Viral Hepatitis: HCV and HBV Screening and Treatment Support






• Describe the transmission of HCV and HBV, including common drivers, at-risk populations, and long-term consequences of untreated infection
• Implement screening recommendations and support follow-up to care for patients with positive test results
• Educate patients on the effectiveness of treatment options and facilitate adherence to therapy



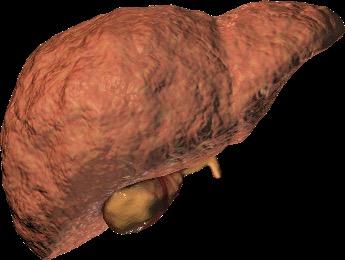
• A contagious liver infection caused by the hepatitis virus that is transmitted through blood or bodily fluids
• 5 main types of hepatitis virus (A-E); we will focus on HCV and HBV




























ESLD, end-stage liver disease; HCC, hepatocellular carcinoma; , person-years. 1. Hepatitis C Online. https://www.hepatitisc.uw.edu/go/evaluation-staging-monitoring/natural-history/core-concept/all; 2. Centers for
https://www.cdc.gov/hepatitis/statistics/2020surveillance/hepatitis

Psychiatric Depression

Blood Anemia
Impaired blood clotting
Blood cancers

Joints
Arthritis

Immune System
Abnormal immune responses
Connective tissue disease

Kidney
Acute/Chronic kidney inflammation/dysfunction
Excess fluid retention

Eye Inflammation
Ulcerations

Blood Vessels
Immune-triggered damage resulting in skin, joint, muscle, gastrointestinal tract, heart, kidney, and nervous system manifestations

Skin
Photosensitivity
Immune-triggered skin rash, lesions, or ulcerations

C, et al. J Clin Med. 2022;11(21):6247; Cacoub P, Saadoun D. N Engl J Med. 2021;384:1038-1052.

Nerves and Muscles
Muscle weakness/pain
Joint inflammation/pain

1769 • 101,525 new cases of chronic HCV1 – Highest rates among ages 30 to 49 years • 2.4 million people with chronic HCV2 – Rate 3.3 times higher in non-Hispanic American Indian/Alaska Natives vs non-Hispanic White people 1 in 3 people with HCV do not know they have it3 HCV-related deaths in 20231

• 17,650 new cases of chronic HBV4 – Highest rates among ages 30 to 49 years • 640,000 people with chronic HBV5
– Rate 9.9 times higher in non-Hispanic Asian/Pacific Islanders vs non-Hispanic White people
1 in 2 people with HBV do not know they have it5

1. CDC. https://www.cdc.gov/hepatitis-surveillance-2023/hepatitis-c/index.html; 2. CDC. https://www.cdc.gov/hepatitis-c/about/index.html; 3. CDC. https://www.cdc.gov/hepatitis-c/hcp/diagnosis-testing/index.html; 4. CDC. https://www.cdc.gov/hepatitis-surveillance-2023/hepatitis-b/index.html; 5. CDC. https://www.cdc.gov/hepatitis-b/about/index.html.
HBV-related deaths in 20234
• Percutaneous or mucosal exposure to infected blood or body fluids via1:
1. IDU2,3
• Includes shared equipment and unsterilized syringes
• Leading cause of hepatitis transmission in the US4,5
2. Unprotected sex2-4
• 38.2% of acute HBV infections (2013-2018)
3. Mother-to-child, typically during delivery2
• HCV-positive pregnancies increased 16-fold (1998-2018)6



• HBV-positive pregnancies increased by 5.5% annually since 19987

1. World Health Organization (WHO). Guidelines for the prevention, diagnosis, care and treatment for people with chronic hepatitis B infection. Geneva; March 2024. https://iris.who.int/server/api/core/bitstreams/34470cc8 -af90-4d7b-a949-ef27e5d0726f/content; 2. CDC. https://www.cdc.gov/hepatitis/php/surveillance-guidance/hepatitisb.html#:~:text=Background,least%207%20days%20(46); 3. CDC. https://www.cdc.gov/hepatitis -surveillance-2023/hepatitis-c/figure-3-7.html; 4. Perez-Molina JA, et al. Pathogens. 2023;12(9):1137; 5. CDC. https://www.cdc.gov/hepatitis-surveillance-2023/hepatitis-b/table-2-3.html; 6. Chen P, et al. JAMA Netw Open. 2023;6(7):e2324770; 7. US Preventive Service Task Force. JAMA. 2019;322(4):349-354.

• ≈70.5 million people (24.9%) have used an illegal drug or misused prescription drugs in the last year, as of 20231
• 51% of people aged ≥12 years have used illicit drugs at least once1 PWID, people who inject drugs.
1. National Center for Drug Abuse Statistics (NCDAS). https://drugabusestatistics.org/; 2. Stone J, et al. Lancet Public Health. 2022;7(2):E136-E145; 3. Ko JY, et al. MMWR Morb Mortal Wkly Rep. 2019;68(39);833-838; 4. Hepatitis B Foundation. https://www.hepb.org/blog/hepatitis-b-injection-drug-use-risks-barriers-care-prevention-strategies/; 5. Fattovich G.
2003;39(suppl 1):S50-S58; 6. National HIV Curriculum. https://www.hiv.uw.edu/go/co-occurring-conditions/hepb-coinfection/core-concept/all.
Age of Individuals Admitted to SUD
Treatment Services, 20211
Top 5 Substances for Admissions to SUD
Treatment Services, 20211

The intersection among opioid abuse, drug injecting, and viral hepatitis infection underscores the need for integrated health services in substance use disorder (SUD) treatment settings to prevent and screen for infection, as well as ensure that those who are infected receive medical care.2
https://www.samhsa.gov/data/sites/default/files/reports/rpt42794/2021
• SVR = sustained virologic response = undetectable virus
• SVR12 = SVR at ≥12 weeks following completion of treatment = HCV cure

SVR12 = HCV cure
• Hepatitis B vaccine is safe, effective, and provides lifelong protection
• For chronic HBV infection, antiviral treatment is effective!
– Suppresses the viral load, which1:
• Improves survival
• Reduces progression of liver disease and risk of HCC
• Decreases risk of transmission
– “Functional cure” is attainable
• Defined as loss of HBsAg and undetectable HBV2

Only of the adult US population is vaccinated against HBV; vaccination rates are often lower among PWID3 %30
1. WHO. Guidelines for the prevention, diagnosis, care and treatment for people with chronic hepatitis B infection. Geneva; March 2024. https://iris.who.int/server/api/core/bitstreams/34470cc8 -af90-4d7b-a949-ef27e5d0726f/content; 2. Lok ASF. Gut Liver. 2024;18(4):593-601; 3. Conners EE, et al. MMWR Recomm Rep. 2023;72(1):1-25.
Who and How?



• HCV screening at least once in a lifetime for all adults aged ≥18 yearsa
• HCV screening for all pregnant women during each pregnancya
ü One-time HCV testing
• Persons who ever injected drugs and shared needles, syringes, or other equipment
• People living with HIV (PLWH)
• Infants born to mothers with HCV infection
• People with selected medical conditionsb
• Prior recipients of transfusions or organ transplants
• Those exposed to HCV-positive blood via needle sticks, sharps, or mucosal exposures
ü Routine periodic testing
• PWID and share needles, syringes, or other equipment
• Persons with selected medical conditions, including persons who ever received maintenance hemodialysis
ü Any person who requests HCV testing should receive it, regardless of disclosed risk
aExcept in settings where the prevalence of HCV infection (HCV RNA-positivity) is <0.1%; bIncludes persons who have ever received maintenance hemodialysis, as well as those with persistently abnormal alanine aminotransferase (ALT) levels.
CDC. Clinical Screening and Diagnosis for Hepatitis C. https://www.cdc.gov/hepatitis -c/hcp/diagnosis-testing/index.html.


• HBV screening for all pregnant women during each pregnancy, preferably in the first trimester, regardless of vaccination status or history of testing
• Pregnant persons with a history of appropriately timed triple-panel screening and without subsequent risk for exposure to HBV (ie, no new HBV exposures since triple-panel screening) only need HBsAg screening
• Testing for all persons with a history of increased risk for HBV infection
• Periodic testing for susceptible persons with ongoing risk for exposures

ACTIVE
(As opposed to spontaneous or treatment-induced viral clearance)
In 2023, the CDC updated their guidance to support this 2-step HCV testing process at a single patient encounter2
Use of strategies that require multiple visits to collect samples should be discontinued2

1. HCV antibody: a positive (+) test result indicates. . .
– Acute (new) or chronic (long-term) infection
OR
– Past infection that has resolved through spontaneous clearance or has been cured with treatment
OR
– Rarely, a false-positive result; all positive results should be worked up
HCV antibodies persist indefinitely; therefore, this test should not be used to assess for reinfection.
HCV antibodies are not protective; a person can be reinfected.
2. HCV RNA: a positive (+) test result indicates. . .
– Active (current) HCV infection
HCV RNA testing is confirmatory.
AASLD/IDSA. HCV Testing and Linkage to Care. https://www.hcvguidelines.org/evaluate/testing -and-linkage.

• 3 proteins encoded by HBV, which are integral to its viral structure


• 3 proteins produced in response to specific antigens recognized as foreign







HbsAg

Anti-HBs Anti-HBc Interpretation1,2
+ ± + Currently infected with HBV
− − − Never infected with HBV; never vaccinated against HBV
− + − Vaccinated/Protected against HBV
− + + Resolved HBV infection; no risk of transmission
− − + Interpretation unclear; resolved infection, chronic infection, occult infection or false positive
Antigens
HbsAg: surface antigen
HbeAg: “e” antigen
HbcAg: core antigen
Antibodies
Anti-HBs: surface antibody
Anti-Hbe: “e” antibody
Anti-HBc: core antibody
Unlike with HCV, people who have cleared the initial acute HBV infection will develop antibodies and have lifelong protection against future HBV infection.
1. North Carolina State Laboratory of Public Health. https://slph.dph.ncdhhs.gov/doc/Hepatitis-A-and-B-Serology-Interpretation-Charts.pdf; 2. Hepatitis B Foundation. https://www.hepb.org/assets/Uploads/Provider-Infographic.pdf?
• Institute opt-out testing
– All adult patients get tested; individuals can decline
– Advantages: normalizes testing and reduces stigma
• Employ triple testing


– Including reflex testing of HCV RNA if HCV antibody is positive
– Advantages: reduces incomplete testing and facilitates earlier linkage to treatment and/or vaccination
• Consider EMR prompts
– Systemwide testing reminders
– Advantages: increases testing and use of preferred tests
EMR, electronic medical records. Slide courtesy of Stacey Trooskin, MD, PhD.




Treatment is recommended for ALL PATIENTS with chronic HCV infection, except those with a short life expectancy that cannot be remediated by treating HCV, by liver transplantation, or by other directed therapy. Patients with a short life expectancy owing to liver disease should be managed in consultation with an expert.
Rating: Class I, Level A


AASLD/IDSA. When and in Whom to Initiate HCV Therapy. https://www.hcvguidelines.org/evaluate/when-whom.
• Past or current IDU
• Concurrent MOUD
• HIV/HCV coinfection
• Previous treatment failure
• Liver cirrhosis

High rates of HCV cure are demonstrated in ALL patients1

• First introduced in 2019 for treatment-naive persons, with the goal of expanding the pool of clinicians who can provide HCV treatment
• Boosts accessibility and delivery of care
• Reduces pretreatment and on-treatment clinician intervention
• Is safe and effective

Bhattacharya D, et al. Clin Infect Dis. 2023;ciad319.

• Adults with chronic HCV (any genotype), including those with HIV, who have NOT previously received HCV treatment


• Adults with ANY of the following:
– Prior HCV treatment
– HBsAg positive (risk of HBV reactivation)
– Compensated cirrhosis with ESRD
– Current or prior decompensated cirrhosis
– Current pregnancy
– Known or suspected HCC
– Prior liver transplantation

ESRD, end stage renal disease. Bhattacharya D, et al. Clin Infect Dis. 2023;ciad319.

1. Laboratory testing
aAssess for cirrhosis
q Calculate Fib-4 score
q Complete blood count
q Hepatic function panel
aEstimated glomerular filtration rate
aQuantitative HCV RNA (HCV viral load)
aHIV antigen/antibody test
aHBsAg
aSerum pregnancy testing and counseling

2. Medication reconciliation
aPotential DDI assessment
3. Patient education
aDAA administration and adherence
aPrevention of reinfection
aAvoiding excess alcohol
Safe, Effective, Short Duration, and Curative Recommended Regimens
• Glecaprevir/Pibrentasvir (Mavyret), 300/120 mg
– Taken with food
– Duration of 8 weeks

• Sofosbuvir/Velpatasvir (Epclusa), 400/100 mg
– Duration of 12 weeksa
aPatients with genotype 3 require baseline NS5A resistance-associated substitution (RAS) testing. Those without Y93H can be treated with 12 weeks of sofosbuvir/velpatasvir. If Y93H is present, see HCV guidance for treatment recommendations. Bhattacharya D, et al. Hepatitis C Guidance 2023 Update: American Association for the Study of Liver Diseases– Infectious Diseases Society of America Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. CID. 2023. https://doi.org/10.1093/cid/ciad319. OR Both regimens offer cure rates over 95%, are once daily, and are well tolerated.



MINMON approach,
components1
1. No pretreatment genotyping
2. Entire treatment course dispensed at entry (SOF/VEL×12 weeks; 84 tablets)
3. No scheduled visits or laboratory monitoring
4. Remote contact at week 4 (adherence) and week 22 (to schedule SVR assessment at week 24)
≥12 weeks following completion of therapy
• Assess quantitative HCV RNA and hepatic function
– To confirm HCV RNA is undetectable (cure)
• If cure not achieved, refer to specialty care
– To confirm transaminase normalization
• If elevated transaminases, assess for other causes of liver disease

Bhattacharya D, et al. Clin Infect Dis. 2023;ciad319.
• Prior DAA therapy
• Advanced decompensated cirrhosis or HCC
• Positive HBsAg
• Patients whose prior authorization requests have been denied
– Large clinics typically have multidisciplinary teams of pharmacists and case managers who are familiar with this process
• Patients on a liver transplant list
– These patients often benefit from being HCV positive, as this can lead to more possible matches

AASLD/IDSA. https://www.hcvguidelines.org/wp-content/uploads/2025/09/HCV-Test-and-Treat-Final-011725.pdf.

a HCV is curable with treatment
a Treatment is both feasible and highly effective in PWUD
a Treatment is as simple as 1 to 3 pills once per day, taken for approximately 8 to 12 weeks in duration
a Treatment is well tolerated
a Posttreatment follow-up is essential to check for cure (SVR12)
a Reinfection can occur and is treatable
a HCV antibody will remain positive indefinitely. HCV RNA must be tested to assess for reinfection



• Adults and adolescents, aged ≥12 years, with chronic HBV (including pregnant women) with:
– Evidence of significant fibrosis, ≥F2 OR
– Cirrhosis (compensated or decompensated)
OR
– HBV DNA >2000 IU/mL and an ALT >ULN OR
– Presence of coinfections; or family history of HCC or cirrhosis; or immune suppression; or comorbidities; or extrahepatic manifestations
– Persistently abnormal ALT levels
ULN, upper limit of normal.
WHO. Guidelines for the prevention, diagnosis, care and treatment for people with chronic hepatitis B infection. Geneva: World Health Organization; 2024. https://iris.who.int/server/api/core/bitstreams/34470cc8 -af90-4d7b-a949-ef27e5d0726f/content.

• Reduce hepatic inflammation and viral load
– Viral suppression; high viral load is associated with cirrhosis and HCC
– Normalize liver enzymes
• Prevent clinical complications, including cirrhosis, HCC, and liver-related mortality
• Prevent transmission of infection
• Lifelong sustained virologic suppression and regression of fibrosis
– Attain functional cure
Hepatitis B Online. https://www.hepatitisb.uw.edu/go/hbv/initial -treatment/core-concept/all.

• Preferred first-line regimens:
– Tenofovir disoproxil fumarate (TDF; Viread)
• Tablet taken daily, for life
– Entecavir (ETV; Baraclude)
• Tablet or oral solution taken daily, for life
• Alternative regimens:
– TDF + lamivudine (3TC)
– TDF + emtricitabine (FTC)

• The following are recommended to be monitored at least annually:
– Noninvasive tests to assess stage of disease and progression of fibrosis or cirrhosis
– ALT levels (and AST for APRI), HBV DNA levels (if available), HBsAg, and HBeAg/anti-HBe
– Treatment adherence should be monitored regularly, at each visit

aMore-frequent on-treatment monitoring (every 3-6 months for the first year) may be performed for people with more-advanced disease; during the first year of treatment to assess treatment response and adherence, if treatment adherence is a concern; with HIV coinfection; and for people with renal impairment. WHO. Guidelines for the prevention, diagnosis, care and treatment for people with chronic hepatitis B infection. Geneva: World Health Organization; 2024. https://iris.who.int/server/api/core/bitstreams/34470cc8 -af90-4d7b-a949-ef27e5d0726f/content.
• Cirrhosis or liver mass
• Platelets <100×109/L
• Coinfection (HCV, HDV, and/or HIV)
• Pregnancy
• Renal dysfunction/disease
• Lack of response to HBV treatment

Dieterich D, et al. Gastro Hep Advances. 2023;2(2):209-218.
a HBV is treatable, with the goal of viral suppression
a Treatment is effective in PWUD
a Treatment can be as simple as 1 tablet daily; it is typically of long duration but may vary case to case
a Treatment is well tolerated
a HCC screening may be necessary, performed every 6 months
a Vaccination can protect against infection and offers lifelong immunity; the entire vaccine series must be completed

Dieterich D, et al. Gastro Hep Advances. 2023;2(2):209-218.

TasP in HBV3
– Reduces perinatal transmission
– Reduces transmission from those with chronic HBV
– A complementary strategy for achieving HIV/HCV eradication goals • While vaccination against HBV is a key strategy for preventing infection and transmission, it is underutilized in high-risk populations U=U,



The Number of People Living With HCV Who Initiated Treatment Declined in the US, 2015-20201
disruptions to
and
in
initiation underscores
• Competing priorities
• Unstable housing
• Lack of transportation
• Limited knowledge of viral hepatitis
• Stigma around infection
• Prior negative experiences in health care settings
• Comorbidities
• Perceived lack of value in treating some patients
• Concerns regarding adherence
• Concerns regarding contraindications
• Competing priorities
• Limited time

System
• Insurance access
• Limited number of treatment providers
• Payer restrictions for treatment approval
• Payer requirements prior to treatment approval

“Everyone with hepatitis C should have access to lifesaving treatment, regardless of race, ethnicity, age or insurance status.” —Debra Houry, MD, MPH, CDC Chief Medical Officer
Adapted from slide provided by Jennifer Price, MD, PhD.


• SUD service centers can play a key role in the expansion of viral hepatitis prevention services, testing, vaccination, and linkage to care1
• Collaboration between SUD service providers and treatment providers is critical to success1
• Systems in which the treatment provider notifies SUD service centers regarding patient engagement, treatment initiation, and treatment completion are needed1
• Feedback from the treatment provider is essential for coordination of patients’ harm reduction services, DAA-adherence support, and postcure monitoring reminders1
• Syringe exchange programs associated with 20% reduction in HCV transmission1,2
• Directly observed treatment associated with 75% adherence rates and 98% SVR12 rates in HCV3,a

Unsafe injection practices account for 32% of HBV infections globally4



Harm reduction programs create trusted access points to engage populations that are often marginalized and at high risk for infection.
aParticipants received oral doses, observed by nursing staff, at the same time they received methadone or buprenorphine.
1. Degenhardt L, et al. Lancet Glob Health. 20175(12):e1192-e1207; 2. Hickman M, et al. Oral presentation at: 7th International Symposium on Hepatitis Care in Substance Users; September 19-21, 2018; Cascais, Portugal; 3. Litwin AH, et al. Oral presentation at: 7th International Symposium on Hepatitis Care in Substance Users; September 19 -21, 2018; Cascais, Portugal; 4. Voice of America. https://www.voanews.com/a/who-says-unsafe-injections-major-hepatitis-death-cause/2874867.html.
Strategies: scale up treatment, optimize harm reduction, provide access, engage at individual and community levels1
1. Rapid scale-up of HCV treatment
– Slow scale-up will create HCV-susceptible PWID without reduction in viremic pool
2. Harm reduction optimization
– Access to SSPs, MOUD
3. Access to HCV retreatment
– Facilitate access without stigma or discrimination
4. Individual level strategies
– Treat HCV in partners of infected individuals
5. Community engagement and partnership
Realities: There will be cases of HCV reinfection following successful treatment. The rate among people with recent IDU is 6.2 per 1002

– Utilize peer navigators and advocates to counsel and educate individuals
Reinfection is not itself a reason to withhold therapy from people with ongoing
• Who should be vaccinated?1
– Everyone, from infants to people aged 59 years, who have not been vaccinated
– Adults aged ≥60 years at risk for HBV
– People with risk factors, irrespective of age
• How does it work?1
– A series of 2 or 3 doses depending on age, the vaccine, and concomitant medical conditions
– Boosters are often not necessary ACIP, Advisory Committee on Immunization Practices. 1. CDC. https://www.cdc.gov/hepatitis-b/hcp/vaccine-administration/index.html; 2.

Must be Anti-HBs negative
HBV vaccination has been recommended for PWID by the ACIP since 1982 but vaccination among this population remains low.2
Strategies such as rapid regimens, offering incentives, and providing vaccination through accessible settings, including SSPs, are needed to improve uptake and series completion.

• Promote viral hepatitis screening and vaccination
• Advise patients that HCV can be cured and that treatment for HBV is effective in suppressing the viral load
• Know who the treaters are in your community and develop seamless, low-barrier referral and vaccination methods
• Apply harm reduction principles that support patients’ linkage to treatment and prevention
• Continue behavioral risk-reduction counseling following treatment