

Brian Biggers, MD



Brian Biggers, MD
July 14-16


September 20







Editor’s Note: All materials for the Journal must be submitted by the first of the month prior to publication.
Co-Editors:
Jim Blaine, MD
Minh-Thu Le, MD
Public Health Editor: Nancy Yoon, MD
Junior Co-Editor: Andrew K. Le
Managing Editor: Dalton Boyer
Editorial Committee:
Michael S. Clarke, MD
David Barbe, MD
Jaya LaFontaine, MD
Dalton Boyer
Andrew Le
Jean Harmison
Barbara Hover
Nancy Yoon, MD
Frank Cornella, MD
SOCIETY OFFICERS
James Rogers, MD President
Vu Le, MD
Secretary
Jim Blaine, MD
Treasurer
Sanjay Havaldar, MD Immediate Past President
Council Members:
David Haustein, MD
Melissa Gaines, MD
Steven Gradney, MD
Keith LeFerriere, MD
Kyle John, MD
Jaya LaFontaine, MD
Nancy Yoon, MD
John Steinberg, MD
Managing Director: Jean Harmison
Executive Office:
4730 S. National Ave. Suite A1 Springfield, MO 65810 email: director@gcms.us
by Minh-Thu Le MD, Allergist/Clinical Immunologist, Associate Professor, University of Missouri, Columbia, Pediatric Associate Clinical Director (ACD) of the Springfield Clinical Campus
I thought I’d put another title most people reading this may not be aware of in my by-line this month. Why, you may ask? This is the journal edition where there is a focus on the medical students and those that teach them. Even on the cover, our new MSMA president, Dr. Brian Biggers, is also an ACD (Associate Clinical Director), which is what we affectionally call the directors of the rotations in Springfield. He’s the ACD for surgery. Fellow GCMS member, Dr. David Haustein is the Dean of the Springfield Clinical Campus and now wears the hat of Vice President of MSMA as noted by our GCMS President in his update.
Do we see a pattern here? Leaders in our profession, those passionate about teaching, are also passionate about medicine in all its forms: advocacy, practicing, and being part of the change that we will inevitably see. It is time to be involved and make our voices heard. It’s time to raise up the next generation of physicians to shape where medicine needs to go and it will go, whether we are part of it or not.
In this issue, you will see some of those voices passionate about medicine, from two students making waves in their class, Josie Ihnat and Destri Eichman, to administrative clinician, Dr. Julia Flax spearheading the effort at Cox for physician wellness, to public health servant, Dr. Nancy Yoon, discussing the focus on nutrition and health, to empathic gynecological oncologist, Dr. Molly Greenwade, who is one of the exceptional preceptors showing passion for teaching in the midst of tragedy. You will see those passionate about helping physicians care for their families and those passionate about the life they lead.
MSMA had their annual meeting where Dr. Biggers was installed as the next president, and he has his goals outlined this issue. The Alliance was also there representing the important spouses who support us and Barbara Hover has their update as well. GCMS President, Dr. James Rogers, also outlines the resolutions that were passed from our GCMS cohort.
Krystyna Clarke, Dr. Michael

Clarke’s better half, recounts her incredible and superhuman experience running 7 marathons in 7 days on 7 continents.
And rounding out this issue, Dr. Jim Blaine, a stalwart of our organized medical community, delivers a passionate promise to our pediatricians: that we have not forgotten the least heard in our community, our children.
Please notice two upcoming CME opportunities: one from Washington University and the other is our annual GCMS summer retreat and CME in Breckinridge. If you haven’t been to Colorado in the summer, there really is nothing quite like it. This will be my third year providing a lecture as well! Come see me!
And don’t forget to RSVP for our first MASH BASH to benefit the GCMS foundation. Come for an evening of food, philanthropy, and festivities! Also, if you would like to sponsor a table and invite all your friends and family, it’s going to be unforgettable! And I’m completely unbiased *wink-wink* even though my husband is the organizer!
May some of the passion in these pages perhaps reignite that spark we all had as we matriculated from our alma maters, to come full circle and be front and center in the future of medicine.

by James Rogers, MD
Wow! One of the first lessons we all learn after transitioning from residency to the “real world” is that there is a plethora of constraints to delivering care that goes way beyond the accuracy of a diagnosis and treatment plan. Frequently, physicians face rules/laws that impede care, burden office efficiency or create unreasonable financial burdens. For these changes we need advocacy to identify the problem, propose solutions, and support legislative change.
Our process for legislative change is through Missouri State Medical Society (MSMA). MSMA has dedicated staff, including two full-time and three part-time lobbyists, who work for the adopted resolutions. The annual meeting concluded April 3-5 and for the first time was held in Springfield.
Our society sponsored over 21 delegates, the most ever for our district! We strengthened our society’s relationship and successfully had all three of our resolutions adopted for action. These resolutions involved: 1. Requiring both parties' permission before recordings are taken during a patient interaction, 2. Improvements in PDMP structure, and 3. Relaxing PDMP requirements for delegates. The summaries of these and all actions taken on the 18 total resolutions this year can be found at GCMS.US/ MSMAresolutions (will need to confirm link and post the resolutions).
We are delighted that the new President of MSMA is Dr. Brian Biggers, surgeon and his 1st Vice President is David Haustein, Associate Dean MU-Springfield campus, and Physical Medicine & Rehabilitation. Both are in Springfield and serve in leadership with GCMS.
Having a strong voice for our patients and a path for legislative reform comes about from our physicians’

community supporting this structure by membership and calling for changes to improve the care we deliver to our patients every day. Join us to strengthen our call for better care for our patients! www. GCMS.US/Join

MSMA 2025-2026 President: Brian D. Biggers, MD, FACS

1st Vice President
David Haustein, MD Associate Dean, Springfield Clinical Campus Professor of Physical Medicine and Rehabilitation



Tailored Tax, Wealth Management, and Family Office to help you prepare for what’s next.
By Jocelyn “Josie” Inhat, M3, University of Missouri-Columbia School of Medicine, Springfield Clinical Campus
“Oh, I guess I better get going.” Dennis’s words hung in the air. Finally, the silence was pierced by a sob from across the room; it had come from his sister. He had made his decision – he was not going to fight. Rather, he would let the newly discovered cancer take him quickly and peacefully. That scene is burned into my memory: my attending, Dr. Mady, knelt on the ground next to Dennis, who sat upright in his chair, his breaths labored and his skin yellowed – hallmarks of the cancer that, in a matter of mere months, had ripped through his lungs and the rest of his body, and was now eating away at his liver. Family members were scattered throughout the hospital room, dabbing at their eyes with tissues. The only dry eyes in the room were Dennis’s. Biopsy, staging, and treatment might have given Dennis months; if he got lucky, maybe even a year. That was not what he wanted, though, and as his medical team, we honored that without judgement. Rather, he transitioned to hospice care and passed away peacefully at home a few weeks later.
There were things I expected to learn from my clinical rotations – medication regimens, note writing, even surgical skills. Those things all have their value, but I found that the greater lessons were unexpected. I could never have anticipated the profound impact that patients like Dennis would have on my future practice as a physician. In the weeks that followed, my mind returned to Dennis and his family frequently, and I found that, rather than feeling like we had failed because our patient had passed away, I felt good about the interaction, about having been able to be there for not only Dennis in his difficult time, but for his siblings as well. There was beauty and value in being able to help guide Dennis through death.
with me for a lifetime.

More than any medication they could prescribe, patients and their families will remember how their physician spoke to them when they were struggling, or when they needed to make an impossible choice. It is that ability to support one’s patients with compassion and grace, regardless of what medical decisions they make, or the situation they are in that sets someone apart as an exceptional physician. The honor of being there for Dennis and his family that day has forever changed who I will be as a physician and has shaped me for the better.

Success in medicine is not always about curing a disease, fixing a problem, or prolonging a life; it is also about supporting your patient and their loved ones through the stage of life in which you encounter them, whether that be birth, adolescence, adulthood, or death. The way Dennis’s brother squeezed my hand, his voice cracking as he thanked me for being there with them that day will stay
Editor’s note: Names have been changed to protect the identities of those mentioned. The photographed painting is painted by the writer of this piece. This patient’s family was presented with an honorary tribute at the annual Legacy Teacher’s banquet this past March 2025 in Springfield, MO.
By Rhonda Sorensen, SVP, Private Banking Manager for Arvest Bank – Springfield Region
Many medical students aspire to achieve financial stability, save for retirement, and build wealth over time. However, the burden of college and medical school debt combined with modest salaries during residency can delay these aspirations significantly, requiring disciplined budgeting and strategic financial decisions.
Managing your finances strategically now will set the foundation for a stable and prosperous future. As a private banker, I work with various medical professionals with a range of financial needs. Here are some tips tailored for new resident physicians.
A solid credit score is essential for securing favorable loan terms and financial flexibility in the future. Here’s how to get started:
• Open a Credit Card : Choose a card with low interest and good rewards. Use it wisely by making small purchases and paying off the balance in full each month.
• Make On-Time Payments: Late or missed payments negatively impact your credit score. Setting up automatic payments can help.
• Keep Credit Utilization Low: Try to use less than 30% of your available credit limit to maintain a strong score.
• Monitor Your Credit Report: Regularly check your credit score and report for errors and fraudulent activity.
As a resident, you may be considering homeownership. Many banks, like Arvest, offer specialized mortgage programs for physicians:
• Physician Loans: These loans often require little to no down payment and waive private mortgage insurance (PMI), making homeownership more accessible.
• Flexible Debt-to-Income Ratio Consideration: Unlike traditional loans, physician loans consider a new contract for employment rather than just your current resident salary.
• Favorable Terms: Some lenders offer competitive interest rates and the ability to refinance easily once you become an attending physician.
• Early Prequalification: If you have a signed contract with your residency program, some lenders allow prequalification before you receive your first paycheck.
While it may seem premature to think about wealth management, starting early is key to long-term financial
security. Consider these steps:
• Automate Your Savings: Even with a limited income, putting a portion of your paycheck into a high-yield savings or money market account can help build a financial cushion.

• Start Investing: Explore employer-sponsored retirement plans, such as a 401(k) or 403(b), and consider opening a Roth IRA to take advantage of tax-free growth.
• Understand Student Loan Repayment Options: Research income-driven repayment plans, refinancing opportunities and Public Service Loan Forgiveness (PSLF) if you plan to work for a nonprofit hospital or academic institution.
• Avoid Lifestyle Inflation: As your income grows, resist the urge to overspend. Prioritize saving and investing over luxury purchases.
Contact a financial provider to talk with someone who can offer personalized financial guidance for medical professionals, such as a private banker or financial advisor. They can assist you with:
• Budgeting and debt repayment strategies
• Investment planning tailored to your career trajectory
• Tax-efficient savings and wealth accumulation
• Risk management, including disability and life insurance planning
The financial habits you build during residency will impact your long-term wealth and stability. By focusing on building credit, exploring physician-specific home loan options, implementing smart wealth management strategies, and seeking professional financial guidance, you can set yourself up for a prosperous future.
Rhonda Sorensen is a Senior Vice President and Private Banking Manager for Arvest Bank – Springfield Region.

By Krystyna Clarke
On November 10, 2024, I flew to Cape Town, South Africa to join 53 other runners in the challenge of running 777; 7 marathons in 7 days on 7 continents. The 54 runners represented Austria, Australia, Belgium, Belarus, Canada, Germany, Great Britain, Italy, Latvia, Lebanon, Nepal, Switzerland, and the USA. A few of the runners chose to run a half-marathon.

At the end of the race, 45 runners completed all 7 marathons, with a few downgrading to a half marathon. One runner could not run an Australian marathon due to a misunderstanding with his entry permit. Forced to skip 1 marathon, this runner was able to join us back in Istanbul and complete 6 marathons. The front male runner from Ireland exited the race after experiencing heat exhaustion during the 6th marathon in South America.


Compared to many runners my age, who have already completed over 100 marathons or a few 100-milers, I am not a very experienced runner. I have run approximately fifteen marathons, plus seven in this race. My longest run was a 55K (34 miles) trail run in Arizona, and a challenging 50K mountain trail run in the Colorado mountains on the Continental Divide at 13,500 feet. At least I tested my endurance before the 777 race. There are many categories of runners. Some of us are sprinters running fast 5Ks; some are endurance runners tackling 100 to 200 milers, and triathletes who combine swimming and biking. Our group of 777 racers included accomplished athletes like a former Olympian, a member of the world trail championship team USA, the front male runner, averaging a marathon time of 2:39, and the rest of us. 2 special runners, both cancer survivors, participated with one functioning lung.
I need to explain my motivation for taking on this challenge. In 2023, I completed a Mount Everest marathon in Nepal. We hiked to the Base Camp of Mount Everest, spent two nights at 17,500 feet, and then ran a marathon. A year later, in May 2024, I hiked the famous Snowman Trek in the Himalayas in Bhutan, crossing over eleven mountain passes. These endurance experiences gave me the confidence to take on the challenge of 777. It became my calling when I noticed a chat among runners I had met about running a marathon on each continent. My first attempt to Google how to accomplish this introduced me to information about the Great World Race. I signed up that day.

My first marathon was in Antarctica. During a briefing in Cape Town, we were informed about the earlier departure to Antarctica. All seven marathons had to be moved one
day sooner. The next morning, we met at 4 am at the historic Winchester Hotel for our departure to the airport. The 5.5hour charter flight on an Airbus A340-300 landed in White Desert on the snow-plowed runway, which we also used for

running. It was important to stay on the snow to avoid slipping onto the crystal-blue ice. The temperature was 3-5 degrees Fahrenheit. We quickly became hot while running and had to peel off layers, but at the same time, a chilly wind was freezing my fingers as soon as I removed my ski gloves. I experienced abdominal cramping and unusual heaviness in my legs. The jet lag was also a negative factor. Despite not feeling strong, I tried to enjoy running on this unique seventh continent. In a sense, it felt magical.
Flying back from Antarctica and arriving at 4 am at my hotel in Cape Town left little time for rest before our second marathon in the morning. Our group lined up for the second marathon at the sunny Seapoint promenade. My tired body felt a significant temperature swing, but my running form improved. At this point, I realized that my primary focus should be on the positive vibe from fellow runners, the sunny weather, my improved running form, and not questioning the decision to run a second marathon after a sleepless night.
After completing the second marathon, we flew on another Boeing 767-300 charter to Perth, Australia. A good meal on the plane and some rest helped me get closer to my goal of a 4-hour marathon in Perth. We showered at the Australian Marathon Clubhouse in Burswood, next to the Optus Stadium. The Australian helpers at the aid stations were extremely nice and ensured we had enough hydration and carbo-electrolyte fuel to run.
We boarded our charter plane in the evening and flew to Istanbul, refueling in Dubai. We started on the European side of Istanbul after 9 pm, amidst darkness and rain. I finished my marathon around 1:30 am. Arriving at the hotel in the early morning, we had only 3.5 hours of sleep before running our 5th marathon on the Asian side of Istanbul across the iconic
Bosphorus. Fortunately, it was a daytime run with nice views of the water. By the time our bus took us to the airport, it was late evening again.
We were on our way to our sixth marathon in Cartagena, South America. It was a hot one with a heat index of 100 degrees. All of us struggled with the intense heat and heavy humidity. Our front runner could not complete the run due to heat exhaustion, and another runner was taken to the hospital and released just in time for the flight to Miami. We departed Cartagena at midnight, landed in Miami at 3:30 am, and had to be ready to run our final marathon, the seventh, on the North American continent.

Running seven marathons on seven continents in seven days was my most challenging running adventure. As the event progressed across the seven continents, I experienced a combination of marathon fatigue, jet lag, sleep deprivation, and a temperature variation of 90 degrees Fahrenheit. I remember the overwhelming joy of crossing the final finish line on Miami Beach Boulevard and seeing my husband, Michael. I became a proud member of the Global Marathon Club.

By David Haustein, MD, MBA, Associate Dean, Springfield Clinical Campus
We are wrapping up another great academic year at the University of Missouri School of Medicine’s Springfield Clinical Campus (SCC). As of May 2025, 148 students have graduated from the program, many of whom are currently in residency or fellowship training across the country. Many physicians in southwest Missouri have contributed to the education and training of these new physicians. This year’s Mizzou School of Medicine class was highly sought after, with 99% matching into residency programs. We are proud to announce the following matches for our SCC Class of 2025 students.
Name Hospital Program
Michael Bodenhausen Medical College of Wisconsin Affiliated Hospitals Internal Medicine
Clayton Brinkley Washington University School of Medicine Urology
Callyn Broyles University of Missouri Hospitals, Columbia, MO Emergency Medicine
Emma Elbert KU School of Medicine – Kansas City Otolaryngology
Rebecka Ernst University of Iowa Hospitals & Clinics Obstetrics and Gynecology
Matthew Gao University of Missouri Hospitals, Columbia, MO Medicine-Preliminary
Matthew Gao St. Luke’s Hospital–Anderson Campus, PA Radiology-Diagnostic
Sally Heil KU School of Medicine – Kansas City Medicine-Preliminary
Sally Heil KU School of Medicine – Kansas City Radiology-Diagnostic
Austin Hotop Western Michigan University Homer Stryker M.D. School of Medicine Surgery-General
Kenlee Jonas University of Missouri Hospitals, Columbia, MO Medicine-Preliminary
Kenlee Jonas St. Luke’s Hospital–Anderson Campus, PA Radiology-Diagnostic
Brooke Kronk University of Missouri Hospitals, Columbia, MO Pediatrics
Noah Kronk University of Missouri Hospitals, Columbia, MO Emergency Medicine
Allison Long University of Arkansas for Medical Sciences Regional Centers Internal Medicine
Aaron Meers University of Arkansas College of Medicine –Little Rock Otolaryngology
Anna Mori-Kreiner Tulane University School of Medicine Pediatrics/Psychiatry/ Child Psychiatry
Raquel Ortiz UC San Diego Medical Center Internal Medicine
Priya Patel University of Missouri–Kansas City Ophthalmology
Jada Phillips Duke University Medical Center Obstetrics and Gynecology
Evan Reeves University of Missouri Hospitals, Columbia, MO Medicine-Preliminary
Evan Reeves University of Missouri Hospitals, Columbia, MO Physical Medicine and Rehabilitation
Evadne Rodriguez Baptist Health, Arkansas Transitional Year
Evadne Rodriguez KU School of Medicine – Kansas City Dermatology
Samuel Schaeffer Case Western Reserve University/University Hospitals Cleveland Medical Center Internal Medicine
Christine Shao University of Missouri Hospitals, Columbia, MO Ophthalmology
Joan Tao St. Luke’s Hospital–St. Louis, MO Medicine-Preliminary
Joan Tao University of Chicago Medical Center Radiology-Diagnostic
Sai Supriya Vuda Cleveland Clinic Foundation Psychiatry
Emily Winfrey CoxHealth, Missouri Family Medicine

Note: Some students chose not to be included on the public match list for personal reasons. Please respect their privacy and refrain from inquiries. Also, some students are listed twice due to completing both preliminary and advanced program matches.
We are proud to see our students match into a wide spectrum of specialties from both the Springfield and Columbia campuses. Of our Springfield graduates who have completed their training, about 25% are now practicing in southwest Missouri, including Springfield, Lebanon, Bolivar, and Fort Leonard Wood. Some of our other graduates are now teaching at University of Missouri-Columbia, Washington University, MD Anderson, and other institutions across the United States. With more than 80% of our SCC students hailing from Missouri, we hope to see many return to practice here.
On March 26th, the Springfield Clinical Campus celebrated the Legacy Teacher program at Highland Springs Country Club, with generous sponsorship from CoxHealth. The program honors patients who have shaped third-year medical students’ understanding of patient-centered care. Through reflective essays and artwork, students recognize these “Legacy Teachers” for the lasting lessons they impart— lessons that will influence our future physicians.
We are also proud to celebrate the 400 physician faculty members in southwest Missouri who volunteer their time to train our students. The Springfield Clinical Campus hosted our 4th Annual Faculty Appreciation Dinner on April 1. Thank you to everyone who attended and made it a joyous evening.
Please join us in congratulating the 2025 award winners:
Dr. Meghan Guthrie-Baker – Family Medicine Preceptor of the Year
· Dr. Jean Guan – Internal Medicine Preceptor of the Year
· Dr. Benjamin Lisle – Neurology Preceptor of the Year
· Dr. Molly Greenwade – Obstetrics & Gynecology Preceptor of the Year
· Dr. Ashley Merrick – Pediatrics Preceptor of the Year
Dr. Kyle John – Psychiatry Preceptor of the Year
· Dr. Anthony Bentley – Surgery Preceptor of the Year
· Dr. James Bonucchi – Subspecialty Preceptor of the Year
Dr. Kody Finstad – Lecturer of the Year
· Dr. Mark Ellis – Empowering Educator
We have much to celebrate and be thankful for in southwest Missouri. To all of you who give your time and talents to raise the next generation of Missouri physicians, thank you. You are making a meaningful difference in the care of our friends and neighbors for years to come.
by Molly Greenwade, MD, Ferrell Duncan Gynolocological Oncology, Cox Medical Group
Editor’s note: This speech was given at the MU Clinical Campus Faculty Appreciation Banquet on April 1, 2025 where Dr. Greenwade was recognized as Outstanding Preceptor in Ob/gyn.
Thank you for this honor. Teaching has been one of the most fulfilling parts of my career, and I’m grateful for the opportunity to help shape the next generation of physicians. One of the most common questions I get from students is, “How do you compartmentalize? What do you do to decompress when the work is so heavy?” For a long time, I answered with things like, “I spend time with my family” or “I go to the gym.” And while those were true, the answers felt rehearsed—like I was saying what I thought I was supposed to say. At the time, I didn’t realize that something deeper was missing. I had mastered the ability to package stress neatly and move on, but I hadn’t yet recognized the cost of that kind of emotional efficiency. The truth is, I’ve had to learn— sometimes the hard way—that while compartmentalization is necessary, but it’s not the whole answer. In fact, too much of it can lead to burnout and emotional detachment.

Exactly one year ago today, this concept of compartmentalization was put to the maximum test. I was in the middle of an extremely challenging robotic surgery, adhesions everywhere, a terrible case of endometriosis. I was also under high levels of stress, simultaneously preparing for oral boards, which were scheduled in two weeks. My phone rang beside me. I looked over at it, and it was my sister. I thought, “I’ll just call her back when I’m done.” I kept working. She called me again. I stopped and thought, “That’s not usual. Something must be wrong.” So I paused the case and answered.
My sister, who is never rattled by anything, sounded short of

breath on the other line and anxiously said, “Molly, they are coding him. He fell, and they are coding him in a gas station parking lot. He’s not going to be okay, is he? I just need you to tell me if he is going to make it.” This was in regard to my brother-in-law, who was diagnosed with a large mediastinal mass compressing his trachea the week before. We had all been awaiting the biopsy results for surgery planning. I said, “No, I’m afraid he’s not going to make it. I’ll be there as soon as I can.”
I took a huge sigh. I looked back into the robot console and continued to operate with tears streaming down my face. My brother-in-law had died at a young age, leaving my oldest sister and their three young children behind. A few minutes later, I felt hands on my shoulders and heard my best friend and colleague in my ear, saying, “Molly, go.” She gave me a huge hug, pushed me out the door, and finished the case for me, and I was able to go be with my family.
In the coming weeks I would watch children try to comprehend the loss of a father while they hoped for an April Fool's Day joke instead, attend a funeral, celebrate a heavenly birthday, comfort my family during the day, prepare for oral boards at night, catch up on my inbox with my own patients' issues, and board a plane to Dallas to take a four-hour oral examination to discuss evidence based medicine and defend treatment decisions that I had made over the past year. Because that's what we do in medicine. The world can be on fire around us, but life goes on. Our job takes the front seat. At least, I think that's what we're taught at some point along the way.
I don’t think I ever fully grieved during those two weeks—I was in complete survival mode, just focused on getting the job done. Ever since April 1, 2024, I don’t think I’ve been the same. I realized that I compartmentalized so much that I wasn’t feeling anything anymore—at work, in my personal life—because I had to protect myself. For a short time, I found myself just going through the motions. I remember thinking, “I’m not being a good teacher today. I’m not talking as much as I normally would. I hope this rotation is still beneficial for the student, and they don’t see how hard this is.” There was even a day I considered not having students because I didn’t want to talk at work. I wanted to go in, finish my work, and leave with as little interaction as possible. And most of you who know me know that’s not me.
For a long time, I thought protecting myself meant shutting things away, but I realized that too much of that leads to burnout. I connect with my patients deeply, and when I found myself pulling away too much, I knew something
had to change.I think the number one way to relieve stress in the workplace is to find like-minded people you can trust— people you can debrief with, unload to, and who will help you carry that weight. I am so lucky to have the best OR team, colleagues, support staff, and medical students—people who see us showing up for our patients every day, who realize that the load is heavy, but also see that we continue to persevere, to listen, to be empathetic, and take good care of our patients, even when life outside of the hospital is hard.
Medical students, whether they realize it or not, provide an outlet. Just acknowledging out loud how difficult it must be to compartmentalize some of this makes everything feel so validating – and so worth it.
So thank you—for continuing to ask me how I compartmentalize, for holding me accountable for taking care of myself, for

reminding me to stay in tune with my emotions, and for making sure I do things outside of work to restore myself, like exercising, writing, listening to music, and spending quality time with my children. I’ve learned to process the weight instead of just carrying it. I debrief with my partners, I move my body to release stress, and I remind myself that feeling the weight of this work is not a weakness—it’s a privilege.
Graduating medical students, if there’s one thing I hope you take with you, it’s this: You don’t have to choose between being a great doctor and being a whole person. Find your ways to process, surround yourself with people who truly understand you – who comfort you, empower you, and support you emotionally. The ones who remind you that your humanity is your greatest asset in this work. And never forget - this work is hard because it matters. Thank you.






by Destri Eichman, M3, 2026 Graduating Class President, University of Missouri-Columbia, Springfield Clinical Campus
Thank you, Dr. Haustein! I would truly like to thank each faculty, staff, and community member for taking the time out of their busy schedules to attend this evening. I wanted to use my time to share a little about my experience as a student.
My Springfield Clinical Campus story is likely similar to others. After choosing Mizzou for medical school, I visited Springfield to see what it was all about. We toured the hospitals and spoke with students who shared how rewarding their experiences were. By the end of the day, some of us looked at each other and said, “You’re coming here, right?” We assumed it would be competitive—turns out, some of us came through the lottery. But once we settled in, it didn’t matter how we got here—we knew we were in the right place.

I knew I was in the right place when, on my very first day of third-year, I rolled up to the neurotrauma ICU (short white coat on and backpack full of things I probably didn’t need) and Dr. Lisle immediately gave my classmate and I two patients to see and write a notes on. We had no clue what we were doing, and Dr. Lisle knew that - but he gave us the space to discover and investigate on our own.
I knew I was in the right place when Dr. Micka used his small whiteboard to draw the mechanism of a biologic medication when it was obvious I wasn’t grasping the concept.
I knew I was in the right place when Dr. John trusted me to talk with one of his adolescent female patients on my own in order to truly find out what was going on.
I knew I was in the right place when Dr. Moore expressed his confidence in my capabilities out loud in front of me and his patient.
I knew I was in the right place when Dr. Hearty took the extra time to walk through exam skills and discussion topics with parents because she knew I aspired to be a pediatrician.
I knew I was in the right place when Dr. Kirk just laughed when I accidentally sprayed saline all over nursing staff with the colonoscope and when Dr. Bentley helped teach me sleight of hand magic in between clinic patients.

I knew I was in the right place because every day I walked into each hospital or clinic with the confidence that I would be learning something valuable.
In healthcare, where efficiency, productivity, and quotas often dictate daily practice, teaching is a deliberate and selfless choice. It’s rarely the most time-efficient task and often comes without immediate rewards—except, of course, when Dr. Hernandez corrected my hand-tying technique (life-changing!). Teaching requires faculty to pause, explain, demonstrate, and guide—often in the least convenient moments.
Yet, despite the demands of patient care and administrative burdens, you choose to invest in us. You take the extra time to walk us through complex cases, challenge our thinking, and ensure we not only learn medicine but also embrace the deeper responsibilities of being a physician. More than just educators, you are mentors who shape us into discerning, compassionate, and resilient individuals, equipping us to navigate the challenges of this profession with integrity and purpose.
I must also mention that our experience would not be what it is without the incredible staff at the Springfield Clinical Campus. Dr. Haustein, Jill, Elizabeth, Jennifer, Tracye, Eden, Dee, Frankie, and the rest of the SCC crew, thank you for your guidance and support. Managing medical students and their clinical experiences is no easy task, but you all do it with such care.
We may never be able to fully express the depth of our gratitude or the impact each of you has had on our journey, but we hope this event conveys even a fraction of our thanks. To my fellow students, I encourage you to take a moment this evening to personally thank at least one faculty member who has influenced you. The truth is, every faculty member here has given us a piece of their knowledge, their practice, and their wisdom—pieces that we will carry forward and shape into our own unique approach to medicine. These pieces will continue to shine through in the way we care for our patients, in the way we navigate challenges, and, perhaps one day, in the way we teach the next generation of students.
Your legacy is living, and we are honored to carry it forward. We cannot thank you enough.
by Nancy Yoon, MD, MPH, Chief Medical Officer Springfield-Greene County Health Department
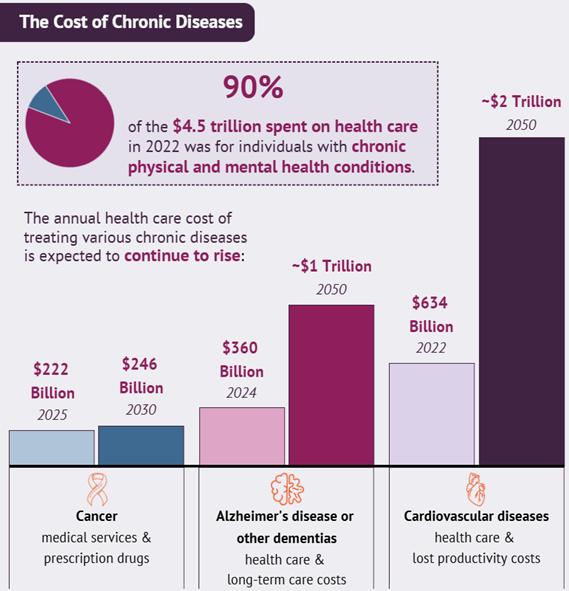
In the American Heart Association’s Presidential Advisory “Forecasting the Burden of Cardiovascular Disease and Stroke in the United States Through 2050”, the prevalence among adults of hypertension is estimated to increase from 51.2% in 2020 to 61% in 2050, of diabetes from 16.3% to 26.8%, of obesity from 43.1% to 60.6%, and of total cardiovascular disease from 11.3% to 15% (including coronary disease, heart failure, stroke and atrial fibrillation)¹. Consequently, U.S. healthcare costs are projected to triple between 2020 and 2050, from $400 billion to $1344 billion. 90% of healthcare costs in 2022 was for individuals with chronic physical and mental health conditions.² It is clear that preventive, more cost-effective strategies need to be implemented at a population level to reverse these concerning trends.

Food is Medicine⁴ models encompass a broad range of approaches that promote optimal health and healing and reduce disease burden by providing nutritious food— with human services, education, and policy change—through collaboration at the nexus of health care and community. Guiding principles for Food is Medicine include recognizing nourishment as essential for good health, well-being and resilience, facilitating easy access to healthy food across the health continuum, uniting partners to build sustained and integrated solutions, and investing in the capacity of underresourced communities.
The American College of Lifestyle Medicine (ACLM)³ recommends a predominantly whole-food, plantpredominant eating plan based on a variety of minimally processed vegetables, fruits, whole grains, legumes, nuts, and seeds. This is an essential strategy in the prevention of chronic disease and treatment of chronic conditions. In intensive, therapeutic doses, lifestyle medicine interventions can put chronic illnesses, like diabetes, heart disease, and high blood pressure into remission.
Many people face barriers of cost and access to healthy foods. The University of Missouri in partnership with Feeding Missouri conducted a 3-year study, Food Assistance & Hunger in the Heartland 2021⁵ that illustrates the critical role food banks and pantries play in supplying food to families struggling with hunger. The report was prepared for Feeding Missouri, the state coalition representing Missouri food banks, using survey data obtained from the six Feeding America food banks in Missouri, including Ozarks Food Harvest. In the Ozarks, food insecurity rates are “dramatically higher” than all Missouri households. This study showed that 64% of households have low food security (reduced quality, variety or desirability of diet). Of that, 30% of these households have very low food security (truly don’t have enough food to meet their needs). Finally, 52% of households served get at least half of their monthly food from a food pantry.
Ozarks Food Harvest assists individuals and families with applying for SNAP, or Supplemental Nutrition Assistance Program benefits, formerly known as “food stamps.” Last fiscal year, Ozarks Food Harvest assisted 1,239 families with submitting their SNAP applications. This generated more than $3.6 million worth of SNAP benefits for food-insecure individuals. The staff at Ozarks Food Harvest (417-429-0853) can help people with applications and answer questions about eligibility.
Since 2014, Springfield Community Gardens has partnered with Ozarks Food Harvest to help reduce food waste by distributing fresh produce directly to food insecure neighborhoods. Since beginning this program, over 100,000 individuals have received over 750,000 pounds of free food. That amounts to more than $1.3 million worth of food that would have otherwise been sent to a landfill.
The mission of the Springfield Community Gardens is to create gardens that strengthen neighborhoods where people can grow healthy relationships, food, and community. They work with a network of volunteer community gardens and market farms to grow healthy food, build relationships, and generate social capital with each new garden. Anyone can learn and grow with Springfield Community Gardens by becoming a volunteer. Home gardeners can donate their garden harvests at the SCG Market Garden at 1126 N. Broadway Ave on Mondays and Tuesdays from 7AM-2PM. Produce will be used to fill Springfield’s community fridges in partnership with the City of Springfield, Community Partnership of the Ozarks, and the Springfield-Greene County Library system.
The Women, Infants, and Children (WIC) program improves the overall health of families by supporting the nutritional health of pregnant, postpartum, and breastfeeding people, as well as infants and children, up to the age of five. WIC also provides nutrition education, breastfeeding education and support, a supplemental food package, and referrals to health care providers and local agencies. Eligible individuals must live in Missouri with a household income no more than 185% of the federal poverty income guidelines. To contact the Springfield-Greene County WIC program, call 417-864-1540 or text 888-754-0693.
National Nutrition Month
National Nutrition Month is an annual campaign established in 1973 by the Academy of Nutrition and Dietetics. During March, everyone is invited to learn about making informed food choices and developing healthy eating and physical activity habits. This year's theme is "Food Connects Us." Food is a connecting factor for many of us. It connects us to

our cultures, our families, and our friends. Health, memories, traditions, seasons, and access can all impact our relationship with food. Here are some ideas for connecting with food:
• Plan to eat more meals together as a family
• Give family members a role in meal planning and let them pick out different recipes to try, with a new fruit or vegetable each week
• Practice mindful eating by limiting screen time at mealtime
• Visit a community garden or farmer’s market and ask how the food was grown and raised.
Fortunately, there are many resources in our community for people to be able to access nutritious foods, which are key to improving health and preventing many chronic diseases.
References
1. Forecasting the Economic Burden of Cardiovascular Disease and Stroke in the United States Through 2050: A Presidential Advisory from the American Heart Association. Kazi D.S., Elkind M.S.V., Deutsch A., et al. Circulation 4 June 2024 Vol. 150, Number 4.
2. The Growing Burden of Chronic Diseases (2025, April 3). NIHCM Foundation. https://nihcm.org
3. American College of Lifestyle Medicine: https://lifestylemedicine. org/
4. Food is Medicine. Office of Disease Prevention and Health Promotion. https://odphp.health.gov/foodismedicine.
5. Chapman, D., McKelvey, B., Bennett, C., Carlos Chavez, F. L., Hermsen, J., & Rikoon, J. S. 2022. Food Assistance and Hunger in the Heartland 2021: Report for Ozarks Food Harvest. University of Missouri, Interdisciplinary Center for Food Security, Columbia, MO.



President
by Brian Biggers, MD, MSMA President, Ferrell Duncan Breast Surgeon, Cox Medical Group
Just one month ago I had the privilege of becoming your Missouri State Medical Association President. As we start this journey, the organization must look at the goals that can be accomplished. One year, 365 days. Together, what can we as an organization accomplish together during this time? A year seems long, but reality goes by faster than we would like. Where do we start? In my opinion, it comes down to your priorities and where we can elicit the most change and impact.

First, let’s first talk about the overall health of our state which affects both physicians and patients. Where do we rank? Here are the facts for Missouri from 2023 data. Missouri is:
• 38th in healthcare in comparison to other states
• 40th when looking at healthy lifestyles
• 15th among the most uninsured
• At the end of June 2024, the tax on cigarettes was $0.17 per pack of 20, the lowest in the United States
• One of the highest rates of tobacco usage in the United States
• One of the lowest retail sales taxes on marijuana in the United States.
These last two are examples of products which negatively affect Missouri patients. It is also a potential source of revenue to put into the health of our state.
The two top groups of “insurance” patients who smoke are uninsured and Medicaid patients. As a state, if we raised the taxes to the same as surrounding states and used this revenue for healthcare, we could improve not only funding for healthcare, but the overall health of the state.
Second, many of us deal with challenges with the scope of practice. We continue to oppose nurse practitioners and CRNAs who want independent practice. Optometrists who want to perform surgery. Pharmacists want to dispense vaccines and
give modified prescriptions. One would think if someone wanted to do any of this, they would simply have gone to medical school.

As physicians, we have the experience of oversight and experience. We hold ourselves to ambitious standards and continue our medical education. We do not just worry about the minimum number of hours we need to fill a requirement, but the acquisition of knowledge. Don’t get me wrong, these members of the healthcare team are essential to the healthcare team in delivering care to patients, but they still need our oversight and leadership. What Patrick Mahomes is to the Chiefs, we should be for the healthcare of this state.
Finally, I am very enthusiastic about medical education. I sincerely enjoy being the clerkship director for our third-year medical students and as an alum from the University of Missouri School of Medicine and I do not take this responsibility lightly. I view our medical students as an investment for the future of medicine, especially for Missouri.
These students leave medical school with an average $170,000 in debt. The amount of debt is even greater for other medical schools. The system places students significantly behind financially. What can we do to decrease this burden?
We need more physicians in the state. We need to invest in training programs to train these students and to stay in Missouri after graduation. The legislature has already started to support the expansion of graduate medical education residency positions, and I hope to see this trend continue as well as continued medical school expansion.
I recall my first third year student from our program here in Springfield, and what an impact we can make. Early in her third year when she started surgery, she said she would never go into surgery. She recently finished her surgical residency at Wichita and then her Breast Surgical Oncology fellowship at Washington University. She now practices in Missouri. She told me that I may have had some impact on this path. We need to remember the influence we can have on these students but also our state if they choose to practice medicine here.
If one is not part of the solution, then he or she is part of the problem. As physicians we must be engaged. We must be the leaders to drive healthcare not only for our facilities, but for our state. In life we can be one of three things, inactive, reactive, or proactive. As physicians, now is the time to be proactive by taking the initiative to create change. Together we can move toward improvement and excellence in the health of our state.
by Julia Flax MD FAAFP Chief Population Hlth Officer, CoxHealth Network
The well-being of physicians is a critical issue that impacts the entire healthcare system. The fact that approximately 350 physicians in the U.S. die by suicide each year, and that over 50% of physicians experience some degree of burnout, underscores the urgency of this matter. Healthcare organizations face numerous challenges, including the current landscape of uncertainty, which can exacerbate these issues. However, while organizations may not be able to control all external factors, they can control their response. CoxHealth is committed to prioritizing physician wellbeing through a structured, systematic, and evidence-based approach, creating an environment where physicians can thrive.
Dr. Tait Shanafelt, a leading authority on physician well-being, urges healthcare organizations to embrace a multi-faceted approach, highlighting the necessity of addressing physician wellbeing. His arguments encompass the moral and ethical case, the business case, the recognition case, the regulatory case, and the tragedy case.The business case, in particular, demonstrates the significant economic costs of physician burnout and turnover, including recruitment and replacement expenses, lost revenue, decreased patient satisfaction, increased medical errors and malpractice claims, reduced clinical quality and productivity, and diminished work effort. By acknowledging that physician burnout is primarily related to systemic factors and the practice environment, healthcare organizations can take meaningful action.

the AMA's Joy in Medicine Health System Recognition Program. These frameworks provide evidence-informed strategies, clear guidelines, and criteria for well-being initiatives. We have adopted a structured, systematic, and evidence-based approach, emphasizing the importance of addressing organizational culture, practice environment, and individual support to promote overall physician wellness and professional satisfaction. Our pursuit of Joy in Medicine recognition has further motivated us to meet high standards and continuously improve our efforts, allowing us to benchmark our progress against other leading health systems.
In line with this commitment, CoxHealth has implemented several key initiatives to support physician well-being. To gain a deeper understanding of the challenges impacting our physicians, we developed and implemented an inaugural physician wellbeing survey. This survey provides valuable feedback on current burnout and satisfaction rates, as well as highlighting specific pain points. The results of this survey, including organizationlevel and service line-level data with relevant benchmarks, are disseminated in a way that encourages work-unit leaders to take action. This data is then used to facilitate meaningful conversations among teams, focusing on identifying the greatest opportunities for improvement. CoxHealth has also established a physician advisory well-being committee, comprising physician leaders working alongside representatives from IT, HR, nursing, and executive and operational leadership. This interdisciplinary approach ensures that a wide range of perspectives informs our well-being initiatives.

The Stanford Model of Professional Fulfillment provides a helpful breakdown of the various aspects of physician wellness and can be used as a framework for engaging leaders on the importance of these initiatives. This model outlines a simple construct that acknowledges the critical role of organizational culture, the practice environment, and the role of the individual in cultivating an environment that promotes professional well-being. CoxHealth has built a comprehensive organizational physician well-being program, leveraging both the Stanford Model and
Furthermore, in order to support physician collegiality and reduce administrative burdens, we have developed better resources for the development of collegiality groups for physicians and work with IT and operational teams on improvement projects to streamline practice workflows. CoxHealth has also taken steps to remove barriers that may prevent physicians from seeking help. We have updated our credentialing language to be consistent with the Dr. Lorna Breen Foundation Wellbeing First Credentialing Champion award. This demonstrates our commitment to changing invasive or stigmatizing language around mental health and substance use disorders in our credentialing applications and processes.
Finally, we provide a comprehensive well-being resource for our physicians. This includes a tiered portfolio of offerings designed to address a spectrum of needs, ranging from peer-supported programs for those dealing with personal or professional

challenges, professional coaching for those navigating more complex issues, and access to mental health resources for physicians experiencing severe burnout, depression, or suicidality. Alongside these direct support services, we are conducting campaigns to reduce stigma, normalize the use of
these resources, and openly discuss barriers to access, ensuring that our physicians feel supported and encouraged to seek help when needed.
In conclusion, prioritizing physician well-being is not just a moral and ethical imperative but also a strategic necessity for healthcare organizations. By addressing the systemic factors contributing to burnout and fostering a culture of well-being, organizations can improve patient care, enhance physician satisfaction, and achieve financial stability. The current climate of uncertainty underscores the importance of these efforts. By taking decisive action, healthcare organizations can cultivate a healthier, more resilient workforce dedicated to providing the highest quality of care. As a famous piece of political advice, often attributed to Winston Churchill, suggests: "never let a good crisis go to waste." The time to act is now, and the benefits of doing so are clear: a healthier, more resilient healthcare workforce dedicated to providing the highest quality of care.






by Barbara Hover, GCMSA President
Missouri State Medical Association Alliance held their annual meeting April 4-6 at University Plaza in Springfield. This was the first Annual Meeting to be held in Springfield and GCMSA was honored to act as host of the events. MSMAA was celebrating its 100th annual meeting anniversary.
Jana Wolfe welcomed the attendees with interesting facts about our city and area. MSMAA President Donna Corrado addressed the MSMA House of Delegates and on a lighter note, the Alliance with their helper Heather Ramsey passed out chocolate filled Easter eggs as everyone exited the room. Ron Jaggers from South Carolina, President-elect of the AMA Alliance, spoke about the current activities, focus of the national Alliance, and why the organization is of value to physician spouses. He will be the first male to be installed president of the AMA Alliance. Ron invited all to attend the AMA Alliance Annual Meeting May 30-June 1 in Charlotte, North Carolina. Jana Wolfe represented AHEI (Alliance Health Education Initiative) and explained its purpose. Our keynote speaker was Chris Davis, Vice President of Prevention

and Youth Support, Community Partnership of the Ozarks (CPO). He gave a brief history of how Ozarks Fighting Back (OFB) was established and later evolved into CPO. OFB is still a vital coalition working to prevent substance misuse and related violence and to build healthier lifestyles in our community. After lunch, Ron Jaggers graciously installed the MSMAA state officers for 2025-26 before the meeting adjourned. Officers included Donna CorradoPresident, Gill Waltman - President-elect, Diana CorzineSecretary, Deb Snyder-Treasurer, Jana Wolfe-VP Membership, Debbie Barbe and Barbara Hover- VPs Health, Gill Waltman and Katthy Weigand-VPs Foundation. Sana Saleh was presented the Sandra Mitchel Member of the Year Award.
As part of our mission for Physician and Family Wellness, GCMSA will hold its annual Physician Family Night at the Zoo on Saturday August 23. Please save the date and we hope to see you there.














by Jonathan Vance, CFP Senior Advisor, Forvis Mazars Private Client
In recent years, personal finance blogs have frequently mentioned the acronym "FIRE," which stands for Financial Independence, Retire Early. While this concept might bring visions of swapping a daily commute for leisurely beach walks, we believe it has a more practical application. Financial independence, simply put, means being able to support the financial demands of your chosen lifestyle without needing to earn an income. This doesn't necessarily mean you have to stop working once you achieve financial independence; rather, it offers the flexibility to work fewer hours or choose a more fulfilling role, even if it is less financially rewarding.
In the following sections, we'll explore actionable steps physicians can take to accelerate their journey toward financial independence, whether or not they aim to retire early.
The first step in determining the amount needed to achieve financial independence is understanding your family's expenses. Consider starting with a rounded monthly figure that covers all essential spending needs. This can be calculated using either a simplified (less accurate) or manual (more accurate) method:
1. Simplified: 60% of your annual gross income and divide by 12.
2. Manual:
• Step 1: Sum all regular monthly expenses.
• Step 2: Remove expenses that will cease upon reaching financial independence, e.g., mortgage payoff, term life insurance policy expiration, child's 529 contributions, etc.
• Step 3: Add expenses that will begin once financial independence is achieved, e.g., trips to Greece, season tickets to attend an alma mater’s football games, etc.
The simplified method will be least accurate for families in the highest or lowest federal tax brackets or those who save a significant portion of their gross income.
Using the calculated monthly lifestyle spending need, you can determine the asset base required to fund your lifestyle. Like above, this can be done using either a simplified (less accurate) or manual (more accurate) method:
1. Simplified: Multiply the monthly lifestyle spending need by 300–360.
2. Manual:
• Step 1: Use a retirement calculator or financial planning software.
• Step 2: Input the monthly lifestyle spending need, relevant inflation, tax, and return rates, investment and retirement accounts, desired financial independence date, and other pertinent financial information.
• Step 3: Review the summary to determine the asset level required for financial independence.
The simplified method will be least accurate for families who have most assets in tax-deferred accounts or who are more
than 10 years away from financial independence, as it does not account for inflation adjustments.

Once the required asset base is determined, use financial planning software or an investment calculator to figure out the additional annual savings needed to meet the financial independence goal, if any. If the annual savings requirement is unrealistic, extend the time to financial independence in five-year increments until it fits your situation. In aggressive scenarios, increasing annual savings can have a compounding effect by reducing the amount needed to fund your lifestyle, thereby decreasing the asset base required for financial independence.
Once goals have been defined, there are several strategies to accelerate the journey to financial independence and remove unnecessary obstacles with minimal effort:
• Planning for lifetime tax impact: Physicians often experience a reduction in taxable income when they stop practicing. If a future decrease in taxable income is anticipated, deferring capital gains or making pretax contributions to retirement accounts now can help realize this income in later, lower-tax years.
• Making sure assets are not dormant: Holding large balances in cash or underperforming investments for extended periods can delay reaching financial independence. It's crucial to make certain that assets are actively working toward your financial goals.
• Eliminating unnecessary insurance policies: While it's essential to protect your family with adequate coverage for life, disability, health, liability, and other risks, it's worth going over current coverage levels to avoid excessive coverage or unnecessary riders. Increasing policy deductibles can also reduce annual premiums, provided you have the cash on hand to cover these deductibles if needed. Lastly, as you accumulate more assets and approach financial independence, the need for life insurance often decreases. It's advisable to review your life insurance policies to determine if you can significantly reduce or even eliminate them, so your coverage aligns with your current financial situation.
In conclusion, achieving financial independence is a practical and empowering goal that offers flexibility and freedom in both your professional and personal life. By understanding your current financial situation, setting clear goals, and identifying ways to overcome obstacles, you can accelerate your journey toward financial independence. This approach not only enhances your financial security but also allows you to make choices that align with your values and passions. Whether or not early retirement is your goal, we hope these steps will guide your family toward a balanced and fulfilling life.
.
by Jim Blaine, MD
The Greene County Medical Society Community Health Advisory Committee (CHAC) has met several times over the past several months to discuss our mission to inform our community about the science based recommendations from medical experts on the topics of concern via TV and other media.
We have decided to initially focus on pediatric patients. Here are three of those topics along with a few examples of resources:
1) Risks associated with recreational marijuana use by youth. Advice to parents from the American Academy of Pediatrics (AAP), "Marijuana use in children can have harmful short-term and lifelong effects on their health and well-being. Marijuana use is often portrayed as harmless, but the truth is that marijuana can be an addictive drug, especially for teens, that can cause serious risks and consequences.
Start talking with your child at an early age about the dangers of marijuana use. Encourage them to ask questions and tell you about their concerns. Remember to listen, and do not lecture or do all the talking. You may find teachable moments from news stories or even TV shows or movies that portray marijuana use in their storylines."
2) Preventing Child Abuse.
According to the AAP, prevention of child abuse and neglect centers around supporting that families maintain safe, stable and nurturing relationships with their children. Fostering the development of these safe, stable and nurturing relationships protects and nurtures children’s development, allowing them to build and increase resilience to factors that may contribute to abuse and neglect. Protective factors, such as access to medical and mental health services, emotional support, positive community relationships and others can serve to prevent abuse and neglect as well. Springfield Child Advocacy Director Kat Dull, “Reporting suspected child abuse is a vital step in preventing further harm, as it allows professionals to intervene early, connect families with support services, and protect vulnerable children by addressing the root causes of abuse before the situation escalates— it's a request for help and assessment, not an accusation.”
3) Vaccine Hesitancy.
According to the World Health Organization, an estimated 107,500 people died worldwide from measles in 2023 – mostly children under the age of five years, despite the availability of a safe and cost-effective vaccine. The Associated Press reported that the U.S. recently surpassed 1,000 measles cases. Two unvaccinated school aged children died from measles-related illnesses in the epicenter in West Texas, and an adult in New Mexico who was not vaccinated died of a measles-related illness.
AAP advice to parents, "Vaccines are under constant study. For a vaccine to be recommended—as part of the childhood and adolescent immunization schedule —it must be tested, found safend closely monitored. Safety testing begins as soon as a new vaccine is made and clinical trials begin, and evidence of safety is
gathered for as long as it is in use.

When it is time for your child to receive recommended vaccines, you may want to know more about vaccines and vaccinepreventable diseases. Pediatricians get a lot of the questions from parents about vaccines. Many questions are sparked by misinformation found online and on social media. No question is too big or too small. It is important to talk with your pediatrician.”
The intent of the GCMS CHAC is to develop Public Service Announcements (PSAs) that can be broadcast on TV and social media to Springfield and the surrounding area. Our plan is to obtain the approval for each PSA from Cox and Mercy Pediatric Departments, the Springfield Greene County Health Department, the American Academy of Pediatrics, Burrell Behavioral Health, and the Greene County Medical Society Executive Council before airing. We are fortunate to have the support of both Cox and Mercy Healthcare systems and their teams. Hopefully, by presenting fully vetted PSAs, we will be successful in educating our community and especially the 9 parents. Having the support of our community partners, especially Cox Pediatric Director Kofi Asare-Bawuah, MD, Mercy Pediatric Director John Burson, MD, Child Psychiatrist Jaya LaFontaine, MD, Child Advocacy Center Executive Director Kat Dull, and MOAAP Executive Councilor Kayce Morton, DO, in this project is the key to success.

We have learned from AAP is currently activating a new immunization public awareness campaign addressing misinformation on a national level. We will hopefully begin our efforts by working with Missouri AAP. We are looking forward to that collaboration!
With Private Banking at Central Bank, you have exclusive access to a host of financial services and products, where we take care of the details across the full spectrum of the bank. You will have access to higher deposit rates, custom credit solutions and home financing, as well as individualized guidance with your investments. Our main goal is to help you maximize your money seamlessly. You have complex needs. We have the concierge level solutions you want.



STEVE GASSEL
Senior Vice President - Director of Private Banking | NMLS # 554828
3333 S. National Ave., Springfield, MO 65807
Phone: (417) 841-4213
Steve.Gassel@centralbank.net
KARA TURNER
Vice President - Private Banking | NMLS # 1833785
3333 S. National Ave., Springfield, MO 65807
Phone: (417) 841-4253
Kara.Turner@centralbank.net
JOYCE WONG-HSU
Officer - Private Banking | NMLS # 1239617
3333 S. National Ave., Springfield, MO 65807
Phone: (417) 841-4214
Joyce.Wong-Hsu@centralbank.net
To Advertise in this directory call Jean Harmison at the Society office: 417-887-1017.
Please Note: Changes to ads will be made quarterly and must be submitted in writing. H Denotes GCMS Membership “A” Denotes GCMS Applicant GCMS Member Ad Rates: $10.00 per 2” sq. • Non-Member Ad Rates: $13.75 per 2”sq.
Bringing physicians together to improve the health of our community.
Dermatology, Procedural
MICHAEL H. SWANN, MD H
BRETT NEILL, MD
MICHAEL KREMER, MD
JOHN CANGELOSI, MD
AUTUMN BERTHOLDI, PA-C
PATSY DUGGAN, PA-C
LORI MILLER, NP-C
HANNAH LEE, FNP-BC
BROOKLYN FORT, FNP-C
3850 S. National Ave, Suite 705 Springfield, MO 65807 (Located inside Hulston Cancer Building-7th floor)
1240 E. Independence Springfield, MO 65804
Phone: 417-888-0858 • Fax: 417-889-0476 www.swanndermatology.com
Hollister Location 590 Birch Rd, Ste 2c Hollister, MO 65672
PH. 417-690-3858 Fax 417-690-3862
Monett Satellite Location (Inside CoxHealth Urgent Care) 2200 E. Cleveland Ave Monett, MO 65708
Phone: 417-888-0858 • Fax: 417-889-0476
Lebanon Location 331 Hospital Drive Suite C Lebanon, MO 65536
Phone : 417-344-7200
Fax : 417-344-7299
Direct Primary Care
ASCENT DIRECT PRIMARY CARE, LLC
MATTHEW GREEN, DO H
Family Medicine www.ascentdpc.com 417-595-0956
413 N McCroskey, Ste 2 Nixa, MO 65714
EYE SURGEONS OF SPRINGFIELD, INC.
C. BYRON FAULKNER, MD H Comprehensive Cataract Ophthalmology
JUDD L. McNAUGHTON, MD H Comprehensive Cataract Ophthalmology Diplomates, American Board of Ophthalmology
1330 E. Kingsley St. • Springfield, MO 65804 Phone 417-887-1965 • Fax 417-887-6499 417eyecare.com
MATTAX • NEU • PRATER
EYE CENTER
JAMES B. MATTAX, JR., MD, FACS H American Board of Ophthalmology
LEO T. NEU III, MD, FACS H American Board of Ophthalmology
DAVID NASRAZADANI, MD
DREW A. YOUNG, MD
THOMAS PRATER, MD, FACS H American Board of Ophthalmology
JACOB K. THOMAS, FACS, MD H American Board of Ophthalmology
BENJAMIN P. HADEN, MD H American Board of Ophthalmology
MICHAEL S. ENGLEMAN, OD
MARLA C. SMITH, OD
MATTHEW T. SMITH, OD
1265 E. Primrose Springfield, MO 65804 417-886-3937 • 800-995-3180
Family Medicine
COXHEALTH
FAMILY MEDICINE RESIDENCY
FAMILY MEDICAL CARE CENTER
3800 S National Ste 700 Springfield, MO 65807 (417) 269-8817
AmericAn BoArd of fAmily medicine
Marc Carrigan, MD
Cameron Crymes, MD
Kristin Crymes, DO
Kristen Glover, MD
Kyle Griffin, MD
Shelby Hahn, MD
Laura Isaacson, DO
Evan Johnson, MD
Katie Davenport-Kabonic, DO
Michael Kabonic, DO
Jessica Standeford, MD
Gynecology
WOMAN’S CLINIC www.womansclinic.net
Leaders in Minimally Invasive Gynecology & Infertility
DONALD P. KRATZ, MD, FACOG H American Board of Obstetrics and Gynecology
AMY LINN, FNP-BC American Academy of Family Nurse Practitioners
ANGIE JONES, WHNP-BC 1135 E. Lakewood, Suite 112 Springfield, MO 65810
Located inside Tri-Lakes Family Care 1065 Hwy 248 Branson, MO 65616
Phone 417-887-5500
Fax 883-8964 or toll free 877-966-2607 Monday-Thursday 8am-4:30pm Friday 8am-12pm
MERCY CLINIC–INTERNAL MEDICINE WHITESIDE
RAJ ANAND, MD
JAMES T. ROGERS, JR. MD, FACP H Board Certified in Internal Medicine
MARIA DELA ROSA, MD
NELSON DELA ROSA, MD
AMANDA MCALISTER, MD
ALEJANDRA ROA, MD
KELLY TRYGG, MD
GABBY BONNER, NP
STEVEN BOWLIN, MD Board Certified in Internal Medicine
STEPHANIE HOVE, NP
CARRIE KUGLER, PA
COURTNEY WEATHERFORD, PA
JENNIFER WHITE, PA
VICTOR GOMEZ, MD
Board Certified in Internal Medicinee 2115 S. Fremont, Suite 2300 Springfield, MO 65804
Phone 417-820-5600 Fax 417-820-5606
MERCY CLINIC UROLOGY (FREMONT)
ERIC P. GUILLIAMS, MD, FACS H American Board of Urology
ROBERT D. JOHNSON, MD, FACS H American Board of Urology
TYRUN K RICHARDSON, MD American Board of Urology
MARK J. WALTERSKIRCHEN, MD, FACS
American Board of Urology
Phone 417-820-0300
Fax 417-882-9645
1965 S Fremont, Ste. 370 Springfield, MO 65804
ADULT MEDICINE & ENDOCRINOLOGY
JONBEN D. SVOBODA, MD, FACE, ECNU
American Board of Endocrinology
JAMES T. BONUCCHI, DO, ECNU, FACE
American Board of Endocrinology
NICOLA W. GATHAIYA, MD, ECNU, FACE, CCD
American Board of Internal Medicine
American Board of Endocrinology
STEPHEN M. REEDER, MD, FACP
American Board of Internal Medicine
ANA MARCELLA RIVAS MEJIA, MD, CCD
American Board of Internal Medicine
American Board of Endocrinology
JACQUELINE L. COOK, FNP-BC, CDCES, CCD
KELLEY R. JENKINS, FNP-C, CDCES
ALINA CUMMINS, PA-C
STACY GHOLZ, FNP-C
SHELLEY L. CARTER, DNP
JESSICA A. CROUCH, FNP-C
Phone (417) 269-4450
960 E. Walnut Lawn, Suite 201 Springfield, MO 65807
Nephrology

SPRINGFIELD NEPHROLOGY ASSOCIATES, INC.
1911 South National, Suite 301 Springfield, MO 65804
Phone 417-886-5000 • Fax 417-886-1100 www.springfieldnephrology.com
STEPHEN E. GARCIA, MD H
American Board of Internal Medicine
American Board of Nephrology
ETHAN T. HOERSCHGEN, MD
American Board of Internal Medicine
American Board of Nephrology
GISELLE D. KOHLER, MD H
American Board of Internal Medicine
American Board of Nephrology
DAVID L. SOMMERFIELD, MD
American Board of Internal Medicine
American Board of Nephrology
SUSAN A. WOODY, DO H
American Board of Internal Medicine
American Board of Nephrology
SPRINGFIELD NEUROLOGICAL AND SPINE INSTITUTE
CoxHealth Jared Neuroscience
West Tower • 3801 S National, Ste 700 Springfield, MO 65807 • 417-885-3888
Neurosurgery:
H. MARK CRABTREE, MD, FACS
EDWIN J. CUNNINGHAM, MD
MAYUR JAYARAO, MD
J. CHARLES MACE, MD, FACS H
CHAD J. MORGAN, MD
MICHAEL L. MUMERT, MD
SALIM RAHMAN, MD, FACS
ANGELA SPURGEON, DO
ROBERT STRANG, MD
Interventional Neuroradiology
MICHAEL J. WORKMAN, MD
Physiatry:
TED A. LENNARD, MD
KELLY OWN, MD
JESSE STOKKE, DO
Physician Assistants:
JOSHUA BARBIERI, PA-C
MARK BROWN, PA-C
ERIC CHAVEZ, PA-C
KEVIN STOKES, PA-C
HEATHER TACKETT, PA-C
Nurse Practitioner:
EMILY CROUSE, NP-C
MINDY GRANT, NP-C
ROZLYN MCTEER, FNP
BRANDON RUBLE, ACNP-AG
ALYSSA CHASTAIN, FNP
COXHEALTH
PRIMROSE OB/GYN
MARCUS D. MCCORCLE, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
THOMAS M. SHULTZ, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
GREGORY S. STAMPS, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
P. MICHAEL KIDDER, DO, FACOOG
Diplomate, American Osteopathic Board of Obstetrics & Gynecology
Phone 882-6900
1000 E. Primrose • Suite 270 Springfield, MO 65807
SPRINGFIELD OB/GYN, LLC
MATTHEW H. TING, MD, FACOG H
American Board of Obstetrics & Gynecology
909 E. Montclair, Suite 120 Springfield, MO 65807
Phone 417/882-4466 • Fax 417/890-5631
ONCOLOGYHEMATOLOGY
ASSOCIATES OF SPRINGFIELD, MD, P.C.
WILLIAM F. CUNNINGHAM, MD, FACP
American Board of Internal Medicine
American Board of Medical Oncology
JIANTAO DING, MD H
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
ROBERT J. ELLIS, MD, FACP
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
BROOKE GILLETT, DO
American Board of Internal Medicine
American Board of Medical Oncology
V. ROGER HOLDEN, MD, PhD
American Board of Hematology
American Board of Medical Oncology
DUSHYANT VERMA, MD, FACP
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
Springfield Clinic 3850 S. National, Ste. 600 Springfield, Missouri 65807
Monett Clinic 802 US Hwy 60 Monett, Missouri 65708
Phone 882-4880 Fax 882-7843
Visit our website: www.ohaclinic.com
MERCY CLINIC–EAR, NOSE & THROAT
BENJAMIN L. HODNETT, MD, PHD H
ERICH D. MERTENSMEYER, DO, FAOCOO
AARON R. MORRISON, MD
A. DANIEL PINHEIRO, MD, PhD, FACS H
RAJEEV MASSON, MD
MARK J. VAN ESS, DO, FAOCOO Diplomates, American Board of Otolaryngology
SHELBY BRITT, PA
MELISSA COONS, FNP
TAHRA LOCK, NP
ELIZABETH (BETSY) MULLINGS, FNP
PAUL STRECKER, FNP Audiology
JASON BOX, AuD, CCC-A
MAMIE JAYCOX, AuD, CCC-A
JENNIFER PLOCH, AUD
ALLISON WHITE, AUD, CCC-A
Phone 417-820-5750 Fax 417-820-5066
1229 E. Seminole, Ste. 520 Springfield, MO 65804
MERCY CLINIC–FACIAL PLASTIC SURGERY
MATTHEW A. KIENSTRA, MD, FACS American Board of Facial Plastic & Reconstructive Surgery American Board of Otolaryngology
Phone 417-887-3223
1965 S. Fremont, Ste. 120 Springfield, MO 65804 facialplasticsurgeon.com
JAMES E. BRIGHT, MD H Diplomate, American Board of Psychiatry & Neurology.
Practice Limited to: Adult Psychiatry
Phone 882-9002
1736 E. Sunshine, Ste. 400 Springfield, MO 65804

At
chAnge Service requeSted
