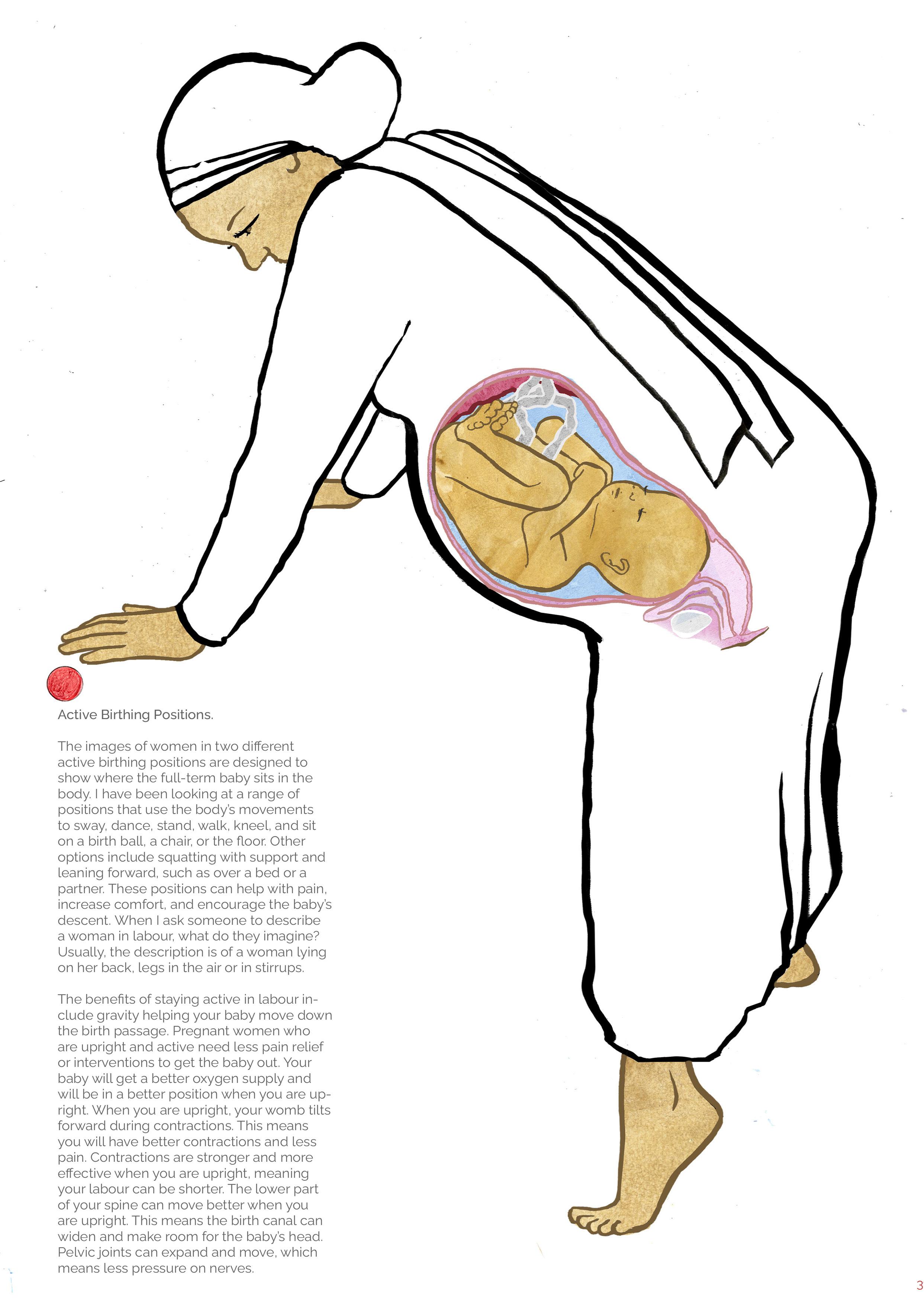
I am keeping these two drawings in this reader as a reminder of how communication and information regarding women’s bodies is still misrepresented.

Thoughts from Reader 9
The new Academic year has been frontloaded, and I have been making numerous new resources in my role as Future Skills and Student Journey Lead - whatever that means. Believing that I have made little progress until I have put this Reader No. 9 together. I have attended the new supervision training for PhD students, which was again a reassurance that PhD projects are not taken on unless they are perceived as a success and not a waste of everyone’s time.
I recently had a visit to my GP to have my HRT prescription increased after the feelings of anxiety and anger had crept up over the last six months. Dr Beattie, whom I have known for 25 years, asked me why I have not had a smear test since my hysterectomy nearly 5 years ago. My reply was that I don’t have a cervix, which is what I was informed in my mophined state of discharge from the hospital between the COVID lockdowns. Her eyebrows shot up towards her hairline as she exclaimed, No, you do have it still, and I am going to do a smear test now if that’s ok. I felt completely blindsided. Also, I was wearing a boiler suit, which meant I was on the funny little bed practically naked. She did it and fasttracked the result, which I received three days later, and thankfully, it showed no early signs of cancer.
How could I have missed such an important communication about my health? I am sure it was due to the rather strange treatment due to the pandemic, where I spent five days in the day surgery unit, had no visitors and no one to advocate for me in the procedure of quite a major operation. If I, someone who is well educated and selfaware with a specific interest in how women’s bodies are presented and understood, can get information about what was left in my body, so wrong there doesn’t hold out much hope for everyone else. The experience has left me shocked and, obviously, hugely relieved that the test came back negative and that the results were so quick. I had a conversation with the amazing Dr
Maggie Grey, who has a ‘baby on board’ badge and is racing through her pregnancy. We discussed the term ‘positionality.’ How a researcher’s own background, identity, and social-political context shape their research. How a researcher’s beliefs, values, and experiences influence every stage of a study, from the research question to data interpretation. Linking to reflexivity, a process of critical self-reflection that helps one understand and acknowledge how one’s positionality impacts the research. My experience of two very different births and this recent event of being reintroduced to my now non-absent cervix have provided a plethora of material.
I had a really interesting conversation with her, where she talked about how she does terrible drawings, but people always want to keep the draw ings. JW
There.......
The whole notion of keeping... Evidence-Evidence, memento, map, guidance, something which enables you to...
This thing about ideation. It’s also about tangibility. Yeah, and how do you remember what the person said? The words can be more slippery and easy to forget, and get tangled up. A mental image is literally an image of something, and having a version of it in front of you or in your pocket is a powerful tool. That’s really important and it’s exciting. GG
You just talked about a plan to have strands of stuff, because maybe at this point, because the thing is, with any PhD, you’re digging, you’re discovering, you’re finding new things. There’s a diversity of intent, in the sense that this is really interesting —I never knew that before.
When you’re confronted with 26 different languages in a single day, the visual suddenly takes on another level. It’s not a luxury item that you put on your wall and have your friends say, ‘I like that, where’d you get that?’ It’s really doing a job. GG
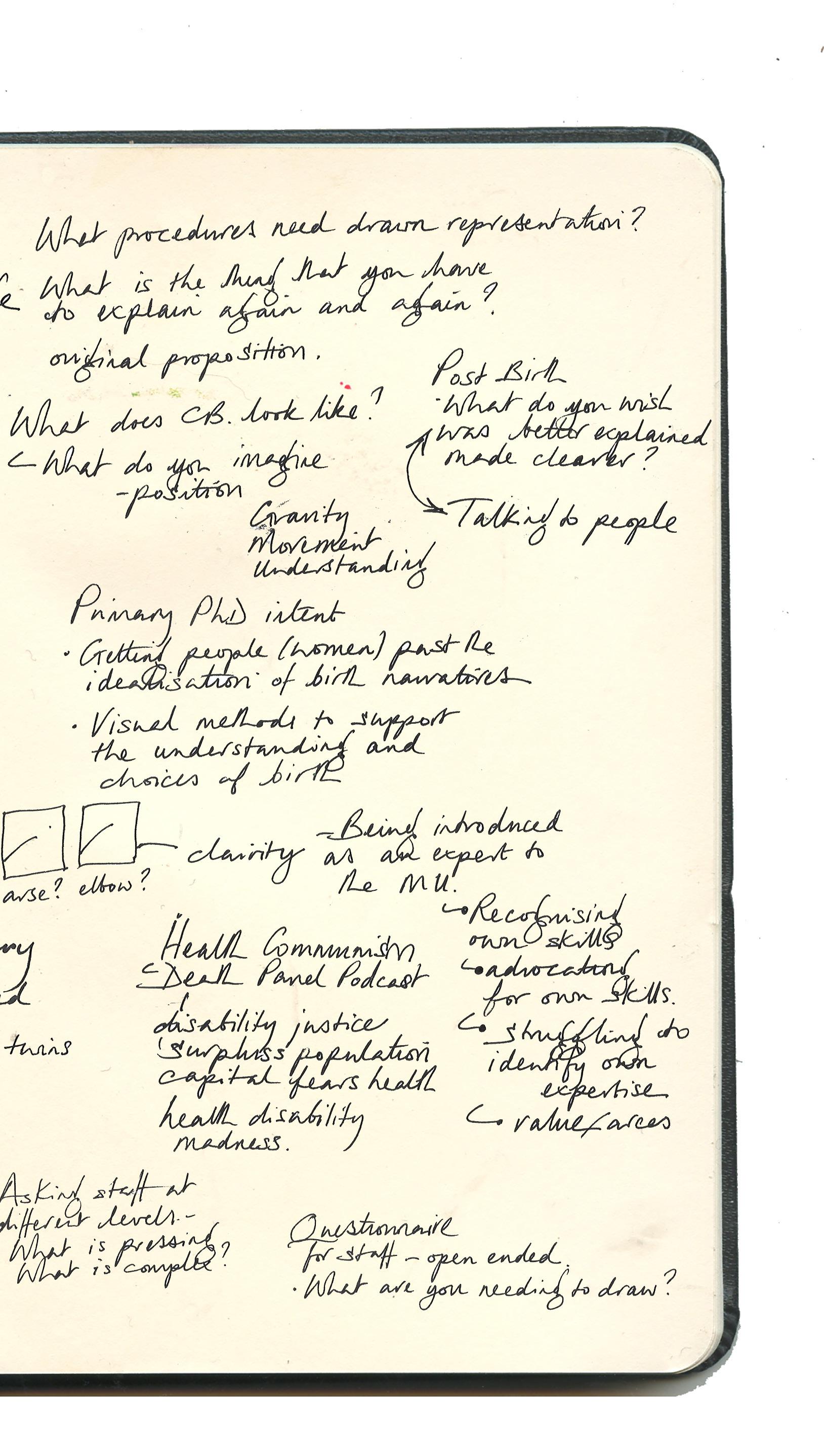
Is it the moment or the coming to the moment where your focus is going to be? I’ve looked at all these things, and from this, I’ve selected. I’m going to have a very clear one, two, three things, and they are going to address the core problem, which I identified right at the beginning, which was that women don’t know, and they don’t know because men don’t tell them, or men have got a different take on it or something. JW
One of your goals is not to simplify, but to clarify a complex, multi layered, multidimensional experience, acting almost like a performance in some ways. That’s impossible because it’s always different for different people. It’s also actually really, really complex, so I think what I’m trying to say is it’s kind of like how do you get that balance between not distorting things the way it’s been distorted by various vested interests over the centuries, how do you make it authentic to the people who you know it really matters. GG
We have an overall process that starts with a relatively broad set of aims that become narrower and more focused. That’s how research projects, in general —not just PhDs —tend to work. However, there is also the consideration that it represents a shift motivated by the opportunity to engage in a specific collaboration. What you’re doing now does count as research, because it’s your own original proposition. You’ve got some relevant participatory research, because, as we discussed, your decisions about which subject matter to focus on for the drawings will come from questionnaires administered to medical professionals. JM
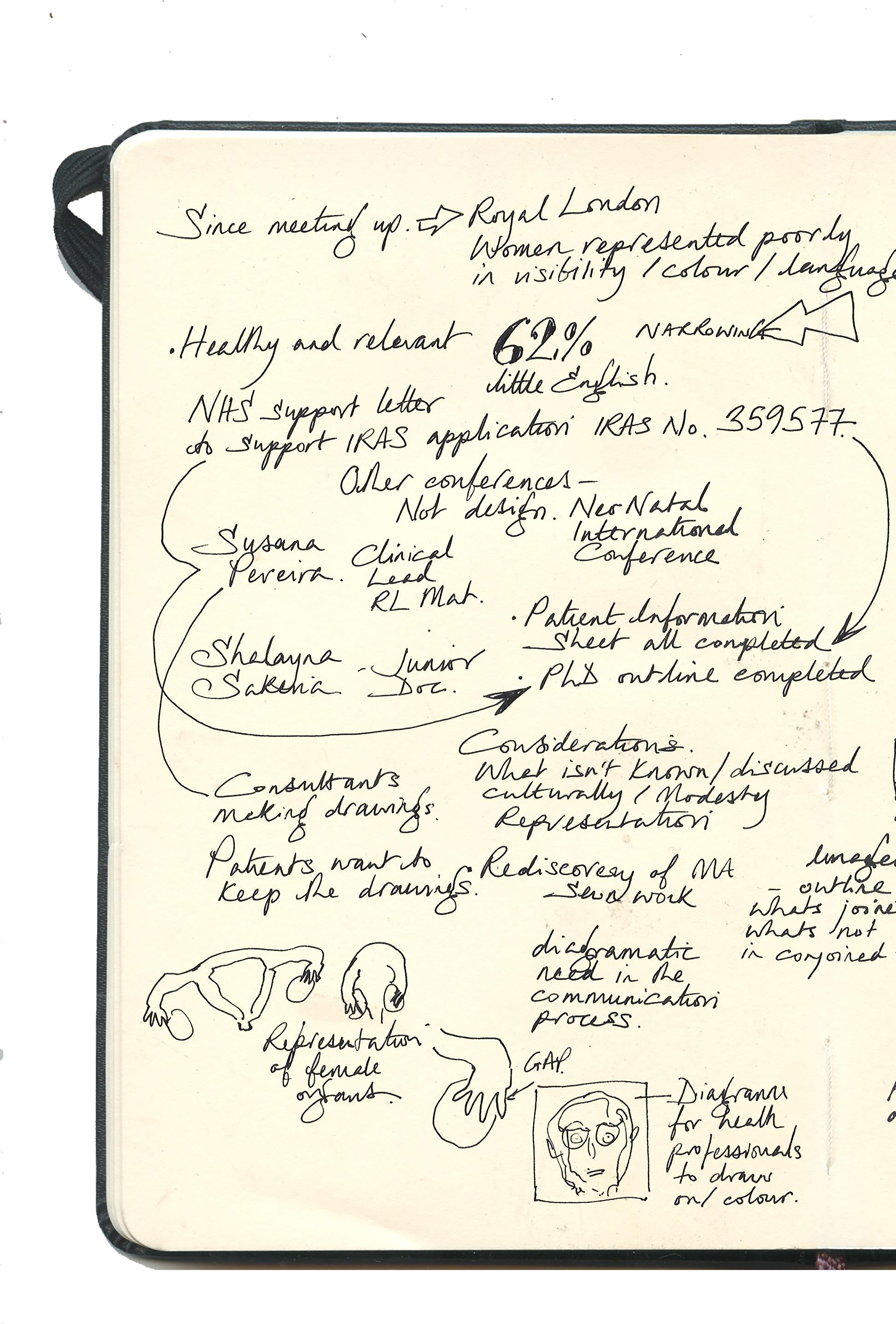
Meeting with Susana Pereria and Shalayna Sakaria at the Royal London Whitechapel, East London.
30/05/25
SP-Blue
SS-Red
JW-Black
Remind me of your PhD question Jane.
It’s how can confidence and choice be encouraged in the experience of birthing mothers through illustration animation practice? So, I’ve narrowed that down to first-time birthing mothers. Because I think otherwise, it’s so vast.
I mean, it’s still enormous. Because you’re looking at antenatal, intrapartum, and postpartum.
Because what I was going to mention is the experience that I saw in this little ward was a massive post-partum haemorrhage. Within a matter of seconds, a buzzer sounded, followed by loud noises, a huge rush, and an influx of people entering the room. And the Dad was holding this newborn baby, and neither of them spoke English very well, and just the look of horror, like I could see the blood drain from his face too. She was wheeled off to the theatre, and nobody stayed to explain anything to the Dad, and he was just horrified, mortified. With a newborn baby, he felt like he couldn’t move. He was holding this newborn baby, and then suddenly, the life of his wife was in a mess. I mean, that’s so traumatic for everyone. Absolutely. Especially for her, of course, but I thought about the Dad at that moment. So I went over and chatted to him, but wouldn’t it be lovely if that was kind of, at least, I don’t know. It’s a way of explaining it without the graphic horror that it is.
Absolutely. Or explaining what we’re going to do to stop it.
Yes, or what are the options?
So remember, Susanna very kindly invited me in to draw the high-risk C-section, Your drawings were a big collection of the work that we all do together.
That collection is now part of the Birthrights Collection, which is housed at the same location in Kent where I took a course last year. It was a bit wild because these people were giving incredibly graphic talks and sharing torturous stories about their experiences, so I was drawing them as they presented.
Okay, a lot is going on at the moment.
This has been happening over the last couple of months (I am showing Susanna and Shalayna two spreads from reader no. 6) with various things emerging. And then, obviously, there’s been the all-party report into birth trauma and what a lottery it can be for women Theo Clark- she stood up and spoke about her horrendous experience in the House of Commons- I’m currently reading her book.
Can I show you the C section I drew? .I drew Marno doing a classical cesarean. This is what I drew in theatre. I came home and digitalised it.
Great. I think the location imagery has a lovely looseness to it.
I also find that many illustrations in obstetrics are excessively flowery and cartoonish. And when it comes to actually understanding the process of what’s happening, the information isn’t there or medically correct.
It’s essential to have some more scientific or anatomical, yet approachable, imagery-Like actually drawing a vulva.
These are the animation exercises that illustrate the weight of a baby in the birth canal and then, suddenly, how the baby’s head ‘pops’ as it enters the world, which, animation-wise, has enormous potential.
So, looking at how, yeah, just this language, as you say, isn’t over-feminised, but is real.
Yeah, and these feel really like they’re real people, you know, and you can see the dynamic there.
I just had a fantastic interview with an ex-student of mine; she really advocated having a home birth for her first baby. She had gestational diabetes, but she was in control of it; she showed her consultanthere’s the app, I’m fine. She had a fantastic experience as a home birth in a water pool. She explained it as seeing the moon in the sky and having to put a rope around it to pull it down. And that’s when the baby was born. And her baby is the most beautiful, chill, and relaxed baby because it never had bright lights or stress; it just, yeah. And she just looked like a goddess. It was reassuring and lovely to hear. I’ve listened to another experience of one poor girl; they took her to Brighton, Brighton was full, they sent her home, and then she ended up having the I baby on the floor, which must have been highly distressing as a first-time experience.
You know, there’s an enormous lot of pressure on everyone.
Yeah, it’s a very fast-paced environment.
Where are these from? (Susanna points at drawings from Reader No. 2)
They’re at the British Museum, the Welcome Collection, and the Hunterian.
Have you been to the Barts Pathology Museum?
Oh, I haven’t for years
It’s probably the same, to be honest.
In the Hunterian collection, there are drawings of surgery by Barbara Hepworth. She created a collection of drawings in theatres, didn’t she? Y
Yes, I studied Barbara Hepworth, and I did.
my GCSE. It also has a museum in Yorkshire
Very nice, Jane, very nice. So, but you were saying you were telling me what is now, what’s next?
Well, what is next? I need to get through this ethics section, and then I’m free to proceed with the project. I might need to reference this as a base to work from. As a kind of referee, you would be very beneficial for my NHS ethics clearance.
I can work on that because we have an R&D department, which is responsible for Research and Development. Okay. And it shouldn’t be a problem.
Great.
I need to determine the proper process. Okay, that would be wonderful.
I was thinking about this; correct me if I’m wrong, but if you went down the route of doing your research as an audit, where you put in your intervention and then see the outcomes and how it improves, then you wouldn’t need ethics?
However, this is not an audit because an audit involves comparing something with a standard. And here, you don’t have standards. So this is a new thing. That’s why it’s research.
I’ve gone through the research tool kit. To determine - Is this your project research? And it is because it isn’t; you’re not measuring against something that already exists. But that’s the PhDness of it.
That’s very cool; I’ve been thinking a lot about how to approach this. There’s a lot of work that I’ve done over the past couple of years as clinical director, which has been very central to the hospital. My understanding at the moment is that once I get the basics right here, with people on the ground leading and exceptional individuals, it’s not by doing more here that we improve the outcomes. The baby is delivered here, but to improve what is happening here, I need to go out of the walls of the hospital to then liaise with the community. Although theoretically, there are numerous buzzwords, such as co-production and focus groups, in reality, I don’t see a strong connection between the community and the hospital, nor any strong links. I was trying to understand where to start. One idea is to start with the religious leaders, as they have a significant influence and often attract hundreds of people on Saturdays or Sundays. Another thing is the schools and the places where the moms meet. That was something I was trying to see, but how can I engage with this? This is what I am thinking here. Then I went to Africa, and I spent a week there, and I almost felt that what is needed, yes, they have nothing, but in obstetrics, we can do a lot of things with very little because the medications we use are very cheap and the ones that are not cheap, like HIV treatment, they are given, they’re for free. So, the question is not only about the resources
but also about engaging the people. And all these misconceptions, the relationships of trust, is a question of what people value, the value of life, even, or the value of, you know. And I was delivering a training session that was supposedly about pre-eclampsia. So, I had a group of maybe 10-15 people, and I started introducing each other. Then I told them about my reality here, and I mentioned that the mortality rate here is around 10%, but we can’t even reach 100,000, can we? And there are like a thousand per year. So it’s like ten times, a hundred times higher. So, I was saying how we could make maternal death for pre-eclampsia extremely rare. But then I said, but some things are not so good. I told them about the inequalities and how a woman of African origin in the UK has three to five times more likelihood of dying. And then they were very curious, oh, why is that, why is that? We had a brief discussion about that. And then I said, okay, why women die here is pre-eclampsia, bleeding and sepsis. So, in any antenatal appointment, when measuring blood pressure, we’re talking a bit of medical terminology. And then I said, ‘Well, there’s another question that we ask in the UK; I’m not sure if it’s a problem here.’ And I said we ask if the family, including the partner or the husband, is caring and supportive.
What happened?
Oh wow. You must have experienced total silence, a thick silence.
It was the male in the room. There were more women than male. But there were maybe four male doctors, midwives, or nurses, and they said, ‘Oh, it’s also a problem here. ‘I saw the same in India. However, it’s not discussed at all, and then the midwives really start telling the stories. Oh, because sometimes they come and they cry because of this, because of that. So, it creates a conversation —a very rich one. So when I mentioned it, I took some cradle devices, specifically blood pressure machines. And we were discussing, okay, so let’s examine the barriers. Okay, I understand. I bring this up because there are not many blood pressure machines. However, what other blood pressure machine only works if we measure the blood pressure or if the woman comes to the appointment? If we take action, we can work on addressing the barriers that prevent it from happening. One of the problems is accessing care.
So, I did my dissertation. So, this is about accessing care.
I’m doing; I didn’t have the chance to share my thoughts and what I’ve been cooking. However, we should conduct a scientific and artistic residency. I’m not sure if you need to mention residency. Yeah, residency. I’m going to get some sponsorships to feature some musicians and people from theatre backgrounds. It was fascinating to speak with some male doctors, surgeons, and those with a surgeon’s mindset who go there and perform surgeries such as fistula and gynaecological surgeries, including fibroids. And they were like, ‘Oh because we’ve been coming here for how many
years and nothing changes.’ I was thinking, ‘Well, maybe we’re not doing the right thing. ‘Yeah. And then they said, and then they said, oh, because, yeah, they don’t have anything. But look, everyone has a mobile. Yeah. And I said, but that’s very good because that’s communication. Well, this is what this came of Africa.
You gave me all that print stuff. And I was just like, wow, first, what a waste of money. Two, it looks terrible once it’s been photocopied. Three, you can’t change the language.
Have you seen Mar Global? It’s a charity that works predominantly in Bangladesh, but they’ve started to expand into Pakistan and other areas. Our community is predominantly Bangladeshi; there are many Bangladeshi women here. However, they have developed an app which creates access issues in Bangladesh, and they have also provided blood pressure monitors. Still, the problem was that they had to charge them, but the people would only have access to charging them once in a blue moon. It was a significant limitation, but they’ve developed an app that enables people to input their blood pressure readings. It was a brilliant talk, and I would like to know if I could put you in touch with them, as they’ve already done this fantastic work.
Well, it works with people like Jenny, and she’s a lovely woman. Because she’s Norwegian, she has a much better sense of herself. They grew up not being embarrassed about nudity, they grew up not being embarrassed about nudity, knowing their bodies, and so on. Where was I going here?
Oh yes,
She was talking about how, if there’s an app that can track gestational diabetes, there must be uses for those apps for other things, allowing people to have ownership of their health.
This app is excellent, and to be fair, it was a talk on, so I know it’s controversial, but it’s about AI in global health, and it’s an AI-powered app, but if there’s patterns that are, you know, wrong or things that are a bit suspicious, I don’t know the other word, but it gets sent straight to the store. AI is great when used in the right way.
I use AI every day. I couldn’t have even started this project because I’m dyslexic and struggle with writing. Still, when I have conversations or read something, I talk into my phone, record it, and then put it into Cockatoo, which converts it into speech. I then put it into Grammarly, and it sounds vaguely coherent. I know that if I sat in front of a blank screen, nothing would happen.
Yes, I have to use a co-reader to help with my dyslexia.
So that’s interesting. There’s a way to do things that don’t have to be the old way because, in the Western world, we’ve
inherited tools from that era. Now we have other tools. So, we can’t just mimic what happened and take another 20 years to get there; it needs to be done in a new way. And even for here, because that’s what I was reflecting, I was thinking, my God, I have a little bit of the same realities, access to care, et cetera, at my doorstep. The challenges are that there’s a bit of crossover in terms of the challenges we face, and that’s why I’m interested in getting some headspace to do things a bit differently.
I also think the premise of this is that you can go online, and you can go on Pornhub. You can see thousands of vaginas with things being inserted in them but in terms of actual information about your vagina and how it works. At the same time, you give birth and also how it tears or how it repairs or how you know the intervention of an episiotomy and then or how to look hard you know there the intervention of an episiotomy and then, or how to look hard, you know, there’s no visual information. Yeah, you’re right. I know I had the word episiotomy explained to me as someone was doing it, and then this lovely person went, and I had a long labour. Stay still while I stitch you up because your husband will appreciate it. And I was just like, oh my God. Yeah, that was 20 years ago.
That’s so mad.
It was this millennium. Yeah, I hate that so much. And in America, it’s called the husband stitch. As they do one more.
And you know what I find? You hear whispers of it still happening. I watched somebody who delivered vaginally in breach, so bum first, and the poor lady was thinking about having an episiotomy. And the husband couldn’t speak English; again, her husband could speak a little bit of English, and he was really adamant about her not having a C-section, which made her give birth vaginally despite being in breach. And she was just kind of like, do whatever he says about it. And then, when it came to the episiotomy, he was just vehemently rejecting it. He said, ‘I do not want that. ‘It will be loose, is what he was about to say before Manlo interjected and went, no, we’re not having that. It might be needed for the sake of mum and baby. Yeah. However, there are no visualisations of that, and there’s nothing that normalises it for our girls.
You mentioned something interesting about the Norwegian patient and the woman, as well as the different cultures.
And they cite, they always cite Norway as doing it perfectly in the all-party parliamentary report. But Norway’s got five million people. And they pay you lots of money to have more kids because they’re desperate to grow the population. Additionally, they’re one of the wealthiest countries in the world because they sit on vast reserves of oil.
Yeah. It’s also the relationship with the body. I’ve done some work in a field called embodiment. I’ve been neglecting my body because I work so much with my head. And,
I have... there’s a leadership guru, almost, who talks about heads on sticks and the burnout and the lack of connection. You know, coming to work with a mask and forgetting that we have a touch and a body and, you know, about the breaks, about eating, about... And I was doing, maybe a year ago, a leadership talk and that thing of the heads on sticks, so much touched me that, you know, yes, like, because there’s so much in our head is so much about the books the reading the the the learning and so little.
In this podcast, there is one episode that discusses the relationship between your brain and your womb, focusing on endorphins and an excellent visualisation technique. It’s a great way to practice, as opposed to someone saying, ‘Do some breathing exercises.’ I found myself just breathing fast and not breathing at all. Because if you had something visual, which is like how you could imagine it coming down from your brain and that part of your brain, and then just around, and then that oxytocin loop visualised, it would be helpful. And I’ve looked and looked and looked, and there’s nothing like that out here.
We’ll be exploring things that might sound a bit controversial or out of the ordinary, but I do believe that we need to experiment with this. But, as you say, suddenly, 20 years have passed, and things are still not quite the same, you know. If you imagine how much the world has changed in 20 years, it has likely changed more than it ever has. I think that a lot has changed, but something I was thinking about when you mentioned that is that with advancements and the future, you’re also experiencing globalisation. And I think the demographics of our population are critical and vital in this conversation about access because if you’re looking at Norwegian women and their culture around bodies, around women’s health, sexual health, you’re not going to get that here.
No, I know absolutely, but I find it interesting that even though I live in a very middle-class part of South London with very different demographics. But my friend who was Norwegian gave birth at Kingston, and because she and her husband were speaking Norwegian, they were treated like they were really stupid.
Oh, yes
They were talked down to. And the pair of them are academics. Yeah. English is like a language, not an accent.
Well, you say that. I had, for a long time, a lot of, like, complex or imposter syndrome or whatever because I have an accent. So, there was always a barrier. I don’t know how much was myself or how much was my perception of what the others were thinking. But it holds me back for quite a long time.
That’s really interesting.
That I’m not good enough to stand in that board meeting because I’m a foreigner
I also wrote about this in my dissertation.
I’m, I have an accent. Something quite interesting that happened in my life is that what I saw at the beginning of my career as an obstacle and a problem turned out to be one of my biggest advantages because any place I go, I mean, I may not sound English here, yeah, and maybe once in a while I make some grammar mistakes, but when I talk for an international audience because probably I speak with a little bit more basic language or because I have a more blunt accent. I don’t have an accent from anywhere. And also because I don’t use those English expressions that only local people understand. My English becomes what people want to hear because they recognise it and relate to it, and so it’s quite interesting.
So you’re stripping back the nuances, which then makes it much more open.
Yes, and then when I speak, it doesn’t matter if it’s for Scandinavians, Italians, Spanish, or Indians; it’s just international English, and then it becomes an advantage.
That’s so interesting.
We need to consider both religious and cultural identities. And I think it’s, although we do want a culture shift, I don’t think we could; I believe that if we find a way to kind of compromise, I guess, or like the small shifts about, you know, accessing care rather than, I don’t think we’ll ever, because people are still very shy and very coy about bodies. And I’m not sure how much we can change it. However, access to care itself is a significant factor.
Huge.
Because you can’t build the biggest, best hospital if people don’t attend or don’t attend promptly, schools are an excellent idea. Now, there’s a very interesting paper. There are two interesting papers, recent papers. One is referring to the CQC, one of our external regulators that classifies maternity services into ‘good’, ‘needs improvement’, and so on, like Ofsted. Good, needs improvement, you know. But all stayed. Yeah. Essentially, they conducted a study and concluded that the classification does not correlate with outcomes. Therefore, you may be outstanding and achieve poor outcomes, or you may need improvement to achieve excellent outcomes. Because all these classifications are very process-related, and some of the processes we need to challenge.
So, that’s one thing.
But the other thing that is even more interesting for what we are talking about is ethnicity, access to care, and why, in England, women of black or Indian origin have three to five times more chance to die during pregnancy. There is a paper, possibly from this year, where researchers examined outcomes in both white and non-white populations within the same institution. And this is something I’ve been wondering,
about, and I’ve been, as I’ve actually been asking this question in these forums. I said, is this population getting less good outcomes because they are in areas where the hospitals are under performing, or are they not sponsored or financed to the level of care that we need to provide? When I was at Kingston, I did this. I reviewed our outcomes and wanted to ensure that there were no discrepancies. However, in Kingston, I had a large white population and very few black or brown women.
I’ll do an audit for you. Yeah, repeat it. I’ll do an audit for you; it’s my niche. Here, it’s the opposite. Yeah. So, the majority of the population is from a Pakistani or Bengali background. But this paper answers it.
Okay, fine. Because they looked by the institution, there are institutions where the white outcomes are better than the average for the white population in London, in the UK. Within the same institution, the white population is even more favourable. And then the question is, why is that? Is it because people are not accessing care? The care is there, but they don’t access it. Or is it because there’s some institutional racism or some differences in how we provide care? So this is very crucial. And I do think that, based on my experiences in the African context and sometimes what I also experience here, it’s probably a bit of both. However, access to care is something that we need to tackle. How we access the population with new tools and new ways to bring trust is one of the things that I’m utterly interested in.
I mean, if you come in, I was looking at some pregnant ladies that were coming; I was here a bit early because I’m always early. I was looking at some pregnant ladies that were coming; I was here a bit early because I’m always early, and I’m watching some pregnant ladies sort of, you know, milling in, and just thinking, you know, you come, it’s the first time I’ve been to this hospital, it’s like, it’s vast. Where am I going? And it’s like, loads of lifts, signage, and departments.
I’ll go, put on my uniform, put on my cloak and then yeah and then from the other side of when you haven’t seen it or you don’t know it or you know the whole premise of your first-time experience of giving birth, it’s just like it could be like you falling off a cliff and you hope a parachute opens. You know it’s so overwhelming.
I mean, I’ve spent a lot of time in hospitals this year because my Dad had a stroke in the summer, and then he’s had sepsis twice. So he’s alive. He’s a bit of a smaller version of himself. And I’ve had lots of things where people have been trying to explain stuff to him, and it’s just like, he’s had a stroke. He won’t wear hearing aids. He can’t hear you; it’s deafening in here. I had this idea, but I don’t know whether it’s still around. I couldn’t find it, but it’s so simple. So, the premise is that this consultant was sitting at the end of a bed with my Dad there, and he was trying to draw a picture of his head. I just thought that if you had beautifully
drawn all the main structures of the head, it would be more noticeable, but it’s ingrained into the paper. The clinician then identifies the issue, perhaps pointing out the different veins involved or explaining why the concern is significant because it’s affecting this area. The whole premise could be so cheap, yeah? So it’s almost like Post-it notes, so this is your head from this side, this is your head from this side, this is your head from this side, you know, here are all your obstacle bits, and you know, and the fact that they’re presented like that, but actually when they’re inside you it’s much more like that. Yeah. I find that; why is that not normalised? It’s a lot more visual, and you’re right. I mean, you could have everything from your arse to your elbow. You explain it, and then the person’s got something which is a bit of paper, it’s not a medical scan, they can then talk to someone at home about, oh look it’s there, or actually they’ve got this blockage here but look they’re gonna put a shunt in and it’s going to open it out.
It sounds so simple.
Yeah. But that whole premise of it’s not costly to the institution.
Yeah. It’s yeah or even it being you know where it could be presented on a phone.
You can colour it in. Jane, you know how bad I am with drawing, but I keep making drawings for biomedicine to explain what I see in the babies. For example, if it’s a missing kidney, a blockage, or something else.
Just tell me what you want drawings of, and I’ll create them, and we can review them.
What I find amazing is that the parents want to take my drawing. I feel embarrassed about it, and I say yes, you can take it.
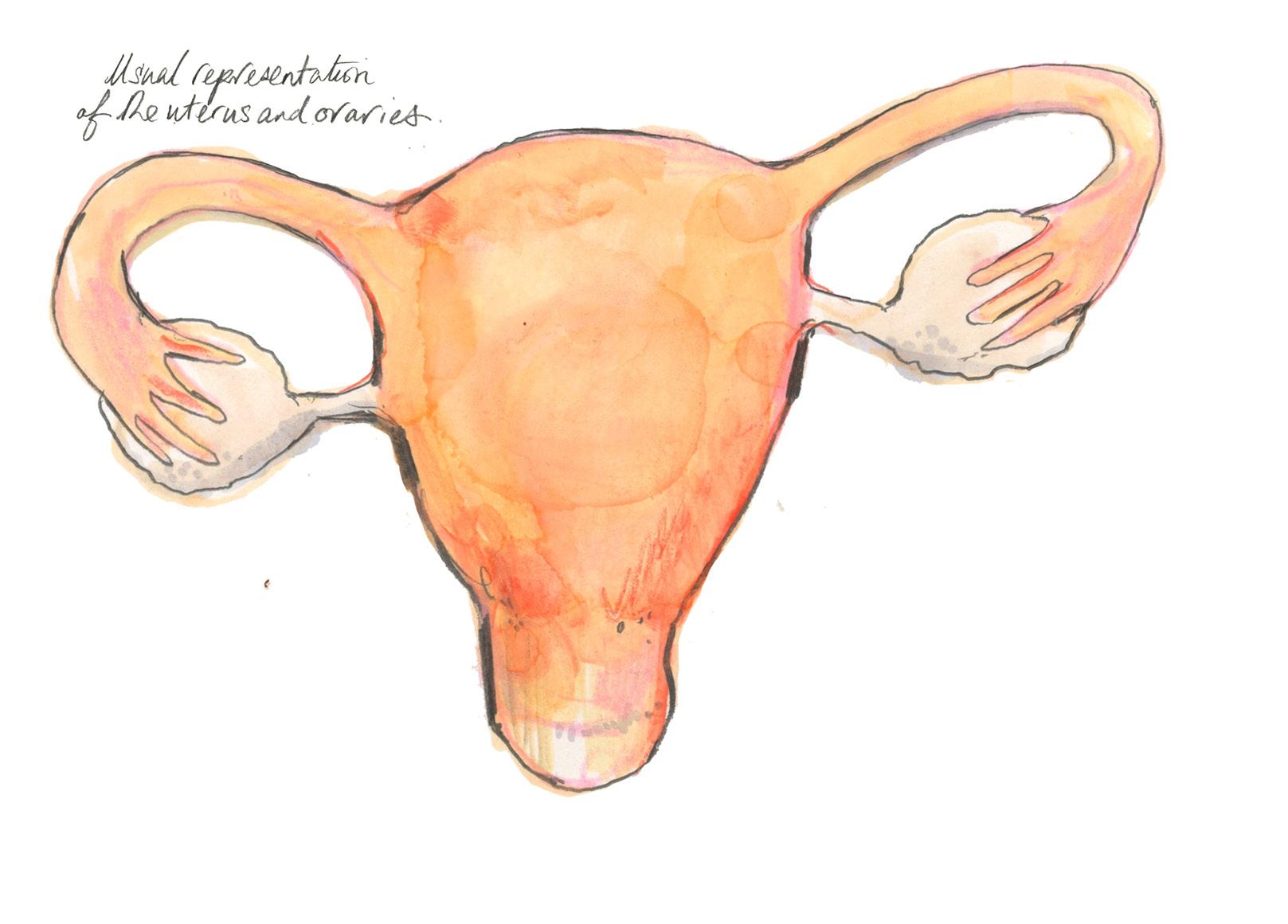
This was a kind of example where I had fibroids and had a hysterectomy. I mean, the language of lots of things to do with women’s reproductive systems is determined around a fruit bowl.
Yes.
Yes- Baby size of a grapefruit.
Yeah, absolutely, and so but yeah, this whole premise of, you know, but, if you had those, so all the structures are kind of, you know, accurate, but it doesn’t feel like a medical diagram, but it’s got a kind of fluidity.
Let’s do that as a small project. Let’s do it as a test. That’s a good starting point with the fetal medicine unit, which is very dear to me. But also, you can’t see inside yourself. Additionally, an ultrasound scan appears differently. To a normal person, looking at a black-and-white ultrasound scan is like, ‘What are you looking at? ‘I’m looking at a baby in space. In theory. It’s like a distant idea that you’re showing me my baby.
I’ve been reading a lot about the connection between as soon as you see your baby
on a scan, it changes the way that you associate your pregnant self; you know, to the absolute horror where in America, you are forced to see a scan of your foetus before you have an abortion, and that’s by law. Isn’t that awful?
Yes.
That could be a nice project. Let’s start with that, yeah, because then it’s like, and then we can start thinking about I just really like women to understand how their underneath looks before, during and after birth.
How does your vagina manage birth through a specific period? Birth can be slow, and it can be too fast.
Yeah. Yeah. Yeah.
I mean, I was talking to my friends who all have kids sort of 20 years ago, and then my poor, oh my god, my poor friend Hayley had loads of operations afterwards. They referred to what happened to her as a Michael Palin, which was a grade 4 pole-to-pole tear because he had done a program ’Pole to Pole’. Isn’t that incredibly insensitive?
Yeah.
Then there’s another book that was just released last week called Poor Woman. She had a, her vagina collapsed. It has just come out; it’s called The Stitch Up, How Medical Misogyny Harms Women.
Oh. Yeah. What’s the name?
The Stitch Up by Emma Suzuzak. It’s in here. I’ll give you these.
Thank you so much. There is so much ground cover. If they could find any models, we could explain even simple things, such as monochorionic and dichorionic, to the mums. There’s twin-to-twin syndrome.
Yes
Communicating these kind of things. But I’d be happy to do so. You’re a load of drawings, yeah, or ones where you could say, ‘This twin is this big,’ you know, so that you could use the premise of this... However, this is what we’re going to do.
There are no visuals of these high risk pregnancies and the specific issues.
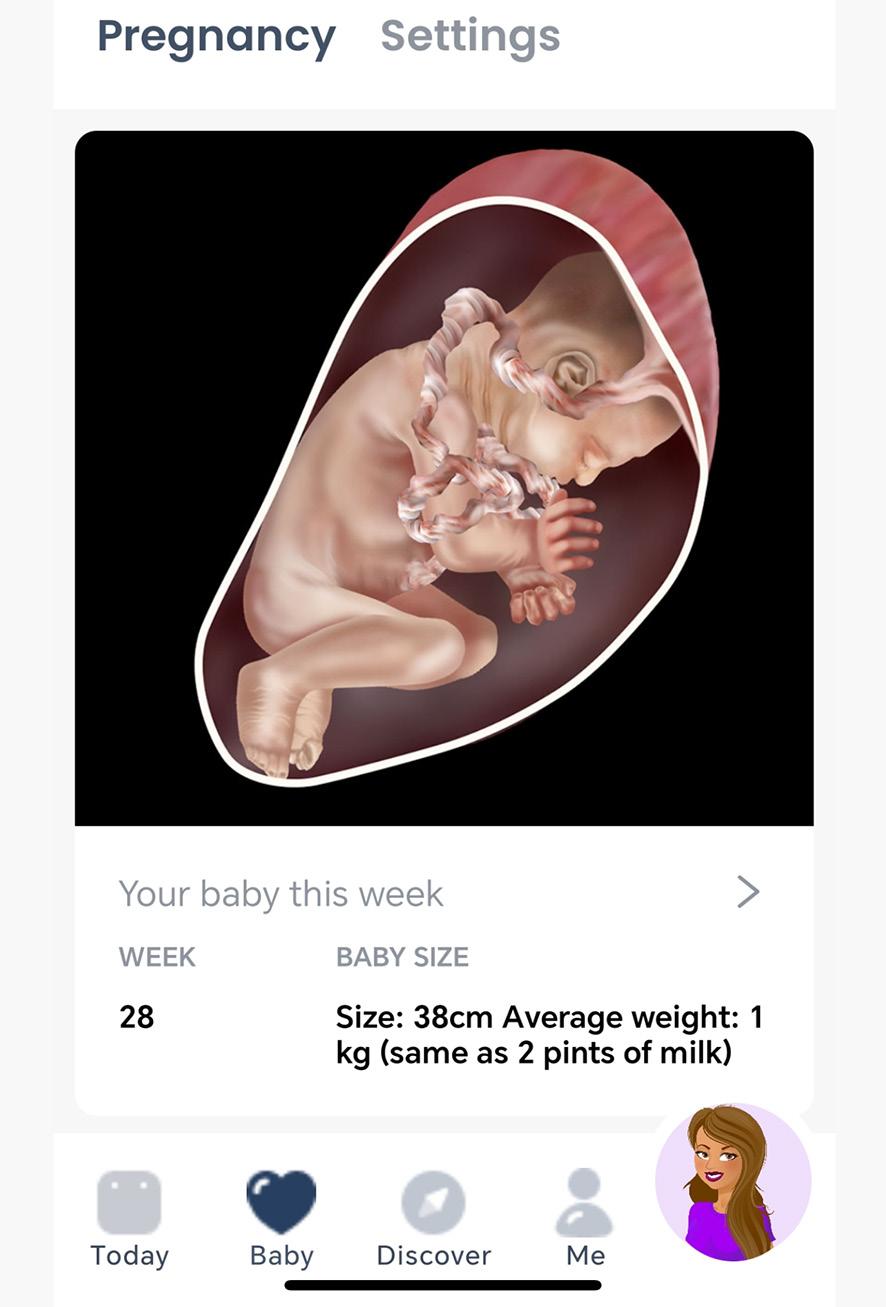
I was writing about this- the visuaisation of a baby in utero - looks as if the baby is a separate entity from the mother- why is this visually presented in this way? It’s the one with the animation cells on it. It might be that one, yeah. So I was looking at something, and then I had a big rant about the Virgin Mary, which just made me very cross. Like the premise of what a load of junk. What do we feed? I was looking at how I just did a completely random test.
That’s what you mean by it being in space?
Yeah, yeah, so here we go. Look, it resem-
bles a car, but this one looks gross. It looks like a volcano; it’s about to blow. Yes, and so these are horrible and odd, so this is a very classic diagram. Yeah, it’s like the birth of, the birth of the birth of, of like 3D, 3D model making. Yeah, but the whole thing is like, there’s no mother.
It represents that I don’t need you as a mother for me to develop and grow into a full term baby- and it’s also just black and white.
Yes, it discusses, to some extent, the idea of capitalism, where you don’t need anyone but yourself.
Have you read Health Communism?
No, I haven’t.
Come and meet Shane. Shane, let me introduce you to one of the Fetal Medicine doctors, Adam. Jane is an illustrator, and she’s pursuing her PhD in medical illustration, focusing on how it helps convey information and enables people to make informed decisions. I have encouraged her to use us because, with all the language barriers we have, images are going to be a key component, and we work with ultrasound, so something interesting will come out in our direction.
Imagine lots of people go yes. Exactly, exactly. And do you need a translator? No. I’ve got my partner.
Even if you feel confident in English, that’s fine; however, when discussing obstetrics and women’s health, nuanced communication is essential.
Oh my God, absolutely. This is like, you put me in a house in Norway, I’m fine. Start talking to me about politics or someone’s medical condition; I’m lost.
And if there’s another sphere on that, and I experiment that as a non-first English speaker, is if you add a level of emotional distress, your mother tongue is your comfort zone. So, people sometimes, you know, if I’m talking in an international setting, Portuguese people say, ‘ Oh, you have such wonderful English; you speak so well. ‘And I say, I still cry in Portuguese. I had a motorbike accident a few years ago, and that experience gave me so much insight into being a patient in healthcare. I’m a better doctor now in terms of understanding. It’s not only about proficiency; it’s not only the subject but also the emotional layer on top. Because even people who have enough English to communicate in the anti-natal, non-stressful environment, in a stressful environment, it all goes out of the window. Or if you need to make decisions that are very emotionally charged.
Yes, or even in bereavement, these are the places where it’s imperative; even if you are a confident English speaker, you need your mother tongue.
God, there’s so much to think about!
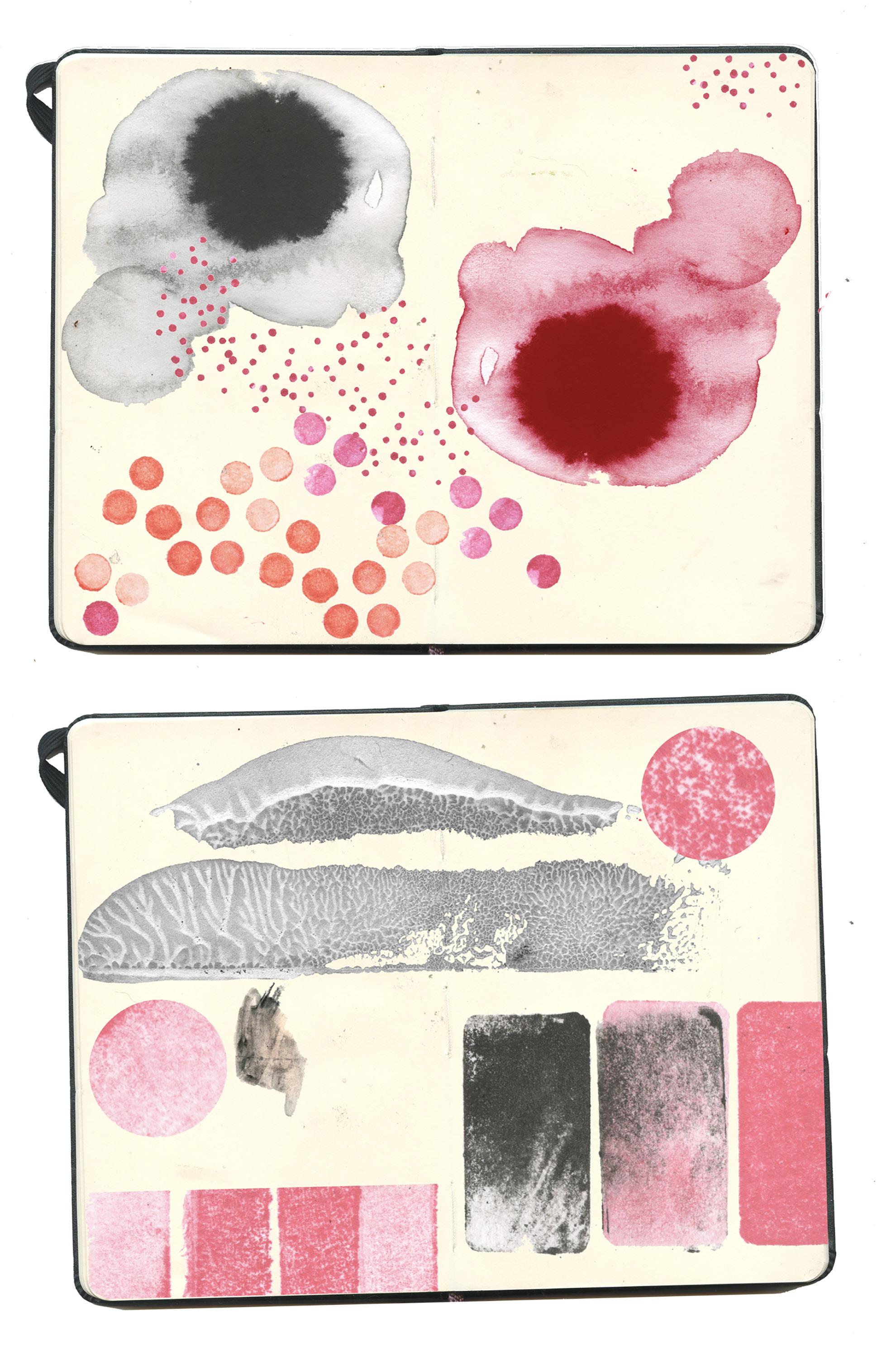
Colour Tests, wet in wet, print tests developing uterine wall imagery

Debrief with Dr John Miers 30/5/25
We’re just reviewing this IRAS form and are considering what the project entails, specifically whether it aligns with my research project. Yes. My project is a qualitative study only.
Yeah. That’s a fundamental question, and it’s worth considering. However, the results you collect will be qualitative rather than quantitative. Apart from anything else, quantitative data only really becomes meaningful if you have quite a large data set. However, this is not something that needs to be addressed in response to that question. But it is, of course, worth thinking about, well, actually, what are you going to collect from your participants so you know you’re going to be wanting to know things like did engage with your work help them to feel more reassured during a birthing process or more aware of the different things that could happen or kind of you know or were they more able to cope with things that arose that were unexpected. Those sorts of things. And then, I suppose, on the other hand, thinking about the visualisation stuff that you’ve been doing, so I suppose there might also be participant feedback about how accessible that information is. Or feedback from medical professionals.
I was discussing the diagram idea with you the other day. And I was talking to Susanna about that, I gave her a whole set of the readers, and she was, ‘oh my God, that’s amazing,’ you know, because it provides a clear idea of, like, it’s invested in. We were talking about, you know, what do the insides of you look like? And the whole premise of health professionals’ drawings - she spoke about that, and they are often terrible! She said to have that would be amazing. Right, right. Yeah. Yeah. That’s one of the things we’re going to trial quickly.
Brilliant. Because I don’t necessarily need to be there. Because if she’s using work that you’ve already done.
So, I’m going to interview her to determine what she needs—so, going through all this very specific medical imagery. And then me drawing what that could look like in a way that is suitable for her to explain it. But also maybe using a colour palette that is black and brown. Because 68% of their service users don’t speak English, English isn’t their first language. But also, we just had an interesting conversation about when you’re stressed, or trauma is involved, you cry in your first language.
That’s interesting.
You can’t speak another language with the nuances of that. They are currently using some interesting tools, which I’ve taken some photos of. It’s a portable machine; you press it, and it will translate for you. So it’s not a phone call; it’s like someone there as a translator. So, there’s a lot of scope for how my PhD can be trialled at RL,
She’s expressed that as soon as you get your ethics clearance,
.That’s great. That’s what you were saying; that ties in exactly with what I was saying. On the one hand, collecting data from medical professionals to determine its usefulness is essential. And then, for the patients or users, participants, there’s also the question of whether I can recognise this as a representation of a body like mine. Fundamentally, do I feel alienated from this?
In the meeting was an interesting young woman who was just about to graduate as a junior doctor. However, her thesis is that she’s Pakistani, and she was discussing poor outcomes for brown women in conversations and through feeling that they can’t access medical treatment. So, it’s exciting to see the significant crossovers between what she’s looking at in her final medical practice and this. And also she’s very good at drawing. So, Susanna, as the clinical lead at the unit. You can have a complete overview of whatever you want here. Can you mentor this woman with her art?
Fantastic.
I was, yes- most certainly.
So there’s another question. This question is drifting away from the ethics clearance strictly and discussing how it fits into the project as a whole. That sounds fantastic and fits into the project; it’s already a type of validation of what you’ve been doing. It raises a question, but it also raises a question about its place within the project. If your work is going to be used and substantially used at the Royal London, is that acceptable? This might now become my main clinical partner and replace the maternity wards with which I already have relationships.
So not sort of, because I suppose I was thinking, you know, is it even potentially a case of right, well, that’s kind of a proof of concept, but I still take the concept over to, you know, to Kingston maternity ward. I think in terms of just wanting to get it done. But also their need is so great. I mean, I’ve just been told such horror stories of, like, emergency c-section, someone gives the baby to the dad, the woman haemorrhages everywhere, and they’ve got no understanding of what’s going on or what they’re doing to that woman. And she said it’s also interesting that, yeah, yeah, yeah, I can understand English, and I can in a Norwegian household, but ask me about politics or governance or health, and I don’t know. So it’s like fascinating that but I think that is such a unique place to trial it as an academic piece of research to go then actually how do we make this bigger so then with potential, I don’t know, knowledge exchange or you know we’re asking for some proper money to do this.
No, it’s fantastic, and, just thinking about it, that whole thing that you said, the observation you just made of saying, well, their need is so much greater. Ultimately, all of that can be included in the methodology section. And actually, you can be very upfront about it and say, ‘Well, look- I began
this project and developed these relationships with these partners.’ This opportunity came up, and you can justify it in practical terms. Still, you can also justify it, thinking ahead to next year, because it will need a theoretical justification as well. Still, looking at it in terms of real-world impact, and looking at it from, in some ways, a kind of utilitarian perspective, of just saying, well, look, a new opportunity came up. It was also an opportunity to direct my work where it could do the most measurable good or have the most impact.
I mean, Susanne was coming back from Africa, and she just went, so basically, everything hasn’t changed in 20 years, apart from the fact that we’ve all got one of these —a mobile phone. And she said I’d like to take you out when I go out next in some residency capacity as an artist.
Amazing. Once you’ve got yourself into one funded situation, as you’re already seeing, the kind of related opportunities start multiplying.
‘Illustration, confidence and choice.’ This is the 70-character entry I am making into the IRAS form.
Yes - it says ‘birth,’ it says ‘illustration,’ it says ‘confidence.’ This is related in general, although it pertains to my project, not yours. However, I was in Amsterdam last week for my new job. And one of the things I was, so Erin, who’s the PI who got the funding, I mean, you know, she’s already a good friend. Still, I was very impressed by the way she’s using the grant she has. Like, you know, we’re right at the start of it. You know it’s a four-year project. I’m in month two, but she’s already- okay, how we develop this further and so one of the things that comes from the funding bit, so if you’ve, these ERC consolidator grants, if you’ve been successful in getting one of those, then you can apply, I think up to six times off the back of the same grant for a further 150,000 euros to do proof of concept projects. On Friday morning, we had a meeting with, actually, an English girl. Still, she’s pursuing a PhD at the medical school in Amsterdam. She’s been working on a project where she’s been collaborating with counsellors and using a technique called rich pictures, which I wasn’t previously familiar with. Essentially, this involves getting cancer patients to create drawings. So, it’s art therapy, but it consists of creating drawings that reflect on their lives and what they hope to resolve or achieve before their time is up. And so we had this meeting, and basically, Erin said, ‘Look, your project looks great.’ You’re entering the final months of your PhD. When your PhD is completed, do you wish to continue in the same role as a postdoctoral researcher? Can we apply for this £150,000 to support you in this endeavour? However, the one condition is that, because this project is all about comics, you’ve to create comics rather than single illustrations. If were in her position, I’d be like, ‘ Yes, this is amazing. ‘ I want to do this. However, Britain is also part of my project, as examining the use of artwork in British healthcare is one of the key areas I need to focus on.
So, if you’re potentially interested in creating sequential images, which you already are, we could explore developing a proof-ofconcept application to further establish this as a post-doctoral project. But it would have to be established around comics.
What’s a comic?
Indeed. Exactly. You know, think of your animations.
Yes, exactly.
Those are comics with loads of panels. They’ve got loads of tiny panels.
Something worth considering: the one thing is that I’d have to do it because I’m not the PI; I can’t make these applications myself, so I’d have to pitch her on it and persuade her that it was a good idea.
You mentioned your contact has just written a book. When you sent me the image, I was going to ask what you thought of the cover design.
It’s not my cover!
It’s better than some of the ones you’ve identified on your reading list, but it’s not my favourite.
Susanna is very pleased with it, and it will have a considerable impact on her medical community, both here and globally. She mentioned that she has a quite thick accent and felt that she didn’t sound British enough or clever enough when presenting her work. However, she said that, for international conferences, her English is perfect because it’s just what it is.
So, referring back to this IRAS form, I’ve just reached the last one here. Right, will identifiable patient data be accessed outside the care team without prior consent at any stage of the project?
Okay, so I’ve done that.
What was the one in red that you answered no to? Is your study exempt?
I don’t... I don’t think it is.
No. It’s quite a confusingly worded question. You could check - you’ve got a little tool tip there that might shed more light.
Is this a list of exempt research requiring approval but not ethical review?
You’re going to get consent; you’re not collecting any samples. A review is not required for research involving the use of or access to care organisations, premises, or facilities, provided that a review is not required for any research undertaken by a university department on NHS premises, including healthy volunteers not recruited as NHS patients, not subjects. It does start to get tricky, especially if, in the first round, it’s going to be Susanna and her colleagues, as you said, like using your stuff directly. You
don’t need to be involved, then, which raises a question about whether the patients they share the information with are your participants or if Susanna is on the team. Still, at some point, you will presumably want to have direct contact with participants. In this context, they have been recruited through their position as NHS patients, so you’re right to say yes. Okay, so what’s next? My projects, my contacts. Well, there must be more sections to fill out. What do you get if you click on the navigate link at the bottom left?
Oh. Here.
Cos, I mean, what you answered there was just...That was just introductory information of a fundamental kind. So, you must go through all of this?
So, project documents will include things like my patient information.
These are the standard things you’ll need for Kurios as well. So, it’s going to be participant information and a data management plan.
Oh, right, now I know where the thing is. It’s going to be a case of just going through this.
There’s going to need to be a literature review, sort of theoretical background, but you know, yeah, those things are the things that say this is why this research should be done.
Yes, this other young lady has also given me her literature review from her dissertation, which covers some of this material. So, it’s all much more in-depth, more medical. Yeah. Okay. I think we’re done here, John. That’s all right.
Okay, so I’m just going to go through this now. Now that I know where it is, I wonder if it’s true that I should probably create an account here myself, just in case you do come. I should do that so that I can see what the actual process is.
I know, I know, but alright. But yeah. Oh, yeah, I’ve got a project ID now. Can I email it to you?
JM -Black JW-Red

INFORMATION GRAPHICS
Sandra Renden - Author Julius Weidemann- Editor 2019 ISBN 978-3-8365-9966-5 TASCHEN

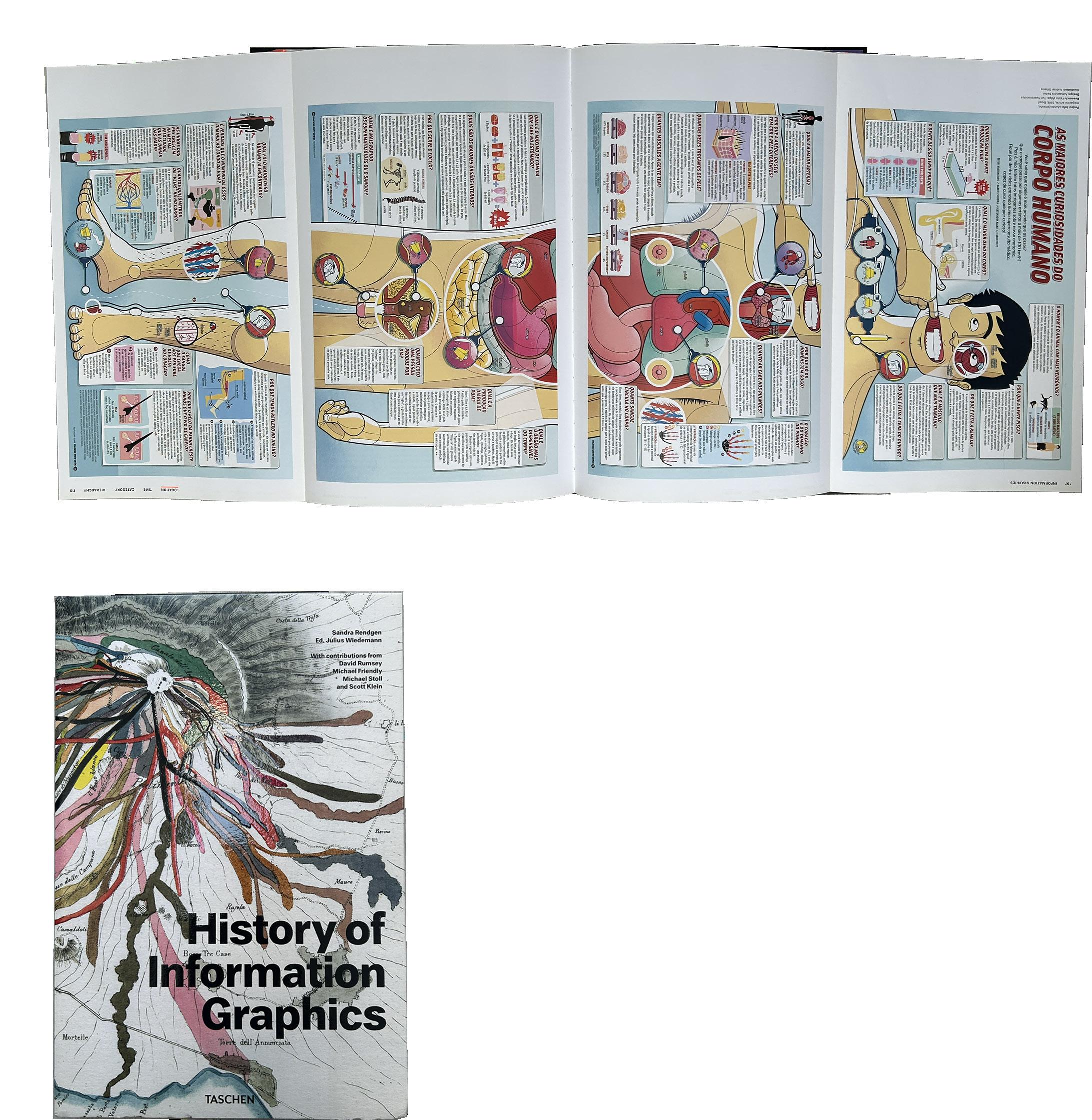
designers, scientists, and journalists have developed a new field of expertise in visualising how knowledge can be presented. There are 400 examples spanning astronomy, cartography, zoology, technology, and beyond—an enthralling exploration into the teachings, research, and lives of generations past. Across medieval manuscripts and parchment rolls, elaborate maps, splendid popular atlases, and early computer-based information design, the works are systematically broken down to each work’s historical context, including a range of gatefold maps. The History of Information Graphics is an unprecedented reference book for data enthusiasts, designers, historians, and anyone seeking knowledge.


You Are Here: Personal Geographies and Other Maps of the Imagination
Katherine Harmon
Princeton Architectural Press 2003
ISBN 978-1568984308
I have used this book as a key teaching text since its publication 22 years ago, because it is brilliant. This is the 4th copy I have owned as students sometimes forget to return a lending of it. Simply because being able to understand the world around us is key to being a functioning human, from understanding a skeletal diagram to navigating a location, to contextualising what failure and despair mean, and how we experience love and emotion. This includes a map of my day, if you see the world from a five year old perspective. The range of charts, maps, and scoping. All of the beautiful examples are inventive and explore the boundaries of geography and convention through the map-maker’s skills in communication design, ranging from the absurd to the critical, from the spaces between heaven and hell to a meal with a partner or an imaginary voyage. Some are real, while many are imaginary; however, as a compendium, this book serves as a go-to source of inspiration and a starting point for a range of my commercial illustration commissions and projects. Even though this book has been on the shelves for such a long time, its relevance and focus remain fresh and compelling. I have recommended Harmon’s book hundreds of time as an inspiration for students to be a key anchoring starting point when they are lost.

Birth- A History
Tina
Cassidy
Black Cat 2007
ISBN 978-080214 3242
‘Why is birth so hit and miss after all this time? I needed to put into perspective my own experience. I needed to know what other women, in other cultures, in other times had done.’
Cassidy’s book is essential reading for anyone with curiosity about the history of birth, or why it is so misunderstood and poorly communicated. I have read several books in the genre of birth and history within my project. Birth, with the simplicity of the title, is a reflection of the straight-talking content of the subject. It is full of shocking patriarchal effects and conditions. From the experience of her mother, in 1969, she was prepped by being given an enema, public shaving, given an injection and woken groggy, with little idea of how the baby came out. The excruciating pain was obvious. The book covers all perspectives, from the industrialisation of healthcare, religious influencesthe bible quotes in Romans 8/22, John 16/2 and Genesis 3/16 that it is a woman’s station is to suffer during labour. The perspectives of mothers, fathers, health care settingsthe hut, the home and the hospital. Pain relief and the caesarean section are closely examined in middle-class, famous and thin women being ‘too posh to push’ Victoria Beckam’s birth scrutinised for falling considerately within the football calendar of husband David. Further reading on maternity reports is grim reading. Today, the WHO cites that in the Western world, maternal deaths constitute 25% from haemorrhage, 15% from infection, 13% from unsafe abortions, 12% from pre-eclampsia and 8% from obstructed labour.

An Intimate History of Premature Birth and What it Teaches Us About Being Human.
Sarah DiGregorio
Harper Collins 2020 ISBN 978-0062820303
No one chooses to have a baby prematurely, as with my discussion with Shalayna, the experience often is a free fall of shock and fear, of a new regime of hour-by-hour vigilance and expressing and freezing milk, kangaroo care, arranged around bleeping machinery and tubes. DiGregorio’s book is written in the sense of a memoir with interwoven history and research surrounding premature birth and the future of neonatology. The neonatal intensive care unit is a strange place of calm and high drama, where precariously early babies can dip and crash, requiring painful and complex ethical decision-making about where a baby’s life starts and can end. The author was a reporter before she wrote this urgent-feeling book with the sharpness and focus of her previous work, but with the emotive and experiential reflection of belonging in this environment of limbo, where every millilitre os milk and gram of weight matters. The margins of viability are constantly pushed - babies survive as early as five months, often with complex needs that follow the child throughout their lives. The stories of the NICU are told through other parents’ experiences and those who work and ‘live’ in the high-tech but sensitive environment that can be experienced by parents for short or gruelling periods of time, where they are trying to get to know their baby within a surreal space.

Research For People Who (Think They) Would Rather Create
Daniel David Freeman
Onomatopee 2021
ISBN 978-9493148437
As the title suggests, it looks sideways at the way we approach practice-based research as practising designers. It is designed and formatted so the reader can dip in and out at any given point. The author is an academic based in Rotterdam who delivers sessions at the RCA. The material covers all aspects and approaches to designing and committing to a project, and salient sections can be curated to your research. The two approaches to design research processes are practice-based and theory-based; although many research projects will constitute a mixture of both. Much of that theoretical research is often undertaken by historians, focusing on specific problems, time periods, or locations. Practice-based, as with my project, centres around one’s design or art practice, where a potentially too large topic is focused through the experience of design, co-design, and working with groups or communities. I would have loved to have had this book at the beginning of my PhD journey; it would have contextualised so much of the terminology that felt alien at that time, when you start and feel too embarrassed to ask. The book’s design doesn’t take itself too seriously; the cover looks poppy and fun. Internally, it offers up cool graphics to explain ways of seeing research threads and punctuation. Every aspect is illustrated through a project’s example, some incredibly familiar examples and others that are granularly specific. The further reading section will help consider the research document, design practice, and a methodology for capturing both.

Health Communism
Beatrice Adler Bolton & Artie Vierkant
Verso Books 2025
ISBN 978-1839765179
Written by the co-hosts of the podcast ‘Death Panel’, which was a huge hit and a lifeline for many in the pandemic. Adler-Bolton and Vierkant’s book ‘Health Communism’ takes the form of a manifesto on the conflicts in the health care systems of the developed world, emphasising that work heals you and that it is in our best interests. Therefore, there is a worker surplus; if anyone is not fully fit or underperforming, the political economy requires that we maintain our health to demonstrate our worthiness and relevance. As health has been defined as things that are not: Non-cancerous, dis-abled. In the capitalist form, you must be normative and productive, then you are entitled to the health care that you can either buy or deserve. The book is complete with histories and examples, such as ACT UP in the late 1980s. It explains how and why the asylum system began the relationship between surplus, unhealthy members of the population and their lesser value in society as non-productive workers. In the UK, we have a socialised healthcare system, the NHS, which this book explores. It is explicit that its intention is not to examine the health insurance system, such as the American model; instead, it looks at how we cannot defeat and move away from health capitalism until we remove the two and base health on a model of productivity and usefulness.

Hands on Research for artists, designers & educators.
Harma Staal, Jojanneke Gijsem & Miriam Rasch
Set Margins Publication 2024
ISBN 978-9083404165
I would have loved this book at the early stages of considering and beginning my PhD journey. This user-friendly book is strong in its content, design, and examples of the research projects covered. The focus presents and surrounds the ‘Circle of Doing Research: a model to get you started in art and design research.’ Prioritising a practice-based research model, based on the art school model. The KSA premise of thinking through making sits comfortably with the way we conduct our research and deliver our curriculum content. Six actions - research by making, research of context, participatory research, prototyping, documenting, publicising and reflecting on the research. This is a non-linear model, where any action can serve as an entry point, whether for conversations or learning resources, depending on the discipline and project needs. This publication is reassuring on one’s research journey, which can feel very isolating, and self-doubt and sabotage can derail the approaches you naturally bring to a project. The publication’s design, from the Willem De Kooning Academy Rotterdam, is easy to dip into at any point to focus on what seems really obvious after seeing it in print. I recommend this to any researcher. It underscores the importance of design and the role that participatory projects play within communities and among participants. The aspect of publicising the research is something that often doesn’t come naturally to some researchers, and this is my takeaway from the book.

Conversation with Shalayna Sakaria 25/07/25
So this is interesting that Susannah sent over. What are your thoughts?
Do you have something you’ve already written?
No, but I can write something about my experience; it’s interesting. I’ve just been reading a book called An Intimate Story, which teaches us about being human and the experience of premature birth. The book is titled ‘An Intimate Story and What It Teaches Us About Being Human’ and Explores Premature Birth. And I was given this as my holiday read and as part of my PhD, but what it’s done has taken me right back to that experience and how the whole of this project came about because of that, and how I came to know nothing. Obviously, there are different types of premature birth, aren’t there? There are some cases where it’s expected, such as when the news comes that there’s something wrong with your placenta, which may be an early indication. Then there are cases that are not expected, such as spontaneous labour, the percentage of previa and abruption, and what’s it called when your blood pressure goes really high? That’s it. And also, no one expects to be in a neonatal unit, do they?
No, absolutely not. Pre-eclampsia- Obstetricians are generally good about prepping you for the unexpected birth. Yeah. You are right that there isn’t much emphasis on what will happen to the baby afterwards, how the baby is treated and supported in the very unique environment of the neonatal unit and NICU.
No and also that environment is so strange in the way that you know you’ve got these babies that are kind of they’re so tiny, and you’re so shocked that your baby’s so small and I think my thing was I had no under
standing of like, what is all that stuff on her? And like, surely all that tape all over her face has got to hurt.
And what I really wanted was someone to explain to me what was happening with her. So, you know, what is CPAP? What is happening inside this incubation, incubator, which is making these three factors work for this baby, which is breathing, feeding, temperature, and, you know, how, and also things like kangaroo care, of like how that works in terms of, you know, maybe in terms of like endorphins or, you know, how that works. I think that information in a visual way, I think, would be really priceless for parents, and I believe also especially if you’re, you know, and all the noises, so the heart rate, the respiratory rate, the blood oxygenation and the fact that you’ve got that boo-boo and the constant... And I was listening to a BBC podcast called Child, and it referenced it, and the noise of that when everything goes off was just like, oh my God, that’s so weird, because that’s so triggering.
Yeah, it brings you right back. So my concern with that is it says that one of the key things that a soundtrack has to contain is data.
Right. I don’t. No.
And it might be too, we’d have to obtain that data from people who would have gathered it.
Yeah, I think what is exciting, I mean, this has been really good actually to make me think about, you know, what are those things that initially led me to start this project.
It’s probably too early to submit this or anything else, as it hasn’t been completed yet.
I mean, the whole premise is, I think, a PhD is a bit like I’m going to go camping. The first part is that I don’t know where I’m going to go camping, so you have to make all these decisions. Then, you have to decide who I’m going to go camping with, and so on. Eventually, you get your ethics clearance, and then you go camping. Then, the rest involves writing it up and deciding what to do post-doctorally. This may be a bit premature, as it would be beneficial to obtain a letter from your hospital confirming that your unit supports my participation, which would enable me to expedite the NHS ethics clearance process. My Kingston one, then we’re like totally ready to go. Well, she said she’s asked someone else, but what I can do is I can send her an email that we’ve discussed this and obviously with the fact that it needs to be data-driven, what is really exciting is that this could potentially be a really key part of this PhD, especially with my interest in, you know, having that experience of not expecting to have, then having one and then, you know, all the different things.
And I think you’re doing it in the obstetrics department. Yeah. I wonder if she’s expecting, because this is just for one specific conference that I have, so I have a lot to handle this time of year. Susanna is a part of it, so she’s speaking at it. However, there are hundreds of conferences that occur all the time. One in particular that I’m sure she’d probably be interested in you submitting to is the Royal College of Obstetrics and Gynaecology. We hold an international obstetrics event every year, If we’re going to run the data and test your creations in an obstetric department, would you prefer to do it neonatally or something more obstetric?
I don’t know. I mean, I think initially I was looking at obstetrics and or you know, like Susannah deals with those cases where your baby might have a hole in the heart, or your bowel might be on the outside, or you’ve got twin to twin.
You can think of it as three stages -So there is perinatal.
*Perinatal is the time from when you become pregnant up to a year after giving birth. You might also have heard of the following terms: Antenatal or prenatal, meaning ‘before birth’ Postnatal or tum, Post-partum -meaning ‘after birth
There’s perinatal, there’s prenatal, and there’s postnatal. So, your prenatal ones could be, so in the context of maternal-fetal medicine, like Susana was talking about, you have twin to twin, and holes in your heart, and the bowel outside, it’s all like things that you find out prenatally. So it’s things that we can then explain, like we could find some animation or Illustration of whatever kind of media you wanted to use to sort of describe, it’s called maternal fetal medicine, so any kind of fetal defects or problems with the baby in that prenatal phase. And then you could do a perinatal assessment, so that’s when you have things like abruption and pre-eclampsia, and other issues that arise during delivery, which require quick action. Or even when, like you’re saying, when baby’s descending into your vagina, when your pelvis is expanding, your cervix is expanding, all of those things could be in that perinatal period. That first stage would be your neonatal phase, your, what’s going on with your baby.
Yes. And then also encourage, so I’ve been making these sorts of animated, not loop, because it doesn’t go back in, so I’ve been making these animated shorts of how a baby comes down and also how your vagina opens up. Because women don’t understand that, and obviously, the whole pressure then you pull in your pelvis, don’t you?
And the premise is that actually, your pelvic floor has to move out of the way. And so, you know, getting ladies to realise that’s what’s happening, because obviously your natural reaction to, you know, things moving is you tell your body to do the actual opposite. Or from understanding how endorphins work from your brain to around your uterus as it contracts, so it’s like a visual kind of breathing exercise, trying to work. I want to do three different things that can then be tested.
This is a suggestion, but the childbirth pathway has three parts.
That sounds great.
This allows you to submit three projects, three abstracts, or three research pieces to three separate journals. You could have one for a maternal feed, so there’s a British Journal of Maternal Feed Analysis, BMFMS, which is an international conference for your prenatal section. And then you could do the Royal College one, so your perinatal one, that’s very interstitial related. And then for your postnatal one, you could do that for your paediatrics and neonatal one, that’s like three publications from one project. That’s brilliant.
That would make chronological sense. Yes. That’s so helpful. No, that’s a straightforward way to put it. Great. So, I’ll text Susanna and say that I don’t have anything feasible in terms of measurement. However, it was invaluable talking to you, as it really helped me sort out the project’s structure, which makes perfect sense.
But it won’t be for this specific...No. But for your project as a whole, it could be nice. When it comes to nailing down exactly what you want to do, or figuring out what you want to do, such as mood boarding, I can help you tailor it so that it can be publishable in all these scientific journals.
Amazing, that’s absolutely amazing, thank you. And in return, let’s go drawing.
Let’s go drawing. Absolutely. Well, if your PhD will work like this, many clinicians, such as doctors pursuing PhDs alongside their clinical work, often have these sub-projects, which are usually split into three, as yours would be. They have numerous sub-projects, and then they frequently hire master’s students or undergraduates to support them, collecting data and performing similar tasks. At the same time, you serve as the mastermind of your project. If you want to do that, I have a range of students who would be eager to assist.
Oh, that’s fantastic. Thank you so much. If I can get a letter from The Royal London to confirm, that would really support my NHS application. It’s not just me making it up. This work could be really valid. She didn’t, no. But obviously, she’s one of the busiest women in the world, and I don’t feel like I want to hassle her. But if you know that person, that would be great. And I could email you what I sent to Susanna.
I don’t know that person, but I do know that if it’s this person in particular, she’s challenging to get in touch with and also to reply to emails, as I also try to obtain ethics approval for my project. I’ve not finished the project, and I still don’t think she’s approved it, so it’s a bit naughty, but okay. I’ll ask her again. I’ll ask her again.
I mean, this is great that she stepped out and said, You know, do you have something? However, I haven’t yet because I haven’t obtained the ethics approval, so I will explain to her and say something like, ‘I think we’ll give this conference a miss because I haven’t yet collected any data.’
I would love to go drawing really soon, but unfortunately, I am back in my parents’ house in the Midlands because I no longer have a home in London to stay at.
Just give me a shout when you’re done. Yes, I should be back in London towards the end of August.
Excellent, then let’s do it. So let’s do it then.
Thank you so much for your time.
No problem. If you want to just kind of fire off ideas that you’ve been brewing for your PhD.
Oh, I really appreciate it. Thank you so much.
Have a lovely time off work.
Thanks,
Enjoy Norway.
I will do. Very clean living and fresh air.
Exactly. Take care.
Hungry mothers and dirty wards - maternity care ‘much worse’ than anticipated, review chief says

Michael Buchanan
Social affairs correspondent
Published
9 December 2025
Hungry mothers, dirty wards and poor care are blighting England’s maternity services while staff receive death threats for working in some units, according to a new report. Baroness Amos, who is chairing a review into maternity care, said that what she has seen so far “has been much worse” than she’d anticipated.
Some women had felt blamed for their baby’s death, while others suffered from a lack of empathy, care or apology when things had gone wrong, with poor and black mothers often at the end of discriminatory services. Health Secretary Wes Streeting, who set up the review, external, said “the systemic failures causing preventable tragedies cannot be ignored”.

Speaking to BBC R4’s Today programme on Tuesday, Baroness Amos said she was “confident... that change will happen” as a result of her review. She said that while she did not have the powers afforded by a statutory public inquiry, she was seeking to identify “systemic changes” that could improve the quality of care in hospital trusts across the country. She said she had heard stories of women who are “being left in... rooms for hours on end”, adding: “women are bleeding out in bathrooms”. But she stressed that she was looking into the worst cases. “There is lots of good care out there” and many trusts are doing a “good job”, she said. Streeting said the update from Baroness Amos “demonstrates that too many families have been let down, with devastating consequences”.
The National Maternity and Neonatal Investigation is meant to draw up a series of national recommendations to improve maternity and neonatal services after previous inquiries had exposed the problems but not led to enough sustained improvements. The final report from Baroness Amos will be published in the Spring, but the interim report - her reflections and initial impressions three months into the inquiry - highlight how ingrained poor care is.
The former UN diplomat said that she recognised there was “scepticism” and “criticism” of her approach.
“Time and time again, families feel that the system has failed them. I am very keen that that does not happen this time. And I think the fact that the Secretary of State has taken such a close interest is the thing that will make a big difference.”
Several inquiries over the past decade, including investigations into maternity services in Morecambe Bay, Shrewsbury & Telford and East Kent, have led to 748 recommendations for improvements being made, according to the Amos review. Yet still the harm continues – the biggest maternity inquiry in the history of the NHS, examining around 2,500 case in Nottingham, is due to report in June while another inquiry was recently announced into care at Leeds Teaching Hospitals NHS trust.
Following visits to seven NHS trusts as well as meeting over 170 families, Baroness Amos said she had consistently come across:
a lack of cleanliness, women not receiving meals, or getting help to use the bathroom with catheters not being emptied
women not being listened to, including concerns about reduced fetal movements women of colour, working class women and those with mental health problems receiving discriminatory care
NHS organisations “marking their own homework” when babies died or were harmed, with poor behaviours, including inappropriate language not being tackled
The review has also engaged with staff in maternity services. Some reported having rotten fruit thrown at them, while others said they faced death threats after negative publicity or were attacked on social media.
Adverse media attention could make delivering high quality care more difficult, they said, although it had also acted as catalyst for improvements.
Baroness Amos’s inquiry is controversial. Some families believe that limitations on what it can do, and the short time is has to do it, will mean that meaningful action cannot follow.
Emily Barley of the Maternity Safety Alliance, which wants to see a statutory public inquiry into maternity failings, said the initial reflections had “prioritised” staff feelings while minimising the “avoidable harm taking place in NHS maternity services every day”. “This is entirely the wrong process to fix the deep seated and long standing failings in maternity care and we do not understand why [Wes Streeting] is allowing this farce to continue.”
Tom Hender, whose son Aubrey was stillborn in 2022, believes a full public inquiry is the “only credible option”.
“The review is already finding more than the chair expected,” he said. “That should be the clearest sign that the scope isn’t suitable and that the issues are bigger than the timescale can handle.”
Streeting will chair a new National Maternity and Neonatal Taskforce in the New Year which will be responsible for implementing Baroness Amos’s recommendations. He promised that families who’ve suffered poor care “will remain at the heart” of what follows the review.
James Titcombe, a long standing maternity safety campaigner since he lost his son Joshua in 2008, said that while the issues identified by Baroness Amos “mirror long-standing problems we’ve known about for years,” he was supportive of its work as representing “the best opportunity in a generation to finally put maternity services on a safer path.”
Rhiannon Davies, who lost her daughter Kate in 2009 and was instrumental in setting up the inquiry into Shrewsbury and Telford Hospital NHS Trust, said she believes Baroness Amos “is listening, and we must ensure her work leads to real, urgent change when she publishes her findings next year”.

Victims of maternity failings say they are “disappointed” by the findings of an interim report they fear will have “no teeth” to make changes.
An investigation into NHS maternity services is under way after a series of shocking scandals.
The National Maternity and Neonatal Investigation (NMNI) is being led by Baroness Amos, who said “nothing prepared her” for the amount of “unacceptable care” families currently receive.
A report has been released documenting her initial reflections and impressions after meeting families and visiting hospitals.
She will investigate 12 NHS trusts in total, including Oxford University Hospitals (OUH), which runs the world-renowned John Radcliffe Hospital.

Rebecca Matthews formed a campaign for families failed by OUH after her own traumatic births.
Asked to discuss the care she received, she said she “could only describe it as callous”.
“There wasn’t any kindness there. I was left in my own blood,” she added.
Ms Matthews recently took part in evidence-gathering sessions held by Baroness Amos. But when she read her interim report, she said it was “disappointing”, as it appeared to be “a bullet point list of failings that actually we’ve seen time and time again in independent reviews”.
“The reflections don’t mention accountability at all,” she said. ‘Why are we struggling to provide?’
Based on her initial inquiries, Baroness Amos found common themes, including women not being listened to and being “disregarded” when they raised concerns.
Many weren’t given the right information to make informed choices about their care.
She was told of discrimination against women of colour, working-class mothers, or parents who were younger.
A “staggering” 748 recommendations have been made about NHS maternity services in recent years, Baroness Amos revealedand she does “not understand why change
has been so slow”.
She asked: “Why are we in England still struggling to provide safe, reliable maternity and neonatal care everywhere in the country?”
Baroness Amos told Sky News’ Mornings with Ridge and Frost: “I have been shocked… I’ve been shocked because there have been so many reviews before.”
She said she had been asked to come up with “clear national recommendations that will stop this and will make a difference”. “It just cannot continue, there’s too much harm, too much distress, too much trauma,” Baroness Amos said, describing the longterm consequences for families as “almost unbearable”.
Asked if there was “systematic racism in the NHS”, she said there was “clearly discrimination”.
“When a woman tells you that she is making choices that she knows may be detrimental to her because of her previous experience of healthcare, because of the racism that she has experienced, there is something additive here in terms of race,” she said.
“Inequalities is a key strand of the work that we’re doing.”
The most recent health watchdog findings paint a depressing picture of maternity services.
Almost two-thirds of acute hospital maternity services were judged either inadequate or required improvement for safety. This investigation is not due to report back fully until the spring.
But some campaigners are already worried it won’t bring meaningful change to maternity services.
Ms Matthews said it “seems as though it’s heading the same way that other reviews have gone in the past, leading to some recommendations but no teeth”.
“We need some mechanisms that are going to hold people and systems to account,” she said.
OUH chief nurse Yvonne Christley said in a statement that “feedback received from patients using our maternity service over the last year is positive overall”.
“However, we know we have more to do to improve our maternity services,” she added.
“Our present focus is on listening to the experiences of women and families, which is helping us to identify opportunities for improvement.”
“If you don’t try to unpick why previous recommendations haven’t been implemented and what’s going wrong with toxic cultures in maternity, what’s going wrong with misogynistic practices in maternity, then how on earth are we is the harm going to come to an end? Rebecca Matthews’ children are now nine and four but she still remembers the trauma of their births. I was in so much pain that I just wanted to die. I was screaming in pain and I asked for pain relief and I was just off the paracetamol. I felt that not being listened to was what caused the harm.“
“Rebecca formed a campaign for families failed by Oxford University hospitals. One of 12 trusts under investigation by a national review. Rebecca gave evidence to the chair Baroness Amos. but is disappointed with her initial findings. failings with a total of over 700 recommendations made. But overall our maternity services are still performing really poorly. Baroness Amos says nothing prepared her for the scale of unacceptable care that women and families have received and continue to receive. But so she’s heard how parents aren’t listened to, how mother’s instincts are disregarded, and how there’s a lack of empathy, care or apology when things go wrong. And she found poor standards of basic care, like a lack of cleanliness or women not being given meals. It’s definitely not what many wanted to hear, but this is only the beginning. The full report will be out in the spring.”

Original 18 Key Frame drawings to base the animated sequence of the cervix softening and opening.

Skin Tone Tests
Sketch book pages looking at a wider range of skin tones that are represented in existing material centred around birth communication.



In terms of visual work, following the conversations I have had with Susana and Shalayna, brown women are underrepresented in much literature, and modest clothing is also missing from the visual representation of the women the Royal London supports. I have been developing my time-based skills and have been working on the representation of a pregnancy from 12 weeks to full term- this is obviously not new knowledge. I started with 18 key-frame drawings as seen on pages 20 and 21. I then drew frame by frame, with the foetus bouncing through week by week, to 100-plus frames of the head being born. This stage of birth is usually a slow process, especially for first-time mothers, and is different for every birth. Once the shoulders are born, the baby seems to shoot out with the waters if they haven’t broken or been broken.,
I have been focusing on the visual of how the cervix shortens, softens and opens as labour progresses. We are taught from an early age to hold the contents of our bodies in; the pelvic floor acts as a device to stop us leaking urine. Be aware of your pelvic floor and the exercises you need to do post-pregnancy and in the peri and menopause. We have an inner sphincter within our external sphincter, which signals the external sphincter to relax so our brain can relax and pass a bowel movement. Everything we are encouraged to do is defenestrated during labour: we can visualise the pelvic floor opening and be aware of the oxytocin that a birthing mother’s brain produces to build contractions that enable the uterus to contract and the cervix to soften and open. The baby moves from having the head engaged to moving down the birth canal to the head being born and the body sliding out once the shoulders are clear. If we could see this, would it be easier to stay present and not panic when we experience painful contractions? Then, panic triggers the release of opposing chemicals in the brain, such as adrenaline. Adrenaline blocks the release of endorphins, which then stops the contraction. The BBC podcast Series 1. ‘Child’ episode 14, named ‘Pain’, presented by India Rakkasan, explains this with guest experts, covering this as an audio. The podcast made me consider- how could a visualisation of this help women understand how their bodies work in labour and thus not work against their bodies as we panic at the perceived and reality of pain during labour.
Key Frames for baby being born and on next page the placenta exiting the womb.
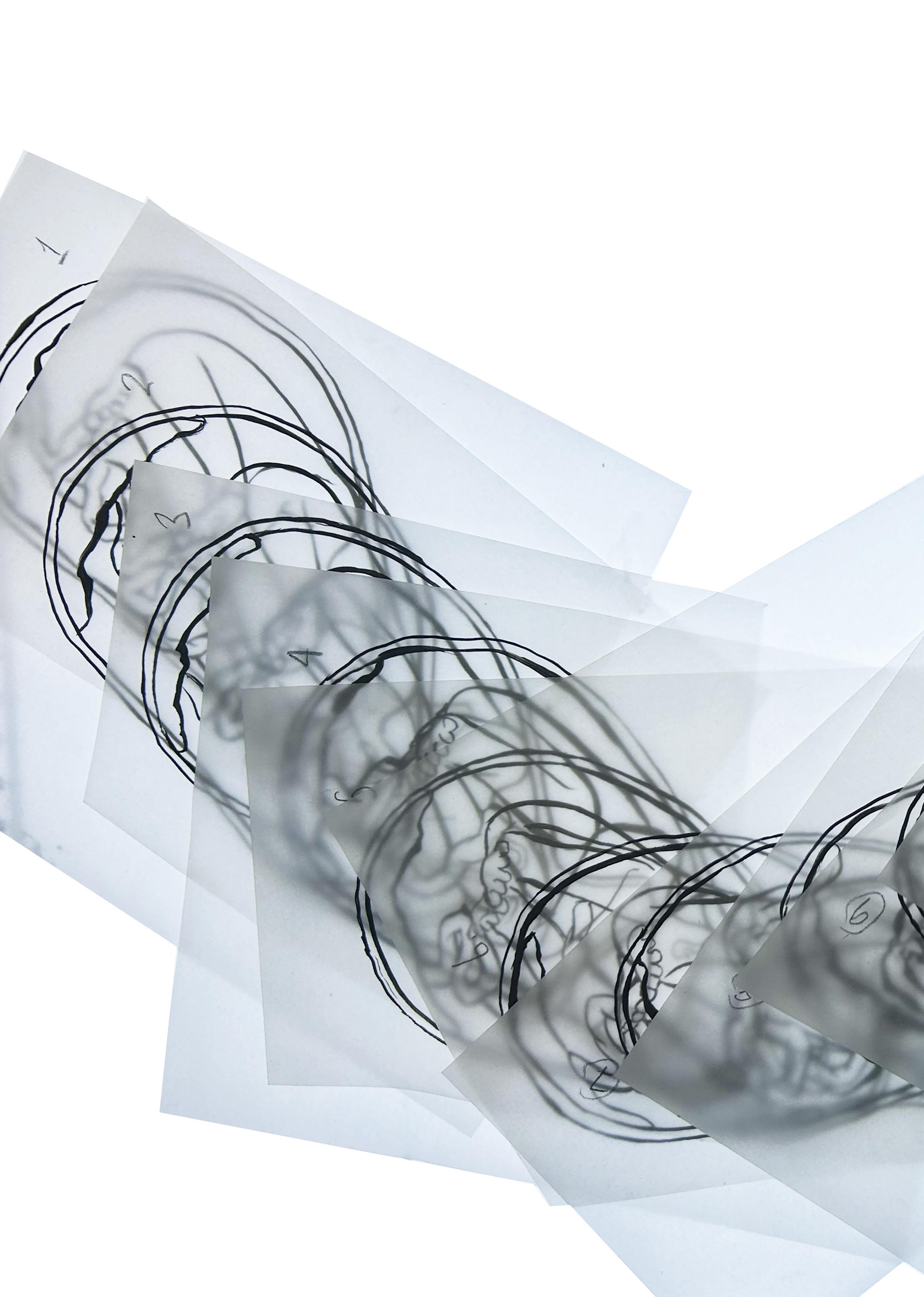





The pages show my experiments with the colour of a baby in utero, the amniotic fluid, the umbilical cord, and the placenta. As a food illustrator, one of my rules for making drawn food visually appetising is to avoid black within the image. I have applied this principle to these illustrations. I have no evidence of this, but I assume we don’t see our insides as black, unless they’re seen as sinister or as a foreign object. I have made a palette from the second reader, translating a set of watery black ink marks into a full-colour palette using Photoshop’s colour balance and levels settings. To avoid a black key line, I have created the key line in a darker tone than the information below. My daughter pointed out that Peppa Pig has a similar visual language! The eyeballs and plimsoles are the only black elements in the visual field, apart from Zoe Zebra’s stripes.



Developed imagery of a fetus in utero, Looking at wider skin tone representation, how the cervix softens and opens before delivery.

Whilst researching over the past weeks, I have been sent a range of Instagram posts, obviously thinking I am having a baby. Some of the biology posts have included the real diagram of the uterus and how it sits within other digestive organs, with the fallopian tubes snugly at the sides and the ovaries next to the neck of the womb. Imaging examples have been sent, showing the differences between an X-ray, MRI, and CT scan of a banana. The following image shows how a fetus presents as an MRI scan, which is downright terrifying and the reason that women have Ultrasound scans, which do no damage to a developing fetus. X-rays can pose a slightly increased risk of childhood cancer and, in very high doses during the first trimester, potentially lead to congenital disabilities or other developmental issues. The other imagery on these pages is from Dr Maggie Gray’s pregnancy. Maggie has updated me with the range of fruits and comparable vegetables to illustrate her growing baby. Surely a butternut squash comes in an array of sizes? Oddly, fruit and veg are so commonly used in communication regarding women’s biology and health. Fibroids are also compared to grapes, plums, peaches, oranges, and even melons if you are really suffering! I am currently being bombarded with a range of historical baby names from Instagram. Maggie sent me this disgustingly rendered image to communicate and congratulate her on reaching 28 weeks of gestation. If I thought my baby was going to look like this, I would be thinking twice about delivering and keeping it! It is truly spooky, emaciated, with swollen joints, resembling an older adult, yet it remains babyish.