12 minute read
Sacropelvic Fixation
Indications, Options, Techniques, and Future Directions
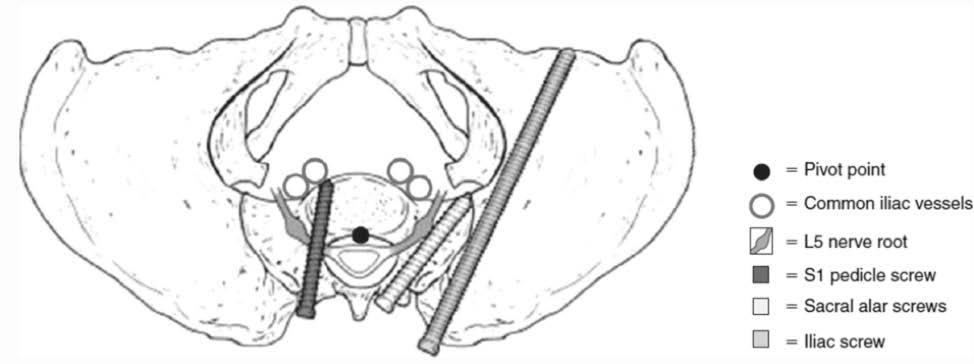
With an increasing number of long fusion constructs in adult spinal deformity (ASD), the rate of pseudoarthrosis and fixation failure at the lumbosacral junction remains high. Kim et al found that the overall prevalence of pseudoarthrosis following long adult spinal deformity instrumentation and fusion to S1 was 24%, which was significantly higher than those who were fused to L5.1,2 This is in part due to the poor bone quality of the sacrum and the high biomechanical forces at the lumbosacral junction. To combat these complications, pelvic fixation was introduced. By incorporating the ilium there are multiple long paths for screw trajectories through dense bone to decrease the rate of pseudoarthrosis and fixation failure (Figure 1). This approach provides a more stable foundation for long spinal constructs.

Pelvic fixation is often considered in scenarios that place increased mechanical stress on the lumbosacral junction and posterior instrumentation, increasing the risk of construct failure. Key indications include long spinal constructs, high pelvic incidence, planned large sagittal deformity corrections, osteoporosis, lumbosacral transitional anatomy, obesity, and revision surgeries with compromised sacral bone quality.3 Lee et al found that among 327 patients who underwent fusion to the sacrum using S1 pedicle screws, there was a higher nonunion rate with constructs greater than 3 levels, thus urging the need for stronger pelvic fixation.3 However, fusing to the pelvis is not indicated in all patients. Fusing to the pelvis may be avoided in patients with a healthy L5S1 disc without instability or stenosis, short-segment fusion constructs that end above L5, and functionally active or young patients who want to preserve lumbosacral motion.
Iliac Fixation Evolution, 1980s-2020
Iliac fixation has undergone many changes over the past half century (Table). It was first described by Allen and Ferguson in the 1980s with the introduction of the Galveston technique.5 They utilized a Steinman pin to develop their intraosseous trajectory from the lower margin of the posterosuperior iliac spine (PSIS) through the ilium between the inner and outer tables ending above the sciatic notch. This was then replaced with an L shaped rod. The classic Galveston technique was associated with high rates of pseuoarthrosis, and inserting the contoured rod into the ilium was very difficult.6
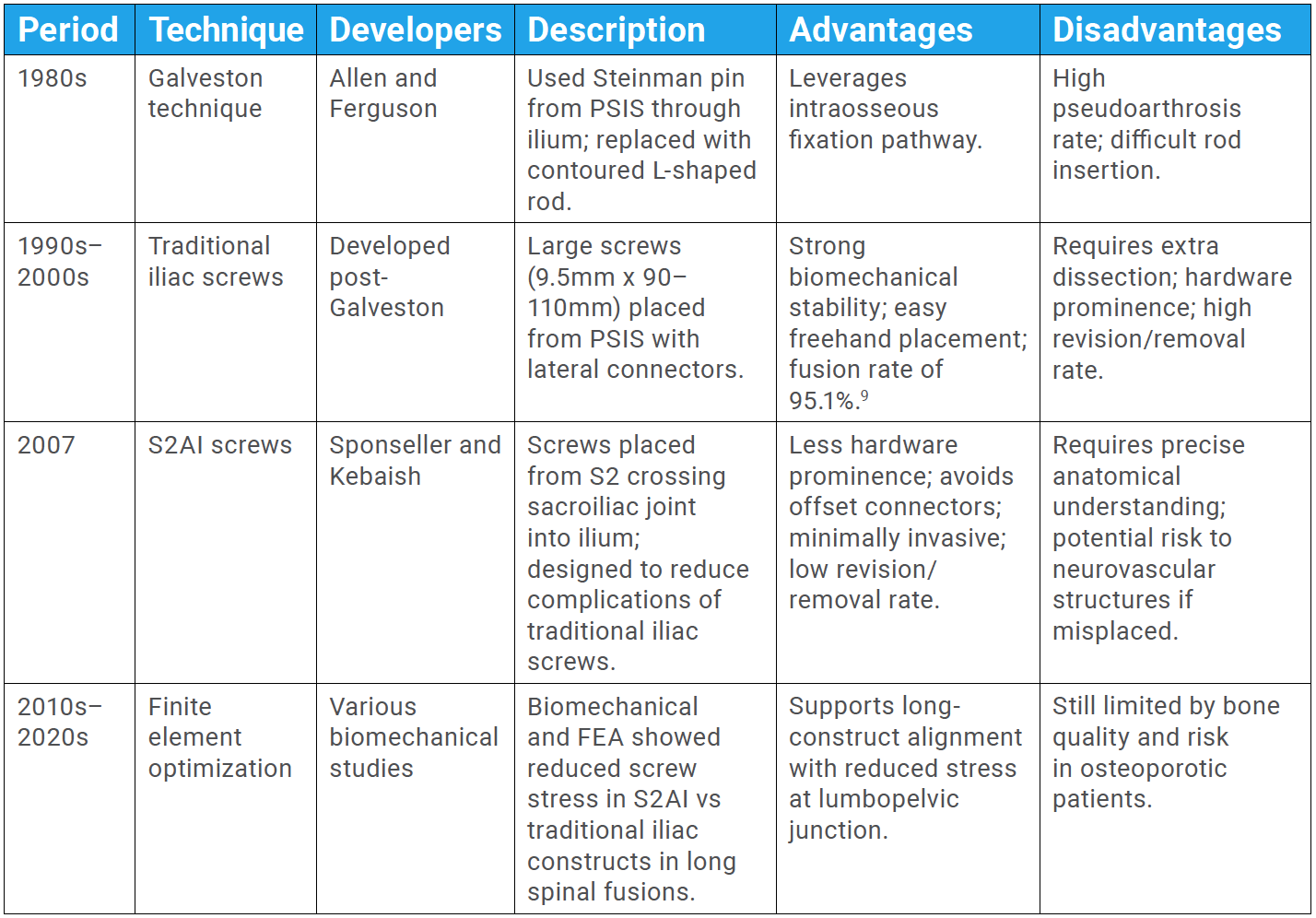
Building upon the biomechanical properties of the Galveston technique, iliac screws were developed. When measuring the maximum moment and stiffness at failure between various bovine constructs, biomechanical analysis revealed that long iliac screws and Galveston constructs performed the best.7 Traditional iliac screws with lateral connectors have many advantages, including a large channel of bone for fixation, relatively easy freehand placement, and ability to place large screws of 9.5 mm diameter and 90-110 mm length.8 Kuklo et al found that when incorporating bilateral iliac screws to lumbosacral fusions, they had a fusion rate of 95.1%.9 However, traditional iliac screw placement requires additional dissection, often results in prominent hardware, and carries a high rate of revision or removal.6,10
The evolution of iliac fixation progressed to crossing the sacroiliac joint with a S2 alar iliac (S2AI) screw developed by Sponseller and Kebaish in 2007.11 Finite element analysis of screw stress in L1-pelvis and L3-pelvis posterior spinal fusions without interbodies showed that S2AI screws had the least amount of screw stress compared to iliac screw fixation.12,13 There are many advantages to using a S2AI screw for sacropelvic fixation, including ability to place the screws using more minimally invasive techniques, strong inline connection with cranial screws, low rate of removal and revision, no need for an offset connector, and less hardware prominence.
Surgical Techniques
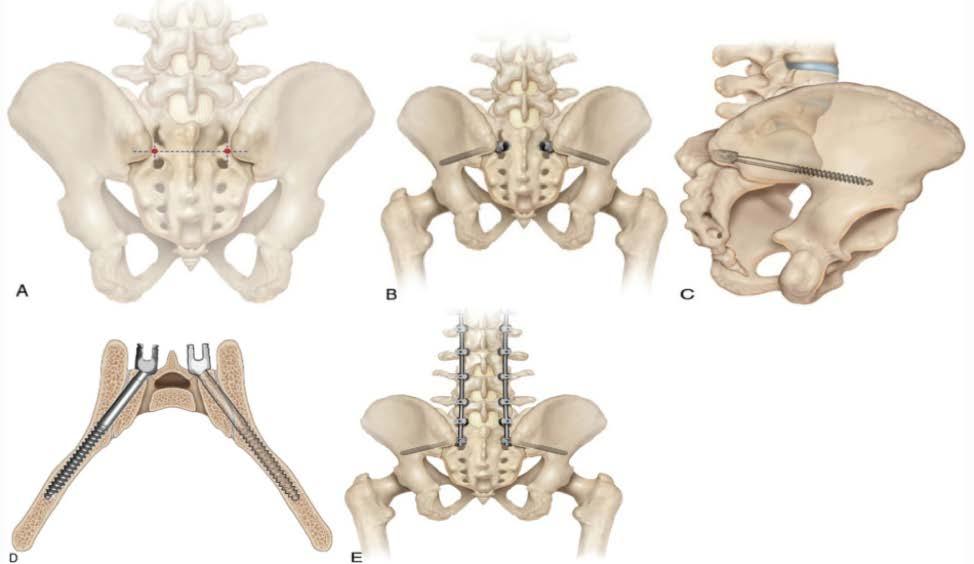
Whether placing iliac screws, S2AI screws, or hybrid constructs, the positioning, radiographic views, and incisions are similar. The patient is positioned prone on a radiolucent frame. Adequate fluoroscopic views are obtained, including an iliac oblique view and a teardrop view. The iliac oblique view is a 45° rollover view toward the contralateral side and should include the greater sciatic notch to ensure the screw is cranial to the notch. The teardrop view is a 40° rollover view toward the contralateral side and a 30° slant caudal. On the teardrop view, the beam should be coaxial with the screw, in line with the column of bone that runs from the PSIS to the anteroinferior iliac spine (AIIS), and the screw tip should be within the teardrop.
Iliac Screws and Modifications
The traditional starting point for an iliac screw is on the PSIS with a trajectory toward the superior portion of the acetabulum or toward the AIIS. Palpation of the ipsilateral greater trochanter can help with the correct trajectory. Biomechanical studies have shown no difference between the two trajectories of iliac screws on insertional torque, but the greatest torque is observed at screw lengths greater than 80 mm.14
In thin patients, a prominent PSIS increases the risk of symptomatic hardware and wound complications when using the traditional starting point. Two described strategies to lessen iliac screw prominence include recessing the screw head in the ilium with a PSIS osteotomy or moving the starting point more medial, on the medial aspect of the upslope of the PSIS so that the screw head is underneath the iliac crest. Even with a PSIS osteotomy, similar issues persist with a large dissection and soft tissue insult, and one may still need an offset connector. With a more medial start site there is less of a soft tissue insult, and one may not need an offset connector.
Additionally, to place multiple iliac screws to enhance fixation, one should start low in the teardrop and place the most caudal screw just above the sciatic notch. The second iliac screw will be just below the iliopectineal line. The additional screw cephalad can be used for a kickstand rod as well as further enhancing the stability of the base and helping with coronal alignment correction.
S2AI Screw Placement
The S2AI screw starts midway between the S1 and S2 dorsal foramina and the lateral border of the foramen, created using a high-speed burr.11 The trajectory is 45° to the floor and 20-30° caudal. Note that the aim should be for the AIIS so the trajectory may vary with a patient’s pelvic obliquity and sacral tilt. The optimal screw placement is proximal to the sciatic notch in the bottom of the teardrop (Figure 2C). While, S2AI screws have many advantages, if there is a cortical breach of an S2AI screw, this can lead to devastating consequences, including injury to the major vessels: internal iliac artery (anterior breach) and the superior gluteal artery (caudal breach).15
Accessory Rods
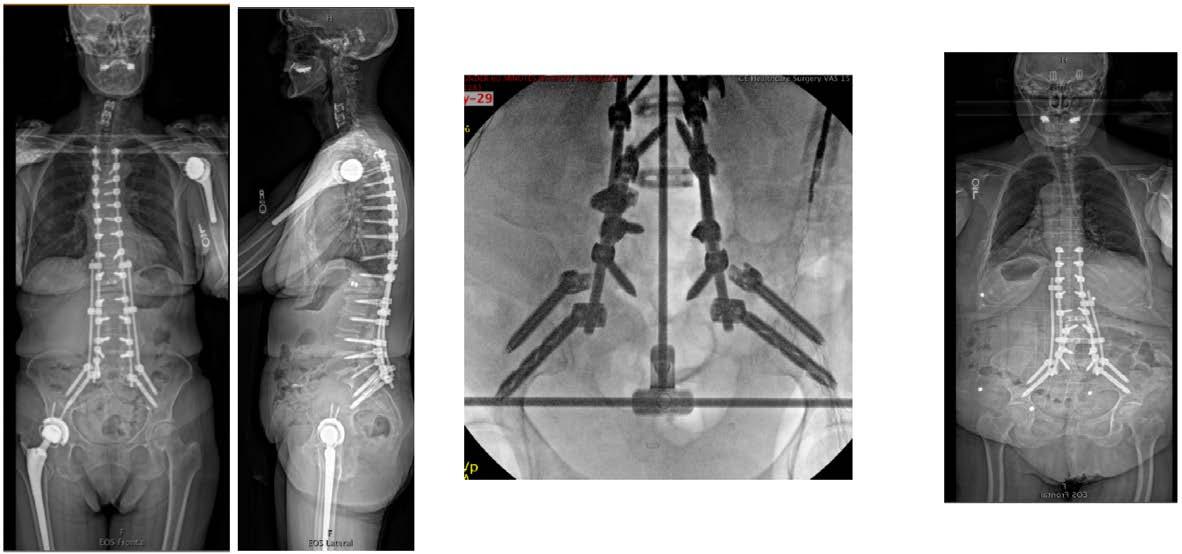
Multi-rod constructs, including satellite rods not connected to the main instrumentation and accessory rods directly attached, are increasingly utilized to augment posterior spinal fusion in complex ASD cases, particularly following extensive osteotomies (eg, pedicle subtraction osteotomy, 3-column osteotomy) or at high-stress junctions (lumbosacral, thoracolumbar), where long thoracolumbar instrumented fusions extend to the pelvis (Figure 3).17 Accessory rods have notably gained favor in techniques such as the kickstand for coronal malalignment.18 The primary benefit of these constructs lies in their ability to create locally increased stiffness. This in turn reduces rates of nonunion and instrumentation failure, specifically rod breakage across the lumbosacral junction and PSO sites.19 However, the advantage of regional stiffening raises critical questions regarding its potential remote impact on the proximal junctional biomechanics, with previous studies offering heterogeneous findings on the incidence of proximal junctional kyphosis (PJK).20 Future investigations should explore how accessory rod configurations, including their connection to pelvic fixation and their spinal termination level, influence adjacent segment motion. This can be beneficial in optimizing multi-rod strategies for enhanced long-term outcomes while mitigating the risk of PJK.
Future Directions: Role of Robotics and Navigation Systems
Robotic-assisted spinopelvic fixation offers significant advantages over traditional freehand or fluoroscopy-guided techniques, particularly for precise S2AI screw placement where the margin for error is minimal. Robotics enhance screw trajectory accuracy while reducing radiation exposure, blood loss, and operative time.21 Compared to fluoroscopy, robotics eliminates the need for repeated imaging and technical adjustments, streamlining workflow and improving safety for both patient and surgeon.22 Studies have shown comparable or superior accuracy with minimal complications, making robotic guidance a valuable tool, especially in complex spinopelvic constructs.21
Augmented reality (AR)–assisted navigation has demonstrated high accuracy in spinopelvic fixation, particularly for S2AI screw placement, with studies reporting accuracy rates exceeding 95%.23 AR enables real-time, in-situ visualization of screw trajectories, reducing cortical breaches and improving precision in anatomically complex regions like the sacroiliac joint.24 Compared to freehand or fluoroscopy-based methods, AR offers enhanced control over screw length and trajectory, minimizing the risk of neurovascular injury. While challenges such as line-of-sight issues and dependence on intraoperative CT remain, current data suggest AR-guided systems provide accuracy comparable to robotic platforms with added flexibility and lower cost.25
References
1. Kim YJ, Bridwell KH, Lenke LG, Cho KJ, Edwards CC, Rinella AS. Pseudarthrosis in adult spinal deformity following multisegmental instrumentation and arthrodesis. J Bone Joint Surg Am. 2006;88(4):721-728.
2. Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976). 2006;31(20):2329-2336.
3. Lee CS, Chung SS, Choi SW, Yu JW, Sohn MS. Critical length of fusion requiring additional fixation to prevent nonunion of the lumbosacral junction. Spine (Phila Pa 1976). 2010;35(6):E206-E211.
4. Kebaish KM, Devlin VJ. Instrumentation and fusion at the lumbosacral junction and pelvis. In: Delvin VJ, ed. Spine Secrets [ebook]. 3rd ed. Elsevier; 2020:298.
5. Allen BL, Ferguson RL. The Galveston technique of pelvic fixation with L-rod instrumentation of the spine. Spine (Phila Pa 1976). 1984;9(4):388-394.
6. Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS. Outcome and complications of long fusions to the sacrum in adult spine deformity: Luque-Galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976). 2002;27(7):776-786.
7. McCord DH, Cunningham BW, Shono Y, Myers JJ, McAfee PC. Biomechanical analysis of lumbosacral fixation. Spine (Phila Pa 1976). 1992;17(8 suppl):S235-S243.
8. Fridley J, Fahim D, Navarro J, Wolinsky JP, Omeis I. Free-hand placement of iliac screws for spinopelvic fixation based on anatomical landmarks: technical note. Int J Spine Surg. 2014;8:3.
9. Kuklo TR, Bridwell KH, Lewis SJ, et al. Minimum 2-year analysis of sacropelvic fixation and L5-S1 fusion using S1 and iliac screws. Spine (Phila Pa 1976). 2001;26(18):1976-1983.
10. Tsuchiya K, Bridwell KH, Kuklo TR, Lenke LG, Baldus C. Minimum 5-year analysis of L5-S1 fusion using sacropelvic fixation (bilateral S1 and iliac screws) for spinal deformity. Spine (Phila Pa 1976). 2006;31(3):303-308.
11. O’Brien JR, Yu WD, Bhatnagar R, Sponseller P, Kebaish KM. An anatomic study of the S2 iliac technique for lumbopelvic screw placement. Spine (Phila Pa 1976). 2009;34(12):E439-E442.
12. Shin JK, Lim BY, Goh TS, et al. Effect of the screw type (S2-alar-iliac and iliac), screw length, and screw head angle on the risk of screw and adjacent bone failures after a spinopelvic fixation technique: a finite element analysis. PLoS One. 2018;13(8):e0201801.
13. Sohn S, Park TH, Chung CK, et al. Biomechanical characterization of three iliac screw fixation techniques: a finite element study. J Clin Neurosci. 2018;52:109-114.
14. Santos ERG, Sembrano JN, Mueller B, Polly DW. Optimizing iliac screw fixation: a biomechanical study on screw length, trajectory, and diameter. J Neurosurg Spine. 2011;14(2):219-225.
15. Yamada K, Abe Y, Satoh S. Safe insertion of S-2 alar iliac screws: radiological comparison between 2 insertion points using computed tomography and 3D analysis software. J Neurosurg Spine. 2018;28(5):536-542.
16. Polly DW, Latta LL. Spinopelvic fixation biomechanics. Semin Spine Surg. 2004;16(2):101-106.
17. El Dafrawy MH, Adogwa O, Wegner AM, et al. Comprehensive classification system for multirod constructs across three-column osteotomies: a reliability study. J Neurosurg Spine. 2020;34(1):103-109.
18. Mundis GM, Walker CT, Smith JS, et al. Kickstand rods and correction of coronal malalignment in patients with adult spinal deformity. Eur Spine J. 2022;31(5):1197-1205.
19. Zhao J, Nie Z, Zhang Z, Liao D, Liu D. Multiple-rod constructs in adult spinal deformity surgery: a systematic review and meta-analysis. Asian Spine J. 2023;17(5):985-995.
20. Ye J, Gupta S, Farooqi AS, et al. Use of multiple rods and proximal junctional kyphosis in adult spinal deformity surgery. J Neurosurg Spine. 2023;39(1):320-328.
21. Arora A, Berven S. Challenges and complications in freehand S2-alar-iliac spinopelvic fixation and the potential for robotics to enhance patient safety. Global Spine J. 2022;12(2 suppl):45S-51S.
22. Shillingford JN, Laratta JL, Tan LA, et al. The free-hand technique for S2-alar-iliac screw placement: a safe and effective method for sacropelvic fixation in adult spinal deformity. J Bone Joint Surg Am. 2018;100(4):334-342.
23. Azad TD, Horowitz MA, Tracz JA, et al. Augmented reality versus freehand spinopelvic fixation in spinal deformity: a case-control study. Surg Innov. 2025;32(1):36-45.
24. Dennler C, Fekete TF, Bauer DE, et al. Augmented reality navigated sacral-alar-iliac screw insertion. Int J Spine Surg. 2021;15(1):161-168.
25. Lee MY, Shahzad H, Singh VK, Price RL, Phillips FM, Khan SN. S2 alar-iliac screw insertion safety with augmented reality–assisted surgical navigation. J Am Acad Orthop Sug Glob Res Rev. 2025;9(4):e25.00012.
Contributors:
Kelsey Hideshima, MD
Hania Shahzad, MD
Hai Van Le, MD
Safdar N. Khan, MD
Yashar Javidan, MD
From the Department of Orthopaedic Surgery at UC Davis Health in Sacramento, California.








