TABLE OF CONTENTS





Editor’s Note: All materials for the Journal must be submitted by the first of the month prior to publication.
Co-Editors:
Jim Blaine, MD
Minh-Thu Le, MD
Junior Co-Editor: Andrew K. Le
Managing Editor:
Dalton Boyer
Editorial Committee:
Michael S. Clarke, MD
David Barbe, MD
Jaya LaFontaine, MD
Dalton Boyer
Andrew Le
Jean Harmison
Barbara Hover
SOCIETY OFFICERS
James Rogers, MD
President
Vu Le, MD
Secretary
Jim Blaine, MD
Treasurer
Sanjay Havaldar, MD
Immediate Past President
Council Members:
David Haustein, MD, MBA
Melissa Gaines, MD
Steven Gradney, MD
Keith LaFerriere, MD
Kyle John, MD
Jaya LaFontaine, MD
John Steinberg, MD
Managing Director: Jean Harmison
Executive Office: 4730 S. National Ave. Suite A1 Springfield, MO 65810 email: director@gcms.us
All
by Minh-Thu Le MD, Allergist/Clinical Immunologist, Associate Professor, University of Missouri, Columbia, Pediatric Associate Clinical Director (ACD) of the Springfield Clinical Campus
As time marches forth, we are reminded of how it never stands still and we must change with it. There is so much we can do together and fostering our professional and personal relationships in our physician community is how we will continue to march along without time stealing our own lives.
This edition has our annual Physician Family Day at the Zoo which is always such a reminder that we are stronger together and happy when we see each other and spend time with each other. The 150th celebration of GCMS and fundraiser for the foundation was also recently attended by me and over 180 others. It was a rousing evening and a success on all fronts. We are strong physician community from all walks of life, especially if we continue to foster these relationships. I was very happy to see retired and long-time Springfield allergist, Dr. Wayne Miles at the event and reconnecting with him. You will see other familiar faces while perusing these pages featuring both these important events.
We also have the pleasure of reading two dermatology articles. One from Dr. Michael Swann, a familiar face and respected name in Springfield. The other from Dr. Murphy Mastin, a newer face in our community, in Bolivar, MO, but with roots in this area, attending MU and one of the first graduates of the Springfield Clinical Campus. These are both their first articles for our journal and we are happy to have them!
Executive council member and psychiatrist, Dr. Jaya LaFontaine, converts her CME presentation from Breckinridge into a compelling article about suicide prevention in children and adolescents. We should support our most vulnerable and she reminds us why.
Supporting our pediatric colleagues with public service announcements is one way GMCS is putting our words into action. Marijuana education and the dangers of its use as well as combating vaccine hesitancy and child abuse are more important than ever. A summary of these is here too.
Arvest, the predominant sponsor for GCMS 150th celebration, has a article this issue as well, and reminds us how to make our profession work for us.
Dr. Rogers, current GCMS president, has some words of encouragement in these uncertain times. Do what we always do and on our own “platforms.” And we will go far if we go together!
The practice of medicine is still relevant and communication with our colleagues reminding us of our calling and our reasons why we do this extends to how we affect change in our community. Thank you for engaging in Greene County and the surrounding area, supporting our advertisers, and giving to the foundation! We appreciate you and your membership! Here’s to 150 more years!

PRESIDENT'S PAGE
by James Rogers, MD
As physicians we have a great responsibility to hold ourselves accountable primarily to our patients’ care. We are obligated to advise the best in diagnosis, care, and outcomes while protecting them from harm, bad advice, and our own self-interests. This is a daunting task that we all accept and aspire to live up to through our lifetime of practice.
Realized or not we each have our “platforms” in which we deliver our care. It may be an exam room, OR, procedure suite, institutional grey or beige walls bedecked with stretchers and equipment. This is where we carry out our duties, mostly on an individual basis. This traditional delivery system is the platform by which we deliver care.
If you want to fast – go alone; If you want to far – go together.
These traditional platforms leave schedules full, urgent care’s and ED’s overrun and large swaths of care undelivered. What if we “go together” to deliver care from a different platform?
DWI task force : the horrible mortality and morbidity of drunk driving could not be addressed in the traditional setting. Together, GCMS docs, police, city leaders, and community action groups identified the problem, crafted solutions to intervene, and petitioned for action. This resulted in countless lives saved and injuries. Some of this work enabled the national 0.08 standard for impairment we use today.
High-risk flu vaccines : this simple vaccine with proven benefits was only available in physicians’ offices and a few public health departments – completely inadequate


for traditional distribution over a narrow fall window. Together, GCMS docs, hospital systems, health department, nursing schools, and community partners obtained vaccine, created locations, and gave shots for 13 years and over 30,000 immunizations, drawing national attention and praise.
Caduceus Doctors’ Band: the passion for their music brought this group of docs together and then involved administrators, accountants, lawyers, nurses, and spouses to form the Springfield Music Foundation to provide nursing scholarships. This has continued over the last 36 years and was performed at the GCMS BASH 150year celebration last week.
Each of us makes a difference, every day on our traditional platforms. Just think how we can expand or change our platform and make an impact that changes us and the community we serve!

Tailored Tax, Wealth Management, and Family Office to help you prepare for what’s next.
Modern Strategies for Preventing Skin Cancer
By Michael Swann, MD MS
As a Mohs surgeon and skin cancer expert, I see the effects of chronic sun damage every day—from the subtle signs of photoaging to the more concerning emergence of precancerous lesions and skin cancers. Prevention is not perfect, but it is powerful. Today, we have more tools than ever before to reduce risk, manage early changes, and protect skin at a cellular level.
This article outlines the key preventive strategies I recommend in practice, including cutting-edge therapies like photodynamic treatment and accessible interventions such as mineral-based sunscreens and oral nicotinamide. The best outcomes come from a layered, proactive approach.
Daily Prevention: Mineral-Based Sunscreen
Sunscreen remains the cornerstone of skin cancer prevention. But not all sunscreens are created equal. In our practice, we emphasize mineral-based sunscreens that contain zinc oxide and/or titanium dioxide—physical blockers that reflect UV rays rather than absorb them. Unlike chemical sunscreens, these are photostable, start working immediately, and are less likely to cause irritation or hormone disruption. Chemical sunscreens work like resistors, generally for less than 2 hours and poorly block UVA. UVA is known to cause not only aging rays (elastosis, brown dyspigmentation and blood vessel proliferation), but also melanoma. I do not recommend chemical sunscreens at all and advocate for physical or mineral sun block.
Key recommendations :
-- Daily mineral UVA/UVB protection (look for zinc oxide, titanium dioxide, iron oxide as the primary ingredient)
-- Water resistance if active outdoors
These sunscreens are ideal for daily use, especially on highrisk areas like the face, scalp, neck, and hands. Incidental sun exposure—from walking the dog or sitting in the car— adds up over time. Daily sunscreen use can reduce the risk of squamous cell carcinoma by nearly 40%. 1
For patients with sensitive skin or those wanting cleaner formulations, mineral SPF is the best choice. I keep 10-12 of my favorite sunscreens in office for patients to try that are all mineral based.
Nutritional Support: Oral Nicotinamide

A particularly exciting development in prevention is the use of oral nicotinamide—a form of vitamin B3. In a landmark randomized, placebo-controlled trial published in The New England Journal of Medicine, high-risk patients taking 500mg of nicotinamide twice daily experienced a 23% reduction in new non-melanoma skin cancers over 12 months. 2
Unlike niacin, nicotinamide does not cause flushing. Its protective effect stems by enhancing DNA repair in UV-damaged skin cells & also reducing UV-induced immunosuppression.
I often recommend nicotinamide to:
1- Fair-skinned patients with a history of actinic keratoses or NMSC, particularly patients who get lots of lower extremity squamous cell carcinomas.
2- Organ transplant recipients or immunocompromised individuals
3- Patients with extensive photodamage who want to lower future cancer risk
It is inexpensive, well-tolerated, and evidencebacked—making it one of the most effective preventive supplements we can offer.
Field Therapy: Topical Chemotherapy
For patients with widespread actinic damage—especially those developing clusters of actinic keratoses (AKs)—we use topical chemotherapy to clear damaged cells. The most common agents are:
-- 5 -Fluorouracil (5-FU) – a topical chemotherapy that destroys precancerous cells by interfering with DNA synthesis.
-- Imiquimod – an immune response modifier that stimulates the body to attack atypical skin cells.
These treatments are applied to sun-damaged skin over several weeks, often producing visible redness, scaling, and inflammation as lesions are cleared. The process can be intense, but it’s highly effective in preventing the development of squamous cell carcinoma from untreated actinic keratoses. ³
We often rotate these therapies every few years in patients with significant field cancerization or prior NMSC history. Patients report smoother skin and fewer recurring lesions following treatment.
Precision Therapy: Photodynamic Therapy (PDT)
One of the most targeted ways to treat sun-damaged skin is photodynamic therapy (PDT). This procedure combines a photosensitizing agent (like aminolevulinic acid, or ALA) with a specific light source to selectively destroy precancerous cells.
The process:
-- ALA is applied to the skin and absorbed by abnormal cells.
-- After an incubation period, a blue or red light activates the agent.
-- The resulting chemical reaction selectively destroys actinic keratoses and other damaged cells.
PDT is generally covered by insurance and is especially beneficial for:
-- Patients with extensive AKs on the face or scalp
-- Individuals seeking both medical and cosmetic benefit
-- Patients who prefer a non-topical approach
It’s often better tolerated than topical chemotherapy and leads to smoother skin and fewer recurrences over time. 4,5
Post-procedure redness and peeling may last a few days, but many patients prefer PDT for its convenience and rapid results. This is my preferred method of preventing skin cancer surgery on my own face!
Multimodal Strategy
The most effective skin cancer prevention isn’t built on a single intervention—it’s a comprehensive strategy:
-- Mineral sunscreen every morning, year-round
-- Oral nicotinamide for internal UV defense
-- Topical chemotherapy or photodynamic therapy for widespread actinic damage
This multi-tiered approach allows us to treat both the visible signs and subclinical effects of chronic sun exposure. Prevention isn’t just about avoiding future skin cancers— it’s also about maintaining healthy, resilient skin.
Final Thoughts
Skin cancer is preventable, treatable, and—most importantly—manageable with the right tools. I think having all of the tools at your disposal is important. As a dermatologist, I find prevention far more rewarding than reaction. Whether you’re a high-risk patient or simply someone who wants to protect their skin long-term, these strategies work best when started early and maintained
consistently. In treating skin cancer, the future will be less surgical. Newer PD-1 inhibitors are going to change the landscape of skin cancer treatment. With modern therapies, scientific evidence, and patient-centered care, we can dramatically reduce the burden of skin cancer—one layer of protection at a time.
Warning: Board Certified Mohs does not mean FellowshipTrained
When it comes to surgical treatment of skin cancer, Mohs surgery is gold standard. Fellowships in Mohs surgery are 1-2 years where fellows treat 1000+ skin cancers and perform complex reconstructions and learn cutaneous oncology. Here is the dirty little secret. Over the last 5 years the American board of dermatology has allowed dermatologists with minimal to no Mohs experience to become “board certified” in Mohs by taking an online test without ever training n a fellowship. The politics of this are beyond the scope of this article, but suffice to say that patients have been duped into believing that their “board certified in Mohs” dermatologist actually has fellowship training. Patients are not savvy to understand the difference, but by all intents and purposes if someone is advertising that they are board certified in Mohs but do not say they are fellowship trained, they are a general dermatologist.
Dr. Michael Swann is a board-certified dermatologist and fellowship-trained Mohs surgeon. He is the founder of Swann Dermatology Partners, a comprehensive dermatology group serving Missouri and surrounding regions and has a team of dermatologists and all of the Mohs surgeons are fellowshiptrained and board certified.
References:
1. Narayanan DL et al., Int J Dermatol. 2010;49(9):978–986
2. Chen AC et al., NEJM. 2015;373:1618–1626
3. Szeimies RM et al., Clin Exp Dermatol. 2009;34(6):700–705
4. Szeimies RM et al., J Dtsch Dermatol Ges. 2007;5(12):1065–1076
5. Wang I et al., Lasers Med Sci. 2013;28(2):585–591

Hidradenitis Suppurativa (HS): Rapid Clinical Guide for Physicians
by Dr. Murphy Mastin, MD
Hidradenitis suppurativa is often mistaken for “recurrent boils,” but a quick diagnosis can be made using three criteria: (1) typical lesions—painful nodules, abscesses, draining sinus tracts, and scars; (2) typical locations—axillae, groin, perineal region, inframammary folds, and buttocks; and (3) chronicity—two or more flares in six months. Pearl: patients with “recurrent abscesses in the armpits or groin” likely have HS, not MRSA.
Severity is staged using the simple Hurley system: Hurley I features isolated nodules or abscesses without sinus tracts; Hurley II shows recurrent lesions with sinus tracts or scarring in a limited area; Hurley III presents with diffuse interconnected sinus tracts and disabling disease. This system is fast and adequate for treatment decisions. Diagnosis is clinical; biopsy only if atypical. Order basic labs if systemic therapy is planned and screen for obesity, smoking, metabolic syndrome, depression, inflammatory bowel disease, and arthritis.
Management Principles focus on early recognition to prevent irreversible scarring, a multimodal approach (lifestyle, medical, procedural), and long-term control rather than flare-only treatment. Lifestyle measures include smoking cessation, ≥10 % weight loss (which can reduce severity), loose clothing to minimize friction, antiseptic washes (chlorhexidine or benzoyl peroxide), and mental health support.
Medical therapy varies by severity.
Topical: Clindamycin 1 % lotion twice daily, often with an over-the-counter benzoyl peroxide wash, is first-line for Hurley I or as adjunct therapy.
Oral antibiotics: Doxycycline 100 mg twice daily for 12 weeks is preferred over minocycline for safety. If inadequate, clindamycin 300 mg plus rifampin 300 mg twice daily for 10–12 weeks is supported by evidence, though relapse is common because the effect is anti-inflammatory, not curative.
Hormonal therapy: For women with PCOS features, spironolactone 50–200 mg/day or combined oral contraceptives (avoiding androgenic progestins) can be effective.
Metformin: Especially useful in patients with metabolic syndrome or insulin resistance; studies show lesion reduction with good tolerability and low cost.
Oral roflumilast: A PDE-4 inhibitor (500 µg daily) shows early promise for mild-to-moderate HS with favorable safety but is not yet standard of care.
Biologics: Mainstay for Hurley II–III disease (adalimumab, secukinumab, bimekizumab) and may warrant dermatology referral.
Procedural options include intralesional triamcinolone for rapid relief of nodules and incision and drainage using a punch tool (“mini-I&D”) for acute relief—do not pack wounds, as this increases pain without benefit. Deroofing is
an effective office procedure for Hurley I–II. Wide local excision is the definitive treatment for Hurley III and carries lower recurrence. CO₂ or Nd:YAG laser can be a useful adjunct in surgical centers.
Quick Algorithm

Hurley I (mild)—Lifestyle optimization, topical clindamycin ± short doxycycline course, intralesional steroids for acute nodules, and consider metformin or roflumilast when comorbidities exist.
Hurley II (moderate)—Oral antibiotics (tetracyclines, then clindamycin/rifampin), hormonal therapy in women, transition to biologics if refractory, and deroofing for localized sinus tracts.
Hurley III (severe)—Biologic therapy, surgical referral for wide excision ± laser, and comprehensive supportive care for pain, depression, and metabolic issues.
Key Points for Busy Physicians
HS is a chronic inflammatory disease, not an infection. Recurrent “boils” in skin folds should trigger HS consideration. Avoid routine I&D; if performed, use a punch tool and do not pack. Biologics are standard of care for moderate-to-severe disease. Evidence-based adjuncts include metformin and the emerging option of roflumilast. Multidisciplinary care— dermatology, surgery, primary care, and mental health— improves outcomes.
About Dr. Murphy R. Mastin, MD
Dr. Mastin is a board-certified dermatologist and Medical Director of the Dermatology Department at Citizens Memorial Hospital in Bolivar, Missouri. He graduated from the University of Missouri- Columbia School of Medicine and was one of the first classes to do his clinical rotations in Springfield/Greene County with the joint Springfield clinical campus. He is experienced in medical and procedural dermatology and is actively involved in clinical research. Dr. Murphy is accepting new referrals for HS in his Bolivar clinic.
References
1.North American clinical management guidelines for hidradenitis suppurativa: A publication from the United States and Canadian Hidradenitis Suppurativa Foundations Alikhan, Ali et al. Journal of the American Academy of Dermatology, Volume 81, Issue 1, 76 - 90
2.North American clinical management guidelines for hidradenitis suppurativa: A publication from the United States and Canadian Hidradenitis Suppurativa Foundations Alikhan, Ali et al. Journal of the American Academy of Dermatology, Volume 81, Issue 1, 91 – 101
3.Kimball AB, Jemec GBE, Sayed CJ, et al. Efficacy and safety of bimekizumab in patients with moderate-to-severe hidradenitis suppurativa (BE HEARD I and BE HEARD II): two 48-week, randomised, double-blind, placebo-controlled, multicentre phase 3 trials. Lancet. 2024 Jun 8;403(10443):2504-2519. doi:10.1016/S0140-6736(24)00101-6. PubMed ID: 38795716
4.Ring HC, Egeberg A, Zachariae C, Thomsen SF, Gyldenløve M. Considerable improvement in hidradenitis suppurativa with oral roflumilast therapy. Br J Dermatol. 2022 Nov;187(5):813815. doi: 10.1111/bjd.21744. Epub 2022 Aug 1. PMID: 35791762; PMCID: PMC9805069. 5.Alhusayen R, Dienes S, Lam M, et al. North American clinical practice guidelines for the medical management of hidradenitis suppurativa in special patient populations. J Am Acad Dermatol. 2025 Apr;92(4):825-852. doi:10.1016/j.jaad.2024.11.071. PubMed ID: 39725212
Bringing Physicians Together To Improve the Health Of Our Community Update
by Jim Blaine, MD
Our May/June article in the GCMS Journal detailed our intention to reach out to our patients through local media and social media to provide scientific facts on various topics including:
• Risks associated with use of marijuana by youth
• Preventing Child Abuse
• Vaccine Hesitancy
Unfortunately, this has become necessary due to misinformation (unintended) and disinformation (intended) that has become increasingly prevalent.
We have eight messages on the topic of marijuana use by youth:
Talking Points for Parents and Teens:
1. Marijuana is not a benign drug for teens. The teen brain is still developing, and marijuana may cause abnormal brain development.
2. Teens who use marijuana regularly may develop serious mental health disorders, including addiction, depression, and psychosis.
3. Recreational use of marijuana by anyone under the age of
21 years is illegal and, if prosecuted, may result in a permanent criminal record, affecting schooling, jobs, etc.
4. Never ride in a car with a driver who is under the influence of marijuana. Adults and teens regularly get into serious car accidents while under the influence of marijuana.
5. Marijuana smoke is toxic, similar to secondhand tobacco smoke. The use of vaporizers or hookahs does not eliminate the toxic chemicals in marijuana smoke.
6. Parents: You are role models for your children, and actions speak louder than words. So if you use marijuana in front of your teens, they are more likely to use it themselves.
7. A recent analysis of 4 large trials found that marijuana use during adolescence is associated with reductions in the odds of high school completion and degree attainment.
8. The American Academy of Pediatrics discourage cannabis
use during pregnancy and breast feeding due to safety concerns for the fetus and infant.

These talking points were approved by the American Academy of Pediatrics, the Greene County Medical Society Council, Cox Health System, Mercy Health System, and Burrell Behavioral Health.
To maintain approval from these groups we have agreed, through a Memorandum Of Understanding, summarized below, that we intend to honor for all of the above supporters:
GCMS will:
• Facilitate production and distribution logistics
• Provide full access to MOAAP for collaboration at all stages: scripting, filming, post-production, and finalization
• Ensure transparency and timely communication regarding media timelines and deliverables
• Coordinate with key community health stakeholders and local healthcare systems (CoxHealth and Mercy Health Systems) for content alignment and distribution.
Both parties shall:
• Have equal rights to edit, proofread, and provide substantive input on all materials throughout the production process
• Work collaboratively to ensure content reflects the shared mission and standards of both organizations.
Final Review and Approval:
• No PSA shall be released to the public without written approval from MOAAP and the GCMS Executive Council.
Most of our recordings are complete and we anticipate that we will begin broadcasting soon on local TV, the GCMS web site and social media in an effort to educate teenage patients and their parents. Please call the Greene County Medical Society at 417 887-1017 if you are interested in helping us communicate through the GCMS Community Action Committee.
You can see the list of our current speakers on these topics on the next page.
GCMS PSA Speakers











David Barbe, MD, Mercy Family Practice and Former AMA President
Kofi Asare-Bewuah, MD, Cox Director of Pediatrics
Jennifer Freeman, MD, Mercy Pediatrician
Pat Dix, MD, Cox Neonatologist and High Risk ObGyn
John Burson, MD, Mercy Director of Pediatrics
Jaya LaFontaine, MD, Burrell Child Psychiatrist
Sanjay Havaldar, MD, Cox Gastroenterologist and Former GCMS President
Kyle John, MD, Child Psychiatrist
Kayce Morton, DO, Pediatric Hospitalist and Missouri American Academy of Pediatrics Executive Council
David Haustein, MD, Dean MU School of Medicine, Springfield Campus
Melissa Gaines, MD, Cox Internest and GCMS President Elect
Kat Dull, Executive Director of the Child Advocacy Center
Financial Advice for Health Care Professionals at Every Stage
by Catherine Luikart, Private Banking Advisor, AVP for Arvest Bank – Springfield Region
Health care professionals provide essential services to our community, but one important service banks like Arvest provide for medical professionals is trusted financial advice. This applies to everyone, whether they are a recent med school graduate or new resident, are mid-career or nearing retirement. Careers in the medical field are often demanding, with unique financial situations. An expert financial advisor can help individuals and business owners navigate complex finances, protect assets, plan for retirement and get them on track to achieve long-term financial goals.
Here are some of the tips I would share with health care professionals during different stages of their career.
Early Career Advice (For medical professionals less than 10 years into practice)
• Build and Maintain Strong Credit – Choose a credit card with low interest rates and good rewards, and use it wisely, aiming to spend less than 30% of your available credit. Set up automatic payments to pay the balance off in full and on time each month. Resist the urge to overspend as your income grows. Check your credit score regularly and report errors and fraudulent activity. Research student loan refinancing opportunities and repayment plans that you may qualify for.
• Implement Wealth Management Strategies Early –Automating your savings and putting a portion of your paycheck into a savings or money market account can help build a financial cushion. Contribute to employer-sponsored 401(k)or 403(b) retirement plans – especially if there is an employer match – and consider opening a Roth IRA to take advantage of tax-free growth.
• Explore Physician-Specific Home Loan Options – Some banks, like Arvest, offer specialized mortgage programs for physicians. These loans often allow pre-approval with a signed residency contract, require little to no down payment, waive private mortgage insurance and offer competitive interest rates for easy refinancing.
Mid-Career Mindset (For medical professionals around 10–20 years into practice)
• Maximize Retirement Contributions – Increase 401(k), 403(b) and/or Roth IRA contributions and consider using catchup contributions if you are eligible. Take full advantage of any employer matching and consider deferred compensation plans if they are offered.
• Review and Rebalance Investment Portfolio – As your income stabilizes and your goals become clearer, regularly reassess your asset allocation to align with your timetable,
risk tolerance and changing financial priorities, such as college savings or elder care.

• Protect Income and Build Legacy Plans – Make sure you have disability and life insurance that adequately covers your current earnings, especially if others rely on your income. Create or update your estate plans, including a will, power of attorney and possibly a trust.
Senior Strategy (For professionals 20-plus years into practice or nearing retirement)
• Conduct a Retirement Readiness Check – Assess projected income streams such as Social Security and retirement accounts to plan withdrawal strategies and determine if you are on track or need to adjust allocations.
• Reallocate Assets Strategically – Simplify your finances by paying off any remaining debt, downsizing property and consolidating accounts for easier management. Consider tax strategies for required minimum distributions and health care costs in retirement. If your debts are paid and your dependents are financially independent, consider adjusting large life policies or converting them from term to permanent or using permanent life insurance as part of an estate or tax strategy.
• Transition Planning and Exit Strategy
If you own a private practice, develop a succession or sale plan. If you are employed, consider phased retirement or part-time consulting. Plan how to transition your benefits, maintain your licensure (if desired) and sustain a personal identity beyond medicine.
Bonus Tip for all Stages: Partner with a Financial Advisor
Private banking services offer personalized financial guidance for medical professionals and can assist you with various needs, ranging from lending services to investment planning to disability and life insurance planning. Many professionals may not realize they could qualify for private banking solutions. While qualifying amounts differ by each financial institution, those who utilize a private banker can expect a more tailored experience than traditional banking provides.
The foundation for long-term financial well-being is built by making disciplined and strategic financial decisions now, adjusting your strategy to fit your personal needs at each stage of your career and seeking professional financial advice and assistance.
Catherine Luikart is a Private Banking Advisor, VP for Arvest Bank – Springfield Region. They can be reached at cluikart@arvest.com.
Managing Suicidality and Suicidal Behaviors in the Primary Care Setting
By Jayaprabha V. LaFontaine, MD, MPH, FAPA
Suicidality in the Primary Care Setting
Nearly 45,000 people in the US and more than 800,00 worldwide die by suicide each year. Primary care providers are in a unique position to prevent suicide because of frequent interactions in their clinics with suicidal patients. A meta-analysis published in the Psychiatric Services journal in 2018, showed that 80% of patients had contact with their primary care physician within a year of completed suicide, whereas only 25 to 30 percent had contact with their psychiatrists within a year of their death.
Despite this, there is no data to show that routine screening for suicidality works. It is not possible to determine suicidal intent to suicidal attempt with a high degree of sensitivity or specificity as yet.
Asking

About Firearms And Safety Locks Does Not Increase The Risk Of Suicide. Firearms are the most common method used in more than 50% of suicides in 2023. Federal and state laws in the United States permit clinicians to ask patients about ownership of firearms and to discuss gun safety and courts have affirmed that such inquiries and discussions are permissible. One way to ask this question without judgement would be,
“IF you have guns in the home, are they safely stored?”
It is important to document the presence or absence of guns in the home, as well as whether they are safely stored or not. In many instances, especially in rural areas where hunting is common, guns are not stored under lock and key, and many children are taught to use a gun appropriately in the context of hunting. It then becomes especially important to counsel the parents of those children who know how to hunt with guns, and who express suicidal ideation, that for the purposes of keeping your child safe, certain precautions would be appropriate until such time as the child has recovered from the mental health emergency.
Other risk factors often associated with suicides are history of Previous Suicide Attempts, Psychiatric Disorders, and Severity of Illness.
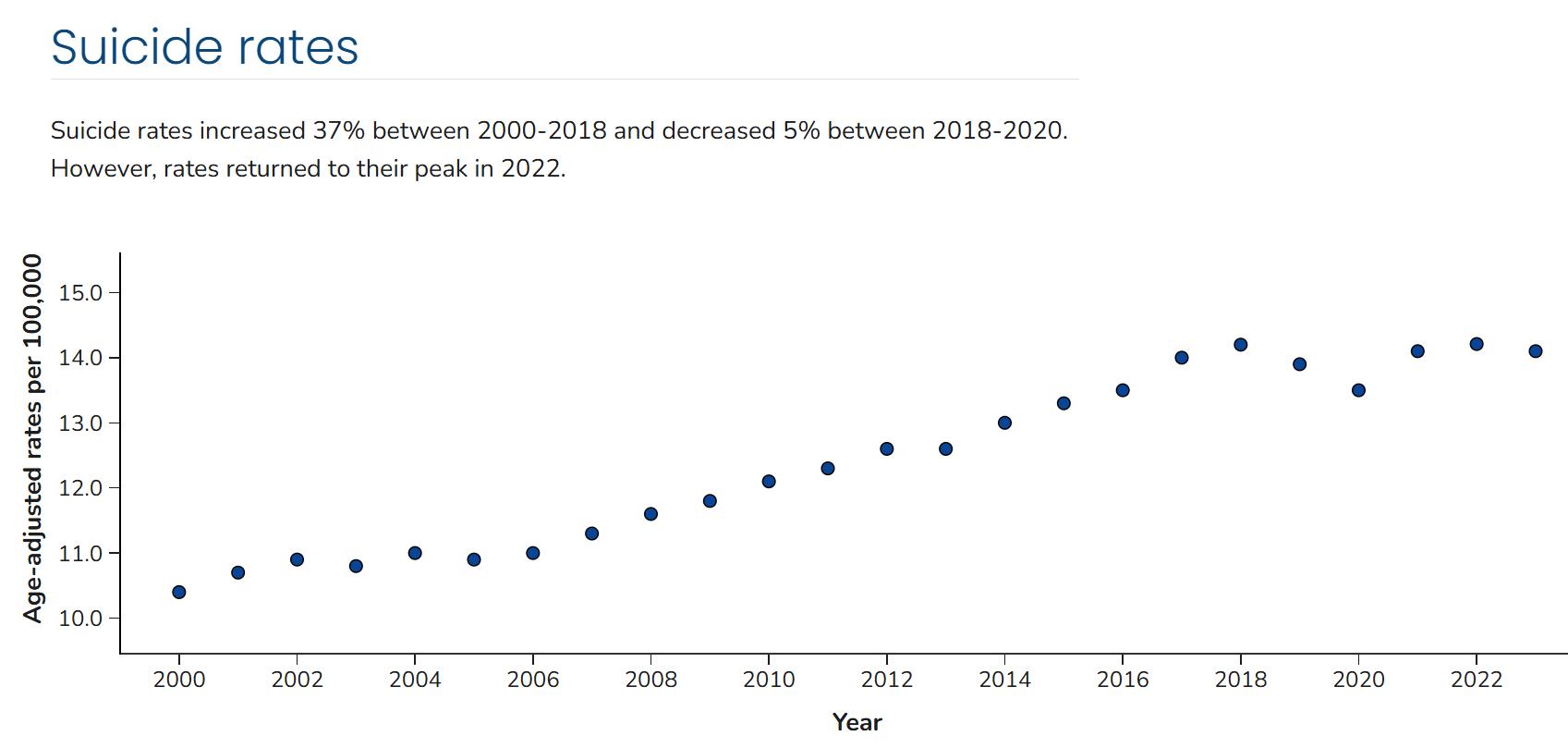
Over 49,000 people died by suicide in 2023, which is 1 death every 11 minutes. While 12.8 million seriously thought about suicide, 3.7 million made a plan for suicide, and 1.5 million attempted suicide.
Age-adjusted death rates by suicide in the US are high, with several states having between 20.31 to 28.15 per 100,000. Missouri’s age adjusted death rate by per 100,000 is 18. Statistics provided by the CDC show that some groups have disproportionately higher rates of suicide than others. Non-Hispanic American Indian and Alaskan Indian have the highest rates of 23.8 per 100,000, followed by Non-Hispanic White at 17.6 per 100,000 and Non-Hispanic Native Hawaiian/Other Pacific Islander at 17.3 per 100,000.
Males make up 50% of the US population and 80% of completed suicides. Age adjusted rates of suicide for men is 22.7 per 100,000 and 5.9 out of 100,000 in women. People 85 and older had the highest rates of suicide at 22.7 per 100,000, followed by those 75- 84 years of age, at 19.4 per 100,000.
The lifetime risk of suicide is 8.6% with previous inpatient for suicidal ideation, while it is only 0.5% in general population. Of these, 41% completed suicide, and had been psychiatrically hospitalized in the previous year. Most shockingly, 9% of suicides occurred within one day of discharge.
Suicides are most associated with MDD, Personality Disorders, Bipolar depression, Anxiety Disorders including Panic Disorder, Alcoholism and Substance Use, PostTraumatic Stress Disorder, Schizophrenia, Delirium.
Psychological risk factors include hopelessness, occupation- worse in unskilled than skilled jobs, marital status (single > married), nurses > physicians, sexual preference (bisexual: 16%, gay or lesbian: 11%, straight: 6%, lifetime suicide attempts 4x higher in sexual minorities), military service, medical illness (asthma, cancer, COPD), chronic pain. Additionally, childhood history of adversity results in up to a four-fold increase in suicidality adults when compared to the general population (sexual abuse >
physical abuse > emotional abuse > physical neglect).
The heritability of suicide is in the range of 30 to 50 percent, which makes it important to ask about family history of suicidal attempts and completed suicides just as we would ask about cancer, diabetes, and cardiovascular illness. The highest rates of suicide in the US are found in rural areas.
The Neuroscience Of Depression: Depression is characterized by Dysfunction in the hypothalamic-pituitary-adrenal axis, the nucleus accumbens, hippocampus, amygdala, anterior cingulate gyrus, dorsolateral prefrontal cortex, and orbital frontal cortex.
Despite various analyses done to associate regions of the brain with specific mental health states have been done, all of these have resulted in inconsistent results. Some of the PET and SPECT scans done in treatment states for mental illness has shown the following: that ECT turns “down” the frontal cortex, as does CBT, however anti-depressants, vagal nerve stimulation, and transcranial magnetic stimulation turns “up” the prefrontal cortex, with all of these modalities being used for the treatment of major depression.
Functional connectivity has been used to explain some of these inconsistencies. Functional connectivity refers to a mathematical calculation estimating correlations between different regions of the brain, whereby different illness states are explained by the interaction of various regions of the brain with each other. For example, the default mode network refers to the state of the brain at rest. In depression, there is a hypoconnectivity in the frontoparietal network; hyperconnectivity between the frontoparietal network and the default mode network.
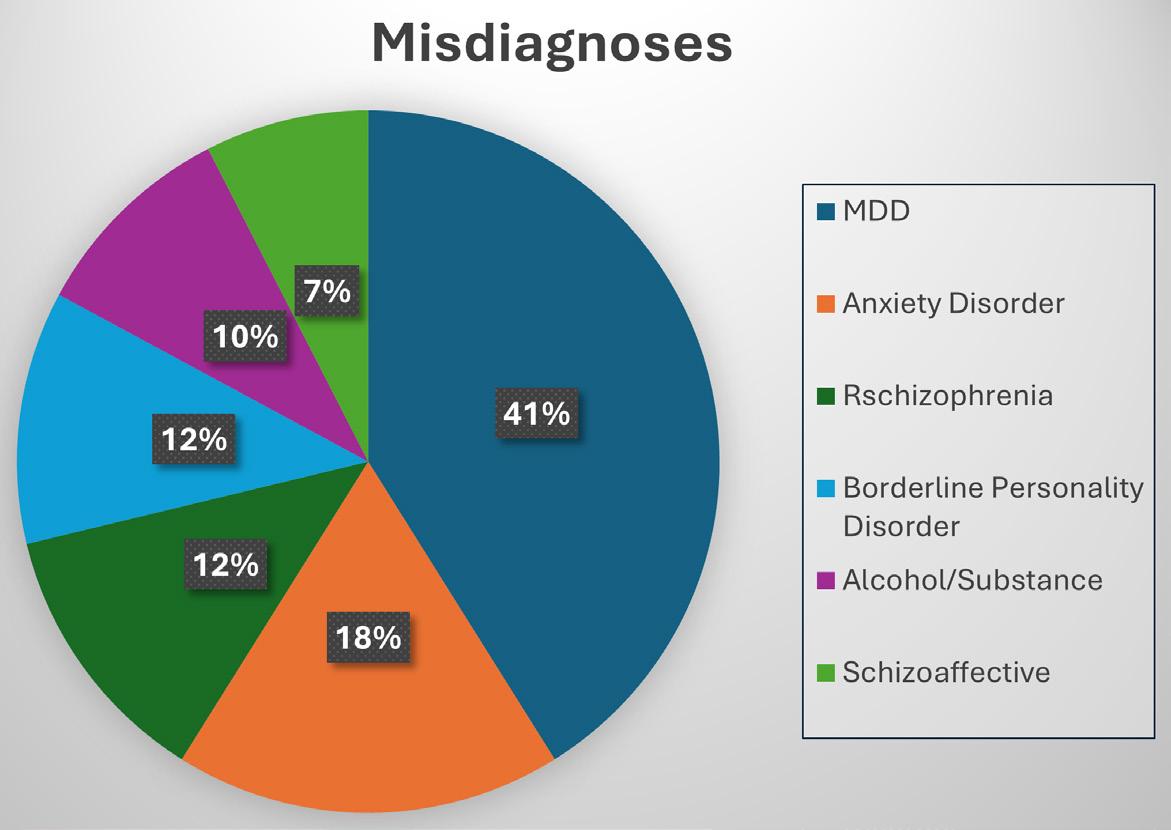
Misdiagnoses:
In the year 2000, researchers performed a wide-reaching survey to evaluate the rates of bipolar disorder in the population. They found that 69%of patients with bipolar
disorder were misdiagnosed when tested for the illness several years after initial evaluation; of that s69%, 60%were misdiagnosed as unipolar depression, twenty-six percent as anxiety disorder, 18% as schizophrenia, 17% as borderline or antisocial personality disorder, 14% as alcohol abuse/ dependence, and 11% as schizoaffective disorder.
This is especially concerning as suicides in bipolar disorder are very high. Bipolar disorder is one of the most lethal of all psychiatric conditions, where morbidity in Bipolar II is potentially higher than in Bipolar I. 25% to 60% of those with diagnosed bipolar disorder attempt suicide at least once, 4% To 19% complete suicide. Individuals with Bipolar II use significantly more violent and lethal methods than do individuals with Bipolar I.
Psychopharmacology: Anti-Depressants And The Fda
In 1990, case reports described intense suicidal ideation with fluoxetine. In 2003, the FDA published an advisory in response to numerous reports of suicide ideation, suicide attempts, and completed suicides in children on antidepressants. By 2004, this advisory was elevated after data from pediatric randomized trials of bupropion, citalopram, scitalopram, fluoxetine, fluvoxamine, mirtazapine, nefazodone, paroxetine, sertraline, venlafaxine, showed an increased risk of suicidal ideation, preparatory acts for self-harm, or nonfatal self-harm occurring during the first weeks of treatment with an antidepressant, compared with placebo.
In 2005, the FDA published an advisory about suicidality in adults treated with antidepressants, and in 2007, they extended this advisory to adults 18 – 24 years, though did not advise against the prescribing of these meds for depression and anxiety.
Despite this, there are countless studies also showing that the risk of suicidality in untreated depressed patients is much higher than the risk of suicidality in those not on antidepressants.
Anti-Depressants And Bipolar Disorder
Nonetheless, the practice of using antidepressant (AD) monotherapy in the management of bipolar disorder has a lack of evidence for efficacy. The following are specific studies showing data relating to the use of anti-depressants:
• Fornaro et al (2018): A meta-analysis of 12 prospective studies showed the cumulative incidence of antidepressant treatment-emergent mania in 1,316 BP depressed patients over 20 randomized controlled trials was 11.8%.
• Another meta-analysis done by the same group of 15 retrospective studies (4,767)- 30.9% cumulative incidence of treatment-emergent mania.
• The discrepancy may be related to possible underreporting in RCTs, and over-reporting in observational studies. Another variable may be the different criteria
used in studies.
• Tondo et al (2010): A meta-analysis of 35 studies showed that the risk of spontaneous switch from depression to mania was high (13.8%), but risk of switch after AD initiation was slightly higher (15.3%).
• 2015: NHS Retrospective cohort study of 21,000+ adults with dx of unipolar depression on anti-depressants showed an increased risk of subsequent mania/bipolar disorder, with a significant association with SSRIs and venlafaxine.
• Other studies: have implicated Tricyclics and SNRIs > SSRIs.
So, What Do We Do?
Given the statistics that show a lack of change in the rate of suicides over the years, especially in the child and adolescent population, one suggestion would be that medical providers do not hesitate to make the diagnosis of bipolar disorder if they see more than 3 of the following symptoms:
• lack of or the need for sleep over several days.
• unusual energy
• increased goal-directed activities
• family history of bipolar disorder
• earlier onset of illness
• seasonality
• number of past episodes
• history of psychiatric hospitalization.
• mixed states
• mood reactivity
• history of treatment-resistant depression
• anti-depressant-related mania/hypomania
- Taken from: Make the Diagnosis: “Progression from MDD to Bipolar Disorder”Fiedorowicz JG, et al Am J Psych. 2011
Mood Stabilizers And Antipsychotics
Management of bipolar depression is limited because only three medications (olanzapine-fluoxetine combination, quetiapine, and lurasidone) are approved by FDA, whereas 10 FDA-approved medications are available for manic/hypomanic states: lithium, divalproex sodium,

carbamazepine ER, risperidone, ziprasidone, aripiprazole, asenapine, cariprazine, olanzapine, and quetiapine.
Other Pharmacological Options:
For several decades, lamotrigine has been used as first-line for bipolar disorder in various states, including depression, mania/hypomania, and mixed states. It is generally prescribed as 25mg by mouth daily for two weeks, then increase to 25mg twice a day. The dosage can be doubled every two weeks. Risk of Stevens Johnsons Syndrome, a severe hypersensitivity reaction with 50% mortality once the condition spreads to mucosal membranes, is extremely rare. However, it is due to this rare possibility that it is often not considered as a treatment by providers. A benign rash is much more common in some patients, which resolves easily with stopping the medication, and coverage with antihistamines. However, it remains a viable option in bipolar disorder, especially due to its lack of metabolic dysregulation, weight neutrality, and lack of sedation effects- all of which are very common with anti-psychotic medications.
The Gold Standard: Lithium
Lithium has long remained the gold standard for bipolar disorder, and in recent years has been used as adjunctive medication in major depression as well to prevent suicidality specifically. A meta-analysis of four trials (485 patients with either condition) compared lithium with placebo for continuation and maintenance treatment for 20 –104 eeks. Most responded acutely to open label lithium as monotherapy or in combination with an anti-depressant. The target lithium level 0.8 to 1.2 mEq/L. Despite this, lithium is rarely considered as first line by medical providers due to various side effects to the thyroid, parathyroid, and kidneys. Also, due to the narrow therapeutic window and the need to monitor levels closely, it increases the burden on the patient to maintain treatment on the substance. Of particular note is that being on lithium and its particular effects on the kidneys, dehydration can be a significant cause of lithium toxicity, especially if exposed to heat and the sun.
Prior meta-analysis found maintenance treatment with lithium prevented suicide in patients with all types of mood disorders. All-cause mortality was also less likely with lithium than other compounds. It is generally prescribed with an adult starting dose of 300mg two to three times a day, but can be increased to 300mg – 600mg every one to five days. The child's starting dose would be: for weight less than 30kg, 300mg twice daily and increase by 300mg/day/ week, with a maximum dose of 40mg/kg/day.
Monitoring is done generally 3-7 days after initiation of treatment, with a morning trough level (12 hours after last dose), with adjustment to the dosage based on the therapeutic level and symptom improvement.
In summary, treating depression is always better than not. wait times for psychiatry appointments are very high nationally. Locally in Springfield, Wait times are much lower, especially at Burrell Behavioral Health for both adults as well as children and adolescents. Still, there is opportunity at every single medical visit in every clinic to intervene in a meaningful way for patients suffering with mental illness. Therefore, please DO NOT WAIT to treat. Suicidality is most often caused by depression and an SSRI or SNRI will help. However, if you see “activation” on an anti-depressant, check for family history and risk factors. If the patient is meeting most criteria and at least three risk factors, consider switching the anti-depressant to a mood stabilizer/second generation anti-psychotic, and refer to psychiatry. As always, if acutely suicidal, call 911/988 or send the patient immediately for evaluation for psychiatric hospitalization. Together, we can step up for our mentally ill children and adolescents no matter what doctor’s office they walk into, if we are willing to accept mental health as health.
References:
• Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS). Leading Causes of Death Reports 1981 - 2016. Atlanta, GA. U.S department of Health and Human Services. https://www.cdc.gov/ injury/wisqars/fatal.html (Accessed on April 17, 2018).
• Suicide Data and Statistics | Suicide Prevention | CDC
• Walby FA, Myhre MØ, Kildahl AT. Contact With Mental Health Services Prior to Suicide: A Systematic Review and Meta-Analysis. Psychiatr Serv. 2018 Jul 1;69(7):751-759. doi: 10.1176/appi.ps.201700475. Epub 2018 Apr 16. PMID: 29656710.
• Bostwick JM, Pankratz VS. Affective disorders and suicide risk: a reexamination. Am J Psychiatry. 2000 Dec;157(12):1925-32. doi: 10.1176/appi.ajp.157.12.1925. PMID: 11097952.
• Ribeiro JD, Huang X, Fox KR, Franklin JC. Depression and hopelessness as risk factors for suicide ideation, attempts and death: meta-analysis of longitudinal studies. Br J Psychiatry. 2018 May;212(5):279-286. doi: 10.1192/bjp.2018.27. Epub 2018 Mar 28. PMID: 29587888.
• Kyung-Sook W, SangSoo S, Sangjin S, Young-Jeon S. Marital status integration and suicide: A meta-analysis and meta-regression. Soc Sci Med. 2018 Jan;197:116126. doi: 10.1016/j.socscimed.2017.11.053. Epub 2017 Dec 22. PMID: 29227910.
• Salway T, Ross LE, Fehr CP, Burley J, Asadi S, Hawkins B, Tarasoff LA. A Systematic Review and Meta-Analysis of Disparities in the Prevalence of Suicide Ideation and Attempt Among Bisexual Populations. Arch Sex Behav. 2019 Jan;48(1):89-111. doi: 10.1007/s10508-018-1150-6. Epub 2018 Feb 28. PMID: 29492768.
• Milner A, Spittal MJ, Pirkis J, LaMontagne AD. Suicide by occupation: systematic review and meta-analysis. Br J Psychiatry. 2013 Dec;203(6):409-16. doi: 10.1192/bjp.bp.113.128405. PMID: 24297788.
• Davis MA, Cher BAY, Friese CR, Bynum JPW. Association of US Nurse and Physician Occupation With Risk of Suicide. JAMA Psychiatry. 2021 Apr 14;78(6):1–8. doi: 10.1001/jamapsychiatry.2021.0154. Epub ahead of print. PMID: 33851982;
PMCID: PMC8047773.
• Juurlink DN, Herrmann N, Szalai JP, Kopp A, Redelmeier DA. Medical illness and the risk of suicide in the elderly. Arch Intern Med. 2004 Jun 14;164(11):1179-84. doi: 10.1001/archinte.164.11.1179. PMID: 15197042.
• Petrosky E, Harpaz R, Fowler KA, Bohm MK, Helmick CG, Yuan K, Betz CJ. Chronic Pain Among Suicide Decedents, 2003 to 2014: Findings From the National Violent Death Reporting System. Ann Intern Med. 2018 Oct 2;169(7):448-455. doi: 10.7326/M18-0830. Epub 2018 Sep 11. PMID: 30208405; PMCID: PMC6913029.
• Devries KM, Mak JY, Child JC, Falder G, Bacchus LJ, Astbury J, Watts CH. Childhood sexual abuse and suicidal behavior: a meta-analysis. Pediatrics. 2014 May;133(5):e1331-44. doi: 10.1542/peds.2013-2166. Epub 2014 Apr 14. PMID: 24733879.
• Egeland JA, Sussex JN. Suicide and family loading for affective disorders. JAMA. 1985 Aug 16;254(7):915-8. PMID: 4021024.
• Qin P, Agerbo E, Mortensen PB. Suicide risk in relation to family history of completed suicide and psychiatric disorders: a nested case-control study based on longitudinal registers. Lancet. 2002 Oct 12;360(9340):1126-30. doi: 10.1016/S01406736(02)11197-4. PMID: 12387960.
• Rubin R. Suicide Rates Higher in Rural Areas for Most Demographic Groups. JAMA. 2017 Nov 28;318(20):1969. doi: 10.1001/jama.2017.17273. PMID: 29183084.
• Kaufman EJ, Morrison CN, Branas CC, Wiebe DJ. State Firearm Laws and Interstate Firearm Deaths From Homicide and Suicide in the United States: A Crosssectional Analysis of Data by County. JAMA Intern Med. 2018 May 1;178(5):692-700. doi: 10.1001/jamainternmed.2018.0190. PMID: 29507953; PMCID: PMC5885268.
• Wintemute GJ, Betz ME, Ranney ML. Yes, You Can: Physicians, Patients, and Firearms. Ann Intern Med. 2016 Aug 2;165(3):205-13. doi: 10.7326/M15-2905. Epub 2016 May 17. PMID: 27183181.
• Teicher MH, Glod C, Cole JO. Emergence of intense suicidal preoccupation during fluoxetine treatment. Am J Psychiatry. 1990 Feb;147(2):207-10. doi: 10.1176/ ajp.147.2.207. PMID: 2301661.
• Reports of Suicidality in Pediatric Patients Being Treated with Antidepressant Medications for Major Depressive Disorder (MDD) October 27, 2003. Available at: http://www.fda.gov/Drugs/DrugSafety/ PostmarketDrugSafetyInformationforPatientsandProviders/ DrugSafetyInformationforHeathcareProfessionals/PublicHealthAdvisories/ ucm168828.htm (Accessed on October 05, 2010).
• Gunnell D, Saperia J, Ashby D. Selective serotonin reuptake inhibitors (SSRIs) and suicide in adults: meta-analysis of drug company data from placebo controlled, randomised controlled trials submitted to the MHRA's safety review. BMJ. 2005 Feb 19;330(7488):385. doi: 10.1136/bmj.330.7488.385. Erratum in: BMJ. 2006 Jul 1;333(7557):30. PMID: 15718537; PMCID: PMC549105.
• Sharma T, Guski LS, Freund N, Gøtzsche PC. Suicidality and aggression during antidepressant treatment: systematic review and meta-analyses based on clinical study reports. BMJ. 2016 Jan 27;352:i65. doi: 10.1136/bmj.i65. PMID: 26819231; PMCID: PMC4729837.
GCMS Celebrates 150 Years



























Physician Family Day at the Zoo
by Barbara Hover, GCMS Alliance Chair
Physician Family Day was celebrated at the Dickerson Park Zoo on August 23. The weather was perfect and the docents and volunteers at the zoo provided personal encounters with snakes, giraffes, and other animals. We would like to thank Dr. Ed and Pam Gwin for serving as docents again this year. Thanks to the generosity of Ferrell Duncan Clinic Foundation, the GCMS Foundation, and GCMS Alliance, over 350 physicians and family members spent a fun filled evening with their families and colleagues in the relaxed atmosphere of the zoo. Greene County Medical Society Alliance is focused on providing activities and programs to mitigate the impact of work stress on the physician. This is one of our most popular events.
Our 2026 membership drive has begun, and we hope you will consider becoming a part of the Alliance. Our mission is to improve the health and well-being of the community around us with a special emphasis on physician and family wellness. We offer both social and volunteer opportunities. Our next Alliance event is brunch at JW’s Kitchen on Oct. 21 at 10:30 am. Please join us for great food and conversation. We hoped to see you there.











































WE TAKE PRIVATE BANKING PERSONALLY.
With Private Banking at Central Bank, you have exclusive access to a host of financial services and products, where we take care of the details across the full spectrum of the bank. You will have access to higher deposit rates, custom credit solutions and home financing, as well as individualized guidance with your investments. Our main goal is to help you maximize your money seamlessly. You have complex needs. We have the concierge level solutions you want.



STEVE GASSEL
Senior Vice President - Director of Private Banking | NMLS # 554828
3333 S. National Ave., Springfield, MO 65807
Phone: (417) 841-4213
Steve.Gassel@centralbank.net
KARA TURNER
Vice President - Private Banking | NMLS # 1833785
3333 S. National Ave., Springfield, MO 65807
Phone: (417) 841-4253
Kara.Turner@centralbank.net
JOYCE WONG-HSU
Officer - Private Banking | NMLS # 1239617
3333 S. National Ave., Springfield, MO 65807
Phone: (417) 841-4214
Joyce.Wong-Hsu@centralbank.net
professional
To Advertise in this directory call Jean Harmison at the Society office: 417-887-1017.
Please Note: Changes to ads will be made quarterly and must be submitted in writing.
H Denotes GCMS Membership “A” Denotes GCMS Applicant
GCMS Member Ad Rates: $10.00 per 2” sq. • Non-Member Ad Rates: $13.75 per 2”sq.
Mission Statement
Bringing physicians together to improve the health of our community.
Dermatology, Procedural
MICHAEL H. SWANN, MD H
BRETT NEILL, MD
MICHAEL KREMER, MD
JOHN CANGELOSI, MD
AUTUMN BERTHOLDI, PA-C
PATSY DUGGAN, PA-C
LORI MILLER, NP-C
HANNAH LEE, FNP-BC
BROOKLYN FORT, FNP-C
3850 S. National Ave, Suite 705 Springfield, MO 65807 (Located inside Hulston Cancer Building-7th floor)
1240 E. Independence Springfield, MO 65804
Phone: 417-888-0858 • Fax: 417-889-0476 www.swanndermatology.com
Hollister Location 590 Birch Rd, Ste 2c Hollister, MO 65672
PH. 417-690-3858 Fax 417-690-3862
Monett Satellite Location (Inside CoxHealth Urgent Care) 2200 E. Cleveland Ave Monett, MO 65708
Phone: 417-888-0858 • Fax: 417-889-0476
Lebanon Location 331 Hospital Drive Suite C Lebanon, MO 65536
Phone : 417-344-7200
Fax : 417-344-7299
Direct Primary Care
ASCENT DIRECT PRIMARY CARE, LLC
MATTHEW GREEN, DO H
Family Medicine www.ascentdpc.com 417-595-0956
413 N McCroskey, Ste 2 Nixa, MO 65714
Eye Surgery/Ophthalmology
EYE SURGEONS OF SPRINGFIELD, INC.
C. BYRON FAULKNER, MD H Comprehensive Cataract Ophthalmology
JUDD L. McNAUGHTON, MD H Comprehensive Cataract Ophthalmology Diplomates, American Board of Ophthalmology
1330 E. Kingsley St. • Springfield, MO 65804 Phone 417-887-1965 • Fax 417-887-6499 417eyecare.com
Eye Surgery/Ophthalmology
MATTAX • NEU • PRATER
EYE CENTER
JAMES B. MATTAX, JR., MD, FACS H American Board of Ophthalmology
LEO T. NEU III, MD, FACS H American Board of Ophthalmology
DAVID NASRAZADANI, MD
DREW A. YOUNG, MD
THOMAS PRATER, MD, FACS H American Board of Ophthalmology
JACOB K. THOMAS, FACS, MD H American Board of Ophthalmology
BENJAMIN P. HADEN, MD H American Board of Ophthalmology
MICHAEL S. ENGLEMAN, OD
MARLA C. SMITH, OD
MATTHEW T. SMITH, OD
1265 E. Primrose Springfield, MO 65804 417-886-3937 • 800-995-3180
Family Medicine
COXHEALTH
FAMILY MEDICINE RESIDENCY
FAMILY MEDICAL CARE CENTER
3800 S National Ste 700 Springfield, MO 65807 (417) 269-8817
AmericAn BoArd of fAmily medicine
Marc Carrigan, MD
Cameron Crymes, MD
Kristin Crymes, DO
Kristen Glover, MD
Kyle Griffin, MD
Shelby Hahn, MD
Laura Isaacson, DO
Evan Johnson, MD
Katie Davenport-Kabonic, DO
Michael Kabonic, DO
Jessica Standeford, MD
Gynecology
WOMAN’S CLINIC www.womansclinic.net
Leaders in Minimally Invasive Gynecology & Infertility
DONALD P. KRATZ, MD, FACOG H American Board of Obstetrics and Gynecology
AMY LINN, FNP-BC American Academy of Family Nurse Practitioners
ANGIE JONES, WHNP-BC 1135 E. Lakewood, Suite 112 Springfield, MO 65810
Located inside Tri-Lakes Family Care 1065 Hwy 248 Branson, MO 65616
Phone 417-887-5500 Fax 883-8964 or toll free 877-966-2607 Monday-Thursday 8am-4:30pm Friday 8am-12pm
Internal Medicine
MERCY CLINIC–INTERNAL MEDICINE WHITESIDE
RAJ ANAND, MD
JAMES T. ROGERS, JR. MD, FACP H Board Certified in Internal Medicine
MARIA DELA ROSA, MD
NELSON DELA ROSA, MD
AMANDA MCALISTER, MD
ALEJANDRA ROA, MD
KELLY TRYGG, MD
GABBY BONNER, NP
STEVEN BOWLIN, MD Board Certified in Internal Medicine
STEPHANIE HOVE, NP
CARRIE KUGLER, PA COURTNEY WEATHERFORD, PA
JENNIFER WHITE, PA
VICTOR GOMEZ, MD Board Certified in Internal Medicinee 2115 S. Fremont, Suite 2300 Springfield, MO 65804
Phone 417-820-5600 Fax 417-820-5606
Urology
MERCY CLINIC UROLOGY (FREMONT)
ERIC P. GUILLIAMS, MD, FACS H American Board of Urology
ROBERT D. JOHNSON, MD, FACS H American Board of Urology
TYRUN K RICHARDSON, MD American Board of Urology
Phone 417-820-0300
Fax 417-882-9645
1965 S Fremont, Ste. 370 Springfield, MO 65804
ADULT MEDICINE & ENDOCRINOLOGY
JONBEN D. SVOBODA, MD, FACE, ECNU
American Board of Endocrinology
JAMES T. BONUCCHI, DO, ECNU, FACE
American Board of Endocrinology
NICOLA W. GATHAIYA, MD, ECNU, FACE, CCD
American Board of Internal Medicine
American Board of Endocrinology
STEPHEN M. REEDER, MD, FACP
American Board of Internal Medicine
ANA MARCELLA RIVAS MEJIA, MD, CCD
American Board of Internal Medicine
American Board of Endocrinology
JACQUELINE L. COOK, FNP-BC, CDCES, CCD
KELLEY R. JENKINS, FNP-C, CDCES
ALINA CUMMINS, PA-C
STACY GHOLZ, FNP-C
SHELLEY L. CARTER, DNP
JESSICA A. CROUCH, FNP-C
Phone (417) 269-4450
960 E. Walnut Lawn, Suite 201 Springfield, MO 65807
Nephrology
SPRINGFIELD NEPHROLOGY ASSOCIATES, INC.
1911 South National, Suite 301 Springfield, MO 65804
Phone 417-886-5000 • Fax 417-886-1100 www.springfieldnephrology.com
STEPHEN E. GARCIA, MD H
American Board of Internal Medicine
American Board of Nephrology
ETHAN T. HOERSCHGEN, MD
American Board of Internal Medicine
American Board of Nephrology
GISELLE D. KOHLER, MD H
American Board of Internal Medicine
American Board of Nephrology
DAVID L. SOMMERFIELD, MD
American Board of Internal Medicine
American Board of Nephrology
SUSAN A. WOODY, DO H
American Board of Internal Medicine
American Board of Nephrology
Neurosurgery
SPRINGFIELD NEUROLOGICAL AND SPINE INSTITUTE
CoxHealth Jared Neuroscience
West Tower • 3801 S National, Ste 700 Springfield, MO 65807 • 417-885-3888
Neurosurgery:
H. MARK CRABTREE, MD, FACS
EDWIN J. CUNNINGHAM, MD
MAYUR JAYARAO, MD
J. CHARLES MACE, MD, FACS H
CHAD J. MORGAN, MD
MICHAEL L. MUMERT, MD
SALIM RAHMAN, MD, FACS
ANGELA SPURGEON, DO
ROBERT STRANG, MD
Interventional Neuroradiology
MICHAEL J. WORKMAN, MD
Physiatry:
TED A. LENNARD, MD
KELLY OWN, MD
JESSE STOKKE, DO
Physician Assistants:
JOSHUA BARBIERI, PA-C
MARK BROWN, PA-C
ERIC CHAVEZ, PA-C
KEVIN STOKES, PA-C
HEATHER TACKETT, PA-C
Nurse Practitioner:
EMILY CROUSE, NP-C
MINDY GRANT, NP-C
ROZLYN MCTEER, FNP
BRANDON RUBLE, ACNP-AG
ALYSSA CHASTAIN, FNP
Obstetrics/Gynecology
COXHEALTH
PRIMROSE OB/GYN
MARCUS D. MCCORCLE, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
THOMAS M. SHULTZ, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
GREGORY S. STAMPS, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
P. MICHAEL KIDDER, DO, FACOOG
Diplomate, American Osteopathic Board of Obstetrics & Gynecology
Phone 882-6900
1000 E. Primrose • Suite 270 Springfield, MO 65807
Obstetrics/Gynecology
SPRINGFIELD OB/GYN, LLC
MATTHEW H. TING, MD, FACOG H
American Board of Obstetrics & Gynecology
909 E. Montclair, Suite 120 Springfield, MO 65807
Phone 417/882-4466 • Fax 417/890-5631
Oncology/Hematology
ONCOLOGYHEMATOLOGY
ASSOCIATES OF SPRINGFIELD, MD, P.C.
WILLIAM F. CUNNINGHAM, MD, FACP
American Board of Internal Medicine
American Board of Medical Oncology
JIANTAO DING, MD H
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
ROBERT J. ELLIS, MD, FACP
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
BROOKE GILLETT, DO
American Board of Internal Medicine
American Board of Medical Oncology
V. ROGER HOLDEN, MD, PhD
American Board of Hematology
American Board of Medical Oncology
DUSHYANT VERMA, MD, FACP
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
Springfield Clinic 3850 S. National, Ste. 600 Springfield, Missouri 65807
Monett Clinic 802 US Hwy 60 Monett, Missouri 65708
Phone 882-4880 Fax 882-7843
Visit our website: www.ohaclinic.com
MERCY CLINIC–EAR, NOSE & THROAT
BENJAMIN L. HODNETT, MD, PHD H
ERICH D. MERTENSMEYER, DO, FAOCOO
AARON R. MORRISON, MD
RAJEEV MASSON, MD
MARK J. VAN ESS, DO, FAOCOO
Diplomates, American Board of Otolaryngology
SHELBY BRITT, PA
MELISSA COONS, FNP
TAHRA LOCK, NP
ELIZABETH (BETSY) MULLINGS, FNP
PAUL STRECKER, FNP
Audiology
JASON BOX, AuD, CCC-A
MAMIE JAYCOX, AuD, CCC-A
JENNIFER PLOCH, AUD
ALLISON WHITE, AUD, CCC-A
Phone 417-820-5750 Fax 417-820-5066
1229 E. Seminole, Ste. 520 Springfield, MO 65804
Plastic Surgery
MERCY CLINIC–FACIAL PLASTIC SURGERY
MATTHEW A. KIENSTRA, MD, FACS
American Board of Facial Plastic & Reconstructive Surgery
American Board of Otolaryngology
Phone 417-887-3223
1965 S. Fremont, Ste. 120 Springfield, MO 65804 facialplasticsurgeon.com
Psychiatry
JAMES E. BRIGHT, MD H Diplomate, American Board of Psychiatry & Neurology.
Practice Limited to: Adult Psychiatry
Phone 882-9002
1736 E. Sunshine, Ste. 400 Springfield, MO 65804

chAnge Service requeSted