
11 minute read
Endoscopic Decompression for Foraminal Stenosis
Lumbar foraminal stenosis occurs due to age-related wear and tear in the spinal discs and facet joints. It commonly develops as part of the natural aging process, which causes a progressive narrowing of neural foramen (through which nerves exit the spine) and compresses the nerve roots in the lower back. This condition most often affects the L4-L5 and L5-S1 segments and is caused by different factors such as reduced height of the foramen, herniated discs, bone spurs, thickened ligaments and enlarged facet joints.1,2 This pathology accounts for about 8% to 26% of degenerative spine disorders that can lead to long-lasting symptoms with a negative impact on quality of life, necessitating surgical intervention.1,3,4
Conventional surgical methods to treat this condition include wide dorsal decompression or a muscle-sparing technique known as the Wiltse approach.5 However, both techniques have limitations in visualizing the nerve as it exits through a hidden zone behind the facet joint.6 As a result, procedures have increasingly focused on minimally invasive spine surgery, and new techniques primarily aim to improve recovery time and reduce complications.7–9
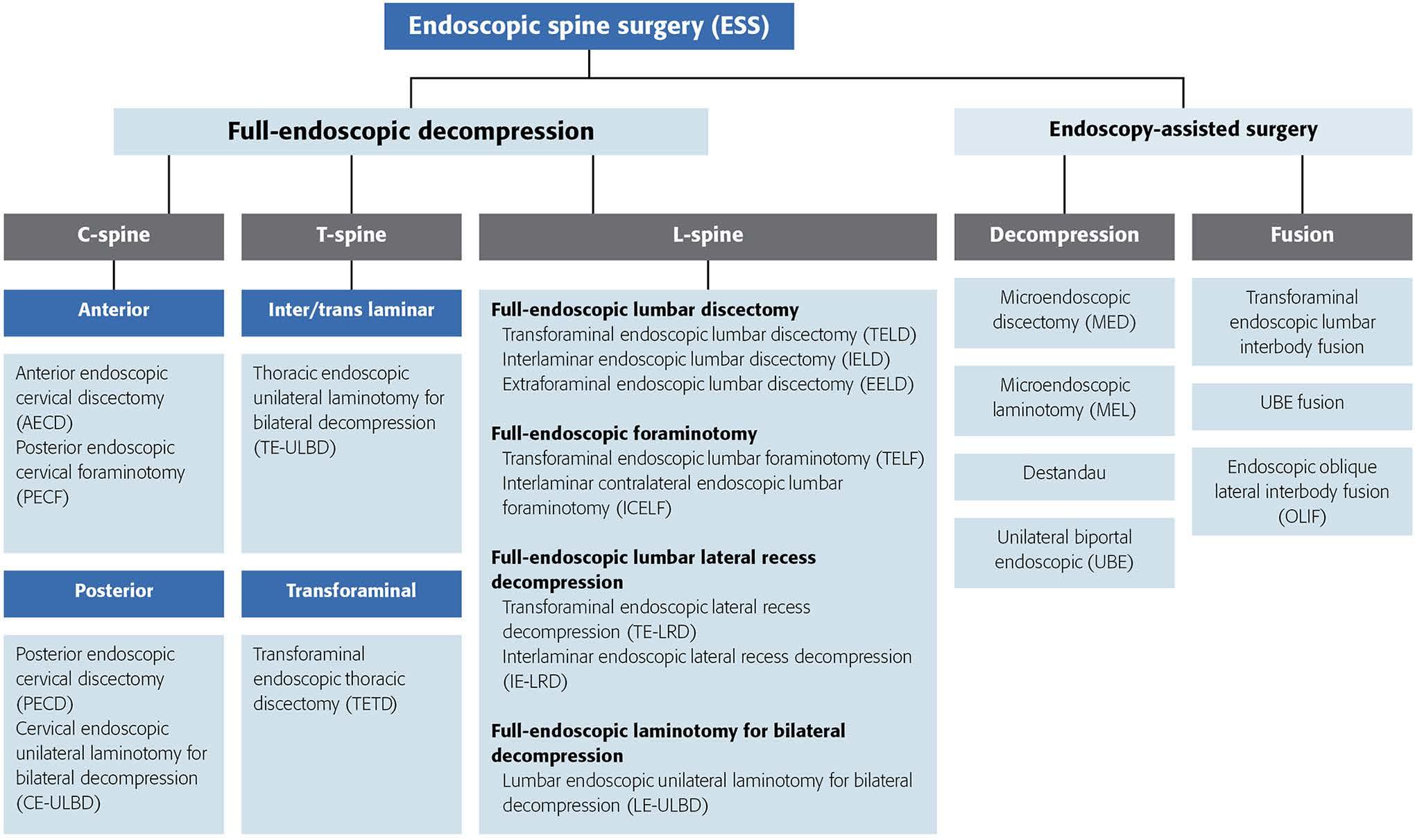
Among a wide variety of minimally invasive techniques, full-endoscopic techniques for lumbar spine have increasingly been used to treat many different spine conditions over decades.10 As various terms were developed for the techniques in this emerging era, the AOSpine Minimally Invasive Spine Surgery task force in 2020 developed a standardized terminology11 (Figure 1). The aim of this review article is to better clarify the application of endoscopic spine surgery (ESS) techniques in the treatment of lumbar foraminal stenosis, clarifying the indications for the procedure, its advantages, and related complications.
Indications and Different Endoscopic Techniques for Treatment of Foraminal Stenosis
Endoscopic decompression, for which there exists robust evidence of its efficacy in treating lumbar foraminal stenosis, has been widely adopted for lumbar foraminal and lateral recess stenosis.12 Indications for transforaminal endoscopic lumbar discectomy (TELD) typically include soft lumbar disc herniations with radiculopathy, with contraindications including significant central stenosis and segmen- tal instability.10 At the advent of endoscopic spine surgery, the main indication for TELD was contained lumbar disc herniation (LDH) without disc migration or stenosis; however, as ESS technology has advanced over time, more complicated cases such as far-lateral, highly migrated, or recurrent LDH can now also be treated with TELD.13 Although the specific indications for transforaminal endoscopic lumbar foraminotomy (TELF) have not yet been fully established, it has been established as a viable technique for patients with foraminal stenosis when preservation of segmental stability is desired. This technique aims to minimize disruption of the facet joint and paraspinal musculature.14
Interlaminar endoscopic lumbar discectomy (IELD) provides an alternative approach to the surgical management of LDH through the interlaminar window and is particularly effective for L4-L5 or L5-S1 pathology where transforaminal access may be limited by anatomical constraints. For instance, a recent systematic review by Kotheeranurak et al recommends TELD for LDH in foraminal and extraforaminal locations across all lumbar levels and for central and subarticular disc pathology at upper lumbar segments.10 Contrarily, IELD is preferred for LDH in the central or subarticular zones at L4-L5 and L5-S1, particularly when limitations such as high iliac crest positioning or high-grade disc migration otherwise prevent transforaminal access.
Interlaminar contralateral endoscopic lumbar foraminotomy (ICELF) utilizes the interlaminar window for contralateral foraminal access, proving particularly effective for unilateral foraminal stenosis with or without lateral recess stenosis at L5-S1, where high iliac crest and narrowed foraminal dimensions may restrict transforaminal approaches.15 For both approaches, complex central stenosis is a relative contraindication.16
Transforaminal endoscopic lateral recess decompression (TE-LRD) and interlaminar endoscopic lateral recess decompression (IE-LRD) address combined pathology involving both lateral recess and foraminal stenosis.17 TE-LRD uses a transforaminal approach, allowing direct access to the lateral recess and foramen, while IE-LRD uses an interlaminar approach, providing a broader decompression corridor for both the lateral recess and foraminal regions. Since TELF is limited in addressing vertical stenosis and central canal pathology, TE-LRD and IE-LRD are superior for lateral recess and foraminal stenosis, which require decompression of both traversing nerve roots.18
Lumbar endoscopic unilateral laminotomy for bilateral decompression (LE-ULBD), indicated primarily for lumbar stenosis and lateral recess stenosis especially when preservation of posterior elements and facet joints is required, takes a unilateral interlaminar approach to decompress both sides of the spinal canal.19 However, it is generally not utilized for foraminal stenosis. LE-ULBD utilizes a single working channel to decompress both sides of the spinal canal via a unilateral approach, whereas unilateral biportal endoscopic decompression (UBE) is a biportal technique that utilizes 2 separate portals: 1 for the endoscope and the other for the instruments, which offers improved flexibility, field of view, and easier manipulation of instruments. UBE provides superior facet preservation and greater radiological decompression compared to uniportal decompression.20,21
Advantages and Complications of Endoscopic Procedures
A systematic review comparing ESS and microdiscectomy for lumbar disc herniation found no difference in patient-reported outcomes and complications, while ESS had shorter hospital times and return to work.22 For other procedures, namely canal and lateral stenosis, which generally require going through bone to decompress the spine, ESS has improved patient outcomes, including reduced back and leg pain and lower complication rates.23 The advantages of reduced tissue damage resulting in more favorable outcomes have been shown in obese patients, where open surgery has long been associated with an increased rate of postoperative complications and worse outcomes resulting from increased tissue trauma. A meta-analysis comparing obese and non-obese patients undergoing ESS for lumbar spine pathology found that nonobese patients had greater improvement in visual analog scale back and leg scores and shorter operative times. However, there was no difference in Oswestry Disability Index, and the incidence of postoperative infection was low in both groups, which is typically a greater concern for obese patients.24
ESS brings many cost savings as well. A comprehensive systematic review found consistent cost savings associated with ESS compared to other techniques, with incremental cost-effectiveness ratios favoring ESS by up to €70,235 per quality-adjusted life year gained. Although ESS was sometimes linked to higher operating costs (eg, $2,972.30 vs $2,359.80), it consistently resulted in shorter hospital stays (eg, 5 vs 8.7 days), reduced indirect costs (eg, 20.1% lower in Choi et al),25 and overall societal cost reductions (eg, $15,090 vs $17,633 in Gadjradj et al).26
Complications with ESS for stenosis are more common in the perioperative period. A large systematic review of ESS techniques for decompression and fusion found a perioperative complication rate for unilateral endoscopic decompression or fusion of 9.26%, with dural tear, transient neurologic deficit, dysesthesia, radicular pain, and early recurrence being the most common.27 In unilateral biportal endoscopic surgery, an ESS technique with a shorter learning curve but considered to have a greater complication profile resulting from increased exposure, a similar trend was found, with higher rates in the perioperative period of 9.9% across decompression and fusion. The most common complications in decompression were intraoperative dural tear and epidural hematoma. Randomized controlled trials have shown significantly decreased complication rates in ESS compared to open and MIS techniques.7,8
Future Directions
In the future, ESS can be enhanced by using advanced imaging techniques. Navigation systems have been used to visualize the approach on intraoperative computer tomography in ESS and improve accuracy. Similarly, better camera technology, such as 4K and 3D equipment, allow for better visualization of tissues that are difficult to visualize. When working in such a small site, minor movements can make a large difference. Robot-assisted ESS can reduce complications or surgical time associated with such tremors.28
References
1. Konbaz F, Aldakhil S, Alhelal F, et al. Iatrogenic contralateral foraminal stenosis following lumbar spine fusion surgery: illustrative cases. J Neurosurg: Case Less. 2023;5(12):CASE2317.
2. Ahn Y, Park HB. Transforaminal endoscopic lumbar foraminotomy for juxta-fusional foraminal stenosis. J Clin Med. 2023;12(17):5745.
3. Kunogi JI, Hasue M. Diagnosis and operative treatment of intraforaminal and extraforaminal nerve root compression. Spine. 1991;16(11):1312-1320.
4. Aota Y, Niwa T, Yoshikawa K, Fujiwara A, Asada T, Saito T. Magnetic resonance imaging and magnetic resonance myelography in the presurgical diagnosis of lumbar foraminal stenosis. Spine. 2007;32(8):896-903.
5. Wiltse LL, Spencer CW. New uses and refinements of the paraspinal approach to the lumbar spine. Spine (Phila Pa 1976). 1988;13(6):696-706.
6. Orita S, Inage K, Eguchi Y, et al. Lumbar foraminal stenosis, the hidden stenosis including at L5/S1. Eur J Orthop Surg Traumatol. 2016;26(7):685-693.
7. Yang CC, Chen CM, Lin MHC, et al. Complications of full-endoscopic lumbar discectomy versus open lumbar microdiscectomy: a systematic review and meta-analysis. World Neurosurg. 2022;168:333-348.
8. Ruetten S, Komp M, Merk H, Godolias G. Surgical treatment for lumbar lateral recess stenosis with the full-endoscopic interlaminar approach versus conventional microsurgical technique: a prospective, randomized, controlled study: clinical article. J Neurosurg Spine. 2009;10(5):476-485.
9. Kim MJ, Lee SH, Jung ES, et al. Targeted percutaneous transforaminal endoscopic diskectomy in 295 patients: comparison with results of microscopic diskectomy. Surg Neurol. 2007;68(6):623-631.
10. Kotheeranurak V, Liawrungrueang W, Quillo-Olvera J, et al. Full-endoscopic lumbar discectomy approach selection: a systematic review and proposed algorithm. Spine. 2023;48(8):534-544.
11. Hofstetter CP, Ahn Y, Choi G, et al. AOSpine consensus paper on nomenclature for working-channel endoscopic spinal procedures. Global Spine J. 2020;10(2 suppl):111S-121S.
12. Liu Y, Van Isseldyk F, Kotheeranurak V, et al. Transforaminal endoscopic decompression for foraminal stenosis: single-arm meta-analysis and systematic review. World Neurosurg. 2022;168:381-391.
13. Lee SG, Ahn Y. Transforaminal endoscopic lumbar discectomy: basic concepts and technical keys to clinical success. Int J Spine Surg. 2021;15(suppl 3):S38-S46.
14. Vande Kerckhove M, d’Astorg H, Ramos-Pascual S, Saffarini M, Fiere V, Szadkowski M. SPINE: High heterogeneity and no significant differences in clinical outcomes of endoscopic foraminotomy vs fusion for lumbar foraminal stenosis: a meta-analysis. EFORT Open Rev. 2023;8(2):73-89.
15. Kim HS, Wu PH, Jie Chin BZ, Jang IT. Systematic review of current literature on clinical outcomes of uniportal interlaminar contralateral endoscopic lumbar foraminotomy for foraminal stenosis. World Neurosurg. 2022;168:392-397.
16. Chen KT, Song MS, Kim JS. How I do it? Interlaminar contralateral endoscopic lumbar foraminotomy assisted with the O-arm navigation. Acta Neurochir (Wien). 2020;162(1):121-125.
17. Li CY, Hu MH, Li CH, Chung YH. Full-endoscopic transforaminal decompression with modified reaming technique on lateral recess stenosis: outcomes of 155 cases and five years’ experience. A case series study. World Neurosurg. 2025;199:124073.
18. Li Y, Wang B, Wang S, Li P, Jiang B. Full-endoscopic decompression for lumbar lateral recess stenosis via an interlaminar approach versus a transforaminal approach. World Neurosurg. 2019;128:e632-e638.
19. McGrath LB, White-Dzuro GA, Hofstetter CP. Comparison of clinical outcomes following minimally invasive or lumbar endoscopic unilateral laminotomy for bilateral decompression. J Neurosurg Spine. 2019;30(4):491-499.
20. Tang Z, Tan J, Shen M, Yang H. Comparative efficacy of unilateral biportal and percutaneous endoscopic techniques in unilateral laminectomy for bilateral decompression (ULBD) for lumbar spinal stenosis. BMC Musculoskelet Disord. 2024;25(1):713.
21. Wu PH, Chin BZJ, Lee P, et al. Ambulatory uniportal versus biportal endoscopic unilateral laminotomy with bilateral decompression for lumbar spinal stenosis— cohort study using a prospective registry. Eur Spine J. 2023;32(8):2726-2735.
22. Qin R, Liu B, Hao J, et al. Percutaneous endoscopic lumbar discectomy versus posterior open lumbar microdiscectomy for the treatment of symptomatic lumbar disc herniation: a systemic review and meta-analysis. World Neurosurg. 2018;120:352-362.
23. Pairuchvej S, Muljadi JA, Ho JC, Arirachakaran A, Kongtharvonskul J. Full-endoscopic (bi-portal or uni-portal) versus microscopic lumbar decompression laminectomy in patients with spinal stenosis: systematic review and meta-analysis. Eur J Orthop Surg Traumatol. 2020;30(4):595-611.
24. Liawrungrueang W, Cholamjiak W, Sarasombath P, et al. Endoscopic spine surgery for obesity-related surgical challenges: a systematic review and meta-analysis of current evidence. Asian Spine J. 2025;19(2):292-310.
25. Choi KC, Shim HK, Kim JS, et al. Cost-effectiveness of microdiscectomy versus endoscopic discectomy for lumbar disc herniation. Spine J. 2019;19(7):1162-1169.
26. Golan JD, Elkaim LM, Alrashidi Q, Georgiopoulos M, Lasry O. Economic comparisons of endoscopic spine surgery: a systematic review. Eur Spine J. 2023;32(8):2627-2636.
27. Compagnone D, Mandelli F, Ponzo M, et al. Complications in endoscopic spine surgery: a systematic review. Eur Spine J. 2024;33(2):401-408.
28. Gunjotikar S, Pestonji M, Tanaka M, et al. Evolution, current trends, and latest advances of endoscopic spine surgery. J Clin Med. 2024;13(11):3208.
Contributors:
Andrea Pezzi, MD1
Cole T. Kwas, BS1
Maximillian K. Korsun, BS1
Tomoyuki Asada, MD PhD1,2
Sravisht Iyer, MD1,3
From the 1Department of Orthopaedics at the Hospital for Special Surgery in New York City, New York; 2Department of Orthopedics at the University of Tsukuba Hospital in Tsukuba, Japan; and 3Weill Cornell Medical College in New York City, New York.








