Course in Spirometry WORKBOOK

In completing this course, you will learn how to effectively perform a spirometry test.


In completing this course, you will learn how to effectively perform a spirometry test.
“Spirometry is simple but when testing people even the simple is very difficult!”
A successful spirometry relies on a few things:
Skill of the tester
Accurate instructions
Successful Spirometry
Active and maximal patient participation
1. Identify clinical indications for performing spirometry
2. Perform High quality spirometry/ Recognise poor quality spirometry
3. Understand how spirometry tests assist in the diagnosis and management of lung conditions
4. Interpret spirometry in terms of underlying lung physiology
5. Understand the reference values and relatively to local populations
6. Use spirometric readings as a feedback tool for patient education
7. Implement a quality assurance program for your spirometry
8. Minimise cross-infection risks associated with the measurement of spirometry
Review of respiratory component of the coal mine workers’ health scheme:
https://www.monash.edu/medicine/sphpm/coeh/research/review-of-the-coal-mineworkers-health-scheme
Audit findings: Spirometry practices | Resources Safety & Health Queensland (rshq.qld.gov.au)
Spirometry is the most common test of lung function. It is used to measure speed in and out of the lungs. It is a reproducible and objective measurement, which is simple and expensive to perform. Spirometers can cost between $1,000 to $3,000.
It is also safe and very quick to perform and with the correct coaching almost all people can correctly perform the test.
It can be used as a diagnostic tool to evaluate dysfunction and to evaluate symptoms. Spirometry is very useful in screening for early diagnosis in at risk populations such as smokers and those exposed to dust, etc.
Workplace, pre-employment assessments and disability evaluation are other areas where spirometry is very useful.
Spirometry results are determined by lung size, airway calibre and the driving force of the respiratory muscles.
Therefore, used in conjunction with clinical assessment, spirometry is an invaluable clinical tool to:
• detect diseases that impair ventilatory function.
• assess the severity of any existing impairment; and
• monitor the effects of intervention, occupational exposure, or disease progression.
High quality spirometry is vital for accurate interpretation. Lack of adherence to these standards will result in the delivery of poor-quality spirometry, which may compromise clinical diagnosis and management.
What occupations do you think are at risk populations?
Spirometry can be used in clinical research and for the monitoring of disease. Some drugs can be toxic to the lungs, and therefore it is important to closely monitor the lung function.
Pulmonary toxic drugs include:
The global initiative for Chronic Obstructive Pulmonary Disease (COPD) uses spirometry as a screening tool for the early detection of COPD in smokers. The Global Initiative for Asthma guidelines (GINA) measures airflow limitation and its reversibility to assist in establishing a diagnosis of asthma.
A spirometer is an instrument which is used to measure volumes and flow of air both into and out of the lungs. There are two types of spirometers: volume sensing and flow sensing. There are four different types of technology which are currently used in spirometers: pneumotach, rotating vane turbine, mass flow sensor and the most modern, ultrasonic technology.
Spirometers should be capable of accumulating volume for 15 seconds and their range should record for up to 8 liters. This is because we don’t expect patients to exhale longer than 15 seconds, and 8 Liters tends to be the largest lung capacity we see, usually in males.
Should you wish to purchase a new spirometer a good resource to compare the latest spirometers on the market can be found on the National Asthma website.
Quality of spirometry and related diagnosis in primary care with a focus on clinical use. May 2020 : https://www.nature.com/articles/s41533-020-0177-z

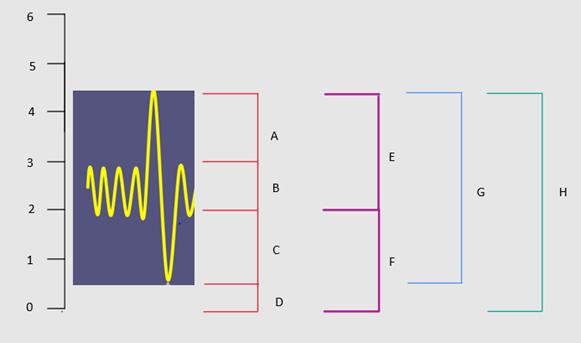
Lung volumes and capacities refer to the volume of air in lungs at different phases of the respiratory cycle. The average total lung capacity of an adult human male is about 6 litres of air.
In this exercise you will label the below lung volume diagram.
Watch the demonstration video of lung volume testing by Plethysmography: https://www.youtube.com/watch?v=OcvIrz1N7-g
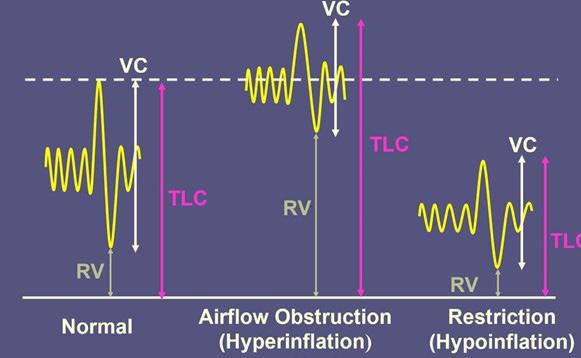
Body plethysmography is used to confirm restrictive lung disease and identify gas trapping in patients with sevre obstruction.
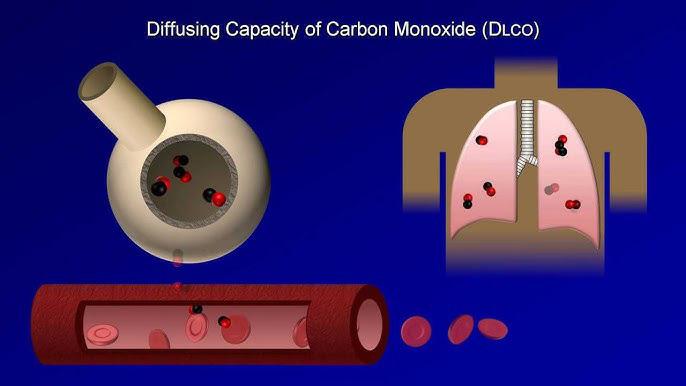
Diffusion capacity testing is used to assess the lung tissue for scarring (fibrosis) or breakdown of alveolar membrane (COPD). This test uses a mixture of gases including carbon monoxide,nirogen, helium and xoygen to assess the gas diffusion into the blood.
Spirometry Definitions
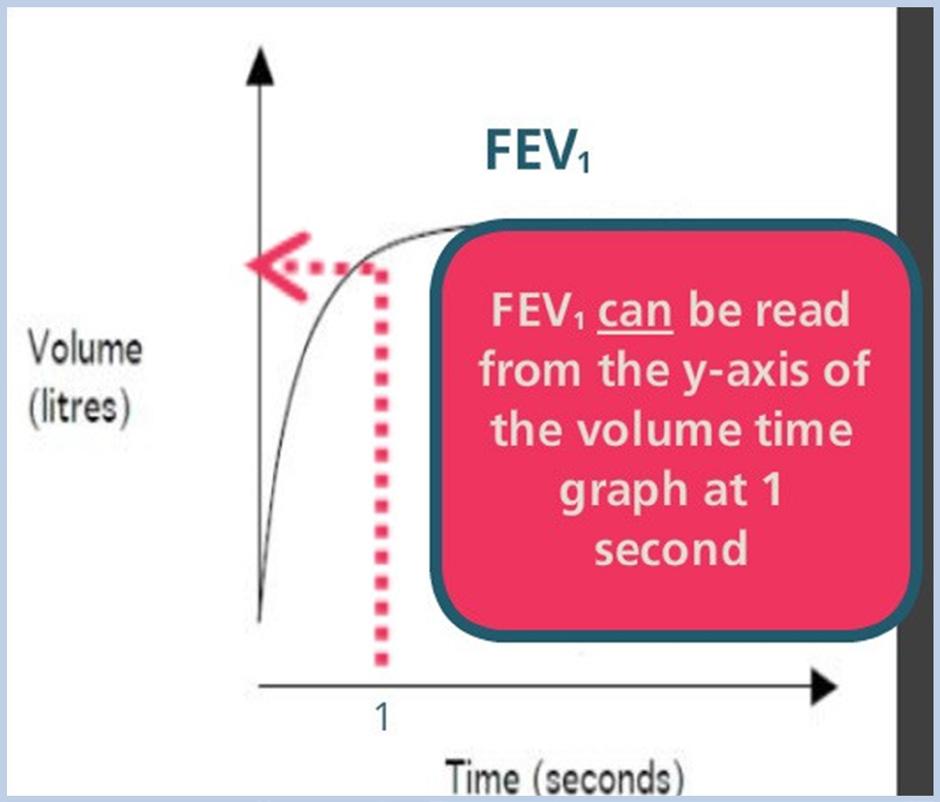
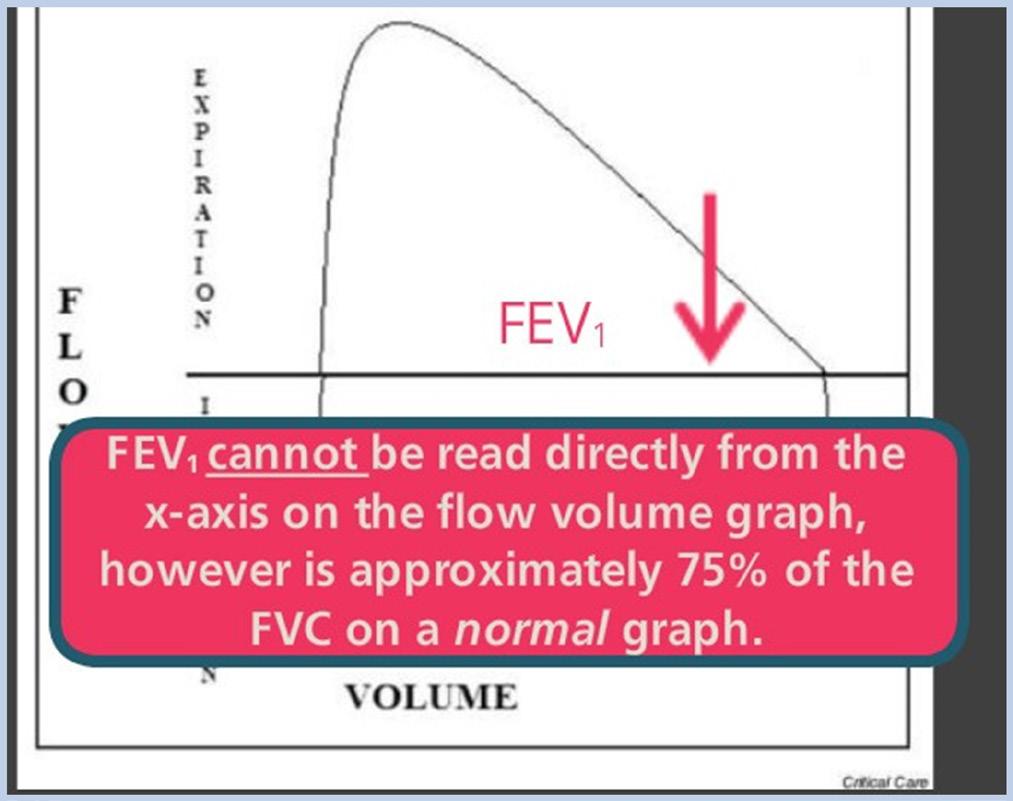
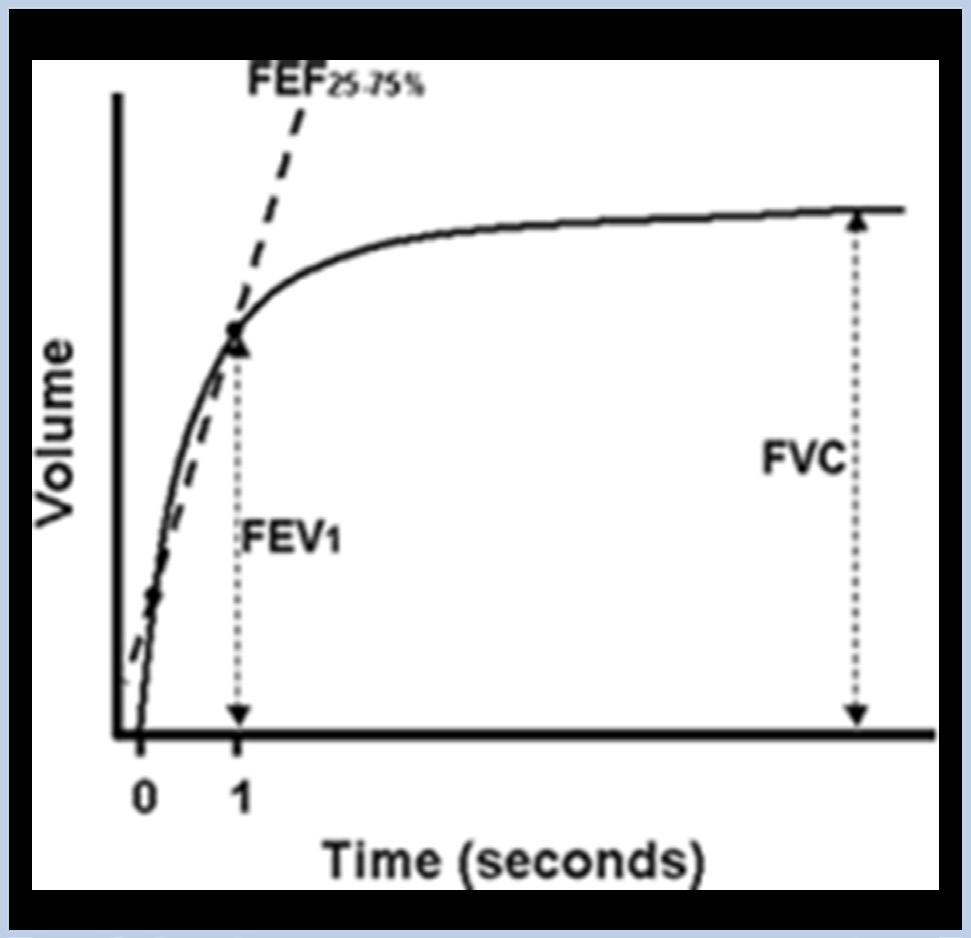
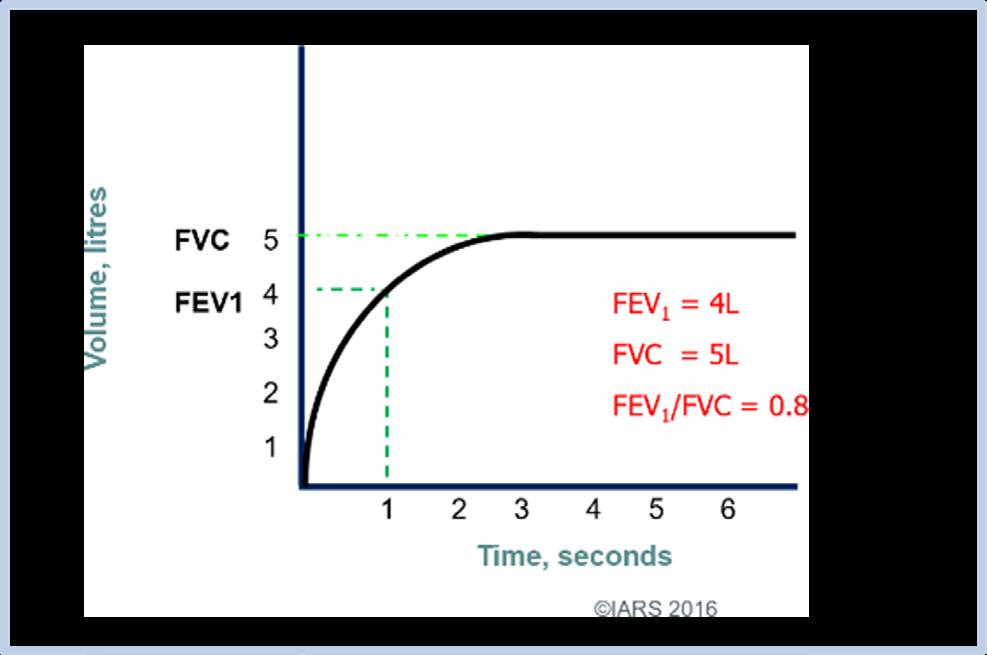
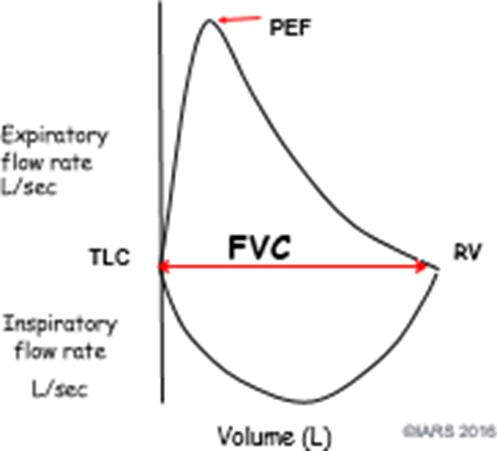
FEV1 (Forced Expiratory Volume in 1 Second) – The amount of air which can be exhaled from the lungs in 1 second
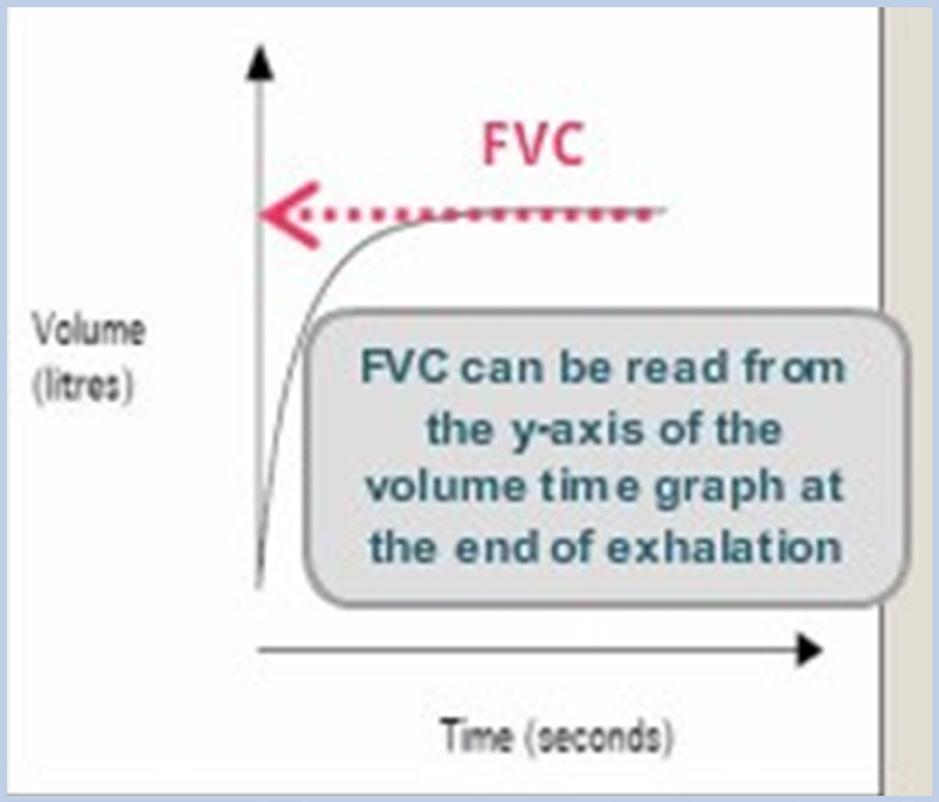
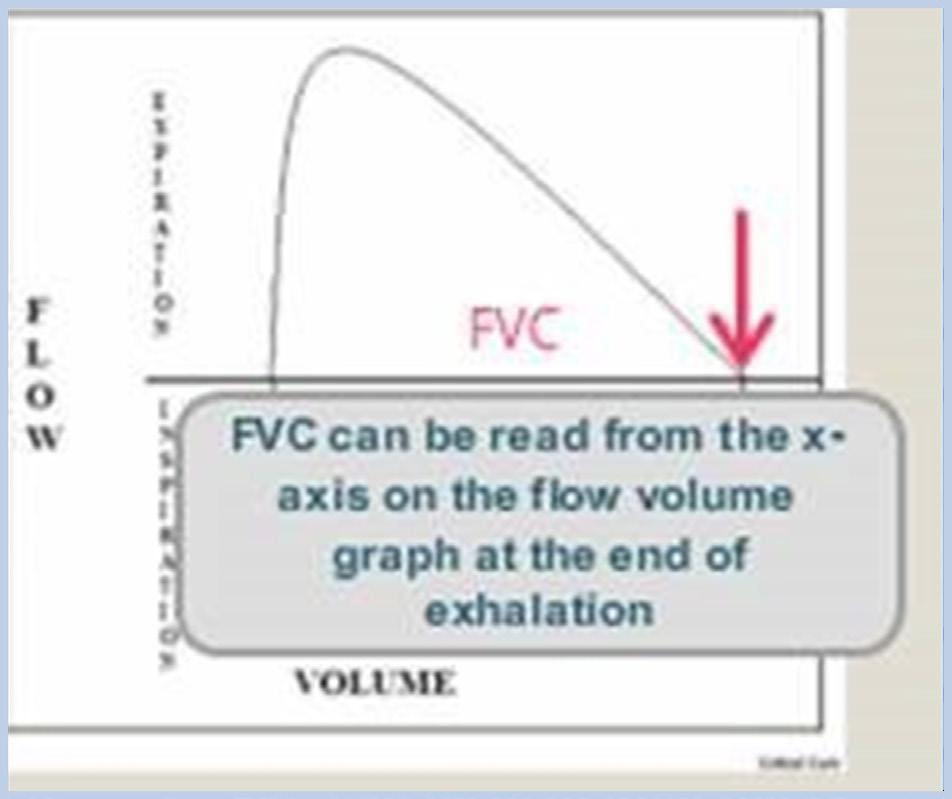
FVC (Forced Vital Capacity) – The total amount of air which can be exhaled from the lungs forcibly
FEV1/FVC ratio - This ratio is a useful index of airflow limitation or obstruction. In the healthy lung 75- 85% of FVC is expired in one second.
FET (Forced Expiratory Time) – Time required to perform the FVC maneuver. In normal healthy adults it usually takes about 6 seconds but can take up to 15 seconds in patients suffering from obstructive diseases such as COPD.
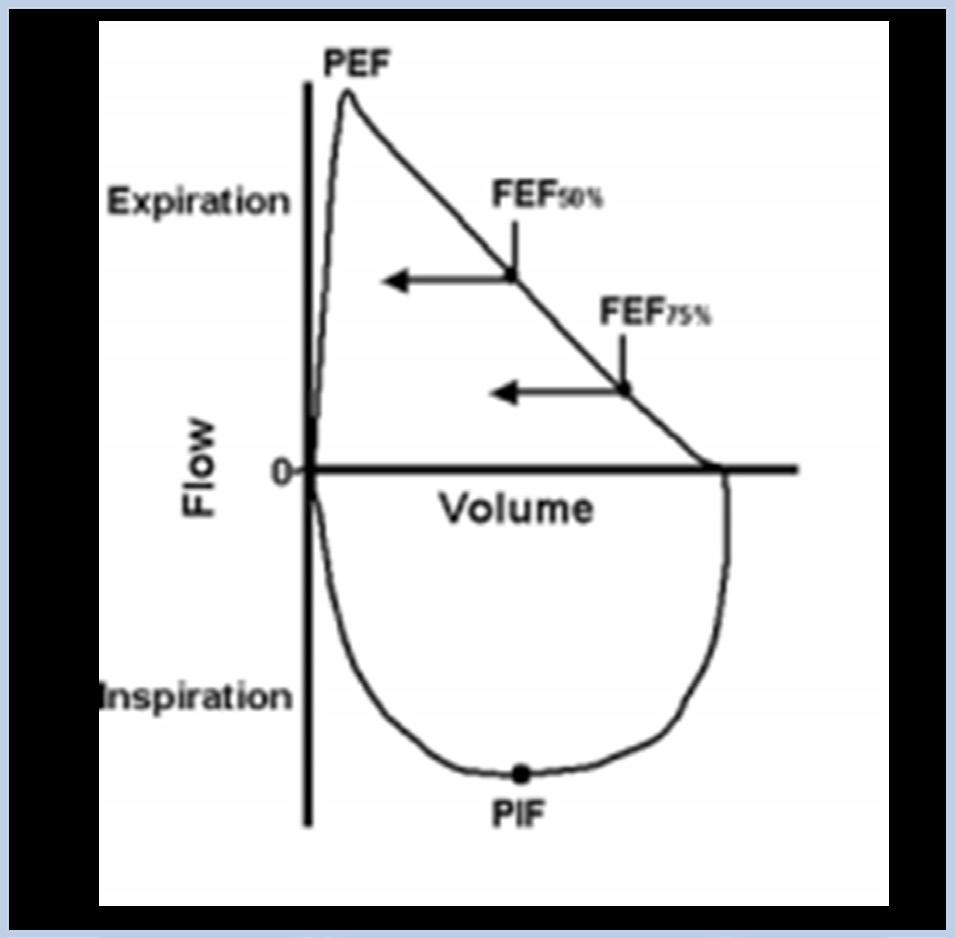
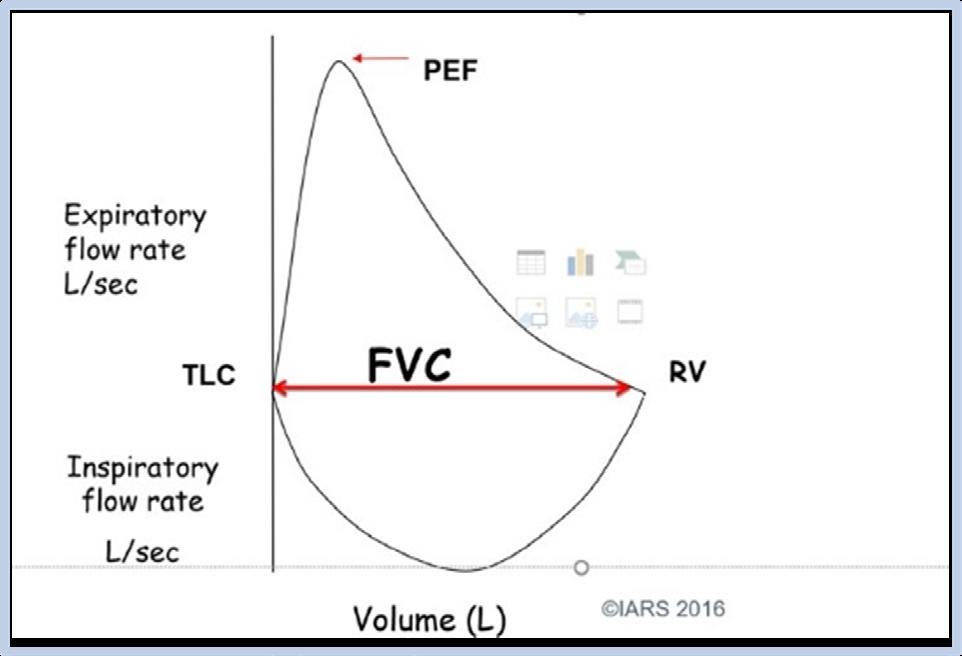
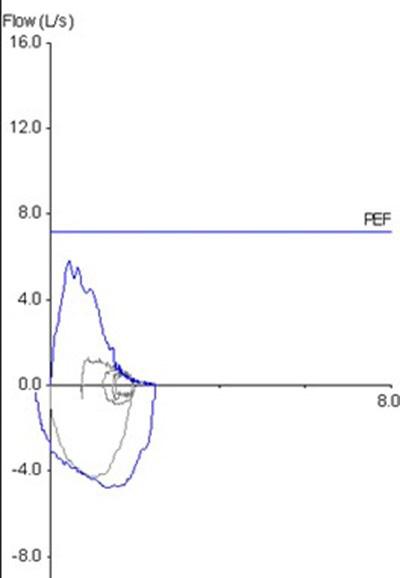
PEF (peak expiratory flow) - Largest expiratory flow achieved during the forced expiratory maneuver initiated at full inspiration
Flows within the small airways:
• FEF25–75% -(forced expiratory flow between 25% and 75% of FVC)
• FEF50% -(forced expiratory flow at 50% of FVC)
• FEF75% - (forced expiratory flow at 75% of FVC)
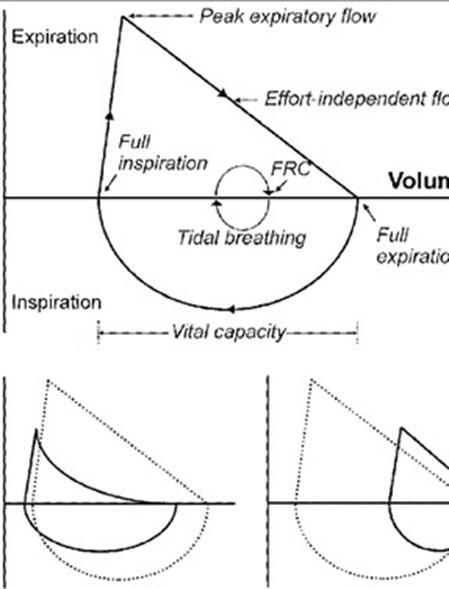
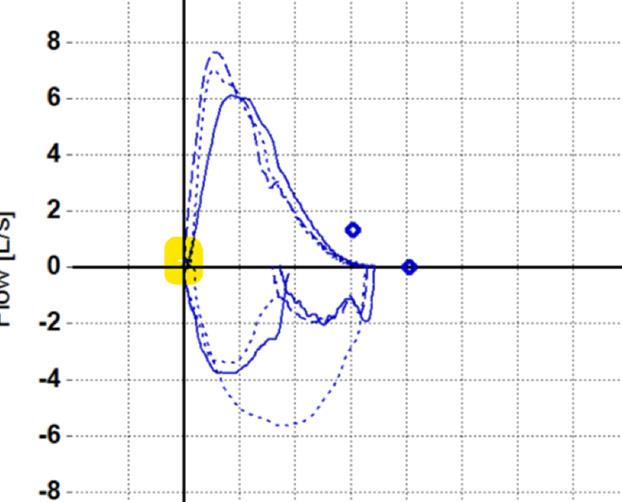
Why use both graphs
The below describes situations to withhold the spirometry test on an individual.
Due to increases in myocardial demand changes in blood pressure
• Acute myocardial infarction (within 1 week)
• Systemic hypotension or severe hypertension
• Significant atrial/ventricular arrhythmia
• Non compensated heart failure
• Uncontrolled pulmonary hypertension
• Acute cor pulmonale
• Clinically unstable pulmonary embolism
• History of syncope related to forced expiration/cough
Due to increases in intracranial/intraocular pressure
• Cerebral aneurysm
• Brain surgery (within 4 week)
• Recent concussion with continuing symptoms
• Eye surgery (within 1 week)
Due to increases in sinus and middle ear pressures
• Sinus surgery middle ear surgery or infection (within 1 week)
Due to increases in intrathoracic and intraabdominal pressure
• Presence of pneumothroax
• Thoracic surgery (within 4 week)
• Abdominal surgery (within 4 week)
• Late-term pregnancy
Infection control issues
• Active or suspected transmissible respiratory or systemic infection - including tuberculosis
• Physical conditions predisposing to transmission of infections, such as hemoptysis, significant secretions, or oral lesions or oral bleeding
• Smoking and/or vaping and/or water pipe use within 1 hour of testing (to avoid acute bronchoconstriction due to smoke inhalation)
• Consuming intoxicants within 8 hours before testing (to avoid coordination, comprehension, and physical ability problems)
• Performing vigorous exercise within 1 hour before testing (to avoid potential exercise-induced bronchoconstriction)
• Wearing clothing that substantially restricts full chest and abdominal expansion (to avoid restricting lung function)
Watch the demonstration video learn more: https://www.youtube.com/watch?v=aS6Jt5KUSYU
It is important to measure the correct height of the individual as this value does affect the test outcome.
Therefore when measuring the person’s height, keep the below do’s and don’ts in mind to get the most accurate measurement. Do’s
Stand straight with heels together without shoes
Actively stretch to a fully erect position
Look straight ahead
Compress the hair as much as possible with the horizontal arm remaining at 90 degrees
Self-reported height
Measuring with shoes on
Hair accessories not removed
Equipment not properly installed
Height should be recorded to the closest mm Knees bent
Head out of position
Correct patient Testing Position:
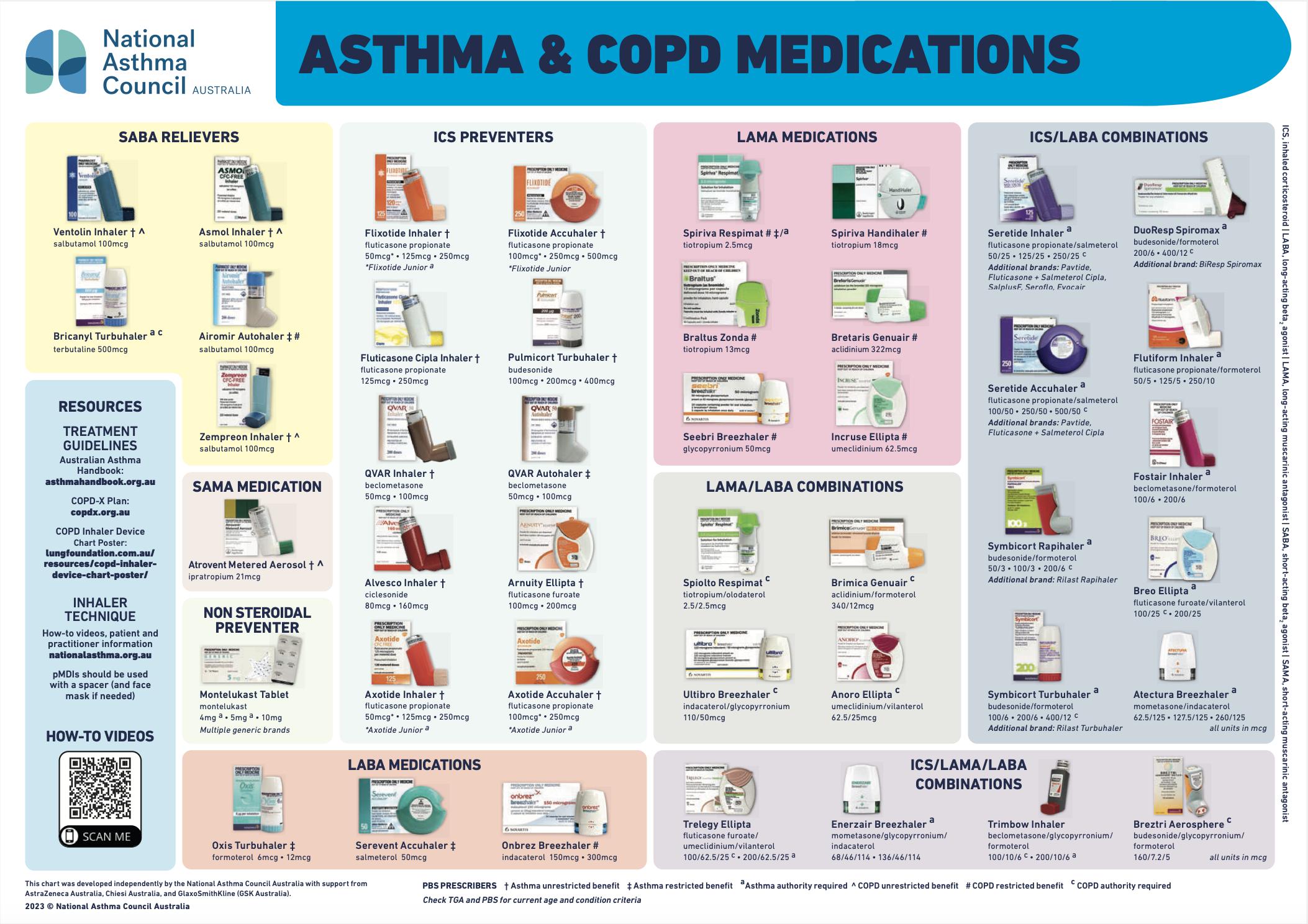
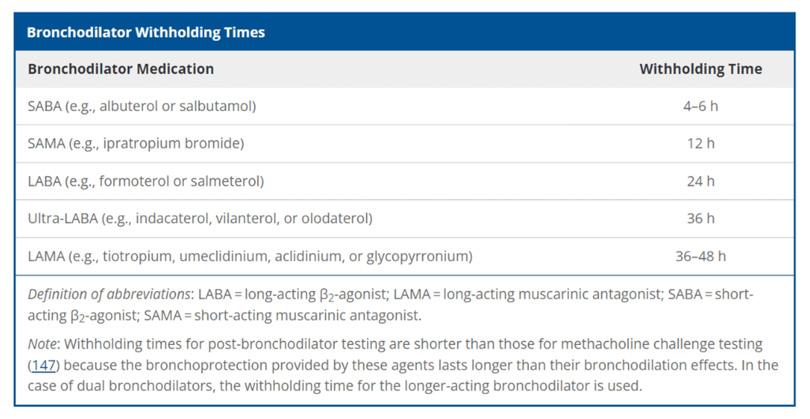
The following medication may need to be withheld prior to performing spirometry. If medications are taken this should be noted in the spirometry report, along with the time elapsed since the last dose.
For pre-employment medicals medications can be continued but medication amount and time taken should still be recorded in the clinical comments.
• Short acting beta agonists (SABA)
• Short acting muscarinic antagonists (SAMA)
• Longacting muscarinic antagonists (LAMA)
• LAMA/LABAcombinations
• Long acting beta agonists (LABA)
• ICS/LABA combinations
• Inhaled corticosteriods (ICS)
• ICS/LAMA/LABA
• ICS/ LABA combination
The below is a list of medication that make breathing easier by relaxing the muscles in the lungs and widening the airways (bronchi), which can be used to help perform a spirometry test.
Source: https://files.nationalasthma.org.au/resources/NAC028-Asthma-COPD-MedicationsChart-2023_A4_WEB.pdf
Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical STatement
What is the difference between the open and closed-circuit method of spirometry?
What are the advantages of performing the closed-circuit method?
Please list the testing requirements required for mobile spirometry:
After this section you should be able to:
• Explain and demonstrate the spirometry procedure
• Activate/ Zero the spirometer
• Instruct throughout the test
• Observe for any issues or test errors
• Terminate once successful measurement as been achieved/ issues arise
You must complete a minimum of _______ trials and up to a maximum of _______ trials.
Acceptability and Reproducibility criteria must be met.
Record the largest FVC and FEV1, they do not need to come from the same test. If you obtain a larger VC from an inspiratory manoeuvre or a Slow Vital Capacity (SVC) manoeuvre this can be added to your technical comments.
Encourage the subject to inhale as much air as possibly, until they are full or at TLC. Without a full inspiration all the spirometric indices will be underestimated.
Key indicators are (refer to Pg. 76 and 77 of ATS Standardisation of Spirometry 2019 update):
Use words like “BLAST” and “FORCE” or “Thump” to indicate the speed of the breath required. Without a blast the PEF and FEV1 will be underestimated.
What are you encouraged to look for during the forced exhalation? 1. 2. 3. 4.
Use words like “keep going, keep going” or “push, push, push”
Failure to expel all the air leads to underestimation of FVC and overestimation of the FEV1/FVC ration which could mask true obstruction or even indicate restriction.
Expiration should be:
• Smooth and uninterrupted
• Maximal effort on entire maneuver
• Expiration should have a 1 second plateau in the volume time curve (<0.025ml change in the last second) or meet one of the End of Forced Expiration (EOFE) criteria
Inhalation back to TLC.
The 2019 Spirometry Standard requires that FIVC be reported. (page e82, table 9).
The 2019 Standards mandates that the flow-volume loop is an integral part of spirometry. (page e82, column 3, paragraph 2)
FIVC – FVC must be <100ml or 5% of FVC whichever is greater
RSHQ - Webinar series to support high quality spirometry.
The following videos have been released by RSHQ clinical audit lead to assist in improving spirometry quality.
Three 30-minute sessions covering the following areas:
Accessing the webinar recordings
Spirometry Webinar 1 – Writing a Spirometry Procedure Manual: https://youtu.be/HExbjjd6EX4
Spirometry Webinar 2 – Performing Spirometry Quality Control: https://youtu.be/ZbpFqzjMUiE
Spirometry Webinar 3 – Requirements of a Spirometry Report: https://youtu.be/eju4P3BYtWQ
Contact:
Jarrod Warner, Manager, Clinical Quality 07 3199 4853
jarrod.warner@rshq.qld.gov.au
• Do not use third party templates
• Use lots of images of your equipment and settings
• Have staff performing procedure make simple bullet point information
• Easy to understand
• Have it reviewed by staff performing the test
• Final review and sign off by senior staff
• Review and update annually
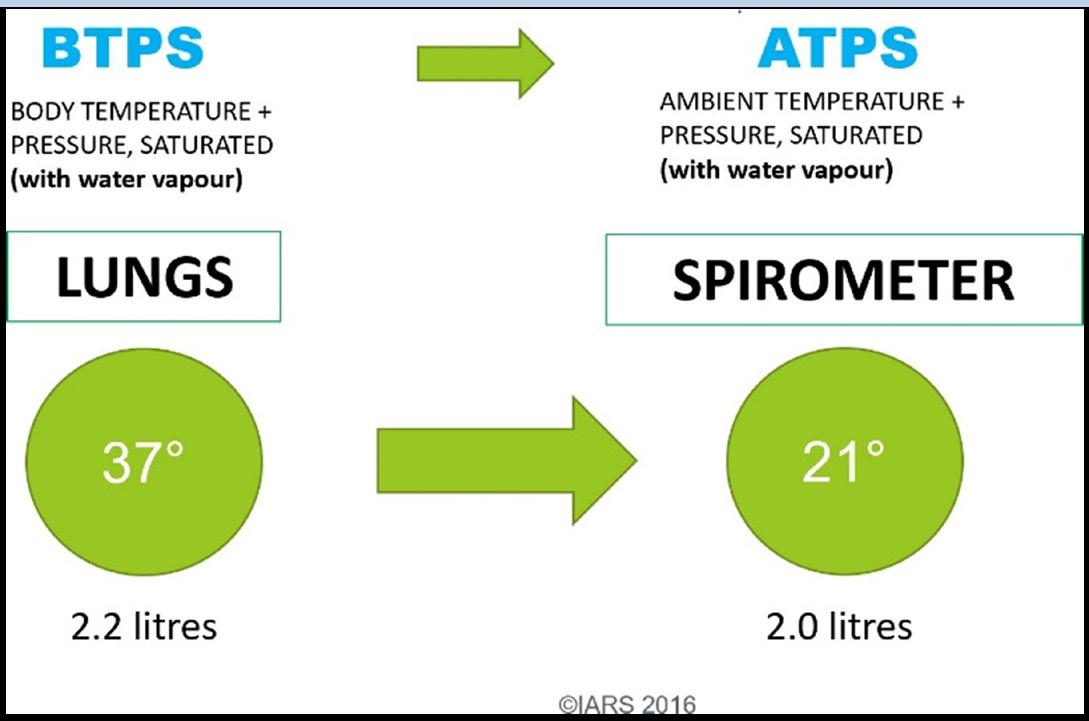
Spirometers are very sensitive to changes in temperature, therefore each room where spirometry testing is being performed should have its own thermometer.
It should be placed close to the spirometer.
If the room changes by more than ______ degrees, the spirometer should be recalibrated.
Barometric pressure or Altitude may also need to be entered into the Spirometer. For example, the Easy On PC requires altitude. The altitude only needs to be entered once, if the spirometer is not used elsewhere. The altitude is then converted to barometric pressure.
How to find your local barometric pressure and humidity
Find your nearest weather station on the website.
1. Click on your region on the top right-hand area
2. Scroll down to observations and select your most local weather station.
3. Pressure is in hPa, convert to mmHg using this factor - (1.3322387415 hPa = 1mmHg) or google a “hPa to mmHg converter
Weather stations can be purchased for your testing room which measure all these ambient conditions. Some spirometers have inbuilt weather stations, but these can sometimes fail.
Warm moist air from the lungs at 37°C & BTPS enters the cooler spirometer at 21°C, the gas molecules shrink and the volume is reduced.
Instrument maintenance – keep a logbook:
• Cleaning and disinfection procedures
• Electrical operation and safety checks
• Mechanical operation and safety checks
• Software/database maintenance and back-up
Ensure appropriate instrument maintenance according to your spirometer’s instruction manual calibration with a syringe of a known volume, usually 3 Litres.
3 litres should record between:
• A 3 litre syringe verification should read within 3% of 3 litres according to the 2019 ATS/ERS standard. This allows for 2.5% spirometer error and 0.5% syringe error.
3% (+) 3.09 Upper limit in Litres
Multiflow/Linearity/Non-biological
3% (-) 2.91Lower limit in Litres
Linearity checks should be performed _________________ according to 2019 standards of spirometry. Linearity checks assess that your spirometer is working across low, medium and high flow rates.
The syringe should be injected and/or withdrawn at least 3 times, at varying flows
• < 2L/s
• 4L/s – 6 L/s
• >8L/s
You can perform a non biological control instead of biological controls (using a staff member to check their results monthly). To do this you must set up a fake patient. You can call them QC Syringe. Any details can be entered for the rest of the demographic data. Enter the patient data as follows:
• First Name: QC
• Last Name: Syringe
• Weight: 150 lbs. (or 68 kg)
• Height: 163 cm
• Age: 40
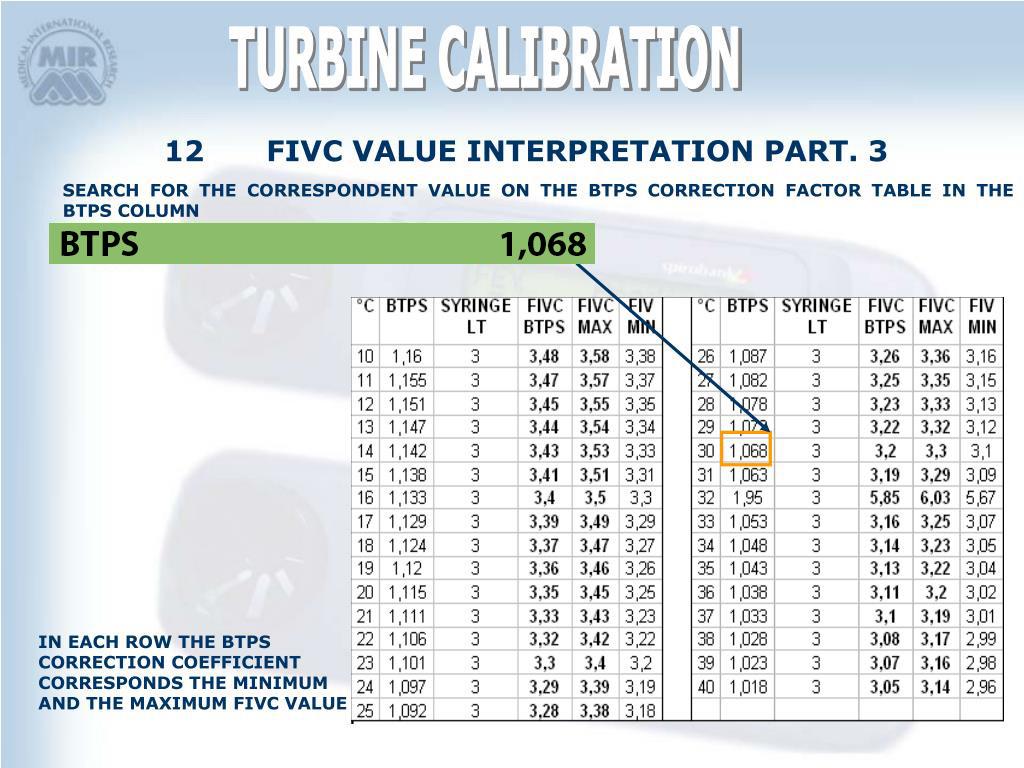
If you test in patient mode remember that the volumes are converted to BTPS by a correction factor.
This will affect the FIVC values. You should still see that the FVC values fall within the 2.91-3.09 range. You show consult the room temperature and read the chart below to ensure that the FIVC is falling within an acceptable range for that particular temperature.
Linearity checks and biological control should also be performed after repairs, maintenance and software changes. Also consider quarterly timing accuracy.
A regular biological control check by a healthy subject. Biological controls are to be conducted at least once every four weeks. However, they can be conducted more frequently, often weekly and provide useful information if a spirometer is suspected of being acutely out of calibration and as a problem- solving tool for troubleshooting errors such as volume or gas analysis errors or leaks in the system.
The following advice on the use of a biological control program is provided:
Individuals within a biological control program must be healthy, non-smokers and free of known respiratory disease.
• Spirometry of the biological control should be recorded every working day at approximately the same time of day. A minimum of 10 recordings is required and should be obtained in as short a time as possible, allowing for normal working patterns.
• Calculate the mean (average) for each spirometry parameter: i.e., add up all the readings for that parameter and divide by the number of recordings.
• Calculate 2.5 STD of the mean
• Finally, obtain the normal range for repeated measurements by adding and subtracting this 2.5 std value to the mean value You can now use this individual and this range as a guide to verify the accuracy of your spirometer.
• If used, these data must be recalculated every two years to account for normal age-related decline in lung function
• Syringe re-validation: re-validated on a yearly basis or as specified by the manufacturer
• Syringe leak test: Tested for leaks and smoothness of operation minimally on a weekly basis.
The syringe should be tested from a full (drawn back) position by placing a hand over the outlet and depressing the syringe handle gently. No air should escape. Secondly the syringe should be emptied, and in an empty position should be checked by again placing a hand over the outlet, then pulling gently on the syringe handle. No air should enter the syringe. Syringes that leak may not measure proper volume and should be sent for service.
Move the syringe handle back and forth to check that the action is smooth, without catching or stuttering. Syringes that do not move smoothly may not deliver proper volume and should be sent for service.
Reasons why calibration fails?
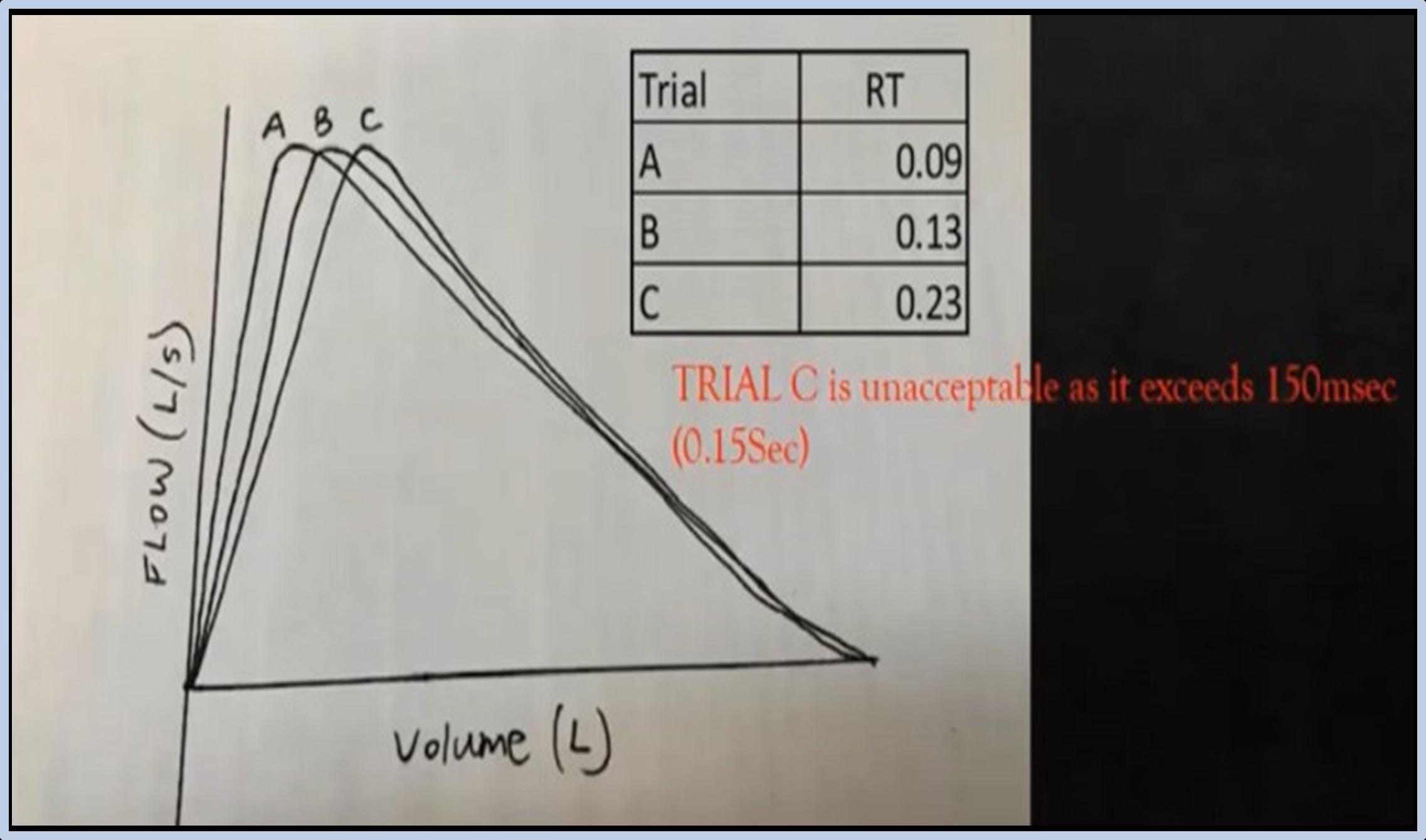
Begins from full inspiration has a rapid start of test, If the manoeuvre has an obviously hesitant start then the trial should be terminated early to avoid unnecessary prolonged effort.
Short rise time (less than 10msec)
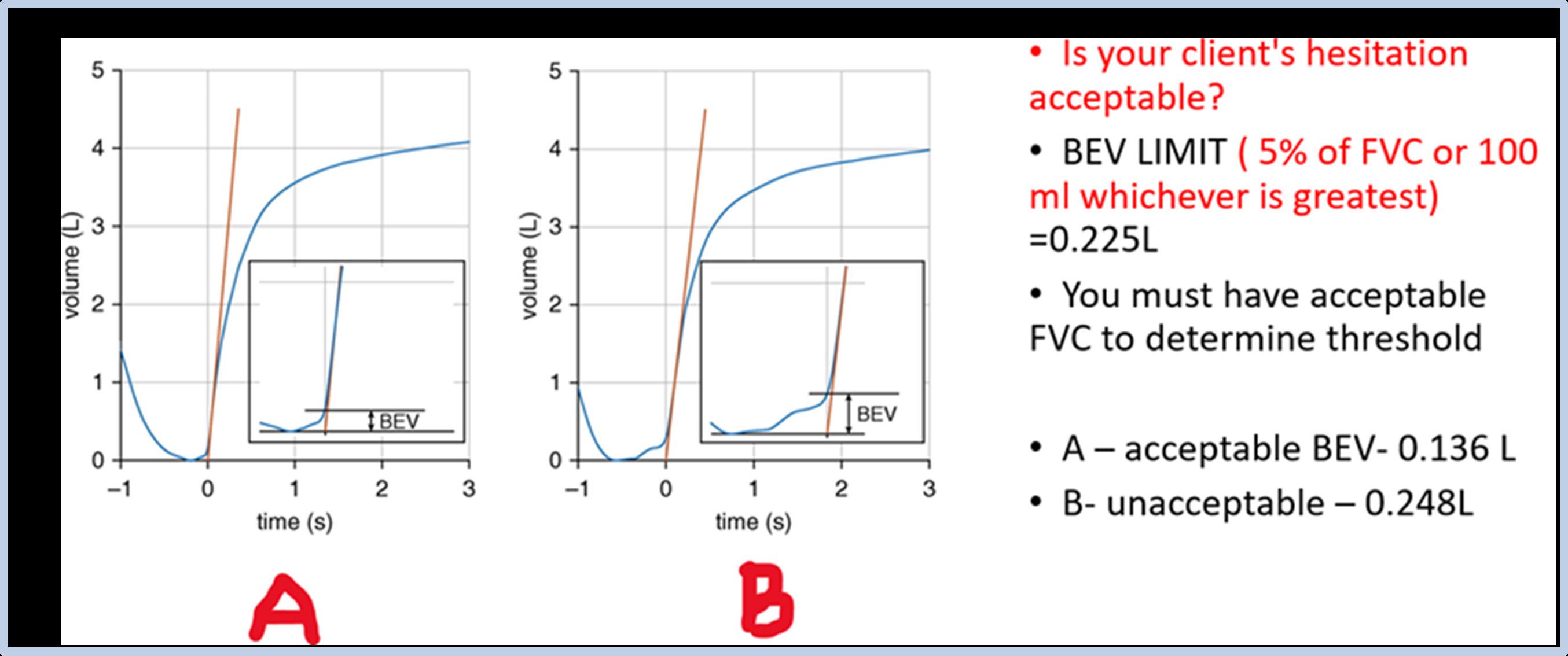
A back-extrapolation line is positioned on the straightest part of the curve, creating a new ‘zero’. To ensure that the FEV1 comes from a maximal effort the BEV must be 5% of the FVC or 0.100L, whichever is greater. The 0.100-L is a reduction from the 0.150L tolerance in the 2005 standards.
PEF repeatability of 1 L/sec or _______% (insert percentage) is an indicator of a good effort
Variable effort changes the shape of the FV curve due to the ffort dependence
A maintained forced effort increasing therick of syncope and therefore expration technique after the first 2-3 seconds should not be forced.
Cannot increase flow rates due to effort independence
Increased effort will cause client to be red in the face, there is an increase in intracranical and intraocular pressure. This is what increases the risk of syncope.
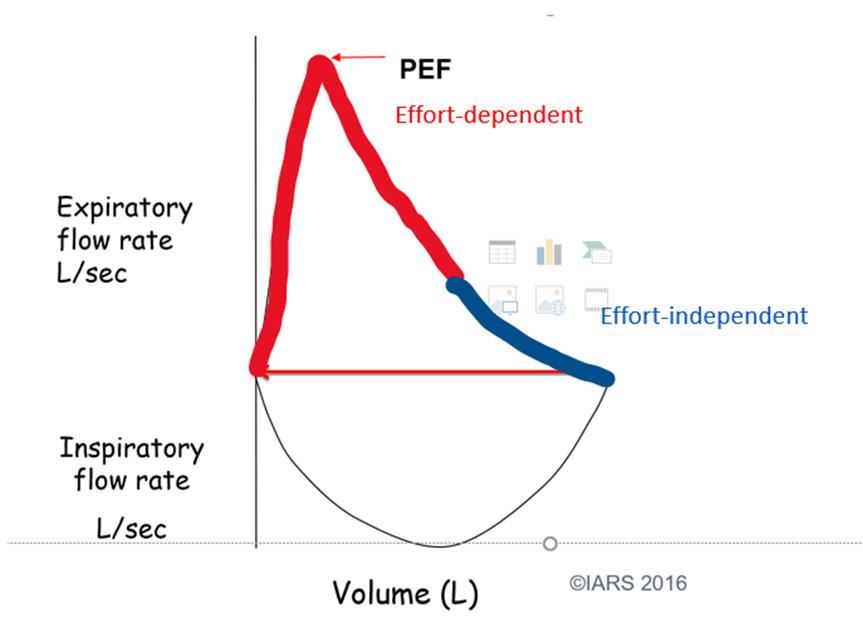
There are two regions of the expiratory FV curve
Effort dependent – air flow is produced by mass flow (fast)
Effort independent – air flow by diffusion (slow)
No obstruction, hesitation or artefact impeding the blow including:
• Cough during the first second of exhalation
• Glottic closure that influences the measurement
• Early termination or cut-off
• Effort that is not maximal throughout
• Air leaks at mouth
• Obstructed mouthpiece (due to tongue or teeth in front of the mouthpiece, or mouthpiece deformation due to biting).
Standardisation Of Spirometry 2019 Update
Previous standards used the term “end of test” and the abbreviation “EOT” to denote end of forced expiration (EOFE). These standards stress the importance of a maximal inspiration after the forced expiration. As such, the end of forced expiration is not the end of the manoeuvre, and hence the term EOFE is used.
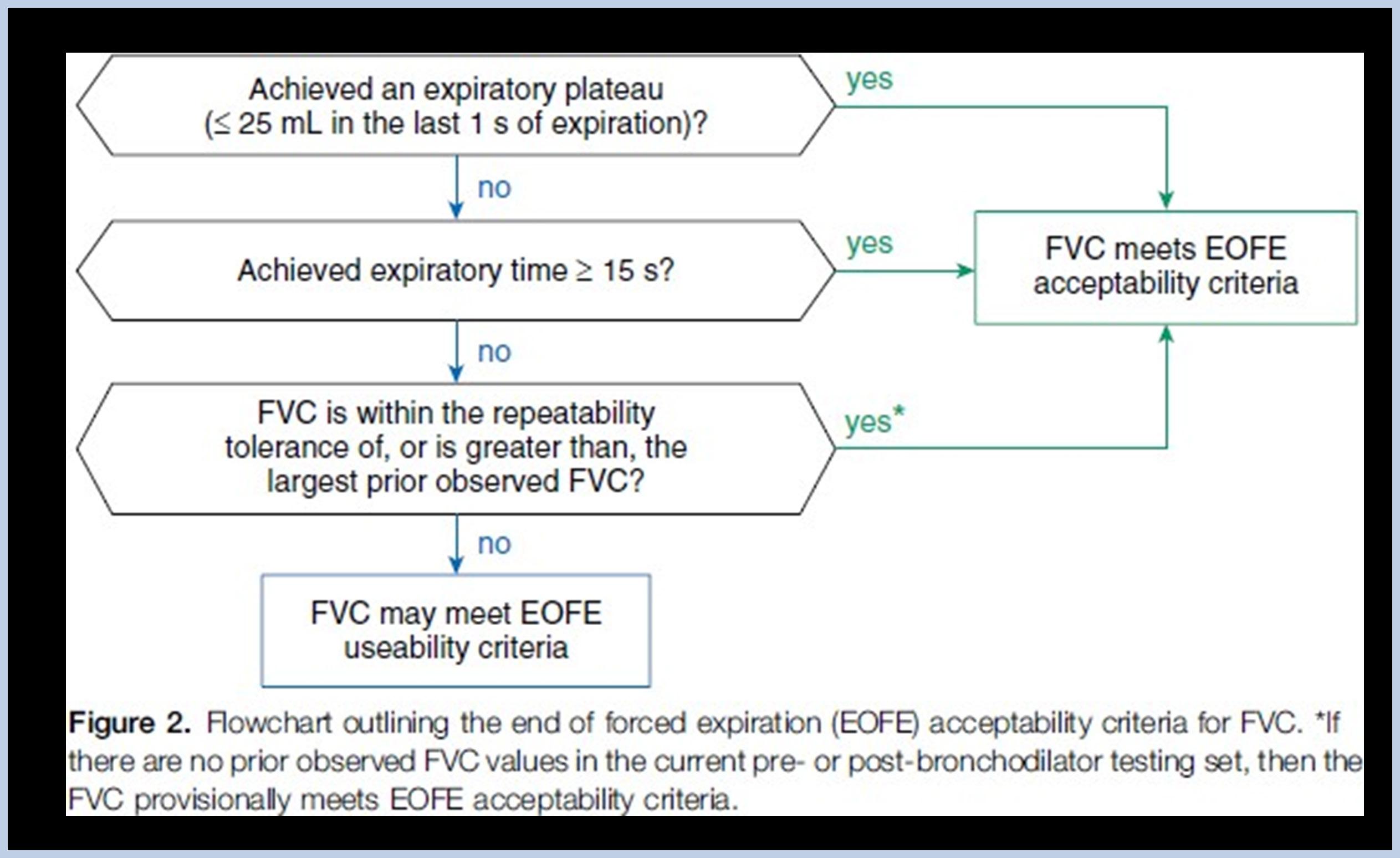
Recognizing a satisfactory EOFE is important to ensure that a true FVC has been achieved. Achieving one of the following three recommended indicators of EOFE is required.
Focus on: 1. 2. Plateau may not be achieved in 1. 2. 3.
After three acceptable spirograms have been obtained, the following checks are used to assess for repeatability:
The two largest values of FVC or VC must be less than or equal to __________ L of each other
The two largest values of FEV1 must be less than or equal to __________ L of each other
For patients with an FVC or VC of ≤1.0L the two largest FVC or VC and FEV1 values must be within __________ L of each other
A minimum of three acceptable manoeuvres should be saved and utilised for analysis/ interpretation.
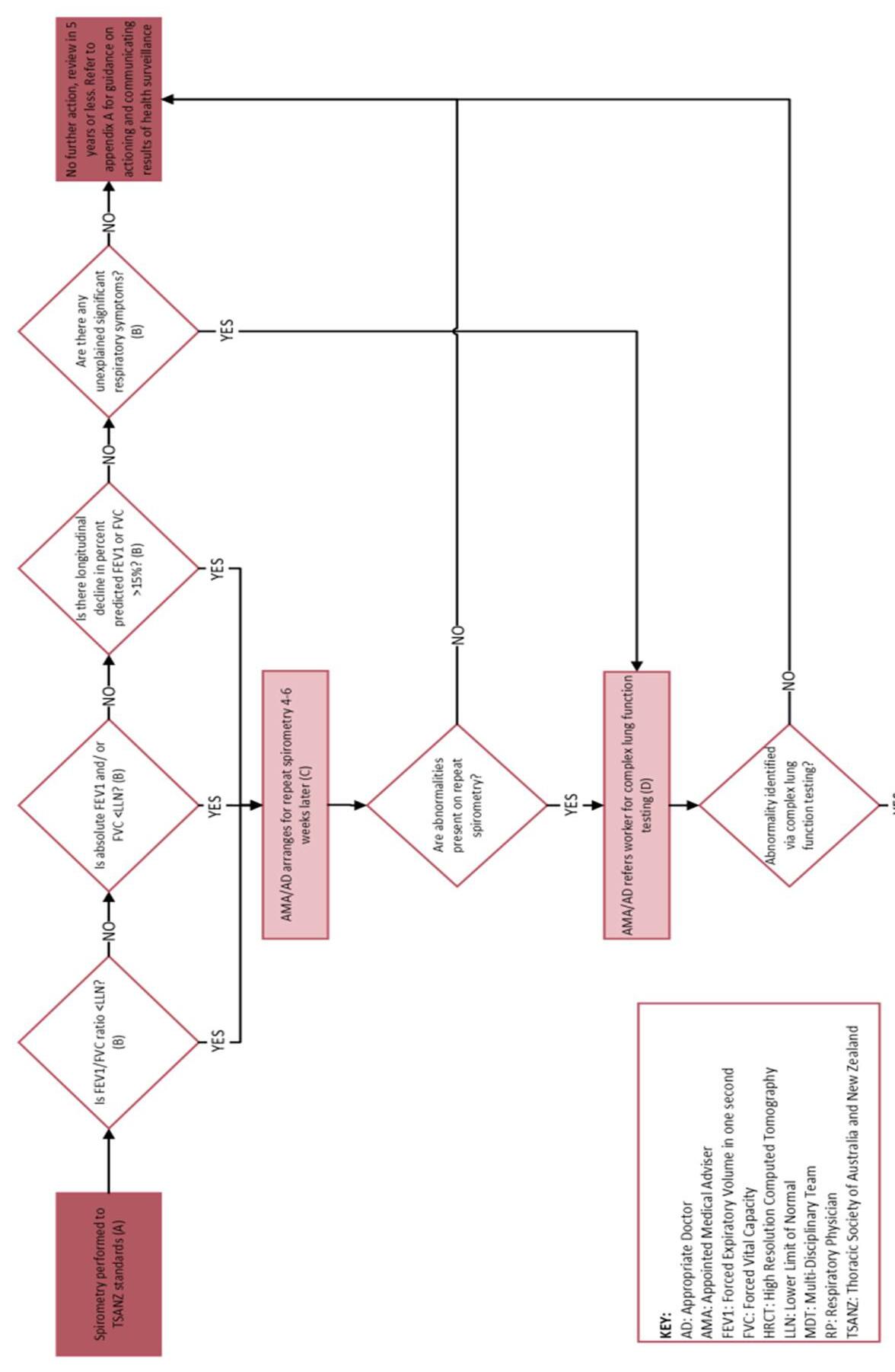
Figure: Process for Performing Spirometry for Resource Sector Workers.
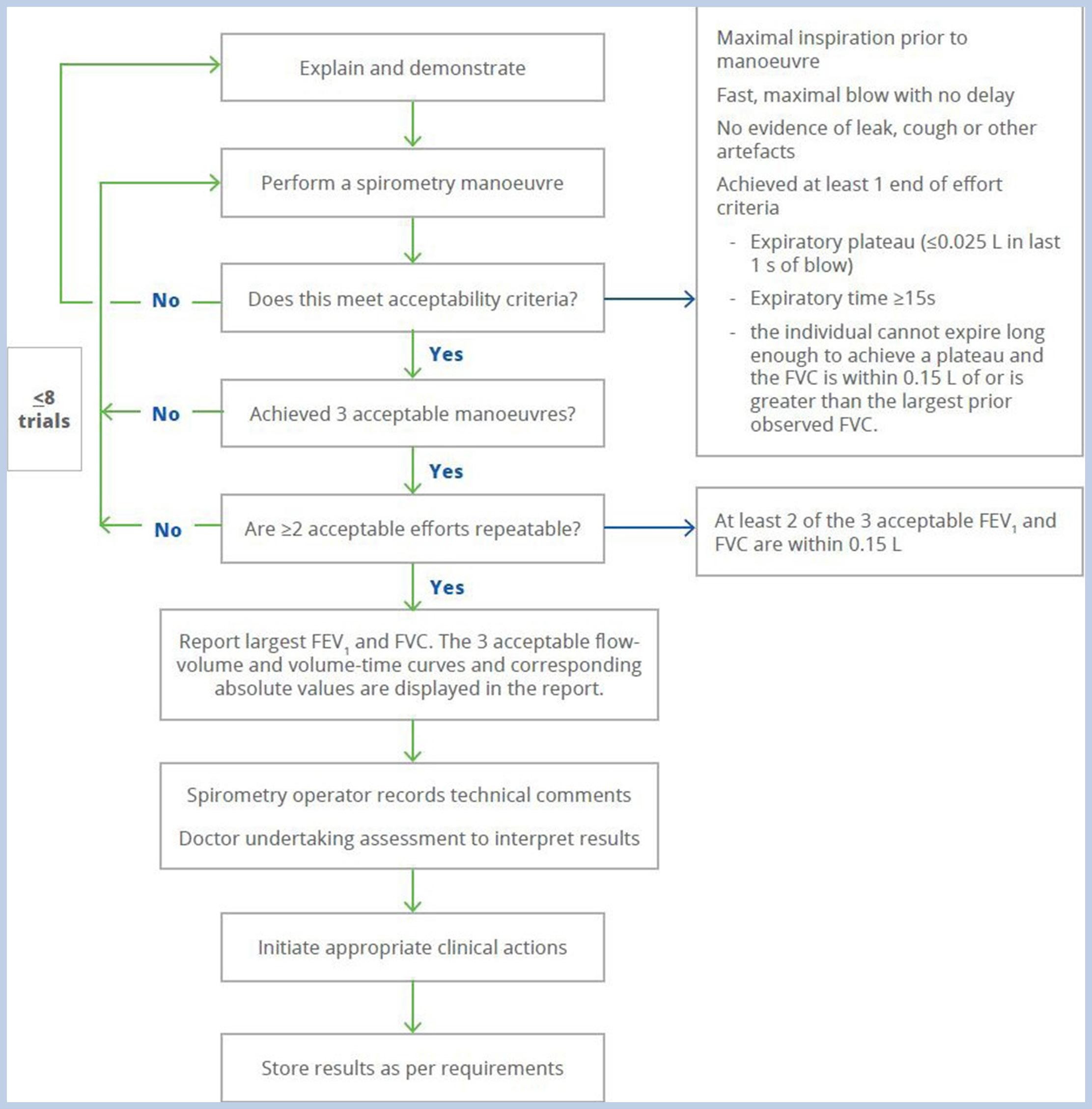
Available for download from our knowledge base: Click here to download.
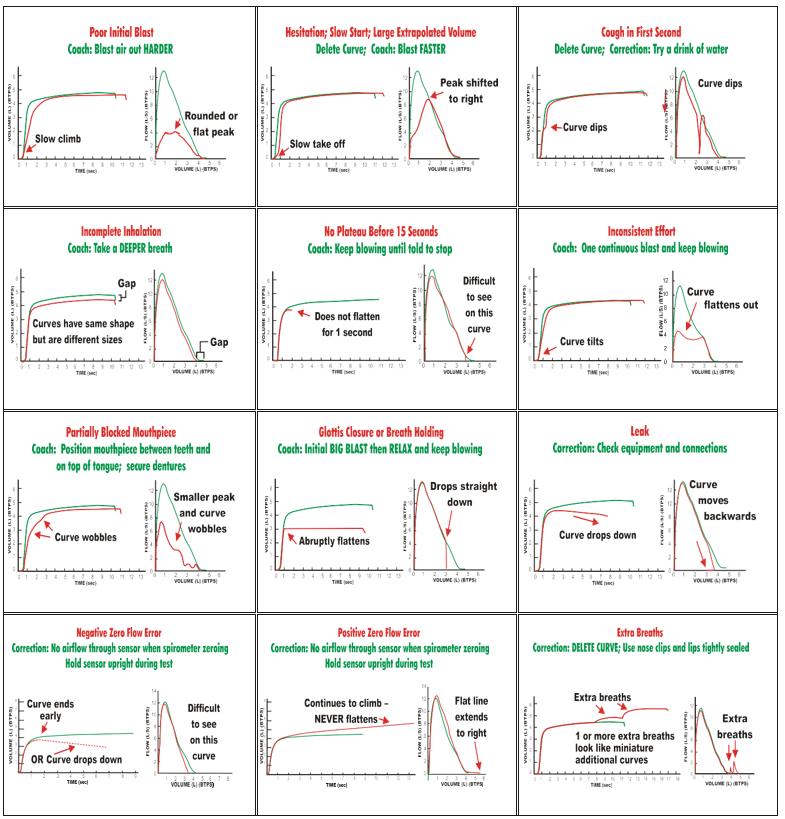
2012 NIOSH Spirometry Quality Assurance: Common Errors and Their Impact on Test Results
The below table outlines ways to correct the results.
FIVC-FVC > 0.100L or 5% of FVC whichever is greater, are not acceptable, but usable (pg.79 of 2019 standards)
Sub Maximal Inhalation:
Excessive Extrapolated Volume:
Sub Maximal Effort:
Cough in the First Second:
Early Termination:
Variable Effort:
Cessation of Airflow. Glottic Closure or Breath-Holding:
Partially Obstructed Mouthpiece:
Leak:
Extra breath:
Positive Flow Error:
Negative Flow Error:
Other Errors
Vocalisation – you will hear vocal sounds during exhalation
Solution: Demonstrate manoeuvre with puffed cheeks “like blowing candles out”
Opening mouth – noticeable as no trace or very small trace
Solution: Remind subject to seal mouth, or use a flanged mouthpiece
Uncooperative patient – at times subjects cannot or will not perform test. May be due to mental health or possible lack of trying
Solution: The harder you blow the more damage we can see in the lungs
If acceptability criteria is not met after 8 trials document it “Poor patient technique, best effort selected. Interpret with care!” Remember technical comments help with interpretation.
• FEV1 from loop with best PEF
• FVC – Largest VC. It can be selected from inspiratory or expiratory loop, or if obstructed perform an SVC
• “The largest FVC and the largest FEV1 (BTPS) should be recorded after examining the data from all of the usable curves, even if they do not come from the same curve.”
• All other parameters and loop should be selected from loop which has the largest combined FVC and FEV1
• Remember to look at your loops, a slow start can give a higher FEV1!!
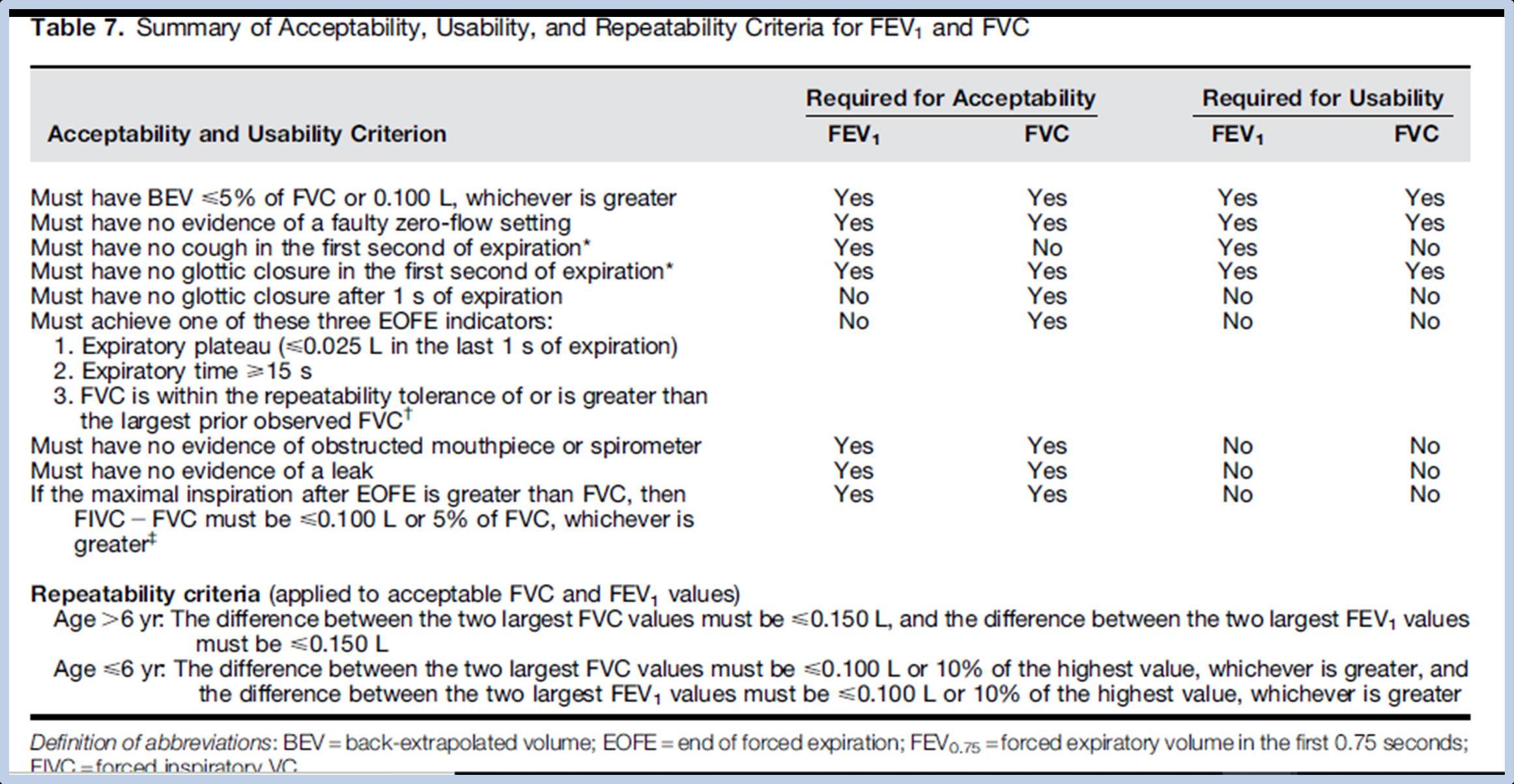
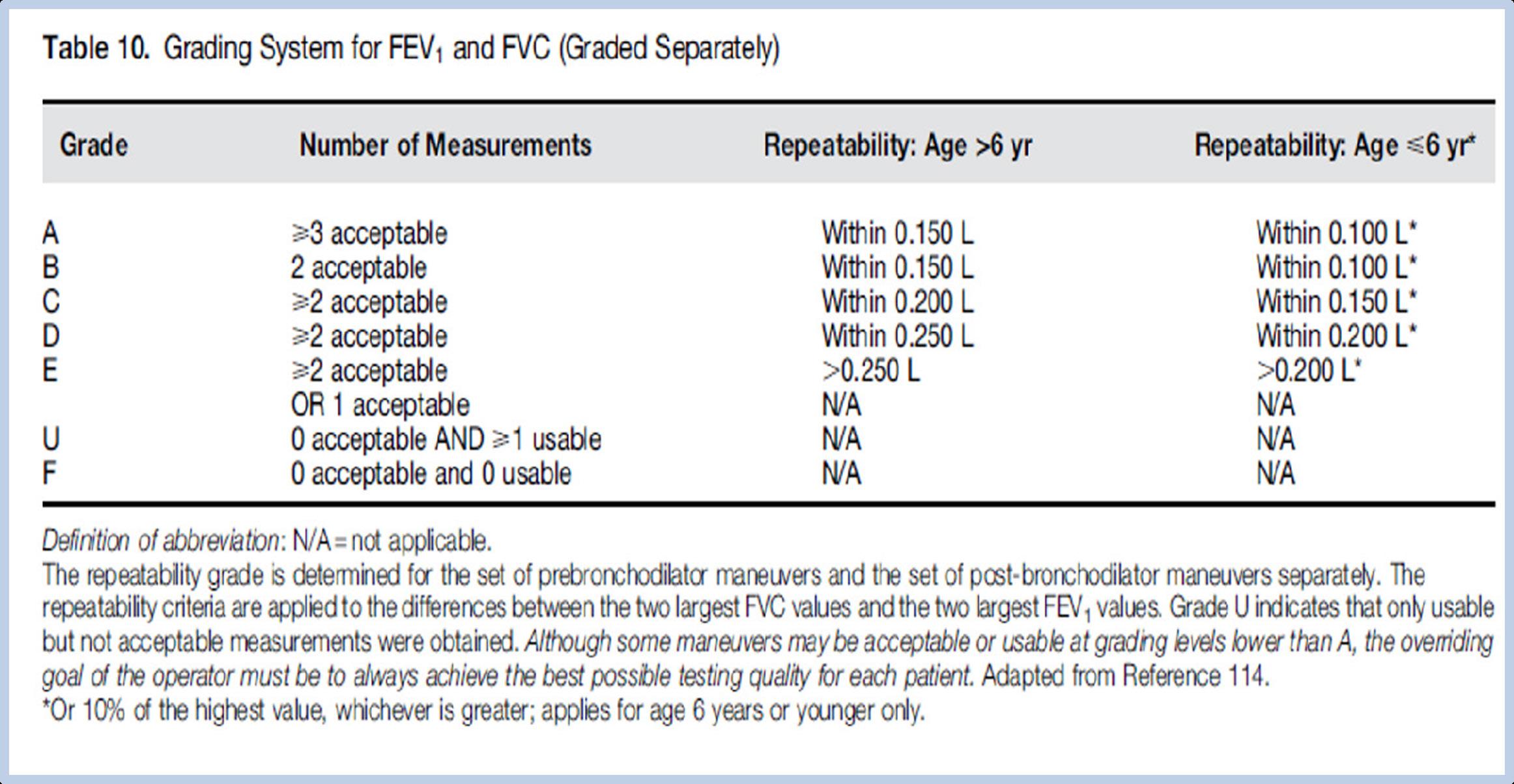
Grading your Spirometry
Syncope is a temporary loss of consciousness usually related to insufficient blood flow to the brain. The following are signs that syncope is about to occur:
• Colour drains from the face
• Patient appears to convulse slightly - this will then lead to patient losing consciousness and becoming flaccid.
• Patient will come around and may not be aware of “what just happened.”
• Use a chair without wheels and with arms
• Keep an eye on the subject, especially if a history of syncope is noted on the file
• Should signs of syncope arise the manoeuvre should be stopped, this will most likely lead to a reduced forced vital capacity (FVC). However, a slow vital capacity (SVC) can be performed to give a more accurate measure of VC.
• A relaxed manoeuvre could also be attempted where the subject exhales forcibly for the first 3 seconds and then instructed to relax the exhalation for the reminder of the manoeuvre. This is called the modified expiration technique
• Subsequent blows can be attempted if subject is closely monitored. Give at least a one-minute rest between subsequent manoeuvres.
• Document on the subject’s test result:
» “Syncope occurred during spirometry, FVC may be underestimated” or
» “Syncope occurred during spirometry; VC taken from an SVC manoeuvre”
» Ensure to place a note on subjects file, so that future assessors are aware that the subject may experience syncope upon testing.
Depend on accurate evaluation of:
• Height or arm span
• Age (natural aging effect)
• Sex (Women have smaller lungs)
• Race (often 10-20% less for non-Caucasians)
• Adult (>18 years)
• Paediatric (5-17 years)
• Obesity status (not essential but useful for interpretation)
The most recent comprehensive study was published in 2012. The GLI looked at data from 74,187 healthy non-smokers (57.1% females) in 40 countries aged 3-95 years
First global multi-ethnic reference equations for spirometry that span all-ages which has been endorsed by five international societies:
• Multi-ethnic reference equations using modern statistical methods, including development of age dependent lower limits of normal
• Previously each hospital selected their own preferred reference equations with which to interpret spirometry results
• However, since use of different equations has been shown to lead to different interpretation, this meant that results from any given individual could differ depending on where they were assessed.
• What reference equations do I apply for non-caucasians?
See Resouce on page 77
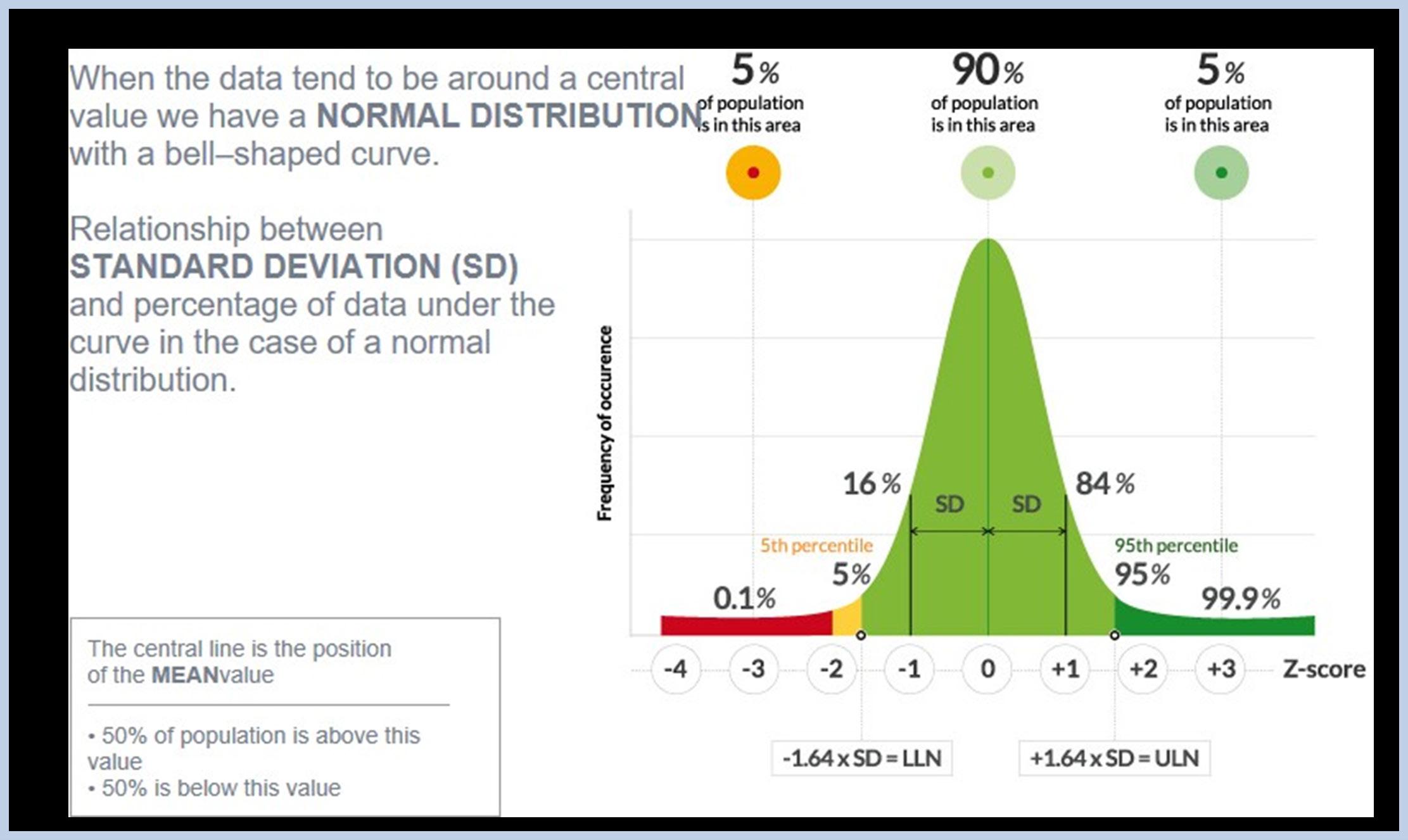
The chance the observed result falls within the distribution of values in healthy individuals.
At the 5th percentile(z score -1.645) there is a 5% chance that the results in a healthy individual would be below this level.
In spirometry, the LLN is the 5th percentile.
This means 5% of healthy individuals will have a false positive result
The 5th percentile is a trade-off between incorrectly classifying a low value in a healthy person and missing a clinically significant reduction in lung function.
The LLN does not necessarily indicate a pathophysiological abnormality, nor is it a clinically meaningful threshold to diagnose disease. It provides an indication of whether the observed result can be expected in otherwise healthy individuals of similar.
• age
• sex
• and height
A result within the expected range for a subject does not exclude the presence of a disease process impairing function. Results close to the LLN should be interpreted with caution and the individual’s medical history, physical findings, and pre-test probability of disease taken into consideration during interpretation.
This further emphasizes that the interpretation should be informed of the patient’s clinical notes and not solely rely on the numbers generated in the report.
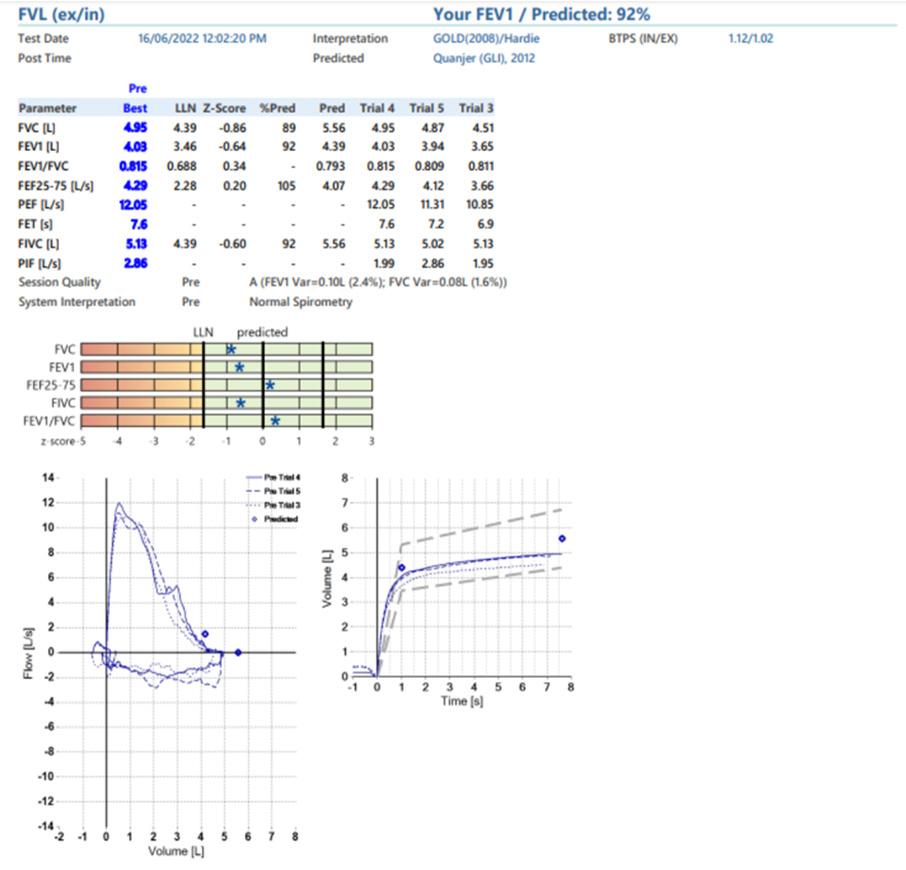
• The measured FEV1/FVC is 67% which is above the LLN of 62%, with the GLI 2012 Z-score being −1.01.
• Therefore, the measured FVC is then evaluated and at 4.70 L (Z-score of 0.97), the FVC is also above the LLN of 2.98 L.
• Thus, this spirometry result is within the normal limits.
• The dots on the Z-score pictogram clearly show that all values are within the normal range.
• Although the measured FEV1/FVC is <0.7, these spirometry results do not indicate an obstructive spirometric pattern because the LLN is 62% for this individual.
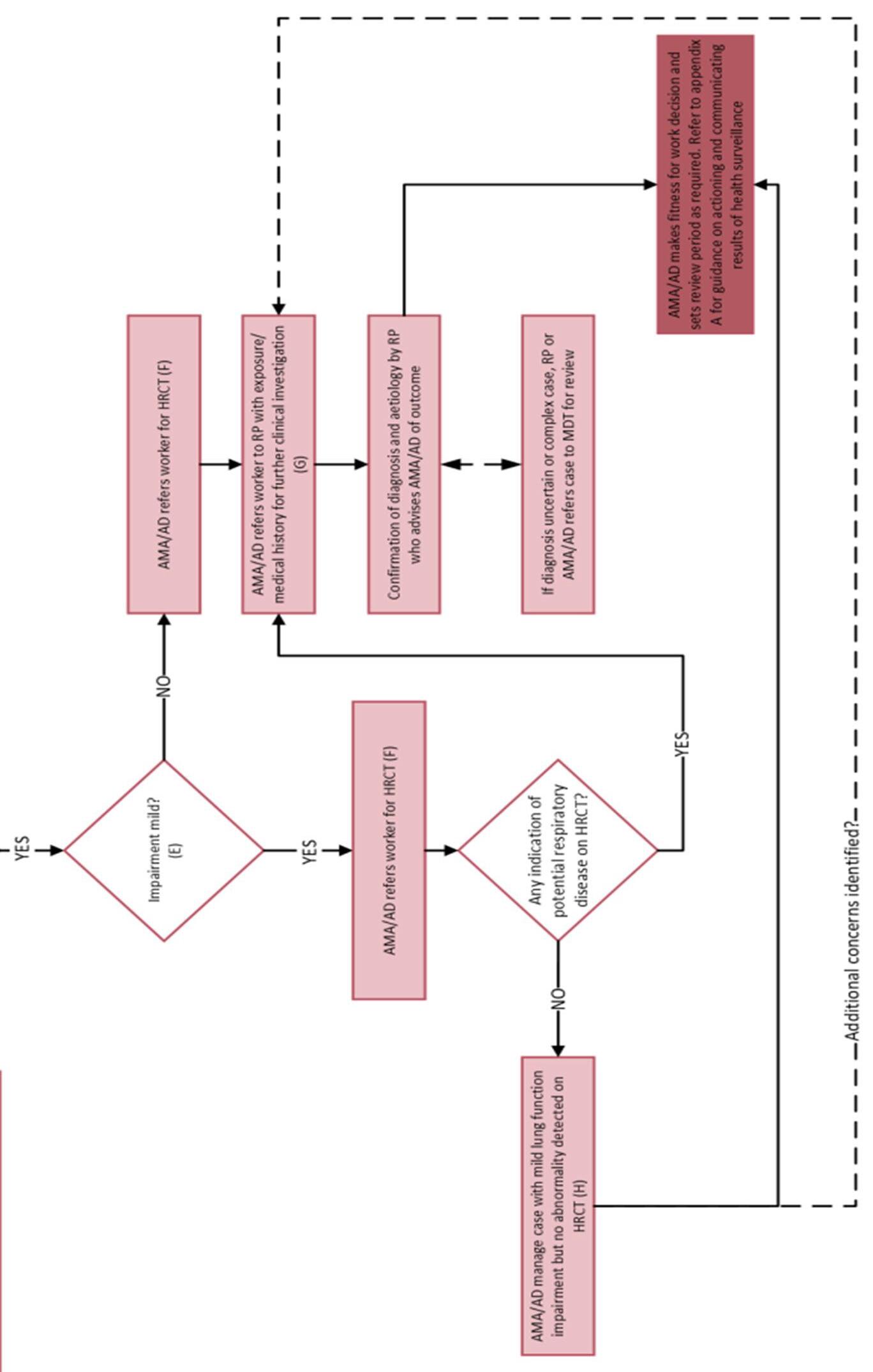
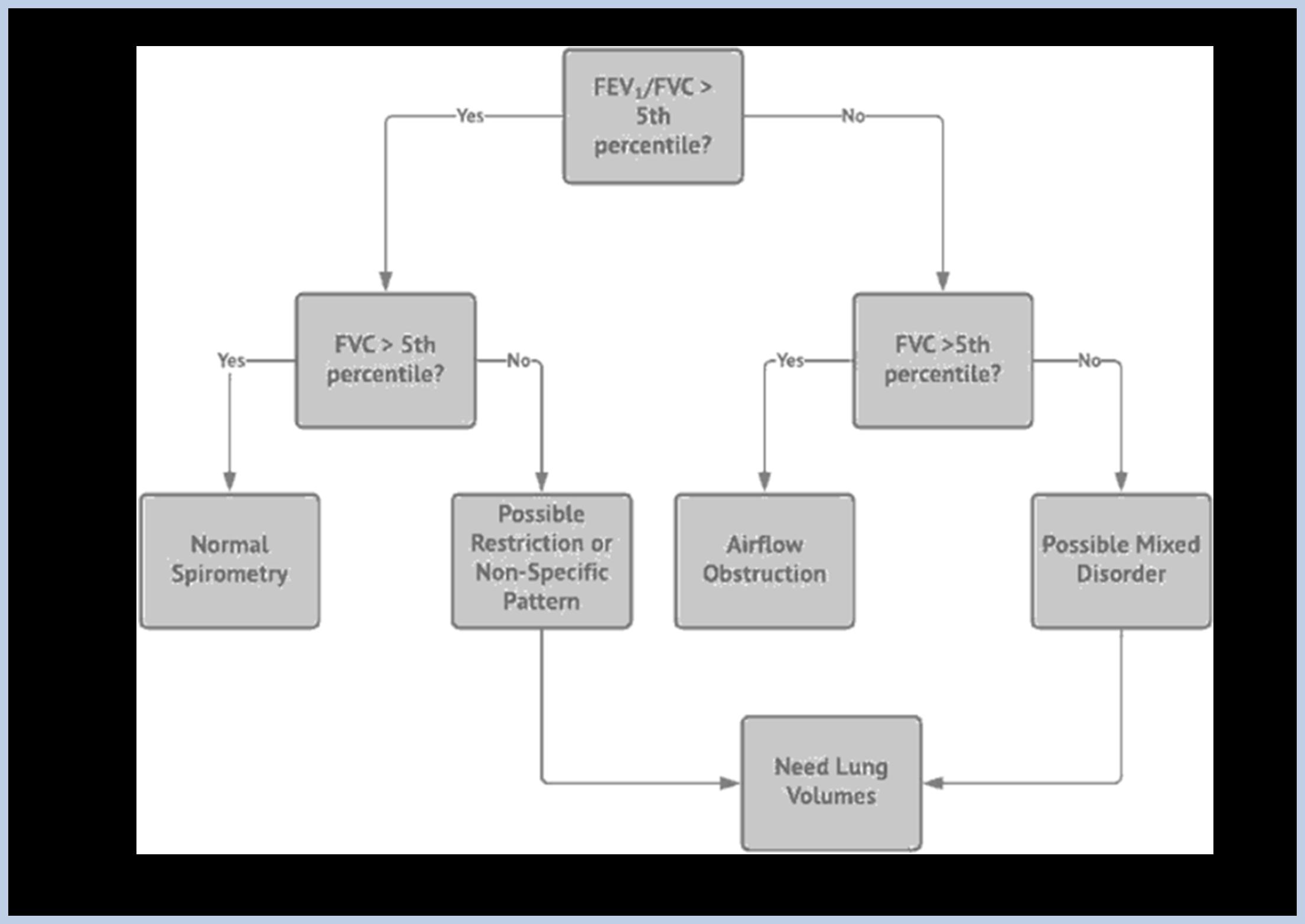
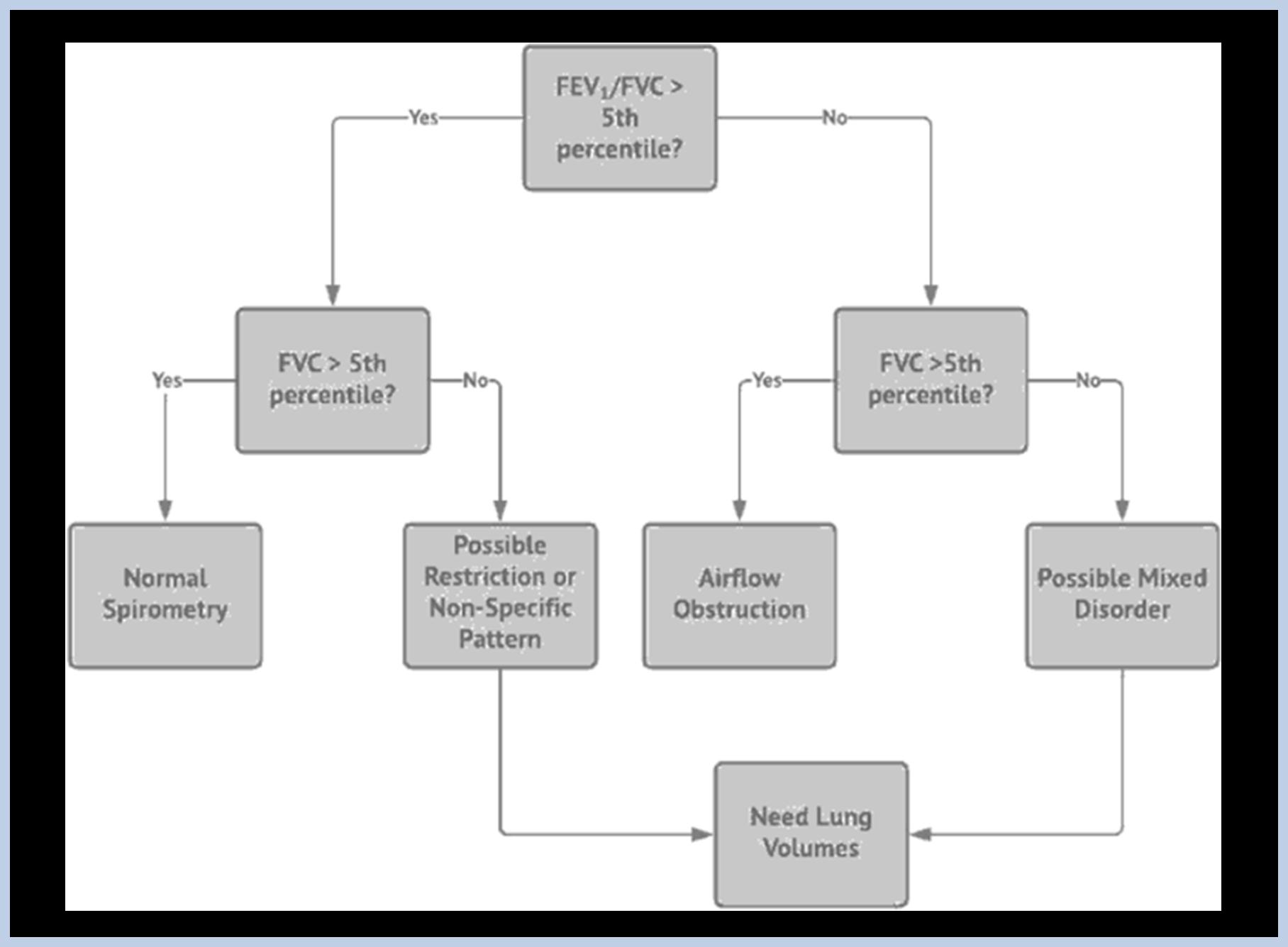
Spirometry results must be interpreted in line with any clinical guidelines (see clinical pathway guideline on page 36) mandated within the worker’s jurisdiction. Otherwise, the most recent ATS/ERS Pulmonary Function testing Interpretation guidelines should be followed(see diagram below). The doctor responsible for reporting on the health assessment must use the appropriate guidelines to determine the appropriate process for follow-up investigation and referral as clinically appropriate. A clinical interpretation of the spirometry assessment must be included in the spirometry report or linked clinical records (as mandated within the worker’s jurisdiction).
These TSANZ Standards recommend that:
• Spirometry of lower quality (ATS/ERS graded C or lower) is generally not be suitable for interpretation.
• Providers should consider retesting workers to ensure appropriate spirometry results are available.
• Individuals should be referred to a respiratory and/or occupational physician as appropriate to the clinical findings if the following conditions are met:
• Absolute FEV1, forced vital capacity (FVC) or FEV1/FVC is less than the lower limit of the normal (LLN) as determined using the GLI reference equations, or
• FEV1 or FVC, expressed in GLI % predicted, declines by > 15% predicted from baseline test over any period.
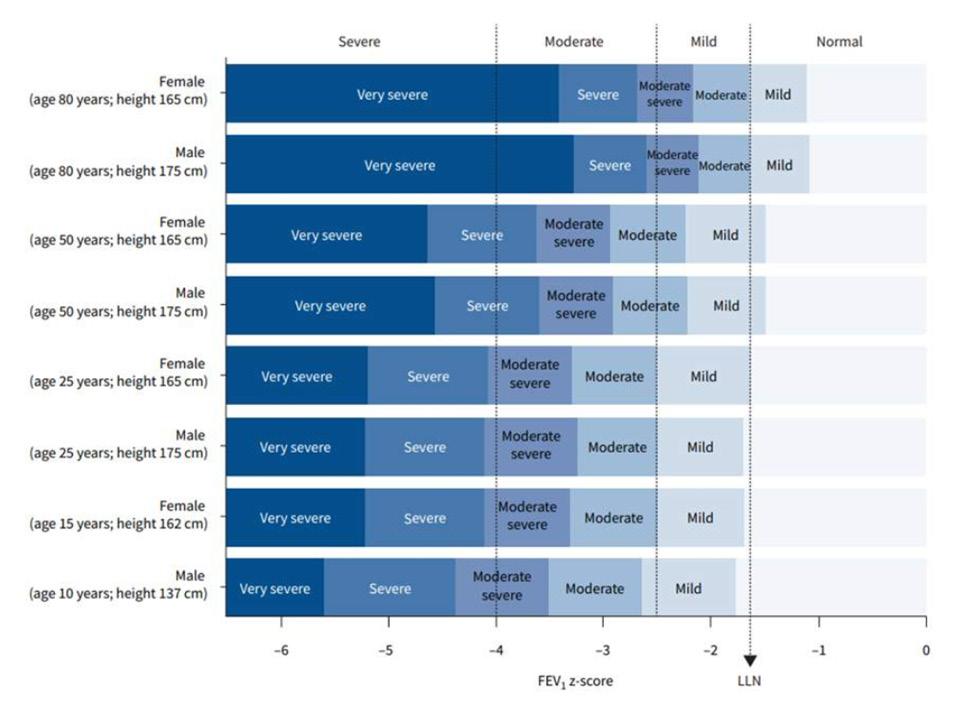
Z- score Classification
Independent of:
• Age
• Height
• Sex
For example, if the Z–SCORE for any parameter is –1.64, this signifies in males, females, children, and adults that the measured value is at the 5th percentile. In lung function testing this is regarded as the LLN.
A plot comparing the old 2005 grading thresholds to the new 2022 proposed z-scores - ERS/ ATS technical standard on interpretative strategies for routine lung function tests (2022).
The 5th percentile (LLN) which represents a z-score of -1.645 is shown as the vertical arrow.
The new proposed cut levels of -4 and -2.5 are shown as solid lines with the new grading at the top of the figure.
You can see how as the subject ages using the predicted there are more people falling into the mild obstructive zone. When interpreted using the z score these subjects fall into the normal zone.
In the younger subjects, you can also see some that would have been considered normal now fall into the mildly obstructed zone.
ERS/ ATS technical standard on interpretative strategies for routine lung function tests. (2022).
How should restriction be classified.
Ideally restriction should be classified using the TOTAL Lung Capacity (TLC) z score. This is why further complex lung function should be organized if a clients results show a restrictive pattern.
In the example below, you can see that in example one the classification is moderate with both the TLCand the FVC z score. BUT, in example 2 the female client is classified as severe when using the TLC z score but only mild when using the FVC z score.
FEV1 can be affected by obstruction. FVC defined by changes in the TLC and residual volume (RV).
Interpretative strategies for lung function tests:
• https://www.thoracic.org/statements/resources/pft/pft5.pdf
Standardisation of spirometry. 2005:
• https://www.thoracic.org/statements/resources/pfet/PFT2.pdf
Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement:
• https://www.atsjournals.org/doi/10.1164/rccm.201908-1590ST
Stanojevic S, Kaminsky DA, Miller M, Thompson B, Aliverti A, Barjaktarevic I, et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur Respir J. 2021 Dec 23:2101499. doi: 10.1183/13993003.01499-2021
It is critical to evaluate an individual’s lung function over time rather than an assessment of a single point in time compared against reference equations. This includes monitoring known abnormalities or assessing the effect of an intervention or occupational exposure.
A meaningful change over time must be greater than the inherent variability of the measure, which tends to be greater over weeks to months, than daily in biological controls.
Measures of FEV1 or FVC, expressed in GLI % predicted, that decline by > 15% from baseline test over any period should be considered to be outside the normal longitudinal variability of spirometry.
The following worked example illustrates how to appropriately determine a change in spirometry over time in an individual. The use of appropriate alignment with robust predicted equations allows for changes with age to be accounted for. This example highlights that a significant decline in lung function can occur in individuals whose lung function remains within the normal range of the broader population.
A female worker, of Aboriginal ancestry, 170.5 cm tall enters the resource sector workforce at age 25.5 years. The Global Lung Function Initiative Spirometry ‘Other’ predictive equations are used as per ANZSRS recommendations.
Her lung function on entering the workforce was:
• FEV1 3.48 L (103.1% predicted, LLN = 2.74 L)
• FVC 3.94 L (100.8% predicted, LLN = 3.16 L)
• FEV1/FVC 0.88 (101.7% predicted, LLN = 0.762)
Her spirometry is within normal limits. She does not report taking any respiratory medications.
At age 30.0 her respiratory health is reassessed. There are no reported symptoms, she does not report taking any respiratory medications and her lung function is:
•
FEV1 3.31 L (95.1% predicted, LLN = 2.65 L)
• FVC 3.87 L (99.4% predicted, LLN = 3.15 L)
•
FEV1/FVC 0.81 (95.2% predicted, LLN = 0.750)
Her lung function remains within normal limits. Her change in FEV1 (% predicted) over the five-year period is 8.0% (103.1% - 95.1%) and within acceptable limits.
At age 33.6 years she changes employers and undergoes a repeat assessment. She has no reported symptoms and does not report taking any respiratory medications. Her spirometry is:
• FEV1 2.85 L (87.6% predicted, LLN = 2.599 L)
• FVC 3.79 L (98.0% predicted, LLN = 3.131 L)
•
FEV1/FVC 0.75 (81.9% predicted, LLN = 0.741)
Her spirometry is within normal limits. Her change in lung function since entering the resource sector workforce at age 25 years is 15.5% (103.1% to 87.6% - after adjusting for age-related changes by using the GLI predicted equations). Based on the recommendations (above) her age-related longitudinal decline over the 8.1 years of employment exceeds 15.0%. She should be referred to an occupational and/ or respiratory physician for further assessment.
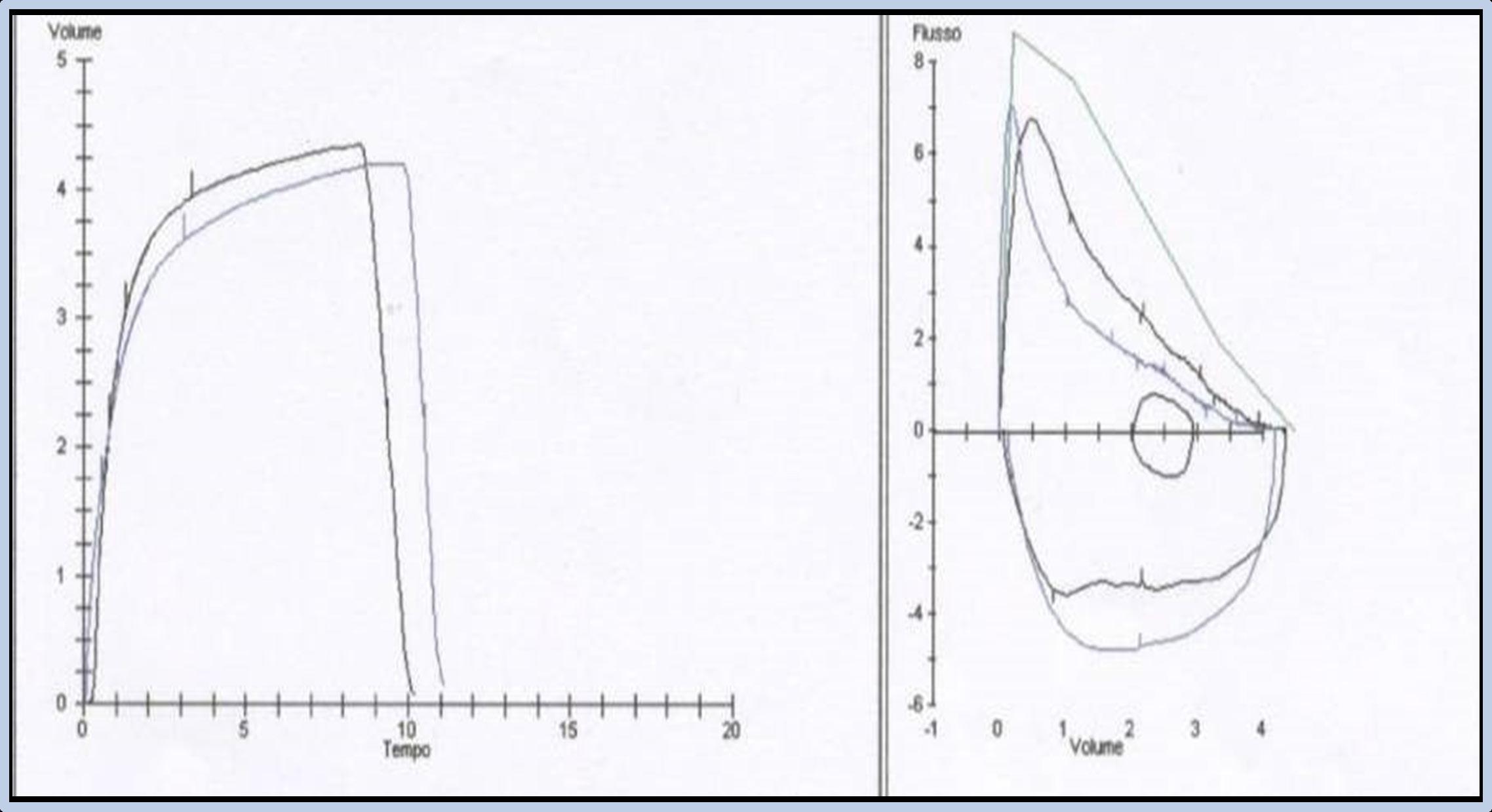
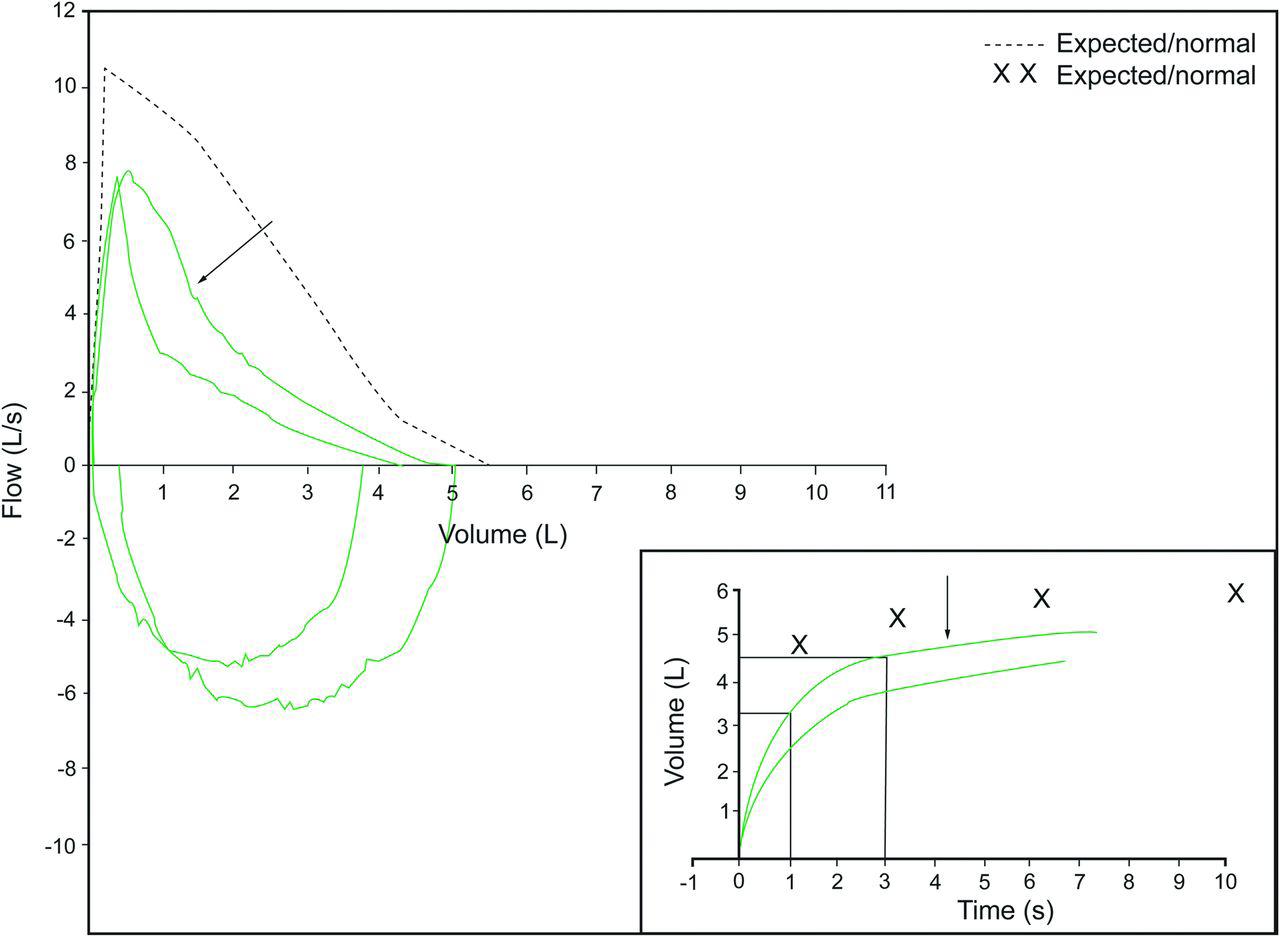
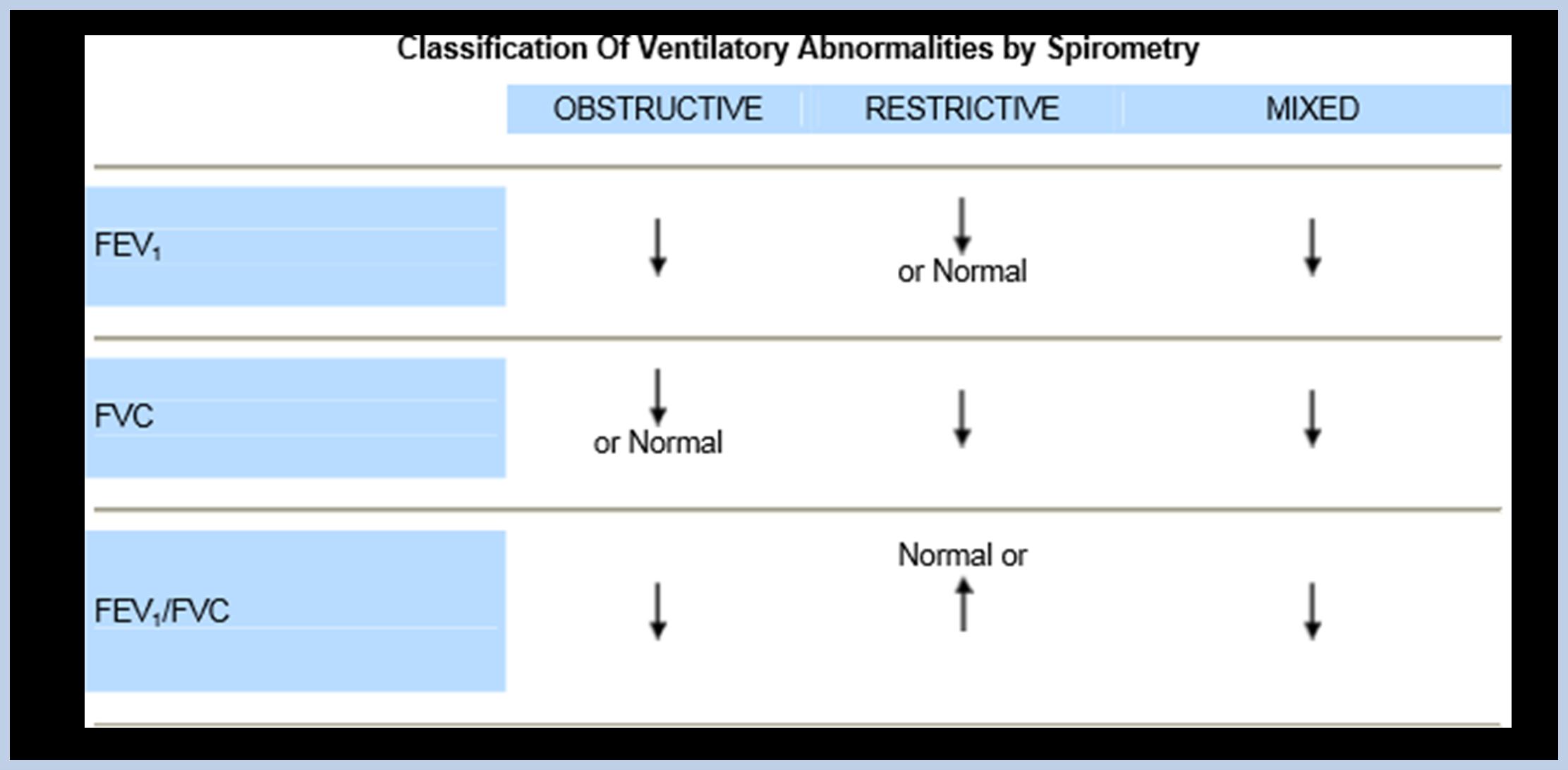
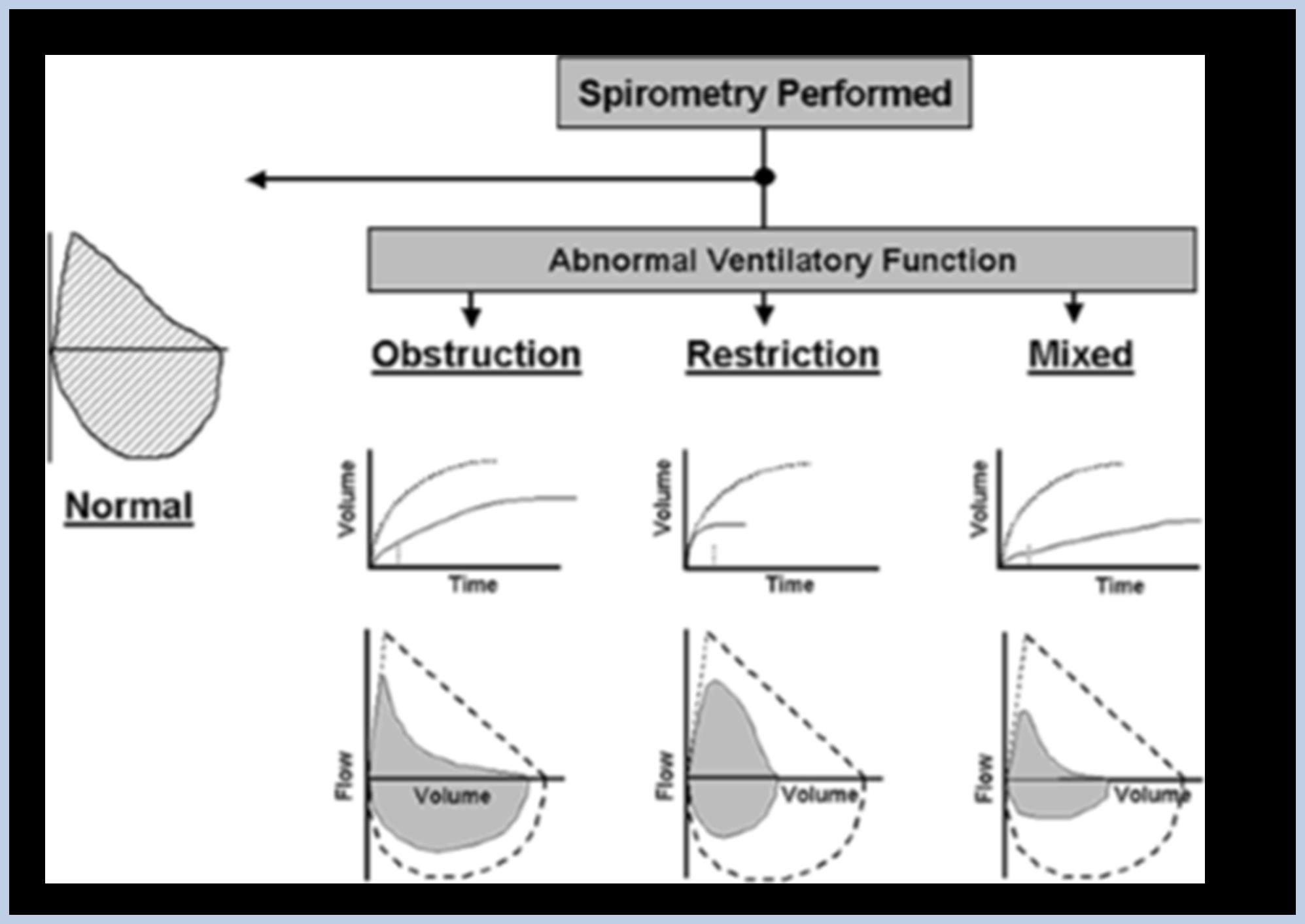
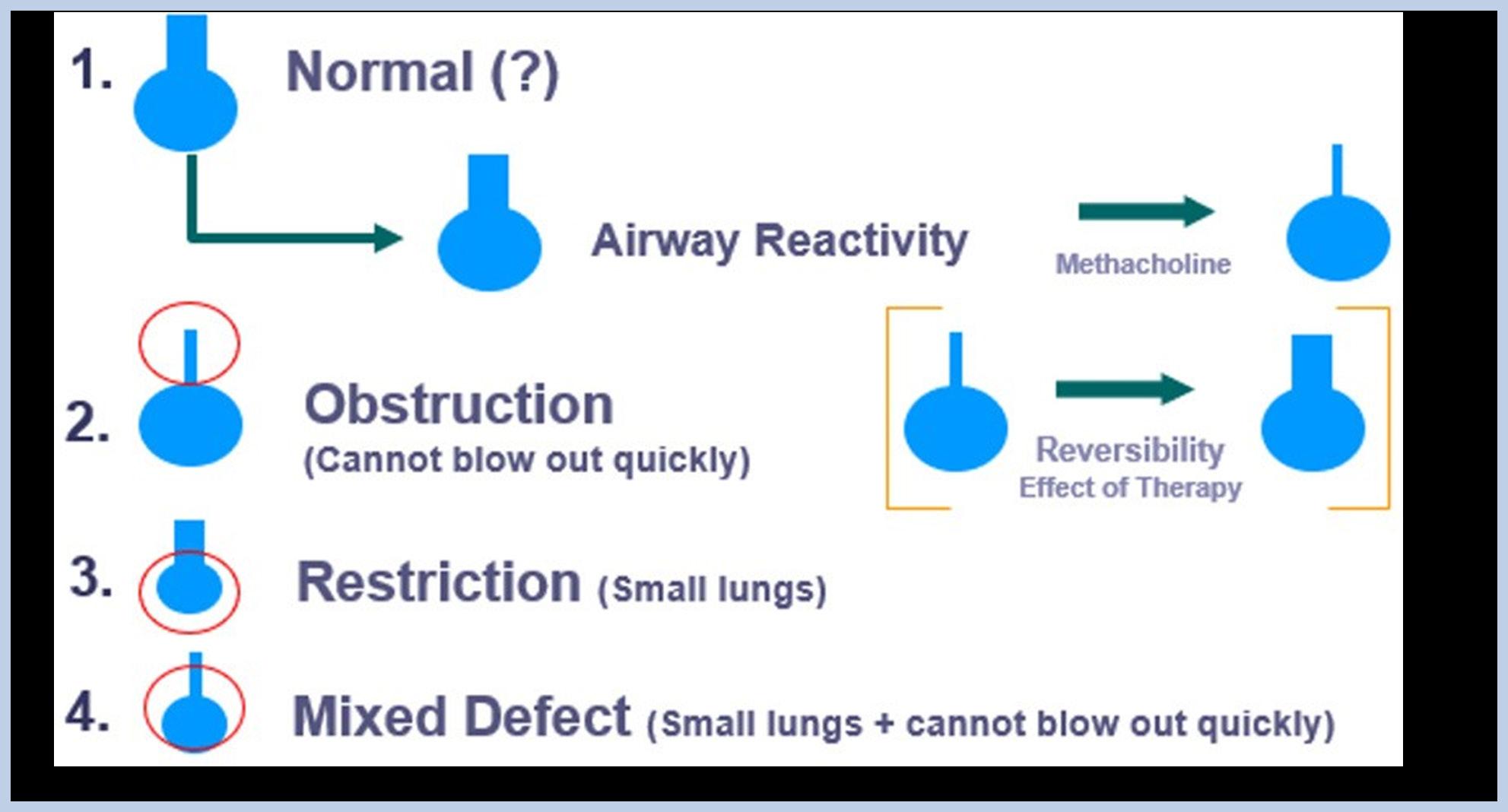
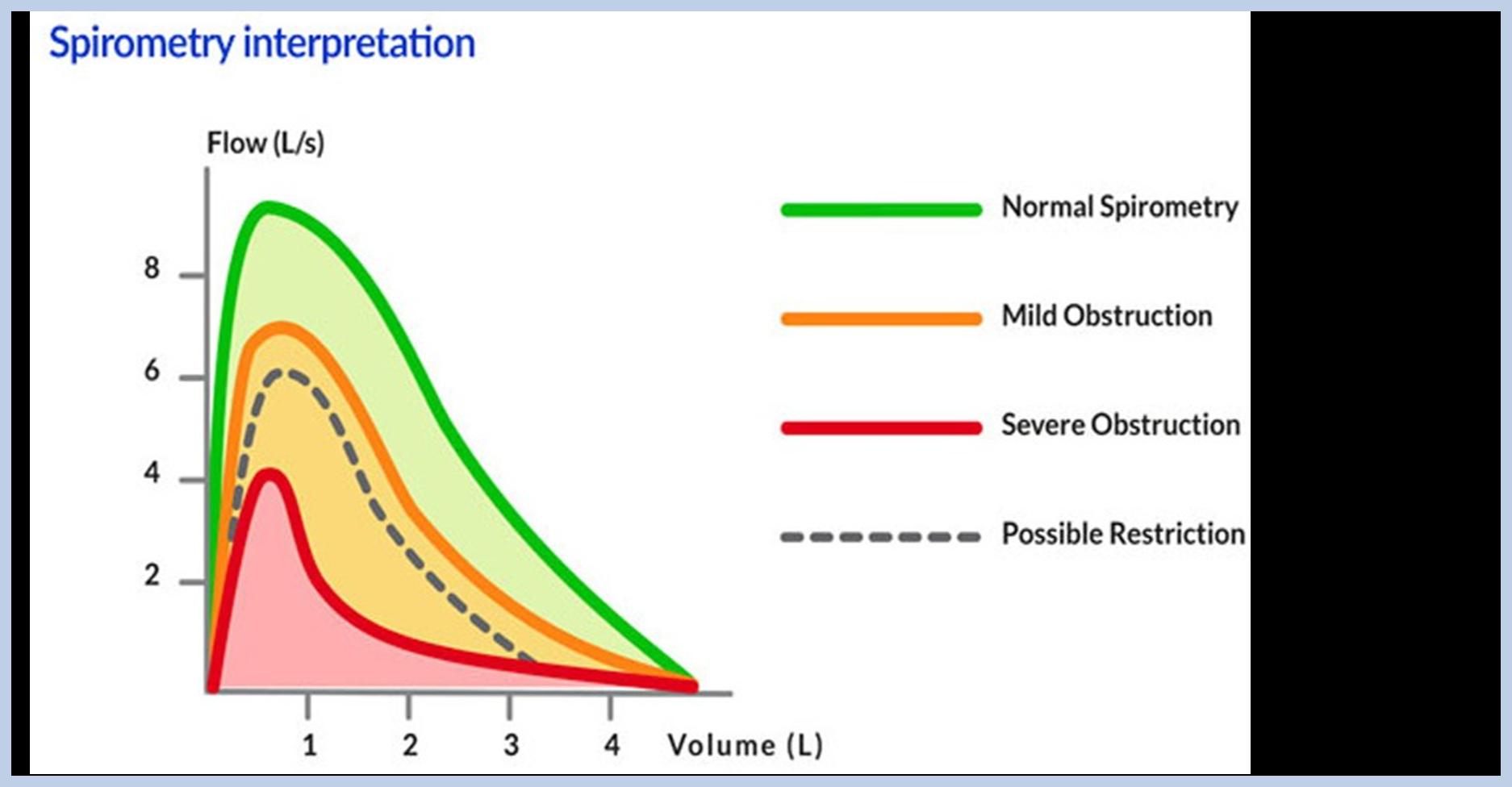
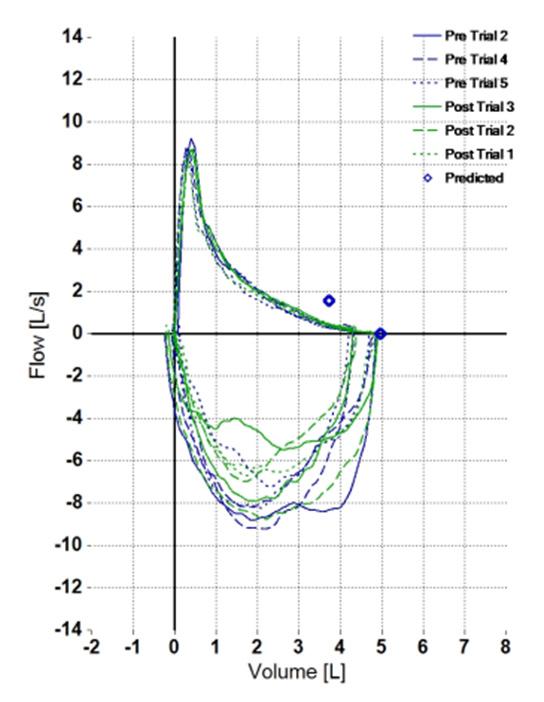
How is an obstructive curve charterised? What are examples of obstructive lung disease?
How is asthma differentiated from COPD?
Mild vs Severe Obstruction
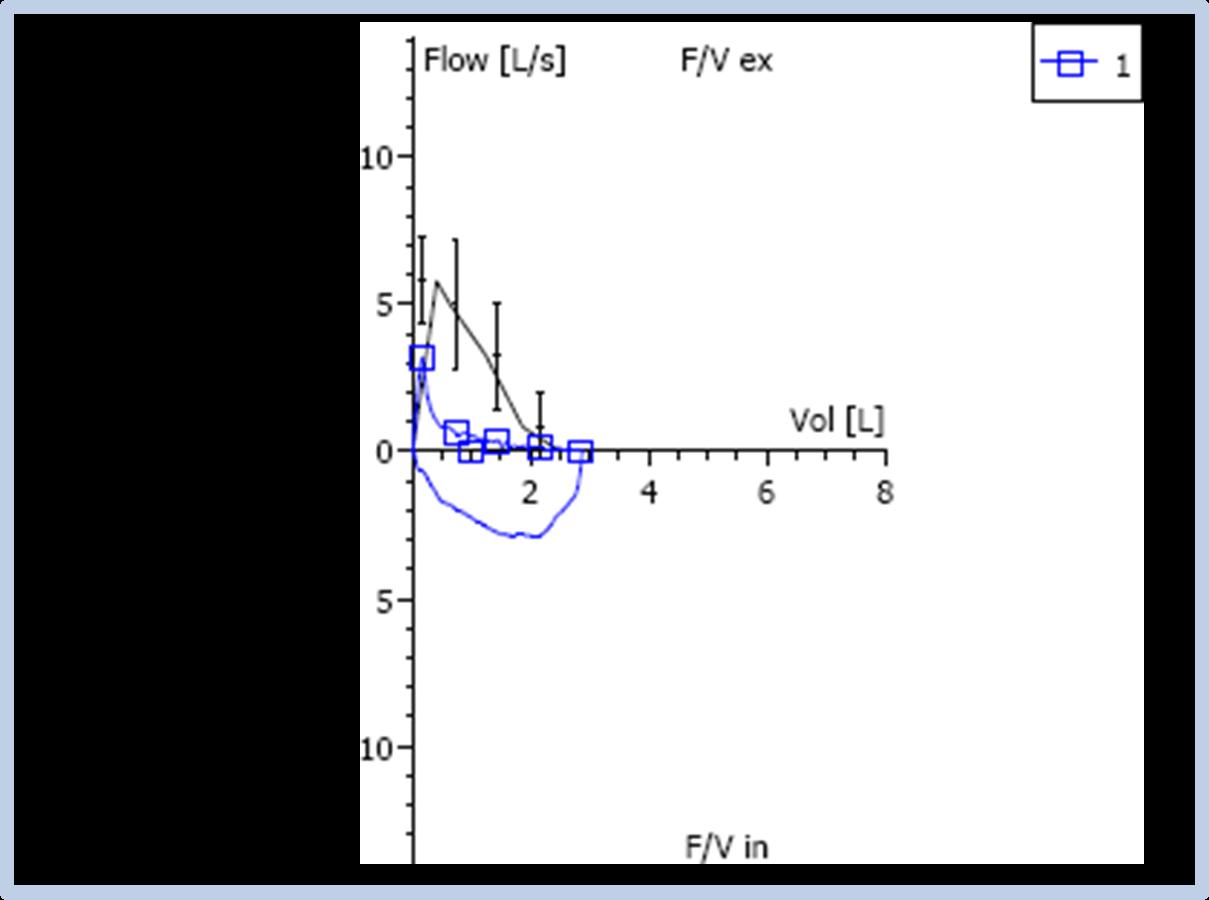
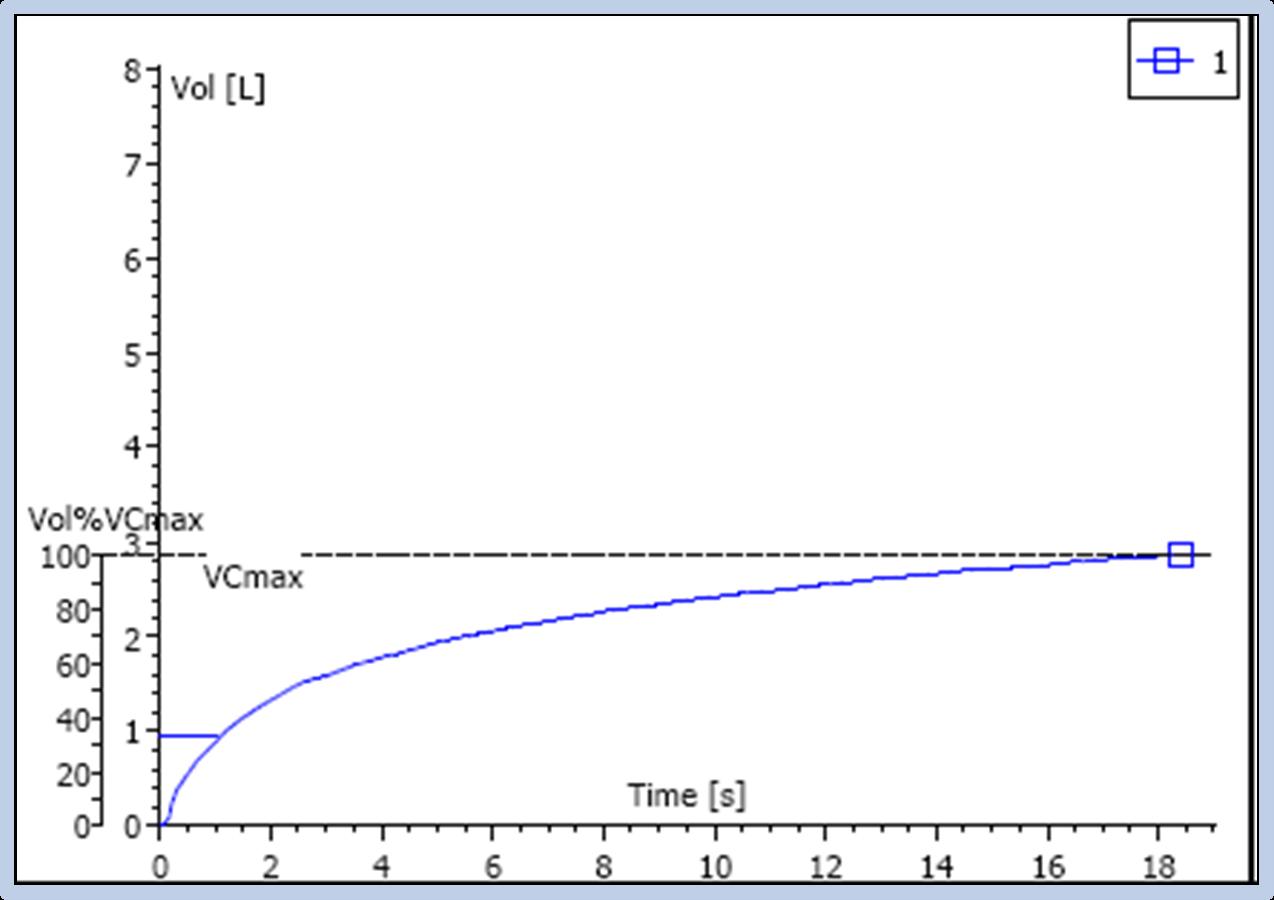
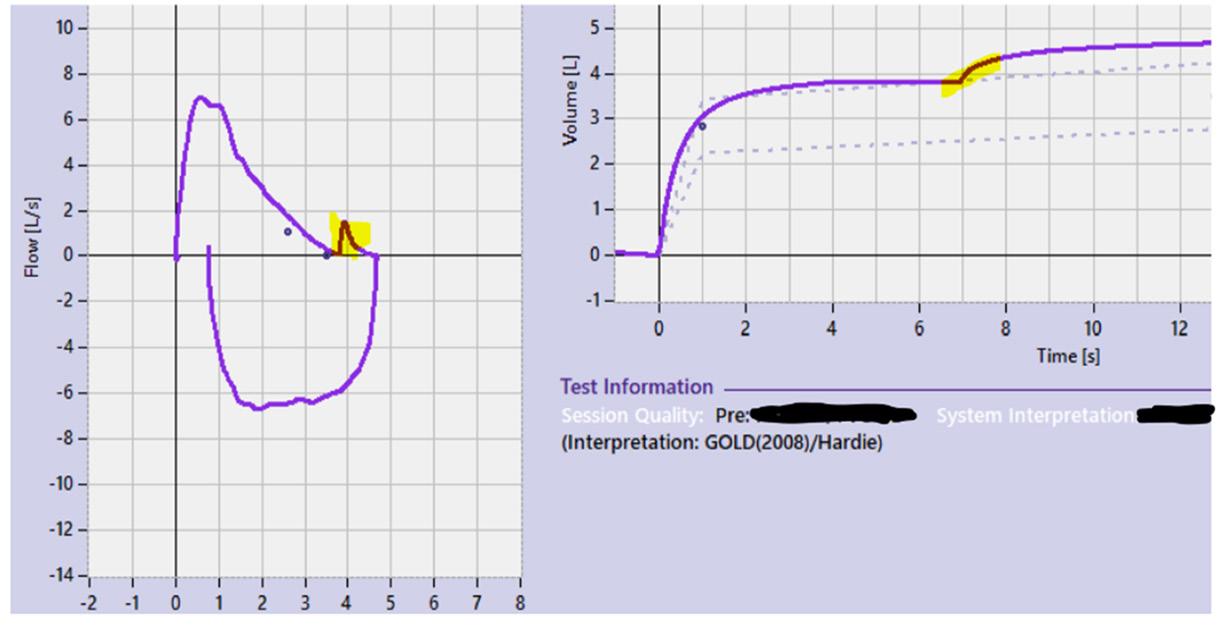
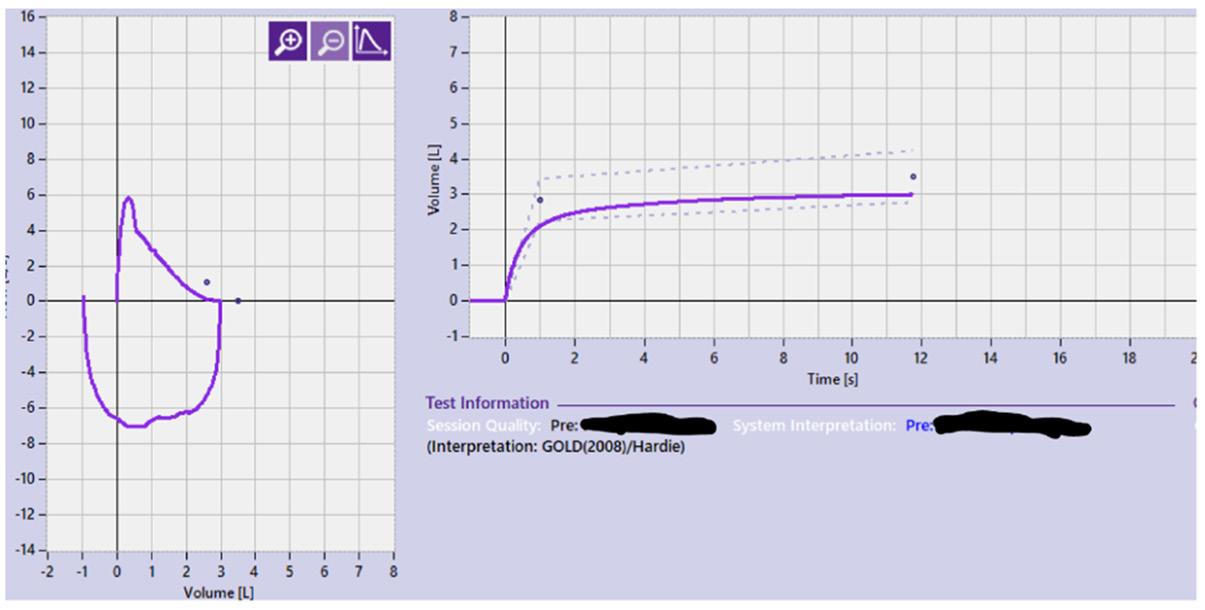
Below is an example of a severe obstruction:
Note the concave shape
Exhalation time- 18 seconds
Spirometry is repeated at least 15 minutes following the administration of standardised bronchodilator therapy.
For optimal effect, it is suggested that four separate doses of 100µg of SABA (e.g., salbutamol) be administered by a metered dose inhaler (MDI) via a spacer at approximately 30 second intervals.
• After a gentle and incomplete expiration, actuate the SABA metered dose inhaler at the beginning of a slow inhalation to TLC from a spacer. The breath is then held for 5–10 seconds before the patient exhales
Trigger for performing Bronchodilator Responsiveness Test.
If any Value (FEV1 or FVC or FEV1/FVC) is < LLN. AND
If FEV1/FVC ratio is <80% (KINNECT students ONLY - if it can be accommodated clinically)
A low ratio and FEV1 indicates obstruction.
A low FVC could indicate gas trapping- performing a BD test will allow the interpreter to see if there Is a response to BD which can assist in determining disease.
There has been a change to what is considered a significant bronchodilator response. The calculation has been amended to include predicted value (determined using the appropriate GLI spirometry equation).
A significant response used to be 12% and 200 ml this has been updated to >10%
Example of how to perform calculation
Post BD value - Pre BD value x 100 Predicted GLI value
Post BD FEV1 = 4.53
Pre BD FEV1 = 4.04
not significant using the 2022 BDR equation
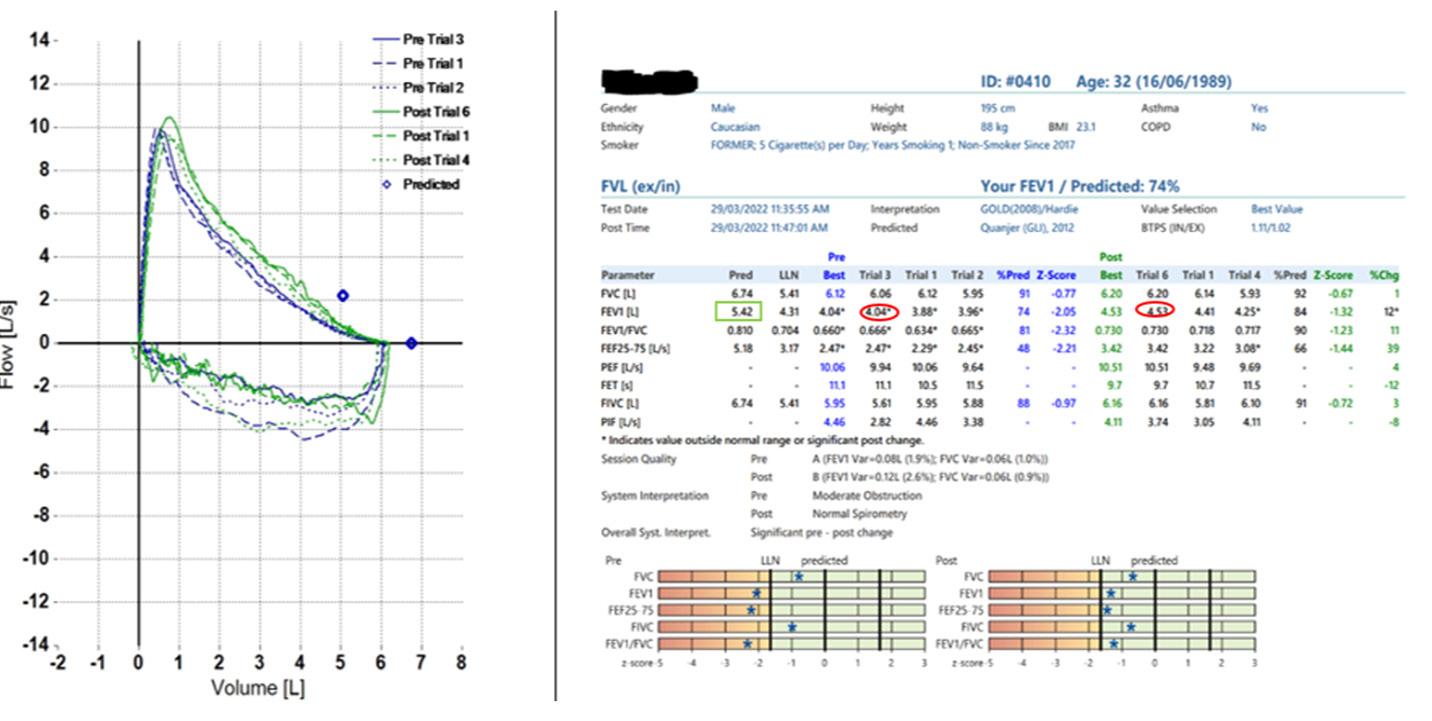
The old criteria favoured a BD response in those with a lower FEV1 Start value and the 200ml criteria favoured males.
The outcome of the change:
A study was carried out to evaluate the effects of this change. Below are the results of this study.
3051 patients (54% male) with FEV1/FVC z-score <-1.645
Old criteria (.12% start FEV1 + 200mls)
New criterion (>10% predicted FEV1)
1070 responsive (60% male)
768 responsive (52% male)
302 fewer responsive (28% drop)
25 new responders (64% female)
327 no longer responders (77% male)
What is dynamic compression, and why should an SVC be performed?
Slow Vital Capacity
• A maximum of 8
• Performed before FVC
• Stable baseline - at least three tidal breaths with end expiratory lung volume within 15% of the VT - should be achievable within 10 breaths
• Breath all the way out to RV and then take a deep breath in to TLC, and then breath normally
• Acceptability = difference between largest and next largest is>150ml or 10% VC whichever is smallest
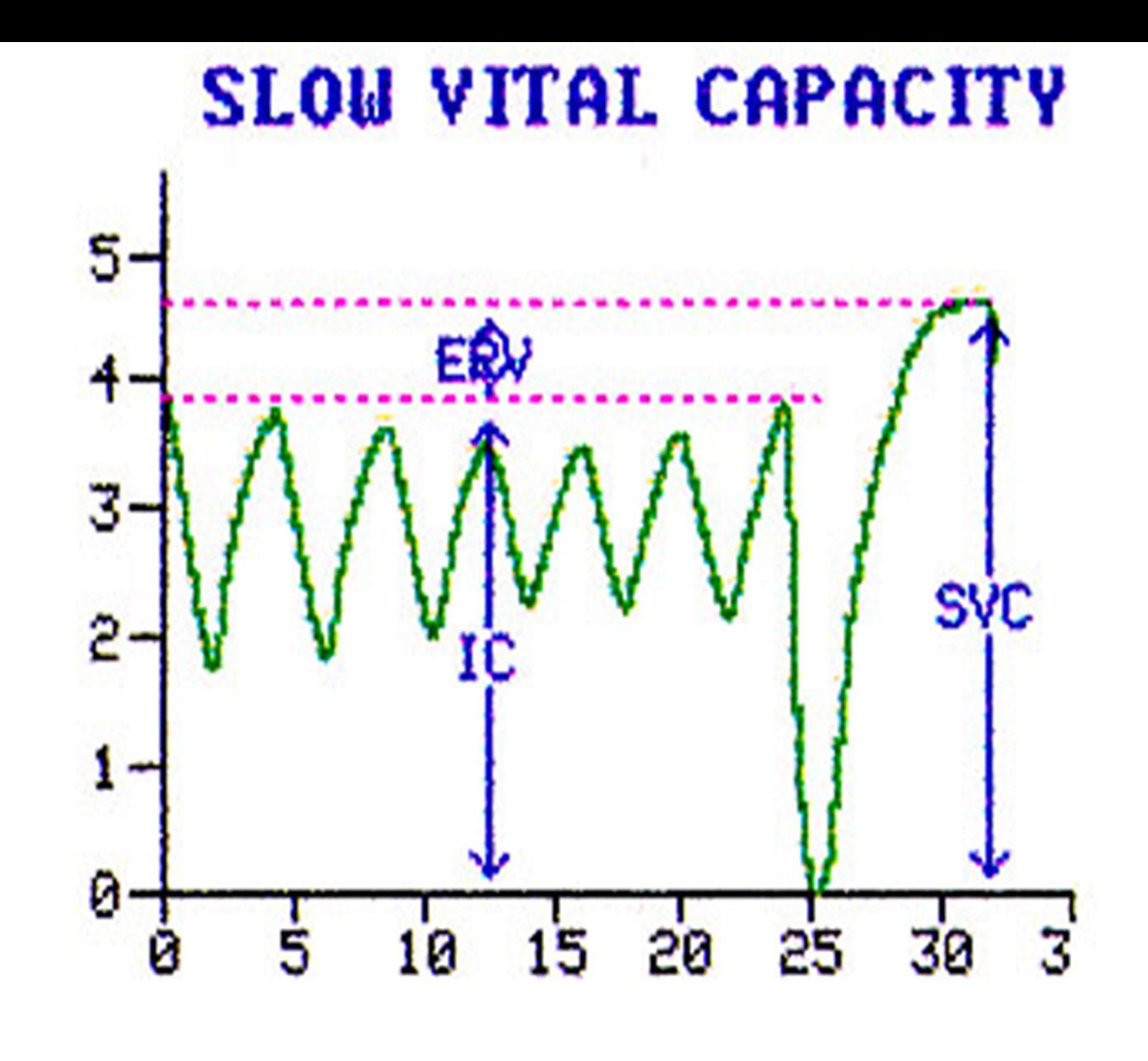
• Largest value of three acceptable should be selected. Restrictive Lung Disease
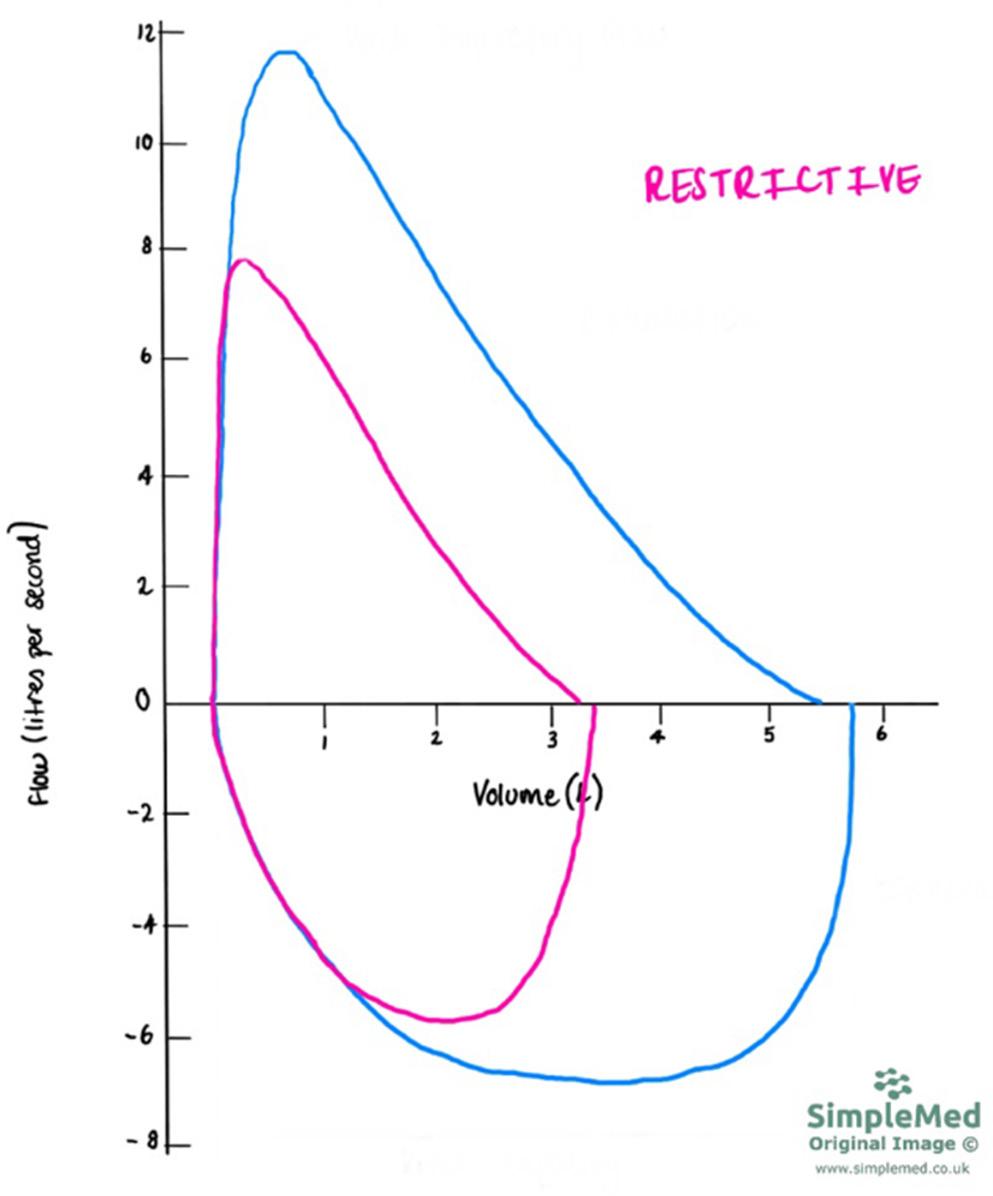
How is a restrictive curve characterised? What are example of restrictive lung disease?
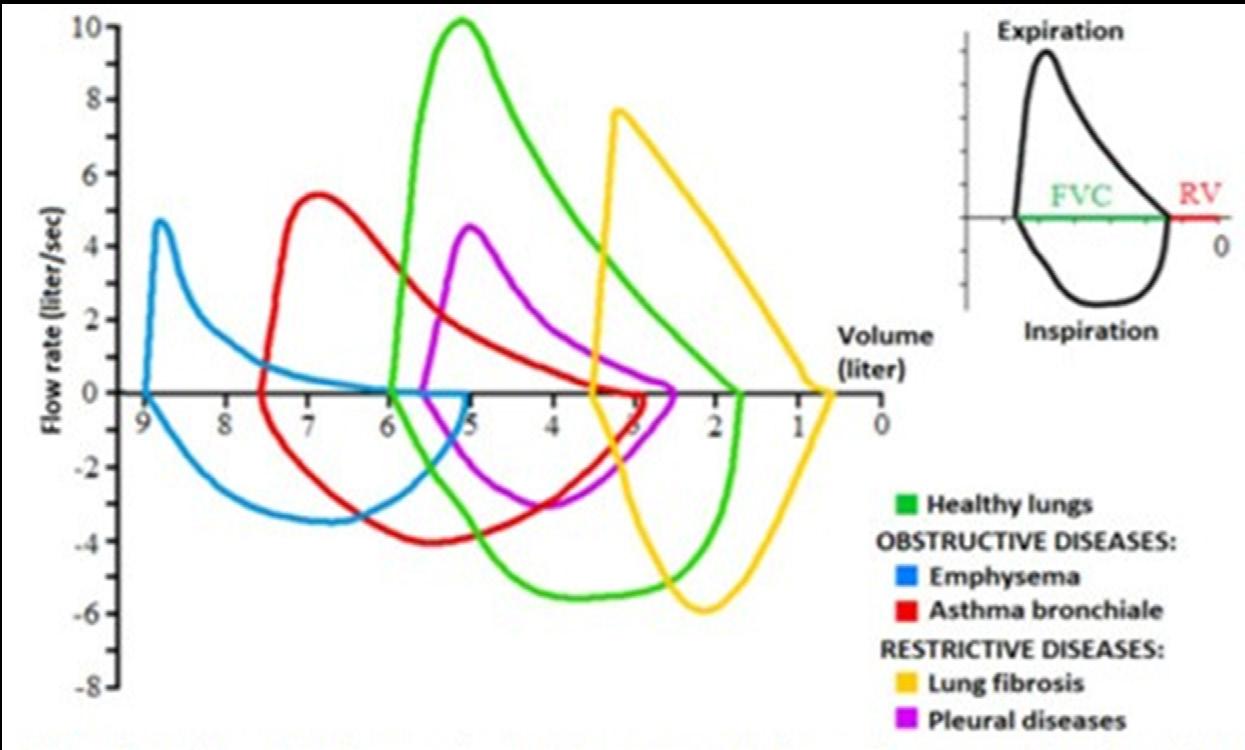
Flow-Volume loop (output of the spirometry) showing FVC manoeuver for healthy and diseased lung.
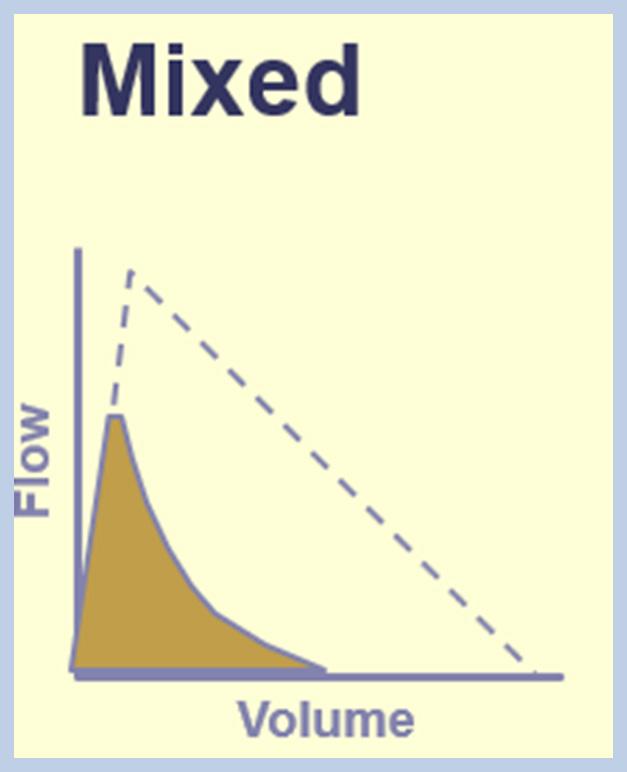
• The mixed Obstructive and Restrictive Spirometry curve is characterised by both airflow obstruction and loss of lung volume.
• This defect is relatively uncommon.
• An example is sarcoidsosis.
Since May 2015, there have been six confirmed cases of coal workers’ pneumoconiosis (CWP), one form of coal mine dust lung disease (CMDLD), reported among former and current Queensland coal mine workers, and the outcome of at least one suspected case is still pending.
• Prolonged Exposure - coal mine dust lung disease, which includes CWP, emphysema, chronic bronchitis, and lung function impairment
These diseases develop gradually, usually after at least 10 years of exposure, however in sensitive miners or in cases of intense exposure symptoms may occur sooner.
• Typical symptoms - cough, sputum production and shortness of breath
• Early Disease may be asymptomatic but still show findings on PFT’s and x- ray. Early detection is the key!
Cases of MDLD reported to RSHQ for all mining since 1984 by financial year (current as at 28 February 2023)
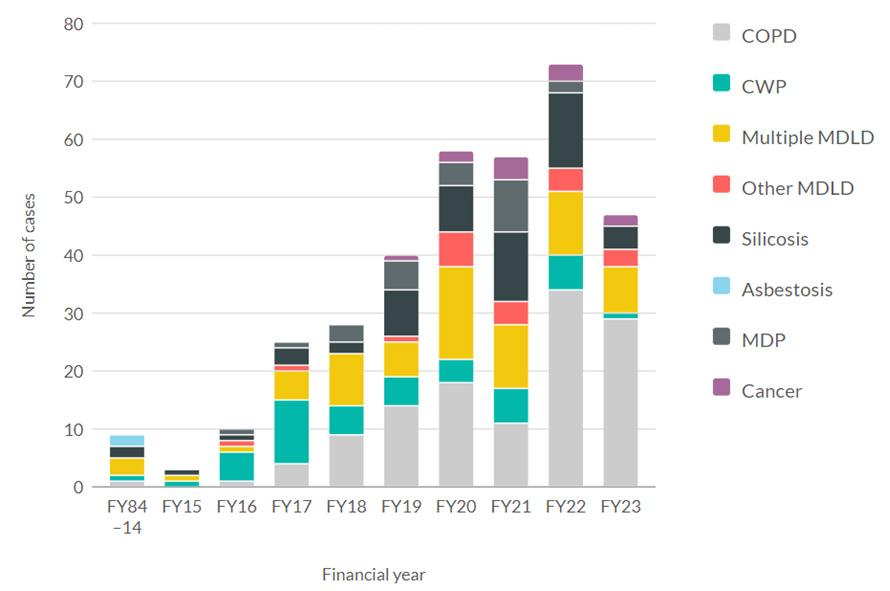
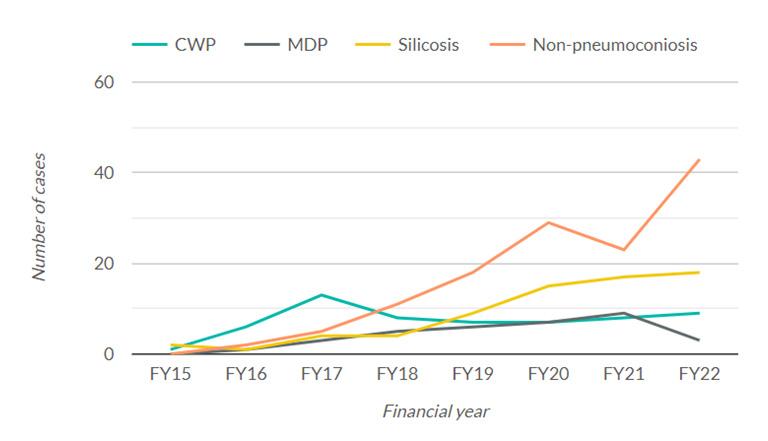
Cases of MDLD reported to RSHQ for all mining since 2014-2015 by financial year and disease type (current as at 28 February 2023)
Cases of pneumoconiosis reported to RSHQ for all mining, since 1984 (current as at 28 February 2023) 177
pneumoconiosis cases
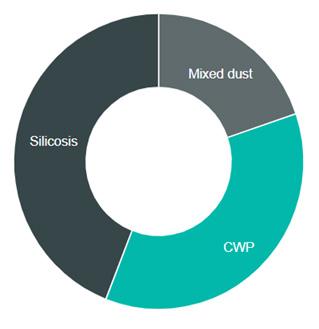
Mine dust can lead to a range of pathological changes in the lungs. In general terms, the resulting lung changes can be divided into two groups; those which are fibrotic or nodular (example CWP, mixed dust pneumoconiosis and silicosis), and those which are non-nodular (example COPD and lung cancer). Due to being nodular in nature, CWP, mixed dust pneumoconiosis, and silicosis can be graded according to a scale of severity under the ILO classification.
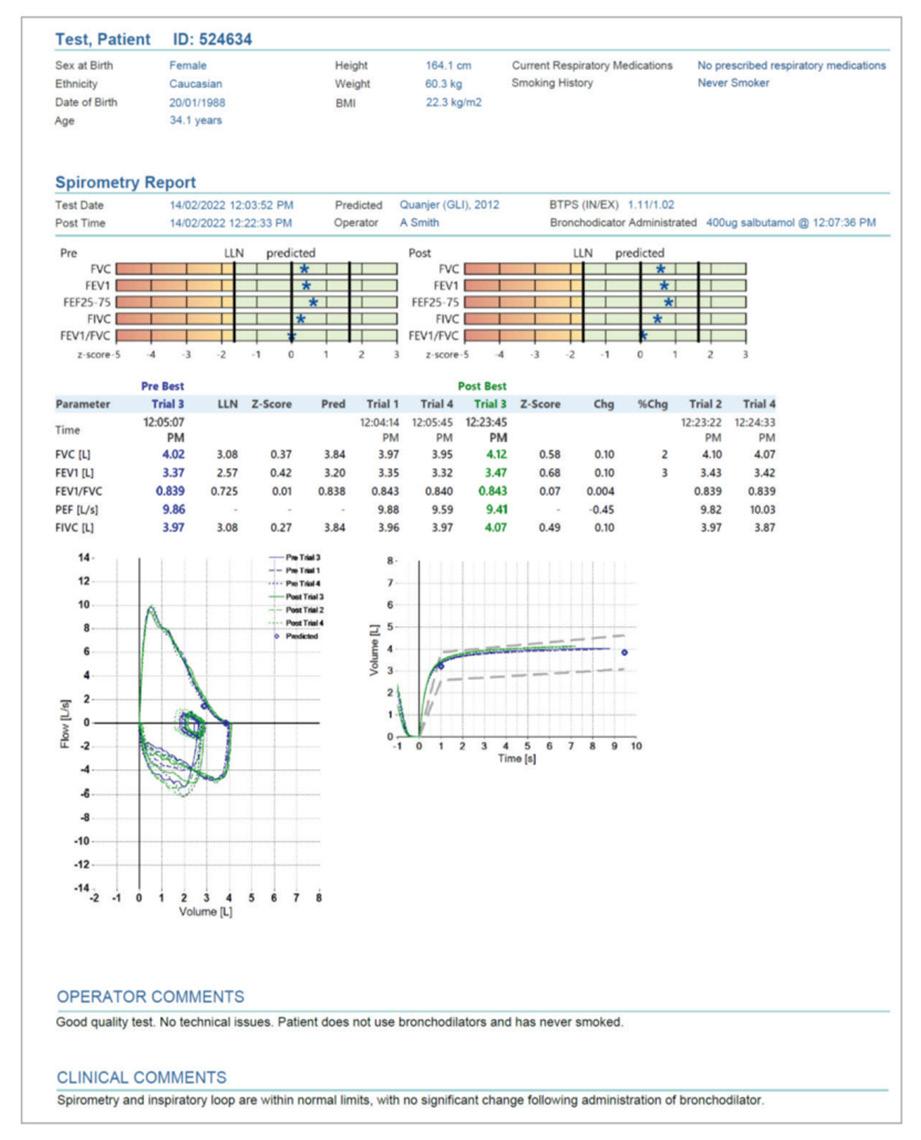
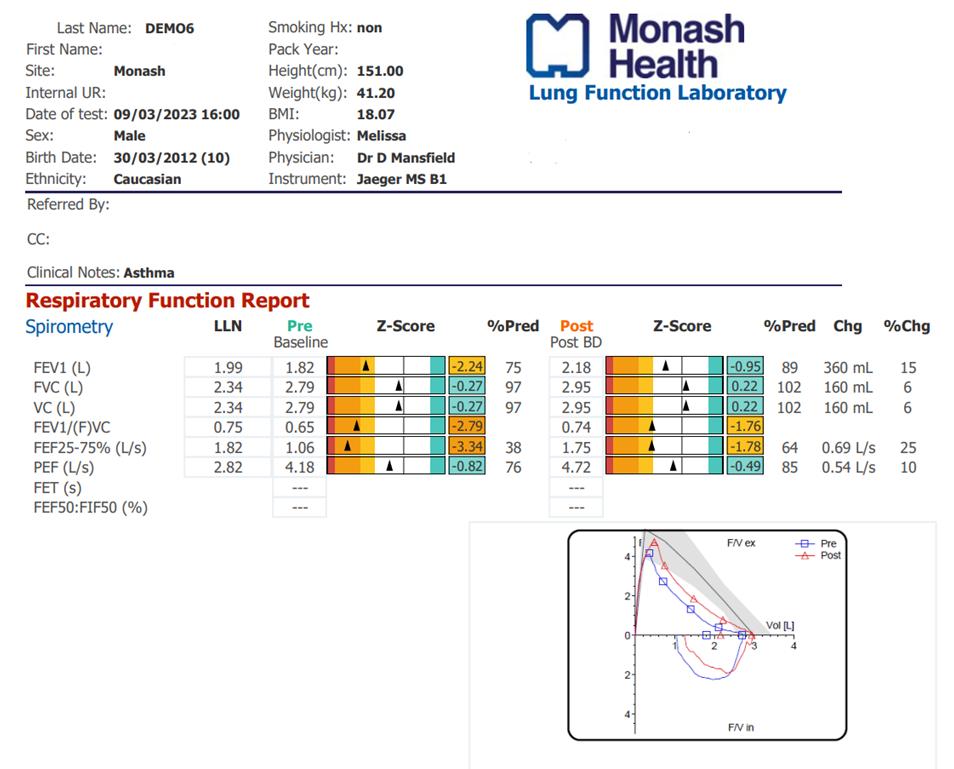
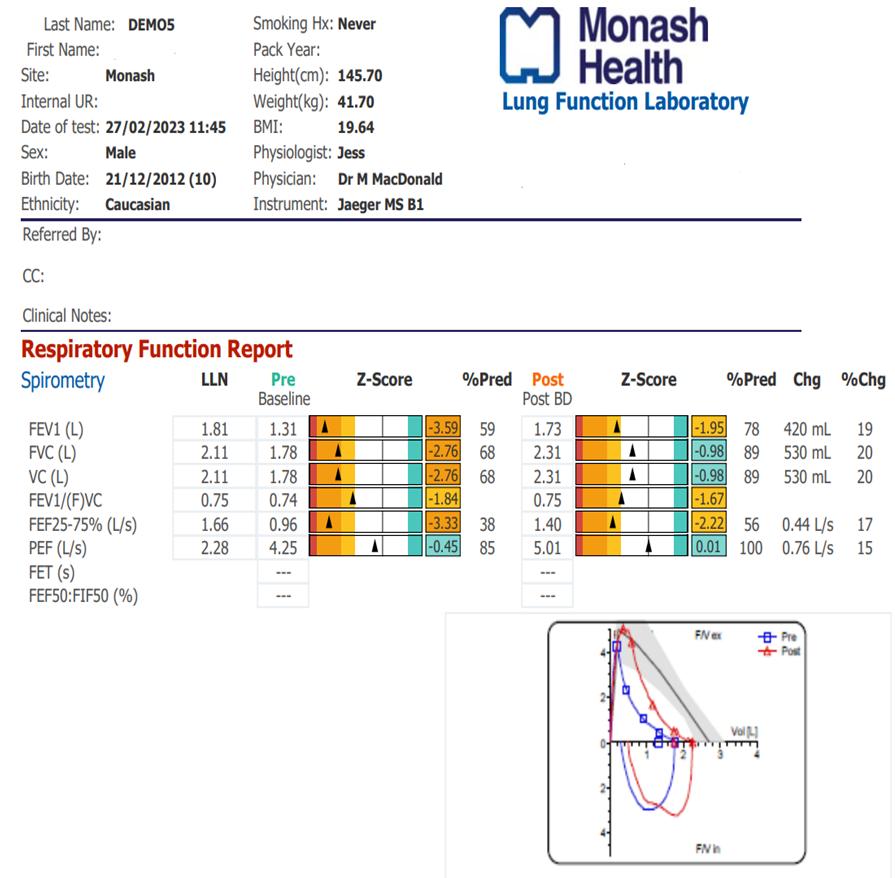
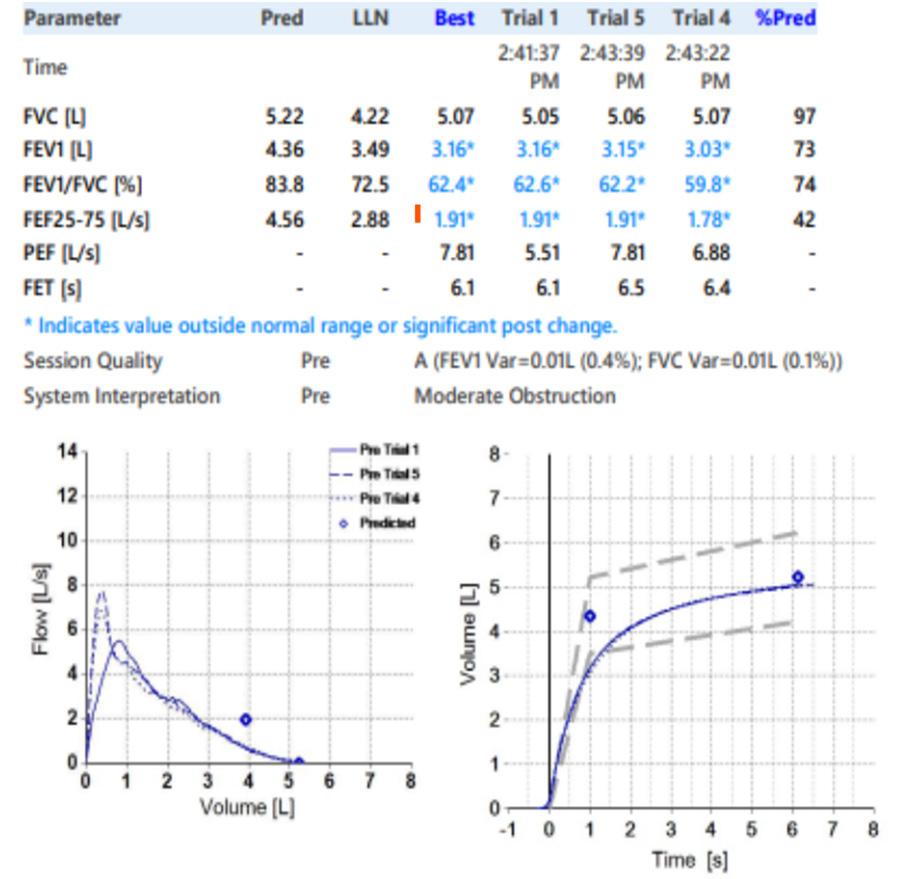
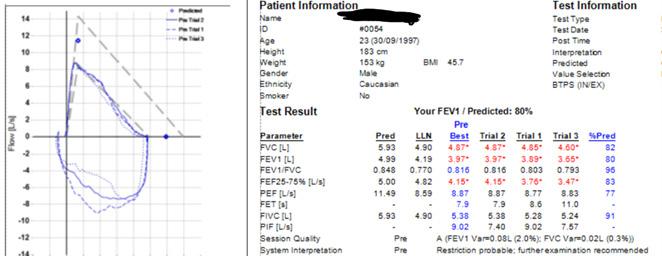
Sample report: Pre and post - bronchodilator spirometry report.
Male, 73-year-old, smoker. Hx of SOB, Chest infections, Cough, x 2 hosp. admissions.
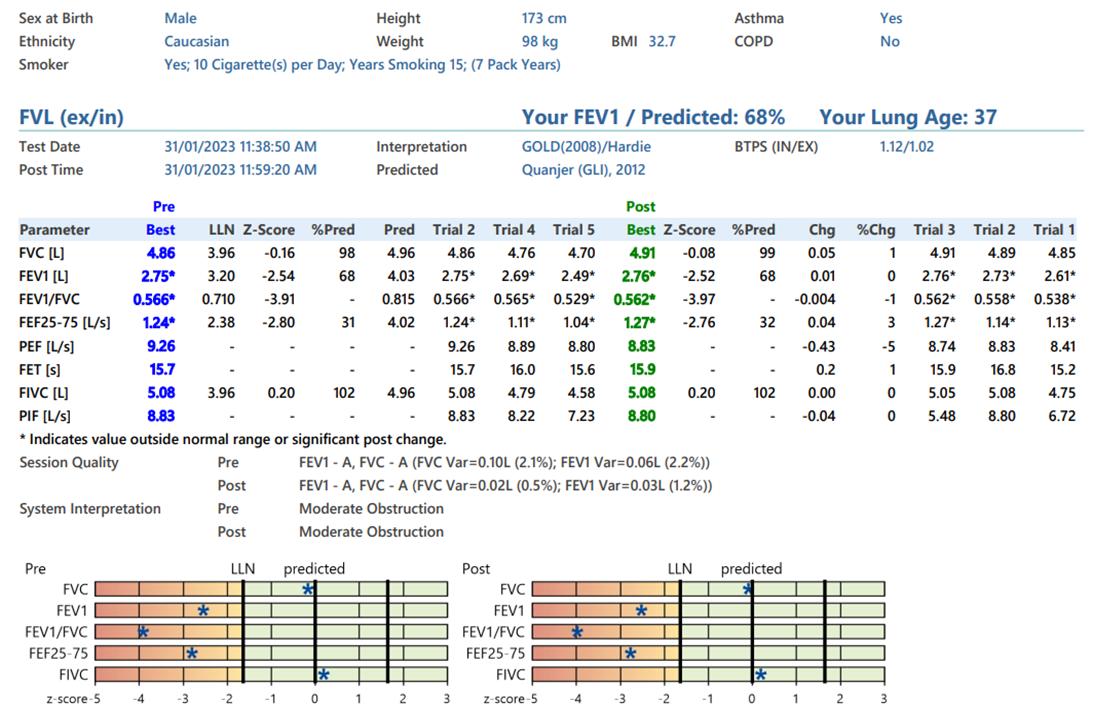
Diagnosis:
Non-smoker, no history of respiratory problems, 5 years of joint aches and morning stiffness, recent chest x ray shows diffuse lung infiltrate, referred for dyspnoea.
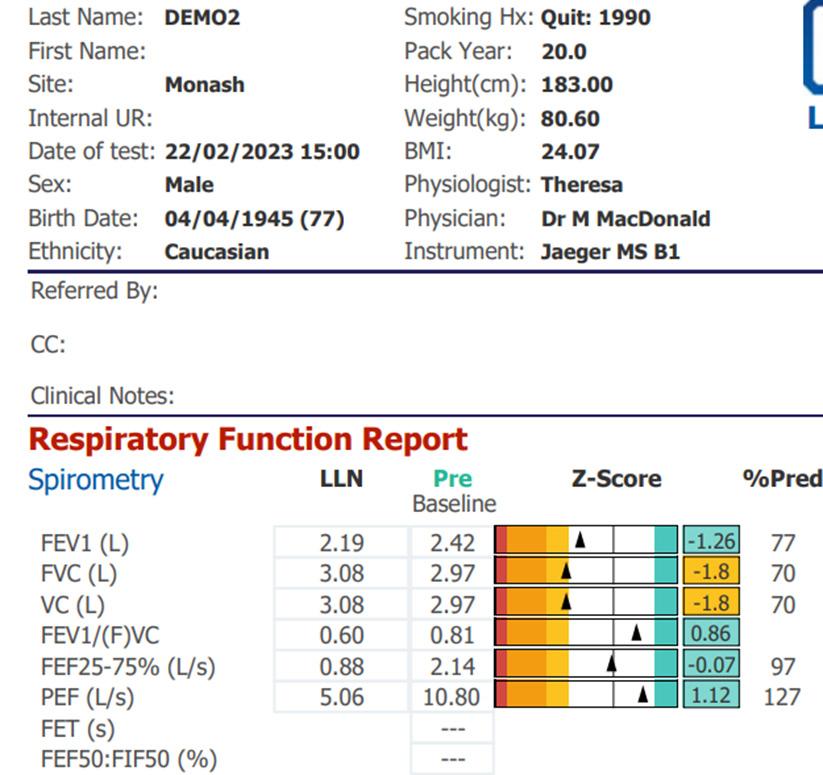
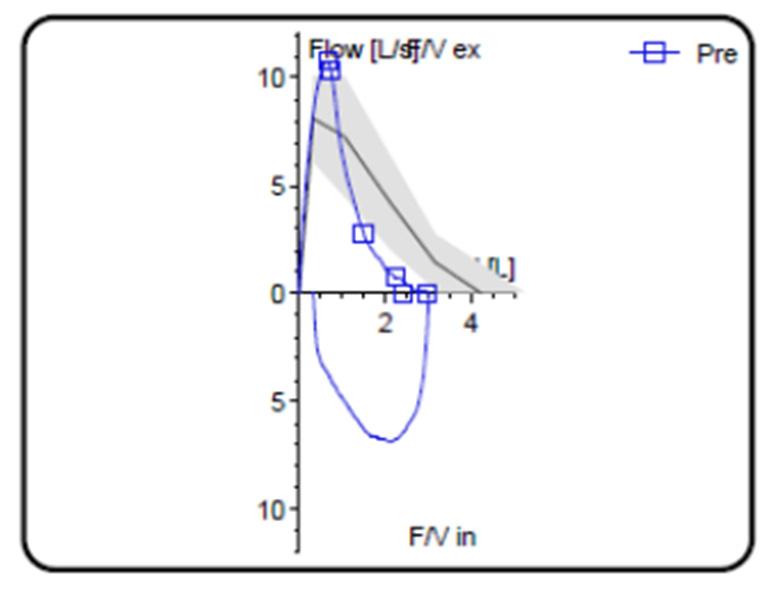
Diagnosis:
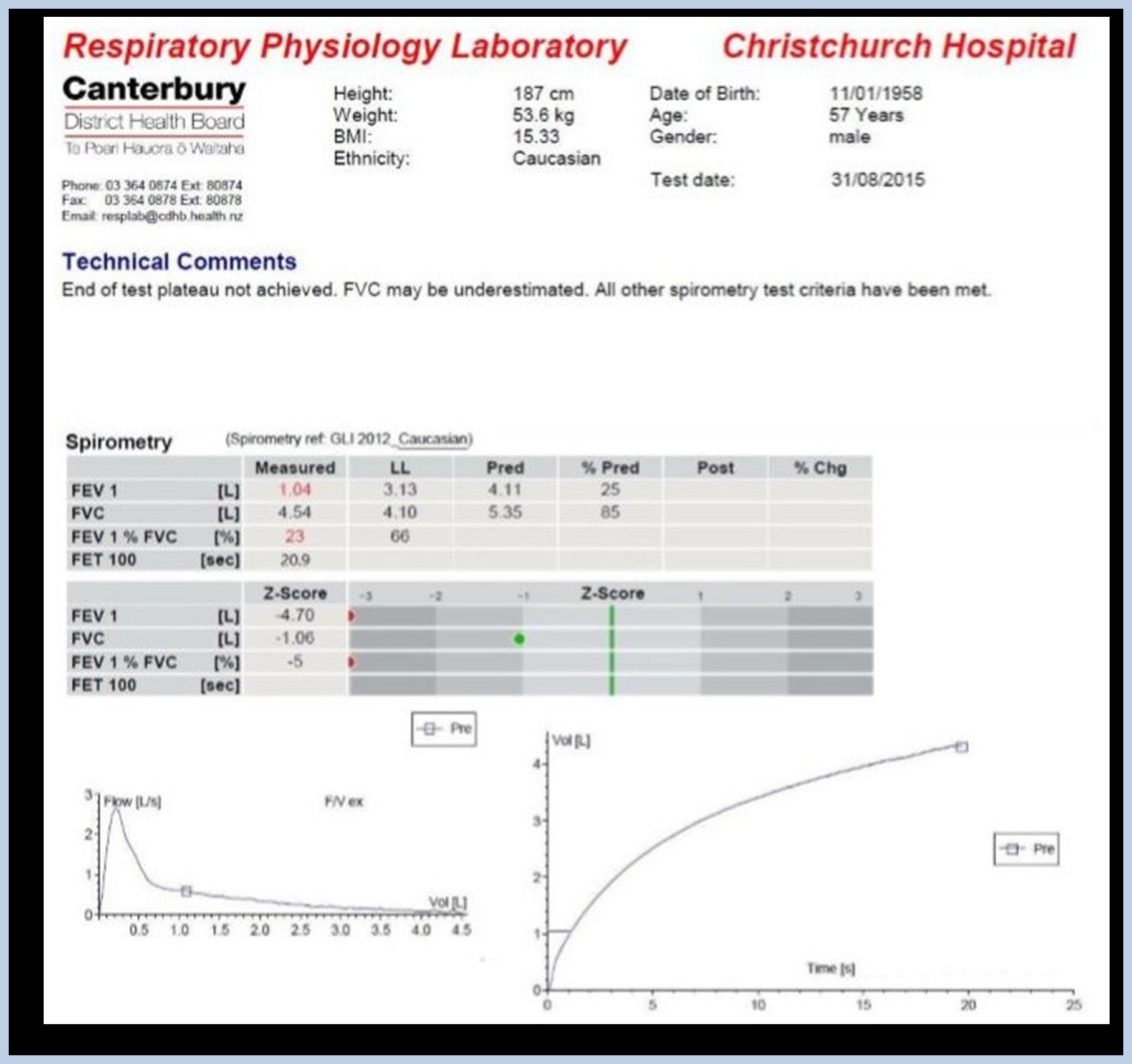
Roger (57 years) has just been released from prison. He is coming to see you because he is short of breath walking up and down the local beach; he wonders if he has lost fitness during his time in prison.
Please list equipment requirements:
How would you ensure that your equipment is functioning properly prior to commencing the test?
What other measures are taken prior to commencing spirometry?
What type of defect is represented in the report?
Can you comment on the technical comments made? Will this make any difference to his result?
Can you classify the disease defect using the algorithm provided?
What other test would have been useful in this case?
Diagnosis:
Question 1: Is this test acceptable?
What errors can you see?
Question 2: Is this test acceptable?
What errors can you see?
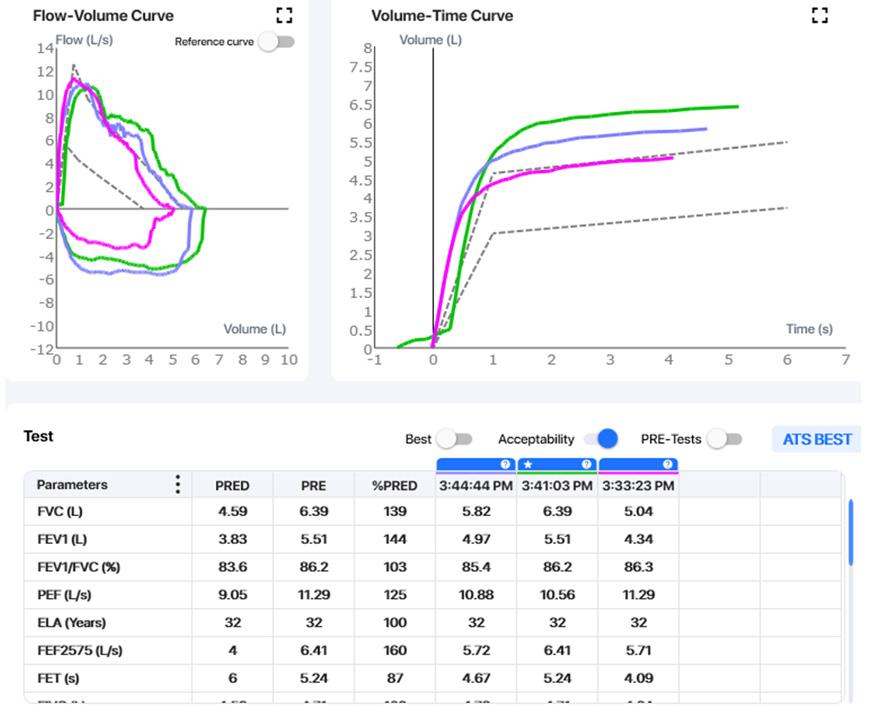
Is this test acceptable?
What errors can you see?
Question 4:
What errors can you see?
What errors can you see?
What errors can you see?
Question 5: Is this test acceptable and reproducible?
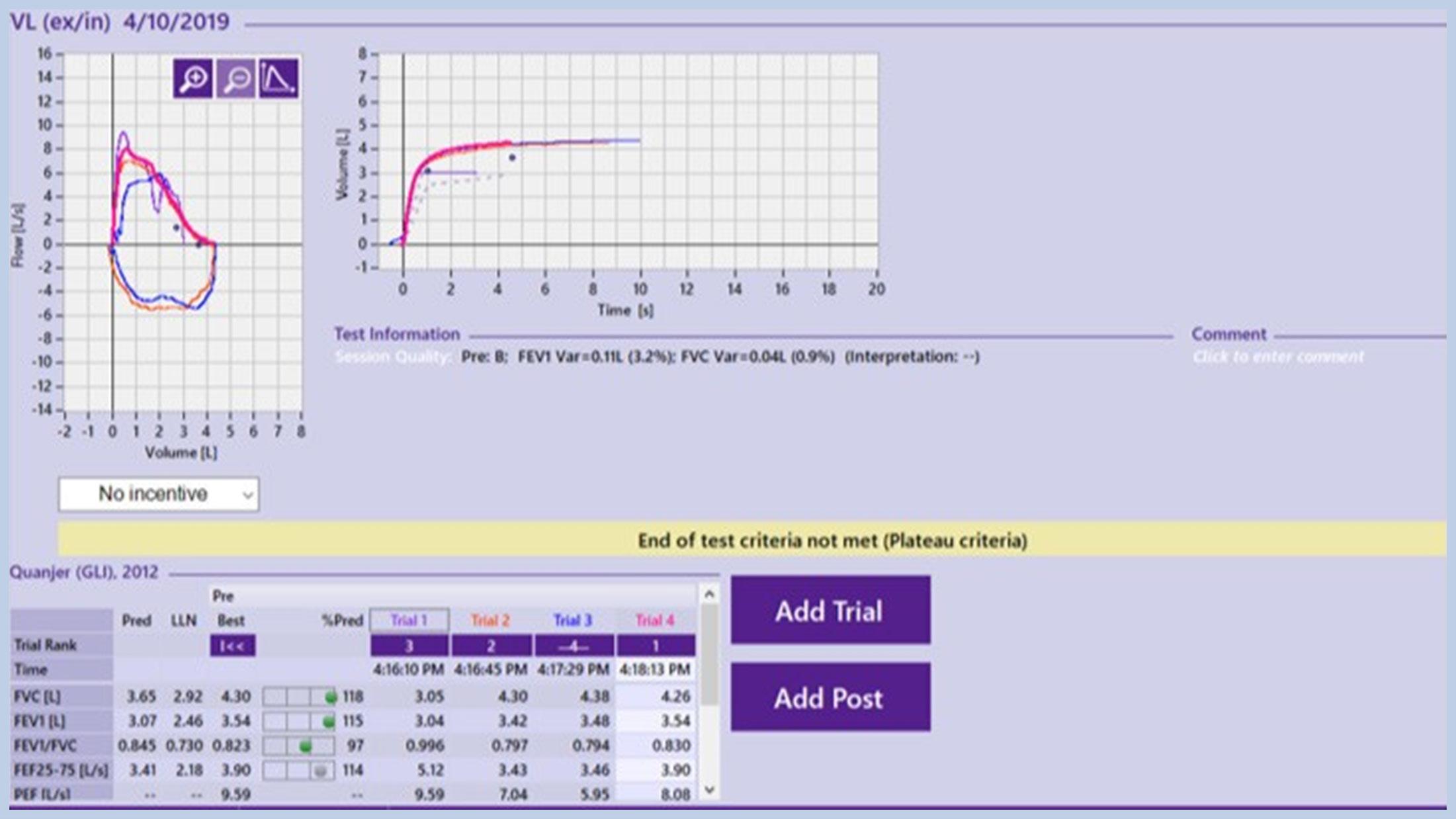
Question 6: Has this person true restriction?
We have uploaded some helpful resources that you can print out and put on your spirometry test room walls. All you’ll need to do is go to https://kb.kinnecttraining. com.au/knowledge-base/spirometry-resources/ or scan the qr code below:
We offer a range of products including spirometers, calibration syringes and filters on our online shop: shop.kinnecttraining.com.au or scan the qr code below:
Choosing the most appropriate reference values for an individual can be difficult. The assignment of ethnicity for an individual can be uncertain, particularly for those of mixed ethnicity. Good data is lacking for many populations and there may be morphologic changes with subsequent generations of an immigrant population. Shown below are the populations for which each of the GLI-2012 equations are known to be representative.
Caucasian
Europe, Israel, Australia, USA, Canada, Mexican Americans, Brazil, Chile, Mexico, Uruguay, Venezuela, Algeria, Tunisia
Black African American
South East Asian
Thailand, Taiwan, and China south of the Huaihe River and Qinling Mountains (including Hong Kong)
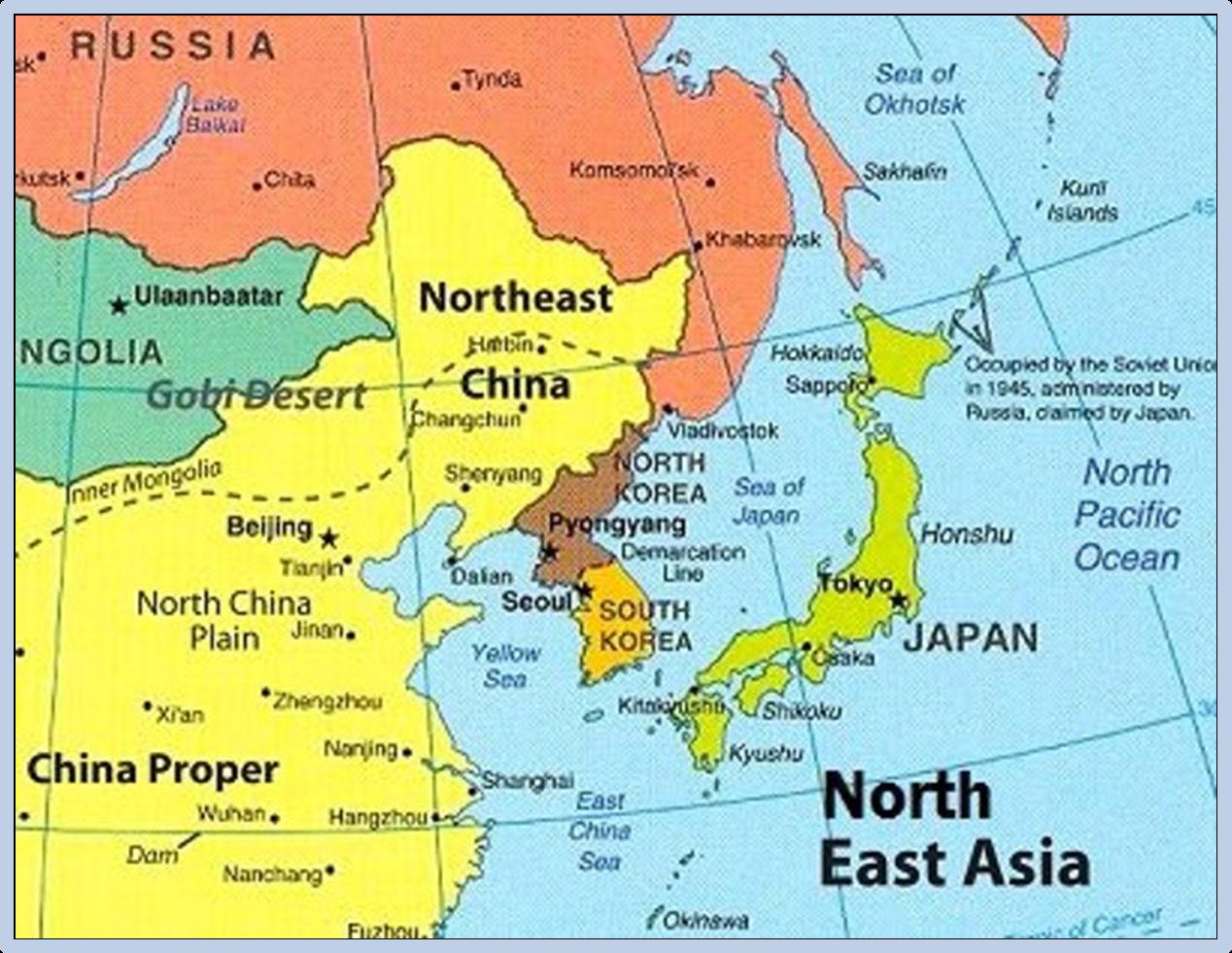
North East Asian Korea and China north of the Huaihe River and Qinling Mountains
In addition to the countries listed, it would be reasonable to apply the group reference equations to others with geographic or ethnic proximity. Thus the Caucasian equations could be used for any person having origins in any of the original peoples of Europe, the Middle East, or North Africa and for any non-indigenous person of South America. Similarly, the Southeast Asian equations may be reasonably extended throughout that region.
However, significant populations remain missing, including Native Americans, Alaska Natives, the Indian sub-continent and Japan. There are many reports of spirometry reference values (and some for other tests) from individual countries or ethnic groups, but the population size and data quality may vary.
For the Japanese, Kubota M, et al Reference values for spirometry, including vital capacity, in Japanese adults calculated with the LMS method and compared with previous values. Respir Investig 2014; 52(4): 242-250).
Within the Indian sub-continent, there appear to be regional differences in spirometry values that cannot be encompassed in the same equations.
GLI-2012 provides a fifth set of equations, “Other”, made up as a combination of the four groups above, which may be applied as a first approximation to individuals not represented by one of the groups or who are of mixed ethnicity. This should be noted in the report and results interpreted with awareness of increased uncertainty.

• Review of respiratory component of the coal mine workers’ health scheme for the queensland
• department of natural resources and mines final report - https://www.dnrm.Qld. Gov.Au/ data/ assets/pdf_file/0009/383940/monash-qcwp-final-report-2016. Pdf
• Tsanz spirometry standards for delivery of spirometry in coal miners. July 2017. - Https://www. dnrme.Qld.Gov.Au/ data/assets/pdf_file/0003/1274421/tsanzspirometry-standards.Pdf
• Spirometer users’ & buyers’ guide - https://www.Nationalasthma.Org.Au/livingwith-asthma/ resources/health-professionals/information-paper/spirometryusers-buyers-guide
• Queensland health guideline – spirometry (adult) respiratory science - https:// www.Health.Qld.Gov. Au/qhpolicy/docs/gdl/qh-gdl-386.Pdf
• Spirometry handbook - https://www.nationalasthma.Org.Au/living-with-asthma/ resources/health- professionals/information-paper/spirometry-handbook
• Global lung initiative - http://www.ers-education.Org/guidelines/global-lungfunction-initiative. Aspx
• Gli advantages and consequences - https://www.Ers-education.Org/media/ media. Aspx?Idmedia=266696
• Easy on –pc operators manual https://cdn.Shopify.Com/s/files/1/1046/1086/ files/ndd-medical- easy-on-pc-spirometry-operators-manual.Pdf
• Queensland coal mining industry slammed in black lung review - Http://www. Abc.Net.Au/news/2016-07-12/queensland-coal-mining-industry-slammed-inblack-lung-review/7589918
• Standardisation of spirometry. 2005 - https://erj.Ersjournals.Com/content/ erj/26/2/319.Full.Pdf
• Standardisation of spirometry. 2019 Update - https://www.Atsjournals.Org/doi/ pdf/10.1164/ Rccm.201908-1590St
• An update to contraindications for lung function testing - https://thorax.Bmj. Com/content/ thoraxjnl/66/8/714.Full.Pdf
• TSANZ spirometry standards for delivery of resource sector workers. April 2022
• Stanojevic S, Kaminsky DA, Miller M, Thompson B, Aliverti A, Barjaktarevic I, et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur Respir J. 2021 Dec 23:2101499. doi: 10.1183/13993003.01499-2021
Irish Association of Respiratory Scientists (AIRS). Spirometry for healthcare professionals. 2016 Spirometry training course. National Asthma Council Australia 2008
Useful websites
https://spirxpert.ers-education.org/en/spirometry/welcome-to-spirxpert http:// www.pftforum.com/
www.kinnecttraining.com.au