










TAPPING INTO THE IMMUNE SYSTEM TO DIAGNOSE AND TREAT HEARING LOSS
PITT A MAJOR COMPONENT OF ARPA-H PROJECT ON EYE TRANSPLANTATION
EXPANDING GLOBAL OUTREACH GIFT HONORS AN ENDURING COMMITMENT













TAPPING INTO THE IMMUNE SYSTEM TO DIAGNOSE AND TREAT HEARING LOSS
PITT A MAJOR COMPONENT OF ARPA-H PROJECT ON EYE TRANSPLANTATION
EXPANDING GLOBAL OUTREACH GIFT HONORS AN ENDURING COMMITMENT

The Eye & Ear Foundation 5 9 6 7 8 10 A FOCUSED APPROACH TO TREATING RARE OCULAR DISEASES
VOCAL OUTREACH: CARE BEYOND THE CLINIC
VIRGINIA MONTANEZ DISCOVERS THE VISION INSTITUTE 11
Welcome to the latest edition of the Sight + Sound newsletter, brought to you by the Eye & Ear Foundation.
At the Eye & Ear Foundation, we are committed to advancing the fields of ophthalmology and otolaryngologyhead & neck surgery through innovative research and exceptional patient care. Our mission is to improve the quality of life for individuals affected by diseases and disorders of the eye, ear, nose, throat, head and neck. Your support is crucial to our success.
In this edition, we highlight several remarkable initiatives, including groundbreaking research projects, community outreach programs, and advancements in patient care that are making a significant impact.
Your engagement and generosity enable us to continue this vital work. Together, we are making a difference and paving the way for a brighter future. Thank you for being part of our journey!
Warm regards,

Lawton Snyder Chief Executive Officer
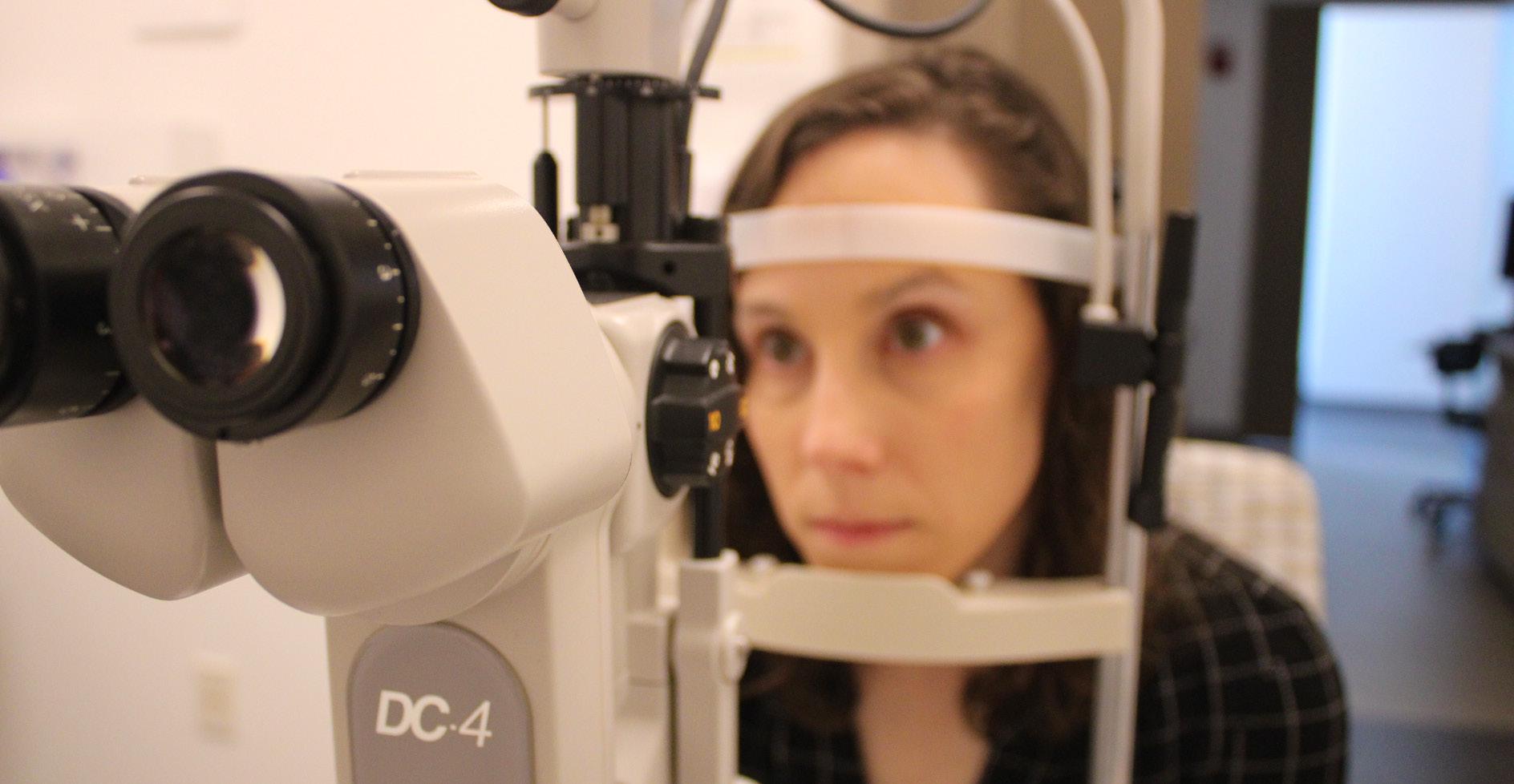
Orphan eye conditions present several unique challenges but addressing them is just par for the course at the Department of Ophthalmology in the UPMC Vision Institute.
What is an orphan eye condition? It is a rare eye disorder that affects a small number of individuals, typically fewer than 200,000 people in the United States, according to Dr. Joseph Martel, Assistant Professor of Ophthalmology and Vice Chair, Patient Experience and Access. Several inherited retinal degenerations fall under this designation, for example.
The challenges include genetic complexity as many have diverse genetic causes with hundreds of potential mutations; small patient populations, which make clinical trials difficult to organize and less financially viable; slow disease progression, which complicates measuring treatment efficacy in clinical trials; and limited research funding, as less common conditions often attract less investment.
It is important to research and focus on orphan eye conditions for several reasons. They have a significant impact on quality of life. Researching rare genetic eye conditions often leads to broader understanding of eye biology and disease mechanisms. And there is an ethical imperative, “ensuring healthcare advances benefit everyone, not just those with common conditions,” Dr. Martel said. Last, but not least, “with improved genetic testing and diagnostic capabilities, there’s theorical opportunity to intervene before significant vision loss occurs.”
To that end, the Vision Institute boasts a multidisciplinary retinal dystrophy clinic, which integrates retina specialists, ophthalmic genetic counselors, and low vision therapy optometrists. A low vision rehabilitation team helps patients maximize their remaining visual capabilities. The Vision Institute is participating in innovative studies to better understand these diseases as well as evaluating different approaches, including gene therapies. And the Vision Institute is also involved in the Foundation Fighting Blindness’ “UNIRARE” study.
To schedule an appointment, call 412-647-2200.

The Department of Otolaryngology-Head & Neck Surgery at the University of Pittsburgh has started an immunological hearing division thanks, in part due to a significant donation from the Greg Carr Foundation.
“There are a lot of conditions in hearing that we don’t have a reason for, such as sudden sensorineural hearing loss, Meniere’s disease, and fluctuating hearing loss.” said Dr. Peter Santa Maria, MD, PhD, Chief, Division of Otology/Neurotology and Co-Leader of this new division. “We call them idiopathic.”
So, the idea is to have an “immune mediated inner ear center that is a world leader where we can start to unlock some of the mechanisms that cause these things,” Dr. Santa Maria explained. “We can start to understand and diagnose patients
correctly according to immune system issues and potentially offer new immune treatments that might be better than steroids for helping patients with hearing loss.”
This Division will house discovery, translational, and clinical research.
Animal models will be used to study the mechanisms and how the immune system in the ear works, so potential therapies can be better identified. A couple of different targets that act on macrophages or the innate immune system are already being worked on. The innate immune system seems to underlie a lot of why hearing loss occurs, such as noise-induced hearing loss. Some people get a large degree of hearing loss when they are exposed to a little noise, yet others don’t end up with much hearing loss despite a lot of noise exposure. One of the things underlying that is the immune response to that noise and the protective mechanisms that do or


Dr. Peter Santa Maria, MD, PhD, Chief, Division of Otology/ Neurotology and Co-Leader of the new Immunological Hearing Division
do not kick in that can prevent that. There are also potential treatments for hearing loss associated with vestibular schwannoma.
On the translational side, the Division is also looking at potentially doing some drug discovery and drug development for these targets. On the clinical side, “we want to make sure that we’re not only delivering the best level of care to all these patients with these conditions, but also working them up, seeing them appropriately, and giving them the best available therapies,” Dr. Santa Maria said. In addition, they are looking to test their samples to look for immune mediated markers that can drive future research on the translational side.
“We’re aiming to be the first Division that is complete from discovery research through translation into clinical research,” Dr. Santa Maria said.

To make whole eye transplants that restore sight a reality, the Department of Ophthalmology at the University of Pittsburgh is part of a project team for a program called Transplantation of Human Eye Allografts, or THEA.
The project will receive an up to $56 million award from the Advanced Research Projects Agency for Health (ARPA-H), an agency within the U.S. Department of Health and Human Services (HHS). Pitt will likely receive around $9 million for its role in the project, the largest Pitt has received for optic nerve regeneration.
“It’s a very audacious project to have a living functional human eye transplant in a patient and then the patient has functional vision after the surgery,” said John Ash, PhD, Vice-Chair of Ophthalmology and Director of Research. “A successful eye transplant has occurred already, but it’s not functional, so the eye can’t process images and connect to the brain. We want to extend that and go into the next step where we get the eye to reconnect to the brain.”
Jeffrey Goldberg, MD, PhD, Chair of Ophthalmology at the Byers Eye Institute at Stanford University, will be the primary investigator leading more than 40 doctors, researchers, and industry experts from around the country. José-Alain Sahel, MD, Ophthalmology Chair at the University of Pittsburgh, will co-lead.
Dr. Sahel praised the strong collaborations necessary for scientific breakthroughs. “By combining the deep knowledge about ophthalmology, tissue preservation and regeneration, immunology, and surgery of world-class scientists at Byers Eye Institute, University of Pittsburgh, and consortium members from top institutions, we are well-positioned to set the foundational steps toward restoring vision using a whole eye transplant.”
This work is not anything new for Pitt, as this project simply taps into what the Department has already been doing.
The major hurdle is removing the eye from a donor and preserving it for up to 48 hours so that it can be collected and processed before being matched with the donor recipient. Hence, the first phase of the project is removal and preservation, which is being done by a team at Pitt led by Leah Byrne, PhD; Ethan Rossi, PhD; and Shauhua Pi, PhD, with Dr. Sahel. They will also measure its functioning and survival. This is the THEA program’s technical area 1.
Technical area 2 is looking at different ways to stimulate the eye. “We can stimulate the eye to regrow ganglion cell nerve fibers to go from the retina all the way to various targets in the cellular system,” Dr. Ash said. A large group of people at Pitt including Dr. Ash, Larry Benowitz, PhD; Kun-Che Chang, PhD; Takaaki Kuwajima, PhD; Boris Rosin, MD, PhD; and Tonya Stefko, MD, are looking at various strategies to apply to ganglion cells so they survive when the optic nerve is cut. The goal is to stimulate them to grow into the reconnected optic nerve, and then the cortex, where they will allow functional vision. Ian Sigal, PhD, Director, Image Acquisition and Analysis Core Module, Ophthalmology and Visual Sciences Center, Dr. Kuwajima, and Stephen Badylak, DVM, PhD, MD, from the McGowan Institute for Regenerative Medicine, are looking at ways to develop nerve wraps to allow the two ends of nerve fibers to align and then regrow. At least six members of the group at Pitt are involved in this part of optic nerve regeneration, the largest single group.
Technical area 3 involves implanting an eye into animals or patients and then getting the other components to work, like reconnecting to the blood vessels and reconnecting the nerves. To do this, the immune system must be blocked to prevent rejection. Heath Skinner, MD, PhD, Chair & Medical Director of Radiation Oncology Clinical Networks, Radiation Oncology, specializes in tissue and transplant rejection. He will look at ways to apply appropriate immune suppression to block tissue rejection. Walter Schneider, PhD, Professor of Psychology at Pitt, will look at mapping the structure of the optic nerve so it can be determined whether once reconnected and regrown, if the entire structure of the optic nerve from the back of the eye all the way into the cortex needs to be regenerated. All technical area groups will work concurrently.
“It’s really an ambitious project,” Dr. Ash said. “It’s hard to say whether we’ll have final success at the end. We will make a lot of progress in understanding how to keep ganglion cells alive and functioning and where we currently stand in how to promote axon regeneration. If we get to a certain point – such as achieving through the second technical area– the chances of succeeding in an actual transplant go up dramatically.”

The Department of Otolaryngology-Head & Neck Surgery has expanded its global outreach, thanks to the addition of Dr. Gregory J. Basura, MD, PhD. His leadership in this area -- in which he has worked to develop sustainable educational and clinical initiatives in underserved nations -- continues with his Departmental position as Director of Global Outreach.
Dr. Basura helped launch the first otology fellowship established in Africa in 2022. He is continuing his involvement in the program, which is about to graduate its third fellow. Dr. Basura’s role is a weekly Zoom lecture for the fellow, along with twice a year in-person visits to work in the temporal bone lab with the fellow. In November 2023, Dr. Basura launched the African Otological Society, a once per month online meeting to build otology and audiology capacity in Africa.
Dr. Basura is also overseeing the International Visiting Scholars Program, started by Dr. Eugene Myers, MD, FACS, FRCS, Emeritus Distinguished Professor and Department Chairman. The global partnership program was created to provide visiting international providers an opportunity to shadow in the clinic and operating room. Some have stayed longer than the typical onemonth rotation to engage in research. “I am honored
Dr. Gregory J. Basura, MD, PhD Director, Global Otolaryngology

to oversee this phenomenal program started by Dr. Myers, who is considered the father of global outreach in otolaryngology,” Dr. Basura said.
Other current global efforts include building long-term medical educational partnerships with Mozambique and Peru. “We have a cooperative with South Africa and Dr. Johan Fagan who trained here in Pittsburgh and completed fellowships in otology and head and neck surgery,” Dr. Basura said.
From a clinical/patient care standpoint, Dr. Basura brings a set of skills in lateral skull base surgery that are being broadened and implemented with his neurosurgical colleagues. He was also recently awarded a RO1 grant from the National Institutes of Deafness and Communications Disorders to investigate objective brain changes in human tinnitus using innovative brain imaging with functional near infrared spectroscopy (fNIRS). He is also investigating using fNIRS to study brain plasticity in patients with single-sided deafness and post-cochlear device implantation.
Dr. Basura’s labs are getting up to speed and data will be collected in the near future. “I hope to have meaningful data to share in the next few months,” he said.
Diane Barati’s late parents generously supported the Eye & Ear Foundation. This motivated her to continue doing so in their memory to honor them.
Diane’s parents both struggled with age-related macular degeneration, which prompted them to support research to find a cure. They also had hearing loss. She decided to create two endowed research funds – one for the Department of Ophthalmology, and one for the Department of Otolaryngology-Head & Neck Surgery -because the money is held by EEF, and she can add to it every year.
“We live in a sighted world and people who lose their vision have their lives extremely negatively impacted by that loss,” Diane said. “It is a great privilege to be able to play a small part in the ongoing effort to cure macular degeneration and to help maintain a higher quality of life for those afflicted by it. As someone who has lived with vision impairment, I also greatly appreciate the importance of maintaining good hearing, which is why I created an endowment for hearing research as well.”
Indeed, establishing an endowment allows a donor to establish a legacy that will ensure their philanthropic interests are carried out beyond their lifetime. Endowments also provide stability to the organization that the donor supports, enabling it to weather economic, social, and political shifts. “This ensures the continuation of support even during challenging times,” EEF CEO Lawton Snyder said.
What exactly is an endowment? It is a financial asset, of donated funds or other property, that is invested to generate income for a nonprofit organization. The principal amount of the donation is kept intact while the investment income is used to support the organization’s mission or specific programs as designated by the donor.
“Endowments are vital for the Eye & Ear Foundation as they provide the financial foundation needed to support our mission of improving vision and hearing health, voice, or cancers of the head and neck through research, innovation, and patient care,” Snyder said. “If you have any more questions or need further details, feel free to contact us!”


The Voice, Airway & Swallow Center within the Department of Otolaryngology-Head & Neck Surgery has always strived to provide tailored outreach to the community. Director Dr. Libby Smith, DO, FAOCO, is pleased to announce their ongoing and new initiatives to engage the community in health and wellness in voice.
“Voice is critical for everyone’s ability to communicate and engage with other, as well as be advocates for themselves,” she said. “Voice production is often taken for granted until there is an issue. Thus, we believe it is important to engage and educate the community about what they can do to prevent voice injury in addition to how to go about rehabilitation when needed.”
This year, Dr. Chloe Santa Maria, MD, MPH, initiated a new Vocal Injury Prevention (VIP) program for the resident artists of the Pittsburgh Opera to extend current support of the opera. Dr. Santa Maria described the program as “a way to educate and empower resident singers regarding vocal health and injury prevention, as well as provide a targeted vocal health plan for each singer.” She called it an overwhelming success and well received by Pittsburgh Opera artists.
For the general community, Nichole Sommers, PA-C, is heading the Vocal Outreach Program, which provides education seminars to local high school and collegiate music programs, worship groups, and other professional voice users, like teachers.
Tracey Thomas, CCC-SLP, one of the Center’s senior speech-language pathologists, has been integral in the success of the vocal outreach programs for years. “Our Vocal Outreach Program is important because it educates both vocational and avocational voice users in normal voice function and voice disorders,” she said. “Most people do not realize the complexity required for voice
production. Even less known is how to prevent voice problems before they face a challenging voice issue.”
Each outreach includes an interactive presentation of vocal anatomy, physiology of phonation, common voice disorders, and prevention strategies to optimize vocal health. Additionally, team members introduce voice therapy techniques and host Q&A segments for personalized learning.
By centering programs on health and wellness principles, the Center fosters an environment for both prevention and treatment via community engagement. “Through our Vocal Outreach Programs, we aim to empower voice users, provide resources, foster professional partnerships and highlight the importance of seeking a medical voice evaluation when needed,” Thomas said. “As specialty healthcare providers in the city of Pittsburgh, we take pride in collaborating with a variety of organizations to deliver these valuable programs.”
“The response has been incredibly positive,” said Sommers. “Many groups have shown great enthusiasm, expressing excitement about building connections with our laryngology team and starting important conversations about vocal health. Our local community groups have shown a genuine interest in learning more about their voices and how to care for them, and many have highlighted how the vocal wellness seminars provide valuable insights and resources for their groups. It has been great to see such a welcoming and engaged community, eager to further explore and prioritize vocal wellness.”
“Our expert team has passion for voice and education. Everyone has dedicated their professional life to help others use their voice most effectively,” Dr. Smith said. “Engagement with the community is key to what we do. We want everyone to have a voice.”
Virginia Montanez recently visited the one-stop-shop ophthalmology jewel in Pittsburgh that is the Vision Institute at UPMC Mercy Pavillion.
Montanez is a familiar name in these parts. Known for her former PittGirl blog, the humorist now writes about life in Pittsburgh on Substack and published her first novel. She pens essays and columns when she’s not working on her forthcoming Pittsburgh history app, PastFinders, or studying for her master’s in history.
So when she posted on Bluesky, “For a few weeks I’ve been dealing with some scary vision issues. I got good news today, but I wanted to tell you, Pittsburgh, how lucky we are to have the UPMC Vision Institute at the new Pavilion at Mercy. Incredibly sincere, thorough care by every doc I saw right up until 4 pm today, Christmas Eve,” we wanted to find out more.
Remarkably candid about her experience, Montanez shared that she has worn eyeglasses or contacts for nearsightedness since she was a preteen. About five years ago at age 45, she started noticing vision issues and “floaters,” at which time it was noted that her optic nerves were pale and “huge.” Tests ruled out brain tumors and other more serious ailments.

Last October, Montanez began struggling with computer work. It was so bad that by December, she was barely able to finish her penultimate semester of graduate school. She could tell her vision had changed.
“I did a bit of research to see if there was a way I could combine all of my vision care into one place, and that’s how I learned of the Vision Institute at UPMC Mercy,” Montanez said.
Montanez brought all her eye health paperwork for her appointment with Dr. Chanin Funair-Woods, so she could see the complexity of her case. “Compounding the issue was a rare double carotid dissection I’d suffered 10 years ago that was never explained, but was thankfully treated without catastrophe,” Montanez said.
“Additionally, I’m profoundly hearing impaired, so my vision is exceptionally precious to me. Dr. Woods spent quite a bit of time with me and was able to determine that my color perception in my right eye had diminished while the vision in my left eye had worsened by two full steps since just February.”
Montanez was fitted for computer glasses with blue light blocking and referred to the Neuro-Ophthalmology Department for additional evaluation.
The next visit was with Dr. Islam Zaydan, who diagnosed Montanez with optic nerve disease. He screened her for other ailments that might be affecting her optic nerves and referred her to Dr. Asad Durrani.
Dr. Durrani explained exactly what was happening to her optic nerves, how it was slowing the dilation speed of her pupils, impacting her color perception and vision. He told her he does not believe she is in any danger of losing her eyesight in the immediate future, and that he suspected a genetic issue was at play, much like her hearing loss.
“He was incredibly patient answering my questions and I was the last patient out of that Department on Christmas Eve at 4 pm,” Montanez said.
Montanez’ brain MRI came back clean, and genetic testing was approved by the insurance company. As she awaits the genetic testing results, she is grateful for the care she has received.
“I honestly only transferred my care to the Vision Institute because it seemed to be the only one-stop-shop in the city where I could have all of my eye doctors working as a team, sharing information with each other about my care,” she shared. “It felt like it had been a long while since an eye doctor was really hearing me instead of just trying to fit me for glasses and sending me on my way.
I was so grateful to have been given such thorough and meaningful care by the entire team that I wanted to share with the rest of the city what a valuable resource it is for anyone with vision issues, and that’s when I decided to share my experience on my social media accounts.
Regardless of what all these upcoming tests reveal, I’m fully confident I’m getting the best possible vision care in Pittsburgh.”
eyeandear.org
203 Lothrop Street
Suite 251 EEI
Pittsburgh, PA 15213
412.864.1300 O
412.864.1305 F

If you no longer wish to receive our newsletter, please submit requests to our mailing address, or email optout@eyeandear.org
The official registration and financial information of the Eye & Ear Foundation may be obtained from the Pennsylvania Department of State by calling toll free, within Pennsylvania, 1-800-732-0999. Registration does not imply endorsement.

The Eye & Ear Foundation of Pittsburgh is a nonprofit 501 (C)(3) organization. Our mission is to support the research and academic efforts of the Departments of Ophthalmology and Otolaryngology-Head & Neck Surgery at the University of Pittsburgh. Donations to support our research initiatives can be made online at eyeandear.org or by returning the enclosed envelope. For more information on the Foundation, our research, or the articles in this newsletter, please contact Katherine Troy, Director of Operations, at katherine@eyeandear.org or 412-864-1300.
Medical Disclaimer: The Eye & Ear foundation does not assume any responsibility or risk for the use of
risk. All information and content found in this newsletter were created for educational purposes
your physician or another qualified health provider with any questions you may have regarding
We encourage you to view our full disclaimer by visiting the eyeandear.org website.
The Eye & Ear Foundation, an independent 501(c)(3) organization, was founded in 1985 to foster support for the Departments of Ophthalmology and Otolaryngology–Head & Neck Surgery at the University of Pittsburgh through the generous support of individuals and organizations.
In supporting these world-class Departments, we hold ourselves to the same high standards. The goal is to keep moving forward, expanding EEF’s support network, and helping the Departments of Ophthalmology and Otolaryngology–Head & Neck Surgery stand peerless in the distinction of research and education and, ultimately, the highest level of care provided to our patients.
“The Eye & Ear Foundation’s support enhances patient care,” said CEO Lawton Snyder. “We do this by supporting the work of the outstanding clinical and research faculty in the Departments of Ophthalmology and Otolaryngology–Head & Neck Surgery at the University of Pittsburgh. EEF has played a major role in making these departments worldwide leaders in the field and in research and development pathways for care.”
• Bequests
• Charitable Gift Annuities
• Charitable Trusts
• IRA Charitable Rollover Gift
• Life Insurance Gifts
• Stock Transfers
• Cash
Online donations are accepted at eyeandear.org checks can be mailed to
Eye & Ear Foundation
203 Lothrop Street Suite 251 EEI Pittsburgh, PA 15213