






Imagine a world where the sounds of laughter, conversation, and music fade away. As I began to experience hearing loss, that world became my reality. My relationships suffered, my joy diminished, and I found myself increasingly isolated. The fear of being left out loomed large, and the silence felt suffocating. Those around me couldn’t see the struggles I faced, but the impact on my life was profound.
and most people have a loved one with hearing loss and know how it has impacted their lives.
• Over 1.5 billion people around the world, about 20% of the population, live with hearing loss.
• 1 in 500 infants are born with or will develop hearing loss in early childhood in the United States.
• 5% of all adults and more than 50% of seniors in the United States have disabling hearing loss.
• 10% of adults live with chronic tinnitus with 2% having severe tinnitus.
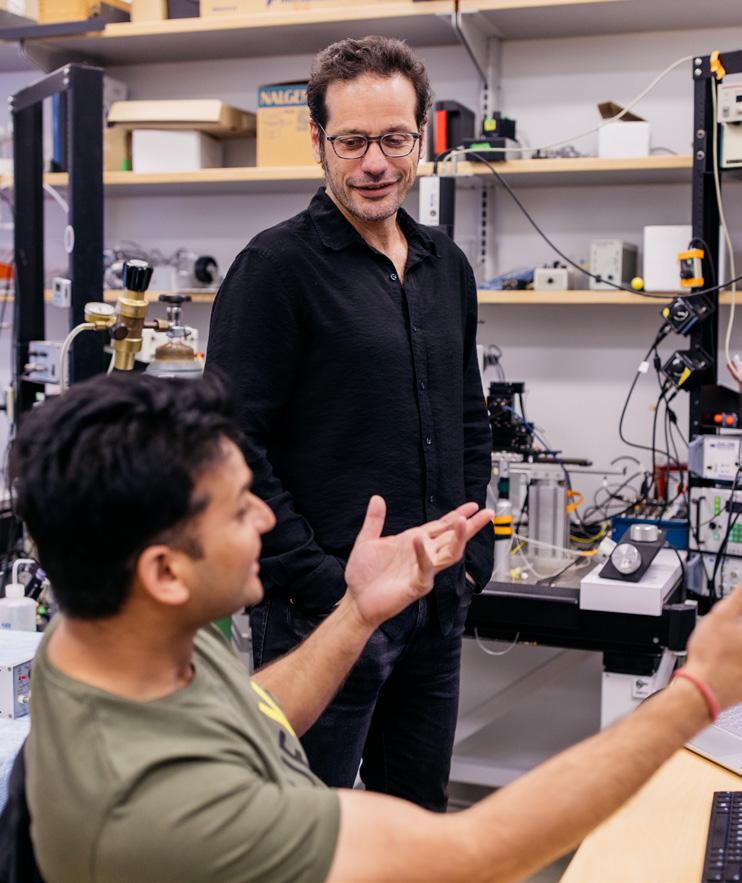
• Common causes of hearing loss include aging, noise exposure, ear infections, and genetics.
• In children, hearing loss delays language development and limits access to future education and employment, among numerous other challenges.
• In older adults, hearing loss leads to social isolation, loneliness, anxiety, and depression. Hearing loss also can increase the risk of falls and other accidents.
• Having hearing loss leads to memory and concentrations issues and is associated with cognitive decline.

We stand at a critical juncture in our research for hearing loss and tinnitus. Despite our advancements, there remain too many hearing conditions that current treatments can’t effectively address. The time for action is now. We urgently need innovative diagnostics and treatments to transform lives, and we are on the brink of groundbreaking discoveries in hearing and tinnitus research. Let’s use everything we have to take an accelerated pathway to get there.”
- Peter Santa Maria, MD, PhD Professor, Division Chief, Otology & Neurotology

The University of Pittsburgh stands at the forefront of hearing and tinnitus research, recognized for its leadership in discovery, clinical treatment, and innovation. By uniting one of the largest healthcare systems in the world with one of the highest ranked groups focused on hearing research, it fosters a dynamic environment for advancement. This collaboration between clinicians and scientists is instrumental in developing effective solutions for hearing challenges.
Private funding empowers us to pursue bold, high-risk research with the potential for significant rewards. It facilitates groundbreaking discoveries that can overcome current obstacles, accelerating the introduction of new treatments into clinical settings. Additionally, this support creates multiple pathways for advancing the search for effective cures for hearing loss.
Pittsburgh is a hub for hearing device innovation, particularly with cochlear implants and personalized solutions like Earflo, which leverages user experience. The Pittsburgh CREATES Lab plays a vital role in this landscape, fostering collaboration between hearing researchers and industry to develop advanced technologies.

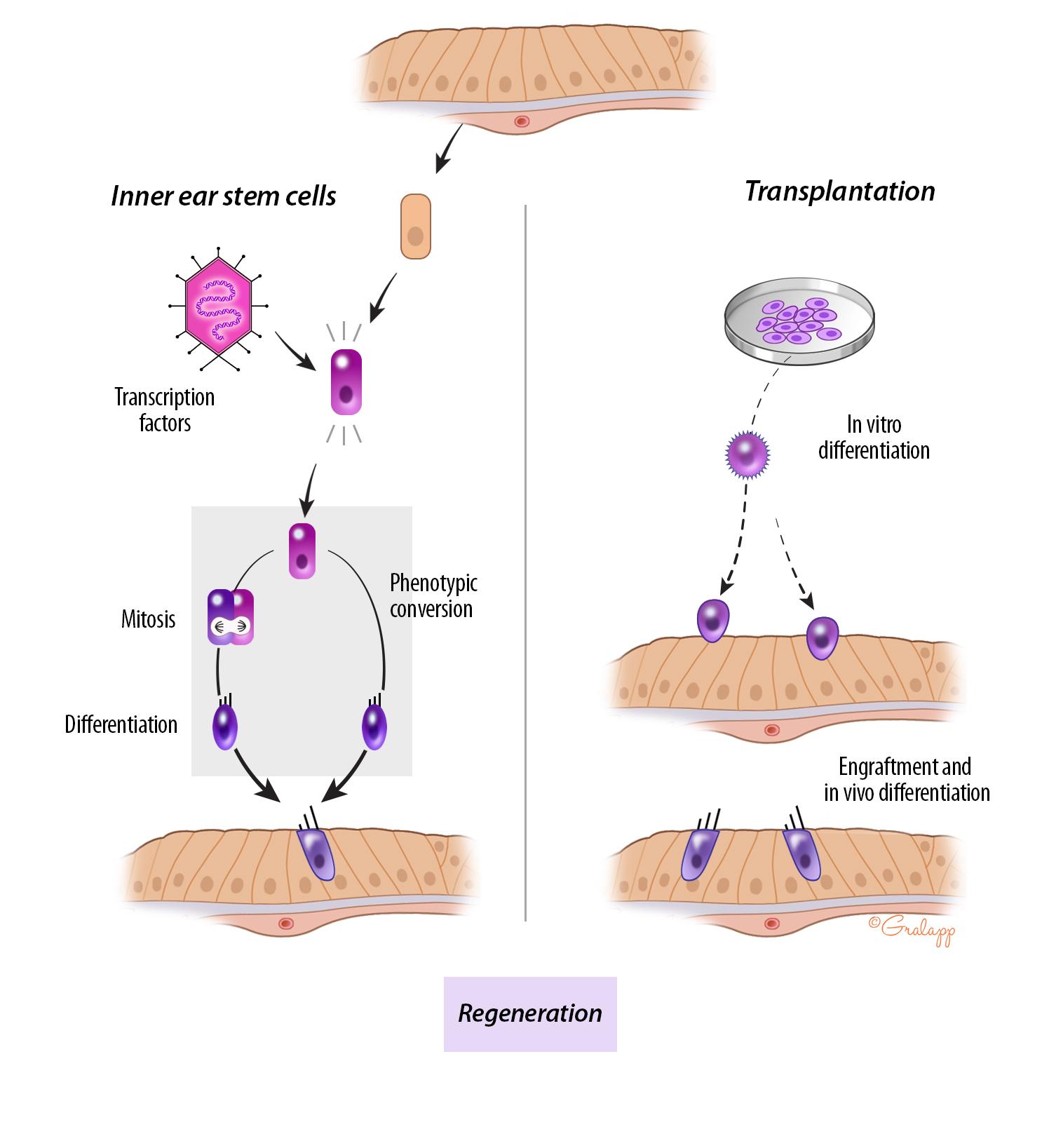
Research in stem cell therapy for hearing loss aims to regenerate damaged auditory cells and restore hearing function. Pittsburgh scientists are investigating the use of stem cells to repair or replace hair cells in the inner ear, which are crucial for hearing but do not naturally regenerate.
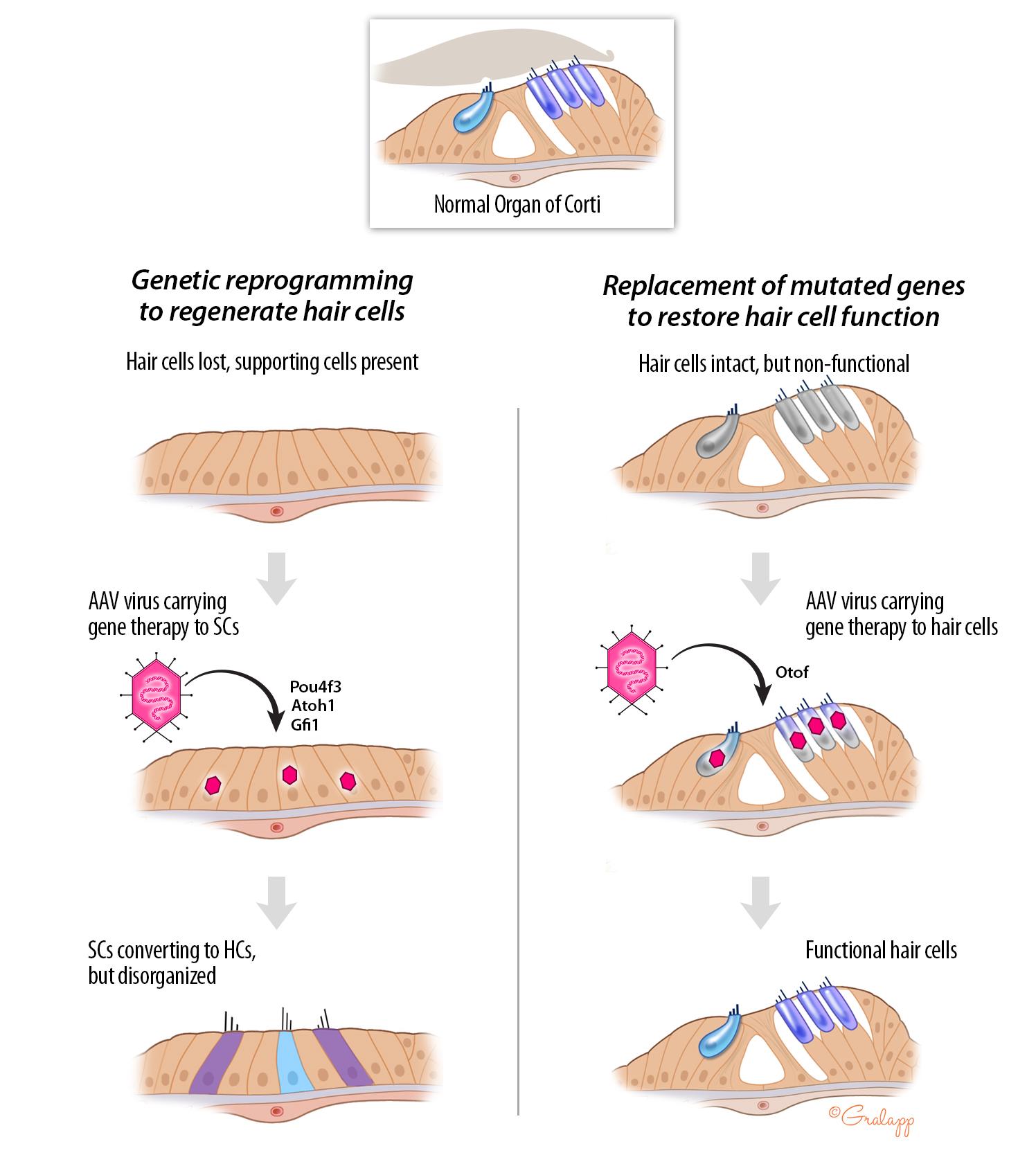
Gene therapy research for hearing aims to address genetic hearing loss by delivering therapeutic genes that can restore or improve auditory function. Researchers are exploring various strategies, including developing some lead candidates for gene therapy being taken forward towards the clinic.
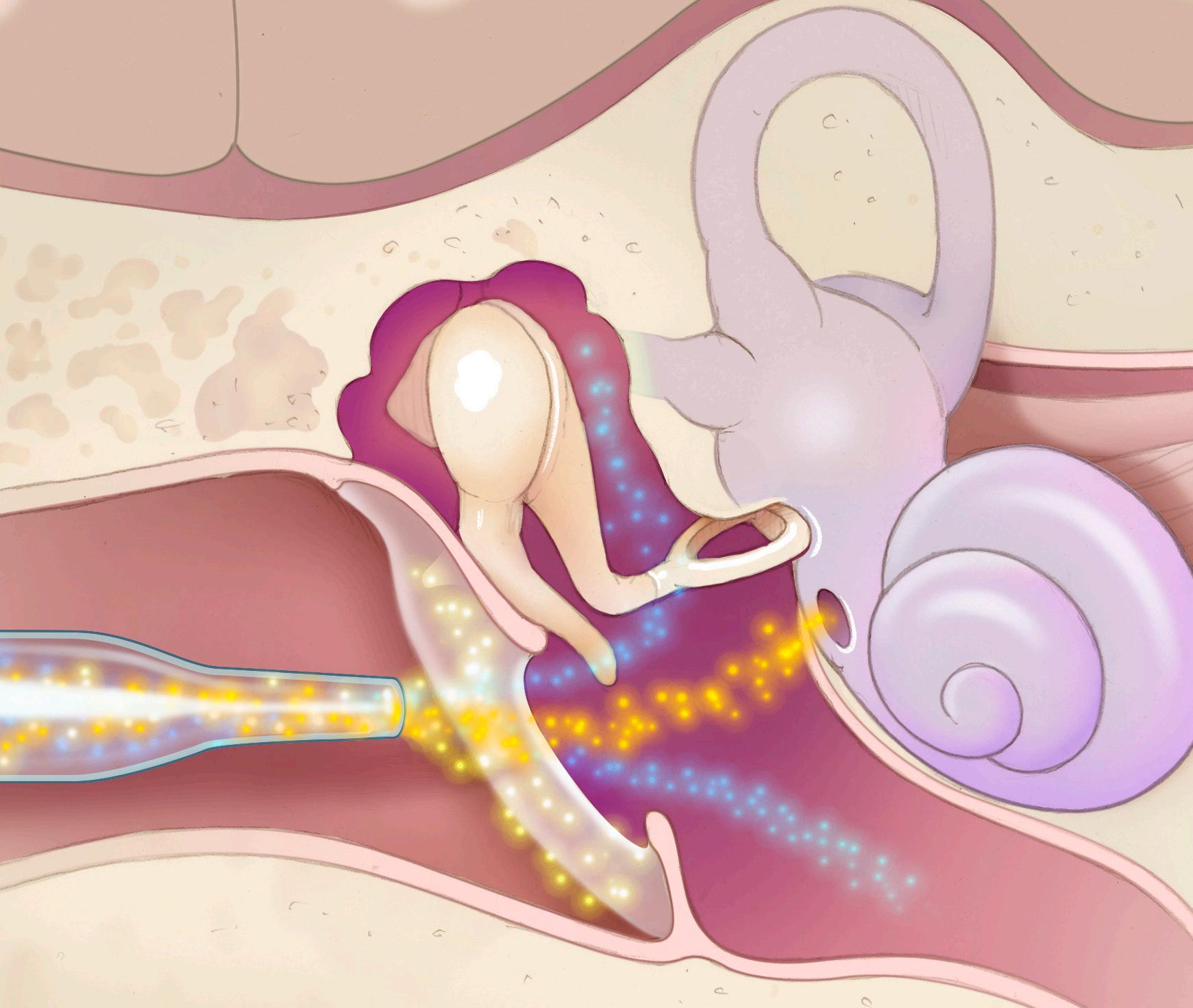
Molecular and Nano Therapy in hearing research focuses on utilizing molecular techniques and nanotechnology to treat hearing loss and related auditory disorders. This approach involves the development of targeted drug delivery systems, which can effectively transport therapeutic agents to specific sites in the auditory system, potentially reversing damage to hair cells or other auditory structures.
Initiatives in Pittsburgh by otologists and audiologists provide essential hearing healthcare services to underserved communities. These programs often involve mobile clinics and community partnerships, making screenings, consultations, and educational resources more accessible to residents in remote areas. By addressing barriers to care we aim to better the quality of life for individuals with hearing loss in Pittsburgh’s rural regions.
Global outreach in hearing focuses on expanding access for individuals with hearing loss worldwide. The initiative involves collaborating with international organizations, including the Gorongosa National Park in Mozambique, otolaryngologists in Ukraine, and many others, to provide training, resources, and innovative treatment methods, enhancing the quality of care in underserved communities.
Pittsburgh CREATES (Center for Research, Evaluation, and Advanced Technologies for Health Systems) focuses on enhancing healthcare delivery through research, technology, and collaboration led by OtolaryngologyHead & Neck Surgery. By integrating cutting-edge innovations Pittsburgh CREATES promises to solve many unmet needs in hearing.
Vertigo and balance problems significantly impact individuals with hearing loss, compounding their challenges. The inner ear, responsible for balance, is closely linked to hearing; dysfunction can lead to both auditory and vestibular issues. Individuals may experience dizziness and unsteadiness, increasing the risk of falls and injuries. This often results in reduced mobility and social isolation, as people may avoid situations requiring balance. Researchers are advancing in-office testing and developing devices to capture vertigo attacks at home, aiming to improve diagnosis and management for those affected.
By addressing balance disorders often associated with auditory issues, this specialized therapy helps patients regain stability and confidence in their movement. Improved vestibular function can lead to better overall physical health and reduce the risk of falls. Additionally, a holistic approach that includes auditory and vestibular assessments fosters a comprehensive understanding of the individual’s needs, promoting tailored interventions for optimal outcomes. Researchers are developing tools to optimize rehabilitation in the home and looking into the impact of vestibular therapy on tinnitus management.












Peter Santa Maria, MD, PhD, Co-Director Professor and Chief, Otology/Neurotology and Vice Chair of Translational and Clinical Research
• Tympanic Regeneration
• Immune Mediated Inner Ear Disease
• Chronic Ear Infections
Greg Basura, MD, PhD Professor and Director of Global Health
• Tinnitus Devices
• Implantable Hearing Devices
• Global Health
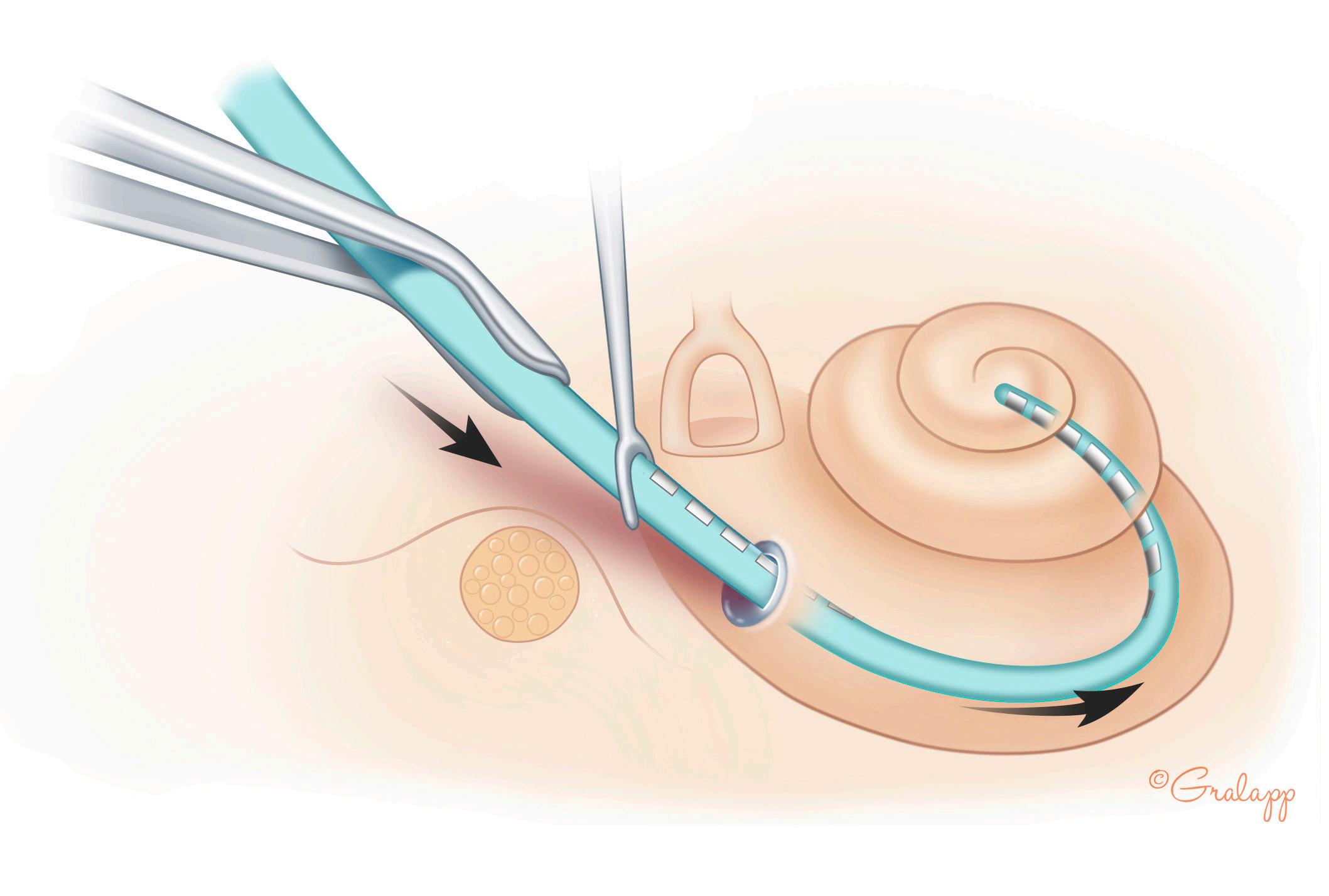
Hari Bharadwaj, PhD
Assistant Professor
• Neural Mechanisms Of Listening-In-Noise
• Addressing Suprathreshold Hearing Deficits
Patrick Cody, PhD Research
Assistant Professor
• Artificial Intelligence
• Machine Learning



Christopher L. Cunningham, PhD
Assistant Professor
• Genetics Of Hearing Loss
• Gene Therapy
• Critical Auditory Proteins
Joseph Furman, MD, PhD Professor, Director, UPMC Center for Balance Disorders
• Otoneurology
• Vestibular Disorders
• Balance Disorders
Samantha Hauser, PhD
Assistant Professor
• Precision Diagnostics For Hearing Loss
• Lead Selection For Hearing Therapeutics
Michele Insanally, PhD
Assistant Professor
• Auditory Perception, Learning, And Plasticity

Manoj Kumar, PhD Assistant Professor
• Difficulty Hearing In Noisy Environments
• Hyperacusis
Thanos Tzounopoulos, Co-Director Endowed Professor and Vice Chair of Basic Research, Department of OtolaryngologyHead & Neck Surgery
• Tinnitus, Hyperacusis, And Hearing Loss Therapeutics
• Neuroplasticity And Hearing Loss
• Auditory Physiology And Processing

Melissa M. McGovern, PhD
Assistant Professor
• Inner Ear Regeneration
• Genetics
• Gene Therapy
Adele Moatti, PhD Assistant Professor
• Inner Ear Drug Delivery
• Nanomedicines

Catherine Palmer, PhD Professor, Chair of Department of Communication Science and Disorders, Director of Audiology
• Hearing Rehabilitation
• Development Of Pathways To Care


Aravind Parthasarathy, PhD
Assistant Professor
• Hearing Loss Diagnostic Development
• Preclinical Hearing Loss Models
Philip Perez, MD
Assistant Professor
• Hearing Loss In Veterans
• Implantable Hearing Devices




Mohit Singhala Research Assistant Professor
• Innovation & Entrepreneurship
• Medical Robotics
• Global Health
Susan Whitney, PhD DPT, NCS, ATC, FAPTA Director, Vestibular Rehabilitation Program, Professor
• Vestibular Physical Therapy
Ross Williamson, PhD Assistant Professor
• Auditory Processing
Anping Xia, PhD Research Professor
• Immune Mediated Inner Ear Disease
• Chronic Ear Infections
• Noise Induced Hearing Loss
Vincent Yuan, PhD Research Assistant Professor
• Meniere’s Disease
• Immune Mediated Inner Ear Disease
Yanjun Zhao, PhD Research Assistant Professor
• Neuroplasticity
The success of the Pittsburgh Hearing Institute largely hinges on its ability to attract and retain top-tier researchers and clinician scientists while fostering a collaborative environment equipped with sufficient space and essential resources. Furthermore, the institute is committed to supporting ancillary services that create a comprehensive care network for both children and adults affected by hearing loss.
Visionary donors who share this mission can help bring the aspirations of the Pittsburgh Hearing Institute to fruition, benefiting the hundreds of millions around the globe experiencing some form of hearing loss. Charitable contributions to the Pittsburgh Hearing Institute will propel it toward its goal of preventing and curing hearing loss.
We are witnessing rapid advancements in medical knowledge, particularly in stem cell biology, genomics, molecular therapies, and new diagnostics for dizziness and balance rehabilitation.
Stem Cell Biology: Research is focused on the potential of stem cells to regenerate damaged inner ear tissues, offering hope for restoring hearing by repairing or replacing essential structures.
Genomics and Gene Therapy: Advances in genomics help identify genetic factors contributing to hearing loss, including developing some lead candidates for gene therapy being taken forward towards the clinic.
Molecular Therapy: These therapies aim to treat the biological mechanisms of hearing loss at the molecular level, restoring normal auditory function by repairing or replacing damaged components in the auditory system.
Nanomedicine: This field leverages nanotechnology to enhance drug delivery systems for targeted inner ear treatments, improving efficacy and minimizing side effects. Nanoparticles also aid in advanced diagnostic tool development for deeper insights into hearing loss.
Immunology: The University of Pittsburgh has established the first Immune Mediated Inner Ear Disorders Center, focusing on innovative diagnostics and treatments for autoimmune ear diseases, Meniere’s disease, and sudden sensorineural hearing loss.
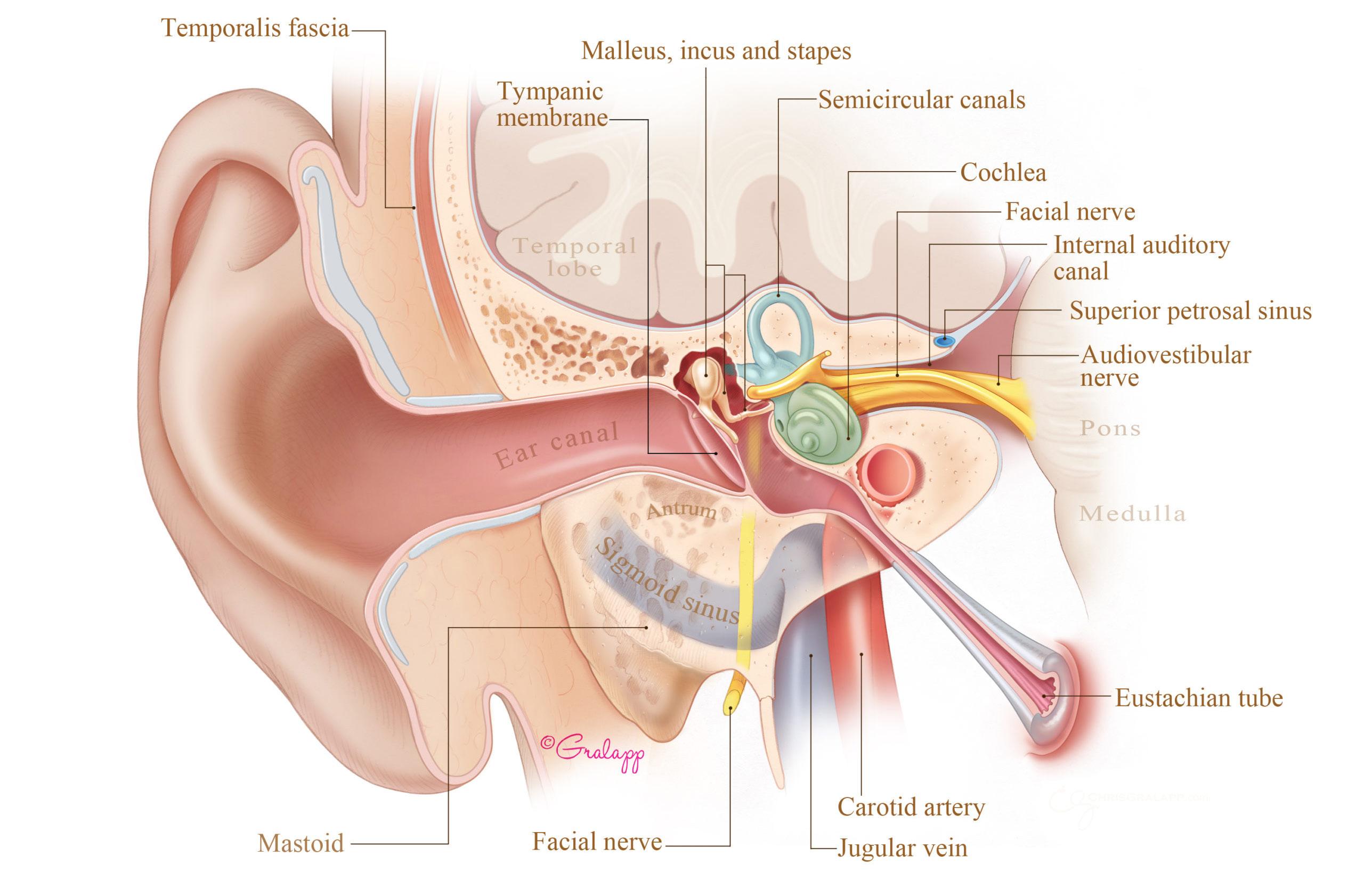
Implantable Devices: Collaborating with robotics experts, we are advancing cutting-edge hearing devices and the next generation of implantable solutions.
Vestibular Disorders: Researchers have developed a wearable monitor for vertigo attacks and are investigating new medical and surgical therapies for vertigo, while our leading rehabilitation center sets a new standard of care.
Together, these fields are enhancing our understanding of hearing loss and paving the way for innovative treatments. As research progresses, we expect more effective prevention and rehabilitation strategies, improving the quality of life for millions with hearing issues.
University of Pittsburgh Department of OtolaryngologyHead & Neck Surgery
Eye & Ear Institute, Suite 500 203 Lothrop Street Pittsburgh, PA 15213
Clinics: 412-647-2100 The Eye & Ear Foundation of Pittsburgh 203 Lothrop Street Eye and Ear Institute, Suite 251 Pittsburgh, PA 15213

More about the Department of Otolaryngology-Head & Neck Surgery at the University of Pittsburgh and UPMC Hearing Institute can be found at otolaryngology.pitt.edu or scan the QR code.
412-864-1300
https://eyeandear.org/
