
School of Medicine Department of Ophthalmology



School of Medicine Department of Ophthalmology

As we look back on 2024, I am deeply proud of the exceptional strides we’ve made at the UPMC Vision Institute. Our commitment to improving quality of life through the preservation and restoration of vision continues to drive everything we do. This year, we have advanced our mission across the three pillars of patient care, research, and education—each contributing to our vision of being a leader in eye care, advancing the frontiers of eye research, and shaping the future of eye health and treatment.
Our research program, ranked eighth in NIH funding, continues to make impactful strides in ocular immunology, retinal disease, glaucoma, and advanced diagnostic technologies. These efforts are directly improving the care we provide to our patients.
In education, we continue to train the next generation of ophthalmology leaders. Our residency program, with six new residents each year, along with our fellowship programs in retina, cornea, glaucoma, oculoplastics, and pediatric ophthalmology, are shaping both future clinicians and researchers.
Our clinicians continue to deliver personalized, high-quality care while expanding our subspecialties to meet the evolving needs of our patients. New faculty positions have helped us stay at the forefront of advancements in treatment.
The campaign that our Eye & Ear Foundation launched shortly after I joined Pitt and UPMC has met all its objectives and beyond. This is an excellent time to celebrate what we have achieved thanks to the unprecedented support of the Eye & Ear Foundation team, board and donors, the local philanthropies working synergistically with our institutions, the University of Pittsburgh School of Medicine, and the Medical Center.
I am excited for the future as we continue to innovate and make strides in all areas of ophthalmology. These programs must continue and grow. As long as people continue to be affected by blinding conditions, we must extend our efforts and launch new initiatives. Among many examples, we need to design and run innovative clinical trials for untreatable conditions, e.g., ultra-rare gene defects, advanced glaucoma, retinal degenerations, optic nerve trauma, and tumors, and ensure that our city is a place where all can benefit from such breakthroughs.
Thank you for your ongoing support as we work together to advance eye care.

José-Alain Sahel, MD
Distinguished Professor and Chairman, Department of Ophthalmology,
The Eye & Ear Foundation, Endowed Chair, The University of Pittsburgh School of Medicine
Director, Vision Institute, University of Pittsburgh Medical Center
Emeritus Professor of OphthalmologySorbonne Université
Founding Director of the Institut Hospitalo-Universitaire FOReSIGHT (2019-2023)
Adjunct Professor of Robotics and Bioengineering, Carnegie Mellon University, Pittsburgh
Adjunct Professor of Ophthalmology, Hebrew University of Jerusalem, Israel
Honorary Professor, Institute of Ophthalmology, University College London
Here are a few examples of the initiatives made possible by the support of the Eye & Ear Foundation, UPMC, Pitt, and our funders. This also demonstrates that the investment in our teams was leveraged and amplified multiple times.
• We grew the Louis J. Fox Center for Optic Nerve Regeneration into one of the strongest in the world, leveraging existing support into major funding and recruiting leading talent. Important recruitments are reaching the final stage and a major ARPA-H grant supporting eye transplantation research started in November 2024, co-led by Stanford and Pitt.
• We are bringing our corneal stem cell program, the brainchild of the late Jim Funderburgh, to the clinical stage.
• We have preserved and expanded our ocular infections and immunity expertise around the Campbell Laboratory. The lab has obtained all accreditations.
• We established a platform assembling the most advanced high-resolution imaging of all eye structures, with multidisciplinary expertise in optics, engineering, artificial intelligence, and biomarkers for the progression of genetic and inflammatory diseases.
• We launched the most innovative vision restoration programs, including prosthetic vision, cortical stimulation, gene therapy, and optogenetics, and performed first-in-human trials.
• We are developing novel patient-centered methods to assess the impact of visual impairment in real life and the transformative benefit of vision restoration, based on the quantification of daily activities in the StreetLab, the driving simulator, and incorporating the patient voice using narrative research methods.
• We provide fully integrated vision rehabilitation with leading, caring experts using our novel life-skills apartment, and other novel technologies, including augmented reality.
• We are assessing and continually improving the quality of care, using constant monitoring of multiple metrics and a digital twin approach.
• We offer the most advanced surgeries, including multidisciplinary techniques—using high resolution, three-dimensional imaging for retinal surgery, novel lasers for cataract and refractive surgeries, and innovative drainage systems for glaucoma. Multidisciplinary teams are involved in very complex surgeries, bringing the best possible care to our patients.
• We are ensuring access to care is possible for all, continuing and expanding our community initiatives such as the Community Outreach Service (formerly the Guerrilla Eye Service), Mission of Mercy, Street Medicine, the EyeVan offered by the Brother’s Brother Foundation, and the constant commitment of our patient advocate. In parallel, we are analyzing the impact of social determinants of health and developing solutions to improve the follow-up of patients affected with complex, chronic conditions.
• At the E. Ronald Salvitti, MD Surgical Training Laboratory, we are training the current and next generations of surgeons in the most advanced techniques.
• For the past three years, we have offered community ophthalmology technician training programs and jobs. We have also trained Hillman Scholars from underserved communities to conduct scientific projects, and several of them have successfully applied to elite college programs.
• In its second year, our Gene Therapy Bootcamp has exposed a wide range of individuals to the most advanced methods, contributing to the building of a workforce in our region, and now growing into a national program.
150,671


Pittsburgh is consistently recognized with accolades from major travel and financial organizations as one of the most livable cities with one of the most viable economies. For several years, it has been honored as a first-rate city for livability, culture, and economy. It was the only U.S. city selected as part of the Lonely Planet’s Global Best in Travel 2025 list.
Academically, there is much to offer. The University of Pittsburgh – which is considered one of the best medical schools in the country – is located mere blocks from Carnegie Mellon University, a top technology and science school. With over 30 colleges and universities in the region, it is easy for faculty to collaborate.
These partnerships are not just limited to Western Pennsylvania. The University of Pittsburgh School of Medicine and the French National Institute of Health and Medical Research, Inserm, are establishing an International Vision Institute, the first such partnership for Inserm. This joint lab will focus on the development of novel therapeutic strategies as well as markers for relevant disease staging and the choice of appropriate and personalized therapy for patients.
Other collaborations include the i2Eye Conference, a joint Paris to Pittsburgh symposium, which was established as a forum for innovative imaging of eye
diseases. The Hearing and Vision Sciences (HVS) graduate certificate program was created to train the next generation of hearing and vision researchers in basic and translational research. Pitt is a co-leader of Transplantation of Human Eye Allografts, or THEA, a program that intends to enable whole functional eye transplantation to restore vision for the blind and visually impaired. In addition, THEA aims to develop new technologies or therapies to preserve or regrow nerves from the eye to the brain. These regenerative solutions could help prevent degenerative blindness and are a necessary step toward successful whole-eye transplantation. And since the Western Pennsylvania School for Blind Children has horticulture incorporated into its curriculum, its students and staff collaborate with UPMC to help with the gardens and landscaping at the Vision Institute.
Additionally, the Healthy Vision Lab at the University of Pittsburgh is unique in its focus on social determinants of health, use of a wide range of analysis (from large datasets to patient-level interviews and health services research), and interdisciplinary relationships with scholars from the School of Public Health and the School of Health and Rehabilitation Sciences. The lab’s mission is to implement collaborative research programs related to ophthalmology and public health that aim to improve access to eye care and to reduce preventable vision loss. These programs include (continued)
research on initiatives to increase access to quality eye care; research on interventions to decrease loss to follow up in chronic eye diseases; and research on the influence of social determinants of health on vision-related outcomes.
The StreetLab also boasts a multidisciplinary team of low vision experts, including ophthalmologists, optometrists and rehabilitation experts, human factors, biomedical engineers, neurologists, psychologists, neuroscientists, psychiatrists, and psychologists.
With six health sciences schools at Pitt and a sprawling hospital system that serves 5 million people, there is an abundance of resources, and these are just some examples. Two-thirds of Pitt graduates stay in the region after graduating. Cutting-edge industry in the region is growing, with facilities like BioForge, the biomanufacturing facility Pitt is building just one example.
Pittsburgh ranks among the top cities in the United States for green certified building space and is consistently ranked among the top 10 tech cities in the country, according to Visit Pittsburgh, which also calls Pittsburgh an advancing leader in aerospace, AI, medicine, education, health care, robotics, software

• PUBLISHED
Amgad Eldib, Alkiviades Liasis. Glaucoma and Electrophysiology –Childhood Glaucoma: Current Trends and Future Prospects. Springer. doi. org/10.1007/978-3-031-61073-8.
ISBN 978-3-031-61073-8, Published: 31 August 2024
• 15 PEER REVIEWED PUBLICATIONS PUBLISHED

engineering, and other tech-forward industries. Companies with research and development facilities in the region are here, including Apple, Disney, Microsoft, and Zoom. Duolingo is headquartered here, and Google has its regional headquarters here – just to name a few.
To support its reputation as an innovation hub, Pittsburgh International Airport’s new modernized renovation that is described as a “smart and efficient airport that advances the region’s role as a world leader” will open in 2025. Pittsburgh has 135 nonstop flights a day, with new ones being added all the time.
The City of Bridges – with over 446, Pittsburgh has more than any other city in the world, including Venice – also has affordable housing, major sports teams, nine theatres in the Cultural District downtown, a world-renowned symphony, a wealth of museums and galleries, and is a foodie destination.
With the addition of the Vision Institute, Pittsburgh is truly making its mark as a hub for education, health care, and technology. Come visit!
• 2 GRANTS AWARDED
Johnson & Johnson Educational Grant for an Ocular Genetic Counseling Conference (Grant ID 2023-RMS-MED -41650, awarded November 15, 2024 / Hannah Scanga - co-awardees Michelle Alabek, Morgan Brzozowski, Kelly Tripi – $31,500
R01-EY030546 2020 to 2025 Identifying Chromosomal Regions
Underlying Eye Disease via Models of Evolution – $3,200,000 - Nathan Clark : co-PI Ken K Nischal
• KEN K. NISCHAL, MD, FAAP, FRCOphth OBTAINED VISITING PROFESSORSHIP FROM COLUMBIA UNIVERSITY IRVING MEDICAL CENTER
• 34 VISITING LECTURES
• 4 ACTIVE CLINICAL TRIALS
by José-Alain Sahel, MD and John Ash, PhD
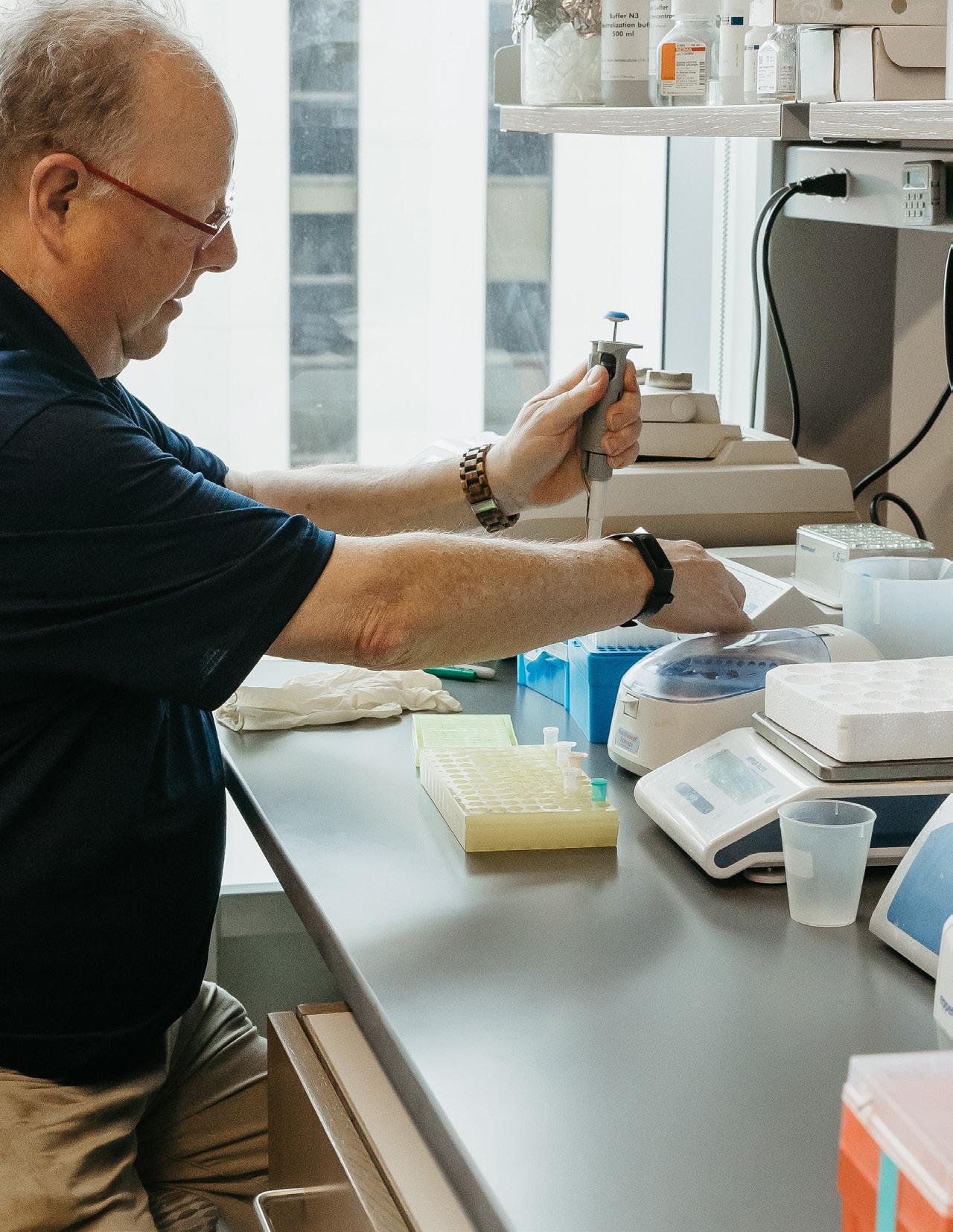
Our research programs span from understanding the biology of vision, from corneal transparency to brain mechanisms of perception, to deciphering the mechanisms of diseases – infectious, inflammatory, traumatic, toxic, degenerative, and genetic – with the ultimate goal of developing effective strategies to prevent and reverse blinding conditions.
Around 40 principal investigators, either scientists, clinicians, or both, team up to construct multidisciplinary programs supported by the Eye & Ear Foundation-led philanthropies and federal funding (NIH, DOD, NSF, and more recently, the new ARPA-H agency). The regenerative medicine approaches (cell and gene therapy), as well as the vision restoration technologies (e.g., prosthetic vision, optogenetic, cortical stimulation), are brought to the clinic by our investigators, surgeons, and industrial partners.
We also seek to better understand the impact of vision impairment and vision restoration in daily activities using naturalistic environments, such as the StreetLab and our driving simulator. Now among the top programs in the country, our fully integrated translational perspective has the ultimate goal of giving back the joy of sight to our patients.


In 2024, at the UPMC Vision Institute Clinical Trials Center, we increased our capacity to conduct early phase and complex gene therapy studies.
Additional new trials were initiated: age-related macular degeneration to include advanced gene therapy, hyperopia, keratoconus, and two for inherited retinal disease. Two trials were successfully closed.
Our facility was enhanced to include usage of our innovative StreetLab and increased collaborations with several departments within the UPMC network.
In 2025, we are preparing for additional studies including, but not limited to, neuro-ophthalmological and glaucoma sub-specialties. We are broadening our relationships with fellow community ophthalmologists so that our trials, and all our facility has to offer, can be accessible to all of Western Pennsylvania and beyond.
By Roberta Zeff Director of Strategic Communications at Pitt Health Sciences
The University of Pittsburgh School of Medicine and the French National Institute of Health and Medical Research, Inserm, will establish an International Vision Institute, the first such partnership for Inserm.
Didier Samuel, Chair and Chief Executive Officer of Inserm, and Anantha Shekhar, John and Gertrude Petersen Dean of the University of Pittsburgh School of Medicine, signed an agreement on Oct. 29 at the French Embassy in Washington, D.C., affirming their intent to collaborate on the lab, a five-year project. The coordinators will be Serge Picaud, Director of the Institut de la Vision in Paris and José-Alain Sahel, Director of the UPMC Vision Institute in Pittsburgh.
“We are all working to develop effective treatments for people with blindness or severe vision loss,” Dr. Sahel said. “We hope that by teaming up, we can do even more to improve or preserve their vision through cutting-edge therapeutic strategies.”
About 2.2 billion people around the world have vision problems. Among them, more than 280 million have severe visual impairment, and 40 million are blind. With an aging population and rising cases of diabetes and other long-term health problems, these numbers are likely to double or even triple in the coming decades.
Currently, there is no known effective treatment that can prevent or reverse vision loss or restore functional vision in inherited and age-related ocular degenerative diseases.
This project aims to develop a better understanding of vision health and diseases while finding new ways to prevent vision loss and help restore sight.
The two institutes develop complementary therapeutic strategies for vision restoration, including gene and cell therapies, optogenetics, and visual prostheses. This joint lab will focus on the development of novel therapeutic strategies as well as markers for relevant disease staging and the choice of appropriate and personalized therapy for patients.


A project that the Chair of Ophthalmology at the University of Pittsburgh, Dr. José-Alain Sahel, MD, started in Paris, has continued in Pittsburgh. “We have been fortunate to develop this model of a digital twin that is helping us try to make the right decisions for patients in a very systematic way,” Dr. Sahel said at the start of the Eye & Ear Foundation’s November webinar, “Digital Twin of the Eye.”
Individualized treatment and safety monitoring are the goals when treating every patient, said Dr. Jay Chhablani, MD, Professor of Ophthalmology and Director of Clinical Research at the Vision Institute. The digital twin model is a complex process in which several factors are used to help offer the best treatment for individual patients. It involves AI-based image analytics, clinical analytics, advanced imaging, quality, and social determinants of health.
The clinical analytics team at UPMC has helped develop an app that allows physicians to see patient details. “It provides us all the possible information, not only about the ophthalmology, but their systemic disease, including all the demographics as well as various factors which can influence the ophthalmologic outcome,” Dr. Chhablani said.
In the last year, two injections have been approved which can slow down progression of dry AMD. Dr.
Chhablani’s lab is focusing primarily on screening as well as predicting the progression of the disease. His research wants to understand how patients will respond to treatment when converted from dry to wet.
AI-based feature extraction can help diagnose a condition before it advances as well as predict progression.
While several other ophthalmology departments are working on AI and adapting it to imaging, the Department of Ophthalmology at Pitt is unique in how it is trying to integrate every parameter. Other centers have contacted Pitt to collaborate. “The goal is really not to work in isolation,” Dr. Sahel said. “We need to share knowledge, because the more data that’s integrated, the more experience you get, and the more patients are involved, the better it’s going to be.”
Pittsburgh has several existing trials. “The main focus for many of us is on genetic diseases of the retina,” said Dr. José-Alain Sahel, MD, Chair and Distinguished Professor of the Department of Ophthalmology at the University of Pittsburgh School of Medicine, and Director of the UPMC Eye Center. “We are trying to target various stages of the disease.” The ideal therapy is to correct the gene defect. If this is done early enough, the course of disease can be stopped, and the patient can potentially recover or keep useful vision.
One of the key projects of Dr. Sahel’s team is to protect the remaining cells. He has been working on this for years.
Currently only a small number of patients can be treated with existing approaches. The team focuses on the main one, which is early onset disease that occurs in children leading to early on certain loss of vision. Pittsburgh treats patients with Luxturna.
Dr. Sahel’s team has been concerned about possibly having to treat patients later in the course of the disease. As a result, they have been working for years on trying to protect the central vision. They identified a key mechanism that maintains viable photoreceptors. This therapy is now in clinical trials.
Dr. Joseph Martel is principal investigator on the study that is trying to rescue the cones by providing the signaling that is underlying the survival. This is in
clinical trials, with key sites in Paris, Pittsburgh, Miami, Portland, Boston, and Dallas.
Another approach is optogenetics, “where we express in the remaining cells of the retina proteins that are sensitive to light,” Dr. Sahel said. GS030 optogenetic therapy is combined gene therapy and a medical device to restore retinal light sensitivity.
Dr. Martel was the local principal investigator in the study that demonstrated in the first patient, treated in Paris, the ability to move from being totally blind to being able to see. “This is a key milestone on the path to restore vision,” Dr. Sahel said. Other patients who were previously blind have experienced a similar benefit.
They were able to show that this is correlated with reactivation of the brain in the visual area, thanks to the support of leading cognitive neuroscientists in Paris and Pittsburgh. Now data is being collected and the therapy is being improved to provide much better vision. Dr. Sahel said they are working on the next generation of this promising therapy.
A new tool has been developed where instead of replacing a gene, the mutation can be rewritten. “The promise of gene therapy is that you’ll get a permanent solution to the problem after a single injection,” said Dr. Leah Byrne, PhD, Assistant Professor in the Department of Ophthalmology. “I think gene therapy holds a lot of promise for that reason.”



To make whole eye transplants that restore sight a reality, the Department of Ophthalmology at the University of Pittsburgh is part of a project team for a program called Transplantation of Human Eye Allografts, or THEA.
The project will receive an up to $56 million award from the Advanced Research Projects Agency for Health (ARPA-H), an agency within the U.S. Department of Health and Human Services (HHS). Pitt will likely receive around $9 million for its role in the project, the largest Pitt has received for optic nerve regeneration.
“It’s a very audacious project to have a living functional human eye transplant in a patient and then the patient has functional vision after the surgery,” said John Ash, PhD, Vice-Chair of Ophthalmology and Director of Research. “A successful eye transplant has occurred already, but it’s not functional, so the eye can’t process images and connect to the brain. We want to extend that and go into the next step where we get the eye to reconnect to the brain.”
Jeffrey Goldberg, MD, PhD, Chair of Ophthalmology at the Byers Eye Institute at Stanford University, will be the primary investigator leading more than 40 doctors, researchers, and industry experts from around the country. José-Alain Sahel, MD, Ophthalmology Chair at the University of Pittsburgh, will co-lead.
“This group of people has been working for decades now on figuring out how to promote optic nerve regeneration and retinal neuron survival in diseases like glaucoma and countless other blinding diseases,” Dr. Goldberg said. “That positions this group of collaborators to be the best situated to take on optic nerve regeneration and neuronal cell survival in the context of eye transplant.”
Dr. Sahel praised the strong collaborations necessary for scientific breakthroughs. “By combining the deep knowledge about ophthalmology, tissue preservation and regeneration, immunology, and surgery of worldclass scientists at Byers Eye Institute, University of Pittsburgh, and consortium members from top institutions, we are well-positioned to set the foundational steps toward restoring vision using a whole eye transplant.”
This work is not anything new for Pitt, as this project simply taps into what the Department has already been doing.
The major hurdle is removing the eye from a donor and preserving it for up to 48 hours so that it can be collected and processed before being matched with the donor recipient. Hence, the first phase of the project is removal and preservation, which is being done by a team at Pitt led by Leah Byrne, PhD; Ethan Rossi, PhD; and Shauhua Pi, PhD, with Dr. Sahel. They will also measure its functioning and survival. This is the THEA program’s technical area 1.
Technical area 2 is looking at different ways to stimulate the eye. “We can stimulate the eye to regrow ganglion cell nerve fibers to go from the retina all the way to various targets in the cellular system,” Dr. Ash said. A large group of people at Pitt including Dr. Ash; Larry Benowitz, PhD; Kun-Che Chang, PhD; Takaaki Kuwajima, PhD; Boris Rosin, MD, PhD; and Tonya Stefko, MD, are looking at various strategies to apply to ganglion cells so they survive when the optic nerve is cut. The goal is to stimulate them to grow into the reconnected optic nerve, and then the cortex, where they will allow functional vision. Ian Sigal, PhD, Director, Image Acquisition and Analysis Core Module, Ophthalmology and Visual Sciences Center; Dr. Kuwajima; and Stephen Badylak, DVM, PhD, MD, from the McGowan Institute for
ARPA-H
José-Alain Sahel, MD
John Ash, PhD
Boris Rosin, MD, PhD
Susan Stefko, MD
Takaaki Kuwajima, PhD
Larry Benowitz, PhD
Ian Sigal, PhD
Kun-Che Chang, PhD
Steve Badylak, MD, PhD, DVM
George Hussey, PhD
Rakie Cham, PhD
Shaohua Pi, PhD
Ethan Rossi, PhD
Leah Byrne, PhD
Mario Solari, MD
Heth Turnquist, PhD
Walter Schneider, PhD
Alan Watson, PhD
Yijen Wu, PhD
NIH
Issam al Diri, PhD
John Ash, PhD
Leah Byrne, PhD
Xing Chen, PhD
Paul Kinchington, PhD
Alessandra Larimer‐Picciani
Ekaterina Lobanova, PhD
Joseph Martel, MD
Kelly Martin
Robert Shanks, PhD
Anthony St. Leger, PhD
Shawn Willett, PhD
DOD
Takaaki Kuwajima, PhD
Industry
Jay Chhablani, MD
Eric Romanowski, MS
Gary Yam, PhD
Foundation
Yuanyuan Chen, PhD
Xing Chen, PhD
Katherine Du
Takaaki Kuwajima, PhD
Debasish Sinha, PhD
Bingrui Wang, PhD
+ Expected: Gilbert Family Foundation
At the UPMC Vision Institute, our clinical research program is a cornerstone of advancing eye health, integrating innovative clinical trials with multidisciplinary collaboration.
We work closely with basic scientists, harnessing discoveries in genetics, molecular biology, and high-resolution imaging to inform groundbreaking treatments. Our research spans not only clinical divisions including retina, cornea, dystrophies, glaucoma, and comprehensive eye care, but also addressing critical issues such as access to care, low vision, occupational therapy, and social determinants of health.
By partnering with leading researchers, clinicians, and industry experts, we aim to transform patient outcomes and improve vision care globally. Through our clinical trials, we offer patients access to cutting-edge therapies and play a pivotal role in shaping the future of ophthalmology.


Jay Chhablani, MD Director of Clinical Research, UPMC Vision Institute Professor of Ophthalmology

A multidisciplinary research team from the University of Pittsburgh and Carnegie Mellon University was awarded a National Institutes of Health U01 Grant to explore the specific targeting capabilities of Adeno-Associated Viruses (AAVs) in neuroscience studies. This project is directed by principal investigators William Richard Stauffer, PhD (Pitt); Andreas Robert Pfenning, PhD (CMU); Afonso Silva, PhD (PITT); and Leah Byrne, PhD, from the Department of Ophthalmology at the University of Pittsburgh, who specializes in developing gene therapies for retinal diseases using adeno-associated viral vectors (AAVs) and gene editing approaches using CRISPR/Cas9 and proprietary tools.
A research team from the UPMC Vision Institute is at work on a multidisciplinary project to test a new retinal adhesive thermoresponsive gel for delivering an adeno-associated virus (AAV)-mediated gene therapy to the outer retina for treating Leber Congenital Amaurosis (variant NPHP5-LCA). This ambitious project is funded by two complementary grants, one a National Institutes of Health R01 award and the other a grant from the U.S. Department of Defense (DOD) Military Operational Medicine Research Program (MOMRP).
In a paper published in Nature Communications, the Pitt researchers explain how they developed a new clinical tool that predicts which patients will respond to adoptive therapy. The work, supported by UPMC Enterprises, is helping improve personalized therapies and avoid futile treatments for metastatic uveal melanoma.

UPMC Vision Institute’s E. Ronald Salvitti, MD Surgical Training Lab Provides New Technology
Surgical training and surgical simulation training play a crucial role in shaping competent and confident ophthalmologists. Coinciding with the opening of the new UPMC Mercy Pavilion, headquarters of the UPMC Vision Institute, was a purposebuilt and designed new surgical training and simulation lab created specifically for aiding in the training of new residents.
In July 2024, the UPMC Vision Institute treated its first patient with the gene therapy Luxturna® for inherited retinal dystrophies (IRD) caused by biallelic mutations in the RPE65 gene. Luxturna® was the first gene therapy for any disease approved by the U.S. Food and Drug Administration (FDA) in late 2017.
“While IRDs in general are rare diseases and the biallelic RPE65 mutation variants even more so, Luxturna’s demonstrated efficacy provides our patient population the ability to halt the progression of their disease and hopefully maintain their remaining functional vision capacity,” says Joseph Martel, MD, assistant professor of Ophthalmology in the Department of Ophthalmology at the University of Pittsburgh School of Medicine.
Physicians and researchers from the UPMC Vision Institute, UPMC Children’s Hospital of Pittsburgh, and the University of Pittsburgh Department of Ophthalmology continuously produce and publish new research in a variety of medical journals throughout the year. Recent research published in July and August include topics such as optogenetic vision restoration, diabetic retinopathy, pediatric ophthalmology, retinal gene therapy, and more.
Pitt Team Gets Millions From ARPA-H for
To make whole eye transplants that restore sight a reality, the Department of Ophthalmology at the University of Pittsburgh is part of a project team for a program called Transplantation of Human Eye Allografts, or THEA.
The project will receive an award of up to $56 million from the Advanced Research Projects Agency for Health (ARPA-H), an agency within the U.S. Department of Health and Human Services. Pitt will likely receive around $9 million for its role in the project, the largest Pitt has received for optic nerve regeneration.

Addressing the unmet clinical need of patients and the strategic interests of pharmaceutical companies is made possible by AnkyrBio’s introduction of anchors that bind drugs to the ocular surface and other areas prone to drug wash out like the oral cavity, nasal passages, joints and female reproductive system. These anchors hold the drugs in contact for hours or days allowing the full therapeutic effect to take place. The anchors overcome the wash out problem with topical administration in a breakthrough manner that simply does not exist in the market at this time.
FOUNDERS
H.P. Beers
Robert Shanks, PhD
Deepinder Dhaliwal, MD
Learn more: ankyrbio.com

Avista’s mission is to develop innovative gene therapies for retinal diseases, including rare ophthalmic conditions that have a profound impact on quality of life. Avista’s computationally guided, in vivo scAAVengr platform leverages a high-throughput approach with built-in quantitative validation of novel cell-specific AAVs, enabling the rapid translation of transformative gene therapies to the clinic for diseases impacting people’s vision. The company recently announced a partnership with Roche to develop novel AAV gene therapy vectors for the eyes. The partnership aims to apply Avista’s single-cell adeno-associated virus (AAV) engineering (scAAVengr) platform technology to develop intravitreal AAV capsids matching a capsid profile defined by Roche.
FOUNDERS
Lea h Byrne, PhD
José-Alain Sahel, MD
Paul Sieving, MD, PhD
Learn more: avistatx.com

NetraMind Innovations is a company dedicated to advancing ophthalmic care through the development of artificial intelligence (AI) and machine learning (ML) technologies. Founded by a multidisciplinary team of ophthalmology and AI experts, and mentored by successful ophthalmology professionals, the company is focused on developing automated tools to enhance the efficiency and accuracy of diagnosing various retinal diseases. The primary goal is to address the critical unmet need for scalable, automated methods to detect and monitor Age-Related Macular Degeneration (AMD), a leading cause of vision loss in older adults.
FOUNDERS
Jay Chhablani, MD
Kiran Vupparaboina, PhD
Sandeep Chandra Bollepalli, PhD
José-Alain Sahel, MD
Learn more: netramindinnovations.com

Phosphoenix B.V. is a pioneering MedTech startup, with a mission to restore functional and life-enhancing vision to those who have lost it. The visual prosthesis bypasses the eyes and directly interfaces with the brain. Its patented technology offers dense coverage of the visual field, using high-density and ultraflexible probes to stimulate nerve cells in parts of the brain responsible for vision. By activating specific combinations of electrodes, we aim to generate recognizable shapes and patterns that will enable blind individuals to identify objects, navigate, and regain autonomy in daily life.
FOUNDERS
Xing Chen, PhD
Bert Monna
Pieter Roelfsema
Learn more: phosphoenix.nl

Science Corporation’s mission is to create a world of bionic vision for those who have lost their sight, enabling them to regain visual perception and greater autonomy. Science Corporation’s bionic vision systems are associated with a surgical intervention and a rehabilitation period. Prima System sub-retinal miniature photovoltaic wireless implant is in clinical testing for patients who have lost their sight due to outer retinal degeneration, initially for atrophic dry age-related macular degeneration (dry AMD).
José-Alain Sahel, MD
Jose-Alain Sahel, MD co-founded Pixium Vision which has been acquired by Science Corporation.

Sparing Vision is a clinical-stage genomic medicines company leading a step shift in how ocular diseases are treated. We are going beyond single gene correction therapies to deliver new treatments to patients affected by Inherited Retinal Diseases (IRDs), regardless of genetic cause. It’s goal is to harness the potential of gene therapy and genome editing to bring cutting-edge innovation into ocular disease drug discovery and development.
FOUNDERS
José-Alain Sahel, MD
Thierry Léveillard, PhD
Learn more: SparingVision.com

Elizabeth Wood applied to the Pittsburgh Gene Therapy Bootcamp on a whim. The husbandry technician, or “monkey nanny” at the University of Pittsburgh learned about it from a mass email. Then she forgot all about it until she was accepted. “The first thing that went through my head was this must be a mistake,” she recalled.
This thought process is understandable, given that the bootcamp advertised the opportunity for graduate students and postdoctoral fellows, though no prior experience is required. Wood left college before finishing her degree over 20 years ago.
The Pittsburgh Gene Therapy Bootcamp was launched in 2023 by the Byrne Lab with the goal of hosting it annually. All guest speaker presentations are open to the community. The program includes one intensive week of hands-on wetlab experiments in AAV viral vector packaging and purification, followed by eight weeks of one-day-a-week wetlabs and once-a-week guest lectures.
As part of the wetlab training, students run singlecell RNA-Seq experiments and produce and analyze data on the topic of in vivo viral vector-mediated gene delivery. Data collected during the course will be reported in a manuscript that will be submitted to a preprint server, and course participants will receive coauthorship on the paper. Students have opportunities to shadow and network with professionals working in the field of gene therapy, including genetic counselors, local biotech companies, physicians, and academics.
Wood began the bootcamp feeling extremely intimidated. “From the instructors to the other students in the class, they were extremely kind and helpful and answered any questions I had along the way. It was a wonderful feeling to have all these strangers turned to friends help me succeed.”
Indeed, the experience was life-changing.
As part of bootcamp, Wood worked on a hypothetical project. After investigating different mental illnesses, she settled on bipolar disorder. “I know from watching friends and family suffer from it but also the struggle I have combating it, I have seen what damage this monster of destruction can do to someone,” she shared.
Wood’s idea is to treat bipolar disorder through gene therapy by combining optogenetics and nanoparticles. “My end goal is to modify the symptoms and make them more manageable to deal with,” Wood explained.
“I did not want the bootcamp to end,” she said. “On my way home after our last day, I cried because it was over. I would do it all over again in a heartbeat.”

The UPMC Vision Institute / University of Pittsburgh School of Medicine Department of Ophthalmology is a leader in innovative education, training future leaders in eye care and research through programs that span the medical, technical, and advanced practice spectrum.
Our commitment to excellence in medical student education aligns with the PittMed Three Rivers Curriculum (3RC), providing pre-clinical and clinical medical students with a modern ophthalmology curriculum tailored to adult learners. This ensures students gain both foundational knowledge and clinical acumen in this vital specialty.
Our residency program in ophthalmology is among the most highly ranked in the nation, training six residents annually. This competitive program attracts top-tier applicants from across the globe. Residents benefit from a robust didactic curriculum and comprehensive hands-on experiences in medical and surgical ophthalmology, guided by expert mentors. The Department’s state-of-the-art surgical training lab, featuring 16 networked workstations and three virtual reality simulators, sets a national benchmark for ophthalmic surgical education.
The Department also offers advanced post-residency fellowships in all ophthalmic subspecialties — cornea, glaucoma, orbit and oculoplastics, pediatric ophthalmology, neuro-ophthalmology, and retina. These fellowships provide in-depth training in both clinical and procedural aspects of each field, fostering the development of future leaders in ophthalmology. Fellows work closely with expert faculty, engage in

Evan “Jake” Waxman, MD, PhD Vice Chair, Medical & Resident Education Director,
Comprehensive Eye Service
Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
cutting-edge research, and gain exposure to a diverse and complex pathologies.
In addition, the Department hosts an optometry residency program, offering advanced training in Low Vision and Ocular Disease. This program provides an unparalleled opportunity for optometrists to deepen their expertise and contribute to interprofessional collaboration in vision care.
As the first in the nation to establish a large-scale Advanced Practice Provider (APP) training program in ophthalmology, we prepare APPs to excel as frontline responders in urgent, emergency, and inpatient eye care. This groundbreaking program addresses critical needs in the delivery of comprehensive eye care services.
Finally, the Department addresses workforce challenges through its ophthalmic technician training program. By expanding the pool of skilled technical staff, this program has become essential in supporting clinical operations and enhancing patient care across the field.
Through these initiatives, the Department of Ophthalmology at Pitt stands at the forefront of ophthalmic education, advancing the national profile of the field while meeting the evolving needs of modern eye care.

The UPMC Vision Institute is dedicated to improving access to eye care and ensuring patients follow through with necessary treatments, particularly for underserved and remote populations. Our community service and remote care initiatives embody this commitment, bridging gaps in care and bringing vital services to those who need them most.
Several times each month, our medical students and eye care physicians volunteer their expertise at primary care centers serving patients without financial means. Using our mobile eyeVan units, we bring comprehensive eye exams and diagnostics directly to these sites. Our goal is not just to provide one-time care but to establish enduring patient relationships, serving as their ongoing eye care providers.
Each year, we proudly participate in the Call to Care Mission of Mercy event. Over two days, our team provides free eye exams to hundreds of individuals, collaborating with the Essilor/Luxottica Foundation

& Resident Education Director, Comprehensive Eye Service Professor, Department of Ophthalmology University
to deliver eyeglasses at no cost. This event also includes advanced diagnostic imaging to screen for diabetic retinopathy and other conditions that can impair vision, helping to address the complex needs of our community.
To further expand access to eye care, we have launched the Ophthalmology Remote Access Initiative. A dedicated team—including a project manager, two research fellows, and an ophthalmic technician—is driving efforts to make eye care more accessible through remote screening, monitoring, and consultation. By leveraging ocular telehealth and mobile eye care, we aim to redefine how services are delivered. Using implementation science methods, we are actively contributing to the advancement of teleophthalmology, with a focus on making care equitable and sustainable.
Through these programs, the UPMC Vision Institute exemplifies its mission to reduce barriers to eye care, ensuring that no individual is left behind in the fight for better vision and eye health.
The Eye & Ear Foundation in partnership with Call to Care hosts this annual two-day event that provides free care for vision, hearing, and dental for ages two and up. Last year it was held November 1-2, 2024.
“On Friday and Saturday, the eye care community in Pittsburgh came together and stepped up for our neighbors in need,” said Jake Waxman, MD,
PhD, Director, UPMC Eye Center Mercy. “We prescribed and ordered glasses. We diagnosed cataracts, macular degeneration, macular holes, and diabetic retinopathy. We arranged for follow up care and helped people apply for funding.”
He went on to say that as large as the numbers are, everyone was treated as a person and not a number. The Vision clinic served 693 patients and ordered 552 pairs of glasses.
We prescribed and ordered glasses. We diagnosed cataracts, macular degeneration, macular holes, and diabetic retinopathy. We arranged for follow up care and helped people apply for funding.


The Vision Institute at UPMC Mercy Pavilion is the first of its kind in the nation, a one-stop shop for people with vision issues.
When José-Alain Sahel, MD, arrived in Pittsburgh in July of 2016 to assume the Distinguished Professor and Chair of Ophthalmology role at the University of Pittsburgh, UPMC leadership saw an opportunity. With his skills and experience as the Founder of the Institute de la Vision in Paris, this was a chance to create an asset in the community for people with vision loss worldwide.
The $510 million project took nearly six years to complete, with the 410,000-square-foot building opening May 1, 2023. The nine-story pavilion is also home to the UPMC Rehabilitation Institute.
In the vision tower section of the building, everything was designed, chosen, and built intentionally, and it is all dedicated to ophthalmology. There are eight eye disease operating rooms, 83 eye exam rooms, 10 rehab
exam rooms and 100,600 square feet of research space, including a collaborative staircase that brings together education and research with the goal of having people meet.
A pharmacy, café, and optical shop housed in the Vision Institute are open to the public. The ground floor has an Urgent Care Eye Clinic, one of the few clinics in the country dedicated to the care of eye emergencies, one of only two in Pennsylvania, and the only one in the region. Comprehensive care and outpatient testing are also on this floor.
Floor two has clinical services for people with glaucoma, retina, and cornea issues with exam rooms configured for flexibility of use between services. Patients do not have to move back and forth between waiting rooms; they are guided right to their location.
The popular Dry Eye Clinic on the third floor is unique because of its coordinated, multi-disciplinary care model. Dedicated surgical space is also on this floor. The fourth floor is for innovation and education, a world-renowned
(continued)





The
Vision Institute at UPMC Mercy Pavilion
(continued)
education and training center educating patients, practitioners, and providers. There are meeting spaces on this floor for this purpose.
The Fine Foundation Winter Garden is an indoor space meant to be used by staff and scientists but can also welcome events and visitors. Just next to the Winter Garden is the Bruce and Barbara Wiegand Roof Terrace, also used by faculty, staff, and visitors. Some of the gardens are designed and maintained by the Western PA School for Blind Children in partnership with UPMC. The sensory garden has different landscape pathways and other features to make it accessible to people with vision issues.
Low vision and rehabilitation spaces include a Street Lab to assess functional vision loss and a driving simulator that looks at driving performance in a variety of conditions and help patients develop better strategies on how to drive safety. There is also a life skills apartment with a kitchen, living room, bedroom, and laundry room, to allow patients to simulate real-world activities.
The E. Ron Salvitti, MD Surgical Training Laboratory is a state-of-the-art surgical education training center with 16 workstations. The fifth-floor houses clinical trial space. It is fully equipped to develop all the
The $510 million project took nearly six years to complete, with the 410,000-square-foot building opening May 1, 2023.
new approaches to therapies and contains real life assessment. Research suites are housed on floors seven through nine.
In addition to various clues to help patients navigate, there is a thoughtful color scheme along with special lighting so people with low vision can adapt. Great thought was put into the navigation design for people with low vision, as well as those who use a cane, to find their way to their location.
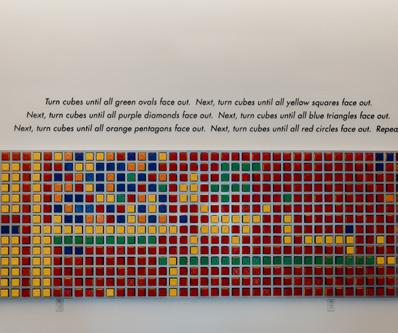
A national call for artists resulted in the artwork that is integrated as part of the holistic care experience. Several of the pieces are kinetic, and two are interactive, responding to touch and sound. All artists considered the needs of patients and caregivers, and their work is meant to stimulate conversation and facilitate connection. In publicly accessible areas, the art also assists in wayfinding. Two of the artists are from Pittsburgh, and three self-identify as artists with disabilities, including one who lost his vision in the Vietnam War.
In the Vision Institute’s first year, there were 47,013 total patient visits, with 9,712 new patients. The number of total surgeries performed that year was 6,171. Looking back on the inaugural year, Dr. Sahel said that patient experience and the ability to attract clinical and research talent exceeded his expectations.

The Vision Institute at Mercy Pavilion is home to state-ofthe-art eye clinics on four floors that comprise comprehensive, glaucoma, neuro-ophthalmology, oculoplastics, glaucoma, cornea, low vision, refractive surgery, retina, as well as an ophthalmology operating suite and urgent clinic.
The clinic pods are designed with a “patient owns the room model,” so that the patient can safely leave personal items in their room as they are taken for testing or minor procedures. The pods have designated procedure rooms in close proximity to the examination rooms for patient convenience and clinic efficiency.
The specialty clinics include:
• Several large minor procedure rooms on the first three floors
• A low vision suite that houses a fully functional apartment to allow patients to be educated on independent living in a realistic setting
• A refractive surgery suite including two intralase machines
• A dry eye clinic with the latest equipment for treatment of this common yet impactful condition
• A retinal dystrophy clinic with in-house genetic counselors
• The Campbell Laboratory, unique in the country as a processing center for analysis of all ophthalmic specimens
• A venipuncture lab for preparation of serum tears
• A compounding pharmacy across the connected walkway in Mercy Hospital
The operating suite includes:
• 8 operating rooms with ceiling-mounted microscopes
• Multiple machine platforms from different suppliers for cataract, corneal, glaucoma, and retinal surgery
• In-suite satellite pharmacy
The Urgent Eye Care Clinic opened in October of 2023, and is unique in the ophthalmology community nationwide with a separate street entrance, examination suite, and waiting room. The clinic is overseen by general ophthalmologists with subspecialty care available upstairs, and supported by a team of optometrists, residents, and physician assistants.

The UPMC Vision Institute has a patient-centered approach to low vision rehabilitation that involves novel technologies.
According to Dr. Jose-Alain Sahel, Chair of the Department of Ophthalmology, there is a tendency to be focused on therapies and ways to fix visual conditions. Assessments are based on classical testing, but this may not fully reflect what occurs in patients’ daily lives. It is also important to demonstrate therapy’s benefit in daily life. This is part of a continuum of care that begins at diagnosis and aims to return patients to the lives they previously enjoyed.
To that end, the mission of the StreetLab at the Paris and Pittsburgh Vision Institutes is to enhance the quality of life of people with low vision. This involves improving their function, promoting their independence, and promoting their productivity in society.
Rakié Cham, PhD, researcher and full professor in the Departments of Bioengineering, Ophthalmology, and Physical Therapy at the University of Pittsburgh co-leads the StreetLab with Dr. Sahel. The StreetLab boasts a multidisciplinary team and is housed on the fifth floor of the Vision Institute.
The StreetLab assesses an individual’s needs and their perception of their impairments, which may include visual field loss and visual acuity deficits.
Vision loss is a big risk factor for falls, so balance assessment is the first thing done at the StreetLab. Additionally, in collaboration with Paris colleagues, the StreetLab has a state-of-the-art mobility assessment called the Mobility Standardized Test (MoST) in Virtual Reality.
“One of the questions that might come up is what’s the connection between work that is happening in low vision at the Vision Institute and in the area of low vision rehabilitation?” asked Clive D’Souza, PhD, MS, Assistant Professor and researcher in the Department of Rehabilitation Science and Technology at the University of Pittsburgh School of Health and Rehabilitation Sciences.
That connection is driving, which is vital to access and independence. A driving simulator at the Vision Institute allows patients’ driving skills to be assessed and evaluated in a safe environment. It has the look and feel of an actual driver station and captures the physical movement of a real car.
“We are able to give feedback and training so they can develop more safe driving habits,” Dr. D’Souza concluded.
William Smith, OD Director of Low Vision Service Program Director of the Optometry Residency Low Vision Program Assistant Professor of Ophthalmology

S treetLab at the Vision Institute aims to enhance the quality of life of people with low vision by improving their function and promoting their independence and productivity in society.

The Vision Institute has a life skills apartment with a kitchen, living room, bedroom, and laundry room where patients can simulate daily activities. Patients can engage in the activity instead of us trying to show them some things on the counter and then hope they can translate that at home.

The driving simulator features original vehicle components such as the steering wheel, gas/brake pedals, driver seat, and dashboard-mounted on a wheelchair-accessible motion platform, a 180-degree field-of-view using three large visual displays, blindspot displays, and surround sound audio feedback. The motion platform is calibrated to reproduce movement cues exactly corresponding to the driver’s responses. The software program running the simulator contains various customizable driving scenarios from basic to more complex situations, safe to more hazardous road conditions, and impaired and distracted driving.

This Sensory Garden has landing strips of gravel, turf, brick, and pavement, along with stairs. This allows the team to assess people’s mobility and make recommendations to help them maneuver more safely. Lighting and contrast assessments are also conducted outside, in the sensory garden’s natural environment. The plants are tactile and fragrant. The Western Pennsylvania School for Blind Children helps maintain the garden.
The Dry Eye Clinic – which opened at the Vision Institute in November 2023 – is unique because of its coordinated care. It has grown tremendously in the short time it has been open, according to Sabrina Mukhtar, MD, Assistant Professor of Ophthalmology and Director of the Dry Eye Clinic.

“There is a significant need for a more in-depth approach to dry eye disease, especially for the complex patients we see at the UPMC Vision Institute,” she said.
Among the features that make the clinic stand out is the machine learning program, CSI Dry Eye, which was created by one of the previous UPMC Cornea Fellows, Dr. Ahmed Al-Ghoul. The program helps document and track dry eye metrics to provide objective data for diagnosis and monitoring prognosis. The clinic has a multidisciplinary approach to dry eye disease; working with all members of the team at the UPMC Vision Institute to provide exceptional care. It is also considered a “one-stop shop,” where available products are suggested to patients, and serum tears are drawn and delivered to the patient during the appointment. Providers can spend time with the patients, due to longer patient blocks built into the schedule. This allows them to “really dig deep into the underlying mechanism of dry eye disease specific to the patient so that we can provide holistic and targeted treatment,” said Dr. Mukhtar.
Having this clinic is important because dry eye disease is a significant cause of ocular morbidity with several studies showing how it impacts quality of life. It is a complex disease process anchored in inflammation with several risk factors – some of which are modifiable.
Appointments start well before the scheduled clinic day when the front desk staff calls patients to schedule. Lengthy questionnaires are sent that require patients to share lifestyle factors, medications, diet, sleep, hydration, and other factors that may affect dry eye disease. Upon check in, technicians review the questionnaires and provide targeted imaging/testing based on the reason for referral, and then Dr. Mukhtar sees the patient and helps come up with a targeted treatment plan. A coordinator helps schedule procedures and provides patient education. At the end of the appointment, a file is available for patients to review their testing and next steps in the plan. On follow ups, dry eye questionnaires are administered so patients can monitor their prognosis.
The next goal is to integrate advanced levels of imaging, including confocal imaging to image corneal nerves and inflammatory cells into diagnostics. They are working to also provide personalized biomarker diagnostics so that they can help patients navigate the myriad of medications available in the market. Lastly, the clinic is collaborating with scientists to help advance care in dry eye disease.
The Dry Eye Clinic is located on the third floor of the Vision Institute, in the Refractive and Ocular Surface Suite. Clinic is typically on Fridays from 8 a.m. to 5 p.m., but procedures are performed on certain Wednesday afternoons of the month as well, specific to dry eye treatment.

José-Alain Sahel, MD
RETINA SERVICE
Distinguished Professor and Chairman, Department of Ophthalmology, The Eye & Ear Foundation, Endowed Chair, The University of Pittsburgh School of Medicine
Director, Vision Institute, University of Pittsburgh Medical Center



John D. Ash, PhD
Vice Chair of Ophthalmology and Director of Research
E. Ronald Salvitti, MD Endowed Chair Professor of Ophthalmology
University of Pittsburgh School of Medicine
Kunal K. Dansingani, MBBS, MA, FRCOphth
RETINA SERVICE
Vice-Chair, Operations and IT
Associate Professor of Ophthalmology
University of Pittsburgh School of Medicine
Deepinder K. Dhaliwal, MD, L.Ac
CORNEA SERVICE
Vice Chair, Communications and Wellness
Director, Refractive Surgery Service
Professor, Department of Ophthalmology
Director and Founder, Center for Integrative Eye Care
University of Pittsburgh School of Medicine

Marie-Hélène Errera, MD, PharmD, PhD
RETINA SERVICE
Vice Chair Diversity, Equity & Inclusion
Associate Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine


Jerome I. Finkelstein, MD, FACS
COMPREHENSIVE EYE SERVICE
Vice Chair, Clinical Operations
Clinical Associate Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Vishal Jhanji, MD, FRCS (Glasgow), FRCOphth, FARVO
CORNEA SERVICE
Vice Chair, Quality Director, Cornea Service
Professor, Department of Ophthalmology
Co-Director, Clinical Trials
Clinical Co-Director, Funderburgh Cornea
Regeneration Project
University of Pittsburgh School of Medicine


Joseph N. Martel, MD
RETINA SERVICE
Vice Chair, Patient Experience and Access
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Ken K. Nischal, MD, FAAP, FRCOphth
PEDIATRICS OPHTHALMOLOGY SERVICE
Executive Vice Chair, International Director, Pediatric Ophthalmology Service
Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Medical Director, Digital Health
Assistant Medical Director, UPMC International Medicine


S. Tonya Stefko, MD
OCULOPLASTIC AND ORBITAL
SURGERY SERVICE
Vice Chair, Continuity of Care and Consults Director, Oculoplastic and Orbital Surgery Service
Professor, Departments of Ophthalmology, Otolaryngology, and Neurological Surgery
University of Pittsburgh School of Medicine
Evan L. Waxman, MD, PhD
COMPREHENSIVE EYE SERVICE
Vice Chair, Medical & Resident Education
Director, Comprehensive Eye Service
Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine






Gabrielle R. Bonhomme, MD
NEURO-OPHTHALMOLOGY SERVICE
Director, Neuro-Ophthalmology Service
Assistant Professor of Ophthalmology
Director, Neuro-Ophthalmology Fellowship
University of Pittsburgh School of Medicine
Ellen Butts, OD
OPTOMETRY SERVICE
Director, Optometry Service
Assistant Professor of Ophthalmology
University of Pittsburgh School of Medicine
Jay Chhablani, MD
RETINA SERVICE
Director of Clinical Research, UPMC
Vision Institute
Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Ian P. Conner, MD, PhD
GLAUCOMA SERVICE
Director, Glaucoma and Cataract Service
Assistant Professor, Department of Ophthalmology
Associate Residency Program Director
University of Pittsburgh School of Medicine
Andrew W. Eller, MD
RETINA SERVICE
Professor, Department of Ophthalmology
Director, Retina and Vitreous Services and Fellowship
Director, Ocular Trauma Service
University of Pittsburgh School of Medicine
William Smith, OD
LOW VISION SERVICE
Director, Low Vision Service
Assistant Professor, Department of Ophthalmology
Program Director, Optometry Residency Low Vision Program
University of Pittsburgh School of Medicine


Issam Al Diri, PhD
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Alexander J. Anetakis, MD, MBA
RETINA SERVICE
Clinical Assistant Professor, Department of Ophthalmology
Retina and Vitreous Service
University of Pittsburgh School of Medicine
Senior Advisor, Translational Sciences team at UPMC Enterprises







Marlene Behrmann, PhD
Professor of Ophthalmology
University of Pittsburgh School of Medicine
Member of National Academy of Science
Larry Benowitz, PhD
Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Emeritus Professor, Harvard University
Miguel Betegon, PhD
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Robert Bittner, OD, FAAO
OPTOMETRY SERVICE
Clinical Assistant Professor of Ophthalmology
University of Pittsburgh School of Medicine
Sandeep Bollepalli, PhD
Research Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Leah Byrne, PhD
Assistant Professor, Departments of Ophthalmology, Neurobiology and Bioengineering
University of Pittsburgh School of Medicine
Kun-Che Chang, PhD
Assistant Professor, Director of Ophthalmology
University of Pittsburgh School of Medicine






Michael Chang, MD
COMPREHENSIVE EYE SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Yuanyuan Chen, PhD
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Xing Chen, PhD
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine



Joshua Clermont, OD
OPTOMETRY SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Susana da Silva, PhD
Assistant Professor, Departments of Ophthalmology and Developmental Biology
University of Pittsburgh School of Medicine
Emily DePew, OD, FAAO
OPTOMETRY SERVICE
Assistant Professor, Department of Ophthalmology
Director, Medical Student and Externship Optometry
University of Pittsburgh School of Medicine



Morgan DiLeo, PhD
Associate Professor, Departments of Ophthalmology, Bioengineering and Clinical & Translational Sciences
University of Pittsburgh School of Medicine
Pavle Doroslovački, MD
OCULOPLASTIC AND ORBITAL SURGERY SERVICE
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Asad F. Durrani, MD
RETINA SERVICE
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Frank Dyka, PhD
Research Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Amgad Eldib, MD
PEDIATRICS OPHTHALMOLOGY SERVICE
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Thomas R. Friberg, MD, FACS
Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine







Kevin Fuller, PhD
Associate Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Chanin J Funair, OD
OPTOMETRY SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Meghal Gagrani, MD
PEDIATRICS OPHTHALMOLOGY SERVICE
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Denise S. Gallagher, MD
RETINA SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Anna G. Gushchin, MD
COMPREHENSIVE EYE SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh Medical School
Richard Hagan, PhD
PEDIATRICS OPHTHALMOLOGY SERVICE
Assistant Professor, Department of Ophthalmology
Director, Electrophysiology Service
University of Pittsburgh School of Medicine
Marissa Heary, OD
OPTOMETRY SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine






Erick Henderson, OD, FAAO
OPTOMETRY SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
James P. Herman, PhD
Assistant Professor, Departments of Ophthalmology and Bioengineering
University of Pittsburgh School of Medicine
Nathan E. Isaacson, OD
OPTOMETRY SERVICE
Clinical Assistant Professor, Department of Ophthalmology
Director, Low Vision Services and Primary Care Optometry
University of Pittsburgh School of Medicine
Farzad Jamshidi, MD, PhD
RETINA SERVICE
Assistant Professor Department of Ophthalmology
University of Pittsburgh School of Medicine
Roheena Kamyar, MD
CORNEA SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Paul (Kip) R. Kinchington, PhD
Professor, Departments of Ophthalmology, Molecular Genetics, and Biochemistry
The Joseph F. Novak, M.D., Chair in Ophthalmology Research
Director, Department of Ophthalmology
Molecular Biology and Gene Expression/Array Module CORE Facility
University of Pittsburgh School of Medicine



Takaaki Kuwajima, PhD
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Kira L. Lathrop, MAMS, PhD
Assistant Professor, Department of Ophthalmology
Co-Director, Imaging Module
University of Pittsburgh School of Medicine
Jennifer Liu, OD
OPTOMETRY SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine








Ekaterina Lobanova, PhD
Associate Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Craig A. Luchansky, OD
PEDIATRICS OPHTHALMOLOGY SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Alex Mammen, MD
CORNEA SERVICE
Clinical Assistant Professor, Department of Ophthalmology
Director, Cornea, External Disease and Refractive Surgery Fellowship
University of Pittsburgh School of Medicine
Najate Ait-Ali Maamri, PhD
RETINA SERVICE
Research Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Jonathan B. Mandell, PhD
Assistant Professor, Department of Ophthalmology
Clinical Laboratory Manager, Campbell Ophthalmic Laboratory
University of Pittsburgh School of Medicine
J. Patrick Mayo, PhD
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Sarah J Michelson, MD
COMPREHENSIVE EYE SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Sabrina Mukhtar, MD, MPH
CORNEA SERVICE
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine









Zachary Nadler, MD
GLAUCOMA SERVICE
Assistant Professor, Department of Ophthalmology
Assistant Residency Program Director
University of Pittsburgh School of Medicine
George T. Park, DO
NEURO-OPHTHALMOLOGY SERVICE
Assistant Professor of Neurology and Neuro-Ophthalmology
University of Pittsburgh School of Medicine
Preeti Patil, MD
PEDIATRICS OPHTHALMOLOGY SERVICE
Associate Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Shaohua Pi, PhD
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Matthew Pihlblad, MD
PEDIATRICS OPHTHALMOLOGY SERVICE
Assistant Professor, Department of Ophthalmology
Fellowship Director, Pediatric Ophthalmology Fellowship
University of Pittsburgh School of Medicine
Scott L. Portnoy, MD
COMPREHENSIVE EYE SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Maria Constanza
Potilinski, PhD
Research Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Gaurav Prakash, MD
CORNEA SERVICE
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Colin Prensky, MD
RETINA SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine









Pamela Rath, MD
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Eric Romanowski, MS
Research Instructor of Ophthalmology
Research Director, Charles T. Campbell
Ophthalmic Microbiology Laboratory
University of Pittsburgh School of Medicine
Boris Rosin, MD, PhD
RETINA SERVICE
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Ethan A. Rossi, PhD
Associate Professor, Departments of Ophthalmology and Bioengineering
University of Pittsburgh School of Medicine
Kateryna Sanders, OD
OPTOMETRY SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Rajesh Sasikumar, MD
GLAUCOMA SERVICE
Associate Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Robert M.Q. Shanks, PhD
Basic Science Director, Charles T. Campbell
Microbiology Lab
Associate Professor, Departments of Ophthalmology
Microbiology and Molecular Genetics
University of Pittsburgh School of Medicine
Tarek Shazly, MD, MSc, PhD, FRCS
GLAUCOMA SERVICE
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Ian A. Sigal, PhD, MASc
Associate Professor, Departments of Ophthalmology and Bioengineering
Director, Image Acquisition and Analysis
Core Module, Ophthalmology and Visual Sciences Center
University of Pittsburgh School of Medicine








Vaneet Singh, MD, MBBS, MS, FRCOphth
COMPREHENSIVE EYE SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Emma Smiley, OD
PEDIATRICS OPHTHALMOLOGY SERVICE
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Anthony St. Leger, PhD
Assistant Professor, Departments of Ophthalmology and Immunology
University of Pittsburgh School of Medicine



Marshall W. Stafford, MD, FACS
COMPREHENSIVE EYE SERVICE
Clinical Assistant Professor, Department of Ophthalmology
Director, UPMC Eye Center St. Margaret University of Pittsburgh School of Medicine
John Swogger, DO
GLAUCOMA SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Lillian To, MD
GLAUCOMA SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Kiran Kumar Vupparaboina, PhD
Research Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Xiangyun Wei, PhD
Associate Professor, Departments of Ophthalmology, Microbiology and Molecular Genetics, and Developmental Biology
University of Pittsburgh School of Medicine
Andrew Williams, MD
GLAUCOMA SERVICE
Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Kirsten Winter, OD
OPTOMETRY SERVICE
Clinical Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Gary (Hin-Fai) Yam, PhD
Research Associate Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine

Hongmin Yun, MS, MD, PhD
Research Assistant Professor, Department of Ophthalmology
University of Pittsburgh School of Medicine
Islam M. Zaydan, MD
NEURO-OPHTHALMOLOGY SERVICE
Associate Professor of Neurology and Neuro-Ophthalmology
Co-Director, Multiple Sclerosis and Comprehensive Care Center
University of Pittsburgh School of Medicine
Co-Director, Multiple Sclerosis Center of Excellence
Pittsburgh VA Hospital



John Gote, MD Resident in Ophthalmology

Gagan Kalra, MD Resident in Ophthalmology

Eitan Shemuelian, MD Resident in Ophthalmology




Oliver Beale, MD Resident in Ophthalmology

Amani Davis, MD Resident in Ophthalmology

Aidan Dmitriev, MD Resident in Ophthalmology

Colin Xu, MD Resident in Ophthalmology
Haniah Zaheer, MD Resident in Ophthalmology
Ryan Zukerman, MD Resident in Ophthalmology
Crystal Lee, MD, MPH Resident in Ophthalmology
Samyuktha Melachuri, MD Resident in Ophthalmology
Ryan Williamson, MD, PhD Resident in Ophthalmology



Patricia Campos, MD Resident in Ophthalmology

Raven Diacou, MD, PhD Resident in Ophthalmology

Doowon Huh, MD, PhD Co-Chief Resident







Anas Abusief, MD Pediatric Ophthalmology Fellow
Karl Andersen, MD Cornea Fellow


Tatyana Beketova, MD Retina Fellow

Gunjan Chadha, MD Pediatric Ophthalmology Fellow
Farid Kalantaritarari, MD Neuro-Ophthalmology Fellow
Pearson Miller, OD Optometry Fellow
Saloni Kapoor, MD Co-Chief Resident
Christina Kong, MD Resident in Ophthalmology
Gideon Nkrumah, MD Resident in Ophthalmology
Matthew Sommers, MD Glaucoma Fellow
Anna Terrarosa, MD Oculoplastic and Orbital Surgery Fellow
Anthony Thieu, MD Cornea Fellow



Aditya Uppuluri, MD Retina Fellow
Bushra Usmani, MD Glaucoma Fellow
Ariel Wong, OD Optometry Fellow

José-Alain Sahel, MD, received EURORDIS Scientific Award 2024
José-Alain Sahel, MD, Distinguished Professor and Chairman of the Department of Ophthalmology at the University of Pittsburgh School of Medicine and Director of the UPMC Vision Institute, received the EURORDIS – Rare Disease Europe Scientific Award 2024 at the annual EURORDIS Black Pearl Awards event on Feb. 20, 2024, a hybrid ceremony that took place both online and in Brussels, Belgium.
Leah Byrne, PhD, Named Senior Member of the National Academy of Inventors
Leah Byrne, PhD, Assistant Professor of Ophthalmology at the University of Pittsburgh School of Medicine, has been named a Senior Member of the National Academy of Inventors (NAI).
The NAI is a member organization of universities, government agencies, and nonprofit research institutes from around the world that aims to recognize, encourage, and celebrate inventors and raise awareness about how new inventions benefit society.
José-Alain Sahel, MD, received Macula Society Michaelson Award
José-Alain Sahel, MD, Distinguished Professor and Chairman of the Department of Ophthalmology at the University of Pittsburgh School of Medicine and Director of the UPMC Vision Institute, received the Macula Society Michaelson Award, delivered the Michaelson lecture on gene-independent strategies for retinal degenerations, and organized a related symposium at the society’s 47th Annual Meeting in Palm Springs, Calif., on Feb. 7.
Expertscape Recognizes UPMC Vision Institute Faculty
Expertscape, an online resource for biomedical information and leading physicians in various disciplines, has named four UPMC Vision Institute faculty members as world experts in their subspecialties:
José-Alain Sahel, MD; Ken Nischal, MD; Vishal Jhanji, MD; and Jay Chhablani, MD. According to its website, Expertscape determines expertise based solely on a physician’s scientific publications; those who rank in the top 0.1% of all published authors on a topic are termed world experts.
José-Alain Sahel, MD, Featured on Neuroscience Perspectives Podcast
José-Alain Sahel, MD, Distinguished Professor and Chairman of the Department of Ophthalmology at the University of Pittsburgh School of Medicine and Director of the UPMC Vision Institute, was the keynote speaker at the 33rd Biennial Center for Visual Science Symposium at the University of Rochester. He recently joined John Foxe, PhD, for a “Neuroscience Perspectives” podcast episode to discuss his gene therapy research and clinical trial efforts.

Xing Chen, PhD, Receives 2024
NIH Director’s New Innovator Award
Xing Chen, PhD, an Assistant Professor of Ophthalmology at the University of Pittsburgh School of Medicine and researcher at the UPMC Vision Institute specializing in visual neuroscience, recently received the 2024 National Institutes of Health (NIH) Director’s New Innovator Award, which aims to support high-impact research from an early-stage investigator. The award is one of four in the NIH Common Fund’s high-risk, high-reward research program, an initiative that provides funding for innovative research with the potential for broad impact in biomedical, behavioral, or social sciences.
José-Alain Sahel, MD, Receives 2024 Wolf Prize in Medicine
José-Alain Sahel, MD, Distinguished Professor and Chairman of the Department of Ophthalmology at the University of Pittsburgh School of Medicine and Director of the UPMC Vision Institute, received the prestigious Wolf Prize in Medicine together with his colleague Botond Roska, MD, PhD, of the Institute for Molecular and Clinical Ophthalmology Basel (IOB), for their work to restore sight using optogenetics, a research tool that uses light to control cell activity.
19 UPMC Ophthalmologists Recognized on Pittsburgh Magazine’s Top Doctors List
These physicians are part of the Top Doctors® list, which is compiled by Castle Connolly. The Castle Connolly Top Doctor selection process is entirely meritbased. Castle Connolly’s peer-to-peer nominations and rigorous research process ensure only the most qualified physicians are included.
Alexander Anetakis, MD
Gabrielle Bonhomme, MD
Joel D. Brown, MD
Ian P. Conner, MD
Deepinder K. Dhaliwal, MD
Denise Gallagher, MD
Anna G. Gushchin, MD
Roheena M. Kamyar, MD
Alex Mammen, MD
Joseph N. Martel, MD
Kanwal Ken Nischal, MD
Matthew S. Pihlblad, MD
Colin Prensky, MD
Pamela P. Rath, MD
Tarek Shazly, MD
Marshall W. Stafford, MD
Susan Tonya Stefko, MD
John S. Swogger, DO
Evan L. (Jake)
Waxman, MD, PhD


Karima Khimani, MD, received the Outstanding Clinical Fellow of the Year Award presented by the Senior Residents of the Department of Ophthalmology University of Pittsburgh School of Medicine
David Mora-Boellstorff, MD, received the Jay G Linn Award presented by the Faculty of the Department of Ophthalmology University of Pittsburgh School of Medicine
MEDICAL STUDENT AWARDS
Haniah Zaheer received the Andrew Keverline Memorial Award for excellence in May 2023.
FACULTY AWARDS AND RECOGNITION
Marlene Behrmann, PhD – 2023 Howard Crosby Warren Medal, Society of Experimental Psychologists (SEP)
Leah Byrne, PhD – 2023 University of Pittsburgh Office of Innovation Emerging Innovator Award
Deepinder Dhaliwal, MD, L.Ac – International Society of Refractive Surgery’s Founders’ Award
José-Alain Sahel, MD – Elected as a Fellow of the National Academy of Inventors (induction in June 2024)
Andrew Eller, MD – 2024 Albert C. Muse Award for Excellence in Innovation and Service in Ophthalmology
Debasish Sinha, PhD – Edward N. & Della L. Thome Memorial Foundation Award for Age-Related Macular Degeneration Research
Andrew Williams, MD – David Epstein Clinical-Scientist Award, Chandler Grant Glaucoma Society
José-Alain Sahel, MD, Distinguished Professor Chairman of the Department of Ophthalmology at the University of Pittsburgh School of Medicine and director of the UPMC Vision Institute, received the prestigious Wolf Prize in Medicine together with his colleague Botond Roska, MD, PhD, of the Institute for Molecular and Clinical Ophthalmology Basel (IOB), for their work to restore sight using optogenetics, a research tool that uses light to control cell activity.
Cells in the retina convert light into electrical signals, which travel through the optic nerve to the brain. When these cells are damaged, vision loss can occur. Optogenetics uses gene therapy to reprogram retina cells, making them sensitive to light. Specially engineered goggles accompany this therapy, emitting light pulses that activate the reprogrammed cells, partially restoring vision.
Dr. Sahel and Dr. Roska have collaborated in the field of optogenetics for many years. In 2021, the pair published, with his collaborators at the Paris Institut de la Vision, which Dr. Sahel founded and directed, a
groundbreaking study in Nature Medicine that outlined the first instance of partial vision restoration in a human patient. This is the first-ever published clinical application of optogenetics; the trial was conducted in Paris, London, and Pittsburgh.
“It is deeply gratifying to see José’s life-changing work honored with the Wolf Prize, one of the most prestigious awards in science,” said Anantha Shekhar, senior vice chancellor for the health sciences and John and Gertrude Petersen Dean of the School of Medicine at Pitt. “He brings a brilliant mind and genuine humility to the tireless pursuit of helping to restore vision to patients. We are very fortunate to have him on the faculty at the University of Pittsburgh.”
Since 1978, the Wolf Foundation awards the Wolf Prize to scientists and artists to recognize outstanding achievements that contribute to the betterment of humanity. An international committee reviews nominations each year and selects the prize laureates. Dr. Sahel and Dr. Roska join a distinguished group of more than 380 scientists and artists from around the world whose work transcends societal barriers and aims to improve the human experience.

Ophthalmology is a key priority for UPMC and the University of Pittsburgh. This commitment was highlighted in a virtual panel discussion that featured Alexander Anetakis, MD, a vitreo-retinal surgeon at UPMC and physicianadvisor at UPMC Enterprises, and leaders of two companies developing gene therapies to treat inherited vision disease.
The University of Pittsburgh Department of Ophthalmology and the UPMC Vision Institute were well represented at the 6th annual i2EYE event with multiple faculty members sharing their clinical and research expertise in a series of panel sessions and discussions.
The prestigious interdisciplinary i2Eye conference, hosted by UPMC, the University of Pittsburgh, and Institut De La Vision, focuses on innovative imaging of eye diseases. The event was held at the newly constructed UPMC Mercy Pavilion,
the Vision Institute’s headquarters. The pavilion opened in May 2023 and is a state-of-the-art facility where the clinical and research expertise of UPMC and the Department of Ophthalmology help to prevent vision loss and restore sight.
World leaders in eye treatments and imaging came together in Pittsburgh to share advances in their disciplines at the i2Eye Conference, which was hosted in September by the University of Pittsburgh Department of Ophthalmology, the UPMC Vision Institute and world-renowned institutions in Paris.
Hundreds of volunteers, including faculty members, trainees, alumni, and staff from the UPMC Vision Institute, Department of Otolaryngology, University of Pittsburgh School of Health Sciences Communication Science
and Disorders Department, and University of Pittsburgh School of Dental Medicine delivered free care to patients in need at the eighth annual Mission of Mercy Pittsburgh event on Nov. 1 and 2 at the David L. Lawrence Convention Center in Pittsburgh.
The University of Pittsburgh School of Medicine Department of Ophthalmology hosted its second annual Alumni Reunion Thursday, Sept. 26 through Saturday, Sept. 28. Events began with a welcome reception on Thursday, Sept. 26 at the Pittsburgh Marriott City Center, followed by two days of engaging presentations at the UPMC Vision Institute’s headquarters at the new UPMC Mercy Pavilion in Uptown Pittsburgh.


The 13th annual Louis J. Fox Center for Vision Restoration Conference was held at the Vision Institute at UPMC Mercy Pavilion October 8-9, 2024. For the first time, the pathways towards clinical trials were discussed in terms of what to consider in getting research ready for that stage. While there is still a way to go, this illustrates the progress being made.
The meeting was organized by University of Pittsburgh faculty members Takaaki Kuwajima, PhD; Kun-Che Chang, PhD; Issam Al diri, PhD; Larry Benowitz, PhD; and John Ash, PhD. It attracted well over 80 attendees that included scientists, students, postdocs, ophthalmologists, and philanthropists.
For two full days, cutting-edge research was presented on optic nerve preservation and regeneration. The conference featured an outstanding keynote presentation by Zhigang He from Harvard Medical School and Boston Children’s Hospital. There were an additional 25 speakers who are world leaders in the field who came from prestigious institutions, including Harvard, Stanford, the University of Pennsylvania, Washington University, Johns Hopkins Hospital, the Wilmer Eye Institute, UCSF, and the University of Pittsburgh.
“This conference is getting even better every year,” said José-Alain Sahel, Director of the Vision Institute and Chair, Department of Ophthalmology. “It was clear that major progress has been made in developing
therapies to regenerate the optic nerve. This year, new transformative science from related but different fields was shared. The partnership with the Gilbert Family Foundation, Brightfocus, the Glaucoma Foundation, and the start of the upcoming ARPA-H program hold immense promise.”
Exciting new research was presented on developing new gene and stem-cell therapies to promote ganglion cell survival and regeneration of damaged axons. Multiple new approaches were presented. For the first time, researchers showed promising results of axon regeneration from the damaged nerve to the brain with modest vision restoration in preclinical models. Also, for the first time, clinical trial data was presented for gene therapies to treat optic neuropathies, and additional speakers discussed strategies to overcome barriers to developing new clinical trials.
In his concluding comments, Dr. Benowitz said, “We’re in a very, very exciting era, and thanks to the work of people in this room, I think the future is looking sunnier.”
Interviews with additional attendees included similar praise for the meeting and optimism for the field.
“[All the speakers] say this has become one of the more important meetings each year for the field, because it’s very focused on optic nerve regeneration alone,” said Lawton Snyder, Eye & Ear Foundation CEO.
Leonard Levin viewed the conference as a chance to catch up in the field he’s part of. It was also an opportunity to see where the leaders – many of whom are friends – are at. “We’re getting the cutting-edge (continued)
The 13th Annual Louis J. Fox Center for Vision Restoration Conference
(continued from page 43)
work told to us, even before it’s published in many cases,” he said. He described the community as close, because they all have the same goal to restore vision.
“A big theme from the two-day conference was that advancements have been made in all areas,” said Lawton Snyder, Eye & Ear Foundation CEO. “As Larry Benowitz (Co-Director of the Fox Center) stated in his remarks, ‘The work 20 years ago when this all started looks very different than it does today.’” This includes multiple modalities having a profound impact on optic nerve regeneration.
Jeff Gross said this conference and past Fox Center conferences have really pushed the field forward. He praised the synergy that occurs in bringing everyone together, saying so much more progress comes after the meeting as a result.
i2Eye, the sixth annual interdisciplinary conference on innovative imaging of eye diseases, was held in September at the UPMC Vision Institute. Around 165 people from all over the world attended the three-day event, with 40 from France.
Speakers and attendees were a mix of physicists, biologists, and ophthalmologists. This year’s conference experimented with broadening the scope to include more biological and neuroscience topics, as well as more industry participation and professional development programming for trainees.
In his introductory message, Department Chair JoséAlain Sahel said, “We are thrilled to host the i2Eye conference at the Vision Institute of Pittsburgh. This conference was started six years ago by Kate Grieve, Michel Paques and Ethan Rossi and has become an annual event bringing together a growing community of researchers around innovative imaging of eye diseases and now many other areas of vision science.”
Topics included innovative imaging technologies for structural imaging of the anterior segment and retina, functional retinal imaging, ocular immunology and inflammation, eye movements, age-related macular degeneration, glaucoma, animal models, organoids and novel vision restoration therapies such as optogenetics. Scientific sessions consisted of invited and submitted talks grouped by topic followed by lengthy discussions. These discussion sessions are a unique aspect of
In a conversation with Snyder, Louis J. Fox said he and José-Alain Sahel, MD, Chair of the Department of Ophthalmology, have a similar view. They do not like the word no. He said the researchers and clinicians come self-motivated. It is not about the money or fame; it is about the idea of getting the job done. Everyone is working toward the same goal.
“It’s exciting to see new and unpublished work showing promising discoveries in optic nerve regeneration,” Dr. Ash said. “While there is still a long way to go, research presented at the meeting demonstrated significant progress in the field. Every year, we are getting closer to restoring functional vision to patients with optic nerve injury.”
the i2Eye format, where “we aim to bridge between disciplines for fruitful discussions on how to move our interrelated fields of investigation forward together,” the conference website stated.
Additional programming included a poster session, roundtable discussion with industry, hands-on demonstrations of innovative imaging technologies, Vision Institute laboratory tours, and professional development activities for trainees.
On-site and online registration was free of charge to all invited speakers and attendees working in academia or at nonprofit institutions. Online participants were able to join virtually for certain sessions.
Dr. Sahel said one of the key strengths of the conference was the people. “The ability to bring together people from the U.S. and Paris and so many important researchers from all the countries [means that there is] lots of expertise,” he said. “They wish to work together and bridge the gaps and knowledge and provide better care for our patients.”
Director of the IHU FOReSIGHT, Christophe Baudouin, expressed how important it is to continue the strong relationship between Paris and Pittsburgh, which means meeting repeatedly in both countries. He lauded the fascinating achievements in imaging. “Innovation in terms of imaging right now and potential application in the future has been absolutely amazing,” he said.

i2Eye Conference attendees
The
collaborative staircase where scientists and clinicians meet to discuss work to advance patient care.
Digital Twin of the Eye featuring Jay Chhablani, MD
Ocular Inflammation featuring Alex Mammen, MD
Glaucoma and the Role of a Patient Navigator in Vision Care
featuring Andrew Williams, MD
Seeing the Future of Gene Therapy
featuring Michelle Alabek, MS, LCGC, and José-Alain Sahel, MD
Leveraging the Microbiome to Alleviate Ocular Surface Disease
featuring Anthony St. Leger, PhD
AMD and Geographic Atrophy – Advancements in Research and Care
featuring Kunal Dansingani, MBBS, MA, FRCOphth and John Ash, PhD
Introducing StreetLab –Improving Functional Outcomes in Low Vision Rehabilitation featuring Rakié Cham, PhD
Everything You Want to Know About Keratoconus
featuring Gaurav Prakash, MD, and Vishal Jhanji, MD, FRCS (Glasgow), FRCOphth, FARVO
Cerebral Visual Impairment
featuring Ken Nischal, MD, FAAP, FRCOphth
Scan for blog and webinar libraries:

The Eye & Ear Foundation, an independent 501(c)(3) organization, was founded in 1985 to foster support for the Departments of Ophthalmology and Otolaryngology –Head & Neck Surgery at the University of Pittsburgh through the generous support of individuals and organizations.
In supporting these world-class departments, we hold ourselves to the same high standards. The goal is to keep moving forward, expanding EEF’s support network, and helping the Departments of Ophthalmology and Otolaryngology – Head & Neck Surgery stand peerless in the distinction of research and education and, ultimately, the highest level of care provided to our patients.
“The Eye & Ear Foundation’s support enhances patient care,” said CEO Lawton Snyder. “We do this by supporting the work of the outstanding clinical and research faculty in the Departments of Ophthalmology and Otolaryngology – Head & Neck Surgery at the University of Pittsburgh. EEF has played a major role in making these departments worldwide leaders in the field and in research and development pathways for care.”
To learn more about the Foundation or to support the Department of Ophthalmology, please visit eyeandear.org or scan this QR code.

WAYS TO GIVE
• Bequests
• Cash
• Charitable Gift Annuities
• Charitable Trusts

UPMC Vision Institute at UPMC Mercy Pavilion 1622 Locust Street, 5th Floor Pittsburgh, PA 15219
• IRA Charitable Rollover Gift
• Life Insurance Gifts
• Stock Transfers
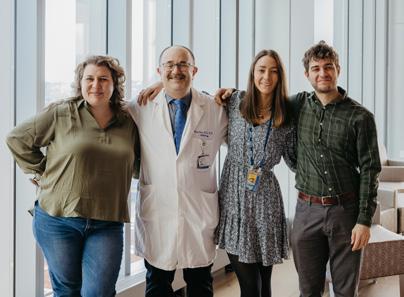







School of Medicine
Department of Ophthalmology
Supporting Research to Improve how we Hear, See, and Live
UPMC Vision Institute at UPMC Mercy Pavilion 1622 Locust Street 5th Floor
Pittsburgh, PA 15219
Clinics: 412-647-2200
Optical Shop: 800-446-3797
Urgent Eye Care: 412-647-2200
Clinical Trials: 412-642-7888
Research: research@eyeandear.org Eye & Ear Foundation: 412-864-1300
More about the Department of Ophthalmology at the University of Pittsburgh and UPMC Vision Institute can be found at ophthalmology.pitt.edu or scan the QR code.
