The
Singing Doctors of Greene County, MO



July 14-16








July 14-16








Editor's
Jim
President's
Kayce
Respiratory
Drury



Editor’s Note: All materials for the Journal must be submitted by the first of the month prior to publication.
Co-Editors:
Jim Blaine, MD Minh-Thu Le, MD
Public Health Editor: Nancy Yoon, MD
Junior Co-Editor: Andrew K. Le
Managing Editor: Dalton Boyer
Editorial Committee:
Michael S. Clarke, MD
David Barbe, MD
Jaya LaFontaine, MD
Dalton Boyer
Andrew Le
Jean Harmison
Barbara Hover
Nancy Yoon, MD
Frank Cornella, MD
SOCIETY OFFICERS
James Rogers, MD President
Vu Le, MD
Secretary
Jim Blaine, MD
Treasurer
Sanjay Havaldar, MD Immediate Past President
Council Members:
David Haustein, MD
Melissa Gaines, MD
Steven Gradney, MD
Keith LeFerriere, MD
Kyle John, MD
Jaya LaFontaine, MD
Nancy Yoon, MD
John Steinberg, MD
Managing Director: Jean Harmison
Executive Office:
4730 S. National Ave. Suite A1 Springfield, MO 65810 email: director@gcms.us www.gcms.us
by Jim Blaine, MD
This Journal is part of the GCMS 150 Year Celebration, and that would not be complete without a look back at our “Singing Doctors” who are celebrating their own 65th anniversary. Much thanks to the only surviving Singing Doctor, Dr. Jim Cook, and Singing Doctor leader Dr. Jim Brown’s daughter Mary Louise, and son Dr. Trig Brown for their contributions. Also reprinted in this issue is a booklet including the Singing Doctors timeline authored by Mary Louise and Dr. Trig Brown. Mary Louise wanted to be sure that we mentioned that the Singing Doctors Scholarship Fund is still helping MU medical students and would appreciate your donations! Please call GCMS o ice at 417 887-1017 for information.
Retired Senior Vice President and COO of Mercy Springfield Communities Jay Gu ey, and Retired President and CEO of CoxHealth Steve Edwards announce in this issue a joint e ort between Drury University, CoxHealth, Mercy Springfield Communities, and Burrell Behavioral Health in the development of a Drury Master of Health Administration (MHA) program. GCMS salutes these community leaders as they continue to donate their talents to our community!
Former MSMA, AMA, and World Medical Association President Dr. David Barbe is a new member of our GCMS Journal Editorial Board and poses the question, “Who needs the WHO?” In his insightful article.
Pediatrician Dr. Kayce Morton reminds us that influenza is the most significant respiratory illness a ecting the pediatric population.

GCMS Journal Public Health Editor Dr. Nancy Yoon updates us on respiratory illnesses in a very active season.

Dr. John Steinberg wrote a poignant article in a 2012 Missouri Medicine issue about Dr. John “Bucky” Buckner’s “Extraordinary Dedication: Family, Profession, Country”. That article is reprinted in this issue with the kind permission of Editor Dr. John Hagan and MOMed. This issue also contains a recent followup interview with Dr. Buckner about his challenges in an e ort to contribute to the safety of young U.S. soldiers during his four deployments overseas.
Upcoming events in our 150th Year of GCMS include a family CME trip to Breckenridge Colorado. This is our third straight year trip to Breck and it always is a pleasure to spend time with colleagues and their families. It is a unique experience; please give GCMS a call at 417 887-1017 for additional information for the July 13-19 “Rocky Mountain Medicine”. The Greene County Medical Society 150 Year Celebration (MASH Bash) will be held on September 20, 2025.
Finally, former GCMS President and former GCMS Editor Dr. Brian Biggers will be installed as 2025 MSMA President at the MSMA Convention in Springfield April 4-6 (see below). Congratulations Brian!


Former GCMS President Dr. Brian Biggers will be installed as MSMA President at the Springfield University Plaza Hotel April 4-6. Please register now to join us for a great MSMA Annual Convention and to celebrate Brian.
by James Rogers, MD
Community – Greater Good
This issue of the Journal celebrates another proud highlight of our society, The Singing Doctors of Springfield. This group of professionals, admittedly much better at healing than singing, created a brother like bond. Through this supportive relationship they created an array songs and satire that brought laughs and reflections to our colleagues.
One of the members recalls that we were very popular in medical audiences and not so with general public, most of them didn’t really get it. After a while we had invitations from across the country for meetings and conventions. The Singing Doctors, with support of this physician community, brought laughter, joy, and a chance for selfreflection to their professional audiences and infused a dose of self-humility. Indeed, their message struck such a nerve as to create unexpected profits and popularity. This caused the tight knit troubadours to pause and consider




“what’s next”? Group member, Dr. Jim Cook, tells that the unanimous decision had no hesitation; “we all donated our time to send any profits to fund low interest loans for local area medical students”.
Dr. Cook told us stories about the joy of working together to create something special and sustained good. Today the endowment has over $800,000 and provides area MU medical freshmen with scholarships.
None of these good works would have been possible without the physician community supporting, caring, and now appreciating these good works. It starts with a first step of engagement. Please accept my invitation to join up and let’s see how caring for each other will create more opportunities to care for each other!
Scan and join, we are ready to do more “good”!



Tailored Tax, Wealth Management, and Family Office to help you prepare for what’s next.











By Kayce Morton, DO
Influenza remains one of the most significant seasonal respiratory illnesses affecting the pediatric population. Due to their developing immune systems and high exposure in community settings such as schools and daycare centers, children are at increased risk of contracting and spreading the virus. As of February 22, 2025, the United States has experienced a severe influenza season, with the Centers for Disease Control and Prevention (CDC) estimating at least 33 million illnesses, 430,000 hospitalizations, and 19,000 deaths. Making this the most severe flu season in 15 years, with two aggressive influenza strains predominantly circulating, posing significant risks, especially to young children and unvaccinated individuals. Pediatric populations have been notably affected, with 86 influenzaassociated pediatric deaths reported so far this season.

I think for us to understand the history of influenza, its evolving nature, and strategies for prevention, particularly focusing on pediatric care then we as physicians can better communicate with our patients and play an important role in mitigating the spread and severity of influenza in children. If we can continue to emphasize the importance of immunization efforts and public health initiatives it will not only benefit pediatric health, but also the health of the community.
This is not a new problem, influenza has been a documented human illness for centuries, with pandemics occurring periodically due to significant viral shifts. It continues to pose a threat to the pediatric population. The most infamous pandemic, the 1918 H1N1 outbreak, caused millions of deaths worldwide and

highlighted the virus’s potential severity. Since then, influenza strains have continuously evolved due to antigenic drift and shift, leading to new seasonal outbreaks each year. These mutations necessitate regular updates to vaccines and public health responses to combat the disease effectively.
The development of the influenza vaccine is an ongoing process requiring global surveillance and predictive modeling. Each year, the World Health Organization (WHO) collaborates with health agencies to determine which strains are most likely to circulate based on previous and emerging patterns. The flu vaccine's effectiveness varies depending on strain matching and antigenic drift but remains a critical tool in reducing disease burden. Even partial protection from vaccination can lessen the severity of illness, lower hospitalization rates, and reduce overall transmission, particularly in pediatric settings where flu spreads rapidly. While not always a perfect match, annual flu vaccinations play a vital role in protecting individuals and communities by decreasing viral virulence and overall spread.
Children and the elderly are particularly susceptible to severe complications from influenza. In pediatric populations, immature immune systems result in higher infection rates, increased viral shedding, and a greater likelihood of secondary bacterial infections such as pneumonia. Additionally, infants under six months, who are ineligible for vaccination, rely on herd immunity and

maternal antibodies for protection. Meanwhile, the elderly experience immunosenescence, or the gradual decline of immune function, leading to higher hospitalization and mortality rates. These vulnerabilities underscore the importance of targeted preventive strategies in these age groups.
The 2023–2024 influenza season witnessed a significant

increase in pediatric cases compared to the previous year. The CDC reported 200 flu-related deaths among children, surpassing the previous record of 199 pediatric deaths during the 2019–2020 season. This alarming rise underscores the heightened vulnerability of children to influenza and the critical need for effective preventive measures.
Influenza isn’t just a bad cold and can lead to severe complications in pediatric patients, including pneumonia, dehydration, and exacerbation of chronic medical conditions like asthma or diabetes. Notably, neurologic complications such as encephalopathy and encephalitis have been observed. Recent data indicates that influenza-associated neurologic complications occur in approximately 7%–10% of hospitalized children with influenza. These complications can result in prolonged hospital stays, long-term neurological deficits, or even death, emphasizing the severity of influenza infections in children.
Effectively conveying the significance of annual flu vaccination to patients and their families is paramount in reducing influenza-related morbidity and mortality. Healthcare professionals can employ several strategies to enhance vaccine uptake.
You can share real-life cases, such as that of Mia Klyczek, a 9-year-old who tragically lost her life to influenza complications, can resonate deeply with parents and caregivers, highlighting the potential severity of the flu, which has been on the news and in magazines. Sadly, there is always a story you can find. I personally remember my
last year as a resident, I was in Columbia and my cousin’s daughter was admitted for dehydration secondary to influenza to CoxHealth. She was hospitalized for 3 days, and I was lucky to know the doctor and thankful she improved. That isn’t always the case.
We must engage in open, empathetic dialogues allows healthcare providers to address concerns, dispel myths, and provide tailored information that aligns with the patient's values and beliefs. We know people trust their doctors. We also know the statistics don’t win and neither does guilt. If you make your parent or patient feel defensive of their stance, we have lost any rapport that we may have developed.
Utilize clear, concise, and culturally sensitive information about the benefits and safety of flu vaccination can empower patients to make informed decisions. Reinforce that even partial protection from the vaccine can reduce the severity of illness and prevent serious complications is crucial. By integrating these approaches, healthcare professionals can foster trust and encourage higher vaccination rates, ultimately safeguarding pediatric populations against severe illness.
With the escalating number of pediatric influenza cases and associated complications during the 2023–2024 season it is of critical importance for increasing preventive strategies, particularly annual vaccination. This year only about 45% of Americans received an influenza vaccine. It is our job as healthcare professionals to understand the evolving nature of the influenza virus and its disproportionate impact especially on vulnerable populations so we can better advocate for and implement effective interventions. Engaging patients and their families through personalized communication and education is essential in enhancing vaccine acceptance and coverage. Collectively, these efforts contribute to reducing the burden of influenza, protecting children's health, and preventing severe outcomes. Now more than ever with a general lack of trust in science and medicine, this is so important. It is too late for some this season that have already lost their lives or been affected by the loss of a child, but it is never too late to try. We must do better.
References
CDC.gov
https://www.jpeds.com/article/S0022-3476(21)00731-9/abstract https://www.axios.com/local/washington-dc/2025/03/03/flu-severeseason-kids-dc
https://apnews.com/article/flu-vaccine-shots-kids-braincomplication-af4d9e28952f89f260fb0848ebe80626
By Jim Blaine, MD and Mary Louise Brown
This article combines a current Dr. Jim Cook interview by me with an earlier interview of Jim by Mary Louise Brown (Dr. Jim Brown’s daughter).
Blaine : Good morning Jim, you are a member of the famous Singing Doctors.
Jim Cook : The last remaining Singing Doctor!
Blaine : I first met you when I came to town in 1977, but when did you come to town?
Jim Cook : 1964
Blaine : You were not one of the original Singing Doctors?
Jim Cook : No. I was not a member of the original six, but I was the first recipient of the Singing Doctors Medical School Fund for students! My total debt was $1,500. I was also the first to repay the Singing Doctors’ loan. They actually waived the final $500. So I got through medical school for one thousand dollars. I understand that now the average debt post medical school is $124,000. So I got a pretty good deal!
Blaine : When did you join the Singing Doctors?
Jim Cook : They began with a quartet they called the Four

Suppositories. Whenever someone could not go, Jim Brown asked if I could fill in. When Dr. Fred Collar died (way too young), I became the fourth Suppository.

Blaine : So you guys travelled all over the country as a Comedy/ Singing group and you were in high demand?
Jim Cook : We were in demand for medical groups. Lay people as a group did not understand the nuances as well as doctors.
Blaine : How many performances did you do on average?
Jim Cook : At the most, two per week. We were all doing full time practices; no one was retired at that time. Jim Brown was our leader and he would usually give us a couple of weeks notice. We would lease an airplane, fly to our performance site, perform, fly home, and get up at 4:30 a.m. the next morning to go to work.
Mary Louise Brown (Dr. Jim Brown’s daughter) : Jim, you wanted to say something about each member of the Singing Doctors? How about Dr. Fred Coller?
Jim Cook : Fred Coller was a pathologist and in the group the shortest time that I was there because he died shortly after I joined. He was really a funny guy. Jim brown had Fred play a pregnant lady for one of the skits in the show. I remember that I had to do that one time, and I immediately grew a beard so I wouldn’t have to do that again (laughs)! That was the reason for the onset of my beard, He did the pregnant lady awfully well and seemed to enjoy it a lot. Of all the guys I would have picked out to be in a singing group, I think Fred would not have been in the first twenty, but he really did fit in well. He ended up being our bass singer and was wonderful. He seemed to enjoy our group as much or more than anybody. His wife Kitty was a great trouper on the shows and seemed to enjoy them very much. They were happy participants!
Brown : What would you like to share about Dr. F.T. “Hogan” H’Doubler?
Jim Cook : I guess one of the strangest relationships I developed was with H’Doubler. I took a course on acupuncture and helped him with an old shrapnel wound he had. He was a very competent thyroid surgeon and ended up studying acupuncture and practiced that solely until he retired. Hogan was the funniest guy in the world. Everything he was was funny, and he made it funny for everyone around him! He was wonderful to be around! I loved his sense of humor and being around him and he was always fun to have him on a trip!
Brown : What about Dr. Hal Lurie?
Jim Cook : I spent more time with Hal because he lived the longest. Hal was an Internist. We went out to North Carolina to see your dad when he was ill. Hal was amazing! He enjoyed the Singing Doctors more than anybody except maybe your dad. He just absolutely loved it. And he especially loved it when we sent the Scholarship fund up to MU because he was on the MU Board. He felt like that was a contribution that he was able to make, and it perpetuated the Singing Doctors. Hal was a remarkable guy. He did a “After the Show Show” when the wives were on the trips, and we spent the night.
Brown : Tell me about Dr. Charlie Lockhart.
Jim Cook : Lockhart was the only real talent besides your dad. He really had an awfully nice voice, and he liked using it. He wrote all his own songs. They were of a different sort especially since he sang them himself. He put a lot of himself into it, and they were really good. It gave a good balance to the show I thought. He was the only one who wrote a whole song. Charlie was a general surgeon, and, at the hospital, he was very quiet and reserved, but on the trips, he seemed more relaxed and had as much fun as anyone. That’s the thing that I remember most about him.
Brown : What About Professor Wilfred (Wimpy Adler)?
Jim Cook :He was just wonderful! How he ever put up with us I have no idea. Everybody knows what a great musician he was, and he had a great sense of humor. He loved all those guys as much as anybody. It had to be nuisance for him to hang around with us and try to suggest how to stay in tune, but he carried on with great charisma and courage. He was a wonderful musician with a great tolerance for pain that we inflicted upon him.
Brown : Please share some thoughts about Dr. Don Gose.
Jim Cook : Don was a surgeon and he was wonderful! He always knew his lines, and did his part. He was hilarious as Emmett! He was pretty hilarious as himself too. He saw something funny in just about everything. The trips were never dull when the “Rear Admiral” was along.
Brown : What would you like to share about Dr. Jim Brown?
Jim Cook : Your dad is probably the only person I ever knew that had at least 15 or 16 people who considered him their very best friend. Without Jim, there wouldn’t have even been any Singing Doctors. The thing I think I remember about him most was that he was always in a good mood. I never - when things were not going well - saw him in a bad mood or take it out on anybody. He just absolutely was
always on top of everything. He was my idol. He just handled everything perfectly, I thought.
Brown : He loved all of you - his friends and family were his reason for living.
Jim Cook : Well, he was a good friend, but it was interesting that he could be that good a friend to that many people.
Brown : Thank you Jim. That is very kind of you to say.
Blaine : Jim, the Singing Doctors made a lot of albums including cassettes, CDs and vinyl records to sell and benefit the students. How did that work?
Jim Cook : Actually, we never did many in recording studios. Jim Brown simply recorded everything off of live shows. Jim was the brains of our outfit. He wrote all of the songs except for a couple that Charlie Lockhart wrote. Jim had a great wit and he could make serious things very funny.
Blaine : I recall him well. Jim also wrote a book called “Hippocrates Oaf” that was very funny.
Jim Cook : And he was even funnier in person!
Blaine : Those Singing Doctor albums are still around. We have several cassettes and vinyl records at GCMS. When did the Singing Doctors break up?
Jim Cook : The last formal performance was when Hal Lurie became President of the Greene County Medical Society (1989 ). That was the way Jim planned it.
Blaine : Thoughts over the years when you consider your career as an anesthesiologist and your experience with the Singing Doctors. How high did the Singing Doctors rank on the totem pole?
Jim Cook : Tops! It was by far the most fun I ever had! All were people I liked and admired and we were helping others. I think that, over the years, the Singing Doctors raised around $500,000 to help medical students financially. That may be overestimating it, but it was close to a half million dollars.
Blaine: Do you have any idea how much money is in the Singing Doctors’ Fund currently?
Jim Cook : No
Blaine : $850,000, and that is considering that the later recipients were given scholarships not loans.
Continued on page 17.....Interview with Jim Cook, MD
by Nancy Yoon, MD, MPH, Chief Medical Officer Springfield-Greene County Health Department
This has been a very active respiratory virus season. There have been at least 33 million illnesses, 430,000 hospitalizations, and 19,000 influenza-linked deaths in the U.S., according to the Centers for Disease Control and Prevention (CDC). The agency also confirmed 18 new flurelated deaths in children, bringing the total for the 202425 flu season to 86. As of February 21, the amount of acute respiratory illness causing people to seek healthcare is at a high level. CDC assesses the severity of weekly influenza activity using information on influenza-like illness, flurelated hospitalizations, and flu-coded deaths.

Wastewater viral activity is high for influenza A, while it is moderate for COVID-19 and low for RSV. Other respiratory illness at high levels include pertussis (whooping cough), Mycoplasma pneumonia, and group A Streptococcus infections.
Statewide influenza activity in Missouri has also been high. In week 7, there were 114 influenza-associated deaths reported. 4.3% of ED visits were due to influenza-like illness. The weekly percent positivity of influenza tests was 27.3%, with 95% being due to Influenza A. The Springfield-Greene County health department’s flu dashboard is also updated weekly. There has been a downward trend in the number of cases for the past few weeks.
Another respiratory virus that is being monitored is H5N1. H5 bird flu is currently widespread in wild birds and is causing outbreaks in U.S. poultry and dairy cattle. There have been 70 human cases in the U.S. since 2024 and 1 death. The majority have been from exposures to dairy cattle and poultry farms. The current public health risk is low (according to the CDC), and there is no known person-to-person spread at this time.
Most cases have been clinically mild.

People who have been exposed to H5N1 should be monitored for symptoms for 10 days a er the last date of exposure, including conjunctivitis, fever, chills, sore throat, myalgias, headache, fatigue, dyspnea, nausea, vomiting, and diarrhea. In patients with suspected or confirmed influenza, ask about potential exposures to wild and domestic animals, including pets (e.g., cats), animal products (e.g., poultry, dairy cows, raw cow milk and raw cow milk products, raw meat-based pet food) or recent close contact with a symptomatic person with a probable or confirmed case of influenza A(H5).
Bird flu viruses have been known to sometimes infect mammals that eat (presumably infected) birds or poultry, including but not limited to wild animals, such as seals, bears, foxes, skunks; farmed mink; stray or domestic animals, such as cats and dogs; and zoo animals, such as tigers and leopards.
The public should be cautioned to avoid direct contact with wild birds or other animals suspected to be infected with avian influenza A viruses. If direct contact cannot be avoided, appropriate PPE should be worn. People should also avoid unpasteurized (raw) milk and products made from raw milk.
Pertussis levels in Greene County have also been very high in 2024 and 2025. There were 70 cases in 2024. In January 2025, there were 59 reports of pertussis (25 confirmed or probable). 40% of the cases were up to date on their pertussis vaccinations. Whenever possible, clinicians should obtain a nasopharyngeal swab or aspirate from all persons with suspected pertussis. The same specimen can be used both for culture and PCR. Ideally, specimens should be collected during the first 2 weeks of illness following cough onset.
A 5-day course of azithromycin is used for treatment and postexposure prophylaxis. Clinicians should consider treating prior to test results if any of the following are present:
•Clinical history is strongly suggestive of pertussis
•The person is at risk for severe or complicated disease (e.g., infants)
•The person has or will soon have routine contact with someone that is considered at high risk of serious disease (e.g., pregnant women)



Post-exposure prophylaxis (PEP) through antimicrobial therapy options is recommended for:
•All household contacts of a pertussis case.
•High risk contacts within 21 days of exposure to an infectious pertussis case. High risk persons include:
•Infants and women in their third trimester of pregnancy.
•All people with pre-existing health conditions
•All people in high -risk settings (i.e., neonatal intensive care units, childcare settings, maternity wards).
Immediately contact the Missouri Department of Health and Senior Services’ (DHSS) Bureau of Communicable Disease Control and Prevention at 573-751-6113 or 800-392-0272 (24/7) regarding any patient suspected or confirmed of having infection caused by avian influenza A(H5N1) viruses or pertussis.
Vaccination with DTaP or Tdap provides protection from pertussis. It is recommended that children receive five doses of DTaP in a series. Adults should receive a booster dose of Tdap every 10 years. The flu vaccine is recommended for everyone six months and older and is widely available in Greene County. It is not too late for people to receive their immunizations for

influenza, COVID-19 and RSV. While vaccination may not prevent infection in all cases, it has been shown to reduce severity of illness and risk of hospitalization. Vaccine locations can be viewed at vaccine417.com.
For more information: SGCHD Health Alert Website: https://health.springfieldmo. gov/5656/Health-Alert
References
1) CDC 2024-2025 United States Flu Season: Preliminary In-Season Severity Assessment: https://www.cdc.gov/flu/php/surveillance/in-seasonseverity.html
2) CDC Respiratory Viruses Data Channel: https://www.cdc.gov/ respiratory-viruses/data/
3) Missouri DHSS Flu dashboard: https://health.mo.gov/living/ healthcondiseases/communicable/influenza/dashboard.php
4) Springfield-Greene County Health Department Flu dashboard: https://health.springfieldmo.gov/2909/Flu
5) CDC H5 Bird Flu: Current Situation: https://www.cdc.gov/bird-flu/ situation-summary/index.html
by Steve Edwards & Jay Guffey

On January 17, 2025, Drury University announced a new graduate degree program focused on Health Administration which will start in the Fall of 2025. The Master of Health Administration (MHA) at Drury is unique as it is a joint e ort between Drury University, CoxHealth, Mercy Springfield Communities and Burrell Behavioral Health. “This innovative MHA program exemplifies how academic excellence and industry partnership can create extraordinary educational opportunities,” said Dr. Beth Harville, Drury University Provost. “By bringing together the expertise of distinguished healthcare leaders and our strong academic foundations, we are creating a program that will develop healthcare administrators who understand both the theoretical frameworks and practical challenges of modern healthcare delivery.”
This promising initiative is designed to prepare the next generation of healthcare leaders. Spearheaded by Jay Gu ey, retired Senior Vice President and COO of Mercy Springfield Communities, and Steve Edwards, retired President and CEO of CoxHealth, the program exemplifies Springfield’s spirit of cooperation and innovation in healthcare.
You must go back over 30 years where the spark of an idea for the program originated. The genesis for the program was written in a life plan of an aspiring healthcare leader. Steve Edwards mapped out goals for his career on his personal life plan looking to a future when he would teach at the university level. A er achieving one of his many life goals by serving and retiring as the CEO of CoxHealth, he moved forward to make this plan come true at his alma mater, Drury University. Edwards developed the vision to bring together health systems in the community to educate the next generation of healthcare professionals. As Edwards describes the program, “Built on the foundation of a liberal arts university, I believe Drury’s MHA program will set a new standard. We will combine c-suite healthcare leaders and healthcare academicians to teach future healthcare leaders the skills, knowledge, integrity, and character necessary to lead in this important industry.”
In Springfield, healthcare is the largest employer providing care throughout Southwest Missouri, Northern Arkansas and Western Kansas. The need for well-trained leaders in all aspects of the field is vitally important to the ongoing success of the region’s health providers.


Edwards approached Gu ey to partner with him in developing the curriculum and structure for the program. Gu ey has been active in community projects throughout his 40-year career with Mercy and has continued his community work since his retirement in 2020. He and Edwards, even as competitors, worked together on several initiatives supporting the community during their careers. One of their key collaborations resulted in the Missouri University Medical School campus extension in Springfield. It seemed natural to join forces again and partner with Drury to bring this unique healthcare leadership program to Springfield. Gu ey said, “The opportunity to collaborate with Drury University and the regions healthcare providers to develop the MHA program is an exciting next step for our community.” The entire curriculum is designed around meeting the university’s academic standards alongside the real-world practicality of seasoned leaders and educators in the field.
The program consists of 36 credit hours covering the key aspects of health administration from large health systems to smaller clinical operations. A well-rounded healthcare leadership curriculum is a key aspect of this initiative. Courses focus on operations, finance, healthcare policy, strategy, healthcare law and ethics. The program is also unique by developing course work specific to community behavioral health engagement and leadership. Learning objectives for the MHA program focus on leadership, critical thinking, strategic planning, ethics and communication. Aspiring leaders from many areas of healthcare will benefit from this program.
Students interested in the program or needing additional information can contact the Drury College of Graduate Studies at Drury, grad@drury.edu or (417) 873-7530. There is a competitive admission process which requires a minimum 3.0 undergraduate GPA. All applicants will provide letters of reference as well as a personal statement on their motivation to participate in the program. Applications are available at drury.edu/graduateapplication.
As Gu ey noted, “Developing future pioneers in healthcare is a legacy worthy of Drury and the healthcare leaders in our region.” The community is better when there is collaboration and cooperation to improve the welfare of those who live in the Ozarks. Feel free to reach out about the program, Jay Gu ey, Program Director, jgu ey007@drury.edu or (417) 873-6813.

by David Barbe, MD ,MHA Former President MSMA (2005), AMA (2017), WMA (2020)
EXECUTIVE ORDER 14155
January 20, 2025
By the authority vested in me as President by the Constitution and the laws of the United States of America, it is hereby ordered: …
Sec. 2. Actions. (a) The United States intends to withdraw from the WHO.” 1
And so began the current controversy over the announcement that Pres. Trump intends to withdraw the U. S. from the WHO. It is no surprise that this announcement set o a firestorm of opposition. I think we can all agree that the past 15-20 years have seen a significant increase in the polarization of political ideologies in this country. The causes are multifactorial and include debates about how to increase health care coverage (recall the A ordable Care Act 2010) and the multiple controversies surrounding the Covid-19 pandemic. This has been accompanied by 4 changes in the presidency in less than 10 years. (Barak Obama 2009-2016, Donald Trump 2017-2020, Joe Biden 2021-2024, Donald Trump 2025)
The combination of these and other factors has resulted in increasingly broad and rapid swings in public opinion and public policy. The U.S. participation in and funding of the WHO has been one of the public policies impacted by these swings.
Near the end of his first term in April 2020, then President Donald Trump halted discretionary U.S. funding of the WHO. In July 2020, he notified the WHO of the U.S.’s intent to withdraw from the WHO as referenced in section 2 of the Executive Order noted above. Following the inauguration of President Joe Biden in January 2021, that notice to withdraw was rescinded.
Immediately following his inauguration on January 20, 2025, President Donald Trump issued the executive order including notification to withdraw from the WHO, halt all U.S. funding to the WHO, recall U.S. government personnel working in any capacity with the WHO, and to cease negotiations on the WHO Pandemic Agreement and the amendments to the International Health Regulations. Reasons given in Section 1 of the Executive Order included “WHO’s mishandling of the COVID-19 pandemic… failure to adopt urgently needed reforms, and its inability to demonstrate independence from the inappropriate influence of WHO member states,” and concerns over the “onerous payments” disparities between the U.S. and other member states, particularly China. 2
How is the WHO funded?

WHO funding is a combination of “assessed contributions” (a.c.) and “voluntary contributions (v.c.).” Only 20% of WHO’s total budget of $6 billion is covered by assessed contributions. The remainder is a combination of voluntary contributions by member states and other organizations and foundations. For example, over the 2022-23 2-year biennium, the U.S. paid $260 million (M) in a.c. and just over $1 billion in v.c. By comparison, China paid approximately $170 M in a.c. and $30 M in v.c. The next largest total contributions were Germany at $300 M, the U.K. at $200 M, and Japan at $150 M.
Note that China and the U.K. contributed the same total amount (approx. $200 M) even though the population of China is 21 times that of the U.K., and the U.S. contributed 6 times as much as China despite being less than one-fourth the population.
India, U.A.E., and Saudi Arabia each contributed less than $80 M despite their size and economic status. Significant voluntary contributions came from the Bill & Melinda Gates Foundation ($700 M), the Vaccine Alliance (GAVI - $500 M), the European Commission ($390 M), the World Bank ($250 M), and Rotary International ($180 M).3
A brief history of the WHO
WHO was formed in 1948 as a subunit of the newly formed United Nations (1945) in the a ermath of World War II. However, it was not the first health organization to bring together multiple countries to address health issues in common. One example was the League of Nations Health Organization (LNHO) established in 1920 following World War I mainly to address the spread of infectious diseases such as cholera, smallpox, and typhoid. The role and scope of the LNHO expanded over the next two decades, but the significant disruption produced by World War II dictated that the LNHO could not continue in its previous form.
In early 1943, Raymond Gautier an LNHO o icer wrote a report entitled “International Health in the Future.” This report contained an outline of a future “supranational” organization that could intervene in emergencies “without waiting for a governmental request.” In 1944, Gautier, US Surgeon General Thomas Moran, and others met and agreed on the need to build an international health organization and the importance of the United States taking the initiative to convene a conference on world health as soon as possible. It was out of this conference that the World Health Organization would emerge. 4
The WHO Constitution that came into force in 1948 established three governing organs: the World Health Assembly, the policy-making body comprising all member states, each with a single vote; the executive board, a subset of WHO members; and the Secretariat including the director general, to carry out the decisions of the Assembly and board.
The WHO was born as a “normative” organization with treaty making powers under its Constitution. However, by the 1960s, it had mostly abandoned international lawmaking as a tool to advance initiatives. Instead, it focused on developing technical guidance on biomedical advances through its International Health Regulations (IHR) process and passing on the skill and knowledge needed to attack a specific health problem. This approach was very e ective at significantly reducing or eliminating prominent infectious diseases such as malaria, tuberculosis, plague, cholera, yellow fever, and smallpox.
However, by the 1970s, politics became an increasingly important influence in WHO policy. Many of the member states were pushing for a “new international economic order” with health equity and a “health for all” agenda. The o en cited “Declaration of Alma-Ata” was adopted in 1978 declaring primary health care should be available to all persons. 5 In 2019, the United Nations and WHO universal health coverage an explicit goal. 6
One certainly must admit that the WHO has been responsible for significant improvements in global health. Some of these milestone accomplishments include substantial reduction in infectious diseases including eradication of smallpox (1980), adoption of regulations governing infant formula marketing and encouraging breast-feeding (1981), global response to HIV/AIDS (initially in the 1980s, then an even greater emphasis in the early 2000’s), integrated management of childhood illnesses strategy (1990s), founding member of the Global Alliance for Vaccines and Immunization (Gavi, now the Vaccine Alliance 1999), establishment of the Global Outbreak Alert and Response Network (2000), Global Strategy for Women’s, Children’s, and Adolescents health (2016), and numerous other initiatives focused on management of infectious diseases, antimicrobial resistance, as well as mental health and chronic diseases.7
As noted, the announcement of the planned U.S. withdrawal from WHO has drawn widespread concern and criticism. Multiple negative implications of U.S. withdrawal have been asserted. Many concerns involve the potential negative impact on the disruption of global information sharing of health data and research findings between the U.S. and other countries that would hamper identification of new infectious disease threats, modes of transmission, potential for international spread, development of diagnostic and
treatment options, development and distribution of vaccines, and sharing of prevention and control strategies during outbreaks of existing or new infectious diseases. The ease of global travel and importance of global commerce and tourism present a new level of global health threat. All countries, including the U.S., are vulnerable to the spread of disease and a delayed response to epidemics and pandemics if global communication and collaboration are disrupted by the U.S. withdrawal from the WHO.
A second concern is the direct impact of reduced U.S. funding on other important programs of the WHO including ongoing e orts to eradicate polio, respond to HIV/AIDS, strengthen the health capabilities and capacity of middle- and lowincome countries in areas such as maternal and child health and management of chronic diseases, and to monitor and respond to public health emergencies. 8
The other significant issue is the potential negative impact on U.S. influence and standing in world health leadership. We lead by participation in current negotiations to improve the governance and function of WHO and revision of the International Health Regulations to help avoid some of the deficiencies identified during the recent COVID pandemic. We also reinforce our key global leadership in large measure due to contribution of resources and financial support of WHO programs that improve the health of people around the world. The significance of that support is not lost on the countries that benefit. 9 In addition, the void in funding and influence created by a U.S. withdrawal would almost certainly give the BRICS countries (Brazil, Russia, India, China, and South Africa) and the middle eastern Gulf States an opportunity to increase their influence which is not always aligned with U.S. interests. 10
So, with so many reasons to stay engaged with WHO, why consider withdrawing? Many observers have recognized the need for improvements in the WHO policies, processes including greater transparency, less political influence (especially from China), and revised funding mechanisms. Although the WHO Secretariat has acknowledged those concerns and has been working on some of those for the past few years, WHO’s response and progress on those issues has not satisfied all parties including President Trump.
However, for historical context, President Trump’s 2020 and current intent to withhold funding and withdraw is not the first. Then President Ronald Reagan with the support of Congress withheld US funding from WHO for over 2 years in 1986-1988 over concerns that the WHO had become an unaccountable, bloated bureaucracy and was working against free enterprise and other American interests. 11 The Art of the Deal What does President Trump intend to accomplish by his
planned withdrawal from WHO? In my opinion, this is primarily his use of “The Art of the Deal” approach to bring greater pressure on WHO to go further, faster to remedy the expressed concerns and secure greater U.S. influence on revisions to the International Health Regulations (IHR) and the dra ing of a new pandemic agreement both requiring greater compliance by member states. At this point, the U.S. has ceased participation in those discussions for which U.S. endorsement is seen as critical. He can reverse the decision to withdraw and restore some degree of U.S. funding and participation as easily as he decided to withdraw as soon as he believes there is su icient movement on the U.S.’s concerns.
A second expressed intent in the Executive Order is to explore developing another organizational alternative to the WHO. Section 2 (d) (iii) directs the Secretary of State to “identify credible and transparent United States and international partners to assume necessary activities previously undertaken by the WHO.” 12 Again, it is my opinion that this is both a negotiating position with the WHO as well as a “plan B” if the WHO does not satisfy his concerns.
My expectation is that President Trump will reach an agreement with the WHO and avoid U.S. withdrawal. He doesn’t want the implications that would come with withdrawal as much as he wants change. It may not be a pretty process, but it may turn out to be the catalyst for the needed changes in the WHO policies, processes, and funding.
Jim Cook : Is it really? That is wonderful! Yes, later on we began giving scholarships rather than loans (even the loans were good deals at 1% interest). We have received many letters from students who said that they understood that they did not need to repay the scholarships, but intended to do so anyway just to help future students.
Blaine : What a time! What a great story and legacy you guys left for us!
Jim Cook : I miss them all! Especially Jim Brown; he was


References
1.Executive Order 14155 Downloaded 1/24/25 from: https://www. whitehouse.gov/presidential-actions/2025/01/withdrawing-the-unitedstates-from-the-worldhealth-organization/#:~:text=The%20United%20 States%20noticed%20its,to%20demonstrate%20independence%20from%20the
2.Executive Order 14155
3.https://open.who.int/2022-23/contributors/top25
4.The World Health Organization A History , pp. 10 – 33 DOI: https://doi. org/10.1017/9781108692878.002
Publisher: Cambridge University Press Print publication year: 2019
5.The WHO’s 75th anniversary: WHO at a pivotal moment in history, pp. 1-10.
BMJ Global Health 2023;8:e012344. https://doi:10.1136/ bmjgh-2023-012344
6. https://www.who.int/campaigns/75-years-of-improving-publichealth/
7.75 Years of improving public health
8. https://www.infectioncontroltoday.com/view/reflecting-on-the-uswithdrawal-from-the-world-health-organization
9.Rapid Response to: The US withdrawal from the WHO: a global health crisis in the making. BMJ 2025;388 doi: https://www.bmj.com/ content/388/bmj.r116/rr-1
10.The US withdrawal from the WHO: a global health crisis in the making. BMJ 2025;388:r116. http://doi.org/10.1136/bmj.r116
11. https://publichealth.jhu.edu/2020/the-other-time-a-us-presidentwithheld-who-funds
12.Executive Order 14155
something special. However, they were all special in their own way, and each one brought something unique to the group.
Blaine : Would you be okay with us linking some of your songs to the GCMS web site for future generations to enjoy?
Jim Cook : Sure! And I would be happy to help you pick out some of the songs!
















by Jonathan Vance, CFP Senior Advisor, Forvis Mazars Private Client
It’s well known that the cost of goods and services tends to rise over time. Recently, this trend has accelerated beyond historical norms. For instance, the manufacturer’s suggested retail price for a Toyota Camry was $25,420 in 2020. The 2025 model starts at $28,700. At first glance, this might not raise any eyebrows, but if this trend continues for the next thirty years, the Camry that once cost $25,420 could more than double in price, reaching an astonishing $52,653 by 2055.
It’s easy to pick an unusually inflationary period, focus on a single product, and use dollar amounts instead of percentages to illustrate this. However, it’s worth noting that the example provided actually understates historical inflation in the United States. According to J.P. Morgan, the average annual inflation rate over the past 50 years, as measured by the Core Consumer Price Index, has been 3.7%. If a Camry’s price increased at this average rate, it can be expected to cost $85,358 by 2055.
Through some mix of increased patient volume, insurance reimbursements, membership fees for self-employed physicians, or healthcare systems adjusting to retain talent, physicians in the Midwest have seen a 4.63% annualized increase in compensation over the past ten years. The figures used to calculate the above were derived as broad averages from Medscape’s 2014 and 2024 physician compensation reports. While isolating the “North Central” region in these reports, the data show there is considerable variability between specialties, employers, and other factors. As income grows at a similar pace to the cost of living, purchasing power erosion is less apparent.
However, stagnant assets tell a di erent story. In our example, $28,700 in a non-interest-bearing checking account is enough to buy the Camry in 2025. But by the following year, an additional $705 will be needed to purchase the same car.
This highlights the importance of ensuring that idle cash, investment accounts, and retirement accounts are not only invested, but also invested with inflation in mind to achieve positive, “real” returns (returns a er accounting for inflation).
There are some positives to inflation, despite there o en being a negative connotation to the term.
Not all expenses inflate equally. For example, a home purchased with a 30-year fixed-rate mortgage will have the same monthly
payment (on the debt obligation itself) in the 30th year as in the first year, assuming no refinance. The same applies to a level premium term life insurance or disability insurance policy.

The above examples provide an opportunity to proactively monitor our personal rate of lifestyle inflation, or lifestyle creep. As certain expenses remain steady or disappear entirely, such as student loan payo , individuals can anticipate an increased stream of discretionary income to allocate elsewhere. How these additional funds are spent or used is entirely up to the individual, as is the responsibility to honestly assess personal situations to determine if unintentional lifestyle creep is consuming more than its fair share of earnings.
Physicians can protect purchasing power by:
1.Minimizing idle cash: Keep only enough cash on hand to cover living expenses and potential emergencies.
2.Evaluating investment returns: Ensure all investments, including real estate and private businesses, yield a reasonable return relative to their risk.
3.Tracking annual expenses: Monitor yearly expenses and allocate free cash flow to priorities that matter most.
Forvis Mazars Private Client services may include investment advisory services provided by Forvis Mazars Wealth Advisors, LLC, an SEC-registered investment adviser, and/or accounting, tax, and related solutions provided by Forvis Mazars, LLP. The information contained herein should not be considered investment advice to you, nor an offer to buy or sell any securities or financial instruments. The services, or investment strategies mentioned herein, may not be available to, or suitable, for you. Consult a financial advisor or tax professional before implementing any investment, tax or other strategy mentioned herein. The information herein is believed to be accurate as of the time it is presented, and it may become inaccurate or outdated with the passage of time. Past performance does not guarantee future performance. All investments may lose money.

by Jim Blaine, MD
Dear Springfield area pediatricians and family physicians,
You will recall that, at the beginning of the availability of COVID19 vaccine, there was much misinformation that was being spread by politicians and others. The Greene County Medical Society (GCMS), in an e ort to improve communication from a scientific perspective, secured a grant from the Ozarks Community Foundation, and aired 15 second Public Service Announcements (PSAs) on KOLR10 that supported COVID vaccination. A month later the Springfield Greene County Health Department added funding for two additional months of the GCMS PSAs on KY3.
Last year, following the initiative petition passage of Recreational Marijuana by the marijuana industry, GCMS recorded PSAs encouraging voters to support the Springfield City Council ballot issue to add a 3% additional tax to recreational marijuana that could be used for prevention, treatment and research for recreational marijuana. Several other nearby municipalities had similar




ordinances on the ballot.
The PSAs aired throughout the KY3 broadcast area. The measure passed in all seven KY3 broadcast areas by over 70%.
The GCMS is now seeking to formalize our e orts to communicate directly to our patients through the media and plan to begin with pediatric patients. We feel strongly that those media messages should be led by physicians who take care of children. We have been working with Drs. John Burson and Kofi Asare-Bawuah in developing our first topics which include: Child Abuse Is Preventable, Vaccine Hesitancy, and The Risks of Marijuana. This
If you have an interest in knowing more about this e ort, please call, text or email me at: 417 861-9286 jimblaine@aol.com

















Everyone has different financial goals and priorities, and they change and grow as you do. That’s why it’s important for me to get to know you and
































by John Steinberg, MD
Dedication is evident in many forms. O en there is the subtle smile, word of praise, or the knowledge that one is supported by a close friend or spouse. Other times, there is much more sacrifice required. John “Bucky” Buckner, MD, epitomizes all forms of dedication. He demonstrates an unconditional love and support to his family and friends. He devotes countless hours to his patients in his general surgical practice. He takes an active voice in his church. Beyond these common demonstrations of devotion, he has dedicated an extraordinary amount of time and energy to the medical care of our American troops in the states and overseas.

Dr. Buckner initially joined the United States Air Force to aid his medical studies. He has always harbored a strong sense of loyalty to the men and women in the military services. The desire to administer excellent surgical care to our troops has always been paramount in his constitution. The first deployment was Desert Storm during the Gulf War in 1991. Subsequently, reenlisting in the United States Army, there have been four additional tours in Iraq and Afghanistan. During each tour he has dedicated himself to administer the world’s best trauma surgical care to our U.S. troops, and the soldiers and civilians of other countries.
In order to render his surgical expertise overseas, Dr. Buckner has sacrificed much that is dear to him at home. Each tour required a commitment of “90 days boots on ground” in the country of destination. This did not include the weeks, and even months, spent at di erent military bases before and a er

each deployment. His well established surgical practice in Springfield is placed on hold, covered by his dedicated partners. There is also the absence from his family during these long months. There were activities of his children missed, including football and volleyball games, senior banquets, birthdays and even a presentation of a Red Cross Hero Award given to his eldest son. A Thanksgiving Holiday and one wedding anniversary were missed.
Fortunately, Dr. Buckner’s family is very supportive and dedicated to him. His three children, John, Christina, and Jake, understand their father’s desire to serve. All three have demonstrated their own dedication as they grow into adulthood by being successful in college and challenging themselves to be productive members of society. Following his father’s example, John has recently joined the Missouri National Guard.
The largest measure of sacrifice and dedication comes from Dr. Buckner’s wife of 28 years, Rochelle. Beginning in medical school and spanning the grueling and demanding years of a surgical residency, Rochelle has always been the epitome of support. During the months of deployment, she has been the CEO of the family at home, keeping their children on the right track and the doors of the home open. She understands and respects the dedication that Dr. Buckner has to these deployments; her devotion never waivers.
With each deployment it has become a tradition of mine to send Dr. Buckner books to read. One such o ering was Harper Lee’s To Kill a Mockingbird. I found this to be appropriate as the protagonist, Atticus Finch, mirrors the dedication of my good friend “Bucky” Buckner. Both have the strong desire to do the right thing for their fellow man without fanfare. Though this takes time away from their other obligations, their strong sense of loyalty to family and friends never falters. We need more people like Atticus Finch and Dr. John “Bucky” Buckner in this world.
Original article published by Missouri Medicine 2012 reprinted by permission.
by Barbara Hover, GCMSA President
Over 200 physician family members enjoyed the exhibits and visiting with other physician families at the Discovery Center on February 28. Greene County Medical Alliance has worked to serve community physicians since 1924. Our primary focus has always been on physician families and projects to support community health. Thanks to the support of Ferrell Duncan Foundation and Mercy, beginning in 2016, we have focused our e orts on physician wellness.
The AMA has designated physician burnout as a serious issue a ecting the profession of medicine. Our physician family evenings provide relaxing quality time with the family and fellowship with others in the same occupation. Camaraderie with others who understand the pressures of patient care are
known to alleviate the feelings of burnout.
We invite you to join GCMSA and help us plan other interesting activities for physicians and their families. We welcome new ideas and new members. Our next scheduled event will be Physician Family Night at the Zoo on Saturday August 23. We hope to see you there.















































With Private Banking at Central Bank, you have exclusive access to a host of financial services and products, where we take care of the details across the full spectrum of the bank. You will have access to higher deposit rates, custom credit solutions and home financing, as well as individualized guidance with your investments. Our main goal is to help you maximize your money seamlessly. You have complex needs. We have the concierge level solutions you want.



STEVE GASSEL
Senior Vice President - Director of Private Banking | NMLS # 554828
3333 S. National Ave., Springfield, MO 65807
Phone: (417) 841-4213
Steve.Gassel@centralbank.net
KARA TURNER
Vice President - Private Banking | NMLS # 1833785
3333 S. National Ave., Springfield, MO 65807
Phone: (417) 841-4253
Kara.Turner@centralbank.net
JOYCE WONG-HSU
Officer - Private Banking | NMLS # 1239617
3333 S. National Ave., Springfield, MO 65807
Phone: (417) 841-4214
Joyce.Wong-Hsu@centralbank.net
by Mary Louise Brown & Dr. Trig Brown reprinted by their kind permission.

Cover Art: Caricature by anesthesiologist George R. “Skip” Gay (1931-2008), which appeared on the album cover of the Singing Doctors’ 4th album, Singing Doctors on Stage, released in 1966. The front row L-R depicts Dr. F.T. H’Doubler, Dr. Jim Brown, Dr. Fred Coller. The back row L-R includes Dr. Don Gose, Dr. Charles Lockhart, and Dr. Hal Lurie.




The Singing Doctors of Springfield, MO Medical Scholarship Fund has been providing financial assistance to deserving medical students since 1959. But who were those madcap mavens of medical mirth?
In 1958, Dr. Jim Brown was named entertainment chairman for the Greene County, MO Medical Society Annual Banquet - but no funds were available. He approached other doctors to perform a handful of medical parodies he wrote to the tunes of popular songs. The show was a big success, and the group was off and running. Initially performing their “Medical Hit Parade” under the name “The Greene County Boys,” the group included Drs. Jim Brown, Fred Coller, Don Gose, F.T. H’Doubler, Charles Lockhart, and Hal Lurie. Other originals, Drs. Guy Calloway and Wilfred Wooldridge, were not able to travel with the group once the requests started rolling in. Wilfred Adler, professor of music at Southwest Missouri State University (now Missouri State University), was the musical director. The long-suffering wives of the group helped maintain the costumes and provided audience support in what would become nation-wide appearances.
Within months of their first performance, the group established the Greene County Medical Society Foundation to administer low-interest loans to deserving medical students. Funded with proceeds from the sale of records and tapes, the Foundation was administered by the staff of the Greene County Medical Society. The Singing Doctors received no compensation for their appearances other than reimbursement for traveling expenses.
Dr. Jim Cook joined the group initially as a substitute in 1968. An early recipient of the Foundation scholarship fund himself, Dr. Cook soon became an invaluable permanent member of the Singing Doctors.
Over the years, the Singing Doctors produced seven albums, including Borborygmi, Placenta Preview, Medic Emetics, Singing Doctors on Stage, Singing Doctors Keep You in Stitches, Thanks for the Miseries, and The Best/Worst of the Singing Doctors.
The format of the Singing Doctors performances was an upbeat variety show and featured at least two regular acts. Trichomonas Trigger and his oldest boy Emmett were recurring characters who parodied the country music-themed songs. The Four Suppositories delighted the crowds as the “harmonizing” quartet.
It goes without saying that the members of the Singing Doctors had a wonderful time performing, but the real purpose was the financial assistance they extended to more than 200 medical students over their 40-year run. In 1998, the Singing Doctors Scholarship Fund was transferred to the University of Missouri-Columbia where it continues to grow and provides financial support in the form of grants to medical students each year.



1958 Brown is named Entertainment Chairman of Greene County Medical Society Annual Banquet –then told there is no budget for the program.
1958 Greene County Medical Society President’s Inaugural Banquet initial performance with six original members: Brown, Gose, Coller, H’Doubler, Wooldridge, Callaway, and Adler at the piano.
1958 Missouri State Medical Society in St. Louis is their first out of town performance.
1958 (August) Lurie joins cast for performanceb eforethe American Medical Association Public Relations meeting in Chicago. Callaway and Wooldridge decline t o travel and leave the group except as occasional substitutes.
1958 Borborygmi released as first of what would be seven record albums.
1959 The Greene County Medical Society Foundation is established as a separate and distinct not-for-profit organization.
1959 Oklahoma State Medical Association performance in Tulsa and,for the first time, the group is introduced as the Greene County Boys.



1959
Second album, Placenta Preview released.
19 Third album, Medic Emetics released. Woolridge re-joins the group for the recording session.
19 Don Richardson hired as public relations director.
19 5 Threemembers of the group (Brown, Gose, Lockhart) appear on “I’ve Got aSecret” television broadcast.
19 5 Appearance on the “Today Show.”
19
Fourth album entitled, Singing Doctors on Stage, released.
19 8 Jim Cook joins the group as a substitute and soon becomes permanent member.
19 9 (August) Singing Doctors featured on the cover of Resident and Staff Physician journal.
19 Greene County Medical Society files suit against the Internal Revenue Servi ce after being required to pay back taxes on record sales for 1964, 1965, 1966, effectively suspending Singing Doctors scholarship work. GCMS receive s a favorablejudgment in 1972 and again on appeal in 1973 -and the group is finally back in the scholarship business.



19 1 Performance before the American Medical Association Annual Meeting, Atlantic City, NJ.
19 Singing Doctors Keep You in Stitches is released, the group’s fifth album.
19 Thanksfor the Miseries is released as sixth record album.
19 8 Singing Doctors receive the AMA Special Award for Service to the community and medical education.
1981 On cover of Springfield! Magazine, vol. II, Feb. 1981.
198 Best /Worst of The Singing Doctors, seventh album, is released.
198 Dr. Fred Coller dies.
1985 Springfield Mayor George Scruggs declares October 25, 1985,Singing Doctors Day.
198 (March 2) Missouri Senate Resolution(sponsored by Senator Bradshaw)honoring the Singing Doctors, 81st General Assembly.
1989 The Singing Doctors’ final performance at the Greene County Medical Society Installation of Officers. Hal Lurie is installed as president.
1991 Don Richardson, Singing Doctors publicist, dies.
199 (October)Greene County Medical Society votes to rename the scholarship fund theSinging Doctors Fund, rather than the General Loan Fund.
1995 Dr. Charles Lockhart dies.
1998 Transfer of funds to University of Missou ri –Columbia as the Singing Doctors of Springfield, MO Medical Scholarship Fund.
Prof. Wilfred “Wimpy” Adler dies.
5 Dr. Jim Brown dies.
1 Dr. F.T. H'Doubler dies.
11 Dr. Don Gose dies.
15 Dr. Hal Lurie dies.

a. AMA News, October 6, 1958, featuring the new Singing Doctors. The backrow, L-R, Drs. Hal Lurie,F.T. H’Doubler, Fred Coller. The front row, L-R, Drs. Charles Lockhart, Jim Brown, and Don Gose.
b. The Four Suppositories! Including L-R, Drs. Hal Lurie, Don Gose, Fred Coller, and F.T. H’Doubler, ca. 1962.Photo by Duncan Studio, Springfield, MO.
c. The Singing Doctors , L-R, Drs. Hal Lurie, F.T. H’Doubler, Don Gose, Charles Lockhart, Jim Brown, Fred Coller, and Prof. Wilfred “Wimpy”Adler at the piano. From “Springfield’s Musical Medcaps,” Sunday News & Leader, Springfield, MO, Oct. 14, 1962.
d. Trichomonas Trigger and his oldest boy Emmett , early 1960s.
e. Advertisement promoting the release of the 4th album, Singing Doctors on Stage, 1966.
f. The Four Suppositories’ calypso rendition o f Borborygmi. From “Springfield’s Musical Medcaps,” Sunday News & Leader, Springfield, MO, Oct. 14, 1962.
g. Album cover for Singing Doctors Keep You in Stitches, thegroup’s 5th release, 1972.
h. The Singing Doctors were featured on the cover of Springfield!Magazine, February 1981.
i. Cover for The Best, Worst of the Singing Doctors, released in 1982, their final album.
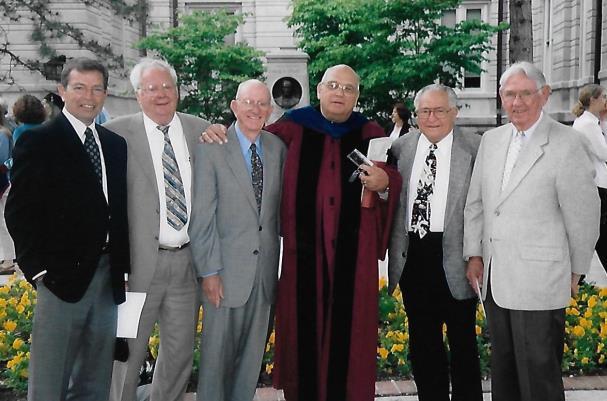
j. Some of the Singing Doctors attended the 2003 graduation ceremonies for the University of Missouri School of Medicine.L-R, Drs.Jim Cook, F.T. H’Doubler, Jim Brown, MU faculty member William B. Bondeson PhD, Drs. Hal Lurie, and Don Gose. Photographer unknown.
k. The Singing Doctors of Greene County, L-R, Drs. H’Doubler, Gose, Coller, Brown, Lurie, and Lockhart, 1964. Photographer unknown.

Here are the lyrics of just a very small sample:
(Sung to the tune of “There’s no Business like Show Business”)
There’s no business like doctoring business
No business I know
Everybody thinks the doctor’s busy
They all think we never have time off Well, I’m here to tell you why we’re busy
We either count our money or play golf
There’s no business like doctoring business
Let’s go on with the show
We’ve got tunes that top the medic hit parade Songs that died in the last decade
But they’re songs we’ve written for the likes of you Without further ado, here are medical songs for you.

(Sung to the tune “Thanks for the Memories”)
Thanks for the miseries
From Singing Doctors songs in keys so often wrong But if it feeds a student’s needs, we hope you’ll sing along Yes, thank you so much.
Thanks for the miseries
We know we’ve caused a few as doctors often do We’ve tried to make you happy and we hope you weren’t abused So, thank you so much.
That we retired was a rumor
We’re back on your doorstep, you see, Thanks for your sense of humor
Tho’ ours is sick - It’s your pockets we pick
So, thanks for the miseries
We’ve caused throughout the years with laughter and with tears We’ve tried to raise some money by ingratiating ears
We thank you so much.
Thanks for the miseries
You know it’s all in fun but when the day is done If you can smile a little while, there’s hope for everyone We thank you so much!
(Sung to the tune of “Jimmy Crack Corn”)
Listen my boys and I’ll relate
The story of man and his cruel fate The topic deals with glans prostate The message is massage.
When I was young I paid no mind To daily habits of the bathroom But now that I am forty-two I envy what the young boys do.
CHORUS:
If you hesitate a lot Seek relief and find it not You poor man here’s what you’ve got Benign hypertrophy.
My bones were fused at twenty-three I’m just as tall as I used to be My shoe size is the same I know So why, oh why, must my prostate grow?
CHORUS:
Hypertrophy means getting big Like bicep muscles when ditches you dig If use increases size I fear My prostate should have disappeared.
I asked a girl to dine and dance Despite my age even tried romance I blushed but this is nothing strange I did not have a diaper change.
CHORUS:
The sound of water often calls No sight is better than Niagara Falls A river’s stream is what I seek Why must I watch a faucet leak?
I’ve monogrammed my catheters I even labeled them “his and hers” It solves no problem but, at least, It’s quite a conversation piece.
CHORUS:
Most men get up at night I know Some young ones go home - but me I just go
Please, doctor, hear my urgent plea Won’t someone cure my urgency?
This old cliché you’ve heard, I know You’ve gotta go when you just gotta go I play the Army game of late I hurry then I hesitate!
CHORUS:
If you hesitate a lot
Seek relief and find it not You poor man here’s what you’ve got Benign hypertrophy!
(Sung to the tune of “Detour”)
There is much you can say about medicine today We’ve made great strides in drugs and surgery
But there’s still one disease That we can’t treat with ease
To say you can is perjury!
CHORUS:
Hemorrhoids. Often itch and always burn. Hemorrhoids. Give you that look of concern. Hemorrhoids: If you think your life is void, You should have a hemorrhoid!
We use creams and oils and such But it just don’t help us much. And sitz baths give relief for just awhile. So we switch to Medicone and a shot of Yellowstone, But still can’t sit and still can’t smile.
Now a man ain’t no good And can’t act like he should If his seat of learnin’ is so burnin’ hot. If he’s cautious when he walks And a-frownin’ when he talks Then you can bet here’s what he’s got.
CHORUS:
Hemorrhoids. Often itch and always burn. Hemorrhoids. Give you that look of concern. Hemorrhoids. If you think your life is void, You should have a hemorrhoid!


(Sung to the tune of “Has Anybody Seen my Gal?”)
That ole bad breath…ole bad breath
That awful odor’s worse than death
But halitosis beats no breath at all
A turned-up nose means you’re one of those
Who should use Sen-Sen or chew cloves
But halitosis beats no breath at all
Now all the dentists say if you can pay
They’ll cure this disease
It isn’t so, so save your dough
Be grateful for a malodorous wheeze.
So don’t be sad if your breath is bad
You’ve every reason to be glad
For halitosis beats no breath at all
Now you will find a few, best friends who Won’t tell you of your scent
Let insults lay. There’ll come the day
You’ll wonder where the yellow went.
So don’t be sad if your breath is bad
You’ve every reason to be glad
For halitosis beats no breath at all…all…all
Halitosis beats no breath at all!

(Sung to the tune “That’s Entertainment”)
The word has been going around
Have you heard of new talent in town
It’s absurd but we’re here to expound The Singing Doctors!
We’ve all left our worries at home
Not on call to the rings of a phone
Have a ball making fun of our own We’re Singing Doctors!
A Brando, Sinatra, we know we are not And Bernstein might not think our music so hot
There’s one tradition we’ve got
Well, if anyone’s gonna keep score, we can safely say we “Barrymore”
So smile if you’re proud of the clan Laugh awhile, sing along if you can It’s worthwhile for a medical man
For symptoms described A song is prescribed By Singing Doctors!




by Jim Blaine, MD
Jim Blaine : Hi Bucky, it’s good to see you. I have been looking forward to this interview.
Bucky Buckner : Good to see you too Jim. It’s been awhile.
Blaine: I recall that you went to UMKC for med school.
Buckner : Yeah, I was a 1979 graduate of Parkview high school in Springfield and attended UMKC for six years. I went to the University of Oklahoma for my surgical training for five years. Following that I went into active duty Air Force in Omaha for three years (90 to 93). I then moved back to Springfield and I've been here since. Doctors John Steinberg, Carl Price, and I are in town because we were interns together and doing all of our surgical training in Oklahoma City.
Blaine: So you were in University Hospital in Oklahoma City?
Buckner : Yes, University Hospital along with Children’s and some Presby (Presbyterian Hospital). I was basically in Oklahoma 19851990. I come from the family of teachers and preachers; my dad's a university professor and my mom’s a psychologist. Both of my grandpas were Southern Baptist preachers from Arkansas so I borrowed money to get in to get through my first bit of school and, once I couldn't find any more money to borrow, I joined the military. So I strictly put the uniform on to pay for school. Now I like wearing it and stayed in of course, but in fact I wanted to be a heart surgeon along with Steinberg.
in academia. A lot of surgeons get stuck in little bitty hospitals and so I was lucky!

Blaine: How many years were you in the military as a military surgeon before you came into private practice?
Buckner : Three years. Operation Desert Storm broke out in 1990-92 and happened literally a week after I came on service in Omaha and I got deployed to Germany for about about 2 1/2 months and basically did nothing. I just drank a lot of very good beer, and I came back from that a little disappointed. A funny story was, when we were coming into Dover, and they were having celebrations because “we won the war”, and I felt that I didn't do squat and had to go through a line of people. Two kids stopped me and said, “Hey, are you a marine?” I said, “I'm just an Air Force doc” and


All the “cool kids” wanted to become heart surgeons. Of course this was in the 80s and basically the Air Force said “No. We will give you the deferment to become board eligible especially for five years in general surgery.” I asked permission to do a one or two year cardiac surgery fellowship and they basically said, “ No, we already have three heart surgeons, and only need one. We need 150 general surgeons, so you'll be a general surgeon.” That was the best thing that ever happened to me! So I had to go into active duty and was fortunate I got to go to an Air Force Base in Nebraska where we had Creighton and the University of Nebraska. We had residents rotating and I was a clinical faculty member at the University of Nebraska so we were able to stay

they said, “Let's go find a Marine!” So I came home from there feeling as though I missed my war, you know. It is said that great surgeons are made in war time right? So I got home from that and wasn't feeling like I I did what I was sent there to do. However, I do thank the Lord it wasn't another Vietnam lasting for years and years and tens of thousands of casualties, but I came home from that a little disenchanted as you can imagine.
Blaine : So you were sent to war to fulfill a need and you basically weren’t needed?
Buckner : Yeah! So I finished up my active duty time and began to look back in Oklahoma City, Kansas City
and Omaha and got offers in all of those places, but I came back and looked in Springfield because my Dad was still here and I told him I would. Additionally, we had a one year old, a 3 year old, and a 5 year old so coming back to Springfield was just too good for a

young family to turn down. I got a great offer at FerrellDuncan; I also got an offer at Mercy, and Smith Glynn Callaway Clinic.
Blaine: That would have been 1993?
Buckner: Yes! The integration did not happen until after 1996. I did about 20% of my surgery at St. John’s; as you know, we went on both sides of the street. ER called and we went.
Blaine: So, you sub-specialized into breast cancer then?
Buckner : Yes, I had some influence. We had a guy named Alan Hollingsworth who was coming close to your time actually. He went to Med school at OU and then he went to California. Alan came back as a junior staff guy in 1987 and he brought this crazy idea about breast surgeries. He had been on the West Coast for about four or five years and breast surgery was already a specialty there. The lumpectomy trials were just beginning to come out so if you had a breast lump you took it out and if you had breast cancer you do a mastectomy and that's it. No more complicated than that so, at that time, these surgeries went to the junior residents. The chiefs wanted to be at the vascular clinic to find the AAA's and the general surgeons wanted find the

pancreatic and colon cancers and do the Whipple’s or whatever. Well Hollingsworth came back and said that breast surgery truly should be a specialty of its own and so that was an early influence on me. Joni Scott was one year ahead of me and that's where she basically got her her inspiration as I did to do breasts. So, even when I was in the Air Force I made it known that I had a special interest in taking care of ladies with breast cancer. Fellowships didn't exist at that time, but I always had that interest. When I came to town I did major vascular, colorectal, thyroid, parathyroids and everything else. I did a lot of vascular access.
Blaine : Who were your partners at that time?
Buckner : Don Gose, Jim Cordonnier, Marc Whitmer, Jim Gibson, and Tom Moffe
Blaine : I did get to know all of them in the ER and those were all good guys
Buckner: Yeah, and they have now all finished their careers. I think that, between Ferrell-Duncan and Springfield in general, they probably average around 32 years career for each of them. And I'm there now you know; pretty good!
Blaine : Shall we go back to your military experiences?
Buckner : Sure!
Blaine: When did you first deploy from here?
Buckner: So I came to Springfield and the fine print is that you owe them the years in active duty that they sponsored you in training, but you have a minimum of 8 year service. So this was unbeknownst to me previously, and I was a little chagrined. My wife wanted me out right then, but I was kind of glad honestly that I got to stay connected because I had to stay in the reserves. I had five year mandatory reserve duty so I would go up to air base at Knobnoster and do drills at least every other weekend and the military gave the doctors a lot of leeway in reserve status. They're okay as long as you're ready to go and you’ve got your stuff done. You don't have to be here all the time and they would give you credit for CME. You were doing your full time medical job everyday just as you did in wartime versus a lot of the troops who had non medical jobs. Some of the surgical techs were working at non medical jobs and they were
only surgical techs in the military. So I got here in 1993, and in about 2000, I was thinking that “This is this is a waste time.” I was crazy busy with a young family; I'd


drive up there on Friday nights and drive back Sunday evening and then start a crazy busy week! I finally had had enough, so I resigned my Commission in 2000 from the Air Force. I was done! And then 9/11 happened. So I recommissioned in the army because Jose’ Dominguez (one of my good friends and partners) was actually with the unit here in town with the 325th combat support hospital and I knew that I could drill at home. I then had a heart to heart with my wife and she said “Okay; you know I understand.” I felt at the time that the army was probably gonna be doing the heavy lifting and it made sense to drill in town so I raised my hand again right after 9/11. Basically, I started the calls literally about three days after 911 and it took me about 5 months to get back in. I can't tell you how many times I had to refax stuff and find stuff; it was crazy Jim! Although it was painful to get back in a time of war as a surgeon, I persisted and I was finally recommissioned in the army as a major which was the rank I was at in the Air Force.
Blaine: Why did you feel compelled to go?
Buckner: I was aware of the risk that these young soldiers were facing, and I simply felt obligated to help provide the best care possible for them.
Blaine : You actually changed branches; you went from Air Force to Army and that was in 2002?
Buckner: Yes; it took me a few months after September 2001. It was probably March/April 2002 that I was finally
recommissioned and, as I recall, Doctor Dominguez did my oath to re-enlist in the Army. I got a call in March of 2003 at 8:30 a.m. saying we needed to be at the unit tomorrow and you're going to deploy to Iraq. So I told my staff we need to reschedule everything beginning tomorrow. I had a full surgery schedule and I just literally walked out of my office.
Blaine : No negotiation with the Army?
Buckner : No! Monday morning I got a call saying, “You need to report to the unit tomorrow; you'll be deploying to Iraq from Fort Lewis in Washington state and you'll be flying to to Fort Lewis within the next 24-48 hours”.
Blaine: Who got your cases?
Buckner : I don't know I just said, “You got it” and my partners handled it for me.
Blaine : Like getting hit by a train?
Buckner : Yes! I was supposed to be a Toby Keith concert that Friday night with some of our hospital people and my wife and and I didn't make it. I was landing in Seattle Washington and arrived on Friday and then we got stuck there and it was like Groundhog Day every day and we were literally stuck there for two months because Turkey wouldn't open up and never did give us the green light to go through Turkey into northern Iraq. So that is how I ended up being gone from home for 7 1/2 months and it was supposed to be 3 months. That's the deal they made with this 90 days boots on the ground, and that is why I took a picture of the first time I put my foot in the Iraq sand to prove to the army that we had finally arrived. So it was not busy in 03, but it was tough! I was about 18 pounds lighter than I am right now when I got back. Dealing with the heat and eating MRE’s (Made Ready to Eat); it was not a great deployment and I was kind of disillusioned with the army simply because we waited and we sat a lot. We had a lot of the enemy that had gone to ground so the troops weren't doing much. We were convoying across Iraq all the time in a Humvee. I always thought we'd have helicopters overhead taking care of us, but we were driving. My XL would say, “just hang out the window with your M16 and keep it moving”. They were dropping grenades and there was a lot going on in 03 that was not good; it was like the Wild Wild West!
Blaine : Did you take care of many casualties?
Buckner : Oh yeah! We definitely had some business,
but it was really intense for a day and then nothing for a whole week. I had a DVD set of Band of Brothers that I would allow myself to watch one hour per night because I needed something to look forward to. I came back from that really kind of BS on the whole thing and thinking that I'm done with this! But, I just couldn't let it go. A fellow over there told me that he “kept going back and was trying to figure it out”. So, I think I was also just trying to figure it out and for me I was also escaping a crazy practice and it was the one time that I did not have a cell phone to answer. So, it was a little bit therapeutic.
You know people say “Thank You for your service” and you think “Whatever”? The comment itself is becoming a bit trite. They really do not want to talk about it. Perhaps the better response might be just to say “Welcome home!” Especially to Vietnam vets!
So I went back in 2005, 2007, and 2010. I was taking care of prisoners in 2005 in a big prison hospital; Camp Bucca which was named after one of the captains who died heading up the World Trade Center. We had 10,000 prisoners and I was kind of BS about that deployment because I signed up to take care of troops and it was a very high visibility right after Abu Ghraib. Every time anything didn't go well with the detainees, IG rolled in wanting to talk about it! We had a lot of deaths. We called ourselves the Walter Reed of Iraq because there was no other place for these guys to go! I was taking care of 70% burns on an army cot, and that often doesn't go well. I had to cut one guy's last leg off and skin graft from that limb to try to save him. I couldn't let any skin go to waste.
Blaine : You called it the Walter Reed of Iraq, but did you you have any of the facilities you needed? Did you have any type of burn unit?
Buckner: Nope! We didn't even have running water, but we had electricity and we had air conditioning. They put this prison out in the middle of nowhere in way South Iraq and needed a 10 or 20 mile perimeter because they didn't want to be attacked and have 10,000 prisoners unable to be defended. Next, I was in the peak of the surge the summer of 2007 in Iraq and I was in Afghanistan the summer of 2010 at the peak of the surge in Afghanistan and those were very busy deployments.
Buckner : Yes! In 2003, we were operating out of a tent and through a hole cut in a patient gown. We would do a lap with dirty feet sticking out and we would wear a battery powered headlight because we'd lose electricity all the time. It was pretty rough. Our first case I took my gown off and splashed water on myself to wash off the sweat because it was 130. We kept the windows open until we got a casualty coming in. We would then close the windows and sweep the sand out and it was between 130 and 140 in that room by the time we finished the case and the commander went to the base commander and told him, “ Sir, they have to have one window; we gotta do something”. However, my troops could handle it. I never saw heat casualties over there Jim. Not until I got home that summer and firemen were falling out with a heat index of 110, and I wondered what the problem was and then I realized the reason those firemen are falling out is because they live in a 70° Firehouse all day and then they run right out into the heat. We lived in heat; we were acclimated. They were not. In 2003, I was unloading my weapon on a pallet and there was a little bit of a breeze on the tarmac and it felt kind of good. I then looked over at the thermometer on the tents and it was 122. I remember thinking that I must be acclimated now.
Blaine: How was your post op mortality under those conditions?

Buckner: "Afghanistan has traditionally been a tough place for women, and of course, a woman was felt to be useless if she lost a leg."
Blaine: Contrasting your 2007 and 2010 deployments with your 2003 and 2005 deployments, were they better equipped?
Buckner: We did lose a lot of prisoners in 2005, because of the degree of injury and just our limited resources and other challenges, but, if you arrived at any surgical facility FST in Iraq or Afghanistan, you had about a 98.5% chance of going home alive. So we did really good.
Blaine : I was expecting you to say 50%.
Buckner : No; we did very good saving our guys. Also, our guys were well protected. The Iraqis or Afghans were wearing ball caps and had very little armor if any and and so they were the ones that had devastating injuries. I saw the decapitations and other severe injuries with our people too so there were non survivors on our side, but, if you got to our place alive, you were very likely to survive.
Blaine : How many cases would you do in a day or week?
Buckner : There was a day where I think we probably operated for 18-22 hours.
Typically, when we got hit, we might have four or five Class 1 traumas. There were twenty of us and sometimes I was the Lone Ranger. I almost always had an orthopedic surgeon and there were times when there were three trauma docs, but it was always a little daunting when you got there and I was the only general surgeon on duty. Sometimes, there were situations that were overwhelming, especially to docs who were not trained in trauma, and, in that case, I was the Lone Ranger and it was kind of daunting, Jim, when the buck always seems to stop in the same place for the next 100 days 24 hours per day, but, whatever happens, it needed to get fixed.
Blaine : Just trying to think about that and you being inundated with that type of schedule with those restraints and not having modern surgical resources, how did you weather that stress for 100 days at a time? Especially with your heart being back home with your wife and kids.
Buckner: The team; you really just lean on your team because you’re all in the same boat. We all have different jobs, but every night we smoked cigars and drank Diet Coke. There were phones and, later on, Internet, but it was tough. We had “walking blood banks” later on in my last two appointments which is amazing giving people warm whole blood. You call for a blood type and people were there to volunteer! They didn't ask who was shot. They were just there to help. We had a lab tech who was amazing! She would get us blood fast and when they reviewed that data Jim, it's pretty solid and there were no problems. Of course you've got a population that's been checked out and everybody's got their shots and everybody's been HIV checked. You know every time coming and going that your HIV was checked and your hep C was checked. Through this all, the troops were always so cool because they didn't care whoever was shot up, they they just showed up and put their arm out and and gave blood! You just
knew your limitations and you couldn't change that so you just did the best you could. I just always hoped that nobody died because one of us didn't know how to do something and I don't think that happened, but, if it did, it didn't happen much. One case still bothers me. There was a night when my commander said " Major, you can't have one more unit of blood. You're done and I’m cutting you off because we have a very limited supply left". I had a critical patient and this was before the “Walking Blood Bank” was happening. He said that we wouldn’t get respite till sun up and said, “I'm cutting you off unless you tell me that two more units of blood saves this guy's life.” I couldn’t say that, and he died. That would have been an illegal order later in the war and that was the tough thing as rules of engagement kept changing.
As far as the military, I kept going back and it was hard on my family for sure. I missed a lot of stuff, and, although I'm very proud of my service, I think what bothers so many troopers, and I think probably me is the moral injury thing and that's something I dove into a few years ago. I did several lectures on it and have read 10 books and I think that's really when I began to realize a little bit of crisis in my life. I never related to PTSD and still don’t, but moral injury is not just a military thing, it's also doctors doing that everyday. As ER doctors, we know that you see people do things to each other when you know that they shouldn't have that right to do that. That just it gets into every fiber of you concerning how humans are supposed to behave; especially to each other. When you have seen that violated so many times that you kind of just can lose faith a little bit. You do!
There are things worth fighting for there is no doubt! Politicians don't take it as seriously as they should! They tend to squander the courage of troopers and they abuse their rights and I will include every two star and above because they're all politicians too. Once you get a star you have to go before the Senate so you now become a politician. You gotta politic your next shot and you're no longer in the chain of command of troops that are being promoted based on their merit. I am reading a book that says that there's 44 four-star generals right now, and, at the peak of World War 2, there were 7 four stars and 20 million troops. So, currently, that’s top heavy and everyone of those Generals in the Pentagon has 100 staff members and about 95% of them within weeks of getting out or working for a defense contractor and making a lot of money because they know everybody. It’s just such a disservice to the guys in the service that many of them are losing their lives and losing their limbs and that's what happens when you get back and you think of what you saw and
the things that happened and you start looking into why. And if it makes sense it makes sense because there are reasons to risk your life, but if it doesn't make sense when troops start taking their own lives. Suicide went up and when we bailed in Afghanistan and we lost a bunch of marines due to suicide; more in one day than we lost in two years. Who is responsible for that! When I got back from one of my deployments, I could not find my multi tool and had to pay the army $50 in reimbursement. The army left $8 billion worth of equipment in Afghanistan, and who paid for that? There just seems that there is no accountability on the politicians’ side for anything!
People talk about the greatest generation; this generation of troops that I experienced in Iraq and Afghanistan were the best! There was a lot of stuff in World War II that was never reported. We know that! Bad things happen, but, man, we're under a microscope now and our guys generally did really well.
Blaine : What age were the troops you were around?
Buckner : Mostly early 20s I mean these guys walked through hell with their all the sweat lines of salt on their shirts. They were sleeping under their Humvees in the streets in Iraq. Sometimes you would say, “How you doing trooper?” And they would say “Good army day Sir!”. These guys were always an inspiration and that is why you wanted to do good by them! It was the privilege of a lifetime to have the opportunity to care for them! To be there for those guys. I always felt as though I came back better for it.
Blaine : You mentioned earlier that you have had an epiphany recently about your four combat deployments.
Buckner : Yes! I heard a trooper talk about the fact that he just realized that this whole Iraq war destabilized Iraq and and has made Iran more dangerous, and security contractors made billions of dollars. I have always been a huge fan of of President Bush; he's a good man and I think his intentions were good. Does that mean he did good? I think that he probably had some bad people around him. This just kind of finally made me say, OK, I give up. I'm gonna quit saying it makes sense, and that had been my defense mechanism just to make me feel better about my service, or maybe make me feel better about what I saw and what the sacrifices of so many may not include. I did what I wanted to do and and it made me feel good and that's why I did it. That's why I don't really care to go to ceremonies and have people honor me. I've never had a retirement ceremony. I just walked away because that's not why I was doing it. I didn’t really know at the time why it makes me so
emotional, but I can see it now if you care about all those kids over there putting their lives on the line.
I can tell you about one day in 2010 and it was the last Chapel service, and we had some guys blown up in Afghanistan. We cut both legs off one of the troopers and then sent him home. He survived, but we had one dead trooper, and his name was Specialist Crow. The next day at Chapel service, the Chaplin asked us to keep a Missouri National Guard soldier in your prayers. I was there with the unit from the Salt Lake City regiment. I asked him if he was talking about Specialist Crow that we lost last night, and he said “Yeah, he’s from Joplin MO.” Three days later it was on the front page of the Springfield News-Leader, “ Local Soldier Lost”. I always wanted to meet his family and I tried to look for them. Last year they named the Armory in Joplin after Specialist Crow. He was posthumously promoted and I went to that ceremony. I actually got to go say hello to his wife which was really cool. He was 42 and on his fourth deployment. He ran a minesweeper; basically he was out there trying to make the route safe for others. That happened 12 years ago, and she lost her husband. I just went up and told her that I want you to know that I was with him.
Blaine : How did she react to that?
Buckner : Well, she was very appreciative. I really just wanted her to know that he had good care. I told her that we had a top notch team and he got blown up right outside our gate and and that it was just a devastating injury. She asked the thing that both you and I have heard people in this situation ask. She asked if I thought that there was any pain. I told her that I did not think that he felt a thing or knew a thing. It was cool to be able to speak to her because I've tried multiple times to speak to families but in the early going we didn't even know people's names.
Blaine : Do you have any sons in the military?
Buckner: I do! My son John was in the Missouri Guard, but never deployed. He’s an ER doc. He works out of Oxnard and Camarillo hospitals in the LA area.


ASCENT DIRECT PRIMARY CARE, LLC
MATTHEW GREEN, DO H
Family Medicine
Mission Statement
Bringing physicians together to improve the health of our community.
Dermatology, Procedural
MICHAEL H. SWANN, MD H
BRETT NEILL, MD
MICHAEL KREMER, MD
JOHN CANGELOSI, MD
AUTUMN BERTHOLDI, PA-C
PATSY DUGGAN, PA-C
LORI MILLER, NP-C
HANNAH LEE, FNP-BC
BROOKLYN FORT, FNP-C
3850 S. National Ave, Suite 705 Spring eld, MO 65807 (Located inside Hulston Cancer Building-7th oor)
1240 E. Independence Spring eld, MO 65804
Phone: 417-888-0858 • Fax: 417-889-0476 www.swanndermatology.com
Hollister Location 590 Birch Rd, Ste 2c Hollister, MO 65672
PH. 417-690-3858 Fax 417-690-3862
Monett Satellite Location (Inside CoxHealth Urgent Care) 2200 E. Cleveland Ave Monett, MO 65708
Phone: 417-888-0858 • Fax: 417-889-0476
Lebanon Location 331 Hospital Drive Suite C Lebanon, MO 65536
Phone : 417-344-7200 Fax : 417-344-7299
To Advertise in this directory call Jean Harmison at the Society o ice: 417-887-1017.
Please Note: Changes to ads will be made quarterly and must be submitted in writing. H Denotes GCMS Membership “A” Denotes GCMS Applicant
GCMS Member Ad Rates: $10.00 per
Family Medicine
COXHEALTH
FAMILY MEDICINE RESIDENCY
FAMILY MEDICAL CARE CENTER
www.ascentdpc.com
417-595-0956
413 N McCroskey, Ste 2 Nixa, MO 65714
EYE SURGEONS OF SPRINGFIELD, INC.
C. BYRON FAULKNER, MD H Comprehensive Cataract Ophthalmology
JUDD L. McNAUGHTON, MD H Comprehensive Cataract Ophthalmology Diplomates, American Board of Ophthalmology
1330 E. Kingsley St. • Spring eld, MO 65804 Phone 417-887-1965 • Fax 417-887-6499 417eyecare.com
MATTAX • NEU • PRATER EYE CENTER
JAMES B. MATTAX, JR., MD, FACS H American Board of Ophthalmology
LEO T. NEU III, MD, FACS H American Board of Ophthalmology
DAVID NASRAZADANI, MD
DREW A. YOUNG, MD
THOMAS PRATER, MD, FACS H American Board of Ophthalmology
JACOB K. THOMAS, FACS, MD H American Board of Ophthalmology
BENJAMIN P. HADEN, MD H American Board of Ophthalmology
MICHAEL S. ENGLEMAN, OD
MARLA C. SMITH, OD
MATTHEW T. SMITH, OD
1265 E. Primrose Spring eld, MO 65804 417-886-3937 • 800-995-3180
3800 S National Ste 700 Springfield, MO 65807 (417) 269-8817
AMERICAN BOARDOF FAMILY MEDICINE
Marc Carrigan, MD
Cameron Crymes, MD
Kristin Crymes, DO
Kristen Glover, MD
Kyle Griffin, MD
Shelby Hahn, MD
Laura Isaacson, DO
Evan Johnson, MD
Katie Davenport-Kabonic, DO
Michael Kabonic, DO Jessica Standeford, MD
Gynecology
WOMAN’S CLINIC www.womansclinic.net
Leaders in Minimally Invasive Gynecology & Infertility
DONALD P. KRATZ, MD, FACOG H American Board of Obstetrics and Gynecology
AMY LINN, FNP-BC American Academy of Family Nurse Practitioners
VANESSA MCCONNELL, APRN, DNP, FNP-C 1135 E. Lakewood, Suite 112 Spring eld, MO 65810
Located inside Tri-Lakes Family Care 1065 Hwy 248 Branson, MO 65616
Phone 417-887-5500
Fax 883-8964 or toll free 877-966-2607
Monday-Thursday 8am-4:30pm Friday 8am-12pm
MERCY CLINIC–INTERNAL MEDICINE WHITESIDE
RAJ ANAND, MD
JAMES T. ROGERS, JR. MD, FACP H Board Certi ed in Internal Medicine
MARIA DELA ROSA, MD
NELSON DELA ROSA, MD
AMANDA MCALISTER, MD
ALEJANDRA ROA, MD
KELLY TRYGG, MD
GABBY BONNER, NP
STEVEN BOWLIN, MD Board Certi ed in Internal Medicine
STEPHANIE HOVE, NP
CARRIE KUGLER, PA
COURTNEY WEATHERFORD, PA
JENNIFER WHITE, PA
VICTOR GOMEZ, MD Board Certi ed in Internal Medicinee 2115 S. Fremont, Suite 2300 Spring eld, MO 65804
Phone 417-820-5600 Fax 417-820-5606
MERCY CLINIC UROLOGY (FREMONT)
ERIC P. GUILLIAMS, MD, FACS H American Board of Urology
ROBERT D. JOHNSON, MD, FACS H American Board of Urology
TYRUN K RICHARDSON, MD American Board of Urology
MARK J. WALTERSKIRCHEN, MD, FACS American Board of Urology
Phone 417-820-0300
Fax 417-882-9645
1965 S Fremont, Ste. 370 Spring eld, MO 65804
ADULT MEDICINE & ENDOCRINOLOGY
JONBEN D. SVOBODA, MD, FACE, ECNU
American Board of Endocrinology
JAMES T. BONUCCHI, DO, ECNU, FACE
American Board of Endocrinology
NICOLA W. GATHAIYA, MD, ECNU, FACE, CCD
American Board of Internal Medicine
American Board of Endocrinology
STEPHEN M. REEDER, MD, FACP
American Board of Internal Medicine
ANA MARCELLA RIVAS MEJIA, MD, CCD
American Board of Internal Medicine
American Board of Endocrinology
JACQUELINE L. COOK, FNP-BC, CDCES, CCD
KELLEY R. JENKINS, FNP-C, CDCES
ALINA CUMMINS, PA-C
STACY GHOLZ, FNP-C
SHELLEY L. CARTER, DNP
JESSICA A. CROUCH, FNP-C
Phone (417) 269-4450
960 E. Walnut Lawn, Suite 201 Springfield, MO 65807
Nephrology

SPRINGFIELD NEPHROLOGY ASSOCIATES, INC.
1911 South National, Suite 301 Spring eld, MO 65804
Phone 417-886-5000 • Fax 417-886-1100 www.spring eldnephrology.com
STEPHEN E. GARCIA, MD H
American Board of Internal Medicine
American Board of Nephrology
ETHAN T. HOERSCHGEN, MD
American Board of Internal Medicine
American Board of Nephrology
GISELLE D. KOHLER, MD H
American Board of Internal Medicine
American Board of Nephrology
DAVID L. SOMMERFIELD, MD
American Board of Internal Medicine
American Board of Nephrology
SUSAN A. WOODY, DO H
American Board of Internal Medicine
American Board of Nephrology
SPRINGFIELD
NEUROLOGICAL AND SPINE INSTITUTE
CoxHealth Jared Neuroscience
West Tower • 3801 S National, Ste 700 Spring eld, MO 65807 • 417-885-3888
Neurosurgery:
H. MARK CRABTREE, MD, FACS
EDWIN J. CUNNINGHAM, MD
MAYUR JAYARAO, MD
J. CHARLES MACE, MD, FACS H
CHAD J. MORGAN, MD
MICHAEL L. MUMERT, MD
SALIM RAHMAN, MD, FACS
ANGELA SPURGEON, DO
ROBERT STRANG, MD
Interventional Neuroradiology
MICHAEL J. WORKMAN, MD
Physiatry:
TED A. LENNARD, MD
KELLY OWN, MD
Physician Assistants:
JOSHUA BARBIERI, PA-C
MARK BROWN, PA-C
ERIC CHAVEZ, PA-C
BLAKE MARTIN, PA-C
HEATHER TACKETT, PA-C
Nurse Practitioner:
EMILY CROUSE, NP-C
BILL HAMPTON, ANP-BC
ROZLYN MCTEER, FNP
BRANDON RUBLE, ACNP-AG
ALYSSA CHASTAIN, FNP
Obstetrics/Gynecology
PRIMROSE OB/GYN
MARCUS D. MCCORCLE, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
THOMAS M. SHULTZ, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
GREGORY S. STAMPS, MD, FACOG
Diplomate, American Board of Obstetrics and Gynecology
P. MICHAEL KIDDER, DO, FACOOG
Diplomate, American Osteopathic Board of Obstetrics & Gynecology
Phone 882-6900
1000 E. Primrose • Suite 270 Spring eld, MO 65807
SPRINGFIELD OB/GYN, LLC
MATTHEW H. TING, MD, FACOG H
American Board of Obstetrics & Gynecology 909 E. Montclair, Suite 120 Spring eld, MO 65807
Phone 417/882-4466 • Fax 417/890-5631
ONCOLOGYHEMATOLOGY
ASSOCIATES OF SPRINGFIELD, MD, P.C.
WILLIAM F. CUNNINGHAM, MD, FACP
American Board of Internal Medicine
American Board of Medical Oncology
JIANTAO DING, MD H
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
ROBERT J. ELLIS, MD, FACP
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
BROOKE GILLETT, DO
American Board of Internal Medicine
American Board of Medical Oncology
V. ROGER HOLDEN, MD, PhD
American Board of Hematology
American Board of Medical Oncology
DUSHYANT VERMA, MD, FACP
American Board of Internal Medicine
American Board of Hematology
American Board of Medical Oncology
Springfield Clinic 3850 S. National, Ste. 600 Spring eld, Missouri 65807
Monett Clinic 802 US Hwy 60 Monett, Missouri 65708
Phone 882-4880
Fax 882-7843
Visit our website: www.ohaclinic.com
MERCY CLINIC–EAR, NOSE & THROAT
BENJAMIN L. HODNETT, MD, PHD H
ERICH D. MERTENSMEYER, DO, FAOCOO
AARON R. MORRISON, MD
A. DANIEL PINHEIRO, MD, PhD, FACS H
RAJEEV MASSON, MD
MARK J. VAN ESS, DO, FAOCOO
Diplomates, American Board of Otolaryngology
SHELBY BRITT, PA
MELISSA COONS, FNP
TAHRA LOCK, NP
ELIZABETH (BETSY) MULLINGS, FNP
PAUL STRECKER, FNP Audiology
JASON BOX, AuD, CCC-A
MAMIE JAYCOX, AuD, CCC-A
JENNIFER PLOCH, AUD
ALLISON WHITE, AUD, CCC-A
Phone 417-820-5750
Fax 417-820-5066
1229 E. Seminole, Ste. 520 Spring eld, MO 65804
MERCY CLINIC–FACIAL PLASTIC SURGERY
MATTHEW A. KIENSTRA, MD, FACS American Board of Facial Plastic & Reconstructive Surgery American Board of Otolaryngology
Phone 417-887-3223
1965 S. Fremont, Ste. 120 Spring eld, MO 65804 facialplasticsurgeon.com
JAMES E. BRIGHT, MD H Diplomate, American Board of Psychiatry & Neurology.
Practice Limited to: Adult Psychiatry
Phone 882-9002
1736 E. Sunshine, Ste. 400 Spring eld, MO 65804

At Arvest we understand how valuable your time is. Our Private Bankers proudly serve our local medical community with dedicated financial expertise. Let an experienced Private Banker coordinate your full financial picture, including your business needs. With specially tailored services, we’re here to take tasks o your plate & make every life stage easier.
Call us today to learn more.
CHANGE SERVICE REQUESTED