From Back Pain to Back on the Farm
Bob returns to his hobbies after working with our pain management team. page 8

This issue of Touching Lives will introduce you to some exciting changes and additions to our campus, including our walking path, Prairie Trail, and our new pain management serviceline.
Springtime in Minnesota Brings the Promise of New Life and New Growth.
That is the feeling that many of us in healthcare are experiencing - hope that the worst of the pandemic is behind us. We can again focus more of our energy on partnering with our community to create opportunities for health and wellness.
Every three years, Glencoe Regional Health conducts a Community Health Needs Assessment (CHNA). The purpose is to ensure that we understand the health needs of our community. We have engaged many of our community leaders, business leaders, and community members in this effort. We are grateful for all who agreed to be a part of this process. We strive to meet the needs of our community through expansion of services, addition of new services, or partnerships with entities that can meet those needs. Our goal is to make sure high-quality care is always conveniently located close to home.
The result of our last CHNA revealed several community needs: mental health support, care for diabetes and prediabetes, and interventions in obesity — namely increased options for exercise. We have created a partnership to bring mental health services to GRH (read more on page 6), we’ve continued our focus on outpatient diabetes education (read tips on page 15), and partnered with the Glencoe Regional Health Foundation to create a walking path, Prairie Trail, to encourage activity within our community. We’re excited to host the Glencoe Days Fun Run and Walk on Prairie Trail for the first time ever this year! Read more about Prairie Trail on page 5.
This edition of Touching Lives will highlight some of our new service offerings, spotlight new providers, and reintroduce existing providers and services.
Sincerely,
Patty Henderson, MBA, BSN President & CEOWE WANT TO HEAR FROM YOU
We’re always interested in hearing from our patients, friends, and neighbors about how we’re doing. If you have thoughts you’d like to share with Patty, send an email to asktheceo@grhsonline.org. Your message will be sent privately to her office.

Care & Services
MEDICAL SERVICES
Acute Care
Allergy Medicine
Anticoagulation Clinic
Audiology
Birthing Services
Cardiac Rehabilitation
Cardiology
Diabetic Care & Education
Ear, Nose, & Throat
Emergency Services
Family Medicine
Hematology
Hospitalists
Imaging Services
Infusion Services
Internal Medicine
Laboratory Services
Mental Health
Midwife Services
Nephrology
Neurology
OB/GYN Services
Occupational Therapy
Oncology
Orthopedics
Pain Management
Pediatrics
Physical Therapy
Podiatry
Preventive Health Services
Pulmonology
Respiratory Therapy
Sleep Medicine
Speech-Language Therapy
Surgery
Transitional Care
Urgent Care
Urology
Wound Care
Vascular Consultations
SKILLED NURSING CARE

GlenFields Living with Care
SENIOR LIVING
Orchard Estates
HEALTHCARE NEEDS YOU!
Are you seeking a rewarding career where the work you do makes a difference? We want to meet you!
Check out our current job openings: grhsonline.org/careers
14
We Care For You Like Family
Scan the QR code below to watch our new video and learn about GRH.

16
2 VERTIGO
Learn about the symptoms of vertigo. Conoce los síntomas del vértigo.
5
GLENCOE DAYS FUN RUN AND WALK
For the first time ever, the Fun Run and Walk will be held at our walking path, Prairie Trail.

7
PAIN MANAGEMENT
Stay Connected
Get to know GRH! Follow us on social media and learn more about our organization. grhsonline.org/connect
Your feedback is important to us. Contact the GRH Marketing Team at marketingteam@grhsonline.org with suggestions and comments.
Our new serviceline gives hope that pain relief is possible.
8
FROM BACK PAIN TO BACK ON THE FARM
Bob of Hutchinson returns to his hobbies after working with our pain management team.

12
PUT YOUR SLEEP APNEA TO BED
Matthew Patterson, MD, FACS, MBA, MHA, explains obstructive sleep apnea.
13
ACID REFLUX DISEASE
Learn 5 things you should know about reflux from surgeon Elizabeth Colsen, MD, FACS.
14
MEET MACKENZIE LOBITZ, MD

A new provider joins our family medicine team in Glencoe and Lester Prairie.

16
GLENFIELDS GROWS OUR FAMILY
Our Extended Family Program is bringing a new vibrancy to the households.
PUBLISHER
Glencoe Regional Health 1805 Hennepin Avenue North Glencoe, MN 55336

MANAGING EDITORS
Ana Alexander
Lynn Beranek
Stephanie Beste
Jill Hatlestad
Denise Lemke
FIVE THINGS TO KNOW ABOUT VERTIGO
Jenni Keltgen
 PT, MPT
Physical Therapist
Terapia Física
PT, MPT
Physical Therapist
Terapia Física
Clark Christianson

PT, ScD, COMT
Physical Therapist
Terapia Física
ARE YOU SUFFERING FROM VERTIGO?
A referral is required to be seen by our physical therapists for vertigo. To talk with your provider about a referal, make an appointment by calling us at 320-864-3121. Learn more: grhsonline.org/vertigo
¿SUFRE DE VERTIGO?
Necesitará que lo refieran para que el departamento de terapia física pueda atenderlo por vértigo. Para hablar con su proveedor de salud sobre este referimiento, haga una cita llamando al 320-864-3121. Para mayor información: grhsonline.org/vertigo
Dizzy spells and spinning sensations can feel unsettling and scary – but if you’re experiencing vertigo, you are not alone. Dizziness and vertigo are more common than you may think, and at GRH, we’re here to help. Our physical therapy team treats vertigo – check out the five things our physical therapists want you to know about vertigo.
BY JENNI KELTGEN, PT, MPT1. 2.
The number one cause of vertigo related to an inner-ear problem is benign paroxysmal positional vertigo (BPPV). With BPPV, small crystals from one part of the inner ear move into the wrong area, causing the dizzying sensation. La causa número uno del vértigo está relacionada con un problema del oído interno llamado vértigo posicional paroxístico benigno. (VPPB o BPPV según sus siglas en inglés). Cuando se tiene VPPB, los pequeños cristales que se encuentran en el oído interno se mueven al área equivocada, causando sensación de mareo.
Symptoms of BPPV generally last less than one minute following a position change. BPPV can cause a spinning sensation that is sometimes accompanied by nausea and/or balance impairment. Symptoms of BPPV can occur with position changes, such as rolling over in bed, getting in and out of bed, bending over and returning upright, and tipping the head back. Los síntomas de VPPB duran menos de un minuto después de un cambio de posición. VPPB puede causar una sensación de que todo gira acompañado por nauseas y/o deficiencia del balance. Los síntomas VPPB pueden ocurrir con cambios de posiciones, como darse vuelta en la cama, levantarse o acostarse en la cama, inclinarse hacia adelante y volver hacia arriba, o inclinar la cabeza para atrás.
CINCO COSAS QUE DEBE SABER SOBRE EL VÉRTIGO
Los mareos y la sensación de que todo gira es preocupante y aterrador – pero si sufre de vertigo, no es la única persona a la que le pasa. Los mareos y el vértigo son más comunes que lo que usted piensa, y en GRH, estamos para ayudarlo. Nuestro equipo de terapia física trata personas con vértigo - lea a continuación las cinco cosas que nuestros terapistas físicos quieren que sepa sobre el vértigo.
TRANSLATED BY OUR GRH INTERPRETERS. LEARN MORE AT GRHSONLINE.ORG/SERVICIOS-DE-INTERPRETACION
3. 4. 5.
Dizziness is one of the most common reasons that older adults seek medical attention. Left untreated, dizziness can affect your balance and leave you at risk of serious injury from falling. Often, dizziness is caused by a problem with the vestibular system, which includes parts of the inner ear and brain that help control balance and eye movement.
Los mareos son una de las causas más comunes por las que los adultos mayores buscan atención médica. Dejar los mareos sin tratamiento puede afectarle el balance, causarle caídas y sufrir una lesión seria. A menudo, los mareos los causa un problema del sistema vestibular, lo que incluye partes del oído interno y el cerebro que ayuda a controlar el balance y el movimiento de los ojos,
Some causes and problems with dizziness can be treated with physical therapy. Treatment includes the canalith repositioning manuever, which involves a series of head movements that help move the crystals back to the correct place in the inner ear. Canalith repositioning manuevers can be performed by trained physical therapists, including our team at GRH.
La terapia física puede tratar las causas y los problemas que causan los mareos. El tratamiento llamado la maniobra de reposicionamiento canalicular, incluye una serie de movimientos de la cabeza que ayudan a mover los cristales al lugar correcto en el oído interno. A la maniobra de reposicionamiento canalicular puede realizarla un terapista físico entrenado como nuestro equipo en GRH.
There is a high success rate for treatment of vertigo and dizziness through physical therapy. For approximately 80 percent of people treated, symptoms are gone after one or two therapy sessions. Existe un alto índice de recuperación de las personas que realizan terapia física para tratamientos contra el vértigo y los mareos. Aproximadamente el 80 por ciento de las personas que hicieron tratamiento no tienen más síntomas después de dos sesiones de terapia. una o dos sesiones de terapia.
TAKE WELLNESS ONE STEP AT A TIME
Sometimes it's not enough to talk the talk, you've got to walk the walk.
Walking is a free and easy way to add an extra dose of wellness to your daily routine. With benefits like burning calories, strengthening your heart, easing joint pain, and improving your mood, adding a brisk walk to your day is a great way to help you lead a healthier life.


Set Goals
Start with a simple goal, like taking a walk during your lunch break. Experts recommend aiming for 30 minutes of exercise each day, but it's okay to start slow! Try adding a five minute walk to your daily routine, and slowly increase the time each week. If you're not able to work in a full 30 minutes into your day, try breaking up the time into pieces - shorter, combined sessions of activity are still good for your health.
Stay Safe
Make sure you wear sturdy shoes with good heel and arch support, and wear sunscreen and sunglasses if you go for a walk during the day. If you opt for an evening stroll, wear bright colors or reflective tape so you’ll remain visible as it gets darker. Make sure you warm up, stretch afterward, and drink plenty of water.

Get Outdoors
Boost your mood by taking a break outdoors! Soak up the sun and breathe in fresh air - both much needed after a winter in Minnesota. Spending time outdoors helps you get a dose of Vitamin D, something many Minnesotans are lacking after a long, cold winter. Vitamin D helps beat the winter blues, and keeps your immune system, blood cells, and bones healthy.
Take a stroll outside on our new walking path, Prairie Trail, which can be found on our Glencoe campus.
Learn ways to get involved or donate at: grhsonline.org/walking-path
Haven’t had the chance to check out Prairie Trail?
Lace up your sneakers and swing by during this year’s Glencoe Days Fun Run and Walk! This year’s event will be taking place on our brand new walking path for the first time! The new route will be approximately 2.37 miles for runners and walkers.
Saturday, June 25, 2022

Start times: Run - 8:30 a.m. | Walk - 9 a.m.
There’s no entry fee or pre-registration required, though you may consider making a donation to Prairie Trail by scanning this QR code or by visiting our website: grhsonline.org/fun-run


All participants of the Fun Run and Walk will receive a free t-shirt, while supplies last. We hope to see you celebrating our first Fun Run and Walk on our new trail this year!

GLENCOE IN MOTION
Interested in getting active? Check out Glencoe in Motion! This group of community members seeks to create and support opportunities for the entire Glencoe community to get active. Follow them on Facebook for healthy tips. Learn more: glencoemn.org/glencoe-in-motion
An Evening of Awareness
GRH provides Premier Sponsorship in support of 2B CONTINUED ’s “Dancing Like the Stars” event.





We’re proud to support community organizations, like 2B CONTINUED, who work hard to create a brighter future for the communities we serve. In support of their mission to increase education on suicide prevention and mental health awareness, 2B CONTINUED recently organized a “Dancing Like the Stars” event to fundraise for their excellent community efforts. We are proud of our providers who participated in the event: GRH chief medical officer Kristine Knudten, MD, who emceed for the evening, and Kari Knodel Vettel, MPAS, PA-C, who danced the night away with her husband, Brandt, as competitors in the contest.
THANK YOU
to our providers for bringing their skills to the stage, and to 2B CONTINUED for their impactful work in our community. Learn more about 2B CONTINUED: 2bcontinued.org

Mental Health Therapy Services Now at GRH
We’re also proud to partner with the Lorenz Clinic, who provides mental health care 5 days a week at our Glencoe Clinic or via telehealth. To schedule an appointment, call us at 320-864-3121.
Pain, Pain, Go Away
Pain isn’t just an uncomfortable sensation – it can be debilitating, affecting not only an individual’s physical well-being, but their mental well-being.
Chronic pain is a common issue for many adults, but many communities have a gap in pain management care, forcing patients to drive far away to be seen for care.
At GRH, we’ve recently introduced new, full-time pain management services at our Glencoe Clinic, offering minimallyinvasive, non-surgical options for pain relief that are always close to home.

Our pain management services are led by Glencoe native, board-certified pain management specialist Joslin Thiemann, APRN, CRNA, NSPM-C. Joslin provided anesthesia services at GRH for 15 years and served as the Director of Anesthesia for nearly six years before transitioning into her current role.
“Our goal is to help you decrease your level of pain and suffering, so you can do the things you enjoy.”
After completing her fellowship in nonsurgical pain management, Joslin began providing part-time coverage for pain procedures and saw the need for a more comprehensive program to help patients manage their pain.

“We want our patients to return to lives that are uninterrupted by pain as quickly as possible,” said Joslin. “No one should live with chronic pain. At GRH, we’re engaged in educating you about pain and the options to relieve it, so you can do the things you enjoy.”
Treatment options can include medication management and procedures to numb or block pain, such as injections, nerve blocks, and
radiofrequency ablations. We offer a holistic approach to manage all aspects of pain, including physically and mentally, with input from various specialties, such as nutritional education, occupational therapy, orthopedics, psychological therapy, physical therapy, and sleep medicine.
“Our goal is to help you decrease your level of pain and suffering, so that you have a high quality of life. We want to inspire hope that pain relief is possible,” said Joslin.
Pain Relief is Possible
Patients may self-refer if their insurance allows. To schedule an appointment with Joslin or to consult with your primary care provider, call us at 320-864-3121 Learn more about our pain management services. grhsonline.org/pain
If you struggle with pain, you are not alone. New services bring pain relief close to home.
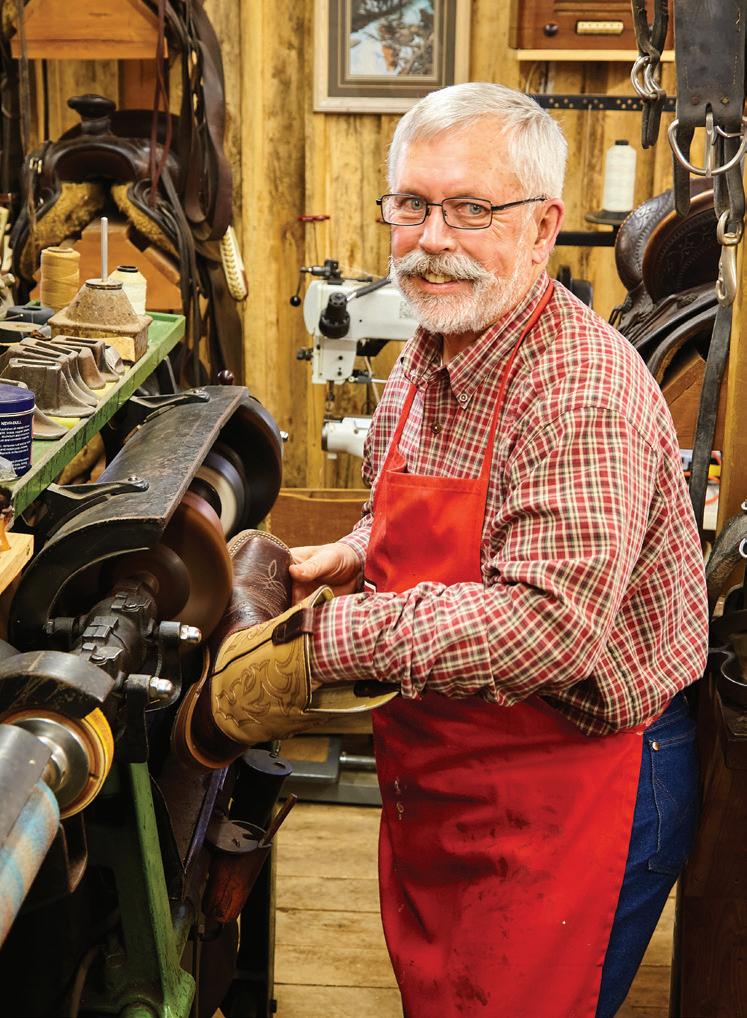
FROM BACK PAIN TO BACK ON THE FARM

“I couldn’t even stand up.” said Bob. “To this day, I don’t know what triggered it. I’ve never had back pain before, ever.”
Bob runs a charming hobby farm just outside of Hutchinson, where he devotes time to his many interests, including his leather-working shop, where he primarily repairs saddles; his set of horses he tends to each day; and his shop, where he’s been proudly restoring his rare 1956 Oliver Tractor. According to Bob, he spends most of his time out in his shop during the winter months.


“I don’t sit. I’m pretty active,” said Bob. “But when the pain hit, I had to hire somebody to do my chores, because I couldn’t do it. I didn’t go any place for five weeks.”
Bob was not a GRH patient at the time, but he decided to give us a try - he visited our website and found a bio for orthopedic physician assistant Terese Haasken, MPAS, PA-C, and decided to seek care.
“There was an appointment available the next day. It just clicked,” Bob said. “For me, it was just like a dream.”
Due to his intense levels of pain, Bob required a wheelchair to make it to his appointment, as he was unable to stand or walk. During his appointment with Terese, Bob had x-rays taken. After reviewing the imaging, Terese informed Bob that the root of his problem wasn’t his hip, as he’d thought, but his back. Terese put in orders for Bob to get an MRI done. When our patient access staff called him to schedule the appointment, the next available slot was two weeks away.
When Bob Elliott woke up on a cold winter morning in early February, his hip and back pain was so unbearable he couldn’t walk.
“I said ‘Oh my God,’ and the scheduler asked if I was okay. I told her I couldn’t even stand up because of my pain. She said, ‘Let me see what I can do,’ and when she called back, she had gotten me in the next day,” said Bob. “I could hardly believe it."
After his MRI, he was referred to see pain management specialist Joslin Thiemann, APRN, CRNA, NSPM-C.

A shot at relief
“Joslin was very, very good at explaining what was causing the pain, and how she thought she could heal it - and she was upfront enough to say that the injection may not be 100 percent effective, but it’s going to give you some relief,” said Bob. “And that word ‘relief’ right then, was very important.”
Bob was surprised by how quickly the injection helped - he describes it as an instant relief that made him “feel like a million bucks,” and which gradually took more and more of the pain away over the course of the next few days. He also saw our physical therapists, who gave him exercises to do at home. They also did dry-needling, a technique that targets areas of pain.
“I got off the table and walked out like nothing had ever happened to begin with,” said Bob.
“AS FAR AS I’M CONCERNED, THAT TEAM IS WALKING ON WATER.”
Bob was proud to return to his followup appointment without needing a wheelchair - he was able to walk once again. Before he left his appointment, Joslin told Bob if he experienced any additional pain, to call without hesitation, stating we don’t want anyone to be in pain any longer than they have to be.
Story continues on the following page.
Once she had reviewed the MRI of Bob’s spine, Joslin conducted a physical exam, in which she tested his muscle strength, observed how Bob was walking and moving, and did different types of movements to see which caused pain, all of which helped in her assessment. Joslin recommended a nerve pain medication, physical therapy, and a steroid injection in his back.
“Bob had pain that had started in his lower back, but his main symptom was that it was radiating down into his leg,” said Joslin. “That’s often caused by a nerve root that’s being pinched in your back, either by a bony structure or a disc that has moved.”
“I THINK THE STAFF REALLY CARE. THAT’S THE BIGGEST THING THAT JUMPS OUT. THEY’RE SMILEY AND FRIENDLY.”
“We have a lot of discussions in our clinic about remembering what got us back to feeling well, and how to continue to do that. We only have one life, so make it a good life with as little pain as can be, and as much function as possible,” said Joslin. “Going to a pain management specialist can get you back on track and living the life you want to - not focused on pain.”
For one month, Bob felt wonderful. He went back to doing his chores on his farm and enjoying time in his shop. And on one abnormally warm, 60-degree spring day, Bob decided to take out one of his tractors, which is when he twisted his back, triggering his pain again.
“Joslin and the physical therapy team warned me about twisting,” said Bob. “I never should have twisted my back - it came back to haunt me. By Monday, the pain was back with a vengeance.”
Bob called our clinic, and once again we were able to get him in the next day, when he received a second steroid injection. Again, he felt immediate relief that increased over the next few days until the pain gradually disappeared.


Back to his hobbies
After his second injection, Bob was happy to get back to his hobbies, while remembering not to push himself or twist his back.
“I was most excited to be able to walk again, and to get back to my shop,” said Bob. “For a 72-year-old-guy, I’m in pretty good shape.”
When Bob received a survey in the mail from us, he gladly returned it, even adding his own note to the back. He was shocked when he received a handwritten letter from our president and CEO, Patty Henderson, in response.
“What the hay!” said Bob. “It wasn’t something run off the computer, it was a handwritten note. That kind of action flows down through your whole operation - and it shows. In her note, Patty shared how much my note meant to the GRH team, and she would make sure everyone on the team heard my praise.”
When Bob returned for his next appointment, each of the members of the team thanked him for his kind note.
“Patty followed through with what she said she was going to do - and the rest of her team is exactly the same. When they told me they would do something, they did it. No delays,” said Bob.
Looking back, Bob is glad he chose to try a new healthcare organization when he first gave us a call that February morning.
“I think the staff really care,” said Bob. “That’s the biggest thing that jumps out. They’re smiley and friendly. I know they’re busier than busy, but they still take the time to talk with you and explain things. I like the whole feeling I get when I go to GRH.”
And we thank you, Bob, for choosing us!
2022 S C HO L ARSHI PWinners
Carl Sanken, a farmer from the Biscay area, and Don Hatz, a farmer and postal clerk from the Glencoe area have made an incredible impact on our area students through their gifts to the Glencoe Regional Health Foundation. Both Carl and Don remembered the Foundation in their wills with generous bequests, which established and maintain our Sanken-Hatz Scholarship Program. Sanken-Hatz scholarships are awarded annually to encourage and support students pursuing healthcare careers. This year, the Glencoe Regional Health Foundation awarded scholarships to 70 deserving applicants who are studying for careers in healthcare.
The legacy Carl and Don have left behind has touched the lives of so many – from the students who are supported in their pursuit of higher education, to the patients those students will eventually care for and serve.
Interested in supporting the GRH Foundation and future Sanken-Hatz scholarship recipients? Scan this QR code or visit our website: grhsonline.org/donate

GRADUATING HIGH SCHOOL SENIORS POST-SECONDARY STUDENTS


Buffalo Lake High School
Emilie Hable
Alexandra Maiers
Emma Peirce
Leslie Rodriguez
Tori Schmalz
Madison Wulkan
Central High School
Anna Meeker
Kalli Wischnack
Glencoe-Silver Lake
High School
Emma Gepson
Alisia Goettl
Kendall Guerrero
Connor Hallaway
Karlee Karg
Madeline Manteuffel
Malayh Metcalf
Margaret Schuft
GRADUATE STUDENTS
Abigail Butler
Samantha Good
Kali Grimm
Alexis Fronk
Beth Jerabek
Paige Litzau
Anna Mackenthun
Jackson Stifter
Isabel Villarreal
Gibbon-Fairfax-Winthrop
High School
Brody Hentges
Emilee Kuehn
Hutchinson High School
Riley Borka
Morgan Peck
Miranda Piehl
Nolan Prokosch
Kyla Struck
Lester Prairie High School
Riley Haas
Sibley East High School
Taylor Bachman
Aaron Elseth
Zachary Halverson
Elizabeth Anderson
Cole Becker
Lillian Beneke
Leah Bettcher
Miah Busse
Grace Daak
Destiney Exsted
Emma Fury
Anna German
Hayden Glander
Jayda Goldschmidt
Alexandra Hansch
Teagan Hansch
Ellie Harens
Abbie Hatlestad
Sydney Lepel
Jessica Novotny
Kennedy Pexa
Kaitlyn Popp
Madalyn Prokosch
Miranda Rannow
Erin Schultz
Audrey Seifert
Lynn Otto
Abagail Raiter
Ellie Schmidt
Victoria Sweely
Jaci Tourtellott
April Trebelhorn
Addyson Struck
Connor Sturges
Emily Thalmann
Rachel Trebesch
Mikayla Witte
GET
TO KNOW New Members of Our Foundation Board
Larry Anderson Board Chair State Farm - Owner
“The GRH Foundation Board wants to continually improve services and bring improved health to our service area. Our scholarship program is top notch by providing ongoing dollars toward students in a variety of medical fields. The Foundation wants to improve health and well-being of all in our service area, and are a wonderful group of positive people, which makes this a rewarding service opportunity.”
Laura Kuvaas Board Member Ridgewater College Director of Marketing, Recruiting, and
Communication
“GRH has been part of my history since the day I was born there. I also worked in the marketing department at GRH for 13 years - after leaving, I was asked to serve on the Foundation Board, so I could continue to make an impact. As a leader in higher education, I’m able to share my insight and perspective to support the educational side of the Foundation’s work. I want to give back to help this amazing health system continue its mission.”
Tina Rosckes Board Member Security Bank & Trust Co. - Senior Vice President Trust Officer
“I hope to contribute to the Foundation by using my voice, ideas, and passion to continue to help others. I want to be the voice for the amazing families and individuals that have entrusted the Foundation in carrying out their wishes. Be good, do good!”
The Foundation Board of Directors also includes Mary Ann Drew, Cindy Klaustermeier, Mary Ott, Orville Trettin, and Karen Wendlandt.
Put Your Sleep Apnea to Bed
BY MATTHEW PATTERSON, MD, FACS, MBA, MHA
Are you experiencing chronic sleepiness or fatigue during the day? These symptoms can sometimes be caused by a condition called obstructive sleep apnea.
What is obstructive sleep apnea?
Obstructive sleep apnea is a condition in which a blockage occurs of the upper airway during sleep. In obstructive sleep apnea, blood oxygen saturation decreases, which raises an alarm in the individual’s body. This alarm causes the body to rise out of deeper sleep levels and into shallow levels of sleep, or even full wakefulness, in order for the body to reopen its airways and bring blood oxygen levels back to normal.
Because of this constant disruption from deep sleep, the individual may experience chronic fatigue or sleepiness during the day. Obstructive sleep apnea
can also result in tightening of blood vessels in the body, including around the heart and head. Over time, this can cause high blood pressure, stroke, or cardiovascular events.
Symptoms of obstructive sleep apnea can include:
• Snoring
• Night sweats
• Headaches
• Daytime sleepiness or fatigue
• Restlessness during sleep
• Sudden awakenings with a sensation of gasping or choking
• Dry mouth or sore throat upon waking
• Forgetfulness, trouble concentrating, or irritability
There are three primary means of therapy for obstructive sleep apnea:
• Dental appliance. This option is most appropriate for snoring without sleep apnea and mild sleep apnea. Dental appliances prevent the tongue from blocking the throat, which helps to keep the airway open during sleep.
• Continuous Positive Airway Pressure Device (CPAP). These devices are most often used to treat moderate or severe sleep apnea. A CPAP device ensures the individual is breathing a continuous stream of air with enough pressure to keep the upper airway passages open.
• Surgery. This option is most often used to treat moderate or severe obstructive sleep apnea. There are several surgical options which can be performed to increase airflow for individuals while sleeping. Talk with your provider about what surgical options may be best for you.
EXPERIENCING OBSTRUCTIVE SLEEP APNEA OR OTHER SLEEP CONDITIONS, SUCH AS INSOMNIA OR RESTLESS LEG SYNDROME?
4 Things to Know About Acid Reflux Disease
BY ELIZABETH COLSEN, MD, FACS
Acid reflux disease is caused when the ring of muscle at the bottom of your esophagus is open or weak, letting acid “reflux” back into the esophagus. Reflux can also be caused by a hiatal hernia, when the upper portion of the stomach moves above the diaphragm.
There can be many symptoms of acid reflux disease.
Common symptoms include: heartburn, bloating, burping, nausea, weight loss for no known reason, wheezing, dry cough, dysphagia (the sensation of food being stuck in your throat), and regurgitation (bitter acid, or even food, coming up in your throat or mouth).
Certain factors make you more at risk for acid reflux disease.
Such factors include being overweight or obese; eating large meals before lying down; smoking; high alcohol intake; pregnancy; and eating certain foods that trigger reflux, such as coffee, tea, or chocolate.
3
Acid reflux can sometimes be managed with diet and lifestyle changes.
Lifestyle changes to consider include: Quit smoking.
Make diet changes and incorporate exercise into your routine if your acid reflux is caused by obesity.
Eat smaller portions and modify the types of foods you are eating.
Put blocks under the head of your bed to raise it at least 4 inches to 6 inches.
Eat at least 2 to 3 hours before lying down.
· Don't wear tight clothes or tight belts. Ask your provider if any medication could be triggering symptoms of acid reflux disease.
IS ACID REFLUX GETTING IN YOUR WAY?Meet our general surgeons.
Elizabeth Colsen, MD, FACS

Acid reflux disease can also be treated through surgery. If lifestyle changes and medications don’t resolve your symptoms, your provider may recommend surgery. Before surgical treatment, your surgeon will need a definitive diagnosis. This may require an EGD, or the use of a camera to look in your esophagus and stomach for other potential causes of your symptoms. You may also require a procedure to place a monitor in your esophagus, called a Bravo test, or a manometry test, both of which allow your surgeon to monitor the function of your esophagus and acid levels.
Once there is a definitive diagnosis, one surgical option is a fundoplication. This procedure creates an artificial valve using the top of your stomach, which prevents further acid reflux. Surgeons perform this procedure through small incisions in your abdomen. We recently started a program to perform transoral incisionless fundoplication (TIF), which creates a wrap using endoscopy without using incisions.

MACKENZIE LOBITZ, MD JOINS OUR FAMILY MEDICINE TEAM
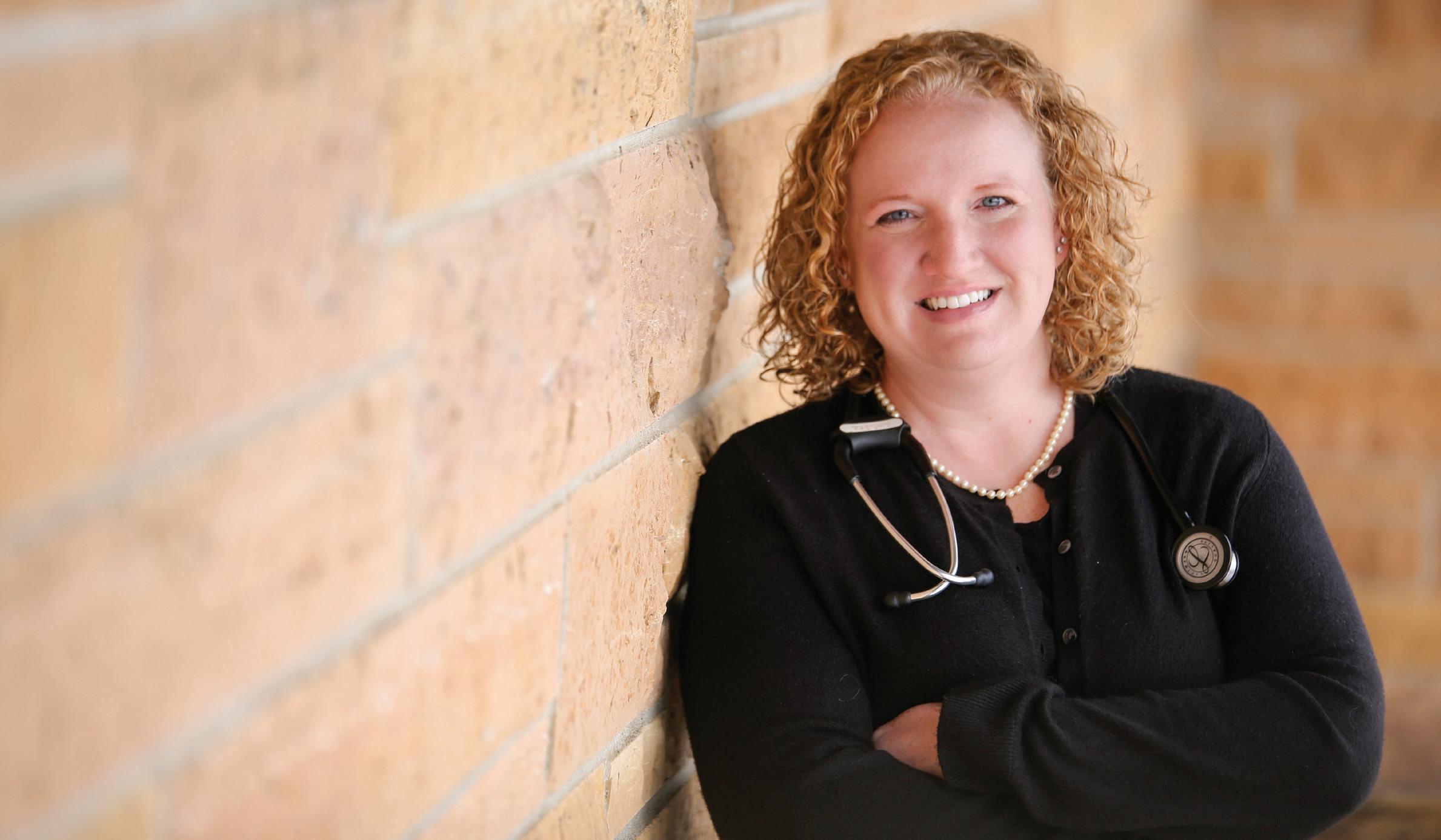
Dr. Lobitz will see patients in our Glencoe and Lester Prairie Clinics.
Mackenzie Lobitz, MD, was first drawn to the medical field through her love of science.
“Medicine is the perfect blend of my passions: keeping up with scientific advancements, and being able to help people,” said Dr. Lobitz.
In her practice as a family medicine
provider, Dr. Lobitz sees patients of all ages for a range of medical concerns and routine care. She enjoys the variety that a family medicine practice brings, especially being able to care for entire families.

“From well child visits to end-of-life conversations, my goal is to support my patients wherever they are in life,” said Dr. Lobitz.
Dr. Lobitz is particularly passionate about providing care for adolescents, weight loss management, and mental health.
“My favorite part of my job is partnering with my patients to make decisions about their health,” said Dr. Lobitz.
That love for helping people influences the way she approaches her practice, as well as conversations with her patients.
“I love helping patients understand their conditions and empowering them to take an active role in their treatment options.”
“I encourage my patients to talk with me about their concerns and what’s important to them – I want them to feel comfortable being open and honest with me during our appointments.”
After hours
Dr. Lobitz enjoys spending time with her family, especially during trips fishing, golfing, and attending her two sons’ sports games.
“I am a family person and love the simple joy of hanging out with family over a cup of coffee,” said Dr. Lobitz.
Learn more about Dr. Lobitz by visiting grhsonline.org/mackenzie-lobitz, or make an appointment by calling 320-864-3121.
Preventing & Managing Prediabetes
1 IN 3 AMERICAN ADULTS HAVE PREDIABETES, AND 8 OUT OF 10 DON’T KNOW IT YET.
Prediabetes can occur at any age, including children, but lifestyle changes can prevent prediabetes!
Most people with prediabetes do not have any symptoms. But what are the symptoms of Type 2 diabetes?
• Feeling tired
• Numbness/tingling in hands and feet
• Infections/sores that heal slowly
• Excessive thirst and urination
• Increased hunger
• Weight loss, in spite of eating more
• Blurry vision
• Dark discoloration on the skin
It’s important to know your risk for prediabetes. Organizations like the CDC have developed prediabetes risk tests, which can help you understand your level of risk – to try the assessments, visit: cdc.gov/prediabetes/takethetest or diabetes.org/risk-test. Risk factors include:
• Mother, father, sister, or brother with diabetes
• Overweight
• Body Mass Index (BMI) of 25+ (23+ for Asian Americans). Visit cdc.gov/bmi to learn more.
• Age 40+
• Women with a history of gestational diabetes
• High blood pressure
• Physically inactive
• Women with a diagnosis of PCOS (Polycystic Ovarian Syndrome)
• Some individuals may require screening at an earlier age: African Americans, Asian Americans, Hispanic individuals, and Native Americans
If you’re at risk, get screened! Request a screening for diabetes at your annual physical exam – early detection of prediabetes can help make lifestyle changes to prevent diabetes. There are several types of screenings. The A1C test is a blood test which shows the average blood glucose, or blood sugar, over 2 – 3 months. The fasting blood sugar test shows your blood glucose levels after not eating overnight. The glucose tolerance test shows your blood glucose after not eating overnight, and is remeasured after drinking a glucose liquid. The random blood sugar test shows your blood glucose at the time of testing, with no fasting required.
ACTION IS THE BEST MEDICINE!
If you have prediabetes, there are four key areas to consider to reduce your risk of diabetes:

• Healthy eating. Choose foods low in fat and calories and high in fiber. Focus on fruits, vegetables, and whole grains.
• Weight loss. Losing 5% of your body weight can reduce the risk of Type 2 diabetes.
• Activity. Exercise can help control blood sugars even if you do not lose weight.
• Medications. Medication is considered if lifestyle changes aren’t improving blood sugar levels.
To schedule an appointment with a GRH provider, call us at 320-864-3121
GLENFIELDS GROWS OUR FAMILY
Our Extended Family Program is bringing more vibrancy to the households.
The most important parts of our homes are often who we share them with.
That’s exactly what GlenFields leaders had in mind when they created the Extended Family Program.
“The Extended Family Program is all about connecting and relationship-building,” said Julie Schmidt, Vice President Senior Services.
GlenFields was designed with a household model of care, which means residents live in “households,” or living units made up of 18 private resident rooms, and shared community spaces such as a kitchen and dining room, living room, and sunrooms. Through the Extended Family Program, individuals are able to join one household as an extended family member, and participate in activities, share their talents with the households, or simply chat one-on-one with the residents.
The program initially began with the GlenFields staff, who were invited to be an extended family member in a household they did not work in. Staff have engaged in activities with the residents such as frosting cookies, playing bingo, bringing in their pets, and making homemade treats and meals. Staff have even organized a fish fry for the residents!
“We want to invite folks to share their gifts and talents with our residents,” said Julie. “It adds a vibrancy of life to the households. It brings variety, a different pace, new perspectives and connections, and it opens up time for sharing memories and reminiscing.”



Paula Verch, Silver Leaf Household Coordinator, has helped organize the Extended Family Program.

“It’s a great way to learn what our residents enjoyed outside of GlenFields,” said Paula.

“We enjoy reminiscing with the residents and finding out what brings them joy.”
Several households have even started their own baking clubs, which has continued to add to the feelings of home – the smell of brownies floating through the households, homemade noodle soup warming stomachs during chilly winter days, and groups gathering in the kitchens to discuss their favorite recipes and memories associated with them.

“The kitchen is the heart of the home, and we want to foster that warm feeling in our households,” said Julie.
Not only did the Extended Family Program bring in the delicious smell of baked goods to waft through the households, but it added more opportunities for residents to gather and listen to music. GlenFields Rehab Services Manager Shannon Alsleben is
an extended family member, and she has coordinated sing-alongs for the holidays, sometimes even bringing in an instrument.
“I love to share my musical talents through singing and bringing my ukulele in for small group songs,” said Shannon.
“This is a great program that gets the residents talking about their favorite memories, and spreads smiles and laughter.”
It hasn’t only been cookies and caroling – several extended family members have dedicated their time and skills to decorate the households for the holidays, including Donna Trebelhorn, Finance Specialist.
“Each holiday, I help decorate the household to make it feel more like home,” said Donna.
For Easter, Donna and Paula hung colorful banners and bunny-cutouts with each of the residents’ names on them, and decorated a tree they keep in the living room, an ever-rotating array of decorations based on the upcoming holiday.
Interested in getting involved?
“Engaging with the residents in this way helps them to feel more at home, not so lonely, and more cared for,” said Donna. “I have always felt the residents are like my own family, so I couldn’t resist the chance to grow closer to them and support their day-to-day activities through this program.”
GlenFields is looking for individuals who would like to share their time and talents in the Extended Family Program.
Activities can include:
• Support special events
• Visit with residents in group settings or individually
• Walk with residents on Prairie Trail, our walking path
• Enjoy a cup of coffee with the resident(s)
• Bring your children to GlenFields to visit the residents
• Help with festive decorations
• Cook or bake
• Share stories
• Play cards
• Help write letters
Volunteers must be 16 years of age or older to participate in the Extended Family Program.
Want to see if the program is for you before committing?
Get started by visiting GlenFields for one hour to share your skills and abilities with the residents. If interested, please call our Volunteer & Marketing Events Coordinator at 320-864-7703 to learn more or tour our space.