
















Traveling Blender, LLC. 10036 Saxet Boerne, TX 78006
PUBLISHER: Louis Doucette louis@travelingblender.com
BUSINESS MANAGER: Vicki Schroder vicki@travelingblender.com
GRAPHIC DESIGNER: Jennifer Nelson jennifer@travelingblender.com
ADVERTISING SALES: AUSTIN: Sandy Weatherford sandy@travelingblender.com SAN ANTONIO: Gerry Lair gerrylair@yahoo.com
For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.
San Antonio Medicine is the ofcial publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS
EDITORIAL CORRESPONDENCE:
Bexar County Medical Society 4334 N Loop 1604 W, Ste. 200 San Antonio, TX 78249
Email: editor@bcms.org
MAGAZINE ADDRESS CHANGES: Call (210) 301-4391 or Email: membership@bcms.org
SUBSCRIPTION RATES: $30 per year or $4 per individual issue
ADVERTISING CORRESPONDENCE: Louis Doucette, President Traveling Blender, LLC.
A Publication Management Firm 10036 Saxet, Boerne, TX 78006 www.travelingblender.com
For advertising rates and information Call (210) 410-0014
Email: louis@travelingblender.com
SAN ANTONIO MEDICINE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily refect the opinion of BCMS, its members, or its staf. SAN ANTONIO MEDICINE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our ofce to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national origin, or an intention to make such preference limitation or discrimination.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and ofer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.
Copyright © 2025 SmithPrint, Inc. PRINTED IN THE USA



TMA Insurance Trust’s agents have been advising and guiding Texas physicians through the complexities of properly protecting their incomes with disability insurance for seventy years. We recognize the importance of maintaining your income if you can’t practice due to illness or injury – and what it means to you, your family and your future. We are uniquely positioned to build the best income protection solution for your situation.
We have advised thousands of physicians across multiple generations on the best ways to protect their incomes. This has afforded us with knowledge and experience that you can beneft from. You see, to us you are unique, but your situation is not.
Are you just starting your career, or looking to increase your disability benefts? Should I consider a group plan or an individual policy? Do I need a short term or long term plan? Should I keep my current policy or replace it? Is there a beneft to stacking multiple policies? We are planning for a family; what are my considerations? How can I protect my salary as it grows over time or when it is higher than the limits companies will underwrite? We have answers and will devise a personalized income protection strategy for your situation and budget.

As a full-service insurance agency, we work with the leading individual disability insurance companies in Texas. And we developed TMA member plans with “Own Occupation” coverage so we have the product fexibility to protect more of your income affordably. Some of these plans come with discounts and there are additional savings for TMA members. Having this breadth of products and savings affords us more opportunities to enact the best possible income protection plan for you.
Unlike other insurance agents and brokers, our advisors do not receive any sales-based commissions. This ensures that our advice and recommendations are unbiased and focused solely on meeting your needs.
TMA Insurance Trust is well positioned to help you protect your income. Call an experienced advisor today and begin this important conversation. They can be reached Monday to Friday at 800-880-8181 between the hours of 8:00 AM and 5:00 PM CST, or by scanning the QR code with your mobile device. If you prefer, you can visit us online at tmait.org It will be our pleasure to serve you.


John Shepherd, MD, President
Lyssa Ochoa, MD, Vice President
Jennifer R. Rushton, MD, President-Elect
Lubna Naeem, MD, Treasurer
Lauren Tarbox, MD, Secretary
Ezequiel “Zeke” Silva, III, MD, Immediate Past President
Woodson “Scott” Jones, Member
John Lim, MD, Member
Sumeru “Sam” G. Mehta, MD, Member
M. “Hamed” Reza Mizani, MD, Member
Priti Mody-Bailey, MD, Member
Dan Powell, MD, Member
Saqib Z. Syed, MD, Member
Nancy Vacca, MD, Member
Col Joseph J. Hudak, MD, MMAS, Military Representative
Jayesh Shah, MD, TMA Board of Trustees Representative
John Pham, DO, UIW Medical School Representative
Robert Leverence, MD, UT Health Medical School Representative
Cynthia Cantu, DO, UT Health Medical School Representative
Lori Kels, MD, UIW Medical School Representative
Ronald Rodriguez, MD, UT Health Medical School Representative
Alice Gong, MD, Board of Ethics Representative
Melody Newsom, BCMS CEO/Executive Director
George F. “Rick” Evans, Jr., General Counsel
Melody Newsom, CEO/Executive Director
Yvonne Nino, Controller
Al Ortiz, Chief Information Ofcer
Brissa Vela, Chief Membership and Development Ofcer
Jacob Hernandez, Advocacy and Public Health
Phil Hornbeak, Auto Program Director
Betty Fernandez, BCVI Director
Jennifer C. Seger MD, Chair
Timothy C. Hlavinka, MD, Member
John Robert Holcomb, MD, Member
Soma S. S. Jyothula, MD, Member
George-Thomas Martin Pugh, MD, Member
Adam Ratner, MD, Member
John Joseph Seidenfeld, MD, Member
Amith Skandhan, MD, Member
Francis Vu Tran, MD, Member
Subhashini Valavalkar, MD, Member
Louis Doucette, Consultant
Brissa Vela, Staf Liaison
Gabriella Bradberry, Staf Liaison
Trisha Doucette, Editor
Ayomide Akinsooto, Student
Elizabeth Allen, Volunteer
Rita Espinoza, DrPH, Volunteer
Ramaswamy Sharma, MS, PhD, Volunteer

Dr. Andrew Nagy is a vascular and endovascular surgeon with nonsurgical and surgical experience. He is now accepting patients at our downtown and medical center o ces.





By John Shepherd, MD, President, Bexar County Medical Society
I never planned to be president of the Bexar County Medical Society. A decade ago, you would’ve found me in the operating room or at home with my family — avoiding extra commitments and thinking leadership roles in organized medicine were for someone else.
But my wife, Jenny, had other plans. Already deeply involved with the Texas Medical Association, TEXPAC and the Texas Medical Association Alliance, she patiently convinced me of the value of getting involved. With a little nudge (okay, maybe a big one), she showed me the tremendous impact we can have when we step up and engage.
Fast forward to today, and I !rmly believe that being involved in organized medicine isn’t just about personal growth or professional connections. It’s about shaping the future of our profession and ensuring our collective voice is heard. Because if we don’t speak up for ourselves and our patients, someone else will — and they may not fully understand the realities of what we do.
at’s why I’m especially grateful to the dedicated members of our BCMS Board of Directors who’ve stepped up to serve this year. Each of them made a choice — a choice to give their time, energy and perspective to something bigger than themselves. ey’ve said yes to extra meetings, complex policy discussions, and the kind of behind-thescenes work that rarely gets recognition but truly makes a di erence.

Swearing in the 2025 BCMS Offcers: Ezequiel “Zeke” Silva, III, MD, Immediate Past President; Lauren Tarbox, MD, Secretary; Lubna Naeem, MD, Treasurer; Lyssa Ochoa, MD, Vice President; Jennifer R. Rushton, MD, President-Elect; John Shepherd, MD, President

ese are busy physicians with full lives, yet they still make room to lead. eir commitment reminds me that leadership in organized medicine isn’t about having extra time — it’s about making time, because the work matters.
When I look around our boardroom, I don’t just see physicians; I see advocates, problem solvers and bridge builders — people who understand that the future of medicine doesn’t just happen to us, it’s something we help shape. Whether it’s addressing physician burnout, tackling legislative hurdles, preserving physician autonomy, or mentoring the next generation, the work of our board is deeply rooted in service. It starts with a simple but powerful question: “How can we help?” And then it’s followed by action. at kind of leadership doesn’t always come with recognition, but it comes with real, lasting impact.
And that impact is exactly why involvement matters. I know it’s easier to sit on the sidelines and assume someone else will step up. I’ve done that myself. But what I’ve learned — and what this board demonstrates so clearly — is that when we engage, we gain more than we give. We build a community that reminds us we’re not alone in the trenches. We amplify our voice when it matters most — not only to protect our profession, but to serve our patients better.

Bexar County Medical Society 2025 Board of Directors
Standing L-R: Melody Newsom, BCMS CEO/Executive Director; Woodson “Scott” Jones, MD; Alexander Arena, MD; John Pham, DO, UIW Medical School Representative; Ezequiel “Zeke” Silva, III, MD, Immediate Past President; Jayesh “Jay” Shah, MD, TMA Board of Trustees Representative. Seated L-R: Lauren Tarbox, MD, Secretary; Jennifer R. Rushton, MD, President-Elect; John Shepherd, MD, President; Lubna Naeem, MD, Treasurer; Lyssa Ochoa, MD, Vice President
One of the most important lessons I’ve learned is that you don’t need a formal title to make a meaningful contribution. You don’t have to be a board member or policy expert. You just need to care — and be willing to take the !rst step.
BCMS o ers a wide range of committees focused on everything from public health and legislative advocacy to medical education and physician wellness. ese committees are where the heart of our work gets done — and they o er incredible opportunities for connection, growth and real-world impact.
So, if you’ve been quietly supporting from the sidelines, I invite you to take the next step. Don’t just renew your membership — get involved. Join a committee. Come to a meeting. Reach out and ask where you can help. You don’t have to start big — just start somewhere. e more people who get involved, the stronger we become. We need new voices, fresh ideas and diverse experiences to meet the challenges ahead. Whether you’ve been practicing for three years or thirty, your perspective matters. Your involvement matters. Even the smallest step forward sends a powerful message: that physicians in Bexar County care deeply about the future of medicine and are willing to lead the way.
We don’t want to merely react to change — we want to shape it.
As we engage, we also carry the responsibility of spreading the word. Many physicians in our county don’t fully realize what BCMS does on their behalf — how we advocate at the Capitol, support medical students and residents, respond to public health crises, and stand up for our peers navigating an increasingly complex system. We can’t a ord to keep this work a secret.
It’s on us — those already engaged — to share this message. Over lunch, in hospital lounges or even on social media, we must help our peers understand the value of organized medicine. Because the more informed our members are, the more uni!ed and e ective we become.
To my fellow board members: thank you. Your dedication is more than appreciated — it’s inspiring. You represent the best of Bexar County physicians with compassion, integrity and the courage to lead, even when it’s inconvenient. e in$uence of organized medicine is only as strong as the people who participate in it. And I’m proud to serve alongside individuals who consistently rise to the occasion.
To everyone else reading this: I encourage you to !nd your place in this work. ere’s something for everyone. Your voice matters. Your experience matters. And your presence matters.
Let’s shape the future of medicine — together.
John Shepherd, MD, 2025 President of the Bexar County Medical Society, has been an active advocate for the Family of Medicine at the Texas State Capitol and has held several “Party of Medicine” events, introducing physicians on how to get involved with legislation that a ects medical issues. He has been Chief of Surgery at Christus Santa Rosa Children’s Hospital and a past member of the Board of Directors of Tejas Anesthesia. Dr. Shepherd is currently a Pediatric Anesthesiologist with University Medical Associates, and serves on the BCMS Legislative Committee and the Bexar Delegation to TMA.


By Sue Bernstein
It’s so important for us all to !nd a way to be active and create mental “space” not only to avoid burnout and stress-related illnesses, but to be happy! If you start with yourself, you can then inspire your family, employees or coworkers and patients. e answer for my husband, Dr. Eric Bernstein, and I has become hiking and visiting National Parks.
While navigating the twists and turns of raising three children, supporting our aging parents, and running our private medical practice and other businesses, the path of least resistance was to neglect ourselves and our health. Our feeling of overwhelm was growing while our energy waned. We wanted to be more intentional with our choices and be role models for those around us. But how would we make that change?
Eric and I were both inspired and awed in our youth by visits to U.S. National Parks and other experiences in nature with our families, and realized that we had put that on the back burner for too long. Now, over the past several years, our passion for hiking and exploring has blossomed again and brings us so much joy both in and out of the o%ce!
It started with a quick trip with our children to Phoenix’s Camelback Mountain to whet our appetites. It worked! We then started exploring our local city and state parks as it was hard to travel, and we wanted to feel the same serenity and positive energy we felt on the trail more regularly. We did everything from weekend day hikes to !nding 30 minutes a&er work to simply “get out there.” We realized that if we kept our shoes, water and sunblock in our cars, we could literally pull over and have an amazing break even on our busiest days. Some of our favorite local places are Eisenhower Park, Friedrich Wilderness Park and Government Canyon State Natural Area. We also love San Antonio’s Greenway Trail System of biking and hiking trails that twist and turn in and around the city — truly an underutilized local gem!
We expanded our journey with an ambitious road trip to the Rocky Mountains, Arches, Canyonlands, Grand Canyon and Zion National Parks (all in 10 days!). We were hooked! We then suggested to our extended family that we plan gatherings together in nature, which took us to places including the Smoky Mountains, the Poconos and Lake Tahoe. Our family relationships blossomed as we prioritized having fun and being healthier together. We also started adding hiking excursions to all of our vacation and business trips, including New York, Chicago, Atlanta and, most recently, Saguaro National Park/ Tucson for our wedding anniversary.
We notice that people we meet on trails always seem refreshed and happy and we feel that way, too. Of course, connecting to nature and
being active are proven scienti!cally to help with stress, but experiencing it regularly is another level entirely.
We recently decided to expand our passion to our everyday work life to inspire ourselves and others by out!tting our medical practice o%ces with gorgeous National Park and nature photos. e images are a hit with patients and a great talking point.
We encourage you to take a step towards something that you enjoy that will increase your activity and provide some fun and stress relief. Find a way to incorporate that joy into your everyday life to help you feel more refreshed and alive!

Sue Bernstein, MS, is Director of Business Development at San Antonio Family Physicians, a Healthy Lifestyle Transformation Coach and a current member of the Bexar County Medical Society Alliance.




By Nora Vasquez, MD, Certifed High-Performance Coach for Physicians, Healthcare Professionals and Executives
Being a physician isn’t just a job — it’s a calling. It requires so much of you: your mind, your heart, your time and your energy. e long days, endless decisions and emotional toll of caring for others can leave even the most passionate clinicians and leaders feeling drained, discouraged and disconnected — especially by the time you walk through the door at home.

As an internist and leader, I know that feeling well. I’ve experienced mental and emotional exhaustion, and the question we o&en ask ourselves a&er a long day: How do I keep doing this without burning out?
at’s what inspired me to share what helped me begin to shi& from mental and emotional depletion to a sense of empowerment. ese powerful habits helped me reclaim my energy, reset my mindset, and show up with more presence — for my patients, my team and my family. I am con!dent they will help you, too.
e !rst big shi& for me wasn’t about doing more — it was about being more intentional. I stopped starting my day on autopilot and instead asked myself: “Who do I want to be today — for my patients, my team and my family?”
That single question helped me reconnect to my purpose and gave me control over my mindset — even when the day got stressful.
Try is:
• Before your workday starts, choose 1–2 words that describe the energy you want to bring (e.g., calm, focus, compassion).
• Between tasks or meetings, take a 60-second pause to breathe deeply and repeat those words to yourself.
• Use small cues (like walking through a doorway) to reset: “Who do I want to be on the other side of this moment?”
A physician I coached chose the words present and calm each morning. Even on packed days, this helped him stay grounded, listen fully, and avoid the guilt of being rushed or reactive.
One of the most helpful things I ever did was stop letting the end of the workday “just happen.” I created a simple, intentional transition ritual to shi& gears.
During my commute, I used that time with purpose — sometimes calling an encouraging friend, other times parking and taking a brief walk around the block to breathe and clear my mind.
Before stepping into the house, I’d ask: “What do I need to take good care of me right now?”
Everything shifted by listening to and attending to my own emotional, mental and physiologic needs each day. I began to
extend compassion to myself and prioritize my own well-being. I released frustration and resentment. I learned that by fulfilling my own needs, I had more energy and stamina to be present for my loved ones, too.
en, I’d ask: “Who do I want to be when I walk through this door?”
Instead of bringing in frustration and fatigue, I’d choose a word like grateful, loving or fun. at small reset changed how I received and embraced my kids and how I communicated with my husband.
Try is:
• Take 5–10 minutes at the end of your day to pause — sit in your car, walk in the sunshine outside, or listen to your favorite song.
• Re$ect on one thing that went well or someone you helped.
• Choose your “home energy” word. Say it to yourself, breathe it in, and let that version of you walk in the door.
A nurse practitioner I worked with used to walk in frustrated from work and snap at her family. When she began pausing and choosing the words lovingconnection, she shi&ed her energy. Her relationships improved, her evenings felt calmer and her family responded more positively — because she led with connection instead of frustration and exhaustion.

Habit 3: Protect Your Energy by Reducing Decision Fatigue
It’s not just the physical work that drains us — it’s the mental load. Physicians make hundreds of decisions a day, and by the time we get home, even simple questions like, “What’s for dinner?” can feel triggering.
So, I started simplifying. I made decisions in advance, shared the load, and created systems to protect my mental energy.
Try is:
• Batch decisions weekly: meals, out!ts, workouts, schedules before the week begins.
• Outsource: grocery ordering, housework, yardwork, appointment scheduling.
• Delegate: huddle with your team to enhance communication, assign tasks, and improve work$ow e%ciency.
• Create healthy boundaries with simple rules:
• “A&er6:00p.m.,Idon’tcheckworkmessagesunlessurgent.”
• “IwriteandcompletemynoteswhileI’mwitheachpatient.”
• “IfI’mtootiredtocook,weordertakeout—andthat’sokay.”
• Use your highest-energy hour (o&en in the morning) for your hardest or most important work. Huddle each day with your team so they know when to bring questions or paperwork to sign at this appointed time to avoid multiple interruptions throughout the day.
Case Study:
I helped a busy hospital leader create a daily “shutdown checklist”:
1. Write one win a day and celebrate to feel accomplished and encouraged.
2. Set three priorities for tomorrow.
3. Close the laptop.

is one habit saved her over 30 minutes of worrying and overthinking each night — and helped her relax and fall asleep more easily.
You Deserve to Love Your Life and Leave Work Feeling Accomplished and Energized
e work you do is meaningful, demanding and nonstop. We can honor the struggle and also prioritize our wellness. You can take back control of your energy. You can create intentional habits that support your peace and presence. And you can walk through the door at the end of the day feeling accomplished and proud of your impact and contributions.
Start small:
• Choose a word in the morning.
• Take a 60-second pause between tasks.
• Give yourself !ve quiet minutes before walking in the door to set your intentions.
ese tiny shi&s create powerful results over time. ey remind you that you’re not powerless — you have in!nite capacity and resourcefulness, and your peace and well-being are worth protecting.
Want more support?
If you’re ready to create more harmony, energy and joy in your work and life, join us for our next Physician Leadership & Wellness Masterclass Visit www.renewyourmindmd.com/renewed for details, or scan the QR Code to sign up. Saturday, May 17, 2025

SAVE THE DATE:
A Wellness Retreat for Physicians, Spouses and Colleagues! Join us for the frst Recharge and Reconnect Wellness Retreat.
Bexar County Medical Society 4334 N Loop 1604 W, Suite 200 San Antonio, TX 78249


Nora Vasquez, MD, CHPC, is a triple Certified HighPerformance Coach for Physicians, APPs and Executives. Dr. Vasquez is a board-certi ed Internist with over a decade of experience. She is the Chair of the Physician Wellness Committee for the Bexar County Medical Society and serves on the Texas Medical Association’s Council for Member Experience. Dr. Vasquez developed the Physician Coaching and Wellness Masterclass Series for BCMS physician members to empower healthcare professionals with evidence-based coaching strategies to mitigate burnout and enhance their well-being. You can learn more about Dr. Nora Vasquez at www.renewyourmindmd.com/renewed or email her at renewyourmindmd@gmail.com. Dr. Vasquez in a member of the Bexar County Medical Society.

“Ha ppy families are a alike; every unhappy family is unhappy in its own way.”
- Leo Tolstoy, “Anna Karenina”
By Holly Day, MD
Recent years have seen much interest in characterizing and addressing the “unhappiness” in our healthcare “family.” e term used most commonly to describe this unhappiness — “burnout” — was !rst de!ned in the 1970s by psychologist Dr. Christina Maslach as a syndrome of emotional or mental exhaustion, depersonalization or detachment from work, and a reduced sense of personal accomplishment, which arises as a prolonged response to chronic job-related stressors. 1 While studies have shown that large segments of the physician population experience burnout, e orts to meaningfully address it have been hampered by the complex interplay of factors contributing to high burnout rates, and lack of systemic investment in meaningful changes to facilitate wellness in our healthcare workforce.
Burnout among physicians has been a prevalent and persistent problem over the past decade in the U.S. healthcare industry, and it was heavily exacerbated by the widespread su ering of the COVID-19 pandemic. A group of researchers has been tracking the rates of burnout among U.S. physicians and the broader U.S. workforce using a statistically rigorous survey methodology every three years since 2011. Our community saw a previous peak in 2014, with 54.4% of U.S. physicians experiencing burnout, but during the height of the pandemic we far surpassed this, with burnout rates rising to 62.8% in 2021. at year also saw the highest reports of disillusionment and regret with career choice, as just over half of the physicians surveyed (57.1%) reported that they would still choose to become physicians, if they could go back and choose again. As our nation has begun to recover from the COVID-19 pandemic, we have seen some improvement in these measures — in the 2023 survey, burnout rates had dropped back down to 45.2%, and 65.1% of physicians surveyed stated that they would choose this career again if given a second chance. However, physicians still show much higher rates of burnout than the general U.S. working population — we are about twice as likely to experience high levels of emotional exhaustion (odds ratio 2.08), depersonalization (OR 1.94) and overall burnout (OR 1.82 a&er adjusting for hours worked per week, gender, age and relationship status).2
Such high levels of job dissatisfaction and disillusionment among U.S. physicians pose a serious problem, not only because of the su ering of the workers struggling with burnout, but also because of the costs borne by patients and the larger healthcare system. When patients are cared for by a physician experiencing burnout, they may experience a decline in the quality of communication, their perception of the physician-patient relationship, and overall satisfaction with the care provided., Multiple surveys of physicians and healthcare providers have found a correlation between burnout and higher rates of perceived medical errors or patient-safety issues.4,5,6 A limitation of many of these studies is that they rely on the participants’ subjective assessment of patient-safety, or recall of medical errors, but there have also been a limited number of studies with objective data to demonstrate that higher burnout rates
correlate with worse patient outcomes. For instance, a 2015 study across 54 intensive care units in Switzerland, tracked burnout and workload among the ICU nursing and physician sta , as well as objective data on patient length of stay and standardized mortality ratios. ey found that emotional exhaustion among the sta correlated with an increased mortality risk, and higher workloads for the sta were correlated with increased patient length of stay in the ICU.7
Apart from the costs borne by patients when physicians su er high levels of burnout, the wider healthcare system bears a !nancial cost. Burnout has been correlated with decreased clinical productivity via reduced clinical time, increased use of sick leave, and increased physician turnover.( One model published in the Annals of Internal Medicine in 2019 estimated that physician turnover and reduction in clinical hours related speci!cally to burnout costs the U.S. healthcare industry about $4.6 billion dollars per year, and that individual organizations may see costs of about $7600 per physician per year.)
What can be done to combat physician burnout and promote wellness in our healthcare system? Part of the challenge in addressing burnout is the multitude of factors that have been shown to play into it. From the excessive workloads placed on physicians, to strict time pressures, high administrative burdens, poor work$ow conditions, moral distress and loss of autonomy10 — the list of work stressors leading to physician burnout is as long as the list of infectious pathogens that can cause a fever. Given the overwhelming array of systemic causes that need to be addressed, it is not surprising that healthcare institutions and researchers have found it more appealing to invest in exploring interventions to combat burnout on an individual level. A meta-analysis in the Lancet in 2016 showed that programs focused on stress-management and selfcare, communication skills training, mindfulness initiatives and smallgroup exercises can have meaningful impacts on the wellbeing of the participants. In particular, mindfulness-based trainings were shown to have a modest, but statistically signi!cant impact on emotional exhaustion and depersonalization scores assessed with the Maslach Burnout Inventory (with 4.68 point and 2.01 point decreases respectively).11 However, there is a limit to the e%cacy of building up resilience among physicians to combat burnout — a 2020 study in JAMA demonstrated that even among physicians with the highest resilience scores, 29% were still experiencing burnout.12 Considering that average U.S. workers have experienced largely steady rates of burnout around 28% since 2011,2 this is a strong testament to the demands of healthcare as a profession, and demonstrates the need to start approaching physician wellness from the other side of the equation: the healthcare system.
Research on larger-scale, systemic interventions to reduce burnout and promote wellness is, sadly, sparse. In the same Lancet systematic review and meta-analysis, as well as another published in JAMA the following year, both groups of researchers found that about 60% of their
included studies analyzed individually-focused interventions, while only 40% looked at systems-based interventions (20 studies total in the !rst paper, 7 in the second).11,13 However, both analyses showed that system-based interventions had larger e ect-sizes in reducing burnout compared to individually-focused interventions. e JAMA paper speci!cally demonstrated in subgroup analysis that individually-focused interventions achieved a standardized mean di erence of -0.18 in reducing physician burnout rates, while system-based interventions achieved a standardized mean di erence of -0.45, which was statistically signi!cant.13 e types of interventions varied signi!cantly across studies, with a large portion of data coming from cohort analyses of the e ects of the 2003 resident duty-hour restrictions (which saw a reduction in resident burnout rates from 62% to 50%).11 Other studies focused on scheduling changes to combat burnout, such as reducing the number of continuous days on service, changing to shi&-work from 24-hour calls, or providing protected time to sleep during a 24-hour call.13 Not surprisingly, these interventions to reduce the overall workload expected of physicians, or to transition to more physiologically-humane schedules, had signi!cant positive impacts on physician wellness. While system-level interventions to reduce physician workload in general may have signi!cant cost-barriers to implementation, the improvements in burnout seen with relatively simple scheduling adjustments represent a potentially cost-neutral opportunity to improve wellness on a broader scale.
ere still exists a broad range of systemic-interventions that could be implemented to improve physician wellness, from removing stigma and improving mental healthcare access, to reducing compliance and regulatory burdens, setting more reasonable productivity expectations, and utilizing technological advances to reduce workload and preserve physicians’ time at the bedside, among many other theoretically-promising possibilities. e National Academy of Medicine outlined a 106page National Plan in 2022 to advocate for the implementation of these system-wide interventions to preserve the wellness and integrity of our country’s physician workforce.14 ough achieving policy-changes on such a broad scale will likely be a slow process, this was an important !rst-step in directing national e orts to improve working conditions for U.S. physicians. Perhaps most important is the need for additional funding to provide rigorous research proving the e%cacy, necessity and cost-e ectiveness of these systemic interventions. Given the high costs of physician burnout, we have a moral and practical imperative to restructure our healthcare system towards improving physician wellness, not just for the sake of our physicians, but for our patients and society.
References:
1. Maslach, C., Schaufeli, W.B., & Leiter, M.P. (2001). JOB BURNOUT. Annual Review of Psychology, 397. https://link-gale-com. libproxy.uthscsa.edu/apps/doc/A73232715/HRCA?u=txshracd2607&sid=bookmark-HRCA&xid=4e70ee0e
2. Shanafelt, T.D., West, C.P., Sinsky, C., Trockel, M., Tutty, M., Wang, H., Carlasare, L.E., & Dyrbye, L.N. (2025). Changes in Burnout and Satisfaction With Work-Life Integration in Physicians and the General US Working Population Between 2011 and 2023. Mayo Clinic proceedings, S0025-6196(24)006682. Advance online publication. https://doi.org/10.1016/j. mayocp.2024.11.031
3. Dewa, C.S., Loong, D., Bonato, S., & Trojanowski, L. (2017). e relationship between physician burnout and quality of healthcare in terms of safety and acceptability: a systematic review. BMJ open, 7(6), e015141. https://doi.org/10.1136/ bmjopen-2016-015141
4. Hall, L.H., Johnson, J., Watt, I., Tsipa, A., & O’Connor, D.B. (2016). Healthcare Sta Wellbeing, Burnout, and Patient Safety: A Systematic Review. PloS one, 11(7), e0159015. https://doi. org/10.1371/journal.pone.0159015
5. Salyers, M.P., Bon!ls, K.A., Luther, L., Firmin, R.L., White, D.A., Adams, E.L., & Rollins, A.L. (2017). e Relationship Between Professional Burnout and -uality and Safety in Healthcare: A Meta-Analysis. Journal of general internal medicine, 32(4), 475–482. https://doi.org/10.1007/s11606-016-3886-9
6. Shanafelt, T.D., Balch, C.M., Bechamps, G., Russell, T., Dyrbye, L., Satele, D., Collicott, P., Novotny, P.J., Sloan, J., & Freischlag, J. (2010). Burnout and medical errors among American surgeons. Annals of surgery, 251(6), 995–1000. https://doi.org/10.1097/ SLA.0b013e3181bfdab3
7. Welp, A., Meier, L.L., & Manser, T. (2015). Emotional exhaustion and workload predict clinician-rated and objective patient safety. Frontiers in psychology, 5, 1573. https://doi.org/10.3389/ fpsyg.2014.01573
8. Shanafelt, T.D., Mungo, M., Schmitgen, J., Storz, K.A., Reeves, D., Hayes, S.N., Sloan, J.A., Swensen, S.J., & Buskirk, S.J. (2016). Longitudinal Study Evaluating the Association Between Physician Burnout and Changes in Professional Work E ort. Mayo Clinic proceedings, 91(4), 422–431. https://doi.org/10.1016/j. mayocp.2016.02.001
9. Han, S., Shanafelt, T.D., Sinsky, C.A., Awad, K.M., Dyrbye, L.N., Fiscus, L.C., Trockel, M., & Goh, J. (2019). Estimating the Attributable Cost of Physician Burnout in the United States. Annals of internal medicine, 170(11), 784–790. https://doi. org/10.7326/M18-1422
10. National Academies of Sciences, Engineering, and Medicine. 2019. Taking action against clinician burnout: a systems approach to professional well-being. Washington, DC: e National Academies Press. https//doi.org/10.17226/25521. pages 85 - 106.
11. West, C.P., Dyrbye, L.N., Erwin, P.J., & Shanafelt, T.D. (2016). Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet (London, England), 388(10057), 2272–2281. https://doi.org/10.1016/S01406736(16)31279-X
12. West, C.P., Dyrbye, L.N., Sinsky, C., Trockel, M., Tutty, M., Nedelec, L., Carlasare, L.E., & Shanafelt, T.D. (2020). Resilience and Burnout Among Physicians and the General US Working Population. JAMA network open, 3(7), e209385. https://doi. org/10.1001/jamanetworkopen.2020.9385
13. Panagioti, M., Panagopoulou, E., Bower, P., Lewith, G., Kontopantelis, E., Chew-Graham, C., Dawson, S., van Marwijk, H., Geraghty, K., & Esmail, A. (2017). Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-analysis. JAMA internal medicine, 177(2), 195–205. https://doi.org/10.1001/jamainternmed.2016.7674
14. National Academy of Medicine. 2022. National Plan for Health Workforce Well-Being. V. J. Dzau, D. Kirch, V. Murthy, and T. Nasca, editors. NAM Special Publication. Washington, DC: e National Academies Press. https://doi.org/10.17226/26744.

Holly Day, MD, is a board-certi ed Hospitalist who joined UT Health San Antonio as an Assistant Professor/Clinical in August 2018. She has had a personal and professional interest in compassion and wellness in medicine throughout her career. She was recognized as a two-time recipient of the “Gold Foundation Humanism and Excellence in Teaching Award” (2017, 2018), and recently was awarded the Division of Hospital Medicine’s “Clinician of the Year” award in recognition of her superlative patient care. Dr. Day is a member of the Bexar County Medical Society.

By Alison Bartak and Ramaswamy Sharma, MS, PhD
Healthcare employees, numbering 17 million in 2023, make up the largest employment sector in the United States. Yet, workplaces for healthcare professionals can be highly stressful environments due to a number of reasons: high workload involving an overwhelming number of patients; long unusual hours; potential for fatal errors; shi& work, which disrupts sleep patterns; excessive administrative burdens due to complex healthcare regulations that are further complicated by understa%ng; professional expectations that limit taking breaks and vacations; and emotional as well as traumatic strain due to close interaction with sickness and death on a regular basis. Together, these conditions of physical, mental and emotional exhaustion increase the risks of fatigue and burnout if not mitigated. Indeed, e Physicians Foundation’s 2024 Survey of America’s Current and Future Physicians reported that 60% of physicians experienced burnout, which is almost double that of the general population; this number has not changed in the past four years. Yet, 40% of physicians do not seek help for mental health for fear of having to report it in licensure and credentialing applications. Healthcare consolidation is further negatively impacting physicians.
With businesses constantly on the lookout for ways to optimize and sustain maximal productivity, a commonly overlooked asset involves employee health strategies. Workforce productivity and value provided per employee closely correlates with the health and wellness of the employee. A report in the AmericanJournalofPreventiveMedicine calculated a yearly cost between $3,999 for an hourly worker to $20,683 for an executive due to burnout and its ensuing loss in productivity; burnout costs per physician averages to $7,600. Decreased hours, high physician turnover and costs associated with new recruitments were estimated to range from $2.6 billion to $6.3 billion per year in 2019 — this number does not include e ects related to medical errors, malpractice-related lawsuits, and loss of current patients who may not feel supported. Understanding the value of workplace health initiatives is imperative for professional sustainability and organizational success, whether one is a private practice owner seeking to optimize a current medical practice or an employed physician navigating complex work dynamics. is article explores the importance of investing in health deliverables as “triple dividends,” which enhance business performance, strengthen organizational stability, and foster a resilient company culture.
e !nancial performance and pro!tability of a business is a measurable impact of their employee health initiatives. When businesses have employees experiencing health issues, costs multiply far beyond the medical expense due to increased healthcare premiums, workers’ compensation claims and disability management, as well as productivity loss associated with either absent employees (absenteeism) or with employees working when still injured or ill (presenteeism). e
converse is also true. Deloitte calculated that purely a $1 investment into mental health and wellness programs resulted in an average return of $1.62 through increased productivity and decreased presenteeism. Johnson & Johnson saved $2.71 for every dollar spent on their employee wellness program from 2002 to 2008 while also increasing productivity due to employees working with higher energy, focus and greater resilience. Moreover, a metanalysis of 22 studies conducted by the American Journal of Health Promotion showed that the implementation of wellness initiatives within workplaces reduced employee absenteeism by 25% and increased productivity by 22%. e return on investment from well-designed health initiatives consistently appears to outweigh the costs associated with implementing these programs.
In addition to !nancial results, the implementation of wellness initiatives strengthens organizational resilience and position within the market. Knowledge preservation and workforce stability are important pillars of organizational structures, especially when there is a dearth of physicians. e cost of turnover — replacing a skilled and e%cient employee — ranges from 150-200% of their annual salary, which includes recruitment, training and lost productivity time. us, it is imperative that trained and experienced personnel continue to provide value without developing any premature health issues that could potentially lead to irreplaceable loss of accumulated knowledge and productivity. By incorporating wellness initiatives, businesses can solidify workforce stability and ensure a positive organizational reputation by focusing on employee wellbeing. For example, businesses providing disability accommodation for employees experiencing serious health conditions had an 87% retention rate. ese transparent approaches centered around employee health and wellness could further enhance their recruitment and retention advantages and o er them a competitive edge in their business.
e third dividend of the employee health initiative approach is based on organizational culture and regulatory standing. e most profound impact of health initiatives for an individual is the development of a company culture where individual employees feel genuinely valued. Cultural sensitivity, demonstrated by awareness and respect for diverse cultural beliefs, values, lifestyles, languages and narratives within the organization and enforced by regular feedback and commitment from leadership, will promote inclusivity and retention. Businesses that rank highly on compassionate leadership indices had a 34% increase in employee engagement and a 26% decrease in employee turnover. Beyond ethical and humanitarian concerns, businesses have a legal obligation regarding an employee’s health and safety. is is important for physicians who are exposed on a regular basis to infectious diseases and hazardous materials.
When attempting to capture these triple dividends, businesses should consider a strategic approach to employee health by:
1. Assessing current health risks using anonymized health data, surveys, operational metrics and calculating costs
2. Developing a comprehensive strategy with integrative approaches addressing physical, mental and social wellbeing of the employee
3. Assigning leadership with visible executive support for wellness programs indicating organizational priority
4. Implementing workplace changes that make these integrative approaches easier by creating a dedicated wellness team that o ers screenings, tailored onsite programs, mental health support, social and !nancial wellness programs, wellness stipends, and workshops
5. Embedding a culture of wellness
6. Tracking participation metrics and outcomes as well as analyzing employee feedback and adjusting accordingly.
ere is an o&en-hidden opportunity in investing in employee health deliverables to enhance business performance, strengthen organizational stability, and foster a resilient company culture. Reducing health risks within the workforce may boost competitive advantage through improved !nancial performance within the company, organizational stability, and cultural resilience and strength.
References:
1. American Medical Association (2024, October 31). AMA Physician Well-Being Program. https://www.ama-assn.org/ practice-management/physician-health/ama-physician-well-being-program
2. Berg, S. (2020, May 28). e 12 factors that drive up physician burnout. American Medical Association. https://www. ama-assn.org/practice-management/physician-health/12-factors-drive-physician-burnout?form=MG0AV3&form=MG0AV3
3. Berry, L.L., Mirabito, A.M., & Baun, W.B. What’s the Hard Return on Employee Wellness Programs? Harvard Business Review. 2010 Dec;88(12):104-12, https://hbr.org/2010/12/ whats-the-hard-return-on-employee-wellness-programs
4. Deloitte. (2020). e ROI in workplace mental health programs: Good for people, good for business. In A Blueprint for Workplace Mental Health Programs. https://www2.deloitte.com/ content/dam/Deloitte/ca/Documents/about-deloitte/ca-enabout-blueprint-for-workplace-mental-health-!nal-aoda.pdf
5. Freer, E. (2021, November). Self-Investment: Physician Wellness Programs Bolster a Beleaguered Workforce. Texas Medical Association. https://www.texmed.org/Self-Investment/
6. Hayes, J., II. (2024, May 7). 82% of the workforce is at risk for burnout. Here’s what CEOs can do. Forbes. https://www.forbes. com/sites/julianhayesii/2024/04/29/82-of-the-workforce-is-atrisk-for-burnout-heres-what-ceos-can-d0/
7. Hayes, J., II. (2025, March 17). Employee burnout: the hidden threat costing companies millions. Forbes. https://www.forbes. com/sites/julianhayesii/2025/03/17/employee-burnout-the-hidden-threat-costing-companies-millions/
8. Martinez, M.F., O’Shea, K.J., Kern, M.C., Chin, K.L., Dinh, J.V., Bartsch, S.M., Weatherwax, C., Velmurugan, K., Heneghan, J.L., Moran, T.H., Scannell, S.A., John, D.C., Shah, T.D., Petruccelli,
S.A., White, C., Dibbs, A.M., & Lee, B.Y. (2025). e health and economic burden of employee burnout to U.S. employers. American Journal of Preventive Medicine. https://doi.org/10.1016/j. amepre.2025.01.011
9. Mitchell, R.J., & Bates, P. (2010). Measuring Health-Related productivity loss. Population Health Management, 14(2), 93–98. https://doi.org/10.1089/pop.2010.0014
10. National Center for Health Workforce Analysis. (2024). State of the U.S. Health Care Workforce, 2024. https://bhw.hrsa.gov/ sites/default/!les/bureau-health-workforce/state-of-the-healthworkforce-report-2024.pdf
11. Neira, M. (2010). Healthy workplaces: a model for action. World Health Organization https://iris.who.int/bitstream/handle/10665/44307/9789241599313_eng.pdf?sequence=1
12. Powell, A. (2019, July 12). Study: Doctor burnout costs health care system $4.6 billion a year. Harvard Gazette. https://news. harvard.edu/gazette/story/2019/07/doctor-burnout-costshealth-care-system-4-6-billion-a-year-harvard-study-says/
13. Reilly, C. (2020, June 9). Wellbeing positively impacts !rm performance. Forbes. https://www.forbes.com/sites/colleenreilly/2020/06/09/wellbeing-positively-impacts-!rm-performance/
14. Rojanasarot, S., Bhattacharyya, S.K., & Edwards, N. (2023). Productivity loss and productivity loss costs to United States employers due to priority conditions: a systematic review. Journal of Medical Economics, 26(1), 262–270. https://doi.org/10.1080 /13696998.2023.2172282
15. Roy, C. (2025, February 27). Establishing an e ective wellness program for hospitals and HR leaders. inHealth Strategies. https://inhealth4change.com/hospital-wellness-programs-reduce-burnout-improve-health-and-lower-costs/
16. Rowland, S. (2023, October 3). Reducing absenteeism through employee wellness initiatives. Wisterm. https://wisterm.com/ insights/employee-bene!ts/reducing-absenteeism-through-employee-wellness-initiatives/
17. Society for Human Resource Management (SHRM). (2024.). Employee Bene!ts survey. https://www.shrm.org/topics-tools/ research/employee-bene!ts-survey
18. e Physicians Foundation. (2024, September 17). Examining physician, resident and student wellbeing and impact of the current healthcare landscape. https://physiciansfoundation. org/research/examining-physician-resident-and-student-wellbeing-and-impact-of-the-current-healthcare-landscape/
19. Unsal, N., Weaver, G., Bray, J.W., Bibeau, D., & Saake, G. (2020). Return on investment of workplace wellness: Evidence from a long-term care company. Workplace Health & Safety, 69(2), 81–90. https://doi.org/10.1177/2165079920953052 e


Alison Bartak is a medical student at the University of the Incarnate Word School of Osteopathic Medicine, Class of 2027. Her current interests include Preventative Medicine and Surgery.
Ramaswamy Sharma, MS, PhD, is a Professor of Histology and Pathology at the University of the Incarnate Word School of Osteopathic Medicine. He is interested in delineating the multiple molecular and cellular roles of melatonin in maintaining our quality of life. Dr. Sharma serves on the BCMS Publications Committee.


By Jorge Alvarez, MD, FACC, FSCAI
As a cardiologist, I am routinely asked for recommendations regarding exercise. Unfortunately, more o&en than not, it’s a&er a signi!cant event has already occurred. Regular exercise has been shown to have a wide range of health bene!ts. ere is even evidence to suggest a sedentary lifestyle may be a stronger predictor of mortality than established risk factors like smoking, hypertension and diabetes. Epidemiologic studies demonstrate that un!t individuals are two to three times more likely to die during follow-up compared to their more !t counterparts regardless of their risk pro!le, body habitus or presence of cardiovascular disease.
Because physical inactivity is a modifiable risk factor, clinicians should routinely assess and prescribe structured exercise and increased lifestyle activity to all patients. Often, as physicians we fall short when it comes to giving formal advice about exercise. I like to start by understanding my patient’s goals. Is it for general health, or specifically for prevention and management of disease like cardiovascular disease, obesity, diabetes and mental health? Once goals are established and understood, then prescribing should be easier. I often incorporate the FITT mnemonic into my
patients’ “prescriptions”: Frequency – number of days per week; Intensity – moderate or greater; Time – number of minutes per session; and Type – aerobic activity of choice.
Abundant evidence suggests that spreading the total weekly time for aerobic exercise across three or more days produces consistent health benefits and decreases the risk of injury. Increasing the intensity of aerobic exercise can produce similar benefits in a shorter period. As an example, 15 minutes of jogging appears to confer the same health benefit as 30 minutes of moderate-intensity walking. The time required for aerobic exercise each week depends on both frequency and intensity. Benefits can be accrued in many ways and a flexible approach is encouraged. Bouts of exercise can be performed in 30- to 60-minute blocks or accumulated throughout the day in five to 10-minute periods using a wide range of activities to achieve exercise goals. Walking is often considered the default activity for a beginning aerobic exercise prescription because it is simple, requires no equipment, and is easily measured by time, distance or step count. Although walking may be easiest for beginning exercisers, any comparable activity performed at a moderate pace and for the same total duration provides similar health benefits to brisk walking. Activities such as bicycling, water aerobics, doubles tennis or pickleball, ballroom dancing, or gardening can be done to satisfy weekly exercise goals.
As with taking prescription medications, getting patients to comply with an aerobic exercise prescription can be challenging. Often the major barrier is the perceived lack of time due to competing work and family responsibilities. When patients say they cannot find time to exercise, I often give specific recommendations such as using a workday walking routine. To start the day, they can park their car farther away from their place of work and walk 10 minutes to their worksite. At lunchtime, they could walk five minutes away from work and five minutes back before eating lunch. At the end of the day, taking that same 10-minute route back to their car completes their minimum recommended daily exercise.
Alternatively, if exercise during the week is not possible, taking 75-minute walks on Saturday and on Sunday appears to provide similar health benefits as the same total amount of walking during the week. Again, increasing workout intensity delivers the same benefit in less time. I often encourage my patients to find a partner to exercise with or join a group exercise program. This makes exercising more social and fun and increases the likelihood that they’ll keep it up. Joining a group of like-minded exercisers, such as a walking group or pickleball league, or a gym can provide necessary encouragement and support. For some, a home exercise program works best. When time is short, being able to jump on a stationary bicycle or treadmill without driving to a gym is a great solution.
Another approach to helping patients perform regular aerobic exercise is using a phone app or online fitness program. Such programs range from yoga to aerobics to resistance exercise circuit training. Participants should be sure, however, that the program they choose is appropriate for their fitness level, goals and includes
proper instruction about exercise technique. Joining a local gym or working with a qualified fitness coach can be extremely helpful for some patients who are struggling to start an exercise program.
As physicians, we should advocate a flexible approach to incorporating activity in our patients’ lives and recommend using whatever methods are best suited to individual constraints — especially in the context of the workplace. Moderate to vigorous physical activity, corresponding to any activity of least three metabolic equivalents (METs), has been consistently shown to reduce the health risks associated with chronic diseases and the risk of developing them. Other reports suggest that replacing sedentary time with even brief periods of light physical activity (approximately two minutes per hour) may confer a survival benefit. Accordingly, frequent bouts of light to moderate activity can improve health, especially if the total energy expenditure is comparable to shorter periods of more strenuous physical exertion. So, the deskbound worker who jogs 30 minutes on three days per week may not derive any greater exercise benefits than the worker who does frequent bouts of light to moderate physical activity throughout the day. In addition to encouraging my patients to park their car farther from the workplace and walk, I recommend standing or walking desks to reduce sitting time, which is associated with increased morbidity and mortality; replacing e-mails or phone calls with personal visits; and holding standing or walking meetings instead of sitting.
Once a patient has started an exercise program, I like to have a plan for encouraging their continued participation and monitoring their health. The schedule for this kind of surveillance will vary depending upon patient age, comorbidities and possibly the intensity of their exercise regimen. Strategies for improving compliance and incorporating more exercise into the workday should be encouraged. Ultimately, our goal for helping patients achieve control and overcome disease does not always have to be in the form of a pill.

Jorge Alvarez, MD, FACC, FSCAI, is an Interventional and Structural Heart Disease Cardiologist board certi ed in cardiovascular disease and interventional cardiology, and he practices out of Methodist Cardiology Clinic of San Antonio’s Medical Center location. Always on the leading-edge of advances in cardiovascular science and technology, Dr. Alvarez was among the rst in the region to perform transcatheter aortic valve replacements (TAVR). He also performs minimally-invasive, catheter-based procedures to repair other structural heart defects like atrial septal defects and mitral regurgitation, and to treat atrial brillation (AFib) with the Watchman™ le atrial appendage occlusion device to prevent strokes in patients who cannot take Coumadin (warfarin). His passion for heart disease prevention is re ected in his extensive community e orts to inspire and motivate San Antonians to eat healthy and be more physically active. Dr. Alvarez is a member of the Bexar County Medical Society.

By Manpreet S. Chhabra, MD
With screen use now embedded into nearly every aspect of everyday living, digital devices have become essential tools but they also present signi!cant challenges to visual health. From laptops and tablets to smartphones, prolonged exposure to digital screens is increasingly linked to eye discomfort and fatigue. Understanding how to support and maintain eye health in this digital era is essential for sustained productivity and overall wellness.
Digital Eye Strain, also referred to as computer vision syndrome, is one of the most common issues reported by working professionals. Symptoms can range from dry or irritated eyes to headaches and difficulty focusing. For many, these signs accumulate gradually throughout the day, affecting not only comfort but also focus and performance.
Before the pandemic, it was estimated that at least half of all adults experienced symptoms of Digital Eye Strain. Since COVID19 increased our reliance on screens for work, socializing and enter-
tainment, those numbers have only gone up. Some researchers now estimate that over 60 million people globally may be affected.
The more time we spend on screens, the more likely we are to experience Digital Eye Strain. This continuous digital engagement can lead to a variety of symptoms including:
• Dry, irritated or watery eyes
• Blurred or double vision
• Eye fatigue
• Headaches
• Di%culty focusing
• Neck or shoulder discomfort
Left unaddressed, these symptoms can reduce efficiency, increase errors, and contribute to overall fatigue.
Several factors can intensify Digital Eye Strain:
• Reduced blinking: Concentration on a screen can reduce blinking by up to 66%, decreasing eye lubrication.
• Poor posture: Improper ergonomics place additional strain on both eyes and musculoskeletal structures.
• Inadequate lighting and glare: Bright displays, re$ections or poorly matched room lighting increase visual stress.
• Multitasking across multiple screens: Constantly shi&ing focus between devices can challenge the eyes’ ability to refocus quickly.
Additional risk factors may include undiagnosed vision problems and outdated prescriptions. Visual fatigue can also be intensified by reading lengthy or dense blocks of text without sufficient formatting breaks or visual guidance.
Implementing small changes can significantly reduce symptoms of Digital Eye Strain. Consider the following approaches:
• e 20-20-20 Rule: Every 20 minutes, look at an object at least 20 feet away for 20 seconds. is technique helps reset accommodation and reduces fatigue.
• Conscious blinking: Making an intentional e ort to blink fully and frequently helps maintain tear !lm stability.
• Optimized screen placement: Position monitors at or just below eye level, approximately an arm’s length away. is reduces the need for excessive head tilting or squinting.
• Lighting adjustments: Use di used, indirect lighting to minimize glare and balance screen brightness with ambient light. Consider positioning screens perpendicular to windows.
• Display settings: Modify text size and contrast to comfortable levels. Enable dark mode if preferred. High-contrast settings can also aid those with mild vision impairments.
• Reduce visual clutter: Keeping a clean desktop, both digital and physical, minimizes distractions and excessive visual scanning, which can exacerbate fatigue.
Proper ergonomic alignment can reduce physical strain and improve visual comfort. A brief assessment of your workspace might include:
• Feet flat on the floor
• A centered monitor, directly in front of the user
• Adequate lumbar support
• Neutral wrist position during typing
Adjustments such as external keyboards, monitor risers or ergonomic seating can be simple yet effective interventions. Ensuring that your screen is angled to reduce glare and neck tension can also enhance comfort during extended periods of computer use.
• Limiting screen use at night to support better sleep quality
• Taking regular breaks from digital devices on weekends
• Getting adequate sleep, which allows the eyes time to recover from daily visual stress
• Scheduling non-screen activities, such as walking or social interaction, to give the eyes a chance to focus on natural distances and light
Establishing a “digital wind-down” routine in the evening, such as dimming lights, stepping away from screens, and using warmer screen tones, can help reset your body’s natural sleep rhythms and give your eyes a break.
Routine eye exams are essential. Adults should schedule a comprehensive eye examination every one to two years, or more frequently if symptoms arise. For those requiring vision correction, up-to-date prescriptions are critical to minimizing visual stress.
Specialized computer glasses may also be appropriate for individuals who spend significant time in front of screens, as they are tailored for intermediate distances and can help reduce strain.
Ophthalmologists can also identify underlying eye conditions, such as convergence insufficiency or uncorrected astigmatism, that may be contributing to screen-related discomfort.
As digital screens continue to define much of our environment currently, preserving visual health must be a proactive priority. Implementing healthy screen habits, supporting proper ergonomics, and scheduling regular eye care can collectively reduce strain and improve both comfort and performance.
Clear, focused vision contributes to more than just task completion. It plays a vital role in quality of life, professional effectiveness and long-term wellbeing. The small adjustments we make today can preserve eye comfort and visual clarity for years to come.
References:
1. Cleveland Clinic. Computer Vision Syndrome. Cleveland Clinic Health Library. 2023. Available from: https://my.clevelandclinic. org/health/diseases/24802-computer-vision-syndrome
2. Harvard Health Publishing. Blue light has a dark side. Harvard Health Blog. 2020. Available from: https://www.health.harvard. edu/staying-healthy/blue-light-has-a-dark-side
3. National Eye Institute. Eye Exams. National Institutes of Health. 2022. Available from: https://www.nei.nih.gov/learn-about-eyehealth/healthy-vision/eye-exams
4. American Academy of Ophthalmology. Tips for Computer Eye Strain. AAO.org. 2021. Available from: https://www.aao.org/ eye-health/tips-prevention/computer-usage

Manpreet S. Chhabra, MD, is a board-certi ed Ophthalmologist with focus on Pediatric Ophthalmology and related conditions. He did his ophthalmology residency at the University of Cincinnati in Ohio and pediatric ophthalmology fellowship at the Northwestern University in Chicago. Dr. Chhabra has over two decades of clinical experience in his eld. He practices at Alamo Pediatric Eye Center, and is a member of the Bexar County Medical Society.

By Trisha Doucette
Employee wellness programs have a become a cornerstone of modern workplace culture, o ering myriad bene!ts that extend beyond physical health. ese programs are designed to support employees’ overall wellbeing, encompassing physical, emotional and !nancial health while driving organizational success through increased productivity, engagement and retention.
One of the primary bene!ts of employee wellness programs is the improvement in physical health. Regular health screenings, !tness challenges and nutritional guidance can help employees maintain a healthy lifestyle, reducing the risk of chronic diseases and absenteeism. But company resources can extend beyond physical wellness.
Work-Life balance is a crucial aspect of employee wellness, emphasizing the importance of maintaining a healthy equilibrium between professional responsibilities and personal life. In the context of employee wellness programs, work-life balance initiatives aim to reduce stress, prevent burnout and enhance overall being.
Furthermore, !nancial wellness is an essential component of employee wellness programs, aiming to support employees in managing their !nances e ectively and reducing !nancial stress. By integrating a series of !nancial wellness objectives into employee wellness programs, organizations can help employees achieve !nancial stability and peace of mind
USAA, an employer of more than 38,000, uses a holistic approach that enhances individual well-being. Colleen McAdams, Communications Manager Senior of Corporate Communications, USAA, explained, “ e primary goal of wellness programs is to help employees achieve their personal best in physical, emotional and !nancial wellness. USAA believes that when employees are at their best, they can provide the best service to our members. USAA’s Total Rewards is designed to o er an exceptional career experience and empower employees to be their best.”
USAA’s Total Rewards Bene ts:
Health and Wellness: Extensive medical, dental and vision plans, along with supplemental health bene!ts like Accidental Injury Insurance, Critical Illness Insurance and Hospital Care Insurance, ensure employees have robust coverage. Reimbursement for weight management and tobacco/smoking cessation programs are in place to provide tools to support employees when they need it.
Work-Life Balance: Parental bene!ts, paid family leave, paid time o and $exible spending accounts support employees in managing their personal and professional lives e ectively.
On-Site Amenities: Child development centers, cafeterias, clinics, pharmacies, Employee Assistance Programs and !tness centers provide convenience and promote a healthy lifestyle. Activities, such as 5ks, promote healthy engagement between employees and their families. Additionally, wellness reimbursement programs are available to encourage remote employees to be active.
Emotional and Recreational Programs: A variety of emotional wellness programs and recreational activities contribute to overall employee well-being and morale.
Development and Retirement: Development programs include tuition assistance and company paid time for professional development. e retirement program features $2 for every $1 contributed, up to 4% of eligible earnings, and a pension bene!t.. ese programs demonstrate a strong commitment to employees’ long-term growth and !nancial security.
To encourage employee participation, USAA’s programs o er healthy lifestyle incentives, including discounted healthy items in the cafeterias, gi& cards for healthy behaviors and reduced insurance premiums for participation in employee wellness programs.
e foundation of improving and maintaining employee wellness is evident at Spurs Sports and Entertainment (SS&E) as well. O ering a variety of both virtual and in-person resources, their primary goal is helping employees stay healthy from their !rst day of employment and throughout their career, realizing that it not only impacts their employees but also their family members and their communities. “We understand that employees have di erent experiences, and having resources available for them in life’s moments is important,” said Stephanie Charlise Ashe, Associate Director Risk, Bene!ts & Wellness, Spurs Sports & Entertainment.
SS&E assesses employees’ needs and interests through surveys and other data, adjusting resources as needed. Ashe explained that the diversity of o erings allows SS&E to support employees at di erent stages of their health, and adjust based on changing needs.
In an organization of employees with a very competitive spirit, SS&E incentivizes participation with time o , franchise-branded raf$e prizes, discounts and more. Engagement is tracked through event participation and program usage. “We typically see engagement from employees all across the organization because we o er a wide range of programming. Our goal is to meet a variety of interests and needs, which sometimes means creating more intimate, tailored experiences, while other programs are designed to resonate with a broader “allsta ” audience,” said Ashe.
SS&E Bene ts:
Health and Wellness: Fitness activities and challenges, mental health activities and resources, on-site biometric wellness screenings, nutrition and lifestyle resources, routine dental services and vaccination clinics.
Work-Life Balance: Generous PTO program plus additional company-wide days o throughout the year.
Financial Education: Complimentary !nancial planning and budgeting services, and legal bene!ts that include free access to legal documents and attorney discounts.
Environmental Wellness: On-site gardening classes.
SS&E measures success of the program through participation and health outcomes such as biometric aggregate data and healthcare costs, and importantly, through employee feedback, which guides the organization in re!ning and improving o erings.


By Emmalind Aponte, MD
My decision to study medicine was inspired by its integration of fundamental research, epidemiology, social health, clinical research and innovation in enhancing patient care. I remember how as a trainee I learned to be committed to evidence-based medicine. I have recently been re$ecting on what drove me to study medicine and how science has advanced since I became a Hematologist and Medical Oncologist. I felt the need to emphasize the importance of research in these times when misinformation is rampant and a threat to progress.
Clinical research leads to the development of new treatments, diagnostics and medical technologies. Research not only aids in understanding diseases and conditions more comprehensively, but also ensures that the treatments and interventions used in clinical practice are safe and e ective. As physicians, we are aware that research is a cornerstone in the advancement of medicine, but we need to transmit this information to our patients that are not as well informed as we are in this regard. Physicians should inform patients about the significance of research in their treatment. e involvement of volunteers in previous clinical trials has enabled us to achieve improved health outcomes today.
Providing information on the types of studies can assist patients in understanding the research process. Observational studies are instrumental in understanding the natural progression of diseases and identifying associated risk factors. Interventional studies evalu-
ate new treatments for effectiveness and safety. Diagnostic research aims to identify diseases or mutations to enhance diagnosis and treatment. Additionally, research can focus on disease prevention. By systematically testing new treatments and interventions, we can advance the field of medicine towards developing more effective and safer therapies. Also, we can improve health outcomes by establishing better practices for managing diseases. We can practice personalized medicine due to research that has tailored treatments to specific genetic mutations in cancer, resulting in improved efficacy and fewer adverse events.
The defined stages of clinical trials, along with oversight by regulatory agencies, ensure that the objectives of safety and efficacy are achieved.
The phases of clinical trials are:
Phase I: Assess the safety of a new treatment in a small group of healthy volunteers or patients.
Phase II: Broaden the study to include a larger cohort of patients to assess efficacy and further evaluate safety.
Phase III: Involve a larger group of patients to confirm the treatment’s efficacy, monitor side effects, and compare it to standard treatments.
Phase IV: These post-approval studies monitor long-term effects and effectiveness in the general population.
It is crucial to emphasize that rigorous measures are implemented to guarantee adherence to the highest ethical standards, thereby safeguarding the rights and well-being of participants. Institutional review boards evaluate studies to ensure that they are ethical, and that participants’ rights are safeguarded. Participants can withdraw from a clinical trial at any point in time.
Clinical research is progressing with the aid of technologies such as arti!cial intelligence and big data, which are altering the methods of conducting research. ese advancements enable the rapid and precise analysis of extensive data sets, resulting in quicker and more e%cient treatments. Precision medicine customizes treatments for patients based on their genetic and molecular pro!les.
Conducting research o&en involves challenges such as resource limitations and regulatory constraints. ere are physician-based barriers, such as lack of awareness of clinical trials available in their community, and the demand on the clinician’s time for those that participate in clinical research. Patient-related barriers are also signi!cant, as patients may hold negative beliefs or attitudes toward research. Additionally, inadequate representation of certain communities in clinical trials raises doubts about the applicability of trial data to the real world.
Research is fundamental to the progress of science and the improvement of health outcomes in our community. I encourage all physicians to advocate for clinical trials and remain informed about the available options within our community, thereby enhancing our ability to provide better guidance to patients. We can also correct any misconceptions patients have about clinical trials, aiming to increase medical knowledge and ensure patient participation reflects the real world.
References:
1. Zhang, H., & Jiang, X. (2025). Importance of clinical trials and contributions to contemporary medicine: commentary. Annals of Medicine, 57(1). https://doi.org/10.1080/07853890.2025.2451190
2. Mohan S.V., Freedman, J. A Review of the Evolving Landscape of Inclusive Research and Improved Clinical Trial Access. Clin Pharmacol er. 2023 Mar;113(3):518-527. doi: 10.1002/cpt.2832. Epub 2023 Jan 26. PMID: 36536992
3. (National Library of Medicine, n.d.) www.clinicaltrials.gov
4. Cancer Society medical and editorial content team, Clinical Trials: What you need to know What You Need to Know about Clinical Trials | American Cancer Society

Dr. Emmalind Aponte is a board-certi ed Hematology and Medical Oncology physician at Texas Oncology-San Antonio Medical Center. She completed her Fellowship in Medical Oncology/Hematology, along with her Residency and Internship in Internal Medicine, at the University of Puerto Rico-School of Medicine, where she earned her Medical Doctorate with honors. Fluent in English and Spanish, Dr. Aponte leads research for Texas Oncology in San Antonio and is actively involved in clinical trials and research with the US Oncology Network and Sarah Cannon Research Institute. She is also a member of the American Society of Clinical Oncology and the Bexar County Medical Society.
Please join Dr. Emmalind Aponte and Texas Oncology in Celebrating Clinical Trials Day this year on Tuesday, May 20, 2025. This year’s theme, “Collaborate. Innovate. Advance.” refects the collective impact of our community.
Together, we can shape the future of clinical research by sharing knowledge, fostering innovation, and driving meaningful change.
More information is available at https://www.clinicaltrialsday.org/ or https://www.socra.org/.
Courtesy of The University of Texas Health Science Center at San Antonio
Physicians are trained to care for others, o&en putting their patients’ needs ahead of their own. But the medical community is beginning to recognize that the well-being of physicians and other medical professionals is not just important — it is essential.
e University of Texas Health Science Center at San Antonio is pushing the provider wellness conversation forward with the Ripples: Physician Well-Being podcast. Made possible by the Joe R. and Teresa Lozano Long School of Medicine O%ce for Graduate Medical Education’s e Wellness Home, the podcast explores burnout, mental health, work-life balance, career satisfaction, mindfulness, resilience, nutrition, compassion and personal relationships.
On the show, hosts Adriana Dyurich, PhD, LPC, Veena Prasad, PhD, MBA, LPC, and Jon Courand, MD, speak with UT Health San Antonio faculty and other guests who share real stories about their challenges and triumphs in practicing wellness while practicing medicine. e idea for the podcast came about in 2021, as the wellness team found they were addressing the same topics over and over in their sessions and wanted to provide more people the opportunity to hear and practice wellness initiatives.
“We didn’t want it to feel like a lecture, rather we wanted to invite guests that not only understood the challenges our residents face, but that have been successful themselves in overcoming them,” said Dr. Dyurich.
In the !rst episode Dr. Prasad mentioned a quote from the Dalai Lama, “Just as ripples spread out when a single pebble is dropped into water, the actions of individuals can have far-reaching e ects.” From this, the podcast hosts knew their focus would be the interconnectedness of all our actions and the potential impact on well-being. Based on the concept of the Wellness Home, Dr. Prasad said the podcast emphasizes holistic well-being while in residence. Dr. Dyurich also proposed that every episode end by leaving a “pebble,” an invitation or
call to action that listeners can integrate into their own lives and spread to others. True to its name, Ripples was born from, and continues to be shaped by, the community it serves.
“We create a space where vulnerability is welcome, where laughter can coexist with the weight of responsibility, and where, ultimately, we aim to bring hope and motivation,” said Dr. Dyurich.
While most guests are physicians from UT Health San Antonio, the show also features guests from other national institutions and speakers with insight into holistic well-being. eir third season, titled “Facets of Compassion,” was based on a compassion course for residents and faculty, taught by Dr. Courand and Holly Day, MD. e hosts highlighted self-compassion as an important element to mitigate professional burnout and moral injury. e season featured special guests Roshi Joann Halifax, founder and abbot of the Buddhist Upaya Zen Center in New Mexico, and San Antonio Mayor Ron Nirenberg, who spoke about how to make San Antonio a more compassionate city.
Now in their fourth season, the team is focusing on life beyond medicine, and how hobbies and activities outside the workplace help overcome compassion-fatigue burnout. Some season highlights include guests Richard Kogan, MD, a psychiatrist and concert pianist; Dudley Harris, MD, an ophthalmologist, potter and photographer; and Rajam Ramamurthy, MD, a professor emeritus of UT Health San Antonio and a dancer.
Dr. Prasad said it’s been exciting to see the Ripples audience expand to now include professionals from many di erent healthcare !elds, upcoming medical students and people from all walks of life.
For inspiring voices and real talk about physician wellness, catch up on past episodes and subscribe to the Ripples podcast wherever you listen to podcasts.

www.UTHSCSA.edu/medicine/education/gme/wellness/ripples-podcast-directory


By Joseph Garcia, City of San Antonio, Metropolitan Health District
May is Asthma Awareness Month — a time dedicated to raising awareness about asthma, a serious and sometimes life-threatening chronic respiratory disease that a ects millions of people, especially children. It’s also a time to remind our community that with proper management, asthma can be controlled, allowing those a ected to lead healthy, active lives.
In San Antonio, families of children living with asthma have access to a valuable and free resource through the SA Kids BREATHE (SAKB) program. Operated by the City of San Antonio, this program is designed to improve the quality of life for children ages 3 to 17 in Bexar County who have been diagnosed with asthma. rough personalized education, support and community partnerships, the program helps families manage their child’s condition — keeping kids out of the hospital, in school, and allowing parents to stay at work.
What makes SA Kids BREATHE unique is its hands-on, personalized approach. Community Health Workers work directly with families, either in-person or virtually, over the course of 12 months. Most families receive three visits at home, coordination with a healthcare provider, and with the child’s school or daycare in the !rst six months. Continued follow-up may occur during the second half of the year as needed.
e program is available to children who live within San Antonio and Bexar County and meet at least one of the following criteria: one or more asthma-related hospitalizations in the past year, two or more emergency or urgent care visits, multiple steroid bursts, frequent school nurse visits for asthma, or chronic school absences due to the condition.
Anyone can refer a child to the SAKB program — including caregivers, school nurses (with parental consent), healthcare providers, hospitals, clinics or managed care organizations.
A key component of asthma management is the Asthma Action Plan (AAP). Every child with asthma should have a written AAP in their preferred language. is essential tool outlines a clear plan for families, schools and caregivers to follow in case of symptoms or emergencies. Using a tra%c light format (green, yellow, red), the AAP helps identify the severity of symptoms, recommends appropriate medications, and provides emergency instructions. It’s an important document that should be shared with anyone responsible for the child’s care — including parents, teachers, grandparents and a&er-school sta . A copy of the AAP should always be kept at home and at school.
As we observe Asthma Awareness Month, let’s continue to support and upli& the families in our community who are managing this chronic condition. With the right tools, education and community support, children with asthma can thrive.


With heavy hearts, we share the news of Dr. Lorence Trick’s passing on March 14, 2025. He was a cherished physician, veteran, mentor, colleague and friend. We are grateful for his dedicated service with the Bexar County Medical Society.
Dr. Trick became a member of the Bexar County Medical Society in 1975. During his membership, he served on both the Board of Directors and in the Delegation to TMA. Dr. Trick was always eager to attend annual BCMS events and was certain to attend annual !shing trips with his fellow physician members.
He was a highly respected orthopaedic surgeon, served in the United States Air Force as Chief of Orthopaedic Services, and his dedication to his cra& and country was unwavering. In addition to being a BCMS member, Dr. Trick was also an active participant in several medical societies, such as the American Academy of Orthopaedic Surgeons, Texas Orthopaedic Association, Alamo Orthopaedic Society, and many more.
Bexar County Medical Society extends its deepest condolences to the Trick family and friends. Dr. Lorence Trick leaves behind a lasting impact on his community and is fondly remembered by his fellow physicians.
By Jacob Hernandez
April’s First Tuesdays at the Capitol event was a special one: this third of four advocacy days throughout the 89th Legislative Session prioritized medical students and young physicians, and many Bexar County medical students showed up to !ll out our delegation and share their stories as physicians-in-training with legislators and sta ! We were overjoyed to be joined by medical students Meenal Cascella, Michaela Kelly, Isabel Kilday, Kevin Nguyen, Ethan McGonagle, Emma Tao, Patrick ompson and John Austin. Other attendees included John M. Shepherd, MD, 2025 BCMS President; Jenny Shepherd, TMAA President; Ezequiel “Zeke” Silva, MD, BCMS Immediate Past President; Jayesh Shah, MD, TMA President-Elect; Gerardo Ortega, MD; Sarah Hernandez, MD; Amita Kumar, MD; Michael Gardner, MD; Antonia Helbling, MD; Sue Bernstein, BCMS Alliance; Cassidy Bernstein; Catherine Ortega; and members of the BCMS sta . e delegation met with legislators and sta from each of the State House and State Senate o%ces representing Bexar County to discuss TMA’s 2025 legislative priorities. New since last month’s event, the

“Life of the Mother Act,” introduced as SB 31 and HB 44, seeks to provide clarity on exceptions to the Texas abortion ban, in order to allow physicians to safely treat patients when their lives are at stake due to crises during pregnancy. is bipartisan legislation aims to protect the patient-physician relationship from criminalization, and TMA is glad to support this vital clari!cation. We also spoke with legislators about the rami!cations of the 2025 Texas measles outbreak, and the importance of routine childhood vaccinations, such as the MMR (measles, mumps, rubella) vaccine, in protecting against infectious diseases such as measles, which is extremely contagious and has killed two children in Texas since the outbreak began. Our delegation also continued to speak about good and bad legislation concerning the issues most important to the practice of medicine, such as the scope of practice, prior authorization reform, graduate medical education, and Medicaid rate increases for physicians in Health Professional Shortage Areas. As always, we are incredibly grateful to TMA’s hardworking Division of Public A airs for working every day to safeguard and advance the interests of physicians and patients.








The Texas Legislature meets every odd-numbered year for 140 consecutive days and will convene again January 14, 2025. Legislators need to hear from you — their physician, medical student and alliance constituents — during the session to understand how proposed legislation can potentially impact the practice of medicine in Texas.
Mark your calendar for May 6, the fnal 2025 First Tuesdays at the Capitol.


Courtesy of Methodist Physician Practices
San Antonio and South Texas residents choose Methodist Healthcare when they or their family members need care, and Methodist Physician Practices is an important part of why. Our extensive network of highly skilled primary care providers, specialist providers and surgeons provide comprehensive, coordinated and compassionate care — all in the communities they serve.
Our physicians are committed to delivering personalized, high-quality services that meet our patients’ diverse needs, and we continue to grow. You may be surprised to learn just how much Methodist Physician Practices now o ers.
1. Availability and access to care: With dozens of locations across San Antonio and South Texas, we are committed to scheduling patients in a timely manner and o ering appointments in a community convenient to your patient.
2. Collaboration and communication: We want to partner with you to o er your patients the specialty care they need. When you entrust us with one of your patients, we’ll ensure they are seen quickly in a convenient location and get the best care possible. We’ll also make sure to keep you in the loop at all times with ongoing communication and a collaborative approach.
3. A longstanding tradition of excellence: Our expert physicians are well known for providing high-quality care in San Antonio. For example, we have the largest cardiology group in the San Antonio area, as well as one of the most experienced neurosurgical practices in the nation.
4. Seamless, integrated care: We’re part of Methodist Healthcare’s system, which means ease of access to patient information. We’re known for our multidisciplinary coordination, backed by the might of Methodist Healthcare.
5. A wide range of services: Methodist Physician Practices has been growing steadily over the last few years. We now o er expertise in a wide variety of medical and surgical specialties, including:
• Adult congenital heart disease
• Advanced heart failure and transplant cardiology
• Bariatric surgery
• Blood and marrow/stem cell transplant
• Cardiac electrophysiology
• Cardiology
• Cardiovascular/cardiothoracic surgery
• Colorectal surgery
• Congenital heart surgery
• Diabetic foot and ankle
• Family medicine
• Gastroenterology
• General surgery
• Hepatology
• Internal medicine
• Interventional cardiology
• Lung transplant
• Neurology
• Neurosurgery
• Orthopedic surgery
• Pain management
• Pediatric blood and marrow/ stem cell transplant
• Pediatric cardiology
• Pediatric orthopedics
• Pediatric gastroenterology
• Pediatric hematology/oncology
• Pediatric neurosurgery
• Pediatrics
• Primary care
• Rheumatology
• Solid organ transplant
• Structural heart disease
• Trauma surgery
• Vascular surgery
Over the past few years, Methodist Physician Practices has been expanding our renowned practices and adding subspecialist providers in high-demand specialties. Here are a few of the newest capabilities to join our practice recently:
Neurosurgery: Our neurosurgery experts have earned a national reputation for exceptional neurosurgical and endovascular care in the treatment of brain and spine complexities. Our team continues to excel in managing intricate craniocervical junction abnormalities, performing precise craniotomies, pioneering deep brain stimulation, and addressing the diverse spectrum of spinal challenges, including problems in the cervical, thoracic and lumbar regions.
Cardio-obstetrics: Our region-leading cardiovascular capabilities are even more robust with the addition of cardio-obstetrics care for women with, or at risk of developing, cardiovascular complications during pregnancy.
Pediatric cardiology: For more than 40 years, our pediatric cardiologists have provided compassionate, state-of-the-art, family-centered cardiac care for children and their families. We o er full evaluation and management of a wide range of cardiac problems in neonates, infants, children, adolescents and adults with congenital heart disease.
Pediatric orthopedics: Our experienced team specializes in treating infants, children and teens with musculoskeletal conditions, including broken bones and congenital conditions such as clubfoot and hip dysplasia.
Bariatrics and weight loss: Our bariatric surgery team provides surgical and medical management options for the treatment of obesity. ey o er a positive environment where patients feel supported throughout their weight-loss journey to reach their goals and achieve an improved quality of life.
Primary care: We’re available in locations across the region, o ering convenience and exceptional care.
At Methodist Physician Practices, we are proud to provide access to care in your patients’ communities. We will o er cardiology services at the newly open Methodist Hospital – Westover Hills. We are also growing our vascular and cardiac surgery presence downtown and expanding our satellite clinics throughout the region.
Everything we do is backed by the strength of Methodist Healthcare. From an emergency to ongoing care, we o er your patients access to top-notch care, where they live. We look forward to partnering with you as we continue to live up to our mission of providing accessible, world-class healthcare for all.
Methodist Physician Practices is a Silver Member of the BCMS Circle of Friends Program. MethodistPhysicianPractices.com

During their annual Bike Rodeo event on April 3, 2025, Kinder through 5th grade students and their parents from East Terrell Hills Elementary School in San Antonio were treated to bike helmets and a presentation on bike safety, courtesy of the Bexar County Medical Society Alliance (BCMSA) and the Texas Medical Association (TMA). Neha Shah, PT, a member of BCMSA, along with her daughter, Prachi Shah, a soon-to-be resident doctor in July and a medical stu-


dent member of BCMS/TMA, helped with !tting 25 helmets on kids, while parents participated in a Q&A education session on bike safety where TMA videos were shared. Maria Cansino, the school’s family specialist, provided Spanish translation. “I would like to thank Tammy Wishard with the TMA for her help with the helmets and supplies needed for this event. e school was very appreciative of receiving helmets and they loved the $yers of bike safety,” shared Neha Shah.
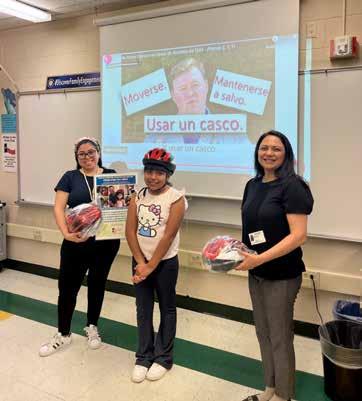



















Continued on page 42




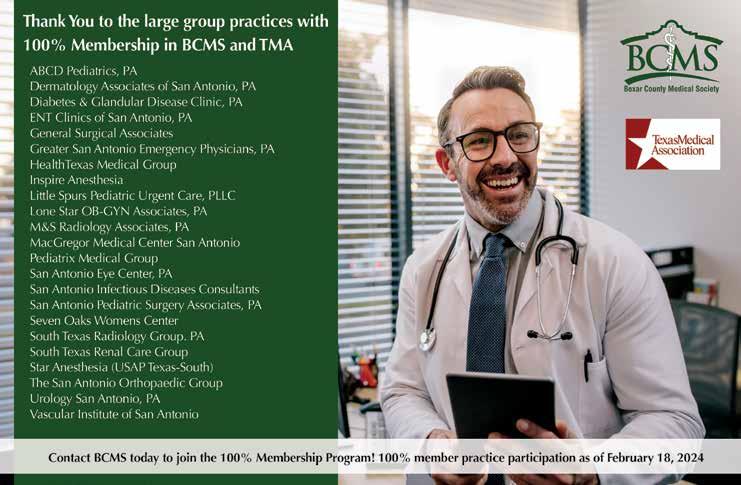

By Stephen Schutz, MD
BMW’s venerable 5-Series sedan has long been a paragon of luxury, performance and innovation. Now in its eighth generation, it is still all that, but the automotive world has seemingly passed it by as SUVs and crossovers have taken over.
Nevertheless, allow me to pour some sugar on the 5-Series, because in the 1970s and ‘80s, when BMW was nothing like the luxury juggernaut we know today, the 5-er grabbed our attention and held it until, umm, maybe 10 years ago when the X5 SUV shoved it aside like Facebook did to MySpace.
It’s not the same world anymore, but with the introduction of the all-electric (BEV) i5 sedan, BMW moves the not-yet-irrelevant 5-Series into the modern era.
Is that a good thing? We’ll see, but for now I’ll just say it’s di erent. Also di erent, and I would say smart, was BMW CEO Oliver Zipse’s decision about !ve years ago to develop new vehicles with con!gurable powertrains, such that they could be manufactured with BEV, hybrid or internal combustion (ICE) propulsion systems, depending on customer demand. As BEV demand declines and hybrid/ICE orders climb, that decision is looking prescient.

Design-wise, the BEV i5 M60 xDrive I tested exudes a nice blend of tradition and futurism. Its silhouette re$ects classic 5-Series models of old, but it’s been updated with a sleek pro!le and modern proportions. e front end features a large version of BMW’s iconic kidney grille, which has been reimagined with no openings and a smoked glass kind of cover that adds subtle illumination at night that hints at its electric powertrain. e rear end is tapered with thin horizontal tail lights that work to minimize visual mass.
Inside, the i5 M60 xDrive is all about luxury meeting technology. When the dude who delivers press cars gave me the keys, he said, “ is car is like from the future.” And he’s right. Ambient lighting, which you can pick yourself, further adjusts according to driving modes, and the latest iteration of BMW’s iDrive user interface is showcased through a majestic curved display that integrates infotainment and driver information seamlessly (and futuristically). I was happy to !nd that the new tech I experienced in the i5 is not just visually stunning but also approachable and intuitive.
Five years ago, I thought that Audi had the best screens and infotainment user interfaces. Now it’s BMW, with Porsche in second place.


e i5 M60 xDrive features a dual-motor BEV system delivering 593HP and 586 lb-& of torque, which can propel the sedan from 0 to 60MPH in an impressive 3.7 seconds. And equipped with an 84.3 kWh battery pack, the i5 M60 xDrive o ers an EPA-estimated range of approximately 240 miles.
Which brings me to my usual words of caution about BEVs: Before buying any all-electric vehicle, think about how you’ll use it. If you have a home charger, commuting and running errands in a BEV are a cinch — no more going to the gas station! — but long trips will be challenging. Automotive News and the Wall Street Journal have reported that the charging infrastructure isn’t what it should be to support long trips in a BEV, and outages or lines at existing charging stations are a continuing challenge.
On the road, the i5 M60 xDrive exhibits good steering, balanced handling and a comfortable ride quality that is undeniably pleasant but not really like previous 5-Series models. While I appreciate the i5’s massive power and acceleration, the always-on-the-balls-of-my-feet agility that I associate with older 5-Series sedans is missing, which is a shame. I blame the i5’s porky 5,225 pounds curb weight.
Rear-wheel steering (RWS) enhances maneuverability, particularly in urban settings such as parking garages. I used to turn my nose up at RWS, but now I appreciate its pluses.


e i5 M60 xDrive comes with adaptive suspension, which adjusts in real-time to varying road conditions. It was invisible to me during my time with the car, and I’m not sure if that’s good or bad.
Positioned as a $agship within the electric 5-Series lineup, the i5 M60 xDrive is priced at $84,100, and of course that number will increase with optional features and additional customization.
It’s worth noting that Porsche and Mercedes BEV models have experienced more depreciation than their internal combustion counterparts so consider leasing.
e BMW i5 M60 xDrive signi!es a pivotal moment in the evolution of the beloved 5-Series sedan. It provides full electri!cation plus a lot, but not all, of the driving pleasure synonymous with the 5-er. And it’s not an SUV. However, range anxiety and depreciation are realities, as they are with all BEVs, so think about how you’ll use it before you buy.

Stephen Schutz, MD, is a board-certi ed Gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.

Auto Group
11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Anthony Garcia 210-681-3399
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Domingo Saenz 210-341-3311
Auto Group
Northside Honda
9100 San Pedro Ave. San Antonio, TX 78216
Jaime Anteola 210-744-6198
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
James Godkin 830-981-6000
14610 IH 10 West San Antonio, TX 78249
Tim Rivers 832-428-9507
North Park Lexus 611 Lockhill Selma San Antonio, TX
Jose Contreras 320-308-8900
Bluebonnet Chrysler Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Auto Group
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX
James Cole 210-816-6000
Kahlig Auto Group
Northside Ford 12300 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
North Park Lincoln 9207 San Pedro San Antonio, TX
Sandy Small 210-341-8841
Auto Group
Cavender Toyota 5730 NW Loop 410 San Antonio, TX
Spencer Herrera 210-581-0474
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX
Chris Martinez 210-366-9600
Kahlig Auto Group
North Park Toyota 10703 Southwest Loop 410 San Antonio, TX 78211
Justin Boone 210-635-5000
9455 IH 10 West San Antonio, TX 78230
Jordan Trevino 210-764-6945
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson 877-356-0476


