
11 minute read
The Evolution of Cervical Disc Replacement Implant Design
Cervical disc replacement (CDR) has become an increasingly popular alternative to anterior cervical discectomy and fusion (ACDF). Meta-analyses support CDR’s equivalence, and in some studies, superiority over fusion regarding long-term outcomes and adjacent-segment preservation.1 Today in the United States, there are 5 different commercially available devices for CDR following the recent departure of the M6 from the market. Each device has unique biomechanical features with implications for clinical performance. Because of this variability, spine surgeons performing CDR should understand these design-related implications in order to choose the optimal implant for each patient’s individual anatomy and pathology.
Design Characteristics of CDR Devices
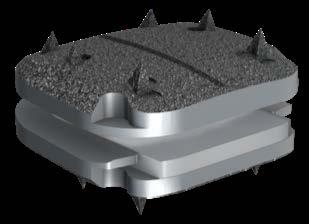
Clinically relevant design characteristics of CDR implants center on their ability to replicate natural spinal kinematics while ensuring long-term stability, biocompatibility, and appropriate mechanical constraint. A differentiating factor among implants is the degree of constraint—ranging from constrained devices (eg, ball-and-socket designs like Prodisc C) that restrict motion to a fixed center, to semi-constrained (eg, Prestige LP), and nonconstrained or mobile-bearing designs (eg, Mobi-C, Simplify) that allow some translation or independent core motion. The level of constraint influences facet joint loading, motion coupling, and potential for adjacent segment stress; for example, overly constrained designs may preserve motion but fail to mimic physiologic biomechanics, while under-constrained devices risk instability or implant migration if improperly placed. The choice of bearing surface materials—for example, metal-on-polyethylene, metal-on-metal, or newer ceramic-on-polymer combinations—affects not only the implant’s wear characteristics and durability but also its appearance on postoperative advanced imaging. Additionally, endplate fixation strategies and sizing are critical for implant stability and long-term success; designs may use central keels, lateral spikes, or porous titanium coatings to promote bony ongrowth and reduce the risk of implant migration or subsidence. Different designs offer different ranges of endplate size. Endplate sizing is thought to be important for resisting subsidence as well as maximizing coverage of bleeding cancellous bone with the goal of minimizing heterotopic ossification. The integration of these design features must be carefully balanced to optimize biomechanical performance, ease of implantation, and long-term clinical outcomes.
Implant Design Evolution
The Bryan disc, developed by Medtronic and approved by the US Food and Drug Administration (FDA) in 2009, was a cervical disc arthroplasty device featuring a viscoelastic polyurethane nucleus encased between titanium alloy endplates. Designed to replicate natural spinal kinematics, it preserved segmental motion and demonstrated excellent long-term clinical outcomes in multiple trials. At four years, the Bryan disc showed a composite success rate exceeding that of ACDF, with lower reoperation rates and maintained segmental motion.2 A 10-year follow-up IDE trial confirmed sustained safety and device integrity without evidence of nucleus degradation or spontaneous fusion.3 Despite strong data, the Bryan disc was discontinued in 2020 as newer devices with simpler instrumentation and broader indications supplanted it in the marketplace.

The Prestige LP disc, a metal-on-metal ball-in-trough design made of titanium-ceramic composite, evolved from earlier stainless-steel models like the Prestige ST. It received FDA approval in 2014 for 1-level and in 2016 for 2-level cervical disc arthroplasty. The Prestige LP was shown in a prospective, randomized IDE trial to provide noninferior or superior outcomes compared to ACDF, with significantly lower rates of reoperation and adjacent segment degeneration. At 7 years, 2-level recipients experienced fewer serious implant-related adverse events and sustained range of motion.4 Ten-year follow-up data supported the continued safety and effectiveness of the Prestige LP for both 1- and 2-level indications.5

The Mobi-C disc from Highridge (formerly Zimmer Biomet) uses a mobile ultra-high molecular weight polyethylene (UHMWPE) core situated between cobalt–chrome endplates with keel and spike fixation. It allows 1 mm of translation and 8 degrees of rotation, providing 5 degrees of freedom. Variable footprint sizes and disc heights enhance endplate loading accuracy. Preclinical and clinical data show preserved motion at 2 years and reduced revision rates compared to ACDF.6 Long-term clinical studies on the Mobi-C cervical disc have demonstrated its sustained safety and efficacy, particularly in both single-level and 2-level cervical disc replacement. In a pivotal FDA investigational device exemption (IDE) trial, Mobi-C showed noninferiority to anterior cervical discectomy and fusion (ACDF) at 1 level and statistical superiority at 2 levels, with significantly lower reoperation rates and improved Neck Disability Index (NDI) and visual analog scale (VAS) scores over a 7-year follow-up.7 Continued analysis of the IDE cohort through 10 years confirmed these benefits, with maintained segmental motion and no evidence of late device failure or implant migration.8 The 10-year data also indicated a persistent advantage over fusion in terms of overall success rates and adjacent segment degeneration, particularly in two-level procedures. These results have supported Mobi-C’s adoption as one of the most widely used artificial cervical discs in the United States, in part related to receiving the first FDA approval for 2-level implantation.

The ProDisc-C, one of the longest standing implants on the market, utilizes a fixed polyethylene core with a ball-and-socket interface. This design limits motion to a single axis and is highly constrained, making it predictable but less adaptable to natural kinematic variability. Its central keel allows for strong axial fixation, and the device is known for its low profile and straightforward insertion. However, the lack of translational or axial compliance has raised concerns about increased adjacent segment stress. A 2023 meta-analysis did find a higher incidence of heterotopic ossification with ProDisc-C compared to less constrained constructs. 9 Despite lacking a 2-level indication in the United States, its simplicity and track record have made it a reliable choice for single-level disc replacement.
The M6-C, developed by Orthofix, represented a unique approach by mimicking native disc mechanics with a silicone nucleus and polyethylene fiber annulus that allows compression, rotation, and translation. The viscoelastic core of the M6-C provides a degree of axial compressibility absent in more rigid implants, potentially offering a closer replication of native disc function. Early outcomes were promising, but structural issues such as sheath rupture and debris-related inflammation have been reported.10 Orthofix recently discontinued the M6-C cervical disc, shifting its commercial focus away from motion-preserving devices to prioritize higher-margin technologies. Communication from the company indicated that the withdrawal was driven more by strategic business considerations than clinical performance concerns. Nonetheless, emerging safety concerns—including FDA Manufacturer and User Facility Device Experience (MAUDE) reports of polyurethane core and fiber sheath delamination, late-onset infections, and osteolysis—may have contributed to the decision. Orthofix stated that it will continue postmarket surveillance and clinical study follow-up while halting new implants in the United States, ensuring continued support for existing patients and long-term data collection.

The Simplify disc, manufactured by NuVasive/Globus, received FDA approval for 1- and 2-level cervical replacement in 2021 and demonstrated higher success rates than ACDF at 2 years, showing an overall success rate of 86.7% in a 182-patient trial.11 It consists of polyetheretherketone (PEEK) and plasma-titanium endplates with a zirconia-toughened ceramic core, offering radiolucency and clear MRI visualization. Its design is biconvex with dual articulation, enabling translation, coupled motion, and a variable center of rotation. The disc is available in multiple footprints and disc heights, including a unique 4-mm height option. This lower profile may help avoid facet joint or endplate overload in patients with collapsed disc heights or tight posterior elements. Despite its unique design characteristics, some concern has been raised regarding particulate wear, osteolysis, and device failure given that this is the first CDR device utilizing a ceramic-on-PEEK bearing surface. To date, the MAUDE database has not demonstrated a clear difference in revision rates when compared with other device designs.12

Clinical Factors Affecting Choice of Implant
Selecting the optimal CDR implant requires consideration on how device characteristics impact the patient’s clinical scenario. For patients with significant facet arthropathy or segmental instability, a more constrained or semiconstrained design (such as Prodisc C or Prestige LP) may offer enhanced mechanical control and reduce the risk of postoperative hypermobility. In contrast, patients with preserved facet joints and normal sagittal balance may benefit from nonconstrained or mobile-core implants (such as Mobi-C or Simplify) that allow translation and more natural kinematics. Similarly, anatomical considerations—such as small endplate dimensions or shallow vertebral body depth— may necessitate low-profile or anatomically contoured implants, as overly large or aggressive fixation elements (eg, keels or wide footprints) can increase the risk of subsidence or endplate violation.
Patient activity level and postoperative imaging needs may also influence implant selection. High-demand or younger patients may benefit from viscoelastic designs (eg, M6C) or mobile-core implants that better distribute loading forces and absorb impact during motion. However, these same implants may be less suitable in cases where postoperative imaging clarity is a priority due to the metal artifact associated with cobalt-chromium or titanium components. In such cases, implants with MRI-compatible materials—such as the Simplify Disc, which uses PEEK and ceramic components—may be preferable. Furthermore, in revision scenarios or cases with borderline bone quality, implants with simplified fixation mechanisms or porous-coated endplates that promote osseointegration without deep keel cuts may reduce surgical risk. Ultimately, no single CDR design is universally superior; the ideal choice must reflect a nuanced consideration of biomechanics, imaging requirements, and patient-specific anatomical and functional demands.
Conclusion
Cervical disc replacement designs have evolved to closely emulate spinal anatomy and function. Modern implants offer diverse biomechanical profiles, but each design introduces unique clinical considerations. By matching implant mechanics to patient-specific factors and maintaining a commitment to long-term surveillance, surgeons can optimize outcomes and further establish CDR as a cornerstone of motion-preserving cervical spine care. While device design characteristics are important, modern CDR success still requires appropriate patient selection and precise technique. As surgeons gain more experience with these technologies, future iterations will likely emphasize better personalization of implant geometry and intraoperative kinematic feedback. As the field progresses, a deeper understanding of device-tissue interaction, validated through clinical trials and biomechanical studies, will help define the next generation of cervical arthroplasty devices.
References
1. Wang Q li, Tu Z ming, Hu P, Kontos F, Li Y wei, Li L, et al. Long-term results comparing cervical disc arthroplasty to anterior cervical discectomy and fusion: a systematic review and meta-analysis of randomized controlled trials. Orthop Surg. 2020;12(1):16–30.
2. Sasso RC, Smucker JD, Hacker RJ, Heller JG. Clinical outcomes of BRYAN cervical disc arthroplasty: a prospective, randomized, controlled, multicenter trial with 24-month follow-up. J Spinal Disord Tech. 2007;20(7):481–491.
3. Lavelle WF, Riew KD, Levi AD, Florman JE. Ten-year outcomes of cervical disc replacement with the BRYAN cervical disc: results from a prospective, randomized, controlled clinical trial. Spine (Phila Pa 1976). 2019;44(9):601–608.
4. Gornet MF, Lanman TH, Burkus JK, et al. Cervical disc arthroplasty with the Prestige LP disc versus anterior cervical discectomy and fusion, at 2 levels: results of a prospective, multicenter randomized controlled clinical trial at 24 months. J Neurosurg Spine. 2017;26(6):653–667.
5. Gornet MF, Lanman TH, Kenneth Burkus J, et al. Two-level cervical disc arthroplasty versus anterior cervical discectomy and fusion: 10-year outcomes of a prospective, randomized investigational device exemption clinical trial. J Neurosurg Spine. 2019;31(4):508–518.
6. Davis RJ, Kim KD, Hisey MS, et al. Cervical total disc replacement with the Mobi-C cervical artificial disc compared with anterior discectomy and fusion for treatment of 2-level symptomatic degenerative disc disease: a prospective, randomized, controlled multicenter clinical trial: clinical article. J Neurosurg Spine. 2013;19(5):532–545.
7. Radcliff K, Davis RJ, Hisey MS, et al. Longterm evaluation of cervical disc arthroplasty with the Mobi-C© cervical disc: a randomized, prospective, multicenter clinical trial with seven-year follow-up. Int J Spine Surg. 2017;11(4):244–262.
8. Nunley PD, Hisey M, Smith M, Stone MB. Cervical disc arthroplasty vs anterior cervical discectomy and fusion at 10 years: results from a prospective, randomized clinical trial at 3 sites. Int J Spine Surg. 2023;17(2):230–240.
9. Sheng XQ, Wu TK, Liu H, Meng Y. Incidence of heterotopic ossification at 10 years after cervical disk replacement: a systematic review and meta-analysis. Spine (Phila Pa 1976). 2023;48(13):E203.
10. Häckel S, Gaff J, Pabbruwe M, et al. Heterotopic ossification, osteolysis and implant failure following cervical total disc replacement with the M6-CTM artificial disc. Eur Spine J. 2024;33(3):1292–1299.
11. Coric D, Guyer RD, Bae H, Nunley PD, Strenge KB, Peloza JH, et al. Prospective, multicenter study of 2-level cervical arthroplasty with a PEEK-on-ceramic artificial disc. J Neurosurg Spine. 2022;37(3):357–367.
12. Altorfer FCS, Kelly MJ, Avrumova F, Zhu J, Abjornson C, Lebl DR. Reasons for revision surgery after cervical disc arthroplasty based on medical device reports maintained by the United States Food and Drug Administration. Spine (Phila Pa 1976). 2024;49(20).
Contributor: Brandon P. Hirsch, MD
From DISC Sports and Spine Centers in Newport Beach, California.








