

My Blood My Health


Welcome to My Blood, My Health Digital Magazine
Welcome to our second issue of My Blood My Health digital magazine. In this edition, we delve into the real face of transfusion dependency. Transfusion-dependent patients face many factors other than a simple "top-up." They face challenges that transfusions bring to their lives, the cost of their time, and the cost to the healthcare system. Blood Transfusions are not curative but only one option.
With this magazine, we aim to pursue Heal Canada's mission to empower patients to access better and equitable services across Canada. We're deeply grateful to our readers for their continued interest and support. Your engagement drives us to bring insightful and valuable content to encourage patient-centricity in healthcare.
If you haven't already, we encourage you to subscribe and stay connected with My Blood, My Health digital magazine for future issues, where we'll continue to explore topics that matter to you and the healthcare community.
Thank you for participating in our journey, and welcome to this enlightening issue!
From your dedicated team

Cheryl Petruk, MBA B.Mgt. CEO & Founder of Heal Canada

Brigitte Leonard, Ph.D
Chied Scientific Officer My Blood, My Health Director
Heal Canada is a registered Not For Profit Organization in Canada healcanadaorg
Disclaimer: The Patient Advocacy Digital Magazine provides general information and resources to promote patient empowerment and awareness. The content is not a substitute for professional medical advice or treatment. Always consult with qualified healthcare professionals for personalized guidance regarding your specific medical condition or situation






T h e I m p o r t a n c e o f Q u a l i t y
o f L i f e f o r B l o o d C a n c e r
P a t i e n t s
b y C h e r y l P e t r u k , M B A
Blood cancers, including leukemia, lymphoma, and myeloma, are challenging and impactful diseases that affect millions worldwide. The diagnosis and subsequent treatment of blood cancer can significantly alter the quality of life (QoL) for patients and their families. This article explores the importance of QoL for blood cancer patients, the associated challenges, and the multifaceted burden of the disease It concludes with strategies to enhance QoL for these individuals
Understanding Quality of Life in Blood Cancer Patients
Quality of life is a multidimensional concept that encompasses physical, psychological, and social well-being. For blood cancer patients, QoL is critically important as it impacts their ability to cope with the disease and its treatments According to the World Health Organization (WHO), QoL includes an individual’s perception of their position in life, in the context of the culture and value systems in which they live, and in relation to their goals, expectations, standards, and concerns (WHO, 2023)
Physical Challenges
Blood cancer patients often endure extensive physical challenges, including chronic pain, fatigue, and the side effects of treatments such as chemotherapy, radiation, and stem cell transplantation These treatments can lead to immunosuppression, increasing the risk of infections and further complicating the patient’s condition (Smith, 2021)
Psychological Challenges
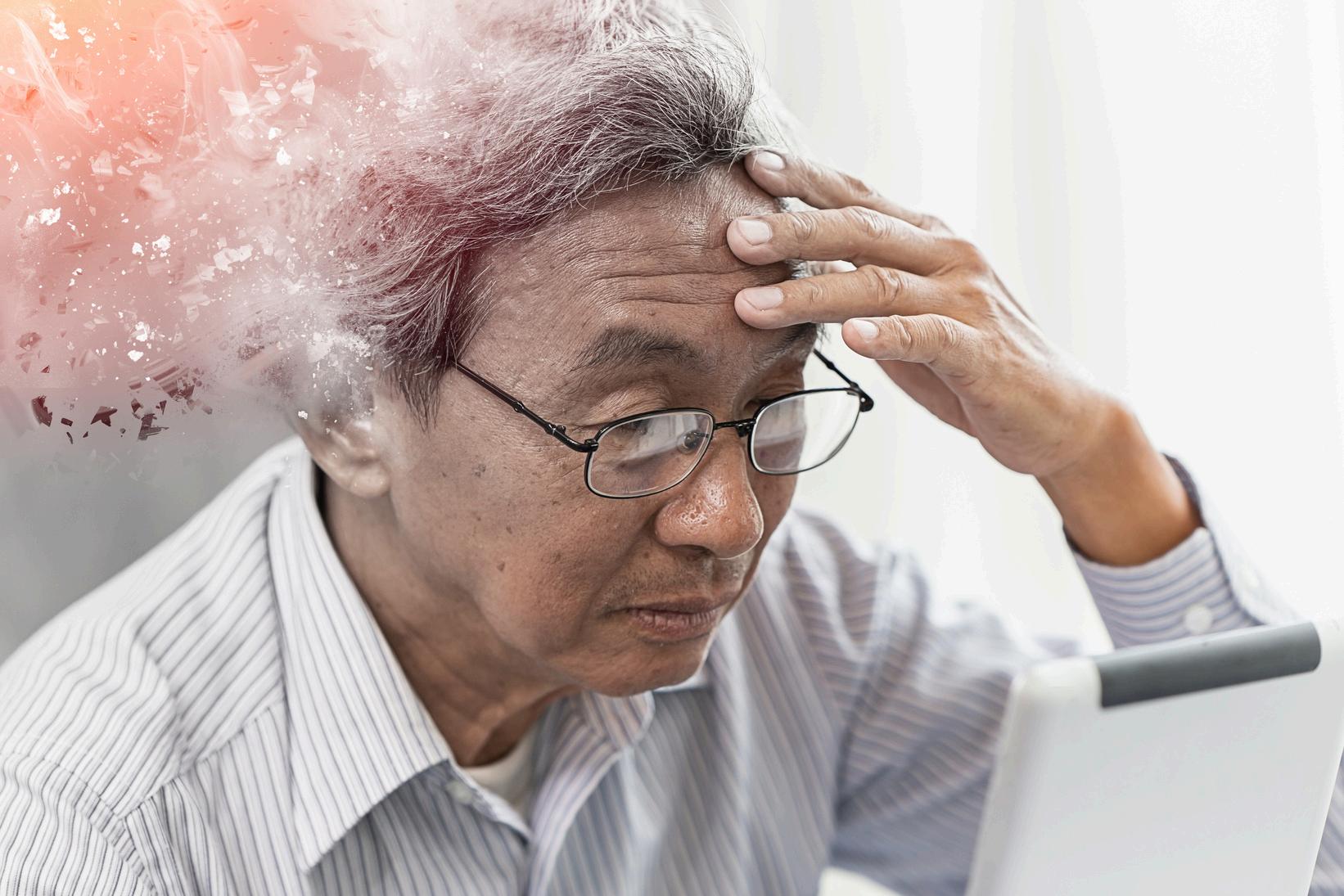
The psychological impact of a blood cancer diagnosis can be profound Patients may experience anxiety, depression, and fear of recurrence or progression of the disease. The uncertainty surrounding their prognosis can exacerbate these feelings, leading to significant emotional distress (Brown et al., 2022).
Social Challenges
Blood cancer patients may face social isolation due to prolonged hospital stays and the need for infection control measures This isolation can strain relationships with family and friends and disrupt daily life and social activities, further diminishing QoL (Green & Clark, 2021)

Realities of Living with Blood Cancer
Curable and Treatable Cancers
For patients with curable blood cancers, such as certain types of acute leukemia, the focus is often on aggressive treatment to achieve remission. While the potential for cure offers hope, the intensity of treatment can be overwhelming. Patients must endure cycles of chemotherapy, frequent hospital visits, and the constant fear of relapse (Jones et al, 2023)
Non-curable but Treatable Cancers
Patients with non-curable but treatable blood cancers, such as chronic lymphocytic leukemia (CLL) or multiple myeloma, often undergo long-term treatment to manage the disease. These patients live with the knowledge that their condition is chronic, requiring ongoing monitoring and treatment adjustments. The prolonged nature of their illness can lead to a sense of perpetual uncertainty and stress (Miller, 2022)
Non-Curable and Non-Treatable Cancers
For those with non-curable and non-treatable blood cancers, the focus shifts to palliative care, aimed at relieving symptoms and improving QoL rather than achieving remission. These patients often confront the reality of limited life expectancy, necessitating discussions about end-of-life care and advanced directives (Johnson & Smith, 2021).

Patient Burden
The Burden of Blood Cancer
The burden of blood cancer on patients is immense. They face physical discomfort, emotional turmoil, and social isolation. The relentless nature of the disease and its treatment can erode their sense of normalcy and independence, making it difficult to maintain a positive outlook (Anderson et al., 2021).
Caregiver Burden
Caregivers of blood cancer patients also experience significant burdens They must manage the patient’s medical needs, provide emotional support, and often juggle these responsibilities with their own personal and professional obligations. The stress and fatigue associated with caregiving can lead to burnout and affect their physical and mental health (Smith, 2021)
Family Burden
The impact of blood cancer extends to the patient’s family. Family members may experience emotional distress, financial strain, and disruptions to family dynamics The need to support the patient through their journey can lead to sacrifices and adjustments in family roles and routines (Brown et al., 2022).
Healthcare System Burden
The treatment and management of blood cancer place a significant burden on the healthcare system. The costs associated with hospital stays, medications, and specialized treatments are substantial Additionally, the need for long-term care and follow-up further strains healthcare resources (Green & Clark, 2021).
Enhancing Quality of Life for Blood Cancer Patients
Holistic Care Approaches
Adopting a holistic approach to care can significantly enhance QoL for blood cancer patients This involves addressing not only the physical symptoms of the disease but also the psychological, social, and spiritual aspects of the patient’s well-being (Johnson & Smith, 2021).
Psychological Support
Providing psychological support through counseling, support groups, and mental health services can help patients cope with the emotional challenges of their diagnosis and treatment Interventions such as cognitive-behavioral therapy (CBT) have been shown to reduce anxiety and depression in cancer patients (Miller, 2022).
Social Support Networks

Strengthening social support networks is crucial for improving QoL. Encouraging patients to maintain connections with family and friends, participate in community activities, and engage in peer support groups can alleviate feelings of isolation and provide a sense of belonging (Jones et al, 2023).
Symptom Management

Effective symptom management is essential for improving QoL. This includes pain management, nutritional support, and interventions to reduce fatigue Palliative care teams play a vital role in providing comprehensive symptom relief and enhancing patient comfort (Anderson et al, 2021)
Empowerment and Education
Empowering patients through education about their disease, treatment options, and self-care strategies can improve their sense of control and confidence in managing their condition Providing resources and information tailored to their needs can enhance their ability to make informed decisions (Smith, 2021)


Integrative Therapies
Integrative therapies such as acupuncture, meditation, and yoga have been shown to complement traditional treatments and improve QoL. These therapies can help manage symptoms, reduce stress, and promote overall well-being (Brown et al., 2022).
Personalized Care Plans
Developing personalized care plans that take into account the unique needs and preferences of each patient can enhance their QoL These plans should be dynamic, adapting to changes in the patient’s condition and circumstances (Green & Clark, 2021).
The importance of QoL for blood cancer patients cannot be overstated. Addressing the physical, psychological, and social challenges they face is essential for improving their overall well-being While the disease's burden is significant, both patients and their caregivers can take positive steps to enhance QoL
By adopting holistic care approaches, providing psychological and social support, managing symptoms effectively, empowering patients through education, and incorporating integrative therapies, healthcare providers can make a meaningful difference in the lives of blood cancer patients Through these efforts, we can help patients navigate their journey with greater resilience, hope, and dignity



Q u a l i t y o f L i f e f o r B l o o d
C a n c e r P a t i e n t s : T h e
S u r v e y
b y B r i g i t t e L e o n a r d , P h . D .
In our previous article, we highlighted the impact of blood cancer on quality of life and discussed potential solutions Heal Canada is dedicated to enhancing healthcare services to improve the quality of life for patients and their families. To achieve this, we surveyed patients diagnosed with blood cancer to understand daily challenges This article summarizes responses from thirty-two patients who took the time to complete the survey Thanks to them for supporting us in our mission.
Diagnosis
Patient diagnosis can be a long and stressful process for some patients Only 13% of patients were successfully diagnosed within a week, while 19% received their diagnosis within one month, 29% within three months and 39% more than three months. Only 50% of patients fully understood the need for each test and procedure during this process Confirming their diagnosis helps most patients better understand their condition and treatment. Only 33% of patients struggled to understand their condition and treatment better. So, having access to educational sessions at the cancer centre or via a patient organization is essential, and only 52% of patients mentioned having support other than their cancer specialist.
Symptoms burden
The diagnosis is only the first step of their journey. The results show that most patients experience debilitating symptoms (Table 1). A majority of patients mention symptoms like fatigue, pain, sleep issues, and reduced functional capabilities, even if they received treatment They attribute this poor QoL to disease, treatment side effects, or lack of efficacy

Emotional & Mental burden
67% of patients mentioned that the diagnosis affected their mental and emotional well-being, while most cancer centers and hospitals don't offer mental health support; only 14% of patients mentioned having received support for mental health. Most patients needed to reach support on their own and paid for it. Most patients must rely on their family or close friends during this journey. Only 60% of respondents have joined a support group The healthcare system will need to step up and improve its offer considering current demographic changes: fewer married persons, smaller nuclear families, and increased solitude.
Social burden
Blood cancer diagnostics impacted patients' QoL and interaction with their entourage While around 35% to 40% of respondents didn't observe any change with their spouses, children, friends, or co-workers, 15% to 25% of patients have experienced a deterioration of their relationships in different spheres of their lives. For example, some people had to stop seeing their family members or friends because of their reluctance to receive COVID vaccine (anti-vax movement) Some people feel fortunate, have a better relationship with their entourage, and appreciate people more.
Blood cancer diagnostics negatively impacted the social activities of 86% of respondents More than 56% had to reduce their social activities by more than 50% Also, 10% of respondents mentioned a significant reduction in their social life to the point they felt they did not have one anymore.
Financial burden
71% of the respondents mentioned that the disease negatively impacted their finances They had to reduce their work hours, move to another city to receive stem cell transplantation, retire earlier than anticipated, or go on disability. Most participants (60%) mentioned that remote work can improve their situation and significantly reduce the risk of multiple infections So, hybrid mode or work at the office significantly impacts their work capability and increases stress
What they need
We asked them what improvements they would like to see in the healthcare system. They hope for better access to new treatments (50%), more mental health support (45%), and prevention and early detection (50%) Access to specialists and primary care physicians remains problematic, and patients appreciate telemedicine (45%). Patients and their entourage need help understanding all the services offered to them, and 40% of patients wish for a streamlined process





What`s next
Thanks to participating patients, we grasp some valuable and actional aspects of their journey and can work on projects to favour their QoL:
Better diagnostic processes that facilitate early detection and quick diagnosis can improve QoL and response to treatment Better integration of AI capabilities at the primary care level can improve diagnosis efficiency, especially for rare blood cancers. With AI's support, better patient management in cancer centers can improve processes, timelines, and patient experience while freeing healthcare professionals time to focus on patients' care
Improving access to new treatment is critical to enhancing QoL; more efficient targeted treatment should provide better symptom management and avoid disease progression associated with QoL degradation
Telemedicine and remote work significantly simplify patients' lives. By reducing their social contacts when their system is vulnerable or by providing more flexibility at work, they can stay active longer and contribute positively to society These inclusive approaches can improve their QoL and reduce the financial burden their disease had on their life.
We hope this survey overview helps you better understand the daily challenges patients and their entourage can face and favours the adoption of more inclusive practices.

CommunityEngagementandEducation
KYBengagesthecommunitythroughvariouseventsandworkshopsdesignedtoeducateandraise awareness Theseinclude: WorkshopsandSeminars:Hostingeducationalsessionswithguestspeakersand healthcareprofessionals.
CommunityEvents:Participatinginhealthfairsandfestivalstoconnectwithcommunitymembers
SocialMediaCampaigns:Utilizingsocialmediaplatformstoshareinformationand engagewithabroaderaudience
HealthcareCollaborations:Partneringwithlocalhealthcareproviderstopromoteblooddonationsand offerfreehealthscreenings
JoinUs
KYBinvitesindividuals,healthcareprofessionals,communityleaders,andorganizationstojointhismission Together,wecanworktowardsreducinghealthdisparitiesandimprovingoutcomesforindividualswith blooddisordersintheAfrican/Caribbeancommunity Whetherthroughdonatingblood,volunteering,or simplyspreadingtheword,everycontributionhelpscreateahealthierfuture
Formoreinformationonhowyoucangetinvolved,sendanemailto knowyourblood2024@gmail.comorfollowusonsocialmedia:Instagram:@Knowyourblood; TikTok:know.your.blood
Together,wecanmakeadifference




T h e h u m a n c o s t o f f r e q u e n t
b l o o d t r a n s f u s i o n s
b y B r i g i t t e L e o n a r d , P h . D
Blood transfusions have saved many lives since their introduction into clinical practice. In 1818, the British obstetrician James Blundell successfully transfused human blood to a patient to treat postpartum hemorrhage. The use of transfusions in the early decades of the twentieth century became safer with the discovery of the major blood groups (the blood alphabet). Today, it is one of the most frequent procedures worldwide
Blood transfusions are essential for patients who experience blood loss They can replace the blood lost during surgery or because of an injury. Some treatment can cause temporary anemia, necessitating blood transfusion for a short period. However, some medical conditions require frequent blood transfusions continuously. These conditions include blood cancers or noncancer blood diseases such as anemia, hemophilia, and sickle cell disease
Challenges associated with transfusion-dependency
Being dependent on transfusions has drastic consequences on patients and their entourage. Frequent transfusions are associated with poor quality of life (QoL) and several complications, some of which can be life-threatening.
A person who requires frequent blood transfusions can quickly develop iron overload The daily iron intake should be between 87 and 148mg, depending on the sex and age. Each blood bag contains around 250 mg of iron. It takes roughly 250 days for the body to eliminate this excess of iron. So, ten transfusions delivered in a short period (5 months) can be enough to develop meaningful iron overload
Untreated iron overload can lead to severe heart and liver problems; for people who need frequent transfusions, a treatment to reduce the iron level in the body (iron chelator) is necessary.
Adding an iron chelator to the treatment regimen for non-cancer blood disorders is part of the clinical practice because these disorders are diagnosed at a young age However, for patients affected by blood cancer, because of their older age, monitoring iron overload and prescribing chelation is not as automatic.

Real-life patient experience with frequent blood transfusions
We surveyed transfusion-dependent people to assess this condition's impact on their lives. The participants were all diagnosed with blood cancer; they were all older than 35 years old.
Survey participants mentioned receiving a blood transfusion every week to every second week for two to five years
Frequent transfusions impacted their and their caregiver's working status Often, they had to precipitate their retirement, reduce their working hours or even go on a disability program. Only 75% of them are receiving treatment for iron overload.
On average, each transfusion takes 65 to 95 hours, including transportation time Some participants need to drive more than four hours to receive their transfusion Also, depending on the patient's hemoglobin level, sometimes patients won't receive it

Real-life patient experience with frequent blood transfusions (con`t)
The main reasons for receiving a transfusion are: fatigue anemia low Hemoglobin (Hg)
Most participants (75%) experienced adverse reactions during the transfusion: fatigue (50%), blood pressure drop (25%) allergic reactions (25%)
Most participants (75%) experienced adverse reactions after the transfusion: restless leg syndrome associated with iron overload (75%), reduced daily living and functional capabilities (50%), emotional and mental health issues (anxiety, depression) 50%, fatigue (50%) pain (50%).
For all patients, the benefit of blood transfusion is not sustained over time
Participants scored their stress level regarding transfusion at 75%, with 100% being very stressful.
Participants scored the transfusion impact on QoL at 86%, with 100% having a significant impact
Participants scored the transfusion impact on their mental and emotional well-being at 89%, with 100% having a significant impact
Participants scored the transfusion impact on their social activities at 83%, with 100% having a significant impact

For participants, receiving frequent transfusions is associated with several challenges: mental Health (100%), family responsibilities (75%), work-life balance (75%), having a good QoL (75%), transportation (25%), housing responsibilities (25%), budget struggles (25%), work challenges (25%)

Some blood cancers are associated with extreme fatigue, linked to anemia Blood transfusion is a treatment offered, assuming that increasing hemoglobin (Hg) levels will improve fatigue and QoL. However, the analysis does not find a clear correlation between Hg levels and fatigue. Moreover, cancer patients experienced a decline in their functioning capability and QoL despite frequent transfusions, as observed in the survey
Recently, studies have demonstrated a correlation between some debilitating symptoms (fatigue, depression, pain) and inflammation markers called cytokines. In these cancers, the level of cytokines in the blood is abnormally high. These observations explain why patients are still experiencing fatigue despite frequent transfusions. Also, anemia is often the consequence of cancer progression, so a targeted treatment provided earlier in the disease course could significantly benefit patients' anemia and symptoms burden
Two products currently under revision by Health Canada illustrate this exciting novel approach well.
Ivosidenib (TIBSOVO) Momelotinib (Ojjaara)

Ivosidenib (TIBSOVO)
In AML, the current standard of care for AML patients who cannot receive intensive chemotherapy is Azacitidine (Aza) Patients with a mutation involving IDH1 have a poorer treatment response rate and survival
Based on the AGILE trial, combining ivosidenib with Aza improves critical clinical aspects for most IDH1 patients. Many patients became transfusion-independent and improved over time, which is very encouraging. The combination also provides additional benefits such as increased survival, reduced infections and fewer adverse reactions while improving QoL, functional capacities and symptoms (fatigue, pain, insomnia)
Momelotinib (Ojjaara)
Myelofibrosis is a rare cancer in which blood cell production is abnormal and inflammation markers called cytokines are overproduced Anemia is often present at diagnosis and eventually develops in nearly all patients due to cancer progression Anemia and blood transfusion are adverse risk factors for leukemic transformation and survival.
Most available treatments for myelofibrosis exacerbated disease-related anemia, limiting their efficacy Momelonitinb, a recent targeted treatment, is as efficient as others in the same category However, unlike other therapies, momelotinib can improve anemia by facilitating the production of blood cells SIMPLIFY trials have demonstrated that patients can reach healthier blood levels and become transfusion-independent Some patients could even delay complex procedures such as transplantation due to this treatment.
Blood transfusion is ineffective in addressing specific issues observed in cancer patients. It is critical to continue to develop effective treatments to address the underlying cause of anemia and symptoms in these patients, reserving this precious resource for medical conditions that can be treated only by transfusion
The end



A M L t r e a t m e n t s i n
t r a n s i t i o n
b y B r i g i t t e L e o n a r d , P h . D
AML treatment has become very complex over the years due to a better understanding of the disease, the role of mutations in disease progression, and new treatment options Advancements in assessing clinical response to treatment and introducing targeted medications have complexified the treatment paradigm to the point that the medical community needs to reassess its approach. Transition periods are exciting for the community. However, how can we guarantee that no patient is left behind?
The backbone of AML treatment
AML treatments are divided into three sections:
Induction/remission
Elimination of minimal residual disease (MRD)
Salvage relapsed disease
Therapy aims to prolong the period patients are in remission as long as possible to delay relapse Patients who achieve MRD negativity (MRD-) have better odds than patients who are still positive (MRD+) after the induction treatment So, the traditional approach was to provide quickly an intensive chemotherapy regimen as induction (1) followed by an allogenic transplantation (2) to eliminate the residual disease as much as possible.
In 2024, it is still the preconized approach However, some targeted agents can be added to the intensive chemotherapy to improve results Some targeted therapies can be used regardless of the mutation status; some will be specific to the mutation found during the diagnostic assessment
The impact of transplantation is not always positive. The precise assessment of the response to induction achieved by a patient can help assess if transplantation is necessary.
Assessing response to treatment and the minimal residual disease (MRD)
The difficulty in assessing MRD in AML is due to molecular heterogeneity. Unlike CML, where 100% of patients carried the t(9;22), several mutations and fusion genes can be involved. European guidelines recommend monitoring all patients by flow cytometry (FC) for MDR after two treatment cycles and at the end. This technique allows for the monitoring of more than 90% of patients
The issue with this technique is its relatively low sensitivity compared to PCR and sequencing methods, so bone marrow is the preferred sample source for FC. It is not ideal for patients compared to blood because bone marrow biopsy is invasive and potentially painful. Despite its relatively low level of detection, a clear correlation has been established between MRD and survival outcomes in patients with AML
MRD+ >01%: Patients with more than 01% of tumour cells in the sample have poorer survival than patients who do not have detectable tumour cells
Some patients can be MRD positive but below 0.1%; these patients do better than patients with MRD+ >0.1% but poorer than patients MRD-.
Access to predictable and sensitive techniques to assess MRD is crucial to optimizing patient management These techniques help personalize treatment with a better risk-benefit assessment It has been demonstrated in AML patients with NPM1 mutation that the postinduction MRD status predicts relapse and death (MDR-90% vs MDR+40%) These types of analyses highlight the relevance of a personalized approach. In fact, in patients who are MDR+, allogenic transplantation improved OS. However, for patients who achieved MRD, the outcome is better than one who received allogeneic transplantation.

Proper treatment for each patient
The treatment will be chosen primarily based on these factors:
Diagnostic
Patient personal risk
Patient fitness, including age
Patient preference
The diagnosis of AML has evolved with the increased understanding of the disease Discordance among classification methods, such as ICC 2022 and WHO, can complicate treatment decisions and access For example, patients can be diagnosed as MDS instead of AML, reducing their possibility of accessing potentially life-changing treatments.
Influenced by disease risk, HCPs might be privileged palliative therapy for unfit patients with poor prognostic However, novel targeted therapies can induce a meaningful response and improve survival with historically poor prognosis So, regimens, in addition to cytogenetic and molecular aberrations, should be considered in predictive models
Typically, patients diagnosed with AML are rushed into treatment without mutation analysis because the disease can progress very fast. To reach MDR negativity, intensive chemotherapy is given as induction therapy. Older or unfit patients often couldn’t tolerate intensive chemotherapy very well, so they receive less effective treatment but better tolerated
New options for unfit patients
Five new concepts emerge from EHA for ineligible patients to intensive chemotherapy
2.
For patients with IDH1 mutation, adding targeted therapy such as Ivosidenib to Aza increases the odds of survival by 56% Survival reached two years compared to 8 months with Aza alone. The combination seems well-tolerated, with the same amount of discontinuation in both arms (AGILE Trial).
1 Patients with FLT3 mutation should receive an FLT3 inhibitor in addition to the standard treatment
3 Fitness status needs to be reassessed during the treatment course because novel targeted treatments reduce transfusion needs and can improve patient status So, a patient who is unfit to receive an allogenic transplantation at diagnosis can become suitable after receiving treatment.
5.
For patients without IDH1 mutation, adding targeted therapy such as venetoclax to Aza increases the survival to 15 months compared to 10 months with Aza alone However, the combination increases hematological complications. Doctors have developed new strategies to reduce adverse reactions to improve the treatment period and maximize responses: changing the dosing schedule, reducing the initial dose, and reducing the initial tumour burden with an initial short treatment of HU or Ara-C
4 The time needed to reach MRD negativity might be longer when HCPs use targeted treatment rather than intensive chemotherapy. So, continuing the treatment is essential before concluding that there is no clinical benefit
These strategies represent new approaches and completely change the AML treatment


C l i n i c a l T r i a l s a n d S u r v e y s





A l l i a n c e s a n d
C o l l a b b o r a t i o n s



Improving lives of MPNs patients
The Global MPN Scientific Foundation (GMPNSF) is a charitable non-profit organization dedicated to advancing research and management of MPNs. Our ultimate goal is to raise awareness, facilitate collaboration, and improve the lives of people affected by MPNs.
Our Mission
At Global MPN Scientific Foundation, we understand the challenges and gaps in the current management of MPN, such as:
Lack of awareness and education among patients, physicians, and scientists
Limited access to specialized testing and care
Variability in diagnostic criteria and treatment guidelines
Insufficient data on the natural history and outcomes of MPN
Limited availability of effective therapies and clinical trials
That's why we are committed to providing a source of professionally backed information, building and facilitating an MPN community, and advocating for patients affected by this rare group of blood cancers. Global MPN Scientific Foundation is run by volunteers comprising MPN patients and healthcare professionals who share this vision.
On our platform, you will find a wide range of unbiased and medically backed information, including leaflets, newsletters, and forums where you can meet and hear about the latest MPN research. You will also learn about our investment in research and support for clinical trials. Moreover, you will discover how we are developing links with MPN groups worldwide to become more visible in advocating for MPN patients.
We invite you to join us in our mission to improve the lives of people living with MPN. Whether you are a patient, a physician, or a pharma representative, you will find valuable resources and opportunities to connect with others who share your interest in MPN.
Together, we can make a difference! www.gmpnsf.org.



Created in 2017, the Acute Leukemia Advocates Network (ALAN) is an independent globalnetworkofpatientorganizationsdedicatedtochangingtheoutcomesofpatients withacuteleukemiabystrengtheningpatientadvocacyinthatarea.OurroleatALANis to support our members in supporting patients and their families, raise awareness of leukemia, and conduct work that is best done internationally, like generating data and evidence Allouractivitiesarepatient-led,collaborative,andevidence-based
Whoarewe?
In March 2024, the network counts 56 member organizations from 52 countries and is governed by a steering committee. All steering committee members are leaders of national patient organizations focusing on leukemia and blood cancers from different regionstoensureglobalrepresentation.
Howdowework?
AtALAN,weareconvincedthat:
A strong collaboration between contributors of a multi-stakeholder project will likely generatebenefitsforallpartiesinvolved
Patients' and patient advocates' perspectives are unique. Therefore, they should be considered specialist knowledge complementary to other experts, academia, and industry.
So, we collaborate on various projects with the pharmaceutical industry, other patient organizations,medicalsocieties,researchers,clinicians,andotherexperts
Whatdowedo?
1-CapacityBuilding:
2-Raisingawareness
3 Evidence basedadvocacy







My blood, My Health and Pat ADV Hub in the USA have embarked on a collaborative journey, aiming to revolutionize the realm of patient advocacy across North America. This pioneering partnership brings together two influential organizations from neighboring countries,combiningtheirextensiveexpertiseandresources.
The objective is to expand and enhance the access to critical information for patient advocates, ensuring that individuals across the continent receive the best possible support andguidanceintheirhealthcarejourneys
By bridging the gap between Canadian and American healthcare advocacy, this alliance promises to foster a more informed, empowered, and connected community of patient advocates, significantly contributing to the improvement of healthcare experiences for countlessindividuals.
email: patadvhub@gmail.com

www.patadvhub.org


Care partners
Join My blood, My Health's Patient Advisory Council
Be part of the My blood, My Health Resource Advisory Council. Provide ongoing feedback on issues relevant to Patient Advocacy in Canada. We are looking for Patients, Care-partners, and General Advocates
Send you information to:
Admin@healcanada.org or visit our website and fill out our application form and find out more details about time commitment required.





Partners





My Blood, My Health Team
Brigitte Leonard, Ph.D

BrigitteLéonardistheChiefScientificOfficeratMyblood,My Health,aregisterednot-for-profitorganizationadvocating equitableaccesstoqualityhealthcareacrossCanada.Shehadthe privilegeofworkinginPharmaforover20years,contributingto bringinglife-changingtreatmentstopatientswiththehighest ethicalstandards.Now,shewantstoshareherknowledgeand utilizeherscientific,strategic,andcommunicationskillstohelpthe patients’community
SheobtainedherPh.D.inBiomedicalSciencesfrom Universitéde Montréalin2003.Herdoctoralresearchwasconductedunderthe supervisionofDr.Denis-ClaudeRoyatGuy-Bernier,MaisonneuveRosemontHospitalResearchCenter.Shedevelopedaquantitative diagnosticassayinnon-Hodgkin'slymphomaandevaluatedthe relevanceofthismarkerinthepatient'soutcome.
Cheryl Petruk, MBA B.Mgt.
CherylA.Petrukisamultifacetedprofessionalwhosecareerspans acrosspatientadvocacy,business,andpost-secondaryeducation, showcasingherdedicationtomakingasignificantimpactineach oftheseareas.

Cheryl'stransitionintopatientadvocacywasdrivenbyapassion fromherfamilycircumstancesandadeepcommitmentto ensuringpatients'rightsandaccesstocare.Cherylhasworked tirelesslytobridgethegapbetweenthehealthcaresystem, patients,andpharmastakeholders,ensuringthatpatients'voices areheardandtheirneedsaremet.Herworkinvolvescollaborating withStakeholdersandPatientAdvocacyOrganizations,lobbying forpatientcentricity,andprovidingpatientsupportandguidance.
Cheryl'sempatheticapproachanddedicationtoadvocacyhave madeherarespectedfigureinthisfield,admiredbypatients, healthcareprofessionals,andfellowadvocates
Cherylalsoleadsandistheleadfacultymemberat CACHEducation,PatientAdvocacyTraining.

References
Anderson, R., Brown, K., Clark, S., & Jones, T. (2021). Symptom management in blood cancer patients: A palliative care approach Journal of Palliative Medicine, 24(6), 820-827
Brown, K, Green, S, & Clark, S (2022) The psychosocial impact of blood cancer: A review of patient experiences. Psycho-Oncology, 31(4), 463-471.
Green, S., & Clark, S. (2021). Social isolation in blood cancer patients: Strategies for support. Supportive Care in Cancer, 29(9), 5119-5126.
Johnson, T, & Smith, M (2021) Palliative care in hematologic malignancies: Enhancing quality of life. Blood Reviews, 45, 100710.
Jones, T., Miller, R., & Anderson, R. (2023). The journey of blood cancer survivors: From diagnosis to remission. Cancer Survivorship Journal, 5(2), 101-112.
Miller, R (2022) Chronic blood cancers: Living with uncertainty Hematologic Oncology, 40(3), 299-309
Smith, M. (2021). The caregiver's role in managing blood cancer: A comprehensive guide. Journal of Caregiving, 12(1), 45-59.
World Health Organization (WHO) (2023) WHOQOL: Measuring quality of life Retrieved from https://wwwwhoint/tools/whoqol

