LOCAL 1014 HEALTH PLAN MESSAGE
A Message from the Local 1014 Health Plan
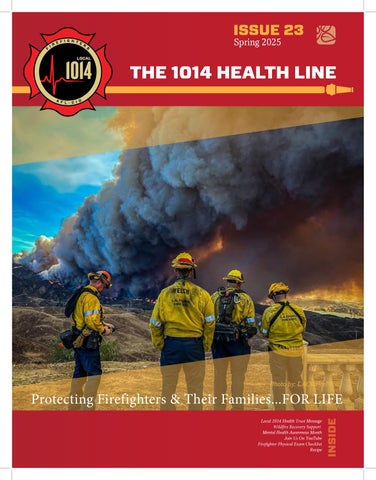
As spring begins, we take a moment to honor the resilience of our members and their families who endured the hardships brought by the devastating January 2025 Los Angeles wildfires. The physical danger, emotional toll, and disruption to daily life have left a lasting impact on our fire family—and we want you to know, we see you, we support you, and we are here to help.
In this issue of The Health Line, we’re focusing on recovery, resilience, and proactive care. You’ll find resources and guidance for navigating the path forward, including:
Wildfire Recovery Support – Practical tools and care strategies for those still feeling the effects of the January fires.
Mental Health Awareness – In honor of Mental Health Awareness Month, we’re spotlighting the importance of turning awareness into action, especially for those in high-stress roles like ours.
Firefighter Physical Exam Checklist – A must-read for staying on top of your health, this checklist ensures you’re covering all the bases in your annual physical.
This spring, let’s continue to look out for each other—on and off the job. Whether you’re rebuilding, healing, or simply checking in with yourself, this issue is for you.
In Strength and Solidarity, The Local 1014 Health Trust
This spring, let’s continue to look out for each other—on and off the job. Whether you’re rebuilding, healing, or simply checking in with yourself, this issue is for you.”
PLAN UPDATE

Plan Update
: We Heard You. We Took Action. And We’re Just Getting Started.
Over the past seven months, we’ve been listening closely to your feedback, and we’ve been working hard behind the scenes to improve the service, speed, and support you receive from your health plan.
Thanks to your input and our team’s commitment to change, we’ve made significant strides in improving how we serve you:
Claims Are Moving Faster Than Ever
We’ve reduced our average claims processing time to just 15 days. That’s more than a 75% improvement! That means faster responses and faster resolutions.
You’re Waiting Less on the Phone
We’ve upgraded our systems and staffing models so we can answer your calls faster, with better service and fewer transfers.
Auto-Approvals Are on the Rise
Our claims auto-approval rate has jumped from 11% to 55%, which means more claims are processed instantly, without delay.
Member Reimbursements Are Flowing
We’ve processed over 4,500-member reimbursement requests during this time. But we’re not stopping there because we know this process can still improve, and we’re focusing on making reimbursements faster and easier going forward.
At the Los Angeles County Fire Fighters Local 1014, our goal is simple: To get you the right care at the right time, with the level of service you deserve.
Thank you for your continued trust and partnership as we work to build a stronger, more responsive plan for you and your family.
Protecting Firefighters’ Health:
The Ongoing Risks After Wildfire Exposure
The dangers of wildfires extend well beyond the initial flames. For Los Angeles County firefighters, especially those who responded to the Eaton and Palisades fires in January 2025, there is an enhanced risk of lingering physical and mental health effects due to intense smoke exposure, toxic particulates, and extreme working conditions.
If you’ve experienced symptoms after working these incidents—such as persistent coughing, shortness of breath, fatigue, headaches, trouble sleeping, or heightened anxiety—do not ignore them. These may be signs of exposure-related conditions that can worsen over time without proper care. The Eaton and Palisades fires were marked by prolonged exposure to dense urban-wildland interface smoke, increased presence of hazardous airborne chemicals, and extreme heat conditions —all of which elevate both respiratory and psychological stress.
Firefighters involved may face higher-than-normal risks for post-incident complications.
Recognizing Common Symptoms
Firefighters often experience a range of symptoms after wildfire exposure, including:
Respiratory Issues:
•Persistent cough
•Shortness of breath
•Wheezing or chest tightness
•Increased mucus production
Cardiovascular Symptoms:
• Irregular heartbeat
• Chest pain
• High blood pressure
Skin and Eye Irritation:
• Rashes or burns
• Red, itchy, or watery eyes

Mental Health Concerns:
•Anxiety or depression
•Difficulty sleeping or nightmares
•Post-traumatic stress symptoms (PTSD)
Fatigue and General Discomfort:
•Chronic fatigue
•Headaches or dizziness
•Nausea or vomiting

Immediate Steps to Take
If you’re experiencing any of these symptoms, consider the following actions:
1.Seek Medical Evaluation:
oVisit a healthcare provider to assess your condition, especially for respiratory or cardiovascular symptoms.
oRequest a lung function test if you have ongoing breathing difficulties.
2.Monitor and Document Symptoms:
oKeep a log of your symptoms, noting when they started and any potential triggers.
oShare this information with your doctor for better diagnosis and treatment.
3.Prioritize Rest and Recovery:
oGive your body time to heal by getting enough sleep and avoiding strenuous activities.
oStay hydrated and maintain a balanced diet to support your immune system.
4.Utilize Respiratory Protection and Decontamination:
oIf returning to wildfire duty, wear a properly fitted respirator (N95 or higher) to reduce smoke inhalation.
oShower and change clothes immediately after exposure to remove toxins from your skin.
5.Address Mental Health Needs:
oSpeak with a counselor or therapist specializing in trauma and stress management.
oConnect with fellow firefighters to share experiences and support one another.
LONG-TERM HEALTH CONSIDERATIONS
Firefighters exposed to wildfires over time may face increased risks of chronic respiratory diseases, cardiovascular issues, and cancer. Regular health screenings and early detection are key to mitigating long-term health effects.
Advocating for Health Resources
Our battle didn’t end when the flames died out. The air we breathed, the water we worked through, the ash we wore on our skin—these weren’t just uncomfortable. They were hazardous. Fires are extinguished, but the health consequences linger.
Your Local 1014 Union knows that our job doesn’t end on the fireline—it continues in the doctor’s office, in the hospital room, and in the halls where policy is made.
Immediately following the fires, we began engaging heavily in testing and documenting our members’ exposure to an unprecedented level of toxins. Local 1014 supervised blood draws and monitoring. We will be marking this moment in time correlated with the exposure as part of the California Firefighter Cancer Research study led by Captain Jamie Gabriel and Local 1014 Director and Engineer Derek Urwin, PhD, UCLA Jonsson Comprehensive Cancer Center, along with researchers from the UC Davis Comprehensive Cancer Center. This study will expand on previous studies of carcinogenic exposure/effect and to include measures of sleep disruption, activity, and comprehensive metabolic and lipid panels. For information about the study contact 1014 Union Director Derek Urwin.
Your health and well-being are as important as the communities you protect. If you experience symptoms after responding to wildfires, take them seriously and seek appropriate care. By prioritizing health and safety, we can continue to serve while maintaining long-term well-being.


MENTAL HEALTH AWARENESS MONTH
Mental Health Awareness Month: Turning Awareness Into Action
Supporting First Responders in the Wake of the Los Angeles Wildfires
May is Mental Health Awareness Month, and this year’s theme, “Turn Awareness Into Action,” serves as a powerful reminder that understanding mental health is just the beginning—we must also take steps to care for ourselves and support those around us.
Mental health challenges such as depression, anxiety, PTSD, trauma, marital and family issues, and even suicidal thoughts have become all too common. Many of us have faced these struggles personally, or know someone who has. Across the country, mental health continues to decline—and it’s time we prioritize emotional wellness just as we do physical health.
Since 1949, Mental Health America has led the charge in raising awareness, promoting education, and increasing access to mental health resources. Today, we carry that mission forward—especially for our first responders.
The Psychological Toll of Wildfire Response
First responders put their lives on the line to protect our communities—but the emotional burden of their work is often invisible. The recent Los Angeles wildfires have only deepened that impact. Common mental health issues among first responders include:
• PTSD: Flashbacks, nightmares, or avoiding reminders of the incident
• Anxiety & Depression: Constant worry, hopelessness, or withdrawal
• Sleep Disturbances & Burnout: Chronic exhaustion and insomnia
• Family & Relationship Struggles: Strained communication, emotional distance
Actionable Steps for Mental Health Recovery
1. Reach Out for Help
You’re not alone. Connect with professionals who understand the unique challenges faced by emergency personnel. The LACoFD Peer Support Team is here for you, offering culturally competent, trauma-informed support.
Key Contacts:
• Dr. Steve: 818-645-9027
• Dr. Lyndee Venosta: 760-805-4127
• Dr. Carl King: 818-359-5732
• Niki Stepanian: 909-908-3390


SCAN FOR PEER SUPPORT
2. Use Trusted Resources
Explore a wide range of support tools from national and local organizations:
• IAFF Behavioral Health
• Healing Our Own
• FireStrong
• Didi Hirsch Mental Health Services
• Suicide Prevention
• Substance Use Help
• Alcoholics Anonymous
• SAMHSA Helpline
• 988 Suicide & Crisis Lifeline or call 988
3. Engage in Healthy Coping Practices
• Practice mindfulness, meditation, or breathwork
• Stay physically active—exercise can be a powerful stress reliever
• Lean on your peer support network; talk to those who understand
You Are Not Alone
Your courage and service during the wildfires was nothing short of heroic—but your mental health matters, too. Asking for help is not a weakness; it’s a strength. This Mental Health Awareness Month, let’s commit to turning awareness into action—for ourselves, our families, and our fire family.
Prioritize your mental health. Support one another. Take action.
Unlocking the Power of Your Healthcare Benefits:

From understanding insurance coverage to deciphering medical bills, many of us find ourselves overwhelmed and confused when it comes to utilizing our healthcare benefits effectively.
We are pleased to announce the launch of our new Local 1014 Health Plan YouTube channel dedicated to empowering you with the knowledge and tools needed to make the most out of your healthcare benefits. Whether you’re a seasoned veteran of the healthcare system or a newcomer looking to demystify the process, our channel offers invaluable insights and practical advice to guide you every step of the way.
So, why should you subscribe?
One of the biggest challenges in healthcare is understanding what services are covered by your insurance plan. Our videos break down the jargon and explain the ins and outs of insurance coverage.
Did you know that many people miss out on valuable healthcare benefits simply because they don’t know they exist? From preventive services to wellness programs, our channel will show you how to take full advantage of everything your healthcare plan has to offer.
At the heart of our channel is the belief that everyone deserves access to high-quality healthcare and the knowledge to advocate for themselves. By arming you with the information you need, we empower you to take control of your healthcare journey and make informed decisions about your health.
Whether you’re dealing with a specific health issue, planning for the future, or simply looking to stay informed, our YouTube channel is your go-to resource for all things healthcare-related. Join us on this journey towards better health and discover the power of unlocking your healthcare benefits today!
Scan the QR Code to watch the first of our many videos unpacking the power of The Local 1014 Health Plan.


https://www.youtube.com/@TheLocal1014HealthPlan
A HEALTHCARE PROVIDER’S GUIDE TO FIREFIGHTER PHYSICALS
YOUR PATIENT IS A FIREFIGHTER

by Bernie Deyo
FIREFIGHTERS FACE UNIQUE
OCCUPATIONAL HEALTH RISKS DUE TO THE DEMANDS OF THEIR JOB
Firefighters routinely operate in harsh work environments
Firefighters wear more than 70 pounds of equipment
Firefighters breath compressed air
Firefighters represent a distinct subset of the general population
TAKE THIS HEALTH GUIDE WITH YOU TO YOUR NEXT PHYSICAL EXAM
It is meant to assist healthcare providers in the evaluation, treatment, and ongoing observation of the health and wellness of Firefighters. The recommendations in this document are supported by ongoing clinical research of Firefighters’ health and by the expertise of the providers caring for them. These recommendations are offered as assistance for healthcare providers making clinical decision regarding the medical fitness and/or treatment of Firefighters. They are not to take the place of your medically reasonable, appropriate and necessary medical evaluation of the Firefighter.
PHYSICAL EXAM CHECKLIST
RECOMMENDED YEARLY SCREENING
Vitals: BP, HR, RR, Wt, Body Fat Percentage
Multi-System PE: skin, mouth, thyroid, vascular, neurologic and musculoskeletal Labs: CMP, CBC, Lipid Panel, TSH, Urinalysis, HbA1c
Testing: 12-lead EKG, eye exam, hearing test, oxygen saturation
Family History: CVD, sudden cardiac death, diabetes and cancer
Personal Health Behaviors: tobacco use, alcohol, exercise, dietary
CARDIOVASCULAR HEALTH AND FITNESS

Significant cardiovascular demands of firefighting lead to acute coronary events that account for 45% of deaths among on-duty firefighters, in contrast to 15% of all deaths occurring on conventional jobs. Myocardial infarction is the leading cause of death of Firefighters, and these events occur almost exclusively in susceptible Firefighters with underlying cardiovascular disease (CVD). It is therefore prudent to thoroughly screen for, and aggressively treat, all CVD risk factors, including diabetes, in this very high-risk group of patients.
Ischemia is best evaluated by an imaging exercise stress test (nuclear or echocardiography) beginning at age 40 or earlier for clinical suspicion. Exercise stress testing without imaging is not recommended as it may fail to identify one-third of those who may need cardiac intervention (angioplasty or bypass surgery).
Echocardiography is recommended once as a baseline to evaluate significant cardiac structural abnormalities, including LVH and HCM.
CANCER
Chronic exposures to heat, smoke, and toxic flame retardants through inhalation, ingestion, and skin absorption put firefighters at risk for many cancers. The National Institute for Occupational Safety and Health (NIOSH) performed a multi-year study of nearly 30,000 Firefighters to better understand the potential link between firefighting and cancer. The Firefighters studied showed higher rates of certain types of cancer than the general U.S. population in digestive, oral, respiratory, and urinary cancers. Providers should be especially vigilant to conduct cancer screening efforts in these particular areas. The following cancer screening recommendations for Firefighters do exceed those of the USPSTF guidelines for the general population. It is because of our extensive clinical experiences dealing with Firefighter health issues that we are strongly advocating for these screening tests in this high-risk group. We rely on your medical judgment to prescribe the most appropriate screenings in this unique patient population.
Colonoscopy or other appropriate colon cancer screening beginning at age 40.
Annual PSA with digital rectal exam between 40-45. Sufficient information regarding the risk and benefits of screening and treatment should be discussed.
Annual pap smear.
Annual mammograms beginning at age 40. Discuss screening at an earlier age if there is a family history or any patient concern. Annual testicular exam and instruction about self-examination. Annual head to toe skin examination and appropriate dermatology follow-up.
Urinalysis annually for microscopic hematuria.
MUSCULOSKELETAL INJURIES
The high intensity and dynamic work environment of firefighting leads to a high incidence of musculoskeletal injuries. Low back injuries represent approximately 50% of all job-related musculoskeletal injuries among Firefighters. These include strains, sprains, and intervertebral disc injuries, often leading to significant morbidity with the possibility of permanent disability. Obesity and deconditioning are strong predictors of musculoskeletal injuries.
Address underlying musculoskeletal issues. Assess for full range of motion, low back strength and flexibility as well as core muscle strength
Refer as necessary for treatment
Encourage flexibility and core strengthening exercises
BEHAVIORAL HEALTH
The mental and physical stress of firefighting and repeated exposure to trauma can lead to depression, anxiety, acute stress reactions, post-traumatic stress, and suicidal ideation. Self-medication with alcohol and drugs can result in substance abuse disorders
Behavior health screening
LUNG DISEASE
In the line of duty, Firefighters are often exposed to carbon monoxide and other inhaled toxins, or irritants that may lead to acute respiratory issues such as hypoxemia or bronchoconstriction. Repeated exposure may cause chronic pulmonary disease and abnormal lung function. Changes in lung function and the development of lung disease may be detected with baseline and periodic assessment and should include the following tests.
Spirometry: Baseline and annual pulmonary function testing in those with a history of respiratory health problems and in healthy individuals; to include FEV1, FVC, and the absolute FEV1/FVC ratio.
Chest x-ray: Baseline chest x-ray in those with any respiratory symptoms or disease and in healthy individuals. Repeat chest x-rays every 5 years or sooner if medically indicated.
SLEEP DISORDERS
Sleep disorders are highly prevalent in Firefighters and include sleep apnea, insomnia, shift-work disorder, and restless leg syndromes. It is imperative to screen Firefighters for these disorders since they substantially increase the risks for motor vehicle accidents, cardiovascular disease, diabetes, depression, dementia, and anxiety in Firefighters.
Assess sleep and use of sleep medications.
Screen for sleep apnea and consider sleep study as indicated.
INFECTIOUS DISEASES
Firefighters are often first on the scene of an emergency and may be exposed to HIV, hepatitis (A, B and C), TB and other infectious diseases.
Establish immunity by vaccination record review and/or titers and update vaccines including Tdap, MMR, HBV, and Varicella. Consider hepatitis A vaccine.
Baseline and periodic screening for HIV, HBV, HCV and other communicable diseases. Provide annual influenza vaccine.
Source: Firefighter Safety Through Advanced Research May 2017
High-Protein Almond Vanilla Cake
A delicious, fluffy, and protein-packed cake that’s perfect for a healthy treat!
Ingredients:
1 cup almond flour
1/2 cup vanilla protein powder (whey or plant-based)
1/2 cup oat flour (or whole wheat flour)
1 tsp baking powder
1/2 tsp baking soda
1/2 tsp cinnamon (optional)
1/4 tsp salt
3 large eggs
1/2 cup unsweetened applesauce
1/3 cup unsweetened almond milk
1/4 cup honey or sugar-free sweetener (monk fruit, stevia, or erythritol)
2 tbsp melted coconut oil or olive oil
1 tsp vanilla extract
Why It’s High-Protein & Healthy:
Directions:
1
2
3
Preheat oven to 350°F (175°C) and grease an 8-inch round cake pan.
Mix dry ingredients: In a large bowl, whisk together almond flour, protein powder, oat flour, baking powder, baking soda, cinnamon, and salt.
Combine wet ingredients: In another bowl, whisk eggs, applesauce, almond milk, honey (or sweetener), melted coconut oil, and vanilla extract.
4 5 6
Mix together: Gradually add the wet ingredients into the dry ingredients, stirring until smooth.
Bake for 25-30 minutes, or until a toothpick inserted in the center comes out clean.
Cool completely before slicing. Enjoy as is, or top with Greek yogurt and fresh berries for extra flavor!
Protein-Packed – Protein powder + almond flour + eggs = muscle-friendly cake.
Refined Sugar-Free – Uses honey or natural sweeteners instead.
Gluten-Free Option – Use certified gluten-free oat flour if needed.
High-Protein Greek Yogurt Frosting
A creamy, delicious, and protein-packed frosting to pair with your high-protein cake!
Ingredients:
1 cup non-fat Greek yogurt
1/4 cup vanilla protein powder (whey or plant-based)
1 tbsp honey or sugar-free sweetener (monk fruit, stevia, or erythritol)
1 tsp vanilla extract
1 tbsp unsweetened almond milk (if needed, for consistency)
Why It’s Great:
Directions:
1
In a mixing bowl, whisk together Greek yogurt, protein powder, sweetener, and vanilla extract until smooth and fluffy.
2
3
4
If the consistency is too thick, add almond milk 1 teaspoon at a time until it reaches your desired texture.
Spread over your cooled cake and refrigerate for 15-20 minutes before serving for a firmer texture.
Optionally, top with fresh berries, chopped nuts, or a sprinkle of cinnamon.
Protein-Packed – Adds even more protein to your cake.
No Butter or Cream – A lighter, healthier alternative to traditional frosting.
Low Sugar – Naturally sweetened and heart-healthy.