





NON PROFIT ORG US POSTAGE PAID SAN ANTONIO, TX PERMIT 1001 SAN ANTONIO


PUBLISHED BY: traveling Blender, llC. 10036 Saxet Boerne, tX 78006

PUBLISHER louis doucette louis@travelingblender.com
BUSINESS MANAGER: vicki Schroder vicki@travelingblender.com
ADVERTISING SALES:
AUSTIN: Sandy Weatherford sandy@travelingblender.com
CHILDREN’S HEALTH
San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EditoriAl CorrESpondEnCE: Bexar County Medical Society 4334 n loop 1604 W, Ste. 200 San Antonio, tX 78249
Email: editor@bcms.org
on Awareness Month – The Science Behind Eating the Rainbow By
MAGAZinE AddrESS CHAnGES: Call (210) 301-4391 or Email: membership@bcms.org
SuBSCription rAtES: $30 per year or $4 per individual issue
AdvErtiSinG CorrESpondEnCE: louis doucette, president traveling Blender, llC.
A publication Management Firm 10036 Saxet, Boerne, tX 78006 www.travelingblender.com
For advertising rates and information Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national orgin, or an intention to make such preference limitation or discrimination.
SAN ANToNIo: Gerry lair gerrylair@yahoo.com
PRojECT CooRDINAToR: denise tapia denise@smithprint.net


For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.
SmithPrint, Inc. is a family owned and operated San Antonio based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2023 Smithprint, inc. prin tE d in tHE u SA
SAN ANTONIO 4 SAN ANTONIO MEDICINE • March 2023
TABLE OF CONTENTS
THE OFFICIAL PUBLICATION OF THE BEXAR COUNTY MEDICAL SOCIETY • WWW.BCMS.ORG • $4.00 • MARCH 2023 • VOLUME 76 NO.3
Helping Children with Cerebral Palsy Thrive By Alice K. Gong, MD 12 Pediatric Mental Health Issues: Treatments and Challenges By Grizelda Anguiano, MD 14 Understanding Adolescent Eating Disorders By Noel C. Ales, DO 16 Concerning Youth and Vaccination Hesitancy By Bethanne Bradshaw and Marcy Snyder 18 Nutriti
Julia D’Isabella, Alexandra Fekete, Abigail Joy Garcia, Deonte Jefferson and Bridgette Kielhack 20 Increasing Awareness of Pressure Ulcers in Those with Physical Limitations Due to Disabilities By Rebecca Wang and Christina Pierce ....................................22 CommuniCare and the Multi-Assistance Center (MAC) at Morgan’s Wonderland By Robert P. Sanders, MD, MHA, FAAP, CPE 24 The San Antonio DoSeum: Creating Unique and Unforgettable Experiences for Families By Richard Kissel, PhD, Chief Program Officer, Interviewed by Monica Jones, COO, BCMS 26 BCMS President’s Message 8 BCMS Alliance Message 10 Creative Writing in Medicine – Eve By Tanima Arora 28 Conversations By Holly Ratcliff, Community By Nisha Kalyanpur 30 Cross-Stitch Heart By Sarah Suhood, Untitled By Grace Cooper 31 Imposter Syndrome By Stephanie Batch, Such a Lovely Smile By Danny Parris 32 TMA Kicks-Off 20th Anniversary of First Tuesdays at the Capitol By Mary E. Nava, MBA, Chief Government Affairs Officer 34 Texas Medical Association - 2023 Winter Conference 38 BCMS Vendor Directory 40 Auto Review: Porsche Track Experience By Stephen Schutz, MD 44 Recommended Auto Dealers 46

ELECTED oFFICERS
John Joseph nava, Md, President
Brian t. Boies, Md, Vice President
Ezequiel “Zeke” Silva iii, Md, Treasurer
John Shepherd, Md, Secretary

Brent W. Sanderlin, do, President-elect
rajeev Suri, Md, Immediate Past President
DIRECToRS
Woodson "Scott" Jones, Md, Member
Sumeru “Sam” G. Mehta, Md, Member
priti Mody-Bailey, Md, Member
lubna naeem, Md, Member
lyssa n ochoa, Md, Member
Jennifer r rushton, Md, Member
raul Santoscoy, do, Member
Amar Sunkari, Md, Member
lauren tarbox, Md, Member
Jenny Case, Alliance Representative
ramon S. Cancino, Md, Medical School
Representative
lori Kels, Md, Medical School Representative
robert leverence, Md, Medical School
Representative
Keiko McManus, Md, Board of Ethics Chair
John pham, do, Medical School Representative
Cheryl pierce-Szender, Alliance Representative
ronald rodriguez, Md, phd, Medical School
Representative
Col. tim Switaj, Md, Military Representative
George F. “rick” Evans, Jr., General Counsel
Jayesh B. Shah, Md, TMA Board of Trustees
Melody newsom, CEO/Executive Director
BCMS SENIoR STAFF
Melody newsom, CEO/Executive Director
Monica Jones, Chief Operating Officer
Yvonne nino, Controller
Mary nava, Chief Government Affairs Officer
Brissa vela, Membership Director
phil Hornbeak, Auto Program Director
August trevino, Development Director
Betty Fernandez, BCVI Director
Al ortiz, Chief Information Officer
PUBLICATIoNS CoMMITTEE
norys Alexandra Castro-pena, Md, Co-chair
John Joseph Seidenfeld, Md, Co-chair
louis doucette, Consultant
david Schulz, Community Member
Elizabeth Clanton, Md, Member
Kristy Yvonne Kosub, Md, Member
neal Meritz, Md, Member
Jaime pankowsky, Md, Member
Alan preston, phd, Member
rajam S. ramamurthy, Md, Member
Adam v ratner, Md, Member
Faraz Yousefian, do, Member
Moses Alfaro, Student Member
Winona Gbedey, Student Member
tue Felix nguyen, Student Member
niva Shrestha, Student Member
Bethanne Bradshaw, Student Member
Monica Jones, BCMS Coo, Staff Liason
nancy Salas, Editor
6 SAN ANTONIO MEDICINE • March 2023
BCMS BOARD OF DIRECTORS
Seeing the Inner Child in Everyone - Part I
By John J. Nava, MD, 2023 BCMS President

I hope to explore what each of us can do to better the health status of children in San Antonio, Bexar County, and the surrounding counties. In part one, I will discuss frameworks that have been used to address the needs of those children and the larger population. In part two, I hope to report and frame a snapshot of the current health status of those children and families, and offer some ideas about how best to improve their status, from a community health perspective.
During my undergraduate education, I took many Sociology classes. I learned about Maslow’s hierarchy of needs, typically represented as a pyramid, each being built upon the next as the lower needs were met. These progress through physiological needs, safety needs, love, and belonging, esteem and self-actualization. This theoretical structure was first proposed in 1943, and though outdated, gives us something to hang our hat on. The theory has been much criticized for lacking conclusive validating evidence, and the construct as proposed by Maslow required that progress could not occur until a lower level had been completed. Nevertheless, it has still been used to explain how effort and motivation are correlated in the context of human behavior. I recall studying how Russian and American child rearing practices differed with regard to guidance into professions, with individualism emphasized in the USA over the needs of the collective in the USSR. Of course, cultural differences abound. Though I continued as a pre-med student with a curriculum heavily weighted in hard science, I always remembered the principles of that area of human behavior. As I furthered my studies, I hoped to eventually become a pediatrician.
When I was in medical school, I enjoyed ambulatory pediatrics, as children with minor ailments bounced back quickly. Then I rotated through inpatient pediatrics, where I met a three-year-old child, that had never spent a day outside of the ICU due to complications after repair of a tracheoesophageal fistula. After seeing children with terminal cancer, I knew I wouldn’t be able to handle a career filled with those sorts of cases. I imagined I would have been miserable trying to meet their major needs.
I then chose family medicine, where I could still see ambulatory pediatric patients, followed by public health practice. It was during these years that I was first sensitized to the social determinants of health
(SDOH). Tools were developed to assess five need areas, specifically food, housing, utilities, transportation and safety. Then more areas of needs were added, with various lists of up to 15 total being developed.1 Currently, Healthy People 2030 continues to prioritize many of these same issues.2 Thankfully, diagnostic codes to compensate clinicians for the time it takes to address these items have been developed and efforts are underway to make these industry standards.
After decades of discussion of these risk factors, what has changed? Specifically for our community of San Antonio and Bexar County, has the political will developed to modify these risk factors, and improve the health status of the people living here? Maybe in some areas, but a larger consensus has been elusive. Anytime it involves tapping into the tax base, many skeptics must be convinced that early investment in prevention is better than waiting to address costly health problems.
Trauma Informed Care (TIC)
A couple of years ago, a local public health leader was invited to a meeting of the BCMS Public Health and Patient Advocacy Committee. I asked that person about the theoretical connection between ACEs (Adverse Childhood Experiences) and epigenetic changes later discovered in families of trauma victims. I was promptly informed by this community leader that it was not just a theory, but a proven fact, and there had been developed a large body of evidence to support this. Maybe I am just an old country doctor, but to help me convince others to support using tax dollars to direct resources at the root causes of ACEs, I wanted to see the data, and make my own conclusions. Last year in the August 2022 issue of our San Antonio Medicine magazine, Drs. Edward Dick and Kristen Plastino co-authored an article on TIC and provided resources. Here in San Antonio, the South Texas TraumaInformed Care Consortium (STTICC) is active and willing to help.
I wonder how SDOH intersects with TIC, and how can this inform clinical care? Is TIC an evolution of the concept of SDOHs, or are they separate structural frames of reference? I have noted that some agencies involved with TIC have recently shifted the focus from ACEs
8 SAN ANTONIO MEDICINE • March 2023 PRESIDENT’S MESSAGE
to resiliency factors that protect against the long-term health problems associated with higher ACEs scores on screening tools. I hope this does not portend a similar fate for this newer effort. Have the leaders of the TIC movement realized that the concept is too large for people to wrap their minds around, especially when it requires collaboration to fund a response? We will see how this plays out.
Specifically, to address early childhood development, Medicaid expansion would meet some needs of the most at risk children in Texas. Just ensuring that Medicaid coverage is extended from 6 months to 12 months for both the newborn and the mother is a step in the right direction. As the legislative season continues, let us keep this in mind for what it represents as a worthy investment. Our advocacy voice, as a profession, can easily be lent to this effort
Coming in Part II: Healing the inner child and inner child work. Can an app help people do this without actual face to face interaction with a therapist/counselor?
References
1. United States, US Department of Health and Human Services, Centers for Medicare and Medicaid Services. (2017, September 05). Accountable Health Communities Model. https:/ /innovation.cms.gov/initiatives/ahcm.
2. Office of Disease Prevention and Health Promotion. Healthy People 2030. U.S. Department of Health and Human Services. https://health.gov/healthypeople
John J. Nava, MD, is the 2023 President of the Bexar County Medical Society. He is interested in Primary Care, Clinical Research and Public Health.

PRESIDENT’S MESSAGE
Visit us at www.bcms.org 9
Bexar County Medical Society Alliance
By Cheryl Pierce-Szender, Alliance Co-President
We had our first baby in December 2007. High blood pressure, proteinuria, and clonus at my 38-week checkup bought me an immediate transfer via wheelchair across the street to labor and delivery. I was "fortunate" enough to be sufficiently sick that I got one of the last beds, soon after, the Alaska Native Medical Center went on diversion during a snowstorm. I heard other women were laboring in triage and even in the hallways.
We hadn't fully prepared to bring our baby home. Though I hadn't practiced any relaxation techniques, hadn't packed a bag, didn't have a proper nursery set up, and my mom had to run to the store for smaller onesies to take our baby home in, we felt ready. We foolishly thought of welcoming our baby into the world as the finish line.
The birth was the culmination of years of effort. Over a year and a half of infertility. Over five and a half hours of surgery to remove large bilateral endometriomas, implants and adhesions from stage four endometriosis. Diagnostic tests, procedures and countless injections for IVF. Then cholestasis and preeclampsia. I had learned to medically advocate for myself to get treatment every step of the way. We had overcome all these obstacles we finally had our baby.
It never occurred to us that she might be sick.
I don't know if there's any scientific proof of a mother's intuition. My background is in structural engineering, not medicine. I'd never even been around babies before I gave birth to my own, but I knew something wasn't right. Babies spit up, but surely not that much. Having to hold my baby all night long on a bed covered in towels couldn't be normal. My husband was a medical student, usually either at the hospital or studying, so I was the one home with her and the one to raise the first alarm bells. Well-meaning family and friends tried to reassure me that everything was fine.
Most likely our baby had reflux and while painful for her and frustrating for us, some medication would relieve most of the issue. But her pediatrician listened to and believed the two new and young parents and or-
dered a barium swallow test. I stood outside the radiology suite, sick to my stomach worrying that I might be correct, that our beautiful, barely 10-pound baby might have something wrong. My then-inexperienced, medical student husband immediately recognized our baby's malrotated intestine in real time.
Our daughter was 65 days old when her surgeon performed a Ladd's procedure (untwisting her intestines, removing her appendix, and repositioning her small intestine and colon). In the middle of the surgery, a resident found us and excitedly displayed a picture of our baby's intestines. The doctors also found a duplication at the cecum which required a resection. I spent the next several days in the hospital with her, holding her tiny hands in a fruitless effort to stop her from repeatedly pulling the IVs out of her forehead and legs.
Our son's gastrointestinal issues have been harder to diagnose. We knew when he turned one and went from our best eater to refusing food altogether that something was wrong. His first real word was "hurt," said while pointing to his stomach. We wished we still lived near our daughter's pediatrician, the one who had listened to us and ordered the barium swallow test.
Luckily when we moved back to San Antonio after my husband’s fellowship, we were able to establish our son with a wonderful pediatric gastroenterologist. He was two when he had a Nissen fundoplication and Gtube placement. We're still struggling with his various medical issues, but are thankful that his team takes our concerns into real consideration.
Having four kids who have endured pediatric NICU stays, polycystic kidney disease diagnoses, an early autism diagnosis, multiple surgeries and diagnoses. These experiences have taught me the value of always trust my instincts and advocate our children. We are forever grateful to the doctors and nurses.
Cheryl is the co-President of the 2023 BCMS Alliance. She previously served as Treasurer.
10 SAN ANTONIO MEDICINE • March 2023 BCMS ALLIANCE

Helping Children with Cerebral Palsy Thrive
 By Alice K. Gong, MD
By Alice K. Gong, MD
Cerebral Palsy (CP), the most common motor disability of childhood, is a group of conditions that affects a child’s ability to move and maintain balance and posture. CP can be caused by abnormal brain development or damage to the developing brain of the fetus and newborn. It literally means that the brain has problems connecting with the muscles of the body. The symptoms are variable, ranging from one who walks awkwardly to a person who needs specialized equipment to ambulate to someone who cannot walk and need lifelong care.
William Osler, the father of modern medicine, first introduced the term “cerebral palsies” to describe a group of varied neurological disturbances in children. Not until 2007 did medicine come to a consensus definition, i.e., a group of permanent disorders of the development of movement and posture, causing activity limitation that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain.1
Typically, CP is not diagnosed until about 18 months of age, because the signs and symptoms are not always obvious.3 There are risk factors such as prematurity, especially those whose neonatal course had been compromised by intraventricular hemorrhages (IVH), periventricular leukodystrophy (PVL), or encephalomalacia that accompanies those born exposed to hypoxic-ischemic encephalopathy (HIE). Without biomarkers, physicians must rely upon delays of key milestones which have a broad range of entry in childhood neurodevelopment. Assessments of posture, reflexes and muscle tone can be difficult at times in infants. There was also the need to rule out other causes of findings and a fear of a false positive. Infants have developing voluntary motor possibilities, making it difficult to determine if dysfunction may be permanent. The discussion of the diagnosis with families is not an easy one. Despite all of these, the need for early diagnosis had been recognized for a long time so as to implement early intervention, especially with early brain plasticity.
Early screening for CP for high-risk newborns has gain clinical traction since the publication of the International Clinical Practice Diagnostic Guidelines.2 Maître et al demonstrated a decreased from 19.5 months to 9.5 months for CP diagnosis using Hammersmith Infant Neurologic Examination (HINE), General Movements Assessment (GMA) and standardized assessment of motor function.4
In 2022, American Academy of Pediatrics (AAP) published guidance for a primary care medical home for children with CP.5 Physicians who care for children should be familiar with the definition, manifestations and management of CP. Risk factors for this motor disability include intrauterine and perinatal infections, IVH, HIE, stroke, brain malformations and certain genetic disorders. These causes are permanent and nonprogressive in that the brain disruption does not worsen. The physical manifestations of postural and motion problems do change over time as the child grows and develops. A common system for describing the gross motor abilities is the Gross Motor Functional Classification System (GMFCS). Although CP is a motor disorder,
12 SAN ANTONIO MEDICINE • March 2023 CHILDREN’S HEALTH
difficulties in other areas of the nervous system and other comorbidities may occur. Common problems include seizures, cognitive, communication disabilities, gastrointestinal and urinary problems as well as pain. The primary care physician’s responsibility is to integrate and coordinate care across multiple sub-specialists while helping families with resources such as early childhood intervention (ECI) for management and therapies, insurance, transition to education systems, and others to help the child thrive.
Preterm birth is a risk factor to about half of the people with CP. In addition to the disparate social factors that contribute to prematurity, population studies reveal that CP is more common among children who are non-Hispanic, black and in families of lower socioeconomic status. As physicians we should be attuned to implicit biases and barriers to screening, identification, treatment, and support for those whose lives are also impacted by social determinates of health.
Over half of children with CP are born at term and do not have identifiable neonatal risk factors making early diagnosis challenging. Rouabhi et al published a prognostic tool for low-risk term newborns using the Canadian Cerebral Palsy Registry with data from the Alberta Pregnancy Outcomes and Nutritional study for controls.6 In their casecontrol study, they were able to develop a prognostic model using 12 clinical variables that identified 2.4-fold more cases with CP than would have if presented with encephalopathy. This tool can be accessed at: https://jamanetwork.com/journals/jamapediatrics/fullarticle/ 2800550?utm_campaign=articlePDF&utm_medium=articlePDFlink&utm_source=articlePDF&utm_content=jamapediatrics. 2022.5177, Supplement 2. This tool is simple, uses information that is routinely collected, and can be quickly calculated in the author’s Excel sheet that is shared. The screening tool found that a threshold greater than 0.3 had sensitivity of 65% and specificity of 71%. These newborns with normal exams should be referred for evaluation with HINE and standardized evaluation of motor function. Monica et al published a new algorithm for early diagnosis of CP.7
Early active movement and intervention helps infants continue with brain development and refinement of cortical connections and dedicated function. Infants’ developing motor behavior help them discover and interact with their surroundings that will control, grow, and develop the neuromuscular system. Early specific interventions have been shown to expand neuroplasticity and decrease deleterious changes to muscle and bone growth and developmental. A medical home for children is CP should be standard care to optimized brain neuroplasticity, prevent complications and enhance parents’ well-being.
References
1. Rosenbaum P, Paneth N, Leviton A, et al. A report: the definition and classification of cerebral palsy April 2006 [published correction
appears in Dev Med Child Neurol. 2007;49(6):480]. Dev Med Child Neurol Suppl. 2007;109:8–14.
2. Novak I, Morgan C, Adde L, Blackman J, Boyd RN, BrunstromHernandez J, Cioni G, Damiano D, Darrah J, Eliasson AC, de Vries LS, Einspieler C, Fahey M, Fehlings D, Ferriero DM, Fetters L, Fiori S, Forssberg H, Gordon AM, Greaves S, Guzzetta A, Hadders-Algra M, Harbourne R, Kakooza-Mwesige A, Karlsson P, Krumlinde-Sundholm L, Latal B, Loughran-Fowlds A, Maitre N, McIntyre S, Noritz G, Pennington L, Romeo DM, Shepherd R, Spittle AJ, Thornton M, Valentine J, Walker K, White R, Badawi N. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy: Advances in Diagnosis and Treatment. JAMA Pediatr. 2017 Sep 1;171(9):897-907. doi: 10.1001/jamapediatrics.2017.1689. Erratum in: JAMA Pediatr. 2017 Sep 1;171(9):919. PMID: 28715518; PMCID: PMC9641643.
3. te Velde A, Morgan C, Novak I, Tantsis E, Badawi N. Early Diagnosis and Classification of Cerebral Palsy: An Historical Perspective and Barriers to an Early Diagnosis. J Clin Med. 2019 Oct 3;8(10):1599. doi: 10.3390/jcm8101599. PMID: 31623303; PMCID: PMC6832653.
4. Maitre NL, Burton VJ, Duncan AF, et al. Network Implementation of Guideline for Early Detection Decreases Age at Cerebral Palsy Diagnosis. Pediatrics. 2020;145(5):e20192126
5. Noritz G, Davidson L, Steingass K, et al; AAP Council on Children With Disabilities, THE AMERICAN ACADEMY FOR CEREBRAL PALSY AND DEVELOPMENTAL MEDICINE. Providing a Primary Care Medical Home for Children and Youth With Cerebral Palsy. Pediatrics. 2022;150(6):e2022060055

6. Rouabhi A, Husein N, Dewey D, et al. Development of a Bedside Tool to Predict the Diagnosis of Cerebral Palsy in Term-Born Neonates. JAMA Pediatr. Published online January 17, 2023. doi:10.1001/jamapediatrics.2022.5177
7. Monica T, Catherine M, Iona N. New Screening Tool for TermBorn Infants Enables Update to the Clinical Practice Guideline for Early Diagnosis of Cerebral Palsy. JAMA Pediatr. Published online January 17, 2023. doi:10.1001/jamapediatrics.2022.5189
Alice K. Gong, MD is Professor of Pediatrics at UT Health, San Antonio. In that role, Dr. Gong also holds the William and Rita Head Distinguished Chair in Developmental and Environmental Neonatology. She is also the Medical Director of the Premiere Program, a follow through clinic for Neonatal Intensive Care Survivors. Dr. Gong is the president-elect for Texas Pediatric Society. She lives in San Antonio with her husband, Richard and is most proud of her three adult children and four grandchildren.
Visit us at www.bcms.org 13
CHILDREN’S HEALTH
Pediatric Mental Health: Issues, Treatments and Challenges
By Grizelda Anguiano, MD
Wouldn’t it be nice if patients could arrive to see their primary provider with a classic presentation of a problem, start the recommended treatment, and then have the patient return with the presenting complaint resolved two weeks later! Unfortunately, mental health does not work like this and even less when you have children involved. The presenting symptoms may be headaches, vision changes, difficulty swallowing, chest pain, shortness of breath, nausea, vomiting, abdominal pain, numbness, sleep disturbances and so many others or all of these at once. Often, the time constraints that providers have with their schedules make it nearly impossible to give patients the well-deserved time to determine the cause or put the puzzle together. With experience, it gets easier to figure
out the diagnosis and appropriate treatment plans, but that is the easy part. The dilemma really comes with getting patients in for the needed treatment which, in many cases, is psychotherapy. Often physicians provide medication as a “Band-Aid” while they wait for the “real medication” of psychotherapy.
Although now it is more common for celebrities to discuss their own mental health challenges, for many, a mental health stigma prevents early presentations. The COVID pandemic forced society to isolate and ultimately contributed to the spike in mental health emergencies. The CDC noted that, in 2020, suicide was the 2nd leading cause of death for children between the ages of 10 and 14.1 The American Academy of Pediatrics (AAP) noted that 1 in 5 children in the US have a

14 SAN ANTONIO MEDICINE • March 2023 CHILDREN’S HEALTH
diagnosable mental health disorder and only 20% of those that seek treatment get the services needed.2
The wait time to get a patient into therapy or a prescribing mental health provider can take months which creates the unfortunate barricade to needed treatment. In October 2021, the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry (AACAP), and the Children’s Hospital Association (CHA) collaboratively declared a National State of Emergency in Children’s Mental Health.3
So, what do we do? How can we help change the direction of these numbers? The answer: awareness and acceptance. Though not entirely sufficient, awareness of what we can do and acceptance of taking that responsibility is pivotal. We can gain the comfort in assessing, diagnosing, and prescribing medications for the most common presenting diagnosis such as anxiety and depression, while having a plan in place that
includes resources for our patients to get the momentum going in the right direction as soon as possible. This will not only decompress the demands on psychiatric providers to enable availability for the more complex patients, but will empower us in the comfort in providing the care in the moment which can literally save lives.
In 2019 the AAP published an article, “Mental Health Competencies for Pediatric Practice”, which outlined steps toward achieving competencies which will broaden the ability and comfort to provide the needed services as a pediatric provider.4 There have been amazing programs such as the Patient-Centered Mental Health in Pediatric Primary Care, provided by The REACH Institute, whose mission is to provide evidence-based training that will empower primary care providers to make the needed contributions to influence the change that is possible.

Further support has been made available by federal funding through the Child Psychiatry Access Network (CPAN) program, which is free for pediatric providers to obtain on the spot consultations, training and support with care coordination. Utilizing all these resources alter the direction of care that we can provide to be participants in the improvement of mental health care and life saving encounters.
Improving the comfort in providing this care can help decrease the reservations we may have in asking about these diagnoses, promote discussions during all visits about the available support through primary providers, and provide reassurance that anxiety and depression are treatable conditions. Emphasizing that prompt discussions promote quicker recoveries, and that medication does not always have to be part of the current or lifelong treatment plan can provide the encouragement that families need to present with these concerns.
We can do this together.
Learn more about Dr. Anguiano’s Services & Programs www.anchoredtx.com
Resources
1. https://www.cdc.gov/suicide/facts/index.html
2. https://www.aap.org/en/patient-care/mental-health-initiatives/
3. https://www.aap.org/en/advocacy/child-and-adolescent-healthymental-development/aap-aacap-cha-declaration-of-a-nationalemergency-in-child-and-adolescent-mental-health/
4. https://publications.aap.org/pediatrics/article/144/5/e2019 2757/38256/Mental-Health-Competencies-for-Pediatric-Practice
Grizelda Anguiano, MD is a board-certified general pediatrician, specializing in pediatric mental health. She is the founder of Anchored, a pediatric mental health practice providing medication management, parent training and life coaching. She is also a member of the Bexar County Medical Society (BCMS).

Visit us at www.bcms.org 15
CHILDREN’S HEALTH
Understanding Adolescent Eating Disorders
 By Noel C. Ales, DO
By Noel C. Ales, DO
A
norexia has the highest mortality rate of any mental illness. One in five anorexic deaths is by suicide, and it is the third most common chronic illness among adolescents. Over the past decade, the incidence of eating disorders (EDs), anorexia nervosa (AN), bulimia nervosa (BN), and binge eating disorder (BED), has increased among children under 12 and as young as 5, with a hospital admission increase of 119%. The true incidence may be skewed due to under diagnosis, a scarcity of studies, and the new DSM V which includes patients who previously would not have met diagnostic criteria. The general prevalence in adolescents of AN, BN, and BED are 0.3%, 0.9%, and 1.6% respectively, with a mean age of onset of 12.5 years and an overall prevalence of 2.7%. Unfortunately, EDs continue to be under and misdiagnosed by physicians. With a fivefold increase in mortality risk for all EDs, it is imperative that physicians queue into the subtle signs and symptoms of eating disorders in children to diagnose these patients at disease onset maximizing their chance of full recovery. The misdiagnosis of EDs is multifactorial. Patients with EDs are often secretive due to shame or fear and will not disclose their behaviors. Others take pride in their ED and do not see the disorder as problematic.
Additionally, the medical complications of anorexia are often silent and present late in the disease process. Electrocardiogram (EKG) and laboratory values are often normal until a patient is near death. Other symptoms such as constipation, orthostasis, bradycardia, dry skin, hair loss, amenorrhea, fatigue, and inattention mimic other disorders and are sent for subspecialist
evaluation, or treated empirically as common childhood ailments. This leads to a litany of diagnoses rather than the unifying diagnosis of an eating disorder. A thorough review of a child’s growth charts should be done at every visit while the patient is present. Any subtle changes in weight, stature, or BMI should lead the physician to question the patient further regarding EDs. Patients with slight changes should be reevaluated within a month and referred for further care with a dietician and mental health provider. Societal norms, cultural bias towards thinness, and genetics all play a role in the masking of eating disorders making an accurate diagnosis more complicated. If a child appears thin and looks like their thin mother who secretly has an ED, healthcare providers may assume a family resemblance and not pursue specific
CHILDREN’S HEALTH
16 SAN ANTONIO MEDICINE • March 2023
questioning. The parent with the ED will not be forthcoming with eating disordered behaviors, 50% - 80% of the risk for AN is genetic. If there is a family history of an ED, a patient is 7-12 times more likely to develop one. Children diagnosed with chronic illness, such as insulindependent diabetes mellitus or mental illness are also at increased risk. Questioning the family history beyond hypertension, diabetes and cancer is paramount. Physicians should ask about a family history of EDs, mental illness and weight loss. If these are present, physicians should pursue targeted questions about personal and familial exercise habits, diets, food rules and weight standards. Unless a physician asks, dangerous behaviors will persist until a significant medical complication occurs. Physician bias and the previous misconception that EDs are diseases of non-Hispanic white, affluent adolescent girls, gymnasts, wrestlers, and ballerinas puts adolescents at risk for misdiagnosis. Current research demonstrates eating disorder behaviors in all racial and ethnic groups, lower socioeconomic classes and males. There are also increased rates of disordered eating in sexual minority youth with up to 16 times the rate of EDs than their cisgender, heterosexual female peers. The recognition and consideration of EDs in these populations would significantly decrease the morbidity and mortality of EDs. Patients in larger bodies are a unique population that deserves special consideration. These adolescents experience damaging influences through media, adults, and peers resulting in depression, anxiety and poor self-image. Weight stigma results in these patients being overlooked or triggered when health care providers stress weight loss, Initial attempts to lose weight may progress to severe dietary restriction, starvation, self-induced vomiting, diet pill and laxative abuse. Patients with BMIs in the normal to obese range may have significant EDs and are at risk for the same severe medical complications as their underweight peers. A study of adolescents seeking treatment of an ED states that 36.7% had a previous weight greater than the 85th percentile for age and sex. To prevent a delay in diagnosis for these patients, clinicians should offer a sensitive approach that allots appropriate time to address the health concerns of obesity and EDs. Patients in larger bodies or with high BMIs should be referred to registered dieticians trained in EDs who know the science behind weight records, can recommend and monitor weight loss or gain. In combination with mental health therapy, family therapy, and medical management, these patients have improved outcomes. The medical outcome data is clear; early detection, diagnosis, and intervention in EDs leads to better prognosis and even full recovery in adolescent patients. Most medical complications are re -
versible, and this population can grow into adulthood without negative sequalae. More advanced cases of ED are not as likely to achieve recovery and face long-term health consequences such as osteoporosis, stunted growth, cognitive dysfunction, chronic gastrointestinal issues, persistent mental illness and frequent relapse. Primary care physicians with high indexes of suspicion and knowledge of eating disorders are key to the diagnosis and play a pivotal role in the treatment of ED patients. Working closely with nutritional experts and mental health professionals to break down the stigma of EDs and provide the best treatment to those affected will improve future outcomes for this underrecognized patient population.
References
1. Golden, N. H., Schneider, M., Wood, C., COMMITTEE ON NUTRITION, COMMITTEE ON ADOLESCENCE, & SECTION ON OBESITY (2016). Preventing Obesity and Eating Disorders in Adolescents. Pediatrics, 138(3), e20161649. https://doi.org/10.1542/peds.2016-1649
2. Murray, S. B., Ganson, K. T., Chu, J., Jann, K., & Nagata, J. M. (2022). The Prevalence of Preadolescent Eating Disorders in the United States. The Journal of adolescent health: official publication of the Society for Adolescent Medicine, 70(5), 825–828. https://doi.org/10.1016/j.jadohealth.2021.11.031

3. Muhlheim, L. (2015, July 12). 9 Essential Facts About Eating Disorders. Verywell Mind; Verywellmind. https://www.verywellmind.com/eating-disorder-myths-and-truths1138395
4. Campbell, K., & Peebles, R. (2014). Eating disorders in children and adolescents: state of the art review. Pediatrics, 134(3), 582–592. https://doi.org/10.1542/peds.2014-019
5. Hornberger, L. L., Lane, M. A., & COMMITTEE ON ADOLESCENCE (2021). Identification and Management of Eating Disorders in Children and Adolescents. Pediatrics, 147(1), e2020040279. https://doi.org/10.1542/peds.2020-040279
6. Mairs, R., & Nicholls, D. (2016). Assessment and treatment of eating disorders in children and adolescents. Archives of disease in childhood, 101(12), 1168–1175. https://doi.org/10.1136/archdischild-2015-309481
7. O'Brien, K. M., Whelan, D. R., Sandler, D. P., Hall, J. E., & Weinberg, C. R. (2017). Predictors and long-term health outcomes of eating disorders. PloS one, 12(7), e0181104. https://doi.org/10.1371/journal.pone.0181104
Noel C. Ales, DO is a Board-Certified Internist and the staff physician at Esperanza Eating Disorder Center in San Antonio, Texas. She is a member of the Bexar County Medical Society (BCMS).

CHILDREN’S HEALTH Visit us at www.bcms.org 17
Concerning Youth and Vaccination Hesitancy
By Bethanne Bradshaw and Marcy Snyder
The classic picture of a rebellious teen generally entails breaking curfew or skipping class, but in a post-Covid world, rebellion has taken on a new form. Nicolas Montero, a 16-year-old Pennsylvania junior, was at odds with his anti-vax parents and opted to go to Philadelphia where the city permits children 11 and up to be vaccinated without parental consent. In Louisiana, a mother filed a complaint after her 16-year-old son received the Covid vaccine at a school-hosted mobile vaccination session. The consent form he had completed did not require the signature of a parent. Both of these cases raise an essential question: Are all minors clamoring to be vaccinated, and what role do teens want to play in their health?
Stories like the one above, have made for splashy news coverage, but are they representative of teenagers’ views on vaccination? The data is somewhat mixed on this point. Assuming a teen is undergoing the routine vaccination schedule that is recommended to all US teenagers (age 11+) with average risk levels, they need to receive two doses of human papillomavirus Vaccines (HPV), a yearly influenza vaccine, a twodose series of the meningococcal vaccine, and a Tdap vaccine with a booster dose (CDC vaccination schedule). However, only about 80% of teens make it all the way through this series. According to a recent survey by UNITY (a nonprofit dedicated to increasing vaccination rates in America), 23% of people aged 14-24 believe that vaccines are “only for babies” and 34% don’t know how vaccination
helps them. 47% of teens do not like talking to their pediatricians or health care providers at all, which may be a cause for this information gap.
The long-term sequelae of avoiding vaccination can be deadly. HPV is a sexually transmitted disease that has become so common that almost all sexually active men and women will be exposed to it. The majority of infected people will be asymptomatic and heal on their own; but long-term exposure to an oncogenic strain can result in cancer. HPV is considered to be the cause of 90% of all cervical and anal cancers. It is also the cause of a variety of oropharyngeal, vulvar, vaginal and penile cancers. In the United States, an estimated 39,000 HPV-related cancers are diagnosed each year. 28,500 of these cancers are directly connected to HPV subtypes that may be prevented with the 9-valent vaccination. 10 The population that is most susceptible to developing an HPV-related malignancy is young adult and childhood cancer survivors. Despite being three times more likely than the general population to acquire a secondary neoplasm later in life, this demographic is vaccinated less than the general public.7

Interestingly, while it is broadly known that the vaccine hesitancy is a problem for uptake of the Covid19 vaccine, the pandemic impacted all vaccination rates negatively.
After March of 2020, visits to pediatricians plummeted and many children fell through the cracks of the system and didn’t receive their routine vaccinations.1 Vaccination rates have since returned to
CHILDREN’S HEALTH
18 SAN ANTONIO MEDICINE • March 2023
pre-pandemic levels, however the proportion of all children who are up to date on their vaccinations overall is down.1 While vaccine hesitancy due to misinformation is a massive problem, there are likely many teens who didn’t get vaccinated simply because they didn’t see their doctors as they might have otherwise during the pandemic. Given this situation, it is important to alert teenagers and their families to check with their pediatricians to make sure they are up to date on all of their vaccines, not just their recommended covid shots.
The covid vaccine is not currently considered part of the CDC’s routine vaccination schedule for children, though it is strongly recommended that teenagers receive the vaccine. Only about 68% of people ages 14-24 have received at least one dose of the covid vaccine, meaning its uptake is significantly lower than that of routine immunizations. 3 This is lower than the roughly 80% of teenagers who receive all of their recommended vaccines, and at least some of this discrepancy is likely due to vaccine misinformation posted by TikTokers and social media moms aimed at teens. Common myths targeted at teens included statements that it would harm someone’s future fertility or affect their journey through puberty adversely. Interestingly, many of the most pervasive myths about covid stem from facts or at least half-truths. It is true that many women reported changes to their periods after the vaccine, but it has not been demonstrated to change someone’s fertility.
Despite the pervasive myths and personal anecdotes shared via TikTok and Facebook, not all teens are turning to these platforms to receive information pertinent to their health. In fact, some teenagers have taken to the internet to encourage others to take responsibility for their own health. Kelly Danielpour, an undergraduate student at Stanford, created VaxTeen, a website designed to educate teenagers and young adults on the dangerous tide of misinformation, and encourage unvaccinated youth to catch up on the vaccines they are missing. The website includes resources that help teens to engage in difficult conversations with anti-vax parents and links to minor vaccination consent laws in each state. It even includes a link to a site that allows people to practice having vaccination conversations with skeptics.

Social media and the internet are not necessarily the enemy to increasing numbers of teenage vaccination. A hallmark of adolescence is the start of independent decision making, and equipping teens with the information they need to make informed decisions on their health, as well as the resources to carry out those decisions is the best way to raise up a generation of happier and healthier young people.
References
1. Brian P. Jenssen, M. D. (2022, January 1). Covid-19 and routine childhood vaccinations. JAMA Pediatrics. Retrieved January 17, 2023, from https://jamanetwork.com/journals/jamapediatrics/ fullarticle/2784889
2. Centers for Disease Control and Prevention. (2022, February 17). Birth-18 years immunization schedule. Centers for Disease Control and Prevention. Retrieved January 17, 2023, from https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html
3. Children and covid-19 vaccination trends. Home. (n.d.). Retrieved January 17, 2023, from https://www.aap.org/en/pages/2019novel-coronavirus-covid-19-infections/children-and-covid-19-vaccination-trends/
4. Daley, K. (n.d.). La. Mother threatens lawsuit after teen son gets covid-19 vaccine at school without permission. https://www.fox19.com. Retrieved January 17, 2023, from https://www.fox19.com/2021/10/25/la-mother-threatens-lawsuit-after-teen-son-vaccinated-against-covid-19-school-withoutpermission/

5. Danielpour, K. (n.d.). VaxTeen. Retrieved January 17, 2023, from https://www.vaxteen.org/
6. Feldman, N. (2022, February 16). This 16-year-old wanted to get the COVID vaccine. he had to hide it from his parents. NPR. Retrieved January 17, 2023, from https://www.npr.org/ sections/health-shots/2022/02/16/1074191656/this-16-year-oldwanted-to-get-the-covid-vaccine-he-had-to-hide-it-from-his-pare
7. Henderson TO, Fowler BW, Hamann HA, Nathan PC, Whitton J, Leisenring WM et al. Subsequent malignant neoplasms in the Childhood Cancer Survivor Study: Occurrence of cancer types in which human papillomavirus is an established etiologic risk factor. Cancer 2022; 128: 373-382.
8. Pandemic myths are all over social media-and they're dangerous for kids. National Geographic. (2021, October 6). Retrieved January 17, 2023, from https://www.nationalgeographic.co.uk/family/2021/10/pandemic-myths-are-all-over-social-media-and-theyr e-dangerous-for-kids
9. Vaccine Resource Hub. (n.d.). Retrieved January 17, 2023, from https://vaccineresourcehub.org
10. Viens LJ, Henley SJ, Watson M, Markowitz LE, Thomas CC, Thompson TD et al. Human Papillomavirus-Associated Cancers - United States, 2008-2012. MMWR Morb Mortal Wkly Rep 2016; 65: 661-666.
CHILDREN’S HEALTH Visit us at www.bcms.org 19
Bethanne Bradshaw and Marcy Snyder are medical students at the Long School of Medicine and are the Co-Presidents of the Pediatrics Interest Group.
Nutrition Awareness Month–The Science Behind Eating the Rainbow
By Julia D’Isabella, Alexandra Fekete, Abigail Joy Garcia, Deonte Jefferson and Bridgette Kielhack
Childhood obesity has become a global public health crisis that poses many physical, emotional, and financial burdens on those affected.1 In an effort to reduce the health impact of childhood obesity, the American Academy of Pediatrics (AAP) recommends that pediatricians should offer weight loss pharmacotherapy and bariatric surgery to treat obesity.2 While these may be considered effective methods for treatment, maintenance of long-term, healthy weight is not guaranteed.
Although obesity is complex, it is reversible and preventable. In this article, we will address prevention through dietary changes by discussing the nutritional aspect of whole foods, using example colors from a teaching tool called “Eat the Rainbow.” This tool can be used in pediatric care settings to encourage healthy eating from a young age and to create long-term healthy habits throughout adulthood to prevent obesity and associated comorbidities such as hypertension, cardiovascular disease and cancer.3
Eat the Rainbow Red - Orange - Yellow
Lycopene is a non-provitamin A carotenoid that is responsible for the red hue seen in foods such as tomatoes and strawberries.4 Lycopene’s benefits include antibiotic, anti-inflammatory, antioxidative, cardiovascular, and immunostimulating effects in cells.5 Red beets have also been found to improve endothelial function by increasing nitric oxide precursors which reduce arterial stiffness and lowers blood pressure.6,7 Red fruits have a two-fold effect at mealtime due to the vibrant color adding flare to the plate as well as lowering the risk of cardiovascular disease and preventing comorbidities later in life.
Orange and yellow foods such as carrots, oranges, and bell peppers contain similar antioxidant properties as red-pigmented foods, but are also highly nutritious in various carotenoids such as α-carotene, βcarotene, β-cryptoxanthin, lutein and zeaxanthin.11 Carotenoids’ effects on adipose tissue include inhibiting adipogenesis via down-regulating adipogenic transcription factors, and thus deficiencies in carotenoids have been linked as a risk factor for obesity.12,13 Higher pro-vitamin A carotenoids, especially α and β-carotene serum levels have been associated with lower risk of obesity in children.14
Green
Green cruciferous vegetables are packed with fiber which helps lower one’s risk for cardiovascular disease by reducing LDL levels, and also helps regulate satiety levels.8 Inflammation is implicated in many disease states including obesity, hypertension, cardiovascular disease, autoimmune disorders and cancer. Cruciferous vegetables contain a
phytochemical called sulforaphane which has powerful antioxidant, anti-inflammatory and anti-cancer properties.9 For children who do not like the texture or bitterness of cruciferous vegetables, broccoli sprouts are 20-50x more potent than broccoli and may be more palatable for children.10 Also, steaming kale, broccoli, or bok choy for 1-3 minutes, and then having children create their own dressing is an engaging and empowering way for children to get creative and curious in the kitchen.
Blue - Purple
Foods of blue-purple color such as blueberries, blackberries, eggplant, and purple carrots contain important polyphenols called anthocyanins which have been found to have antioxidant, glucoregulatory, anti-inflammatory, cardioprotective and neuroprotective effects.15,16,17 Multiple studies have found that anthocyanins also help lower serum triglyceride and cholesterol levels, increase serum HDL levels, decrease blood pressure and prevent obesity.15,18 Anthocyanins and other beneficial nutrients are mostly found in the colorful blue-purple part of the fruit or vegetable, so be sure to encourage pediatric patients to eat every bite of these vibrant blue-purple foods.
Brown
Whole grains such as oat, quinoa, and barley are associated with a 21% lower risk of cardiovascular events.19,20 Additionally, consuming almonds can decrease cholesterol levels.21 Because the process of atherosclerosis begins in the first decade of life, whole grains and almonds may decrease pediatric patients’ risk of cardiovascular events later in life.22 Furthermore, beans contain a natural source of magnesium.20 Low dietary magnesium intake has been shown to correlate strongly with high blood pressure.23,20,24 Because pediatric hypertension is a leading determinant of cardiovascular disease in adults, increasing intake of steamed or boiled beans with no additional salt or fat may reduce incidence of pediatric hypertension.22,24,25
Additionally, pinto beans, lentils, and black beans provide a better source of protein than animal sources because they do not include the saturated fats, cholesterol and higher calorie count.26 Patients who consume these plant proteins would also gain the added benefits of fiber, phytonutrients, vitamins and minerals.27 Therefore, consuming more plant sources of protein than animal sources in childhood may help prevent cardiovascular diseases and dyslipidemia.
Conclusion
Children learn by example. Helping children establish healthy eating patterns that continue into adulthood should begin with simpli-
CHILDREN’S HEALTH
20 SAN ANTONIO MEDICINE • March 2023
fied approaches, like the “Eating the Rainbow” color categorization, that focuses on nutrient-dense whole foods with benefits for the entire family.
References
1. Ling, J., Chen, S., Zahry, N. R., & Kao, T. A. (2022). Economic burden of childhood overweight and obesity: A systematic review and meta‐analysis. Obesity Reviews.https://doi.org/10.1111/ obr.13535.
2. Hampl, S. E., Hassink, S. G., Skinner, A. C., Armstrong, S. C., Barlow, S. E., Bolling, C. F., Edwards, K. A. C., Eneli, I., Hamre, R., Joseph, M. M., Lunsford, D., Mendonca, E., Michalsky, M. P., Mirza, N., Ochoa, E. R., Sharifi, M., Staiano, A. E., Weedn, A. E., Flinn, S. K., . . . Okechukwu, K. (2023, January 9). Clinical Practice Guideline for the Evaluation and Treatment of Children and Adolescents With Obesity. American Academy of Pediatrics. https://publications.aap.org/pediatrics/article/doi/ 10.1542/peds.2022-060640/190443/Clinical-Practice-Guideline-for-the-Evaluation-and?autologincheck=redirected.
3. Blumfield, M., Mayr, H., De Vlieger, N., Abbott, K., Starck, C., Fayet-Moore, F., & Marshall, S. (2022). Should We “Eat a Rainbow”? An Umbrella Review of the Health Effects of Colorful Bioactive Pigments in Fruits and Vegetables. Molecules, 27(13), 4061. https://doi.org/ 10.3390/molecules27134061.
4. Story, E. N., Kopec, R. E., Schwartz, S. J., & Harris, G. K. (2010). An Update on the Health Effects of Tomato Lycopene. Annual Review of Food Science and Technology, 1(1), 189–210. https://doi.org/10.1146/annurev.food.102308.124120.
5. Friedman, M. (2013). Anticarcinogenic, Cardioprotective, and Other Health Benefits of Tomato Compounds Lycopene, α-Tomatine, and Tomatidine in Pure Form and in Fresh and Processed Tomatoes. Journal of Agricultural and Food Chemistry, 61(40).https://pubs.acs.org/ doi/full/10.1021/jf402654e?casa_token=Q8M RkS44r7wAAAAA%3A DqCGpBljoNhGDVcbjMI3M40-WYR00cNNyuxvpCYEDuBz1wGuc KXR6QMH2N0c98sAmykgqLVCjjk0E3c.
6. Babarykin, D., Smirnova, G., Pundinsh, I., Vasiljeva, S., Krumina, G., & Agejchenko, V. (2019). Red Beet (Beta vulgaris) Impact on Human Health. Journal of Biosciences and Medicines, 7(3), 61–79. https://doi.org/10.4236/ jbm.2019.73007.
7. Baião, D. S., da Silva, D. V. T., & Paschoalin, V. M. F. (2020). Beetroot, A Remarkable Vegetable: Its Nitrate and Phytochemical Contents Can be Adjusted in Novel Formulations to Benefit Health and Support Cardiovascular Disease Therapies. Antioxidants, 9(10), 960. MDPI AG. Retrieved from http://dx.doi.org/10.3390/ antiox9100960.
8. Bazzano, L. A. (2008). Effects of soluble dietary fiber on low-density lipoprotein cholesterol and coronary heart disease risk. Current Atherosclerosis Reports, 10(6), 473–477. https://doi.org/10.1007/s11883-008-0074-3.
9. Kubo, E., Chhunchha, B., Singh, P., Sasaki, H., & Singh, D. P. (2017). Sulforaphane reactivates cellular antioxidant defense by inducing Nrf2/ARE/Prdx6 activity during aging and oxidative stress. Scientific Reports, 7(1). https://doi.org/10.1038 /s41598-017-14520-8.
10. Anft, M. & Johns Hopkins Magazine. (2008, April). A Nibble of Prevention. Johns Hopkins Magazine. Retrieved January 1, 2023, from https://pages.jh.edu/jhumag/0408web/talalay.html.
11. Higdon, J., et al. “Carotenoids.” Linus Pauling Institute, 3 Jan. 2023, https://lpi.oregonstate.edu/mic/dietary-factors/phytochemicals/ carotenoids.
12. Mounien, L., Tourniaire, F., & Landrier, J. F. (2019). Anti-Obesity Effect of Carotenoids: Direct Impact on Adipose Tissue and Adipose Tissue-Driven Indirect Effects. Nutrients, 11(7), 1562. https://doi.org/ 10.3390/nu11071562
13. Yao, N., Yan, S., Guo, Y., Wang, H., Li, X., Wang, L., Hu, W., Li, B., & Cui, W. (2021). The association between carotenoids and subjects with overweight or obesity: a systematic review and meta-analysis. Food & function, 12(11), 4768–4782. https://doi.org/10.1039/d1fo00004g
14. Tang, W., Zhan, W., Wei, M., & Chen, Q. (2022). Associations Between Different Dietary Vitamins and the Risk of Obesity in Children and Adolescents: A Machine
Learning Approach. Frontiers in endocrinology, 12, 816975. https://doi.org/ 10.3389/fendo.2021.816975
15. Greger, M.; Stone, G. (2015). How Not to Die. Flatiron Books. Kindle Edition.
16. Kalt, W., Cassidy, A., Howard, L. R., Krikorian, R., Stull, A. J., Tremblay, F., Zamora-Ros R. (2020). Recent Research on the Health Benefits of Blueberries and Their Anthocyanins, Advances in Nutrition, Volume 11, Issue 2, Pages 224–236, https://doi.org/10.1093/advances/nmz065.
17. Pratt, S. G., Matthews, K. (2005). SuperFoods HealthStyle (pp. 190-193). HarperCollins e-books. Kindle Edition.
18. Sharma, M., & Kaushik, P. (2021). Biochemical Composition of Eggplant Fruits: A Review. Applied Sciences, 11(15), 7078. MDPI AG. Retrieved from http://dx.doi.org/10.3390/app11157078.
19. Mellen P.B., Walsh T.F., & Herrington D.M. (2008). Whole grain intake and cardiovascular disease: a meta-analysis. Nutrition, Metabolism and Cardiovasc Diseases, 18(4), 283-290. https://doi.org/10.1016/j.numecd. 2006.12.008
20. Rakel, D. (2018). Integrative Medicine (4th ed.). Elsevier.
21. Li S.C., Liu Y.H., Liu J.F., Chang, W.H., Chen, C.M., & Chen, C.Y.O. (2011). Almond consumption improved glycemic control and lipid profiles in patients with type 2 diabetes mellitus. Metabolism, 60(4), 474-479. https://doi.org/10.1016/j.metabol .2010.04.009
22. Candelino, M., Tagi, V.M., & Chiarelli, F. (2022). Cardiovascular risk in children: a burden for future generations. Italian Journal of Pediatrics, 48, 57. https://doi.org/10.1186/s13052-022-01250-5
23. Joffres, M.R., Reed, D.M., & Yano, K. (1987) Relationship of magnesium intake and other dietary factors to blood pressure: the Honolulu heart study. American Journal of Clinical Nutrition, 45(2), 469-475. https://doi.org/10.1093/ ajcn/45.2.469

24. Song, Y., Sesso, H.D., Manson, J.E., Cook, N.R., Buring, J.E., & Liu, S. (2006) Dietary magnesium intake and risk of incident hypertension among middle-aged and older US women in a 10-year follow-up study. American Journal of Cardiology, 98(12), 1616-1621. https://doi.org/ 10.1016/j.amjcard.2006.07.040
25. De Ferranti, S.D., Steinberger J., Ameduri, R., Baker, A., Gooding, H., Kelly, A.S., et al. (2019). Cardiovascular risk reduction in high-risk pediatric patients: a scientific statement from the american heart association. Circulation, 139(13),e603–634. https://doi.org/10.1161/CIR. 0000000 000000618
26. American College of Lifestyle Medicine. (n.d.) Plant Protein vs. Animal Protein. https://embeelifestyledocs.com/wp-content/uploads/2020/ 01/ACLM-PlantVAnimal-Protein-043019.pdf
27. Frates, B., Bonnet, J.P., Joseph, R., & Peterson, J.A. (2021). Lifestyle Medicine Handbook (2nd ed.). Healthy Learning.
Julia D’Isabella, MPH is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, class of 2025.
Alexandra Fekete, MS is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, class of 2025.


Abigail Joy Garcia is a predoctoral fellow and medical student at the University of the Incarnate Word School of Osteopathic Medicine, class of 2025.

Deonte Jefferson, MBA is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, class of 2025.
Bridgette Kielhack is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, class of 2025.

CHILDREN’S HEALTH Visit us at www.bcms.org 21
Increasing Awareness of Pressure Ulcers in Those with Physical Limitations Due to Disabilities
By Rebecca Wang and Christina Pierce
What are pressure ulcers?
Decubitus ulcers, commonly referred to as pressure ulcers or “bed sores,” are injuries of the skin or soft tissue that occur due to lack of movement and remaining in the same position for prolonged periods of time.1 Continued pressure in a specific region of the body, such as the hips, tailbone, ankles, and heels, lead to damage and injury of the skin causing pressure ulcers to develop.2 Pressure ulcers can first appear as a scrape or blister with the area of skin being discolored in comparison to the surrounding healthy skin. In those unable to feel physical pain, pressure ulcers can progress rapidly before being detected. The development of pressure ulcers can lead to infection and physical deformities which can further exacerbate underlying health conditions.
Who is at risk of developing pressure ulcers?
Those with disabilities ranging from physical limitations, mental
challenges, and psychological conditions that are unable to change positions without assistance and/or remain in bed for long periods of time are at risk of developing pressure ulcers. Specifically, patients with certain conditions that cause impaired consciousness, lack of sensation, or decreased mobility all increase the risk for developing pressure ulcers, such as patients with cardiovascular or neurologic disease, patients under prolonged anesthesia or surgery patients.1 In these patients, the lack of sensation of pain or discomfort causes them to be unaware of the developing ulcers and thus not change positions to relieve pressure from their bodies. Additionally, many of these patients are also physically incapable of moving their own bodies. Many internal factors can also increase the risk of developing pressure ulcers such as malnutrition, anemia and fever.1
Pressure ulcers are very common in elderly or debilitated populations. A study demonstrated that 83% of patients in one hospital who

CHILDREN’S HEALTH
22 SAN ANTONIO MEDICINE • March 2023
developed pressure ulcers did within five days of admission.1 Additionally, elderly patients are more at risk for developing sacral pressure ulcers with approximately two-thirds of ulcers occurring in patients 70 years and older. Another study determined that most of the patients who developed ulcers were ICU-level care patients.1 Almost 60,000 patients die each year due to complications from pressure ulcers.3
What are the complications of pressure ulcers?

A patient who remains in the same position for even two hours can create the basis of a pressure ulcer.1 With long-term pressure on blood vessels, capillary beds can become occluded and blood flow can decrease to the surrounding tissue.1 With time, the tissue can become ischemic and release toxic metabolites.1 Finally, the ulcer can develop and tissue necrosis can occur.1 External factors, such as moisture from the skin or urine in immobilized patients or friction between the skin and material, e.g., the bed or clothing can worsen the developing ulcer and lead to breakdown within the skin.1
Infection is the most common complication of pressure ulcers. Both aerobic and anaerobic bacteria can infect the open wound.1 With deeper wounds that expose bone, such as pressure ulcers on the ischium, trochanters, sacrum, or heels, severe infections such as osteomyelitis or septic arthritis can form.1 Osteomyelitis requires prolonged, high-dose antibiotics for treatment, and septic arthritis often requires surgical intervention. Additionally, in a patient population that is already debilitated, an infection can adversely affect patient recovery and be challenging to manage. Due to the catabolic nature of pressure ulcers, other complications that can develop include severe protein and fluid loss, leading to malnutrition and anemia.1
There are no clear studies documenting the exact prognosis of pressure ulcers. However, lifelong treatment of these ulcers and prevention are often required to manage debilitated patients who develop pressure ulcers.1 Pressure ulcers in the sacral region are also highly susceptible to recurrence.1 Additionally, patients with underlying chronic conditions, such as diabetes, malnutrition, hypoxia, or older age are all at increased risk of decreased wound healing.3
What is the prevention and treatment for pressure ulcers?
The most crucial treatment for pressure ulcers is prevention. The current standard of care is turning and repositioning the patient in twohour intervals to prevent prolonged pressure on any one body part.1 However, items such as pressure dispersion cushions or supportive mattresses can all be used to relieve pressure on specific body parts and prevent ulcers.1 Proper skin care and usage of urinary catheterization or rectal tubes for patients with incontinence can also prevent skin barrier damage and the development of ulcers.1 Additionally, patients at risk for developing pressure ulcers should not be bathed with harsh products such as soaps, hot water, or lotion with alcohol, as they can all dam-
age the protective skin barrier.3 Daily skin examination is essential to identify any signs of pressure ulcers.
Once a pressure ulcer develops, antibiotic coverage is the standard of care to prevent sepsis.1 The depth of the ulcer measured by the National Pressure Ulcer Advisory Panel (NPIAP) must be determined, as deeper wounds, usually Stage II or IV, may require surgical treatment.1 The ulcer must be cleaned thoroughly to remove dead tissue and prevent infection. Hydrocolloid dressings are often used to provide a moist environment for proper wound healing.1 Proper nutrition must be maintained for the patient to promote proper wound healing, and the patient should ambulate with physical therapy as often as possible.3
The management of pressure ulcers requires a team - which includes primary care physicians, dermatologists, home and wound care nurses, rehabilitation professionals and surgeons. It is important to reduce or relieve pressure on the skin, debride the necrotic tissue, cleanse the wound, and maintain clean wound dressings that are changed periodically to manage the bacterial load and colonization of the wound.4 Therefore, it is important to prevent the development of pressure ulcers through education to prevent hospital admissions and their associated costs.
What can be done to increase awareness?
Patient education is an excellent way to increase awareness of pressure ulcers. By teaching patients about the prophylactic treatment and turning every two hours, patients can take charge of their own care. We encourage those with physical limitations to request help with moving if they have not been repositioned within two hours. Additionally, educating patients’ families about pressure ulcers and prevention can help arm the families with tools to take care of the patients once they have been discharged from the hospital.
Resources
1. Zaidi, S. R. H., & Sharma, S. (2021). Pressure Ulcer. In StatPearls [Internet]. StatPearls Publishing.
2. Bedsores (pressure ulcers). Mayo Clinic. (2022, April 19). Retrieved January 18, 2023, from https://www.mayoclinic.org/diseases-conditions/bed-sores/symptoms-causes/syc-20355893
3. Al Aboud, A. M., & Manna, B. (2018). Wound pressure injury management.
4. Bluestein, D., & Javaheri, A. (2008). Pressure ulcers: prevention, evaluation, and management. American family physician, 78(10), 1186-1194.

CHILDREN’S HEALTH Visit us at www.bcms.org 23
Rebecca Wang and Christina Pierce are medical students at UT Health San Antonio interested in Dermatology.
CommuniCare and the Multi-Assistance Center (MAC) at Morgan’s WonderlandWorking Together to Improve the Lives of People with Disabilities in Bexar County and Beyond
By Robert P. Sanders, MD, MHA, FAAP, CPE
s of 2019, there were more than 297,000 people living with disabilities in Bexar County, representing 15% of the population, and more than 369,000 when the seven contiguous counties are included.1 People with disabilities encounter social and economic disparities which affect their ability to work, obtain insurance and get access to care. Vital medical, therapy, and social services are often unavailable, and where they do exist, the complex nature of our healthcare system means their delivery is often delayed, uncoordinated, and scattered throughout multiple sites and healthcare organizations. As a result, people with disabilities suffer poorer health outcomes than the general population, with higher rates of medical complications, lower quality of life, and ultimately reduced life expectancy.
San Antonio is now home to the Multi-Assistance Center at Morgan’s Wonderland (The MAC TM), the first facility of its kind in the world, designed to improve the lives and health outcomes of people of all ages with disabilities by creating a one-stop shop for medical, ther-

apeutic and social service needs. San Antonio real estate developer Gordon Hartman was inspired by his daughter Morgan, who lives with autism and other disabilities, to create a place where people with any level of ability can come to have fun, and in 2010 opened Morgan’s Wonderland, the first and only ultra-accessible theme park in the world. Since then, his team has gone on to create an ultra-accessible water park, sports program, and summer camp, which are now under the umbrella of Morgan’s Inclusion Initiative. The MAC is the next phase of that evolution, and was created through a combination of private donations and state and local government funding, in partnership with a diverse group of community-based organizations such as medical, dental and therapy providers.
The MAC is a new state of the art 165,000 square foot building located across the street from Morgan’s Wonderland in northeast San Antonio, and officially opened October 2, 2022. While the building is remarkable, the critical innovation at The MAC is The MAC Care
CHILDREN’S HEALTH
A 24 SAN ANTONIO MEDICINE • March 2023
Model,2 which places the patient (known as a MAC Member) and their caregivers at the center of the model, and works to address all the Member’s social determinants of health (SDOH), as well as their medical and therapy needs. The core of the MAC Model of Care is The MAC Navigation System, where each MAC Member is served by a dedicated MAC Navigator, who does an extensive intake and then coordinates referrals to an array of partner organizations addressing SDOH and medical needs. This process is made possible through use of The MAC Nav, a novel software platform designed in partnership with the Dedalus corporation, a division of Microsoft, that connects the Navigator and MAC Member with all The MAC’s partner organizations. Over 30 community organizations are represented on-site to support the full range of SDOH needs, including access to food, transportation, case management and legal services. Therapies on-site at The MAC include physical, speech/feeding and occupational therapy provided by TEAMability, Our Lady of the Lake University and the Children’s Hospital of San Antonio and applied behavioral analysis (ABA), provided by BlueSprig.
Essential medical services at The MAC are provided by CommuniCare Health Centers. CommuniCare is a Federally Qualified Health Center system that has cared for the underserved of San Antonio for over 50 years. CommuniCare was founded in 1972 as a two-room pediatric clinic in the back of a church on San Antonio’s West side by Sister Dolores Girault, D.C., a retired nurse and pharmacist, in response to an outbreak of diphtheria.3 Since then, CommuniCare has grown to include 23 sites providing primary and specialty medical, dental, and behavioral health care in Bexar, Kendall and Hays Counties.
CommuniCare at The MAC is a 21,000 square foot clinic providing primary care and behavioral health counseling to individuals with special needs from birth to 60 years of age; once enrolled, patients will never age out. The clinic also includes pulmonology and women’s health services, with plans to add a range of other specialty services as the facility grows. As part of The MAC Medical Home, CommuniCare works closely with other partner organizations, including a Center for Health Care Services behavioral medicine clinic, a Children’s Hospital of San Antonio clinic providing autism diagnosis, therapy, and pediatric specialty services, the Happy Ohana Smiles special needs dental clinic, the Sponsel Eye Experts ophthalmology and optometry clinic, and an audiology clinic run by Our Lady of the Lake University. Construction is now starting on Phase II of The MAC, which will include a full ambulatory surgery center, a Baptist M&S imaging center, an employment center, a drop-in daycare center and a special needs spa and salon. Working closely with public health and data science researchers from the University of Texas at San Antonio (UTSA), The MAC, along with CommuniCare and its other partner organizations, will conduct ongoing outcomes research to ensure that this extraordinary collaborative effort improves all aspects of life and health for individuals with disabilities. The goal of The MAC is to serve as a model for special needs care to be emulated throughout the San Antonio region and ultimately the rest of Texas and beyond.
References
1. People with Disabilities: A Texas Profile. Texas Investment Council. March, 2019. https://gov.texas.gov/uploads/files/organization /twic/Disabilities-Summary.pdf

2. The MAC Multi-Assistance Center at Morgan’s Wonderland. White Paper. Updated June 15, 2022. Available at morganswonderlandmac.org
3. https://communicaresa.org/about-communicare/
Robert P. Sanders, MD, MHA, FAAP, CPE is the Director of Complex Care at CommuniCare Health Centers. In this role he serves as the Medical Director of the CommuniCare at The MAC clinic. He is also the Chair of The MAC Medical Home Committee, which coordinates medical services at the MAC. He is a board-certified pediatrician, pediatric hematologist/oncologist and a certified physician executive.

CHILDREN’S HEALTH Visit us at www.bcms.org 25
Photographs copyrights the CommuniCare and the Multi-Assistance Center (MAC) at Morgan’s Wonderland.
The San Antonio DoSeum Creating Unique and Unforgettable Experiences for Families
 By Richard Kissel, PhD, Chief Program Officer, Interviewed by Monica Jones, COO, BCMS
By Richard Kissel, PhD, Chief Program Officer, Interviewed by Monica Jones, COO, BCMS
“Explorius Infinitum”
Done with the intention of examining something in order to find out more. Commonly observed at The DoSeum.
The DoSeum opened its doors to the San Antonio community on June 6, 2015. Serving families with children ages birth through 11, our mission is to grow curious minds, connect families, and transform communities through joyful learning and discovery. The DoSeum offers 70,000 square feet of indoor and outdoor exhibits, as well as a broad portfolio of programming and events during the year—all rooted in science, technology, engineering and math (“STEM”), as well as the arts and early literacy.
Prior to its current location on Broadway, the museum was located on Houston Street as The San Antonio Children’s Museum, and the evolution of the museum to Broadway permitted more space for exhibits and programming. In 2022, we welcomed more than 330,000 members and guests, over 10,000 students on field trips, and we designed and led professional-development programs for more than 250 local teachers. As we continue beyond the COVID pandemic, these numbers continue to increase.
How does the DoSeum help with Children’s Health?

The DoSeum is a leisure-based social venue that offers families and friends the opportunity to spend time with one another, and a place where they can explore their curiosities while learning together. Our goal with any exhibit or program development is to design to not only STEM concepts, but to also incorporate social and emotional frameworks. We consider concepts of self-awareness, social-awareness, self-
management, relationship skills, and responsible decision-making, for example. The DoSeum is a welcoming and safe place for all of San Antonio’s families, a place where they truly feel a sense of belonging and a freedom to follow their curiosity and wonder. “Explorius Infinitum!” The DoSeum helps families create special memories for parents and children alike.
Our programs are also designed to accommodate learners of all types, such as our sensory-friendly Beyond Limits program.
Tell us about the Teacher CPE Programs
In addition to serving families via the physical museum itself, we are honored to also work with local and regional educators. We offer a range of professional development opportunities for fellow educators, focusing on maker-centered learning, visual thinking strategies, inquiry-based instruction, the nature of science, and the engineering design process. These frameworks are rooted in problem-based learning and the process of science—asking questions, making observations, and presenting potential solutions based on the information collected. It is our hope that these concepts of reasoning will help our young learners be prepared for future challenges and opportunities.
Tell us about the Family Workshops.
The DoSeum’ s Family Workshops represent a new part of our program portfolio. We wanted a program that was designed to have families working together as a single unit. We limit each session to 10 to 12 families, with up to five members per family, and then help lead them through an activity that will either be extraordinarily memorable or provide a great item to take home. For example, in the shark dissec-
CHILDREN’S HEALTH 26 SAN ANTONIO MEDICINE • March 2023
tion program families receive a three-foot-long dogfish shark to dissect—a truly memorable experience for those families. We have also created stained glass panels and led workshops on Halloween makeup. These programs are held in the spring and fall seasons, typically on the last Sunday of each month.
Do you offer any special pricing or discounts for our community in San Antonio?
We understand that admission to any museum can be one barrier for local families, and we are proud to offer many discounts for the community, all of which can be found on our website. For example, we were the first museum in San Antonio to participate in the Museums for All program, which offers significantly reduced admission for any family presenting a SNAP or WIC Electronic Benefit Transfer (EBT) card and matching ID. We also offer group pricing, as well as discounts for Educators, Seniors, and members of the Military, all of which can be found on our website. We are currently looking forward to working with the Bexar County Medical Society to have a “Doctors Day” for BCMS family members!
What are the upcoming events for this year?

As we continue to refine and expand our programming, we are excited to be introducing “Night at The DoSeum.” This program invites families to spend an evening of play within our galleries, followed by sleeping in the museum and a nice continental breakfast before departure. We’ll have STEM stations set-up throughout the museum during the evening, as well, to create unique and memorable experiences for families in San Antonio. The first public overnight is scheduled for March 24-25, and
registration is live on our website. We also can separately host individual Scout groups for an overnight program.
The DoSeum’s very popular camp program is also returning for 2023. Registration for our Spring Break and Summer camps is already open. You can visit our website to register and learn more information.




Further, we are very excited to have our Special Events office return, following a temporary hiatus as a result of the Covid-19 pandemic. Our special events office manages our Birthday Party programs and private event rentals.
On behalf of the DoSeum’s staff and myself we would like to thank you for your service to our community. We realize how important it is to spend family time together and we invite you to visit the DoSeum. To find more information about DoSeum’s Programs and Services visit: www.thedoseum.org
Photographs copyrights The DoSeum.
Dr. Richard Kissel is the Chief Program Officer at The DoSeum, where he oversees guest experience, educational programming, and special events for San Antonio's only museum dedicated to early learners. He also serves as an instructor and course developer for the online Museum Studies graduate program at Johns Hopkins University. Richard also served as the Director of Public Programs at Yale's Peabody Museum, Director of Teacher Programs at the Paleontological Research Institution and Science Program Specialist at The Field Museum. He is a featured scientist online at NOVA's scienceNOW, serves as a scientific consultant for NOVA/BBC programming, and was a featured speaker at the 2016 TEDx Yale conference.
CHILDREN’S HEALTH Visit us at www.bcms.org 27
Creative Writing in Medicine – Eve
 By Tanima Arora
By Tanima Arora
It was the second time I was rotating through our neonatal intensive care unit, now used to the constant beeping of monitors, weak cries of infants and having to use more math than I ever have since graduating high school. It was Christmas Day and “Santa Claus” had visited the afternoon before taking photos with the babies’ isolettes and wishful parents that were around. I peered through the isolette at one of our new admissions the day before: a 24-week micro-preemie, a mere 600g, thin tangled tubes connecting her umbilical vessels to numerous drips and an endotracheal tube secured to her frail mouth connected to a heaving oscillator. Her isolette had a photo of Santa Claus standing next to her, but there was no parent in the picture. And how could there be, the whole family having suffered a tragic accident on Christmas Eve.
This family of three: father, pregnant mother 24 Weeks of Gestation (WOG) and three-year-old girl, had planned to visit their grandmother on Christmas Eve, when a drunk driver collided into their vehicle after running a stop sign. This tragic accident had landed all the family members in the hospital. The three-year-old was admitted to the PICU, suffering from cervical spine fractures and a concussion. The father was the most stable of the lot, admitted to the internal medicine floor with bilateral rib fractures and a minor splenic contusion. The mother was impacted the most, her left lung completed transected, intubated on a propofol drip, and via emergent C-section, birthed a beautiful angel into the world. “Eve” is what I named her.
I had nine babies that day, five of which were in level four, all connected to ventilators and some of which were TPN dependent. I spent half of my morning calculating their calories and interpreting their arterial blood gases, playing the game of vent setting adjustment vs blood gas results. I wanted to reserve half my pre-rounding for Eve. As I quickly jotted down the rates of her drips, making note of what was flowing through what line, our respiratory therapist (RT) tapped my shoulder and presented Eve’s 8 am blood gas. Her pH was down to 6.9, her respiratory acidosis worse. I sent the results in our group chat for the day, asking my fellow if it was okay for me to bump up her amplitude. He agreed, and I let the respiratory therapist know, who gave me a look of hesitation but made the change. I looked back down at my notes, resuming my calculations when my fellow appeared at the bedside. He had been there with her overnight, and told me that her gases had been becoming exponentially worse. “Can we change the frequency?” I asked, remembering that in some cases, frequency adjustments have a greater impact. “We can try,” he responded and called the attending. I went back to my workstation, getting my ducks in order before my attending arrived for rounds. Eve will be okay, she is in good hands, I promised myself.
My attending decided to round on Eve first, the typical order for our day would be sickest to relatively healthiest infants. Our team, complete with the attending, fellow, pharmacist,
nutritionist, three residents, respiratory therapist, two bedside nurses and mob of COWS (computer on wheels) huddled by her bedside. I peered through the isolette one last time at Eve to say hello, a tradition I started from my first day of the rotation and turned back to the crowd to start my presentation. As I strategically went through my presentation, detailing the overnight events, current vent settings, most recent gas and proposing my respiratory system plan, one of Eve’s nurses appeared at my side. “I’m sorry to interrupt, but her Mean Arterial Pressure (MAPs) is dropping.” I whipped around, the eyes of the team following, and saw her monitor reading a MAP of 10. The next thing I know, my attending was at her bedside, talking silently with the nurse and calling another provider (the one carrying her overnight). He peered over at me “Thank you, Tanima. The team may continue with rounds, I will join in a bit.”
Our fellow led the team onto different bays, rounding on the other babies, and even as I presented my other patients for the day, my eyes kept wandering over to Eve’s bay. There was some commotion and I was desperate to step away and help in any way I could. And that’s when I saw the door to the NICU open, a man being wheeled into the ICU, his head hanging low, and an old lady accompanying him. I immediately knew this was Eve’s father and possibly grandmother. I held my breath. They were ushered over to Eve’s isollete, and the next few minutes were
SAN ANTONIO MEDICINE
28 SAN ANTONIO MEDICINE • March 2023
a blur. I could hear muffled sobs, drowned by my co-resident presenting the last patient of the day. As soon as rounds finished, I walked over to the bay. My attending had authorized her morphine drip to be increased as much as it could, the time was close, the decision made by a grieving father. Another fellow had made her way over to the Medicine Intensive Care Unit (MICU), where Eve’s mother was housed, intubated and heavily sedated, in an attempt to allow her to see her baby, the only and last time, before her surgery. My heart was aching, my throat starting to close and I blinked rapidly attempting to dissolve the tears that would soon be streaming down my face. Could I cry? Is it even appropriate, for the provider to cry in front of the family? I didn’t know, but what I did know was that I was feeling helpless and wanted to help in any way that I could. So, I stepped up to the isolette and asked Eve’s nurse if I could hold the iPad, and assist with the Facetime. I hovered over Eve, taking in her fragility and beauty, and after a few minutes received an incoming call from my fellow.
Eve’s mother was in her ICU bed, a large endotracheal tube obscuring her significantly edematous face. She could not speak, she could not see, but I would like to believe, that just being there in this virtual presence of her baby, that she could feel, and that was something.
I stepped away after the Facetime ended, walking as quickly as I could out of the NICU to catch a breath by the windows overlooking our garden. It wasn’t fair. Eve and this entire family did not deserve so much heart ache. Tears were streaming down my face, collecting below my mask. After a few deep breaths, I made my way back to Eve’s bay. Her ventilator had been disconnected, her ET tube removed, her umbilical arterial and venous catheter removed and her skin was being cleaned from residual blood. Her nurses dressed her in a pink onesie, with
a matching cap and mittens, while her father and grandmother prepared to hold her in her last breaths. I sat at the workstation directly in front of her bay, catching glances at these precious moments of Eve with her father and grandmother. They talked to her, they prayed to her, they sang to her, they held her close, and they cherished every single second they had with her. A few hours later, they took Eve up to the “Butterfly Suite” (our department’s palliative care room where family can room in with their babies privately and comfort care is provided). That was the last I saw of Eve.
Mortality in the NICU is not uncommon, and one can argue that no matter how many deaths you’ve witnessed in the world of medicine, one can never really be completely prepared. Eve was not the first death I have witnessed during my medical training, nor will she be the last. Working in any intensive care unit, where all your patients are critical and require constant monitoring can become very overwhelming, but each instance of death is a learning opportunity. An opportunity to broaden our skillset outside the world of medicine and clinical knowledge, by refining our compassion, empathy, human connection and coping mechanisms. I feel fortunate enough to have been supported well by my attendings, fellows and co-residents through de-briefing sessions and I feel fortunate enough to have been a part, albeit maybe a small one, of this patient’s and family’s journey. I will always remember Eve, on happy days and sad days, in good times and bad times, for she made my education and my empathy stronger.
Eve had passed away by the following morning when I returned to work, a small box left at her bay ready to be shipped to her home. It was a memorial box, with pictures of her being held and loved by her family, a notebook and her pink onesie, cap and mittens. I peered at the bottom of the box, and the last few lines of a poem from Eve to her mother caught my eye and I smiled with a heavy heart. Goodbye, Eve.
I know that in Heaven there is no marriage, but surely there can be some acknowledgement of Motherhood, Because there’s one thing I don’t only wonder about, It is something that I really hope for When I


SAN ANTONIO MEDICINE
Tanima Arora, MD MHS, PGY-2 Pediatric Resident at UT Health San Antonio.
Visit us at www.bcms.org 29
do get to heaven I want to feel a hand in mine And hear the words, “Mommy, it’s me”
Conversations
By Holly Ratcliff

“Don’t we all think about it sometimes?” The fellow joked.
“Every single day,” the resident laughed.
“You know that bridge by my house? It would be so easy to make it look like an accident.”
“After a long shift, who would think it wasn’t an accident?”
“Just drive right off and it would all be over.”
I sat in the corner, wondering when the conversation had stopped sounding like a joke.
Holly Miller is a student at the UT Health San Antonio Long School of Medicine, Class of 2023


Community
By Nisha Kalyanpur
SAN ANTONIO MEDICINE
Nisha Kalyanpur is a student at the UT Health San Antonio Long School of Medicine, Class of 2023
30 SAN ANTONIO MEDICINE • March 2023
Cross-Stitch Heart
 By Sarah Suhood
By Sarah Suhood

Untitled
 By Grace Cooper
By Grace Cooper
Artist Note: My mom taught me how to cross stitch when I was young. We would spend our summers in Sri Lanka with our grandmother and I would do a kid’s cross stitch every summer. My mom makes them as birthing announcements and wedding announcements for her friends and family. I used to think it was such an old lady hobby. It wasn’t until I was in an unhealthy living situation and working through the pandemic as an overwhelmed as a nurse tech that I began cross stitching again for the first time in 10 years. Something so simple about making an “X” over and over again helped me find a peace I desperately needed. It’s one of the reasons I’ll hopefully be an old lady one day.

SAN ANTONIO MEDICINE
Sarah Ruth Suhood, MS 2LT USAF, is a student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2025
Grace Cooper is a student at the UT Health San Antonio Long School of Medicine, Class of 2023
Visit us at www.bcms.org 31
Imposter Syndrome
By Stephanie Batch

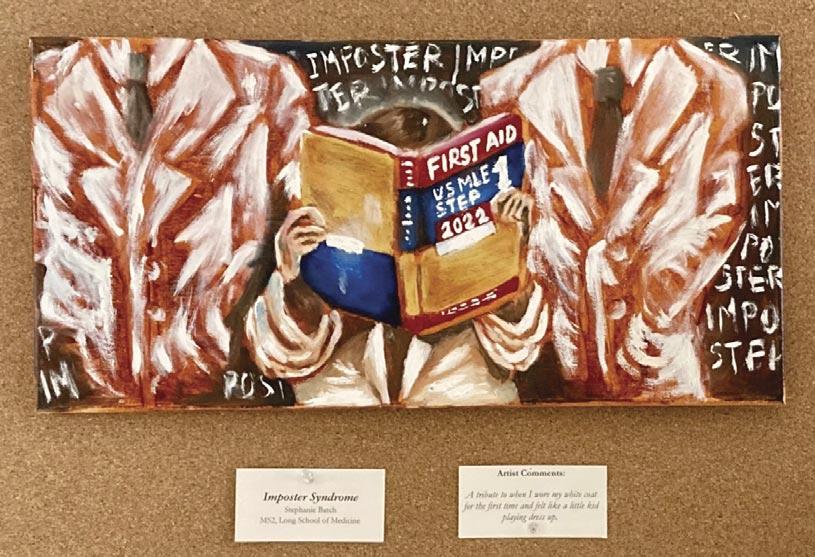
Artist Note: A tribute to when I wore my white coat for the first time and felt like a little kid playing dress up.
Stephanie Batch is a student at the UT Health San Antonio Long School of Medicine, Class of 2025.


Such a Lovely Smile
By Danny Parris
Danny Parris is a psychology student at the University of the Incarnate Word, Class of 2022
SAN ANTONIO MEDICINE
32 SAN ANTONIO MEDICINE • March 2023
TMA Kicks Off 20th Anniversary of First Tuesdays at the Capitol
By Mary E. Nava, MBA, Chief Government Affairs Officer
With the 88th Legislative Session now in full swing, the first ‘First Tuesdays at the Capitol’ took place on Feb. 7. Physicians and BCMS Alliance members participated in several meetings with legislators and staff. A number of topics were discussed, including: scope of practice; tobacco prevention; prior authorization; vaccinations and Medicaid funding for women and children’s health.
Many thanks to the attendees, who made our visits a success: Dan Deane, MD; Sanjiv Kumar, MD; BCMS President John Nava, MD; Michael “Mickey” Seger, MD; Jayesh Shah, MD; John Shepherd, MD and Alliance members, Jenny Shepherd and Martha Vijjeswarapu.



The next First Tuesdays at the Capitol is on March 7. We encourage all BCMS members to get involved and make plans to attend at least one First Tuesdays this legislative session. All you have to do is plan to travel to Austin during one of the First Tuesdays and BCMS staff does the rest, including scheduling appointments for our visits with legislators and their staff and gathering handouts pertinent to our visits. To register, please visit texmed.org/firsttuesdays.
For local discussion on these and other legislative advocacy topics, consider joining the BCMS Legislative and Socioeconomics Committee by contacting Mary Nava at mary.nava@bcms.org.
LEGISLATIVE NEWS
34 SAN ANTONIO MEDICINE • March 2023
On Feb. 7, State Representative Dr. Tom Oliverson (House District 130), at podium, greets First Tuesdays attendees in the TMA Thompson Auditorium.
Right: Pausing for a photo on Feb. 7 with State Representative Elizabeth “Liz” Campos (House District 119) are (l-r): Rep. Campos; BCMS Alliance member Jenny Shepherd; John Shepherd, MD; Mary Nava, BCMS chief government affairs officer and Dan Deane, MD.
BCMS physicians, Alliance members and staff pause for a photo just outside the north entrance to the Texas State Capitol during the Feb. 7 First Tuesdays event.


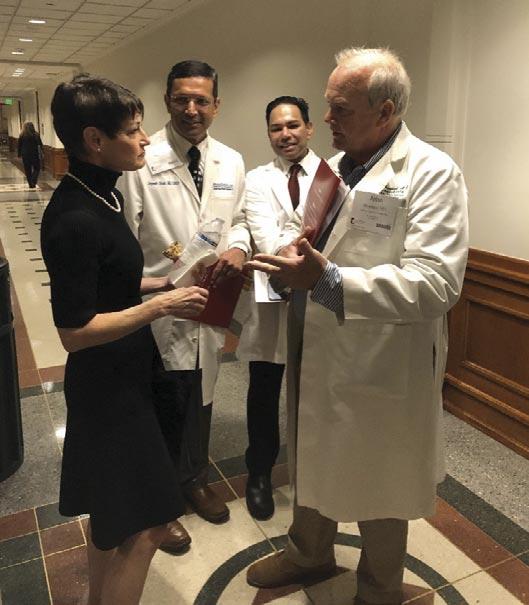

LEGISLATIVE NEWS Visit us at www.bcms.org 35
BCMS physicians and guests visit with Alexandra Calve (seated right), policy analyst in the office of State Senator Jose Menendez (Senate District 26) during the Feb. 7 First Tuesdays visits to the Capitol.
State Senator Roland Gutierrez (Senate District 19) (center) pauses for a photo with BCMS physicians, Alliance members and guests during the Feb. 7 First Tuesdays visits to the Capitol.
John Shepherd, MD (standing right) shares details on medicine’s issues with State Senator Donna Campbell (Senate District 25) during the Feb. 7 First Tuesdays visits. Looking on are (l-r): Jayesh Shah, MD and Sanjiv Kumar, MD.
BCMS physicians and staff, along with TMA staff met with State Representative Steve Allison (House District 121) (seated in dark suit) to discuss key issues of importance to medicine on Feb. 7 during the First Tuesdays visits.



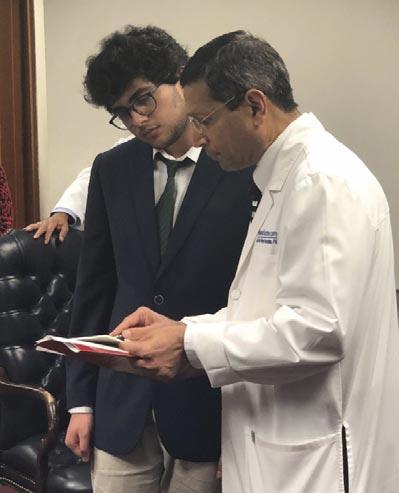


36 SAN ANTONIO MEDICINE • March 2023 LEGISLATIVE NEWS
Standing (l-r) in the office of State Representative Philip Cortez (House District 117) during the Feb. 7 First Tuesdays visits are: Dan Deane, MD; Mary Nava; Jenny Shepherd; John Shepherd, MD; State Representative Mary Ann Perez (House District 144); Rep. Cortez and BCMS President, John Nava, MD.
On Feb. 7, during the First Tuesdays visits to the Capitol, BCMS physicians, Alliance members, guests and staff pause for a photo with State Representative John Lujan (House District 118) (center).
During the Feb. 7 First Tuesdays visits, BCMS physicians, Alliance members and guests met with State Representative Josie Garcia (House District 124) (standing left) to discuss key issues of importance to medicine.
State Representative Diego Bernal (House District 123), standing, shares a laugh with Jayesh Shah, MD and BCMS President, John Nava, MD (foreground), during the Feb. 7 First Tuesdays visits to the Capitol.
Dan Deane, MD shares information on medicine’s issues with Cesar Obregon, legislative director in the office of State Representative Ray Lopez (House District 125) during the Feb. 7 First Tuesdays visits to the Capitol.
On Feb. 7, during the First Tuesdays visits to the Capitol, Jayesh Shah, MD provided information on medicine’s issues to Tariq Ahmed, legislative staff member in the office of State Representative Barbara Gervin-Hawkins (House District 120).
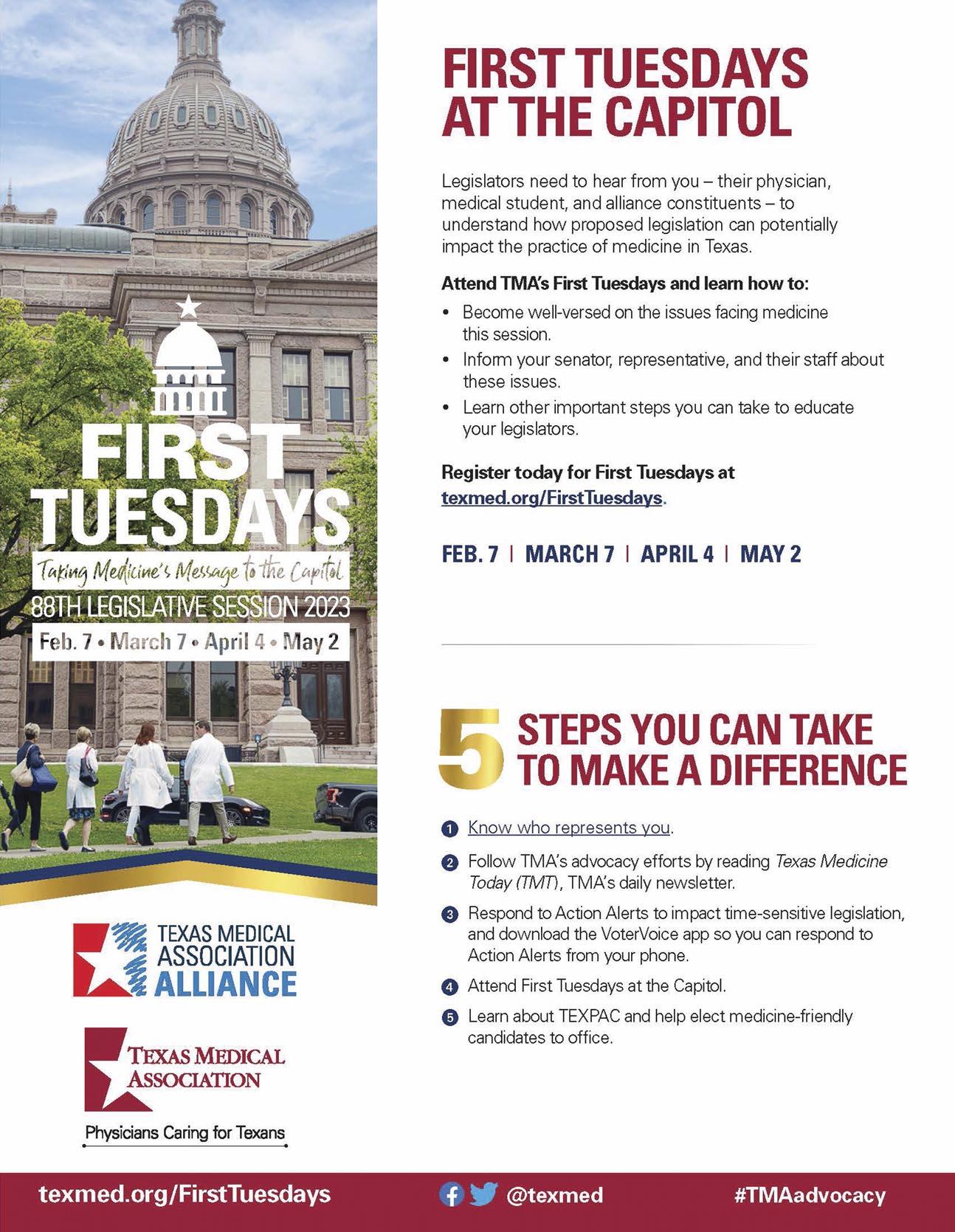
Texas Medical Association – 2023 Winter Conference



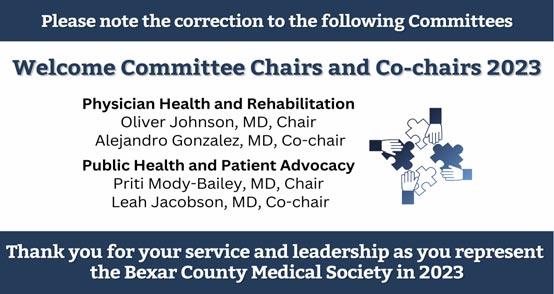

38 SAN ANTONIO MEDICINE • March 2023 LEGISLATIVE NEWS
At left: Organized medicine starts with the grassroots. Thanks to all our county medical society executives and membership teams met at TMA Winter Conference representing physicians across Texas. Right: Dr. John Nava, BCMS President attending meeting with his colleagues from across the State of Texas

Shop Vendors Who Support BCMS
BCMS Vendor Directory
We encourage you to use our supporting vendors whenever you or your practice needs supplies or services.
ACCOUNTING FIRMS
Sol Schwartz & Associates P.C. (HHH Gold Sponsor)

Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Jim Rice, CPA 210-384-8000, ext. 112 jprice@ssacpa.com www.ssacpa.com
“Dedicated to working with physicians and physician groups.”
ACCOUNTING SOFTWARE
Express Information Systems (HHH Gold Sponsor)

With over 29 years’ experience, we understand that real-time visibility into your financial data is critical. Our browser-based healthcare accounting solutions provide accurate, multi-dimensional reporting that helps you accommodate further growth and drive your practice forward.
Rana Camargo
Senior Account Manager
210-771-7903
ranac@expressinfo.com www.expressinfo.com
“Leaders in Healthcare Software & Consulting”
ATTORNEYS
Kreager Mitchell (HHH Gold Sponsor)
At Kreager Mitchell, our healthcare practice works with physicians to offer the best representation possible in providing industry specific solutions. From business transactions to physician contracts, our team can help you in making the right decision for your practice.
Michael L. Kreager
210-283-6227
mkreager@kreagermitchell.com
Bruce M. Mitchell
210-283-6228
bmitchell@kreagermitchell.com
www.kreagermitchell.com
“Client-centered legal counsel with integrity and inspired solutions”

ASSET WEALTH MANAGEMENT
Aspect Wealth Management (★★★ Gold Sponsor)

We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark, President
210-268-1520
mclark@aspectwealth.com www.aspectwealth.com
“Get what you deserve … maximize your Social Security benefit!”
Bertuzzi-Torres-Fernandez
Wealth Management Group (HHH Gold Sponsor)
We specialize in simplifying your personal and professional life. We are dedicated wealth managers who offer diverse financial solutions for discerning healthcare professionals, including asset protection, lending and estate planning.
Mike Bertuzzi
First Vice President Senior Financial Advisor
210-278-3828
Michael_bertuzzi@ml.com
Ruth Torres Financial Advisor
210-278-3828
Ruth.torres@ml.com
http://fa.ml.com/bertuzzi-torres
Will C. Fernandez, CEPA Senior Portfolio Advisor Financial Advisor
210-278-3812
wfernandez@ml.com
https://fa.ml.com/texas/san-antonio/bertuzzi-torres-fernandez
BANKING Broadway Bank (HHH Gold Sponsor)
Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead
210-283-6640
TDuran@Broadway.Bank
www.broadwaybank.com

“We’re here for good.”
The Bank of San Antonio (HHH Gold Sponsor)

We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community. Brandi Vitier
210-807-5581
brandi.vitier@thebankofsa.com
www.thebankofsa.com
Synergy Federal Credit Union (HH Silver Sponsor)
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help Physicians get the banking services they need.
Synergy FCU Member Services
210-750-8333 info@synergyfcu.org www.synergyfcu.org
“Once a member, always a member. Join today!”
CLINICAL DIAGNOSTICS
rate, comprehensive and reliable results to our partners and patients. Genics Laboratories is committed to continuous research, ensuring our protocols are always at the peak of current technology.
Yulia Leontieva
Managing Partner, Physician Liaison (210) 503-0003 (Phone)

yulia@genicslabs.com (Email)
Kevin Setanyan
Managing Partner (210) 503-0003

kevin@genicslabs.com
Artyom Vardapetyan Managing Partner (210) 503-0003
www.genicslabs.com
“Accurate results in record time.”
CREDENTIALS VERIFICATION ORGANIZATION
Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor) Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for health care entities.

Betty Fernandez Director of Operations
210-582-6355
Livingston Med Lab
(HHHH 10K Platinum Sponsor)
High Complexity Clia/Cola accredited Laboratory providing White Glove Customer Service. We offer a Full Diagnostic Test Menu in the fields of Hematology, Chemistry, Endocrinology, Toxicology, Infectious Disease, & Genetics. Robert Castaneda (CEO) 210-316-1792
Robert@livingstonmedlab.com
Joey Martinez (Director of Operations)
210-204-7072
Joey@livingstonmedlab.com
Dwight Chapman (Account Manager)
210-591-2649
Dwight@livingstonmedlab.com
www.livingstonmedlab.com/home

“Trusted Innovative, Accurate, and STAT Medical Diagnostics”
Betty.Fernandez@bexarcv.com www.BexarCV.com
“Proudly serving the medical community since 1998”
FINANCIAL ADVISORS
Oakwell Private Wealth Management (HHHH 10K Platinum Sponsor) Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.

Brian T. Boswell, CFP®, QKA Senior Private Wealth Advisor 512-649-8113 SERVICE@OAKWELLPWM.COM
www.oakwellpwm.com
Genics Laboratories (HHH Gold Sponsor)
Genics Laboratories offers accu-
“More Than Just Your Advisor, We're Your Wealth Management Partner”

40 SAN ANTONIO MEDICINE • March 2023
Elizabeth Olney with Edward Jones (HH Silver Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney, Financial Advisor
210-858-5880
Elizabeth.olney@edwardjones.com www.edwardjones.com/elizabeth-olney
"Making Sense of Investing"
FINANCIAL SERVICES
Aspect Wealth Management (HHH Gold Sponsor)

We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark, President 210-268-1520 mclark@aspectwealth.com www.aspectwealth.com
“Get what you deserve … maximize your Social Security benefit!”
Bertuzzi-Torres-Fernandez
Wealth Management Group ( Gold Sponsor)
We specialize in simplifying your personal and professional life. We are dedicated wealth managers who offer diverse financial solutions for discerning healthcare professionals, including asset protection, lending & estate planning.
Mike Bertuzzi
First Vice President Senior Financial Advisor
210-278-3828
Michael_bertuzzi@ml.com
Ruth Torres
Financial Advisor
210-278-3828
Ruth.torres@ml.com
Will C. Fernandez, CEPA
Senior Portfolio Advisor Financial Advisor
210-278-3812
wfernandez@ml.com
https://fa.ml.com/texas/san-antonio/bertuzzi-torres-fernandez
GERIATRICS/PRIMARY
CARE
allows physicians to deliver high quality, personalized care and achieve better outcomes, while feeling free to focus on health equity and patient outcomes.
Kim Gary Senior Physician Recruiter
(812) 272-9838
KGary4@humana.com
www.ConvivaCareers.com
“Fuel Your Passion & Find Your Purpose”
HEALTHCARE BANKING
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Jeanne Bennett
EVP | Private Banking Manager
210-343-4556
Jeanne.bennett@amegybank.com
Karen Leckie
Senior Vice President | Private Banking
210-343-4558
karen.leckie@amegybank.com
Robert Lindley
Senior Vice President | Private Banking

210-343-4526
robert.lindley@amegybank.com
Denise C. Smith Vice President | Private Banking
210-343-4502
Denise.C.Smith@amegybank.com www.amegybank.com
“Community banking partnership”
HOSPITALS/ HEALTHCARE FACILITIES
UT Health San Antonio MD
Anderson Cancer Center (HHH Gold Sponsor)
UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
Regina Delgado
Business Development Manager (210) 450-3713
delgador4@uthscsa.edu
UT Health San Antonio MD

Anderson Mays Cancer Center
Laura Kouba
Business Development Manager (210) 265-7662
norriskouba@uthscsa.edu
https://uthscsa.edu/
Appointments: 210-450-1000
UT Health San Antonio 7979 Wurzbach Road San Antonio, TX 78229
INFORMATION AND TECHNOLOGIES
“We offer BCMS members a free insurance portfolio review.”
Humana (HHH Gold Sponsor)
Humana is a leading health and well-being company focused on making it easy for people to achieve their best health with clinical excellence through coordinated care.
Jon Buss: 512-338-6167
Jbuss1@humana.com
Shamayne Kotfas: 512-338-6103
skotfas@humana.com
www.humana.com
INSURANCE/MEDICAL MALPRACTICE
Texas Medical Liability Trust (HHHH 10K Platinum Sponsor)

Conviva Care Center (HHH Gold Sponsor)

Conviva’s value-based care model
Nexus Neurorecovery Center (HHH Gold Sponsor)

A post-acute rehabilitation facility focusing on brain injuries. Programming provides individual and group physical, occupational, cognitive, and speech therapy. We help residents return to lives of productivity and meaning.
Sydney Kerr Liaison
346-339-2654
skerr@nhsltd.com
Caitlyn Tewksbury
ctewksbury@nhsltd.com
Justin Sanderson CEO 210-854-4732
jsanderson@nhsltd.com
Nexus Neurorecovery Center
227 Lewis St, San Antonio, TX 78212
https://nexushealthsystems.com
“To return patients to lives of productivity and meaning”
Express Information Systems (HHH Gold Sponsor)

With over 29 years’ experience, we understand that real-time visibility into your financial data is critical. Our browser-based healthcare accounting solutions provide accurate, multi-dimensional reporting that helps you accommodate further growth and drive your practice forward.
Rana Camargo
Senior Account Manager 210-771-7903
ranac@expressinfo.com
www.expressinfo.com
“Leaders in Healthcare Software & Consulting”
INSURANCE
With more than 20,000 health care professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of health care for patients by educating, protecting, and defending physicians.
Patty Spann
512-425-5932
patty-spann@tmlt.org
www.tmlt.org
Recommended partner of the Bexar County Medical Society
The Bank of San Antonio Insurance Group, Inc. (HHH Gold Sponsor)

We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Katy Brooks, CIC 210-807-5593
TMA Insurance Trust (HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service insurance agency offering a full line of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.

Wendell England Director of Member Benefits 512-370-1776 wendell.england@tmait.org
800-880-8181 www.tmait.org
katy.brooks@bosainsurance.com
www.thebankofsa.com
“Serving the medical community.”
MedPro Group (HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze
512-658-0262
Kirsten.Baze@medpro.com
www.medpro.com
continued on page 42
Visit us at www.bcms.org 41
BCMS Vendor Directory
INVESTMENT ADVISORY REAL ESTATE
Alamo Capital Advisors LLC (★★★★ 10K Platinum Sponsor)


Focused on sourcing, capitalizing, and executing investment and development opportunities for our investment partners and providing thoughtful solutions to our advisory clients. Current projects include new developments, acquisitions & sales, lease representation and financial restructuring (equity, debt, and partnership updates).
Jon Wiegand, Principal 210-241-2036
jw@alamocapitaladvisors.com www.alamocapitaladvisors.com
MEDICAL BILLING AND COLLECTIONS SERVICES
tom.rosol@henryschein.com
www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”
MILITARY
San Antonio Army Medical Recruiting office (★★Silver Sponsor)
Mission: Recruit highly qualified and motivated healthcare professionals for service in the Army Reserves or Active Duty Army, in support of Soldiers and their families.
1LT Thomas Alexandria 210-328-9022
Alexandria.n.thomas12.mil@army. mil
https://recruiting.army.mil/mrb/ “Service to Country, Army Medicine, Experientia et Progressus”
MOLECULAR DIAGNOSTICS
LABORATORY
Wave Online (★★★ Gold Sponsor)
Our team of professionals will act as your extended AR office enhancing your revenue through our proprietary metrics and claim management systems. In addition, you keep 100% control of your RCM. Contact us today for a no cost evaluation.
Saranraj (Raj) Venkatesh
Vice President – RCM | Sales and Client Relations
726-228-1097
saranraj@wavemt.com
https://rcmwave.com/ “Innovation towards Solutions”
Commercial & Medical Credit Services (HH Silver Sponsor)
A bonded and fully insured San Antonio-based collection agency.
Henry Miranda 210-340-9515
hcmiranda@sbcglobal.net www.cmcs-sa.com
“Make us the solution for your account receivables.”
MEDICAL SUPPLIES AND EQUIPMENT
Henry Schein Medical (HH Silver Sponsor)

From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Tom Rosol
210-413-8079
continued from page 41
PROFESSIONAL ORGANIZATIONS
The Health Cell (HH Silver Sponsor)
“Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more!
Kevin Barber, President 210-308-7907 (Direct) kbarber@bdo.com
Valerie Rogler, Program Coordinator 210-904-5404
Valerie@thehealthcell.org www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA) (HH Silver Sponsor)
SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising.
Brian T. Boswell, CFP®, QKA
Senior Private Wealth Advisor
512-649-8113
SERVICE@OAKWELLPWM.COM
www.oakwellpwm.com
“More Than Just Your Advisor, We're Your Wealth Management Partner”
STAFFING SERVICES
Favorite Healthcare Staffing (HHHH 10K Platinum Sponsor)
Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle.
Cindy M. Vidrine
Director of Operations- Texas 210-918-8737
cvidrine@favoritestaffing.com
iGenomeDx

(
Gold Sponsor)
Most trusted molecular testing laboratory in San Antonio providing FAST, ACCURATE and COMPREHENSIVE precision diagnostics for Genetics and Infectious Diseases.
Dr. Niti Vanee Co-founder & CEO
210-257-6973
nvanee@iGenomeDx.com
Dr. Pramod Mishra Co-founder, COO & CSO
210-381-3829
pmishra@iGenomeDx.com
www.iGenomeDx.com
“My DNA My Medicine, Pharmacogenomics”
PRACTICE MANAGEMENT
Lindsey Herman Nolan, MHR, CMPE, President info4@samgma.org www.samgma.org
REAL ESTATE SERVICES COMMERCIAL
“Favorite Healthcare Staffing offers preferred pricing for BCMS members.”
Wave Online (★★★ Gold Sponsor)


Our team of professionals will act as your extended AR office enhancing your revenue through our proprietary metrics and claim management systems. In addition, you keep 100% control of your RCM. Contact us today for a no cost evaluation.
Saranraj (Raj) Venkatesh
Vice President – RCM | Sales and Client Relations 726-228-1097
saranraj@wavemt.com
https://rcmwave.com/ “Innovation towards Solutions”
Alamo Capital Advisors LLC (
★★★★ 10K Platinum Sponsor)
Focused on sourcing, capitalizing, and executing investment and development opportunities for our investment partners and providing thoughtful solutions to our advisory clients. Current projects include new developments, acquisitions & sales, lease representation and financial restructuring (equity, debt, and partnership updates).
Jon Wiegand, Principal 210-241-2036 jw@alamocapitaladvisors.com www.alamocapitaladvisors.com
RETIREMENT PLANNING
Oakwell Private Wealth Management (HHHH 10K Platinum Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.

42 SAN ANTONIO MEDICINE • March 2023


Visit us at www.bcms.org 43
Porsche Track Experience




 By Stephen Schutz, MD
By Stephen Schutz, MD
AUTO REVIEW
44 SAN ANTONIO MEDICINE • March 2023
I just did the best manufacturer track day of my life, the Porsche Track Experience at Barber Motorsports Park in Birmingham, Alabama.
For the record, I have spent many days at race tracks, mostly at Laguna Seca Raceway in Monterey, CA, but also Sonoma Raceway in Sonoma, CA, Thunderhill Raceway north of Sacramento, CA, and now, Barber Motorsports Park. And in case you’re wondering, I paid for the experience, receiving neither a freebie nor discount from the $2000 price tag from Porsche.
Most of my time at tracks has been for automotive journalist gatherings or manufacturer events, but I have also done official BMW, Lexus, and Audi track experiences as well. Until my time with Porsche in Alabama, Audi’s at Sonoma was the best one, with BMW’s near Palm Springs number two, and Lexus’ at Laguna Seca a (very) distant third.
Ultimately the Porsche event at a relatively obscure track just north of Birmingham was better than the others because you get more laps at higher speeds, among other pluses.
For starters, Porsche does an excellent job, “concierging” customers through the process. Once you sign up there are logistics galore, as there are with most automotive and non-automotive trips: airplane tickets, hotel reservations, ground transportation, meals, etc. Porsche helps with those challenges by coordinating with a terrific luxury hotel close to the track, the Grand Bohemian Birmingham, providing a very responsive Porsche liaison there, and offering shuttles to and from the airport. Could the liaison arrange charging for my Battery Electric Vehicle (BEV) press car at the hotel as well as dinner reservations for eight at an excellent restaurant after my day at the track? Yes she could, and did.
Promptly at 7AM the morning of my track day a Mercedes Sprinter van drove us to the venue for breakfast and a “chalk talk”, during which our lead instructor went through the dos and don'ts of driving on the track (do pay attention to your surroundings, don’t crash the car). I’ve listened to many chalk talks, and this was the first one done while I ate a meal—thank you Porsche!
After that orientation, my group headed off to do off-track performance drills: acceleration/braking while turning, skidpad and autocross. Accelerating and braking while turning takes concentration, autocross takes concentration and is fun, and the skidpad took little brainpower and was uproariously fun.
Then we hit the track, where we drove three different Porsche sports cars, all very quickly and for many laps, as noted above.
First up was the Porsche Cayman GTS, which has less power than the 911 GTS and Turbo models that we drove later, but which may have been more fun than those cars because it had less power and grip
and was therefore easier to take to its handling limit.
Next was the 911 Turbo S, which was so capable, thanks to prodigious power and All-Wheel Drive (AWD), that I felt more like it was driving me than I was driving it.
Finally, we hit the 911 GTS, which felt just right—more potent and with higher cornering limits than the mini-me Cayman, but more approachable than the all-conquering Turbo. Part of my preference for the 911 GTS may have been due to the fact that my daily driver is a 2022 911 S, but two of my team members who don’t own Porsches agreed with my assessment.
Anyway, the Barber track is a technical 2.4 mile circuit with sixteen corners, so achieving big MPHs on the two (relatively short) straightaways is less important than maintaining your speed through those many corners.
Like most manufacturer track experiences, Porsche uses a lead-follow driving technique where three or four cars driven by students follow a lead car piloted by an instructor. As the day progressed the instructors increased their speed, to the point where, not very long into the program, the students had to hustle to keep up.
And I do mean hustle—I spent most of my time on track close to or at my limits. Did things ever get uncomfortable? Not really, probably because following an expert driver behind the wheel of exactly the same car you’re driving with exactly the same tires is very reassuring—if he’s not flying off the track then I probably won’t either—but we were certainly driving fast.
Why do I think that Porsche’s track experience is better than its competitors’? While BMW and Audi let us drive quickly but rationed laps, and Lexus limited speed severely and rationed laps, Porsche let us run and gave us many laps. So many laps, in fact, that I lost count and was exhausted when they finally told us that we were finished. Exhausted and exhilarated, of course.
If you’re thinking of doing a manufacturer track experience, my strong recommendations are: 1) do it, you won’t regret it despite the cost, and 2) choose Porsche. It’s the best one.
As always, call Phil Hornbeak, the Auto Program Manager at BCMS (210-301-4367), for your best deal on any new car or truck brand. Phil can also connect you to preferred financing and lease rates.
Stephen Schutz, MD, is a board-certified gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the US Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.

AUTO REVIEW Visit us at www.bcms.org 45
11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Rick Cavender 210-681-3399

Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Charles Williams 210-912-5087
Chuck Nash Chevrolet Buick GMC 3209 North Interstate 35 San Marcos, TX
William Boyd 210-859-2719
Bluebonnet Chrysler Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Kahlig Auto Group
Northside Ford 12300 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
Kahlig Auto Group
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX
James Cole 210-816-6000
9455 IH 10 West San Antonio, TX 78230
Douglas Cox 210-764-6945
Kahlig Auto Group
Audi North Park 15670 IH-35 North Selma, TX 78254
Camden Steele 325-374-9897
Northside Honda 9100 San Pedro Ave. San Antonio, TX 78216
Paul Hopkins 210-988-9644
Kahlig Auto Group
14610 IH 10 West San Marcos, TX 78249
Mark Hennigan 832-428-9507
North Park Lincoln 9207 San Pedro San Antonio, TX
Sandy Small 210-341-8841
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200
North Park Mazda 9333 San Pedro San Antonio, TX 78216
John Kahlig 210-253-3300
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson 877-356-0476
Land Rover San Antonio 13660 IH 10 West San Antonio, TX
Cameron Tang 210-561-4900
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
James Godkin 830-981-6000
Cavender Toyota 5730 NW Loop 410 San Antonio, TX
Gary Holdgraf 210-862-9769
North Park Lexus 611 Lockhill Selma San Antonio, TX
Tripp Bridges 210-308-8900
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX
Al Cavazos Jr. 210-366-9600
North Park Toyota 10703 Southwest Loop 410 San Antonio, TX 78211
Justin Boone 210-635-5000
 Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group



















 By Alice K. Gong, MD
By Alice K. Gong, MD




 By Noel C. Ales, DO
By Noel C. Ales, DO
















 By Richard Kissel, PhD, Chief Program Officer, Interviewed by Monica Jones, COO, BCMS
By Richard Kissel, PhD, Chief Program Officer, Interviewed by Monica Jones, COO, BCMS






 By Tanima Arora
By Tanima Arora





 By Sarah Suhood
By Sarah Suhood

 By Grace Cooper
By Grace Cooper


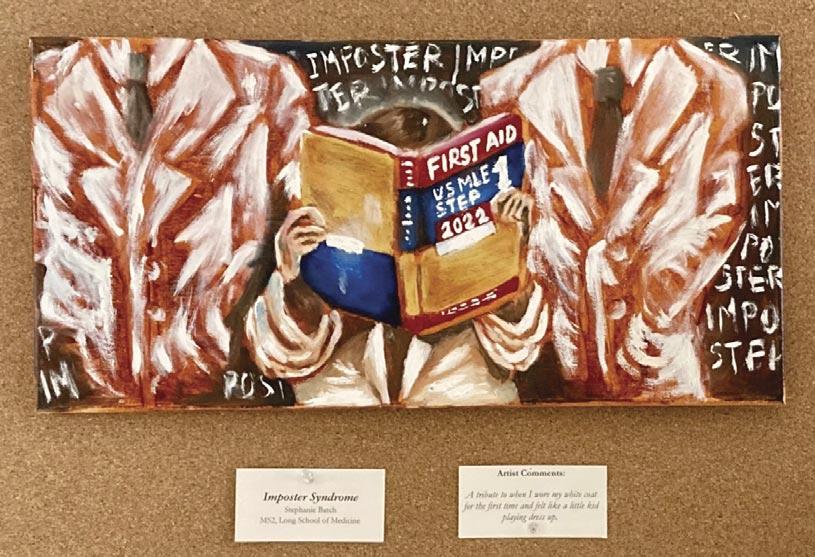













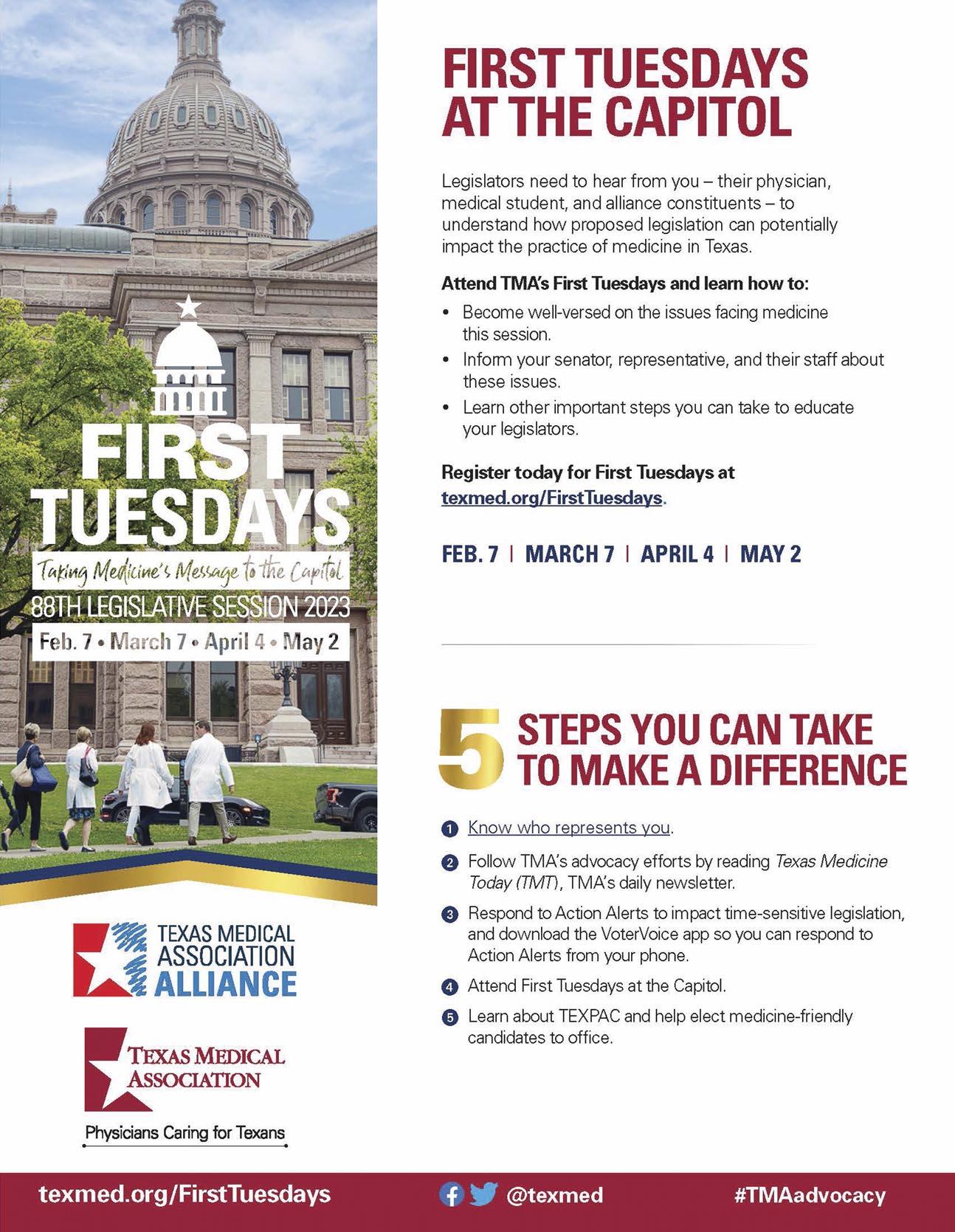
































 By Stephen Schutz, MD
By Stephen Schutz, MD


 Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group
Kahlig Auto Group

