



Sarah Sungurlu, DO Assistant Professor of Medicine Division of Pulmonary and Critical Care Medicine





Sarah Sungurlu, DO Assistant Professor of Medicine Division of Pulmonary and Critical Care Medicine
• Characterize disease phenotypes, exacerbation risks, and treatable traits
• Discuss recent clinical trial evidence and guideline updates
• Tailor maintenance regimens for patients with chronic obstructive pulmonary disease (COPD) to reflect disease severity, minimize exacerbation risks, and account for comorbidities and patient preferences
• Learn how to educate patients with COPD


• Heterogeneous lung condition characterized by chronic respiratory symptoms (dyspnea, cough, sputum production, exacerbations)
– Due to abnormalities of the airways (bronchitis, bronchiolitis) and/or alveoli (emphysema) that cause persistent, often progressive airflow obstruction
• Focuses on patient characteristics and removes etiology to emphasize COPD factors beyond tobacco
• In low- and middle-income countries, nonsmoking COPD may be responsible to 60%-70% of cases
























B, billion; K, thousand; M, million. 1. Liu Y, wt al. MMWR Morb Mortal Wkly Rep. 2023;72:1250-1256; 2. National Center for Health Statistics. https://www.cdc.gov/nchs/fastats/copd.htm. Accessed January 14, 2025; 3. Press VG, et al. Ann Am Thorac Soc. 2019;16(2):161-170; 4. Shah CH, et al. Appl Health Econ Health Policy. 2023;21(6):915-924; 5. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/cdi/indicatordefinitions/chronic-obstructive-pulmonarydisease.html#:~:text=In%202020%2C%20there%20were%20247%2C314,with%20COPD%20as%20any%20diagnosis.&text=In%20addition%2C%20COPD%20coexists%20with,that%20have%20high%20hospitalization%20rates.; 6. American Lung Association. https://www.lung.org/getmedia/6289ff19-cef1-4f47-8b70-fdba2764cac3/2023-COPD-State-Briefs-New-York.pdf. Accessed March 15, 2025; 7. NY State Department of Health. https://nyshc.health.ny.gov/web/nyapd/emergency-department-visits-in-new-York. Accessed March 17, 2025.














1. American Lung Association. https://www.lung.org/getmedia/6289ff19-cef1-4f47-8b70-fdba2764cac3/2023-COPD-State-Briefs-New-York.pdf. Accessed March 15, 2025; 2. Behavioral
Factor Surveillance System (BRFSS). https://www.health.ny.gov/statistics/brfss/reports/docs/2022-22_brfss_copd.pdf. Accessed March 15, 2025.
Participants residing in the most-disadvantaged neighborhoods had a:
• 56% higher rate of COPD exacerbation
• 98% higher rate of severe COPD exacerbation
• 1.6-point higher CAT score
• 3.1 points higher SGRQ • 24.6 meters less six-minute walk distance. . .
Compared with participants living in the least-disadvantaged neighborhoods.

In addition to SES, neighborhood disadvantage has a major impact on COPD outcomes.


2 to 3
AECOPD are experienced on average by patients each year1

1.34
HR of acute CV EVENTS within 30-days following 1st AECOPD1

1.79

HR of ALL-CAUSE MORTALITY within 30 days following 1st AECOPD1


ü Decreased lung function, physiologic deterioration, and increased airway/ systemic inflammation2 ü Large reductions in QoL, physical fitness, and increased morbidity2


ü Incremental increases in mortality risk following each AECOPD1 50% of AECOPD are NOT reported by

• Recognize patients with symptoms potentially indicative of COPD and assess for the disease
• Recommend appropriate treatment strategies based on disease severity and predominant symptoms
• Regularly reevaluate patients using validated assessment tools
• Adjust and escalate pharmacologic and nonpharmacologic treatment approaches in patients with uncontrolled symptoms and/or frequent exacerbations





• Definition of Emphysema: abnormal enlargement of airways distal to terminal bronchioles due to destruction of their walls without obvious fibrosis
• Definition of Chronic Bronchitis: chronic productive cough for at least 3 consecutive months in 2 consecutive years – Mucous gland enlargement and hyperplasia of goblet cells are hallmarks of chronic bronchitis Chronic Obstructive



Mitzner W. N Engl J Med. 2011;365(17):1637-1639; Braman S. Chest. 2015;129(1):104S–115S.


• Diagnosis cannot be made without proven fixed obstruction
• Can help with therapeutic options depending on severity of airflow obstruction
• Can help with differential diagnosis

2025 report. https://goldcopd.org/2025-gold-report/. Accessed January 14, 2025.




• Chest X-ray
– Hyperinflation
– Flattened diaphragm
– Increased retrosternal airspace
– Bullae
• Chest CT
– Emphysema
– Bullae
– Pulmonary vascular changes suggestive of pulmonary hypertension
– Utility for lung cancer screening, differential diagnoses, and LVR




Spirometrically confirmed diagnosis
Postbronchodilator
FEV1/FVC <0.70
Assessment of airflow obstruction
Assessment of symptoms/risk of exacerbations
≥2 moderate exacerbations or ≥1 leading to hospitalization

0 or 1 moderate exacerbation (not leading to hospitalization)

Please mark the box that applies to you (one box only)
mMRC Grade 0 I only get breathless with strenuous exercise
mMRC Grade 1 I get short of breath when hurrying on the level or walking up a slight hill q
mMRC Grade 2
I walk slower than people of the same age on the level because of breathlessness, or I have to stop for breath when walking on my own pace on the level
mMRC Grade 3 I stop for breath after walking about 100 meters or after a few minutes on the level
mMRC Grade 4 I am too breathless to leave the house or I am breathless when dressing or undressing


Because COPD impacts patients beyond dyspnea, comprehensive assessment is recommended.
Patient-Administered Self-Assessment Tool
I never cough I cough all the time
I have no phlegm (mucus) in my chest at all
My chest does not feel tight at all
When I walk up a hill or one flight of stairs, I am not breathless
I am not limited doing any activities at home
My chest is completely full of phlegm (mucus)
My chest feels very tight
When I walk up a hill or one flight of stairs, I am very breathless
I am very limited doing activities at home

I am confident leaving my home despite my lung condition

I am not at all confident leaving my home because of my lung condition
I sleep soundly I don’t sleep soundly because of my lung condition
I have lots of energy I have no energy at all


A total score of 10 or greater is indicative of COPD symptoms that are clinically significant (low



LABA + LAMAa (consider LABA+LAMA+ICSa if blood eos ≥300 cells/µL)
LABA + LAMAa A bronchodilator
mMRC 0-1; CAT <10
mMRC ≥2; CAT ≥10
ICS, inhaled corticosteroids; LABA, long-acting β-agonist; LAMA, long-acting muscarinic antagonists.
aSingle inhaler therapy may be more convenient and effective than multiple inhalers; single inhalers improve adherence to treatment. GOLD, 2025 report. https://goldcopd.org/2025-gold-report/. Accessed January 14, 2025.




• Previous exacerbations • Severe/very severe airflow limitation • Smoking/exposure to irritants • Older age • Chronic mucus secretion • Poor exercise capacity • Significant comorbidities Budde J, et al. Chronic Obstr Pulm Dis

Accessed


Exacerbation defined as:2 “an event characterized by increased dyspnea and/or cough and sputum that worsens in <14 days”

COPD patient with suspected AECOPD
Confirm AECOPD diagnosis and episode severity
Severity
Variable thresholds to determine severity
• Dyspnea VAS <5
• RR <24 breaths/min
Mild (default)
• HR <95 bpm
• Resting SaO2 ≥92% breathing ambient air (or patient’s usual oxygen prescription) AND change ≤3% (when known)
• CRP <10 mg/L (if obtained)
Consider differential diagnosis


• Heart failure
• Pneumonia
• Pulmonary embolism

• Dyspnea VAS ≥5
• RR ≥24 breaths/min
Moderate (meets at least 3 of 5)a

Severe
• HR ≥95 bpm
• Resting SaO2 <92% breathing ambient air (or patient’s usual oxygen prescription) AND/OR change >3% (when known)
• CRP ≥10 mg/L
aIf obtained, ABG may show hypoxemia (PaO2 ≤60 mm Hg) and/or hypercapnia (PaCO2 >45 mm Hg) but NO acidosis (pH <7.35)
• Dyspnea, RR, HR, SaO2 and CRP same as moderate
• ABG show new onset/worsening hypercapnia and acidosis (PaCO2 >45 mm Hg and pH <7.35)

Appropriate testing and treatment

Determine etiology: viral testing, sputum culture, other
ABG, arterial blood gas; CRP, C-reactive protein; HR, heart rate; PaCO2, partial pressure of carbon dioxide in arterial blood; RR, respiratory rate; SaO2, oxygen saturation of arterial blood; VAS, visual analog scale. GOLD, 2025 report. https://goldcopd.org/2025-gold-report/. Accessed January 14, 2025.
• REDUCE trial: shorter course of systemic steroids yields equal length to next exacerbation1
• Steroids shorten recovery time, reduce risk of treatment failure, and reduce risk of early relapse

• Preferred dosing of prednisone 40 mg for 5 days
– Oral prednisone is equally effective to intravenous administration if oral access is available and intact – Widely varying practices regarding the dose of systemic corticosteroids in ICU mechanically ventilated patients (low dose <240 mg/day)2 Leuppi JD, et al. JAMA. 2013;309(21):2223-2231 2. Kiser TH, et al. Am J Respir Crit Care Med. 2014;189(9):1052-64.

• Controversial, but some evidence of benefit with antibiotics in absence of pneumonia
– Most exacerbations are triggered by viral infection. Bacterial infection or environmental factors can also trigger
– To reduce overexposure to antibiotics, suggest use of antibiotics if increase in dyspnea, sputum volume, and sputum purulence
• Sputum purulence more specific
• Or require mechanical ventilation (invasive or noninvasive)
• Duration: 5 days
• Choice: should be based on local resistance pattern (macrolide, tetracycline, amoxicillin)
– If frequent exacerbations or require mechanical ventilation recommend sputum culture


• Inhaled bronchodilators:
– Increase dose and/or frequency of short-acting bronchodilator
– Combine SABA and short-acting anticholinergics as initial bronchodilator for acute exacerbation
– Use spacers or nebulizer when appropriate
• Oxygen therapy: use minimum flow rate to maintain SpO2 (or PaO2) at an acceptable level, as high FiO2 can result in worsening hypercapnia
• Noninvasive ventilation: first mode for acute respiratory failure to improve gas exchange, reduce work of breathing/need for intubation, decrease hospitalization duration, and improve survival


• Reassess oxygen needs
• PFTs are recommended at 8-12 weeks of discharge (baseline conditions) to establish diagnosis
– Can have significant improvement in FEV1 > 8 weeks after acute exacerbation
• Can consider acute spirometry in hospitalized patient or shortly after discharge to try to reduce overdiagnosis

GOLD, 2025 report. https://goldcopd.org/2025-gold-report/. Accessed January 14, 2025.


• Transitional care excellence team consult for all COPD and pneumonia discharges
• Discharge pathway includes:
– Education and supervision/correction of inhaler technique
– Medication optimization (inhalers, smoking cessation)
– Assessment and recommendations for comorbidity management
– Telephonic follow-up within 2 days of discharge
– Post discharge appointment within 14 days
– AND MORE!


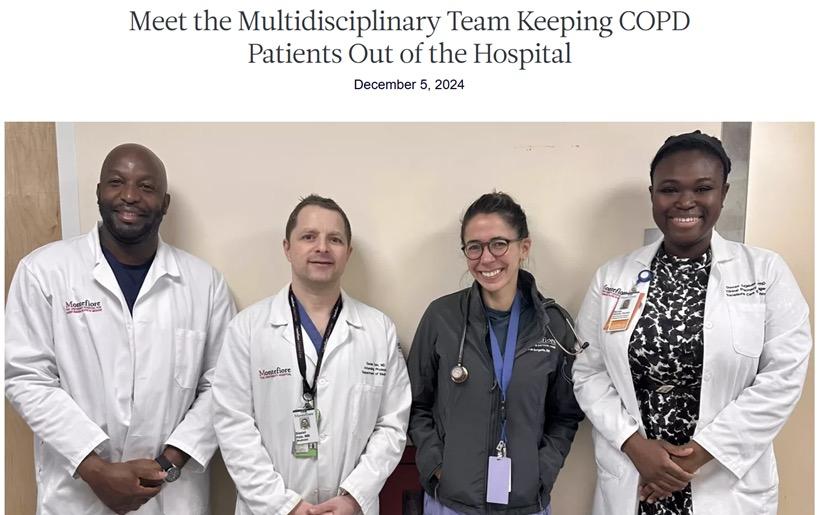
• Multidisciplinary team of pharmacists, nurse practitioners, and research associates that drives and supports continuity of care and collaboration across the health system
– Responsible for the delivery of patient-centered transitional care interventions
• Mission: safely transition patients from hospital to next point of care
• Vision: innovate hospital medicine through an acute and chronic care continuum model that holistically encompasses multimorbidity disease management and social determinants of health


… the 30-day readmission rate is 23%
… the 5-year rehospitalization risk is 44%
… the 5-year mortality rate is 55%
Admissions for COPD exacerbations have an estimated mortality rate of 10% 1. Shah T, et al. Chest. 2016;150(4):916-926; 2. Portillo EC, et al. Fed Pract. 2018;35(11):30-36; 3. GOLD, 2025 report. https://goldcopd.org/2025-gold-report/. Accessed January 14, 2025.
Mortality relates to patient age, presence of acidotic respiratory failure, the need for ventilatory support, and comorbidities.





Class Agent
Bronchodilators LABAs; LAMAs; LABA + LAMA
LABA + ICS
Corticosteroidcontaining regimens
Anti-inflammatory
LABA + LAMA + ICS
Roflumilast; dupilumab
Evidence
Single inhaler triple compared to dual LABD relative risk reduction: IMPACT HR 0.72 (95% CI: 0.53, 0.99); ETHOS HR 0.51 (95% Cl: 0.33, 0.80)

Anti-infectives Vaccines; long-term macrolides
Mucoregulators N-acetylcysteine; carbocysteine, erdosteine
Smoking cessation

Others
Pulmonary rehabilitation
Lung volume reduction
Vitamin D
Shielding measures
HR for usual care group compared to intervention group (smoking cessation)
HR 1.18 (95% Cl:1.02, 1.37)
Old trials: RR 0.28 (95% Cl: 0.10, 0.84)
New trials: RR 0.68 (95% Cl: 0.28, 1.67)



Relationship between blood eosinophil counts and effects of ICS on exacerbation prevention in COPD patients
Low Likelihood of Benefit
High Likelihood of Benefit




1 Fluticasone furoate/ umeclidinium/ vilanterol (FF/UMEC/VI)

2,3 Budesonide/ glycopyrrolate/ formoterol fumarate (BGF)
100/62.5/25 µg
0.91/year vs FF/VI, 1.07/year (RR, 0.85) & UMEC/VI, 1.21/year (RR 0.75) FF/UMEC/VI HR 0.72 vs UMEC/VI FF/UMEC/VI HR 0.89 vs FF/VI
320/18/9.6 µg
1.08/year vs GF, 1.42/year (RR, 0.76) & BF, 1.24/year (RR 0.87)
HR 0.72 vs BF
BID, twice daily; QD, once daily; DPI, dry powder inhaler; HR, hazard ratio; pMDI, pressurized MDI; RR, rate ratio. aSymptomatic patients (CAT ≥10) with a history of frequent (≥2 moderate AECOPD) and/or severe AECOPD (≥1 requiring hospitalization).
1. Lipson DA, et al. Am J Respir Crit Care Med. 2020;201(12):1508-1516; 2. Rabe KF, et al. N Engl J Med. 2020;383(1):35-48; 3. Martinez FJ, et al. Am J Respir Crit Care Med. 2021;203(5):553–564.

FAVORS USE

• History of hospitalization(s) for AECOPDa
• ≥2 moderate AECOPD per yeara
• Blood eos ≥300 cells/µL
• History of, or concomitant, asthma
FAVORS USE



• 1 moderate AECOPD per yeara



AGAINST USE
• Blood eos 100 to <300 cells/µL




• Repeated pneumonia events
• Blood eos <100 cells/µL
• History of mycobacterial infection


(Note the scenario is different when considering ICS withdrawal).
aDespite appropriate long-acting bronchodilator maintenance therapy. Blood eosinophils should be seen as a continuum, quoted values represent approximate cut-points; eosinophil counts are likely to fluctuate. GOLD, 2025 report. https://goldcopd.org/2025-gold-report/. Accessed January 14,, 2025.
• No current exacerbations




• Previous positive treatment responsea Consider changing to LABA + LAMA

Continue treatment





aPatient previously had exacerbations and responded to LABA + ICS treatment. GOLD, 2025 report. https://goldcopd.org/2025-gold-report/. Accessed January 14, 2025. No relevant exacerbation history Current exacerbations



• Review proper use of (compliance to) prescription medicine, eg, correct inhalation maneuvers
• Adherence issues, eg cost, adverse events

• Symptoms
• Dyspnea
• Exacerbations



• Current symptoms and exacerbation history
• Clinical tools
– Spirometry, blood eosinophils, 6-min walking distance, SGRQ, mMRC, and CAT

SGRQ, St. George's Respiratory Questionnaire. GOLD, 2025 report. https://goldcopd.org/2025-gold-report/. Accessed January 14, 2025.

• Escalate


• Switch inhaler device or molecules
• De-escalate Adjust



• Inhaler technique and adherence
• Nonpharmacological approaches (including pulmonary rehabilitation and self-management education)









gold-report/. Accessed January 14, 2025.
• IL-4Rα biologic; 300 mg SQ, Q2W (single-dose prefilled syringe or pen) • BOREAS P3 study
– N=939 patients with a blood eos ≥300 cell/µL and an elevated exacerbation risk despite use of triple therapy
– Significantly improved lung function and health status; decreased risk for AECOPD


LABA + LAMAa

• Consider switching inhaler device or molecules
• Implement or escalate nonpharmacologic treatment(s)
• Consider adding ensifentrine
• Investigate (and treat) other causes of dyspnea


aSingle inhaler therapy may be more convenient and effective than multiple inhalers; single inhalers improve adherence to treatment. Consider de-escalation of ICS if pneumonia or other considerable side effects. In case of blood eos ≥300 cells/µL, de-escalation is more likely to be associated with the development of exacerbations. Exacerbations refers to the number of exacerbations per year. GOLD, 2025 report. https://goldcopd.org/2025-gold-report/. Accessed January 14, 2025.
• Dual phosphodiesterase-3 and -4 (PDE3/4) inhibitor; 3 mg/2.5 mL inhalation suspension, Q12H
• ENHANCE 1 and ENHANCE 2 P3 studies
– N=760 and N=789 patients aged 40–80 years with moderate to severe symptomatic COPD
– Exclusion: patients with history of AECOPD in the last 3 months were excluded
– Not designed to assess impact on top of dual LABA/LAMA or triple ICS/LABA/LAMA; thus, difficult to position in algorithms
– Ensifentrine significantly improved lung function, dyspnea, and health status
Placebo Ensifentrine





• Dual phosphodiesterase-3 and -4 (PDE3/4) inhibitor; 3 mg/2.5 mL inhalation suspension, Q12H
• ENHANCE 1 and ENHANCE 2 P3 studies
– N=760 and N=789 patients aged 40–80 years with moderate to severe symptomatic COPD
– Exclusion: patients with history of AECOPD in the last 3 months were excluded
– Not designed to assess impact on top of dual LABA/LAMA or triple ICS/LABA/LAMA; thus, difficult to position in algorithms
– Ensifentrine significantly improved lung function, dyspnea, and health status















Up to 60% of patients with COPD are noncompliant to the prescribed regimen; only 1 out of 10 patients with an MDI performs all essential steps correctly.
• How deeply can patients inhale?
• How long can patients hold their breath?
• Do patients have the dexterity to use the device?







• What are the manual instructions for MDI? DPI? SMI? Nebulizer?
• How do you clean the device?
• How do you know when the device is empty?












• Smoking cessation
• Pulmonary rehabilitation
• Vaccines – Updated guidance in the 2025 GOLD Report
• Education and self-management (COPD action plan, physical activity)



Smoking cessation is the only evidence-based intervention proven to slow down the accelerated decline in lung function.
Budde J, et al. Chronic Obstr Pulm Dis. 2019;6(2):129-131; Ramsey SC, Hobbs FDR. Proc Am Thorac Soc. 2006;3(7):635-640; Mantero M, et al. Int J Chron Obstruct Pulmon Dis. 2017;12:2687-2693; GOLD, 2025 report. https://goldcopd.org/2025-gold-report/. Accessed January 14, 2025; van Eerd EAM, et al. NPJ Prim Care Respir Med. 2017;27(1):41.
• Benefits:
ü Improves dyspnea, fatigue, emotional function (symptoms of anxiety and depression), health status, and exercise tolerance in stable patients
ü Reduces hospitalization among patients who have had a recent exacerbation (≤4 weeks from prior hospitalization)
ü Evidence supporting reduced mortality
ü Cost-effective
LESS THAN 1% of patients receive PULMONARY REHAB following hospitalization

• Indicated in all patents with relevant symptoms and/or at high risk for AECOPD
• Optimal benefits: 6-8–week programs
• Barriers: accessibility, availability, uptake
activity



1. GOLD, 2025 report. https://goldcopd.org/2025-gold-report/. Accessed January 14,2025; 2. Griffiths TL, et al. Lancet. 2000;355(9201):362-368; 3. McCarthy B, et al. Cochrane Database Syst Rev. 2015(2):CD003793; 4. Maddocks M, et al. Respirology. 2015;20(3):395-404; 5. University of Michigan. https://www.michiganmedicine.org/health-lab/less-1-copd-patients-receive-pulmonary-rehab-following-hospitalization/. Accessed January 14, 2025.
What are the referral criteria for PR from pulmonary providers?
• COPD
– Pulmonologist diagnosis of COPD
PLUS
– GOLD E disease or GOLD B disease with high preintervention likelihood of benefit from pulmonary rehabilitation
• Pre- or post-lung transplant
• Interstitial lung disease with high preintervention likelihood of benefit from PR
• Pulmonary hypertension with high preintervention likelihood of benefit from PR


• Encourage communication with health care professionals
• Increase/maintain physical activity
• Practice expiration exercises that facilitate sputum excretion and reduce exhaustion due to coughing

• Nutritional support and healthy diet
• Adequate sleep
• Written COPD action plan –includes avoiding triggers, monitoring symptoms, constant information



GOLD, 2025 report. https://goldcopd.org/2025-gold-report/. Accessed January 14, 2025; COPD Foundation. https://www.copdfoundation.org/Learn-More/Educational-MaterialsResources/Downloads.aspx#MyCOPDActionPlan. Accessed January 14, 2025.
















• Severity of symptoms
– Progressive dyspnea that significantly impacts daily activities
– Frequent or severe COPD exacerbations requiring hospitalization
– Persistent cough with significant sputum production
• Diagnostic uncertainty
– Suspected underlying conditions that may contribute to COPD symptoms, eg, pulmonary hypertension, bronchiectasis
• Pulmonary function tests (PFTs)
– Severely decreased FEV1/FVC ratio indicating significant airflow obstruction


• Medication management
– Inadequate symptom control despite maximal tolerated dose of standard treatment
– Need for complex medication regimens or combination therapies
• Patient factors
– Desire to participate in pulmonary rehabilitation
– Difficulty managing self-care related to COPD
– Significant psychological impact from COPD symptoms
Watson JS, et al. Br J Gen Pract. 2020;70(693):e274–e284.
• Detailed medical history – eg, smoking status and COPD exacerbations
• Current medications and dosages
• Recent pulmonary function test results
• Relevant clinical findings – eg, chest exam and oxygen saturation levels
• Specific concerns or questions regarding patient’s COPD management


Watson JS, et al. Br J Gen Pract. 2020;70(693):e274–e284.
• COPD is a common and chronic disease that can be managed effectively
• Key objectives of management are alleviation of symptoms and prevention of exacerbations, in both short-term and long-term treatment
• Exacerbations significantly increase patient morbidity and risk of death
• Pharmacologic and nonpharmacologic management strategies can reduce the risk of exacerbations and mortality
• Evidence-based guidelines for COPD management are also available and regularly updated by the GOLD committee
• Simple and reliable questionnaires (eg, CAT, mMRC) should be routinely used to assess symptoms, risk of exacerbations, and patient health status
• Maintenance therapy should be matched to individual patient needs
• Supportive clinician and patient resources are available




Bookmark this page and be on the lookout for new downloadable posters, patient flyers and more! https://ExchangeCME.com/COPDBridgeResources








