






































It’s a sad irony that, when it comes to long-term care, there’s so much short-term thinking by employers and the government.
creating unsafe conditions for residents and the people who
long-term care homes during the pandemic should have been a
It’s time for urgency. Ontario’s population is aging in numbers we’ve never seen, with huge implications for our health-care system. If investments aren’t made in long-term care - and especially in the people who provide the care - we’ll feel the disruption in our hospitals, our communities, and our homes.













Cancer remains the leading cause of death in Canada. An estimated two in five Canadians will be diagnosed with cancer in their lifetime and about one in four will die from cancer. In 2023, the most recent statistics we have, it was expected that 239,100 Canadians will be diagnosed with cancer and 86,700 will die from the disease.
This is why it was so surprising that a February World Health Organization (WHO) report on cancer went largely unnoticed and unremarked upon. The report predicts a staggering global increase in cancer cases of 77 per cent by 2050.
What’s Canada doing to prepare? Not enough – and certainly nothing with a long-term focus. It’s time our governments crafted a concrete and sustainable cancer preparedness plan.
In addition to the recent WHO report, there are specific cancer predictions for Canada in a 2023 issue of the journal, Preventive Medicine. The authors estimate an increase in new cancer cases of 40 per cent from 2020 to 2040, and by 45 per cent in some of the mostly commonly diagnosed cancers: breast (27 per cent), colorectal (45 per cent), lung (45 per cent) and prostate (34 per cent). These are due to demographic factors including aging of the population, greater longevity, better detection, immigration and the true increased risk of certain cancers.
The authors also project the number of cancer deaths will increase by 44 per cent from 2020 to 2040. The journal article concludes that these estimates highlight the importance of planning for increasing investment and
JUNE 2024 ISSUE
EDITORIAL: May 10
ADVERTISING:
Display – May 24 | Material – May 28
Monthly Focus:
Precision Medicine/Volunteers and Fundraising/ Pharmacy and Medication Management: Developments in the field of personalized medicine. Innovative approaches to fundraising and the role of volunteers in healthcare. An examination of safe and effective use of medications in hospitals including medication management.
Annual Pharmacist Supplement & Special Focus Hospital Management
capacity in cancer control in Canada. This is clearly an understatement.
Canada is facing a cancer cataclysm with strategies, tactics and policies that are inadequate to control the present cancer crisis, let alone these dire predictions.
Future estimates can easily sound just like numbers and more numbers. But, no! Each number is a family member, friend, coworker, neighbour, person in stores where we shop -- and on and on goes this tragic list. It would be difficult to find anyone in the country who has not known someone in their life who has been impacted by cancer, Canada’s biggest killer.
We must have a long-term preparedness plan. Though we already have not prepared for the predictably increased numbers we face today, we have time to prepare for the upcoming wave; we must not squander it.
To date, both the federal government and our provincial/territorial governments lack a robust and comprehensive cancer control strategy.
So, what do we have?
The federal 2019 Canadian Strategy for Cancer Control is a 10-year action plan which aspires to achieve equitable access to quality cancer care in Canada, and promises to ensure a sustainable system for the future. It has eight priorities, all laudable, and a budget to help meet them – but it’s set to expire in a few years time.
Most of our provinces have cancer programs with similar goals and aspirations. But generally, the plans include tactics to control cancer in specific ways, for specific disease areas, in the short term.
Continued on page 6
EDITORIAL: June 7
ADVERTISING:
Display – June 21 | Material – June 25
Monthly Focus:
Cardiovascular Care/Respirology/Diabetes/ Complementar y Health: Developments in the prevention and treatment of vascular disease, including cardiac surgery, diagnostic and interventional procedures. Advances in treatment for various respiratory disorders, including asthma and allergies. Prevention, treatment and long-term management of diabetes and other endocrine disorders. Examination of complementary treatment approaches to various illnesses.
Patient Rooms Focus
THANKS TO OUR ADVERTISERS Hospital News is provided at no cost in hospitals. When you visit our advertisers, please mention you saw their ads in Hospital News.
610 Applewood Crescent, Suite 103 Vaughan Ontario L4K 0E3 TEL. 905.532.2600|FAX 1.888.546.6189 www.hospitalnews.com
Editor Kristie Jones editor@hospitalnews.com
Advertising Representatives
Denise Hodgson denise@hospitalnews.com
Publisher
Stefan Dreesen stefan@hospitalnews.com
Accounting Inquiries
accountingteam@mediaclassified.ca
Circulation Inquiries info@hospitalnews.com
Director of Print Media
Lauren Reid-Sachs
Helen Reilly, Publicist Health-Care Communications
Bobbi Greenberg, Health care communications
Sarah Quadri Magnotta, Health care communications
Dr. Cory Ross, B.A., MS.C., DC, CSM (OXON), MBA, CHE Vice President, Academic George Brown College, Toronto, ON
ASSOCIATE PARTNERS:
Hospital News is published for hospital health-care professionals, patients, visitors and students. It is available free of charge from distribution racks in hospitals in Ontario. Bulk subscriptions are available for hospitals outside Ontario. The statements, opinions and viewpoints made or expressed by the writers do not necessarily represent the opinions and views of Hospital News, or the publishers.
Hospital News and Members of the Advisory Board assume no responsibility or liability for claims, statements, opinions or views, written or reported by its contributing writers, including product or service information that is advertised.
Changes of address, notices, subscriptions orders and undeliverable address notifications. Subscription rate in Canada for single copies is $29.40 per year. Send enquiries to: subscriptions@ hospitalnews.com
Canadian Publications mail sales product agreement number 42578518.

Chronic back pain affects nearly eight million Canadians and is a condition that can become quite debilitating. For Dave Myen, a clinical neuroscience patient at London Health Sciences Centre (LHSC), chronic back pain led to sciatica in his right leg, and extreme pain in his lower back.
“It was very debilitating, to the point that the shooting pain in my right leg caused me to stumble and fall,” explains Myen. “It was difficult to live with and started to negatively affect my day-to-day life.”
After many visits with his family doctor, chiropractors, and massage therapists, Myen turned to LHSC and became the first patient in Canada to receive a robotic assisted surgery on his spine, called a direct lateral spine surgery, using the MazorX Spinal Robot.
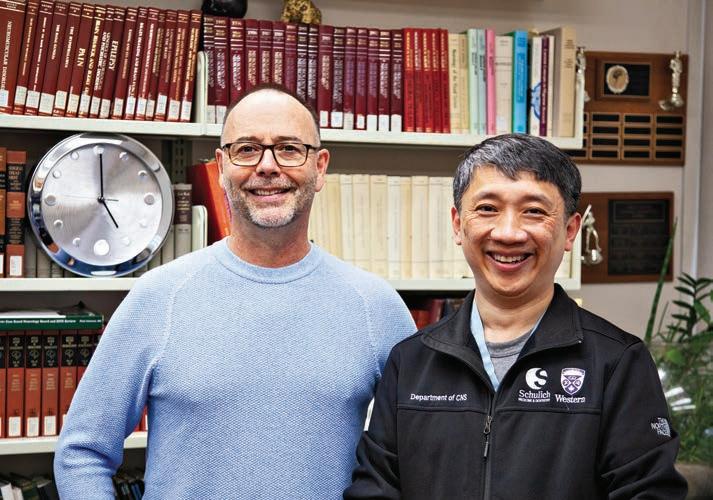
“Usually, we would do this surgery from the back, which means the patient would lie on their stomach,” says Dr. Victor Yang, Physician, Inpatient Clinical Neurosciences at LHSC. Because Myen needed surgery in two spots on his spine, the surgical team was able to use this new robotic technology to perform a minimally invasive surgery from the side, called a direct lateral spinal surgery
“Performing a surgery from this position can be quite challenging, but with the robot, it allows us to virtually see where the bone is within the patient’s body, and then the robot maintains the trajectory we need and guides us towards the right direction,” explains Dr. Yang. “This meant we were able to perform two minimally invasive surgeries at once without having to also reposition the patient.”
Eliminating a second surgery also led to decreased surgical time and a faster recovery, meaning Myen was able to go home in just a number of days.
“When I woke up from the surgery, the sciatica pain in my leg was immediately gone. It was amazing,” recalls Myen. “The surgery definitely did its job.”
The Clinical Neurosciences team, which includes members from vascular surgery and neuroanesthesia, at LHSC has successfully performed six minimally invasive surgical spinal procedures using this state-of-the-art technology.
“I think the use of robotic assistance will become more common for this type of procedure as it provides more consistency and, in general, better outcomes and care.” says Dr. Yang.
As for Myen, he admits it is an honour to be the first in Canada to receive this surgery, but what is even more exciting is what this means for his future.
“I am excited to get back to my everyday life and some of the things I enjoy and also have a summer that is not full of pain, but rather freedom to do the things I want.” ■ H
LHSC is grateful to our partnership with the Schulich School of Medicine & Dentistry at Western University, who funded the original cost of the robot for research purposes prior to generously transferring the equipment to LHSC for clinical use.

“I THINK THE USE OF ROBOTIC ASSISTANCE WILL BECOME MORE COMMON FOR THIS TYPE OF PROCEDURE AS IT PROVIDES MORE CONSISTENCY AND, IN GENERAL, BETTER OUTCOMES AND CARE.”
Fraser Health and Burnaby Hospital Foundation are partnering on a new robotic-assisted surgical system for the Jim Pattison Surgery Centre at Burnaby Hospital.
The new $2.3 million Mako Robotic-Arm Assisted System – the first of its kind in Western Canada – allows surgical teams to perform hip and knee replacement surgery with greater precision and accuracy.
“The robotic-assisted system will improve our precision and safety in total joint replacement,” says Dr. Tim
Kostamo division head, Orthopedics, Burnaby Hospital. “I’m excited to see how it helps us decrease complications and revisions and continue our quest for great outcomes for our patients.”
The new system uses CT imaging to create a 3D image of the joint, allowing surgeons to make a customized plan based on their patient’s anatomy. A surgeon guides the robotic arm during surgery, adjusting as necessary, based on visual and audio cues from the arm’s software. At all times, the surgeon, not the robotic arm, is controlling the operation.
“Burnaby Hospital Foundation is excited to lead the charge by fully funding the addition of the Mako system,” says Steven McKoen, Board Chair, Burnaby Hospital Foundation. “Robotic-assisted surgery will be a game-changer for the way orthopedic surgeries are performed at Burnaby Hospital. We are grateful to our donors who give so generously to fund advancements in healthcare in our community.”
Medical teams are currently training with the new system and the first surgeries are expected in the coming weeks. ■ H
New research examining the characteristics of physicians with the largest share of patients unvaccinated against SARS-CoV-2 may help increase vaccination rates going forward. The study, published in CMAJ (Canadian Medical Association Journal), found that family physicians in Ontario with the largest percentage of unvaccinated patients generally served patients living in marginalized neighbourhoods and had less support in their practices.
Researchers analyzed linked data on 9060 family physicians with more than 10 million enrolled patients and calculated the percentage of patients unvaccinated against SARS-CoV-2 per physician. They compared family physicians (n = 906) caring for the largest proportion of unvaccinated
Continued from page 4
patients (top 10 per cent) with the rest of the comprehensive-care family physicians in Ontario. They found the group with the largest proportion of unvaccinated patients were more likely to be male, to have trained outside Canada, to be older (mean age of 56 v. 49 years), and to work in a fee-for-service model than the remaining 90 per cent of physicians.
“The family physicians with the most unvaccinated patients were also more likely to be solo practitioners and less likely to practise in team-based models, meaning they may have fewer support staff in their clinics,” says Dr. Jennifer Shuldiner, lead author and scientist, Women’s College Hospital, Toronto, Ontario. “This illustrates the ongoing inverse relationship between the need for care, and its accessibility and utilization. In other words, the
There are also limited bilateral health agreements between provinces/ territories and the federal government on cancer control. They also have specific and important short-term objectives.
These plans are not going to prepare us for a cataclysm – they are not even adequate for today’s cancer reality. They are not fit for purpose. None of these existing plans constitutes a country-wide, coordinated and sustainable long-term cancer preparedness strategy, which is what we need.
The cancer plan must be comprehensive, created in collaboration with all relevant stakeholders and experts. It must include increased investment and capacity in cancer control. And it must be heavily weighted toward prevention, early diagnosis and appropriate testing and treatments. Prevention is always sorely underfunded.
We need a realistic plan that recognizes discrete strategies for different cancers. In order to ensure early diagnosis, we also need direct, effective pathways from a first doctor’s visit to diagnosis. Governments must pay for proven tests and treatments, thereby saving significant amounts in other parts of the healthcare budget through prevention and early diagnoses.
By investing wisely and equitably, cancer cases and deaths could be prevented.
What it must not be is a political exercise, considering short term “wins” for political gain. It must be a properly resourced and coordinated multisectoral, multidisciplinary approach based on relevant data.
The WHO has sounded the alarm with plenty of time for us to prepare. If we do nothing different than present tactics, the Cassandra-like warnings of WHO will surely come true. ■ H
Dr. Sandeep Sehdev is an oncologist at The Ottawa Hospital. The views here are his personal views and not those of the University of Ottawa or The Ottawa Hospital. Louise Binder is the health policy consultant for the Save Your Skin Foundation.
practices with the highest need receive the fewest resources.”
As many of the physicians with the largest percentage of unvaccinated patients served people living in marginalized neighbourhoods, awareness of cultural differences in perspectives on vaccination should be considered.
“Many marginalized communities have a history of neglect from government (municipal, provincial, federal) and health care, and this may lead to mistrust in public health initiatives,” the study authors write. “Interventions to support these communities should include meaningful community engagement and consideration for age, language-, and culturally appropriate communication tools to assist primary care in boosting vaccine uptake.”
Although the majority of SARSCoV-2 vaccines were not administered by family physicians, clinicians
have an important role to play in educating patients about the benefits of vaccination.
“We know that relationships with trusted family physicians can positively influence patients’ decisions,” explains Dr. Noah Ivers, senior author and clinician scientist, Women’s College Hospital. “Our study highlights the need to create equitable systems and processes that create opportunities for primary care teams to play a crucial role in influencing both general and SARS-CoV-2-specific vaccine-related decision-making.”
Expanding primary care teams in marginalized neighbourhoods and using hotspot strategies to focus public health resources in under-vaccinated communities could help support public health initiatives like vaccination.
SARS-CoV-2: a cross-sectionalcohort study” was published April 8, 2024. ■ H
COVID-19 vaccination as effective for adults with common mental disorders as for those without
Alarge multi-state electronic health record-based study from the Centers for Disease Control and Prevention’s (CDC’s) VISION Network has found that COVID-19 vaccines are as effective for adults with anxiety or depression or mood disorders as for individuals without these common diagnoses. This is one of the first studies to evaluate COVID-19 mRNA vaccine effectiveness for those living with mental illness.
While vaccination provided similar protection regardless of psychiatric diagnosis (none, one or multiple conditions), in contrast, unvaccinated adults with any of these conditions had a higher rate of hospitalization for COVID-19 – a marker for severe disease – than did those without a psychiatric diagnosis.
Both these findings held true whether two, three or four vaccinations were received and for ages 18-49, 50-64 and 65 and older.
“Although mental health conditions can tax the immune system, putting stress on the body, we saw similar COVID-19 vaccine effectiveness in people with psychiatric diagnoses compared with those without. That’s encouraging,” said study co-author Shaun Grannis, M.D., M.S., Regenstrief Institute vice president for data and analytics.
“But we also found that the risk of COVID-19 associated hospitalization is higher among unvaccinated patients with a psychiatric diagnosis,” added Dr. Grannis. “For patients with a diagnosis of depression, anxiety, or mood disorders who are wondering if the COVID vaccine would be valuable, this paper gives us evidence that the vaccine maintains its effectiveness even in the face of mental illness. So, I would encourage vaccination because it reduces the risk of hospitalization significantly.” ■ H
Premature deaths related to opioids doubled between 2019 and 2021 across Canada, with more than 1 in 4 deaths among young adults aged 20-39 years attributable to opioids, according to new research published in CMAJ (Canadian Medical Association Journal).
Opioid-related deaths have continued to increase over the past decade across Canada, with 6222 deaths occurring in 2021. This trend worsened during the COVID-19 pandemic, although the scale and rapidity of increases varied across provinces and territories. These changes have been attributed primarily to the unregulated drug supply, which became increasingly volatile and unpredictable during the pandemic.
“During the COVID-19 pandemic, the loss of life from opioid toxicities has worsened in nearly every part of Canada, with Alberta, Saskatchewan, and Manitoba experiencing enormous increases in deaths – particularly among their younger population,” says Dr. Tara Gomes, senior author on the study, and scientist at Unity Health Toronto. “Without adequate investments in widespread, accessible treatment and harm-reduction programs, and broader social supports like housing, these preventable deaths are having devastating effects on communities across the country.”
To understand the trends and impact of opioid-related deaths, researchers looked at data on accidental deaths from opioid toxicity across 9 provinces and territories in Canada: British Columbia, Alberta, Saskatchewan, Manitoba, Ontario, Quebec, New Brunswick, Nova Scotia, and the Northwest Territories. In just 3 years (2019–2021) the annual number of opioid-related deaths rose from 3007 to 6222. More striking is the number of years of life lost (YLL) to premature death from opioid toxicity, which more than doubled in Canada over the study period, reaching over a quarter of a million in 2021 (256 336 YLL).
“Alarmingly, 1 in 31 deaths among people aged 85 and younger were at-
tributed to opioids in 2021, a number that increases to 1 in 4 deaths among young adults aged 20–39,” said Shaleesa Ledlie, Leslie Dan Faculty of Pharmacy, University of Toronto. “This scale of opioid-related harm – particularly among young people – is unprecedented and illustrates the magnitude of this public health crisis across the country.”
Although the concentration of harm in younger populations was consistent across the nine Canadian provinces and territories included in this study, some provinces were disproportionately affected. For example, in Alberta, nearly half of all deaths among those aged 20-39 were opioid-related.
In Canada, access to social supports and health care services was severely reduced or restricted during the pandemic, resulting in changes in patterns of drug use and accessibility of community-based services for people who use drugs. However, despite the reopening of services in recent years, the rates of opioid-related deaths remain elevated across the country, identifying an urgent need to work with communities to scale up services designed to support people who use drugs.
“Opioid-related deaths between 2019 and 2021 across 9 Canadian provinces and territories” was published April 15, 2024. ■ H
First Nations patients in Alberta leave emergency departments (EDs) without completing treatment more often than comparable non–First Nations patients, due in part to anti-Indigenous racism expressed by providers, found new research published in CMAJ (Canadian Medical Association Journal).
Higher proportions of incomplete ED care for First Nations patients compared with non–First Nations patients occurred even in cases of serious diagnosis, and were found across all parts of Alberta. Provincially, 6.8% of First Nations visits end without completing care, compared with 3.7% of non–First Nations visits.
Results from sharing circles with First Nations patients, and interviews with health care providers, show that racism and stereotyping are a reason First Nations patients leave care, which members from Alberta’s White majority do not face. The study also identified that patient–provider communication issues, transportation barriers, long wait times, and perceptions of being
made to wait longer than others were additional reasons why First Nations patients leave EDs.
Leaving without completing care matters because it delays needed treatment and interrupts care journeys. About 1 in 20 patients in the study required hospitalization within 72 hours of leaving. We do not know what proportion of patients may miss needed care entirely, because they do not return to the ED.
The work was conducted with the Alberta First Nations Information Governance Centre and involved 7 other First Nations organizations.
“There are multiple factors that influence the decision to leave the emergency department without being seen. Some of these include how First Nations [patients] are treated while waiting to be seen, such as minimizing and dismissing the urgency of presenting symptoms, feeling unsafe and the use of inappropriate language directed at them while in the emergency department,” explains Lea Bill, RN, executive director of the Alberta First Nations Information Governance Centre.
“Although leaving care seems like a purely personal decision, more First Nations patients are making that decision than non–First Nations patients. This shows that those personal decisions are actually driven by overarching social factors and health system inequities,” notes Patrick McLane, PhD, Department of Emergency Medicine, University of Alberta, Edmonton, Alberta.
Higher rates of First Nations patients leaving without completing care is of immediate concern as “crowding continues to worsen in emergency departments across Canada, and the proportion of patients leaving emergency department care has risen in several jurisdictions,” the authors write.
The authors hope that study findings will encourage EDs to work with local First Nations to find ways to reduce disproportionate premature departures from care.
“Leaving emergency departments without completing treatment among First Nations and non–First Nations patients in Alberta: a mixed-methods study” is published April 22, 2024. ■ H
Ayear-old pilot project at St. Paul’s Hospital to track unnecessary use of preventative blood thinners in hospital patients has seen a decline in use by 53 per cent.
The Anticoagulation Stewardship Program (ACSP) is the first in British Columbia and Canada to focus on these preventative blood thinners, known as heparin medications, with a view to reducing inappropriate use. By extension, the ACSP also aimed to decrease associated drug costs, negative health effects on patients, and nursing workloads.
Dr. Wan knew that data and research show that overprescribing has had negative effects on patients, health-care workers, and health-care budgets. The cost of heparin meds in 2022 at St. Paul’s Hospital alone was almost $280,000.
Preventative heparin medications needed a big rethink, he says, especially since the risk of a clot forming in most hospitalized medical patients is relatively small, occurring in just one per cent of low-risk patients. Meanwhile, a major risk of blood thinners is excess bleeding, in addition to the pain and discomfort from receiving the daily injection.
IN THE FIRST FEW MONTHS SINCE THE PILOT LAUNCHED IN JANUARY 2023, ABOUT 60 PER CENT OF THE TIME, DOCTORS ACCEPTED THE PHARMACIST’S RECOMMENDATIONS.
The pilot, a collaboration with thrombosis specialists and Providence Health pharmacy support services, has met and even exceeded its goals, says Dr. Tony Wan, who leads the ACSP with fellow thrombosis physician Dr. Taylor Drury and Dr. Stephanie Garland, Clinical Pharmacy Specialist in hematology and thrombosis at Providence.
Hospitalized patients have a higher risk of blood clots because they are less active than usual. So, the current practice is to prescribe most patients with injectable heparin medications to prevent against clots.
“Most people who get admitted to hospital receive heparin,” says Dr. Wan. “Surgery patients in particular do, but so do people coming in for a range of medical illness, from minor infections to diabetes to kidney diseases.”
Key to the program was identifying patients who were at low risk of developing clots. Pharmacist Dr. Garland was funded to work on the pilot for half of her time and used a tool, tested on a large group of patients, to determine risk. It factored in a person’s previous history of clots, cancer or paralysis of lower limbs, along with mobility levels and age. (Clotting risks increase in those over 60.)
Patients whose risk was calculated at one per cent or less were considered low. A higher-percentage risk was considered moderate to high.
The pilot started with patients in St. Paul’s Medicine, Urban Health and Acute Care for Elderly units, which, combined, have 165 beds.
Dr. Garland reviewed patient charts to calculate their risks, then advised their doctor accordingly. The doctor had discretion in heeding the recommendation or not.
“We are a consulting service, so we don’t change orders unless the most responsible physician is involved,” says Dr. Garland. “We leave notes in the chart. Physicians have the choice to agree or not.”
In the first few months since the pilot launched in January 2023, about 60 per cent of the time, doctors accepted the pharmacist’s recommendations. After six months, that number increased to about 80 per cent, reports Dr. Wan.
Chart screening to determine clot risk resulted in 11,000 fewer heparin injections used in the year.
Reduced heparin prescribing resulted in a yearly savings of $75,000 to the hospital, which exceeded the cost of half of a pharmacist’s salary.
A significant patient benefit was a reduction in a serious condition called heparin-induced thrombocytopenia (HIT). It is caused by an exposure to heparin and ironically, it causes clots instead of thinning the blood. The estimated risk of HIT is about 0.2 per cent from the use of enoxaparin, the mostused heparin medication in the hospital. HIT carries a 10-to-20 per cent mortality rate while many who survive are left with serious, permanent disabilities such as leg amputation.
More selective administering of heparin resulted in big time savings for nurses. They spend about 5.5 minutes per injection, according to the pilot’s data. That equates to about 20 extra minutes a day in their schedule that could be spent providing other types of patient care. The pilot resulted in 1388 nursing hours saved in the year.
With each nursing shift lasting 12 hours, that extra time could free up 115 more shifts, helping to ease nursing demand.
That wasn’t the only nursing benefit. Another was their improved safety. Dr. Wan explains that 90 per cent of nurses

Dr. Tony Wan leads the ACSP with fellow thrombosis physician Dr. Taylor Drury and Dr. Stephanie Garland, Clinical Pharmacy Specialist in hematology and thrombosis at Providence.
surveyed experienced verbal or physical violence when administering the sometimes-painful injection, which is usually given in the evening when patients might be tired and sleepy. “Many elderly patients may be confused or delirious at that time of day,” Dr. Wan adds.
With all these benefits, the pilot’s leaders would like to grow it to all in-patient units at St. Paul’s and at Mount Saint Joseph Hospital. That would require more pharmacist support, but the program is currently investigating the role that artificial intelligence (AI) could play in performing some of the screening tasks the pharmacist performs. This would allow for a larger number of patients to be screened with the same amount of pharmacist time.
Donors to St. Paul’s Foundation and The Department of Medicine (DOM) Innovation Platform provided support to the pilot. ■ H
Ann Gibbon works in communications at Providence Health Care, Vancouver.Food is more than just sustenance, it is a powerful tool for healing, a source of comfort and a method of connection. Despite its centrality to the patient experience, hospital food systems have historically taken a short-term view of food and been constrained by external pressures.
At the time of hospital admission, an alarming 45 per cent of people across Canada are at risk of malnutrition due to illness and injury. Malnutrition contributes to poor patient outcomes and extended hospital stays. Prioritizing providing appealing, nutrient-dense meals to patients not only accelerates their recovery but also reduces waste and makes financial sense for the whole health care system. It’s clear that we need a culinary revolution in our health care institutions.
Global industrialized food systems are responsible for one-third of all greenhouse gas (GHG) emissions. The impact of the current industrial food system extends to hospital food services and are at odds with the health care mandate to first “do no harm”. It also places immense environmental pressures on local land, water sources and biodiversity undermining the determinants of health for both present and future patients. Additionally, the resources used to grow, process, transport, package, prepare and deliver food to patients are all wasted if patients ultimately do not eat the food they are served.
Knowing all this, it’s important to find a way for hospital food to actually get into patients’ mouths and out of landfills. The Planetary Health Menu Project is re-imagining how hospitals can positively contribute to their patients’ well-being and the planet’s health, starting with what is served on hospital menus. This pioneering collaboration between Vancouver Coastal Health (VCH), the UBC Planetary Healthcare Lab, VGH & UBC Hospital Foundation and Boehringer


Ingelheim Canada, alongside Culinary Director Executive Chef Ned Bell and non-profit organizations Nourish and Greener by Default aims to make hospital food healthier and more appetizing for patients.
The project at Vancouver General Hospital initially developed more than 50 new and modified recipes that align with the latest evidence on healthy and sustainable diets. The new menu items prioritize fresh fruits and vegetables, whole grains, and plantbased proteins over animal proteins, dairy, and ultra-processed foods. The menus also integrate seasonal and local ingredients produced through environmentally-friendly farming practices with lower carbon footprints.
But this project isn’t just about creating more sustainable menu items. It’s also about crafting a more appetizing culinary experience for patients. The Planetary Health Menu Project ensures that hospital menus offer a diversity of flavourful meal
options, aiming to increase meal consumption and satisfaction among the patients at Vancouver General Hospital. To do this, 20 recipes were selected from those evaluated by patient partners, dieticians and food services staff, and served on a trial basis to patients during a six-month period. Feedback from patients was solicited through surveys and interviews and inferred from food waste measurements. This information allowed for further refinement of the individual dishes.
Preliminary results from the project have been promising, showing positive patient experiences suggesting acceptability of new menu items – including plant-based options – and reduced environmental impacts. The Planetary Health Menu Project is an integrated patient health and experience improvement strategy and climate mitigation initiative, with thought behind every ingredient. The aim is to
transform health care and cultivate a future where health, well-being and sustainability are synonymous in local Vancouver hospitals and beyond. Upon completion, VCH plans to use the project findings to expand the implementation of the Planetary Health Menu across the health authority and become a model for the future of hospital food.
Through this innovative approach to patient care and resource stewardship, we can create a health care system that serves its communities while adopting good environmental practices and championing a much-needed culinary revolution in hospitals. This is a crucial step in creating a health care system that is truly holistic, considering both the well-being of the patient and the world they inhabit. We believe this is the way forward for health care – a path that leads to healthier people, healthier communities, a healthier environment, and ultimately, a healthier future for us all. H




Like many parents, Diana Drake updates social media frequently with photos of her daughter, Ryan, who is almost one year old. From a trip to Disney World to her first steps, there’s lots to celebrate.
The photos are particularly poignant as, just a few years ago, Diana didn’t think a pregnancy was possible after an ATV accident. “I broke my back in two places and was paralyzed,” says Diana. “I was worried my lifelong dream to become a parent wasn’t possible.”
Last year, Diana did become pregnant, and received care from Sunnybrook’s Accessible Care Pregnancy Clinic. Now, experts from the clinic have partnered with the Provincial Council for Maternal and Child Health to create the ‘Disability and Pregnancy: Accessible Pregnancy Care Planning Toolkit’, aimed at helping healthcare professionals address the unique challenges faced by pregnant individuals with physical disabilities.
“At the heart of this resource is encouraging healthcare teams to think ahead and pre-plan to ensure the best possible outcomes and experience for patients,” explains Dr. Anne Berndl, Director of Sunnybrook’s Accessible Care Pregnancy Clinic. “Individual-
ized care is key, as each disability can impact a pregnancy differently.”
The audience for the resource, available on PCMCH’s website, is sweeping and includes primary care providers, obstetricians, midwives, nurses, occupational and physical therapists, social workers, physiatrists, neurologists, pain medicine specialists, anaesthetists, lactation consultants, dietitians and others involved in all stages of prenatal, labour and delivery and postpartum care.
A key focus is making sure there’s a coordinated team approach to prenatal, birthing and postpartum care. “Before a patient even visits Sunnybrook, we have a long phone call with them to learn about their disability, their fears and what would help them,” says Liz Jung, an advanced practice nurse with the clinic. “We also keep in mind practical considerations, like whether they will need more time to visit the washroom at the hospital.”
Once the initial call with a patient takes place, Dr. Berndl and Jung encourage practitioners to work with all of the multidisciplinary teams who will support the patient as early as possible.
Many people with disabilities can have healthy pregnancies; however, there is an increased risk of adverse outcomes for pregnant individuals and their babies, including preterm birth,
preeclampsia and Caesarian delivery. On top of this, there are significant barriers to accessing prenatal care for people with physical disabilities, including transportation complexities, lack of accessible care spaces and difficulties finding physicians comfortable providing obstetrical care.
“As healthcare practitioners, we can do a lot to take worry and anxiety away for patients by preparing early, coordinating the right care team and asking the right questions. This toolkit provides a framework for this model of care,” she adds.
Jung agrees, and acknowledges while some clinical settings may not have numerous resources, it comes back to the ‘small things’ like taking the time to have conversations with patients and embodying a person-centred approach for individualized care.
“People with disabilities are experts in their own lives and own care,” says Jung. “Whenever I meet with a new patient, I always ask, ‘I know your diagnosis, but I don’t know what that means to you. What would be helpful for you?’”
Diana can attest firsthand that the approach works well, and appreciated the longer intake appointment. She recalls Jung asking her about how she would be getting to appointments, her comfort moving in and out of her
wheelchair, what her daily routine was like and any worries or fears she had.
“The time spent chatting at the onset really set my mind at ease for what was to come,” says Diana. “She wanted to get to know me, what my day-to-day was like and the supports I have. I also appreciated the coordinated care – all of the team were talking to each other about my pregnancy and delivery. It meant a lot.”
The team behind the toolkit urge care teams to think outside of the box and be creative. Jung gives the example of a patient using a wheelchair, and notes sometimes you can perform a fetal ultrasound while the patient is still sitting in their wheelchair.
“Hearing ‘We will take care of you, we will build a plan with you, and we are happy for you’, is such a simple but powerful statement to patients,” adds Dr. Berndl.
Both Sunnybrook and PCMCH say the collaboration was positive and productive. “This resource aims to pave the way for improved care experiences for pregnant individuals concurrently living with physical disabilities. We hope that this toolkit will be widely embraced in all care settings, transforming the landscape of healthcare, and ensuring quality care for every individual in Ontario and beyond,” Alexandra Thorp, Senior Program Manager, PCMCH. ■ H
Marie Sanderson is a Communications Advisor at Sunnybrook Health Sciences Centre. Photo credit: Kevin Van Paassen, Sunnybrook Diana just before and after her delivery












As one of Canada’s largest acute care hospitals, Humber River Health (Humber) is dedicated to empowering its patients, while providing them with comprehensive, quality care closer to home. In the realm of healthcare, especially at the end of life (EOL), the setting in which one receives care can profoundly impact their experience. Traditional hospital environments often do not provide the support and comfort desired by those in their final days. Time that should be spent surrounded by family and loved ones in a familiar environment, is often disrupted in a busy and institutional hospital setting.
Humber services a densely populated area in Northwest Toronto, a region characterised by a significant elderly population, a high material deprivation index and a higher-than-average number of EOL hospitalizations. In this region, there are 610 deaths per 100,000 residents, where the majority of these deaths occur at Humber. Thus, the excessive strain caused by palliative patients on hospital resources becomes a significant bottleneck in enhancing efficiency. Limited hospice beds and community support have traditionally hindered the ability for many to die at home, despite their wishes, as only 36 per cent of Canadians receive palliative care at home.
Recognizing this critical gap, Humber has pioneered the integrated Hospice @ Home program, a transformational approach to palliative care that emphasizes comfort, dignity, and familial presence by providing a holistic approach to care, right in the patient’s home while addressing financial barriers and health equity concerns.
Hospice @ Home assists palliative care patients, most of whom are older adults, through the last year of their lives. With a specialized and dedicated interdisciplinary team, consisting


of registered nurses, personal support workers, social workers, spiritual care, and other complementary therapists and volunteers, and access to a 24/7 phone line, the goal is to support these patients and their families at home without compromising the quality and breadth of EOL services they are provided. This pilot program – which launched in January 2024 – goes beyond what is provided through home care services, by integrating hospice and community services that cares for the patient and their caregiver.
Humber is supporting patients who have life-limiting or life-threatening diagnoses, including those with primary palliative diagnosis of cancer or a chronic illness, such as chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), renal disease, and pulmonary fibrosis, among others.
Patients no longer have to endure long hospital stays and can spend their last weeks surrounded by loved ones. “No price can be attached to the act of allowing a loved one to pass away in the comfort of their own home,” says Kathleen Kirk, Manager of Schulich Family Medicine Teaching Unit and
Integrated Care Services at Humber. “Not only does this support their wishes, but from a Hospital perspective, it frees up additional hospital beds for acute care patients, alleviating some of the strain on the healthcare system.”
The Hospice @ Home initiative represents a collaboration between Humber, Dorothy Ley Hospice, Home and Community Care Support Services, and Etobicoke Services for Seniors (ESS) Community Support Services provider. To support the reduction of avoidable repeat ED visits, hospital readmissions, and hospital deaths related to palliative care, Humber’s partnership with Dorothy Ley Hospice provides the necessary care coordination, physicians, and psychosocial services required to keep patients in their homes, with their loved ones. They help oversee the program, identify and enroll patients, as well as support the patient transition from a hospital setting back into their homes with the assistance of ESS through a dedicated comfort fund. In addition, the program provides counselling and other psychoso-
cial services to patients and their families early in their palliative journey as an upstream approach to ensure time to plan for EOL in a supportive environment. With the support of Women in Kindness (WINK) and Humber, the program has secured the necessary funding to cover various expenses, from medical equipment and supplies, to comfort fund items such as transportation and meals, ensuring no patient is left without the care they deserve.
Since its launch, Hospice @ Home has made significant strides, supporting the transition of five patients back to their homes. These patients were discharged with an initial care plan, which provided guidance and support for the first few days at home. Once back in their homes, the dedicated teams from Dorothy Ley Hospice and Home and Community Care Support Services evaluated the patient’s and family’s needs, with a care plan that is fluid and changes with the needs of the person. The program’s flexibility allows for care plans that adapt to
changing needs, ensuring personalized and comprehensive support.
The effect of the Hospice @ Home program is multi-dimensional. For patients, it means receiving high-quality palliative care in the comfort and privacy of their own homes, surrounded by loved ones. For families, it provides support and relief during a challenging time, ensuring they are not alone in their caregiving roles. For the healthcare system, it represents a shift towards more integrated, sustainable and patient-centered care models.
The success of the Hospice @ Home pilot project marks the shift towards integrated care and a population health approach in palliative care within our region. With continued support from donors, community partners, and the dedicated team at Humber, the program is poised for scale and spread, bringing hope and comfort to more families. “Ultimately, we want to ensure that patients and their families feel supported and valued by their care providers,” says Beatrise Edelstein, Vice President of Post-Acute Care and Health System Partnerships at Humber. “Our hope is that their wishes are respected and their needs are met within a compassionate and caring way during a very challenging time.” By sharing the benefits of this program, Humber’s hope is to encourage scale and spread of this integrated model of palliative home care delivery across Ontario. In a society that often shies away from discussions of death and dying, Hospice @ Home demonstrates the importance of facing these realities with compassion, dignity, and respect. It challenges us to reimagine EOL care, not as a series of medical interventions, but as a holistic journey that honours the individual and their loved ones. Through programs like Hospice @ Home, Humber is not just transforming palliative care; it is lighting new ways in healthcare. ■ H
Shahana Gaur Senior is a Writer/ Communications Specialist at Humber River Hospital.


St. Michael’s Hospital patient Walter Tauro has officially been named the oldest kidney transplant recipient in the world by the Guinness World Records after receiving the kidney at age 87.
Tauro began his journey at St. Michael’s in July 2020 when he was assessed by the Kidney Transplant program team for a transplant as a last resort after 15 years of living with kidney disease.
With many tests to face, he was concerned his age could impact his chances at qualifying for surgery, but after several assessments and conversations with the care team – he was finally cleared for a kidney transplant.
“I was so relieved, I had felt tired for so long and was ready for my new beginning,” he said. “I knew it would be a long road, but I was ready for a second chance.”
St. Michael’s Kidney Transplant program is a specialized centre for people with severe kidney disease. Founded in 1969, the program is one of the largest in Canada. The team’s ability to tackle the most complex transplant surgeries and provide fol-
low-up care gives patients who have often been waiting for a new kidney for years a chance to live free from dialysis and renal disease.
“In our program, it is not the age of the patient that matters, it is their overall health,” said Meriam Jayoma-Austria, a registered nurse in the program. “Walter went through the program seamlessly, from his heart assessments to a bone marrow analysis.”
Jayoma-Austria was very involved in his journey from the day he arrived in the clinic. While Tauro knew he had a much higher risk of complications going into surgery, he felt ready to take the next step with his transplant team.
The surgery was a success, and Tauro has immense gratitude for his care at St. Michael’s, and for the deceased donor he received his kidney from.
“I felt reassured and supported by the team here, everyone communicated with me so well,” said Tauro. As someone who values family over everything else, he is looking forward to spending time with them as he embraces his new normal without dialysis.
And adventure awaits post-surgery for Tauro, who now has his sights set on a trip to Europe.
Dr. Ramesh Prasad, a St. Michael’s physician who worked closely on Walter’s case is in awe of his quick recovery and resilience.
“The program is constantly pushing for excellence, my hope is this is only the beginning of treating the aging population with such great results.”
As the health care system grapples with the impacts of an aging population, there is an opportunity to give older adults like Tauro a chance at a significantly improved lifestyle post-transplant.
Projections suggest the over-75 population will rise faster than past annual rates over the next few years.
A case like Tauro’s is a testament to the innovative and quality care Unity Health Toronto and health care networks across Ontario can continue to provide for the aging population.
What’s next for Tauro? It’s time to book flights, he says. Having not been able to travel far distances in over 15 years, it is the one of two things he is most looking forward to after his years on dialysis – the other is spending time with his family.
The sky is the limit when you have a second chance at life, and he says he plans to enjoy every second of it. ■ H
rowing up surrounded by pets, 13 year-old Anthaea-Grace Patricia Dennis originally wanted to be a veterinarian.
But, seeing first-hand how close family members were impacted by neurological illnesses such as Alzheimer’s disease and having benefited from the influence of her mother and grandmother – both scientists themselves –
new initiative brings day surgery closer to eastern Ontario families, supported by the expertise of medical teams at CHEO and regional hospitals, while also targeting the longstanding surgical wait-list.
Working through the Kids Come First health team, this new program sees surgeries like a tonsillectomy and umbilical hernia repair conducted at the Carleton Place & District Memorial Hospital and the Brockville General Hospital approximately four times per month.
Surgeries have begun at each hospital. The program aims to complete 300 surgeries by 2025, which brings much-needed surgical care closer to home for families. “Being able to perform surgeries locally helps in many ways. By leveraging the footprint of additional hospitals like Brockville and Carleton Place, we’re able to schedule more surgeries and finally address the long surgery wait-list,” said Dr. Jean-Philippe Vaccani, Chief of Surgery at CHEO.
The initiative, supported by a historic investment by the Ontario government to CHEO last summer, helped 13-year-old Tianna van de Kamp get surgery closer to her home in Morrisburg, Ont.
Tianna had osteochondroma – the most common noncancerous bone
sparked an interest that has led her toward a career in science and medicine.
“When you think of a 13 year-old, you typically think of a middle school student, not a university graduate, which I am,” says Anthaea-Grace.
“I want people to know that I may be 13, but I’m also a master’s student, I’m a researcher studying Parkinson’s disease, and…” she adds, smiling, “…maybe in a few years you’ll see me being your doctor.”
Anthaea-Grace has been breaking stereotypes all her life.
“My mom was teaching me to read from an early age, keeping me active, interested, helping me learn, and she noticed that I was picking up on material quicker than she would’ve expected,” recalls Anthaea-Grace.
That realization kicked off a journey which saw Anthaea-Grace fast-tracking her elementary and high school educa-

growth – on her lower leg. She needed surgery because the bone kept growing and the pain was getting worse.
The drive to CHEO usually takes about an hour and 20 minutes, according to her mom Tania van de Kamp. When CHEO called to offer Tianna surgery in Brockville, the family jumped at the opportunity.
The drive to Brockville was half the distance and Tianna got the surgery earlier than expected.
“Shortening the drive by half was huge for her. Like, just to get her home and then recover that much faster,” said Tania.
“The launch of this regional pediatric surgical program is another example of the innovation through partnerships happening across the health care system that is helping connect children and their families to the surgeries they need, in their community,” said Sylvia Jones, Deputy Premier and Minister of Health. “This program builds on our
tion through a combination of specialized individualized programs at U.S.based schools and home schooling.
At age nine, she graduated high school and started studying biomedical science at the University of Ottawa.
“The program was really wonderful for me because there were foundational courses in biology, chemistry, math and physics – all of those different areas that would allow me to find what I
government’s historic investment of an additional $330 million each year into pediatric care that is improving capacity, while reducing wait lists so children and youth can connect to the care they need, close to home, for years to come.”
The regional pediatric surgical program is the latest Kids Come First program to bring care closer to home, completing procedures such as an appendectomy, tonsillectomy, removing a hernia, and orthopedic surgeries. CHEO has been working with medical teams in Carleton Place and Brockville including their expert clinicians, while providing on-site training and collecting supplies.
The Kids Come First (KCF) Health Team is a collaborative that features more than 60 organizations, youth and family partners and nearly 1,100 physicians that connects high-quality care for children and youth in the region to simplify their healthcare journey.
“By combining funding, space and a team of clinical experts from CHEO, Brockville and Carleton Place, we have a winning formula. We can meet children’s needs quicker and as a bonus, we’re building capacity across the region,” said Alex Munter, President and CEO of CHEO.
The initiative also plans to expand to complete more surgeries at more hospitals in eastern Ontario. ■ H
was interested in and make a path for myself,” she says.
That path led her to graduate with an honours bachelor degree from the University of Ottawa in May 2023. Last fall, she began studying for her master’s degree at the University of Toronto and found a coveted research position with Dr. Antonio Strafella, a neurologist and world-renowned expert in movement disorders, at UHN’s Krembil Brain Institute.
“Anthaea-Grace’s unconventional pathway in education showed to me that she was not afraid of dealing with hurdles along the way,” says Dr. Strafella. “Challenges are always encountered in research and it is important how we deal with them in order to succeed.
“Anthaea-Grace is an exceptional, goal-oriented, hard-working student who is highly motivated and driven by curiosity and a love of learning.”
He adds: “This drive and curiosity in neuroscience brings her to explore ‘uncharted territories’ without being afraid to be outside of her comfort zone.”
That includes a research project using machine learning techniques and
artificial intelligence to predict whether a patient has Parkinson’s disease, or will develop the disease, five, 10, or even 20 years in advance.
“I’m currently working on using a neuroimaging biomarker called a dopamine transporter, SPECT molecular imaging, along with different bio fluid-based biomarkers such as alpha synuclein and beta amyloid – proteomic biomarkers that have a biological basis in the brain of patients living with Parkinson’s,” says Anthaea-Grace.
As part of her research, she completed a literature review, looking at research that has already been done in machine learning techniques to investigate and differentiate Parkinson’s.
“I discovered how little research there really is using multiple biomarker sources, such as neuroimaging and cerebrospinal fluid,” she says. “Finding out about the gap in the research fueled my passion to contribute to filling that gap, and support clinical validity for combining different biomarkers.”
Anthaea-Grace says the most rewarding part is thinking about the
This article was submitted by UHN news.
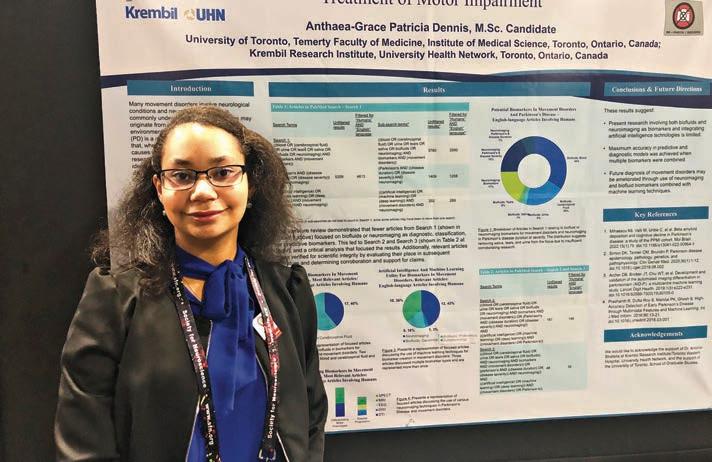
impact her research and medical training could have for patients one day, and on the Parkinson’s field as a whole.
“To be able to have a lasting impact on clinical practice for Parkinson’s would mean the world, both for myself as a researcher and also for patients who live with the disease,” she says.
“I’m hopeful I can make a difference in their lives one day.”
And she has some inspiring words for others who follow in her footsteps.

Anthaea-Grace Patricia Dennis is a Master’s student in Dr. Antonio Strafella’s lab at UHN’s Krembil Brain Institute, studying Parkinson’s disease.
“It’s really important to believe in yourself first of all, but also to take that belief and propel yourself forward, to work hard,” she says. “You know, Rome wasn’t built in a day, but Rome also wasn’t built alone.
“Even if you have big dreams, you also have to have support so you can get there. I wouldn’t be able to be in this position without the support of my family, of my mentors, my teachers.
“So, grow your network, always work hard and never stop believing in yours. ■ H







As a Caribbean woman who received a living kidney from a stranger, Jennen Johnson recognizes the importance of telling her story.
Diagnosed with kidney failure in her early 40s, Jennen put an advertisement in a newspaper for a donor after being told it would take nearly six years on the wait list for a kidney. When she received the call from a woman offering to donate, it meant that Jennen was on track to receive the best treatment for kidney failure – one from a living donor.
“When I found out she was a match, I was just over the moon,” says Jennen, recalling the joyous moment when she received the call from Toronto General Hospital (TGH).
Thanks to TGH’s surgical team her transplant was a success, but Jennen knew her experience with living organ transplantation was not one commonly shared amongst patients from African, Caribbean and Black (ACB) communities, something she attributes to mistrust in the health care system.
“When it comes to living organ donation, the Black community shies away from it because they feel if they’re in trouble and a white person is in trouble, (health care professionals) are going to save the white person,” says Jennen, who is a member of UHN’s ACB Organ Health YouTube Channel Advisory Committee, which aims to provide informative and trusted video content and resources for ACB patients, caregivers, clinicians and communities.
Living kidney donation is the fastest access to a kidney transplant for someone in need and may offer a quicker recovery and longer functioning than a deceased donor kidney. It also results in significant improvements in quality of life and productivity of people living with kidney failure.
Despite this, there are not enough living donors to meet the demand.
Access to living donor kidney transplant is even more reduced among ra-


cialized groups in Canada, with studies reporting up to 70 per cent lower likelihood of living donor transplantation for patients from South and East Asian, African, Caribbean and Black populations.
Barriers to transplantation and any type of health care might include language, cultural differences, experiences with racism and discrimination, less knowledge about the specific treatment and underrepresentation of different racialized groups among health care professionals, especially among physicians.
Dr. Istvan Mucsi, a transplant nephrologist at UHN’s Kidney Transplant Clinic, and his team, in collaboration with Dr. Jagbir Gill and his team in Vancouver, have been working to help ACB and South Asian populations reduce inequities in access to living kidney donation and transplantation in Ontario and British Columbia.
Together with patient and community partners, they formed the
A.C.T.I.O.N project – Improving Access to Living Donor Kidney Transplantation (LDKT) in Ethno-racial Minority Communication in Canada – which was funded by Health Canada in 2019. Dr. Mucsi and his team have systematically identified gaps and barriers that may prevent patients with kidney failure who are from racialized communities accessing living donor kidney transplantation.
“Our outreach seeks to address the suspicion and mistrust that ACB communities have towards the health care system with the objective of starting a dialogue between the communities –the research community, clinical community and ACB communities,” says Dr. Mucsi.
Currently, the A.C.T.I.O.N. project is running multiple ACB Health fairs, which focus on regenerative medicine – replacing organs and tissues damaged by diseases, injury, age or other issues. The fairs also address kidney
and organ health, organ failure related issues, including diabetes, high-blood pressure and heart diseases, all of which may contribute to higher rates of kidney disease.
“Our community engagement is essentially about creating a more trusting health care environment, collaborating with researchers from ACB communities and building a team that is diverse and representative,” says Dr. Mucsi.
“We are creating a network that can mobilize culturally responsive knowledge about kidney health and other relevant chronic medical conditions, and to create a culturally safe environment for patients with kidney failure to discuss and consider kidney health, kidney disease and living donation.”
Jennen now uses her story to advocate for living organ donation in ACB communities across Canada – those who are amongst other racialized groups where access to living donor kidney transplantation is most needed, but the need is not met.
“We create content to show what really happens when you donate an organ,” says Jennen, who says that issues surrounding representation among medical professionals are at the core of why Black populations are most unlikely to engage with donation, either on the donor or the recipient side.
For example, Jennen says that some might hold the mistaken belief that a kidney or organ from a white person would not function in replacement of a kidney in a racialized person and vice versa – the same assumption may be held with blood transfusion.
“Our dialogue can help Black communities say, ‘hey, maybe the information that I’ve had all this time isn’t right, because this person from our community had a transplant and they’re perfectly fine,” says Jennen, who is living proof.
“Being a living organ donor and receiving a living donation is important because it could save your life, it could save your family member’s life,” she says. ■ H



















Evelyn Aguilar
Humber River Family Health Team
Rosa Anasory
Alberta Health Services
Rhea Faye Caesar Argeulles
Alberta Health Services
Jennifer Arruda
Sunnybrook Health Sciences Centre
Ivana Matic Bacelic Trillium Health Partners
Elvie Basit Fraser Health
Emily Beke
Children’s Hospital of Eastern Ontario
Sauna Amyn Bhagat
The Ottawa Hospital
Nicole Boenig
Alberta Health Services
Dawn Borja University Health Network
Karen Fantinic Boyadjian Children’s Hospital of Eastern Ontario
Christopher Braz University Health Network
Miriam Brenes The Ottawa Hospital
Roberto Calantoc The Ottawa Hospital
Austin Chen
Alberta Health Services
Daniel Chiarelli Westpark HealthCare Centre
Maria Chiera-Lyle University Health Network
Beverly Chung Brown Oak Valley Health
Fortuna Clipa
Trillium Health Partners
Michelle Co Sunnybrook Health Sciences Centre
Abby Browne Children’s Hospital of Eastern Ontario
Charisse Callaghan Oak Valley Health
Dona Chen
Oak Valley Health
Cheryl DeLugt
Trillium Health Partners
uring Nursing Hero Week, let us take a moment to extend our deepest gratitude to the true superheroes among us – the nurses. The stories that fill the pages of Hospital News’ 19th annual tribute to Nursing Heroes are a testament to the heroic work they do every single day.
To our 88 nominees, thank you. To every nurse who has ever gone above and beyond, we salute you. With boundless compassion and unwavering dedication, you stand as pillars of strength, providing comfort and care to those in need.
In the face of adversity, you rise above, selflessly putting others be-
Margaret Desousa University Health Network
Janet Evans
Sarsfield Colonial Home
Kevin Fernandes
Trillium Health Partners
Jocelyn Galan
University Health Network **
Alex Galixia University Health Network
Jessica Galletta Oak Valley Health
Karen Ganchua Trillium Health Partners
Rachel Garner Providence Health BC
Mark Anthony Gravoso University Health Network
Karen Halden Trillium Health Partners
Sharmila Haniff University Health Network ***
Gerry Henry
Trillium Health Partners
Margaret Hernandez
fore yourselves. Your tireless efforts, day in and day out, do not go unnoticed. You are the backbone of our healthcare system, the guiding light in moments of darkness.
Your kindness knows no bounds, your expertise is unmatched. With every patient you touch, you leave a lasting impact, a beacon of hope in their journey to wellness.
So, to each and every nurse, we say “Thank You.”
Thank you for your sacrifices, your compassion, and your unwavering commitment to healing. You are true heroes.
If you are a nominee and would like to read your nomination, please email editor@hospitalnews.com ■ H
Ann Lescisin
Oak Valley Health
Katia (Kat) Lietz
Alberta Health Services
Janice Lin
University Health Network
Michelle BruceLockhart
Trillium Health Partners
Mediatrix (Gaby)
Mbombo
Trillium Health Partners
Diane (Dee Dee)
McEwan
VHA Home Healthcare
Janet Narciso
Mount Sinai Hospital **
Maya Nathani
Universal Health Hub
Susan Ng
Oak Valley Health
Joanne Ngo
Trillium Health Partners
Njeri Ntwiga
Trillium Health Partners
Jose Oliveria
Trillium Health Partners
Cathryn Paxon
Trillium Health Partners
Semona Piera
Melody Rowhani
Children’s Hospital of Eastern Ontario
Lucinda Leanne
Sapinosa
University Health Network
Mehrdad Shams
Micheal Garron
Hospital
Sharon Singh Trillium Health Partners
Susan Song
Trillium Health Partners
Carmen Stiller Sunnybrook Health Sciences Centre
Kalli Stilos Sunnybrook Health Sciences Centre
Sandra Stuckless Trillium Health Partners
Harry Uppal Healthcare on Yates
Slavka Vujic Mackenzie Health
Sonya Wajdie
Saint Elizabeth Healthcare
Kristie Jones
Editor, Hospital NewsTrillium Health Partners
Rowena Isla
Oak Valley Health
Ana Jalosinski
Alberta Health Services
Prabhjot (Jyoti)
Kaur
Trillium Health Partners
Charlene Kent
VHA Home Healthcare
Bonnie Kissick
Alberta Health Services
Yulia Kontos
Alberta Health Services
Shahnaz Lalnani
Oak Valley Health
Lindsay Lauer
Trillium Health Partners
Allan Lee
Mackenzie Health
Sunnybrook Health Sciences Centre
Sarah Pollock
Alberta Health Services
Valeriya (Valerie)
Potapov
Sunnybrook Health Sciences Centre
Domino Puson
Trillium Health Partners
Kelly Richer
Kemptville District
Hospital ********
Nicole Roberts
St. Joseph’s Health Care London
Emily Rosenblum
Sunnybrook Health Sciences Centre
Angelita Rosete
Alberta Health Services
Patricia Welsh Sunnybrook Health Sciences Centre
Relu Wiegner University Health Network
Jennifer Willard Holland Centre
Janice Williams University Health Network
Megan Wilson Oak Valley Health
Ingrid Wiltshire Stoby
Oak Valley Health
Taylor Woodhouse Alberta Health Services
Monica Zarello University Health Network




have been inspired, encouraged, and empowered by fellow nurse Mark Anthony Gravoso. He is not only my colleague in nursing but a great leader who truly cares for his members.
Mark has 16 years of clinical nursing experience from the Philippines, Abu Dhabi UAE and Canada. He is an internationally educated nurse (IEN) and is currently working as an RN in General Internal Medicine at Toronto General Hospital (UHN) and on the
Vascular Access Team at Sunnybrook Health Sciences Centre. He has completed his Clinical Educator Certificate from the Michener Institute of Education at UHN, is the President of the Integrated Filipino-Canadian Nurses Association (IFCNA) and a
Member of the Canadian Vascular Access Association.
He started as an RPN and later became an RN, working full-time at Toronto General Hospital within the fast-paced and challenging General Medicine in-patient unit. Mark is
known for his attention to detail and dedication to getting work done. He values the importance of patient-centered care, and he enjoys working with his team to ensure his patients are receiving the best care possible. While in this position, he prided himself on being a mentor/preceptor to newly hired nurses on the floor, students, and internationally educated nurses completing their Supervised Practice Experience Partnership (SPEP) program. He engaged in activities to strengthen competence in nursing skills by providing in-person help to the nursing team. He found his passion for clinical mentorship as he obtained his Clinical Educator’s Certificate from Michener Institute of Education at UHN, and attended the Preceptorship Workshop and RNAO Best Practice Champion Program to gain more knowledge and training to become a more effective mentor.
He also became an RNAO Consultation Representative of the York East Region to the RNAO 98th Annual General Assembly 2023. He is also the 2024 Recipient of the TeamUHN Declaration of Values Compass Pin for his exceptional clinical care, which included empathy and compassion that went a long way to making his patient truly feel seen and cared for. This recognition from patients to TeamUHN staff members during their challenging times in the hospital highlights the five core values of UHN Patient Declaration of Values (DOV), emphasizing Empathy and Compassion as essential components of quality healthcare. His love for Vascular Access (Difficult IV insertion and troubleshooting CVADs) led him to join Sunnybrook Health Sciences Centre (Bayview Campus) VAT Team where he shares his expertise to improve patient’s experience in getting IV access with a better success rate of insertion. He also provides education in Vascular Access Care and Maintenance, providing further opportunities for him to meet IENs and encourage them to pursue their nursing career.

As the President of the Integrated Fil-Canadian Nurses Association (IFCNA), I commend Mark’s unwavering support, unrelenting guidance, and mentorship abilities that helped in leading the path to Success for Filipino Internationally Educated Nurses(IENs) in Canada. Mark is an avid supporter of all IEN,s providing tremendous support because he believes that everyone has the power to lift others up with motivational words that can change someone’s outlook on life.
With his passion for nursing and commitment to serving the community, he advocated for the credential recognition of Internationally Educated Nurses (IENs) to address Canada’s looming nursing shortage. He pushed for acknowledging credential recognition and streamlining the process of nursing registration of IENs and assistance to those IENs with immigration issues in the roundtable discussions with Parliamentarians and policymakers. He advocated for the need to act quickly to get the country’s many internationally trained, but currently underutilized, nurses and other
medical professionals back to work. He identified the obstacles IENs face in Ontario, Canada’s most populous province, and gathered recommendations that could help IENs throughout the country reach their career goals.
As an advocate for IENs, He presented his recommendations to government during the roundtable conversations he had on mitigating today’s challenges in the healthcare industry.
Mark presented his recommendations and requested parliamentarians to review them, considering the current shortage of Nurses in Ontario.
1. Extend the duration of the working permits for Registered Nurses
2. Support for nurses applying for permanent residency through the creation of additional spots designated specifically for high-demand occupations such as nursing.
3. Review of the requirements set forth by both OINP streams alongside individual employer-based applications from those same companies that did not assist in either process (work visa renewal or provincial nomination program)
As President of IFCNA, Mark has improved the mentorship programs for all Filipino-Canadian Nurses and enhanced the collaboration with other
organizations and government agencies to support IENs like myself in the journey to our Canadian RN dream and successful integration into the Canadian healthcare system by providing information sharing among members and free educational learning opportunities and referral to our employment. Some IENs like myself, do not meet the eligibility criteria of publicly funded employment and educational programs because of immigration status, thus making it difficult to meet CNO’s nursing registration requirements. IENs holding work visa permits like me face a of challenge unique set of challenges but with Mark’s support we are overcoming these hurdles. He makes all things possible for IENs having immigration issues with his initiatives of collaboration with other organizations so we could have free learning opportunities, information sharing, and training. He effectively collaborated with other government agencies so we could have a platform to raise our concerns as IENs and better access to the programs that would help us achieve our nursing license. He is a nurse who has gone above and beyond the call of duty. He is the nursing hero in our IEN community. ■ H
Nominated by Froilan A. Imatong, RPN
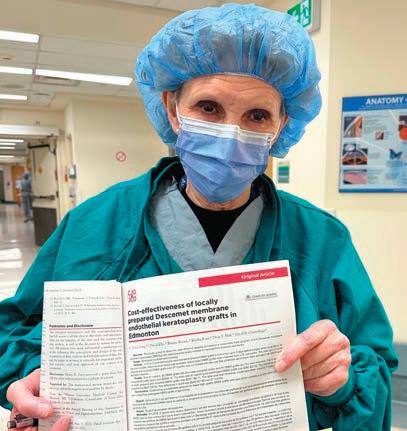
am writing in strong support of Ms. Bonnie Kissick Nurse for Nursing Hero award 2024. Bonnie was the nurse manager at the Royal Alexandra Hospital, Ophthalmology and ENT Operating room in Edmonton, Canada until her retirement one week ago. Bonnie is the most exceptional patient advocate with whom I have ever had the pleasure of working.
I am an ophthalmologist and retina sub specialist based at the Royal Alexandra Hospital. I have been in practice for 20 years and throughout this time Bonnie Kissick led our op- erating room as head nurse manager. Without question I believe the Royal Alexandra Hospital Ophthalmology and ENT operating room to provide the finest surgical care in the country. Bonnie Kissick is the reason we can provide such exceptional care.
1. There is no one who is more dedicated or harder working than Bonnie Kissick. Regardless as to the time of day or day of the week, Bonnie could be found in her office or around the operating room helping out. If a special form had to be completed to access restricted medication or specialty medical device Bonnie would personally make it happen.
2. Bonnie always puts patient care first, regardless of the situation or concern of overtime, Bonnie would ensure that patients would receive timely access to surgical care. Many many times, when I was worried that an emergency case might not move forward due to bureaucratic difficulties Bonnie would would say to me “Dr. Tennant, we will do what is best for the patient”. This policy has allowed me to provide the
very best surgical care for my patients over the past 20 years.
3. Bonnie always would go above and beyond for patients. As an example, two months ago a patient, who happened to be a recent immigrant to Canada with limited resources and English as a second language was having difficulties getting to the operating room in time for her emergency retinal detachment surgery.
The entire operating room was waiting for the patient to come from her home to the hospital on a Friday evening. Bonnie personally called the patient’s husband and convinced him that timely eye surgery was imperative to save the vision in his wife’s eye. Bonnie gave step by step directions for the patient’s husband to drive his wife to the hospital. Upon arriving at the Hospital the patient was unable to find the operating room. Bonnie left the operating room on foot, travelled to the corner of the hospital property, found the patient and her husband waiting in their car, then got into the car with the family and directed them to the operating room entrance. She then brought the young lady into the operating room for admission and surgery. This example was by no means unique. Bonnie performed such acts of kindness every day.
Bonnie is a nurse who has dedicated her life to helping others through her work as a nurse. This life of service has been an example to all those who work with her. When I think of why I love working at the Royal Alexandra Hospital; an inner city hospital that treats all those that would otherwise be forgotten, I realize it is because of people like Bonnie. An individual who has

spent a lifetime giving back and never expecting anything in return. I can think of no one more deserving than Ms. Bonnie Kissick, nurse manager from the Royal Alexandra Hospital, Edmonton, Alberta.
Respectfully, Matt Tennant, MD, FRCSC, Ophthalmologist, Clinical Professor Department of Ophthalmology, University of Alberta
Nurse Bonnie Kissick is an amazing Nursing Hero, who just retired this month after decades of service to the patients in Edmonton and Northern Alberta. As the surgical patient manager at the Royal Alexandra Hospital G O.R. she helped patients and surgeons from multiple services complete their emergency and elective surgical cases in an expert and timely fashion. Bonnie’s work ethic was nonpareil. I usually arrive in the hospital before 7
am and leave after 7 pm. Bonnie would always be working at her station before I arrived and after I left, optimizing the surgical lists, finding shift replacements, and obtaining supplies.
The Kissick motto was, “Patients come first”. She was a steadfast advocate for what was best for patients and would do her utmost to make the operating room time and resources available for her patients, staff, and surgeons. She found a way to incorporate new medications and new surgical instruments into her limited budget. Her infectious, caring, can-do attitude established the excellent surgical reputation at the Royal Alexandra Hospital. Every single surgeon and nurse on multiple surgical services had the utmost respect for Bonnie’s unwavering dedication. We were deeply saddened when Bonnie retired a few weeks ago.
Continued on page 24
n the heart of Holland Centre, you will find an inspiring and cheerful nurse with a commitment to excellence. This nurse, Valerie, demonstrates leadership through her dedication, willingness, expertise and positive demeanor. Valerie’s leadership qualities, support for the entire team and commitment to all patients make her a true nursing hero.
Valerie has embarked on her nursing journey at the Holland Orthopaedic & Arthritic Centre for 13 (fantastic) years. Throughout her career, she has embraced every opportunity to learn, develop professionally and strive for excellence in her practice. She is an active advocate and proud member of nursing council. Her peers describe her as a team player, advocate, and she is known to go the extra mile for patients to provide them with hope and comfort. Valerie has a depth of knowledge and a compassionate approach to patient care, she makes a lasting impact in the lives of many individuals each day.
Valerie embodies integrity and compassion while inspiring those around her. She often works in the capacity of team leader for 6 and 7 East, guiding the team through challenging situations. She leads by example while maintaining a contagious, positive attitude. Our patient population consists of post-operative and transitional care patients, some of the population include patients who demonstrate highrisk behaviors. During unpredictable situations, she is able to remain calm and composed to efficiently coordinate care, provide comfort and emotional support to families and staff. She has been recognized for her responsiveness and courage in code scenarios, as well as regularly providing support. Her approach to care is person-centred, respectful and dignified. She is skilled at recognizing the unique needs

of patients and creating individualized care plans. It is not uncommon for patients and family members to recognize her hard work and dedication. Mr. C and his wife we’re enthusiastic to share how Valerie has positively influenced their hospital stay in support of her Nursing hero nomination- “I feel she is God sent, I can feel the love in her nursing care. Because of her I don’t feel like I am in a hospital, it feels like I am a part of a family. This is important to me. I include Valerie in my prayers, she provides me comfort because she does not rush and takes time to explain things to me.”
Another example of Valerie’s patient-centred focus: We recently had a patient request for MAID procedure, this was the third time that MAID was performed at our facility since it has
been legalized. Immediately recognizing some of the team members feelings and moral/religious objections, Valerie had honorably volunteered to be the primary nurse caring for this patient during the day of the procedure. Valerie had developed a special rapport with the patient and his family, so much so that the patient had even shared with other team members that he was hoping she would be the nurse present to “wish him goodnight.” Valerie participated in many conversations to educate, comfort and validate feelings of staff. Most notably, she wore the most bright yellow sweater the day prior to the MAID procedure. When complimented, she had shared that she wore the sweater to brighten the patient’s day, since yellow was his favourite colour- it reminded him of sunshine and his favourite place, Florida. Valerie also helped orchestrate the collection of staff signatures on a big, bright (you guessed it…) yellow
card to give to the patient prior to his passing.
Valerie continuously shows support and dedication to nursing scholarship and ongoing learning through the mentorship of nursing students, new hires and being an active member of nursing council. She supports best practices and is dedicated to implementing quality improvement initiatives (i.e: calorie counts, early mobility, medpass, skin & wound best practices). She is very supportive of the allied healthcare team through supporting safe discharge needs, and liasing with community healthcare partners when needed.
In every interaction with Valeriya, it is a testament to her professionalism and dedication to the nursing profession. Recognizing her outstanding contributions to the Holland Centre team, we wholeheartedly nominate Valeriya as a Nursing Hero. Her leadership, dedication, supportiveness, expertise and positivity act as an inspiration to us all.
– Mackenzie Conn, 6/7East APN, Chantal Letang, 6/7East PCM & Patient/family recognition
The most admirable quality of Valerie is that she is always doing more than she is supposed to do. She always goes above and beyond no matter how small or big the task is. For example, she provides showers to patients when they are not scheduled for one or will paint/ trim patients nails. She is extremely accommodating when providing care to patients and ensures that their voice is heard. I have witnessed several occasions when she will purchase personal hygiene items if the patient does not have any. These may seem like minor acts to most people, but it makes a world of difference in our patients stay, sense of belonging and overall well-being. She has done many great things for patients and families.
– Ekaterina Zharinova, 6/7East RPN & Pilar Ramirez, 7East PT
Nominated by: Chantal Letang, Mackenzie Conn, Ekaterina Zharinova and Pilar Ramirez ■ H
It is our honour and pleasure to nominate Susan Ng (Advanced Practice Nurse) Hospital News Nursing Hero Awards. She is the nurse navigator for Seniors Home Support, an interdisciplinary primary care program for homebound seniors. As a full-time nurse navigator since 2021, she is the first point of contact to triage and respond to patient concerns, provide timely follow-up, and help patients and caregivers navigate hospital resources.
The testimonials below offer profound accounts of Susan’s impact on our program, underscoring her exceptional clinical knowledge, effective triaging skills, and compassionate care for our patients and caregivers by helping patients and their families to navigate through health care system. She demonstrates remarkable leadership by taking the initiative to propose innovative and thoughtful patient-centered solutions, clearly outlined in the example provided by W.S. She is an excellent and dedicated advocate, not only for our patients when she acts as a liaison in the emergency department but also for homebound seniors in general. Susan is extremely passionate about improving the lives of vulnerable se-
Continued from page 22
niors, proposing workflow solutions, sharing resources with our team, and implementing quality improvement initiatives. She has volunteered to be part of the Ontario Health Team palliative care table, led an environmental scan of geriatric resources and needs in Uxbridge, and also led our program’s quality improvement research, which she will present internationally in April 2024, impacting the lives of homebound seniors worldwide. We are so fortunate to have Susan as a member of our team and strongly believe that she deserves recognition for the profound impact that she has on the lives of our seniors.
It is with great pleasure that I share this endorsement of Susan Ng for the Hospital News Nursing Hero awards.
I have had 3 family members in the Seniors Home Support Program for several years now. One who recently passed away from a very challenging 12-year battle with a rare, degenerative illness, and 2 others who have various cognitive, health, and mobility issues that require round-the-clock supervision and care. As a working single mother, this program and in particular Susan Ng and Dr. Mui have
However, we are comforted that in times of adversity we will remember her shining spirit, ask ourselves, “What would Bonnie do?”, and this will lead us on the correct path.
In summary, Nurse Bonnie Kissick is a Medical Hero that kept the Royal Alexandra Hospital safe and above water despite tumultuous seas. Her profound commitment to patient care makes her most deserving of your Nursing Hero Award.
Nominated by: Dr. Edsel Ing Professor & Chair, University of Alberta, Depart-

given me such hope for the future of Health Care for Seniors in our province. That is no exaggeration. The personal, knowledgeable, compassionate, efficient, and thorough treatment we receive with this clinic is phenomenal. I rave about them regularly to anyone who will listen, so I’m happy to have a chance to put it down on paper.
Susan’s responsiveness and personalised approach to care have been invaluable to me and my family. Whenever I reach out, whether by phone or
voicemail, Susan consistently responds within an hour, demonstrating her unwavering commitment to our well-being. She is well aware of my family members’ health histories and issues, enabling her to provide tailored and timely recommendations and support. Susan expertly deduces, triages, and determines where we need to go next, whether it’s a phone call or a home visit with the doctor or paramedics, or an emailed (through Medeo) requisition from the doctor. Susan’s leadership in
ment of Ophthalmology & Vision Sciences, Chief of Ophthalmology Division, Edmonton Zone and Professor, University of Toronto DOVS
***
Re: Bonnie Kissick, RN, Royal Alexandra Hospital For over more than 25 years, my colleague surgeons and I have been inspired, encouraged, supported, and coached by this wonderful nurse. She has, by her significant energy and devotion to patient care, made the BOR (shared mainly by Ophthalmology/ENT) the very best OR in Canada
for eye and ENT surgery. There is no question in my mind of this statement, having visited all the major eye/large hospital centres in Canada. She has repeatedly pushed back any suggestion of a nomination for an award. She retired last month and wanted no celebration. She said emphatically that her reward was caring for the patients, nurse and surgeons and making the best outcomes possible. I am saying these words having witnessed the development of the amalgamation of 6 hospital programs into a regional eye centre in
1996, and then the construction of a purpose built OR for Ophthalmology. She should be very proud, as we all are, of her significant accomplishments and advocacy for our program. Because of her, we have a solid foundation, a hub that everyone can depend upon – patients, trainees, nurses, and surgeons. She is truly a “Bonnie lassie”.
Sincerely yours, Ian MacDonald, MSc, MD CM, FCCMG, FRCSC, FACHS Past Department Chair 1992-2014 Past Regional Alberta Health Services, Clinical Chief, Edmonton/Ophthalmolog ■ H
this facet is implacability. Moreover, Susan’s follow-up care is seamless and thorough. She never goes overboard and never minimizes the issues. Susan takes the time to re-explain in detail what the next steps will be, to ensure I fully understand the doctor. She tells me what any new prescriptions will look like and never makes me feel like an imposition when I reach out to her with additional questions, amidst her business schedule. Susan has even coordinated my large extended family into group meetings with Dr. Mui via video conference and trust me, managing all of us is no easy feat, that alone is worthy of an award!
When emergencies arise, which they tend to do with three fragile seniors, Susan is always calm and centred (which keeps me calm and centred too). Susan even went extra mile to visit my father when he was in the ER and hospital after a fall. It was extremely touching and comforting to know Susan, the “voice on the other end of the phone”, was there in person, holding his hand and being an advocate for him.
And when the time came and my mother was ready to pass away, Susan and Dr. Mui were there with us, by phone and in person, explaining what to expect. Susan, with her deep experience in palliative care, knew exactly how to do it. She gently connected me with the funeral home and helped with a lot of details behind the scenes that I don’t
even remember because of the loss.
The consistency of care and the time saved by being a part of this incredible program as a busy caregiver is so helpful. From the first call to the appointment, to simple tests being administered here at the house, to medications being phoned in and hand-delivered from the pharmacy, it saves me from countless trips, missed work days, and from the risks of bringing fragile seniors with mobility issues into hospitals and clinics where they are susceptible to falls and/or contracting infections. Being a caregiver to seniors is often an emotionally complicated and stressful business. Having a team of Health Care Providers like Dr. Mui and Susan Ng behind us is 100 per cent the reason I can keep them here at home, comfortable and connected to family, friends, and their community. This support offered my mother the security and dignity to stay home with her husband until her death. And it allows me to maintain some semblance of balance. I am extremely grateful.
***
My wife with advanced Alzheimer’s condition has benefitted immensely from Susan Ng’s outstanding palette of caring attributes. Susan took the initiative to find a smarter way to replace
erry is not only an exceptional nurse, but an exceptional person overall. Gerry has worked at Trillim Health Partners for many years as a nurse, educator, and now as a clinician specialized in wound, ostomy and continence care. His knowledge and experience in wound management through his various roles has made him an expert in his specialty with many colleagues of different professions hoping to learn from him. You can feel his joy in this specialty when he teaches, he is a natural educator. Being such an expert, he is also humble and ea-
the tiny broken external Y-connector for the permanent G-tube Francine depends on for all meds and nutrition. Instead of the stressful, resource-heavy transport, long wait in the ER, and the expensive trip home, she suggested I photo that part and site and email it to her; she showed this to the Interventional Radiology staff who quickly provided the simple part. She called for me to pick it up and with the help of our regular nurse, the part was easily replaced.
On a different more recent situation at the ER, I was deeply impressed with her visit to advocate and facilitate my wife’s procedure. Not only that but imagine how grateful I was when she arrived with a toasted sesame bagel for this anxious caregiver!
***
Our family has been a patient at the SHS clinic for a short period and in that time, Susan has made a huge impact on our family. She is constantly following up on test results, touching base with family members after a test to see what the outcome is, and also meets with patients when they need anything. For instance, while waiting in hospital for an appointment, Susan provided us with a blood requisition so that we could do both appointments at the same time
and minimize the amount of time necessary to get the information the clinic needed. Another example is the time she called on her way home from work to touch base about a test result that was pending, indicating it was on her radar, and that she would be following up on the test the next day when she returned to the office. Susan constantly goes above and beyond connecting between care providers, patients, and their family members.
I first met Susan in Markham Stouffville Hospital ER when she came to see my late husband. He was already having dementia and was not being very cooperative. From the outset, I was impressed by Susan’s kind and patient manner. She spoke to him calmly and quietly and assured him he would have good care.
Since then, I have had numerous interactions with Susan, and each time I find her to be very knowledgeable, professional, compassionate, and supportive. Her tone of voice is always warm and friendly and I never feel I am being stupid with my questions. When I have to leave a message, I know it will be answered as soon as possible and Susan will pass my information to Dr. Mui appropriately.
Altogether, I think Susan is well qualified to receive Hospital News Nursing Award.
– Annie Cheung, Physician, anncheung@oakvalleyhealth.ca, A.M. (caregiver) ■ H
G HMger to learn new things and listen to different perspectives. He makes every person he is speaking to feel like the most important person dedicating his attention and time to matters at hand, whether its a patient, family or a colleague. I don’t know anyone who works here who doesn’t know Gerry because he makes an impact on everyone he meets. He will often be seen in the halls being stopped by everyone to say hi or catch up because he brings joy and kindness to each encounter. One moment in particular he was a few minutes late to a meeting, because a family member stopped him to tell him
that a patient he is following is receiving end of life care. He was so important to this patient and family that they wanted him there to say goodbye. He took the time out of his busy schedule to spend the time and pay respect to the patient, and support the family during the patient’s passing. He is an example of what every nurse should hope to be; compassionate, kind, skillful and courageous.
honourable mention
Nominated by: Allison Da Silva, RN, NSWOC WOCC ■ H

Slavka Vujic is a registered nurse who works on our C4 Orange Complex Care Unit at Mackenzie Richmond Hill Hospital. She started at Mackenzie Health (when it was still York Central Hospital) in July 2008 in complex continuing care. When Mackenzie Health moved Slavka’s unit to the Reactivation Care Centre in 2018, she was so committed, she moved with her unit and team. In October 2023, as planned, Slavka came back with her unit and team to Mack-

enzie Richmond Hill Hospital. Slavka demonstrates patient care excellence in her everyday work. She is an incredibly patient-centered nurse. On C4 Orange, there is only one RN on every shift and that RN is always the MRN. All staff request to work with Slavka. Staff describe feeling “safe and secure” when Slavka is on duty. “She takes care of everything when you need her!”


There is a solution. Introducing the Health Care Providers Group Insurance Plan, a distinctive program designed to either supplement your existing coverage or provide a comprehensive option, all without increasing hospital expenses.
Coverage is tailored to meet the needs of your workforce and can help protect them from unexpected events.
For employees already covered by a spouse's or another group plan, there's an exclusive option including Life, ADD&D, and LTD coverage, all for under $32 per month. Peace of mind at an exceptional value.
HCP honours the invaluable contributions of nurses. Join us in


SLAVKA’S STRENGTHS ARE HER LEADERSHIP SKILLS, ADVOCACY, WORK ETHIC, RELIABILITY, FLEXIBILITY, CLINICAL KNOWLEDGE AND SKILLS, CONFIDENCE, AND CREATIVITY.
In 2021, Slavka stepped up and became a Clinical Facilitator for her program. Her formal and informal leadership skills shine through everyday! When it comes to advocacy for patients and families, she always puts them first. The relationships she builds with the complex care patients and their families is incredible. She is always the first nurse the leadership team goes to for a quick safety review or new idea that needs an honest opinion on its potential.
Slavka’s strengths are her leadership skills, advocacy, work ethic, reliability, flexibility, clinical knowledge and skills, confidence, and creativity. She is known as the cheerleader for her team. Recently, she signed up for Strides for Mackenzie Health (the 5km walk/run at Canada’s Wonderland) and is running her own campaign on the unit to raise funds for the hospital. Furthermore, she has imbedded High Reliability Organization (HRO) universal skills in her practice. She will be the first one to ‘cross check’ and ‘speak up’ or ‘stop the line’ for safety. She understands that every
vulnerable patient in a complex bed is someone’s picture person and she will advocate with empathy every time! She has also led many mini patient care improvement projects on her unit. For example, she created an award system where new nurses could get tokens of appreciation for best mouth care and best trach care of our complex patients. She continually elevates passion and quality for the very vulnerable populations of patients and families in the complex and continuing care program. In addition to unit specific projects, Slavka is always involved in unit council and any other “superuser” initiatives rolled out corporately.
In addition to everything listed, Slavka is the nurse that all new hires want as their mentor. She openly shares her 16 years of Mackenzie Health experience with her peers and leaders. Her goal is to have C4 Orange be the magnet unit at Mackenzie Health! The collaborative culture she fosters is outstanding and there is no one that would deserve a hero award more than Slavka Vujic! ■ H





































nna is one of the respected charge nurses of the in-patient psychiatric unit of Royal Alexandra Hospital and is also the clinical educator. With more than two decades of providing world-class quality nursing care, Anna has honed her skills, knowledge and critical thinking. With her natural confidence and expertise, it has been seamless with Anna leading the group. In my own experience, Anna is well organized and has that clinical eye in leadership. She is the go-toperson during the trouble shooting of challenging situations like handling complaints and conflicts. Moreover, she also advocates the safety of the staff and patients in the workplace by ensuring that the needs and concerns of the patients and staff are met. She is able to get along with a diverse and multi-cultural group of nursing staff in a way that encourages staff and patients to work as a team. She provides solutions to the issues she can fix and involves others when required. She is also a volunteer in their community daycare and helps out by providing basic education for kids and assists in cleaning the toys and organizing.
Anna fosters a collaborative approach to care and is one of the pioneers of collaboration at Royal Alexandra Hospital, especially in addictions and mental Health. As a charge nurse, Anna attends the rapid rounds where most of the heath care team are present to discuss the treatment plan of the patients. The team is composed of the main attending physician, pharmacist, social worker, nurse, physical therapist, and occupational therapist. This treatment plan is further discussed with the patient during their rounds. Anna advocates for the need of having family conference as part of the treatment plan for the patient. She ensures

that patients and their families are able to express their needs and address any concerns as preparation for their discharge home and going back to the community. Anna initiates care huddles before, during and after each shift. With these, any patient concerns and needs are addressed.
Anna is one of the Connect Care champions and as Super users when Connect Care was implemented. She attends workshops, training and seminars that improve the care provided
to the addiction and mental health patient population. She reads nursing journals and articles that highlight patient’s safety. Moreover, Anna ensures the staff from Addictions and Mental Health to have an annual education program for. In addition, Anna has completed the Leaders in Rehab program through the Glenrose Rehabilitation Hospital. While completing this course, Anna had to complete a leadership project in which we had to implement a positive change within
our work environment. Anna’s project was focused on increasing communication during times of transfer, between sending and receiving sites and bed management. Her project is the reason bed management now connects the two sites and the sending nurse provides a verbal report to the receiving nurse – bridging a gap in care.
With her role as a charge nurse, Anna emphasizes the importance of LPNs in Addictions and Mental Health. She initiates care huddles to identify the needs and concerns of the patients. LPNs report any changes in patient health status basing on their assessment and clinical judgment to the team. And whenever there are any challenges and issues, Anna asks for suggestions from her colleagues. She is open minded and listens to recommendations and suggestions of her team members.
Anna encourages every member of the health care team to perform at their optimal scope of practice. She reiterates that when we provide care it should be the best, effective, and quality care for the mental health patients. She highlights the importance of continuing to have the rapid rounds and family conference with the patients, and doing care huddles with the nursing staff so that the needs and concerns of the patients are met. In addition, when she noticed that any staff have struggled in a certain task or procedure, she takes the time to talk to them. She provides orientation for new staff, booking buddy shifts for new hires and ensures they feel supported and ready to work independently. Providing any educational supports for new skills and any changes in policies and procedures.
In summary, Anna is perfect fit for a Nursing Hero Award. A born leader, down-to-earth nurse, highly qualified, professional and competent individual who is a recipient of recommendations from patients, families, and management.
Nominated by: Jun Christian Odtojan ■ H








It’s an honour for us to nominate Ingrid Wiltshire-Stoby!
Ingrid began her Oak Valley health journey in 2008 as an RN in Inpatient Mental Health, skillfully working in the PICU with challenging situations and special needs patients. Ingrid is a true patient advocate and team player. Ingrid also served as facilitating nurse (FN) and professional practice lead (PPL), leading by example, never hesitating to support and coach staff to identify and strive for their career goals.
In 2018 after completing her NP certification, Ingrid transitioned to adult Outpatient Mental Health, pioneering our first ever NP program in the Rapid Access Psychiatry clinic. Ingrid’s effort has significantly decreased patient wait times for initial psychi-
atric assessment by months decreased. As a full-time NP, she had a direct, measurable impact on improving patient experience and decreasing risk.
Ingrid’s works include the full scope of NP practice, consisting of collaborating daily with stakeholders including patients and families, physicians, allied health, clerical, and crisis. Ingrid strives to build trust relationships with our psychiatrist group as we were offering something innovative-diagnostic and prescribing mental health patient care service for the first time by an NP, not a psychiatrist. Also showing innovation by collaborating community partner organization CMHA, supporting them by providing

psychiatric assessments in the community for their clients where no hospital visit is required!
Ingrid’s excellence and perseverance were evident within a year, leading to compelling evidence supporting the hiring of a second adult NP. Ingrid created a roadmap to meet patient needs for rapid psychiatric access. As a result of her hard work, we’re currently hiring an NP for child and adolescent outpatient mental health services; and we know this will work too!
Recent feedback from an adult OPMH patient highlights Ingrid’s exceptional ability to listen and respond effectively. He states, “Ingrid heard and responded to what I was saying
and to what I wasn’t comfortable saying, she understood me and I felt heard for the first time in years. She was kind and gentle and I got the help and support I needed.”
Ingrid’s colleagues describe her as a dedicated, caring nurse, and committed to the patient’s full recovery (physically, spiritually, psychologically, and intellectually). Ingrid is patient-focused, acting as an advocate, particularly in situations where patients aren’t able to, or struggle to advocate for themselves. Ingrid is an exemplary role model for women. Establishing goals, moving quietly forward, and accomplishing them through the many roles she’s held at our hospital. Prioritizing patient care, practicing diligent-

INGRID’S COLLEAGUES DESCRIBE HER AS A DEDICATED, CARING NURSE, AND COMMITTED TO THE PATIENT’S FULL RECOVERY (PHYSICALLY, SPIRITUALLY, PSYCHOLOGICALLY, AND INTELLECTUALLY).
ly, thoughtfully, and professionally. Working with Ingrid is always enjoyable, and her dry sense of humour adds joy to each day.
Ingrid is a true inspiration; not only does she complete her NP while working full time at Oak Valley Health, but she has also taken on active roles with the College of Nurses of Ontario (CNO) and University of Ontario Institute of Technology (UOIT) as a clinical instructor with nursing students, providing mentorship for new nurses. Ingrid uses her professionalism to uphold the standards of the CNO, advocating to protect the public, shaping the nursing profession by strategic decision making and planning, advancing practice through educating,
and preparing future nurses to carry the baton.
Ingrid is a super role model for nurses, showcasing tenacity and grit. She possesses an unparalleled work ethic and was ground-breaking in the role of the first NP in our Rapid Access Psychiatry clinic program. Ingrid carries herself with a calm modest manner, with a smile, and self-deprecating sense of humour, putting others at ease. She is a team player, approachable, and cherished by colleagues and patients too.
Ingrid embodies excellence in professional nursing practice. Thank you for considering Ingrid for this award. :)
Nominated by: Teresa Givelas, Patient Care Manager ■ H


aren Fantinic-Boyadjian is an all-star nurse at CHEO (Children’s Hospital of Eastern Ontario)!
Karen has been an RN at CHEO for many years, changing the lives of many patients over the course of her nursing journey. Karen has spent the majority of her nursing career working in eating disorders, and has become an expert in the field. With her knowledge, kindness, and caring nature Karen not only impacts the lives of patients and families, but also of her colleagues. She is quick to offer support, mentor a new nurse, or help staff better understand
the complex realm of eating disorders and they affect they have on patients.
Recently, while working with a newly diagnosed patient and her family, a mother told me that Karen had helped her to see and understand eating disorders in a whole new light, and that for the first time she understood the internal struggle her daughter was facing. THe mother explained that she no longer felt frustration and anger towards her daughter, but that she felt compassion for what her daughter was experiencing. This led to the mother being better able to connect with her daughter, and they have been taking
Every day, Sunnybrook nurses demonstrate commitment, compassion and strength. Our nurses have an extraordinary and lasting impact on the health of patients, residents, families and each other.
As we embrace this year’s theme – Changing Lives, Shaping Tomorrow, we will learn, grow and provide exceptional care when it matters most.
With our deepest gratitude for all that you do.
HAPPY NATIONAL NURSING WEEK 2024.

steps towards recovery that previously seemed impossible. This is not out of the ordinary. Almost every family that connects with Karen feels the impact that her knowledge and guidance have. Even in some of the most challenging and longterm cases our team has dealt with, Karen maintains optimism and patience; she can support a patient struggling to eat a granola bar day after day, without complaint - she feels the patient’s struggle and connects with them in a meaningful way. I have learned a lot from watching Karen over the years, and try to emulate her positivity and empathy in every patient interaction. Her stellar patient interaction is not the end of it. Karen is also very smart, and recognizes arising medical issues and trends quickly, jumping into action to help turn things around. She
HMrecently read a referral and noted some concerning medical features; Karen advocated for a quick assessment and helped to prevent major complications from presenting in the community.
Karen has held a variety of roles within the eating disorder program, and shines wherever she goes. Karen has worked at the bedside with some of the sickest patients, as well as in the day program where she helps patients to work towards independence and recovery. Karen has also held roles as case manager, doing triage, and even joined the team the helped our hospital go live with Epic. Wherever she works, Karen brings a compassion and advocacy that is unparalleled.
Karen’s work with the eating disorder community is so important and valued. I hope that she can be recognized for all of her hard work! ■ H

or 17 years and counting!
FSharmila Haniff has been my nursing hero! She is an empowering nurse from PMH 18B Short Term Care is exactly what a nursing hero encompasses. As I write this, I become emotional since she was my first encounter on 18B as my nursing preceptor in 2007. She fills you with confidence and encouragement to her colleagues, members of the interdisciplinary team and most importantly, the patients who need this care and affection the most. To each new staff member that enters the busy unit of 18B, she is always there to help them transition and offer advice or support when needed. There has been quite a staff turnover on our unit, and never has she become weary of offering her skills and knowledge to them. I have never seen any other
nurse go above and beyond like this. She keeps her patients smiling despite the challenges of treatment they encounter.
Sharm, after 22 years of nursing, continues to exude the utmost care and compassion to the people she touches. Not only should she be recognized for this reward, but she should also know it was her that made me who I am today as an oncology nurse and also a personal friend who I refer to as my sister.
You have your nursing hero on what we refer to as the penthouse suite of Princess Margaret Cancer Centre.
Nominated by: Michelle Ganesh ***
I wanted to nominate Sharmila Haniff Oncology Nurse on 18B Short Term Care Unit at Princess Margaret Cancer Centre.
Sharmila is a dedicated nurse who advocates for patients to ensure safe and timely treatment is provided. Patients are always made to feel they are in good hands with her caring, empathetic and funny approach. She is able to respond to crisis in a calm and collected manner, always ready to take the lead. She is organized and has the ability to prioritize patient care based on patients’ needs. She goes above and beyond for everyone that is under her care.
ing approach and she will support you if you feel you are not being treated disrespectfully by others. Always encouraging and gives you validation.
Sharmila has been a preceptor for nursing students and new nurses. All her learners have done well, some hired at PM. She teaches with patience and understanding and her expertise is definitely passed on to the learner.
Sharmila is a huge advocate for fellow nursing colleagues. New staff are always welcomed with a kind mentor-
Sharmila is a special person. She encompasses what nursing is, especially oncology nursing. She is an integral part of 18B and is definitely worthy of this nomination and award and so much more.
Nominated by: Bindu Patel RN CON(C) ■ H



Iam writing to nominate a colleague, Taylor Woodhouse that has demonstrated an inspiring and encouraging spirit in the wake of the Pandemic. At a time when healthcare feels more exhausting than ever, those still working in the field have persevered, though certainly have been feeling the weight of the aftermath (staffing crisis, low morale, burnout, etc.).
Taylor worked throughout the Pandemic on the frontlines in a busy hospital within the psychiatric emergency setting, and consistently demonstrated an adaptable spirit to the constant changes and sought ways to improve both staff and patient safety as well as staff morale throughout. Post-pandemic, Taylor has taken initiative to “bring-
ing back team fun” and has initiated monthly fun activities and topics to encourage all staff to participate. Each month, Taylor sends out a fun monthly activity topic for staff to participate in, started a Kudos shoutout box, started a book exchange, and sends out save the dates for outside of work activities too (which she organizes) that everyone is included to participate in. Below is an example of one of her emails.
As we know, patient care is improved when staff have better work satisfaction. Taylor has taken initiative to boost the teams’ morale in a critical time and the effects of this kindness and compassion are immeasurable. Taylor would never want to be called a Nursing Hero, though I believe that is precisely what makes her one.
Nominated by: Tamara Wegren ■ H

RNAO celebrates the expertise, resilience and dedication of nurses throughout the year. Nursing Week offers a unique chance to highlight our collective achievements and spotlight the significant contributions nurses make towards fostering health for all.
A most notable accomplishment is our leading role ensuring evidence-based, patient-centred care, which is essential for individual wellbeing and healthier systems. As we mark the 25th anniversary of RNAO’s Best Practice Guidelines (BPG) Program, we thank deeply the thousands of nurses and others who have participated in developing, implementing and evaluating RNAO BPGs. We praise the 150,000 champions who lead the way in our Best Practice Spotlight Organization® (BPSO®) Program, now in its 21st year with over 1,500 BPSOs at home and abroad.
On the policy front, increases in educational seats for RNs, NPs and RPNs, alongside RN prescribing and expansion of NP-led clinics are tremendous outcomes of RNAO’s steadfast advocacy and our collective mobilization to improve access to care for all. Nurses’ unwavering commitment and teamwork enhance the health of Ontarians and lay the groundwork for future nursing generations.
Success – individual and/or collective – often involves overcoming challenges within our health system and sometimes within ourselves. You each have crafted remarkable stories as you face these challenges. Together, we make progress and emerge stronger.
We salute all nurses and in particular our 51,650+ members. Know that RNAO will continue to move from strength to even greater strength, as we remain focused
on addressing RN and NP retention and recruitment, competitive compensation in all roles and sectors, harm reduction, the environmental crisis, and systemic racism and all forms of discrimination in nursing and in health care.
We wish every RN, NP, RPN and nursing student across Ontario a joyous Nursing Week.

 Dr. Doris Grinspun RN, BScN, MSN, PhD, LLD(hon), Dr(hc), DHC, DHC, FAAN, FCAN, O.ONT RNAO CEO
Dr. Doris Grinspun RN, BScN, MSN, PhD, LLD(hon), Dr(hc), DHC, DHC, FAAN, FCAN, O.ONT RNAO CEO
would like to nominate my colleagues as a nursing DUO for the nursing Hero award. I realize that the award is likely intended for an individual nurse, but this pair truly shows a level of exceptional family-centred care that can only be achieved through collaboration and partnership.
Lindsay and Jose are the Co-Leads of our Paediatric Oncology Clinic at Credit Valley Hospital. This clinic is a satellite site of the larger paediatric cancer programs at children’s hospitals in Ontario, such as SickKids or McMaster Children’s Hospital. When children are first diagnosed with cancer, they typically receive intensive treatment at the larger programs within children’s hospitals for weeks to months before their first visit to a






satellite POGO clinic. These satellite clinics enable families to receive care closer to home, but families often share how scary it is to come to a satellite clinic when they have built such a comfort level and trust with the larger site. Children’s hospitals are known for their expertise in paediatric care and families worry about how their care will change when they move to a community hospital setting. It is generally not a change in care that they look forward to during an already stressful journey of childhood cancer.







Enter Jose and Lindsay. It is not long before children and their families feel at home in our clinic because of the compassionate care, advanced skill, and expert knowledge that Jose and Lindsay provide on a daily basis. Families share how much they appreciate the calm environment and personalized care they receive at our clinic. Jose and Lindsay quickly build rapport with children, and their families know they can trust Jose and Lindsay to communicate with their children’s hospital cancer team to ensure seamless coordinated care. Truly, Jose and Lindsay are the experts in paediatric oncology at our hospital and they advocate for the unique needs of children and their families in the POGO clinic. They provide a calming presence that encourages children and teens to share their worries and feel heard during their treatment. They will adapt their care for each child’s preferences to help them feel safe and recognize their own courage during their journey. Jose and Lindsay support families during some of the darkest days imaginable for parents - offering comfort and compassion to build strength when parents need it the most. But they also bring joy and a light-heartedness to each day that can allow kids to just be kids, no matter their diagno-
sis. It is not uncommon to find Jose busting a dance move to celebrate a teen’s success during treatment or distract a child during a difficult procedure, or to see Lindsay enjoying some fresh tea and cupcakes that the children cook up in the pretend kitchen in our playroom. They embody the best of the nursing profession.
One of the many examples of the sentiments that our families share with us can be found below:
“Jose and Lindsay have made my daughter’s cancer journey brighter since the day we met them. After 2 months of the journey, their expertise and knowledge aided them to change one of Charlee’s least favourite part of chemo – The Flush! (yucky!)
Every day Charlee knew we were going to Credit Valley Hospital – or “Jose and Lindsay’s” was a happy day. We love you both Jose and Lindsay! Charlee’s mom, Charlotte (Charlee bear’s mom)
Please accept this nomination for the Nursing Hero DUO that we are privileged to work with at Credit Valley Hospital.
Nominated by: Emily Synnott ■ H












On National Nursing Week, we thank the nearly 4,500 nurses at Trillium Health Partners (THP). Your commitment to Changing Lives and Shaping the Future is inspiring. With compassion, courage, and excellence, you drive our patient-centered and quality-focused care.
Thank you for your vital role in redefining nursing and creating a new kind of healthcare for a healthier community.
Celebrating National Nursing Week: Changing Lives. Shaping Tomorrow May 6 – May 12, 2024
Visit us at thp.ca or donate at trilliumgiving.ca
Iwould like to nominate Ivana Matic Bacelic RPN on 2C general medicine at C-site. I have been working with Ivana for well over a decade and have been meaning to do this but always miss the deadline. I don’t even know where to begin.
Ivana is the type of nurse that I want to care for my loved ones. The countless times she has literally saved people’s lives is ridiculous! Even this week, she advocated for her pt to get a specific treatment. If she had not, that pt might not be here today. During the height of covid, we were a designated Covid unit. I remember so many shifts the nurses were short. There was one
shift in particular that I remember, we had 2 externs, and 2 nurses for the day shoft. 1 RN and 1 RPN. Ivana was the RPN on that day. Our patients were so sick. We had at least 5 pt’s on Airvo. We were running out of body bags on a daily basis. Moral was below rock bottom. The shift was seamless. You wouldn’t have thought we were short. Patients received amazing care. She continued to support staff professionally and personally. Lifting up our spirits. We would look to her to give us hope, that one day this would be over. I remember her saying “don’t worry, in 2 years this will all be better.” I personally held
Nursing Week is a special time to celebrate the amazing work of nurses worldwide. This year’s theme, “Changing lives. Shaping tomorrow,” truly speaks to the heart of what over 4,000 nurses do here at The Ottawa Hospital, and the nursing profession as a whole.
In 2023 alone, our nursing team made a tremendous impact on our patients and community, managing over 1.3 million patient visits and providing compassionate care in 1,188 beds across 61 units of varying clinical settings and specialties. Changing the lives of many.
Nurses are not only caregivers; they’re educators, researchers, mentors, leaders, advocates and much more. Their dedication to expanding their skills and expertise through education, professional development, research and innovation play a vital role in shaping the future of health care and the next generation of nurses.
Despite facing numerous ongoing challenges, nurses show unwavering dedication to providing exceptional patient care. A true testament to the strength of our nursing community.
As a nurse myself, I am so proud of our profession. On behalf of everyone at The Ottawa Hospital, I want to express our heartfelt gratitude to all nurses.
Happy Nursing Week!
Suzanne Madoreon to that, and I know a lot of other staff did as well.
She has brought in clothing for pt’s that don’t have any friends or family, or are homeless. She mentors junior staff without asking. She is a wealth of knowledge. She educates not only the nursing staff, but also allied and physicians. She’s the first one to show up when help is needed. Doesn’t hesitate when a code is called. She’s actually prepared before the code even begins. She just knows. She’s there ready with the cart, calling the doctors, prepping the team on what needs to be done as soon as that lever gets pulled. She definitely lives by the motto “everyone’s patient.” She will advocate for her patients, especially when they cannot. She’s not afraid to
speak to physicians and discuss their cases with them, getting the best possible outcome. She never expects recognition or praise. Her mentality is very much “this is my job; this is what I do.” Whenever she’s working, you feel that you can let your shoulders down, because you know if anything happens, she has your back. She does not get paid a fraction of her worth! The organization is so lucky to have her call THP her place of employment. I know that when the day comes that she leaves us here on 2C, the unit will feel a huge sense of loss. I know I’m not doing her justice with this e-mail. But I hope that she finally gets the recognition that is long overdue.
Nominated by: Mariza Saverino■ H








ngelita aka “Angie” is one of the respected charge nurses in Unit 3D specialize in Geriatric care of Glenrose Rehabilitation Hospital. With more than two decades of experience providing world-class quality nursing care, Angie was able to sharpen her skills, knowledge and critical thinking. With that confidence and expertise, it was easier for Angie to lead the group. In my own experience, Angie is well organized and has that clinical eye in leadership. She is able to get along with diverse and multi-cultural group of nursing staff in a way that the staff and patient work as a team. She is the go-to-person in trouble shooting of challenging situations like handling complaints and conflicts. Moreover, she also advocates the safety of the staff and patients in the workplace by ensuring that the needs
and concerns of the patients and staff are met. There was an incident where she suspected the patient was a victim of abuse from his wife. Angie immediately raised her concerns to the attending physician and social worker and as a result measures were taken to ensure the patient’s safety. She provides solutions within her scope as the charge nurse to issues that need her immediate attention and relays further concerns to the patient care manager and unit manager. Furthermore, she is also an active volunteer in the community. She served as altar server coordinator at St. Charles Parish since 2010, and at her kids school and their
basketball community. In addition, she is also the President of a non-profit cultural organization called Pinoy Roots Rondolla which is a group of kids that plays Philippine indigenous instruments.
Nurses are an integral part of our healthcare team, playing a vital role in ensuring the well-being of patients. They are often the initial point of contact for patients and their families and display unwavering commitment to providing the highest quality care to our patients.
At Humber River Health, we are grateful for our resilient nurses who embody our values of compassion, professionalism, and respect in many ways. Our nurses go beyond to demonstrate kindness and empathy, and ensure patients are treated with dignity and respect in receiving the best possible care and outcomes.
Our nurses remain up-to-date with medical trends and innovations to better collaborate with physicians and other healthcare professionals in providing in-depth knowledge and clinical expertise. They adhere to ethical and professional standards to continuously act in the best interests of patients and families.
We recognize the daily, high-quality care our nurses provide to assist with care and recovery journeys. We appreciate the outstanding contributions they have on improving the health of our diverse communities. We are proud to have such dedicated, compassionate, and hardworking individuals on our clinical teams. To all our nurses at Humber River Health, thank you for the essential role you play in our health and our community.
Angie fosters a collaborative approach in providing care and is one of the pioneers at Glenrose Rehabilitation Hospital.
First, Angie, as a charge nurse attends the rapid rounds where most of the heath care team are present to discuss the treatment plan of the patients. The team is composed of the main attending physician, pharmacist, social worker, nurse, physical therapist, and occupational therapist and this treatment plan is further discussed with the patient during their rounds. Second, Angie advocates for the need of having family conference as part of the treatment plan for the patient. She ensures that patient and family are able to address their needs and concerns as preparation for their discharge to home and going back to the community. Lastly, Angie initiates care huddles before, during and after the shift. With these, any patient concerns and needs are addressed.
Angie is a certified CIHI evaluator. She is also one of the Connect Care champions and a Super users when Connect Care was implemented. She attends workshops, training and seminars that improve the care for the
geriatric patient population. She reads nursing journals and articles that highlight patient safety.
Angie advocates that each member of the health care team perform at their optimal scope of practice. She reiterates that when we provide care it should be the best, effective, and most quality care for the geriatric patients. She highlights the importance of continuing to have the rapid rounds and family conference with the patients, and doing care huddles with the nursing staff so that the needs and concerns of the patient is met.
In addition, when she notices that a staff member is struggling with a certain task, Angie takes time to talk to them and assist them. She is like an extra clinical educator who reviews the procedures or tasks with the staff by checking it under the policies and procedures set by the company. She also provides tips and information for staff to complete further readings like nursing journals utilizing the e-learning modules provided by vendors.
In summary, Angie is perfect for the Award. A born leader, down-to-earth, highly qualified, professional and competent individual who is a recipient of recommendations from patients, families, and management. She was nominated twice for the Daisy Award. Received an award last year 2023 in CLPNA with the Interprofessional Development Award. ■ H

aria came into Complex Continuing Care (CCC) full of energy and enthusiasm and just kept going and going, much like a famous “battery bunny”. Armed with over 25 years of experience and contributions in neuroscience nursing care on the acute side of the hospital, Maria dedicated herself to a new role as Advanced Practice Nurse Educator (APNE) on the rehab/CCC side of the house. She very quickly engaged leadership and pointof-care nurses to identify practice gaps
and opportunities for learning. For example, in 2018, no nurses in CCC were able to initiate or manage IV’s; this situation, of course, limited the capacity of CCC to accept certain patients.
Maria very quickly identified this gap and engaged with key internal and external stakeholders to develop the educational and training resources specifically tailored for nurses in CCC. As the most senior Nurse Educator in CCC, Maria has been instrumental in
providing leadership and insight to UHN-wide Vascular Access training for nurses, and has been working in collaboration and partnership with her professional practice colleagues to develop and implement educational materials to support local on-boarding of nursing staff and to create the conditions where nurses can work to full scope. Maria’s leadership has also seen the growth of our CCC Education Simulation resources--where nurses and allied health members alike can practice different interventions or Code Blue resuscitation techniques on life-like mannequins in a simulated patient room. A staff nurse said this about Maria: “I was encouraged to continue my education in nursing because of Maria...I obtained my baccalaureate degree and am now finishing my Masters degree in Nursing...every nurse should be as lucky as I to have someone like Maria to show them the way...”
Maria has also been a leader in introducing “gamification” in the education of nurses. Maria recognized early that digital citizens and tech-savvy nursing students are among us and that we need to educate using different modalities from those that have been used in the past--Maria believed the nursing workforce was are ready for gaming as part of their ongoing educational needs. Maria, with the help of her husband, designed a “Describe
that Drug” spinning wheel to teach nurses pharmacology. When a nurse spins the wheel, he/she needs to be prepared to describe the class of drug, its actions and side-effects when the wheel’s pointer stops at a particular medication. This wheel has also been used during mock Code Blue training, where Maria reviews with staff the commonly used drugs in emergency situations.
Through all of her work, aside from nursing staff, Maria has never lost sight of the most important beneficiaries of her education--the patients in CCC. Some of the most vulnerable patients at UHN are found in CCC. Most patients are older, have multiple co-morbidities that require complex treatment regimes. Some patients are palliative, some have cognitive impairment and unpredictable behaviour. Maria has worked tirelessly to ensure staff understand patient needs and that the patients receive the best care possible. She has also been a champion for revising hospital policies so that these incorporate the needs (and realities) of CCC patients and reduce health inequities.
Maria has been a key driver in changing the (sometimes negative) views of others about complex continuing care, decreasing stigma, encouraging more nurses to the field, and, ultimately, enhancing the patient experience. ■ H
Ihave worked with many incredible nurses over my career, but would like to especially nominate one of the most passionate, dedicated, and hard working Nurses that I know.
Katia (Kat) Lietz and I worked on PCU 54 together for several years. She is one of the AHN’s and has an incredible way with patients and with other staff. Kat will stay later, pick up extra, and do whatever needs to be done to ensure the patients needs are met, even sometimes to her own detriment. People do need to sleep, after all.
Kat is an inspiration to her colleagues, taking time to get to know each patient and going the extra mile with many patients on the unit at any given time. Not only does she ensure that her patients are cared for from a
KAT IS AN INSPIRATION TO HER COLLEAGUES, TAKING TIME TO GET TO KNOW EACH PATIENT AND GOING THE EXTRA MILE WITH MANY PATIENTS ON THE UNIT AT ANY GIVEN TIME.
nursing standpoint, she helps them to feel safe and taken care of emotionally as well. I have seen patients seek her out for hugs, and heard her interacting with patients and their families to offer comfort. Despite the incredible amount of work she has to take care of as the AHN, she always takes time to ensure that her patients are cared for, and that the unit runs as smoothly as possible.
During the COVID-19 Pandemic, Kat acted as Nurse, Porter, Care
Scarborough Health Network (SHN) is proud to celebrate all nurses and the pivotal roles they play in the healthcare journey of our patients.
Our nurses are the cornerstone of patient safety and quality, their commitment driving them to excel each day. They are the champions of care, the advocates for patients, and the leaders in our quest for healthcare excellence.
Thank you, SHN nurses, for your tireless efforts and for leading the charge as we forge ahead in shaping the future of care for our Scarborough community.
support person, patient and family advocate, and so much more. Kat proves that a Nurse is not only the functions that a Nurse needs to do during any given shift, but so much more. While we suffered many losses during the Pandemic, Kat maintained excellence in her nursing role, as well as looking after her three adult children. A single parent too, due to the loss of her husband, Kat is what people had in mind when they deter-

mined what a nurse is. She is caring, compassionate, driven, an example to everyone on the unit regardless of profession, and one of my hero’s. Once the other professionals go home at the end of a business day, Kat and the other nurses remain. Where some nurses will do their jobs and only that, Kat takes assignments, is a consistent point of contact for anyone who needs patient information, and a consummate advocate for her patients.
Nominated by: Ryan Chopin BSW, RSW, Credential Trainer ■ H












t is with immense pleasure and privilege that I submit this nomination in support of Allan Lee.
Allan has been Registered Nurse (RN) in the Emergency Department at Mackenzie Health’s Richmond Hill Hospital for 16 years.
Our journey as new ED nurses started together. At times during our schooling, we were a bit competitive, but we were always the biggest support for each other. We have laughed, cried, yelled, cried some more, but mostly laughed. I am honored to have Allan as part of our team, I am privileged to be his manager and everyday he amazes me”
HMAllan is one of the most caring nurses and individuals that I have ever met. He cares with his entire heart, whether he has just met you, or known you his entire life. Anyone who has met Allan always remembers him. They may notice him because let’s face it he is bit loud, but they remember for the care, and compassion, he demonstrates whether directly involved in the care or supporting the team.
honourable mention
Allan is a leader in the department, and now in his older years, refers to himself as father, or at times grandfather. The ED team is truly his family, and there is nothing he will not do for his team. He will triage the patient, jump into the code, com-

We recognize and celebrate our nurses who go above and beyond to provide excellent mental health care and are #RisingUp to make a meaningful difference in the lives of our patients and each other. Our nurses have the right attitude and take action to anticipate and advocate for the needs of others. Our Nurses Care
ALLAN IS AN ASSET TO THE MACKENZIE HEALTH TEAM AND DESERVES THIS NOMINATION, AND SO MUCH MORE, HE IS THE LEADER OF THE FUTURE GENERATIONS OF NURSES.
plete a round of compressions, grab every piece of equipment you need, run the code, support the family, and debrief with the staff afterwards. He is the department Superman.
Late last year the Emergency Department in Richmond Hill received an unprecedented number of critical pediatric, which did not end successfully despite the efforts of the ED. Allan was involved in almost every code, and his priority was firstly the patient and the family, but it was his actions when it was over that were remarkable. Allan ensured a detailed debrief occurred, connected with the staff involved personally, and checked on them multiple times over the next couple of weeks. Having children himself, I knew he was
hurting, but he stayed strong for everyone else. Approximately, one month later, the senior leadership at Mackenzie met with the ED team to show their support. When asked if he would say a few words at the meeting, he went above and beyond. On his day off, he came in, and gave his speech, acknowledging everyone involved, how amazing the keep is, and there was not a dry eye in the room. But of course, it would not be Allan, if there were not a few jokes, a couple swear words, and an enormous hug to Altaf.
Allan is an asset to the Mackenzie Health team and deserves this nomination, and so much more, he is the leader of the future generations of nurses. ■ H
am writing to wholeheartedly nominate Janice Lin for the Hospital News Nursing Hero Award. Janice, through her dedication and compassionate care, has played a pivotal role in the recovery journey of my wife, Linda, at the Lyndhurst Centre.
Linda’s path to recovery began after a terrifying fall at home, which resulted in multiple fractures, including a severe injury to her spine. After undergoing cervical decompression surgery at Sunnybrook Hospital, Linda faced a daunting road to recovery. It was during her subsequent rehabilitation at Lyndhurst that we had the good fortune to meet Janice.
From the outset, Janice distinguished herself not just as a skilled nurse but as hope and warmth for Linda and me. Her kindness, ever-present




smile, and readiness to engage deeply and meaningfully with us were instrumental in transforming the rehabilitation centre from a place of clinical recovery to one of warmth and healing.
Janice’s approach to care is marked by an exceptional blend of professionalism and personal touch. She always made herself available to answer our questions, no matter how small or complex, with patience and clarity. This not only helped Linda in her physical recovery but also provided us with much-needed reassurance and comfort during a tumultuous period in our lives.
bly welcomed and cared for throughout her stay. Her ability to create a nurturing environment, coupled with her professional demeanor, made a significant difference in Linda’s overall well-being and outlook on her recovery process.
her patients, her ability to connect on a human level, and her unwavering commitment to excellence in care are qualities that deserve the highest recognition.
Perhaps what stood out most was how Janice made Linda feel incredi-
For these reasons and many more, I believe Janice embodies the essence of a Nursing Hero. Her dedication to
We are profoundly thankful for Janice’s presence in our lives during such a critical time. It is with great admiration and gratitude that I nominate her for the Nursing Hero Award, confident that her contributions to nursing and patient care are truly exemplary.
Sincerely,David Kennedy and Linda Kennedy. ■ H
would like to nominate Nurse Karen Ganchua for THP Nursing Hero. My husband, Samson Andres is a peritoneal dialysis patient. We’ve been serviced by different nurses either in kidney clinic and hospital. They are all helpful. But one particular nurse, her named is Karen Ganchua. She had shown a very remarkable assistance and support to my family over and beyond of what is expected of her to do as a nurse. Karen become our contact nurse for a couple of years now . Karen never change. Consistently providing guidance and emotional support to my family. If I call the clinic and she is not available someone is usually ready to assist us. Then Karen later always give us a call to check that everything was done to our satisfaction for our peace of mind. Karen always give an advice on what to do.
In a couple of times that my husband was admitted in the hospital. No one can really explain the delayed dialysis or no dialysis at all for 24 hours. This

causes emotional stress on me about the side effect on my husbands health of not having dialysis on the proper time. To lessen my fear and worry, I

The Bridging Educational Grant in Nursing (BEGIN) program provides eligible PSWs and RPNs with up to $10,000 per year in tuition reimbursements to grow their careers.

New enrollees also now have the opportunity to gain experience in one of four priority sectors: Hospitals, Primary Care, Long-Term Care or Home and Community Care.

always call Karen to ask questions. She always tried to find an effort to contact me and explained to me the process or even outside her work hours on her way home she will pass by the hospital or in our house to give us some moral support , comfort and ease our mental tension. Karen’s kind gesture means a lot specially to us being seniors losing patience. Sitting in the waiting room area, same comments we received from other patients, about Karen’s kindness and special support to dialysis patients. Karen is so patient, understand the patients feeling. Her guidance and emotional support outside of her line of work is very much appreciated. All nurses deserve a recognition. But I nominate Karen Ganchua as the THP nursing hero.
Nominated by Marlyn Andres ■ H

Spaces are limited. Apply today.
Learn more at begin.werpn.com
















Thank you to the 60,000 RPNs across Ontario. Your expertise, experience, and compassion keep our communities healthy and safe – despite the many challenges faced from day-to-day.
Your care makes a difference – to patients, to families, to the healthcare system – and we are proud to advocate for you and stand alongside you in support.
The Registered Practical Nurses Association of Ontario (WeRPN) thanks all RPNs for making us a healthier province and a stronger profession. Together, we will continue championing improvements to our healthcare system and inspire change.
To learn more, please visit werpn.com.

Guided by expert hands, the wire moves through the patient’s blood vessels inch-by-inch. The physician’s eyes follow its procession on the screen in front of him as he gently works the wire forward. Activity in the room is hushed; the only consistent sound is the repeated ‘beep-beepbeep’ of the monitoring system as it announces the patient’s steady pulse.
Once in place, the wire will be used to insert a tiny tube – called a micro-catheter – as close as possible to a cancerous tumour located in the patient’s liver. The micro-catheter will then deliver a precision dose of radiation to destroy that tumour. The treatment is called radioembolization and this is the first time it’s being performed at St. Michael’s Hospital.
Getting the wire to its destination is like navigating a maze. The images on the screen are X-rays taken in real-time that act as a map. Though Dr. Andrew Brown – who is performing the radioembolization – knows where the wire needs to go, getting it there is still a delicate process with many opportunities for wrong turns and setbacks.
The natural flow of blood through the vessels can easily carry the wire in the wrong direction. Blood vessels branch off from one another like the root system of a tree, getting narrower and narrower. Positioning the wire in the right branch can take anywhere from two to four hours.
The reward for reaching the target is well worth the effort: an opportunity to cure the patient – Dave McManus – of cancer.
Born and raised in Toronto, McManus worked most of his career as a Fedex delivery person. Now six years into retirement, family and music figure most prominently in his life. He lives with his wife, Cathy, in the Junction neighbourhood and they have an adult daughter named Sarah. He also plays bass guitar in blues bands around town a couple of nights a week.
McManus has experienced cancer once before. The first time, he received surgical treatment at St. Jo-

seph’s Health Centre, a site of Unity Health Toronto. This time, his oncologist discovered a tumour in his liver when he received a CT scan as part of an annual check-up.
When he first learned about the liver tumour he had a sense of resolve.
“I’d been through cancer once already and through good fortune and good management, I came through okay,” says McManus. “So I thought, ‘Okay, here we go. We’ll just have to deal with this.’”
His main focus has been on his loved ones and how they’re coping with his diagnosis.
“What I’m looking forward to after the treatment is allowing my family some peace of mind because they’re all wrapped up in this whole thing emotionally,” he explains. “If it’s successful, then it will be a good release.”
The care he provides to his patients is personal for Brown.
He was in the last year of his residency, preparing for exams when he found out that his mother had metastatic gastric cancer, which meant that cancer originating in her stomach had spread to other parts of her body. She received surgery and palliative care at St. Michael’s.
That experience was Brown’s first time “on the other side of the bed,” as he describes it, and he will always be grateful for the compassion and support that his mother and his family received.

Dr. Andrew Brown looks intently at the screen while performing Dave McManus’ radioembolization treatment.
Radioembolization is one example of emerging cancer treatments that provide a more targeted approach than traditional therapies. External beam radiation – the most common form of radiation therapy – focuses beams of radiation at cancerous tumours from outside of the body inward, hitting and hurting any healthy tissue in their path.
In contrast, radioembolization releases tiny beads that contain a radioactive isotope called Yttrium-90 (or Y-90) to the blood vessels directly surrounding a liver tumour. Radiation from the beads only travels millimeters – directly targeting the cancer.
The side effects are usually minor –especially when you compare them to the weeks of pain and fatigue that can accompany external beam radiation. Patients go home the same day after treatment and might experience nausea or fatigue in the days after. Some will experience an on-and-off fever in the following weeks.
Radioembolization can only be used to treat certain kinds of liver cancer.
“Patient selection is very important. You really want to be treating people that have cancer confined to one place – in this case, their liver – and who have good liver function,” says Brown. “For folks who are well selected, you’re looking at a significant improvement in their length and quality of life.”
Brown is an interventional radiologist and radioembolization is a form of interventional radiology. Intervention-
al radiologists are physicians who use imaging tools that typically help with making diagnoses – such as ultrasounds, CT scans and X-rays – to provide image-guided, minimally-invasive care that will treat an injury, illness or disease.
McManus is awake and aware for the duration of his procedure, with a local anesthetic to help manage his pain. He’s a model patient, following every request from the care team – to put his hands above his head or hold his breath for the cone beam CT scan – without complaint. Cone beam CT scanners use less radiation and focus on a smaller area than tradition CT scanners.
There are four core members on the care team. Brown is the lead interventional radiologist. Throughout the hours-long procedure – he remains steady and calm. Michele Orridge, a nurse, assists in the procedure and helps to ensure McManus is as comfortable as possible, checking in on him often.
Heather Armstrong, a medical radiation technologist, operates the imaging devices in the angiography suite – the room where the procedure is taking place – with a confidence that reveals her depth of experience. Dr. Steven Cooper, a physician, assists Brown. This procedure is part of his medical fellowship as he trains in the specialty of interventional radiology. At last, a breakthrough. After hours of careful navigation, Brown has placed the micro-catheter for the radiation treatment. The room springs into action.
A call is made to the Nuclear Medicine department to deliver the dose of radiation that has been specially formulated for McManus’ treatment. Nuclear medicine is a medical imaging specialty that uses radioactive materials to diagnose and treat disease. The tiny radioactive beads have been stored in the Nuclear Medicine department with safety protocols in place to prevent a radiation leak. Now similar safety protocols will be enacted in the angiography suite.
The beads arrive in a small, grey, lead-lined canister that is handled with the utmost care. While it looks unassuming, within it lies radiation ex-
posure equivalent to 1.2 million chest X-rays or, in this case, enough radiation to destroy a cancer tumour.
The care team must follow a methodical process to ensure all of the beads safely reach their target. Special instruments – including tubes, clamps and shields – control the delivery of the beads and protect McManus and the care team from unintended radiation exposure. Every item that comes in contact with the beads must be discarded as potentially radioactive waste.
After approximately three minutes, Brown has completed administering the full dose of radiation.
Two months later, McManus returns to St. Michael’s for a follow-up CT imaging appointment. A couple days after, he gets a call from Brown.
“Bright and early at 8 o’clock Dr. Brown called to give me an update. He’s very upbeat,” recounts McManus. “I was very heartened by what Dr. Brown had to say. He’s got a very reassuring manner about him.”
The procedure was a success.
“There’s a big hole in the tumour, which means the centre is dying. There’s also some inflammation around it, which is exactly what we want to see,” Brown describes the imaging results. “The rest of the liver looks good too, which means we’re moving in the right direction.”
As with most cancer treatments, McManus will continue to be monitored with imaging scheduled in another three months.
That morning, McManus’ wife and daughter were getting ready for work but hung back at the door with their coats on for the conversation with Brown to finish so they could hear the news.
“It’s always good to share this kind of news and help patients like Dave,” says Brown. “I’m grateful that our team was able to get this done and excited that others like him will be able to benefit.”
As of right now, St. Michael’s is one of only four hospitals in Ontario that provide this treatment. Across Canada, it’s only offered in a few major centres. Part the motivation for bringing radioembolization to St. Michael’s is to ensure more patients in Ontario will have access.
“It’s a burgeoning treatment,” explains Brown. “These types of minimally invasive and targeted procedures really are the future of cancer therapy.” ■ H


In 2021, during the peak of the third wave of the COVID-19 pandemic, the health-care system’s capacity was stretched and hospitals across Canada relied on each other to share resources and provide care. To help in decision-making, team members from London Health Sciences Centre (LHSC), Ivey Business School and King’s University College developed a simulation model to help LHSC leaders make decisions on resources and capacity to ensure the hospital was ready to accept inbound patient transfers from outside the hospital’s catchment area, including Toronto and Manitoba.
The pandemic required collaboration across the health-care system to ensure capacity was balanced across hospitals while maintaining the ability to care for non-COVID patients. In addition to strategies like having field hospitals at the ready, patient transfers between hospitals were critical to managing the pandemic response. To enable the most efficient use of resources during a crucial time, LHSC leaders needed a solution.
Building on previous partnership work, hospital leadership saw an opportunity to work with a team of researchers from Ivey Business School and King’s University College. The collaboration resulted in the development of a Monte Carlo* simulation tool designed to predict the likelihood of whether the hospital would be over capacity in responding to several COVID-19 related impacts, including changes in hospital admission rates, managing the impact of COVID-19 outbreaks and balancing the COVID-19 response with planned hospital activity.
The tool, created in Excel so that any hospital could use it, helped forecast the usage of Critical Care and Medicine Unit beds over a one-week period based on data from the previous week, including admission rate and average length-of-stay for both COVID-19 and non-COVID-19 patients. The tool also factored in assumptions about future arrivals of patients from outside the region to predict capacity needs and whether additional beds dedicated solely for COVID-19 patients would be required.
“The tool allowed us to maintain optimal care for all LHSC units by
making decisions grounded in real-time data,” shared Tim Rice, Senior Director, Victoria Hospital at LHSC.
“By inputting this data into the model, the impact to overall hospital bed capacity was better understood and provided LHSC leaders the information they needed to make objective decisions, including the resources required to meet the ongoing demands of the pandemic.”
When Manitoba hospitals required support from LHSC at a time where they were already supporting both the London region and requests from Toronto hospitals, the team was prepared and confident in making decisions on how many patients LHSC had the capacity to accept from other hospitals and how to most effectively use hospital resources.
“The tool serves as a future resource for emergency preparedness and new iterations of the model are in development to help with ongoing capacity planning, ” said Rice. “It is our hope that the legacy of this partnership will live on in the future work it supports.”
This work was recently published in BMC Public Health. ■ H
From left to right: Tim Rice, Senior Director, Victoria Hospital at London Health Science Centre; Mehmet A. Begen, Associate Professor, Management Science; Gregory S. Zaric, Professor, Management Science; Felipe F. Rodrigues, Assistant Professor The research team included Mehmet A. Begen, Associate Professor, Management Science, Ivey Business School at Western University; Felipe F. Rodrigues, Assistant Professor, Operations Management and Analytics at King’s University College at Western University; Tim Rice, Senior Director, Victoria Hospital at London Health Science Centre; and Gregory S. Zaric, Professor, Management Science, Ivey Business School at Western University. *What Is Monte Carlo Simulation? | IBMIt has been two months since Bojan, a 51-year-old man, attended the Minimally Invasive Cardiac Surgery (MICS) Clinic at St. Michael’s Hospital. After experiencing two major open-heart surgeries in the past, Bojan was offered an alternative pathway of care by Dr. Gianluigi Bisleri that uses a less invasive surgical approach to reduce trauma and return patients to their regular lives faster.
The Research Institute of McGill University Health Centre (RI-MUHC) has enrolled this week the first patients to take part in an early-stage, multi-centre clinical trial of Actinium-225, a radioactive isotope used as a treatment for metastatic prostate cancer. The RI-MUHC is proud to be selected as the first site worldwide to launch this new clinical trial, which introduces a promising new therapy in precision medicine for patients who have exhausted all other options in the treatment of their disease.
The third leading cause of cancer-related-death in men, prostate cancer will affect approximately 1 in 8 Canadian men during their lifetime and cause the death of one in 30, according to the Canadian Cancer Society.
Led at the RI-MUHC by Dr. Ramy Saleh, Medical Oncologist at the MUHC’s Cedars Cancer Centre and Medical Director, Oncology, at the Centre for Innovative Medicine (CIM) at the RI-MUHC, the study will evaluate the safety (i.e. the drug’s ability to act without adverse effects) and tolerability (i.e. the subject’s ability to withstand
Bojan had previously undergone surgery to fix a hole in his heart –known as ventricular septal defect.
Unfortunately, in 2017 he also had to undergo an emergency surgery due to a tear in his aorta, which required another invasive heart operation. To his surprise, last year he was found to have a leaky mitral valve, which would have required him to undergo a third cardiac surgery through the front of his chest. Another such surgery
brought up significant concerns about the associated risks, and Bojan was obviously concerned about how well he could recover from a third open-heart operation.
Bisleri, director of the Minimally Invasive Cardiac Surgery Program at St. Michael’s Hospital, was able to successfully repair the mitral valve by using a minimally invasive approach through a small (less than 2 inches) incision between the ribs. This approach
avoided entering the chest from the front and cutting the breastbone again for the third time. The procedure was extremely successful, allowing Bojan to return home only four days after his surgery.
With conventional open-heart surgery, patients usually stay longer in hospital and require prolonged time to recover and return to their normal daily activities, Bisleri says. However, with the innovation of minimally inva-
adverse effects) of Actinium-225, which works by targeting the prostate-specific membrane antigen (PSMA).
PSMA, which is found in more than 80 per cent of patients with metastatic prostate cancer, is highly expressed in prostate tumoral cells, but is very little present in the rest of the body. Actinium-225 binds to PSMA receptors, finds the cancer cells and emits radiation to kill them by breaking their DNA strands. A potential advantage of this targeted mode of action is the sparing of healthy organs.
“We are very excited to be testing Actinium-225 and to be the first centre in the world to start this clinical trial,” says Dr. Saleh. “It’s a great satisfaction for our team because it’s the result of our sustained efforts to bring the latest therapeutic advances to our patients.”
The experimental treatment, developed by the US company POINT Biopharma, will be administered by intravenous injection to 50 patients with metastatic castration-resistant (mCRPC) or biochemically recurrent (BCR) prostate cancer, for whom standard of care treatments have failed. Different doses will be tested and pa-
tients will be followed for five years to monitor any side effects.
In addition to assessing the safety of the drug for patients, the study will monitor how the drug interacts with tumours and healthy organs, find out if it is well tolerated, and determine the right dose that could be used in future studies.
“Other clinical trials have shown that similar treatment with drugs that target PSMA can reduce prostate cancer tumour burden and potentially improve prognosis. So, although we don’t know if the drug we’re studying will improve the health of our patients, we see this trial as our best hope,” adds Dr. Saleh, who is also Medical Director of the Phase 1 Research Unit at the CIM, Investigator in the Cancer Research Program at the RI-MUHC and Assistant Professor in the Gerald Bronfman Department of Oncology at McGill University.
Research is essential to improve cancer treatments and survival rates. Phase 1 clinical trials are a critical part
of research, because they can determine whether to continue or stop development of a new drug.
Established in 2018, the Phase 1 Research Unit at the CIM is dedicated to providing high-quality care to its cancer patients while supporting the drug development process. One of the distinguishing elements of the unit is its state-of-the-art facilities and equipment, which allow for precise and efficient study conduct. In addition, the unit often works with a multidisciplinary team of experts to ensure comprehensive and robust clinical trial designs.
“This world first confirms that the RI-MUHC, by fostering collaboration between its researchers and industry experts, has established a leadership position in Canada’s clinical trials ecosystem. The Centre for Innovative Medicine not only brings the latest experimental therapies to patients, but also attracts the most innovative pharmaceutical companies, both nationally and internationally, at every stage of clinical trials,” says Dr. Louise Pilote, Director (interim) of the CIM and Deputy Director of the RI-MUHC. ■ H
sive surgery, patients are going home in only a few days and most importantly, they can recuperate much faster and easier.
“It’s notable how fast Bojan was able to go home and return to his usual activities, as it was his third operation. Patients undergoing conventional surgery typically take weeks, sometimes months, to fully recover,” Bisleri said, adding that he is very pleased with the outcome.
“The surgery was extremely complex and challenging, but it really shows how far we have come with our minimally invasive cardiac surgery program at St. Michael’s Hospital.”
Bojan said that a few days after surgery he was completely mobile. “The recovery was not as bad as the past. Very different,” he said.
Bisleri says minimally invasive cardiac surgery is still a relatively new concept in Canada. Not many patients are aware of the alternative care pathways that are available unless they do

their own research or are referred like Bojan.
It was Bojan’s cardiologist, Dr. Marc Allard from William Osler Health Sys-
tem, who recommended he see Bisleri at St. Michael’s Hospital.
“St. Michael’s Hospital has established itself as a leading centre in Canada for innovative and less invasive techniques for managing individuals with valvular heart disease,” Allard said.
“Recognizing this, our local program has developed a strong link with the St. Michael’s team so that our patients can access and benefit from these procedures and surgeries. In this particular case, I was really concerned about putting Bojan through a third invasive and complex heart surgery, and so it was great that we were able to refer him to Dr. Bisleri for a less invasive approach.”
Bojan said that he considered the option of minimally invasive surgery, but thought it was always something that was just too far out of reach for him.
“I was very optimistic and hoped it was going to happen,” Bojan said. “I truly hope it can be offered to more people. Day and night from other experiences. That is not to diminish the incredible life-saving procedures performed by surgeons everyday, because they are great too and saved my life. This experience was just so different.” ■ H





















 John Schonewille
John Schonewille
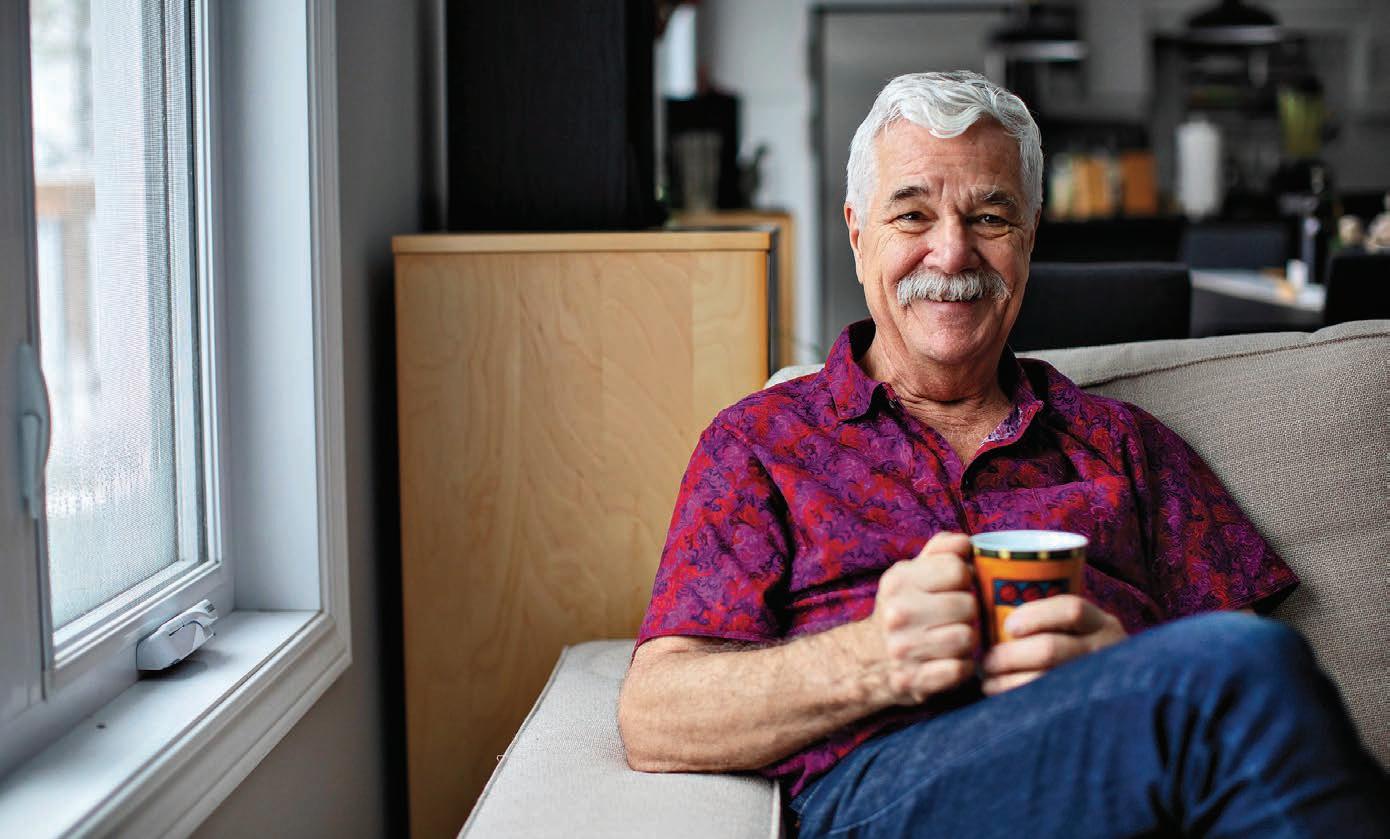
After a year of living with a tube that delivered food directly to his stomach, John Schonewille, then 66, had begun to despair that he might never be able to enjoy the everyday pleasure of eating again. Robbed of his ability to swallow by late complications of a stroke, Schonewille had faithfully carried out rehabilitation exercises prescribed by a speech-language pathologist (SLP), but when he tried eating again, food particles ended up in his lungs, causing pneumonia. Faced with the prospect of remaining permanently dependent on a feeding tube, “my life had no hope,” he recalls. Schonewille, who now lives in Haliburton, is among the estimated 10 to
13 per cent of Canadians over age 45 with swallowing difficulties, known medically as dysphagia. The process of swallowing requires a complex combination of nerves, muscles and parts of the brain to work together. When just one element doesn’t function properly – due to anything from a stroke to cancer to multiple sclerosis – a person with dysphagia might choke on foods and liquids, and in some cases, might even be unable to swallow their own saliva.
Desperate, Schonewille’s husband, Harry Lewis, reached out to their SLP, Susan Watt, who recommended they see Prof. Catriona Steele, a senior scientist and Director of the Swallowing Rehabilitation Research Laboratory at
UHN’s KITE Research Institute, who is also an SLP. According to Prof. Steele, Schonewille’s situation isn’t unique.
“The unfortunate thing is that there is very little therapy available for people with swallowing impairment in Ontario, but really, anywhere,” she notes. “And we don’t have a lot of good data to say which therapies work and which don’t work.”
With repeated testing, Prof. Steele finally discovered the ring-shaped muscle that’s supposed to relax when food or liquid approaches was staying stubbornly closed. Only by turning his head just the right way and doing a maneuver called an “effortful swallow” could Schonewille make the muscle open, and at first only briefly before he tired.
In recent years, Prof. Steele has quietly transformed the assessment and treatment of swallowing disorders. Her interest in the field was sparked while at her first job as the only SLP for 600 residents at Baycrest’s Home for the Aged an academic health sciences centre for older adults in north Toronto, between 1991 and 1994. Swallowing problems were common among the aging population there, as older people are more likely to develop the condition, and she saw the enormous impact not being able to eat or drink normally could have on people’s lives.
“Food and drink are central to the way that we live our lives,” she ex-
plains. “I can’t think of a rite of passage that doesn’t involve eating together or drinking together.”
During this same period, Prof. Steele also became frustrated with the limited tools for assessing and treating dysphagia.
Take the test that SLPs use to try and pinpoint exactly what part of the complex swallowing process has gone awry. Using fluoroscopy – a sort of X-ray movie – an SLP monitors the patient as they swallow to determine the source of their difficulty. The problem with fluoroscopy is that it’s up to an individual SLP to interpret what they see, making test results subjective, rather than objective.
One focus of Prof. Steele’s research has been to create an objective grading system for this fluoroscopy test. With nine key events to look for
Wendy Haaf is a writer.



during swallowing, any SLP can use strategies like measuring the position of certain structures in the throat, and the time between each of these events, to arrive at the same score as another SLP. The goal, she notes, is to provide results similar to a blood test, with low, high and normal ranges for swallowing.
Prof. Steele and her team are well on their way to success. “We have developed reference ranges for healthy adults aged 20 to 82, and our current work is collecting a whole new sample to validate those references,” she says.
Prof. Steele also uses this objective system to map out how specific interventions affect those results. “For example, if we ask someone to swallow with their head tucked down as opposed to in a normal position, how does that change the numbers?” she says.
Similarly, she’s looking at what happens when liquids are thickened to one of four standardized consistencies, or when food is chopped or mashed to
different degrees – and which is best for each swallowing problem. “We’re mapping swallowing right across the continuum of texture,” she explains.
Prof. Steele hopes to create a more tailored approach to modifying foods and beverages, so they’re suited for an individual patient’s needs. Until now, “we had one tool in our kits, which was to thicken everybody’s liquids and purée their foods. It’s still true that most clinicians jump very easily to thickening and puréeing. It’s a very blunt instrument,” she says. “I would love to be able to offer people with swallowing impairment more options in their diets, but also offer them treatments that would get them back to eating more variety and enjoying food and liquid like most of us do.” For example, further research using Prof. Steele’s scoring method could improve treatments by measuring the effective-
ness of different exercises for a given swallowing problem.
That said, it is still possible to prepare puréed foods in such a way that they’re visually appealing and tasty. For example, Prof. Steele and her team once worked hand-in-hand with the chef at a foodie patient’s favourite restaurant so she could enjoy a family birthday dinner before she eventually regained her ability to eat regular foods. “The chef prepared a gorgeous meal that was all texture modified. She thoroughly enjoyed it – we all thoroughly enjoyed it,” she says.
Working with Prof. Steele, Schonewille has gradually regained sufficient swallowing ability to eat foods prepared to a certain consistency, and he’s continuing to improve. He can now enjoy such dishes as soups, ground meats and his favourite lasagna brimming with finely chopped vegetables.
“The types of foods are starting to expand, because the more I eat, the better I can eat,” he says. “That’s all due to Dr. Steele.” ■ H































aregivers are the invisible backbone of our healthcare systems. They contribute three times as much unpaid care for every hour of care given in the formal healthcare system. Most Canadians will give or receive care: one in four Canadians over the age of 15 is a caregiver, with as many as 5.2 million working people aged 19 to 70 taking care of a loved one for over 30 hours a week while working full-time.
Whether they are tending to an aging parent, supporting a family member with a chronic illness, or caring for a loved one with a disability, caregivers do the unpaid work that makes our system run. Canada’s caregivers contribute an estimated 5.7 billion hours of care per year; an economic value of $97.1 billion. Not surprisingly, the demands of caregiving often take a toll on physical, emotional, and mental health, and many caregivers find themselves neglecting their own wellbeing as they prioritize the needs of their loved ones.
A survey of over 3,000 caregivers conducted in the summer of 2023 by the Canadian Centre for Caregiving Excellence (CCCE) found that while for many Canadians, caregiving is a rewarding experience, it can also negatively impact their wellbeing. Nearly half of caregivers (47%) reported feeling tired, or overwhelmed (37%) as a result of caregiving, while one in four caregivers reported fair or poor mental health.
Canadian caregivers are in crisis. CCCE is responding with free mental health and wellness support, and with a new tool – social prescribing for caregivers.
Social prescription integrates social and medical approaches to care by prescribing non-medical interventions. This can include joining a peer support


group, taking an art class, going on a hike or to see a movie and reconnect with friends; supports are customized based on the individual’s needs and interests.
“The dynamic and demanding nature of my caregiving role can only work when I feel energized, rested and well.” – Helen Ries, Co-Founder, Siblings Canada.
Since its introduction, social prescribing has found a foothold in approximately 17 countries worldwide. The National Health Services of the UK, recognizing the benefits, has woven social prescribing into its overarching framework for personalized
care, and it is a key pillar its National Strategy to Reduce Social Isolation. In Canada, the Public Health Agency of Canada, under the leadership of the Canadian Red Cross, launched the Canadian Institute for Social Prescribing (CISP) in 2022.
CISP is rooted in a collective impact approach. Since its opening, it has worked to link people, evidence, and share practices that connect people to community-based supports and services that can help improve health and wellbeing.
These networking efforts include a new collaboration between CCCE and CISP to address caregivers’ challenges and enhance their health and wellbeing opportunities. Through a $1.8 million investment over two years, the initiative will support Caregivers Alberta, Caregivers Nova Scotia, Family Caregivers of British Columbia, and the Ontario Caregiver Organization to improve access to social prescribing initiatives for caregivers in each of those provinces.
Social prescribing initiatives in Canada and abroad have succeeded in decreasing loneliness, enhancing a sense of connectedness and belonging, and improving mental health. The Ontario Hospital Association has found that social prescription programs demonstrated improvements in anxiety, depression, health-related quality of life, mental and general wellbeing, isolation, social connectedness and self-care.
Social prescriptions can also have meaningful long-term benefits. By engaging in activities that promote selfcare and stress management, caregivers can develop coping skills that can serve them well in the long run. By accessing resources that promote healthy lifestyles and self-care practices, caregivers can mitigate the risk of burnout and fatigue, ensuring their ability to sustain their caregiving role over time.
Social prescribing has also been linked to reducing healthcare visits and deepening integration between clinical care, interprofessional teams, and social supports. In fact, evidence in Canada and the UK indicates that primary care providers spend at least a third of their time on social issues that others can better address. Social prescription referrals have been shown to decrease visits to general practitioners by 28 per cent and an average reduction of 24 per cent for hospital emergency admissions.
To date, social prescription has largely been focused solely on the patient to improve health outcomes of the patient and the caregiver, when the focus should be on the whole care team – caregivers (unpaid relatives/ friends), care providers (those employed to provide care), and care recipients. Caregivers and care providers face unique barriers to participation in

social prescription activities, including financial strain, lack of respite services, lack of connection to services, and not knowing when or how to start.
The CCCE/CISP partnership represents a significant step forward
in addressing the issues that caregivers face. By providing access to support services tailored to their needs, caregivers will be empowered to prioritize their own wellbeing while fulfilling their caregiving responsibilities. As social prescribing initiatives become widely accepted, caregivers can look forward to a future where they are supported, valued, and empowered to thrive in their vital roles.
















