






Katiina
Student Loan Interview with Carlee Lynn, CFP Jon
From

Editor’s Note: All materials for the Journal must be submitted by the first of the month prior to publication.
Co-Editors:
Jim Blaine, MD
Minh-Thu Le, MD
Junior Co-Editor: Andrew K. Le
Managing Editor: Dalton Boyer
Editorial Committee:
Michael S. Clarke, MD
David Barbe, MD
Jaya LaFontaine, MD
Dalton Boyer
Andrew Le
Jean Harmison
Barbara Hover
Frank Cornella, MD
SOCIETY OFFICERS
James Rogers, MD
President
Vu Le, MD
Secretary
Jim Blaine, MD
Treasurer
Sanjay Havaldar, MD Immediate Past President
Council Members:
David Haustein, MD, MBA
Melissa Gaines, MD
Steven Gradney, MD
Keith LaFerriere, MD
Kyle John, MD
Jaya LaFontaine, MD
John Steinberg, MD
Managing Director: Jean Harmison
Executive Office: 4730 S. National Ave. Suite A1 Springfield, MO 65810 email: director@gcms.us www.gcms.us
All communications should be sent to the above address. Those marked for the attention of a particular officer will be referred.
by Jim Blaine, MD
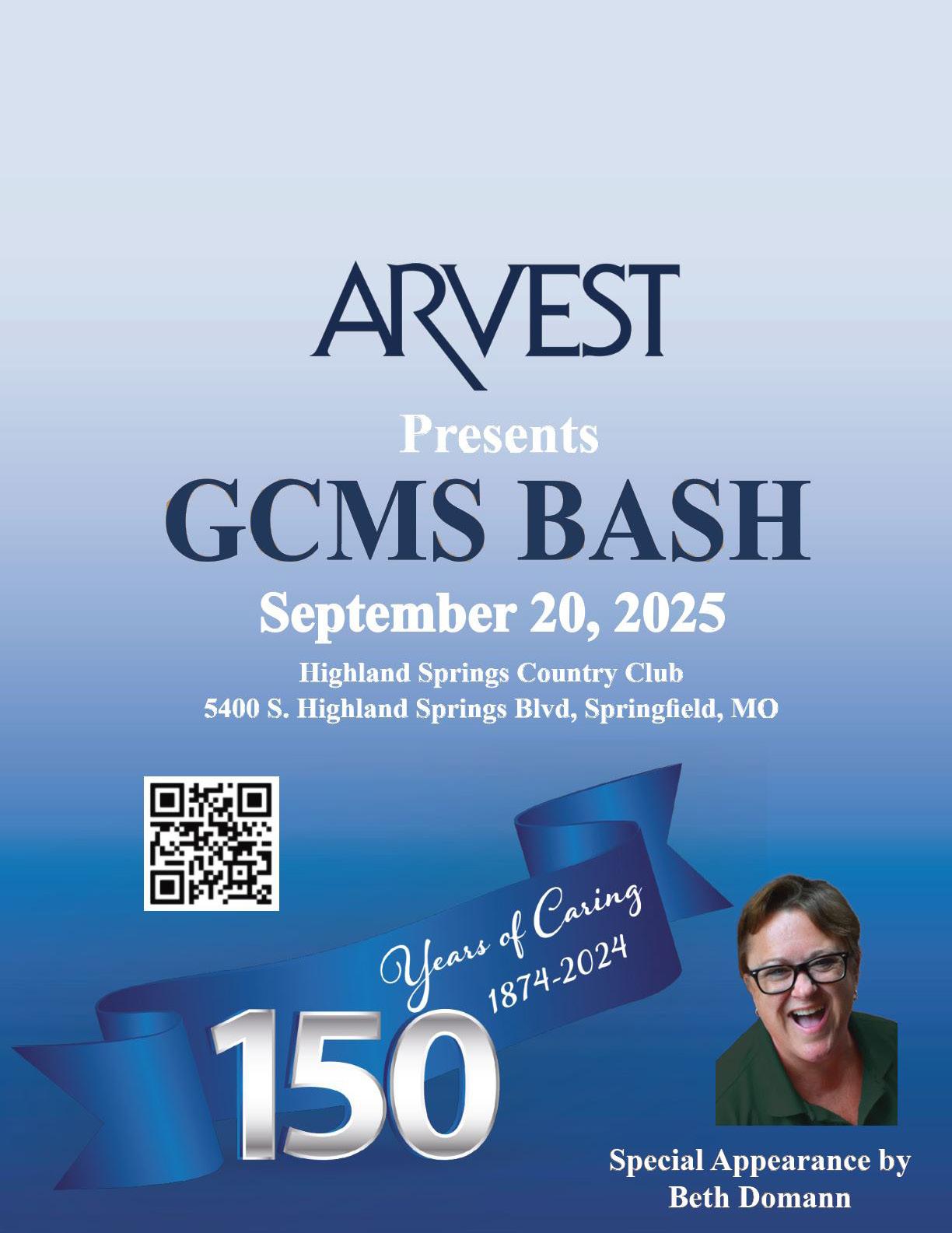
This issue pays tribute to the Greene County Medical Society’s 150th Birthday and the physicians who have devoted their lives to the community they serve!
The GCMS committee tasked with the duty of bringing the celebration to life on September 20th at the Highland Springs Country Club includes Co-Chair Vu Le, MD, GCMS President J.T. Rogers, MD, GCMS President Elect Melissa Gaines, Former GCMS President Keith LaFerriere, MD, Former GCMS President Kayce Morton, DO, GCMS Membership Chair Steven Gradney, MD, and our wonderful GCMS Executive Director and Co-Chair Jean Harmison.
Our GCMS Bash evening will be graced by the stand-up comedy of the amazing Beth Domann. Beth has been making us laugh since she first stepped onto the Landers Stage in 1978. She was named “The funniest person in Springfield” in 1990.

Beth recently took time away from her job as Executive Director of the Springfield Little Theater to return to her stand-up comedy roots in the soldout performance of “I Get a Kick Out of You” at the Landers Theater. Barb and I attended the event and witnessed multiple standing ovations as Beth entertained us nonstop for over two hours.
Beth has strong roots with GCMS and did not hesitate to accept when we asked her to share her talent with us at the GCMS Bash. Her father, well known plastic surgeon Darrel Domann, MD was GCMS President in 1992. Her mother Barbara Domann was GCMS Alliance President in 1995. It will be an evening to remember, and we hope you will join us to celebrate!
There have been many GCMS accomplishments over the years including the Singing Doctors, the GCMS Flu vaccination program headed by our current GCMS President Jim Rogers, MD., multiple public health related laws passed and many more.
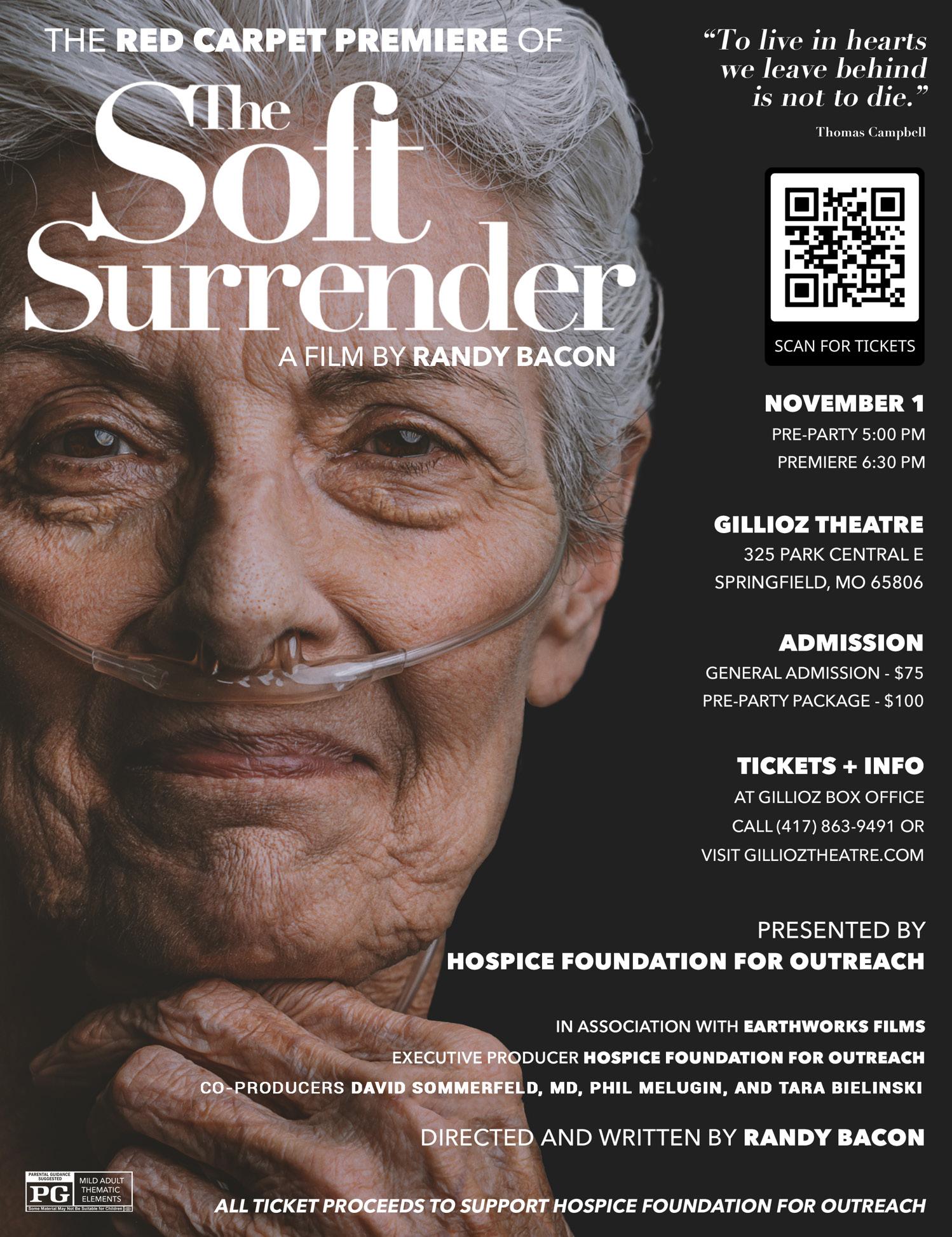
This issue includes an announcement of the much-needed Child Advocacy Center (CAC) Capital Campaign by CAC

Executive Director Kat Dull. The new CAC will be named after former GCMS President John P. Ferguson, MD in recognition of his contribution to the safety of children of Springfield and the surrounding area. The GCMS is proud to have played a small part in the founding of the CAC, and we congratulate them on their 30th anniversary. Molly Jones, M3, also reflects on her time at the CAC during her clinical campus pediatric rotation and sponsored by the GCMS foundation.
Other articles in this issue include two articles on the hot topic Artificial Intelligence (AI). One is by former AMA President and GCMS Editorial Board member David Barbe, MD. The other is by AI Advisor, and Cox/ Ferrell Duncan allergist-immunologist William Micka, MD.
Please also check out our GCMS Rocky Mountain Medicine pictures along with Jean and Jerry Harmison’s 40th Anniversary article and pictures covering their trip to the Canadian Rockies!

by James Rogers, MD
Two months of incessant rain, followed by six weeks of bone-dry weather and overlapped with three weeks of smothering heat; we must be in Missouri! Our weather teaches us the importance of recognizing patterns and trends in helping us manage and mitigate future events. These principles are used by all of us every day in our practice of delivering care. The better understanding of disease patterns and progression integrated into evidence-based interventions is a foundational tool in the practice of medicine. We use these experiences, growing and expanding constantly to deliver our best care every day.
For the last 150 years the Greene County Medical Society has consistently advanced professional medicine, public health, community advocacy, and physician support, adapting to meet evolving healthcare challenges while remaining grounded in its founding mission of improving health throughout SW Missouri. Just a few of the “patterns” from the GCMS include:
Early activities:
• Founded in 1874 in the post–Civil War era, focused on professional development, ethical practice, and sharing medical insights.
• Early 1900’s partnered to educate about tuberculosis via educational articles and public campaigns.
• Established baby clinic and permanent baby ward , providing free or low-cost care to infants and reducing infant mortality.
Last thirty years:
• DWI Task Force reducing morbidity and mortality from MVA’s
• Child Advocacy Center (CAC) : GCMS has been supporting the CAC continually for over thirty years in an

effort to assist pediatric victims of child abuse and neglect.
• AED Center of Excellence creating a model for the country

• Springfield Flu Immunization Coalition , providing flu shots for over 13 years
Additional accomplishments:
• 2017, GCMS member Dr. David Barbe became AMA President and hosted:
• opioid crisis dialogue and educational events
• physician burnout seminars and education
• GCMS Alliance , the spouses’ organization, is celebrating 100 years! Dedicated to physician support and community health through education, they have many wonderful successes:
• “ Smoking makes Me Ugly ” school education about tobacco dangers.
• “ Pills are not a Party ” revealing the dangers to school aged youth.
• Family Zoo night and Night at the Museum long traditions for families to connect, support, and engage in future projects.
Sharing just some of this history hopefully will add to each of our understandings of the rich legacy we have. Please join in* and let us all (doctors and spouses) challenge each other to create the next chapter in public service!
*Come to the GCMS BASH for an evening of great fun and camaraderie, Sept. 20th.
*Sign up for the Family Zoo night and bring the family! It is about good-’ole family fun, Aug. 23rd.
*Join GCMS and Alliance to make your voice heard in our vibrant medical community.

Tailored Tax, Wealth Management, and Family Office to help you prepare for what’s next.
By David Barbe, MD
There is no question that Augmented Intelligence (AI) in healthcare is the most controversial topic currently and will be for years to come. There is also no question that it offers tremendous promise to improve numerous facets of healthcare, but at the same time, raises almost as many concerns.
I use and highly recommend that in the vast majority of cases when we reference “AI” in healthcare that we use Augmented Intelligence as the working definition. The information generated by AI algorithms will be used to inform or “augment” the work of physicians, other healthcare workers, researchers, healthcare administrators, and patient self-care. For the foreseeable future, it will rarely be fully autonomous. Professional oversight and “trust but verify” will be the order of the day for quite some time to come.
The other observation regarding AI in healthcare is that we are in the infancy of the potential use and benefit of this technology. That is, at the same time, the reason for the great excitement about the potential but also the concern. Although it is impossible to predict the rate at which any particular use of AI will progress, my prediction is that progress in all areas will accelerate and result in more rapid and dramatic changes than we think.
The breadth of uses for AI in healthcare is so great that it is not possible to provide more than an overview in this article. However, I will address a few of the current and near-term uses of AI and also some of the major concerns. Current Uses of AI in Healthcare.
Most of us have already been using basic AI technologies. Speech recognition programs such as Dragon™ depend on AI natural language processing. The next step up: Dragon Ambient eXperience (DAX™) Copilot couples speech recognition with other AI algorithms to record and analyze the conversation during a patient encounter in real-time to produce clinical documentation for review and editing by the clinician. Similarly, some EHRs now review incoming patient messages and generate a draft response for use by the clinical team using a process often referred to generative AI.
One step beyond that is a process known as “Agentic AI.” This uses more advanced algorithms to process diverse data sources like clinical notes, patient histories, lab results, and medical guidelines to make clinical decisions and take

action, often with limited human oversight. This differentiates it from generative AI. This technology is already being used by some health systems to provide direct responses to patient inquiries. This autonomous use of AI has been a source of greater concern for physicians, other health technology experts, and regulators.
Another current clinical use of AI decision-support algorithms is the analysis of a patient’s clinical record and the generation of alerts and prompts that help guide and improve clinical decision-making at the point of care. Similarly, proprietary clinical and public search engines employ AI algorithms to rapidly and accurately identify reliable clinical information and summarize responses to clinical queries.
Multiple other current clinical uses of AI include the increasing use of image recognition to enhance radiologic interpretations, predictive analytics to enhance proactive, personalized clinical decision-making which tailor treatments based on an individual patient’s genetic, environmental, and lifestyle data, AI assisted robotic surgery, and virtual health assistants or “chat bots” to support patient engagement, education, and utilization of data from wearable clinical devices.
Research is another area of current use and immense future potential. Advances in pharmacogenomics, identification of promising compounds and their predicted efficacy and toxicity, as well as accelerating timelines for clinical trials are just a few of the ways new drugs and treatment protocols can be delivered faster, more efficiently, and at a lower cost through the use of AI.
Another category for the use of AI is in improved administrative and operational efficiencies. AI programs are already being used to assist with responses to prior authorization requests for medications, diagnostic tests, procedures, and other treatments. AI being used to improve population health management and predict patient outcomes and readmission risk, thereby providing an opportunity for earlier interventions. Hospital uses include automated dispensing, supply chain monitoring and management, patient outcomes monitoring, and AI enhanced quality improvement processes.
The combination of these and other current and future
uses of AI will substantially improve diagnostic accuracy, accelerate use of evidenced-based treatments, reduce ineffective treatments and medical errors, and improve patient access to care all leading to improved patient outcomes and reduced costs. These technologies are also expected to significantly reduce the administrative and cognitive burden on physicians, addressing several of the key contributors to physician professional dissatisfaction and burnout.
Most of the future potential of AI in healthcare relates to continued evolution of the uses that are currently in their infancy resulting in greater accuracy in diagnosis, personalized treatments, disease prediction, and preemptive interventions. These advances will be accompanied by our understanding of how to better utilize the capabilities of AI. An AI guided search of the most aggressive predictions for AI in healthcare over the next 10 to 20 years yielded predictions of AI as the primary diagnostician, full automation of routine procedures and surgeries, major advances in preventive healthcare and longevity, mental health support and AI “companions”, decentralization of healthcare with much more care provided in homes reducing need for hospitalizations, and major advances in telemedicine to serve geographically and economically underserved populations leading to significant improvements in global health equity.
As noted, the list of risks and concerns regarding the use of AI in healthcare is nearly as long as the potential uses and benefits. Development of AI algorithms is not immune to the old adage “garbage in, garbage out.” Significant concerns exist regarding conscious and unconscious bias in the development and training of AI algorithms. Just as in other research, incomplete or inaccurate data or data not representative of the population to which outcomes may be applied will result in inaccurate and unintended outcomes. Similarly, not all AI algorithms and platforms are equally robust (capable). Assuming the accuracy and reliability of one algorithm is as good as another is erroneous.
One of the major features of AI algorithms is their capacity to learn – that is, continually and iteratively evolve their logic based on cumulative data with the intent to become increasingly more accurate at producing the desired outcome. However, even minor biases in initial algorithm logic or in the initial or subsequent data input can lead to significant inaccuracies in outcomes over time.
Due to the potential for such inaccuracies, accountability and liability for adverse outcomes related to the use of AI is a major concern of providers. This is compounded by the lack of deep learning AI models to provide an explanation
for outcomes. They become, in effect, a “black box” leading to mistrust by physicians and other decisionmakers. This also raises safety concerns and complicates the development of regulations regarding AI programs as well as evaluation and adoption of AI-based tools by hospitals and health systems.
Optimum utilization of these algorithms depends on analysis of large volumes of data. This invokes multiple issues involving access to patient data, quality of data, confidentiality of data, patient privacy, transparency, permission, use of the data as well as use of the output of the programs. These issues result in a myriad of ethical concerns in the use of AI.
An additional area of concern involves social and professional risks. Whether spoken or unspoken, many physicians and other healthcare workers wonder “Will I be replaced by AI?” The many uses of AI certainly do have the potential to improve efficiency and should allow all healthcare workers to be more productive and do more of their work at “top of license.” This is also expected to help ease the shortage of physicians, nurses, and other healthcare workers.
However, for the foreseeable future, AI will support or augment, not replace, physicians and other healthcare workers. Human judgment remains essential in healthcare decisions and delivery, just as human interaction is indispensable in the relationship between the patient, his/ her physician, and their healthcare team. Will it change the way care is delivered, and the way these relationships look and feel? Absolutely. Will it do away with the “art” of medicine, the need for physician oversight, and the therapeutic benefit of the relationships between patient and caregiver? Absolutely not – at least not in most of our professional careers, if ever. I’ll come back to this thought.
Our journey into the new world in the use of AI - augmented intelligence – in healthcare is as exciting as it is challenging. It requires our full involvement as physicians to help shape the development and use of this new technology and the application and implications of it. I agree with the conclusion of the AI generated search which stated, “While these changes could bring about unprecedented improvements in human health and longevity, they also require careful navigation of ethical, social, and practical challenges to ensure that the future of medicine is both technologically advanced and fundamentally humane.”
“Fundamentally humane.” That’s where physicians, nurses and other healthcare workers bring the greatest value to healthcare now and for the future. The World Medical
Association’s Declaration of Geneva is an oath or pledge one can take as a member of the medical profession. Some refer to it as a “modern Hippocratic oath.” I have quoted the first 4 lines of the Declaration below. I think it speaks to the altruism and humanity of physicians and many others who work in the medical profession. The beliefs and commitment described in these lines cannot and will not be replaced by AI. I hope this is reassuring and inspiring in the face of an AI driven healthcare future.
I SOLEMNLY PLEDGE to consecrate my life to the service of humanity;
THE HEALTH AND WELL-BEING OF MY PATIENT will be my first consideration;
I WILL RESPECT the autonomy and dignity of my patient;
I WILL MAINTAIN the utmost respect for human life;
References:
1. Laviola, Erin, May 8, 2025, What is Agentic AI and How Can It Be Used in Healthcare. HealthTech. https://healthtechmagazine.net/article/2025/05/ what-is-agentic-ai-in-healthcare-perfcon
2. Canadian Journal of Health Technologies, Vol 5, Issue 3, March 2025. 2025 Watch List: Artificial Intelligence in Health Care. https://canjhealthtechnol.ca/ index.php/cjht/article/view/ER0015
3. Olawade, David B. et al. (2024). Artificial intelligence in healthcare delivery: Prospects and pitfalls. Journal of Medicine, Surgery, and Public Health. Vol 3, Article 100108. https://www.sciencedirect.com/science/article/pii/ S2949916X24000616
4. Chustecki, Margaret. (2024) Benefits and Risks of AI in Health Care: Narrative Review. Interact J Med Res 2024, vol. 13, e53616. https://www.i-jmr.org/2024/1/ e53616
5. Alowais, Shuroug A. (2023) Revolutionizing healthcare: the role of artificial intelligence in clinical practice, BMC Medical Education. Article number 689
6. American Medical Association (2023) AMA Future of Health: The Emerging Landscape of Augmented Intelligence in Health Care
7. World Medical Association (2017) WMA Declaration of Geneva
Hannah Newland - Hello! My name is Hannah Newland, and I am from Neodesha, Kansas. I was part of the inaugural class of the collaboration between Missouri Southern State University and Kansas City University for early acceptance into medical school, so I lived in Joplin for 8 years before moving for my residency. I graduated with a pre-med biology major and a Spanish minor in 3 years, then started at KCU-Joplin College of Osteopathic Medicine. While there, I completed a fellowship in Osteopathic Manipulative Medicine (OMM) and was able to expand my OMM skills, while also teaching the first- and second-year medical students.

the classroom, or in practice.
I live with my 9-year-old daughter, who might love Taylor Swift music more than I do! We enjoy singing at the top of our lungs, going to the aquarium to see our favorite animals (sharks and penguins!), and just about anything Disney. We love the Kansas City Chiefs, and she can’t wait to see them in person. In our free time, we enjoy being back home on the farm with our family.
I am an active member of the Missouri Association of Osteopathic Physicians and Surgeons and seek to advocate for my patients and the osteopathic profession. I have been to Jefferson City to advocate both for and against potential bills that affect our community. After residency, I plan to become board certified in Osteopathic Neuromuscular Manipulative Medicine (ONMM), helping patients, and continuing to teach future DOs, whether in
Cole Irwin - Hello! My name is Cole Irwin, and I am from the town of Van Buren, Arkansas. I went to Missouri Southern State University in Joplin, MO for my undergraduate education where I received a Bachelor of Science in Biology. I then went on to earn a Doctor of Osteopathic Medicine at Kansas City University Medical School in Joplin, Missouri as well. Now, I am at Jordan Valley to complete my residency training in family medicine to better serve communities like the ones I grew up in and went to school in.

In my free time I enjoy playing music (mainly guitar and piano), rock climbing, playing disc golf, watching movies, and hiking. I also frequently compete in recreational sports--mainly pickleball and volleyball. I’m new to Greene County, so I have recently been trying the local restaurants and attractions and have been loving it all so far!
Born, raised, and trained in the Ozarks, I have come to love this area and plan to build my future practice here as well. I am primarily interested in serving as an outpatient clinic physician to serve the communities that have provided for and done so much for me in my life. It is my goal and desire to give back what all I can of that and improve the health and lives that those that live there.
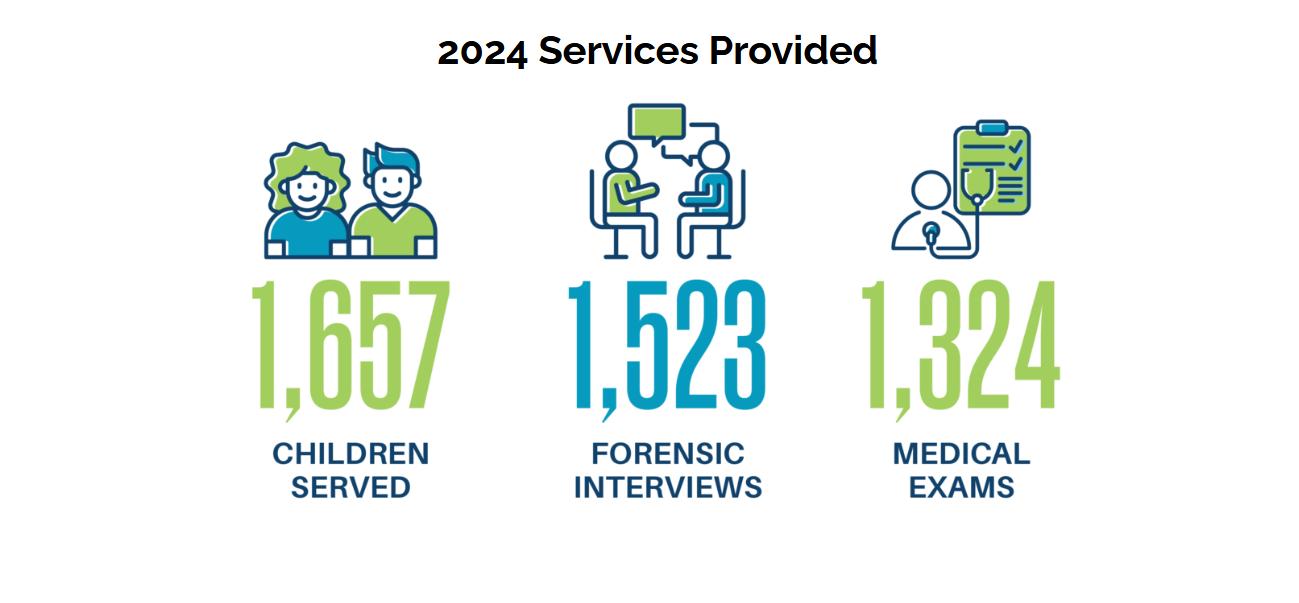
by Katiina Dull, Executive Director, Child Advocacy Center
For 30 years, the Child Advocacy Center has been serving children and families who are navigating child abuse and neglect in our community. Our mission has been focused and unchanged for all of these years.
The Child Advocacy Center exists to support the investigative process of child abuse and neglect concerns. We do this because we know 90% of child victims know, love, or trust their abusers. This makes it incredibly difficult for child victims to share their experiences and for investigative teams to take action that ensures safety and accountability. The Child Advocacy Center provides a safe place where kids can talk about what they may have experienced with a forensic interviewer who can walk with them through tough conversations without causing more pain. They can also receive a medical examination conducted by a SAFE CARE provider. The methods used are backed by research and always put the child first—no matter what.
The Child Advocacy Center operates much like an emergency room – it can not turn away a referral. As caseloads continue to rise, so do wait times. Not long ago, the Child Advocacy Center was meeting its goal of seeing every child within 6 days of referral. Now, wait times are stretching to 10-day averages. Even when a child is not in immediate danger, the weight of the details and the secrets of their abuse is an unbearable burden to carry. Ten days can feel like an eternity.
The Child Advocacy Center’s cozy historic home on Walnut Street, which has welcomed children, families, and investigative teams for 28 years, can no longer meet the needs of the region. Sadly, the demand for services is at an all-time high, and the current facilities are unable to keep up We have exhausted all options to provide the timely and highquality services needed from this home. We have loved it, and it has provided comfort for so many children, but the time has come for the CAC to make a change.

I am thrilled to announce the launch of our transformational capital campaign.
For the past year, we have been working quietly in the background to pursue funding and identify a suitable site

for relocation. After a lengthy search, the CAC is under contract on a location and expects to close on the property in the first week of August. The building being purchased will have a 10,000sq. ft. addition built onto the existing structure to meet the CAC’s space and expansion goals. The new location will be named in honor of Dr. John P. Ferguson.
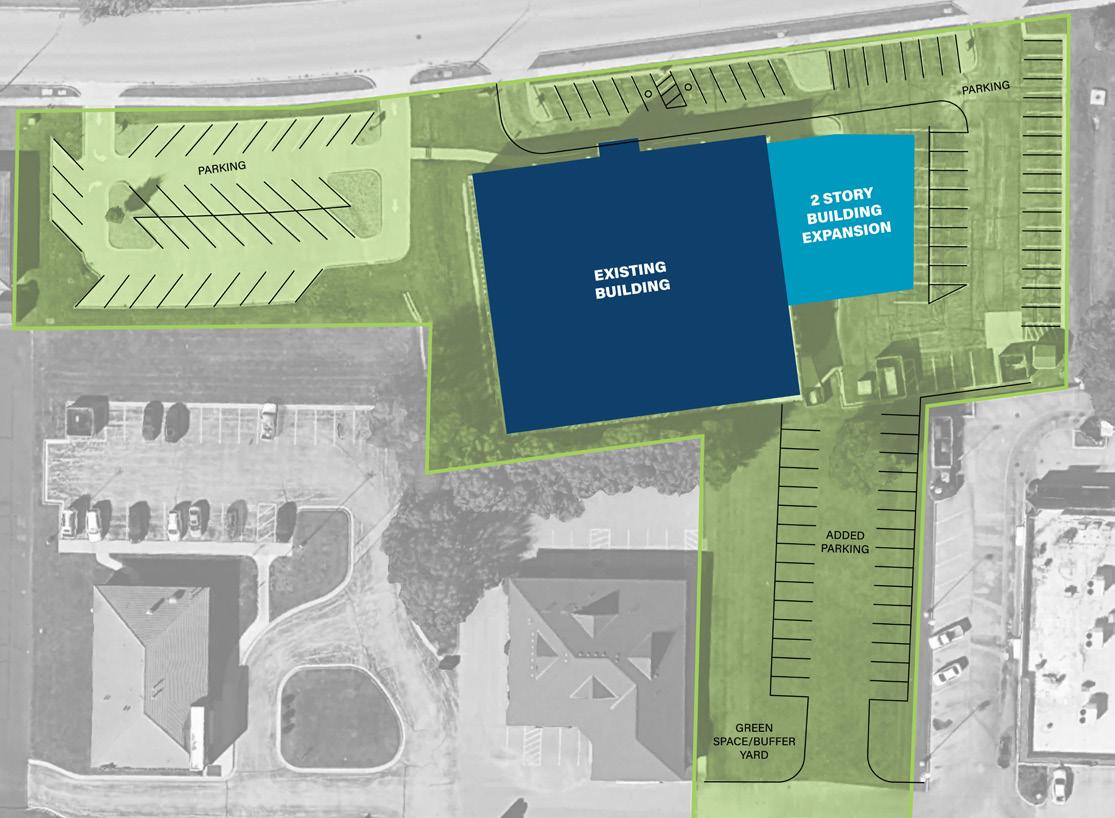
During his lifetime, Dr. Ferguson was committed to helping child victims of sexual abuse. He was one of the few physicians who were willing to perform the most sensitive of exams to ensure children were safe. As he neared retirement, Dr. Ferguson was instrumental in the formation of the CAC. I can think of no one better to name our new location in honor of.
The total campaign goal is $8M – it is unbelievable to share that we already have $5M secured! I want to recognize the Ferguson family, the Musgrave Foundation, the estate of Kathleen Griesemer, Guaranty Bank, Representative Alex Riley, and other donors who have chosen to remain anonymous, whose early support helped kick-start this campaign.
The new CAC location will provide the needed space and programming to ensure children and their families can find safety and healing promptly. Furthermore, it will improve and expand resources and support for the multidisciplinary team professionals working diligently to end child abuse and neglect in our region. We provide services across 14 counties and collaborate with over 70 agency partners, including the children’s division, law enforcement, juvenile officers, and prosecuting attorneys. This is not just a building project—it is a community commitment to ensure that no child waits for help, and every child has the chance to heal.
To learn more about the CAC or its active transformational capital campaign, please reach out to Katiina Dull, Executive Director – kdull@childadvocacycenter.org or call 417.831.2327.
Jim Blaine, MD
Jim Ferguson Alesha Gonzales
John Griesemer Ami Miller
Sean McQueary
By Jonathan Vance, CFP® | Senior Advisor II | Forvis Mazars Private Client
Introduction:
Carlee Lynn, CFP®, is a managing advisor in our Springfield office with five years of experience serving clients. Carlee has had the opportunity to serve several early- to midcareer individuals and couples as they navigate financial questions relevant to those stages of life. Often, one of these questions revolves around debt reduction, with one of the largest debts at this stage being student loans. I asked Carlee to sit down with me and answer questions pertinent to this journal’s readership. Our interview and insights are below.
Jon : Carlee, how did you get started in student loan planning and how many physicians have you helped with student loans as we stand today?
Carlee : I got started with student loan planning because I was working with our physician-focused team here. And as we got introduced to more physicians who were earlier on in their career, we realized that one of the biggest places of need that they had was around student loan planning and that we needed someone to know how to help them. That was around the time right after the pandemic, when a lot of things were changing with student loans. So, I had resources to learn a lot about the programs available around student loans, and just really dug into the information that was publicly available. Then, as I started helping more and more physicians walk through the process, I learned more about what that looks like for people, for physicians who have student loan debt. As far as the number of physicians I’ve helped with student loans, I’d say approximately 24 to 30 individuals and couples.
Jon : What are the most common missed opportunities you come across with physician student loans?
Carlee : I would say there’s two popular ones. The first is related to pursuing forgiveness of student loans and one unrelated to pursuing forgiveness. One of the biggest missed opportunities that I see when physicians are hoping to have some of their loans forgiven is knowing if continuing down the forgiveness path and making those income-based monthly payments is actually going to be worth it for them at the end of those 120 payments. Meaning, has the physician calculated what balance they anticipate being forgiven at the end of their journey? Have they logged into their service or website and checked on what progress has been made and recorded for them? And the number of payments that have been counted

toward their forgiveness of the 120 that they must make, what total are they currently at and how is their career going? Are they advancing in their career and getting considerable increases in their income, which is also increasing their monthly payments every year when they recertify? So, are they really keeping tabs as I go through this repayment process pursuing forgiveness, and does it still make sense along the way? Because sometimes, even midway through, it stops making sense. And then that’s when we should pivot and try to save them a little money month over month, rather than having them still make those higher income-based repayments.
The other missed opportunity that I see is with physicians who are not pursuing forgiveness for whatever reason that they have chosen. They are not always aware of the best way to pay off their student loans on their own. There are opportunities, whether you have federal or private loans, to lower your monthly payments to keep that amount as low as possible to give you flexibility for lump sum payments, either quarterly or annually, to pay down the loans. That can allow the physician to be flexible and use that monthly income maybe for other debts or other savings goals. I think the strategies available when you’re not pursuing forgiveness are also something that aren’t as commonly known. And it’s really easy to miss finding the best way to have the lowest monthly payment.
Jon : Can you speak to the differences of federal versus private student loans and how having more of one or the other might impact your repayment strategy?
Carlee : Yes. Federal student loans are loans funded and issued by the federal government. You’re often going to find federal student loans through the university where you go to school when you’re doing your financial aid. Federal loans have a lot of benefits, such as fixed interest rates and the ability to make income-based repayments once you graduate. It’s an even larger benefit for nonphysicians with lower starting salaries, but they can still be beneficial to physicians. Private loans are going to be issued by banks, credit unions, or other financial institutions and will often have higher interest rates. The terms are going to be set by the lender, so they could always change. As for having a concentrated balance in federal versus private loans for repayment, federal loans are the only type of loan that qualifies for forgiveness of the loan balance at any point in your career. All private
loans have to be repaid in full to the lender, subject to the terms of the lender. The biggest differences you’re going to see are in the options for forgiveness and flexibility, and repayment.
Jon : How do changes in employment, such as transitioning from residency to a full-time position, affect student loan repayment options?
Carlee : The biggest difference with the choice to change employment situation coincides with changes in income. For example, with residency to full-time attending, your income is going to increase drastically. And when you are repaying a federal student loan, if you’re pursuing forgiveness, you will have to recertify every year what your income was for the past year. That determines what your new monthly payment amount is. So, when you transition to a full-time attending income, your monthly payment is going to increase as well based on that new income. The question the physician should ask is, does it still make sense for me to make income-based repayments and pursue forgiveness?
The other change that you can see in employment is your eligibility for forgiveness. If you are going from full-time employment at an institution that qualifies for forgiveness to a private practice that does not, you lose the option to pursue forgiveness and must make a change. If the change in employment is a more important goal than still qualifying for loan forgiveness, then that is great.
Jon : What should physicians consider before they refinance their student loans?
Carlee : Like what we just spoke about, the main consideration is if they are removing themselves from the option of forgiveness of their loan balance. If you refinance a federal loan through a private institution, you will automatically disqualify yourself from having any of the loan balance forgiven. If that’s not a consideration, the next thing you should ask is, why are you refinancing and how are you picking your new lender? Some lenders have programs that offer lower interest rates because you’re a physician. If you determine that private refinancing or consolidation is appropriate, just make sure that you have a reputable lender and that you look for favorable interest rates. Also, check for any prepayment penalties should you decide to pay off your loans that you refinanced sooner than the term you refinanced for.
Jon : Lastly, how might physicians manage their student
loans if they decide to further specialize or obtain additional degrees?
Carlee : At the risk of being repetitive, the main consideration here is if they are pursuing loan forgiveness and expect to decrease the amount of work that they’re currently doing to get a new specialization. You’d anticipate spending time in class and training and working less, along with a decrease in income, which can be good because monthly payments will drop as well, while still qualifying. I recommend that physicians speak with their federal student loan servicer before they make the change just to get their feedback on how things are going to look as they go through more specialization. In addition, depending on how far along they are in the forgiveness track, getting a new specialization increases income drastically from what it was. Will that affect their payments, i.e., increase them even more, once they have that new job? If so, will that cause forgiveness to not make sense anymore? In terms of obtaining additional degrees rather than specialization, that’s something where if they’re taking out new loans, they should consider what type of new loans they are going to take out. Is it something that can or should be consolidated with their old loans when they graduate from their additional degrees? These are all things that the student loan servicer they currently have or their lender through private loans would be able to help with.
Forvis Mazars Private Client services may include investment advisory services provided by Forvis Mazars Wealth Advisors, LLC, an SECregistered investment adviser, and/or accounting, tax, and related solutions provided by Forvis Mazars, LLP. The information in this article should not be considered investment advice to you, nor an offer to buy or sell any securities or financial instruments. The services, or investment strategies mentioned in this article may not be available to, or suitable, for you. Consult a financial advisor or tax professional before implementing any investment, tax or other strategy mentioned herein. The information herein is believed to be accurate as of the time it is presented, and it may become inaccurate or outdated with the passage of time. Past performance does not guarantee future performance. All investments may lose money.

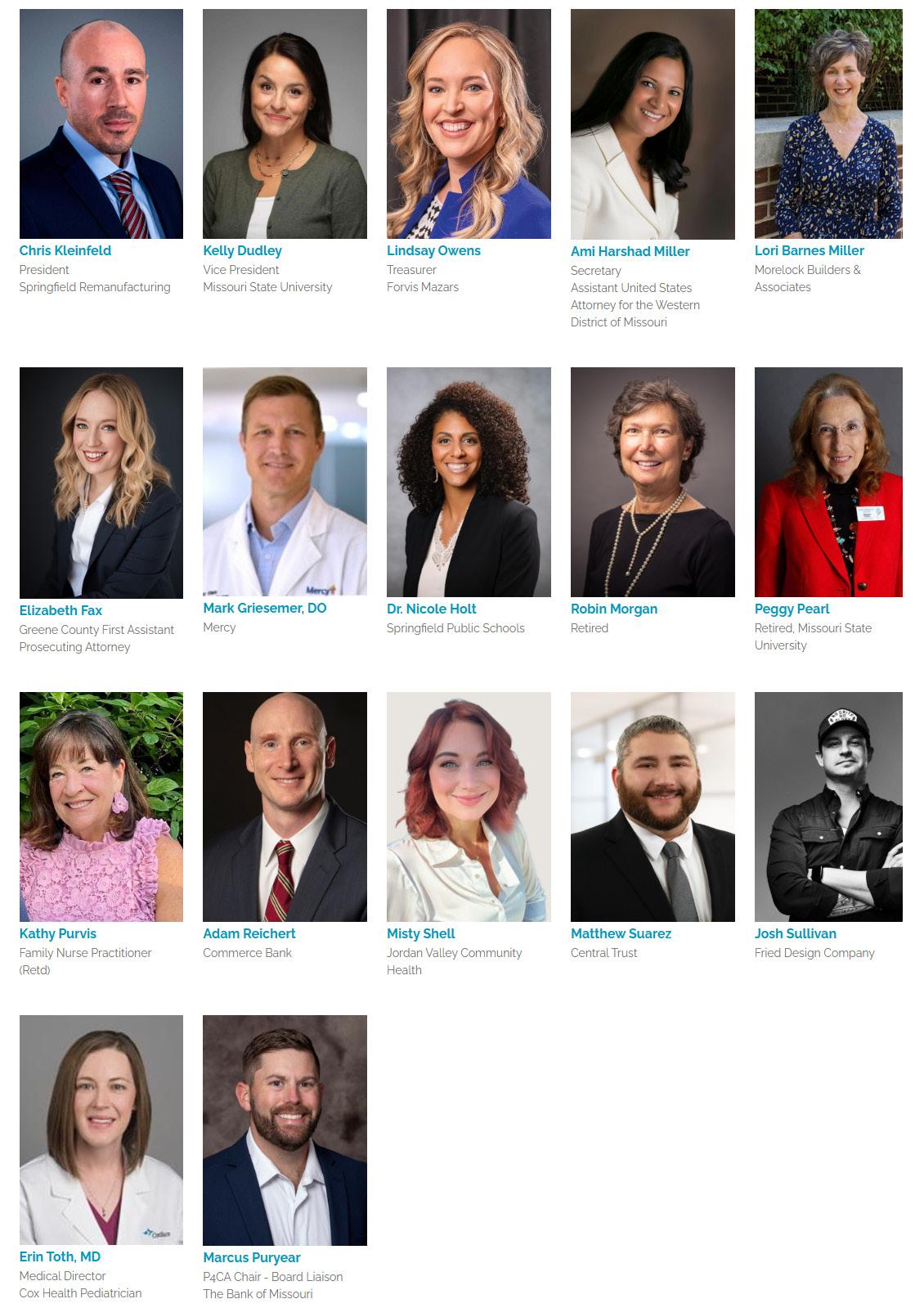
by Brian Biggers, MD
Recently, I had the pleasure of attending the American Medical Association (AMA) meeting as President of the Missouri State Medical Association and as an alternate delegate. Many of us, including myself, have had difficulties with the AMA and some of the policies. It has only been the past few years I have come back into the fold. Many of us would like to think the body of medicine is an easy place to navigate, it is not. I tell my medical students that it takes all of us to make medicine work. It truly does.
As I sat in the reference committee meetings and the body of the house, I listened to all points of view. Did I agree with every resolution or what was said? I did not. At times, I felt that people were trying to push a personal agenda and not looking at medicine. As physicians we tend to focus on issues that are important to us and the patients that we treat. This is human nature and a little self-preservation. Unfortunately, it is these small points that have divided the body of medicine and that some of our members tend to focus on.
While in Chicago, I was invited by a fellow breast surgeon to dinner with physicians from all specialties from across the country. The meal and company were amazing. What I learned is that many of us have similar concerns with the current practice of medicine. We worry about Medicare reform and how we can survive unless we get appropriate reimbursement that is sustainable. We have concerns about the scope of practice and how we combat this. Pre-certification remains a national problem.
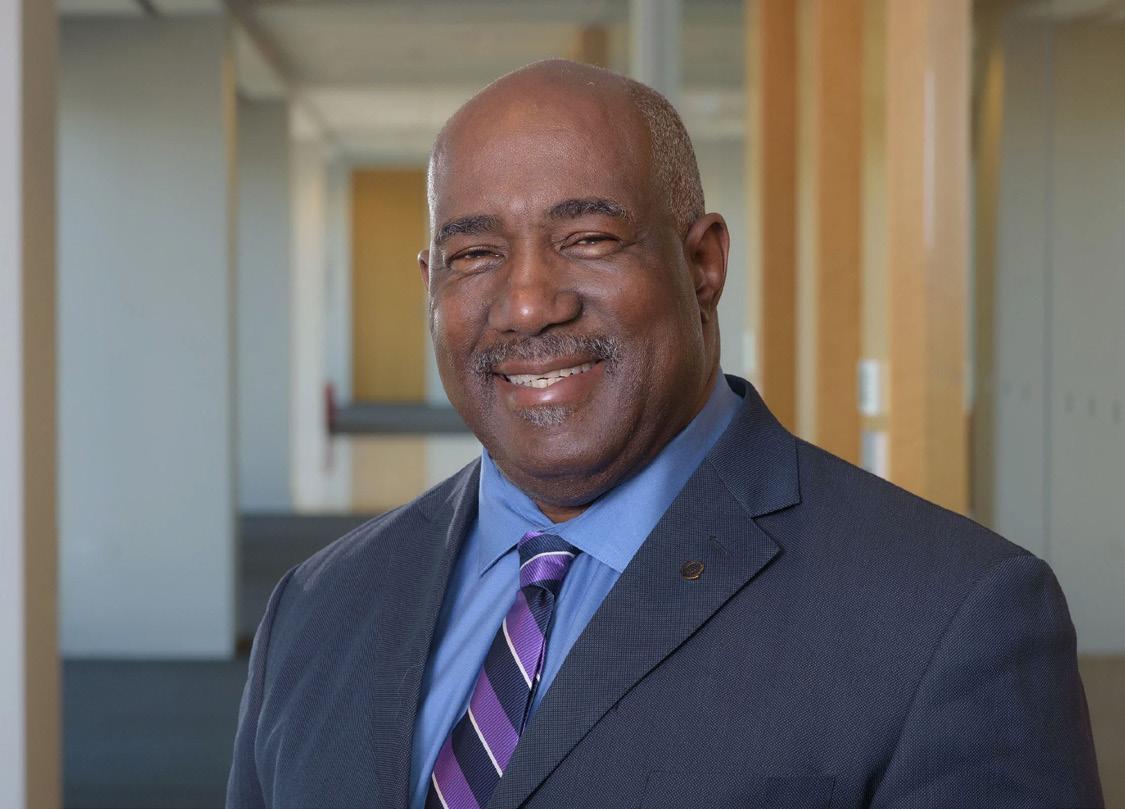

I had the pleasure of meeting Willie Underwood, MD, who became president elect of the American Medical Association. I believe he will be an outstanding president and is an individual who will be a true inspiration to the practice of medicine. Even though I have had the pleasure of many outstanding mentors over my career, I would say he is one of two that has truly inspired me in the practice of medicine.

Locally, I have been talking with area politicians as they are prepared to launch their campaigns. Our own Sam Alexander, MD, is running for Senate District 28 to replace term-limited Senator Sandy Crawford. While his district does not include Greene County, it is important to support all physicians in elections. Closer to home I attended Melanie Stinnett’s campaign kick-off for Senate District 30. I have also given my support to Alex Riley (134th district) as the next Speaker of the House for the state. November may seem a long way away, but we need to know our candidates and those who can be an ally not only to our practice or medicine, but to our patients as well.
The physicians of today are trying to navigate balance. We all only have so many hours in the day and most of us try to balance work, family, and other commitments. The discussion of politics is usually not our top priority. If we don’t get involved with these discussions, then decisions are made without us.

by Jim Blaine, MD
The GCMS Rocky Mountain Medicine CMS Conference met for the third year in a row at the Residents Inn by Marriott in Breckenridge Colorado July 14 - 16, 2025. Our annual CME meetings are usually filled with great presentations, terrific comradery and outdoor fun. This one was especially fun! Gretchen Cliburn treated us all to a late afternoon gathering at Gravity Haus. Please check out our pictures and consider joining us next year; we plan to share date and place soon.








Ashley Ayers, MD – I was born and raised in the small town of Curryville, Missouri—population ~225. I completed my undergraduate studies in Biology at Hannibal-LaGrange University. My passion for medicine, particularly for serving underserved populations, began through international travel with my family, who served part-time as missionaries in Haiti. Those early experiences ignited a desire to care for those with limited access to healthcare. I attended medical school at the University of Missouri–Kansas City (UMKC) School of Medicine, St. Joseph campus, where I continued to explore rural and global health. Memorable experiences included clinical rotations in Ghana and on an American Indian reservation.
I chose family medicine for its breadth, continuity, and the opportunity to build long-term relationships while addressing diverse health needs. I was drawn to CoxHealth for its strong emphasis on comprehensive training and community-focused care. I knew it was the right environment to grow into the physician I aspire to be.
Outside of medicine, I enjoy photography, being outdoors, traveling, and spending quality time with family and friends. I’m excited to continue my training in Missouri and start this new chapter in Springfield!
Carroll Bentley, MD - I am originally from the small town of Lincoln, Arkansas. Growing up in a rural community, I had the chance to see the challenges that many underserved areas face, particularly when it comes to accessing quality healthcare. These experiences inspired me to pursue a career in Family Medicine, with a focus on improving healthcare in rural communities.

As the first person in my family to attend college, I earned a Bachelor of Arts in Psychology from the University of Arkansas. I went on to complete my MD at the University of Arkansas for Medical Sciences. I’ve always been a passionate fan of the Arkansas Razorbacks and make it a point to attend as many games as my schedule allows.
In my free time, I love gathering with family and friends over dinner, catching live concerts and comedy shows, and traveling. One of my personal goals is to visit as many countries as I can and to explore all seven continents.
Chase Bowman, DO - I was born and raised in Wichita, Kansas, as the oldest of three boys. Growing up, my brothers and I spent our days playing sports, hunting, fishing, and exploring the outdoors. I attended Newman University, where I played NCAA Division II soccer while earning my bachelor’s degree in biology, with minors in chemistry and sports medicine. My journey then took me to Fort Smith, Arkansas, where I attended Arkansas College of Osteopathic Medicine (ARCOM). Now, I’m incredibly excited to continue my career as a family medicine resident at CoxHealth in Springfield, Missouri.
My passion for family medicine comes from my desire to build lasting relationships with my community while practicing a broad scope of medicine. I have a particular interest in preventative care, procedures, and sports medicine. I chose CoxHealth because of its strong commitment to serving and supporting the community, and I know this program will provide me with the skills and opportunities needed to grow and succeed.
Outside of medicine, my greatest joy comes from spending time with my wife, two daughters, and our cat, Elsa. We love cooking desserts, playing sports, and exploring nature together. I’m looking forward to making lifelong memories with my family while discovering all that Springfield has to offer.
I’m thrilled to embark on this next chapter and excited to meet and learn from everyone along the way!
Ally Elder, DO - I grew up in Grain Valley, MO, a small suburb outside of Kansas City (Go Chiefs!). I studied biology at the University of Missouri–Kansas City and later moved to Des Moines for medical school at Des Moines University. I chose family medicine after an incredible rural rotation in my third year of medical school. I was drawn to the variety and the opportunity to care for patients through all stages of life. My current interests within family medicine include procedures, dermatology, women’s health, and medical education.
I chose CoxHealth for its broad scope training and emphasis on resident wellness. After meeting the residents and faculty at the AAFP National Conference, I knew I could see myself here. The welcoming environment and supportive culture really stood out
to me throughout the
Outside of medicine, you can find me weightlifting, running, playing tennis, or trying new restaurants or coffee shops. I also enjoy cooking, reading, and listening to live music!
Jenny Funk, DO - I grew up outside a small town on a farm in southeast Kansas. Growing up, I spent much of my time involved in 4-H, student government, and playing tennis. I met my husband, Dylan, in high school. We attended Wichita State University together for our undergraduate degrees. I then attended medical school at A.T. Still University in Kirksville, Missouri.
I chose to practice family medicine because it allows me to directly serve my community by caring for people and families of all ages. My interests are rooted in helping prevent disease and equipping patients with the knowledge and resources they need to manage and improve their health. In my practice, I want to incorporate lifestyle medicine principles and osteopathic manipulative medicine to serve my patients. I am excited to spend the next three years learning and practicing alongside some of the most attentive, intelligent, and inspiring physicians at CoxHealth.
Outside of the hospital, I enjoy spending time with my husband and our standard poodle, Willie. We love being outside hiking or boating on Table Rock Lake. I also enjoy crafting, thrifting, gardening, and baking.
and our pets – a Chihuahua (Beans) and two cats (Frankie and Jack). I love board games, trying new recipes, sewing/ embroidery, and spending time outdoors. My husband and I also enjoy trying new restaurants and treating ourselves to Andy’s afterward!
Joshua Horned, DO - I grew up right here in Springfield, Missouri, and graduated from Hillcrest High School before earning my undergraduate degree from Missouri State University. I went on to attend medical school at ARCOM, where I served as president of the Christian Medical & Dental Associations (CMDA) and deepened my belief that medicine is both my calling and ministry.

I’m incredibly excited to be back home, serving the community that has shaped me. My approach to care is rooted in individualized, whole-person medicine, with a strong passion for lifestyle medicine and helping patients achieve health through sustainable, evidence-based habits.
Outside of medicine, I’m blessed to share life with my amazing wife—my high school sweetheart—and our two wonderful kids. I have a deep love for exercise, nutrition, and functional fitness, and I’m always looking for new ways to promote healthy living. In my free time, you’ll usually find me outdoors with my family or on a quest to find the best espresso in Springfield.

Jessica Gray, DO - I’m originally from Strafford, Missouri. I completed my undergraduate studies at Drury University, where I majored in Biochemistry. While in Springfield, I met my wonderful husband, and we’ve now been married for four years. Before starting medical school, I worked as a phlebotomist in the lab at Cox North. I moved to Tulsa, Oklahoma to attend medical school at Oklahoma State University – Go Pokes!
Throughout medical school, I found myself consistently drawn to family medicine. I love the continuity of care and the opportunity to care for individuals and families across all stages of life as I give them the tools to live their healthiest lives. I’m especially passionate about lifestyle medicine and OMT. Family medicine offers the perfect blend of variety, teamwork, and community I was looking for in a career. I spent a few weeks at CoxHealth as a 4th-year medical student and knew it was the place for me! The residents and faculty were welcoming and supportive, and I am thrilled to be part of their team!
Outside of medicine, I enjoy spending time with family, friends,
Randi Kerr, DO - Raised in Jasper, AR, I moved to Springfield to attend Missouri State University, a city much larger than my hometown. Despite the initial culture shock, Springfield quickly became home, and it was here that I met my husband, Drake. Our first three children were born in Springfield before we relocated to Tahlequah so I could attend medical school at Oklahoma State University. Having spent my entire life in the Ozarks, we are thrilled to return to Springfield as a family of six.

I entered medical school to pursue family medicine due to my passion for building long-term relationships with patients. My interests include women’s health, pediatrics, and osteopathic manipulative techniques. During medical school, I sought out electives in breastfeeding medicine, fertility awareness, and restorative reproductive care.
Even in Oklahoma, I often heard about the exceptional reputation of the family medicine program at CoxHealth, and after spending time with the faculty, staff, and residents, I knew it was the perfect place to continue my training. I am excited to be part of a program that will not only challenge me but also support my growth as a physician in the areas I am most passionate.
Brett Stinogel, DO - I was born and raised in St. Cloud, Minnesota. I lived in Duluth, MN while I completed undergraduate education at the University of MinnesotaDuluth, then moved to Lynchburg, VA to further my education at Liberty University with a master’s degree in biomedical science. During this time, I met my wife, Cerena, and we got married in 2021!

Before medical school, I had a great experience working as a medical scribe at a family medicine outpatient clinic in Forest, VA. It was during this experience that I knew I wanted to be a family medicine doctor. I loved the continuity of care and ability to develop relationships with patients and families, and the comprehensive skills and knowledge of practice.
I completed my first two years of medical school at Liberty University. When my wife, Cerena, matched into residency here at CoxHealth FMR, I transferred to A.T. Still University in Kirksville, MO so that I could complete my 3rd and 4th years in Springfield. This allowed me to stay with my family and not have to live apart at all for those two years.
Everyone at CoxHealth FMR has been so welcoming, genuine, and kind to us. I have seen firsthand how they truly value their residents and try to emphasize individual strengths and wellness while also building lifelong friendships. Springfield has become home to our family, and we look forward to providing care and service to Springfield and the surrounding communities.
My wife and two kids are my pride and joy. I always cherish spending time with them. We love to go for walks, explore local parks, or just be together at home. I also really enjoy reading non-fiction books, working out, eating my wife’s home cooked meals, and I am an avid fan of the Green Bay Packers.
Family medicine has always been close to my heart, especially in the areas of preventative medicine and women’s health. When I started working in my family’s clinic as a teenager, I began building patient relationships that have continued to this day. After residency, I hope to return to the greater Branson area to practice alongside my parents, focusing on providing compassionate, comprehensive healthcare through the lens of an osteopathic physician to my own medically underserved communities back home.
Outside of medicine, I enjoy leading worship at my home church/ synagogue, The Tabernacle, in Branson, horseback riding with my little Lemon girl (golden palomino Fox Trotter mare), spending time with my husband and our two puppy dogs, Thor and Sasha (chi-beag and husky respectively), and playing with my many nieces and nephews, all of whom I love dearly.

Emily Winfrey, MD - I am from a town not far from Springfield called Hartville. I grew up on a cattle ranch that my family still runs today, and had the joy of raising several bottle calves along the way. I have a younger sister who I played basketball with growing up, and I traveled for her AAU basketball tournaments as an assistant. Missouri State University was my home during my undergraduate years before going to Mizzou for medical school. I married my high school sweetheart and became a new mom during my third year of medical school.

Holly Weeks, DO - My hometown of Forsyth, Missouri, is located just about 45 minutes south of Springfield! My wonderful parents, Doctors Leonard and J. Rachelle Bridges, M.D., raised my two younger brothers and me in the groundlevel apartment of my parents’ rural health clinic in Forsyth, so I quite literally grew up in medicine. For the entirety of my childhood education, I was blessed to be enrolled in Riverview Bible Baptist Christian School, which is also where I met my husband, Benjamin Weeks, who has been my constant support throughout this medical journey and in life. I obtained my undergraduate degree from Evangel University in Springfield, Missouri, and I completed medical school at Kansas City University College of Osteopathic Medicine in Joplin, Missouri.
I love family medicine and chose it as my specialty because of the continuity of care I get to have with patients. Relationships are a major part of what fills my cup, and I love that FM allows me to develop those relationships long term and gives me the opportunity to care for patients of all ages. I am so happy to be with CoxHealth FMR because of the excellent training it provides to its residents, its full scope of practice, and the wonderful people I will be spending so much time with over the next few years!
In my spare time, I love spending time with my husband and son, Duke. We love to hang out with our families, serve in our church, and go on walks with our dog. Growing up, we did a lot of floating on the Niangua River, which we still try to enjoy time to time. We are also huge sports fans and love to plan getaways to Arrowhead to root for the Chiefs when we can.
by Molly Jones, M3, University of Missouri School of Medicine, Springfield Clinical Campus
I had a wonderful learning experience at the Childhood Advocacy Center (CAC). I learned that the Springfield CAC is one of the highest volume CACs in the country, which was shocking since I had never heard of a CAC. I was pleasantly surprised by the upbeat demeanor of the staff. It quickly became evident that they make the best out of sad situations so that they have a good attitude when treating the children, which I now see is an especially important way of connecting with these children. After a quick tour and rundown, they told me I would be observing the interviews and medical exams of children being seen for physical abuse. Although I knew this would be something that was emotional to observe, I also knew it would be a great learning experience.
The experience began with sitting in on the pre-brief, where I learned about the case. I then watched the interviews from an observation room and observed the medical exams from the examination room. The most eye-opening thing to me was the skill of the forensic interviewer. They carefully made the kids feel comfortable by asking general questions about their friends and favorite activities. This taught the child the level of detail that would be required for the more difficult abusecentered questions. It was evident that this impressive interview technique required skill and patience. By the end, the children were willing to share accurate information, because they clearly felt heard.

Next was the medical exams. While like a typical well-child, patient comfort was once again at the forefront. The provider carefully talked the children through each step, provided a blanket, and made sure that the exam left no surprises. Meanwhile, she kept a happy attitude and made the children laugh, talk, and smile. I realize that without this level of care, this experience may be traumatic for children, so it was nice to see all the steps that were taken to create a positive environment. This clearly takes a lot of skill and practice from a provider standpoint, which I admire.
This experience was important, because it taught me that while keeping these children safe is the goal, proper information cannot be collected effectively in a negative or traumatic environment.
The CAC does a wonderful job of making this experience as positive as possible, even in terrible situations. The openended interviewing techniques are applicable to pediatric care because they are child-centered and designed to help children communicate accurately without being prompted. I think we can apply the CAC techniques to all patient care. Patients are more willing to share and be open about their health and experiences if we create an environment where they feel comfortable doing so. This was a great experience that I would recommend to every medical student!


by William Micka, MD
I still remember the day the shiny new EHR went live. We were promised instant access to every lab, perfect legibility, and— my favorite buzz-phrase—“more time for patient care.” What arrived instead was a blinking cursor waiting for someone to type every blood-pressure reading, family-history nuance, and treatment plan. That “someone” was often the physician. Hand-written scrawl, once dashed off in seconds (illegible but efficient), was replaced by after-hours typing sessions that stretched late into the night.
Soon I tried documenting during the visit, but that only planted my face in the glow of a monitor while a patient described wheezing across the room. Eye contact vanished; conversation felt transactional. The clerical load frayed my evenings and my patience. I flirted with hiring a human scribe—expensive, hard to train, and usually gone to med-school within a year. Then I watched an early large-language model spin raw speech into structured text almost instantly. In that moment it was obvious: an AI scribe could do what no voice recognition software or short-term scribe ever managed—capture the clinical story faithfully, at the speed of conversation, and give the doctor back to the patient.
Electronic medical records have delivered on some of their early promises: illegible scrawl is gone, decades of labs and imaging are a click away, and a patient’s story no longer lives in a stack of manila folders. Yet those same records are choked with boilerplate and “note bloat,” requiring physicians to navigate through extensive duplicated sections just to find key information. Every data field still has to be typed by someone— usually the doctor—which has turned exam-room clicks into evening “pajama-time” charting. A 2017 study of 142 clinicians found that physicians spend an average of 86 minutes after clinic each day finishing EHR work, including simple actions like renewing prescriptions for ongoing medications, which can involve over 30 clicks. Add the fact that most EHRs still can’t talk seamlessly to one another, and the hidden cost of convenience becomes clear: more hours on keyboards, fewer at the bedside, and a rising undercurrent of burnout that technology was supposed to cure.
Certain specialties feel the EHR burden more acutely than others. Documentation-heavy fields such as primary care, family medicine, internal medicine—and outpatient subspecialties like my own, allergy and immunology—must record meticulous histories, track chronic-disease metrics, and log frequent follow-up visits. Each encounter generates pages of required elements: updated meds, spirometry results, new reactions, prior-auth forms for biologics. The sheer volume of notes,

multiplied by high patient throughput, makes real-time charting impossible; work inevitably spills into the evening, when facts blur and details are harder to recall. Confronted with that growing gap between clinic pace and documentation demands, I found myself searching urgently for a better way.
When the first large-language models appeared, their raw output felt like science fiction—messy, yes, but bursting with promise. Hallucinations popped up, facts sometimes warped, yet each weekly update was a leap; the curve looked exponential. No clinic-ready, HIPAA-secure scribe existed, so I became an overnight student of AI and built my own. That meant solving for encryption, prompt engineering, and regulatory gray zones while the tech shifted under my feet almost daily. Early drafts could invent family histories or fill in details that didn’t exist, but careful prompt tweaks—and rapidly improving models— steadily drove the error rate down.
The result was an in-house ambient scribe that listens to the visit, processes speech in a HIPAA-compliant pipeline, and outputs a concise, professional note that reads as if I typed it myself. Details I used to lose in the frenzy now appear automatically, and the evening documentation grind has vanished. I finish every session with charts closed, see one or two extra patients a day, and feel the weight of clerical work lifted. What began as a curiosity became a daily partner in care.
Today the tool is indispensable; achieving the same productivity and job satisfaction without it would be hard to imagine. As physicians become more familiar with these systems and as they become easier to deploy, I expect AI scribes to be regarded as standard medical infrastructure. A 2024 JAMA Network Open study found that virtual scribes cut physicians’ EHR workload by an average 5.6 minutes per visit—including 1.3 minutes less note-writing and 1.1 minutes less “pajama time.”
Soon every doctor will have a personal, always-available scribe that completes accurate, HIPAA-secure notes—liberating clinicians to focus on patients in busy outpatient settings and, ultimately, across every corner of medicine.
Medicine is already a big-data enterprise: decades of labs, imaging, procedure reports, and now whole-exome or polygenic-risk scores all crowd the modern chart. No human can fully synthesize that torrent, yet an LLM can triage it in seconds—surfacing the three abnormal trends, the family-history red flag buried in a scanned PDF, and the guideline update published last night. The physician remains
indispensable for gleaning nuance from a history and deciding what matters, but AI will point us to the right questions, flag drug-gene interactions, and cross-check every plan against the latest society recommendations.
As genomics moves from novelty to routine, discovery will outpace any doctor’s memory; AI will bridge that gap, instantly mapping variants to therapy or clinical trial eligibility. Drug interactions will be screened in real time, prior encounters retrieved without hunting through tabs, and evidence summaries delivered at the bedside.
Will AI replace doctors? No more than autopilot has replaced airline captains. Aircraft have been able to land themselves for decades, yet a human still takes the controls for the final flare. Likewise, algorithms will propose diagnoses and regimens, but a physician will review and sign off—for safety, context, and human connection. By offloading data grind while amplifying insight, AI can let fewer physicians care for more patients without burning out, positioning us as expert interpreters between the patient and a vast, ever-learning medical knowledge base.
AI can give us back what early EHRs quietly stole: time, connection, and clinical clarity. Health-system leaders should stop treating large-language models as side projects and begin funding them as core infrastructure—fully integrated into the EMR. Physicians must insist that every new tool be judged by a critical metric: does it create more face-to-face patient time than it consumes? And we must remain vigilant that AI does
not repeat the sins of the first digital wave by substituting fresh clerical clicks for old ones.
For our part, clinicians should start building literacy in prompt crafting, data stewardship, and algorithmic bias, because patients will soon expect—and deserve—doctors who can translate terabytes of longitudinal and genomic data into clear, humane care plans. Medicine is changing fast, but if we deploy these systems wisely, AI will not distance us from patients; it will clear the screen, lift our eyes, and help us practice the kind of attentive, data-driven care we imagined when the digital era first began.
William S. Micka, MD is a board-certified allergist-immunologist, department founder at CoxHealth Allergy/Immunology, and advisor on workflow-AI and genomic precision-care. He built one of the first in-house ambient-AI scribes in outpatient allergy practice and consults with clinics and digital-health firms on turning AI into real-world value.
References
Arndt BG, Beasley JW, Watkinson MD, Temte JL, Tuan W-J, Sinsky CA, Gilchrist VJ. Tethered to the EHR: Primary Care Physician Workload Assessment Using EHR Event Log Data and Time-Motion Observations. Ann Fam Med. 2017;15(5):419-426. doi:10.1370/afm.2121
Rotenstein L, Melnick ER, Iannaccone C, et al. Virtual Scribes and Physician Time Spent on Electronic Health Records. JAMA Netw Open. 2024;7(5):e2413140. doi:10.1001/jamanetworkopen.2024.13140



by Jean Harmison, Executive Director, GCMS
In June 2025, Jerry and I celebrated our 40th wedding anniversary with a special trip to Calgary and Banff, Canada. It was a meaningful return to a place we first visited 29 years ago for the Rotary International Convention, when Jerry was the incoming president of Sunrise Rotary.

This time, we made the journey with our daughter, Jessica Harmison-Olson, who is now the incoming president of Sunrise Rotary herself. Her husband, Ryan, joined us as well, making it a wonderful family celebration.
We spent several days in Calgary enjoying the Rotary International Convention sessions and festivities. One of the highlights was an evening at the Calgary Stampede—a fun and lively event full of Western charm.

After the convention, we traveled to Banff and Lake Louise. Lake Louise is a breathtaking hamlet in Banff National Park, famous for its turquoise, glacier-fed lake surrounded by towering peaks. We stayed at the beautiful Fairmont Chateau, which sits right on the lake and feels like something out of a postcard.


One morning, Jessica and I braved the cold and got up at 3:00 a.m. to catch the sunrise at Moraine Lake. It was absolutely magical and well worth the early wake-up call. Throughout our time in Banff, we fit in plenty of hiking on the scenic trails—bear spray in hand, of course!
This trip was the perfect way to celebrate four decades of marriage, reflect on Rotary memories past and future, and enjoy the incredible beauty of Canada with family by our side.





With Private Banking at Central Bank, you have exclusive access to a host of financial services and products, where we take care of the details across the full spectrum of the bank. You will have access to higher deposit rates, custom credit solutions and home financing, as well as individualized guidance with your investments. Our main goal is to help you maximize your money seamlessly. You have complex needs. We have the concierge level solutions you want.



STEVE GASSEL
Senior Vice President - Director of Private Banking | NMLS # 554828
3333 S. National Ave., Springfield, MO 65807
Phone: (417) 841-4213
Steve.Gassel@centralbank.net
KARA TURNER
Vice President - Private Banking | NMLS # 1833785
3333 S. National Ave., Springfield, MO 65807
Phone: (417) 841-4253
Kara.Turner@centralbank.net
JOYCE WONG-HSU
Officer - Private Banking | NMLS # 1239617
3333 S. National Ave., Springfield, MO 65807
Phone: (417) 841-4214
Joyce.Wong-Hsu@centralbank.net
To Advertise in this directory call Jean Harmison at the Society office: 417-887-1017.
Please Note: Changes to ads will be made quarterly and must be submitted in writing. H Denotes GCMS Membership “A” Denotes GCMS Applicant GCMS Member Ad Rates: $10.00 per 2” sq. • Non-Member Ad Rates: $13.75 per 2”sq.
Bringing physicians together to improve the health of our community.
Dermatology, Procedural
MICHAEL H. SWANN, MD H
BRETT NEILL, MD
MICHAEL KREMER, MD
JOHN CANGELOSI, MD
AUTUMN BERTHOLDI, PA-C
PATSY DUGGAN, PA-C
LORI MILLER, NP-C
HANNAH LEE, FNP-BC
BROOKLYN FORT, FNP-C
3850 S. National Ave, Suite 705 Springfield, MO 65807 (Located inside Hulston Cancer Building-7th floor)
1240 E. Independence Springfield, MO 65804
Phone: 417-888-0858 • Fax: 417-889-0476 www.swanndermatology.com
Hollister Location 590 Birch Rd, Ste 2c Hollister, MO 65672
PH. 417-690-3858 Fax 417-690-3862
Monett Satellite Location (Inside CoxHealth Urgent Care) 2200 E. Cleveland Ave Monett, MO 65708
Phone: 417-888-0858 • Fax: 417-889-0476
Lebanon Location 331 Hospital Drive Suite C Lebanon, MO 65536
Phone : 417-344-7200 Fax : 417-344-7299
Direct Primary Care
ASCENT DIRECT PRIMARY CARE, LLC
MATTHEW GREEN, DO H
Family Medicine
www.ascentdpc.com 417-595-0956
413 N McCroskey, Ste 2 Nixa, MO 65714
EYE SURGEONS OF SPRINGFIELD, INC.
C. BYRON FAULKNER, MD H Comprehensive Cataract Ophthalmology
JUDD L. McNAUGHTON, MD H Comprehensive Cataract Ophthalmology Diplomates, American Board of Ophthalmology
1330 E. Kingsley St. • Springfield, MO 65804 Phone 417-887-1965 • Fax 417-887-6499 417eyecare.com
MATTAX • NEU • PRATER
EYE CENTER
JAMES B. MATTAX, JR., MD, FACS H American Board of Ophthalmology
LEO T. NEU III, MD, FACS H American Board of Ophthalmology
DAVID NASRAZADANI, MD
DREW A. YOUNG, MD
THOMAS PRATER, MD, FACS H American Board of Ophthalmology
JACOB K. THOMAS, FACS, MD H American Board of Ophthalmology
BENJAMIN P. HADEN, MD H American Board of Ophthalmology
MICHAEL S. ENGLEMAN, OD
MARLA C. SMITH, OD
MATTHEW T. SMITH, OD
1265 E. Primrose Springfield, MO 65804 417-886-3937 • 800-995-3180
Family Medicine
COXHEALTH
FAMILY MEDICINE RESIDENCY
FAMILY MEDICAL CARE CENTER
3800 S National Ste 700 Springfield, MO 65807 (417) 269-8817
AmericAn BoArd of fAmily medicine
Marc Carrigan, MD
Cameron Crymes, MD
Kristin Crymes, DO
Matthew Dalke, MD
Katie Davenport-Kabonic, DO
Kristen Glover, MD
Kyle Griffin, MD
Shelby Hahn, MD
Laura Isaacson, DO
Evan Johnson, MD
Michael Kabonic, DO
Eric Lesh, DO
Taylor Ross, MD
WOMAN’S CLINIC www.womansclinic.net
Leaders in Minimally Invasive Gynecology & Infertility
DONALD P. KRATZ, MD, FACOG H American Board of Obstetrics and Gynecology
AMY LINN, FNP-BC American Academy of Family Nurse Practitioners
ANGIE JONES, WHNP-BC 1135 E. Lakewood, Suite 112 Springfield, MO 65810
Located inside Tri-Lakes Family Care 1065 Hwy 248 Branson, MO 65616
Phone 417-887-5500
Fax 883-8964 or toll free 877-966-2607
Monday-Thursday 8am-4:30pm Friday 8am-12pm
MERCY CLINIC–INTERNAL MEDICINE WHITESIDE
RAJ ANAND, MD
JAMES T. ROGERS, JR. MD, FACP H Board Certified in Internal Medicine
MARIA DELA ROSA, MD
NELSON DELA ROSA, MD
AMANDA MCALISTER, MD
ALEJANDRA ROA, MD
KELLY TRYGG, MD
GABBY BONNER, NP
STEVEN BOWLIN, MD Board Certified in Internal Medicine
STEPHANIE HOVE, NP
CARRIE KUGLER, PA
COURTNEY WEATHERFORD, PA
JENNIFER WHITE, PA
VICTOR GOMEZ, MD Board Certified in Internal Medicinee 2115 S. Fremont, Suite 2300 Springfield, MO 65804
Phone 417-820-5600 Fax 417-820-5606
MERCY CLINIC UROLOGY (FREMONT)
ERIC P. GUILLIAMS, MD, FACS H American Board of Urology
ROBERT D. JOHNSON, MD, FACS H American Board of Urology
TYRUN K RICHARDSON, MD American Board of Urology
Phone 417-820-0300
Fax 417-882-9645
1965 S Fremont, Ste. 370 Springfield, MO 65804
ADULT MEDICINE & ENDOCRINOLOGY
JONBEN D. SVOBODA, MD, FACE, ECNU
American Board of Endocrinology
JAMES T. BONUCCHI, DO, ECNU, FACE
American Board of Endocrinology
NICOLA W. GATHAIYA, MD, ECNU, FACE, CCD
American Board of Internal Medicine
American Board of Endocrinology
STEPHEN M. REEDER, MD, FACP
American Board of Internal Medicine
ANA MARCELLA RIVAS MEJIA, MD, CCD
American Board of Internal Medicine
American Board of Endocrinology
JACQUELINE L. COOK, FNP-BC, CDCES, CCD
KELLEY R. JENKINS, FNP-C, CDCES
ALINA CUMMINS, PA-C
STACY GHOLZ, FNP-C
SHELLEY L. CARTER, DNP
JESSICA A. CROUCH, FNP-C
Phone (417) 269-4450
960 E. Walnut Lawn, Suite 201 Springfield, MO 65807
Nephrology
SPRINGFIELD NEPHROLOGY ASSOCIATES, INC.
1911 South National, Suite 301 Springfield, MO 65804
Phone 417-886-5000 • Fax 417-886-1100 www.springfieldnephrology.com
STEPHEN E. GARCIA, MD H
American Board of Internal Medicine
American Board of Nephrology
ETHAN T. HOERSCHGEN, MD
American Board of Internal Medicine
American Board of Nephrology
GISELLE D. KOHLER, MD H
American Board of Internal Medicine
American Board of Nephrology
DAVID L. SOMMERFIELD, MD
American Board of Internal Medicine
American Board of Nephrology
SUSAN A. WOODY, DO H
American Board of Internal Medicine
American Board of Nephrology
SPRINGFIELD NEUROLOGICAL AND SPINE INSTITUTE
CoxHealth Jared Neuroscience
West Tower • 3801 S National, Ste 700 Springfield, MO 65807 • 417-885-3888
Neurosurgery:
H. MARK CRABTREE, MD, FACS
EDWIN J. CUNNINGHAM, MD
MAYUR JAYARAO, MD
J. CHARLES MACE, MD, FACS H
CHAD J. MORGAN, MD
MICHAEL L. MUMERT, MD
SALIM RAHMAN, MD, FACS
ANGELA SPURGEON, DO
ROBERT STRANG, MD
Interventional Neuroradiology
MICHAEL J. WORKMAN, MD
Physiatry:
TED A. LENNARD, MD
KELLY OWN, MD
JESSE STOKKE, DO
Physician Assistants:
JOSHUA BARBIERI, PA-C
MARK BROWN, PA-C
ERIC CHAVEZ, PA-C
KEVIN STOKES, PA-C
HEATHER TACKETT, PA-C
Nurse Practitioner:
EMILY CROUSE, NP-C
MINDY GRANT, NP-C
ROZLYN MCTEER, FNP
BRANDON RUBLE, ACNP-AG
ALYSSA CHASTAIN, FNP
COXHEALTH
PRIMROSE OB/GYN
MARCUS D. MCCORCLE, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
THOMAS M. SHULTZ, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
GREGORY S. STAMPS, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
P. MICHAEL KIDDER, DO, FACOOG
Diplomate, American Osteopathic Board of Obstetrics & Gynecology
Phone 882-6900
1000 E. Primrose • Suite 270 Springfield, MO 65807
SPRINGFIELD OB/GYN, LLC
MATTHEW H. TING, MD, FACOG H
American Board of Obstetrics & Gynecology 909 E. Montclair, Suite 120 Springfield, MO 65807
Phone 417/882-4466 • Fax 417/890-5631
ONCOLOGYHEMATOLOGY
ASSOCIATES OF SPRINGFIELD, MD, P.C.
WILLIAM F. CUNNINGHAM, MD, FACP
American Board of Internal Medicine
American Board of Medical Oncology
JIANTAO DING, MD H
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
ROBERT J. ELLIS, MD, FACP
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
BROOKE GILLETT, DO
American Board of Internal Medicine
American Board of Medical Oncology
V. ROGER HOLDEN, MD, PhD
American Board of Hematology
American Board of Medical Oncology
DUSHYANT VERMA, MD, FACP
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
Springfield Clinic 3850 S. National, Ste. 600 Springfield, Missouri 65807
Monett Clinic 802 US Hwy 60 Monett, Missouri 65708
Phone 882-4880 Fax 882-7843
Visit our website: www.ohaclinic.com
MERCY CLINIC–EAR, NOSE & THROAT
BENJAMIN L. HODNETT, MD, PHD H
ERICH D. MERTENSMEYER, DO, FAOCOO
AARON R. MORRISON, MD
RAJEEV MASSON, MD
MARK J. VAN ESS, DO, FAOCOO
Diplomates, American Board of Otolaryngology
SHELBY BRITT, PA
MELISSA COONS, FNP
TAHRA LOCK, NP
ELIZABETH (BETSY) MULLINGS, FNP
PAUL STRECKER, FNP
Audiology
JASON BOX, AuD, CCC-A
MAMIE JAYCOX, AuD, CCC-A
JENNIFER PLOCH, AUD
ALLISON WHITE, AUD, CCC-A
Phone 417-820-5750 Fax 417-820-5066
1229 E. Seminole, Ste. 520 Springfield, MO 65804
MERCY CLINIC–FACIAL PLASTIC SURGERY
MATTHEW A. KIENSTRA, MD, FACS
American Board of Facial Plastic & Reconstructive Surgery
American Board of Otolaryngology
Phone 417-887-3223
1965 S. Fremont, Ste. 120 Springfield, MO 65804 facialplasticsurgeon.com
JAMES E. BRIGHT, MD H Diplomate, American Board of Psychiatry & Neurology.
Practice Limited to: Adult Psychiatry
Phone 882-9002
1736 E. Sunshine, Ste. 400 Springfield, MO 65804

chAnge Service requeSted