










Welcome to the new stylized Sight + Sound! It was time for an update, particularly one that reflects the changes in the Departments of Ophthalmology and Otolaryngology-Head & Neck Surgery at the University of Pittsburgh. The newsletter will also have additional pages and more photos.
The purpose of the Sight + Sound newsletter is to inform you, our readers, of the advancements in care that take place in the Departments of Ophthalmology and Otolaryngology-Head & Neck Surgery. However, we realize that there is far more than “sight and sound” advancements that take place in these two Departments. So, our newsletter has grown and is divided into sections to help you navigate to what is of most importance to you.
I am excited about this version of our newsletter. Thank you for reading; I hope you enjoy it!
Keep in touch,

Lawton Snyder Chief Executive Officer

Progress was made at the 13th annual Louis J. Fox Center for Vision Restoration Conference at the Vision Institute at UPMC Mercy Pavilion
The 13th annual Louis J. Fox Center for Vision Restoration Conference was held at the Vision Institute at UPMC Mercy Pavilion October 8-9, 2024. For the first time, the pathways towards clinical trials were discussed in terms of what to consider in getting research ready for that stage. While there is still a way to go, this illustrates the progress being made.
The meeting was organized by University of Pittsburgh faculty members Takaaki Kuwajima, PhD; Kun-Che Chang, PhD; Issam Al diri, PhD; Larry Benowitz, PhD; and John Ash, PhD. It attracted well over 80 attendees that included scientists, students, postdocs, ophthalmologists, and philanthropists.
For two full-days, cutting-edge research was presented on optic nerve preservation and regeneration. The conference featured an outstanding keynote presentation by Zhigang
He from Harvard Medical School and Boston Children’s Hospital. There were an additional 25 speakers who are world leaders in the field who came from prestigious institutions, including Harvard, Stanford, the University of Pennsylvania, Washington University, Johns Hopkins Hospital, the Wilmer Eye Institute, UCSF, and the University of Pittsburgh.
“This conference is getting even better every year,” said José-Alain Sahel, Director of the Vision Institute and Chair, Department of Ophthalmology. “It was clear that major progress has been made in developing therapies to regenerate the optic nerve. This year, new transformative science from related but different fields was shared. The partnership with the Gilbert Family Foundation, BrightFocus, the Glaucoma Foundation, and the hope to start of the upcoming ARPA-H program hold immense promise.”
continued on next page
Exciting new research was presented on developing new gene and stem-cell therapies to promote ganglion cell survival and regeneration of damaged axons. Multiple new approaches were presented. For the first time, researchers showed promising results of axon regeneration from the damaged nerve to the brain with modest vision restoration in preclinical models. Also, for the first time, clinical trial data was presented for gene therapies to treat optic neuropathies, and additional speakers discussed strategies to overcome barriers to developing new clinical trials.
In his concluding comments, Dr. Benowitz said, “We’re in a very, very exciting era, and thanks to the work of people in this room, I think the future is looking sunnier.” Interviews with additional attendees included similar praise for the meeting and optimism for the field.
“[All the speakers] say this has become one of the more important meetings each year for the field, because it’s very focused on optic nerve regeneration alone,” said Lawton Snyder, Eye & Ear Foundation CEO.
Leonard Levin viewed the conference as a chance to catch up in the field he’s part of. It was also an opportunity to see where the leaders – many of whom are friends – are at. “We’re getting the cutting-edge work told to us, even before it’s published in many cases,” he said. He described the community as close, because they all have the same goal to restore vision.
“A big theme from the two-day conference was that advancements have been made in all areas,” said Lawton Snyder, Eye & Ear Foundation CEO. “As Larry Benowitz (CoDirector of the Fox Center) stated in his remarks, ‘The work 20 years ago when this all started looks very different than it does
today.’” This includes multiple modalities having a profound impact on optic nerve regeneration.
Jeff Gross said this conference and past Fox Center conferences have really pushed the field forward. He praised the synergy that occurs in bringing everyone together, saying so much more progress comes after the meeting as a result.
In a conversation with Snyder, Louis J. Fox said he and José-Alain Sahel, MD, Chair of the Department of Ophthalmology, have a similar view. They do not like the word no. He said the researchers and clinicians come self-motivated. It is not about the money or fame; it is about the idea of getting the job done. Everyone is working toward the same goal.
“It’s exciting to see new and unpublished work showing promising discoveries in optic nerve regeneration,” Dr. Ash said. “While there is still a long way to go, research presented at the meeting demonstrated significant progress in the field. Every year, we are getting closer to restoring functional vision to patients with optic nerve injury.”
“We’re in a very, very exciting era, and thanks to the work of people in this room, I think the future is looking sunnier.”
Larry Benowitz, PhD
Gracilis free muscle transfer study allows for more informed clinical decisions on how to achieve the best possible smile outcome
For patients with long-standing facial paralysis (greater than two years’ duration), the only option for restoring the ability to smile is with a procedure known as a “gracilis free muscle transfer.” However, a small subset of patients go on to develop “resting oral commissure lateralization.” This is when the corner of the mouth is pulled unnaturally at rest, which can be unsightly and distressing for the patient. The risk factors for this phenomenon are poorly understood.
Dr. Christina M. Yver, MD, MBA, Assistant Professor of Otolaryngology-Head & Neck Surgery and Director of the UPMC Facial Nerve Center is one of three authors on a study published in the August 2024 issue of Plastic and Reconstructive Surgery, a peerreviewed medical journal that is the official publication of the American Society of Plastic Surgeons. The article is titled, “Muscle foreshortening after free gracilis transfer for smile: Where, when, why?”
Gracilis free muscle transfer involves borrowing a small slip of muscle from the inner thigh and transplanting it into the face to replicate the function of
smile muscles. In order for it to be successful, the transplanted muscle has to be hooked up to a blood supply as well as a donor nerve in the face. This allows the muscle to contract, creating a smile.
“Our study is the first of its kind to review over 400 patients who underwent gracilis free muscle transfer, identify those with subsequent oral commissure lateralization, and examine various potential risk factors for this phenomenon,”
Dr. Yver said. “We found that the choice of donor nerve used to activate the muscle seems to be the biggest risk factor for oral commissure lateralization, with more robust donor nerves resulting in greater risk.”
Other risk factors include a history of radiation to the face or concurrent use of fascia lata to help support the face at rest.
“A better understanding of these risk factors will allow us to better counsel patients pre-operatively, and to make more informed clinical decisions on how to achieve the best possible smile outcome while minimizing the risk of oral commissure lateralization postoperatively,” Dr. Yver said.
To make an appointment with Dr. Yver, call 412-621-0123.


Dr. Christina M. Yver, MD, MBA, Assistant Professor of Otolaryngology-Head & Neck Surgery and Director of the UPMC Facial Nerve Center. Dr. Yver’s study was published in the August 2024 issue of Plastic and Reconstructive Surgery.
Ernest G. Salvitti left quite a legacy. Now it will be memorialized in the Department of Ophthalmology by his son, E. Ronald Salvitti M.D., funding a Chair in his father’s name.
The elder Salvitti was a coal miner who worked very hard at many odd jobs. When the coal mine closed, he worked as a mechanic at a gas station where he fixed cars and pumped gas. Eventually, he made an offer to the owner and bought the business. He continued to work tirelessly all hours of the day and sometimes the night.
Dr. Salvitti described his father as being energetic, a hard worker, entrepreneurial, and extremely friendly – the kind of person who would do anything for anybody.
“These are qualities which I would also attribute to Dr. Salvitti,” said Lawton Snyder, Eye & Ear Foundation CEO.
If somebody required something, Ernest was there to help. If someone needed their car the next day to go to work, he worked until the problem was solved. He was one of those people who built a lot of very good relationships and friendships over the years.
Ernest worked as long as he could, until the very end. He died at 72 from complications associated with leukemia.

Dr. Salvitti and his brother were the first in their family to graduate from high school and college; neither of their parents did. Dr. Salvitti was motivated to go into ophthalmology because of his father, who had vision loss associated with achromatopsia. He had no color vision and was extremely sensitive to light.
This is the third Chair Dr. Salvitti has funded. The first was in his name because of his interest in treating and solving problems associated with macular degeneration. The second Chair was named after his daughter Jennifer, who is also a graduate of Pitt’s Ophthalmology residency program. She is the managing physician of the practice and surgery center Dr. Salvitti started in 1973.
Dr. José-Alain Sahel, Chair of the Department of Ophthalmology, suggested that Dr. Salvitti name the third chair after his father. He and Snyder knew the story and how special it was. When Snyder asked about Ernest and why he was an inspiration in terms of putting his name on the chair, Dr. Salvitti answered very quickly and clearly, “His work ethic, in spite of his visual disability.”

Dr. Salvitti credits that tireless work ethic for his accomplishments and success. When he graduated, he started a family practice and continued with it until he decided to follow his initial ambition to become an ophthalmologist. During his last year in residency, he had the opportunity to be introduced to phacoemulsification design under the direction of Dr. Charles Kelman. The surgery was new and in development at the time; it is now the gold standard. Dr. Salvitti became a recognized leader and innovator in the field of phacoemulsification.
He now honors his father with the Ernest G. Salvitti Chair in Ophthalmology Research. He has also motivated others to be philanthropic.
A medical device disguised as a sippy cup promises to revolutionize treatment for a common childhood ailment. Called the EarFlo, it is on track for approval by mid-2025.
Otitis media with effusion (OME) is one of the most frequent infectious diseases in children, according to the National Institutes of Health. Between 80 and 90 percent of all children will have it before school age, and between 30-40 percent have recurrent episodes. It is also the most common cause of acquired hearing loss in childhood. OME typically occurs when fluid builds in the middle ear and Eustachian tube. Ear tube surgery is a regular procedure used to treat OME.
With all this in mind, a group including Peter Santa Maria, MD, PhD, Vice Chair of Clinical and Translational Research, Chief, Division of Otology/Neurotology, Director of Faculty Innovation, Office of Innovation and Entrepreneurship, and Director, SPARK Global; Matthew Oldakowski (an engineer in Australia); and Jozef Bartunek (a cardiologist from Belgium) conceived of the EarFlo concept using the Biodesign process. Training to be Global Biodesign Fellows, Oldakowski and Bartunek spent time observing problems in the clinic and saw children having ear tube surgery as a large unmet medical need.
First, the group spent time defining the inner medical need. They had to understand the background on why the problem occurs, weaknesses with existing treatments, and how stakeholders influence the problem.
Next, they created a roadmap before entering an ideation phase where multiple concepts were generated. Various levels of prototypes were made, with each iteration an improvement. From idea to early prototype was about three to four months.
Two studies on the EarFlo device have now been completed. The first study involved children who came in for a consultation about tube surgery for OME. They were taken aside at the doctor’s office and given the EarFlo. After only one session, 70 percent of children saw improvement.


Earflo is designed to give immediate relief and may provide long-lasting benefits to children suffering from chronic ear infections
The second study allowed the children to take home the device. After using the device for four weeks, they received a follow up four weeks later. Only around 10 percent of children were eventually booked for surgery. “These early results suggest the EarFlo is an alternative method that can avoid surgery,” Dr. Santa Maria said.
Now the group is in the final stages of making minor changes to the device before submitting it for regulatory approval. After that, they will look to launch to the public. They are hoping to keep the price below $200, which will be a huge savings if considering the costs of surgery and inconvenience to the family. To make it available as soon as possible, it will first be available as a consumer medical device outside of insurance. Hopefully over time as it continues to show benefit, insurance will help cover it.
The EarFlo has other potential applications. “Not only can it be used for children, but it effectively works in adults, so our next levels of testing and design will be focused on adults,” Dr. Santa Maria said. “These not only include ear infections but those who have Eustachian Tube dysfunction and have difficulty flying, for example.”

The Eye & Ear Foundation is happy to announce this year’s recipients of the Wiegand Fellowship and the Wiegand Entrepreneurial Research Award. The Wiegand Fellowship was established in the Department of Ophthalmology to support research being done on advancing imaging of the eye.
The Wiegand Entrepreneurial Research Award was created to help support research in the Department of Ophthalmology or Otolaryngology-Head & Neck Surgery for projects that show great promise for commercialization. These funds were made possible by generous philanthropic support from Mr. and Mrs. Bruce and Barbara Wiegand.

Dr. Susannah Waxman is a Postdoctoral Researcher in the University of Pittsburgh’s Department of Ophthalmology. She completed her PhD in Cellular and Molecular Pathology in Dr. Ian Sigal’s Laboratory of Ocular Biomechanics. After she earned her bachelor’s degree at Ohio Wesleyan University, she worked as a laboratory manager in Dr. Nils Loewen’s Laboratory for Aqueous Humor Outflow Tract Engineering. Her current research is focused on the role of astrocytes in glaucoma.
In her project, Dr. Waxman will investigate how astrocytes in the human lamina cribrosa respond to increased eye pressure. Using specialized visualization techniques, she will characterize changes in astrocyte structure during the initial stages of elevated pressure and map the corresponding changes in astrocyte gene expression. By uncovering these early changes in the human eye, her goal is to shed light on the mechanisms behind the initiation of optic nerve damage in glaucoma patients. Through learning how astrocytes react to the early stages of high eye pressure, she aims to inform new ways to detect and treat early-stage changes that can otherwise lead to irreversible blindness, ultimately helping to protect vision.

Dr. Xing Chen is an Assistant Professor in the University of Pittsburgh’s Department of Ophthalmology. Dr Chen specializes in brain-computer interfaces, visual neuroscience, blindness, and chronic recording and microstimulation in nonhuman primates. She obtained her bachelors in Neuroscience at the University of Southern California, her PhD in Neuroscience at Newcastle University in 2014, and carried out her postdoctoral work at the Netherlands Institute for Neuroscience before joining Pitt in 2022.
The Chen lab is working to restore lost vision through a neuroprosthesis that bypasses the eyes by interfacing directly with the brain. Key features of this device include ultra-flexible probes with high-channel-count and high-density electrodes yielding higher image resolution, extensive coverage of the visual field, and longterm durability. The goal is to allow blind people to recognize objects and navigate more independently. In addition, the device opens new horizons for more accurate and localized neuromodulation therapies to treat diseases ranging from epilepsy to movement disorders.

Rob Shanks is an Associate Professor in the University of Pittsburgh’s Department of Ophthalmology. He completed a PhD in Molecular and Microbiology at Tufts University Medical School, and a postdoctoral fellowship at the Dartmouth Medical School. He is Director of the Charles T. Campbell Laboratory of Ophthalmic Microbiology. His research focuses on basic and translational projects regarding ocular infections and inflammation.
Dr. Shanks’ project is geared towards improving drug delivery to the surface of the eye. His lab’s solution is to apply “anchors” to biologics to allow them to stay on the ocular surface for a longer time. This study will extend the capability of the anchoring technology using another class of biologics, the growth factors. He proposes that anchored growth factors can be used to help treat nerve related diseases and wound healing problems of the ocular surface. Success of this project will help propel the approach of using anchors as a platform for the biologic class of drugs to be used on the ocular surface and help restore a good quality of life to patients with ocular surface diseases.


One of the byproducts of the war in Ukraine is that that its ENT community is at risk for becoming increasingly isolated in the academic world. Travel to conferences, networking, and financial support for Continuing Medical Education (CME) have become more challenging.
But an exciting collaboration between the Department of Otolaryngology-Head & Neck Surgery and the ENT community in Ukraine is providing them much needed educational support.
It all started years ago when Eugene N. Myers, MD, FACS, FRCS, Edin (Hon), Emeritus Distinguished Professor and Chairman, Department of Otolaryngology-Head and Neck Surgery and Director, International Visiting Scholars Program, visited Ukraine with his late wife so she could see where her mother emigrated from. During their time in Kiev, they visited the Department of Otolaryngology in the Academy of Medical Sciences of Ukraine. Faculty member Professor Svetlana Yaremchuk was assigned to give them a tour since she spoke perfect English.
In the ensuing years, as Drs. Myers and Yaremchuk got to know one another, Dr. Myers invited her to visit the Department to be exposed to some of the latest developments in their specialty. About seven years ago, she was an international visiting scholar in the Sleep Division for one month, working with Dr. Ryan Soose, Associate Professor and Chief, Sleep Division.
Dr. Yaremchuk returned to the Department several times for refresher courses with Dr. Soose. Meanwhile, Dr. Myers kept in touch with her by phone. During one of their conversations, Dr. Myers realized that the ENT doctors in Ukraine were preoccupied with taking care of war injuries, leaving them no time to learn anything new. Going out of
the country to meetings was also forbidden. “I suggested that if they were interested, our Department could organize a teaching course via Zoom,” Dr. Myers recalled. “She was very receptive, so the collaboration was born.”
Since Dr. Soose had a close working relationship with Dr. Yaremchuk, Dr. Myers asked him to take on leadership of the project. A June 2024 letter from the Department addressed to their “Ukrainian otolaryngology colleagues” expressed support and offered resources, including three virtual lectures from subspecialty experts. Faculty were available live on July 3 and via email anytime for questions, clinical advice, and ongoing discussion.
Following that, a CME event organized by Drs. Soose and Yaremchuk originally scheduled for July 3 had to be postponed due to increased bombings and power outages. Rescheduled for September 4, the three-hour event consisted of three lectures delivered by Pitt faculty and produced by the Eye & Ear Foundation. Lectures were translated into Ukrainian language and shown live. More than 50 doctors attended in person and over 400 participated online. Dr. Yaremchuk said the presentations were “met with great enthusiasm, generating many questions and fostering a lively discussion.”
“We hope this serves as a springboard for future collaborations and support – both in-person and virtual,” Dr. Soose said.
“This collaboration is very important to us,” Dr. Yaremchuk said. Direct communication with American colleagues helps fill the gap in being unable to gain new knowledge and improve qualifications, she added.
“I’m so happy that we could provide support for them during these trying times,” Dr. Myers said.

i2Eye, the sixth annual interdisciplinary conference on innovative imaging of eye diseases, was held in September at the UPMC Vision Institute. Around 165 people from all over the world attended the three-day event, with 40 from France.
Speakers and attendees were a mix of physicists, biologists, and ophthalmologists. This year’s conference experimented with broadening the scope to include more biological and neuroscience topics, as well as more industry participation and professional development programming for trainees.
In his introductory message, Department Chair José-Alain Sahel said, “We are thrilled to host the i2Eye conference at the Vision Institute of Pittsburgh. This conference was started six years ago by Kate Grieve, Michel Paques and Ethan Rossi and has become an annual event bringing together a growing community of researchers around innovative imaging of eye diseases and now many other areas of vision science.”
Topics included innovative imaging technologies for structural imaging of the anterior segment and retina, functional retinal imaging, ocular immunology and inflammation, eye movements, age-related macular degeneration, glaucoma, animal models, organoids and novel vision restoration therapies such as optogenetics. Scientific sessions consisted of invited and
submitted talks grouped by topic followed by lengthy discussions. These discussion sessions are a unique aspect of the i2eye format, where “we aim to bridge between disciplines for fruitful discussions on how to move our interrelated fields of investigation forward together,” the conference website stated.
Additional programming included a poster session, roundtable discussion with industry, handson demonstrations of innovative imaging technologies, Vision Institute laboratory tours, and professional development activities for trainees.
On-site and online registration was free of charge to all invited speakers and attendees working in academia or at nonprofit institutions. Online participants were able to join virtually for certain sessions.
Dr. Sahel said one of the key strengths of the conference was the people. “The ability to bring together people from the U.S. and Paris and so many important researchers from all the countries [means that there is] lots of expertise,” he said. “They wish to work together and bridge the gaps and knowledge and provide better care for our patients.”

Director of the IHU FOReSIGHT, Christophe Baudouin, expressed how important it is to continue the strong relationship between Paris and Pittsburgh, which means meeting repeatedly in both countries. He lauded the fascinating achievements in imaging. “Innovation in terms of imaging right now and potential application in the future has been absolutely amazing,” he said.
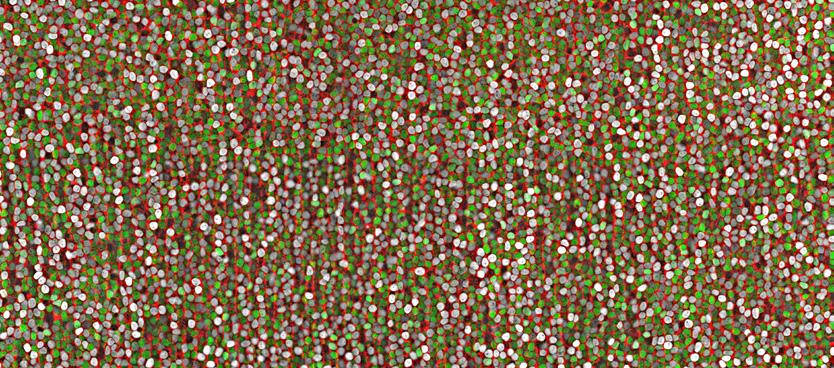
THE VISION INSTITUTE SCIENTIFIC IMAGE WINNER (JUDGES SELECTION) Ian Sigal, PhD

The UPMC Voice and Airway Center is bolstering and expanding its care for the performing arts community in Pittsburgh. This is largely due to the addition of Chloe Santa Maria, MD, MPH, Assistant Professor, Department of Otolaryngology-Head & Neck Surgery.
Dr. Santa Maria came to Pittsburgh following a laryngology fellowship at the USC Voice Center at Keck School of Medicine under the guidance of Dr. Michael Johns III, who is renowned for professional voice care within laryngology. Los Angeles is a hub for professional voice users and singers, so they were privileged to care for a lot of these patients. During her time there, they undertook a formal care relationship with the L.A. Opera, focusing on their new singers. This involved an annual vocal care education session and targeted care for each new singer. It has been a huge success.
After her L.A. fellowship, she joined UPMC because of how dynamic and energizing the team and Department felt. “It is a place where you have an idea and they do everything to support you and make it happen,” she said. “They are driven by providing excellent care and were really excited about my ideas of reforging relationships with the Pittsburgh Opera, the Civic Light Opera, and ultimately expanding this to include musical theatre and Broadway.”

“It really helped me to understand the nuances and the language required for taking care of these patients,” Dr. Santa Maria said. “Looking after celebrities is of course a fun little side part of that, but honestly, what it really hit home is that great quality voice care should be the same for all patients.”
Dr. Santa Maria was drawn to laryngology (care for the voice) very early on because of her love of singing and music. Her family is very musical, and she calls herself a very enthusiastic (and also very amateur) singer. When she discovered she could have a career in medicine that was based around this, she was hooked.
The Department has already started with the Pittsburgh Opera, which has been welcoming. The UPMC Voice and Airway Center plans to be the formal vocal health care team for the singers at the Opera. As of now, they will see any of their sick performers within 24 hours. They are in the process of developing a vocal health education day and targeted care program for their new intake of singers, like L.A.
“The hope is that we provide excellent acute care for singers in need, and that can help with reducing injury and stress for both the patient and the opera team,” Dr. Santa Maria said. “By engaging the newer singers early, we also hope to really encourage healthy vocal habits in a group of people who are very attuned to their vocal needs.”
Dr. Santa Maria is looking forward to collaborating with the rich cultural community in Pittsburgh and said the relationship so far has been very rewarding. This arts lover appreciates the joy in music in singing, and how it can evoke many emotions. “It also has the power to unite people,” she said. “Having a job where I get to be a part of that and taking care of people is an absolute privilege.”
eyeandear.org
412.864.1300 O
412.864.1305 F

If you no longer wish to receive our newsletter, please submit requests to our mailing address, or email optout@eyeandear.org
The official registration and financial information of the Eye & Ear Foundation may be obtained from the Pennsylvania Department of State by calling toll free, within Pennsylvania, 1-800-732-0999. Registration does not imply endorsement.
The Eye & Ear Foundation of Pittsburgh is a nonprofit 501 (C)(3) organization. Our mission is to support the research and academic efforts of the Departments of Ophthalmology and Otolaryngology-Head & Neck Surgery at the University of Pittsburgh. Donations to support our research initiatives can be made online at eyeandear.org or by returning the enclosed envelope. For more information on the Foundation, our research, or the articles in this newsletter, please contact Katherine Troy, Director of Operations, at katherine@eyeandear.org or 412-864-1300.
Medical Disclaimer: The Eye & Ear foundation does not assume any responsibility or risk for the use of any
risk. All information and content found in this newsletter were
or

with
We encourage you to view our full disclaimer by visiting the eyeandear.org website.
and Advancement of
Excellence for Research and Advancement of Care in Ophthalmology
Excellence for Research and Advancement of Care in Ophthalmology

E mily Y. Chew , MD
Excellence for Innovation and Service in Ophthalmology
Excellence for Innovation and Service in Ophthalmology

E mily Y. Chew , MD
E mily Y. Chew , MD
E mily Y. Chew , MD
NIH Distinguished Investigator
NIH Distinguished Investigator Director, Division of Epidemiology and Clinical Applications
Andrew W. Eller , MD
Andrew W. Eller , MD
Andrew W. Eller , MD
Andrew W. Eller , MD
NIH Distinguished Investigator Director, Division of Epidemiology and Clinical Applications
NIH Distinguished Investigator Director, Division of Epidemiology and Clinical Applications
Director, Division of Epidemiology and Clinical Applications
National Eye Institute, National Institutes of Health Chief of the Clinical Trials Branch
Professor of Ophthalmology
Professor of Ophthalmology
Professor of Ophthalmology
Professor of Ophthalmology
Director, Retina and Vitreous Services
Director, Retina and Vitreous Services
Director, Retina and Vitreous Services
Director, Retina and Vitreous Services
Director, Retina and Vitreous Fellowship
Director, Retina and Vitreous Fellowship
Director, Retina and Vitreous Fellowship
Director, Retina and Vitreous Fellowship
National Eye Institute, National Institutes of Health
National Eye Institute, National Institutes of Health
National Eye Institute, National Institutes of Health
Director, Ocular Trauma Service
Director, Ocular Trauma Service
Director, Ocular Trauma Service
Director, Ocular Trauma Service
Chief of the Clinical Trials Branch
Chief of the Clinical Trials Branch
Chief of the Clinical Trials Branch
University of Pittsburgh School of Medicine
University of Pittsburgh School of Medicine Save the date November 21, 2024
University of Pittsburgh School of Medicine
University of Pittsburgh School of Medicine
Save the date November 21, 2024