
LEADING INNOVATION IN OTOLARYNGOLOGYHEAD & NECK SURGERY
FISCAL YEAR 2025 ANNUAL REPORT




FISCAL YEAR 2025 ANNUAL REPORT


It is a tremendous privilege to share the work of the Department of Otolaryngology-Head & Neck Surgery at the University of Pittsburgh and to highlight the remarkable advances that we have made in our fight against head and neck cancer, hearing loss, and other related otolaryngologic conditions. This has been a year of continued clinical and research growth for the Department. We have two new faculty joining the Department: Steven Chinn, MD, specializing in head and neck surgical oncology and microvascular reconstructive surgery, and Joshua Smith, MD with a research focus on unraveling mechanisms of tumor immune evasion and discovery of translational biomarkers of response to immunotherapies. With the support of the Eye & Ear Foundation, we have successfully recruited some of the best surgeons and scientists from across the United States to Pittsburgh. Our recruitment reflects key priorities for the Department, including providing world-class clinical care and conducting groundbreaking translational research. The success of the Department is being recognized. This year, we had a significant improvement in our U.S. News & World Report rankings, from #44 to #19 in the nation. Some highlights from the past year include:
Several new faculty have helped us to further establish the University of Pittsburgh as an international leader in the treatment and research of hearing loss. Peter Santa Maria, MD, PhD, our new Chief of Otology/ Neurotology and Vice Chair for Clinical and Translational Research, has already been busy in the operating room and the clinic. His laboratory, focused on understanding hearing loss in otitis media, has successfully transitioned from Stanford to Pittsburgh. We look forward to many new discoveries. We also welcomed Gregory Basura, MD, PhD, and Adele Moatti, PhD, to the team. Dr. Basura is an experienced neurotologist and scientist who runs a research program focused on cognitive pathways in hearing loss and tinnitus and is leading our Global Otolaryngology efforts. Dr. Moatti joins us from UNC and North Carolina State. Her laboratory explores drug delivery methods for the inner ear using nanoparticles and extracellular vesicles.
Under the leadership of Matthew Spector, MD, FACS, our head and neck surgical oncology and microvascular reconstructive surgery program has ascended to one of the busiest and best in the United States. Steven Chinn, MD and Joshua Smith, MD join the Department as surgeon

José P. Zevallos, MD, MPH, FACS

Deputy Director, UPMC Hillman Cancer Center #19
U.S. News & World Report rankings, up from #44 to #19 in the nation.

With the support of the Eye & Ear Foundation, we have successfully recruited some of the best surgeons and scientists from across the United States to Pittsburgh.
José P. Zevallos, MD, MPH, FACS
The Eugene N. Myers, MD Professor and Chair Department of Otolaryngology-Head & Neck Surgery
The University of Pittsburgh School of Medicine
scientists and will focus on translational research in head and neck cancer.
Dr. Zevallos runs an NIH-funded translational research laboratory at UPMC Hillman Cancer Center focused on understanding the molecular basis for poor outcomes in head and neck squamous cell carcinoma. Most recently, his group pioneered the development of novel liquid biopsy approaches to measuring minimal residual disease after head and neck cancer surgery.
Along with Marci Nilsen, PhD, RN, and with support from the Eye & Ear Foundation, we are embarking on a new program to measure and manage functional outcomes in patients undergoing complex head and neck surgery and reconstruction. Our 2025-2026 head and neck surgical oncology fellowship match reflects the caliber of the program and our standing in the field. In July 2025, we will welcome a class of fellows from Stanford University, Mayo Clinic, and the University of Minnesota.
With the retirement of Grant Gillman, MD, in July, Christina Yver, MD, MBA, our Director of the Facial Nerve Center, will bring these two centers together to offer comprehensive services. We are proud to expand our program to ensure our patients benefit from the latest advances in care for both flaccid paralysis and facial synkinesis. Our patients with facial paralysis benefit from the expertise of our facial nerve-dedicated physical therapy group under the leadership of Amy Cassidy, PT and Darcy Bonaventura, PT, as well as the entire spectrum of surgical interventions including selective myectomy, selective neurectomy, nerve transfers, nerve grafting, and gracilis free muscle transfer.
Helmed by Libby Smith, DO, FAOCO, the Center is proving itself as the go-to for local singing communities, making sure they are available for help as needed. Chloe Santa Maria, MD, MPH, joined the Department having just completed a highly competitive laryngology fellowship in Los Angeles; she brings innovative new techniques to our laryngology division. As an expert in the management of the professional voice, she has been the lead on collaborating with resident artists in the Pittsburgh Opera in the Vocal Injury Prevention (VIP) Program. Many people find dysphagia difficult to treat, but Sandra Stinnett, MD, laryngologist and Director of the UPMC Swallowing Disorders Center, is trying to change that.








We have revitalized the Department of OtolaryngologyHead & Neck Surgery Pittsburgh CREATES program. With support from the Eye & Ear Foundation and the University of Pittsburgh Innovation Institute, we hired Mohit Singhala, PhD, as Executive Director of CREATES. Dr. Singhala is a robotics engineer from Johns Hopkins and a former Stanford Biodesign Fellow who will help establish CREATES as a center for surgical innovation and entrepreneurship. The Department has kickstarted a surgeon-innovator fellowship with a cohort of four faculty members and surgical trainees.
We seek to provide an inclusive learning environment with an unparalleled depth and breadth of exposure to all aspects of otolaryngology. The fundamental principle of the program is that resident responsibility is allocated gradually throughout the five-year program, commensurate with the resident’s abilities and maturity. Our program continues to thrive; we welcomed an exceptional class of interns from the University of Pittsburgh (x2), the University of Pennsylvania, Washington University School of Medicine, and UT Southwestern. This year, the residency program was ranked #13 in the United States by Doximity.
The Department of Otolaryngology-Head & Neck Surgery has expanded its global outreach, thanks to the addition of Gregory J. Basura, MD, PhD. His leadership in this area—in which he has worked to develop sustainable educational and clinical initiatives in underserved nations—continues with his Departmental position as Director of Global Outreach. Dr. Basura helped launch the first otology fellowship established in Africa in 2022. He is continuing his involvement in the program, which is about to graduate its third fellow. He is also overseeing the International Visiting Scholars Program, started by Eugene Myers, MD, FACS, FRCS, Emeritus Distinguished Professor and Department Chairman. Other current global efforts include building long-term medical educational partnerships with Mozambique and Peru through expanding resident rotations to include these two countries.
The Eye & Ear Foundation of Pittsburgh is the engine that drives our clinical and research success in the Department of Otolaryngology-Head & Neck Surgery. The work of the Department is far from over as we take on even bigger challenges to improve the lives of patients facing head and neck cancer, hearing loss, tinnitus, and many other conditions that severely impact quality of life. We are very grateful to our friends and donors in Pittsburgh and across the United States for their continued support and look forward to another exciting year of discovery ahead.
DEPARTMENT

Divisions
104,896 Visits
38,303 Patients
14,251 Procedures
4 MD Fellows
60 Faculty
25 Residents
44 States
6 Clinical SLP Fellows
73 Clinical Providers

The Division of Head and Neck Surgical Oncology and Microvascular Reconstruction is part of the worldrenowned head and neck oncology program at the UPMC Hillman Cancer Center. The vision of this program is to provide exceptional multidisciplinary care to patients with head and neck cancer, accelerate finding a cure through innovative translational research, develop and refine reconstructive techniques to maximize function outcomes, and mitigate treatment-related toxicities and improve survivorship.
The translational research program, which is anchored by the UPMC Hillman Cancer Center SPORE (Specialized Program of Research Excellence) in Head and Neck Cancer grant, has been one of the leading programs in the world for decades. Heath Skinner, MD, PhD, Chair of the Department of Radiation Oncology & Medical Director of Radiation Oncology Clinical Networks, and José P. Zevallos, MD, MPH, FACS, the Eugene N. Myers, MD Professor and Chair of the Department, and Deputy Director of UPMC Hillman Cancer Center, co-lead this, which provides the basic infrastructure for tissue collection, biobanking, and clinical trials. Two additional surgeon scientists, Joshua Smith, MD, and Steven Chinn, MD, have recently been recruited and will focus on translational research in head and neck cancer. Dr. Smith’s research is focused on unraveling mechanisms of tumor immune evasion and discovery of translational biomarkers of response to immunotherapies in head and neck cancers. Dr. Chinn’s research is deeply translational, exploring the molecular genetics of head and neck cancers, including oral cavity cancer and HPV+ oropharyngeal cancer and larynx cancer, with a particular emphasis on cancer plasticity, transdifferentiation, and deconstructing the tumor microenvironment through the integration of spatial-omics, digital pathology/virtual staining, and artificial intelligence.
The UPMC Survivorship Clinic is run by Marci Lee Nilsen, PhD, MSN, RN, CHPN, FAAN. She has funding from the NIH to examine the outcomes of patients after surgery, radiation, and chemotherapy for HNC, specifically looking at radiation-induced fibrosis—especially in the neck. She is studying tailored treatments to improve quality of life and patient outcomes. Dr. Nilsen is also trying to broaden the clinic by incorporating satellite locations and telemedicine.

Matthew E. Spector, MD, FACS
Division Chief of Head & Neck Surgical Oncology & Microvascular Reconstruction
Director, Head & Neck Surgical Oncology & Microvascular Reconstruction Fellowship
Professor, Department of Otolaryngology-Head & Neck Surgery
The University of Pittsburgh School of Medicine
SPORE has collected detailed clinical and pathologic information from more than 12,000 patients who have been followed for over 30 years.
Matthew Spector, MD and Shaum Sridharan, MD conduct research in the functional outcomes program, such as determining the right flap for the right patient and ensuring that what is done during reconstruction is translatable for the future. Their goals are to maximize the functional outcome of surgery and afterwards, so patients can speak, swallow, and participate in society the way they want.
The epidemiology group looks at the broader picture of head and neck cancer, like exploring socioeconomic status and modifiable risk factors, and how they fit into head and neck cancer. Jessica Maxwell, MD, MPH, FACS, Chief of Otolaryngology at the VA, has a number of publications looking at disparities at the VA and how they translate into care that is delivered. Angela Mazul, PhD, MPH, is researching biomarkers and the broader epidemiology of head and neck cancer treatment using statistics from clinic patients.
Dr. Zevallos is nationally known and NIH-funded for research on cancer biomarkers and HPV negative drain fluid to understand what cancers need to be escalated with therapy.
An important aspect of the head and neck cancer program at UPMC Hillman Cancer Center is our tissue
SPORE Seed Grants
Joshua Smith, MD and Zhongping Xu, PhD: Surgical Drain Fluid as a Liquid Measure of the Tumor Environment in Head and Neck Cancer
Matthew Spector, MD: Defining the Role of Viral Integration Structures in OPSCC Progression and Recurrence
CORE Grant
Micah Harris, MD: Surgical Drain fluid as a surrogate of the tumor microenvironment in HPV- HNC

and data biorepository. The organ-specific database is administered through the Head and Neck Cancer SPORE and includes detailed clinical and pathologic information from more than 12,000 patients followed for over 30 years. This allows researchers to discern the biomarker-based understanding of cancer and cancer genomics. It’s a huge resource that we have whenever we want to refer to specimens and treatment outcomes.
Dr. Spector has a RO1 grant looking at HPV genetic integration. The genome of HPV can integrate into the genome in different ways; depending on how it integrates, it can cause mutations that are very stable or unstable. Sometimes these cancers become very easy or hard to treat based on where the genome is altered. His overarching project is to look at where those integration events are happening and how they predict the chance of cure.
Despite the current uncertainty of NIH funding, the Head & Neck Surgery group is still extremely active and pursuing research from current grants and applying for new grants, both within the NIH and without. We are using our Eye & Ear Foundation resources to help leverage other kinds of novel mechanisms of funding through philanthropy. Overall, we’re still going full steam ahead to try to defeat head and neck cancer.
NIH Grant
Matthew Spector, MD: Defining the Role of HPV Integration Structures in HNSCC Molecular Heterogeneity (R01 DE032699-01A1)
Other Grants
Kevin Contrera, MD: University of Pittsburgh Clinical and Translational Science KL2 Scholar
Kevin Contrera, MD: Franklin H. Martin Faculty Research Fellowship, American College of Surgeons - two-year early career award to support research into circulating tumor DNA

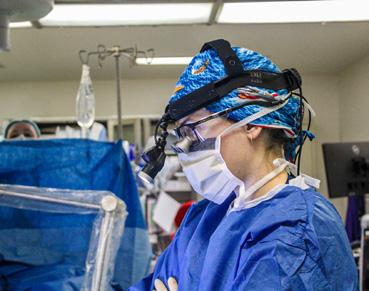
The focus for our division has been to combine excellence in clinical care with excellence in research. We have fostered stronger collaborations with our Pittsburgh Hearing Research Center group and continue to grow clinically.
The Division of Otology & Neurotology is improving clinical pathways, having grown to three advanced practitioner providers from one, and hiring Dr. Greg Basura, an accomplished clinician scientist. We have improved tinnitus referral pathways together with audiology and are developing our in-office procedures, including Eustachian tube procedures. Our implant program continues to grow. We have significantly improved clinic and surgical access times and have set triage systems in the clinics to make sure urgent and semi-urgent cases are evaluated expeditiously.
Design and planning for the new Pittsburgh Hearing Institute at the UPMC Mercy Pavilion is well underway. With insights from clinicians and researchers, we have designed a unique center where surgeons, audiologists, and researchers will work side-by-side to discover the next generation of treatments for hearing loss and tinnitus. The institute will be a first of its kind to directly colocate clinicians and scientists together. We are around one third of the way towards our fundraising goal.
The Department has started an immunological hearing center, which will house discovery, translational, and clinical research. A goal is to go beyond what people traditionally think as immune conditions and look into associated things where the immune system plays a role.

Peter L. Santa Maria, MD, PhD
Professor, Division Chief of Otology & Neurotology
Vice Chair of Translational and Clinical Research
Department of OtolaryngologyHead & Neck Surgery
The University of Pittsburgh School of Medicine
Director Faculty Innovation, Office of Innovation and Entrepreneurship
Adjunct Professor, Bioengineering Carnegie Mellon University
A research assistant professor, Vincent Yuan, MD, PhD, with a strong background in immunology, particularly in the innate immune system, was just hired to co-lead the center. A new clinical trials coordinator just joined the team.
The team has already started looking at immune mechanisms of hearing loss in chronic ear infections and has an expedited pathway for patients with sudden sensorineural hearing loss. They are beginning to investigate their immune markers within the boundaries of insurance.
This has already led to improved treatments for patients with Meniere’s disease and sudden hearing loss.
Greg Basura, MD, PhD, an experienced neurotologist, educator, and funded surgeon-scientist, joined the Department on September 1, 2024. His research, funded through the NIH NIDCD, focuses on human translational studies using functional near-infrared spectroscopy
(fNIRS) to investigate central auditory pathways in unilateral sudden hearing loss and tinnitus. A leader in global otolaryngology outreach, he has worked to develop sustainable educational and clinical initiatives in underserved nations, such as helping launch the first otology fellowship in Africa. As Director of Global Otolaryngology for the Department, he will lead these efforts, including oversight of our international educational programs and ongoing work in South Africa, Mozambique, and Peru.

We plan to expand regionally, including Erie. This will be led by a new clinician scientist hire starting in August. We have an opening for a second position as we look to grow and support the greater Pittsburgh region.

Our group functions under the premise that hearing is a human right. Given this motivation, we spend our time working on alternative pathways to hearing care to make sure that this care is available to everyone across the lifespan. Communication is essential to the human condition. We continue to make great strides towards making hearing care accessible because of the amazing team that exists in Western Pennsylvania, including UPMC audiologists and otologists, the University of Pittsburgh Department of Communication Science and Disorders faculty and students, the Department of Otolaryngology-Head & Neck Surgery faculty and staff, the Eye & Ear Foundation and the amazing greater Pittsburgh community. It is a pleasure to share some of our current work.
The Departments of Ophthalmology and Otolaryngology-Head & Neck Surgery at the University of Pittsburgh are collaborating on a project called THRIVE: Treating HeaRing and Improving Vision: Education. Hearing and vision specialists have teamed up with community health workers to bring hearing and vision support into communities. The project is using guidance from a Community Advisory Panel (CAP) to determine the most relevant content and format for community health worker training in hearing and vision impairment topics. Ultimately, the team will develop the learning materials and disseminate them to community health workers locally, regionally, and nationally.
In the first year of the project, the team gathered information and input about how community health workers interact with patients across Allegheny County. The CAP was formed and included community health worker educators, employers, hearing and vision specialists, and patients. The panel has met several times to generate input on the topics and format that would work best for practicing community health workers. Consensus has been reached in terms of the important topics and now content experts in vision and hearing are working with a Pitt course design expert to create the training.

Catherine V. Palmer, PhD Professor and Chair, Department of Communication Science and Disorders
The University of Pittsburgh School of Health and Rehabilitation Sciences
Professor, Department of Otolaryngology-Head & Neck Surgery
The University of Pittsburgh School of Medicine
Director of Audiology, UPMC
All of our projects now include community partners (stakeholders) who inform the research questions we ask and how we collect and interpret data. Teaming up with community partners is a powerful way to do meaningful projects and it supports dissemination and implementation of the work. For community partners to fully participate in these projects, they need to believe that they can do this impactful work. The belief that you can do something is measured through self-efficacy. Our team is developing the Self-Efficacy for Engagement Scale (SEES) in order to provide research teams with a way to evaluate the self-efficacy for engagement experienced by their community partners. This allows the research team to create better environments to promote self-efficacy. The SEES has been developed and currently is being completed by people all over the country in order to validate the measure.
Over-the-counter hearing aids became available in October 2022. Although this was meant to make hearing aids more accessible for people with mild to moderate hearing loss, the endless choices have proven to be very confusing. The research team includes Catherine Palmer, Elaine Mormer, Aravind Parthasarathy, Hari Bhardwaj, Yashan Wang, and James Katz, who come together with years of clinical, community partner, hearing science, artificial intelligence, information management, and hearing aid industry experience. The development of the clEARdasboard website has been headed up by Dr. Katz. The goal is to support consumers in identifying devices that might be useful to them. Soon you will be able to access the website at www.cleardashboard.info.
This website will help consumers sort through the hundreds of devices by answering questions and indicating preferences. Faculty at the University of Pittsburgh are putting together sophisticated laboratory tests to measure these devices on real people to give a score related to expected function, called the ClearScore. This will allow consumers to compare features and performance if they want to pursue a pathway of self-care when managing their hearing loss.
Audiology is teaming up with the Eye & Ear Foundation and Brother’s Brother to create a hearing and communication mobile unit. This is another way to reach people, especially if they are not coming in for care. It also will be used to include underrepresented populations in important hearing and communication research. The mobile unit should be on the road by early summer 2025!

We added a fourth year-round free clinic at the SHRS Wellness Pavilion in Homewood in the fall of 2025. The clinic involves our Pitt Audiology students and runs every Tuesday. We have already served over 65 people through this clinic including hearing testing and hearing aid fittings.
The Eye & Ear Foundation in partnership with Call to Care has hosted this annual two-day event that provides free care for vision, hearing, and dental for ages two and up. For the past three years, hearing has been part of the event. Each year, the numbers increase, as a lot of people need hearing help, which typically is not covered by insurance. This year, 401 people had hearing tests, with 289 receiving hearing aids and 576 total hearing aids given away. Otology saw 107 patients. UPMC audiologists, UPMC otologists, faculty, audiology students, and audiology alumni all come together to provide these free services.
We are to be partnering with the Western PA Special Olympics Health Athletes. Dr. Ginny Milne, UPMC Audiologist/University of Pittsburgh Clinical Instructor, will be heading this up for our group. We are thrilled to be a part of identifying, evaluating, and treating hearing loss to support participation for this special group of people who have a high incidence of hearing loss.


Joseph M. Furman, MD, PhD, FAAN Director, UPMC Center for Balance Disorders
Professor, Departments of Otolaryngology-Head & Neck Surgery, Neurology, Bioengineering, and Physical Therapy
The University of Pittsburgh School of Medicine
IThe UPMC Center for Balance Disorders utilizes a multidisciplinary approach, as a balance disorder may be a sign of other medical problems. Collaborating with neurology, otolaryngology, physical therapy, neurology, and audiology helps guarantee a comprehensive approach to diagnosis and treatment, beginning with determining the cause. The Center has state-of-the-art technology and a specialized Vestibular Laboratory, which offers several tests to evaluate balance.
Center Director Joseph M. Furman, MD, PhD, FAAN, Professor, Departments of Otolaryngology-HNS, Neurology, Bioengineering, and Physical Therapy, is researching new technology for the laboratory assessment of the inner ear. The vestibular system of the inner ear consists of a group of five sensors on each side of the head, with 10 sensors in all. Six of the sensors respond to rotation, i.e., turning, of the head, and four of the sensors respond to tilting the head. At this time, even the most advanced testing facilities can only reliably test two of the six rotational sensors. The other four rotational sensors, a full 40% of the vestibular system, cannot be reliably tested. Dr. Furman is developing a recently patented technology for testing these four sensors in the balance laboratory.
Dr. Furman is also developing less expensive technology to test the four inner ear sensors that can be transported and used in any clinic. Both technologies rely on high resolution, high speed, infrared cameras to record eye movements while highly accurate gyroscopes and inclinometers measure movement of the head. A computer then processes this information to provide an assessment of the four sensors of the vestibular system that are not currently being evaluated. This research is being performed in collaboration with a local technology company and has been funded by a combination of the National Institutes of Health and the Department of Defense.
Susan L. Whitney, DPT, PhD, NCS, ATC, FAPTA, Director, Vestibular Rehabilitation Program and Professor, Departments of Physical Therapy and Otolaryngology-HNS, is currently funded by two Department of Defense (DoD) grants that support warfighter recovery from mild brain injury with resultant dizziness and balance dysfunction. The PRAXIS study is a multisensory complex retraining program using virtual reality,
Stroop tasks, and complex spatial navigation tasks in rehabilitation at the San Antonio Center for the Intrepid.
At the University of Pittsburgh, we are working on a different DoD grant to determine if an app on a tablet can enhance recovery after a vestibular disorder. The app utilizes facial and eye recognition software to record exercise performance with the goal of providing feedback to the patient and physical therapist to optimize the exercise prescription and get people better faster. With colleagues in New Zealand, Dr. Whitney is working with a team to determine the influence of tinnitus on outcomes after mild brain injury and recently completed a large randomized clinical trial with Drs. Sparto, Kontos and others about the effect of exercise dosing on recovery.
In the clinic, Amy Cassidy, DPT, NCS, and Dr. Whitney are prospectively collecting data about benign paroxysmal positional vertigo (BPPV) by recording precise eye movements. The goal is to begin to recognize patterns of eye movements and then determine which canalith repositioning maneuver is most effective for specific eye patterns of nystagmus. Dr. Whitney is actively engaged in studies with others related to persons with BPPV including recognizing new forms of BPPV, BPPV in older persons related to falls, and offering comments to the World Falls guidelines related to BPPV.
Pam Dunlap, DPT, PhD, NCS, Assistant Professor, Department of Physical Therapy, combines clinical and health services methods to explore factors that influence recovery and patient outcomes in people with balance and vestibular disorders. A primary focus of her work is understanding how fear of movement and activity avoidance affect recovery after a vestibular diagnosis. Dr. Dunlap’s research also examines healthcare quality among individuals with vestibular disorders, aiming to identify and address gaps in care. By addressing individual and healthcare-related barriers, Dr. Dunlap’s long-term goal is to enhance quality of care, promote the adoption of evidence-based practices, and improve quality of life and safe mobility for those experiencing dizziness.
Regan Harrell, PT, DPT, NCS, Assistant Professor, Physical Therapy, is developing a new video head impulse test (vHIT) with Dr. Furman aimed at enhancing the precision and reliability of diagnosing dizziness, especially in patients with vestibular hypofunction. This innovative diagnostic tool seeks to better identify specific impairments, which could, in turn, inform more targeted rehabilitation interventions to enhance patients’
functional outcomes and overall quality of life.
In addition to her work on the vHIT, Dr. Harrell is also deeply invested in understanding the relationship between benign paroxysmal positional vertigo (BPPV) and traumatic brain injury (TBI). She has published several research articles examining how these two conditions interact, and the significant functional challenges faced by individuals who experience both BPPV and TBI. Her research aims to inform clinical practice by shedding light on the functional implications and potential rehabilitation strategies for managing these co-occurring diagnoses, ultimately contributing to more holistic and effective care for those with complex vestibular and neurologic conditions.
Brooke Klatt, PT, DPT, PhD, NCS, Assistant Professor of Physical Therapy, investigated the interplay between vestibular and cognitive function during her postdoctoral fellowship at Johns Hopkins. She continues to investigate this line of research, and in addition to cognition, is interested in exploring other factors that are associated with activity and participation in people with vestibular disorders. Dr. Klatt is currently funded by the National Institutes of Health to conduct her research aiming to optimize vestibular rehabilitation delivery and outcomes.


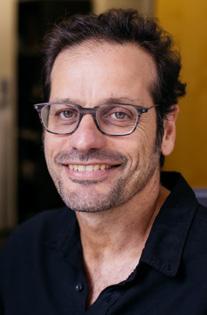
Thanos Tzounopoulos, PhD Vice Chair of Basic Science Research and Professor Department of Otolaryngology-Head & Neck Surgery Director, Pittsburgh Hearing Research Center
The University of Pittsburgh School of Medicine
UPMC Endowed Professor of Auditory Physiology
In 2017, we founded the Pittsburgh Hearing Research Center (PHRC). Since then, six NIH-funded hearing research investigators have joined our PHRC team. The PHRC team currently has a total of 10 NIH grants, which has contributed to the Department of Otolaryngology-Head & Neck Surgery NIH funding increasing from $5.4 million in 2017 to $13.7 million in 2024 and to its 2nd place ranking for NIH funding. The PHRC has emerged as one of the most important and productive hearing research programs in the United States, and I am grateful to the PHR team of faculty, trainees, and administrators for their amazing progress. We are well poised and positioned to drive research, education and innovation in the hearing and neuroscience space and become the top hearing research team in the country.
The hearing research program has expanded. Two physician scientists (MD, PhD) joined the team: Dr. Peter Santa Maria and Dr. Greg Basura, along with two basic scientists (PhD): Dr. Adele Moatti and Dr. Patrick Cody.
The Santa Maria Lab is federally funded to explore the immune mechanisms of hearing loss in chronic infectious ear disease but is undertaking large scale efforts to understand immune mechanisms in the ear, tumor biology, and chronic bacterial infections, and the application of nanotechnology to address these issues.
Pittsburgh Hearing Research Center: Hearing Research From The Ear To The Brain and Back
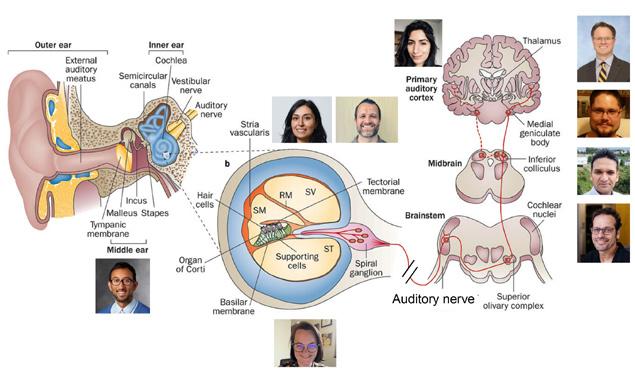
Dr. Basura’s research, funded through the NIH NIDCD, focuses on human translational studies using functional near-infrared spectroscopy (fNIRS) to investigate central auditory pathways in unilateral sudden hearing loss and tinnitus.
The Moatti Lab addresses the significant challenges inherent in developing effective inner ear substance delivery systems. One key hurdle involves not knowing the exact drug formulation for which the delivery system is being designed, affecting drug bioavailability and biodistribution. Another obstacle lies in translating promising findings from preclinical studies, conducted on animal models, into applicable solutions for human patients. Synergistic collaborations between hearing healthcare professionals and scientists, along with technological innovations such as 3D imaging and nanotechnology, would pave the way for transformative advancements in inner ear drug delivery systems.
Dr. Cody leads the data science core for the Pittsburgh Hearing Research Center, focusing on transforming data into solutions for hearing-related disorders. The core combines hearing domain expertise with industryleading AI/ML engineering, data standards, and architecture. By serving as a dedicated interface with existing research data resources across the university, the core enhances efficiency and accelerates the translation of data into impactful solutions.
A team led by Drs. Thanos Tzounopoulos, Amantha Thathiah, and Chris Cunningham, discovered a potential new way to prevent noise-induced hearing loss: trapping excess zinc. This groundbreaking research was highlighted by the NIH Director, UPMC, and many other media outlets.
A unique program at the University of Pittsburgh School of Medicine allows students in existing doctoral programs at the University of Pittsburgh to obtain additional training in hearing and vision research and methodology with a Certificate in Hearing Vision Sciences (HVS Doctoral Certificate) from the University of Pittsburgh, which has many world-class faculty and trainees investigating hearing and vision sciences. It is estimated that students who complete this certificate will add a maximum of six months to their overall graduate studies, as the requirements will be spread over years two to four of graduate study.
• Christopher Cunningham, PhD and Thanos Tzounopoulos, PhD, STTR, NIH: Cell type-specific gene therapy approach for TOMT-linked congenital hearing loss
• Melissa McGovern, PhD and Christopher Cunningham, PhD, DoD: Developing Viral Delivery Strategies for Targeted Hair Cell Regeneration
• Greg Basura, MD, PhD, R01, NIH: Subjective and Somatic Tinnitus; Using Functional Near-InfraredSpectroscopy to Identify Objective Correlates in Auditory and Non-Auditory Cortices
• Adele Moatti, PhD, R00, NIH: Enhanced intratympanic delivery of therapeutics to treat and prevent hearing loss using nanovesicles in the porcine model
• Ross Williamson, PhD, Kavli Exploration Award for Sculpted Light, Kavli Foundation: Brain-wide cortical circuits for sensory-guided behavior
• Manoj Kumar, PhD, Hearing Health Foundation: KCNQ2/3 potassium channel activator mitigates noise-trauma-induced hypersensitivity to sounds in mice
Thanos Tzounopoulos received the prestigious Dr. Richard J. Bellucci Pioneer Award. This honor celebrates his outstanding contributions and dedication to hearing research. His remarkable work has been at the forefront of auditory neuroscience, offering hope for effective treatments for hearing loss and tinnitus, and his leadership efforts have established one of the leading hearing research programs in the United States.
We are collaborating with the French Hearing Institute in common research and training goals. Last year, we visited them in Paris and this year they will be visiting us to advance our collaborations.

Carl H. Snyderman, MD, MBA
Vice Chair, Quality & Patient Safety
Professor, Departments of Otolaryngology-Head & Neck Surgery, Neurological Surgery, and Bioengineering
Co-Director, UPMC Center for Skull Base Surgery
University of Pittsburgh School of Medicine
Co-Director, CREATES

Eric W. Wang, MD, FACS
Executive Vice Chair, Department of Otolaryngology-Head & Neck Surgery
Professor, Departments of Otolaryngology-Head & Neck Surgery, Neurological Surgery, and Ophthalmology
University of Pittsburgh School of Medicine
Director of Education, UPMC Center for Cranial Base Surgery
Chief, Division of Rhinology
Within the Department of OtolaryngologyHead & Neck Surgery, the UPMC Center for Cranial Base Surgery is merged with the Division of Rhinology. Faculty include Drs. Carl Snyderman, Eric Wang and Garret Choby from the Department of Otolaryngology and Drs. Paul Gardner and Georgios Zenonos from the Department of Neurological Surgery. The UPMC Center for Cranial Base Surgery, established in 1987, is a world leader in the medical and surgical management of disorders of the skull base. It just celebrated its 5,000th endoscopic endonasal skull base surgery and is recognized for pioneering many of the surgical techniques in minimally invasive skull base surgery. In recognition of its history, an Endowed Chair in Cranial Base Surgery has been established by Drs. Eugene N. Myers and Joseph C. Maroon, who were the early pioneers of skull base surgery at UPMC. The UPMC Center for Cranial Base Surgery is also a designated Pituitary Tumor Center of Excellence and a North American Skull Base Society Team of Distinction. Recent network analyses of the publications of membership of the North American Skull Base Society demonstrates the central role that UPMC has played in the training of skull base surgeons in North America.
The Center for Cranial Base Surgery attracts patients from across the region, nationally, and internationally. In addition to neurosurgical tumors such as pituitary adenomas, craniopharyngiomas, meningiomas, chordomas, and rheumatoid degeneration of the craniocervical junction, the Center attracts patients with benign and malignant sinonasal tumors. [Working closely with the pediatric skull base team, Drs. Amanda Stapleton (Otolaryngology-Head & Neck Surgery) and Cody Nesvick (a recent faculty recruit in neurosurgery), treat a wide variety of pediatric pathology cases]. We continue to pioneer minimally invasive approaches such as the contralateral transmaxillary approach to the petrous apex, which has greatly improved the complete resection of chordomas. In collaboration with Nuclear Medicine, we have pioneered a new radiation therapy technique (Lutathera) for recurrent olfactory neuroblastomas that combines a radioligand with a targeting molecule to selectively deliver tumoricidal radiation to tumor cells with sparing of normal adjacent tissue when all other therapies have failed. Working

closely with colleagues in Ophthalmology (Drs. S. Tonya Stefko and Gabrielle Bonhomme), a variety of orbital pathology is also managed using minimally invasive transorbital approaches.
The Center for Cranial Base Surgery hosts three skull base courses yearly. These intensive four-day courses emphasize the endoscopic endonasal approach and combine live surgery, anatomical dissections, 3D lectures, and surgical simulation training. Since 2004, more than 2,000 surgeons from across the globe have attended these courses. A highlight of our training program is the development of a team simulation training module for the management of intraoperative vascular injury. Our clinical fellowship matriculates two fellows annually through the American Rhinological Society’s matching program. Highlights of the fellowship training program include extensive exposure to advanced rhinologic and skull base surgical techniques, participation in UPMC courses, research presentations at annual meetings, and anatomical studies. Past fellows have gone on to lead new skull base programs at academic institutions across North America. Educational and training activities also include a Visiting Clinical Observer Program and Anatomical Research Fellowship. Many of our new surgical techniques originate from anatomical research performed in the Surgical Neuroanatomy Lab. The laboratory is also a center for innovation with the
development and testing of new surgical technologies. International teaching activities include courses in Indonesia, Singapore, and Taiwan.
Active areas of research include improving quality of life following endoscopic skull base surgery and improving survival in patients with sinonasal malignancies. Highlights of ongoing studies include proliferative and immunologic profiling of sinonasal mucosal melanoma and helping to lead a multi-site consortium prospectively evaluating survival outcomes and tissue banking of sinonasal malignancies. The UPMC Center for Cranial Base Surgery works closely with the Chordoma Foundation to identify molecular markers that are relevant for the prognosis and treatment of chordomas. The Division of Rhinology is collaborating with multiple national and international research consortiums to improve our understanding of the biologic behavior of sinonasal malignancy. Working closely with our colleagues in Pathology, a tissue bank provides a repository for specimens from a variety of sinonasal tumors that can be used for future studies. With the addition of renowned head and neck pathologist, Dr. Diana Bell, there is an opportunity for new research in the pathology of sinonasal malignancies. Clinical and basic science research activities are made possible through the efforts of Benita Valappil, MPH, Clinical Research Director. She maintains a comprehensive database of all patients and manages collaborative studies and clinical trials.

Christina Yver, MD, MBA
Division Chief, Facial Plastic & Reconstructive Surgery
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery
The University of Pittsburgh School of Medicine
The UPMC Division of Facial Plastic Surgery provides comprehensive care for patients with facial aesthetic and reconstructive needs. Our providers specialize in advanced nasal surgery (including cosmetic and functional rhinoplasty), aesthetic facial surgery (including facelift, blepharoplasty, and chin augmentation), facial nerve disorders and facial reanimation, facial reconstruction, facial trauma, and minimally-invasive procedures. We are committed to providing patients with the highest level of care while simultaneously advancing the field through research and innovation.
The FPRS division is committed to prioritizing convenience of care for our patients. To that end, the launch of our new procedure clinic now allows for minor procedures to be performed in the clinic setting, including skin cancer reconstruction, scar revisions, minor facial reanimation procedures and cosmetic procedures such as blepharoplasty and lip lifts. In addition, the division will soon benefit from a major expansion of the Shadyside clinic. This renovation, which is currently underway, will prioritize an elevated patient experience with brand new clinic rooms, a new waiting room, a state-of-art procedure room, and a dedicated photography room.
For more than 20 years, experts at the UPMC Facial Nerve Center have diagnosed and treated patients with facial paralysis and facial nerve disorders. We are proud to have recently expanded our program to ensure our patients benefit from the latest advances in care for both flaccid paralysis and facial synkinesis. Our facial paralysis patients benefit from the expertise of our facial nerve-dedicated physical therapy group under the leadership of Amy Cassidy, PT, and Darcy Bonaventura, PT, as well as the entire spectrum of surgical interventions including selective myectomy, selective neurectomy, nerve transfers, nerve grafting, and gracilis free muscle transfer. We appreciate the help of the Eye & Ear Foundation in assisting with the launch of a brand-new UPMC Facial Nerve Center website, which now serves as an invaluable patient resource.

We believe that advancing the field through innovation and knowledge goes hand in hand with providing the highest level of patient care. The UPMC Facial Nerve Center has secured a prestigious departmental grant to investigate the effects of facial synkinesis at the level of the neuromuscular junction, in collaboration with the lab of Kacey Marra, PhD. We are also collaborating with an engineering group out of Carnegie Mellon University to develop novel EMG technologies for facial paralysis patients. Research out of our division has been presented at several national meetings in the past year, including those sponsored by the American Academy of Otolaryngology and the American Academy of Facial Plastic Surgery, as well as in highly-esteemed medical journals including Plastic & Reconstructive Surgery. We look forward to the launch of a new facial nerve database at UPMC, EnlightenMD, which will further support our clinical research endeavors.
We have received extremely favorable feedback following the launch of our new satellite clinic in Wexford with the support of Metropolitan Ear, Nose, and Throat Associates, which has allowed us to expand regional patient access. We also welcome the addition of Michelle Thompson, CRNP, who specializes in facial aesthetics and minimally-invasive treatment options including injectables, filler, Sculptra, microneedling and dermabrasion. We continue to grow our regional referral volume, particularly in the domains of Mohs reconstruction, nasal reconstruction, facial paralysis, and synkinesis. We look forward to the recruitment of an additional faculty member in the coming year to help continue to grow the division’s footprint.

David H. Chi, MD Division Chief, Pediatric Otolaryngology
UPMC Children’s Hospital of Pittsburgh
Associate Professor, Department of Otolaryngology-Head & Neck Surgery
The University of Pittsburgh School of Medicine
The Division of Pediatric Otolaryngology builds on the strong foundation from the founding pioneer of pediatric otolaryngology, Dr. Charles Bluestone, with over 20% volume growth in patient care over the past year.
The faculty comprises 12 physicians and eight advanced practice providers with services at Children’s Hospital of Pittsburgh and four regional satellites located in Wexford, South Fayette, Monroeville and Johnstown. We anticipate further expansion of our services in the region starting this summer.
We are active in research with clinical outcomes and clinical trials to investigate best surgical techniques in ear tube surgery and outcomes of hypoglossal nerve stimulation for sleep apnea in Down syndrome patients. We also have active trials investigating methods to minimize postoperative pain after surgery.
We value education and are active in teaching pediatric otolaryngology fellows, otolaryngology residents, and medical students. We have a robust lectures series for didactic education and patient care education in the operating room and clinics.
The division provides excellence in patient care in all aspects of ear, nose, and throat care. We have experts and thought leaders in complex conditions in pediatric rhinology, sleep medicine, cleft and craniofacial care, thyroid disorders, airway disorders, and otology. At the same time, we provide comprehensive care in common primary disorders such as otitis media and tonsillar disease.
Members of the Division are among the most experienced in the world in managing childhood ear disorders, including middle ear disease, congenital ear anomalies, chronic ear disorders, and sensorineural hearing loss. Through the Hearing Center and Congenital Ear Center, they provide expert evaluation, diagnosis, and advanced therapy for disorders of the ear.
This unique regional resource manages a wide range of congenital and

acquired airway disorders in children. When needed, innovative surgical interventions are employed, such as the novel use of lasers, procedures involving cartilage and mucosal grafting, and minimally invasive endoscopic techniques. Ancillary medical conditions, including those involving speech, swallowing, and the pulmonary and gastrointestinal systems, are included in the assessment and treatment plan. Videorecording capabilities complement the structural OR assessment. In addition, a patient database and registry are maintained. Approved by the Institutional Review Board at the University of Pittsburgh, they allow for the collection of specialized patient data.
A team of specialists from the Division of Pediatric Otolaryngology, including physicians, a voice nurse, and pediatric speech and language pathologists, provides comprehensive evaluation and treatment of the full range of voice, resonance, and swallowing conditions, including vocal fatigue, problems with nasality, drooling, and other conditions associated with problems managing salivatory secretions.


Founded within the field of otolaryngology, Pittsburgh CREATES has evolved to serve the entire Pittsburgh healthcare ecosystem, extending beyond its initial boundaries to collaborate with various fields, including engineering and rehabilitative sciences.
Pittsburgh CREATES is committed to addressing unmet needs in healthcare innovation by focusing on understanding the problems that need solving. One of the core principles of the organization is conducting thorough user research to gain diverse perspectives on these challenges, ensuring that any innovation is truly impactful. Whether someone comes in with a specific idea or is looking to become an innovator without a clear concept yet, Pittsburgh CREATES guides them through a needs-based process that centers on the problem, the target population, and the measurable outcomes.
A key part of this approach is creating a “need statement,” which clearly defines the problem, specifies the population it affects, and establishes the criteria for success. This might mean addressing a specific disease or condition in a particular demographic, such as children, women, or individuals that are specifically affected by the issue. For example, in tackling cancer, the question isn’t just about treating the cancer but also about improving quality of life or enhancing diagnostics, not just tackling how to cure the disease. By focusing on one aspect of a problem and understanding which population it affects, Pittsburgh CREATES ensures the solution is both meaningful and achievable.
The process isn’t just about finding the right solution but ensuring that the problem is understood deeply before any prototyping takes place. This requires continuous refinement. For instance, if a physician comes to Pittsburgh CREATES, despite having an initial idea, continues to meet with Pittsburgh CREATES and, multiple times without discussing their concept directly, they are revisiting the problem from all angles. This approach focused on “needs finding,” is imperative and distinguishes Pittsburgh CREATES from other innovation hubs in the area.
Pittsburgh CREATES is co-directed by Peter Santa Maria, MD, PhD, and Carl Snyderman, MD, MBA. Mohit Singhala, PhD, is the lead engineer. Dr. Singhala has a Masters from the Johns Hopkins Center for Bioengineering Innovation and Design (CBID). Both Dr. Santa Maria and Dr. Singhala have gone through Biodesign training at Stanford. Stanford Biodesign is the origin for the needs-based approach to innovation in Medtech. Pittsburgh CREATES is heavily influenced by both institutions.

Mohit Singhala, PhD
Research Assistant Professor, Department of Otolaryngology-Head & Neck Surgery Lead Engineer, CREATES
As such, Pittsburgh CREATES is deeply committed to fostering collaboration across disciplines to accelerate healthcare innovation and improve patient outcomes. One of our key goals is to bridge the gap between the incredible scientific, surgical, and technical talent in Pittsburgh and the ability to bring these innovations into practical, real-world applications. Despite the strength of Pittsburgh’s healthcare talent, the output in terms of translating research into actionable solutions hasn’t reached its full potential. Pittsburgh CREATES seeks to change this by guiding innovators to define their projects more clearly, de-risk their efforts, and ensure that their work reaches patients effectively—whether through traditional licensing routes or by helping them pursue startup ventures.
Interdisciplinary collaboration is at the heart of everything Pittsburgh CREATES does. The complexity of healthcare challenges requires input from a diverse range of expertise. We need to understand not only the patient’s experience but also the constraints faced by healthcare providers, entrepreneurs, hospital systems, and regulatory experts. Whether it’s addressing the economic decisions of hospital administrators or understanding the regulatory hurdles for medical devices, collaboration across disciplines is essential to making meaningful progress. By fostering a culture of collaboration, Pittsburgh CREATES ensures that all relevant perspectives are considered, which leads to more effective and sustainable innovations.
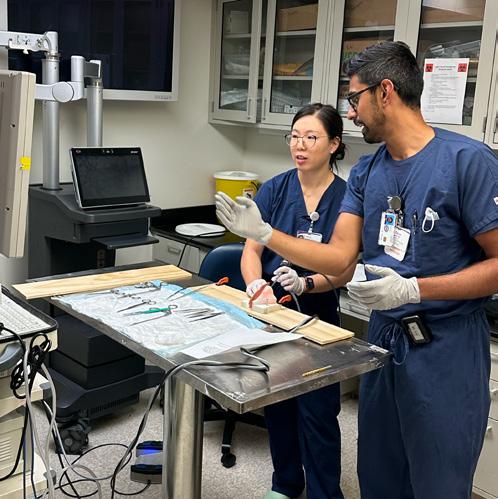
Founded within the field of otolaryngology, Pittsburgh CREATES has evolved to serve the entire Pittsburgh healthcare ecosystem, extending beyond its initial boundaries to collaborate with various fields, including engineering and rehabilitative sciences. This openness ensures that anyone interested in improving healthcare, regardless of their discipline, is welcome to collaborate and contribute to Pittsburgh CREATES’ mission. Through this broad inclusivity, Pittsburgh CREATES is pushing the boundaries of healthcare innovation, making a significant impact on the entire region’s medical and engineering landscape.
Our approach to translation is intentionally broad; it’s not just about creating startups. We understand that innovation in healthcare also occurs at the institutional level—whether that’s developing a new surgical technique or improving internal department workflows. At Pittsburgh CREATES, we encourage innovators to think beyond traditional entrepreneurship and focus on solving immediate, tangible problems within the healthcare ecosystem. We push for practical solutions that can impact both local and global communities.
One of the most important aspects of Pittsburgh CREATES is our commitment to the community. In Pittsburgh, we actively engage with local health initiatives, such as Mission of Mercy, to innovate solutions for those who face barriers to healthcare access. Our goal is to improve the efficiency and accessibility of healthcare for all communities by developing more effective workflows, tools, and devices for both patients and providers.
Ultimately, Pittsburgh CREATES wants to streamline and enhance the healthcare innovation process. Part of our goal is to help individuals and teams navigate the complexity of turning an idea into translational research that can ultimately help patients. This is done by facilitating collaboration and guiding innovators through a structured approach to development—helping them understand what expertise they need and when, so they can make progress more efficiently. By doing so, we aim to create a sustainable and impactful ecosystem that benefits both local and global communities.

One of the most important aspects of Pittsburgh CREATES is our commitment to the community. In Pittsburgh, we actively engage with local health initiatives to innovate solutions for those who face barriers to healthcare access.

HPV-negative squamous cell carcinoma (HNSCC) is the most aggressive and common form, with a high recurrence rate after surgery. Current guidelines for recommending additional radiotherapy or chemoradiation to high-risk patients rely on clinical and pathological criteria that lack precision and objectivity. Furthermore, the absence of a reliable liquid biopsy marker for detecting minimal residual disease (MRD) post-surgery makes it hard to personalize and tailor treatments for these patients.
Droplet has pioneered the development of liquid biopsy technology for HNC, with a specific emphasis on nonblood fluids. In recently published data, we showed that ctDNA in SDF of HPV (+) and HPV (-) HNSCC predicted locoregional relapse and progression-free survival with high sensitivity and specificity. SDF ctDNA significantly outperformed postoperative plasma ctDNA in HNSCC. We now propose a new innovative way to measure MRD in HPV (-) HNSCC. We will screen and select candidate patients, then collect blood and saliva samples before surgery as a baseline. Postoperatively, blood and SDF will be collected 24 hours after surgery, and saliva will be collected during the first postoperative clinic visit. By analyzing circulating tumor DNA (ctDNA), extracellular vesicles (EVs), and immune cells, we can assess MRD more accurately. This approach enhances traditional staging, enabling personalized and tailored adjuvant therapy and reducing locoregional relapse, improving patient outcomes and survival.
Theresa Tribble
Wendy Winckler, PhD
José P. Zevallos, MD, MPH
Aadel Chaudhuri, MD, PhD
Stan Lapidus, Co-founder
DropletBioSci.com
Earflo is a Eustachian tube opening device hidden inside a drinking cup that can treat chronic ear infections without surgery. Chronic ear infections lead to around 700,000 tube surgeries done in the U.S., which many children wait six months to have. During this time, they have hearing loss and may have speech and language delays. So far, the Earflo has been used in approximately 50 patients with over 90% no longer needing surgery.
Peter Santa Maria, MD, PhD
Intan Oldakowska, BEng, BCom, PhD
Matthew Oldakowski, BEng, PhD
Stephen Kargotich, PhD, MBA, LLB earflocare.com
Flotherm is a thermal compression device that prevents patients from becoming hypothermic during surgery. More than 50% of patients who have surgery experience hypothermia, which drives surgical site infections, heart conditions, blood loss and other complications. Flotherm provides heating around key parts of the lower limbs and provides compression to also prevent deep vein thrombosis. In a clinical study, the Flotherm patients became hypothermic in around 15% of the cases, compared to nearly 70% of patients who received forced air warming, the current standard of care.
Founders
Brian Kennard, CEO
Peter Santa Maria, MD, PhD, CSO
Abhinav Ramami, CMO, COO flothermtcd.com
DizzyEx is a wearable dizzy monitor that a patient can wear in the home to diagnose vertigo attacks. Patients who have frequent vertigo attacks can be debilitated, but they are frustrated because they often feel fine when they eventually get to see the doctor. They often end up seeing multiple specialists and having many tests ordered, all while they are feeling fine. The DizzyEx can record eye movements and head position while patients go about their normal activities. If they have an attack, the device records it and then sends it to the physician for an accurate diagnosis.
Founder
Peter Santa Maria, MD, PhD

Auration Biotech is developing a regenerative treatment for the ear drum. Chronic ear drum perforations result in around 170,000 tympanoplasties every year in the U.S. They require surgery, anesthesia, and an outpatient admission. Auration’s topical therapy can heal the ear drum in the office without surgery or anesthesia. It has recently finished an FDA phase 1/2a trial, with current work being done to improve the formulation before entering a Phase 2 human trial.
Founders
Benjamin F. McGraw, III, PharmD
Sanjay Chanda, PhD
Peter Santa Maria, MBBS, PhD, FRACS
aurationbiotech.com
Hearing for Health provides resources, educational materials, and products that support low-cost identification and management of hearing loss. The focus is on hearing and communication as an essential part of overall health and specifically healthy aging. Aging hearing loss is a chronic condition and requires an approach that supports long-term self-management in addition to access to professional assistance when needed.
Founder Catherine Palmer, PhD

Echogenesis Therapeutics was co-founded by Drs. Christopher Cunningham, Thanos Tzounopoulos, and José Zevallos. The goal of Echogenesis Therapeutics is to advance cell-type-specific gene therapy in hearing loss and vestibular disorders. Hearing loss is one of the most prevalent sensory deficits, yet there are no biological therapies. Hereditary (genetic) forms of hearing loss occur in 50-80% of individuals born with hearing loss, thus gene therapy is an attractive treatment strategy. Echogenesis has created a novel therapeutic development pipeline to develop celltype-specific AAV-based gene therapies. We utilize our innovative therapeutic development pipeline to produce therapies to target many of the gene mutations associated with sensorineural hearing loss and vestibular disorders.
Founders
Dr. Christopher Cunningham, CEO
Dr. Thanos Tzounopoulos, CSO
Dr. José Zevallos

Kalperta Laboratories LLC is a biotech startup based in Pittsburgh focused on the development of two ion channel allosteric modulators (ICAMs), KAL-1 and KAL-2, for the treatment of neurological disorders. Rather than directly activating ion channel targets, ICAMs instead enhance the natural function of ion channels, greatly increasing their possible safety and efficacy profiles.
KAL-1 boosts calcium influx at the neuromuscular junction as a novel approach to preventing motor neuron death in ALS. KAL-2 increases potassium channel function to correct hyperexcitable auditory circuits, which are a key factor in developing tinnitus. We are currently seeking partners and investors who are passionate about our ICAM approach and want to help us deliver safe, effective medicines to millions of people in need.
Peter Wipf, PhD
Steve Meriney, PhD Thanos Tzounopoulos, PhD

Respair (RespairMed.com) is a Pittsburgh-based medical device company that builds innovative airway products to support clinicians and patients in critical care environments. Every year hundreds of thousands of patients die from secondary complications they develop while on a ventilator. These complications stem from breathing tubes that fail to protect the lungs from deadly aspirated contents. Our technology replaces the error-prone inflatable cuff used on current breathing tubes with soft, pliable baffles that act like a stopper, comprehensively sealing the airway without adding pressure.
We are recipients of an SBIR grant and are currently working toward FDA submission (Class II medical device; 510k pathway).
Founder
Carl Snyderman, MD, MBA, CTO respairmed.com

At Vine Medical, we believe there is a better way to access the human body. vinemed.com

Ryan J. Soose, MD
Division Chief, Sleep Division Associate Professor, Department of Otolaryngology-Head & Neck Surgery
The University of Pittsburgh School of Medicine
We are in the “Golden Age” of sleep apnea care. Public awareness is at an all-time high. Population numbers are staggering, with 1 billion affected worldwide. The health benefits of better sleep and breathing are too numerous to count. We have more access to convenient, comfortable, accurate diagnostic testing and sleep-tracking wearables than ever before. And we have a rapidly expanding armamentarium of effective medical and surgical treatments.
It’s an exciting time not only to be part of this revolution but to lead it. We are the only Otolaryngology-Head & Neck Surgery Department in the world with three fellowship-trained and dual-boarded sleep surgeons and we remain committed to ongoing growth. The mission of the Sleep Division includes delivering world-class personalized multimodality clinical care, advancing the field through research and innovation, training the next generation of sleep-specialized otolaryngologists, and providing academic leadership across local, national, and international platforms.
Thomas Kaffenberger, MD, opened a CPAP-alternatives clinic at the Pittsburgh VA Hospital combining Sleep Medicine and Sleep Surgery personnel and introducing Inspire hypoglossal nerve stimulation therapy to veterans.
Rachel Whelan, MD, leads a new Refractory OSA Pediatric Sleep Clinic in Wexford.
Ryan Soose, MD, earned the UPMC Excellence in Patient Experience Award in 2024 for the third consecutive year, which recognizes the otolaryngologist in the entire UPMC system with the highest PressGaney patient satisfaction scores (<1% of UPMC physicians).
The sleep physicians and APPs have expanded Sleep ENT services to East and West Mifflin satellites as well as telemedicine visits.
In the last year, we had 12 peer-reviewed publications and multiple grants in submission for future clinical trials.
Drs. Soose and Kaffenberger implanted the first Inspire V in the United States at UPMC Mercy in December 2024.
We are actively involved in the development and clinical trial testing of a novel cryotherapy treatment that reduces fat in the tongue and other soft tissues of the upper airway.
We have a clinical trial site at CHP studying hypoglossal nerve stimulation therapy in adolescents with Down syndrome. Drs. Whelan and Soose are also active members of the GLOBAL Down Syndrome committee developing new medical guidelines for adults with Down syndrome.
We are a clinical trial site for the NFL Brain Health Initiative investigating sleep and brain health trajectories in retired NFL players.
The UPMC Department of Otolaryngology-Head & Neck Surgery has produced more fellowship-trained sleep surgeons than any other program in the country (and it’s not even close!).
We trained a hybrid Sleep Medicine/Sleep Surgery Fellow this year who has accepted an academic Sleep Surgery position at Rutgers University next year.
Residency training in sleep was expanded to CHP (Dr. Whelan) and the VA (Dr. Kaffenberger).
Dr. Soose was recognized with the PACCSM Outstanding Sleep Educator Award.
We had numerous invited lectures and abstract presentations across a wide variety of local, national, and international conferences.
Dr. Soose is course director, and Dr. Kaffenberger is a faculty member, for the national resident cadaver course in sleep apnea and hypoglossal nerve stimulation–now the largest ENT resident cadaver course in the U.S.
We had a strong representation at the 2024 annual meeting of the International Surgical Sleep Society (ISSS), with presentations from two Pitt Med students, three ENT residents, one Sleep fellow, and two attendings. Drs. Soose and Kaffenberger have been appointed to the ISSS Board.
Dr. Soose organized a joint educational conference between the Departments of OtolaryngologyHead & Neck Surgery in Ukraine and the University of Pittsburgh.


Libby J. Smith, DO, FAOCO Division Chief, Laryngology Director, Voice Center Professor, Department of Otolaryngology-Head & Neck Surgery
The University of Pittsburgh School of Medicine
The Voice, Airway & Swallow Center has had an exciting year. A pillar within the laryngology landscape, both clinically and scholastically, the Center provides comprehensive, multidisciplinary care to those with voice, upper airway, and swallowing disorders. Our dedicated team of clinicians and state-of-the-art facilities allow us to provide this expert level care.
Since the inception of the University of Pittsburgh Voice Center, the Voice Center and the Swallow Disorders Center have been two separate entities within the Department of Otolaryngology-Head & Neck Surgery. In the fall of 2024, the Voice Center and Swallow Disorder Center finally joined forces within the Division of Laryngology, bringing voice and swallow disorders under the same roof at UPMC Mercy. Sandra Stinnett, MD, Director of the Swallow Disorders Center, and Tami WassermanWinko, MS, CCC-SLP, lead SLP, showed leadership and grace to make it happen. By bringing these two prominent fields within laryngology, we have improved coordinated patient care and resident education.
The other exciting news is that Chloe Santa Maria, MD, MPH, joined the laryngology team. She completed her laryngology fellowship last year at the University of Southern California. She brings unique talents to the team, namely expertise in open airway reconstruction. As such, she is creating a Complex Adult Airway Clinic in collaboration with the thoracic surgery and interventional pulmonology teams.
The Voice Division remains prolific in comprehensive voice, upper airway, and cough care. In collaboration with the Physical Medicine & Rehabilitation Department, we continue to be leaders in the utility of laryngeal electromyography in the care of patients with vocal fold paralysis or unexplained dysphonia. In-office procedures have expanded with the additional focuses of dysphagia and subglottic/tracheal stenosis.
Our research arm is also growing. Dr. Santa Maria is starting a translational research lab on laryngeal/tracheal scar. Robust clinical research continues in health disparities, dysphagia, and neurolaryngology.
Community outreach has always been a pillar of who we are and what we do. Unfortunately, these were disbanded during the pandemic. We are now re-engaging with our local voice communities with free educational sessions on vocal wellness. Nichole Sommers, PA-C,
our voice-specialized physician assistant, has been doing a stellar job at coordinating these efforts with regional theaters, choirs, schools, churches, and synagogues. Dr. Santa Maria has also spearheaded a renewed collaboration with the Young Artists Program at the Pittsburgh Opera. The inaugural Vocal Injury Prevention program in January 2025 was a success and we look forward to continuing and expanding that partnership to other venues within the vocal performing arts community.
Commensurate with these monumental changes, we have rebranded our name to encompass the full extent of what we do for patients: the Voice, Airway & Swallow Center. We look brightly to the future in 2025 and beyond.



Gregory J. Basura, MD, PhD Director, Global Otolaryngology Professor, Department of Otolaryngology-Head & Neck Surgery
The University of Pittsburgh
School of Medicine
The Department’s Global Outreach programs span the local/regional, university, national and international spaces. On a local and regional level, Greg Basura, MD, PhD is building ties with the School of Public Health and with the Chancellor of Global Affairs at the University of Pittsburgh to expand partnerships for community and rural programs in Pennsylvania and the U.S. Those programs are being developed and include epidemiology and medical outcomes research/impacts on rural health disparities and access to medical care in the U.S.
At the university level, Dr. Basura has assumed the leadership of the storied International Visiting Scholars (IVS) Program with the Department. This program, started by Dr. Eugene Myers in 1991, was established to provide surgical observerships for international providers from across the globe to spend dedicated time in the various subspecialties of otolaryngology at the University of Pittsburgh. During a one to 3-month rotation they observe in the clinic, follow operating room cases and engage in research programs. Over the years, the IVS program has hosted hundreds of international visitors and in 2024 hosted eight scholars with 10 scheduled for 2025.
On a national level, the Department shares a wonderful relationship with the American Academy of Otolaryngology/Head and Neck Surgery (AAO-HNS) where University of Pittsburgh otolaryngology faculty regularly present at the annual meeting and are involved with committee work. Dr. Basura is currently the Chair of the Humanitarian Efforts Committee (HEC) and engages at the national level and coordinates the subcommittees including the scholarly output committee (in charge of mini symposium presentations at AAO), the communications subcommittee (in charge of the monthly “Stories from the road” segment in the AAO Bulletin to showcase global outreach efforts) and the education subcommittee (in charge of annual educational webinars; “Surgical Simulation” in 2024 and “Best Global Surgical Practices” in 2025). The HEC also oversees the International Visiting Scholars program that provides residents financial support through grants/awards to engage in a global outreach experience. All the HEC work and the IVS and Humanitarian Awards are showcased at the annual Humanitarian Efforts Forum at the AAO that Dr. Basura oversees/organizes.
At the international level, University of Pittsburgh residents have an opportunity to travel to engage in a month long medical, surgical and educational service opportunity at the University of Cape Town in South Africa. These rotations, formerly overseen by chairman Dr. Johan
Fagan (University of Pittsburgh Head and Neck and Otology Fellow, 1995-1997), now overseen by Dr. Shazia Peer (Pediatric Otolaryngology), provide residents an opportunity to immerse themselves in the international community to obtain a broader medical, surgical, and educational experience.
The resident rotations will be expanded to newly forming and developing relations in Mozambique and Peru. The Department’s relationship with these two countries is new and more information about the specifics of those cooperatives will be updated within the next year. Drs. Zevallos and Peter Santa Maria
made an initial site visit to Mozambique last fall to begin planning the future cooperative with Dr. Zevallos also traveling to Peru with several residents for a needs assessment and planning.
Lastly, Dr. Basura in November 2023, launched the African Otological Society. This is a monthly online society to build community and otology and audiology capacity in Africa. This community presents monthly with a featured country and is currently crafting otology and audiology resource centric clinical practice guidelines to optimize care in resourceconstrained areas.

At the international level, University of Pittsburgh residents have an opportunity to travel to engage in a month long medical, surgical and educational service opportunity at the University of Cape Town in South Africa.

Noel Jabbour, MD, MS, FACS
Residency Program Director and Vice Chair of Education
Director, Congenital Ear Center at UPMC Children’s Hospital of Pittsburgh
Associate Professor, Department of Otolaryngology-Head & Neck Surgery
It is our great pleasure to announce the UPMC Pittsburgh Otolaryngology Residency Class of 2030! We are delighted to welcome Beatrice Bacon, Ryan Cotter, Tice Harkins, Alejandro Marrero, and Stefanie Seo to our team.


her medical studies at the University at Buffalo.

Otolaryngology Representative, Cleft-Craniofacial Center at UPMC Children’s Hospital
The University of Pittsburgh School of Medicine


Tice Harkins, MD completed his undergraduate studies in Premed/Biomedical Engineering at Penn State and his medical degree at Geisinger University.
Alejandro Marrero, MD earned his undergraduate degree in Biology from the University of Puerto Rico-Mayaguez and his medical degree from the University of Puerto Rico.
Stefanie Seo, MD completed both her undergraduate studies in Public Health and her medical degree at Johns Hopkins University.
We are immensely proud of our graduates who have demonstrated exceptional dedication and skill over the past five years. Their hard work and perseverance have prepared them for the exciting opportunities ahead, and we are confident they will continue to excel in their respective fields. Congratulations to Kelly Daniels, Nicholas Fung, Lauren Gardiner, Nathan Lu, and Terral Patel!

Kelly Daniels, MD will be joining the Skull Base team at UPMC for her Rhinology/Skull Base Fellowship.
Nicholas Fung, MD is heading to Emory University for a Fellowship in Rhinology/Skull Base.
Lauren Gardiner, MD will be pursuing a fellowship in Facial Plastic & Reconstructive Surgery at the University of North Carolina.
Nathan Lu, MD, MPH has accepted a Pediatric Otolaryngology Fellowship at the University of Colorado/Colorado Children’s.
Terral Patel, MD has accepted a faculty position at the University of Minnesota.
We wish them all the best in their future endeavors and look forward to seeing their continued success!
GRADUATING:
Josh Smith: Joining UPMC ENT Faculty
Richard Raad: Joining faculty at Henry Ford Health System in Detroit, MI
Chelsea Gelboin-Burkhart

Chelsea Gelboin-Burkhart, originally from San Diego, California, attended UC Berkeley for undergrad where she studied Molecular and Cellular Biology, followed by medical school at Stony Brook University.
She completed her residency training in Otolaryngology Head and Neck Surgery at the University of Minnesota, where her primary research projects studied the effect of tobacco on wound healing and antioxidant use. Her research interests include genomics of head and neck cancer, cellular senescence and tobacco.
INCOMING: (Continued)
Kelly Staricha

Dr. Kelly Staricha, MD is from Allen Park, Michigan. She earned her undergraduate degree at Northwestern University and attended Medical College of Wisconsin. She completed her residency at Mayo Clinic in Minnesota and plans to specialize in academic head and neck oncology and microvascular surgery.
Future plans: Academic Head and Neck Oncologic and Microvascular Surgery
Yu-Jin Lee

Yu-Jin Lee, MD is from Marietta, Georgia and completed her undergraduate and medical studies and her residency in OHNS at Stanford University. She is excited to join the department in Pittsburgh to further her advanced training in head and neck surgical oncology and reconstruction.
GRADUATING:
Margaret Engelhardt

Margaret Engelhardt, MD completed her undergraduate studies and residency in Otolaryngology - Head & Neck Surgery at the University of Minnesota and medical school at the University of Texas at Houston. She is excited to rejoin the department at the University of Minnesota and the Minneapolis VAMC after fellowship graduation.
INCOMING:
Aneesh Patel

Aneesh Patel is a neurotology fellow at the University of Pittsburgh. He completed undergraduate and medical school training through the Boston University BA/MD program and residency at Boston University Medical Center. His current research interests include healthcare utilization and barriers to healthcare access.
GRADUATING:
Jason Crossley

Jason Crossley will specialize in rhinology and skull base surgery at Allegheny Health Network in Pittsburgh and will be on faculty at Drexel University College of Medicine.
INCOMING:
Kelly Daniels

Kelly Daniels, MD graduated from Sidney Kimmel Medical College at Jefferson University in Philadelphia, and completed an otolaryngology residency at UPMC. Currently pursuing a fellowship in Rhinology and Skull Base Surgery, Dr. Daniels is dedicated to advancing care for patients with sinonasal malignancies, olfactory dysfunction, and advanced inflammatory disease.
Michael Xie

Michael Xie completed his medical school training and residency in Otolaryngology Head and Neck Surgery at McMaster University. He then completed a fellowship in Head & Neck Surgical Oncology and Microvascular Reconstructive Surgery at the University of Toronto. He has expertise in advanced mucosal and cutaneous head and neck cancers and reconstructive surgery. He is a member of the American Head and Neck Society, American Rhinologic Society, and Canadian Society of Otolaryngology. Dr. Xie’s research interests include skull base malignancies, perioperative outcomes and optimization, and the evaluation of diagnostic tests in head and neck surgery.
GRADUATING:
Yoni Reuven Kathryn Deeds
We are proud to celebrate the achievements of our graduating Pediatric Otolaryngology fellows. Your dedication, compassion, and pursuit


of excellence have enriched our program and the lives of the patients and families you’ve cared for. As you take the next step in your careers, we have every confidence that you will continue to make meaningful contributions to our field and uphold the highest standards of clinical care, research, and leadership.
Thank you for being an integral part of our fellowship family. We look forward to seeing all that you accomplish in the years ahead.
Raihanah

Dr. Raihanah Alsayegh earned her Doctor of Medicine from Kuwait University and completed her residency in Otolaryngology–Head and Neck Surgery at McGill University. With a strong foundation in pediatric care, she brings a deep passion for treating children, advancing research, and contributing to medical education. Her clinical experiences have shaped a particular interest in pediatric otolaryngology, drawn by its complexity, continuity of care, and the opportunity to make a lasting impact on young patients’ lives.
Dr. Kylie Perreault earned her Doctor of Osteopathic Medicine from Kansas City University of Medicine and Biosciences in 2020 after completing her undergraduate studies at the University of Michigan. She has completed her residency in Otolaryngology–Head and Neck Surgery at Ascension Macomb-Oakland Hospital, where she has demonstrated strong surgical skills, clinical acumen, and a deep commitment to patient care. Driven by a passion for pediatric otolaryngology, Dr. Perreault is drawn to the specialty for its broad procedural scope, long-term patient relationships, and the profound impact it can have on children’s lives.


Jose P. Zevallos, MD, MPH, FACS
The Eugene N. Myers, MD
Professor and Chair, Department of Otolaryngology-Head & Neck Surgery






Eric W. Wang, MD, FACS
Executive Vice Chair, Department of Otolaryngology-Head & Neck Surgery
Professor, Departments of Otolaryngology, Neurological Surgery and Ophthalmology
Division Chief, Rhinology
Cuneyt M. Alper, MD
Professor, Department of Otolaryngology-Head & Neck Surgery
Carey D. Balaban, PhD
Professor, Departments of Otolaryngology-Head & Neck Surgery, Neurobiology, Communication Science & Disorders, and Bioengineering
Gregory J. Basura, MD, PhD
Director, Global Otolaryngology
Professor, Department of Otolaryngology-Head & Neck Surgery
Zachary Bennett, MD
Clinical Professor, Department of Otolaryngology-Head & Neck Surgery
David H. Chi, MD
Division Chief, Pediatric Otolaryngology, UPMC Children’s Hospital of Pittsburgh
Associate Professor, Department of Otolaryngology-Head & Neck Surgery

Steven B. Chinn, MD
Associate Professor, Department of Otolaryngology-Head & Neck Surgery
Director, Research and Clinical Operations, Computational Pathology & AI Center of Excellence (CPACE)








Garret Choby, MD
Associate Professor, Departments of Otolaryngology-Head & Neck Surgery and Neurological Surgery

Patrick Cody, PhD
Research Assistant Professor, Department of OtolaryngologyHead & Neck Surgery
Kevin J. Contrera, MD, MPH
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery
Christopher L. Cunningham, PhD
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery
Joseph E. Dohar, MD, MS, FACS, FAAP
Professor, Department of Otolaryngology-Head & Neck Surgery
David E. Eibling, MD
Professor, Department of Otolaryngology-Head & Neck Surgery
Joseph M. Furman, MD, PhD, FAAN
Director, UPMC Center for Balance Disorders
Professor, Departments of Otolaryngology-Head & Neck Surgery, Neurology, Bioengineering, and Physical Therapy
Grant S. Gillman, MD, FRCS
Division Chief, Facial Plastic and Reconstructive Surgery, Department of OtolaryngologyHead & Neck Surgery
Associate Professor, Department of Otolaryngology-Head & Neck Surgery
Bridget C. Hathaway, MD
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery


Michele Insanally, PhD
Assistant Professor, Departments of Otolaryngology-Head & Neck Surgery, Neurobiology, and Bioengineering
Noel Jabbour, MD, MS, FACS
Residency Program Director and Vice Chair of Education
Director, Congenital Ear Center at UPMC Children’s Hospital of Pittsburgh
Associate Professor, Department of Otolaryngology-Head & Neck Surgery
Residency Program Director and Vice Chair of Education, Otolaryngology Representative, Cleft-Craniofacial Center at UPMC Children’s Hospital


Jonas T. Johnson, MD, FACS
Emeritus Distinguished Service Professor and Chairman, Department of OtolaryngologyHead & Neck Surgery
Thomas M. Kaffenberger, MD
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery
Seungwon Kim, MD
Director, Shadyside Hospital, Otolaryngology Unit
Associate Professor, Department of Otolaryngology-Head & Neck Surgery

Dennis J. Kitsko, DO
Associate Professor, Department of Otolaryngology-Head & Neck Surgery
Director, Otolaryngology
Subspecialty Medical Student Clerkship at Children’s Hospital of Pittsburgh



Manoj Kumar, PhD
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery
Raymond C. Maguire, DO
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery
Jessica H. Maxwell, MD, MPH, FACS
Chief of Otolaryngology, Pittsburgh Veteran’s Affairs Medical Center
Associate Professor, Department of Otolaryngology-Head & Neck Surgery
Associate Residency Program Director, Department of Otolaryngology-Head & Neck Surgery





Marci Lee Nilsen, PhD, MSN, RN, CHPN, FAAN
Director, UPMC Head & Neck Cancer Survivorship Clinic Co-lead, UPMC Hillman Cancer Center’s Biobehavioral Cancer Control (BCC) Program Professor, Department of Otolaryngology-Head & Neck Surgery

Catherine V . Palmer, PhD
Professor and Chair, Department of Communication Science and Disorders
The University of Pittsburgh School of Health and Rehabilitation Sciences
Professor, Department of Otolaryngology-Head & Neck Surgery
The University of Pittsburgh School of Medicine
Director of Audiology, UPMC


Angela L. Mazul, PhD, MPH
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery
Melissa M. McGovern, PhD
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery

Adele Moatti, PhD
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery
Eugene N. Myers, MD, FACS, FRCS, Edin (Hon)
Emeritus Distinguished Professor and Chairman, Department of Otolaryngology-Head & Neck Surgery
Director, International Visiting Scholars Program




Mohit Singhala, PhD
Research Assistant Professor, Department of OtolaryngologyHead & Neck Surgery
Lead Engineer, CREATES
Joshua D. Smith, MD
Assistant Professor, Department of OtolaryngologyHead & Neck Surgery

Philip Perez, MD
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery
Peter L. Santa Maria, MD, PhD
Professor, Division Chief of Otology & Neurotology Vice Chair of Translational and Clinical Research Department of OtolaryngologyHead & Neck Surgery
The University of Pittsburgh School of Medicine
Director Faculty Innovation, Office of Innovation and Entrepreneurship Adjunct Professor, Bioengineering Carnegie Mellon University
Chloe Santa Maria, MD, MPH
Director, Complex Adult Airway Center
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery
Amber D. Shaffer
Research Assistant Professor

Libby J. Smith, DO, FAOCO
Division Chief, Laryngology Director, Voice Center
Professor, Department of Otolaryngology-Head & Neck Surgery
Carl H. Snyderman, MD, MBA
Vice Chair, Quality & Patient Safety Professor, Departments of Otolaryngology-Head & Neck Surgery, Neurological Surgery, and Bioengineering
Co-Director, UPMC Center for Skull Base Surgery
Co-Director, CREATES


Jeffrey P. Simons, MD, MMM
Surgical Director, Pediatric Thyroid Center, UPMC Children’s Hospital of Pittsburgh
Vice Chair of Faculty Affairs

Ryan J. Soose, MD
Division Chief, Sleep Division Associate Professor, Department of Otolaryngology-Head & Neck Surgery
Matthew E. Spector, MD, FACS
Division Chief, Head & Neck Surgical Oncology & Microvascular Reconstruction
Director, Head & Neck Surgical Oncology & Microvascular Reconstruction Fellowship Professor, Department of Otolaryngology-Head & Neck Surgery
Shaum Sridharan, MD
Associate Professor, Department of Otolaryngology-Head & Neck Surgery
Associate Director, Advanced Head and Neck Surgical Oncology Fellowship

Amanda Stapleton, MD
Associate Professor, Department of Otolaryngology-Head & Neck Surgery
Director, Center for Sinonasal and Rhinology Disorders, Division of Pediatric Otolaryngology
Director, Pediatric Otolaryngology Fellowship Program


Sandra Stinnett, MD
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery
Director, UPMC Swallow Disorders Center
Allison Tobey, MD
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery
Director, Aerodigestive Combined Conference, Children’s Hospital of Pittsburgh
Director, Multidisciplinary Airway Center, Children’s Hospital of Pittsburgh

Thanos Tzounopoulos, PhD
Vice Chair of Basic Science Research, Department of Otolaryngology-Head & Neck Surgery
Professor, Department of Otolaryngology-Head & Neck Surgery
Director, Pittsburgh Hearing Research Center
UPMC Endowed Professor of Auditory Physiology


Lazar Vujanović, PhD
Research Assistant Professor, Department of OtolaryngologyHead & Neck Surgery
Rachel L. Whelan, MD
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery
Co-Director and Professor, Physical Therapy Post-Professional MS Program
Director, Vestibular Rehabilitation Program

Susan L. Whitney, DPT, PhD, NCS, ATC, FAPTA
Professor, Departments of Otolaryngology-Head & Neck Surgery and Physical Therapy
Co-Director and Professor, Physical Therapy Post-Professional MS Program, Director, Vestibular Rehabilitation Program









Ross S. Williamson, PhD
Assistant Professor, Departments of Otolaryngology-Head & Neck Surgery and Neurobiology
Tamara Wincko, MS, CCC-SLP
Director, Speech-Language Pathology Division
Anping Xia, MD, PhD
Research Professor, Department of Otolaryngology-Head & Neck Surgery
Zhongping Xu, PhD
Research Assistant Professor, Department of OtolaryngologyHead & Neck Surgery





Bill J. Yates, PhD
Professor, Departments of Otolaryngology-Head & Neck Surgery and Neuroscience
Vincent Yuan, MD, PhD
Research Assistant Professor, Department of OtolaryngologyHead & Neck Surgery
Christina Yver, MD, MBA
Assistant Professor, Department of Otolaryngology-Head & Neck Surgery
Division Chief, Facial Plastic & Reconstructive Surgery
Yanjun Zhao, MS, MD
Research Assistant Professor
Lori Zitelli, MA, AuD
Managing Audiologist, UPMC Audiology
Adjunct Instructor
Kelly Daniels, MD
Nicholas Fung, MD
Lauren Gardiner, MD










Olivier Bourguillon, MD

Alex Harris, MD

Shivam Patel, MD

Brandon Smith, MD

Kristen Zayan, MD
PGY2 Residents





Francesco Caruana, MD

Wesley Cai, MD, PhD

Sabrina Goyal, MD

Jason Crossley, MD
Advanced Rhinology and Skull Base Surgery
Kathryn Deeds, MD Pediatric Otolaryngology
Micah Harris, MD
Elizabeth Liao, MD
Zoey Morton, MD
Allison Rollins, MD
Jenny Kim, MD

Maryanna Owoc, MD, PhD
Margaret Engelhardt, MD Neurotology

Elizabeth Sell, MD, MSc, MA

Richard Raad, MD
Advanced Oncologic and Microvascular Reconstructive Surgery
Yonatan Reuven, MD, PhD Pediatric Otolaryngology-Head & Neck Surgery

Garret W. Choby, MD received the Clinical Science Runner-Up Award, American Rhinologic Society 70th Annual Meeting, Miami, FL, September 27-28, 2024: Pathologic Dural Invasion is Associated with Regional Recurrence in Olfactory Neuroblastoma: A Multi-Institutional Study.
Kevin J. Contrera, MD, MPH was awarded the University of Pittsburgh Clinical and Translational Science KL2 Scholar, NIHfunded mentored career development award and the Franklin H. Martin Faculty Research Fellowship, American College of Surgeons, Two-year early career award to support research into circulating tumor DNA.
Joseph M. Furman, MD, PhD, FAAN received the 2025 Champion of Vestibular Medicine Lifetime Achievement Award for advancements in research that lead to improvements in clinical care for patients with unexplained dizziness and vertigo.
Marci L. Nilsen, PhD, MSN, RN, CHPN, FAAN named co-lead of UPMC Hillman Cancer Center’s Biobehavioral Cancer Control (BCC) Program.
Carl H. Snyderman, MD, MBA , is the inaugural recipient of the Eugene N. Myers and Joseph C. Maroon Chair of Skull Base Surgery.
Carl H. Snyderman, MD, MBA and Nana Hawwa Abdul Rahman, MS received the Randal Weber, MD Award for Quality, Safety and Value in Head and Neck Oncology. Entitled Work: Improving Prediction of Postoperative Pulmonary Complications Following Oncologic Head and Neck Surgery with Microvascular Free Flap Reconstruction.
Thanos Tzounopoulos, PHD received the Dr. Richard J. Bellucci Pioneer Award in honor of his outstanding contributions and dedication to hearing research.
Eric W. Wang, MD and Shweta Kitchloo received the First Place Poster Award, American Rhinologic Society Combined Otolaryngology Spring Meeting, Chicago, IL, May 8-9, 2024: Characterizing Donor Susceptibility to EBV Infection in the Nasopharynx Using Organotypic Rafts. He also received the Distinguished Service Award, American Academy of Otolaryngology-Head and Neck Surgery.
Susan L. Whitney, DIPT, PhD, NCS, ATC, FAPTA , received the “Citation for Distinguished Service, Pennsylvania Academy of Otolaryngology-Head & Neck Surgery 2025.” The award recognizes non-physician contributions to auditory/ vestibular health across populations.
Women in Otolaryngology (WIO), a group of female otolaryngology attendings and trainees at UPMC created in 2021, meets to discuss the challenges that female surgeons face in the field. Part of a much larger national group that is part of the American Academy of Otolaryngology Head and Neck Surgery, WIO brings in outside speakers to provide knowledge, insight, support, and mentorship.
In the last academic year, the two speakers were Dr. Amber Luong, MD, PhD, Professor and Vice Chair for Academic Affairs in the Department of Otorhinolaryngology-Head & Neck Surgery at McGovern Medical School at UTHealth Houston and Dr. Carol Bradford, MD, MS, Professor and Dean, The Ohio State University College of Medicine, and Vice President for Health Sciences, The Ohio State University Wexner Medical Center.
2025 UNIVERSITY OF PITTSBURGH
AVANT-GARDE HEALTH
ENT RESEARCH ALL STAR S
José P. Zevallos, MD, MPH, FACS
Steven B. Chinn, MD
Garret Choby, MD, MD
Kevin J. Contrera, MD, MPH
Carl H. Snyderman, MD, MBA
Matthew E. Spector, MD, FACS
Chloe Santa Maria, MD, MPH
Peter Santa Maria, MD, PhD
Shaum S. Sridharan, MD
Eric W. Wang, MD, FACS
2025 CASTLE CONNOLLY TOP DOCTORS
José P. Zevallos, MD, MPH, FACS
Joseph E. Dohar, MD, MS, FACS, FAAP
Bridget C. Hathaway, MD
Jonas T. Johnson, MD, FACS
Seungwon Kim, MD
Ryan J. Soose, MD
Carl H. Snyderman, MD, MBA
Matthew E. Spector, MD, FACS
Shaum S. Sridharan, MD
Sandra Stinnett, MD
Eric W. Wang, MD, FACS
2024 TOP SCHOLARS LIST BY SCHOLARGPS
José P. Zevallos, MD, MPH, FACS
Matthew E. Spector, MD, FACS

“These speakers spent their time meeting with our group, sharing their careers, providing guidance for navigating training and career building, how to find mentorship and sponsorship, and answered our questions,” said Dr. Amanda Stapleton, MD, Associate Professor, Department of Otolaryngology-Head & Neck Surgery, Director, Center for Sinonasal and Rhinology Disorders, Division of Pediatric Otolaryngology, and Director, Pediatric Otolaryngology Fellowship Program.
WIO also had its annual retreat and a WIO moment at the Pennsylvania Association of Otolaryngology meeting, where some members met with Dr. Sujana Chandrashakur, past president of the Academy.

The Eye & Ear Foundation, an independent 501(c)(3) organization, was founded in 1985 to foster support for the Departments of Ophthalmology and OtolaryngologyHead & Neck Surgery at the University of Pittsburgh through the generous support of individuals and organizations.
In supporting these world-class Departments, we hold ourselves to the same high standards. The goal is to keep moving forward, expanding EEF’s support network, and helping the Departments of Ophthalmology and Otolaryngology-Head & Neck Surgery stand peerless in the distinction of research and education and, ultimately, the highest level of care provided to our patients.
• Bequests
• Cash
• Charitable Gift Annuities
• Charitable Trusts
• IRA Charitable Rollover Gift
• Life Insurance Gifts
• Stock Transfers
“The Eye & Ear Foundation’s support enhances patient care,” said CEO Lawton Snyder. “We do this by supporting the work of the outstanding clinical and research faculty in the Departments of Ophthalmology and Otolaryngology-Head & Neck Surgery at the University of Pittsburgh. EEF has played a major role in making these Departments worldwide leaders in the field and in research and development pathways for care.”
To learn more about the Foundation or to support the Department of OtolaryngologyHead & Neck Surgery, please visit eyeandear.org or scan this QR code.

University of Pittsburgh Department of OtolaryngologyHead & Neck Surgery
Eye & Ear Institute, Suite 500 203 Lothrop Street Pittsburgh, PA 15213
Supporting Research to Improve how we Hear, See, and Live
Supporting Research to Improve how we Hear, See, and Live
University of Pittsburgh Department of OtolaryngologyHead & Neck Surgery
Eye & Ear Institute, Suite 500 203 Lothrop Street Pittsburgh, PA 15213
Communications Team
L isa A. Goldstein, Senior Writer and Editor
Kelsey Muchnok, Content Strategist/Photographer
Christine Wilson, Operations Manager
Kathy Troy, Director, Marketing & Communications katherine@eyeandear.org
More about the Department of Otolaryngology-Head & Neck Surgery at the University of Pittsburgh can be found at www.otolaryngology.pitt.edu/ or scan the QR code.
