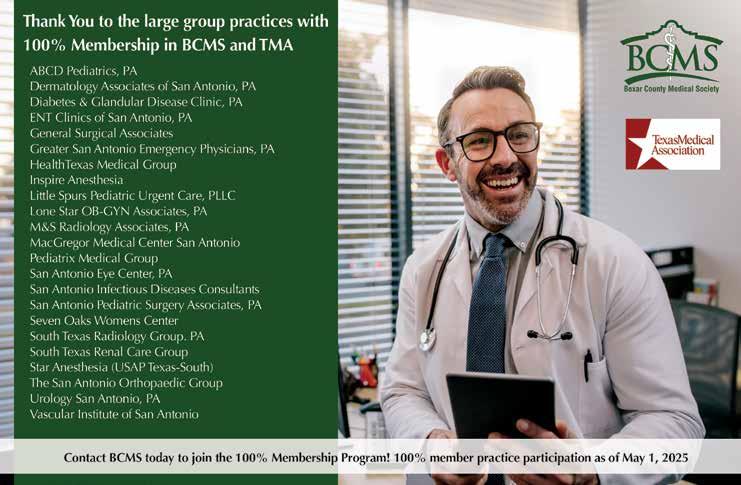

The 2025 BMW M3 with a manual transmission is an outlier in our electrified automotive era. As BMW’s performance M division marches reluctantly toward hybrid and battery-electric (BEV) propulsion, and as dual-clutch and ZF automatic transmissions dominate highperformance vehicles, the idea of a six-speed manual gearbox bolted to a twin-turbo inline-six feels anachronistic. Nevertheless, there’s also an authenticity and connection that even the most modern automatics can’t replicate.
To understand the appeal of this car, you have to forget about numbers. Yes, its engine produces 473 horsepower and 406 lb-ft of torque, but the (RWD-only) manual M3 lacks the relentless launch capability of AWD and the super quick shifts of the ZF eight-speed, so it’s slower than automatic transmission M3s.
BMW hasn’t tried to make things easy with their manual M3, by the way. The clutch is heavy and bites high, and the shift action includes a mechanical notchiness that demands concentration. Automatic rev matching, which I enjoy, can be turned off, though it’s more precise than I could ever be so I left it on.
As noted above, the M3 manual is not as fast as its automatic sibling. The 0–60 mph sprint is in the mid-four-second range, about

half a second slower than the Competition xDrive. But again, that misses the point. The manual car demands engagement. It makes you think about corners, commit to gears, and plan braking points. There’s a rhythm to it that’s increasingly rare in modern cars, especially those with north of 450 horsepower. You don’t drive this M3 because it’s easier, but rather because it’s harder — and that difficulty becomes part of the reward.
The steering is precise but a little filtered — BMW’s electromechanical setup doesn’t quite have the clarity of older hydraulic racks — but there’s real feedback. And despite a base curb weight of around 3500 lbs., its balance is superb when you push it.
For the record, the last gen manual M3, which I owned, was pretty good, but this one is significantly better. The engine sound has been improved, and the steering and shifter are more satisfying to use.
Design-wise, the oversized front grille remains divisive, but the shape is aging into itself — aggressive now feels normal, not shocking — and the more understated rear end helps tamp down the boy racer vibe.
Inside, the M3’s cabin remains a blend of focused aggression and luxury aspiration. The M carbon bucket seats are still available and still punishing over long trips, but the standard sport seats strike a good




balance between support and livability. Interior materials are excellent, with real carbon fiber, brushed metal and Alcantara where it matters. The manual shifter, adorned with the classic BMW M shift pattern, doesn’t really belong in a cockpit dominated by touchscreens, configurable lighting and complicated software menus, but I’m glad it’s there.
The standard iDrive 8.5 user interface runs on a large curved screen that stretches from left of the steering wheel to past the center console. The graphics are crisp with quick responses, but the interface remains too layered. Simple things like changing drive modes or adjusting climate settings still require too many taps or swipes. And while BMW has thankfully retained some hard buttons on the console, I wish they’d add more.
BMW has wisely resisted the urge to turn this car into a special edition or charge a collector’s premium for the manual (like Porsche does). It remains a no-cost option on the base M3 rear-wheel-drive, the last bastion of an analog experience in the M3 lineup. And while this generation might be its final outing with a clutch pedal, BMW hasn’t stripped the experience bare. You still get the full suite of driver aids and connectivity, but you can also switch everything off and drive like it’s 1997 again.


There are flaws. The grille will never win beauty contests. The manual’s slower acceleration and thirstier nature (EPA ratings are 16 city/23 highway mpg) are obvious drawbacks in the numbers race. And the price — just under $78,000 before options — can easily climb into the mid-90s if you start ticking boxes. At that point, a Porsche Cayman GTS or even a lightly optioned 911 comes into view. But they don’t offer four doors, real rear seats or this blend of everyday usability and track-day credibility.
In 2025, the M3 manual is a flawed anachronism. It’s less efficient, less digital and less in tune with the automotive world around it than many other performance cars. But that’s exactly why it matters. This is a car that reminds us what we’re in danger of losing. BMW M still knows how to build soul into metal. The six-speed M3 may not be the future, but it remains a damn good reason to love driving now.

Stephen Schutz, MD, is a board-certified Gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.

11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Northside Honda 9100 San Pedro Ave. San Antonio, TX 78216
Jaime Anteola 210-744-6198
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Anthony Garcia 210-681-3399
14610 IH 10 West San Antonio, TX 78249
Tim Rivers 832-428-9507
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Domingo Saenz 210-341-3311
Auto Group
North Park Lexus 611 Lockhill Selma San Antonio, TX 78216
Jose Contreras 320-308-8900
Bluebonnet Chrysler
Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX 78006
James Godkin 830-981-6000
Cavender Toyota 5730 NW Loop 410 San Antonio, TX 78238
Spencer Herrera 210-581-0474
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX 78216
Chris Martinez 210-366-9600
North Park Toyota 10703 SW Loop 410 San Antonio, TX 78211
Justin Boone 210-635-5000
9455 IH 10 West San Antonio, TX 78230
Jordan Trevino 210-764-6945
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX 78257
James Cole 210-816-6000
Northside Ford 12300 San Pedro San Antonio, TX 78216
Marty Martinez 210-477-3472
North Park Lincoln 9207 San Pedro San Antonio, TX 78216
Sandy Small 210-341-8841
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson 877-356-0476


• Fast prior authorizations assistance for easy scheduling
• Prompt turnaround on standard reports within hours, not days
• Easy-to access physician portal for instant access to reports
• Easily accessible subspecialized radiologists for questions
• State-of-the-art imaging equipment for the diagnostic insights you need for next steps in patient care
• 6 convenient locations throughout San Antonio and New Braunfels
• Same-day and next-day appointments
• Extended and weekend hours to fit your patients’ busy schedules
• In-network with 99% of insurance plans and costs up to 60% less than hospital-based imaging
• Faster scanning technology increases patient comfort with an average MRI scan of 15 minutes or less