Paediatric Advanced Resuscitation Training




To understand:
• The aetiologies of cardiorespiratory arrest in children
• The probable outcome of primary and secondary cardiorespiratory arrest in children
• How the anatomical and physiological differences in children impact their management
Cardiorespiratory arrest is a rare event in children, and the outcome is generally poor. Out-of-hospital unwitnessed cardiorespiratory arrests have a very poor prognosis with only 8% of children surviving and most are neurologically impaired. The survival for in-hospital-arrests is better at 24% with a better neurological outcome. Over half of paediatric cardiac arrests occur in PICU where they have been monitored and witnessed. These generally have the best outcome because treatment is started early.
Aetiologies of cardiorespiratory arrest
The aetiology of cardiorespiratory arrest in infants and children differs from adults. This is due to differences in anatomy, physiology and pathology in children which alter as they grow and develop.
Adults tend to have primary cardiac events with a myocardial infarction leading to a fatal arrhythmia often ventricular fibrillation (VF). This is usually a sudden unpredictable event, and successful treatment is dependent on rapid defibrillation.
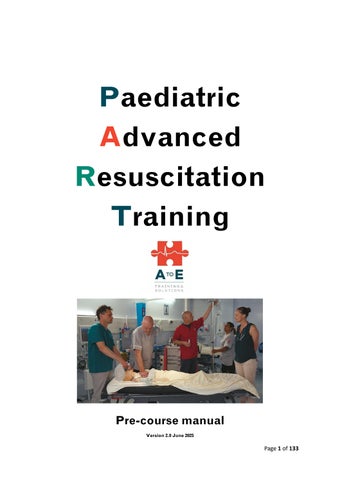
Children tend to have secondary cardiorespiratory arrests due to hypoxia from an underlying illness which leads to respiratory and/or circulatory failure. Cardiorespiratory arrest occurs once compensatory mechanisms have been exhausted. This is generally not a sudden event; hypoxia leads to profound bradycardia which then deteriorates to asystole or pulseless electrical activity (PEA). Asystole or PEA are the initial cardiac rhythms in 85% of paediatric cardiac arrests. Recovery from this has a poor outcome because in the lead up to the cardiorespiratory arrest there is global hypoxia affecting all the vital organs. The signs and symptoms of respiratory and circulatory failure and the compensatory mechanisms can be detected using an ABCDE approach. Early recognition and treatment of respiratory and/or circulatory failure can prevent deterioration to cardiorespiratory arrest
About 15% of cardiorespiratory arrests in children are due to a primary cardiac event. These children usually have underlying congenital heart disease (aortic stenosis, coarctation of the aorta), HOCM, a primary arrhythmia or myocarditis/cardiomyopathy
Airway
Smaller children have smaller airways which are more susceptible to obstruction, however there are other anatomical differences that increase the susceptibility to obstruction.
These differences are in the:
• Head and neck
• Face and mouth
• Nose and pharynx
• Larynx
Head and neck
Infants have large heads in relation to the rest of their body and the occiput is prominent. When placed on their backs the head tends to flex the neck which occludes the airway when conscious levels are reduced. As the child grows and develops the head becomes smaller in relation to the chest and the neck lengthens.
Face and mouth
The infants face is small so equipment needs to be suitably sized. The tongue is proportionally larger taking up more room in the mouth, this increases the likelihood of airway obstruction.
Nose and pharynx
Infants are obligate nasal breathers for their first 6-months, partial or complete nasal obstruction leads to airway obstruction and respiratory compromise
Larynx
In infants and small children the larynx is higher in the neck and ellipsoid in shape not cylindrical as in adults. The epiglottis is larger and floppier. These differences mean that visualisation of the vocal cords
with a laryngoscope is different than in adults and the epiglottis is more prone to damage with airway devices and manoeuvres.
Breathing
There are a number of differences in young children with regards to breathing affecting:
• The lungs
• The mechanics of breathing
• The respiratory rate
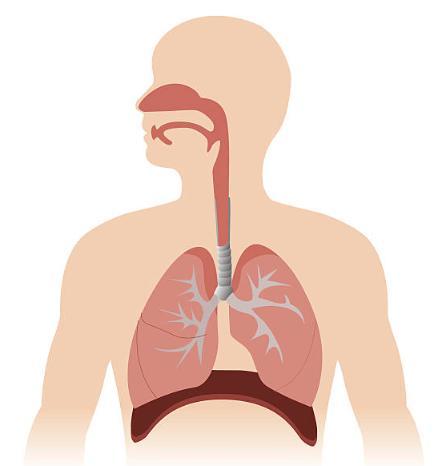
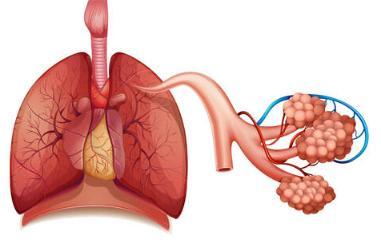
The Lungs
The lungs are not fully developed until 2 years of age, and the resting lung volume and oxygen reserve are much smaller. Infants and young children have a higher metabolic rate and higher oxygen consumption. This means that oxygen reserves are used up very quickly, and oxygen saturations will fall very rapidly in respiratory compromise.
Mechanics of breathing
As children grow and develop the mechanics of their breathing changes. Infants and small children have a pliable rib cage and weak intercostal muscles. They are primarily diaphragmatic breathers with the diaphragm descending during inspiration creating a negative pressure in the chest and drawing air into the lungs. The intercostal muscles contribute very little to the mechanics of breathing. Anything that impedes the descent of the diaphragm, such as gastric or intestinal distension will impede respiration If the diaphragm tires suddenly which means that infants in particular can suddenly become apnoeic. The pliable rib cage means that it is more likely to deform with increased respiratory effort in airway obstruction (bronchiolitis, foreign body obstruction) causing sternal, subcostal and intercostal recession. This makes breathing less effective.
In older children the intercostal muscles become stronger and contribute more to the mechanics of breathing. The rib cage ossifies and is less likely to deform when there is difficulty in breathing due to airway obstruction. In children over 5-yr recession is an ominous sign indicative of serious airway compromise.
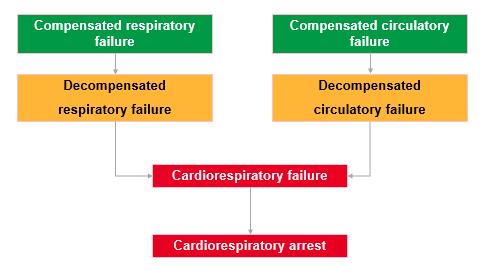
Respiratory rate
The tidal volume (TV) in children is 4-6ml/kg Infants have a relatively high metabolic rate, oxygen consumption and carbon dioxide production, which is the main reason for their increased respiratory rate. Respiratory rate is also increased by fever, anxiety, agitation.
Respiratory rate with age:
Age RR
< 1 y 30-40
1-2 y 26-34
2-5 y 24-30
5-12y 20-24
>12 y 12-20
Circulation
There are a number of differences in young children with regards to circulation. These are to do with:
• Circulating volume
• Cardiac output
• Blood pressure
Circulating volume
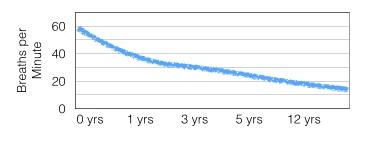
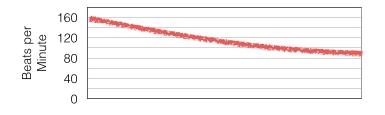
The circulating volume is proportionally higher at birth at 80ml/kg and decreases gradually throughout childhood until adult volumes of 60-70ml/kg are reached after puberty The absolute total circulating volume in infants however, is very small, for example a 5kg infant will have a circulating volume of 400ml whereas a 50kg teenager will have a circulating volume of 3,500ml. This means that relatively small volume losses in infants are a larger percentage of their total circulating volume. Children are able to compensate for up to 30-40% loss of circulating volume (see graph below) before their blood pressure falls
Haemodynamic response to hypovolaemia
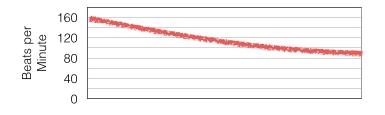
Cardiac Output (CO) = Stroke volume x Heart rate
Stroke volume is the amount of blood ejected with each heartbeat and is very small (1.5ml/kg) at birth and is relatively fixed; it increases with increasing heart size as the child grows. This means that the main determinant of cardiac output in small children is heart rate. An increase in heart rate will increase cardiac output whereas bradycardia will significantly reduce cardiac output. Heart rate is also increased by fever, anxiety, pain.
Normal range of heart rate with age
0-3 m 140 85 - 205 80 – 140
3 m-2 y 130 100 - 180 75 – 160
2 y-10y 80 60 - 140 60 – 90
>10y 75 60 - 100 50 – 90
Mean blood pressure (MBP) is dependent on cardiac output and systemic vascular resistance (SVR)
MBP = CO X SVR
SVR increases as a child grows and develops which is why blood pressure increases with age. Children are able to increase SVR to compensate for a reduced cardiac output to maintain blood pressure and circulation. SVR cannot be measured and so this means that blood pressure is unreliable as a marker of cardiac output (see graph on previous page).
A blood pressure less than the 5th centile for age is a sign that tissue perfusion is inadequate and that the child is unable to compensate further.
An additional tool for clinicians to use in determining whether blood pressure meets the threshold for compensation versus decompensation is the following calculation which works for children aged 1 to 10: Age x 2 + 70. This can be used to calculate the minimum systolic blood pressure for a child before they will be classified as in decompensated circulatory failure. To calculate the average mean this calculation can be used, Age x 2 + 90.
5th centile blood pressure for age
5th centile
50 70 75 80 90
5th centile Mean 40 50 55 55 65
Disability is used to assess the neurological state of the child, in effect it is assessing the interactivity of the child with carers and/or healthcare professionals. Hypoxia and reduced brain perfusion affect the alertness and interactivity of children. Infants and young children have limited communication skills and healthcare professionals have to rely on adult carers to know if the child’s behaviour is normal for them. This may also be true for children with pre-existing disabilities. Children may regress developmentally if in pain, anxious, or unwell. Effective pain control, empathy and appropriate language are essential when assessing interactivity. The presence of parents or carers can ease anxiety and is to be encouraged.
Interactivity or conscious level can be assessed using the Glasgow Coma scale or AVPU scale (Alert, responsive to Voice, responsive to Pain, Unresponsive). Assessing pupil size and reactivity, the child’s tone and any abnormal posturing further assesses the neurological status
To ensure no significant clinical information is missed the child should be fully exposed. Small infants and children become cold quickly when exposed and so appropriate measure must be taken to minimise heat loss. Dignity should be maintained and older children and teenagers may be shy and uncomfortable when undressed and exposed. They may also want to hide injuries particularly if selfinflicted.
Drug doses and fluid requirements in children are based on their weight. In older and larger children the recommended adult dose should not be exceeded.
It is often impractical to weigh a very sick infant or child and so the weight is often estimated.
If the child has recently been weighed and the weight is known use this otherwise estimate using any of the following:
• Age-Weight formula
• Infants at birth 3 - 3.5 kg
• Infants at 6-month 7 kg
• Children at 1 y 10 kg
• For children over 1-y Weight in Kg = 2 x (age + 4 )
• Paediatric emergency drug chart Monash charts etc.
• Body length tape Broselow tapes etc.
Key Learning Points
• The respiratory and circulatory anatomy and physiology of infants and young children influences the aetiology and management of their illnesses.
• Children are more likely to suffer a secondary rather than a primary cardiorespiratory arrest
• Successful resuscitation from respiratory arrest, where there is still a cardiac output, is associated with a good quality long term survivors.
• The mnemonic ABCDE is the basis for assessment and management of seriously ill children.
References
European Paediatric Advanced Life Support 5th Edition Resuscitation Council UK
Paediatric Immediate Life Support 2nd Edition Resuscitation Council UK
Cardiopulmonary Arrest in Children
Roy M. Vega; Hersimran Kaur; Jun Sasaki; Peter F. Edemekong. Stat Pearls https://www.ncbi.nlm.nih.gov/books
Aetiology and outcome of paediatric cardiopulmonary arrest
Laura R. van Banning, Carrick. A.G. Allison
Anaesthesia & Intensive Care Medicine
Volume 21, Issue 12, December 2020, Pages 615-619
Cardiac arrest in children
Erika E Tress, Patrick M Kochanek, Richard A Saladino, Mioara D Manole J Emerg Trauma Shock. 2010 Jul-Sep;3(3):267–272
Images
Haemodynamic response to shock
Shock in Pediatrics, Medscape htpps://ww.emedicine.medscape.com
Heart rate and Respiratory Rate graphs
Spotting the Sick Child htpps://ww.spottingthesickchild.com
To understand:
• The importance of early recognition of the seriously ill child.
• The importance of a structured ABCDE approach to rapidly identify potential respiratory, circulatory and neurological failure.
• The importance of a structured ABCDE approach to prioritise and assess the effectiveness of initial management strategies.
Early recognition of the seriously ill child
In children cardiorespiratory arrest is rare and is usually due to severe hypoxia, it reflects the body’s inability to compensate any further for the effects of the underlying illness. The initial problem may be due to an airway, breathing or circulatory problem but regardless of the aetiology cardiorespiratory arrest is seldom a sudden event. The child will compensate for the underlying illness but unless treatment is instituted will gradually deteriorate and decompensate as respiratory or circulatory failure worsens. Early recognition and effective management of respiratory and/or circulatory failure can prevent the deterioration to cardiorespiratory arrest. The use of an ABCDE structured approach helps to ensure that potentially life-threatening problems are identified and treated in order of priority.
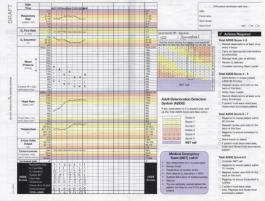
Paediatric early warning system charts such as RDR (Rapid Detection and Response Paediatric Chart), CEWT (Children’s Early Warning Tool) and PEWS (Paediatric Early Warning Score) aid detection of the deteriorating child and alert healthcare workers when and who to escalate concerns to.
The use of a structured physiological approach in the assessment of unwell patients was first introduced in children. It has been in use throughout healthcare systems worldwide for more than 20 years and has been repeatedly validated as a system. The ABCDE approach as detailed overleaf is a stepwise approach and can be completed rapidly, usually within 1-2 minutes and is an adjunctive tool for use by healthcare professionals to identify physiological deterioration in patients. It should be noted that it is adjunctive tool and must be used in the context of clinical judgement.
General principles:
• Ensure personal safety and appropriate personal protective equipment (PPE)
• What is the general impression of the child
• Observe the child for overall level of illness Are they interacting normally with parents/care-givers?
• Speak to the child (were age appropriate) to assess level of responsiveness, ask parents/carers about the child’s usual behaviour and how this compares to current status.
• If not responding to voice administer a tactile stimulation, tug gently on their hair, squeeze the trapezius, pinch earlobe, or tickle their feet.
o If the child responds to voice or to tactile stimulation by crying or talking they have a patent airway, are breathing and have cerebral perfusion.
o If there is groaning, grimacing or movement in response, rapidly assess using the ABCDE approach as below and
o Administer high flow oxygen immediately
o Attach monitors (ECG, SpO2, BP) early
o Gain circulatory access as soon as possible
• If the child is unresponsive check ABC and start BLS as necessary (see next chapter)
A structured ABCDE assessment is easy to remember, it systematically and logically assesses for signs of respiratory, circulatory or neurological failure and prioritises management interventions.
Assessment of the airway and breathing is essentially assessing oxygenation and ventilation, assessment of the circulation is assessing tissue perfusion including skin and kidney perfusion. Disability is assessing the effect oxygenation, ventilation and circulation are having on cerebral circulation and exposure may help in making a diagnosis of the underlying cause for the respiratory/circulatory failure.
System assessed
Assessing effectiveness of Airway Oxygenation and Ventilation
Breathing
Circulation
Disability
Exposure
Oxygenation and Ventilation
Perfusion
Effect of oxygenation, ventilation and circulation on brain
Helps to make diagnosis to underlying problem
Airway
Airway obstruction will obviously lead to respiratory compromise, difficulty in breathing and deoxygenation It can be partial or complete, sudden or insidious, recurrent or progressive. Initial partial airway obstruction can lead to increased work of breathing, respiratory failure, exhaustion and secondary apnoea. Partial airway obstruction can rapidly become complete obstruction resulting in cardiorespiratory arrest.
Depression of the central nervous system and loss of consciousness can lead to loss of airway control.
Causes of airway obstruction
Airway obstruction partial or complete can occur anywhere in the airway from the nose to the trachea.
Nose
Congenital anomaly
• Choanal atresia
• Pierre-Robin Syndrome
Secretions
URTI
Nasal feeding tubes
Nasal cannulae
Foreign body
Oropharynx
URTI
Enlarged tonsils
Oedema
Foreign body
Loss of consciousness
Larynx
Epiglottitis
Laryngospasm
Foreign body
Trachea
Tracheitis
Foreign body
A child who is talking or crying has an open airway. Airway obstruction may be demonstrated by difficulty in breathing, increased respiratory effort or noisy breathing. In a conscious child there may be obvious distress. Often conscious children with partial airway obstruction will assume a position that optimises their airway naturally such as neck extension or leaning forward and supporting themselves in a tripod position. Additional noises such as inspiratory stridor may be apparent in partial airway obstruction. Complete airway obstruction is silent. To assess the airway look, listen and feel for air movement and noises.
The smaller and younger the child the quicker they can go into respiratory failure. Babies under 3months are particularly vulnerable to hypoxia and apnoea.
Leave conscious children in the position they have adopted, leave them with their parents or care givers and administer oxygen in a non-threatening manner. Try not to make them cry as partial obstruction may become worse when they start to cry
In reduced level of consciousness airway compromise must be assumed. Partial airway obstruction may be relieved by head positioning (head-tilt chin-lift or jaw thrust), suctioning and by clearance of foreign bodies. Adjuncts may also be considered.
Breathing
Causes of breathing problems include:
Lung pathology
Congenital
Sequestration
Cysts
Atresia
Acquired
Bronchiolitis
Pneumonia
Pulmonary oedema
Asthma
Trauma
Neurological problems
Metabolic Problems
Respiratory Failure
Any impairment in breathing will cause the child to compensate for the deficit in ventilation and oxygenation.
• Compensated Respiratory Failure
This is a clinical state of an increased work of breathing or respiratory distress in an attempt to overcome a respiratory deficit
• Decompensated Respiratory Failure
This is when the child has lost the ability to maintain adequate blood levels of oxygen and carbon dioxide (i.e. in failure PaO2 < 9KPa, PaCO2 > 6.5KPa). It is recognised clinically to correspond to oxygen saturation (SpO2) < 90% in air.
Respiratory failure:
• Can exist with respiratory rates that are too fast or too slow, either will lead to a ventilationperfusion mismatch with reduced oxygenation.
• Can exist without respiratory distress in reduced level of consciousness, neuromuscular disease and morphine/opiate overdose.
Assessment of breathing
Try to use a “hands off” assessment where possible. Allow the child to assume a position of comfort. Keep the child with their parents/caregiver. Try to assess with the chest exposed; the parents can lift up clothing if necessary.
Ventilation
When assessing breathing we are in effect measuring minute ventilation.
Respiratory Rate
The respiratory rate is easily counted and ideally should be assessed without disturbing or touching the child, as soon as they start crying or coughing the rate will be changed. It can be assessed from a distance ideally with the chest exposed but if this upsets the child can be done through clothing. Assess for at least 30 sec.
The respiratory rate differs with age see below.
Age RR
< 1 y 30-40
1-2 y 26-34
2-5 y 24-30
5-12y 20-24
>12 y 12-20
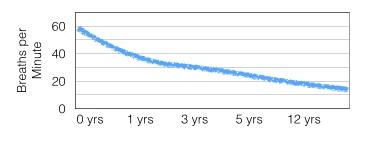
Generally, the respiratory rate increases as an illness becomes more severe until decompensation occurs when the rate slows. This may happen suddenly. Respiratory rate is also affected by anxiety, pain and fever.
Tidal Volume
Tidal volume is the amount of air that moves in and out with each breath. It can be assessed by looking at or feeling for chest expansion.
Assessing the effort of breathing
Normal breathing does not require any effort, increased work of breathing implies airway obstruction or underlying lung pathology.
Signs of increased work of breathing are:
• Recession
• Accessory muscle use
• See-saw respiration
• Nasal flaring
• Positioning
Recession
Recession or retractions means in-drawing of the muscles of the rib cage. Younger children show recession more easily and frequently due to their softer more compliant rib cages and chest walls. Recession can be difficult to pick up in chubby infants. Any recession in children over 5-y old is a sign of severely increased work of breathing. Recessions are usually seen at the same time as measuring the respiratory rate.
Recession includes:
Tracheal tug which is a downward movement of the trachea on inspiration accompanied by drawing in of the supraclavicular structures.
Sternal recession where the sternum becomes depressed during inspiration. This indicates more severe respiratory distress because the sternum is a large bone and requires more effort to draw in on inspiration.
Intercostal recession is in-drawing of the muscles between the ribs, and subcostal recession is indrawing below the ribs
Accessory muscle use
Normally the main muscles of inspiration are the diaphragm and the intercostal muscles. Accessory muscles use refers to the use of sternocleidomastoid and scalene muscles during inspiration which when contracted lift the clavicles and first rib to expand the thorax. In babies this results in head bobbing. With each breath the infant’s head bobs up and down. This makes breathing less effective and is a sign of severe respiratory distress.
See-saw breathing
This is a sign of severe difficulty in breathing and is sometimes called paradoxical breathing. On inspiration the chest is sucked in, and the abdomen expands, whilst on expiration the abdomen is sucked in, and the chest expands.
Nasal Flaring
Nasal flaring is seen more frequently in younger children and is where there is widening of the nostrils during inspiration which reduces airflow resistance at the nostrils.
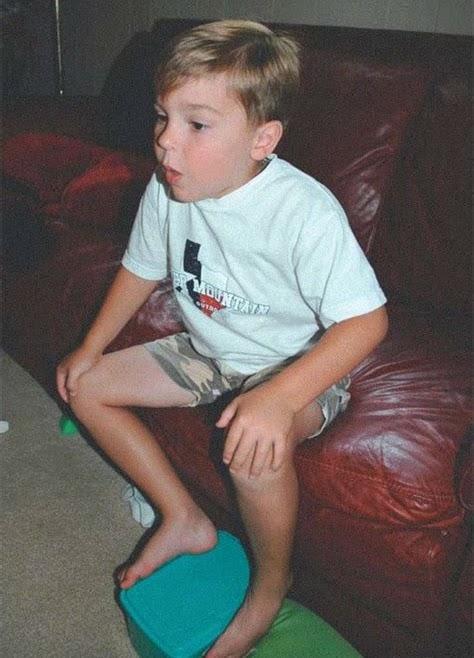
Patients with difficulty breathing are more comfortable upright. Tripod sitting refers to the position assumed when patients with breathing difficulties lean forward and rest their arms on their legs or the bed. This position helps the diaphragm move more efficiently and increases lung expansion as the accessory muscles are also used.
Tripod sitting


Listening to the chest particularly in infants and young children has less value than in adults. Children can become upset when a stethoscope is placed on their chest and start crying so it is impossible to hear any meaningful breath sounds; also because their chests are small, noises tend to be transmitted all over making exact location of additional noises difficult.
Normal breathing is usually quiet, noisy breathing can happen for several reasons and can be classified as inspiratory or expiratory.
The following respiratory noises may be heard:
Wheeze, this is a high pitched musical noise heard on expiration. It is due to lower airway narrowing and is heard in bronchiolitis and asthma. It can often be heard from a distance without a stethoscope. The loudness of the wheeze does not correlate with the severity of the underlying illness.
Stridor is a harsh sound heard on inspiration and is indicative of upper airway narrowing. It is heard in croup, foreign body obstruction, anaphylaxis, tracheitis, and epiglottitis. As with wheezing the loudness of the stridor does not correlate with the severity of the underlying illness. Do not examine the throat if you hear stridor.
Grunting is heard primarily in infants and is due to the infant breathing out against a partially closed glottis; this helps to keep their alveoli open during expiration and is a sign of significant respiratory distress. It is heard in bronchiolitis and RDS.
A silent chest is a medical emergency and is a sign that the tidal volume is very low.
Efficacy of breathing
Pulse oximeter
The pulse oximeter measures the amount of oxygen in the blood (SpO2) and is important for guiding management. It is useful as it is difficult to pick up cyanosis visually; most people cannot detect cyanosis until saturations are below 85%. Most children, especially babies and toddler, can appear fairly happy even with poor saturations. Normal children have saturations greater than 96%, less than 94% implies significant illness and should prompt supplementary oxygen use. Less than 92% is alarming and a sign of decompensated respiratory failure. The accuracy of the saturations detected is dependent on a good trace and will be falsely low if placed on a cold extremity or if the child is moving. Pulse oximetry recording is unreliable in the presence of carboxyhaemaglobinaemia
Effect of respiratory inadequacy on other body organs
Heart
There is often tachycardia to compensate for respiratory failure.
Skin
Hypoxia may lead to cyanosis or pallor
Brain
Hypoxia will lead to a reduced Level of consciousness
Management of respiratory compromise
The treatment of breathing problems is dependent on achieving a patent airway and effective delivery of oxygen. The method of oxygen delivery will vary according to the child’s clinical condition and age. Children with adequate spontaneous breathing should have oxygen delivered in a non-threatening manner, which may be wafting oxygen, simple face mask or non-rebreathing face mask. Children with inadequate (or absent) breathing should have high flow oxygen delivered by bag valve mask ventilation.
Once problems with the airway and breathing have been addressed the circulatory status should be assessed.
Circulation
Circulatory Failure
Circulatory failure is a clinical state where the flow of blood to the body tissues is inadequate for the metabolic needs of the child, and the removal of cellular waste is also inadequate.
Delivery of O2 = Hb x SpO2 x 1.34 x HR x SV
(Where – Hb=haemoglobin, SpO2=Oxygen saturation, 1.34=oxygen carrying capacity of haemoglobin, HR= heart rate, SV=stroke volume).
Delivery of oxygen to the tissues can be affected by changes to any of these parameters. The child has limited ability to compensate for a reduction in these parameters especially heart rate or stroke volume.
The commonest causes of circulatory failure are hypovolaemia, sepsis and anaphylaxis. Less commonly it can occur with underlying heart problems such as cardiomyopathy or congenital heart disease In cardiac tamponade and tension pneumothorax venous return to the heart is reduced and
Page 18 of 133
so the cardiac output is reduced, and when there is severe anaemia or carbon monoxide poisoning as the amount of oxygen carried by the blood is reduced.
Circulatory Failure
Circulatory failure can be compensated or decompensated.
In compensated circulatory failure there is preservation of blood flow to vital organs. This is maintained by an increase in cardiac output by increasing the heart rate (tachycardia) and by peripheral vasoconstriction. These together maintain perfusion to vital organs and maintain blood pressure.
In decompensated circulatory failure the circulation is unable to deliver oxygen to the tissues; the hallmark of decompensated circulatory failure is HYPOTENSION usually defined as a blood pressure less than the 5th percentile for age, this is usually accompanied by bradycardia.
BP mmHg 1 m 1 y 5 y 10 y 15 y
5th centile systolic 50 70 75 80 90
5th centile Mean 40 50 55 55 65
Assessing circulation
Assessing circulation is essentially an assessment of cardiac output and delivery of oxygen and nutrients to the tissues.
Cardiac output (CO) = HR X SV
Oxygen delivery = Hb x SpO2 x 1.34 x CO
When assessing perfusion it needs to be assessed peripherally, centrally and to the target organs (skin, kidneys and brain)
Recognition of Circulatory Failure
Cardiovascular status is assessed by taking the following into account:
• Heart rate
• Pulse volume
• Capillary refill and skin colour and temperature
• Blood pressure
Heart rate
In hospital the heart rate is usually measured by a pulse oximeter or ECG electrodes although placement of these devices may make the child cry. It can also be measured by taking the radial or brachial pulse. The heart rate initially rises to maintain cardiac output, producing sinus tachycardia. Sinus tachycardia is also seen in response to fever, anxiety or pain.
0-3 m 140 85 - 205 80 - 140
3 m-2 y 130 100 - 180 75 - 160
2 y-10y 80 60 - 140 60 - 90
>10y 75 60 - 100 50 - 90
Decompensation occurs when tissue hypoxia and acidosis affect heart function and lead to bradycardia. Bradycardia is a pre-terminal sign.
Pulse volume
How strongly the pulse is felt (pulse volume or amplitude) depends on the stroke volume of the heart. As the stroke volume decreases so does the pulse volume. Peripheral pulses (radial, dorsalis pedis) become weak before central pulses (brachial, femoral, and carotid) because increases in systemic vascular resistance cause peripheral vasoconstriction. It may be helpful to feel peripheral and central pulses simultaneously In infants and babies the brachial and femoral arteries are central pulses and in older children the carotid and femoral pulses are central pulses. Diminishing central pulses is a preterminal sign.


Capillary refill, skin colour and temperature
The skin of healthy children is warm and well perfused unless the ambient temperature is cold. Measuring capillary refill time (CRT) is a good way of assessing skin perfusion. It should be assessed centrally. To assess central CRT press on the centre of the sternum for 5-secs then release the pressure. Blanching should disappear within 2-secs in normal, well children. Delayed CRT indicates poor skin perfusion and implies that systemic vascular resistance is high to maintain blood pressure
Peripheral CRT can be delayed if ambient temperature is low. Skin mottling is also a sign of poor skin perfusion but is less specific than central CRT as it is affected by ambient temperature



Peripheral vasoconstriction also causes the peripheries to feel cool; often there will be a demarcation line between warm and cool skin. This will move towards the trunk as the child’s condition worsens and vice versa if improving.
Blood pressure
Only when the body’s compensatory mechanisms of increasing heart rate, and vasoconstriction fail does the blood pressure fall, and decompensated circulatory failure occur. This is usually a late sign. In hypovolaemia blood pressure only falls once 30-40% of the child’s circulating volume has been lost (20-30ml/kg). Hypotension occurs earlier in sepsis and anaphylaxis.
Blood pressure varies with age and hypotension is defined as a blood pressure less than the 5th centile for age as below:
For children over 1-yr this can be estimated using the following formula:
70 + (Age in years x 2)
Remember to measure blood pressure with the correct sized cuff; it should cover 2/3 of the length of the upper arm and the bladder of the cuff should cover 40% of the circumference of the arm.
HYPOTENSION is a pre-terminal event
Effects on other body organs
Respiratory system
The metabolic acidosis from circulatory failure leads to tachypnoea
Brain
Hypoxia and reduced brain perfusion will lead to agitation and/or drowsiness eventually leading to hypotonia and loss of conscious. This can sometimes be difficult to appreciate in younger children and those with disabilities and so it is important to ask parents /caregivers if the child is behaving normally and responding to them normally.
Kidney
Reduced kidney perfusion will reduce urine output. Urinary output of less than 2ml/kg in infants and less than 1ml/kg in children is inadequate and a sign of reduced renal perfusion.
In children able to use the toilet reduced urinary output may be easily recognised. In babies and children in nappies the number and weight of the nappies gives an indication of urine output.
Management of Circulatory Failure
After ensuring that the airway is patent and that breathing is managed with high flow oxygen, intravascular access should be gained. This may be achieved with a large bore cannula intravenously or by inserting an intraosseous needle. Administer a 10ml/kg bolus of isotonic fluid (0.9% saline or a balanced solution such as Hartmann’s or Plasmalyte-148).
If there is obvious on-going haemorrhage this should be addressed simultaneously with airway assessment and management.
Children with known cardiac defects should receive a smaller initial bolus of 5ml/kg.
After 30ml/kg of isotonic fluid boluses the use of inotropes should be considered.
Disability
Disability in the ABCDE framework is just a convenient word beginning with D which reminds you to do a neurological assessment. Following management of the airway, ventilation and circulation the neurological status should be formally determined again. Respiratory and circulatory failure affect neurological function but some neurological conditions such as status epilepticus, raised intracranial pressure or meningitis can affect the respiratory and circulatory systems.
When assessing the neurological status the following are assessed:
• Conscious level
• Pupils
• 0Posture
• Blood sugar level
Conscious level
This can be rapidly determined using the AVPU scale
A ALERT
V Responds to VOICE
P Responds to PAIN
U UNRESPONSIVE
If required a painful stimulus can be delivered by tugging on the child’s hair or by giving a trapezius squeeze. An alternative to the AVPU score is the Glasgow Coma score which has modifications for non-verbal children. P on the AVPU score is equivalent to 8 on the Glasgow Coma scale.
Drowsiness is commonly seen when children are febrile and irritability is seen with meningitis or raised ICP.
Pupils
Pupils should be assessed for size and reactivity. Medicines and cerebral lesions can affect the pupillary responses. Unequal sized pupils may be due to raised intracranial pressure (ICP) or unilateral cerebral pathology.
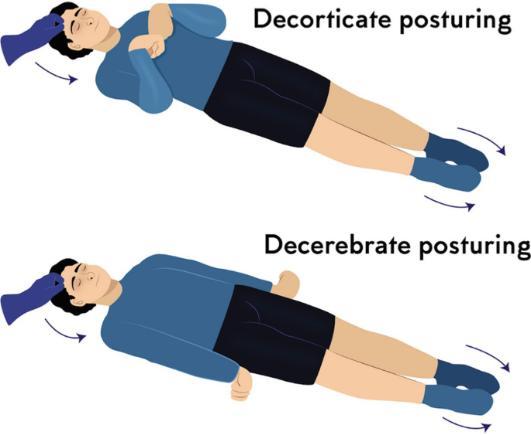
Posture
Seriously ill children are hypotonic or floppy. Posturing which becomes evident when a painful stimulus is given indicates serious brain dysfunction. Decorticate posturing where the arms are flexed and the legs extended or decerebrate posturing where there is extension of both the arms and leg scan be seen. Decerebrate posturing

Respiratory effects
Comatose children can exhibit abnormal respiratory patterns such as Cheynes-Stokes respiration (alternate hyperventilation then apnoea) or complete apnoea.
Circulatory effects
Raised ICP can cause Cushing’s Triad (bradycardia, raised blood pressure and irregular breathing) Cushing’s triad is a pre-terminal sign.
Blood sugar level
In any child with reduced level of consciousness blood glucose must be measured. This may be performed using a specific device or by assessing on a blood gas sample.
Exposure
To ensure that no significant clinical information has been missed the child should be fully exposed. This may give clues to the diagnosis e.g. rashes seen in meningococcal septicaemia, Group A strep sepsis and anaphylaxis, abnormal bruising seen in coagulopathy and non-accidental injury, fractures etc.
Careful attention must be paid to keeping the child warm especially infants and small children, and to respecting dignity in older children
The temperature can be checked using an electronic tympanic thermometer. Alternatively axillary or oral temperature can be recorded using an electronic device or paper strips (Tempadots).
ABCDE Checklist
Assessment
On approaching Child
Information sought
General appearance:
Colour, tone, alertness
Interactivity with parent/caregiver
Airway (what sound(s) can I hear?
Breathing
(what can I see?)
Is the airway:
Patent- talking or crying
At risk – noisy breathing, listless or reduced level of consciousness
Obstructed – quiet, reduced level of consciousness
Look ,listen and feel for breathing
Respiratory rate
Chest expansion
Accessory muscle use
SpO2
Auscultation (if trained to do so)
Possible actions
Call for help were appropriate
Obtain emergency equipment
Suction
Head positioning
Airway adjunct
o oropharyngeal
o nasopharyngeal airway
Reassess
Call for help
Administer high flow oxygen
Wafting
Positioning
Simple face mask
Non-rebreather mask
Bag-valve mask ventilation
Reassess
Call for help
Circulation (is the child in shock?)
Evidence of haemorrhage or fluid loss (vomit or stool)
Heart rate
Presence of peripheral pulses
Central pulse volume
CRT
Skin colour and temperature
Blood pressure
Urine output
Disability (neurological status)
Exposure (everything and anything else)
AVPU score
Muscle tone
Posture
Pupillary size and reactivity
Ask if medication has been administered e.g. for seizures, overdose
Look for:
Haemorrhage
Bruises
Rashes
Wounds
Fractures
Record Temperature if not already done so
Non-accidental injury
History
Medical alert bracelet
Remember to stick to the systematic structure
Treat problems as you find them
Control external bleeding
Attach monitors
Gain intravascular or intraosseous access
Blood samples to laboratory or near patient testing
Blood glucose
Fluid bolus 10ml/kg
Reassess
Call for help (surgical)
Check airway and breathing are being managed as conscious level dictates
Blood glucose if not already checked
Reassess
Call for help
Consider specific management such as blood transfusion, administration of antibiotics
Reassess
Call for help
Concern yourself with the “what” is wrong rather than “why” the child/infant is unwell
Ensure that help is coming and it is the right help
Reassess regularly and as treatments/interventions are instigated
Key Learning Points
• Early recognition of the seriously ill child prevents the majority of cardiorespiratory arrests, thus reducing morbidity and mortality.
• The structured ABCDE approach ensures that potentially life-threatening problems are identified and dealt with in order of priority.
References
European Paediatric Advanced Life Support 5th Edition
Resuscitation Council UK
Paediatric Immediate Life Support 2nd Edition Resuscitation Council UK
Spotting the Sick Child htpps://www.spottingthesickchild.com
Respiratory Assessment
Queensland Paediatric Emergency Care Skill sheet Htpps://www.childrens.health.qld.gov.au
Images
Respiratory system istock, istockphoto.com
Tripod position baby UAC Facebook
Tripod position child htpps://www.Medizzy.com
Tripod Position (epiglottitis) Htpps://www.medicalzone.net
Mottling of skin
Leg, DermNet htpps://www.dermnetnz.org
Baby htpps://www.community.babycenter.com
Arm
Diary of a Caribbean Med Student htpps://www.caribbeanmedstudent.com
Decerebrate and decorticate posturing The Ultimate Medical School Rotation Guide Chapter Neurosurgery pp845-927
Decerebrate posturing researchgate.net
Early onset of Fazio-Londw syndrome: the first case report from the Arabian Peninsula Mohammad Arif Hossain, Tariq Hazwani
Learning Objectives
• To understand the causes and management of airway obstruction
• To understand basic airway opening techniques
• To understand how airway adjuncts can maintain airway patency
• How to use bag-valve-mask (BVM) to effectively ventilate the lungs
Optimising airway patency and the provision of effective ventilation and oxygenation are central components in the management of critically ill children. Unless the airway is patent ventilation is impossible.
Causes of airway obstruction
Foreign body
• Small toys, food
• Mucus, blood, vomit
Loss of consciousness
The tongue falls backwards and occludes the airway, see below.

This occurs in:
• Hypoxia secondary to:
o Respiratory diseases
o Shock
o Cardiorespiratory arrest
• Neurological diseases
o Seizures
o Head trauma
o Intoxication
Recognition of airway obstruction
The most effective way to detect airway obstruction is to look, listen and feel for breathing.
LISTEN for airflow at the mouth and nose
During normal breathing the chest expands and abdomen is pushed slightly outwards If the airway is obstructed “see-saw” respiration may be visible where the chest is sucked in and the abdomen pushed out with each breath
Normal respiration is quiet
Breathing will be noisy in partial airway obstruction
Breathing will be silent in complete airway obstruction
FEEL for airflow at the mouth and nose
Movement of air will be felt in normal and partially occluded airways
There is no movement of air felt in complete obstruction
In a conscious child airway obstruction may be demonstrated by difficulty in breathing with increased respiratory effort. They may look anxious, be tachypnoeic or have recessions. Breathing may be noisy with inspiratory stridor or wheezing.
Unless choking, conscious children will have an airway that is partially or completely open. In general children with partial airway obstruction will assume a position that optimises their airway naturally; they may tilt their head back or lean forward supporting their upper body (tripod). If the child is taking adequate spontaneous breaths they should be supported in the position of comfort that they have adopted and left with their care giver This is particularly important in young children and babies as crying and distress can increase airway obstruction and may cause partial obstruction to progress to complete obstruction. High flow oxygen should be administered in a non-threatening manner that the child will tolerate. This may be by wafting oxygen, or using a simple oxygen mask, nasal cannula or non-rebreathing mask. Further help from anaesthesia, and ENT should be sought in partial airway obstruction.
Unconscious child
Whether or not an unconscious child is breathing the patency of their airway needs to be immediately optimised. There may be noisy breathing such as stridor or snoring indicating partial obstruction. Complete airway obstruction is silent. Partial airway obstruction can quickly deteriorate to complete obstruction. The airway can be optimized by simply repositioning the airway or by inspecting and suctioning the airway. If these measures do not clear the airway adjuncts may be required.
Basic airway opening techniques
Repositioning the airway
This can be performed by using the head-tilt chin-lift position of by using a jaw thrust.
Head-tilt chin-lift
This involves gently tilting the forehead back slightly and lifting the chin which is supported by pressing on the bony part of the lower jaw
The neck should be in a neutral position neither flexed or hyperextended. In the neutral position the plane of the face is flat, with the tip of the nose pointing straight up. A rolled towel under the shoulders may help to maintain neutral position.

The neck should be slightly extended with the nose “sniffing the morning air”.

This is the most effective airway opening manoeuvre in children and the preferred method if cervical injury is suspected. In this manoeuvre the rescuer approaches the child from behind, two or three fingertips of each hand are placed below the ears on the angles of the jaw. The thumbs rest gently on the cheeks. The fingers are lifted up whilst downward pressure is applied with the thumbs to the cheeks. This moves the lower jaw forward/up and pulls the tongue and soft tissues up and out of the airway.


If airway obstruction is not relieved by repositioning the airway, the pharynx should be inspected as there may be a foreign body, blood, vomit or mucus etc. causing obstruction. This will require a tongue depressor or laryngoscope so that the tongue can be pushed down and the back of the throat and pharynx can be properly examined. Suctioning the airway should always be performed under direct vision with a large bore suction catheter such as a Yankauer sucker. Only suck what you can see.
Airway adjuncts may be required if positioning or suctioning of the airways does not relieve airway obstruction. The following airway adjuncts will be discussed:
• Oropharyngeal airway (OPA)
• Nasopharyngeal airway (NPA)
• Supraglottic airway (SGA)
Oropharyngeal Airway (OPA)
• An OPA may help to open the airway in an unconscious child who has no gag reflex.
• An OPA is a rigid curved tube designed to open a channel between the base of the tongue and the posterior pharyngeal wall. They are made of rigid plastic which is reinforced and flanged at the outer end.
• They are available in a number of sizes.

• The appropriate OPA size can be estimated by placing the airway concave along the side of the face and measuring from the central incisor to the angle of the jaw.


• The OPA can be introduced into the mouth in the position in which it will lie; a tongue depressor or laryngoscope may be required to push the tongue down. Alternatively, they can be introduced upside down, pushing the tongue down, then rotated 180⁰ when halfway in and pushed further to lie in position.
• Following insertion, the flange should rest over the mouth and not protrude out of the mouth
Nasopharyngeal Airway (NPA)
• The nasopharyngeal airway is a soft flexible tube designed to open a channel between the nostril and the nasopharynx.

Nasopharyngeal airways
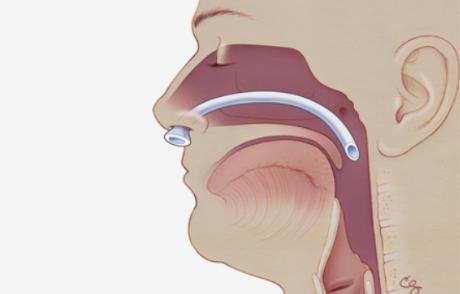
Nasopharyngeal airway in situ
• They are bevelled at the insertion end and flanged at the outer end. If the outer flange is shallow, a safety pin can be fastened at the end of the tube to prevent them passing completely into the nose.
• NPA tubes are usually better tolerated by conscious or semi-conscious children. They are available in a number of sizes but generally do not cater for smaller paediatric patients. In which case a shortened endotracheal tube (ETT) can be used.
• The correct sized tube is estimated by measuring from the nostril to the tragus of the ear. The appropriate diameter can be estimated by measuring against the size of the nostril. The NPA should fit snuggly but not cause blanching of the nostril.


• To insert, the NPA should be lubricated, then inserted into the nostril in the direction that it will lie. With a gentle rotation motion the NPA should be passed directly backwards and posteriorly to sit in the nasopharyngeal space.


• Contraindications to using an NPA are facial trauma, basal skull fracture, coagulopathy and nasal obstruction.
Supraglottic Airway (SGA)
• Supraglottic airway devices sit above the larynx in the supraglottic space. They have a wide distal opening which may have an inflatable or mouldable gel cuff which creates a seal over the larynx. The cuff is connected to a semi-rigid tube that holds the airway open. They can be connected to ventilation devices. They were originally designed for use in surgery to deliver anaesthetic gases, but have subsequently been found to be useful in managing the airway in cardiac arrest and resuscitation.
• In semi-conscious children with an intact gag reflex SGAs will cause gagging, coughing and laryngospasm so should only be used in unconscious patients. There are now several types available the most widely used in resuscitation is i-gel®.
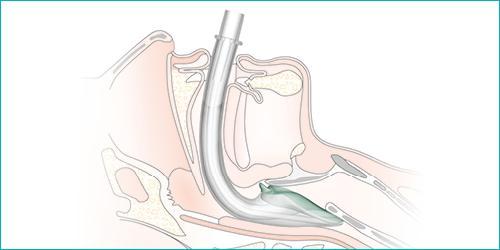




• i-gel® is made from a thermoplastic elastomer which when warmed to body temperature moulds to the shape of the supraglottic space creating a seal. This has the advantage that the seal does not compress or cause trauma to the soft tissues of the airway.
• i-gel® are available in four sizes for use in paediatrics and the appropriate size to use is determined by the weight of the child. They are colour coded and are presented in a plastic cage which clearly shows the size of the i-gel®.

1 2 -5 kg Pink
1.5 5 -12 kg Light blue
2 10 -25 kg Grey
2.5 25 – 35 kg White
• The size and weight guidance are also displayed on the i-gel® and should be visible to the rescuer when inserted

• All i-gel® except the smallest size (size 1) have a gastric channel which allows for early warning of regurgitation and allows for a nasogastric tube to be passed.
• The i-gel® has an integral bite block.
• In trained personnel i-gel® can be inserted in less than 10-seconds.
i-gel insertion technique
• Select the appropriately sized i-gel®

• Apply a small amount of water-based lubricant (such as optilube) to the distal tip and back of the i-gel®, taking care not to occlude the ventilation opening
• Hold the i-gel® in the dominant hand with the distal end which has the cuff facing toward the chin of the patient
• Whilst standing behind the child position the head in the sniffing position. In infants a tongue depressor (or laryngoscope) may be required to push the tongue down and out of the way.
• The tip of the i-gel® is inserted into the mouth and pressed against the hard palate.

Insertion into the mouth with head slightly extended i-gel®
i-gel insertion in an infant using a laryngoscope to depress the tongue
• The i-gel® is gently advanced until the cuff passes beyond the tongue until resistance is felt.
• The i-gel® should be secured in position with tape/ribbon.
• Capnography and BVM can be attached to the connector on the tube.
• Ventilate the patient, confirm placement by auscultation and chest rise
Oxygen delivery devices for spontaneously breathing children
In all seriously ill children oxygen should be given at the highest possible concentration as soon as it is available. Concerns about oxygen toxicity should not prevent its use during resuscitation. Oxygen flow should be regulated using a flowmeter capable of delivering 15L/min; ideally the oxygen should be humidified and warmed to minimise airway irritation and hypothermia. All children receiving oxygen should have oxygen saturations (SpO2) monitored and inspired oxygen titrated to maintain SpO2 9498%.
The method and device for oxygen delivery should be determined by the clinical condition of the child. The following will be discussed:
• Blow-by oxygen
• Nasal cannula
• Simple Oxygen mask
• Oxygen mask with reservoir bag (Non-rebreathe oxygen mask)
Blow-by oxygen
This is also known as wafting oxygen and is the least threatening way to administer oxygen to young children. Oxygen tubing or a mask is held by the parents close to the child’s nose and mouth. The flow of oxygen is directed towards the child without making contact with the face. There is no way of knowing how much oxygen is being delivered but is generally a low concentration; it is usually reserved for children with mild respiratory compromise. The effectiveness can be monitored by pulse oximetry.
Nasal Cannula
Nasal cannula deliver oxygen to the patient via a thin flexible tube that goes around the head and which has short prongs in it that fit into the nose. There are two types of nasal cannula high-flow (HFNC) and low-flow.
Delivering oxygen via low-flow cannula is very useful for stable children of all ages particularly in pre-school children. The delivery of oxygen is dependent on the oxygen flow rate and the nasal resistance. The maximum recommended oxygen flow rate is 4L/min. The amount of oxygen delivered is variable and cannot be precisely measured. It is not suitable for resuscitation. Nasal cannula are also not suitable for children with copious nasal secretions as the prongs become blocked and then do not deliver any oxygen.



HFNC delivers heated humidified oxygen at very high flow rates via a machine comprising of a flow generator, an air-oxygen blender, and a humidifier which warms the gases to 37⁰. See below
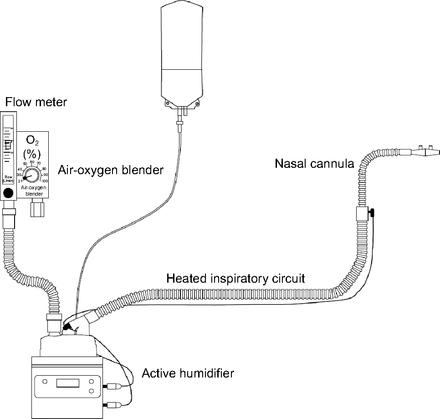
HFNC devices can provide flow rates up to a maximum flow rate of 60L/min in adults. In children the usual flow rates used are 2L/kg/min in children up to 12kg plus 0.5L/kg/min for each additional kilogram thereafter up to a maximum of 50L/min.
Children can eat and drink whilst on HFNC, and can ambulate.
HFNC have a number of beneficial effects on breathing including:
• Increase in functional residual capacity
• Improved mucociliary clearance of secretions
• Delivery of PEEP
HFNC are being increasingly used in the critically ill child to treat bronchiolitis, pneumonia, and lung contusion. They are not used in cardiorespiratory arrest.
Various machines are available including Optiflow, Airvo and Vapotherm (see below)

Simple oxygen masks are disposable clear plastic masks capable of delivering up to 60% inspired oxygen if flow rates are 10-15L/min. Room air is entrained into the mask and around the mask on inspiration diluting the amount of oxygen delivered.
Oxygen mask with reservoir bag (Non-rebreather oxygen mask)
This is the preferred method for delivering oxygen in the seriously ill child who is breathing spontaneously and can deliver up to 90% inspired oxygen. A clear disposable face mask is attached to a reservoir bag which is connected to the oxygen supply. The oxygen flow should be sufficient to inflate the reservoir bag and ensure that the bag does not collapse on inspiration, usually 12-15L/min.




with side valves removed
The mask is often fitted with three one-way valves which ensure that the gases move in only one way and that rebreathing exhaled air or room air is prevented. The first valve is between the reservoir bag and the mask, and the other two are on each side of the mask on the inspiratory holes. During inhalation the valve between the reservoir bag and the mask opens allowing oxygen to flow into the mask. The valves on either side of the mask close and prevent room air from being drawn in. On exhalation the valve between the mask and reservoir bag closes whilst the other valves open to let the exhaled air to escape. If the side valves are removed a lower inspired oxygen is achieved as room air is entrained when the child breathes in.
Oxygen delivery devices for spontaneously breathing children
Methods of assisted ventilation
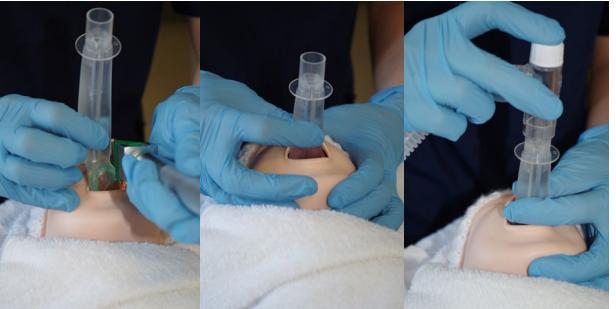
If a child stops breathing completely or spontaneous ventilation is inadequate positive pressure ventilation support is required. In a healthcare setting this will mean using a bag-valve-mask (BVM) device also called a resuscitator or Ambubag. The term Ambubag is taken from the first BVM that was developed and has become outdated terminology but is still used in some healthcare settings.
BVM devices are composed of a self-inflating bag, a non-rebreathing valve and a mask that conforms to the soft tissues of the face. The opposite end of the bag may be attached to an oxygen source and reservoir bag at 15L/min to deliver high concentration oxygen during resuscitation; without the oxygen source and reservoir bag ventilation will be delivered with air. The self-inflating bag can also be attached to an i-gel or endo-tracheal tube to deliver ventilation. A bag-valve-mask device cannot be used to deliver oxygen to spontaneously breathing patients.

When the bag is squeezed the air/oxygen in the bag is directed through the one-way valve. Provided there is a tightly fitting mask on the child’s face and an unobstructed airway the gases will inflate the lungs. Exhalation occurs through a one-way valve at the patient end of the bag. The bag automatically refills once it is no longer squeezed. Although the principle behind BVM ventilation is simple it is a skill that needs training and practice. Poor technique with an inadequate seal will lead to hypoventilation. During prolonged use in resuscitation the stomach becomes distended which can impede ventilation by pressing up on the diaphragm. A distended stomach will also increase the risk of regurgitation and aspiration. Insertion of a nasogastric tube may be required.
Bag-valve-masks
Self-inflating bags are available in a number of sizes depending on the manufacturer (250ml, 400500ml, and 900ml-1.6L). The medium sized 450-500ml bags are suitable for use in paediatric patients; although larger bags (900ml-1.5L) can be used if a smaller bag is not available. The pressure exerted on the bag should only be sufficient to support the tidal volume of the child and see chest rise. The
250ml bag is intended for use in neonates only. The bags used in infants and smaller children should have a “pop-off” pressure limiting valve which alerts the rescuer that excessive pressure is being delivered. The pop-off pressure is set by the manufacturers but is generally around 40 cmH2O. If required the valve can be over-ridden but then excessive pressure may be delivered increasing the risk of pneumothorax.
Masks used to deliver effective BVM should provide a good seal over the nose and mouth ensuring that there is minimal pressure on the eyes. Masks are available in two designs, circular and anatomically shaped, and in a number of sizes. Circular masks are recommended for infants and small children whilst anatomically shaped masks are more suitable for older children. Regardless of the shape, the mask must create a good seal.

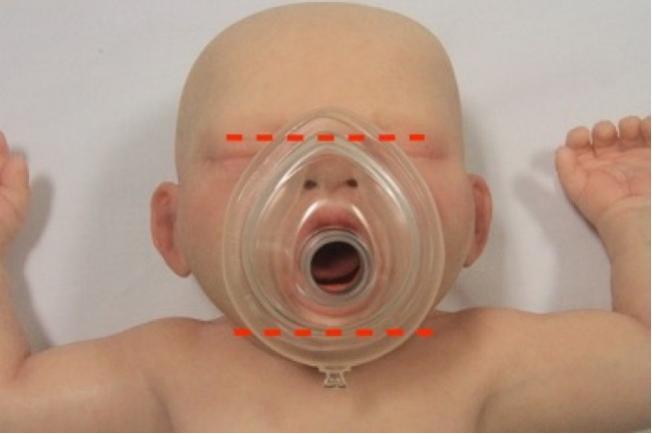


• Having selected the appropriate sized mask the rescuer stands behind the child.
• The oxygen supply should be connected to the self-inflating bag at 15L/min and the reservoir bag allowed to fill.
• The child’s head should be in an appropriate position to open the airway.
• The mask should be applied to the face covering the nose and mouth.
• Downward pressure is applied to the top of mask with the thumb and index finger, whilst the other fingers postioned along the bony part of the chin lift the jaw upwards into the mask.
• The bag is gently squeezed until chest expansion is seen.
• Once the chest is adequately inflated, the rescuer stops squeezing the bag and looks for the chest to fall.
• Repeat as required.
Single rescuers may find it difficult to maintain an air-tight seal and jaw thrust with one hand. If a second rescuer is available, the mask can be held with both hands of one rescuer whilst the second rescuer squeezes the bag. This does tie-up two rescuers in managing the airway, but the second rescuer can also perform chest compressions if required.
If chest expansion is NOT seen there are two possible reasons, either the airway is not patent or there is a leak. Recheck the airway and reposition or check for foreign body obstruction. Ensure that the mask is the correct size and that enough pressure is being applied to create a good seal. Reattempt ventilation once the necessary manoeuveres have been performed.
Key Learning Points
• Airway management and delivery of supplementary oxygen is the first priority in the management of critically ill children.
• Airway obstruction is commonly encountered in critically ill children and head positioning or simple adjuncts may be required to optimise the airway.
• In spontaneously breathing children oxygen can be delivered using various oxygen masks or nasal cannula.
• Children who are not breathing or who are not breathing adequately require positive pressure ventilation initially with a resuscitator or BVM.
• Correctly performed positive pressure ventilation via a BVM is central to successful resuscitation.
References
European Paediatric Advanced Life Support 5th Edition
Resuscitation Council UK
Paediatric Immediate Life Support 2nd Edition
Resuscitation Council UK
I-gel Supraglottic Airway Procedure Guidelines, Protopedia, roaddoc.com
The efficacy of oxygen wafting using different delivery devices, flow rates and device positioning Denise F. Blake, Elizabeth M Shih, Paul Mateos, Lawrence H. Brown
Australasian Emergency Nursing Journal Volume 17, Issue 3 August 2014 Pages 119-125
High-Flow Nasal Cannula
Sandeep Sharma, Mauricio Danckers, Devang K. Shanghavi, Rebanta K Chakraborty StatPearls htpps://www.ncbi.nlm.nih.gov
High-Flow Nasal Cannula Oxygen Therapy Devices
Masaji Nishimura
Respiratory Care June 2019, 64 (6) 735-742; DOI: https://doi.org/10.4187/respcare.06718
Bag-Valve-Mask Ventilation
Joshua T Bucher, Rishik Vashisht, Megan Ladd, Jeffrey S. Cooper Stat Pearls htpps://www.ncbi.nlm.nih.gov
Airway obstruction relieved by shoulder roll
Pediatric airway management
Harless J, Ramaiah R, Bhananker. Int Crit Illn Inj Sci. 201;4(1):65-70. [PubMed] DOI: 10.4103/2229-5151.128015
i-gel paediatric range information sheet https://www.intersurgical.com
Images
Inserting i-gel
Resuscitation Council UK
NLS Provider Course, Airway Guide March 2022
Diagram of occluded airway child https://www.australiawidefirstaid.com.au
Non-rebreathing mask
Nasal cannula
St John’s Ambulance https://www.sja.org.uk
Non-rebreathing mask on child https://stevens.ca
Non-rebreathing mask on mannequin https://bmglobalsupply.com
Nasal cannulae on child https://www.hytape.com
Simple mask on child https://se.intersurgical.com
Simple oxygen mask https://www.medline.com
Bag-valve-mask resuscitator with pressure relief valve https://medbis.mediq.co.uk
BVM in use https://www.rch.org.au
NPA anatomy Bever Medical https://www.bevermedical.com
i-gel in situ https://www.intersurgical.com
Solus LMA https://www.intersurgical.com
This guide is intended for healthcare professionals who have a duty to respond to cardiorespiratory arrest in infants and children in a healthcare setting.
Learning Outcomes:
• To recognise cardiac arrest in infants and children
• To understand how to activate emergency medical services
• To understand he rationale for the sequence of BLS
Good basic life support underpins advanced life support and should be performed whilst awaiting the arrival of advanced practitioners, equipment and drugs.
Cardiorespiratory arrest in infants and children is rare but is usually secondary to an underlying disease process with respiratory failure or shock leading to hypoxia and asystole. Cardiorespiratory arrest is the end result of severe hypoxia and rarely a sudden unexpected event. Children with underlying heart problems however can have primary cardiorespiratory arrest due to a fatal arrhythmia which may be sudden and unexpected and require defibrillation.
Definitions
Infant refers to babies in the first year of life (0 – 12 months)
Child refers to children from 1-y up to puberty which has a variable age of onset and completion. If the rescuer thinks that the patient is a child, the paediatric guidelines should be followed. Certain guidelines around the world have classified children up to 18 years of age given the aetiology of cardiac arrest in this age group. However, all healthcare professionals should use clinical judgement when responding and apply protocols that will maximise cerebral and cardiac blood flow.
Recommended Sequence for Paediatric Basic Life Support
The following sequence with the mnemonic DRS (SSS) ABCD should be followed by first responder healthcare professionals in a healthcare setting:
Dangers (Safety)
Responsiveness (Stimulate)
Send for help (Shout)
Airway
Breathing
CPR
Defibrillator (this may be prioritised where a child is known to have a cardiac abnormality or cardiac condition where a shockable rhythm is increased probability)
Ensure the safety of the patient and rescuers. In a healthcare setting it is rare for rescuers to come to harm during CPR however:
• Check for environmental dangers such as trailing wires, slip hazards from spilt liquids etc.
• Appropriate PPE should be used to reduce infection risk.
Responsiveness
It is important to establish the responsiveness of the unconscious child by using tactile and verbal stimulation. The method used will depend on the age of the child. In babies it can be achieved by talking to the baby or by gently touching or flicking their feet. In an older child it can be established by placing one hand on the child’s forehead and gently tugging their hair or squeezing their shoulders whilst saying “are you okay, wake-up”.
Never vigorously shake an infant or child.
• If the infant or child responds by crying, talking or moving, leave them in a safe position. Call for extra help if necessary and regularly check on their condition whilst awaiting further assistance if required.
• If the child is UNRESPONSIVE
Send for help
• SHOUT for help, or pull/press the emergency buzzer
• The second responder should call the relevant local emergency number stating location of cardiac arrest and specific team required (in this case paediatric)
Assess the child in the following order:
Airway
Open the airway; in an unconscious child with loss of muscle tone the tongue is likely to at least partially occlude the airway. Infants should have their head in the neutral position whilst older children should have mild extension of the head the so called “sniffing the morning air” position.
There are two airway opening techniques.
• Head tilt chin lift
Approach the child from the side, gently tilt the head backwards whilst holding the jaw (head tilt chin lift)
• Jaw thrust
Approach the child from behind and place both hands on either side of the child’s head.
Two or three fingers from both hands should be placed under the angle of the jaw just below the ears.
The thumbs should be placed on the child’s cheeks.
Gentle downward pressure on the cheeks and gentle upward pressure at the angle of the jaw will move the jaw up so that the lower jaw is in front of the upper jaw. This will move the larynx and open the airway.

Neutral position head tilt with chin lift



Once the airway is open inspect the mouth and remove any obvious foreign body if you are confident that it can be removed safely. DO NOT attempt blind finger sweeps as this is more likely to push a foreign body further into the airway and may cause complete obstruction to the airway.
Breathing
Assess for normal breathing and signs of life for no more than 10 seconds.
Signs of life include coughing and swallowing as well as breathing. The presence of a central pulse is a sign of life, but it can be difficult to detect even for experienced healthcare workers and unless a pulse rate greater than 60 bpm can definitely be felt within 10-seconds CPR should be commenced. Assess breathing by:
• Looking for chest or abdominal movement
• Listening for breath sounds at the nose and mouth.
• Feeling for airflow on your cheek.

Recovery Position
Agonal breaths or gasps are NOT normal breaths and should be treated as if the child is NOT breathing.
See-saw respiration (where the abdomen is pushed out and the chest sucked in with each breath) implies airway obstruction.
If the child is breathing normally leave in a recovery position and check regularly whilst awaiting further help. Consider further ABCDE assessment, oxygen, monitoring etc.
• Aims to prevent airway obstruction and reduce the likelihood of aspiration
• The child should be turned on to their side with their mouth facing downward.
• Stabilise with pillow or rolled up towel along to prevent rolling from the side position.
• Reassess regularly.
If the child is not breathing give 2 effective breaths by bag-valve-mask ventilation (BVM). Use 100% oxygen if available. If BVM not available start chest compressions whilst awaiting ventilation equipment.
If after the rescue breaths, there are no signs of life start CPR with chest compressions.
CPR
Method of compression
For effective chest compressions the child should be on a firm surface. There are differences in chest compressions between infants and children which are shown below.
Common features are as follows:
• Position
o Lower sternum one finger breath above xiphisternum
• Rate
o 100-120 compressions per minute
o 15:2 ratio. After 15 compressions give 2 breaths (a ratio of 30:2 is acceptable for not paediatric specialist and should not be corrected if CPR is being performed well)
• Depth
o 1/3 of the depth of the chest (4 cm infants, 5 cm children)
• Recoil
o Allow for adequate recoil, release all pressure on the chest between compressions, this is when the heart refills with blood.
Chest compressions in infants
There are two techniques using either thumbs or two fingers.

Two-Thumb technique
This is the preferred technique as it is more effective for the baby and less tiring for rescuers BUT does require two rescuers.
Technique:
• Place both thumbs flat side by side on lower sternum
• Encircle the lower part of the rib cage supporting the back
• Press down on the sternum with the thumbs
• Depress the sternum by one third of the depth of the chest (4cm)
Two-finger technique
This is the recommended technique for single rescuers but is more tiring for the rescuer.
Technique:
• Place two fingers (index and middle) of one hand on the lower sternum
• Depress the sternum by one third of the depth of the chest (4cm)

Depending on the size of the child the rescuer may need to perform chest compressions with one or two hands. The rescuer positions themselves at the side of the child and the heel of the hand is placed in position on the lower sternum. The elbow is locked and the shoulders directly over the heel of the hand. The fingers should be raised off the chest. The rescuer uses their body weight to depress the sternum by a third of the depth of the chest (5cm) using one hand, or two hands which may be interlocked.


After delivering 15 compressions give 2 breaths.
Continue until the child is responsive with return of normal breathing and other signs of life, or until more help arrives, or the rescuer becomes exhausted.
Chest compressions are tiring and as the rescuer fatigues compressions become less effective. If there is more than one rescuer swap roles to ensure effective compression every 2 minutes.
Defibrillator
Attach a manual defibrillator or AED to monitor the heart rate and rhythm. Use appropriate sized defibrillator pads if available. The majority of cardiorespiratory arrests in infants and children are secondary to hypoxia and defibrillation is not required, but the rhythm will be identified. In a witnessed sudden collapse a primary cardiac arrest is likely which will require defibrillation.
An AED with a paediatric attenuator can be used in infants and children under 8-years, but if not available use a standard AED for all ages.

Universal sign for AED
The pads should be applied with minimal interruption to CPR, and prompts from the AED followed. CPR should be performed up to the point of analysis and immediately after the shock or no shock decision.
Key Learning Points
• Basic life support follows a stepwise approach
• DRS- Once ensuring safety of the patient and ascertaining that the child is unresponsive rescuers should summon aid then start BLS and:
• A - Open the airway
• B - Deliver 2 rescue breaths
• C - If no response start chest compressions with a ratio of 15 compressions : 2 breaths
• D - A manual or automated defibrillator should be attached and the rhythm assessed. If using an AED prompts should be followed
• BLS should continue until further help arrives or the child responds
References
ANZCOR Guidelines
Guideline 3 - Recognition and First Aid Management of the Unconscious Person
Guideline 12.1 - Paediatric Basic Life Support (PBLS) for health professionals
APLS Australia
https://www.apls.org.au
Algorithms
European Advanced Paediatric Life Support Manual 5th Edition Resus Council UK
Chapter 4 Basic Life Support
Clear airway Positional drainage or suction if available and trained to use
Resuscitation – Basic Life Support Algorithm
Collapsed infant or child
Ensure safety of rescuer(s)
Check Responsiveness - Squeeze, Shake & Shout
Infant = under 1
Child = 1 to 18
Shout for HELP! Pull emergency bell Request AED
Inspect airway for signs of obstruction –particularly stomach contents
OPEN AIRWAY
Head Tilt, Chin Lift (or Jaw Thrust)

Infant – neutral position; Child – sniffing position
Assess for signs of life (LOOK, LISTEN, & FEEL as appropriate to circumstance) Look for skin colour & chest rise; Listen for breathing and/or verbal sounds; Feel for air on cheek (if no IPC risk)
NO (or any doubt) YES
Presumed CARDIAC ARREST
Activate Emergency Team/Ambulance
Ensure emergency bag/trolley being collected
5 Rescue Breaths (look for signs of life whilst delivering breaths)
Reassess for signs of life
Assess A, B, C, D, E
Commence CPR 15 Chest Compressions (rate 100 – 120 compressions per minute)
CPR for 1 minute then reassess
Switch on AED and apply pads as soon as possible Follow AED instructions as appropriate Remember attenuated pads for less than 8 years old AED not recommended under 1 year of age
Continue until Advanced or Immediate Life Support available or patient shows signs of life and begins breathing normally
Follow relevant algorithm Reassess regularly
ConsiderRecovery position
Oxygen Monitoring
Handover to emergency team
• Recognition of airway obstruction
• The importance of early management of choking
• Differences in management of choking in infants and children
Choking occurs when the airway is completely or partially blocked making it difficult or impossible to breathe. It can occur with external pressure on the airway but is most often due to a foreign body lodging inside the airway when it is also known as foreign body airway obstruction (FBAO)
From about 9-months babies reach out for objects and start putting these in their mouth. This behaviour is called mouthing and generally continues until two years. Children are therefore at increased risk of choking between these ages. Children with developmental delay may continue to mouth objects for longer and so remain at increased risk of choking for longer. Small objects and toys such as marbles, Lego, hair bobbles, coins etc. can cause choking as can foods such as grapes, berries, raw carrot, sausages, chunks of meat, and round or hard lollies etc.
FBAO is characterised by the sudden onset of respiratory distress associated with coughing, gagging or stridor. Foreign bodies in the airway initiate a cough reflex which attempts to expel the foreign body, however, if the airway is completely blocked immediate assistance is required
If the airway is only partially blocked the child will usually be able to cry or vocalise and breathe. They may be able to clear the blockage themselves by coughing. In fact a spontaneous cough is safer and generally more effective at clearing the airway than any manoeuvre a rescuer might perform. Do not attempt blind finger sweeps as these are likely to push the object further in to the airway. If an object is visible and you are confident that it can be removed with suction or Magill’s forceps attempt to remove it. Otherwise request urgent assistance from ENT and anaesthetics; allow the child to sit upright in a position they feel most comfortable and arrange urgent transfer to theatre for removal under direct vision.
If the blockage is complete the child will quickly become hypoxic and lose consciousness. They will require assistance to clear the blockage as will children with an ineffective cough for other reasons such as neuromuscular weakness.
Signs of choking
Witnessed episode
Sudden onset
General signs
Recent history of eating or playing with small objects
Drooling
Clutching neck with thumb and fingers
Ineffective cough
Distress, anxiety, agitation
Unable to vocalise
Quiet or silent cough
Unable to breath
Decreased conscious level
Cyanosis
Management of Choking
Effective cough
Distress, anxiety, agitation
Crying, talking
Loud cough
Able to breathe before coughing, stridor,
Fully responsive
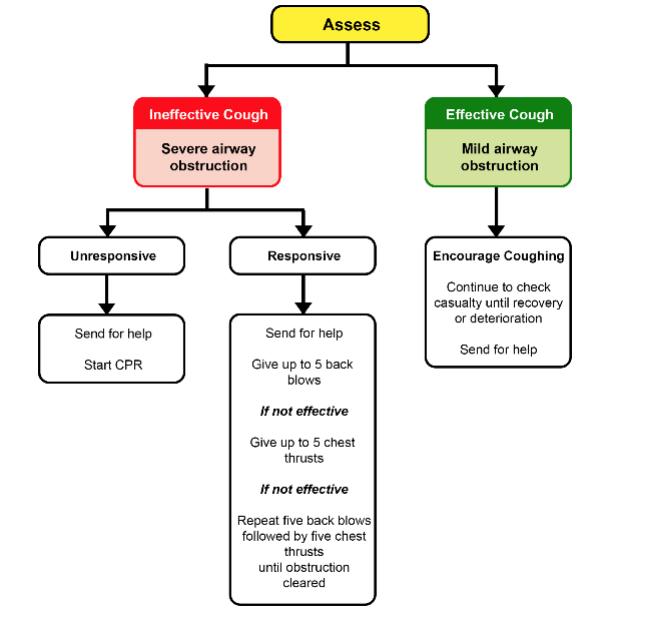
Effective Cough
• Encourage coughing
• Observe closely
Ineffective Cough
Responsive
• Send for help, pull emergency buzzer.
• Call urgently for anaesthetics or ENT.
• Give five back blows, checking after each to see if an object has been expelled.
• If ineffective give five chest thrusts.
• Repeat sequence if required.
Infant
Technique for back blow
• Sit or kneel with the infant across your lap in in a head down prone position.
• Support the head by holding the lower jaw.
• Deliver five sharp back blows with the heel of the hand between the shoulder blades.
• Check if the object has been expelled after every back blow.
• If the object has not been expelled deliver five chest thrusts.
Technique for chest thrusts
• Turn the infant onto their back in a head down position. Place your arm along the infant’s back and hold the occiput/head with your hand.
• Identify the landmark for chest compressions (one finger’s breadth above the xiphisternum).
• Deliver chest thrusts which are like chest compressions but sharper and slower.
• Check after each thrust to see if the object has been expelled.
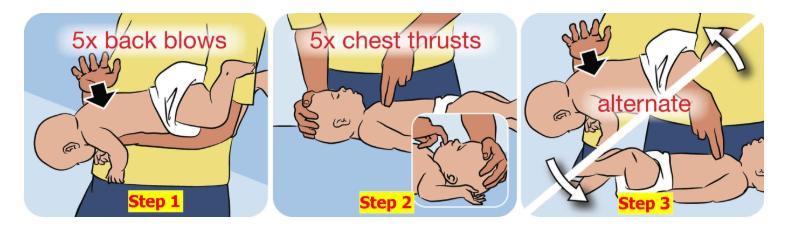
Continue to alternate back blows and chest thrusts until the object has been expelled or until the child loses consciousness when PBSL should be commenced.
Child
Technique for back blows
• A small child can be positioned across the rescuer’s slap or if larger supported in a head down position.
• Deliver five sharp back blows with the heel of the hand between the shoulder blades.
• Check to see if the object has been expelled after each back blow.
• If ineffective deliver five chest thrust.
Technique for chest thrusts
• Kneel or stand behind the child and support in a forward leaning position.
• Deliver thrust using the same technique as chest compressions but sharper and slower. Support the back during each thrust.
• Check after each thrust if the object has been expelled.
• Continue to alternate back blows and chest thrusts until the object has been expelled or the child loses consciousness, then start PBLS.
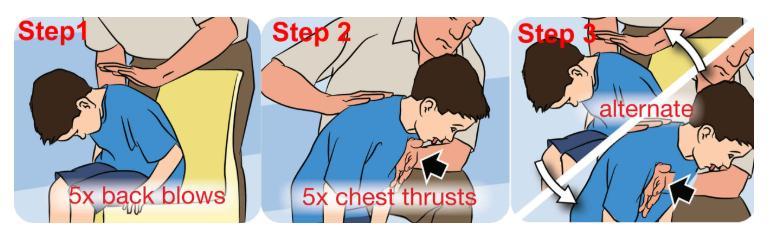
Key Learning Points
• Management of conscious choking infants of children consists of back blows followed by chest thrusts.
• Management of unconscious infants and children as a result of choking requires PBLS to be performed.
References
ANZCOR Guidelines
Guideline 4 – Airway
3.0 Recognition of Upper Airway Obstruction
4.0 Management of Foreign Body Airway Obstruction
Foreign Body Airway Obstruction Algorithm
APLS Australia
Algorithms Choking Child
Royal Children’s Hospital Melbourne ww.rch.org.au
Clinical Practice Guidelines Foreign bodies inhaled
Perth Children’s Hospital https://pch.health.wa.gov.au
Choking
CDC Nutrition www.CDC.gov
Choking hazards
Images
Choking infant and child Back blows and Chest thrusts Htpps://www.healthjade.net
Reference:
Soar J. et al (2020) Adult Advanced Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation & Cardiovascular Care Science with Treatment Recommendations Resuscitation Vol 156; Pg A80 -A119
Resuscitation Council UK (2021) Advanced Life Support Manual 8th
Resuscitation – Choking (FBAO) Algorithm
Assess Severity
Infant = under 1
Child = 1 to 18
SEVERE AIRWAY OBSTRUCTION (Ineffective cough)
UNCONSCIOUS?
Shout for HELP! Pull emergency bell
CONSCIOUS?
UP TO 5 BACK BLOWS
OPEN MOUTH REMOVE OBVIOUS FOREIGN BODY
UP TO 5 CHEST THRUSTS (INFANTS)
UP TO 5 ABDOMINAL THRUSTS (CHILDREN) REASSESS
MILD AIRWAY OBSTRUCTION (Effective cough)
ENCOURAGE COUGHING

Continue to reassess for signs of deterioration or clearance of obstruction
OPEN AIRWAY REASSESS IF NECESSARY START BLS
Continue until Advanced or Immediate Life Support available or patient shows signs of life and begins breathing normally
Learning Objectives
To understand:
• The requirement for circulatory access during resuscitation
• The different routes of emergency circulatory access and their appropriate use
• Intraosseous access
During resuscitation access to the circulation is essential to obtain blood samples, which may give a clue to the reason for the arrest, and to be able to administer fluids and medication.
• Circulatory access can be obtained via the intravascular (IV) route or the intraosseous (IO) route.
• If there is a patent intravenous cannula in situ it can be used, but there may still be the need for additional access.
• In decompensated circulatory failure attempts at intravenous insertion should take no more than three attempts or 90-seconds. If access is not achieved within these limits intraosseous access should be gained.
• Intraosseous access is the recommended route of access in cardiac arrest.
• Any medication given intravenously or through the intraosseous route must be followed by a 2-5ml bolus of 0.9% saline.
Intravenous cannulation
Intravenous access can be gained peripherally or centrally. Central venous access is difficult to achieve in children and should only be attempted by experienced healthcare providers. This is usually the remit of the PICU team. Peripheral venous access should be a priority in unwell children. IV access is preferred to IO in children who are conscious.
Infants and children have small calibre mobile veins, and are usually uncooperative and stressed during attempts at cannulation.
The following may help:
• Visualisation of veins can be improved by the use of trans-illumination, near infrared light or ultrasound
• Anxiety can be reduced by oral sucrose or breast-feeding in infants
• Veins may be more filled and so more visible if a tourniquet is used, the vein is tapped, or by local warming
Any peripheral vein can be cannulated, however, in seriously unwell children large easily accessible veins such as those in the antecubital fossa (cephalic or basilic veins) or the long saphenous in front the medial malleolus are best used.
Scalp veins should not be used for resuscitation because of the risk of extravasation and subsequent tissue necrosis. Their use may also interfere with management of the airway and ventilation.
Sites of peripheral veins
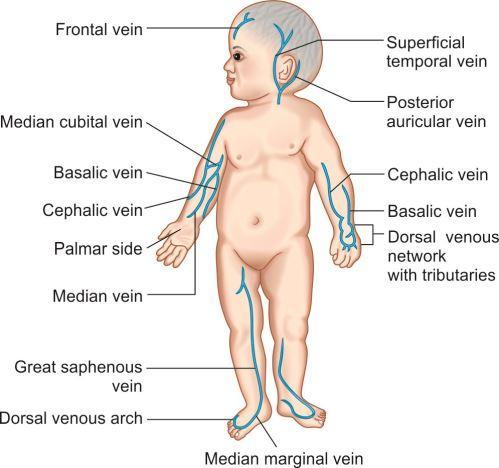
Intraosseous access
During resuscitation of cardiac arrest IO access is the emergency circulatory access of choice. In IO access the cannula is placed through the skin and into the medullary cavity of the bone. The medullary cavity is a non-collapsible vascular space and allows rapid delivery of fluids and medicines into the circulation.
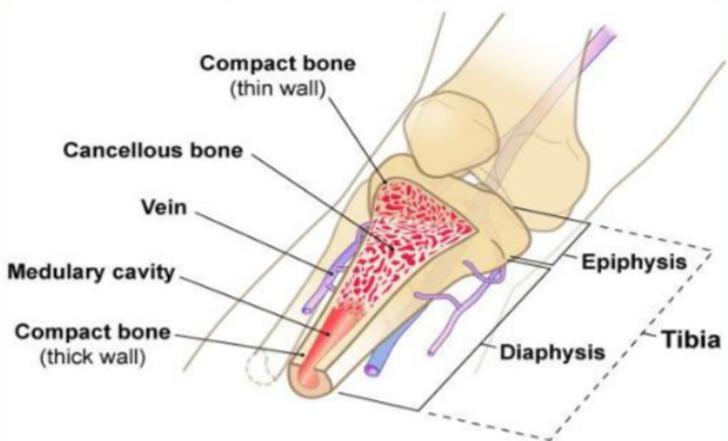
Various types of intraosseous needles are available, including those for manual insertion, manualassisted or gun inserted and those for drill insertion. In most hospital settings a drill device such as EZIO is used.
Manual and gun assisted needles are available in various gauges for adult and paediatric use.
Manual insertion needles

Manual assisted needles




EZ-IO needles
EZ-IO needles are all the same gauge (15G) but vary in length, and colour.
The smallest pink needle and middle sized blue needle are recommended for use in children 3-39 kg, and the longest yellow needle recommended for patients 40 kg and over.
Pain on insertion and use

Insertion of an IO needle can be painful although if a drill is used there is minimal pain. In conscious patients local anaesthesia to the skin using lidocaine can be used prior to insertion.

Instilling/injecting fluids or drugs into the medullary cavity of bone, however, is very painful and if the patient is conscious lidocaine should be instilled in to the medullary cavity before injecting into the IO needle. The extension set can be primed with 2% lidocaine (20mg/ml) with a dose of 0.5mg/kg (0.25ml/kg) max dose 40mg (20ml.)
Advantages of IO access
• Ease and speed of insertion
o Success rates are higher than with iv placement (97% first attempt success rate)
o IO can usually be inserted in less than 10-sec
• Can be used to deliver all resuscitation fluids, medication and blood products
• Allows rapid access of fluids and medicines to the central circulation
• It can be left in situ until intravenous or central venous access gained (max 48-hours)
Disadvantages
• Bone marrow is aspirated, not blood, and this cannot be used for analysis in point of care testing equipment such as blood gas analyser or blood glucose analyser. It can be sent to the laboratory but the laboratory must be made aware that it is bone marrow
• It can be painful to inject fluids/medicines in conscious/aware patients who may need local anaesthetic added to the infusion fluid.
• Force is required to inject medicines or fluids.
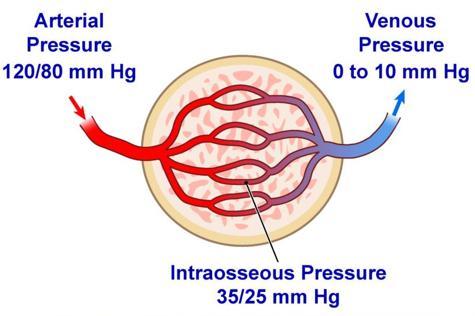
Contraindications
• Fracture of target bone
• IO attempted or placed in target bone within previous 48-hours
• Infection at insertion site
• Osteogenesis imperfecta or other bone abnormality
Complications
• Failure to enter the bone
o Extravasation which can lead to skin necrosis or compartment syndrome
o Subperiosteal infusion
Complications cont.
• Penetration through and through the bone
• Infection
o Osteomyelitis
o Local infection
• Growth plate injury
• Pain
• Bone or fat embolus
Sites of insertion
Upper humerus
Distal femur
• Midline above external epicondyle
Tibia
• Proximal tibia anteromedial surface below tibial tuberosity.
• Preferred site in cardiac arrest
• Distal tibia above medial malleolus
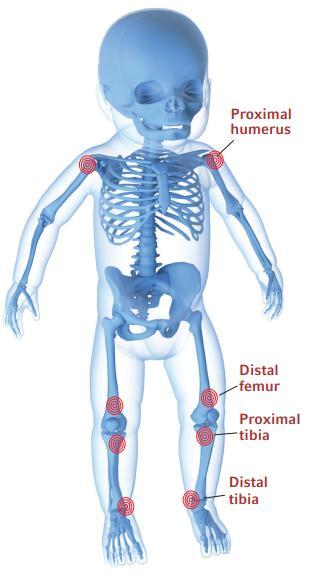
Insertion Procedure



Identify preferred site
Clean skin
Wear gloves and use a no-touch technique
If the patient is conscious use local anaesthesia to skin
Stabilise the limb
Select appropriate needle and attach to drill
Insert the needle into the skin at 90⁰ angle until the tip rests on bone
Ensure that at least one black line is visible (5mm) when the needle is touching the bone
Depress button on drill applying gentle downward pressure
Stop pressing the drill button once needle enters bone.
Usually a “give” is felt.
The needle should be almost flush with the skin
Hold the hub of the needle and remove the drill
Unscrew the stylet/trocar anticlockwise and remove Dispose of needle in sharps bin
Apply dressing over hub of needle
Attach primed extension set +/- three-way tap
Attempt to aspirate cannula, if unable to do so inject 2-5ml 0.9% saline flush and reattempt
Instil medicines or fluids as required under pressure
In conscious patient instil lidocaine before injecting fluids
Removal technique
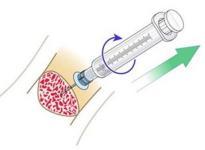
Key Learning Points
Remove extension set and dressing
Stabilise hub of catheter and attach a luer lock syringe
Maintaining alignment twist clockwise and pull straight out
Dispose of catheter and syringe in sharps box
Apply dressing to insertion site
• Vascular access is required in the management of the sick child and in management of cardiorespiratory arrest
• Intraosseous access is the route of choice in cardiorespiratory arrest and in decompensated cardiorespiratory failure
• Intraosseous access is suitable for all fluids and medication required in cardiac arrest
References
Teleflex Arrow EZ-IO mobile phone app
Intraosseous access
Clinical Practice Guideline
Royal Children’s Hospital Melbournehttps://www.rch.org.au
Intraosseous Vascular Access
Peter Dornhofer, Jesse Z. Kellar Stat Pearls https://www.ncbi.nlm.gov
Intraosseous administration of preservative free lidocaine Great Ormond Street https://www.gosh.nhs.uk
Pictures
Cook intraosseous needle https://medtree,co,uk
Three EZIO needles https://www.medscape.com
EZIO drill and needles https://uslmedical.co.nz
EZIO in use
Diagram of bone https://www.slideserve.com
Veins of forearm and hand
Practical Procedures
Vessel Health and preservation 2: inserting a peripheral iv vascular cannula https://www.nursingtimes .net
Vascular access sites
Clinical Nursing Procedures: The Art of Nursing Practice 3rd Edition
Jacob Annamma, Tarachand Jadhav Sonali, R Rekha
Vascular access sites
Vascular Access: From Cannulation to Decannulation
Nissar Shaikh, Arshad Chanda, Adel Ganaw, Mohammad Sameer, Jazib Hassan, Muhmmad Waqas Farooqi & Mohammed Mohsin A. M. Haji
Vascular Access
Kelly Mayo & Joseph R Pare
Learning Outcomes
To understand:
• The type and volume of fluid to be administered in the emergency situation
• The indications, doses and actions of first-line medication used in cardiorespiratory arrest
Fluid administration in resuscitation
During cardiorespiratory failure and arrest hypovolaemia is often a primary contributing factor and intravascular fluids are administered to restore circulatory volume to ensure adequate perfusion of vital organs.
The administration of fluids is essential for children showing signs of circulatory failure but fluid overload due to excessive administration can be detrimental. After each fluid bolus the child should be carefully assessed for signs of fluid overload. These signs are raised JVP (which is difficult to detect in babies) basal crackles and liver enlargement.
Fluid Volumes
An initial fluid bolus of 10-20ml/kg is recommended with careful reassessment after administration. If signs of circulatory failure persist a further bolus should be administered. If there are still signs of shock after administering 30-40ml/kg the child will need PICU support. Consider intubation and inotropes at this stage.
In cardiogenic shock and diabetic ketoacidosis fluids should be used cautiously and a smaller volume bolus is recommended. In cardiogenic shock consider using 5 ml/kg and in DKA start with 10 ml/kg.
Types of Fluid
Crystalloids
Crystalloid fluids are intravenous solutions that contain water and small water soluble molecules such as electrolytes (e.g. sodium, chloride etc.) or glucose. They are cheap, readily available and do not cause allergic reactions.
Crystalloids can be isotonic, hypotonic or hypertonic. Isotonic solutions have an osmolality and sodium concentration similar to plasma and so do not cause big fluid shifts. Hypo or hypertonic solutions have a lower or higher sodium concentration and cause fluid shift; in some cases this can have a therapeutic effect (3% saline to treat raised intracranial pressure) but fluid shift can also be detrimental to the child.
0.9% saline is an unbalanced isotonic solution containing only sodium and chloride ions. The sodium content is similar to plasma but the chloride ion level is higher. Balanced isotonic solutions have sodium concentration similar to plasma but also have other electrolytes included in the solution such as chloride, potassium, magnesium, with concentrations similar to plasma.
In the initial stages of resuscitation unbalanced or balanced crystalloid isotonic solutions are the first line of treatment and should be used empirically. Glucose containing solutions should never be used for volume replacement as they can cause hyponatraemia and hyperglycaemia. Appropriate crystalloids for volume replacement include:
• 0.9% saline
o Unbalanced solution contains only Na and Cl
o Can cause metabolic acidosis if large volumes given
o Cheap and readily available
• Plasmalyte-148
o Balanced isotonic solution (Also contains K, Mg and Lactate in addition to NaCl)
• Hartmann’s Solution
o Balanced isotonic solution (Also contains K, Ca and Lactate in addition to NaCl)
Colloids
Colloid fluids contain electrolytes and large molecular weight particles such as starches, gelatins, dextrans or proteins. In contrast to crystalloids, colloids are relatively expensive and can cause allergic reactions
Other than 4.5% human albumin solution colloids are rarely used in paediatrics and are not recommended as first line in resuscitation.
Blood Products
The use of blood products is reserved for specific indications such as blood loss or coagulopathy. In trauma with on-going blood loss “flying squad” uncross-matched O-negative blood or uncrossed group specific blood may be used as first line treatment
First Line Medication in cardiorespiratory arrest
Adrenaline 1:10,000
Indications for use
• Cardiorespiratory arrest
o Non-shockable rhythm give as soon as possible
o Shockable rhythm give after third shock
• Bradycardia - HR< 60pbm with signs of inadequate circulation
• Fluid resistant shock when it is given as a continuous infusion
• Anaphylaxis
Dosage
Cardiac arrest
0.1ml/kg of 1:10,000 (10mcg/kg) IV or IO.
Repeated every 3-5 minutes in non-shockable and shockable rhythms
Anaphylaxis
Given intramuscularly, strength is 1:1,000
Available as self-injectable device (Epipen, Anapen etc)
Dose is dependent on age as below:
Age Dose 1:1,000 ml (mcg)
< 6m 0.1-0.15 ml (100-150mcg)
6m-6y 0.15ml (150mcg)
6-12y 0.3ml (300mcg)
>12y 0.5ml (500mcg)
Actions
Adrenaline stimulates both alpha and beta adrenorecptors. Stimulation of alpha receptors causes vasoconstriction and so increases diastolic and systolic blood pressure. This is thought to be the most important action in cardiac arrest as increasing diastolic blood pressure enhances coronary and cerebral perfusion.
Stimulation of the beta receptors increases the rate and force of contraction of the heart including the intensity of ventricular fibrillation which increases the likelihood of responding to defibrillation
Precautions
The effects of adrenaline may be reduced in an acidotic environment. Adrenaline is also inactivated by alkaline solutions and should never be given simultaneously with sodium bicarbonate. Administration should be via a separate cannula or followed by a 2-5ml flush.
Amiodarone
Indications for use
Shock resistant VF or pulseless VT
Dosage
5mg/kg maximum dose 300mg. Given after the third shock IV or IO
Actions
Membrane stabilising anti-arrhythmic
Precautions
Causes hypotension due to a mildly negative inotropic effect and vasodilatation. This is related to the rate of delivery. If given in VT with a pulse or SVT it should be infused over 20-minutes.
Lidocaine
Indications for use
Shock resistant VF or pulseless VT as an alternative to Amiodarone
Dosage
1mg/kg (max dose 100mg) IV or IO
Followed by an infusion
Actions
Anti-arrhythmic
Glucose
Indications for use
Hypoglycaemia - blood glucose < 3mmol/l
Dosage
2ml/kg of 10% glucose IV or IO
Sodium Bicarbonate
Indications for use
Sodium bicarbonate has a limited and unproven place in the management of paediatric cardiac arrest and is not a first line medication. It may be considered in severe metabolic acidosis (pH <7.1).
Dosage
0.5-1mmol/kg (0.5-1 ml/kg of 8.4% Sodium Bicarbonate)
Actions
Reverses blood acidosis but produces carbon dioxide which may worsen intracellular acidosis. May also can cause hypernatraemia and hyperosmolality depressing cardiac function.
Key Learning Points
• Fluid resuscitation starts with 10-20ml/kg bolus of an isotonic crystalloid such as 0.9% saline or Plasmaltye-148
• After each bolus the child should be reassessed to determine if further bolus is required.
• Once 30-40ml/kg have been administered consider intubation and use of inotropes.
• The main first-line medication in cardiorespiratory arrest is IV or IO adrenaline which can be repeated every 3-5 minutes if necessary.
References
Paediatric Immediate Life Support 2nd Edition Resuscitation Council UK
European Paediatric Advanced Life Support 5th Edition Resuscitation Council UK
Intravenous Fluid Management in Children
South Australian Paediatric Clinical Practice Guideline Department for Health and Wellbeing. Government of South Australia
Intravenous Fluid Bolus
Queensland Paediatric Emergency Care
Intravenous fluid therapy
Perth Children’s Hospital Government of Western Australia Child and Adolescent Health Service
Paediatric IV Fluid Prescribing Mind the Beep https://mindthebeep.com
ANZCOR Guideline 12.2 – Paediatric Advanced Life Support (PALS) https://www.anzcor.org
Learning Objectives
• To understand the indications for defibrillation
• To understand the indications for cardioversion
• Factors influencing the likelihood of a successful shock
• How to safely deliver a shock
Incidence of shockable rhythms
The initial rhythm in paediatric cardiac arrest is much more likely (80-90%) to be a non-shockable rhythm such as asystole or pulseless electrical activity (PEA), however a shockable rhythm such as ventricular fibrillation (VF) or pulseless ventricular tachycardia (pVT) occurs in 27% of paediatric inhospital cardiac arrests at some point during the resuscitation. The only effective treatment for VF or pVT is defibrillation which should be performed as quickly as possible. For every minute delay in defibrillating the chance of successful ROSC decreases by 10%.
Defibrillation
Defibrillation is a procedure where an electrical current is passed across the heart inducing global depolarisation and cardiac standstill. When the heart restarts the sinoatrial node is then able to reestablish sinus rhythm.
Defibrillation is delivered asynchronously in VF and pVT when it is important to deliver a shock as quickly as possible. An energy dose of 4J/kg is recommended for all shocks required to treat VF or pVT.
Defibrillators can also deliver a synchronised shock, where the shock is delivered at a particular point in the cardiac cycle. This is also called cardioversion. Synchronised shocks are used to treat supraventricular tachycardia (SVT) and ventricular tachycardia with a pulse (VT). Less energy is required for cardioversion which will be discussed later in this chapter.
Defibrillators deliver a biphasic waveform across the heart which is more effective and causes less myocardial damage than previously used monophasic waveforms. The shock is delivered via selfadhesive pads attached to the child’s chest. Self-adhesive pads do not move during chest compressions and enable defibrillation to be delivered at a safe distance from the child. Some pads also have sensors which can monitor the quality of the chest compressions being delivered.
Defibrillation is more effective if impedance to the flow of electricity is low.
Impedance is affected by:
• Pad size – the larger the pad the lower the impedance.
• Interface between the pad and the child’s chest – the pads should be applied firmly onto dry skin and smoothed to ensure no air is trapped underneath. Air will increase impedance.
• The position of the pads – the pads should “bracket” the heart.
• Chest wall thickness and obesity – impedance is lower when the distance between the pad and heart is short.
Manual
Manual defibrillators require the healthcare worker to analyse the cardiac rhythm to determine if a shock is required. Manual defibrillators can deliver a full range of energy requirements, catering for all sizes of children, they can also be used for cardioversion. They should be available in all healthcare settings dealing with infants and children.


AEDs are portable defibrillators available for public access and designed to be used by untrained rescuers. They are available in most public buildings including schools, sports centres, shopping centres, airports and workplaces. The availability of an AED is indicated by easily recognisable signs which will give the exact location and may include other BLS advice (see below).


Once switched on an AED will give audible step-by-step instructions advising what to do. The AED will analyse the cardiac rhythm and determine if a shock is needed. The AED will only deliver a shock if it detects a shockable rhythm. If a shock is needed the device will charge and prepare to deliver a shock. AEDS are pre-set for the energy dose which is usually set for an adult. AEDS with attenuators which reduce the energy dose are available and are safe to use even in children under 8-years of age.
Defibrillator pads are self –adhesive and applied to the chest to deliver a shock. There are smaller pads available for infants, but adult sized pads can also be used with adjustment of positioning.
Position of the pads
The pads should bracket the heart and not touch one another. Although the pads are generally labelled right and left and may have a picture indicating the correct placement it does not matter if the positions are reversed. If placed on the “wrong side”, they should not be removed and changed as this wastes time and causes loss of adherence of the pad.
Positioning of pads
• Anterior- posterior
One pad is placed on the front of the chest over the sternum and the other pad on the upper back in the midline.
• Antero-lateral
Place one pad on the right side of the chest below the clavicle. The other pad should be placed on the lower left chest in the mid-axillary line.
Positioning of defibrillator pads
Infants
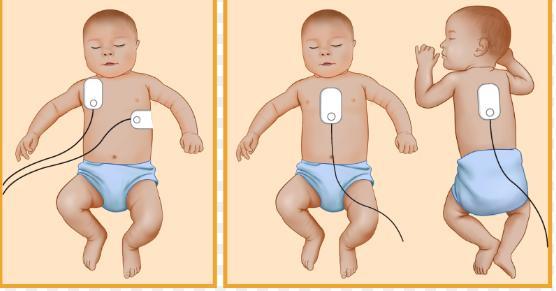
Anterio-lateral

Extra care needs to be taken when applying pads to children with implantable cardioverter defibrillator (ICD) devices or pacemakers and it is recommended that pads are placed at least 12cm from the ICD or pacemaker site.
Energy Levels
Manual defibrillator
An energy dose of 4J/Kg is used for all shocks. The exact energy dose for weight may not be available to select on the defibrillator in which case the next level up should be used e.g. for 12Kg child use 50J, as 48J is not available. Adult doses are set by the individual defibrillator at 120-200J and should not be exceeded for larger children.
In refractory VF/pVT the energy dose may be increased to 8 J/Kg after the sixth shock but expert advice should be taken before increasing dose. Adult doses should not be exceeded.
AEDs
The energy dose in AEDs is pre-set to adult levels unless the AED had an attenuator. The attenuator will lower the energy dose to 50-75J and it is recommended that in children less than 8-years the attenuator should be used. If there is no attenuator adult energy doses can be used. Children over 8years can be shocked at normal adult energy levels.
Timing of shock
A shock should be delivered as soon as a shockable rhythm has been identified. CPR should continue whilst the machine is charging to minimise time off the chest.
Safety
It is important to maintain safety to both the rescuers and patient during defibrillation and the following must be considered:
• Oxygen
Free flowing oxygen delivery devices (oxygen masks which may have been left on the bed) must be at least 1m away from the child.
If the child is ventilated via a sealed airway (ETT/SGA) the ventilation bag or ventilator tubing can be left connected.
• Dry surfaces
Wet clothing should be removed and the child dried
• Contact with patient
The person delivering the shock is responsiblefor ensuring safety and must check that they, other rescuers and relatives are NOT in direct or indirect contact with the child during delivery of the shock. There should be no contact between the pads and any metal objects, or transdermal medication.
• Operator instruction
Operators must issue clear, audible instruction to the rest of the team and bystanders.
BLS should be ongoing then the following should be performed in this order:
• Confirm cardiorespiratory arrest – (5 s simultaneous breathing, pulse/signs life check.)
• Immediately continue CPR (15:2).
• Attach ECG monitoring /self-adhesive pads.
• Briefly pause chest compressions to analyse underlying rhythm (< 5 s).
• If ECG displays VF resume chest compressions apply self-adhesive pads to the chest (if not already done so).
• Team Leader hands over safe defibrillation to defibrillator operator who:
1. Selects appropriate energy (4 J/ kg).
2. Clearly states “Chest compressions continue”.
3. Instructs “Everyone else to stand clear and remove oxygen whilst charging”.
4. Charges defibrillator.
5. When charged, the rescuer in charge of the defibrillator, instructs the chest compression provider to “Stand clear, ready to deliver a shock”.
6. Checks that everyone is clear and that patient still in VF/pVT.
7. Presses button to deliver shock safely.
• CPR recommences immediately without checking for a pulse or reassessing the rhythm.
• After 2-minutes CPR the team leader prepares for next pause to check rhythm.
• If still in VF/pVT deliver 2nd shock.
BLS should be ongoing then the following should be performed in this order:
• Confirm cardiorespiratory arrest – (5 s simultaneous breathing, pulse/signs life check).
• Immediately continue CPR (15:2).
• Switch on AED and attach self-adhesive pads.
• Await prompts from AED.
• Ensure that no-one touches the child whilst the AED analyses the cardiac rhythm and delivers a shock if required.
Cardioversion
Cardioversion is the timed delivery of an electric shock to the heart and is used in the treatment of VT with a pulse or decompensated supraventricular tachycardia (SVT). The shock is synchronised with the R wave of the ECG. The application of the pads and safety considerations are the same as with defibrillation as above but the following differences apply:
• Sedation/anaesthesia will need to be administered as the child will be conscious and cardioversion is painful and unpleasant if aware of it being performed.
• The synchronisation button on the defibrillator must be selected A marker appears on the R wave on the ECG indicating that the defibrillator is in synchronisation mode
• The energy dose is lower than for defibrillation at 1J/Kg for the initial shock increasing to 2J/kg if the first shock is not successful
• There is a delay in delivering the shock because of the synchronisation and so the button delivering the shock needs to be pressed for longer, until the shock has been delivered
• It is useful to have a continuous paper recording of the ECG running at the same time as the cardioversion as this can help the cardiologist to identify the underlying or provoking rhythm and the location of any recurrent entry pathway.
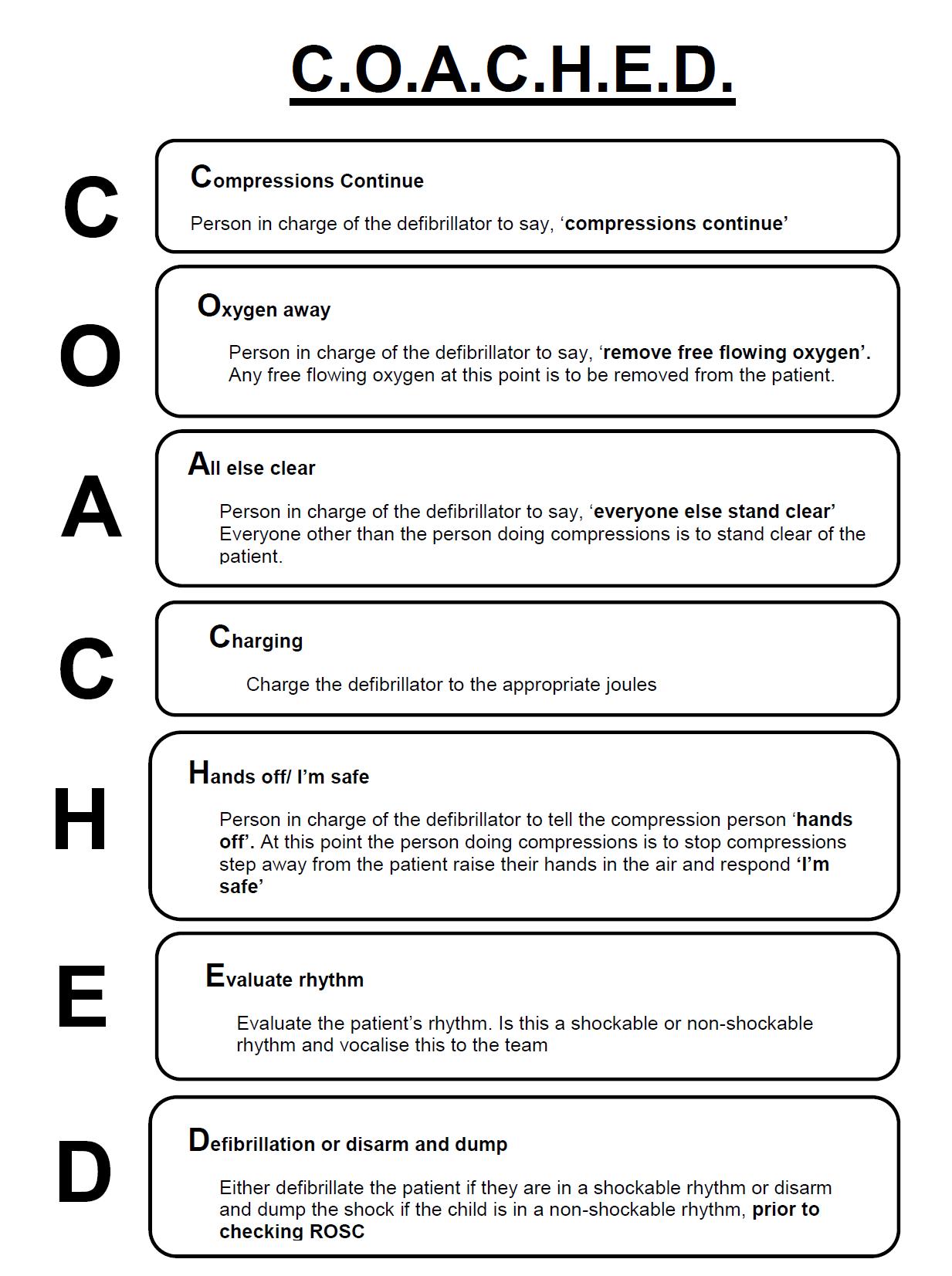
Key Learning Points
• Shockable rhythms occur in up to 27% of in hospital resuscitation attempts in children.
• For the child in VF or pulseless VT, defibrillation is the only effective way of restoring a spontaneous circulation.
• Manual defibrillators should be available in all healthcare facilities caring for children, but AED can be safely used in children.
• Use an AED if not confident with rhythm recognition.
• Energy dose for defibrillation shocks are 4J/kg.
• Energy doses for cardioversion are 1J/Kg increasing to 2J/kg if necessary.
• Chest compressions should be interrupted as little as possible during defibrillation.
• Good communication and teamwork is essential when delivering a shock.
References
ANZCOR Guideline 7 – Automated External Defibrillation in Basic Life Support https://www.anzcor.org
Paediatric Immediate Life Support 2nd Edition Resuscitation Council UK
European Paediatric Advanced Life Support 5th Edition Resuscitation Council UK
Defibrillation
Amandeep Goyal; Lovely Chhabra; Joseph C. Sciammarella; Jeffrey S. Cooper Stat Pearls, National Library of Medicine https://www.ncbi.nlm.nih.gov
Defibrillation in children
Haskell, Sarah E; Atkins, Dianne L
Journal of Emergencies, Trauma, and Shock 3(3):p 261-266, Jul–Sep 2010. | DOI: 10.4103/0974-2700.66526
Pictures Various AEDs https://defibsupplies.co.uk
Position of pads https://www.australiawidefirstaid.com.au
Learning Outcomes are to:
• Understand the normal ECG trace.
• Recognise cardiac arrhythmias associated with cardiorespiratory arrest.
• Understand how to manage bradycardia.
• Understand how to differentiate between sinus tachycardia (ST) and supraventricular tachycardia (SVT).
• Understand the priorities of management in children with compensated and uncompensated tachyarrhythmias.
ECG Monitoring
Once optimal ventilation and oxygenation have been established, all seriously ill children should have their ECG monitored. This allows for continuous monitoring of their heart rate and also allows for assessment of the heart rhythm.
The heart rate in children varies with age with younger children having higher resting heart rates. Heart rate will also vary with level of arousal, pain, fever etc.
See below for a guide to normal heart rate across childhood.
Age Mean Awake Asleep
0-3 m 140 85 - 205 80 - 140
3 m-2 y 130 100 - 180 75 - 160
2 y-10y 80 60 - 140 60 - 90 >10y 75 60 - 100 50 - 90
Cardiac arrhythmias are rare in childhood and are more likely to be the result of an underlying illness rather than a primary cardiac abnormality. Children with acquired or congenital heart disease can however, present with a primary arrhythmia. Electrolyte disturbances and some medications or toxins can also cause arrhythmia in childhood.
Basic Electrocardiography
The ECG from lead II is usually selected on the cardiac monitor or defibrillator to assess the cardiac rhythm. The ECG trace represents the electrical activity of the heart. It does not reflect cardiac output and so the child’s clinical status needs to be assessed alongside the ECG trace. The electrodes can fall off mimicking asystole and vibrations transmitted to the leads may mimic VF.
Treat the child and not the trace.
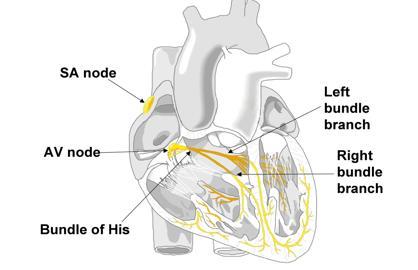
The electrical impulse for the heartbeat starts at the natural pacemaker of the heart, the sinoatrial (SA) node, which is in the right atrium. The impulse spreads to both atria stimulating atrial contraction.
The impulse reaches the atrioventricular (AV) node where there is a brief delay. This ensures that there is enough time for the atria to empty into the ventricles.
The impulse then spreads via the Bundle of His into the right and left bundle branches and into the Purkinje fibres deep in the myocardial cells. This causes contraction of the ventricles.
As the ventricles contract the AV valves shut and blood is pumped from the right ventricle to the pulmonary artery and from the left ventricle into the aorta.
Blood in the pulmonary artery goes to the lungs where gas exchange takes place.
Blood in the aorta goes to the coronary arteries and systemic arterial system providing blood to the rest of the body.
The atria are filling whilst the ventricles are emptying in preparation for the next heartbeat. The ventricles, once empty, need to repolarise and relax so that they can fill ready for the next contraction.
The normal ECG produces a trace on the monitor or on a paper record that is shown below. It consists of P, QRS, and T waves, and PR, QRS, and QT intervals.
The P wave represents atrial depolarisation and contraction
The QRS represents ventricular depolarisation and contraction
The T wave represents QRS repolarisation
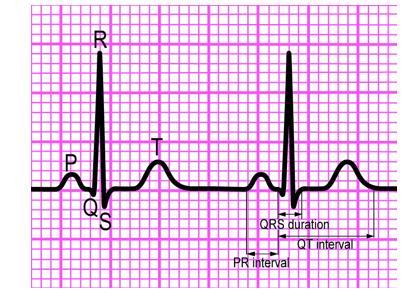
Standard ECG paper is composed of small squares and the paper speed is 25mm/sec, so one small square represents 0.04 sec, and the larger squares which are five small squares represent 0.2 sec. On a paper recording every fifteen large squares (3 secs) there are triangular indicators at the top of the paper. Thirty large squares (or the time between 3 triangular markers) represents 6 secs. The heart rate can be calculated by counting the number of complexes in thirty large squares and multiplying by 10.

The ECG below shows a heart rate of 30 bpm.
Managing cardiac rhythm disturbance depends on four factors which are:
• Presence of a circulation
• Clinical status
• Heart rate
• Width of QRS complex
Presence of a circulation
ABCDE assessment can be used to determine if there signs of life and if there is a circulation with a central pulse palpable.
Absent pulse
The child is in cardiorespiratory arrest. Start CPR and attach ECG monitor.
Rhythms associated with cardiorespiratory arrest are:
VF or pulseless VT when the priority of management is effective CPR and rapid defibrillation
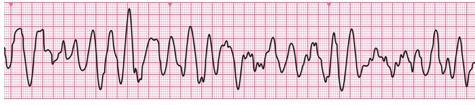

Or Asystole or PEA where the management priorities are effective CPR and adrenaline.
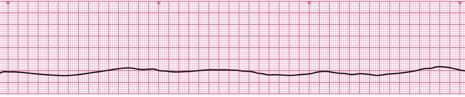

Follow the Paediatric Advanced Life Support (PALS) algorithm for shockable and non-shockable cardiorespiratory arrest. Consider and treat reversible causes.
If there are signs of life and a central pulse is palpable assess the child further as below to determine:
• Clinical status
• Heart rate
• Width of QRS complex
Clinical status
Determine if the child is in compensated or decompensated circulatory failure.
Compensated Circulatory Failure
The child will be conscious with a normal blood pressure for age. The ECG should be attached and the rhythm determined. As the child is stable there is usually time to gain intravenous access and seek expert help from a cardiologist. Anaesthetic help may also be required.
Decompensated Circulatory Failure
The child will have a reduced level of consciousness, prolonged CRT, weak/impalpable peripheral pulses and be hypotensive. An ECG should be attached, intravenous access attempted and expert urgent help from anaesthetics sought.
Heart rate
Varies with age but the defining heart rates are shown below:
Age Bradycardia Tachycardia
< 1yr < 80 bpm > 180 bpm
> 1yr < 60 bpm > 160 bpm
Bradycardia

The commonest cause of bradycardia is hypoxia and acidosis due to respiratory or circulatory failure. It may be a pre-terminal rhythm prior to cardiorespiratory arrest. If there are signs of decompensation, 100% oxygen should be administered, respiration supported and if the heart rate is less than 60 chest compressions started. Adrenaline should be given if there is no improvement with oxygenation and chest compressions.
Atropine should be considered if the bradycardia is likely to have been vagally induced by suctioning or intubation. Rarely pacing is required.
Tachycardia
Tachycardia can have a narrow or broad QRS complex. Usually QRS lasts 1-2 small squares.
Narrow Complex Tachycardia
The two causes of narrow complex tachycardia are sinus tachycardia and supraventricular tachycardia (SVT).
Sinus tachycardia

Sinus tachycardia is a normal physiological response to anxiety, pain, or fever or arises to compensate for anaemia, hypovolaemia etc. In sinus tachycardia P waves will be clearly visible on the ECG. The onset is usually gradual and there will be some beat-to-beat variation in heart rate. In infants the heart rate is usually 180-220 bpm and in children 160-180 bpm.
The treatment of sinus tachycardia is treatment of the cause of the tachycardia. Treatment will result in a gradual reduction of heart rate.
Supraventricular Tachycardia (SVT)

In SVT the sinoatrial node is no longer acting as the pacemaker for the heart and there is usually an accessory pathway between the atria and ventricles. This pathway by-passes the AV node and transmits impulses more quickly than usual causing the tachycardia
In SVT the heart rate is normally very fast with rates greater than 220 bpm in infants and greater than 180 bpm in children. The onset is usually sudden and P wave are not seen consistently on the ECG.
Compensated SVT can be treated with manoeuvres that increase vagal tone such as the diving reflex where a plastic bag filled with ice and water is placed on the infant’s or child’s face, or by wrapping the infant’s arms in a towel and immersing the whole face in an ice water slurry for 5-seconds. Older children can be asked to perform Valsalva manoeuvre by getting the child to blow through a straw or to attempt to blow the barrel out of a syringe. If these fail then chemical or electrical cardioversion is required. If intravenous access is in situ and the child is still compensating, adenosine can be administered but if unsuccessful synchronised cardioversion will be required (starting dose 1J/kg increasing to 2J/kg) This will require anaesthetic support to ensure adequate sedation and analgesia.
Children who are decompensated should receive synchronised cardioversion. Anaesthetic support may be required to administer sedation and maintain the airway. Ketamine intra-nasally or intramuscularly should be used for sedation and analgesia if venous access is difficult as cardioversion should not be delayed.
Amiodarone may be required for refractory SVT but expert cardiology guidance should be sought.
Broad Complex Tachycardia
Broad complex tachycardia is rare in childhood. There are two possible causes, ventricular tachycardia (VT) and SVT with aberrant conduction. Differentiation between these two rhythms is immaterial as they are both treated with synchronised cardioversion. Ventricular tachycardia is a broad complex regular tachycardia with no visible P waves. It can present with or without a pulse. Treatment for VT with a pulse, is synchronised cardioversion. Amiodarone may be required for refractory VT but expert cardiology guidance should be sought.
Pulseless VT is treated by defibrillation at 4J/kg as discussed above.
Drug treatment of arrhythmias

Key Learning Points
• In children life threatening arrhythmias are more likely the result rather than the cause of acute illness.
• The commonest arrhythmia seen in children is bradycardia and asystole as a result of hypoxia; oxygenation is the first line of treatment
• Tachycardia may be narrow complex (sinus tachycardia or SVT) or broad complex (VT or SVT).
• SVT can be treated medically or by synchronised cardioversion depending on the clinical state of the child.
• Broad complex tachycardia is always treated with synchronised cardioversion
References
ANZCOR Guideline www.anzcor.org
Guideline 12.3 Management of other (non-arrest) arrhythmias in infants and children
European Paediatric Advanced Life Support 5th Edition
Resuscitation Council UK
Paediatric Immediate Life Support 2nd Edition
Resuscitation Council UK
Cardiology Teaching Package
Practice Learning Resources
The University of Nottingham www.nottingham.ac.uk/nursing/practice/resources
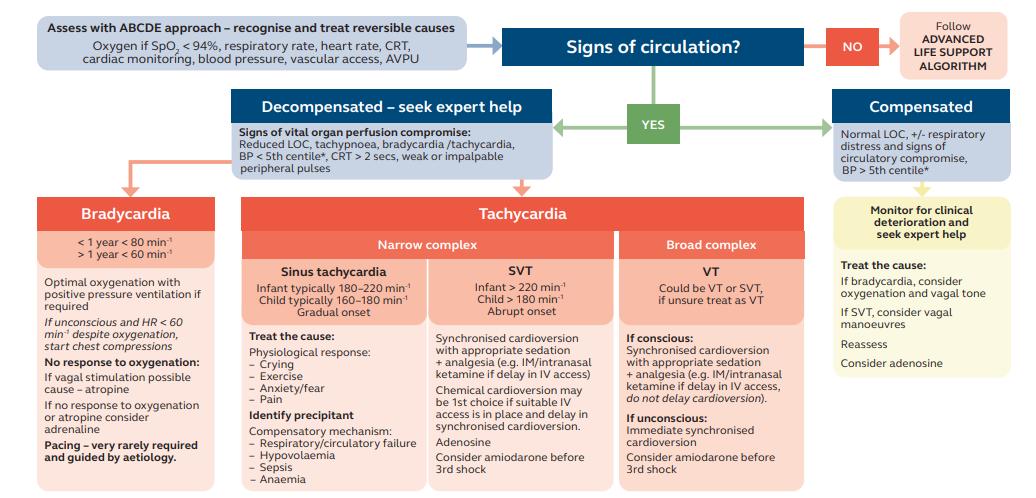
Learning Outcomes to:
• Understand the Paediatric Advanced Life Support Algorithm
• To understand how to recognise and treat non-shockable rhythms
• To understand how to recognise and treat of shockable rhythms
• Consider and treat the reversible causes of cardiorespiratory arrest
Resuscitation is a continuous process from basic life support to advanced life support. High quality basic life support provides the most important foundation for successful resuscitation. All clinical staff within a healthcare facility should be able to:
• Immediately recognise cardiorespiratory arrest
• Start appropriate BLS with adjuncts if necessary
• Summon the clinical emergency team
The epidemiology, pathophysiology and aetiologies of paediatric cardiac arrest are different from adult or newborn cardiac arrests.
• Cardiorespiratory arrest in infants and children is usually secondary to hypoxia caused by an underlying respiratory illness or shock.
• Hypoxia affects all organs but in the heart leads to bradycardia, asystole and PEA.
• The outcome after successful return of circulation (ROSC) is poor as there has been preceding multi-organ hypoxia and dysfunction.
• There is less than a 5% survival rate without neurological sequelae following ROSC.
• As there is usually an underlying illness there is progressive deterioration with recognisable clinical signs; timely medical interventions can prevent deterioration to cardiorespiratory arrest (See recognition of the seriously ill child).
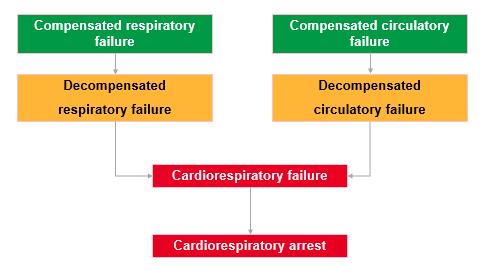
When a child suffers cardiac arrest in a clinical area staff should be able to promptly initiate BLS and summon the clinical emergency/resuscitation team. Appropriate equipment and trained staff should be available. Resuscitation teams will differ daily depending on rotas and working patterns. It is invaluable that the team “huddles” at the beginning of each shift to introduce themselves to each other, discuss the team member’s skills and assign roles. Huddles can also be used to identify patients at high risk of deterioration.
All healthcare providers should be able to recognise cardiorespiratory arrest A single rescuer must not leave the child but should start BLS and summon more help by shouting or pulling the emergency buzzer.
As soon as a second rescuer arrives they should be sent to activate the emergency team and return with readily available emergency equipment
Paediatric advanced life support (PALS) builds on high quality paediatric basic life support (BLS) which should be on-going.
Once the monitor/AED has been attached stop CPR briefly to assess the underlying heart rhythm and decide if the child is in a non-shockable (asystole, profound bradycardia or PEA) or shockable rhythm (VF or pVT) and treat according to the PALS algorithm as below.
Cardiac arrest rhythms
Non shockable
• Asystole
No electrical activity in the heart. “Flat lined”.

• Severe bradycardia <60pbm
• Pulseless electrical activity PEA (co-ordinated electrical activity on ECG but no pulse)

Shockable
• Ventricular fibrillation VF
Chaotic electrical activity “very funny”. Can be coarse or fine.
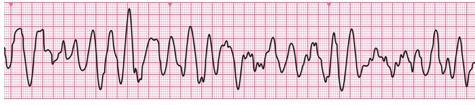
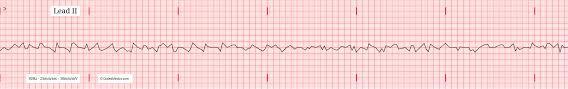
• Pulseless ventricular tachycardia pVT
Broad regular complexes. “Very tidy”. No pulse detectable.
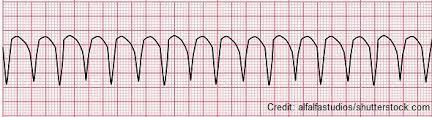
Management
Non-shockable rhythms

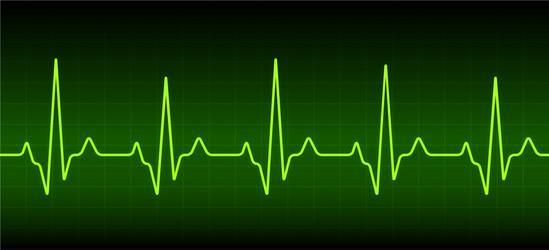
Asystole (Asy) PEA or bradycardia < 60bpm
Management
• Continue CPR with ventilation and chest compressions.
• Gain IV/OI access if no peripheral or central venous access already in situ.
• Administer Adrenaline 10mcg/kg (0.1ml / kg 1:10,000).
• Pause briefly every 2-minutes to check rhythm.
• If in VT or rhythm compatible with life, check a central pulse. If still in a non-shockable rhythm continue CPR, repeat Adrenaline (10mcg/kg) every 3 – 5 minutes.
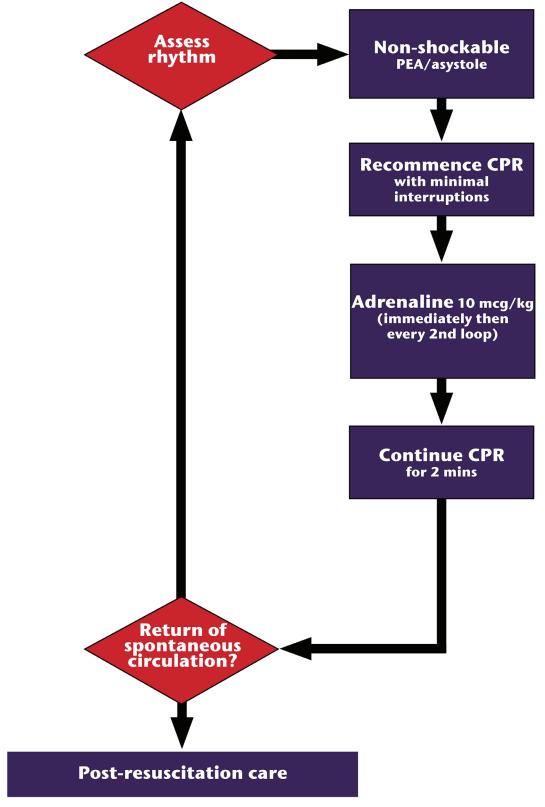
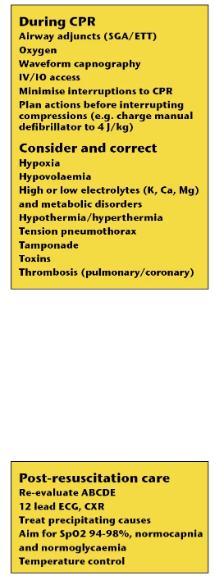
Consider reversible causes 4 H’s & 4 T’s and treat
4 H’s
• Hypoxia ensure ventilating and giving oxygen.
• Hypovolaemia give fluid bolus 10ml/kg of isotonic fluid.
• Hypo/Hyperthermia check temperature and warm or cool as required.
• Hyperkalaemia, Hypocalcaemia check electrolytes on blood gas and treat.
4 T’s
• Tension pneumothorax examine chest thoroughly. Signs of tension pneumothorax include tracheal deviation away from the side of the pneumothorax, hyperexpansion and hyper-resonance with reduced breath sounds on affected side. Immediate treatment is to perform needle thoracostomy in the 2nd intercostal space of the affected side. Follow up with insertion of a formal chest drain.
• Thromboembolism is rare in childhood, ECG and CXR may suggest PE. Sickle cell disease may also be a predisposing factor.
• Toxins take urine for toxicology and treat as necessary.
• Tamponade can occur post cardiac surgery or with stab wound. It is diagnosed by echocardiogram or POCUS. Treatment is emergency pericardiocentesis.
Shockable Rhythms VF pVT
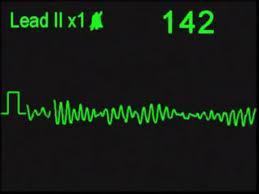
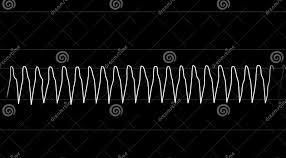
These rhythms are more likely if there is an underlying cardiac defect, and if a primary event will cause sudden collapse; they can also arise during a resuscitation attempt. Rapid defibrillation is the key to ROSC and should not be delayed. For every minute delay in defibrillation the chances of successful ROSC decreases by 10%.
Management
• Administer DC shock of 4J/kg if using manual defibrillator. An AED can be used with or without an attenuator depending on age and size of the child.
• Resume CPR immediately after delivering shock. DO NOT pause for pulse check.
• After 2-minutes pause CPR briefly to reassess rhythm.
• If in VT or rhythm compatible with life, check a central pulse. If still in VF or pVT give a 2nd shock of 4J/kg and immediately resume CPR.
• Give Adrenaline 10mcg /kg 0.1ml/kg 1:10,000 (max dose 1mg i.e. 10ml) after the second shock.
• After 2-minutes pause CPR briefly to reassess rhythm. If in VT or rhythm compatible with life check central pulse. If still in VF or pVT give 3nd shock 4J/kg and immediately resume CPR.
• Give Amiodarone 5mg /kg (max dose 300mg) or Lidocaine 1mg /kg (max dose 3mg/kg up to 300mg) after the 3rd shock.
• Continue to give Adrenaline 0.1ml /kg 1:10,000 every 3-5 minutes (every second shock/alternate cycles) and to deliver shocks every 2-minutes whilst the child remains in a shockable rhythm.
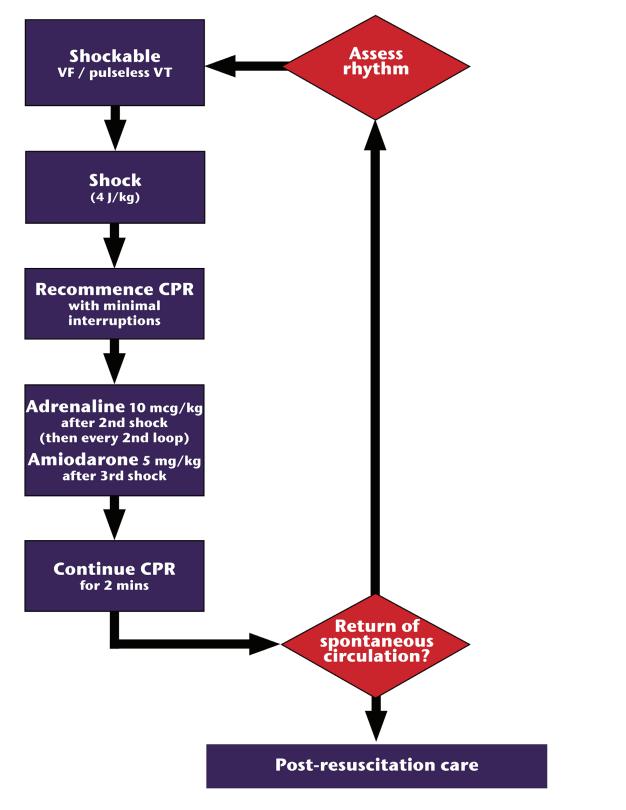
Consider reversible causes 4 H’s & 4 T’s and treat.
General Considerations
Airway management
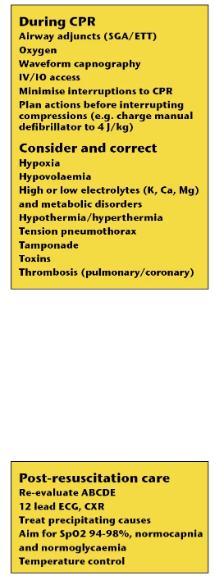
The majority of children can be adequately ventilated with BVM in the initial stages of resuscitation; insertion of a supraglottic device (laryngeal mask airway or igel®) is generally achieved quickly and easily and so should be considered if anaesthetic help is not immediately available. Once medical staff skilled in intubation is available intubation may be attempted as long as it does not interfere with oxygenation and chest compressions. Tracheal intubation is the most reliable way to secure an airway, once an endotracheal tube is in situ chest compressions can be performed continuously provided that they do not interfere with delivery of ventilation breaths.
Ventilation rates vary with age and the following is recommended during resuscitation.
Age Rate/min
Infants 25
1-8 y 20
8-12 y 15
>12y 10 - 12
End-tidal carbon dioxide detection (calorimetric or capnographic) must be continuously monitored once an SGA or ETT is in place.
Oxygen
100% oxygen should be used to ventilate the child during CPR.
Chest compressions
Compressions should be performed:
• at a rate of 100-120 per minute
• at a depth of 1/3 of the chest (infants 4cm, child 5cm)
• allowing for full recoil
• using a ratio of 15:2 (compressions:breaths) unless intubated when they may be continuous
• with minimal pauses, which should be planned
High quality chest compressions are important to maximize the chances of CPR but are very tiring. The quality of chest compressions deteriorates when rescuers fatigue and so it is recommended to change the person performing chest compressions every 2-minutes.
Vascular access
Vascular access will be required for administration of medicines and fluids.
Use existing peripheral or central lines if in situ and patent. If not insert an intravenous cannula. If after 3 attempts or 90 seconds a cannula has not be sited insert an intraosseous cannula.
Consider reversible causes 4 H’s and 4 T’s and treat as above.
Stopping Resuscitation
The decision to stop resuscitation should be based on a combination of factors including:
• Pre-arrest status and likely outcome:
o In some cases, such as terminal cancer, when death is inevitable continuing CPR is futile.
o Children with other life-limiting conditions or severe disabilities may not survive further tissue or brain damage.
• Duration of arrest and response to resuscitation:
o In infants and children the cause of cardiorespiratory arrest is usually progressive hypoxia and hypotension causing irreversible damage to all of the organs and it is unlikely that ROSC will be achieved after 30-minutes of continuous good quality CPR.
o Prolonged resuscitation may be performed in infants and children with hypothermia or those in persistent VF or pVT.
o Prolonged resuscitation may be considered in cases of poisoning whilst awaiting response to a specific treatment or anti-toxin.
• Remediable factors:
o Reversible causes (4H’s and 4T’s) should have be considered and treated.
• Opinions of experienced personnel:
o The team leader is usually the most experienced member of the team and ultimate responsibility to stop resuscitation will lie with them, however, the decision to stop should be the collective decision of the whole team.
• Wishes of the parents or guardians:
o Resuscitation may be continued whilst awaiting the arrival of the parents or guardians.
o The wishes of the parents must be asked for and considered, however, the final decision regarding stopping lies with the team leader.
• Availability of ECMO:
o This can provide on-going life support if there is severe lung disease which is reversible.
The opportunity to be present during the resuscitation of their child should be offered to all parents. Studies have shown that it helps with the grieving process. If parents are present the following should be considered:
• A specific member of staff should remain with the parents to offer support. An interpreter may also be required.
• Physical contact with their child should be encouraged as long as it does not interfere with the resuscitation.
• If resuscitation is unsuccessful parents should be given the chance to say goodbye to their child.
Children in cardiac arrest always test the readiness, skills and abilities of individuals and organisations. A cardiac arrest may result from a preventable deterioration of a child’s condition, and can also result following a mishap or rarely may be sudden and unexpected. Following a resuscitation, a debrief discussion should take place as soon as possible with everyone involved. This allows for the team to reflect on their actions and identify areas for improvement.
The psychological impact of the events surrounding cardiac arrest of a child on healthcare staff should not be ignored and a separate debrief to share personal feelings and reactions with others and to vent emotions may be held separately.
One member of the team should be allocated the role of scribe during the resuscitation to record timings and doses of medications etc. After the resuscitation the team leader should carefully document the resuscitation sequence of events and response to treatment with help from the scribe and other members of the team.
Team members should be listed with their responsibilities and timing of events should be recorded as accurately as possible.
• Paediatric cardiorespiratory arrest is usually secondary to hypoxia or shock which leads to bradycardia or asystole.
• Asystole is a non-shockable rhythm and successful resuscitation depends upon high quality CPR and the administration of adrenaline.
• Shockable rhythms such as ventricular fibrillation and pulseless ventricular tachycardia are much rarer in childhood but do occur. Successful resuscitation depends upon timely defibrillation with high quality CPR. Medication may be required if the arrhythmia does not immediately respond to defibrillation.
• Reversible causes should be considered and treated during resuscitation for both shockable and non-shockable rhythms.
• Parents should be encouraged to be present during resuscitation of their child.
References
ANZCOR Guideline www.anzcor.org
Guideline 12.2 Paediatric Advanced Life Support (PALS)
European Paediatric Advanced Life Support 5th Edition
Resuscitation Council UK
Paediatric Immediate Life Support 2nd Edition
Resuscitation Council UK
British National Formulary for Children BNFC https://bnfc.nice.org.uk
Resuscitation – Advanced Life Support Algorithm
Child/Infant unresponsive & not breathing normally Basic Life Support Algorithm
Commence CPR Chest Compressions (15:2 once BVM available) (rate 100 – 120 compressions per minute)

Shockable (VF/ pulseless VT)
During CPR
1 Shock 4j/kg or AED (attenuated as appropriate)
Immediately resume CPR 15 Chest Compressions: 2 Ventilations FOR 2 MINUTES Minimise interuptions

• Ensure good quality CPR –rate, depth, recoil
• Plan actions before interrupting CPR
• Give oxygen
• Attempt/verify IV/IO access
• Give adrenaline 3 – 5 minutes (10mcg/kg, 1:10,000)
• Correct Reversible Causes (see below)
• Consider advanced airway (LMA)
• Give uninterrupted compressions when airway secure
•Consider: ➢ amiodarone after 3rd shock if available
REVERSIBLE CAUSES
Hypoxia Tension pneumothorax
Hypovolaemia Tamponade, cardiac
Hypo/hyperkalaemia/metabolic Toxins
Hypothermia Thrombosis (cardiac or pulmonary)
Consider ultrasound imaging to identify reversible causes ALL REVERSIBLE CAUSES SHOULD BE EXCLUDED OR TREATED WHERE POSSIBLE

Activate emergency team/ambulance service
Infant = under 1 Child = 1 to 18
Non-Shockable PEA/Asystole)
Immediately resume CPR 15 Chest Compressions: 2 Ventilations FOR 2 MINUTES Minimise interruptions
If ROSC achieved:
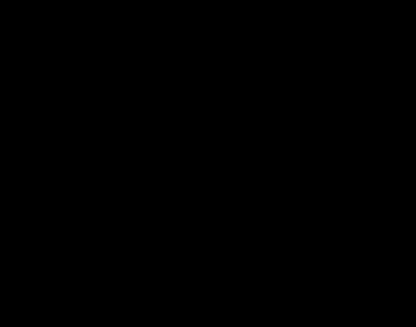
Assess patient A, B, C, D, E
Post event ECG
Secure additional access
Consider catheterisation
Aim for SpO2 of 94 – 98% and normal PaCO2
Targeted Temperature Mgt
Contact relatives
Remember care of family
Learning Outcomes
• Identify common paediatric illnesses
• Understand how the ABCDE approach to assess common paediatric illnesses guides initial treatment
The illnesses and emergencies covered are:
• Anaphylaxis
• Asthma
• Sepsis
• Seizures
• Hypoglycaemia
Anaphylaxis
Anaphylaxis is a severe, whole body, potentially life threatening, allergic reaction. It accounts for 20 deaths per year in Australia and can happen very quickly, usually within minutes of contact with an allergen. The diagnosis is made clinically as there is no diagnostic test for anaphylaxis. The commonest allergens that cause anaphylaxis in children are foods, medicines or insect stings. The only effective treatment for anaphylaxis is Adrenaline: once diagnosed it should be promptly treated with Adrenaline. If in doubt give Adrenaline.
Pathophysiology
Exposure to a triggering allergen leads to release of histamine and other mediators from mast cells in the skin, gut, heart, blood vessels and respiratory tract. The chemical mediators include histamine and typtase. There is also stimulation of the production of prostaglandins, leukotrienes and cytokines. These mediators lead to smooth muscle contraction and increased vascular permeability leading to tissue oedema, bronchospasm and distributive shock. Symptoms may be mild or moderate at first but quickly worsen to a severe reaction. Anaphylaxis can be fatal if not treated promptly with food allergens causing death within 30-minutes, insect stings within 10-15 minutes and by intravenous medication within 5minutes. Food is the commonest allergen causing anaphylaxis in children.
Commonest allergens causing anaphylaxis.
Source of allergen
Commonest allergens
Food Peanut, tree nuts, cow’s milk, egg, fish, sesame seeds, shellfish, wheat, mustard, soya, celery
Medicine
Antibiotics (Penicillins, Cephalosporins)
Anaesthetics, muscle relaxants
NSAIDs
Chlohexidine
Insect stings Bee sting
Others Latex, exercise, idiopathic
Symptoms of anaphylaxis include:
• Hives, welts or generalise erythema
• Swelling of the face, eyes, lips, and tongue
• Tingling of the mouth, tightness in the throat
• Difficulty breathing, stridor, wheeze
• Abdominal pain and vomiting (in insect stings)
• Dizziness or collapse
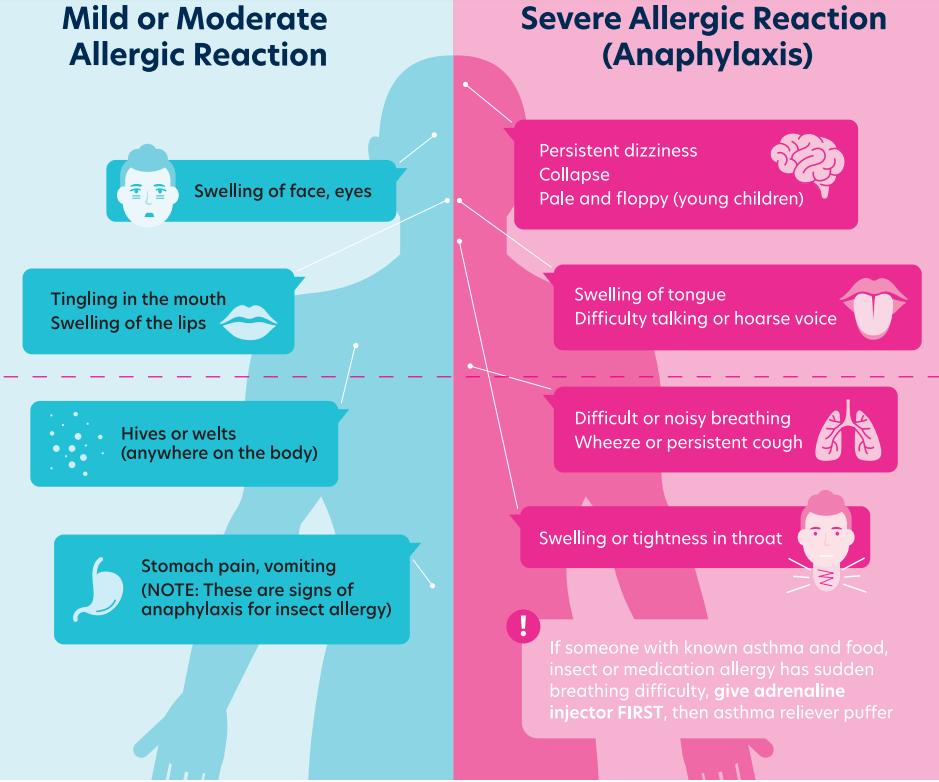
Recognition of Anaphylaxis ABCDE Approach
Airway
• The airway may be at risk because of swelling to the tongue and throat.
• There may be a hoarse voice or stridor due to laryngeal oedema.

• There is usually signs of increased work on breathing with tachypnoea, recession or tracheal tug.
• There may be respiratory arrest.
• Wheeze is heard on auscultation. Although wheeze the hallmark of asthma it may also be heard in bronchiolitis, foreign body aspiration and anaphylaxis. The volume of the wheeze does not directly correlate to the degree of airway narrowing and an increase in the volume may indicate improvement in their condition. A very quiet wheeze or SILENT chest is an ominous sign.
• Reduced oxygen saturation or cyanosis.
Circulation
• There will be tachycardia with signs of shock such as cool peripheries and prolonged CRT.
• Blood pressure will be low and may cause dizziness, collapse or cardiac arrest.
Disability
There may be confusion, agitation or loss of consciousness
Exposure
There may be hives, wheals or urticaria. Skin changes are often the first sign to be present but can be subtle. The rashes are intensely itchy.
ACTIONS
Remove the suspected allergen if possible, then treat liethreatening features
Airway
• Open the airway
Breathing

• Give 100% oxygen via non-rebreathe mask or support ventilation with BVM
Circulation
• Do not allow the patient to stand, they should lie flat or sit.
• GIVE INTRA-MUSCULAR 1:1,000 ADRENALINE and repeat every 5-minutes if features do not resolve. The dose may be drawn from an ampoule or given from an auto-injector device (Anapen or EpiPen).
Dose of adrenaline
IF IN DOUBT GIVE
10% of cases of anaphylaxis require a second dose of Adrenaline.
• Gain intra-venous or intra-osseous access.
Give 10ml/kg bolus of balanced isotonic fluid or 0.9% saline. Repeat as required.
Note Antihistamines are not recommended for the treatment of anaphylaxis. They may be useful for cutaneous symptoms of itching after stabilisation.
Corticosteroids are not recommended for the treatment of anaphylaxis but they may be useful after stabilisation or in refractory shock.
The diagnosis of anaphylaxis may be confirmed by measuring serum mast cell tryptase immediately after the event, 1-2 hr after and at 24 hr.
All patients requiring Adrenaline should be observed in hospital for at least 4-hours after treatment. After discharge they should be referred to a specialist allergy clinic for an anaphylaxis action plan and an adrenaline auto-injector prescription.
Anaphylaxis Action Plan

Anaphylaxis is said to be refractory if on-going treatment is required after 2 doses of intra-muscular adrenaline. Expert help will be required. Treatment consists of repeated intramuscular adrenaline and fluid bolus until an intravenous low-dose adrenaline infusion via a peripheral vein can be started. Ongoing respiratory support may require nebulised salbutamol, BVM or intubation.
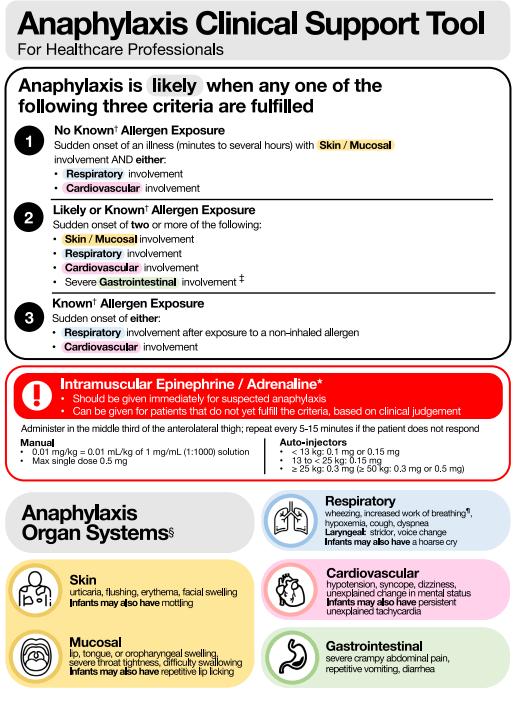
Asthma
Asthma is a common chronic inflammatory disease of the lungs. The inflammation leads to variable airway obstruction due to excessive mucus production and hyper-responsiveness of the smooth muscle in the airways. In childhood it can cause mild daily symptoms such as cough but for most children it is episodic with “acute asthma attacks” causing cough, shortness of breath, chest tightness and wheeze.
8.7% Australian children under the age of 15-y have asthma (411,000 children) with 42% of them having to take time off school because of their asthma.
Acute asthma can be life-threatening; cardiac arrest can be caused by hypoxia, tension pneumothorax, or by arrhythmias due to drugs or electrolyte imbalance.
Intubation and mechanical ventilation can be very difficult in acute asthma so it is important to treat promptly before there is respiratory failure or arrest.
Recognition of Acute Asthma ABCDE Approach
Airway
• Usually open but can become at risk of obstruction if conscious level reduced.
Breathing
During an acute asthma attack there will be:
• Signs of increased work on breathing with tachypnoea, recession or tracheal tug.
• Wheeze is heard on auscultation. The volume of the wheeze does not directly correlate to the degree of airway narrowing and an increase in the volume may indicate improvement in their condition. A very quiet wheeze or SILENT chest is an ominous sign.
• Reduced oxygen saturation or cyanosis.
Severity of acute asthma
Mild/Moderate
Can walk, speak in whole sentences
SpO2 >94%
Circulation
Unable to speak in sentences Visibly breathless Increased WOB
SpO2 90-94% in air
Collapse Exhausted Poor respiratory effort
SpO2 <90%
• May have compensatory tachycardia but may be normal.
Disability
• There may be confusion, agitation or loss of consciousness due to hypoxia.
Exposure
• The child may be febrile if infection has triggered the acute attack.
Airway
• Open airway
Breathing
• Apply pulse oximeter
• Give oxygen 15l/min via non-rebreathe mask or support ventilation with BVM
• Give Salbutamol ± Ipratropium by MDI or nebulised with oxygen and review. Repeat as required
• Give oral or intra-venous steroids
• Consider Magnesium Sulphate, intravenous Aminophylline or Salbutamol if little response to nebulised salbutamol. See table below.
• Gain vascular access for medication
Summary of Treatment Acute Asthma
Can walk, speak in whole sentences
SpO2 >94%
Salbutamol MDI
Repeat every 20-30 mins
Steroids
Unable to speak in sentences Visibly breathless Increased WOB SpO2 90-94% in air
Salbutamol MDI Ipratropium MDI OR
Salbutamol/Ipratropium nebulised in O2 Repeat every 20- mins Steroids (Prednisolone) Magnesium Sulphate i.v. Aminophylline or Salbutamol
Drowsy Collapse Exhausted Poor respiratory effort
SpO2 <90%
Salbutamol/Ipratropium nebulised continuously Steroids (hydrocortisone) Magnesium sulphate Intubation
Sepsis
Infections are the most common reason for children to attend the emergency room. Most infections are mild viral self-limiting illness with fever; some are more serious such as bacterial infections of the respiratory tract e.g. pneumonia or urinary tract infection e.g. pyelonephritis.
Sepsis is defined “a life-threatening organ dysfunction caused by a dysregulated host response to infection”. The immune system essentially goes in to overdrive and the body’s inflammatory response to an infection injures its own tissues and organs. Viral, bacterial and fungal infections can lead to sepsis.
Sepsis is more likely to affect very young children especially those less than one year old.
The first stage of sepsis in children can be difficult to distinguish from simple infection. Sepsis, however, quickly leads to shock, multiple organ failure and death if not promptly recognised and treated. Even if treated promptly 50% of sepsis survivors have long term sequelae. Most countries now have a national sepsis programme and toolkits such as “Sepsis Six” to help with early identification and management.
Pathophysiology
• An infection triggers a local inflammatory response.
• Release of inflammatory mediators (TNF, interleukins, prostaglandins from WBC and macrophages) cause systemic inflammatory response syndrome (SIRS).
• The mediators activate coagulation and inhibit fibrinolysis leading to microvascular thrombosis which impairs oxygen delivery to tissues leading to organ dysfunction.
• The mediators also cause vasodilatation and dysfunction of the vascular endothelium which leads to distributive shock.
• The mediators may also have a direct effect on the myocardium causing cardiogenic shock.
• The overall effect is sepsis and septic shock
Sepsis can be diagnosed if there is evidence of infection plus at least two of the following:
• Altered mental state
• High or low temperature >38.5⁰C or <36.0⁰C
• Tachycardia
• Tachypnoea
• Reduced peripheral perfusion
• High or low WCC >12x109/l or <4.0x109/l
Recognition of sepsis ABCDE Approach
Airway
• At risk of obstruction if level of consciousness reduced.
Breathing
• Signs of increased work on breathing with tachypnoea and recession. This may be due to the underlying triggering infection (pneumonia) or as a compensatory response to shock.
Circulation
There may be signs of shock with:
• Tachycardia
• Weak peripheral pulses and pallor
• Cool peripheries and prolonged CRT
• Hypotension
Disability
• AVPU. There may be an abnormal conscious level due to the underlying condition (meningitis) or due to hypoxia resulting from respiratory or circulatory failure.
• Hypogylcaemia is a feature of sepsis
Exposure
• The temperature may be high (>38.5⁰C or low < 36.0⁰C).
• There may be rashes giving a clue to the underlying diagnosis e.g. petechial or purpura in meningococcal infection, erythema of toxic shock (staphylococcal, streptococcal infection)
Meningococcal infection

Toxic Shock Syndrome


ACTIONS
Summon senior help
Airway
• Open airway if necessary
Breathing
• Give oxygen by nonrebreather mask
• Support ventilation with BVM
• Attach cardiorespiratory monitoring
Circulation
• Gain vascular access- intravenous or intraosseous
• Take blood for blood cultures, FBC, Lactate, CRP, LFT, UEC, venous blood gas, blood glucose, and clotting
• Give broad spectrum antibiotics as per hospital guidelines (generally Ceftriaxone, or Cefotaxime)
• If lactate greater than 2 mmol/l give 10ml/kg bolus of balanced crystalloid or 0.9% saline. Carefully reassess after each bolus. If more than 40ml/kg has been given and normal physiology has not been restored start inotropes adrenaline infusion is first line inotrope and should be administered in a dedicated line.
• Call for anaesthetic support as it is likely that the patient will need to be transferred to PICU and require intubation.
• Monitor urine output and send sample for MC&S.
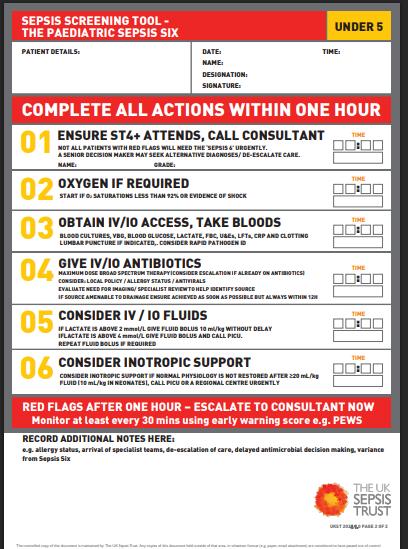
Seizures are common in childhood, most are short-lived and self-terminating lasting a few seconds or 12 minutes only. Seizures lasting more than 5-minutes are less likely to stop spontaneously and are more likely to lead to neurological sequelae, treatment should be started after 5-minutes.
Convulsive status epilepticus is now defined as a single generalised seizure lasting more than 5-minutes or two or more discrete seizures between which there is incomplete recovery of consciousness.
Pathophysiology
Causes of CSE include:
• Febrile seizures
• Epileptic syndromes
• Metabolic abnormalities including hypoglycaemia and hypocalcaemia
• CNS infection
• Brain tumour
• Intracranial haemorrhage or stroke
• Hypoxia
• Shock including septic shock
Recognition of Convulsive Status Epilepticus ABCDE Approach
Airway
• At risk of upper airway obstruction due to secretions, tongue/soft tissue hypotonia or loss of protective reflexes.
Breathing
• Airway obstruction or reduced level of consciousness can lead to respiratory failure.
• Slowing of the respiratory rate because of the seizure or because of treatment may also lead to respiratory failure.
Circulation
• Not generally affected until respiratory failure occurs.
Disability
• Hypoglycaemia may be the cause of the seizure. Always measure in seizing patients.
• If blood glucose <3mmol/l give 2ml/kg of 10% dextrose.
Exposure
• May give a clue to diagnosis if rashes present suggesting meningococcal disease
• There may be evidence of head trauma with bruising of the scalp, or bleeding from the ears
ACTIONS
Airway
• Open the airway. Consider NPA.
Breathing
• Give oxygen via non-rebreathe mask with 15l/min of oxygen
Circulation
• Establish vascular access intravenous or intraosseous
Disability
• Treat hypoglycaemia if detected.
• Seizures should be treated with anti-epileptics once they have continued for more than 5minutes.Use a personalised protocol if this available, otherwise give benzodiazepine (diazepam, lorazepam or midazolam) by quickest available route rectal, intravascular, buccal or nasal). Repeat benzodiazepine after 5-minutes if seizure continues. The second dose may be a different benzodiazepine and given by an alternative route. Do not give more benzodiazepine doses; two is the maximum recommended as respiratory depression is very common with more doses.
• If the seizure does not stop give a second line agent. All second line agents are equally effective but Levetriacetam is easier to give and has a better safety profile.
• If the seizure continues administer an alternative second line agent and call for anaesthetic support.
• If the seizure continues rapid sequence induction of anaesthesia will be required with thiopentone or propofol and the child will need intubation.
• Consider neuroimaging when stable.
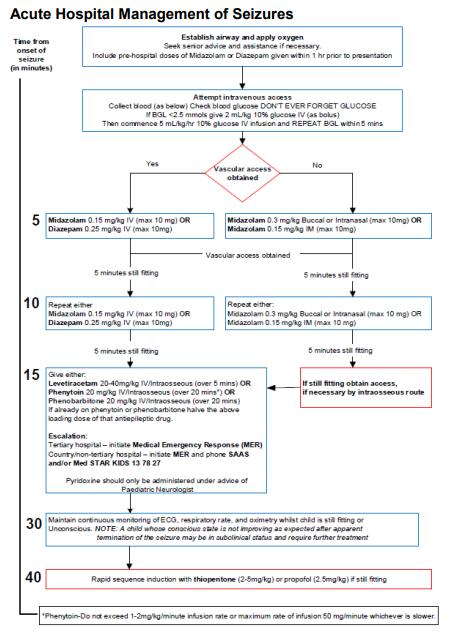
Hypoglycaemia
Clinical hypoglycaemia is defined as a blood-glucose concentration low enough to cause symptoms or signs of impaired brain function. It is generally accepted to be a blood glucose level of less than 3.3mmol/l in non-diabetic patients. A higher level of less than 3.9mmol/l is generally used for people with preexisting diabetes.
Hypoglycaemia is the result of an imbalance between glucose supply, glucose utilisation, and existing insulin concentration.
An altered conscious state or seizure warrant prompt blood glucose assessment and management with a bolus of IV 10% Dextrose (2 mL/kg) or IM glucagon if less than 3.3mmol/l (3.9mmol/l in diabetics).
Prolonged or recurrent hypoglycaemia, especially with clinical features, can cause long term neurological damage or death.
Glucose is the primary source of fuel for all the body’s cells. It is the primary energy source for both anaerobic and aerobic metabolism. The brain can store only trivial amounts of glucose in the form of glycogen There are several different metabolic pathways that maintain glucose homeostasis to ensure a continuous supply of glucose for optimal functioning of the brain
In response to fasting key changes in the endocrine system are triggered, these are:
1. Decrease in insulin secretion
2. Increase in glucose production via several counter-regulatory hormones including glucagon, cortisol, growth hormone and adrenaline which affect the liver causing:
• Increase in glycogenolysis where glycogen is broken down to glucose
• Increase in gluconeogenesis where new glucose is formed from lactate, glycerol and amino acids
• Lipolysis and ketogenesis where fat is broken down to make ketones and free fatty acids beta-hydroxybutyrate and acetoacetate.
Ketones can be used by the brain as an energy source. As glucose production declines and ketones increase, the brain gradually switches to ketones as its primary fuel. It is important to note that although ketone bodies can act as a complementary energy source in times of glucose shortage, they do not replace the need for glucose; they take time to generate and, at higher levels, are associated with ketoacidosis.
Infants and younger children have a 2-3-fold higher glucose use rate than adults and fewer glycogen stores so that interruption of glucose delivery can have devastating consequences on the developing brain and can cause permanent brain injury. Infants and children can also use ketones for cerebral metabolism.
Pathophysiology of Hypoglycaemia
Non-diabetic Children
The imbalance between glucose supply, glucose utilisation, and existing insulin concentration can be due to a number of reasons including:
Age Causes
Neonate-2y
Congenital hyperinsulinism (most common cause of persistent hypoglycaemia <2 yrs)
Inborn errors of metabolism (Fatty Acid Oxidation disorders, Glycogen Storage Disorders)
Congenital hormone deficiencies (eg growth hormone deficiency)
Child Accelerated starvation (previously known as “ketotic hypoglycaemia”)
Hypopituitarism
Growth hormone deficiency
Accidental ingestions (alcohol, sulphonylureas, beta-blockers, aspirin)
Adolescent Insulinoma
Adrenal insufficiency
Eating disorders
All ages Other illness (e.g. sepsis, congenital heart disease, tumour, adrenal insufficiency)
Symptoms of hypoglycaemia include:
• Palpitations, tremor, anxiety, sweating, hunger, paraesthesia
• Lethargy, irritability, uncharacteristic behaviour, hypothermia, confusion, coma, seizures
Recognition of Hypoglycaemia ABCDE Approach
Airway
• At risk of obstruction if level of consciousness reduced.
Breathing
• There may be respiratory depression if reduced level of consciousness
Circulation
• Tachycardia, sweating
Disability
• Tremulous
• AVPU in severe hypoglycaemia the level of consciousness will be reduced
• Blood glucose <3.3mmol/l
Exposure
• Temperature may be normal or raised.
ACTIONS
Airway
• Open the airway
Breathing
• Support breathing with BVM and oxygen if required
Circulation
• If conscious and able to swallow they may be treated with concentrated oral glucose solution (40% glucose gel) e.g. Glucogel, Dextrogel
• If unconscious gain vascular access and give 2ml/kg bolus of 10% dextrose
• If unable to gain vascular access give intramuscular glucagon
• Monitor blood glucose
Further blood tests will be required to determine the cause of the hypoglycaemia. These should be directed by the metabolic team but the following are usually required:
• Plasma glucose
• UEC, LFT
• Growth hormone
• Insulin and C-peptide
• Ketones (Beta-hydroxybutyrate)
• Free fatty acids
• Lactate
• Ammonia
• Cortisol
• Carnitine/Acyl carnitine
• Amino acids
Diabetic Patients
Common clinical precipitants for hypoglycaemia in children with diabetes may include :
• Insufficient food consumption (i.e. missed meals, nocturnal hypoglycaemia), excessive insulin dosing,
• Exercise,
• Alcohol ingestion (in adolescents), and
• Sulfonylureas [unlicensed].
Recognition of Hypoglcaemia
As above except <3.9mmol/l is accepted as the definition.
ACTIONS
• As above
Key Learning Points
• Most common paediatric illnesses can be assessed and treated using an ABCDE approach.
References
EPALS Manual 5th Edition
Resuscitation Council UK
www.nhs.uk/conditions
Anaphylaxis
Signs and Symptoms of an allergic reaction
Allergy and Anaphylaxis Australia allergyfacts.org.au
Recognising and Treating Acute Anaphylaxis
Ausmed.co.uk/learn/articles/anaphylaxis
anaphylaxis.org.uk
Anaphylaxis definition, overview and clinical support tool: 2024 consensus report Journal of Allergy and Clinical Immunology 2025
Anaphylaxis in Children
South Australia Paediatric Clinical Practice Guidelines
Acute Management of Anaphylaxis
https://www.allergy.org.au/hp/papers/acute-management-of-anaphylaxis-guidelines
https://www.allergy.org.au/health-professionals/papers
Asthma
Asthma.org.au
Seizures
Seizures in Children
South Australia Paediatric Clinical Practice Guidelines
Sepsis
Bacterial Sepsis
Benjamin Bullock; Michael D Benham
Stat Pearls ncbi.nlm.nih.gov
Australiansepsisnetwork.net.au
Pathophysiology of sepsis
Am J Health Syst Pharm 202 Feb 15:59Suppl1:S3-8Judith Jacobi
Epidemiology of Sepsis in Australian Public Hospitals
Australian Commission on Safety and Quality in Healthcare Feb 2020 safetyandquality.gov.au
Images of meningococcal rash ausmed.co.uk
Hypoglycaemia
Clinical Practice Guidelines
The Royal Children’s Hospital Melbourne NICE
BNFC
Hypoglycaemia in the ED Niamh Conlon Dontforgetthebubbles.com
Age
Less than 6 month
6 months -
6 Years
Adrenaline 1:1000 !!!Intramuscular route only!!!
100-150 micrograms (0,1ml - 0.15ml)
150 micrograms (0.15ml)
6 Years – 12 years 300 micrograms (0.3ml)
Older than 12 years (adult dosage)
500 Micrograms (0.5ml)
Patient with of one or more of the following:
• Itchy Rash (urticaria)
• Swelling to lips, tongue or throat
• Wheeze
Consider Allergic Reaction
!REMOVE ALLERGEN IF POSSIBLE!
Assess patient
Airway
Breathing
Circulation
Disability
Exposure
If all 3 criteria met
• Unexpected and sudden onset
• Clinical signs (life threating)
o Rapid breathing
o Evidence of poor circulation
o Stridor, Hoarseness or Wheeze
o Tongue Swelling Pale, Clammy, Rash, flushed, skin changes
NO
Reference:
Van de
P. et al (2021)
European Resuscitation Council Guidelines 2021: Paediatric Life Support , Vol 161, pg 327 -387
Mild Allergic Reaction?
• Perform observations (Respirations, oxygen saturations Pulse,)
• Frequent observations for 90 minutes
• Antihistamine orally as prescribed
YES
NO IMPROVEMENT OR PATIENT DETERIORATES
Seek assistance – request emergency team if available or activate 999 system
• M onitor –Perform Resps and Oxygen Saturation Pulse,and BP (if available)
• O xygen – provide high flow supplemental oxygen (15 litres per minute through non-rebreathe mask, if available)
• V enous access – If trained to do so establish intravenous or intraosseous access
• E PINEPHRINE (Adrenaline) USE 1:1000 SOLUTION STRENGTH
• If profound shock immediately life threatening start CPR as appropriate
• Absolute accuracy of small dosage not essential
• IV fluids infused rapidly (must be prescribed) 10ml/kg crystalloid (only of equipment & skills available)
Repeat Adrenaline (1:1000) IM after 5 minutes if no improvement If no improvement after two doses of adrenaline, confirm that help is on the way
• Follow local protocol for transfer of the unwell child
• Clinical staff MUST NOT leave the patient until ambulance service/retrieval team arrive
• Continuous observations –respiratory rate and oxygen saturations, Pulse, BP (if available)
Mild hypoglycaemia?
Patient diabetic or at risk of hypoglycaemia and showing one or more of the following:
• Sweating
• Tremor
• Impaired consciousness
• Combative or aggressive
• Coma
• Convulsions
Assess patient
Airway
Breathing
Circulation
Disability
Check beside blood glucose
Exposure
• Give oral glucose or glucose or sugary drink
• Give carbohydrate (bread or biscuit or crisps)
• Perform observations (Pulse, Respirations, oxygen saturations)
• Give oxygen
• Frequent observations for 90 minutes
REGAINS CONSCIOUSESS?
blood glucose < 4
Patient conscious?
• Repeat blood glucose half hourly NO

NO IMPROVEMENT OR PATIENT DETERIORATES YES
IM Glucagon 1mg aged 8 and above.
0.5mg under 8
Any impaired consciousness?
• Perform observations (Respirations, oxygen saturations BP, Pulse (if possible))
• Give oxygen
• Frequent observations for 90 minutes NO
NO IMPROVEMENT OR PATIENT DETERIORATES
Seek assistance – request emergency team if available or activate 999 system
• M onitor –Perform Resps and Oxygen Saturation Pulse,and BP (if available)
• O xygen – provide high flow supplemental oxygen (15 litres per minute through non-rebreathe mask, if available)
• V enous access – If trained to do so establish intravenous or intraosseous access
• E mergency airway manoeuvers – head tilt chin lift, oral pharyngeal or nasal airway, LMA/i-Gel as appropriate
MUST DO FOLLOWING ACTIONS
• Follow local protocol for transfer of the unwell child
• Clinical staff MUST NOT leave the patient until ambulance service/retrieval team arrive
• Continuous observations – Pulse, B/P, respiratory rate and oxygen saturations and neurological observations
Evidence of bleeding and/or fluid loss/maldistribution and patient showing one or more of the following:
• Tachycardia (usually associated with poor volume and peripheral pulses)
• Poor peripheral perfusion
• Delayed capillary refill
• Altered mental status
• Low blood pressure
• Poor urine output
• Dry mucous membranes
Assess patient Airway Breathing

Circulation
Disability
Check bedside blood glucose
Exposure
Obtain IV/IO access or check patency
Administer 10mls/kg of crystalloid (0.9% saline) YES
Reference:
Van de Voorde P. et al (2021) European Resuscitation Council Guidelines 2021: Paediatric Life Support , Vol 161, pg 327 -387 Resuscitation Council UK (2021) European Paediatric Advanced Life Support th
Reassess ABCDE Improvement?

• Perform observations (Respirations, oxygen saturations, BP, pulse, peripheral perfusion (if possible))
• Give oxygen
• Frequent observations for at least 90 minutes
NO
PATIENT DETERIORATES
Seek assistance – request emergency team if available or activate 999 system
• M onitor –Perform Resps and Oxygen Saturation Pulse,and BP (if available), stop bleeding if apparent
• O xygen – provide high flow supplemental oxygen (15 litres per minute through non-rebreathe mask, if available)
• V enous access – obtain second vascular access site, attempt vascular access if only IO in situ
• E mergency management – further bolus administration of 10ml/kg crystalloids.
MUST DO FOLLOWING ACTIONS
• Follow local protocol for transfer of the unwell child
• Clinical staff MUST NOT leave the patient until ambulance service/retrieval team arrive
• Continuous observations –respiratory rate and oxygen saturations Pulse, BP, and neurological observations
Patient showing one or more of the following clinical signs of meningitis:
Age 0 – 3 – Bulging fontanelle (up to 18 months), unexplained drowsiness. high pitched cry or irritability not easily soothed, pyrexia
Over 3 – headache, photophobia, vomiting, neck rigidity, pyrexia
All ages – non-blanching purpuric rash, sepsis, evidence of raised intracranial pressure (rash may be atypical or absent)
Reassess
NO
Assess patient
Airway
Breathing
Circulation
Disability
Check bedside blood glucose
Exposure
Seek assistance – request emergency team if available or activate 999 system
Reassess

Signs of early compensated shock?

• M onitor –Perform Resps and Oxygen Saturation Pulse,and BP (if available)
• O xygen – provide high flow supplemental oxygen (15 litres per minute through non-rebreathe mask, if available)
• V enous access – If trained to do so establish intravenous or intraosseous access
• E xpert help and emergency drugs – contact paediatrician/anaesthetist, give IV Ceftriaxone 80mg/kg
Volume resuscitation –10ml/kg crystalloid
Satisfactory Response
If there are still signs of shock after 40-60ml/kg fluid resuscitation – will require elective intubation and ventilation
Reference:
Van de Voorde P. et al (2021) European
Resuscitation Council Guidelines 2021:
Paediatric Life Support , Vol 161, pg 327 -387
Resuscitation Council UK (2021) European
Paediatric Advanced Life Support Manual 5th Edition, Pg 137 – 162
• Follow local protocol for transfer of the unwell child
• Clinical staff MUST NOT leave the patient until ambulance service/retrieval team arrive
• Continuous observations –respiratory rate and oxygen saturations, Pulse, BP,
This guidance/algorithm is intended to supplement local Trust guidance and should only be utilised for immediate initial management in the event of a medical emergency situation
Signs of raised intracranial pressure?

• Patient with of one or more of the following:
• Generalised fit/convulsion
• Repeated small fits or patient post ictal
• Localised seizure activity patient post ictal
Assess patient Airway Breathing Circulation Disability

Check bedside blood glucose Exposure
Go to Hypoglycaemia Algorithm YES

blood glucose < 3 NO
Seek assistance – request emergency team if available or activate 999 system
• M onitor –Perform Resps and Oxygen Saturation Pulse,and BP (if available)
• O xygen – provide high flow supplemental oxygen (15 litres per minute through non-rebreathe mask, if available)
• V enous access – If trained to do so establish intravenous or introsseous access
• E nsure that environment is safe for patient – pillows, cotsides, suction available

Normal seizure activity?
• Perform observations (Respirations, oxygen saturations BP, Pulse (if possible))
• Give oxygen
• Frequent observation for 60 minutes
• Neurological observations
NO IMPROVEMENT OR PATIENT DETERIORATES
Reference:
NICE (2021) Treating prolonged or repeated seizures and status epilepticus https://pathways.nice.org. uk/pathways/epilepsy
Resuscitation Council UK (2021) European Paediatric Advanced Life Support Manual 5th Edition, Pg 137 - 162
Seizure self-terminating and lasting < 2 minutes and patient known epileptic
Give buccal midazolam 0.30.5mg /kg (as prescribed) or Ensure effective airway management NO
MUST DO FOLLOWING ACTIONS
• Follow local protocol for transfer of the unwell child
• Clinical staff MUST NOT leave the patient until ambulance service/retrieval team arrive
• Continuous observations –, respiratory rate, oxygen saturations and Pulse, BP and neurological observations
10 MINUTES AND PATIENT STILL FITTING REASSESS PATIENT
REPEAT MIDAZOLAM OR LORAZEPAM
Learning Outcomes
To understand:
• The importance of an ABCDE approach for post-resuscitation stabilisation and optimisation of organ function following cardiorespiratory arrest.
• The specific investigations and monitoring indicated.
• How to facilitate safe transfer of the seriously ill child.
Post-resuscitation care begins with the return of spontaneous circulation (ROSC) with the aim of achieving haemodynamic stability to preserve cerebral function and to prevent secondary organ damage.
The ABCDE approach can be used to focus management. Following ROSC many specialty teams may need to be involved particularly if the child needs to be transferred to a different hospital. One member of the team should liaise with paediatric intensive care to find a suitable bed for the patient and to ask advice regarding further management. The rest of the team should use the ABCDE approach to reassess and manage the patient further.
Continued assessment and Resuscitation
Airway and Breathing
The aim here is to maintain adequate ventilation and oxygenation avoiding hypoxia and hypo/hypercapnia. Continuous monitoring of SpO2 is mandatory. Hyperoxia should also be avoided and oxygen delivery titrated according to saturations to maintain SpO2 between 94-98%.
Blood gases (capillary or arterial) should be checked regularly.
Considerations are:
• Definitive airway with placement of ETT
• Nasogastric tube insertion
Definitive airway with placement of ETT
If the child has been resuscitated using BVM and is still unconscious or requiring respiratory support they will require intubation. An anaesthetist may be required for intubation. If the child starts to make respiratory effort whilst intubated they will need sedation and analgesia until transferred End-tidal CO2 monitoring will be required if the child is intubated.
Endotracheal intubation is accompanied by potential complications which can be remembered by the mnemonic DOPES as shown below:
D Displacement of tube into oesophagus or right main bronchus
O Obstruction with secretions or by kinking of the tubing
P Pneumothorax which may have been caused by excessive airway pressure
S Stomach distension
Nasogastric tube insertion
Following BVM ventilation the stomach becomes filled with air which can impair ventilation and make the child more likely to regurgitate stomach contents. Insertion of a nasogastric tube (NGT) with aspiration of stomach contents is required to prevent this.
A chest x-ray will be required to check the position of the EET (above carina, T2-3), NGT and also to look for underlying lung pathology
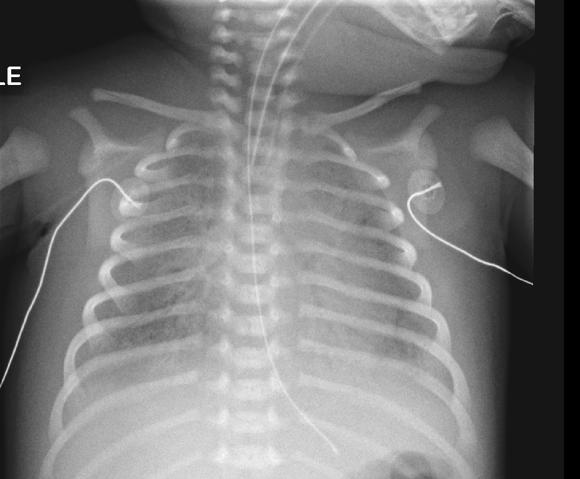
The aim here is to maintain adequate organ perfusion. The heart rate should be monitored continuously using ECG or SpO2. Regular blood pressure monitoring will be required. End-organ perfusion should be assessed using skin temperature or CRT and by measuring urine output.
Considerations are:
• Intravenous access
• Blood sampling
• Inotropes
• Measuring urine output
If an intraosseous line has been used during resuscitation insertion of an intravenous line should be attempted. Central venous access may be required but needs specialised skills and experience.
Blood sampling
Blood samples should be sent to the laboratory for formal analysis of electrolytes, haemoglobin etc. Specific replacement of electrolytes, haemoglobin or clotting factors may be required depending on the results
Further fluid boluses of isotonic fluid may be required. If 30-40ml/kg has been administered inotropes will be required. These need to be administered as a continuous infusion. Adrenaline is the first-line inotrope and can be given peripherally in a well diluted solution if central access is not available.
Urine output should be measured and recorded. This may require insertion of a catheter. In babies and children who still require nappies the weight of the nappy can be used to measure urine output.
The main cause of death after ROSC is brain injury. The brain is vulnerable to ischaemia and hypoxia which may occur as a primary injury or as a secondary injury after ROSC. The aim of post-resuscitation care is to prevent secondary brain injury. An assessment of neurological status should be performed early-on to obtain a post-resuscitation baseline and level of consciousness monitored. AVPU or Glasgow coma scale along with pupillary responses and any abnormal posturing should be recorded. If the child is sedated accurate assessment will be difficult.
Considerations are:
• Stabilising blood pressure
• Analgesia and sedation
• Treating seizures
• Normalising blood gases
• Correcting electrolyte disturbances
• Maintaining blood glucose
• Stabilising blood pressure
Stabilising blood pressure is important to maintain cerebral perfusion which is dependent on mean arterial blood pressure (Cerebral Perfusion Pressure = Mean Arterial Pressure –Intracranial Pressure). Mean blood pressure should be maintained at or slightly above the child’s normal level using fluid boluses or inotropes as required.
• Analgesia and sedation
Children who are unconscious after ROSC and require on-going ventilation with intubation will need adequate analgesia and sedation. Neuromuscular blockade may also be required. PICU staff will be able to give advice on recommended medications. Sedation makes assessment of neurological status difficult.
• Treating seizures
Treat seizures rapidly if they occur with benzodiazepines, or Levetriacetam according to the status epilepticus algorithm; this is important as seizures increase the metabolic requirements of the brain. If the child is intubated and sedated particularly if neuromuscular blockers have been used seizures may be difficult to detect. Remember to check blood glucose level in children who develop seizures.
• Normalising blood gases
Cerebral blood flow is affected by carbon dioxide blood levels (PaCO2), both hypercapnia and hypocapnia can be detrimental. When carbon dioxide levels are too high as in hypercapnia cerebral blood vessels dilate which can increase intracranial pressure, hypocapnia causes the opposite and may restrict cerebral blood flow causing ischaemia. Aim for a normal carbon dioxide blood level (PaO2 4.5-6.0) end-tidal CO2 monitoring will help guide this. Hypoxia is detrimental to cerebral perfusion and hyperoxia may cause oxygen toxicity. Aim for SpO2 94-98% (i.e. normal PaO2 10-13 KPa) and titrate inspired oxygen accordingly. Blood gases can be assessed intermittently using arterial or capillary blood samples.
• Correcting electrolyte disturbances
Maintenance fluids at 2/3 requirement should be started using a balanced or unbalanced isotonic crystalloid solution or 0.9% saline with dextrose. Any electrolyte imbalances should be corrected
• Monitoring for and treating intra-cranial pressure
Signs of raised intra-cranial pressure (ICP) should be reviewed and investigated. Raised ICP causes Cushing’s Triad of bradycardia, hypertension and irregular breathing. It can be treated specifically with hypertonic saline (3%) or Mannitol.
• Maintaining blood glucose
Hypoglycaemia (<3mmol/l) and hyperglycaemia are both associated with worse outcomes after ROSC. Tight control of blood glucose, however, may increase the risk of hypoglycaemia and so is not recommended. Glucose can be delivered continuously in maintenance fluids. Blood glucose should be measured regularly in unconscious or sedated patients.
If not already undertaken a full examination should be undertaken looking for rashes, bruising etc. which may have been missed earlier.
Care should be taken to maintain the child’s body temperature within the normal range, hyperthermia/fever should be avoided and actively treated with passive cooling or anti-pyretics (IV paracetamol). If hypothermic the child should be gently rewarmed with blankets, if their temperature is less than 34⁰ active rewarming with hot air (Bair Hugger) or warmed intravenous fluids should be considered.
Following stabilisation the child needs to be transferred to PICU for further care. This may be within the same hospital or may involve transfer to another facility.
Considerations are:
• Method of transport
• Equipment
• Medication and oxygen for transfer
• Airway and breathing
• Circulation
• Documentation
• Information sharing
• Method of transport
Depending on where the child is to be transferred to, the mode of transport needs to be carefully considered. The safest and quickest transport system that is available should be used which may mean using land transfer by ambulance, or air transfer by helicopter, or fixed wing airplane.
• Equipment
Prior to transfer all equipment required should be assembled and checked. A checklist will help with this.
• Medication and oxygen for transfer
Emergency medication should be available for transfer in addition to medication in current use. There should be adequate oxygen for the journey with extra in case of delays in transfer.
• Airway and breathing
The airway should be secured with the endotracheal tube taped into position. The position should be checked clinically and by X-ray. Just prior to departure the ETT should be aspirated to clear secretions and the stomach deflated by aspirating the nasogastric tube.
• Circulation
Intravenous access should be secured and patency checked. Infusion fluids and medication should be transferred onto syringe drivers or other portable devices. Extra fluids and medication may be required, depending on how long transfer is likely to take.
• Documentation
Copies of hospital notes including resuscitation documentation, X-rays and laboratory results should be available.
• Information sharing
Contact PICU to update on current status and give an estimated time of departure. Inform parents/caregivers of transfer details and ensure they have appropriate means of transport to PICU
Monitoring:
The following may be required:
• ECG
• Pulse oximeter (SpO2)
• Blood pressure (non-invasive or invasive)
• End-tidal CO2
• Respiratory rate
• Central venous pressure
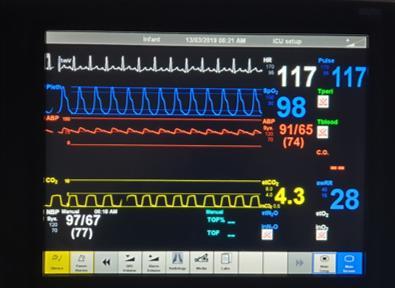
Following ROSC the child’s physiological parameters are likely to be deranged and the following investigations may be required:
Investigation
ABG/CBG including lactate
Biochemistry
FBC
Clotting
Group & save
Blood Culture
CXR
Urine
12-lead ECG
Rationale
Adequacy of ventilation
Assessment of tissue perfusion
UEC
LFT
Mg, Ca
Blood glucose
Infection markers CRP, procalcitonin, ferritin etc.
Hb, WCC, Plt. O2 carrying capacity, sepsis, caogulopathy
Coagulopathy from sepsis of hypoxia
Crossmatch if anaemia and transfusion required If sepsis suspected
Position ETT and NGT
Underlying lung pathology
Pneumothorax
Rib fractures
Toxicology
Culture
Renal function
Cardiac damage
Arrhythmia detection
• ROSC is the first step in continuous resuscitation management and the prognosis for children following cardiorespiratory arrest depends on the quality of post-ROSC care.
• Ongoing management after ROSC includes appropriate monitoring and supportive treatment based on an ABCDE approach.
References
European Paediatric Advanced Life Support 5th Edition
Resuscitation Council UK
Paediatric Immediate Life Support 2nd Edition
Resuscitation Council UK
To understand:
• The role of human factors in resuscitation
• The roles of team leader and team member
• The importance of structured communication in handover
Effective resuscitation requires a number of technical skills such as airway management, chest compressions, vascular access etc. however a good resuscitation team also needs its members to have effective non-technical skills. Non-technical skills (NTS) are defined as “as a constellation of cognitive, social and personal skills, exhibited by individuals and teams, needed to reduce error and improve human performance in complex systems”. Good non-technical skills really make a difference in resuscitation teams.
The importance of non-technical skills became apparent following various disasters in the aviation industry in the 1970s. As technology improved the human contribution to accidents became more apparent such as, poor communication between pilots and air traffic control leading to accidents. The aviation industry developed Cockpit Resource Management (CRM) training for pilots which improved safety. This was expanded to all flight crew as Crew Resource Management and since then the nuclear power industry and healthcare have introduced non-technical skill training and assessment to improve safety.
There are several categories of non-technical skills:
• Situational awareness
• Decision making
• Team working and Leadership
• Task Management
• Communication
Situational awareness
This describes an individual’s awareness of the environment at the moment of an event and the awareness of how an individual’s actions may impact on future events. This becomes important when there are many events happening simultaneously such as at a cardiac arrest. Situational awareness involves information gathering about the cause of the cardiac arrest, interpretation of the situation and planning interventions. Poor situational awareness can lead to poor decision making. In a wellfunctioning team all members have a common understanding of current events.
This is defined as choosing a specific course of action from several alternatives. In a cardiorespiratory arrest team decision making falls to the team leader, who is usually a senior experienced nurse or doctor, however, some decisions are taken by first responders until the rest of the team arrives. These decisions include confirmation of cardiorespiratory arrest and calling the resuscitation team, starting CPR etc. The team leader will have to make further decisions such as considering and ruling out likely reversible causes of the arrest, appropriate treatment including management of the airway, administration of drugs or defibrillation etc. The team leader also ultimately decides when to stop the resuscitation, although the views of all team members is asked.
Once a decision has been made it is essential that clear unambiguous communication is used to ensure that the decision is implemented.
Team working and Leadership
A team is a group of individual working together with a common goal or purpose. Team members usually have complimentary skills and work synergistically. Team leadership can be taught, observed and practised. Team membership can be improved by rehearsal including simulation training, and with reflection through debriefing and coaching. Teams work best when everyone knows each other’s name and they are doing something they perceive to be important.
A team meeting or “huddle” at the beginning of a shift with all team members ensures that the team know each other and their competencies. It allows for the identification of the team leader and allocation of tasks if a cardiorespiratory arrest should occur. Often huddles are also used to identify seriously ill children.
Team Leadership
All resuscitation teams require a team leader who provides guidance, direction and instruction to the team. The team leader should be easily identifiable to the team and requires experience not just seniority. The team leader should remain “hands-off” to have a global perspective of the resuscitation.
An ideal team leader:
• Accepts the role and is experienced and knowledgeable
• Knows everyone in the team by name
• Knows the competencies of the team members
• Delegates tasks appropriately preferably before the event
• Stays calm, and keeps the team focused
• Is assertive
• Is empathetic towards the whole team
• Is a good communicator
• Has good situational awareness
The team leader is responsible for thanking the team and ensuring that all documentation is completed.
Team Members
The traditional “cardiac arrest team” is made up of several individuals from various specialties including nursing, medical, surgical, anaesthetic, and intensivists depending on the facilities within the hospital. The members of the team will change with each shift change and may not know each other. If possible at the beginning of each shift a team meet or “huddle” should take place. Name tags should be used and role stickers can also help.
Resuscitation team members should be:
• Competent in the skill allocated to them
• Committed to achieve the best for the patient
• Following the same algorithm
• Able to communicate openly with the leader and other team members their findings and actions taken
• Supportive and prepared to help, looking out for fatigue in team members e.g. physical fatigue from compressions
• Accountable for their actions
• Able to feedback
Task Management
During a resuscitation there are numerous tasks that need to be performed sequentially or simultaneously.
The following roles are needed:
• Team leader
• Airway management
• Monitor application
• Identifying rhythm and delivering safe defibrillation
• Intravenous access
• Medications
• Chest compressions
• Scribe/record keeper
• Support of parents/caregivers
Some of these tasks may be undertaken by the same individual i.e. vascular access and drugs
Cognitive aids such a copies of algorithms, emergency drug charts or checklists should be used to support team members and guide decision making.
Communication
Communication problems are a factor in up to 80% of adverse events or near-misses. Failure to communicate the seriousness of the situation heightens the anxiety of the responder who may be uncertain of the nature of the problem. Structured handover tools have been devised which can help ensure that the important information is conveyed in such a way that the recipient is clear about what is required of them. SBAR (Situation, Background, Assessment, Recommendation) and RSVP (Reason, Story, Vital signs, Plan) are tools that can be used to improve handover of information.
Situation Reason
Background Story
Assessment Vitals
Introduce yourself and ensure that you are talking to the right person. Identify the patient
State current problem and what you need advice about
Background information including reason for admission
Relevant past medical history
ABCDE assessment PEWS score
Recommendation Plan
Decision
State explicitly what you want the person to do
State when you want the person to do it
Confirm what has been agreed and by when
Ensure that both parties are in agreement with the agreed plan
Example
Hi, I’m Dr Smith
I’m calling about Ellie Jones on ward 4.
She has pneumonia and is septic. Her oxygen saturations have dropped and are now 92% on high flow oxygen
She is 3-yr old and has no pre-existing conditions
She has been unwell for 2-days with fever and cough and is on oral antibiotics
She is responding to voice but is listless She is talking but breathless
Her respiratory rate is 36, and oxygen saturations 92%.
Her pulse is 159 and her BP 90/60
She is drowsy
Her temperature is 39.4⁰
Her CEWT score is 6
I’m going to insert an intravenous cannula
Please can you come straight away and prescribe fluids and intravenous antibiotics
I will come in 10 minutes, please put on high flow oxygen and call me back if any further deterioration
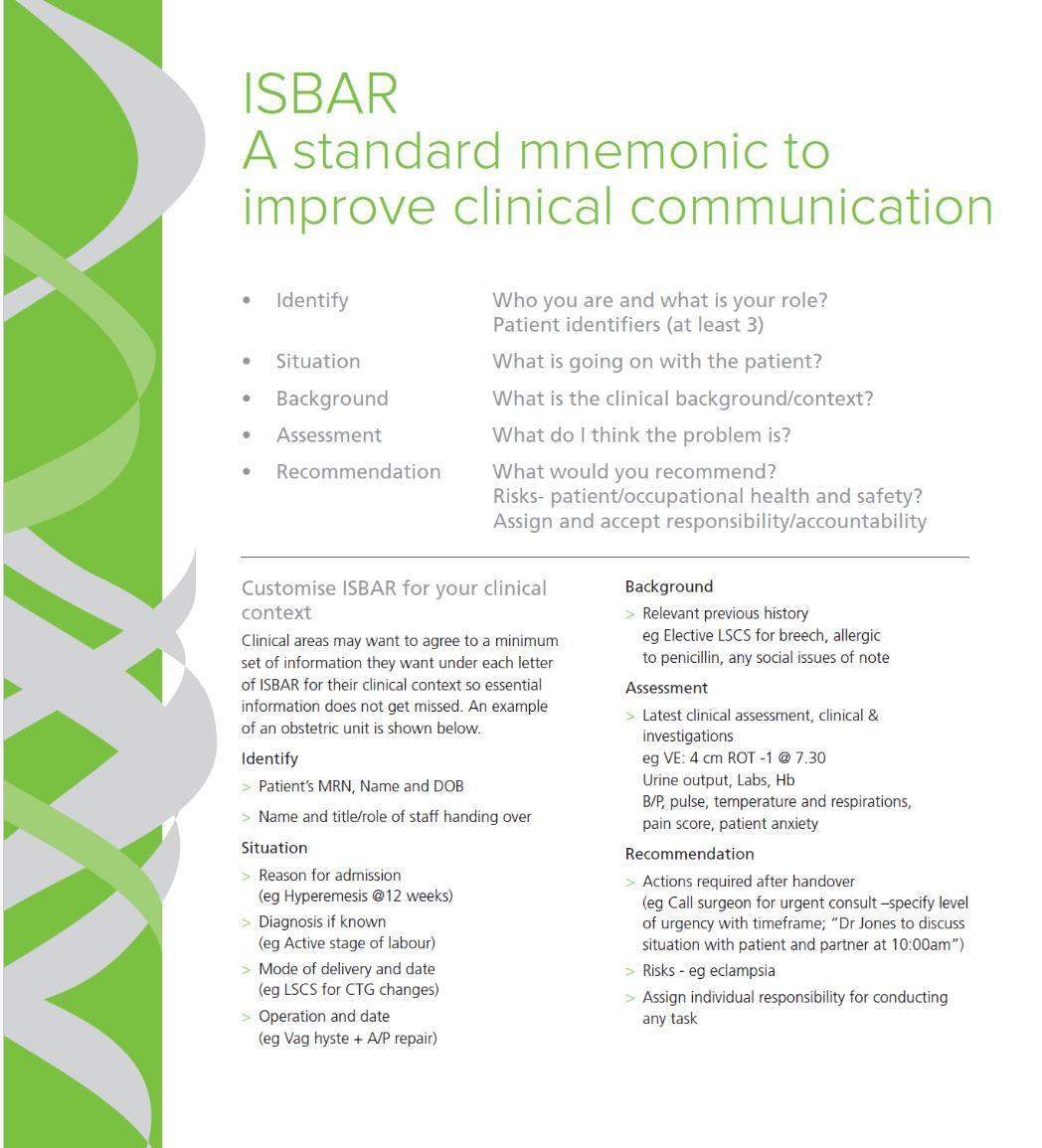
After any resuscitation attempt the team members should be given the opportunity to meet for debrief and submit incident reports. During the debrief difficulties or concerns about performance, equipment etc can be discussed and feedback given. Debriefing has been shown to enhance team performance.
Key Learning Points
• Non-technical skills are important during resuscitation
• Handover tools (SBAR or RSVP) are useful for effective communication
References
European Paediatric Advanced Life Support 5th Edition Resuscitation Council UK
Paediatric Immediate Life Support 2nd Edition Resuscitation Council UK
Non- technical skills in cardiac arrests: a brief practical summary
The Anaesthesia Collective https://www.anaestheticcollective .com
Effectiveness of nontechnical skills educational interventions in the context of emergencies: A systematic review and meta-analysis
María Sánchez-Marco, MSc Silvia Escribano, PhD María Rubio-Aparicio, PhD Rocío JuliáSanchis, PhDa María-José Cabañero-Martínez, PhD Australian Critical Care Vol 36, Issue 6, P1159-1171 November 2023
Non-technical skills in Healthcare Textbook of Patient Safety and Clinical Risk Management [Internet] ncbi.nlm.nih.gov/books
Learning Outcomes
To understand:
• The concept of medical ethics
• When CPR should not be attempted (DNACPR)
• When to stop CPR
Medical Ethics
Medical ethics is the study of the moral principles which guide the behaviour of healthcare professionals. These ethics ensure that the patient’s well-being is prioritized, and that patients are treated with respect and dignity, thus fostering trust and confidence in the healthcare system.
Ethical principles are not static but have changed and will continue to change over time varying with cultural and social practices prevalent at the time.
There are four pillars or principles of medical ethics which are:
• Autonomy
Autonomy is respecting the right for people to make their own decisions. To make their own medical decision patients must have competence or mental capacity to make decisions about their healthcare. They must be free to make the decision and not be under duress or undue pressure. They must be well informed about available options particularly about the risks and benefits of any proposed treatment. Autonomy allows the person to make the choice even if that choice seems illogical or incorrect by others including parents/guardians and healthcare professionals.
Young children or those with learning disabilities lack competence/capacity and parents/guardians make decisions for them.
As children grow and mature they will generally gain competence and are able to consent to their own treatment themselves. People over 16 are entitled to consent to their own treatment. Children under 16 who are Gillick competent are able to give consent to their treatment; they may also refuse life-saving treatment but this decision can be over-ruled by guardians/parents.
• Beneficence
All medical acts must be for the best interests of the patient.
• Non-maleficence
The actions of the healthcare professional should not be harmful to the patient.
• Justice
There should be no discrimination on grounds of age, race, sex, religion, socioeconomics or disability.
Cardiorespiratory arrest in children is rare and unpredictable. It usually occurs in children who are previously well but have suffered severe trauma or have a severe acute illness. There is little time to discuss treatment options before the event and consent for life-saving treatment is presumed and medical professionals have a duty of care to start resuscitation.
Some children and young people have illnesses that are irreversible and death is inevitable. For these patients CPR is unlikely to work and it is futile to start CPR as it will cause more suffering and prolong the process of dying. In such patients it is preferable to make advanced plans regarding realistic and appropriate treatments. Decisions regarding resuscitation should be discussed between the parents/guardians, the healthcare professionals and the patient if possible. Open and honest communication between parents/guardians and healthcare professional is crucial for making informed and appropriate decisions. The decisions which involve not initiating CPR or other resuscitative efforts should be documented in the patient’s medical records. The focus should be on ensuring comfort and relief from distress.
It is important to note that DNACPR does NOT mean stopping or with-holding all treatment, only some life-saving treatments may be stopped whist others continue e.g. continue treatment with antibiotics, nasogastric feeding etc. The palliative care team may become involved.
Parents/guardians are able to change their mind regarding DNACPR decisions if they have doubts about their decision or second thoughts. This will require further discussions with healthcare professionals and documentation in the patients notes of the new decision.
The specific legal framework for DNACPR decisions vary by state and territory in Australia but ethical considerations focusing on the best interests of the child apply to all.
Not all attempts at CPR are successful and resuscitation should be terminated when:
• The rescuer is too exhausted to continue
• The rescuer is in danger
• In children when CPR has been continued for at least 30-minutes without return of spontaneous circulation except in cases of hypothermia, poisoning, persistent VF/pVT
• In newborn babies who fail to respond to resuscitation efforts within 20-minutes
Key Learning Points
• Medical ethics guide the morals of medical treatment.
• The four guiding principles of medical ethics are autonomy, beneficence, mon-maleficence and justice.
• Children with conditions that are likely to lead to natural death and in whom resuscitation is inappropriate can have DNACPR order which should be documented in their medical records.
References
Caring Decisions: Different types of Treatment Clinical Practice Guidelines www.rch.org.au
Legal and Ethical Issues Related to Resuscitation
Section 10: Guideline 10.5 ANZCOR Guidelines www.anzcor.org
EPALS Manual 5th Edition Resuscitation Council UK