Rehabilitation & Return to Work Coordinator Course - QLD
Learner Guide

In completing this course you will learn how to assist with rehabilitation and return to work.

Rehabilitation & Return to Work Coordinator Course - QLD
Learner Guide

In completing this course you will learn how to assist with rehabilitation and return to work.
Injuries in the workplace can be costly and time consuming. The Rehabilitation and Return to Work Coordinator (RRTWC) is an important part in minimising the effect on injured workers and employers and there is some key knowledge and skills that will help a RRTWC achieve great outcomes.
This training includes an introductory understanding and application of relevant legislation and procedures to ensure compliance in workers’ compensation and injury management processes. The course focuses on the early return to work principles, effective engagement of rehabilitation providers, development of suitable duties programs, effective workplace communication, case and system review techniques and continuous improvement.
Theoretical and practical scenarios are discussed in the course, building the prospective RRTWC’s confidence in the process of managing claims, communicating effectively with relevant stakeholders, identifying suitable duties in the workplace, and effectively assisting the injured worker’s rehabilitation needs and graduated return to work.

In Australia, there are 11 main workers’ compensation systems and each of the eight Australian States and Territories has developed their own workers’ compensation laws.
Below is a summary of the evolution of workers’ compensation in Australia.
Late 1800’s
• Originated from British Law.
• Injured workers had to sue employer for negligence – rarely successful.
1901 - After Federation
• New laws incorporated “no fault” principle.
• Only had to prove injury was work related to be eligible, not negligence of Employer.
• Insurance policy not compulsory for Employers.
1920 - 1970s
• Continued to evolve, eligibility broadened.
• As early as 1926 – NSW compulsory insurance.
• Workmen’s Compensation - Only covered male workers, until 1970s women’s movement.
1980’s
• More benefits for injured workers.
1990’s
• Focus shifted to reducing costs of injuries & premiums and administration efficiency.
2000’s
• Focus on Health & Safety, prevention of injuries, rehabilitation of injured workers and reducing costs.
Currently there are 11 main workers’ compensation systems in Australia. Each of the eight Australian states and territories has developed their own workers’ compensation scheme and there are also three Commonwealth schemes, as follows:
1) Australian Government employees and the employees of licensed self-insurers under the Safety, Rehabilitation and Compensation Act 1988 (SRC Act), and Australian Defence Force personnel with service prior to 1 July 2004 under the Safety, Rehabilitation and Compensation (Defence-related Claims) Act 1988 (DRCA).
2) Seafarers under the Seafarers Rehabilitation and Compensation Act 1992.
3) Australian Defence Force personnel for service on or after 1 July 2004 under the Military Rehabilitation and Compensation Act 2004 (MRCA).
[1]Safe Work Australia
Workers’ compensation legislation in all jurisdictions makes it compulsory for employers to take out workers’ compensation insurance.
WorkCover is the largest insurer in Queensland, however there are 28 self-insured employers that manage workers’ compensation claims in Queensland. Self-insured employers apply for a licence through the Workers’ Compensation Regulator.
Insurance, by definition, is a way of spreading risk. Insurance companies calculate a premium based upon the likelihood that there will be a claim.
Both WorkCover and Self-Insured Employers are approved by the Queensland Workers’ Compensation Regulator to manage employers’ Workers’ Compensation insurance policies and injured workers’ compensation claims in Queensland. They also support return to work programs.
WorkCover Queensland calculate their wage payout premiums in two categories:
1) Simplified rate : This is for wages less than $1.5 million. It is calculated by multiplying the workers wage by the industry rate. They then get a rating of 1 - 5 which determines if their policy is multiplied by 80% to 120% of the industry rate. This is determined by previous claims costs.
2) Experience based rate : This is for wages more than $1.5 million. They use wages, industry rate and performance to calculate it. The performance is calculated using the last three years of statutory claims costs and the fourth year is the common law costs. The formula for this is in the Queensland Government Gazette.
In Queensland, it is mandatory to have a Workers’ Compensation Policy with WorkCover Queensland if you employ staff, however sometimes legislation permits large employers to self-insure, rather than take out insurance directly through WorkCover Queensland.
A self-insured organisation needs:
• At least 2000 Queensland full-time workers
• A satisfactory OHS standard
• An unconditional bank guarantee
• A reinsurance cover
• To be deemed fit and proper to be a self-insurer
More details: https://www.worksafe.qld.gov.au/claims-and-insurance/self-insurance
Each State and Territory has its own Workers Compensation Legislation and Regulatory body that administers the legislation.
QLD WorkCover Queensland or Self Insurers
NSW iCare NSW uses Private Agents:
• EML is the default scheme however Allianz, GIO and QBE can be used or Self Insurers
VIC WorkSafe Victoria uses Private Insurers (4):
• Allianz, EML, Gallagher Bassett, XChanging
SA Return to Work SA uses Private Insurers (2):
• EML, Gallagher Bassett or Self Insurers
TAS WorkSafe Tasmania uses Private Insurers (7):
• Allianz, Zurich, GIO, CGU, QBE, Guild Ins, Catholic Church Ins
ACT WorkSafe ACT uses private insurers (7):
• Allianz, GIO, CGU, Guild Ins, Catholic Church Ins, QBE, Zurich or Self Insurers
WA WorkCover WA uses Private Insurers (8):
• Allianz, Zurich, QBE, AAI, Catholic Church Ins, Guild Ins, CGU, WFI or Self Insurers
NT NT WorkSafe uses Private Insurers (5):
• Allianz, GIO, CGU, QBE, TIO or Self Insurers
Office of Industrial RelationsWorkers’ Compensation Regulatory Services
SIRA – State Insurance Regulatory Agency
WorkSafe Victoria, Victorian WorkCover Authority
Return to Work SA or Supreme Court
Workers’ Rehabilitation & Compensation Tribunal / Supreme Court
WorkSafe ACT Conciliation / Arbitration Services
WorkCover WA, Conciliation / Arbitration Services
Work Health Court / Supreme Court
C’wealth
• Comcare (for Australian Defence Forces & Federal Govt)
• Seacare Authority (Seafarers Safety, Rehabilitation and Compensation Authority
• Self Insurers
Comcare & Safety, Rehabilitation and Compensation Commission
There are also specific Acts and regulatory bodies for Commonwealth employees and military forces personnel which will not be covered in this course.
Each of these regulatory bodies has a website where you can seek information regarding the legislation they administer, and locate advice and information on managing workers compensation, rehabilitation and return to work programs in their situation.
You can download the publication Key Workers’ Compensation Information, Australia from the Safe Work Australia website.
The legislation that governs compliance varies between each State or Territory. The below table outlines the legislation that is relevant to each state.
QLD
NSW
VIC
SA
TAS
ACT
WA
NT
C’wealth
• The Workers’ Compensation & Rehabilitation Act 2003
• The Workers’ Compensation & Rehabilitation Regulation 2014
• Workplace Injury Management & Workers Compensation Act 1998 Workers Compensation Act 1987
• Workplace Injury Rehabilitation & Compensation Act 2013
• Return to Work Act 2014
• Return to Work Corporation of South Australia Act 1994
• South Australian Employment Tribunal Act 2014
• Workers Rehabilitation & Compensation Act 1988
• Workers Compensation Act 1951
• Workers’ Compensation & Injury Management Act 1981
• Return to Work Act 1986
• Safety, Rehabilitation & Compensation Act 1988
• Seafarers Rehabilitation & Compensation Act 1992
• Military, Rehabilitation & Compensation Act 2004
Note!
At certain points in the course from here you will be asked to review components of the relevant Act and Regulation for Queensland to help you further understand the expectations for workplace rehabilitation.
You may be asked to refer to key points from sections of the legislation at various times throughout the program.
Employers have an obligation to appoint a Queensland-based Rehabilitation and Return to Work Coordinator if they meet the necessary criteria. The RRTWC plays a pivotal role in supporting a workers’ successful return to the workplace.
Employer’s obligation to appoint Rehabilitation & Return to Work Coordinator
Workers’ Compensation and Rehabilitation Act 2003
Section 226 Employer’s obligation to appoint rehabilitation and return to work coordinator
Workers’ Compensation and Rehabilitation Regulation 2014
Section 115 Criteria for employer to appoint rehabilitation and return to work coordinator—Act, s 226(1)
Workplace Health and Safety Queensland has listed industries deemed to be high risk on:
• https://www.worksafe.qld.gov.au/laws-and-compliance/workers-compensation-laws/guidancematerials/high-risk-industries
This includes industries within agriculture forestry and fishing, mining, manufacturing, construction, transport and storage, health and community services and miscellaneous.
QOTE (Quote-ee) stands for Queensland Ordinary Time Earnings. This changes every 1st of July and is issued in the Queensland Government Gazette. QOTE is an average weekly figure for all Queensland adult full-time workers. QOTE is also used in the determination of calculating an injured worker’s weekly compensation rate of pay whilst they are off work. QOTE figures are published on WorkSafe.qld.gov.au
What is the current rate of Queensland Ordinary Time Earnings (QOTE)?
• NSW – A person who can undertake the role
• SA – Compulsory
• Qld – appropriately qualified*
• VIC – competent (and have appropriate seniority)
• WA – no specific reference.
*Employers are responsible for ensuring that their appointed RRTWC is appropriately qualified to perform the functions of a RRTWC. They can make this assessment by taking a person’s skills, training and experience into consideration. Attending a RRTWC course approved by the Workers’ Compensation Regulator is just one option employers have to ensure that their RRTWC is appropriately qualified.
A Rehabilitation and Return to Work Coordinator works within an evolving framework with changes to legislation and return to work best practices. It is therefore important that all RRTWC’s maintain their contemporary skills and knowledge by undertaking ongoing learning and development and continued professional practice opportunities.
The Workers’ Compensation Regulatory Services provides avenues for professional development with regular evidence-based updates provided through:
• Rehabilitation and Return to Work e-bulletin
○ https://www.worksafe.qld.gov.au/news-and-events/newsletters/rehabilitation-and-return-towork
• Return to Work Queensland Facebook page
○ https://www.facebook.com/RTWQld
If an employer is found to be bound by the above-mentioned Section 226 of the Act, then they are also obligated to have workplace rehabilitation policy and procedures in place. These must be reviewed every 3 years.
Where an employer is required to appoint an RRTWC, they must also provide details of the RRTWC to their insurer, including a statement as to how their appointed RRTWC is appropriately qualified to perform the role. Employers are required to notify the insurer anytime their appointed RRTWC changes.
• The Workers’ Compensation Regulator can approve training courses for RRTWC’s, although attending an approved training course will not be mandatory or the only way to achieve appropriate RRTWC qualifications. It is simply an option for an employer to demonstrate that their RRTWC is appropriately qualified.
• Employers will be required to provide the details of all appointed coordinators within 12 months of 1 July 2020 to their insurer.
Workers’ Compensation and Rehabilitation Act 2003
Section 41 Meaning of rehabilitation and return to work coordinator
Employer’s obligation to assist or provide rehabilitation
Workers’ Compensation and Rehabilitation Act 2003
Section 228 Employer’s obligation to assist or provide rehabilitation
The intention of this section of the Act is to ensure employers not only actively engage in assisting the rehabilitation and recovery process but also find meaningful duties for a worker to do whilst on a suitable duties program. This aids workers by helping to maintain their psychological well-being as well as their physical recovery.
As you will see throughout this course there are a number of stakeholders in the return to work process and all have important roles in ensuring rehabilitation at work is successful. The stakeholders include:
• The Workers’ Compensation Regulator : Maintain a fair and efficient workers’ compensation scheme that balances the needs of workers and employers.
• Insurers : To effectively manage the rehabilitation and return to work of injured workers.
• Employers : Assist with managing a workers’ injury and the return to work.
• Injured Workers : Contribute to their recovery by participating in the return to work processes.
• Medical & Rehabilitation Service Providers : To contribute with best practice evidence based treatment services to assist in the best possible return to work outcomes.
• The Rehabilitation and Return to Work Coordinator (RRTWC) : To assist with the rehabilitation and return to work of the injured worker.
Further details and obligations of these stakeholders is outlined in this booklet.
The Worker’s Compensation Regulatory Services consists of teams specialising in engagement and insurer services, data and evaluation, Medical Assessment Tribunals, reviews and appeals and policy services.
[2] Workers’ Compensation Regulatory Services
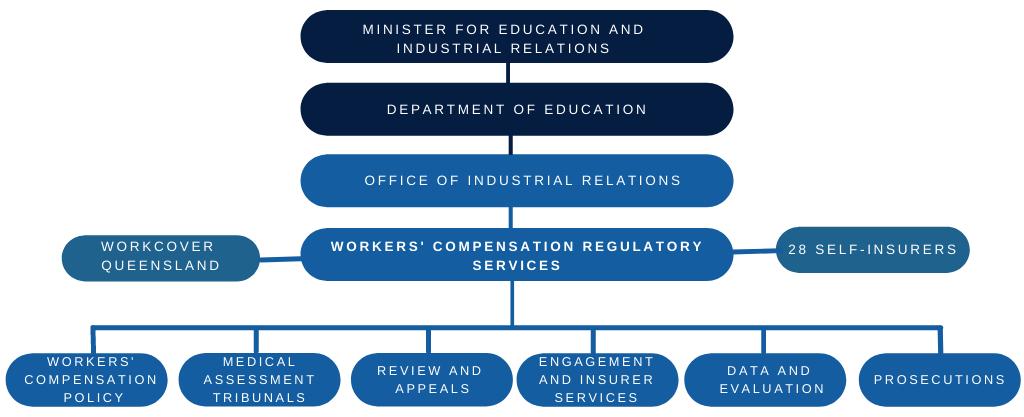
The Office of Industrial Relations (OIR) incorporates several Regulators and they are:
• Workplace Health and Safety Queensland
• Electrical Safety Office
• Workers’ Compensation Regulatory Services (WCRS).
The OIR and WorkCover Queensland both report to Queensland’s Minister for Industrial Relations. These relationships are demonstrated in the below diagram.
The OIR offers educational and online services for industry professionals. A range of free safety and return to work education events are regularly published on: www.worksafe.qld.gov.au

Workers’ Compensation Regulatory Services (WCRS) regulates the Queensland workers’ compensation scheme by undertaking the functions of the Workers’ Compensation Regulator in accordance with S327 of the Workers’ Compensation and Rehabilitation Act 2003 (the Act).
WCRS seeks to promote an equitable and efficient compensation scheme that balances the needs of all scheme stakeholders including workers, employers, insurers, medical and legal representatives.
WCRS works with insurers, employers, workers and health professionals to make sure all workers who’ve experienced a work-related injury are supported throughout their rehabilitation journey and can safely return to work.
WCRS operates independently to:
• Manage insurers’ licences and make sure they follow workers’ compensation laws
• Settle disputes and complaints about workers’ compensation decisions made by insurers
• Take legal action when workers’ compensation laws are broken
• Facilitate medical assessment tribunals
• Promote rehabilitation and return to work
• Give training to medical practitioners
• Gather and analyse data about the workers’ compensation scheme.
WorkCover Queensland and the Self-Insured Employers must abide by the Workers’ Compensation & Rehabilitation Act & Regulation. Their role ensures they:
• Assess and decide on claims for compensation
• Make payments in accordance with the Act, and Regulation and determine ongoing benefits for financial entitlements for accepted claims
• Support workers to return to work as part of their rehabilitation
• Coordinate the development and maintenance of a rehabilitation and return to work plan in consultation with all parties
• Be involved, if necessary, in undertaking an advisory role to assist the employer with their rehabilitation and return to work obligations
• Liaise with all parties to monitor the progress of the worker
• Provide treatment, hospitalisation and pay expenses as per section 144B of the Act.
WorkCover Queensland encourages compliance with the relevant legislation through online wage audits, employer site visits, education and awareness campaigns and identification of under-insured and un-insured employers.
Insurers rights & responsibility for workers’ rehabilitation is predominantly outlined in the following section of the Act.
Workers’ Compensation and Rehabilitation Act 2003
Section 220 Insurer’s responsibility for rehabilitation and return to work
Employers have obligations, rights, and responsibilities under the legislation. It is important employers plan for the worst, and have policies and procedures in place for immediate injury management if an unfortunate event happens.
Employers must document policies and procedures outlining the system to manage workers who suffer a work-related injury or illness if the employer meets the necessary criteria.
This document is known as the Workplace Rehabilitation Policy and Procedures for the management of an injured worker. It forms part of the Workplace Health Safety and Environment (WHSE) Management System.
In contrast, a Suitable Duties Program is developed specifically for an individual injured worker.
This document contains policies or procedures for:
• Identifying the individual rehabilitation and return to work goals of the injured worker
• Processes to ensure that the worker is engaged in the return to work process
• Strategies to ensure that the workplace respond to individual needs of the worker
• Preventing workplace injuries and illness
• Stakeholders roles and responsibilities at the workplace
• Requirements for consulting with workers and unions, if relevant
• Providing suitable duties to enable early return to work
• Ensuring that return to work does not disadvantage injured workers
• How the Suitable Duties Program (SDP) will be developed and implemented
• Training strategies for all workers on the SDP
• Provisions for vocational retraining or job placement assistance if return to pre-injury job role is not successful.
The general definition of a worker aligns with the Australian Taxation Office (ATO) definition in most instances. This means that PAYG workers are generally considered as workers (the definition can be complex and some exceptions do apply).
The definition of ‘worker’ is found in Section 11 of the Act. It covers not only full-time workers on a wage or salary but also those who are:
• Part-time / casual or seasonal workers
• Volunteers - if there is a specific type of agreement in place.
• Workers on commission / piece workers / paid or unpaid interns
• Some working directors - however in Queensland, Directors are not covered unless the employer pays extra / other states working directors are covered
• Certain contract workers.
Workers’ Compensation and Rehabilitation Act 2003
Section 11 Who is a worker
Further information and a Worker determination test is available at:
• https://www.worksafe.qld.gov.au/claims-and-insurance/workcover-insurance/who-should-i-cover/ worker-determination-tests
Workers have a responsibility to:
• Report the injury or illness and get treatment as soon as possible
• Obtain work capacity medical certificates
• Lodge a claim through the employer’s insurer if they wish to lodge a claim for compensation, the worker also -
○ Has the option of lodging a ‘report only’ claim with the insurer
• Be actively involved in their treatment and rehabilitation, including attending all medical or rehabilitation appointments
• Participate in suitable duties within restrictions set by their doctor until they can resume normal duties
• Not provide false or misleading information
• Advise the insurer when they have returned to work - even if just volunteering.
Workers have a right to:
• Make a claim for compensation
• Choose their own treating doctors
• Have all personal information kept confidential
• Have a representative, interpreter or advocate for any meeting to talk about their claim
• Be consulted about their rehabilitation and get a copy of their return to work and suitable duties programs
• Seek advice before signing anything
• Have most insurer’s decisions reviewed
• Access Damages via Common Law in some circumstances.
Injured Workers cannot be dismissed for making a workers’ compensation claim, nor can they be dismissed within 12 months of having an injury solely or mainly because they are unfit for employment because of the injury.
The Rehabilitation and Return to Work Coordinator (RRTWC) can have a positive and lasting impact on business productivity, cost reduction, risk mitigation, workers’ moral, safety, and the holistic health of the workers in the business, which extends to family, friends and the community.
The RRTWC is vital because they:
• Are the communication link between all stakeholders involved in the return to work process
• Are a point of contact to the injured worker for reliable information and guidance
• Ensure the injured worker is supported in an early return to work for best recovery of injury
• Ensure that a worker’s return to work planning aligns with the activities outlined throughout the claims process and all medical information available.
Workers’ Compensation and Rehabilitation Regulation 2014
For section 41(b) of the Act, the following functions are prescribed—
(a) initiate early communication with an injured worker in order to clarify the nature and severity of the worker’s injury;
(b) provide overall coordination of the worker’s return to work;
(c) if a rehabilitation and return to work plan is developed under section 220(5) of the Act—
(i) consult with the worker and the worker’s employer to develop the suitable duties program component of the plan; and
(ii) ensure the program is consistent with the current medical certificate or report for the worker’s injury;
(d) liaise with—
(i) any person engaged by the employer to help in the worker’s rehabilitation and return to work; and
(ii) the insurer about the worker’s progress and indicate, as early as possible, if there is a need for the insurer to assist or intervene.
The rehabilitation and return to work coordinator (RRTWC) is responsible for ensuring that they identify and understand the worker’s individual recovery needs and that suitable duties and workplace accommodations are made to align with these needs where possible.
Contacting the injured worker as soon as possible after injury to find out how they are and what the doctor has recommended.
Being a point of contact for the injured worker at all times, especially if they are not sure what is happening with the process, Insurer decisions or medical treatment.
Helping the injured worker keep in touch with their workplace for socialisation and psychological reasons, or assisting with the transitioning to suitable work options until the worker is fit to return to their pre-injury role.
Explaining the workers’ compensation process and helping the injured worker make a claim with the insurer.
If the injured worker has already made a claim themselves the RRTWC should discuss the workplace expectations and process of return to work. Consider providing the worker with relevant information they can refer to that explains the process such as the workplace rehabilitation policy and procedures so they are adequately informed at the commencement of the process.
Advocating for the injured worker, liaising with treating doctors & specialists or treatment providers eg. Occupational Therapist (OT), Hand Therapist, Physiotherapist etc, to discuss safe return to work options that will benefit their recovery.
Making sure appointments are coordinated so there is a smooth transition throughout the whole process and reduce any waiting times which can cause distress to a worker when they are attempting to return to work and are receiving entitlements.
Overall, this means the injured worker will receive the highest quality care for their injury thus allowing for the best chance of a successful recovery outcome.
Ensuring an appropriate Suitable Duties Program is devised and implemented to assist for a safe return to work.
Collaborate with supervisors and managers to promote open communication and engagement throughout the return to work planning process.
The RRTWC is responsible for maintaining accurate and confidential records relating to a worker’s rehabilitation and return to work. The RRTWC is also responsible for ensuring that this information is stored separately the employment records and is only accessible to approved staff (i.e. remuneration details, leave entitlements etc).
• Rehabilitation and Return to Work Coordinators are often are trusted to collect, use and store information about an injured worker in a way which shows the utmost respect and confidentiality to that person.
• If a request for information is received, it is recommended that the RRTWC liaises with their manager.
• Ensure the injured worker understands and has given consent to their information being collected or disseminated to other relevant stakeholders, such as allied health providers. This can be achieved by requesting the worker to complete an injured worker authorisation form.
The Case Management team must work together to formulate strategies to manage the case. The Case Management Team may consist of:
• Injured / Ill employees
• OIC / Supervisor
• Injury Management Advisor
• Rehabilitation & return to work coordinator
• Treating GP or Specialist
• Allied health professionals
• HR Manager / Payroll (if applicable)
• Human Services Officer (if applicable)
• Executive & Senior Management.
When there is a workplace injury, not all parties are in communication with each other. The RRTWC is the person who ensures everyone is on the same page and all working towards the same rehabilitation and return to work goals. The RRTWC speaks to all parties and encourages all parties to speak to each other.
Until the insurance company has assessed the claim and determined whether they will accept it, you need to keep the worker informed of progress.
A good communication plan consists of:
1) Keeping the worker informed of any changes or updates relating to the workplace, clarifying the worker’s preference for communication
2) At least weekly conversations with injured worker (phone or face-to-face)
3) Text messages for small, quick bits of information back & forth
4) Emails for information that is important to have a record of - such as medical documents/ certificates, letters, decisions of IW or other parties, appointments, meetings, employer requests.
5) Maintain occasional contact with spouse/family members if IW gives permission - especially if serious injury.
Medical providers to an inured worker provide an essential role in rehabilitation and effective communication with medical providers is paramount to effective recovery. Building a good communication channel is one of the priorities of the RRTWC. Medical practitioners value insight that a workplace can provide to help guide their understanding of what duties are available in the workplace to support the worker’s gradual and safe return to work as part of their recovery.
The following will help in building good communication channels with medical practitioners:
• Prepare a standard introduction letter to doctor, asking for their cooperation with return to work. Send this with the Injured Worker.
• Use pre-designed lists of suitable duties available at the workplace. Easy & quick for doctor to read – tick / flick & sign.
• Liaise and collaborate with the Insurer to discuss the options for organising a case conference with the worker’s treating practitioners to discuss rehabilitation needs with complex cases.
• Send the Treating Medical Practitioner the Injured Workers’ signed authority. If no consent from Injured Worker you can still contact the Treating Medical Practitioner to advise them of the return to work support and processes offered in your workplace.
• The [12] WorkCover Queensland Injury Information Pack – A guide for employers and workers , is a good reference document.
It is often considered that the direct supervisor can have significant influence over the outcome of a claim, in some instances above any other person in the injured worker’s life.
Immediate supervisors and managers have a critical role in ensuring the success of any workplace rehabilitation program and play a significant role during all stages of the workplace rehabilitation process. These supervisors and managers:
• Promote a stay at work and recover at work culture
• Ensure workers feel productive, supported and valued
• Determine appropriate suitable duties available
• Create options in other departments, communicating across work areas
• Understand restrictions on medical certificate
• Supervise and enforce worker compliance to any restrictions.
Workers often believe their supervisor’s attitude toward them reflects that of management. Therefore, to foster a feeling of being valued, supervisors should show:
• Support and concern for their employee’s welfare
• Responsiveness, empathy and respect on a daily basis.
The supervisor also plays a key role in encouraging co-worker support for injured workers.
• Strong supervisor and co-worker support affects a worker’s decision to return to work and can reduce disability.
An injured workers initial treatment is critical to the way in which the worker participates in return to work on all levels.
• If an injured worker is left to fend for themselves they are likely to not feel supported or appreciated by their employer and therefore treatment generally lasts longer and is more difficult to coordinate.
[3] WorkCover Queensland
“Work, in general, is good for health and wellbeing; and Long term work absence, work disability and unemployment have, in general, a negative impact on health and wellbeing.”
[4] AFOEM and RACP
Advantages of recovery at work after injury
1) Research has shown that an early return to meaningful work will result in a faster recovery from injury.
2) This approach was first pioneered by sports coaches who, by providing structured training for the injured athlete, and could return them to their sport quicker and healthier than if they just rested.
3) For back injuries - it has been proven that any period of rest beyond 3 days is associated with a worse outcome for the back injury regardless of what caused the back injury.
4) This approach works because early return to activity:
○ Does not allow muscles to weaken and cause the entire area to become unstable
○ Improves the blood flow to the injury, which in turn improves the healing rate
○ Helps maintain your general fitness for your normal life – for eg. sense of balance, fatigue tolerance, body strength to perform normal activities of daily life.
The longer a worker is off work the less likely they will ever return.
• 20 days off = 70% chance of returning to work
• 45 days off = 50% chance of returning to work
• 70 days off = 35% chance of returning to work
1) Harmful to physical and mental health and wellbeing
2) Increased financial pressure
3) Increased mortality rates, specifically:
○ Cardiovascular disease
○ Suicide.
[4] AFOEM and RACP
4) Affects more than the injured worker, i.e. families including children of parents out of work who suffer the consequences:
○ Poorer physical and mental health of family members
○ Decreased educational opportunities
○ Reduced long term employment prospects
○ Intergenerational poverty.
“...long term worklessness is one of the greatest risks to health in our society. It is more dangerous than the most dangerous jobs in the construction industry, or [working on an oil rig in] the North Sea, and too often we not only fail to protect our patients from long term worklessness, we sometimes actually push them into it, inadvertently...”
[4] AFOEM and RACP
When an injured worker returns to work it:
• Ensures some physical activity is undertaken on work days
• Provides a sense of identity, community and social inclusion
• Allows them to feel that they are making a contribution to society and their family
• Gives structure to their days and weeks
• Provides a sense of financial security
• Decreases the likelihood of them engaging in risky behaviours, i.e. excessive drinking
• Improves general health and wellbeing
• Improves mental health.
• We know physical activity has positive effects on health and wellbeing and injury recovery
• Therefore, physical activity should be a large part of the rehabilitation process
• Furthermore, work promotes physical activity and must be an important part of the rehabilitation process.
An athlete continues training and conditioning whilst recovering from an injury.
Like athletes, working involves skills, attitudes and habits, by staying “in-training” even if doing shorter hours or alternate duties; the transition back to health and regular employment is easier to manage and more successful.
All parties must recognise that management of a work injury requires management of the injury AND management of the work.
Management of workplace issues including addressing job satisfaction and belonging. Ensure workers feel part of something not removed through their return to work.
Rehabilitation is about achieving an early and durable recovery and return to work following an injury. It is the employers duty to help rehabilitate the injured worker.
The term rehabilitation is difficult to define as the outcomes depend largely on the severity of the injury, the longevity of impairment and scope of cover.

The Meaning of Rehabilitation
Workers’ Compensation and Rehabilitation Act 2003
Section 40 Meaning of rehabilitation
(1) Rehabilitation, of a worker, is a process designed to—
(a) ensure the worker’s earliest possible return to work; or
(b) maximise the worker’s independent functioning.
(2) Rehabilitation includes—
(a) necessary and reasonable—
(i) suitable duties programs; or
(ii) services provided by a registered person; or
(iii) services approved by an insurer; or
(b) the provision of necessary and reasonable aids or equipment to the worker.
(3) The purpose of rehabilitation is—
(a) to return the worker to the worker’s pre-injury duties; or
(b) if it is not feasible to return the worker to the worker’s pre-injury duties—to return the worker, either temporarily or permanently, to other suitable duties with the worker’s pre-injury employer; or
(c) if paragraph (b) is not feasible—to return the worker, either temporarily or permanently, to other suitable duties with another employer; or
(d) if paragraphs (a), (b) and (c) are not feasible—to maximise the worker’s independent functioning.
Managing a worker’s injuries in the workplace to achieve early return to health and work is a central feature of workers compensation systems.
There is a great deal of evidence to support the concept that an offer of suitable work or employment, and the engagement of key parties (worker, employer, doctor, insurer and other providers) in implementing an injured worker’s return to work, greatly reduces the duration and associated costs of claims and common law payouts, which in turn improves social and health outcomes for the worker concerned.
The Heads of Workers’ Compensation Authorities (HWCA) have endorsed a principles-based framework for the delivery of workplace rehabilitation provider services. These principles have been developed to support Workplace Rehabilitation Providers in the delivery of services to workers with a compensable injury. The adoption of these principles by service providers supports the position for the workplace to encourage an early and safe return to work activities.
1) Adopt a biopsychosocial approach to build capacity through work participation.
2) Empower the worker and employer to achieve the goals of return to work.
3) Deliver outcome driven workplace-based rehabilitation services.
4) An evidenced-based approach to service design and delivery.
5) Services that result in a measurable benefit to the worker and employer Say yes more.
[12] Heads of Workers’ Compensation Authorities
Workers’ compensation legislation specifies requirements for an employer to provide rehabilitation for workers injured through work activities. As a general rule the key elements state the purpose of rehabilitation as a process to return the worker to:
• Their original duties – or if this is not an option then:
○ Suitable duties or job role with their current employer or, if this is not practical
○ Suitable duties with an alternative employer for either an interim or permanent period of time
○ Re-training/re-skilling into a different career or vocation (assistance given by Insurer to do this).
Queensland has the Guidelines for Standard for Rehabilitation , which includes the following seven principles:
1) Employer commitment
2) Providing workers with opportunities to recover at work
3) Actions detailed in rehabilitation and return to work
4) Role of the supervisor
5) Early employer contact with injured worker
6) Appointment of a Rehabilitation and Return to Work Coordinator (the coordinator)
7) Communication with the worker’s treating doctor.
These will be explored in more detail in the upcoming section of Employer Rights and Responsibilities.
Claims Process flow Chart
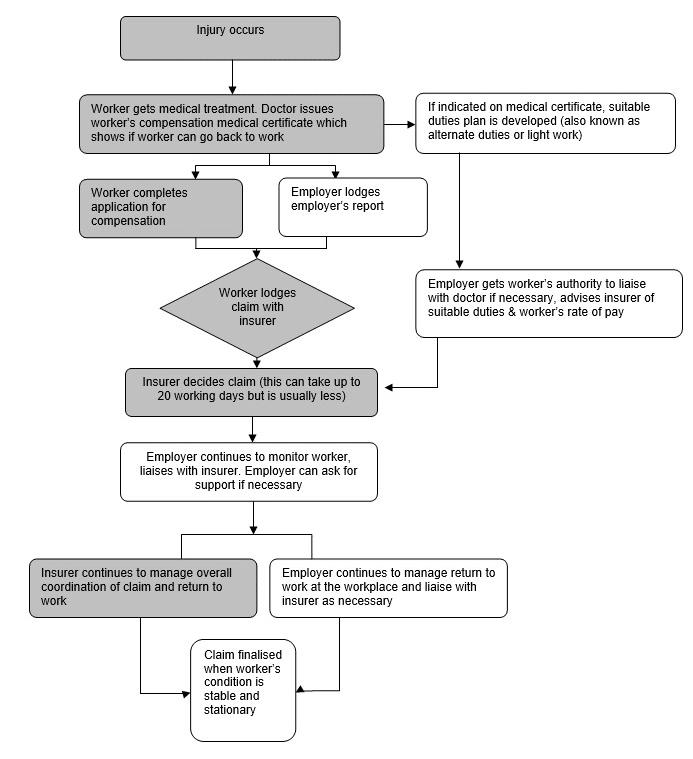
When an injury occurs the first priority is obviously seeking first aid or medical treatment. An application can then be lodged for any injury.
Even though the insurance policy holder is the employer, the injured worker is the one that must lodge the claim for compensation for their injury.
It is advisable that the rehabilitation and return to work coordinator (RRTWC) discusses the claim lodgement with the injured worker and they then either lodge the claim together, or if the worker agrees, the RRTWC can lodge the claim on the worker’s behalf at the same time they lodge the Employer’s Report. The RRTWC can assist the application by ensuring all paperwork is correct for the worker, such as wage information, employer details etc.
For the workers’ compensation claim application to be valid, it must be lodged with a work capacity medical certificate as per the Workers’ Compensation and Rehabilitation Act 2003.
Claims may be lodged online, over the phone, or via the WorkCover Worker Assist App on mobile devices. Once the claim is lodged with the Insurer (WorkCover Queensland or Self-Insured Employer), a claim number will be issued by the Insurer.
The Insurer must make a decision to either accept or reject the claim within 20 business days. If a decision cannot be made in that time the Insurer must give the worker written advice as to why a decision cannot be made yet.
Employers should not wait for the Insurer to make up their mind about the claim before they start a return to work program with the injured worker. Early intervention with rehabilitation and return to work is the most influential factor which leads to a successful recovery outcome.
Regardless of whether the insurer accepts or rejects the claim, the injured worker is still your employee and still requires your help to get better. The system of workers’ compensation is just that - an insurance process which has a beginning date and an end date. Other than that, the injured worker is still your employee that needs to be kept safe, respected and managed within your business.
Whilst the RRTWC should encourage the injured worker to regularly communicate with the Insurer’s representative, the employer should be a key contact with the worker. Either the RRTWC or the Supervisor should be in regular contact with the worker. The RRTWC can update the Insurer about their worker.
Note!
this is an insurance process and as an employer you should be communicating with and managing your employee.
It is the employer’s responsibility to support and assist the worker in completing and lodging their application. This means the employer should have a procedure in place and ensure that all workers know what is required when an injury occurs.
As a Rehabilitation and Return to Work Coordinator, you may need to assist injured workers and other relevant personnel in navigating the workers’ compensation claim process. There are a few important reasons why the RRTWC may need to assist the injured worker in lodging their claim. These include:
• Language and literacy restrictions
• Physical limitations
• Assistance with understanding terminology and processes
• Internet and telephone access.
Workers may also seek further assistance through The Workers’ Compensation Information Service, provided by Queensland Council of Unions. Free and confidential information is provided to both workers and employers if they are unsure about the workers’ compensation process (www.queenslandunions.org/workers-compensation-advisory-service/).
In some instances it may be difficult for the injured worker to complete the claim form due to the injury.
The injured worker may have never heard of workers’ compensation insurance before, let alone know what the claim process is. The RRTWC can explain the process and guide the worker through lodging a claim so they have a better chance of lodging all the correct information first go.
The injured worker will not have access to some of the employer information required when lodging a claim. For eg. The Employer policy number, ABN, bank details, wages & payroll information, any excess paid.
The worker may not be of English-speaking origin and struggles to understand what is being asked of them by the Insurance company.
Similarly, the injured worker may not be able to read or write.
The time frames to report differ between jurisdictions, however all States and Territories require the injury to be reported as soon as possible to the employer and the insurer.
An injured worker has 6 months to apply for Workers’ Compensation in Queensland, however the sooner they claim once they know about the injury, the sooner they can get treatment. The 6 months starts on the day the injured worker first sought treatment from a doctor and the doctor connects the injury to work.
Section 131 Time for applying
(1) An application for compensation for an injury is valid and enforceable only if the application is lodged by the claimant within 6 months after the entitlement to compensation for the injury arises.
(2) If an application is lodged more than 20 business days after the entitlement to compensation arises, the extent of the insurer’s liability to pay compensation is limited to a period starting no earlier than 20 business days before the day on which the valid application is lodged.
(3) Subsection (2) does not apply if death is, or results from, the injury.
(4) An insurer must waive subsection (1) for a particular application if it is satisfied that special circumstances of a medical nature, decided by a medical assessment tribunal, exist.
(5) Also, an insurer may waive subsection (1) for a particular application if—
(a) it is satisfied that a doctor, nurse practitioner or dentist has assessed the injury as resulting in total or partial incapacity for work; and
(b) the claimant lodged the application within 20 business days after the first assessment under paragraph (a).
(6) An insurer may waive subsection (1) or (2) for a particular application if the insurer is satisfied that a claimant’s failure to lodge the application was due to— (a) mistake; or
(b) the claimant’s absence from the State; or
(c) a reasonable cause.
Workers’ Compensation and Rehabilitation Act 2003
Section 735 Discretion of insurer to waive time limit for applying for compensation
Workers’ Compensation and Rehabilitation Act 2003
Section 132 Applying for compensation
(1) An application for compensation must be made in the approved form by the claimant.
(2) The application must be lodged with the insurer.
(3) The application must be accompanied by—
(a) a certificate in the approved form given by—
(i) a doctor who attended the claimant; or
(ii) if the application relates to a minor injury—a nurse practitioner who attended the claimant and who is acting in accordance with the workers’ compensation certificate protocol; and
(b) any other evidence or particulars prescribed under a regulation.
(4) A registered dentist may issue the certificate mentioned in subsection (3)(a) for an oral injury.
(5) If the claimant can not complete an application because of a physical or mental incapacity, someone else may complete it on the claimant’s behalf.
(6) An application for compensation is valid and enforceable if it complies with this section.
An application for compensation should be made as soon as possible. Claims accepted quickly lead to compensation & medical expenses being paid sooner. Financial stress and disruption to the injured worker’s life are minimised whilst employer’s productivity levels are protected. Less stress will also contribute to reduced recovery timeframes for the injured worker and an earlier return to work.
Employers have an obligation to report all injuries, no matter how minor, or even if the injured worker is only treated for a first aid injury at the workplace and does not seek medical treatment from a doctor.
The Worker’s Compensation and Rehabilitation Act 2003 states an employer must send a report to the insurer as soon as an injury, which may be deemed compensable under the Queensland Worker’s Compensation legislation, has been sustained, identified or reported. Claims which go through both WorkCover Queensland and Self-Insured Employers must abide by these same sections in the Act.
Furthermore, the Act particularly states an employer must report the injury to the insurer if “the employer pays the worker an amount, either in compensation or instead of compensation, that is payable by the employer or WorkCover under the Act for an injury sustained by the worker”.
This section is included to address the situation where employers attempt to reduce their injury claim statistics by not reporting the claim. The employer offers to pay medical costs and wages in return for the employee not lodging a workers’ compensation claim.
The employer must send their report to the insurer within 8 business days of having knowledge of the injury, otherwise penalty fines may apply.
Workers’ Compensation and Rehabilitation Act 2003
Section 133 Employer’s duty to report injury
(1) An employer whose worker sustains an injury for which compensation may be payable must complete a report in the approved form and give the report to the insurer.
(2) The employer must complete and give the report to the insurer immediately after the first of the following happens—
(a) the employer knows the injury has been sustained;
(b) the worker reports the injury to the employer;
(c) the employer receives the insurer’s written request for the report.
(3) If an employer fails to comply with subsection (1) within 8 business days after the first of the circumstances mentioned in subsection (2) happens, the employer commits an offence, unless the employer has a reasonable excuse.
Maximum penalty—50 penalty units.
(4) In this section—
insurer means—
(a) if the employer is a self-insurer—the person authorised by the employer as selfinsurer to make a decision under section 134 on any claim for compensation for the injury; or
(b) if the employer is not a self-insurer—WorkCover.
Section 133A Employer’s duty to tell insurer if worker asks for, or employer makes, a payment
133A Employer’s duty to tell insurer if worker asks for, or employer makes, a payment
(1) An employer must give the insurer written notice in the approved form if—
(a) a worker asks the employer for compensation for an injury sustained by the worker; or
(b) the employer pays the worker an amount, either in compensation or instead of compensation, that is payable under the Act by the employer as a self-insurer or WorkCover for an injury sustained by the worker.
(2) If the employer fails to comply with subsection (1) within 8 business days after the request or payment is made, the employer commits an offence, unless the employer has a reasonable excuse.
Maximum penalty—50 penalty units.
(3) In this section—
insurer means—
(a) if the employer is a self-insurer—the person authorised by the employer as selfinsurer to make a decision under section 134 on any claim for compensation for the injury; or
(b) if the employer is not a self-insurer—WorkCover.
For the workers’ compensation insurer to process a claim they will require:
• The worker’s personal details
• The worker’s employment status
• Details of the injury event
• The Workers’ Compensation Medical Certificate from the treating doctor.
Under legislation, workers are required to cooperate with insurers, their employer and their doctors. This helps insurers make a decision on the claim and also helps workers receive appropriate medical treatment and rehabilitation as quickly as possible.
To make sure a claim is made efficiently, a worker must:
• Complete and sign all necessary forms
• Let insurers know if their condition or treatment changes
• Make sure insurers has all current workers’ compensation medical certificates.
Under legislation, a Worker must ensure that:
• All information provided to insurers is true and not misleading e.g. a worker must inform their insurer if they are receiving Centrelink payments
• Insurers know if they are returning to work of any kind – this includes self employment, working for another person and whether or not the worker is paid for performing the activity
• They participate in rehabilitation programs if required to.
Penalties can apply to the injured worker if they do not comply with these requirements. Insurers can suspend a worker’s compensation benefits. The Office of Industrial Relations can prosecute for an offence under the Act if these requirements are not fulfilled.
What does a worker have to prove in order to be eligible for workers’ compensation?
When a claim is submitted to an Insurer there are a number of things that need to be considered in the decision making process to accept or reject a claim.
The following will be considered:
• Has the claim been made in the right timeframe?
• Was the person claiming working for the employer when they were injured?
• Is the person claiming considered to be a worker?
• Did a work-related incident cause the injury?
• Was the person’s job a significant contributing factor to their injury?
In some instances there may also be other criteria applied in the decision making process. Examples of times when this may occur include claims for psychological and psychiatric injuries, industrial deafness, injuries travelling to from or for work or on scheduled breaks, aggravated injuries or ongoing symptoms, work-related respiratory diseases or diseases contracted while doing your job (example Q-fever) or death caused by a work-related event or by illnesses e.g. mesothelioma or malignant skin cancer, that develop over a long period of time.
[5] WorkCover Queensland
Based on the facts presented, the Insurer determines if they will accept or reject the workers’ claim. As noted earlier under Section 134 of the Act, a decision must be made by the Insurer within 20 business days of receiving the application for compensation. Notification will be provided if this cannot be done. Section 134 also details the notification expectations of the Insurer when a claim has been accepted as opposed to rejected.
In relation to support for workers with psychiatric or psychological injuries Section 232AA and 232AB notes the support that may be provided during the determination of their claim.
Compensation
Section 220 Insurer’s responsibility for rehabilitation and return to work
If accepted the worker and employer will be notified. The insurer may then pay the costs associated with the injured worker’s rehabilitation. This can include wages, medical treatment expenses, travel, certain lump sum payments or death and funeral benefits.
If the application is not accepted, the Insurer will speak to the Worker and explain the decision that has been made. A formal letter, called Reasons for Decision, will be provided to the Worker explaining the information considered and the reason why the application was not accepted. Section 540 of the Workers’ Compensation and Rehabilitation Act 2003 and Section 148 of the Workers’ Compensation and Rehabilitation Regulation 2014 provide detail on what needs to be provided to the worker. This includes information on the rights to a review of the decision.
The definition of a worker is provided below.
Workers’ Compensation and Rehabilitation Act 2003
Section 11 Who is a worker
11 Who is a worker
(1) A worker is a person who—
(a) works under a contract; and
(b) in relation to the work, is an employee for the purpose of assessment for PAYG withholding under the Taxation Administration Act 1953 (Cwlth) , schedule 1, part 2-5.
(2) Also, schedule 2, part 1 sets out who is a worker in particular circumstances.
(3) However, schedule 2, part 2 sets out who is not a worker in particular circumstances.
(4) Only an individual can be a worker for this Act.
For employers to further understand who is a ‘worker’ it is recommended they reference the [13] Who is a worker - Guide for Employers’ document provided by WorkCover Queensland .
Note: In many situations, contractors and subcontractors may also be defined as ‘workers’, depending on the circumstances of their working arrangement. To understand more about who is considered a worker in Queensland refer to the Workers’ Compensation and Rehabilitation Act 2003.
Do not presume a contractor is a contractor!
• Some states require Principal Contractors to hold insurance for their sub-contractors anyway.
• Use the decision tools & tests, get advice.
• For Auditing keep records about your decision process & reasons to exempt e.g. copy of contractor’s Workers Comp policy, details of engagement, total amount paid for contracts.
• Make sure to review decisions annually.
• Remember, the insurer ultimately decides!
Cross-border provisions provide coverage for workers who travel to or work temporarily in different jurisdictions, as long as workers meet a ‘state of connection’ test.
An injured worker’s state or territory of connection is determined by the following tests:
• Test A — the territory or state in which the worker usually works in that employment, or
• Test B — if not identified through (A) — the territory or state in which the worker is usually based for the purposes of that employment, or
• Test C — if not identified through (A) or (B) — the territory or state in which the employer’s principal place of business in Australia is located.
If no state of connection can be determined for a worker and a worker is not entitled to compensation for the same matter under the laws of a place outside Australia, a worker’s employment is connected with the state where the injury occurred.
These tests are hierarchical, so if the first test does not provide an answer, the next test is applied until the worker’s status is determined.
[1] Safe Work Australia
This liability determination is based on whether the application has been lodged in time as noted under the Act. As mentioned in the previously, Section 131 of the Act notes an injured worker has 6 months to lodge the claim from the date they first see a doctor.
In the determination of acceptance, the ‘event’ is considered. This essentially refers to a point or points in time where an exposure has resulted in an injury.
Workers’ Compensation and Rehabilitation Act 2003
Section 31 Meaning of event
Broadly speaking, most Workers’ Compensation schemes define an injury as:
• Any physical or psychological injury
• Any disease contracted in the course of employment
• The recurrence or aggravation of any existing injury or disease
• While traveling to and from work, depending on the jurisdiction.
Workers’ Compensation and Rehabilitation Act 2003
Section 32 Meaning of injury
32 Meaning of injury
(1) An injury is personal injury arising out of, or in the course of, employment if the employment is a significant contributing factor to the injury.
(2) However, employment need not be a contributing factor to the injury if section 34(2) or 35(2) applies.
(3) Injury includes the following—
(a) a disease contracted in the course of employment, whether at or away from the place of employment, if the employment is a significant contributing factor to the disease;
(b) an aggravation of the following, if the aggravation arises out of, or in the course of, employment and the employment is a significant contributing factor to the aggravation—
(i) a personal injury;
(ii) a disease;
(iii) a medical condition, if the condition becomes a personal injury or disease because of the aggravation;
(c) loss of hearing resulting in industrial deafness if the employment is a significant contributing factor to causing the loss of hearing;
(d) death from injury arising out of, or in the course of, employment if the employment is a significant contributing factor to causing the injury;
(e) death from a disease mentioned in paragraph (a), if the employment is a significant contributing factor to the disease;
(f) death from an aggravation mentioned in paragraph (b), if the employment is a significant contributing factor to the aggravation.
(4) For subsection (3)(b), to remove any doubt, it is declared that an aggravation mentioned in the provision is an injury only to the extent of the effects of the aggravation.
(5) Despite subsections (1) and (3), injury does not include a psychiatric or psychological disorder arising out of, or in the course of, any of the following circumstances—
(a) reasonable management action taken in a reasonable way by the employer in connection with the worker’s employment;
(b) the worker’s expectation or perception of reasonable management action being taken against the worker;
(c) action by the Regulator or an insurer in connection with the worker’s application for compensation.
Examples of actions that may be reasonable management actions taken in a reasonable way—
• action taken to transfer, demote, discipline, redeploy, retrench or dismiss the worker
• a decision not to award or provide promotion, reclassification or transfer of, or leave of absence or benefit in connection with, the worker’s employment
Labelled differently by each state but they have similar coverage:
• QLD – psychiatric or psychological disorder
• NSW – psychological or psychiatric disorder
• SA – psychiatric injury means pure mental harm
• VIC – mental injury
• WA – diseased caused by stress
• NT – mental injury
• ACT – mental injury
• TAS – an injury (not further defined)
The following graph outlines the tests involved to accept or reject a psychological injury claim.
Does the injury meet the thresholds for a psychological claim in this state?
Was management or administrative action involved?
No - Claim accepted No - Claim accepted
Was the action reasonable & done in a reasonable manner?
Was the psychological injury “mostly” due to the reasonable workplace action?
Claim rejected
Further investigation required
The Queensland Workers’ Compensation system has provisions for claims to be accepted when travelling to, from or for work related purposes. Section 35 Other circumstances and Section 36 Injury that happens during particular journeys of the Act outline the provisions relating to journey claims. Broadly these claims can include travelling:
• Between your home and place of work
• To or from training relating to your work
• To or from medical or rehabilitation treatment that is part of an existing WorkCover claim
• Between jobs with separate employers
• For work-related reasons (i.e. a work conference or meeting) locally, interstate or internationally.
As a general note, you need to have started your journey without any major delays or deviations and be travelling directly between your home and workplace or trade, technical, or other training school (or other location as outlined above).
Injury while at or after worker attends place of employment
Sections 34, 35 and 36 of the Act define journey & recess claims:
• Journey claims are injuries acquired from going to and from any place that is connected to employment.
• Recess claims comprise of injuries which occur whilst on scheduled or unscheduled breaks from work in the work day, e.g. going out to get a coffee at morning tea break and tripping over on the footpath.
The duty of care that an employer owes to its employees extends beyond the traditional physical office and premises of the business to areas in which a worker is performing an activity that was reasonable and incidental to employment and within the terms and expectation of the employment.
As such an employer’s liability in respect of statutory workers compensation and future damages claims may extend to employees working from home who sustain injuries in circumstances where they are involved in an accident. Personal injuries sustained in those circumstances may be deemed to have arisen out of or in the course of employment as the personal injury was sustained in the workplace.
Workers’ Compensation and Rehabilitation Act 2003
Section 34 Injury while at or after worker attends place of employment
Workers’ Compensation and Rehabilitation Act 2003
Section 35 Other circumstances
Workers’ Compensation and Rehabilitation Act 2003
Section 36 Injury that happens during particular journeys
Employers or Injured Workers may be aggrieved by a decision the Insurer makes. For example, an Injured Worker is aggrieved by an Insurer denying their claim, or an Employer may be aggrieved by an Insurer accepting a claim as they don’t believe it is for a work-related injury.
The Employer may raise any concerns with the Claims Officer/Customer Adviser throughout the duration of the claim, however this is especially important before the claim is accepted by the insurer so the Insurer has a chance to fully investigate the concerns raised. For example, an Employer may dispute the injury ever occurred at work or may dispute decisions made about the claim.
If the Employer feels their dispute, or any other issues they have raised have not been resolved to their satisfaction, and disagree with a decision made by the Insurer, they can seek a Review with the Workers’ Compensation Regulator.
Similarly, an Injured Worker can lodge an application for Review with the Workers’ Compensation Regulatory Services if they are unhappy with the decision the Insurer makes.

If the employer or injured worker are aggrieved by a decision that the Insurer makes they can seek a review of that decision. A review application must be lodged within 3 months of the decision.
The Review Unit will make a new decision based on the information they have from the Insurer and any new information from either party. Whatever is submitted will be given to the other party under ‘procedural fairness’, so everyone sees all evidence and has a chance to respond to it.
If The Review Unit upholds the Insurer’s decision then things will stay as they are. If The Review Unit ‘sets aside’ the Insurer’s decision, they will substitute a new decision and all parties, including the Insurer, will be bound to the new decision.
If the claimant is aggrieved by the Workers’ Compensation Regulator’s decision, they have the right to seek an Appeal through the Industrial Relations Commission (QIRC). Decisions by the QIRC can be appealed to the Queensland Industrial Court. The Appellant (the one seeking the Appeal) should consider engaging legal counsel when entering into a court process against Workers’ Compensation Regulator (as they are the ones who made the decision) and their legal team. The Workers’ Compensation Regulator uses its lawyers to defend its decision. A Notice of Appeal must be lodged within 20 days of receiving the review decision. Where the Review Unit send the decision back to the Insurer to make a fresh decision it cannot be appealed in the Industrial Relations Court.
The Appeal process is a lengthy court process with potentially no outcome inside 12 months. If the Injured Worker is seeking for the claim to be accepted by this process they may need to realise they will not have an income during this time if they cannot work.
Both the injured worker and the employer have rights and responsibilities throughout the whole claim process.

If the claim is accepted, the Employer should take every reasonable step to assist or provide the worker with rehabilitation for the period for which the worker is entitled to compensation. Employers should be proactive in keeping the Insurer informed about the worker’s progress in returning to work.
As discussed, Employers have a responsibility when an employee suffers a work-related injury or illness. The basic premise is that the employer provides support in helping the injured worker return to work as soon as possible after the injury is sustained.
Below is an outline of responsibilities that an employer has for rehabilitation:
• Report the injury and start the claim process.
• Contact your worker as soon as you can after the injury.
• Talk with your worker about returning to work being the goal. Encourage them to come back to work if it’s safe for them to do so.
• Take time to understand how the injury is affecting your worker both physically and mentally.
• You can offer flexible working arrangements to help your worker come back to work and find other work for them to do if needed.
• Keep an eye on your worker’s recovery process, making beneficial changes to their work as they improve. Continue to let WorkCover or the insurer know how they are going.
• Make sure your rehabilitation and return to work coordinator (and any other key staff such as a supervisor) have the right skills and training and are supporting your worker as required.
• Put in place and maintain effective workplace rehabilitation policies and procedures.
• Follow the [7] Guidelines for Standard for Rehabilitation seven principles (see below)
Review the 7 principles outlined in the [7] Guidelines for Standard for Rehabilitation below and comment on the employer responsibilities below.
Principle 1: Employer commitment
Principle 2: Providing workers with opportunities to recover at work
Principle 3: Actions detailed in rehabilitation and return to work
Principle 4: Role of the supervisor
Principle 5: Early employer contact with injured worker
Principle 6: Appointment of a Rehabilitation and Return to Work Coordinator (the coordinator)
Principle 7: Communication with the worker’s treating doctor
Contact with the injured worker should be made as soon as the details of the injury are known. It is then the injured worker’s decision to make a claim, however the employer can certainly help & guide the injured worker with this process.
When a worker is injured on the job site or to/from the site and has an incapacity for work, employers have obligations under the law to help them return to work safely.
Under Section 228 of the Act, employers must take all reasonable steps to assist or provide the worker with rehabilitation during the prescribed time of the claim. The rehabilitation must be of a reasonable standard - suitable duties programs must provide meaningful work.
It is essential the employer consults and engages regularly with the worker directly. With worker consent, employers also need to consult with the treating health practitioners and occupational rehabilitation providers to achieve the most successful outcomes for the worker.
Employers should start tentatively planning for their worker’s return to work as soon as they receive notification of the injury, the Work Capacity Certificate - workers’ compensation, or the employer is notified by their insurer that they have received these documents, whichever happens first.
Return to work planning should not wait until a claim has been accepted. This is particularly important for claims for psychological injuries as the claim determination period for these types of injuries is often longer than for physical injuries.
Clarify that return to work planning should not wait until a claim has been accepted. This is particularly important for claims for psychological injuries as the claim determination period for these types of injuries is often longer than for physical injuries.
How soon a worker can return to work on a Suitable Duties Program (SDP) will depend on the injury or illness, capacity for work, and the workplace. Workers do not have to wait until they are 100% recovered to return to work. On the contrary, better recovery occurs whilst working.
Employers should be open to all options to be able to assist an injured worker back to meaningful work. With some out-of-the-box thinking and consultation with all parties the options are limitless.
Workers’ Compensation and Rehabilitation Act 2003
Section 232B Dismissal of injured worker only after 12 months
232B Dismissal of injured worker only after 12 months
(1) Within 12 months after a worker sustains an injury, the employer must not dismiss the worker solely or mainly because the worker is not fit for employment in a position because of the injury.
Maximum penalty—40 penalty units.
(2) This section applies to a dismissal after the commencement of this section even if the worker became unfit before the commencement.
Workers’ Compensation and Rehabilitation Act 2003
Section 232C Replacement for injured worker
(1) This section applies if the employer wants to employ a replacement worker while an injured worker is not fit for employment in a position because of the injury.
(2) The employer must, before a replacement worker starts employment, give the replacement worker a written notice informing the replacement worker of—
(a) the temporary nature of the employment; and
(b) the injured worker’s right to return to work.
(3) In this section—
replacement worker means—
(a) a person who is specifically employed because an injured worker is not fit for employment in a position because of the injury; or
(b) a person replacing a worker who is temporarily promoted or transferred to replace the injured worker.
Just as they have responsibilities, employers also have rights under Workers’ Compensation legislation.
The employer may raise any concerns with the Insurer’s representatives throughout the duration of the claim. This may include disputing the claim, or any decisions made about the claim. If the Employer feels their dispute, or any other issue they have raised with the Insurer, has not been resolved to their satisfaction, they can make an official complaint through the insurer as the initial process to escalate their concern.
If the Employer disagrees with a decision made by the Insurer, they can seek a review with the Workers’ Compensation Regulator if the reasoning is listed in section 540 of the Act. If after this first appeal they are still aggrieved by the decision they may lodge an appeal with the Queensland Industrial Relations Commission (QIRC).
Reviewable decisions are outlined in Chapter 13 of the A Workers’ Compensation and Rehabilitation Act 2003.
WorkCover right to information and information privacy application
Under the Right to Information Act 2009 and the Information Privacy Act 2009, every person has a general right to request access to documents held by government agencies. Employers can seek a release of information for claim information under the Administrative release policy with WorkCover Queensland.
Employers can find more information on lodging an application for review on:
• https://www.worksafe.qld.gov.au/about/right-to-information/right-to-information-and-ip
[8]WorkCover Queensland
Employers should ensure that the Injured Worker has a current Work Capacity Certificate at all times.
Expressions of regret and apologies provided by employers following workplace injuries are now exempt from being considered in a common law claim. This is intended to encourage employers to give apologies and reduce the distress experienced by injured workers. Any expression of regret or apology made prior to 30 October 2019 will be inadmissible if a relevant notice of claim for damages is made after 30 October 2019.
Workers’ Compensation and Rehabilitation Act 2003
Section 320B Purpose of division
The purpose of this division is to allow an individual to express regret about an incident that may give rise to an action for damages without being concerned that the expression of regret may be construed or used as an admission of liability on a claim or in a proceeding based on a claim arising out of the incident.
Workers’ Compensation and Rehabilitation Act 2003
Section 320C Meaning of expression of regret
An expression of regret made by an individual in relation to an incident alleged to give rise to an action for damages is any oral or written statement expressing regret for the incident to the extent that it does not contain an admission of liability on the part of the individual or someone else.
Workers’ Compensation and Rehabilitation Act 2003
Section 320D Expressions of regret are inadmissible
320D Expressions of regret are inadmissible
An expression of regret made by an individual in relation to an incident alleged to give rise to an action for damages at any time before a civil proceeding in relation to the incident is started in a court is not admissible in the proceeding.
There are a range of entitlements for an injured worker with an accepted claim. Details of entitlements can be seen by contacting WorkCover Queensland. Insurers generally cover:
1) Loss of wages (Total or Partial)
2) Medical treatment costs
3) Medication costs
4) Travel or transportation costs >20km
5) Medical Aids or Living Aids / Equipment eg. Wheelchairs / splints
6) Permanent Impairment Lump Sum
7) Fatality – payments to family
8) Common law payouts (some states).
• A calculation called normal weekly earnings (NWE) is completed using the worker’s weekly earnings from continuous or intermittent employment during the 12 months prior to their injury. If worker’s haven’t been employed for 12 months, then the earnings for the period they have been employed will be used.
• Once a worker’s NWE is known this in turn is used to calculate the weekly compensation rate payable for a claim.
• For the majority of workers the weekly compensation rate for the first 26 weeks will be paid at the greater of the following:
○ 85% of their NWE; or
○ 100% of their industrial instrument (most workers will be employed under an industrial instrument and this is confirmed with their employer).
• Visit WorkSafe.qld.gov.au for the NWE calculator tool and further information regarding weekly compensation benefits.
• Employers may pay sick or other accrued leave to the injured worker while the claim is being determined. Upon acceptance of the claim, leave will need to be reimbursed.
• If the claim is accepted, you can choose to pay your worker directly and seek reimbursement from WorkCover or WorkCover can pay weekly benefits directly to your worker.
• You will need to pay an excess on any accepted claim if your worker has taken time off from work due to their injury. WorkCover will advise of the excess amount when communicating acceptance of the claim.
• For workers participating in a suitable duties program, you will pay the worker at the normal rate for work performed. WorkCover will pay a top-up amount either directly to you or your worker.
[9] WorkCover Queensland
If an injured worker is incapacitated long term, there is a threshold time period where benefits cease. See below table for Queensland and other states.
State Rate Threshold
QLD
After 2 years Permanent Impairment (PI) % test to determine pay rate. Max 5 years
NSW At 130 weeks – benefits continue if off work. Max 5 years
SA At 2 years – If PI% >30% then continue to retirement age. Otherwise benefits cease.
VIC Benefits continue to retirement age
WA Benefits can continue until Statutory Maximum is reached.
When a worker sustains an injury and a time lost claim for either total or partial incapacity is accepted, the employer excess is determined by WorkCover. This excess is paid by the employer to the injured worker.
Workers’ Compensation and Rehabilitation Act 2003
Section 65 What is the excess period
Workers’ Compensation and Rehabilitation Act 2003
Section 66 Employer’s liability for excess period
A permanent impairment is when your injury stays the same over time and isn’t likely to improve with further rehabilitation or treatment and has led to a:
• Loss of effective use of a part of your body
• Loss of part of your body
• Psychological or psychiatric incapacity.
When an injury has reached stable and stationary an independent assessment will be arranged and the doctor will assess the level of permanent impairment. From the doctor’s report the degree of permanent impairment (DPI) will be calculated and a lump sum offer made.
Stable and stationary is reached when the examining doctor is of the opinion (i.e. it’s an opinion based statement in that another doctor may disagree) that the injury has reached maximum medical improvement and any further treatment is unlikely going to benefit the injury.
1) Once the injury has been medically deemed to have reached a stable & stationary state, the worker’s degree of permanent impairment must be assessed by a doctor (or the medical assessment tribunal for psychological/psychiatric injuries or audiologist for industrial deafness) in accordance with the Queensland Guidelines for Evaluation of Permanent Impairment 2nd edition
Please note that depending on the date of injury it may be necessary to refer to the relevant legislation for that period.
2) The medical specialists are guided by the Table of Injuries to determine the correct percentage of permanent impairment for the injury, which then equates to a monetary lump sum payout of compensation to the worker - provided they wish to accept that permanent impairment percentage.
Each year in Australia there are over 100,000 workers’ compensation claims for serious (see below) workplace injuries. These injuries have a significant impact on the lives of Australian workers with the social and financial costs being borne by the worker, employer and community. When a workplace injury occurs, the overarching goal is for the worker to return to their pre-injury lifestyle as far as possible. Support is provided from the employer, families, treatment providers, insurer and in some circumstances a workplace rehabilitation provider.
The Workplace Rehabilitation Provider is engaged to provide expert services when additional assistance to support the workers’ return to work is needed. The services of a Workplace Rehabilitation Provider are used to identify and address any risk factors which may impact a successful return to work, to translates functional gains into meaningful work, and provide evidenced-based advice on the best pathway to recovery and return to work. At times a Workplace Rehabilitation Provider may also be engaged to assist with non work related goals or work readiness activities.
A Workplace Rehabilitation Provider will engage with the treating provider(s) and help inform treatment plans, providing insights into the working environment that enable work to be used as therapy.
These Principles of Practice for Workplace Rehabilitation Providers (the principles) guide expectations of quality service delivery. The principles align with the evidence base that good work is a determinant of health. Research shows that good work is not only good for health and wellbeing but that long-term absence from work has a negative impact on physical and mental health. The evidence also supports the value of work as part of recovery and not just as the end goal of rehabilitation.
In this way, the services of a Workplace Rehabilitation Provider are designed to promote and realise the health benefits of good work with early alignment of treatment goals with return to work goals. Supporting a worker to be at work in some capacity provides the best chance of a good outcome following their work injury. The longer someone is off work, the likelihood of returning to work diminishes. Therefore, acting early to assess needs, establish and build work capacity, identify suitable work and set meaningful goals are essential to the workers’ successful recovery.
At the beginning of this course the health benefits of good work were introduced by looking at the Charter of Principles, founded by the Australasian Faculty of Occupational and Environmental Medicine (AFOEM) within the Royal Australasian College of Physicians (RACP). We now look at the health benefits in more detail.
Items found to have a high impact on individual beliefs include:
• Improved ‘personalisation’ of communications in order to increase the worker’s feelings of ownership = Empowerment.
• Consistent messaging to encourage recovery at work, and movement away from a focus on ‘injury management’.
• Encouragement of an active role in recovery, including setting RTW goals for themselves.
• Providing a timely recovery plan that promotes an early RTW.
• Choosing words wisely + using more sympathetic language shows understanding & recognition of the individual’s circumstances. This encourages a positive relationship between RRTWC or Supervisor (good rapport)...which can only increase the likelihood of positive outcomes.
• Important to educate injured individual about mental and physical health benefits that work offers.
[7] Office of Industrial Relations
A person centred approach refers to an individually tailored, holistic approach to meeting a person’s needs and recognizing the client as an active participant in the rehabilitation process.
In a return to work setting, the focus is on the person and what they can do at work. The focus is not on their condition or limitations at that time. The approach is to understand what the injured worker can achieve at work and not what they are not capable of. This approach should also take into account the individual goals of the worker in the rehabilitation process and consider their personal and unique needs and circumstances. This can include things such as personal health status, education and skills, and support structures in place eg family.
A person-centred approach:
• Supports the person, at the ‘centre of the service’, to be involved in making decisions about their life
• Takes into account each person’s life experience, age, gender, culture, heritage, language, beliefs and identity
• Requires flexible services and support to suit the person’s wishes and priorities
• Is strengths based, where people are acknowledged as the experts in their life with a focus on what they can do first, and any help they need second
• Includes the person’s support networks as partners
• Should support and enable a person to build and keep control over their life.
[16] New South Wales Health
Safe Work Australia has designed a health & safety handbook which contains ten principles of good work design as a result of their Australian Work Health and Safety Strategy.
The handbook is a guide to employers to ensure they design work practices to not only reduce workplace injury, but to allow workers to live more happy, healthy and productive lives at work.
The handbook should be used by those with a role in designing work and work processes. The ten principles are split into three sections:
• WHY good work design is important
• WHAT should be considered in good work design
• HOW good work is designed
The 10 principles are:
1) Good work design gives the highest level of protection so far as is reasonably practicable
2) Good work design enhances health and wellbeing
3) Good work design enhances business success and productivity
4) Good work design addresses physical, biomechanical, cognitive and psychosocial characteristics of
work, together with the needs and capabilities of the people involved
5) Good work design considers the business needs, context and work environment
6) Good work design is applied along the supply chain and across the operational lifecycle.
7) Engage decision makers and leaders
8) Actively involve the people who do the work, including those in the supply chain and networks
9) Identify hazards, assess and control risks, and seek continuous improvement
10) Learn from experts, evidence, and experience.
A Return to Work Plan is a goal setting statement which sets out how treatment, rehabilitation, claims management and employment practices are to be coordinated to achieve an overall safe and durable return to work for a specific injured worker. This plan is different to the Suitable Duties Program (which is part of the plan) and is developed in conjunction with the injured worker, the Insurer and the treating medical practitioner recommendations. It includes the goals to be achieved, the steps that are involved in achieving the goals and consideration to the time taken to reach them.
Some things a rehabilitation and return to work plan could include are:
• Personal details as well as the details of support persons and rehabilitation and the return to work coordinator
• The start and finish date of the suitable duties program
• Teturn to work goals
• Any ongoing medical treatment needed
• The ‘stages’ of return to work as recommended by the doctor
• Physical and psychological capacity to perform tasks/duties
• Specific work tasks/duties to be avoided
• Any other changes in the workplace that are required to support an injured worker
• A date for review of the plan.
The [9] Guidelines for standard for rehabilitation provides further understanding on the requirements for a rehabilitation and return to work plan as noted in Principle 3 below.
The insurer’s responsibility is to take the steps it considers practicable to coordinate the development and maintenance of a rehabilitation and return to work plan in consultation with the injured worker, the worker’s employer and treating registered persons.
Actions taken in accordance with a rehabilitation and return to work plan must be reviewed and evaluated at regular intervals as the worker’s rehabilitation progresses. If an employer has concerns with implementing a proposed action these concerns should be resolved as a priority and not cause delay.
The employer has a vital coordinating role in managing workplace issues such as informing managers, supervisors and co-workers of the existence of a rehabilitation and return to work plan. It is important for a successful rehabilitation and return to work plan that individual roles at the workplace are clearly defined so suitable duties programs are implemented effectively.
Returning injured workers to the workforce can be a challenging role for an employer and requires coordination and problem solving skills as each worker’s path to recovery is different. Each worker will approach rehabilitation from a different perspective and will require various levels of support from the employer.
Every worker who is participating in a rehabilitation and return to work plan needs to be treated with respect and equity. It is also important that the injured worker’s supervisor and co-workers are informed of arrangements so that all parties involved at the workplace are engaged in assisting the workers’ safe return to work. If co-workers or others are disadvantaged or are ill informed it can lead to resentment towards the returning worker.

[7] Office of Industrial Relations
Recovery has a psychological element.
Ultimately all recovery has a psychological element, even for physical injuries. How adaptable we are to changes in our lives will govern how we deal with a workplace injury. We all have a values system, on which our beliefs and tolerances lie.
It is estimated that in 75% of cases, psychosocial factors such as a person’s lifestyle & social circumstances are the dominant barriers to successful return to work.
How adaptable we are to changes in our lives will govern how we deal with a workplace injury.
Promote recovery by explaining the following to the injured person:
• Confirm the doctor’s findings and ensure that the worker understands their diagnosis and where to find more information if they are unsure.
• Acknowledge the worker’s experience of pain.
• Clarify that imaging is not always required and the worker should consult with their treating practitioner if they have concerns about examinations required.
• Sometimes movement can promote a quicker recovery - the work capacity certificate will outline the safe range of activity for a worker while they recover. [10] ACC
As a rehabilitation and return to work coordinator, you are obliged to:
• Act early
• Be sensitive
• Focus on opportunities for a return to work
• Talk to treating practitioner personally if necessary
• Provide suitable duties even if claim is pending
• Develop a clear and structured suitable duties plan in consultation with the injured worker
• Offer the suitable duties plan with clear expectations that they are temporary and what is expected
• Use the paper work as a tool to achieve the desired outcome and not a means to an end
• Involve the worker in all stages of return to work planning and ensure that they actively contribute to goal identification.
Return to work programs need to be planned in consultation with all stakeholders. This includes:
• The injured worker.
• The treating doctor/s - What type of work will they be able to do? What hours, shift or days of work will they be able to do?
• The insurer and rehabilitation provider.
• Any other health professionals (such as physiotherapists) - consultation with health professionals and the rehabilitation provider is necessary to determine the injured worker’s capabilities.
• The worker’s manager or supervisor - consultation with the worker and their supervisor or manager is necessary to the worker’s existing skills, interest and knowledge and their current job role. Are they good at a skill outside of work that could be utilised for suitable duties?
It is often likely that the injured worker will not be able to perform their normal duties and will need suitable/alternate duties. The development of these suitable duties requires effective consultation between all parties to be successful.
This is one of the reasons that you need to liaise with the health professionals in order to estimate the length of time that the worker will be absent during the initial phase.
You will need to consult with the work team supervisor or manager, and assist with making arrangements to cover the fact that the worker is absent. They may need to work shorter days/hours/ shifts or be placed on different duties in a different department.
Discussion with health professionals and the worker’s supervisor should occur as early as possible, so that there is time to plan for a successful return to work, both from the point of view of the worker and from the point of view of the organisation.
Considerations during suitable duties development include:
• The medical restrictions and recommendations provided by the treating doctor.
• The psychological stress for the injured worker, due to the pressure of returning to work, feelings of shame, guilt, or feeling a burden/failure.
• The impact of the injury - fatigue/moodiness from pain & lack of sleep, side effects from medication, frustration from not being able to move around, drive, loss of independence.
• Financial Stress from reduced income whilst on workers’ compensation payments.
• Whether they can perform limited duties in their normal position or whether they need to be given different duties during the rehabilitation period.
• The specific tasks that the worker will need to perform and ensuring that they do not aggravate the injury.
• Any special equipment or aids which may assist the worker to perform duties, or any medical equipment that they may need to use in the workplace.
• Job re-design to suit the injured worker’s condition and needs - make modifications to their daily tasks.
Keep everyone who is supporting the return to work program updated and aware of what the next steps are.
Prepare the injured workers co-workers whilst still maintaining a level of confidentiality. Let them know what the facts are, what the process and plan is, and what their part is. Ask them to be supportive & tell them how they can do this.
Set up for success! If all the key players and influencer’s are not on board or not sure what the goal is then a successful return to work will be more difficult.
This form should explain:
1) The role of the Rehabilitation & Return to Work Coordinator (RRTWC)
2) How the RRTWC will help the injured worker
3) How the suitable duties program will be developed, in conjunction with treating doctor’s approval.
4) Confidentiality of information collected
5) Benefits to injured worker of signing the consent for RRTWC to speak to treatment providers.
6) That a worker can withdraw their consent at any time (in conformance with the WCRS performance standards)
If an injured worker signs an authorisation form it allows the rehabilitation and return to work coordinator (RRTWC) to:
• Be the professional link between the workplace & the medical treatment providers to ensure the claim run smoothly for the injured worker
• Liaise with the treating Doctors & Specialists to discuss safe return to work options that will benefit the injured worker’s rehabilitation
• Get the highest quality care for the injured worker by discussing the injury with all treatment providers eg. Occupational Therapist, Hand Therapist, Physiotherapist, Exercise Physiologist etc.
• Make sure appointments are coordinated so there is a smooth transition for the injured worker throughout the whole process and help with any road blocks
• Advocate for the injured worker in the workplace or with Insurer to get the best outcomes.
The RRTWC’s actions are always guided by the injured worker’s Doctor & treatment providers.
1) Prepare a standard introduction letter to doctor, asking for their cooperation with RTW. The injured worker can give this to the treating doctor at their first appointment for the injury.
2) Send the treating medical practitioner (TMP) the injured worker’s signed authority.
3) Use pre-designed lists of suitable duties available at the workplace. Easy & quick for doctor to read – tick / flick & sign
4) All information requested should be based on being used “for Rehabilitation & RTW purposes”.
5) Build rapport with regular medical centres / GP’s / Specialists. Explore the option of case conferencing with all stakeholders to ensure effective return to work discussions.
6) If there is no consent from the injured worker – you can still contact TMP to advise them of what you know about the case or the injured worker’s conduct / lack of participation etc – just advise upfront you have no consent from their patient, however you would like to give them some information so they are more in the picture. Most all doctors are very appreciative of what the other side of the story is, apart from what the injured worker is telling them.
The following people are commonly included in the rehabilitation plan for the injured worker.
• Medical practitioners
• Occupational Therapists
• Physiotherapists
• Chiropractors
• Psychologists
• Pain Specialist
• Injury Management Specialists
• Counsellors
• Dieticians.
The definition of a registered person under the Act is noted in the Schedule 6, Dictionary.
• Peer Support Officer in work area
• Senior Human Services Officer options
• Employee Assistance Programs - if funded by employer. Worker can have set number of sessions with a registered psychologist or psychiatrist.
• Lifeline/Beyond Blue
• The Workers’ Psychological Support Service - which is available to any worker who has a workers’ compensation claim and can connect workers with available community support programs.
There are a range of services available to assist an injured worker to return to work safely and effectively. These services will help understand an injured workers’ capacity for not just physical work capacity but also assist with understanding work skills and abilities, psychological factors, work style, work history and understanding labour opportunities.
The Job task Analysis (JTA) is a risk management tool that provides a baseline for job tasks in specific roles. It allows an understanding of the baseline physical, cognitive and environmental demands associated for each job role within an organisation. Hazards can be identified and strategies can be implemented to minimise risk to workers required to perform these roles. Results can also assist the design of pre-employment assessment tools to determine the suitability of workers for a specific role.
In a return to work setting, a Job Task Analysis is an important tool in minimising the risk when designing suitable duties. Understanding of the demands of a work role and mapping these against the capacity of the worker (as provided in the Work Capacity Certificate) can result in more appropriate duties being assigned for the worker, and therefore promoting the performance of suitable duties. JTA’s assist in developing a safer work environment, reducing the risk of further injury or exacerbation of injury.
Traditionally an allied health professional undertakes a Job task Analysis by observing a worker complete their job tasks by paying attention to the demands and assessing the potential risks within the scope of work. Valuable information can also be gathered by workers, supervisors, safety practitioners, RRTWC’s and others to assist in the development of a JTA.
In summary, the benefits of a Job Task Analysis include -
• Improved design and implementation of graduated return to work plans
• Elimination of harmful tasks for the injured worker
• Improved communication between all stakeholders
• Improved satisfaction with the duties prescribed
• Confidence in the selection of the tasks being appropriate and trust in the Suitable Duties Program by all stakeholders
• Improved understanding of employees competency to perform alternate duties or training needs for these alternate duties
• Improved sustainability in the return to work
• Improved productivity while on a Suitable Duties Program
Is an assessment containing a series of tests to determine a worker’s physical ability to meet the functional demands associated with their pre-injury role, thus, assisting them with their recovery and or return to work.
These evaluations match the worker’s physical abilities to the critical demands of the job requirements that are needed to be met.
These evaluations cover a wide range of tests including but not limited to:
• History
• Current medical concerns
• Discussion of work demands (review of Job Task Analysis if available)
• Medical history reviewed and summarised
• Objective functional testing including lifting, carrying, pushing, pulling, kneeling, squatting, gripping, reaching, bending, walking, standing
• Job specific tasks simulated during the assessment
• Outline of current functional abilities demonstrated during the assessment
• Opinion and recommendations on the workers’ ability to perform the pre-injury duties as outlined in Job Task Analysis / or as reported if task analysis not available.
By conducting a functional capacity evaluation on an injured worker, both the company and the worker will be provided with a clear and defined plan with regards to the injured worker’s safe re-integration back into the workforce.
If a work based FCE is performed, the worker is requested to demonstrate their capacity to perform their usual duties and/or tasks, so that an opinion can be made regarding their safety if they were to return to pre-injury duties.
In certain instances, the worker may also be requested to demonstrate their capacity to perform alternate or suitable duties available within the workplace, thus allowing recommendations to be formulated with respect to the workers return to work if deemed to be unsafe to return to pre-injury duties.
Clinic based FCE’s attempt to replicate an individuals’ pre-injury job demands by simulating their pre- injury duties within one of KINNECT’s clinics. The worker is requested to demonstrate the capacity to perform certain tasks, with the weights, dynamic and positional tolerances tested based on the individuals’ position description or Job Task Analysis.
In the event that either documents are available, KINNECT attempt to reproduce the critical functional demands through subjective reports from both the Employer and worker so as to provide an objective opinion regarding the workers’ capacity to return to work, necessary restrictions and future rehabilitation needs.
By focusing on the current functional ability of the worker while rehabilitating from an injury, suitable duties can be identified reducing the risk of aggravation or re-injury.
A Functional Capacity Evaluation can be used in the following situations to determine:
• The workers’ safety to perform their current role or new role
• Capacity for full duties before receiving a full medical clearance
• Current capacity for suitable duties following an injury/illness.
A Vocational Assessment is a comprehensive evaluation of an individual’s transferrable skills, qualifications and interests, to identify potential future employment and/or training options, whereby a physical or psychological injury prevents the individual from returning to their previous employment.
When should a vocational assessment be used?
A vocational assessment should be used when a worker is unable to return to their:
1) Employer or role due to a physical or psychological injury or illness
2) Role due to an injury or illness, however the employer may have alternative roles within the workplace
3) Employer or role because of being made redundant (outplacement services).
What is the goal of a vocational assessment?
The ultimate outcome of a Vocational Assessment is to identify suitable employment options and to set realistic vocational goals so that an injured employee can return to long term, meaningful and fulfilling employment in a timely manner.
What is included in a vocational assessment?
A transferable Skills Assessment , which includes a(n):
• Review of injury history, current treatment, current functional and/or psychological capacity
• Review of previous employment and training history
• Review of skills, qualifications and accreditations
• Review of literacy, numeracy and computer skills
• Discussion and identification of realistic employment and training options / interests (an interest test may be completed if required, to help the worker to identify alternative work areas of interest)
• Review of current level of job seeking ability / skills
• Review of psychosocial barriers and an analysis of the workers’ motivation with respect to a return to work within a new employment
• Consideration of internal redeployment roles may be considered within the current workplace (if available)
• Aptitude testing and analysis of results.
Labour Market Research , which includes:
• Identification and description of the requirements for a chosen vocational option
• Review of local available positions
• Discussion and analysis of wage requirements
• Analysis of local training availability for identified vocational options
• Contact with employers and/or review of advertised positions to confirm suitability of options.
Job Preparation & Job Seeking , which includes:
• Preparing an individual to search for employment independently
• Assistance with job applications
• Ongoing monitoring of job seeking and vocational counselling as required.
Detailed Report & Communication , which includes:
• A phone call to referrer on completion of Vocational Assessment providing update on the assessment findings and recommendations. The need for further assistance, such as Job Preparation Assistance, is also discussed.
• A comprehensive written report detailing all of the above information and providing clear recommendations regarding future assistance and/or needs, submitted within 48 hours of the assessment.
Independent Medical Examination / Assessment (IME or IMA)
• Independent medical specialist who examines the injured worker, does not treat them but simply reports back to Insurer or Agent as to their opinion of the injury situation.
• The Insurer or the Employer can refer the worker to a Independent Specialist for an IME.
• Used as a 2nd opinion when there seems to be little progress happening on the claim or return to work is difficult to progress.
• Can be used to assess Permanent Impairment or give an opinion on treatment suggested such as surgery.
• Most schemes have a clause stating the worker must attend otherwise benefits may be suspended –some are more stringent & effective than others.
Case conferences bring together the worker, the nominated treating doctor and other parties such as the insurer, the employer and workplace rehabilitation providers to discuss how to deliver the best possible return to work outcomes for the worker.
The Australasian Faculty of Occupational and Environmental Medicine has published a Vocational Rehabilitation Case Conferencing resource.
This publication supports the importance of case conferencing and certifying for capacity across disciplines as a way of bringing together the medical practitioner, employee, employer, the Insurer and rehabilitation providers.
It outlines the key features and participant roles of case conferencing, as well as how it differs from medical consultations.
The work capacity certificate is used in the determination and management of the claim by insurers. The work capacity certificate also acts as a communication tool between insurers, employers, rehabilitation and return to work coordinators, allied health providers, medical practitioners and nurse practitioners due to the information supplied in it.
The work capacity certificate promotes:
• An injured workers ability and focuses on what they can do
• Early return to work
• Rehabilitation and provision of suitable duties
• Health benefits of good work.
“Work Capacity Certificate” is required to be current for the duration of the claim.
A certificate of capacity includes:
• Worker’s Name / DOB / details
• Date of injury or first seen
• Diagnosis (pain is not a diagnosis) and if Doctor considers the injury to be work related
• Treatment period (No gaps) / Treatment recommended / Referrals
• Level of capacity for work / Period able to RTW on suitable duties – if applicable
• Physical function / other functional considerations of injured worker
• Doctor’s signature & dated & practice details.
The Work Capacity Certificate is a critical document in the return to work process and is the basis on which to design appropriate suitable duties. It helps understand the work capacity of the injured worker, the likely progression of the duties over time and the treatments required to assist recovery.
Workers’ Compensation and Rehabilitation Act 2003
Section 42 Meaning of suitable duties
Suitable duties , in relation to a worker, are work duties for which the worker is suited having regard to the following matters—
(a) the nature of the worker’s incapacity and pre-injury employment;
(b) relevant medical information;
(c) the rehabilitation and return to work plan for the worker as developed under section 220(5);
(d) the provisions of the employer’s workplace rehabilitation policy and procedures;
(e) the worker’s age, education, skills and work experience;
(f) if duties are available at a location (the other location) other than the location in which the worker was injured—whether it is reasonable to expect the worker to attend the other location;
(g) any other relevant matters.
Basics
The purpose of suitable duties is to keep the employee in the workplace and help the injured worker develop or maintain feelings of self-worth while accomplishing tasks and to improve or maintain work capacity. During this time colleagues will recognise the injured worker’s contribution to work activities while rehabilitating from injury. It is important, however, to offer meaningful duties in which the injured worker can adequately utilise their skills. It will help them remain motivated, add to a positive work morale and better recovery. It is important to take into consideration the worker’s skills, abilities and experience.
A suitable duties program may involve a number of alterations to the injured worker’s work day to successfully assist them in returning to work. Ideas can be limitless, so long as they are:
• Designed in consultation with the injured worker
• Adhering to the worker’s level of capacity as detailed in the current work capacity certificate - if unsure consult the doctor to seek approval that the duties identified will not cause further harm to the worker
• Approved or at least discussed with any treating allied health professionals
• Safe by the employer’s WHS standards.
Suitable Duties Programs should be goal focused. Primarily the goal is a return to pre-injury duties, however in some complex cases initially the goal may be something different like increasing hours from 2 to 4 per day or introducing a new activity. With complex cases allied health providers may be engaged as early as possible as they can be instrumental in reducing the injured worker’s fears regarding returning to work.
Suitable Duties Program should always set date periods and time limits on days/hours to be worked. The RRTWC should regularly check-in with the injured worker and supervisor to monitor the progress or struggles they are having with the SDP. Ideally, the SDP time periods should coincide with the doctor’s review appointments, so it can be reviewed and updated with the latest information from the treating doctor.
There may be other options available such as reduced hours or days, different shifts, alternative duties in different departments or areas of the workplace, working from home, or working at a host employer who has more suitable work duties for an interim period. Job redesign is also important to consider.
External training or short courses could be an option, supervisory duties of young workers, updating of policies/procedures or stocktaking could be useful.
Workers may have skills or talents which are completely different to their day job but could be used to help the business, for eg. a dozer operator may be good at graphic art and can assist with an advertising project.
Employers should be open to all options to be able to assist an injured worker back to meaningful work.
If medically approved, it is important to ensure the duties or hours/days on the SDP are regularly upgraded to allow the injured workers to feel and see progress in their recovery.
Workers are generally not allowed to upgrade their hours past their normal weekly hours whilst on a SDP. If an injured worker wants to increase their hours to perform overtime whilst on a SDP you should consult their treating doctor and also discuss this with the insurer (claims officer) to determine if this is a safe option for the worker.
• Use current work capacity certificate - workers’ compensation from treating doctor and/or current medical report from IME or treating.
• A Job Task Analysis developed on site by an allied health professional, such as an Occupational Therapist, can assist determining work tasks suitable for the injured worker.
• Ask the injured worker.
• Understand the injured worker’s key strengths or skills. Do they have skills you were unaware of?
• Look for neglected or incomplete projects that are within the current skill set and ability of the worker. E.g. calling customers for surveys, updating or reviewing procedures, stock take?
• Skills training. This could mean working from home or training off-site.
• Buddy up supervision roles in the workplace.
• Host employment – internal and external.
Keep in mind that the suitable duties program always lists the contact details of the injured worker, employer, treating medical professional, and case manager and rehab and return to work coordinator’s contact details. It is recommended that all parties need to sign off on the program before it can be implemented, especially the injured worker as a sign of commitment to the recovery plan. However, it may not be required for simple suitable duties programs to avoid causing unnecessary delay to a worker being able to commence suitable duties if excessive approvals are being sought. The ideal order of sign off is:
1) The treating doctor (injured worker needs to see this is approved by their doctor)
2) The injured worker and supervisor (secure commitment to the process)
3) RRTWC and other parties (mentor and oversee plan implementation).
Keep a record of the suitable duties program, signed by all parties as this could be important later in the claim. Also, be sure to always provide a copy to the Insurer.
Ensure Payroll are regularly updated on changes to hours whilst the injured worker is on a SDP. If the injured worker is only working partial hours each week, then either the RRTWC or Payroll is required to send a Partial Incapacity Form each fortnight to WorkCover/Insurer in order for them to pay ‘top up’ wages for that period. Payroll will also require a copy of the current medical certificate.
You will always be following the guidelines set by the treating practitioners but some basic understanding of anatomy can help identify appropriate duties and assist in the timely implementation of the plan.
Before we can design a suitable duties program for injured workers, it is helpful to have a basic understanding of certain injuries in order to develop the most appropriate plan. Knowing some basic principles helps in the design phase of duties so more appropriate tasks are assigned. You will be guided by the relevant treating practitioners in this area as well but a little understanding helps in the preparation and planning stage, and hopefully a safer and earlier return to work activities.
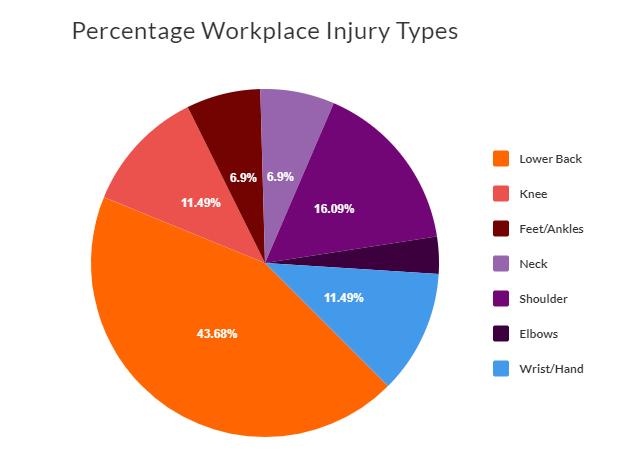
Across the scheme almost half of all workplace injuries are to the spine.
The spine is made up of bones (vertebrae), discs, muscles and nerves forming the ‘backbone’ of the body.
While the vertebrae and discs allow for shock absorption, the muscles and nerves help us remain upright and can also move our torso in various directions. The spine has three curves – the cervical, thoracic and lumbar. When the spine is in a ‘neutral’ position, we are in a strong, safe and efficient posture in which the muscles have to work the least amount. If our spine is not in a neutral position – for example when we bend forward - forces placed on our body increase and can cause pain and damage.

Between each vertebra lies a disc which absorbs the pressure. The spinal curvature plays an important role for disc loading. In an upright posture, pressure is evenly distributed across the surfaces of the discs, however, when bending forward, the discs are compressed at their front edges. Repetitive bent postures can lead to the outer edges of the discs to rupture or ‘bulge’ and press against the spinal cord, causing pain.
In different postures and with various movements, the pressure on our spine changes. This is outlined in the table below. For example, when bending forward, the pressure on our spine increases by 260%!
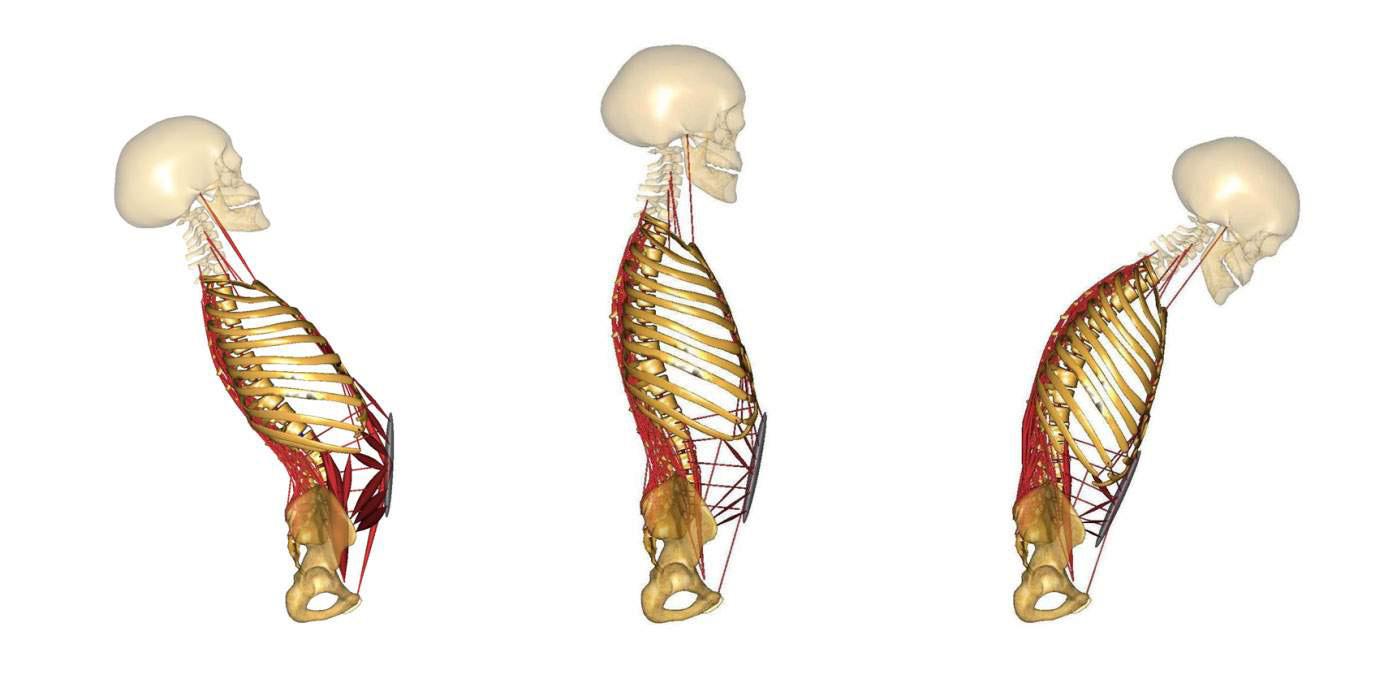
One of the largest muscle groups in the back are the erector spinae that support the trunk. When the muscles in the back are active, they add pressure to the discs. A little pressure is good as it increases the blood flow to the discs, supplying them with nutrients. So ideally, changing postures is good as both muscles and discs may experience alternations in loading and relaxation.
However, if the muscles are repetitively used (especially when we are in an incorrect posture), these muscles and their tendons (attachment points to bones) can strain. This means small tears form and can get inflamed, causing pain, swelling and restricted movement. This can happen in any muscle in the body, but most commonly occur in the wrist, elbow and shoulder joints.
Repetitive strain injuries (also known as overuse injuries) often occur due to:
• Working in a prolonged position for extended periods of time
• Working at a high repetition workplace that does not provide time away from continuous use of equipment (mousing, keyboarding, using tweezers, and sewing, etc.).
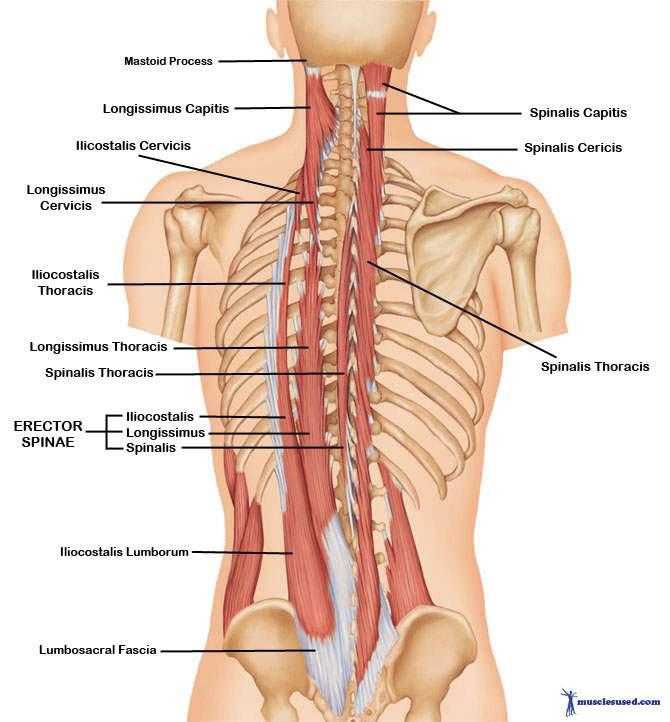
The second most common workplace injuries are to the shoulder (14%)! These often occur due to slips, trips and falls, and through repetitive movements. Poor posture is often a precursor for a shoulder injury, too! Because the shoulder is the most mobile of all joints (i.e. greatest range of movement) it is therefore the least stable.
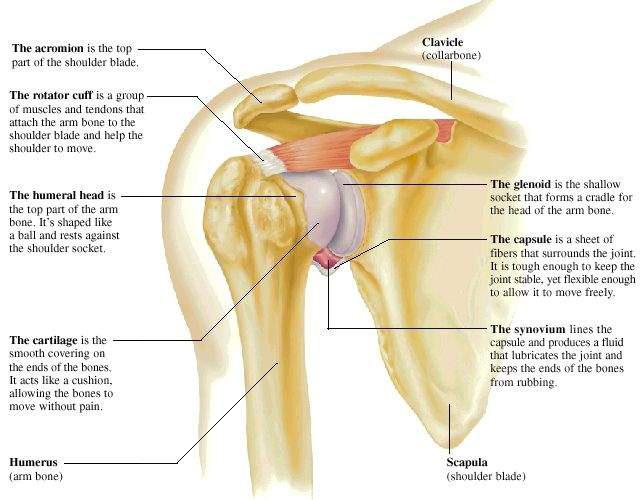
The strongest shoulder position is when the elbow is closest to the body. Extended reaching and overhead lifting can be very challenging in shoulder rehabilitation.
Contrary to the shoulder, the knee joint is a very stable joint as it is supported through large muscle groups, numerous ligaments and cartilages (menisci) which absorb shock from our movements. Injuries to the knee often occur due to sudden twisting movements or from a blow to the knee, for example when we trip or fall. Most commonly, the meniscus or the ligaments in the knee tear.
Both ligaments and cartilage (i.e. meniscus or discs in spine) are not very well supplied by blood. Therefore, the healing process is much longer than for strains of muscles and tendons.
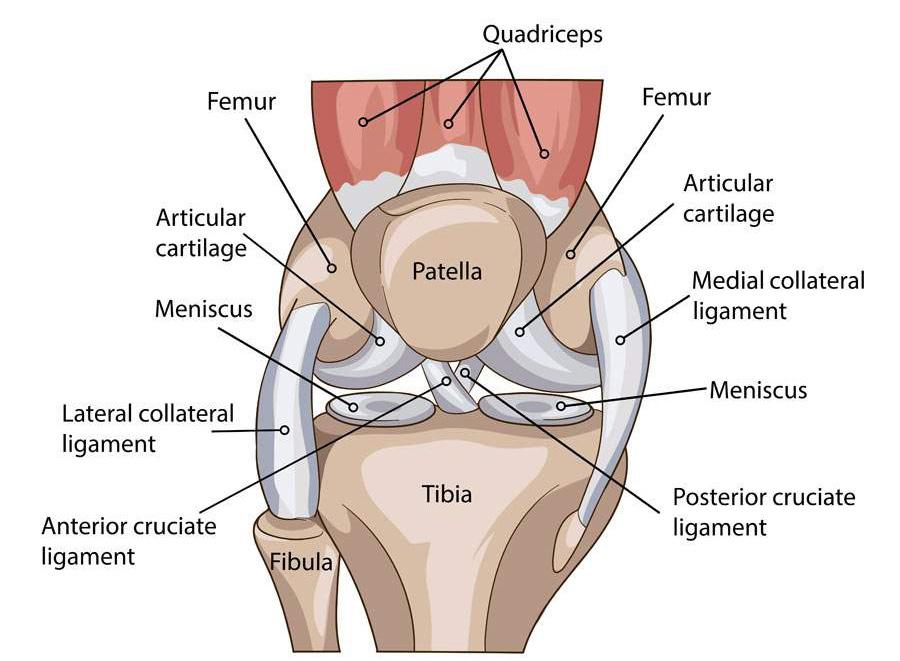
In the previous section you gained some introductory knowledge of the anatomy and physiology of the most commonly injured body parts. Now let us have a look at some of the main considerations in suitable duty design for back, shoulder, knee and repetitive strain injuries.
Please be mindful to always consult with the treating medical professionals when designing a suitable duties programs.
Always encourage a neutral spine position both when sitting and standing – remember, in a neutral position there is the least amount of pressure on our discs and our body can move most efficiently in this posture.
• The worker should avoid bending forward or backward too far. Most activities can be achieved (and maintaining a neutral spine) by bending the knees (e.g. squat or knight’s kneel) when working at lower levels, and by making use of safety steps when working at high levels (to avoid overreaching and hence arching the back too much).
• Twisting movements can be avoided by keeping the ‘nose over toes’.
• Work at extremely high or low levels should be avoided.
• Alternating between sitting and standing duties on a regular basis is encouraged as it allows certain muscle groups to rest.

Always encourage good posture, meaning the shoulders are rolled back, the chest proud, and upper arms in neutral (e.g. not overhead or flaring out to the sides - see below).
When possible keep the arms close to the waist to avoid overreaching. If the worker has to perform work above shoulder height, s/he should make use of safety steps to avoid overreaching, and do so for short periods only.

As with back injuries, twisting should be avoided at all times. This can be achieved by moving the foot with your body (‘Nose over toes’).
Deep squatting, climbing and kneeling for extended periods of time are not generally recommended.
Ensure alternation of tasks is given to reduce constant pressure on the knee (i.e. consider seated duties where appropriate).

Provide micro-breaks of 2-3 minutes as needed to maintain comfort.
Provide task alternation (including duties outside of the normal work station if required).
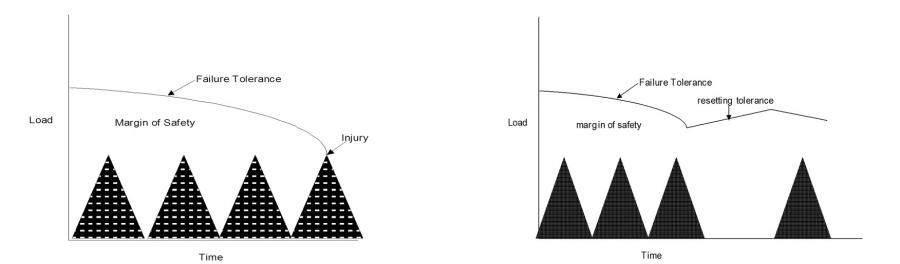
Ensure the worker is self-paced in their duties and not working to KPI’s, as rushing can encourage poor movement patterns.
Include Micro-breaks in your plan to avoid injury aggravation. Hourly breaks (2-5 minutes) to complete exercises and stretches as prescribed by the Physio/ Health Professional are generally beneficial.
Always adhere to restrictions outlined on the medical certificate (i.e. no lifting, squatting, twisting, bending) to avoid the risk of re-injury.
Include further recommendations for the injured worker, such as:
• Education on posture (i.e. Avoid twisting of the back and knees by keeping ‘Nose over toes’)
• Use of regular micro-breaks to avoid injury aggravation
• To contact their RRTWC and supervisor should there be any questions or concerns.
When designing suitable duties plans, there are a couple of other factors to take into consideration. Keep in mind that many injured workers have had some time off work and rested either in hospital and/ or at home. Their bodies and minds are therefore deconditioned, and returning to work can be stressful – both for the mind and body. The worker will have to get used to being on their feet again.
We therefore recommend a graduated return to work plan:
• Return to work at reduced hours and days (i.e. Mon-Wed-Fri, 8am-12pm).
• Gradual increase of hours and days till full recovery/ cleared by treating doctor.
• Conditioning and rest days/periods are important for the recovery (i.e. avoiding aggravation of injury).
Psychosocial flags allow us to identify aspects of the person, their problem and their social context, and how those factors affect the recovery and return-to-work process.
1) The concept was introduced in 1997 by Kendall et al and looked at factors that identified patients who were at risk of developing chronic disability, and did not recover as was expected for their condition.
2) Psychosocial flags enable us to work from a biopsychosocial model and give a framework for assessment and planning.
3) These flags are not a diagnosis or a symptom, but an indication that someone may not recover as expected and may need additional support to return to work.
4) These flags are often referred to as obstacles to recovery.
5) Psychosocial factors determine outcomes such as activity levels, participation and work but appear to be less relevant to the reporting of symptoms.
“Flags” are used to alert us to something about a person or their problem that may be an “obstacle to recovery”.
Below is a table with some examples of a flag colour, the nature of the flag and examples of clinical signs to look for on assessment.
Red Signs of serious pathology
Cauda equina syndrome, fracture, tumour, unremitting night pain, sudden weight loss of 10 pounds over 3 months, bladder & bowel incontinence, previous history of cancer, saddle anaesthesia.
Orange Psychiatric symptoms
Yellow Beliefs, appraisals and judgements
Emotional Responses
Pain behaviour (including pain and coping strategies)
Blue Perceptions about the relationship between work and health
Black System or contextual obstacles
Clinical depression, personality disorder
Unhelpful beliefs about pain: indication of injury as uncontrollable or likely to worsen. Expectations of poor treatment outcome, delayed return to work.
Distress not meeting criteria for diagnosis of mental disorder. Worry, fears, anxiety.
Avoidance of activities due to expectations of pain and possible reinjury. Over-reliance on passive treatments.
Belief that work is too onerous and likely to cause further injury. Belief that workplace supervisor and workmates are unsupportive.
Legislation restricting options for return to work, Conflict with insurance staff over injury claim. Overly solicitous family and health care providers. Heavy work, with little opportunity to modify duties.
The following can impact our capacity to deal with stressors:
1) Our psychosocial environment is interaction of various sources of stress in our lives & how we respond to them, both individually & as communities.
2) Our psychosocial environment includes our responses to stressors in our lives, from temporary ones such as a traffic jam to major stressors such as war, homelessness or major disease.
3) Our relationships with family members, friends, colleagues and other individuals and groups with whom we interact in our communities are an important part of this environment.
Nurturing, supportive relationships allow us to better access all our innate resources to respond to stress in positive ways.
Why Such Poor Treatment Outcomes from the Workers’ Compensation System?
People with workplace psychological injury treated via the workers compensation system typically have worse outcomes than those who are not treated via the workers compensation system. [13]
• Keep the employee engaged with the workplace and co-workers during recovery.
• Check for the presence of psychosocial factors and seek help to address them according to the particular circumstances of the employee and organisation.
The majority of psychological injury claims may be prevented through better management practices and a focus on well-being. It is estimated that 60% of claims may be prevented by:
• Improved Morale
• Work team climate
• Supportive leadership
Note: Develop supportive leadership capability across all levels of management and increased accountability for people-related outcomes (eg. performance appraisals, leadership KPls climate surveys, feedback).
Foster supportive engaging work team climates:
• Facilitate staff discussion and professional debate to address operational challenges
• Increase the level of informal and development oriented feedback
• Proactively clarify values and behavioural expectations
• Empower representative staff project teams to drive organisational improvement initiatives
• Use high quality measurement (eg reliable and valid employee opinion surveys) to identify potential organisational ‘hot spots
• Identify and respond to early warning signs (eg counterproductive and withdrawal behaviours).
[13] P. Cotton
In general, long-term disability relates more to individual and work-related biopsychosocial factors than either the physical demands of work or medical concern i.e. if it was the injury alone, the recover at work process would be easy and probably not need our help!
These factors include a person’s:
• Beliefs about their musculoskeletal condition and pain
• Family situation
• Job satisfaction and attitude to work
Addressing such factors can positively influence outcomes such as pain, disability and sick leave.
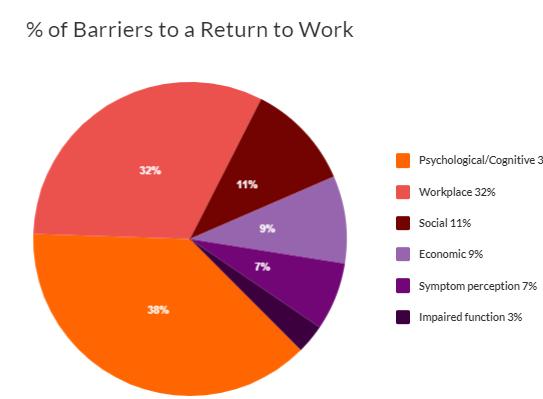
• Catastrophising
• Low self efficacy
• Belief “stress” is a casual factor
• Minimal health literacy
• False beliefs
• Self monitoring of symptoms
• Fear of pain / reinjury
• Job satisfaction
• Issues with claim lodgement
• Lack of employer support / communication
• Unsafe workplace practices
• Workplace culture
• Conflict within the workplace
• Blaming the workplace for the injury
• Alternate sources of income / support
• Legal action / payout expectations
• Single parents / unstable relationship
• An unhelpful family approach (doing everything for the worker or no assistance at all)
• Rented or social housing
• “Victim” of modern society
• Ask all relevant stake holders what they feel are the barriers to RTW
○ If it doesn’t make sense it is often because we aren’t asking the right questions. Ask all stakeholders regarding their concerns to identify their real or perceived barriers to return to work.
○ Utilise skills in negotiation and influence to resolve barriers
○ Provide evidence and rational to insurers on barriers to RTW and why they need to be resolved
• All involved parties must recognise and deal with the barriers as they appear
• Promote open communication between all stakeholders
• Provide workers with accurate and balanced information about their injury / condition and prognosis
• Promote the benefits of psychological treatment if psychosocial issues have been identified; can be more effective than biomedical treatment
• Build self efficacy; the belief in their ability to successfully achieve the desired outcome and avoid cognitive error; a negatively distorted belief about oneself or situation
Encourage Active Coping Strategies:
• Encourage continued functioning despite pain
• Come up with distractions; ways to distract thoughts of pain
Discourage Passive Coping Strategies:
• Dependence on others to ‘fix’ them
• Letting pain dictate and restrict activity
What the role of the rehabilitation and return to work coordinator involves
Assisting the organisation:
• Providing advice and assisting with the development of a workplace rehabilitation policy and procedure
• Managing the implementation of the plan
• Educating the workforce
• Maintaining and analysing data on injuries and rehabilitation programs
• Recommending improvements.
Assisting the injured worker:
• Communicating with the injured worker
• Ensuring the injured worker’s rights to privacy and non-discrimination are protected
• Working with all parties to document the RTW program
• Identifying suitable duties
• Being the central point of contact for all parties in relation to the RTW program
• Monitoring progress in treatment and the worker’s rehabilitation ensuring that appropriate resources are in place to support the worker
• Involve maintaining knowledge of locally based resources such as interpreters, community leaders etc.
• Maintaining and managing all confidential case notes and records.
Keep the employee engaged with the work environment as much as possible, particularly if there is delayed return-to-work.
Communicate and cooperate with the treatment provider
Respond quickly to any communication from the treatment provider - in particular, the initial approach. If the treatment provider does not contact you, make sure you initiate communication promptly.
When communicating with the treatment provider and employee, focus on:
• Open, clear communication
• A cooperative, team approach to the employee’s recovery and treatment goals
• Willingness to accommodate workplace changes as part of “reasonable adjustment”
• Gradual re-building of the employee’s self-management capability
• Acknowledge Psychosocial flags – progression limited if don’t acknowledge.
The absence of a worker for a period of time will have an impact upon their work team and work-in progress.
Provided below are some tips to help in achieving great return to work outcomes. Consider these tips in all your programs.
1) Assist with early claim lodgement to reduce financial and medical treatment delays.
2) Face-to-face communication with injured worker will yield better results.
3) Acknowledge and address early any issues the injured worker may be having in the return to work process.
4) Activity is an integral part of rehabilitation and should be prescribed; reinforce the importance of ‘doing’ to promote recovery over passive ‘pain relief only’ rehabilitation.
5) Provision of modified /alternate duties fosters return to work.
6) Ensure that key motivators to work are addressed and included in suitable duties programs to provide motivation.
7) Return to work is more likely to be successful when undertaken early; foster this when communicating with Doctors.
8) Long periods of worklessness should be discouraged; encourage proactive intervention, timely goals and a clear prognosis.
9) Address barriers as they arise with all key stakeholders.
10) People are best off when they return to productive work in a supportive environment.
11) Support employers to build their skills in effective communication to meet the needs of the worker.
12) Give the worker ownership of their suitable duties program by ensuring they are actively involved in the development.
13) Maintain active and meaningful communication during their suitable duties program.
14) Be at work with the worker on their first day back at work.
15) Be present at the worksite at least every 2 weeks.
16) Utilise positive psychology to focus on what the worker can do, not what they cant do.
17) Don’t focus on pain, instead focus on what they are able to achieve with pain.
18) Refrain from negative terminology or advice that may promote disability.
Injuries that did not happen at work:
• Non-work related injuries/illness can be managed in the same way.
• Early disclosure & treatment is best.
• Praise honesty & behaviour that is proactive.
• Injured employee needs to be honest & forthright with information.
• Encourage workers to tell someone!
• Don’t just come to work & make it worse.
• Culture is “we look after you here”.
• Employer should help where they can with SDP or may even pay for initial treatment.
• Most employers want to help their employees to remain healthy & happy so they are a productive workforce.
The injured worker will be performing duties that may be different from their normal job. They may:
• Be working shorter hours
• Have needed some training to take on a different role during their rehabilitation
• Have required special equipment or facilities to be provided by the employer
• Need time off work for treatment
• Have a reduced income from their work may be supplemented by workers compensation.
Suitable duties programs are not set & forget. It is important to closely monitor the injured worker’s progress, especially at the commencement of the program as that is when they will be the most uncomfortable and most apprehensive to the changes. Monitoring the suitable duties program is required so changes can be made to small problems rather than waiting for it to turn into a bigger issue for everyone.
The documented suitable duties program should include a clear schedule and responsibilities for overseeing and monitoring the program, including making modifications as necessary. These responsibilities may be part of your role, or you may have a supporting role in monitoring.
The progress of the suitable duties program needs to be documented in the injured worker’s case file – both for legislative reasons and in order to have a clear record in case there is any dispute, problem or breach. Accurate recording of progress and any issues that arise is absolutely essential. Case Notes should be documented in an objective way, without bias.
It is important to note that case notes could be subpoenaed and used in a court of law, and you may be required to be a witness in court as well. Ensure you write enough information to be able to remember correctly.
In order to monitor progress, you will need to actively seek feedback from all parties involved, record and evaluate the feedback received. This needs to happen on a regular basis – not just when something is brought to your attention. In the case of RTW, progress needs to be checked regularly.
This can be by a weekly telephone call or email – or if you can have a short face to face meeting this is preferable. Always document the outcome.
One of the main things you are looking for (and need to promote) is communication between the parties. You can act as a conduit for information and ensure that it is passed on. You can also encourage the parties to speak directly to one another.
If you are involved in monitoring the suitable duties program, you will need to ensure that there is open and transparent communication and cooperation between all parties – at the same time ensuring that the worker’s personal information and medical details are kept confidential. No personal or medical information should be communicated to any party without the written consent of the injured worker.
Case notes are used to report and document relevant events, communications and observations relating to a particular person, event or issue.
Case notes are a factual history and chronological recording of data relevant to an injury/illness. They can include details of:
• Information provided verbally to and from key stakeholders in the return to work process
• The progression of a rehabilitation process
• Participation and performance against return to work programs
• Communication.
Case notes supplement other records such as emails, suitable duties programs, medical certificates and may be called as evidence in any legal proceeding.
Case notes need to be:
• Objective
• Concise
• Accurate
• Relevant
• Precise
• Factual.
You write a case note after any contact related to the management of an injured worker with a workers’ compensation claim.
Contents
Case notes must be legible and provide sufficient detail to allow the reader to understand the point of the note, the reasons for any decision made, and how these fit in with the overall management of the case.
The following information needs to be included in a case note:
• the date of the contact
• the name and role of the person making the case note
• the manner and purpose of the contact
• a factual description of the event
• details of information provided verbally
• the purpose of, and reasons for, any decision or action taken in a Worker’s Compensation case
• details of the decision made, proposed action or action already taken in reference to a policy or procedure authorising the decision or action.
Case notes should contain the following information:
Information Received
Action taken
Reasons for Action/Decision
Expected Outcome
Decision Communicated
It is important that case notes:
Provide a brief summary of the information received or provided, and any impact on the process
Summarise any action/decision taken.
Document what your action/decision is and why you made this decision.
Specify the expected outcome of your action/decision.
Describe what method was used to communicate the action/ decision, eg email, in person.
• Only record facts eg behaviour observed and statements heard
• Record facts accurately and completely
• Label any ‘opinion’ as an opinion and not factual evidence
• Avoid metaphors or similes - just say what you mean directly
• Use clear, unambiguous, simple, concise language, including professional terminology if appropriate
• Highlight who is doing what in the process
• Are written in the third person.
Case notes should not:
• Include judgmental opinions, stereotypical comments, or any offensive statements
• Make comments that couldn’t be defended in a court of law
• Use slang or street language, clichés, or jargon
• Include sarcastic comments
• Include comment on details irrelevant to the worker’s participation in rehabilitation and return to work activities
• Use abbreviations unless these are in common use (for example, “eg”) or are previously defined.
14/02/2019 - Received a telephone call from Brian Smith. Brian advises that “he is not managing his suitable duties as he continues to experience an increase in pain in his shoulder”. Brian advises that “he is performing all duties required, however, notes that the amount of typing he needs to undertake seems to be increasing his pain”.
Discussed pacing and alternating duties with Brian, who admitted that he is not performing these activities to the full. Discussed why - Brian “advises he feels uncomfortable stopping work and how this might be seen; he also indicated that he has difficulty in remembering when to stop”.
Action:
It was agreed to meet with Brian and Peter Thimble (Supervisor) to discuss Brian’s progress and concerns. I also discussed installing a work pace system or similar system onto the computer to assist with time scheduling. Brian is to speak with his supervisor and confirm a date to meet by 16/02/2019.
Employers should implement best practice when it comes to maintaining privacy in the workplace. It is important for employers, employees and their representatives to know what information may be collected and retained by employers and whether it can be passed on to others. Best practice creates certainty and security for both employers and employees.
Privacy is the word we give to being able to keep certain information to ourselves and to control what happens to our personal information. It also refers to being able to do things without interference by others. Privacy issues can arise in all aspects of life.
Commonwealth privacy laws regulate the collection and handling of personal information through minimum privacy standards. These are known as the Australian Privacy Principles (APPs). The APPs apply to all private sector businesses with an annual turnover of more than $3 million, all private health service providers nationally, and a limited range of small businesses and all Australian government agencies. Although some small businesses are not required to abide by Commonwealth privacy laws, all businesses should aim to comply with the privacy principles as a matter of best practice.
For specific information about APPs visit the website of the Office of the Australian Information Commissioner at www.oaic.gov.au
[14] The Fair Work Ombudsman
Employers will have access to personal information about employees. This information may be sensitive and employees may wish to keep this information private. This means that employers will need to think about the way in which they collect, use and disclose information they obtain from their employees.
In many cases, Commonwealth privacy laws will not apply when it comes to employee records. Commonwealth privacy laws only apply to employee personal information if the information is used for something that is not directly related to the employment relationship between the employer and the employee. Nonetheless, best practice employers think carefully about any personal information that they have about their employees and treat that information in accordance with the privacy standards set out in the APPs.
It is good privacy practice for employers to tell employees when they collect their personal information. In doing so, the employer could tell the employee why they are collecting the information and who the employer might pass that information on to.
Best practice employers allow employees to access personal information about themselves which is held by their employer. Employees should also be able to have that information corrected or verified if it is incorrect, out of date or incomplete.
The Office of the Australian Information Commissioner’s website contains further information on good practice for organisations dealing with employees’ personal information. The guides deal with:
• Limiting the collection of information
• Providing notice to individuals about the potential collection, use and disclosure of personal information
• Disclosing personal information
• Keeping personal information accurate, complete and up-to-date
• Keeping personal information secure
• Providing access to personal information.
When can you give information to third parties?
[14] The Fair Work Ombudsman
For specific details and considerations on when personal information can be given to third parties we recommend you visit Fairwork Australia and the Office of the Australian Information Commissioner for the Australian Privacy Principles
Employers are obligated to comply with the insurer’s rehabilitation and return to work plan and assist the injured work where deemed reasonably practicable.
The employer’s legal obligations are set out under the relevant state or territory workers compensation or accident compensation legislation. Broadly, an employer’s obligations are to provide a safe and healthy workplace for employees so they are not at risk of any accident or injury because of work practices. Should an employee suffer from a work-related injury or disease, the necessary support and assistance should be available.
Workers’ Compensation and Rehabilitation Act 2003
Section 228 Employer’s obligation to assist or provide rehabilitation
228 Employer’s obligation to assist or provide rehabilitation
(1) The employer of a worker who has sustained an injury must take all reasonable steps to assist or provide the worker with rehabilitation during the prescribed period for the worker.
Maximum penalty—50 penalty units.
(2) The rehabilitation must be of a suitable standard as prescribed by regulation.
(3) Without limiting subsection (1) or (2), the employer must cooperate with the insurer to enable the insurer to meet its obligations under section 220.
(4) If an employer considers it is not practicable to provide the worker with suitable duties programs, as mentioned in section 40(2)(a)(i), the employer must give the insurer written evidence that it is not practicable.
(5) In this section—
prescribed period, for a worker who has sustained an injury, means the period that—
(a) starts on the day the worker is injured; and
(b) ends on the day the insurer’s responsibility for the worker’s rehabilitation ends under section 220.
Obligations
Active participation is essential to successful injury management. It is important that injured workers take an active role in their suitable duties program and make reasonable efforts to return to work.
In Queensland, if the injured worker returns to work in any capacity (even volunteering) they must advise the insurer within 10 business days.
Expectations
• Provide original copies of medical certificates of capacity in a timely fashion.
• Attend medical and other treatment appointments arranged by the treating doctor.
• If unable to attend an appointment, take reasonable steps to make an alternative appointment a soon as possible.
• Communicate with parties in an open and honest manner and reply to reasonable levels of communication without undue delay.
• Carry out agreed actions to the best of their ability, as outlined in the Suitable Duties Program.
• Immediately inform the Rehabilitation and Return to Work Coordinator (RRTWC) and line manager of any difficulties.
• Carrying out the Suitable Duties Program.
• If referred to a workplace rehabilitation provider, actively participate in all aspects of the service and work cooperatively with the service provider.
• Advise of any changes in circumstances.
• Advise of any changes to treating doctor or other treatment providers.
The overarching roles, rights and responsibilities of the injured worker include.
Workers’ Compensation and Rehabilitation Act 2003
Section 232 Worker must participate in rehabilitation
232 Worker must participate in rehabilitation
(1) The worker must satisfactorily participate in rehabilitation— (a) as soon as practicable after the injury is sustained; and (b) for the period for which the worker is entitled to compensation.
(2) If the worker fails or refuses to participate in rehabilitation without reasonable excuse, the insurer may, by written notice given to the worker, suspend the worker’s entitlement to compensation until the worker satisfactorily participates in rehabilitation.
(3) If the insurer suspends the worker’s entitlement to compensation, the worker may have the decision reviewed under chapter 13.
Workers’ Compensation and Rehabilitation Act 2003
Section 135 Examination by registered person
Workers’ Compensation and Rehabilitation Act 2003
Section 136 Worker must notify return to work or engagement in a calling
Throughout the return to work process it is important that the Insurer and the employer are able to demonstrate that they fulfilled all their return to work obligations. Section 220 of the Act notes the Insurer responsibilities including obligations for the rehabilitation and early return to suitable employment of the injured worker.
Workers’ Compensation and Rehabilitation Act 2003
Section 220 Insurer’s responsibility for rehabilitation and return to work
Importantly subsection 7 notes:
(7) In this section—
rehabilitation and return to work plan , for a worker who has sustained an injury, means a written plan—
(a) outlining the rehabilitation objectives for the worker and the steps required to achieve the objectives; and
(b) developed in consultation with the worker, the worker’s employer and registered persons treating the worker.
In addition, the employer needs to be able to demonstrate all their obligations were fair to all parties and had the goal of attempting to return the injured worker back to work during all stages of their recovery.
Being able to show you have done all you can on the claim to facilitate the return to work process will help if the person claims for damages through common law. In some instances the injured worker may have been able to return to work, however, has decided not to return to the same workplace. It is still important to work towards being able to show the worker has a capacity to return to work somewhere.
Hierarchy of return to work options:
1) Same job, same employer
2) Different job, same employer
3) Same job, different employer
4) Different job, different employer
The program should always have the intent to return someone to their original employment status. This is the best outcome for all parties in the great majority of instances. Below is a quick recap of the
services that are available to assist to achieve this goal and also provide guidance in the instances where alternate employment is a consideration. These services will assist to find the most suitable and durable employment.
An assessment containing a series of tests to determine a worker’s physical ability to meet the functional demands associated with their pre-injury role, thus assisting them with their recovery and or return to work.
An assessment of a client’s skills, experience, knowledge and interests, that they have acquired through work and life experiences.
Vocational assessment
A Vocational Assessment is a comprehensive evaluation of an individual’s transferable skills, qualifications and interests, to identify potential future employment and/or training options, whereby a physical or psychological injury prevents the individual from returning to their previous employment.
Re-skilling into a different suitable vocation to improve the return to work opportunities.
Host Employment is a program funded by insurance providers and forms part of a workers gradual return to work. A Host Employment Placement returns a worker to a structured work environment that provides routine and allows for a smoother transition from injury to their pre-injury role or other suitable employment.
If there is no possibility of staying with the same employer, then the insurer should look to arrange a rehabilitation provider to deliver options for a different employer to provide suitable work for the worker.
The host employer is indemnified against further aggravation injury claims in return for hosting the injured worker on a return to work program for an agreed length of time. The goal is facilitating a return to work outcome, which demonstrates a capacity for work.
See Rehabilitation Services in Section 5 for a recap on the services below.
Make sure you can say you have done absolutely everything to help the injured worker back to work and that these activities are evidenced. Have proof - documents, file notes and diaries etc.
Ask insurer to arrange host employment to show capacity for work.
Seek external advice (with consent) – Treating doctors, allied health professionals, Occupational Physician, Independent Medical Examination, Medical Assessment Tribunal (see below).
Check for any internal barriers which are hindering the return to work? It may not be what you think.
An insurer can refer an injured worker to the MAT if there are complex medical questions to be answered. The MAT provides independent, expert medical decisions about injury and impairment sustained by Queensland workers.
The MAT is a panel of medical specialists who have a high level of knowledge, expertise and experience in their field. Eg. Neurologists/Psychiatrists/Orthopaedic Surgeons.
A worker may be required to attend the Tribunal to determine the following:
• Whether employment has been a significant contributing factor to the worker’s injury.
• Whether there is an ongoing incapacity for work as a result of a work injury.
• Assess the degree of permanent impairment resulting from a worker’s injury.
• Degree of permanent impairment for Psychiatric/Psychological injuries or disfigurement or scarring as a result of a worker’s injury.
[17] Workers’ Compensation Regulatory Services
Insurers carefully consider the facts presented when making a decision to stop payments for treatment or compensation. They consider if the necessary and reasonable treatment has been provided and whether the Worker is able to work due to the accepted work-related injury.
A claim may be ceased and payments stopped for different reasons. For example, if the Worker has received all appropriate treatment for the work-related injury, however requires additional treatment for a pre-existing or non work-related condition or injury, Insurers may be unable to pay for the additional treatment. This will be determined on medical evidence.
If the Worker is unhappy about decisions made by insurers, the issues can be addressed through the Workers’ Compensation Regulator’s review process.
If the injured worker cannot return to their pre-injury employment and the medical advice is they should not return to that employer or that type of work, WorkCover will look to assist the injured worker to reskill or re-train or gain some job seeking skills.
At this point (when claim ceases) WorkCover is required to hand the case over to the Employment Connect Team to facilitate the vocational assistance. This cost is not passed onto Employers as the claim has closed.
Under the Queensland workers’ compensation scheme, workers have the right to sue their employer for negligence through a common law or damages claim.
If the worker is able to prove negligence, a lump sum payment of damages is awarded to the worker taking into account their future economic loss (loss of wages) and pain and suffering.
WorkCover will defend the claim on behalf of the employer, keeping them informed and involved throughout the process. They will attempt to resolve the claim with the injured worker as part of the pre- court process which is set out in the legislation. WorkCover will aim to do this informally as this process is more cost effective for everyone involved. If resolution is not reached, a more formal process called a compulsory settlement conference will be arranged.
When a decision to make a common law claim is made, the ‘no fault’ statutory claim for workers’ compensation (if made) will end. At that time the injury might be assessed by a medical practitioner or the Medical Assessment Tribunal (MAT for short). This will determine whether the injured worker has a permanent impairment and to what degree. This is called the DPI (degree of permanent impairment).
Based on this assessment, WorkCover may offer the claimant a lump sum payment in a Notice of Assessment (NOA) letter. From here the claimant can:
• Accept the offer
• Reject the offer
• Defer the lump sum payment offer to make a decision later.
The options also depend on the injured worker’s DPI percentage, which falls into two categories:
If the claimant accepts the permanent impairment and the lump sum compensation payment, the statutory claim can be finalised. Once accepted, the claimant will receive the lump sum payment within seven days. Accepting this offer and lump sum payment means the claimant won’t be able to make a common law claim.
If the claimant decides not to accept the lump sum offer, they can make a common law claim. If the common law claim isn’t successful, the claimant won’t be entitled to the lump sum later.
However, if the decision is deferred the claimant can decide on the lump sum offer later. This deferment will end if you decide to make a common law claim.
The claimant can accept the lump sum compensation and also make a common law claim for damages. The 20% figure can’t be reached by adding two or more DPIs together (for example, a physical and a psychiatric injury) to make 20%.
[15] WorkCover Queensland
All projects go through a process of scoping, where the overall aims of the project are documented. Then a project plan is developed. In this case it is the RTW program. Then it is implemented and monitored.
The last step, once a project is finalised, is to go through a process of review so that you can evaluate its success and profit from lessons learned for future projects.
Critical Success Factors should be identified in the planning stage. They are the key things that the project is intended to achieve.
In the case of a suitable duties program, ideally the goal is to assist the injured worker to recover completely or sufficiently enough to be able to return to their previous duties, however there are so many variables involved in achieving this that it is not a good yard stick to measure against, especially when some medical outcomes are not within your control.
From your point of view as a RTW Coordinator there are other ways that you may measure success other than just the injury recovery outcome.
Asking the worker and Supervisor questions about the process can provide useful data to be able to improve the policies, processes and procedures.
Note: It’s about the process - not the person!
• Find out what is working/what is not with regards to the policy/procedures? Were the policies and procedures effective?
• Did the program achieve its objectives? (Timeframes, milestones achieved, recovery objectives, costs). If not - What would be required to achieve better results next time
• Has the worker been retained in their previous job or has the worker been re-allocated to another job where they can be productive and useful?
• During the program, was there any disruption to work in progress or were there any other problems?
• What were the challenges / what worked well?
• Why experiences with return to work were good or bad?
• Has the incident causing the injury been investigated and led to improvements in safety procedures?
• How did the operation of the program affect the culture of the organization, if at all? What effect was there on co-workers?
• Seek to find out if underlying cultural morale could be effecting best efforts for workplace rehabilitation
• Is there support at the workplace? Support from management?
• Was the RRTWC’s performance effective?
• Were the external rehabilitation providers effective?
This important data & feedback should be used to make improvements to your workplace systems and feedback should be provided to the workforce. Consider recognition for those that contributed to an improvement in the workplace rehabilitation system.
Biopsychosocial – The systematic model used to describe the holistic elements of an assessment designed to understand the complex interactions of biological, psychological, social and economic aspects of health, injury, illness and health care delivery.
Capacity for work – Refers to the functional ability of the worker to participate in work activities as certified by the treating practitioner.
Certificate of capacity – The form required by Workers’ Compensation Authorities to be completed by a treating practitioner to describes what a worker can or cannot do while recovering from injury or illness.
Clinical Framework – ‘The Clinical Framework for the Delivery of Health Services’, which is a set of principles for providing health care services to individuals with a compensable injury and guiding health care professionals in their treatment practice.
Compensable injury – An injury or illness which is determined to be work-related and may be compensated by the relevant worker’s compensation authority.
Early intervention – Action that responds to an identified issue at the earliest opportunity for the benefit of the worker and employer.
Evidence based – An approach which integrates the best available research evidence with clinical expertise and patient values. It involves knowledge translation and application of research evidence to inform health care decision making.
Functional capacity – The extent to which a person can perform tasks or activities.
Health literacy – The degree to which a person can obtain, process and understand health information and services needed to make appropriate health and wellbeing choices.
Medical practitioner - Registered through the Australian Health Practitioner Regulation Agency to practice medicine and may include a general practitioner or specialist such as an Occupational and Environmental Physicians (OEPs). OEPs are medical specialists who provide services related to workers’ and employers’ health. The OEP’s approach is holistic, recognising the health effects of occupational, social, psychological and environmental factors.
Return to work – Refers both to supporting the worker to return to work following an absence from the workplace as well as supporting the worker to stay at work whilst they recover, whichever the case may be; understanding the health benefits of good work will assist to tailor the approach.
Self-management strategies – May be taught to the worker by the treating practitioner or workplace rehabilitation provider to assist in identifying needs and actions to maximise recovery and independence.
Support team – Various parties will support a worker at various times to recover from an injury or illness, including: the employer, insurer, treating practitioners, family members and the workplace rehabilitation provider.
Treating practitioner – Is the medical or allied health practitioner consulted by the worker for treatment services to aid recovery from injury or illness.
Worker – An individual with a compensable injury as per Section 11 of the Workers’ Compensation and Rehabilitation Act 2003.
Work capacity – Refers to the functional ability of the worker to participate in work activities as certified by the treating practitioner.
Workplace rehabilitation – A managed process involving timely intervention with appropriate and adequate services based on assessed need, aimed at maintaining injured or ill workers in, or returning them to, suitable employment.
Workplace rehabilitation consultant – Suitably qualified professional engaged to provide workplace rehabilitations services.
Workplace rehabilitation provider – An organisation who has been approved by a workers’ compensation authority to provide workplace rehabilitation services to assist workers to recover at or return to work following a workplace injury. Where appropriate within the context of workplace rehabilitation service provision, a reference to a workplace rehabilitation provider also includes a reference to a workplace rehabilitation consultant.
Workplace rehabilitation services – Services of a Workplace Rehabilitation Provider used to identify and address any risk factors which may impact a successful return to work, to translates functional gains into meaningful work, and provide evidenced-based advice on the best pathway to recovery and return to work, using work at therapy. At times a Workplace Rehabilitation Provider may also be engaged to assist with non work-related goals or work readiness activities.
Work status – Describes whether the worker is working (with or without income maintenance) or not working (with or without income maintenance). Where a worker is working it also describes whether this is with the same employer or a new employer (refer to the National data set for compensation-based statistics for details).
[1] Safe Work Australia, “Comparison of Workers’ Compensation Arrangements in Australia and New Zealand: 25th Edition,” Safe Work Australia. Canberra, Australia 2019. [Online]. Available: https://www. safeworkaustralia.gov.au/system/files/documents/2001/comparison-report-2019.pdf
[2] Workers’ Compensation Regulatory Services, “Workers’ Compensation Regulatory Services.”WorkSafe. https://www.worksafe.qld.gov.au/about/who-we-are/workers-compensationregulatory-services (accessed Jan. 2021).
[3] WorkCover Queensland, “The Role of Supervisors in Return to Work.” [Online]. Available: https:// www.worksafe.qld.gov.au/__data/assets/pdf_file/0009/22230/role-of-supervisor-in-rtw-shared-version. pdf
[4] AFOEM and RACP, “Realising the Health Benefits of Work: A Position Statement,” The Australasian Faculty of Occupational & Environmental Medicine (AFOEM), The Royal Australasian College of Physicians (RACP), 2011. [Online]. Available: http://www.racp.edu.au/docs/default-source/advocacylibrary/realising-the-health-benefits-of-work.pdf
[5] WorkCover Queensland, “Workers’ Compensation Regulatory Services.” WorkSafe. https://www. worksafe.qld.gov.au/claims-and-insurance/compensation-claims/claim-process (accessed Jan. 2021).
[6] WorkSafe Queensland, “Workers’ Compensation Regulatory Services.” WorkSafe. https://www. worksafe.qld.gov.au/rehabilitation-and-return-to-work/getting-back-to-work/planning-a-return-towork (accessed Jan. 2021).
[7] Office of Industrial Relations, “Guidelines for standard for rehabilitation: Second Edition,” Office of Industrial Relations. Brisbane, Australia, 2016. [Online]. Available: https://www.worksafe.qld.gov.au/__ data/assets/pdf_file/0029/25688/guidelines-for-standard-for-rehabilitation-second-edition.pdf
[8] WorkCover Queensland, “Workers’ Compensation Regulatory Services.” WorkSafe. https://www. worksafe.qld.gov.au/about/right-to-information/right-to-information-and-ip (accessed Jan. 2021).
[9] WorkCover Queensland, “Injury Information Pack: A guide for employers and workers,” WorkCover Queensland. [Online]. Available: https://www.worksafe.qld.gov.au/__data/assets/word_ doc/0005/20021/injury-information-pack_final.docx
[10] ACC, “New Zealand Acute Low Back Pain Guide,” ACC, New Zealand Guidelines Group. Wellington, New Zealand. 2004. [Online]. Available: https://www.healthnavigator.org.nz/media/1006/nz-acute-lowback-pain-guide-acc.pdf
[11] Who is a worker - Guide for Employers’ document provided by WorkCover Queensland. https:// www.worksafe.qld.gov.au/__data/assets/pdf_file/0020/43076/who-is-a-worker-employer-guidance.pdf
[12] Heads of Workers’ Compensation Authorities, “Principles of Practice for Workplace Rehabilitation Providers,” 2019, [Online]. Available: https://www.hwca.org.au/wp-content/uploads/2019/11/HWCAPrinciples-of-Practice-for-Workplace-Rehabilitation-Providers-2019_.pdf
[13] P. Cotton, “Occupational wellbeing: Management of injured workers with psychosocial barriers,” Reprinted from Australian Family Physician Vol. 35, No. 12, December 2006. 2010. [Online]. Available: https://www.racgp.org.au/afpbackissues/2006/200612/20061205cotton.pdf
[14] The Fair Work Ombudsman, “Workplace privacy.” Fairwork. https://www.fairwork.gov.au/how-wewill-help/templates-and-guides/best-practice-guides/workplace-privacy# (accessed Jan. 2021).
[15] WorkCover Queensland, “Common law claims.” WorkSafe. https://www.worksafe.qld.gov.au/claimsand-return-to-work/common-law (accessed Jan. 2021).
[16] New South Wales Health, “What is a person-centred approach?” New South Wales Government. NSW, Australia 2020 [Online]. Available: https://www.health.nsw.gov.au/mentalhealth/psychosocial/ principles/Pages/person-centred.aspx
[17] Workers’ Compensation Regulatory Services, “Medical Assessment Tribunals.” WorkSafe. https:// www.worksafe.qld.gov.au/claims-and-insurance/compensation-claims/medical-assessment-tribunals (accessed April. 2021).
RRTWC Learner Guide v2.8 - 22/07/2021