

DAILY NEWS






A DUTY TO DEFEND THE FRAGILITY OF ACADEMIC FREEDOM
In his cautionary Presidential Address, Professor Volkmar Falk issued a stark warning that the value of Academic Freedom - the right to research, teach and express ideas without undue interference - is under threat and reminded us that we all have a responsibility to maintain its integrity.
Today, we take for granted that we can meet here in Copenhagen for an undisturbed scientific exchange, express different opinions and debate without government interference. But we cannot ignore the signs that indicate times are changing...” he began. “One of the most important advocates of Academic Freedom as we understand it today was the German philosopher and linguist Wilhelm von Humboldt, who believed that true knowledge emerges not from written transmission or dogmatic oversight, but from critical thinking, open-ended discovery, dialogue and personal intellectual development.”
He explained that in the aftermath of World War II, policy makers in Europe understood that Academic Freedom must be protected against future political interference, and it has been protected on a


national and European level. Of course, he acknowledged that Academic Freedom is not absolute: it is subject to professional standards, ethical responsibilities, relevance to the subject matter, and, in some cases, institutional governance.
Many of society’s most significant transformations - from advances in public health to innovations in climate policy - are the result of independent, long-term research, fostered within academia’s protected environment for investigation and open dialogue. Moreover, there is a growing body of empirical research that demonstrates that Academic Freedom contributes not only to intellectual growth and societal wellbeing, but also to economic prosperity, public health and global cooperation. He said the evidence is clear - Academic Freedom is not merely a normative democratic value, a key element of human rights and an expression of human dignity, but a measurable determinant of societal innovation.
“Unfortunately,” he added, “the reverse is also true. When countries restrict Academic Freedom, they inevitably slow down the very engine that drives new technologies, and


Patrick Myers –Secretary General (re-elected)
Gloria Färber – Acquired Cardiac Domain Chair
Lorenzo Galletti Vice President
Mario Gaudino Editor-in-Chief


Continued from page 1
ultimately, progress and prosperity.”
In describing how and why Academic Freedom is under threat, he said that after elections in 70 countries, for the first time in over 20 years, the world has fewer democracies than autocracies. With only 29 liberal democracies in 2024, they have become the least common regime type in the world. At a time when nationalism is again on the rise, in many countries, Academic Freedom is increasingly threatened by populist left- and right-wing parties, through media censorship, undermining elections and civil society, and restricting Academic Freedom.
“So, you may ask why is this our responsibility? I will try to convince you that we, as individuals and as an organisation, must play our part to protect European moral and ethical values, and actively call for Academic Freedom, as it is one of the pillars of our democracy. If we may agree that, based on our position in society, we do have a moral and ethical obligation to act, let’s discuss what can, what should be done.”
Professor Falk reminded us that the fight for Academic Freedom is not new. History offers a long line of remarkable academics who have stood up for the rights of scholars – such as Galileo Galilei, Giordano Bruno, Andrei Sakharov and Rudolf Virchow - often at great personal risk. He emphasised he is not advocating that “We need to go as far as Virchow and form a political party or remonstrate with political leaders until they challenge us to a duel.” Nevertheless, he offered five practical ideas that each of us can do:
Firstly, dare to know. He said that as individuals we need to overcome self-imposed immaturity, to think independently, to question traditional authorities and dogmas, and to use reason courageously in the pursuit of knowledge and freedom.
Secondly, be aware of self-censorship. Rather than avoiding a discussion on politics and hiding personal views, we have to fight alternative truth with the hard facts of science, stressing that we should take every effort to keep arguing, especially with those individuals who believe in obscure myths of oppression or follow populist conspiracy theories. This includes supporting our institutions so that they can withstand the dangers of anticipatory obedience - not an easy task, as it may create personal tensions or may impact essential research funding streams.
Thirdly, engage in public dialogue. He argued that communication is one of the strongest tools at our disposal, and as scientists must explain ourselves and what we do in an easy-to-understand manner to the public. Engaging in an open dialogue sparks enthusiasm for the science, increasing people’s
Volkmar Falk (EACTS President)
“I'm very happy that we came back to Copenhagen. We have been here once before. And I'm very, very excited about this year's winner, which shows that yes, innovation is possible in cardiac surgery.”
Jolanda Kluin (New Technology Task Force Member)
“The Techno-College, for me is the greatest day of the entire meeting. We have the Innovation Award that is granted to the one researcher, the one abstract that we think is the best.”
Marion Durand (Thoracic Robotic Surgery Task Force Chair)
“It's a closer presentation. It's really dedicated to the training level and sharing of expertise. This year’s special highlights of the Techno-College are first 3D ‘live in a box’ of a SP procedure mediastinal surgery, which was unique, the first in Europe.”
Joerg Kempfert (New Technology Task Force Chair)
“So this year at Techno-College we are focusing, of course, as usual, on the live cases. This is, I think, the core of Techno-College. We are the largest live case meeting worldwide and we're the only ones still transmitting in 3D. So we had a complex arch procedure with a frozen elephant trunk with new connecting devices. The room was packed, we had good interaction with the audience. This is something that is really pointing in the right direction for the future. I just learned that this year we are hitting the 1,000 mark for attendees at Techno-College and we have, to my knowledge, more
understanding and building a more informed society that is less prone to conspiracy theories.
Fourth, act at an institutional level. In times such as these, he urged us all to support our institutions, be it a university or a hospital, and to defend their values.
He concluded his Presidential Address with a call to arms: “Professional organisations such as EACTS can enable scholars to join international educational programmes, facilitate international research collaborations and help to form crosscountry alliances, all of which can help to stabilise Academic freedom. As a strong community with more than 4,000 members, we can and we must take steps to support and protect Academic Freedom for ourselves and future scientists. The Motto of this Annual Meeting is ‘Designing the Future – Innovate, Discover, Educate’. Don’t take Academic Freedom for granted. We must engage with people to win the argument, to protect the integrity of science in the future. Colleagues – we cannot pass this responsibility. We must step up to this challenge. I therefore would like to add one more thing: engage!”

than 100 different countries represented. We are not only a European society, we are more globally recognised.”
Anfal Madaci (Algeria)
“I travelled from Algeria to attend this Annual Meeting. I feel like this is a great opportunity to learn about innovations, to network and to meet with great minds in the field.”
Ghada Shahin (Thoracic Robotic Surgery Task Force Member)
“We have the workshop with very interesting machines for treatment and diagnosis of lung cancer. I really love training people because I think it is so important to exchange knowledge and people here are really nice. Everyone is just willing to learn.”
Isaac George (winner of the 2025 Techno-College Innovation Award)
“The Award is really meaningful. It's a really special presentation. So my lecture focused on light application that we can apply to saphenous vein grafts to help improve their durability and primarily reduce neointimal hyperplasia, which is formation of substance inside veins that can cause them to close over time.”
Corrine Messina (Italy)
“Attending the EACTS is very important for me. I think it's a great opportunity for me to deepen my knowledge in cardiac surgery since I'm a resident. It's wonderful. It's like a full immersion in cardiac surgery.”

An interview with the new EACTS President, Professor Rafael Sádaba
We sat down with the new EACTS President, Professor Rafael Sádaba, to discuss the Association's evolution, its strengths, future challenges and his aims for his presidency....
In 1999, Professor Rafael Sádaba was working at Leeds General Infirmary, UK, as a resident in cardiothoracic surgery. That year, the 13th EACTS Annual Meeting was held in Glasglow, Scotland, and although he had heard of the Meeting, this was his first opportunity to attend.
“I remember being so impressed, I was like a child in a toy store. So many surgeons from all over the world, so much science, so many people talking about many interesting things, having the opportunity to listen to very opposing views on how to tackle different problems. I was particularly impressed that there was a lunch session for residents, and it was an opportunity to discuss matters that were relevant to residents, in terms of education and training opportunities, etc.”
The next EACTS Meeting he attended was in 2001 in Lisbon, where he approached the Chair of the Residents’ Committee, Professor Pieter Kappetein (who later became EACTS Secretary General), and told him how impressed he was with the Meeting and asked if he could become involved. To his surprise, Professor Kappetein replied, “You are now nominated, you are now part of the Residents’ Committee!”...and Professor Sádaba has been directly involved in EACTS since then. Over that time, he explained that the Association has changed dramatically.
“When I first became involved with the Annual Meeting, it was organised by Kathy McGree and Sharon Pidgeon, and their team of six or seven people in Windsor. Looking back, for such a small team, they really did an amazing job in organising memberships, training courses and of course, managing the Annual Meeting – which came from nothing to become the biggest cardiothoracic meeting in the world. However, the organisational arrangement of EACTS has had to evolve as
the Association has grown. So, now we have appointed specialists in every key role and I think that we have emerged as a more professional organisation in terms of our personnel, communication and structure.”
For Professor Sádaba, two of the most important aims for EACTS are promoting inter-professional collaboration and increasing the global outreach of the Association. For example, in Copenhagen, there have been numerous joint sessions with other professional associations like intensivists and cardiologists, which is crucial for integrating different views, collaborating on problem-solving and ultimately improving patient care.
“I think it's important to listen to the views of our fellow professionals from different specialties with whom we work every day. We need to understand how they see the problems that we tackle together so we can collaborate to solve them. We also collaborate and have joint sessions with other associations, notably North America and Asian associations, and that's beneficial because you see different perspectives in different parts of the world on the same problems, and you always have new ideas from other parts of the world that you may not have thought of locally. It's enriching for everyone to have a large variety of professionals, both in terms of knowledge in diseases that we treat and geographically. It's quite interesting to listen to fellow colleagues from other parts of the world, who perhaps don't have the resources that we have in Western Europe, and how they manage to overcome shortages.”
One of the key aims of his presidency is to provide educational opportunities to parts of the world with fewer resources, such as Latin America and Africa. EACTS already collaborates closely with organisations like the Society of Thoracic Surgeons (STS) to achieve this, holding joint conferences and sessions, and the focus is primarily on education rather than providing direct care or resources.
“Our Outreach Programme is really about giving those parts of the world that do not have
Handing over the baton
Yesterday, Professor Filip Casselman handed over the reins of the Acquired Cardiac Disease Domain to the new Domain Chair, Professor Gloria Färber. Here, he discusses some challenges and achievements of his term...
“ It is with absolute gratitude that I look back on my term as the Chair of the Acquired Domain. The honour of being selected as a Chair is an immense one but also comes with a substantial responsibility. I have tried to give the best of myself in this role, and I hope my efforts were appreciated by many,” he explained. “A term for the Chair of the Domain is three years, starting right after the Annual Meeting. It has been three intense years during which I learned a lot through the various duties that were assumed. But I also enjoyed very much serving the Association, which remains, I repeat, a true honour.
“One of my main tasks and hence accomplishments was the restructuring of the Task Forces. Task Forces are an essential ‘tool’ in the structure of our organisation. Each Task Force covers a subfield of Acquired (adult) Cardiac Surgery, has a chair and a variable number of members. These people play an important role in the planning of the Annual Meeting and are also assigned for a three-year period. The challenge was to create a structure in which there is a gradual inflow and outflow of members so that expertise remains present without dilution. This may seem an easy process, but creating it was more complicated than I anticipated. However, I am glad to see that this process is now finalised, and it will hopefully continue to work adequately in the coming years. In addition, it is important that each Task Force has some degree of independence, albeit staying aligned with EACTS ethos and priorities. Overviewing all

sufficient resources, more opportunities in terms of education, that they might not otherwise have. Currently, we have a conference in Latin America with first-class educational opportunities for Latin American surgeons, and now we are working actively to bring this to Africa. Education is one of the things that is very much in the DNA of EACTS.”
He said that the Association is able to do this because of its highly skilled and motivated members who volunteer to give up their time and work for free to ensure its continued growth.
A second reason is the "phenomenal" and “highly professional”, EACTS staff at Windsor House.
“We’ve never had so many training opportunities and educational activities. I think we are an example for other societies in the world, and they look up to us. But, we must also face the challenges ahead.”
These challenges come from other specialties, such as cardiology and respiratory medicine, which now offer less invasive treatments for diseases traditionally treated by surgeons. He said another challenge is to shift the Association's focus from treating diseases to treating patients and their outcomes. This involves concentrating on innovation to achieve better results, fewer complications, faster recovery and longlasting effects. The Innovation Summit is seen as a vital platform for this.


this took quite a lot of my time, but was also very rewarding as you interact constantly with very knowledgeable, positively oriented and motivated people.
“My second goal was the further globalisation of EACTS. Traditionally, many members of our organisation are European, but over the years, we have attracted many members outside Europe, and this number continues to grow annually. Our Annual Meeting really has become a global event attended by people from all over the world. This is obviously also a sign that the various Task Forces and Domains do a great job in designing a strong scientific programme!
“In addition, we have introduced the possibility for surgeons active outside Europe to become a Task Force member. This does, however, create some practical issues, and that’s why this process is still very limited. But in addition to this we have given an increasing number of non-European members a forum at our Annual Meeting. No one is excluded, provided the
“What do our patients want? If they are sick, they want to get better without complications, get back to normal life as soon as possible and with long-lasting results. And if we can achieve that, if we are very good at treating diseases better than other specialties, that is the secret for the survival of our specialty. And for that we need innovation. We now have our ‘Innovation Summit’ every year, where experts from different professions, some outside of medicine, come together to debate and exchange ideas on how best to deliver patientcentred surgery. We need to concentrate on things that improve outcomes for the patients as a whole. What matters to the patient, not what matters to the doctors. And for that we need to concentrate and dedicate more time, effort and money to innovation.”
Professor Sádaba believes EACTS members gain unparalleled access to vast knowledge, diverse thinking and direct interaction with experts via an extensive portfolio of educational and training opportunities, particularly beneficial for trainees and early-career surgeons. For those members who want to get involved in helping EACTS, he said they can apply through a self-nomination process on the EACTS website. The primary requirement is a genuine interest in helping the community and a commitment to efficient, dedicated work, rather than self-promotion.
“When my presidency is over, I will not play such a prominent role within EACTS, but I will continue to be engaged and will be happy to collaborate with whatever activity I can help with. But I think it's also important to bring new people. As I said, the strength of EACTS is our membership and we should not be afraid of bringing new people with fresh ideas and fresh views into the organisation.
“What will I do with my time after EACTS? I enjoy golfing with a group of friends, although I'm the worst golfer. I just like going out and spending a few hours on the course, relaxing and forgetting about everything else. So maybe after my presidency, I can try and improve my handicap. My children are adults now, but we are always looking for opportunities to travel together. My wife says, ‘There are two versions of Rafa – one who travels and one who is on call!’ So, we hope to have more chances to travel with our family.”
highest scientific standards are met!
“We have also intensely collaborated with the Society of Thoracic Surgeons from the USA to support and stimulate the Latin American Association of Cardiac and Endovascular Surgery (LACES). Their meeting is also growing and more frequently attended which is of course a very positive evolution. In the future, we should be able to focus more on Africa. This is something I would like to continue working on. International collaboration is important because we have members all over the world. So, we need to support their meetings scientifically in their region of the world. I know the Educational Committee is also very much involved in that, and I think there's still some work to do there.”
“It's a great honour to be the next Chair of the Acquired Cardiac Domain and Filip’s are big shoes to fill! I think the most important observation and task is that our cardiac surgical field is changing very rapidly – we have more robotics, more interventional therapeutic options, etc. This means surgeons have to change, adapt and determine our strategy in this ever-changing field,” said Professor Färber. “I think it's very important that we find a new definition for ourselves, but don't forget our known surgical principles and advantages. This is a complex situation. On the one side, it is very important that the traditional techniques retain their relevance, but on the other side, these techniques may have to be built up in a different way. That frequently means becoming less invasive or performing hybrid procedures. We must therefore continuously train ourselves to perform and master these new techniques. This is a constantly moving target, and I am very happy to support as Chair of the Acquired Domain.”
“There are still many topics we can work on, and at the same time, other topics may become irrelevant after a certain time. So, we need to adapt to that, but I am sure Gloria is going to do very well as the new Chair. I have full confidence she will do the job ten times better than I was able to do.” Professor Casselman added.
Filip Casselman
Past Chair of the Acquired Cardiac Disease Domain
Gloria Färber Chair of the Acquired Cardiac Disease Domain
Rewinding time: Nature’s secret to staying young
Benjamin Franklin once famously said, “But in this world nothing can be said to be certain, except death and taxes.” However, according to this year’s Keynote Speaker, Nicklas Brendborg a PhD student of molecular biology at the University of Copenhagen, plants and animals may have already unlocked the secrets to immortality. In his best-selling book, ‘Jellyfish Age Backwards: Nature's Secrets to Longevity’, published in 2022, he takes the reader on a journey from the farthest reaches of the globe to the most cutting-edge research to explore everything the natural world and science have to offer on the mystery of aging. We spoke with Nicklas about the book and his belief that ageing is a modifiable process, not an unchangeable fate.
“ The book explores the science of ageing. It's basically based on the paradigm that we are fighting a host of different diseases right now, primarily cancer, cardiovascular diseases and dementia, the general idea is that all of these diseases, at the end of the day, are caused by ageing. So, someone my age won’t have dementia, has a really low risk of getting a cardiovascular disease or cancer,” he explained. “If ageing is the main risk factor, you could just slow down the ageing process. Then you had a longer time to live in a healthy body, and you would postpone all of these diseases at once.”
The book is written in three parts. The first part tackles any scepticism, making the reader aware that the whole idea of prolonging life is possible. This is demonstrated by
using cases from the natural world, which is full of examples of animals that live a lot longer than humans and with more complex bodies. He cites the example of the Greenland shark that can live 400, maybe even 500 years.
“The Greenland shark has a brain, a heart, a digestive system, a liver and so on. But for some reason, the shark’s tissue doesn't age as fast as human tissue. Then there are species that live much shorter lives than us. Then there are species that, instead of ageing in this gradual way that we do, do not age at all. The more I looked into it, the more I found these really weird animals, a lobster that does not age, it just goes bigger and bigger and bigger. Then there is the jellyfish, ‘turritopsis dhornii’, that can continually revert back to a juvenile
EACTS Adult Cardiac Database
Using this data for research and developing databases like the ACD and EUROMACS for the cardiac surgery community, helps to identify best practices contributing to improvements in the quality of care for cardiac surgery patients.
“ My role at EACTS is to oversee, together with Edgar Daeter, the Quality Improvement Programme initiatives that we run at the Association. This consists of working with different hospitals and surgeons to look at how we can use data to generate insights to make improvement in patient management, surgery and care,” explained Paola Quattroni, EACTS Quality Improvement Director. “The ACD is a collaborative registry and benchmarking tool of cardiac surgical data for centres across Europe, supporting the development of evidence-based guidelines to improve pre- and post-operative care. Based on real-world data, the database enables the identification of best practice and promotes the importance of

stage. The possibilities are endless.”
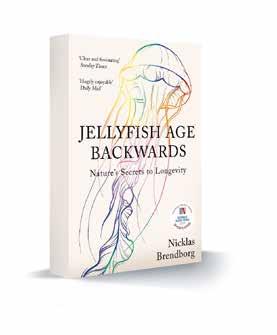
In the second part of the book, he performs a deep dive into the science and outlines what research is currently being performed in preventing the ageing process. In the third and final part of the book, he explains what the reader can do to keep healthy to try and expand their own longevity, whilst we wait for all of these wonder drugs to come to market.
The book has been a tremendous success both critically and commercially, it became the most translated Danish book this century, has been translated into 30 different languages, has sold hundreds of thousands of copies, and it was the bestselling Danish and non-fiction book in 2022 and was shortlisted for the 2023 Royal Society Science Book Prize.
integrating quality improvement initiatives into daily clinical practice.”
The ACD drives improvements by giving surgeons the tools to compare and benchmark their hospital’s data with other centres across Europe. This allows them to identify areas of improvement in their clinical practice, helping to improve patient outcomes. Participation in the ACD is free of charge for hospitals.
Dr. Edgar Daeter, cardiothoracic surgeon at St Antonius Hospital in Niewengein, is the Chair of the Quality Improvement Programme and ACD Task Force, and has been involved since the inception of the renewed ACD.
“We want to collect a limited but significant amount of data about surgical procedures. The aim is to aggregate this data for surgeons to access via an interactive viewer or tool that shows them graphs so that they can get insights from that data. They will be able to see the different trends of surgical procedures over time against certain patient groups. The interactive viewer is also a benchmarking tool for surgeons to compare their own hospital data and outcomes to data and outcomes from other hospitals. By using risk correction outcomes of
“It actually took me a longer time to publish it than it took to write. It took me about a year to write, but it was rejected and rejected and rejected. I think publishers were reluctant to publish a scientific book by someone who was not a professor with a distinguished career. Finally, I found a small publisher who actually jumped on the idea, and since then, its success has been crazy. I already knew that I loved writing, but writing this book, I rediscovered how much I really appreciate the process of researching and learning all these cool facts, and then trying to convey them in a very crisp and clear manner.”
In June this year, he published an English version of the sequel to his first book called ‘Super Stimulated: How our biology is being manipulated to create bad habits – and what we
types of surgery for patients with selectable risk profiles, outcomes can be benchmarked on a hospital or country level to identify potential improvements for participating hospitals. A surgeon can see if their hospital is an outlier for a particular procedure and examine the reasons why there are differences in outcomes. By looking at the data, it might be the case that they are operating on certain patient groups with comorbidities. For example, through the database, a surgeon can look at length of stays, mortality rates, age, comorbidities etc., across different countries and healthcare systems. Importantly, by using the database, surgeons will have a unique opportunity to find useful insights and implement improvements at their hospital.”
Dr. Daeter explained that now that the database includes over 55,000 procedures from about 21 international hospitals and more datasets are expected to be added soon, the QUIP team will soon organise some online community meetings for participant hospitals.
“The ACD and EUROMACS have a research pillar based on a research data request protocol, to ensure trustworthy access to de-identified data. Unique in the protocol is the opting-out system for contributing hospitals. When a research data request is submitted, all participating hospitals will receive the request
can do about it’. He is currently writing the final book of his trilogy. The books are published in Danish first, and then about a year later, an English version is released. He explained that the time between the two releases helps him gauge what people liked and what they did not understand, so he can make the international version even better.
“As humans, we are pretty fortunate as we live longer than most mammals our size, but also that we do have some blind spots. So, in the book, I also dive into the differences between humans. For example, Jeanne Calment is the oldest person ever, and she lived to be 122 years. Genetically, she is obviously very similar to us. But if we could discover what was so special about her, we could break the ceiling of our current lifespan. However, we will need innovation to do so.
“If you're human, you're going to age, and in that way it's kind of the universal topic, it is the one thing that unites us all. In my Keynote Speaker Lecture, I want to share with experts that ageing is something modifiable, even though we don't usually think about it that way. We have all these wonderful solutions in nature, and there are actually a lot of people working on it already. I will present that it's possible to fight ageing, what is being done right now and what the current challenges are.”
and will be able to opt out from the research if they wish. The hospitals will always be able to decide on whether to share their data or not.”
In addition to the database work, QUIP has another dimension as a registry by bringing interested communities together. With the help of the cardiothoracic surgery community and other international registries we are keen to better understand current collection methods, auditing systems, implementation of GDPR, standardisation of cardiothoracic datasets and preparedness for implementation of the European Health Data Space.
She explained that the new database offers the opportunity to participating hospitals in a more consistent and standardised way, which will help improve data completeness and quality. This means that this data can be used much more effectively to improve best practice and inform patient care. In future, it will be possible to use the database for research. Following a trustworthy and thorough data access request process, researchers will be able to submit their study proposals, and following approval, they will be able to use the data for research purposes.
For EACTS members to set up an account and access the ACD, please visit www.eacts.org/ quality-improvement/adult-cardiac-database/

Korkut Bostanci
Filip Casselman
Nabil Hussein
Milan Milojevic
Patrick Myers
Rafael Sádaba
Florian Schoenhoff
Vladimiro Vida
Alicja Zientara
Working alongside the Events Team:
Sharon Pidgeon
Amanda Cameron
Katie Bingham
Maesie Williams
Millie Shaw
Marina Gueli
Nicklas Brendborg
Thoughts and reflections as past Editor-in-Chief of the EJCTS
Professor Matthias Siepe (Cardiovascular Centre, Inselspital, University of Bern, Switzerland) has been involved with the European Journal for Cardiothoracic Surgery (EJCTS) for more than 15 years. During that time, he has risen through the ranks from a reviewer to an assistant editor to an Associate Editor. In 2016, he was selected as Editor-in-Chief of the Interactive Cardiovascular and Thoracic Surgery (ICVTS), and finally, in October 2020, he was selected as the Editor-inChief of the EJCTS. In this interview, he looks back on his challenges, achievements and why you should get involved in the EJCTS...
“ The role of Editor-in-Chief of the EJCTS is really two roles. The first is to manage the manuscript side of the Journal – maintaining the workflow, finding reviewers, organising the Editorial Office, and so on. The other half, I would say, is more political. As Editor-in-Chief, I am a member of the EACTS Council as well as the Executive Committee, so I spend a lot of time working with colleagues, fostering collaborations with other societies and journals, and solving problems. Of course, we maintain good relationships with other societies and journals, but there is also competition to publish the best science, attract the best manuscripts, and increase cross-citations.”
According to Professor Siepe, an Editor-inChief must possess a particular skill set. Most importantly, they must have a thorough knowledge of their specialty and be a competent surgeon, with a deep understanding of the scientific aspects and evidence-based clinical research.
He added that strong leadership skills are equally essential: “In this role, you are responsible for quite a large team. It’s not only the reviewers, Editors, Associate Editors, and Assistant Editors, but also the staff in the
EACTS publication team. While it is fun working with all of the above, this requires good communication skills, so everyone understands their role and how they contribute to the team.”
“One of my main achievements, I believe, is the way we successfully modernised both the ICVTS and the EJCTS. We were the first major cardiothoracic journals to transition from print to online-only. Our main competitors remain in print; they are considering the shift but are concerned about losing quality or impact. We also established a permanent publication team at the EACTS House in Windsor, increased the diversity of our editorial team, and created a ‘virtual editorial office’ for tasks that do not require on-site actors. These changes not only made the journals profitable, but we also achieved them while maintaining our strong reputation for high-quality scientific research and publishing standards.”
Professor Siepe explained that the most demanding part of his job is deciding which manuscripts are most relevant and backed by the strongest evidence. Handling difficult papers, appeals, and cases of malpractice are also among his greatest challenges.
“In such a small community of cardiac surgeons, disagreements inevitably arise, but I have always managed to remain friends with everyone regardless of harsh decisions.
“I really enjoy nurturing manuscripts and deciding which ones will ultimately be published. I am fortunate to work with a brilliant team, with whom I truly enjoy collaborating. As Editor-inChief, you are in a privileged position, in daily communication with the very best researchers and cardiothoracic surgeons in the world.”
For any potential authors thinking about submitting a manuscript to a journal, he offered several bits of advice:
n Research should be carefully planned from the very beginning.
n At the outset, sit down with co-authors to clarify each person’s role – this helps prevent

I consider my time working on the EACTS journals a true privilege. I learned so much in my various roles, gained networks and invaluable knowledge, and it has undoubtedly made me a better academic surgeon.”
disagreements over authorship later.
n Seek support from more experienced colleagues, such as a statistician or a native English speaker, and make use of modern tools and technologies, including AI, to improve the quality of your paper.
n Most importantly, do not overinterpret your data.
“In science, there is often a temptation to make data appear better than it really is. But this serves no one. It compromises integrity and ultimately weakens the paper. Always present the data exactly as it is – without exaggeration or fabrication. The data itself is sufficient, because it represents the truth.”
He encourages all EACTS members to become involved with the EJCTS: “Although it is hard work and time-consuming, it is incredibly
The Multimedia Manual of Cardio-Thoracic Surgery –meet the new Editor-in-Chief
Dr. Miia Lehtinen from the University of Helsinki, Finland, was recently selected as the new Editor-inChief of The Multimedia Manual of Cardio-Thoracic Surgery (MMCTS). She spoke with us about the aims and focus of the journal, the important role video tutorials play in training and her wish to increase the visibility of the MMCTS…
Dr. Lehtinen has been involved with the MMCTS since she was a Surgical Resident and soon became one of the Editors of the Core Skills Domain, which she said was influential for someone who is still in training. She explained that the MMCTS is in many ways more like a textbook than a journal, in that it focuses more on the step-by-step explanation of surgical techniques.
“The MMCTS teaches the surgical steps of each procedure, but also typically mentions ways to troubleshoot possible issues that may arise. It also focuses on case reports, so you can also find rare cases that might help you in your daily clinical work. As the MMCTS is used by both trainees and more experienced surgeons, we label each video tutorial to describe the level of a surgeon’s experience. For example, we have the Core Skills level videos, as well as advanced techniques from surgeons who are pioneering a new technique and who want to teach others.”
Submissions to the MMCTS undergo a peer review just like a regular scientific journal by teams from the Adult, Thoracic, Congenital,
Aortic and Core Skills Domains. The reviewers will try to take into consideration the originality of the technique, as well as looking at the technical quality of the surgeon and the technical quality of the tutorial video itself.
That does not mean the MMCTS only accepts videos that are new, original and have not been presented before. She said that sometimes the MMCTS struggles to get high-quality videos about very basic techniques. As a result, every year they have a competition for Residents to submit Core Skill videos so they can have a comprehensive library of all basic techniques – such as harvesting grafts for bypass surgery or implanting an aortic valve prosthesis.

“So, if someone can reproduce a high-quality video that is already in the library in a very informative way, we still consider those videos as well. Technology moves forward all the time, so some of our oldest videos can start to look a little obsolete as the quality of the definition of the video compares poorly to today’s current standards.”
It is also important to add that video tutorials should not just include the surgical steps, but also explain the thinking process before surgery, what the considerations were when deciding to choose a particular approach, etc. She added that the videos should also include post-operative outcomes.
“When people talk to me about the MMCTS they say it is reliable and credible because the tutorials undergo a rigorous peer-reviewed process, which is not something that the videos on social media can guarantee. This is particularly important for the younger
rewarding. With each review, you expand your knowledge, improve the manuscript, and advance science. By doing a lot of work for the journal and completing many reviews, you become recognised by your peers. It’s a wonderful way to build both your professional and personal network. And ultimately, it makes you a better scientist.”
Asked if he has any advice for Mario Gaudino, his successor as Editor-in-Chief, Professor Siepe responded: “He already brings so many smart ideas for the journal, and together with his publishing experience, I know he will be very successful. He has a strong editorial board and an excellent publication team around him. With these foundations and his vision, the journal will only grow stronger. He has my full support.”
Although his time as Editor-in-Chief is drawing to a close, Professor Siepe will continue to work with EACTS and its journals. At the same time, he looks forward to dedicating more time to clinical studies and trials after five years of intense commitment to the EJCTS. “I consider my time working on the EACTS journals a true privilege. I learned so much in my various roles, gained networks and invaluable knowledge, and it has undoubtedly made me a better academic surgeon.”
When people talk to me about the MMCTS they say it is reliable and credible because the tutorials undergo a rigorous peer-reviewed process, which is not something that the videos on social media can guarantee. This is particularly important for the younger generation of surgeons. I think it’s important that I have been selected for this role as someone who represents the younger generation of surgeons and who uses these videos as part of my training."
generation of surgeons. I think it’s important that I have been selected for this role as someone who represents the younger generation of surgeons and who uses these videos as part of my training.
“During my time as Editor-in-Chief, I would really like to increase the visibility of MMCTS and make sure that we cover all aspects of cardiothoracic surgery and hopefully have videos from those surgeons who have really made their name in this field. So ultimately, we have an online documentation of some of the most amazing procedures that our contemporary surgeons have developed.”
She encouraged those EACTS members who want to become involved in the MMCTS to contact the editorial team, express their interest and submit high-quality videos.
“I'm really grateful to be selected for the Editor-in-Chief role, and I am looking forward to working with the whole team of MMCTs. There are so many people working behind the scenes who do a really great job of keeping us busy surgeons on track, making sure that we meet the deadlines. It is a massive team effort.”
Introducing the new Editor-in-Chief of the EJCTS, Professor Mario Gaudino
We spoke with the new Editor-in-Chief of the European Journal of Cardio-Thoracic Surgery (EJCTS), Professor Mario Gaudino (Professor of Cardio-Thoracic Surgery, Clinical Epidemiology and Health Services Research at Weill Cornell Medicine and an attending cardiac surgeon at NewYork-Presbyterian Hospital and Weill Cornell Medical Center) about why the EJCTS is more than just a journal, overhauling the review process and ensuring journal continues to be the most prestigious CT surgery journal in the world...
“ I have been involved with the EJCTS for many years. I submitted my first manuscript to the journal in the late 1990s when Professor Marko Turina was the Editor-in-Chief. Since that time, I became a reviewer and in the last six or seven years, I was an Associate Editor for both the EJCTS and Interdisciplinary CardioVascular and Thoracic Surgery (ICVTS) journal. There is no doubt that scientific publication has always been an important part of my career and my practice. I was trained in thinking that there is no real separation between academic and clinical work, and the two things essentially go hand-in-hand. To be a good physician, you also need to be a good academician. It is an honour to be selected for the role of Editor-in-Chief.”
Professor Gaudino brings vast experience to the role as he is currently senior editor of the Annals of Thoracic Surgery, feature editor of Journal of Thoracic and Cardiovascular Surgery, and senior editor for Journal of the American College of Cardiology, among others.
“I think the most important part of my position is actually making strategic decisions about the journal, making sure that the Journal fits the needs of the cardiothoracic surgical community, and so the Journal becomes part of the day-to-day life of cardiothoracic surgeons, not only in Europe, but globally. Understanding the needs of the profession and how the Journal can adapt and react to those needs without being outdated and out of context, I think that's actually the most important part of the Editor-in-Chief’s job. As well as fulfilling a strategic function, I also have a strong group of Editors working with me to ensure we can fulfil the manuscript assessment function, and it will be a team effort. Putting together a diverse and smart team of people will actually result in better ideas and a better Journal.”
In his opinion, the EJCTS is the most prestigious of all cardiothoracic surgery journals, which has an unparalleled strategic and political influence on the cardiovascular field. He states that the strengths of the Journal are that is puts the patient first, makes sure that the science is unbiased, and there are no other interests other than the patient’s interest in driving the science.
“I come into this role with an open mind to be able to understand everybody’s perspective and listen to everybody’s views, because in the end the Journal must serve and reflect a very diverse community – from fellows and trainee surgeons to the very senior members of the profession. My ambition is for the Journal to be truly global, not only looking at Europe, but also at North America, Asia, Australia, etc. The fact that I was born in Italy, trained in Europe and currently work in the United States, reflects this global perspective.”
He added that despite focusing on a global strategy for the Journal, he and the Editorial Board need to be creative and understand that the way medical literature is published and how the role of scientific journals is evolving.
“I think there is a perception that a scientific journal should be published in the same way as it has been done for the last 50 years, that they cannot change. I think a journal should be conscious of the current reality, and it should adapt and change. For example, ten years ago, the Journal was not readily available on our phones. So, society journals must adapt to new technologies, reflect the different ways of
publishing papers and communicate with our members and our community. Communication now is different; it's quick, it's fast and there is so much information that must be condensed efficiently. Therefore, I don't think that the scientific journal should only publish science. I think it has to help our fellow CT surgeons to navigate our profession. For example, I think for young surgeons we should communicate to them how to prepare for a job interview, what to look for when they are looking for a new programme or for a place to start their career, and offer advice on how to balance their personal life, their family, motherhood, etc. There are issues that affect all of us. So, the Journal should include all the latest scientific updates, but also news updates, professional guidance and support. I would like to see the Journal become a necessity in our professional lives.”
Changes
It is not only the content and scope of the journal that Professor Gaudino wants to change, but also the reviewing process for manuscripts. He explained that in previous years, when there were not so many manuscripts submitted, the reviewing process using external reviewers worked well. However, with over 2,000+ papers submitted to the EJCTS every year, he believes that the current review process needs an overhaul and a new approach. “In the past, the Editor or the Associate Editor would invite an external reviewer to assess a manuscript and then, based on their comments, they would make a decision. This worked well when there were not thousands of papers submitted each year. In addition, there are also lots of journals, so an individual reviewer is bombarded by review requests, and there are not enough people who have enough time to do a meaningful review. As a result, they will either reject your invitation or accept your invitation but may not write a sufficient review because they do not have the time. Perhaps more importantly, external reviewers do not know what the priorities of the journal are and what direction the journal is taking.”
As a result, he believes that reviewers are often asked to assess a manuscript that, in the end, the Editor-in-Chief or the editorial group will decide is not a good fit for the Journal. Therefore, his vision is to have a very thorough in-house assessment of each manuscript by the Editors. Crucially, although he will be the Editor-in-Chief, Professor Gaudino will introduce
the new role of Editor, not Associate Editor, not Deputy Editor, but Editors. There will be a group of people working with him, and every decision on manuscripts will be collegial. At the same time, there will be an initial filter for manuscripts that reflects the priorities and direction, both strategic and scientific, of the Journal.
“With these changes, we can say very quickly if a manuscript is a good fit or not. And if it is not a good fit for the Journal, it doesn't make sense to go through the review process. This will save the reviewers’ time, and I am sure that if the reviewers get fewer invitations from us, they will be more likely to accept our invitation, and they will also be more likely to do a better job of reviewing because they have more time. In the end, this will make the author's life better and the reviewer's life better, and improve the overall quality of the Journal.”
Professor Gaudino stressed that it is important that the Journal provides balance and represents the four domains of EACTS. Of course, the Adult Cardiac Domain is larger than the Congenital Domain, and the quality of the evidence for congenital surgery is lower because of the very nature of this Domain. For example, it is very difficult to perform a randomised trial to generate high-quality evidence, which needs to be taken into consideration as the Editor-in-Chief. Nevertheless, he emphasised that each Domain would continue to be fairly represented in the Journal.
In addition, he said it is important that everybody is given the chance and opportunity to work for the Journal, and he does not believe the individual who represents the Domain within the society should also represent that Domain on the Journal. Of course, there will be exceptions, but in general, he said there should be communication and interaction, but different representations of the Domain between the Journal and EACTS.
Advice
“In my career, I have been fortunate enough to have some 1,500+ published papers, but that means that I have probably been rejected over 5,000 times – I always joke I am an expert in rejection! In my experience, I think a manuscript can be accepted for essentially two reasons: originality and excellent methodology. Firstly, you must have a really original idea, something that nobody has reported on before, that opens a new perspective or a new window or a new field. Secondly, a paper may not be necessarily novel but methodologically the best. A paper that finally proves or disproves something in the best possible methodological way. My advice to authors, and in particular young authors, is to think smart, think creatively. One of the best pieces of advice I got from my mentor in Italy was that academic work is part of my profession as a surgeon. Every day, in the ward, in the OR and in the ICU, something will happen that deserves academic study and potentially an academic publication. And if you don't see it, you are just not paying enough attention.
Thank you to the 39th EACTS Annual Meeting Social Media Ambassadors
Your efforts in highlighting the latest from Copenhagen and keeping the conversation going before, during, and beyond #EACTS2025 have been invaluable.


Therefore, you should always take inspiration from your clinical work and what you are doing. Don’t invest your time in a project that is not original; instead, try to really invest in something that increases your chances of grabbing our attention.”
In recent years, the advent of social media, open access and artificial intelligence (AI) have had both a positive and negative impact on journals. However, Professor Gaudino believes the negatives are the result of unintended consequences.
“As always with new technologies, there are good things and bad things. Technology is never good or bad; it is how it is used. Dissemination of information and education is a positive thing. I am in favour of debate and difference of opinion, even though some of the opinions may not be very well grounded in science and may be very personal, but that's okay. For a non-native English speaker, AI is a great tool. If AI can help reduce these language barriers, it is a positive. You cannot trust AI to write a manuscript, so there must be human oversight. As long as we have regulated use of AI, I do not see it as a problem, but to think that people will not use AI, is implausible.”
He also revealed that as Editor-in-Chief, he and his colleagues will be very accessible, so if an author has an idea for a manuscript, there will be a process for their ideas to be reviewed early, so they know whether the paper has a good chance of getting published or not.
“Finally, I just want to give a thank you to EACTS for selecting me and a very special thanks to my friend Matthias Siepe, the current Editor-in-Chief. He has done incredible work on the Journal, and he has been a mentor to me in the transition to this new role. I'm happy that even though he will not be the Editor-in-Chief, he will still be heavily involved in the Journal and in the leadership of the Journal. I will rely heavily on Matthias for a number of functions, and together, we will ensure our Journal continues to be the most prestigious CT surgery journal in the world. That's our goal!”

FRANCIS FONTAN FUND FELLOWSHIPS
Robotic Cardiac Surgery in Partnership with Medtronic
Sleiman Sebastian Aboul-Hassan Zbigniew Religa Heart Center “Medinet”, Nowa Sol, Poland
As a cardiac surgeon who completed the Francis Fontan Fund Robotic Cardiac Surgery Fellowship in partnership with Medtronic, I would like to thank EACTS and everyone involved in my fantastic Fellowship. Robotic-assisted cardiac surgery is transforming the field of cardiovascular interventions by offering technological precision, minimally invasive techniques, and better clinical results. This encouraged me to apply for the Francis Fontan Fund Fellowship in robotic cardiac surgery. I began my Fellowship in Leuven in March 2025, and over the next three months, I experienced some of the best moments of my career while learning robotic-assisted MIDCAB under the direct supervision of Professor Wouter Oosterlinck.
The main goal of my Fellowship was to acquire the necessary skills to start our robotic programme at our centre. From the beginning, I received
08:30

intensive simulator training, which greatly impacted my ability to develop robotic skills as a beginner. This training enabled me to pass the Basic Skills Course at Orsi after only three weeks of simulator training. The Basic Skills Course consisted of a two-day, multi-specialty course in robotic surgery, focusing on hands-on training with animal cadaver tissue. Compared to other attendees with no prior simulation experience, I performed better and completed all the tasks sooner. Having an on-site simulator was a game-changer during the course. After the course, I continued training on the simulator, attended all robotic cardiac surgery cases at UZ Leuven, participated in all robotic MIDCAB cases, and received valuable advice from Professor Oosterlinck.
Five weeks into my Fellowship, I attended an advanced robotic MIDCAB course at the Orsi Academy. One of my tasks during the course was performing robotic


LITA harvesting on cadavers and porcine models. It was one of the most memorable experiences of this fantastic Fellowship. During my Fellowship, I attended and participated in 48 robotic MIDCAB cases. Direct vision MIDCAB is a routine procedure that I perform at our centre. Therefore, starting our robotic cardiac surgery programme with a robotic-assisted MIDCAB procedure will make it easier to gain robotic experience before
expanding to other cardiac procedures. This Fellowship has certainly prepared me well for our centre's robotic programme, which will begin very soon.
I recommend the Francis Fontan Fund Robotic Cardiac Surgery Fellowship in partnership with Medtronic to all EACTS members interested in minimally invasive cardiac surgery, as robotically assisted cardiac surgery is undoubtedly the future of the field.
A Journey of Inspiration: My Experience as an EACTS Cardiac Surgery Nursing Fellow in partnership with AtriCure
Karin Hinterbuchner
Tirol Kliniken GmbH, Innsbruck, Austria
Embarking on my Fellowship was a pivotal step in my career. It has allowed me to gain first-hand insights into innovative nursing roles and practices that can shape the future of patient care in my own clinical setting. With the support of EACTS and AtriCure, this Fellowship offered me the invaluable opportunity to engage with leading institutions in the United Kingdom and Denmark, countries renowned for their advanced practice in cardiac nursing.
Fellowship Objectives and Acquired Skills
A primary goal was to explore the various advanced roles nurses play in cardiac surgery and assess their impact on patient care. In Austria, there is a lack of formal roles for Advanced Practice Nurses (APNs) and Clinical Nurse Specialists (CNSs), and such positions do not currently exist in cardiothoracic nursing. The role is largely defined by each individual institution, meaning that there is no standardised national framework and responsibilities are often shaped according to local needs and resources. At both Rigshospitalet and Odense University Hospital in Denmark I observed that CNSs are integral members of the multidisciplinary team, with typically one to two CNS nurses assigned per ward. These nurses take on a broad spectrum of responsibilities, including specialised roles such as valve disease clinical specialists, some of whom are also trained to perform ultrasounds for valve assessment, pleural effusions, and pericardial effusions. This exposure significantly enriched my understanding of the diverse scope of practice, responsibilities, and educational pathways that define advanced nursing roles in cardiac surgery.
I am currently involved in a project focused on telemonitoring-assisted care for heart failure patients prior to cardiac surgery aiming to optimise patients' preoperative condition. Therefore, my secondary objective was to investigate prehabilitation approaches for patients undergoing open-heart surgery. At Rigshospitalet, there is an initiative to start a
prehabilitation project before CABG surgery, where patients receive exercise training and education on nutrition, psychological support, and more.
Benefits of the Fellowship
In the UK, the role of the APN is well established and fully integrated within the hospital setting. At St. Thomas’ Hospital, Ana Alves serves as the Lead APN overseeing all the cardiac surgical CNSs and ANPs. Their responsibilities are wide-ranging and include patient referrals, supporting nursing staff with clinical issues, conducting ward rounds alongside physicians, and managing patients at the outpatient clinic where pre-assessments take place. They also play a vital role in patient education and conducting follow up clinics post procedure. Also, the team utilise a digital wound care platform that allows patients to upload photos of their surgical wounds from home. This technology enables nurses to remotely assess healing and intervene early, reducing the risk of infection-related readmissions.
Throughout my Fellowship, I was privileged to be guided by exceptional mentors at each host institution. Their expertise, support, and dedication were instrumental in shaping my learning journey and professional growth. These experiences underscored the significance of advanced nursing roles in enhancing patient care.
Additional Insights
During my Fellowship, I witnessed the implementation of Enhanced Recovery After Cardiac Surgery (ERACS) protocols at St. Bartholomew’s Hospital in the UK. Patients receive structured perioperative care aimed
at optimising recovery. To ensure the success of such protocols, it is essential to have a well-educated team and adequately trained staff in place.
I also observed that prehabilitation currently lacks clear, standardised structures, with approaches differing widely between institutions. Developing cohesive, evidence-based guidelines and protocols is essential to provide consistent, high-quality preparation for all patients undergoing cardiac surgery, as well as a strong multidisciplinary collaboration.
EACTS Support for Nurses and Allied Health Professionals
I see a valuable opportunity for EACTS to support ongoing skills development for nurses and allied health professionals in cardiothoracic care through further targeted training and educational courses, both online (e.g. webinars) and in-person. These initiatives would enhance clinical competence and empower nursing professionals to contribute more effectively to multidisciplinary cardiac teams, ultimately improving patient outcomes. As President-elect of the Austrian Society of Nursing in Cardiology, I have actively promoted the Fellowship to inspire colleagues both nationally and internationally.

Since returning from the Fellowship, I have initiated important discussions with senior nursing and medical staff at my hospital about implementing changes inspired by the advanced practices I observed abroad. I am currently working on introducing an APN role on our ward, clearly defining the responsibilities and clinical tasks associated with the position.
Overall, this Fellowship broadened my international perspective, fostered global nursing collaboration, and empowered me to contribute meaningfully to the development of nursing research and the professional profile of cardiac surgery nursing in Austria. I would like to sincerely thank EACTS and the programme coordinators for this incredible opportunity and their ongoing support throughout my Fellowship.
Robotic LITA harvesting during the advanced robotic MIDCAB course at the ORSI academy.
FRANCIS FONTAN FUND FELLOWSHIPS
From Riga to Maastricht: My journey in arrhythmia surgery – Francis Fontan Fund Fellowship
Reflections on the FFF Atrial Fibrillation Fellowship in partnership with AtriCure and its role in advancing atrial fibrillation surgery in Latvia
Diana Kalnina
Pauls Stradiņš Clinical University Hospital, Riga, Latvia
Iam a recently certified cardiac surgeon at Pauls Stradiņš Clinical University Hospital in Riga, Latvia. Having completed my certification in February of this year, I am now entering an important new stage in my professional career. From the very beginning of my training, I have been strongly drawn to the field of arrhythmia surgery – an area that continues to evolve and to challenge cardiac surgeons worldwide. Working in Latvia, where advanced arrhythmia surgery is gradually developing, has further inspired me to deepen my expertise and to expand treatment options for patients. This passion was the main motivation behind my application for the Francis Fontan Fund (FFF) Fellowships.
The FFF Atrial Fibrillation Fellowship in partnership with AtriCure, an initiative of the European Association for Cardio-Thoracic Surgery (EACTS), is designed to foster education, collaboration, and the exchange of expertise among young surgeons. My first exposure to the surgical treatment of atrial fibrillation came in 2018, and since then I have remained committed to advancing this field in Latvia. At Pauls Stradiņš Clinical University Hospital, concomitant surgical treatment of atrial fibrillation has been performed for several years, and preparations are currently underway to establish a dedicated programme for stand-alone arrhythmia surgery. I regarded the Fellowship as an excellent opportunity to refine my skills and to broaden my knowledge, ensuring that our future programme is grounded in the latest evidence and best
international practices.
My Fellowship was hosted at Maastricht University Medical Center+ (MUMC+) under the mentorship of Dr. Bart Maesen, whose expertise and guidance were invaluable. Over the course of four weeks, I observed a wide spectrum of atrial fibrillation cases, with particular emphasis on patient selection and perioperative management. I followed hybrid ablation procedures and spent time with electrophysiologists to better understand their diagnostic and interventional perspectives.

In addition to Maastricht, I visited University Hospital Brussels (UZ Brussel), University Hospitals Leuven (UZ Leuven), and Erasmus University Medical Center (Erasmus MC) in Rotterdam. These visits provided further exposure to arrhythmia surgery and hybrid approaches. Together, they highlighted the essential role of collaboration between surgeons and electrophysiologists and underscored the importance of a structured, multidisciplinary approach for achieving optimal outcomes in complex arrhythmia patients.
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia encountered in clinical practice and represents a growing global health challenge. Its prevalence increases with age and is associated with significant morbidity, including an elevated risk of stroke, heart failure, and reduced quality of life. For many patients, symptoms such as palpitations, fatigue, and exercise intolerance significantly affect daily life, while silent AF often remains undiagnosed until complications occur. Medical management, including anticoagulation and rate or rhythm control, remains the cornerstone of
Travelling Leadership Fellowship for Women in Cardiothoracic Surgery in partnership with AtriCure
Nora Goebel
Robert Bosch Hospital, Stuttgart, Germany
The inauguration of the Travelling Leadership Fellowship for Women in Cardiothoracic Surgery in partnership with AtriCure, marked a significant and inspiring initiative by EACTS, offering a truly unique opportunity to engage with and learn from three distinguished leaders within the European cardiothoracic community. Established by the EACTS Women in Cardiothoracic Surgery (WiCTS) Committee, this Fellowship was specifically designed to foster the development of leadership qualities among women in our field – a sphere where structured guidance and mentorship in leadership have too often been overlooked.
This pioneering programme comprises three one-week placements with eminent female leaders in cardiothoracic medicine across Europe. The objective is not merely to observe, but to immerse oneself in diverse leadership environments and reflect upon the multifaceted nature of leadership within modern healthcare. Leadership, as I came to appreciate more deeply through this Fellowship, is fundamentally different from acquiring a new surgical skill or mastering a technical procedure. It is an inward journey – one that requires self-reflection, clarity of personal values, and the ability to act with integrity and purpose in complex environments. This Fellowship provided the space and inspiration
to explore that journey in depth.
Yet the experience extended far beyond leadership alone. What made this Fellowship so profoundly enriching were the people I met –generous, open, and willing to share their knowledge, insights, and experiences. Each placement offered a wealth of new perspectives. I was impressed by the variety of approaches to patient care and departmental structure – even within the highly standardised framework of cardiothoracic surgery. I also gained a clearer understanding of how national healthcare systems, by different funding and reimbursement models, profoundly influence what kind of cardiothoracic care can be provided, and how it is delivered. These systems, I realised, directly impact not only clinical decisions but also the availability of time and resources – both of which are finite and often unequally distributed. This added a new and important dimension to my understanding of the broader context in which we work.
From a leadership perspective, I observed how different hierarchical structures shape the operation of cardiothoracic departments, often in ways very different from those in my home country. I witnessed a wide range of organisational models, team dynamics, delegation practices, and leadership styles. It was particularly enriching to experience the day-to-day lives of colleagues across Europe – geographically close, yet sometimes worlds apart in clinical culture.

therapy. However, recurrence rates are high, and many patients continue to experience symptoms despite optimal treatment. As the global burden of atrial fibrillation rises, the need for effective, durable treatment strategies becomes increasingly urgent.
Surgical treatment of atrial fibrillation has advanced considerably over recent decades. The Cox-Maze procedure, by creating a series of precise atrial lesions, has long been regarded as the gold standard, restoring sinus rhythm with high success rates. Today, less invasive approaches and novel energy sources, such as radiofrequency and cryoablation, have broadened the scope of surgical intervention. In many centres, surgical ablation is performed concomitantly with other cardiac procedures, such as valve or coronary surgery, allowing patients to benefit from rhythm control without additional operative risk. More recently, hybrid approaches that combine minimally invasive surgical ablation with catheter-based electrophysiology techniques have demonstrated promising outcomes, particularly in patients with persistent or long-standing persistent AF. These evolving strategies underline the increasingly important role of surgery alongside catheter ablation in offering durable solutions for complex arrhythmia patients.
The FFF Atrial Fibrillation Fellowship, in partnership with AtriCure, has been an invaluable experience, enabling me to acquire practical skills, observe innovative techniques, and build professional connections that will directly benefit my work in Latvia. My time in Maastricht and other leading European centres has reinforced my conviction that arrhythmia surgery requires not only technical excellence but also close integration with electrophysiology within a multidisciplinary framework.
As we move forward with establishing a dedicated programme for stand-alone surgical arrhythmia treatment at Pauls Stradiņš Clinical University Hospital, I am determined to apply this knowledge to improve access to advanced therapies and to enhance outcomes for patients living with atrial fibrillation in Latvia. I remain deeply grateful to the European Association for Cardio-Thoracic Surgery and the Francis Fontan Fund for supporting this Fellowship and for investing in the future of young surgeons.

I was privileged to spend time with three exceptional mentors, each of whom exemplifies a different facet of leadership and excellence in our field.
My journey began with Jolanda Kluin, Erasmus MC, Rotterdam, the Netherlands, head of one of the largest cardiothoracic departments in her country and the founding chair of the EACTS WiCTS Committee. Her leadership spans clinical care, departmental management, academic research, and institutional development. Despite an incredibly demanding schedule, she welcomed me warmly and offered deep insights into the realities of high-level leadership. I am sincerely grateful for the time and thought she devoted to our exchanges, both professionally and personally, and I remain deeply impressed by the high standards and efficiency of her clinic.
My second placement took me to Marta Sitges, Barcelona, Spain – a cardiologist by
training and now director of the cardiovascular institute of the University Hospital Clinic Barcelona, heading the departments of cardiology, cardiac and vascular surgery, and interventional radiology. Her career is a testament to the evolving and now inseparable collaboration between cardiology and cardiac surgery. During this stay, I was hosted in the surgical department by Eduardo Quintana, an outstanding surgeon and deeply inspiring individual. The entire team created an atmosphere that felt like family – supportive, collegial, and motivated by shared purpose. It was a vivid example of what effective leadership can cultivate: trust, cohesion, and excellence. The final week of the Fellowship brought me to Indu Deglurkar, Cardiff, Wales, UK, the originator and driving force behind this programme. Her professional path, including leadership training at Harvard, is marked by vision, empathy, and profound emotional intelligence. She embodies a style of leadership that is both highly skilled and deeply human – attentive, empowering, and generous with her knowledge. Her commitment to mentoring the next generation of female leaders was evident in every moment, and I learned an extraordinary amount from her example.
In conclusion, the FFF Travelling Leadership Fellowship for Women in Cardiothoracic Surgery, in partnership with AtriCure, is a powerful opportunity to broaden horizons and develop in this often-overlooked area of professional growth – particularly for women. I extend my heartfelt thanks to the EACTS and to my hosts Indu Deglurkar, Jolanda Kluin, and Marta Sitges. A special thank you to Indu Deglurkar, the mastermind of this initiative –thank you for making this possible!
Nora Goebel with Indu Deglurkar
FRANCIS FONTAN FUND FELLOWSHIPS
Francis Fontan Fund: Robotic Thoracic Surgery Fellowship in partnership with Intuitive
Kristiina Pälve
Turku University Hospital, Turku, Finland
Why did I apply to the Francis Fontan Fund (FFF) Robotic Thoracic Surgery Fellowship in partnership with Intuitive? I am a cardiothoracic surgeon working in Turku University Hospital in Finland. Finland’s population is approximately 5.6 million, and Turku is the third most populated urban area in the country. Our hospital’s catchment area is approximately 490,000 people. There are five university hospitals in Finland, and ours is the third largest. Our hospital is a primary care hospital. However, we are quite a low-volume hospital compared to European centres. I have been working as a consultant since September 2018, but our robotic programme is fairly new. My colleague and I started the programme in December 2022 after our operating theatre acquired Intuitive’s da Vinci Xi robot. I completed TR200 training with Dr. Rune Eggum in Oslo, Norway, in 2022. Before starting RATS procedures, I had performed approximately 70 lobectomies, mainly with VATS and approximately 200 smaller thoracic procedures.
08:30 – 09:30 Focus Session Room 180/181
We have the opportunity to use the Da Vinci Xi Robotic Surgical System every Thursday in our theatre, and occasionally we get extra days. Between December 2022 and April 2024, we had performed 57 RATS procedures, so I had a little bit of experience in robotic thoracic surgery before applying for the FFF. The Fellowship included two three-week stays in high-volume robotic centres. I chose to visit Dr. Marion Durand in Groupe Hospitalier Privé Ambroise Paré Hartmann in Paris and Mr. Steven Stamenkovic in St Bartholomew's Hospital in London. I also got the opportunity to see the work of Dr. Agathe Seguin-Givelet, Mr. Kelvin Lau and Mr. Federico Femia.
I have learned a lot during this Fellowship. The instructors have been incredibly welcoming and given me the opportunity to see them operate, discuss with the patients and really make me feel included. During my visits, I have had the opportunity get myself familiar with new technology like 3D modelling and Ion robotic bronchoscopy. I have been shown how to better utilise the robotic instruments I already have at home. I have got ideas to really improve my surgical skills.
Both centres offered a unique perspective on
A Transformative Journey: My Francis Fontan Fund VATS Fellowship at Odense University Hospital
Tay Yen
Hospital Kuala Lumpur, Malaysia.
As a thoracic fellow from Malaysia, I have always been committed to advancing my skills and contributing to the evolution of thoracic surgery in my home country. It was with immense gratitude and anticipation that I embarked on a six-week Francis Fontan Fund VATS Fellowship at the esteemed Odense University Hospital in Denmark. This incredible opportunity, generously supported by the Francis Fontan Fund, was designed to immerse me in the intricacies of multiportal and uniportal VATS within general thoracic surgery, with a strong emphasis on hands-on experience and a stepwise training process. My ultimate goal: to safely perform VATS lobectomy for patients undergoing resection for early-stage lung cancer and to deepen my expertise in all aspects of minimal invasive thoracic surgery.
From the moment I arrived at Odense, I was struck by the dynamic and collaborative environment. The department’s commitment to education was immediately apparent, beginning with daily morning departmental sessions where the entire surgical staff meticulously discussed surgical patients, followed by a radio-imaging meeting before heading for the comprehensive rounds. This routine provided an invaluable framework for understanding patient pathways, surgical planning, and post-operative care, all within a multidisciplinary context. The team at OUH was incredibly welcoming and accommodating, consistently adapting when needed, ensuring a seamless and enriching learning experience. Under the expert mentorship of Professor Peter Licht, a luminary in the field, my training progressed systematically. The Fellowship offered an unparalleled opportunity for direct involvement, allowing me to engage deeply with various aspects of patient



patient selection, operative planning, and postoperative management, and I was able to observe a wide range of complex cases. The exposure to different team dynamics and surgical techniques broadened my understanding of the versatility and precision that robotic surgery can offer. Witnessing how seamlessly these experienced surgical teams integrated cuttingedge technology into daily practice was inspiring and reinforced my desire to further develop our own programme in Finland.
Beyond the operating theatre, I participated in case discussions, multidisciplinary meetings, and teaching sessions, which deepened my appreciation for the collaborative spirit driving

management with a special focus on minimally invasive techniques. From day one, I was right into the operating theatre, getting gowned up and assisting in VATS S6 segmentectomy. I observed and participated in numerous multiportal VATS procedures, gaining critical insights into their nuanced application in general thoracic surgery. While my primary focus was on achieving proficiency in VATS lobectomy for early-stage lung cancer, the breadth of cases exposed me to a wide array of complicated thoracic conditions, further solidifying my understanding and technical acumen. The stepwise training approach truly built my confidence, translating theoretical knowledge into practical, safe surgical skills. Moreover, I was impressed with
innovation in thoracic surgery. The open exchange of ideas and readiness to share knowledge among surgeons from different backgrounds underscored the importance of lifelong learning in our field.
I feel incredibly privileged to have been able to see the big names in thoracic surgery and discuss their work with them. I could not recommend applying for the FFF Robotic Thoracic Surgery Fellowship in partnership with Intuitive enough. It has made a big impact on my personal career and, of course, has highly benefited my patients in Turku University Hospital.
the enhanced recovery protocols after lobectomy, particularly in patients aged eighty years and above, which signifies an important change in perioperative management, and highlights a multifaceted strategy to improve patient recovery.
Odense University Hospital distinguishes itself not only through its clinical excellence but also through its integral connection with the University of Southern Denmark. Research, development, and education are not mere adjuncts but inseparable aspects of OUH’s core function as a leading university hospital. This philosophy permeated my Fellowship experience; I witnessed firsthand how new research ideas from the local fellows, findings were seamlessly integrated into clinical practice, driving innovation and improving patient outcomes. The hospital's dedication to educating highly skilled healthcare professionals and generating research that streamlines and enhances future care pathways is truly inspiring. This holistic approach to healthcare, where cutting-edge research informs daily practice, provided a unique perspective that I am eager to bring back to Malaysia.
The impact of this Fellowship on my professional journey is profound and far-reaching. Upon my return, I will be based in Sarawak, Borneo, Malaysia, as a general thoracic surgeon, with the ambitious goal of establishing a dedicated thoracic unit at Sarawak General Hospital. The comprehensive experience gained at OUH – encompassing advanced surgical techniques, meticulous patient management, and a deeper appreciation for the interplay of research and clinical practice – will be instrumental in achieving this vision. This Fellowship has not just honed my surgical skills; it has broadened my understanding of the entire spectrum of lung cancer care and other complex mediastinal and oesophageal cases, equipping me with the knowledge and confidence to lead and develop a robust thoracic service. I am now better prepared to navigate challenges, implement best practices, and ultimately contribute to improving patient care in a region where specialised thoracic services are critically needed.
My six weeks at Odense University Hospital, facilitated by the Francis Fontan Fund VATS Fellowship, have been nothing short of transformative. It has been a privilege to learn from Professor Licht and the entire OUH team, and I am incredibly grateful for the invaluable lessons and experiences that will undoubtedly shape my career. This Fellowship represents a pivotal step in my commitment to advancing thoracic surgery, and I look forward to applying this knowledge to make a tangible difference in the lives of patients in Sarawak.
EACTS 2025 trial update session
11:15-12:45 Plenary Hall A1
Fame-3 at five years: Implications for PCI and CABG strategy: Where are we heading in revascularization?
The Fame-3 trial is a multicentre randomised trial comparing FFR-guided PCI versus CABG in patients with triple vessel coronary artery disease but not involving the left main coronary artery (n=1500, PCI=757, CABG=743). The study was performed in 48 hospitals throughout Europe, the USA, Canada, Australia and Asia1
At one year, the prespecified threshold for non-inferiority of PCI versus CABG regarding the outcome for death, stroke, myocardial infarction and repeat revascularization was not met (HR 1.5 with 95% CI 1.1 – 2.2; p=0.35 for non-inferiority). In other words, CABG performed better than PCI at one year At three years, the repeat revascularization outcome was banned from the combined endpoint, which remained for death, stroke and myocardial infarction2. The statistical endpoint was met. In other words, at three years, PCI proved statistically to be non-inferior to CABG with regard to the combined endpoint of death, stroke and myocardial infarction. However, this result was at the real statistical edge (HR 1.3 with 95% CI 0.98 – 1.83 with p=0.07). If the lower CI limit had been 1.0 instead of 0.98, the endpoint would not have been met, and the result would therefore have been in favour of CABG. Moreover, there was no difference in death or stroke considered as separate



Filip Casselman Heart Center AZORG, Aalst, Belgium
10:00-11:00 Focus Session Auditorium 10
Navigating the MAZE in different concomitant AF ablation strategies
At this year’s EACTS meeting in Copenhagen, my talk will make a simple but important case: one size does not fit all for concomitant atrial fibrillation (AF) ablation. Cox Maze IV remains the benchmark operation, yet recommending it universally – irrespective of AF type, atrial substrate, concomitant procedure, or team experience – can create early headwinds: iatrogenic flutters, higher pacemaker rates, and a dip in confidence that risks stalling programme growth, especially for young surgeons and low-volume centres. The better path in this scenario is tailoring: match the lesion set to the patient, the surgery, and the capabilities of your institution.
Why ablate – and what else to do
Concomitant ablation during cardiac surgery improves rhythm outcomes and is recommended in contemporary European guidelines for appropriate candidates. Left atrial appendage (LAA) occlusion has also moved to an IB indication, reflecting accumulating evidence that it reduces thromboembolic events on top of anticoagulation. The practical takeaway is straightforward: if you are operating on a patient with AF and rhythm control is a goal, plan an ablation strategy and address the LAA. If not, exclude the LAA.
Not everyone needs a full Cox Maze IV
Several trials and large series remind us that “more lines” do not automatically translate into “more sinus rhythm,” particularly in paroxysmal AF and when the left atrium will not otherwise be opened. In those scenarios –common in AVR or CABG
– a carefully executed pulmonary-vein isolation (PVI) can achieve clinically meaningful freedom from AF with less operative complexity and shorter ischemic times. For centres building experience, starting with durable PVI (and adding lines as the substrate and learning curve demand) is often the most pragmatic, reproducible step.
When to escalate
Patients with persistent or long-standing AF, markedly enlarged or fibrotic atria, or those undergoing mitral surgery usually benefit from a more complete left-atrial lesion set. Here, the goal extends beyond eliminating triggers to interrupting maintenance circuits – roof and floor lines, a robust mitral isthmus, and thoughtful LAA management. If you are already opening the left atrium, the incremental effort of a comprehensive left-atrial set is generally justified by the substrate.

Be cautious with biatrial lines
There is some controversy regarding the effectiveness of adding right-atrial lesions when a complete left-atrial set is in place, but they can increase morbidity and pacemaker implantation. Reserve bi-atrial strategies for selected anatomies, concomitant tricuspid surgery and for teams with the experience to deliver consistently gap-free lines. Early in a program, prioritise quality over quantity: fewer, well-validated lesions outperform ambitious but incomplete patterns.
Mind the flutters – and the pacemakers
Atypical atrial flutters after surgery are frequently the by-product of incomplete linear lesions, especially across the mitral isthmus or posterior wall. Meticulous technique and energy-source familiarity are the best prophylaxis. Similarly, any ablation strategy carries some risk of pacemaker implantation. This is another argument for tailoring: deploy complexity where the substrate demands it, not by default.
Nursing and allied health professionals in cardiothoracic surgery
10:00-11:00 Focus Session Room 18&19.
Navigating the MAZE –the other side
Atrial fibrillation (AF) is the most common arrhythmia worldwide. It can occur silently or manifest with burdensome signs that significantly impair patients’ quality of life. Many patients attribute their discomfort directly to the presence of AF, which makes it crucial for healthcare professionals to offer evidencebased treatment solutions. Among the different therapeutic options, the surgical MAZE procedure has become a well-established technique, demonstrating highly satisfactory outcomes in terms of rhythm control and long-term maintenance of sinus rhythm.
However, not all patients experience symptoms, and those who live with AF in a largely asymptomatic form often need clear and persuasive arguments to understand the importance of undergoing a MAZE procedure. Beyond the surgical technique itself, the long-term success of AF management depends heavily on the integration of comprehensive patient education and support. One of the fundamental pillars for improving the results of the MAZE technique lies in ensuring that patients receive accurate, accessible, and individualised information.
As a nurse specialising in the care of patients with AF, my role is to guarantee that each patient arrives on the day of surgery with an optimal understanding of what to expect, full confidence in the surgical team, and a clear vision of the journey towards long-term
arrhythmia freedom. At our centre, every patient scheduled for an AF ablation procedure undergoes a structured preoperative nursing assessment. During this consultation, we explain the nature of the intervention, clarify potential doubts, and establish realistic expectations regarding the postoperative period.
Patients are informed about how to prepare for admission, what to expect during their hospital stay, and the discharge process. Health education is delivered through structured interviews, open-ended questions, and “teach-back” techniques to ensure patients fully understand the information provided. Importantly, we maintain open communication channels via telephone and email, so that patients can reach the nursing team for any concerns before or after the intervention.
Fifteen days after surgery, patients are invited for an early postoperative nursing evaluation. During this visit, we review wound healing, vascular access sites, and cardiac rhythm status. We also carry out a systematic assessment of cardiovascular risk factors, referring patients to the appropriate
Minimally invasive
Tailoring also means choosing the approach and being imaginative. Advanced lesion sets can be achieved during minimally invasive mitral surgery. Even in patients undergoing MIDCAB, thoracoscopic ablation offers a credible concomitant solution without sternotomy. In more advanced substrates, hybrid programmes that combine surgical durability with endocardial mapping and touch-up can improve outcomes while keeping procedures modular and scalable across different teams.
How I decide – an algorithm you can use tomorrow
1. Define the AF (paroxysmal vs non-paroxysmal) and appraise atrial size, type and duration of AFib.
2. Index operation matters: if no left atriotomy is planned (typical AVR/CABG), default to PVI for paroxysmal AF; if opening the left atrium (mitral work), escalate to a complete left-atrial set. If tricuspid surgery is needed, go for a Cox Maze IV.
3. Escalate for substrate: persistent AF, large LA, or prior failures push toward extended left-atrial lesions; add right-atrial work only selectively.
4. Always consider LAA occlusion as an adjunct to guidelinedirected anticoagulation.
5. Be honest with patients and cardiologists about early atrial tachyarrhythmias, the possibility of pacemaker implantation, and the usual trajectory to long-term success.
6. Grow deliberately: start with what your team can perform reliably; add complexity as outcomes and confidence mature.
We should continue to celebrate Cox Maze IV as the gold standard when it is the right operation. But the field will serve more patients, more safely, if we also champion practical, personalised lesion sets that fit the substrate, the surgery, and the centre. That is how we turn guidelines into everyday wins –sustained sinus rhythm, fewer complications, and a successful AF programme.
specialists according to their needs. Lifestyle advice, secondary prevention, and guidance on living with AF following ablation form an integral part of this consultation. In addition, we dedicate time to promoting therapeutic adherence. Patients receive clear explanations regarding their prescribed medication, particularly anticoagulants, including reasons for treatment, potential risks, and safe administration.

Instructions on “pill-in-the-pocket medication” are also given, ensuring that patients know how and when to use it appropriately. This close follow-up does not end at the early postoperative stage. The nursing team continues to monitor each patient for one full year after the intervention, with structured reviews designed to optimise recovery, support risk factor management, and promote healthy lifestyle behaviours.
Recent randomised studies have highlighted the impact of nurse-led structured education and follow-up programmes in AF management.
The results consistently show that patients who receive comprehensive education and a clearly defined follow-up plan demonstrate fewer arrhythmia recurrences and reduced emergency department visits compared to those receiving standard care.
Managing cardiovascular risk factors, alongside providing patients with structured access to the care team during the first year after ablation, is a cornerstone of improved long-term outcomes. This combined approach not only supports rapid identification and management of complications or recurrences but also promotes secondary prevention, reduces anxiety, and strengthens the therapeutic alliance between patients and their healthcare providers. The MAZE procedure itself is only one component of a broader, multidisciplinary strategy for managing AF. True success relies not only on surgical excellence but also on engaging patients actively in their care, empowering them to participate in decision-making, and ensuring they receive consistent, coordinated support across the continuum of care.
Cardiac nursing has already made significant strides in the field of AF management, particularly in patients undergoing catheter ablation. However, there remains a largely unexplored opportunity for cardiac surgery nursing teams to take a leading role in the perioperative care of patients undergoing the MAZE procedure. By building on the strong foundation established in cardiology nursing, surgical nursing can contribute substantially to patient education, postoperative care, and long-term outcomes. The future of AF management must therefore be collaborative, patient-centred, and multidisciplinary. By combining surgical expertise with the unique strengths of nursing in education, support, and follow-up, we can ensure that patients undergoing a MAZE procedure are not only treated effectively but also empowered to live healthier and more confident lives.
Manuel Carnero Alcázar Clinico San Carlos Hospital, Madrid, Spain
Alba Cano Valls
Hospital Clínic Barcelona, Barcelona, Spain
EUROPEAN BOARD OF CARDIOTHORACIC SURGERY

CVCC Level 1 & 2 Examination – Updated Regulations! Easier than ever to apply, view our updated regulations. The Critical Care Certification is for surgeons who are recognised as leaders of multidisciplinary, high performing teams.
MEBCTS Level 1 Examination
The Membership of the European Board of Cardiothoracic Surgery (MEBCTS) is for surgeons at the end of national training who are ready to work independently.
FEBCTS Level 2 Examination
The Fellowship of the European Board of Cardiothoracic Surgery (FEBCTS) is for surgeons who are already practicing independently. Visit our website ebcts.org for more information
Acquired Cardiac Disease Domain
Long-Term Mechanical Circulatory Support: Who Benefits? Insights from Current Guidelines
Heart failure is a major health concern, characterised by significant morbidity and mortality. It currently affects more than 64 million people worldwide. Despite several advancements in medical management, several patients evolve to end-stage heart failure and need advanced therapies.
The gold-standard treatment for end-stage heart failure is a heart transplant, which currently reaches a median survival of more than 10 years. However, the paucity of organs and some comorbidities leave a significant number of patients with very few options. Mechanical circulatory support was initially developed to bridge
Elena Sandoval
University Hospital Clinic of Barcelona, Barcelona, Spain. Heart Failure Task Force Member 2022-2025
patients to recover after cardiac surgery and to bridge patients to transplant. Since the initial devices, such as the XVE (Thoratec Corporation, Pleasanton, CA, USA) or the Novacor (WorldHeart, Oakland, CA, USA), several devices have been developed and implanted. Initial devices provided pulsatile flow, whereas newer generations are continuous-flow (CF) devices. Initial implants were mostly as a bridge to transplant (BTT) strategy. However, changes in allocation systems and ageing of population has led to a significant rise in destination therapy (DT) implants.

Currently, the HeartMate 3 (Abbott, North Chicago, IL,
Next-generation devices for long-term MCS: Advances in LVAD, BiVAD and total artificial heart
While heart transplantation remains the gold standard for advanced heart failure, the persistent shortage of donor organs has spurred rapid innovation in durable devices. Left ventricular assist devices (LVADs), biventricular assist devices (BiVADs), and total artificial hearts (TAHs) now represent essential components of the therapeutic arsenal.
HeartMate 3: Benchmark of Durable LVADs
The HeartMate 3 is, up to date, the only commercially available LVAD in Europe. It has set a new standard in hemocompatibility: the fully magnetically levitated, centrifugal flow pump has demonstrated a significant reduction in pump thrombosis, stroke, and hemolysis compared with earlier generations. Long-term results from the MOMENTUM-3 trial showed two- and five-year survival free from disabling stroke or reoperation comparable to outcomes of heart transplantation1,2 Importantly, HM3 can also be configured in a BiVAD setup if needed.
CorHeart 6 and BrioVAD: Toward Smaller Pumps and optimised human interface
The CorHeart 6 LVAS (Shenzhen Core Medical Technology Co., Ltd) and the BrioVAD (BrioHealth Solutions), both developed in China, represent an innovation in the field of compact continuous-flow magnetically levitated LVADs. The small profile makes it particularly attractive for minimally invasive approaches as well as for patients
with smaller BSAs. Both devices are currently in early clinical feasibility studies in Europe and the US and, if successful, may expand LVAD implantation to be feasible in smaller patients and further improve patients’ outcomes3,4
CorWave: A Novel WaveMembrane Pump
CorWave, a French start-up, has developed a disruptive LVAD concept based on a biomimetic undulating membrane technology rather than rotary impellers. This design aims to reproduce the natural pulsatility of the human heart, potentially improving vascular physiology and reducing adverse events such as acquired von Willebrand disease or right ventricular dysfunction. Early preclinical testing has demonstrated improved hemocompatibility and physiologic flow patterns. First-in-human implantation has been performed in Australia in May 2025, and if safety and durability are confirmed, CorWave may represent the first true paradigm shift in LVAD technology since the move from pulsatile to continuous flow pumps.
FineHeart FlowMaker: A fully implantable system
Unlike conventional centrifugal pumps, the FlowMaker (FineHeart, France) rather works as a flow accelerator that is synchronised to the native cardiac
USA) is the only available device, having shown excellent results after five years1 (MOMENTUM3). New devices are under ongoing clinical trials, such as the BrioVAD2 , another CF device of smaller size.
Despite the excellent results of left ventricular assist devices, some patients are not candidates as they have biventricular failure, restrictive cardiomyopathies or congenital heart disease. Biventricular support has also evolved from the initial Jarvik 7, currently Syncardia (SynCardia systems LLC, Tucson, AZ, USA), to the Aeson TAH (CARMAT SA, Vélizy, France) the first bioprosthetic total artificial heart, or the newly FDA approved BIVACOR (BiVACOR, Inc, Huntington Beach, CA). Furthermore, new devices, such as reBEAT (AdjuCor GmbH) or FlowMaker (FineHEART, Pessac, France) or providing uni or biventricular support have been developed and have undergone their first-in-human implants and clinical trials.
This presentation will dive into the different published guidelines3,4,5 and will try to present an overview of the spectrum of patients who may benefit from such therapies, from isolated left heart failure to biventricular failure of
cycle by means of an epicardial lead. It is implanted via a mini-thoracotomy without cardiopulmonary bypass and works with transcutaneous energy transfer. Early animal studies indicate excellent hemodynamics, stable hemocompatibility, and improved response to physiologic demands. An early feasibility study has started in Europe.
BiVACOR Total Artificial Heart: Redefining Biventricular Replacement For patients with biventricular failure, TAHs are often the only option beyond transplantation. The BiVACOR TAH (BiVACOR Inc.) is a compact, continuous-flow, electrically powered total artificial heart that employs two centrifugal impellers mounted on a single magnetically levitated rotor. The design incorporates wide flow gaps to enhance hemocompatibility and features an automatic left–right balancing mechanism that dynamically adjusts to changing physiological demands. In vitro, favourable hemocompatibility characteristics could be shown, even under minimal anticoagulation5. In 2024, the first human recipient of the BiVACOR TAH was successfully bridged to transplant – a landmark event for the . If long-term outcomes confirm early success, BiVACOR could emerge as the first widely adopted durable TAH.
The Holland Hybrid Heart: Toward a Fully Implantable Artificial Heart
different etiologies, without forgetting the possibility of recovery.
References:
1. Mehra MR, Goldstein DJ, Cleveland JC, Cowger JA, Hall S, Salerno CT, Naka Y, Horstmanshof D, Chuang J, Wang A, Uriel N. Five-Year Outcomes in Patients With Fully Magnetically Levitated vs Axial-Flow Left Ventricular Assist Devices in the MOMENTUM 3 Randomized Trial. JAMA. 2022 Sep 27;328(12):1233-1242.
2. Pagani FD, Cowger JA, Jorde UP, Salerno C, Naka Y, Bhat G, Milano C, Druker V, Long JW; INNOVATE Clinical Trial Investigators. Design and rationale for the clinical investigation of a novel, magnetically levitated left ventricular assist device for the treatment of refractory heart failure. J Heart Lung Transplant. 2025 Aug;44(8):1290-1299.
3. Potapov EV, Antonides C, Crespo-Leiro MG, Combes A, Färber G, Hannan MM, Kukucka M, de Jonge N, Loforte A, Lund LH, Mohacsi P, Morshuis M, Netuka I, Özbaran M, Pappalardo F, Scandroglio AM, Schweiger M, Tsui S, Zimpfer D, Gustafsson F. 2019 EACTS Expert Consensus on long-term mechanical circulatory support. Eur J CardioThorac Surg 2019; 56 (2): 230-270.
4. Saeed D, Feldman D, Banayosy AE, Birks E, Blume E, Cowger J et al. The 2023 International Society for Heart and Lung Transplantation Guidelines for Mechanical Circulatory Support: A 10-year update. J Heart Lung Transplant 2023; 42 (7): e1-e222.
5. Kirklin JK, Pagani FD, Goldstein DJ, John R, Rogers JG, Atluri P et al. American Association for Thoracic Surgery/ International Society for Heart and Lung Transplantation guidelines on selected topics in mechanical circulatory support. J Thorac Cardiovasc Surg. 2020 Mar;159(3):865-896
The Holland Hybrid Heart is a novel total artificial heart combining soft robotics and tissue-engineered materials to mimic natural cardiac contraction. A pneumatically driven actuator functions as a septum between ventricles, generating gentle pulsatile motion. Preclinical studies show pumping up to ~5.7 L/min with dynamic adaptation to physiological demand (7). Currently in preclinical development, the device holds promise for patients with severe biventricular heart failure, offering potential reductions in long-term complications compared to conventional continuous-flow TAHs. Key challenges that are addressed with novel technologies
n Hemocompatibility: Gastrointestinal bleeding and thromboembolic events remain considerable complications. Biomimetic and magnetically levitated designs aim to mitigate these.
Conclusion
The landscape of mechanical circulatory support is more dynamic than ever. The HeartMate 3 has established durable LVAD therapy as a mainstream option, while novel concepts such as the CorWave and FlowMaker promise to enhance physiologic compatibility, and Corheart 6 and BrioVad could become viable options for smaller patients. For patients with biventricular failure, the BiVACOR TAH has entered clinical practice and finally, the Holland Hybrid Heart represents a European vision of a fully implantable, next-generation artificial heart. Together, these innovations move the field closer to the ultimate goal: safe, durable, and life-enhancing mechanical hearts available to all patients in need.
References
1. Mehra MR, Goldstein DJ, Cleveland JC, Cowger JA, Hall S, Salerno CT, et al. Five-Year Outcomes in Patients With Fully Magnetically Levitated vs Axial-Flow Left Ventricular Assist Devices in the MOMENTUM 3 Randomized Trial. Jama. 2022;328(12):1233-42.
Julia Riebandt
Medical University of Vienna, Austria

n Infection prevention: Percutaneous drivelines remain a weak point; fully implantable systems with wireless power transfer (e.g., FlowMaker, Holland Hybrid Heart) could overcome this.
n Size and Fit: available TAHs remain too large for many patients; virtual implantation and 3D modelling are essential tools for patient selection. BiVACOR is the first device that also fits smaller patients.
n Durability and low maintenance: Simple mechanics, as in the BiVACOR, are essential for good long-term results.
n Smart pumps: AI integration and flow responsiveness to physiological demands (e.g., FlowMaker) can enhance patients’ quality of life.
2. Mehra MR, Uriel N, Naka Y, Cleveland JC, Jr., Yuzefpolskaya M, Salerno CT, et al. A Fully Magnetically Levitated Left Ventricular Assist Device – Final Report. N Engl J Med. 2019;380(17):1618-27.
3. Qiu Z, Song X, Shi H, Zhang X, Chen W, Wu Y, et al. Safety and Efficacy of the Corheart 6 Left Ventricular Assist System. Asaio j. 2025.
4. Pagani FD, Cowger JA, Jorde UP, Salerno C, Naka Y, Bhat G, et al. Design and rationale for the clinical investigation of a novel, magnetically levitated left ventricular assist device for the treatment of refractory heart failure. J Heart Lung Transplant. 2025;44(8):1290-9.
5. McNamee AP, Timms D, Nestler F, Bartnikowski N, Smith A, Tansley GD, et al. In Vitro Hemocompatibility of the BiVACOR Total Artificial Heart in Continuous and Pulsatile Flow. Artif Organs. 2025.
6. Shah AM. First successful implant of BiVACOR's Total Artificial Heart. Artif Organs. 2024;48(10):1075-6.
7. Arfaee M, Vis A, Bartels PAA, van Laake LC, Lorenzon L, Ibrahim DM, et al. A soft robotic total artificial hybrid heart. Nat Commun. 2025;16(1):5146.
The project
Sweating is a natural physiological mechanism essential for thermoregulation. However, when it becomes excessive, it can significantly impact patients both physically and psychologically. Hyperhidrosis, defined as abnormally increased sweating, affects approximately 1–3% of the population and is often associated with social embarrassment, physical discomfort, and a marked reduction in quality of life. Its impact can surpass that of other dermatologic conditions such as atopic eczema, acne, psoriasis, and rosacea. Several treatment options have been developed, ranging from non-invasive therapies – such as topical aluminum salt applications, antimuscarinic agents, iontophoresis, and botulinum toxin type A injections – to more invasive surgical interventions1
Surgical management of hyperhidrosis dates back nearly a century. The first clinical sympathectomy was performed by Alexander in 1889, initially intended as a treatment for epilepsy2. Over time, sympathectomy was explored for a variety of indications, including idiocy, exophthalmic goiter, glaucoma, angina pectoris, Raynaud’s disease, and Sudeck’s atrophy3. In 1919, Kotzareff

The preliminary results
Today, there are still two major shortcomings in the medical and surgical management of hyperhidrosis. The first is the widespread lack of awareness among general practitioners about the condition itself and, consequently, among the specialists responsible for its treatment. This issue was clearly highlighted by Lee in 20221. In their study, the authors showed that neither primary care physicians nor the general public recognise the role of thoracic surgeons in treating primary focal hyperhidrosis.
The second major issue is the absence of updated guidelines. In my opinion, this gap is particularly evident in the field of surgical treatment. Knowledge about postoperative complications, potential side effects, and relapse management remains especially limited. The most recent consensus paper was published by Cerfolio in 20112. While it remains a useful reference for those approaching the disease for the first time, it has several limitations. The document is clearly outdated, does not reflect recent surgical advancements, and the methodology used for the literature review lacks transparency. Most importantly, it fails to thoroughly address complications, side effects, and the management of relapses.
Based on this evidence, ESTS decided to survey its members to obtain a snapshot of the current situation and understand whether its surgeons act in a homogeneous way3. We found that current practice in sympathetic surgery among ESTS responders aligns with the available evidence, although it shows
pioneered the use of sympathectomy for hyperhidrosis, demonstrating its effectiveness in 1920 for unilateral facial sweating4. Subsequently, in 1935, Adson reported favourable outcomes for palmar hyperhidrosis following cervical sympathectomy4. Initially conducted via open thoracotomy, surgical sympathectomy was associated with significant morbidity, limiting its adoption. In 1951, Kux introduced an endoscopic approach targeting the sympathetic chain to treat conditions like duodenal ulcers, angina, hypertension, and . However, it was not until 1975 that the first series of thoracoscopic sympathectomies for upper limb hyperhidrosis appeared in the German literature6. With the advent of videoassisted thoracoscopic surgery (VATS) in the 1990s, the procedure gained popularity.
Since then, various refinements have been made to the technique, including resection, transection, electrocautery, and clipping of the sympathetic chain7. Endoscopic thoracic sympathectomy (ETS) is typically reserved for patients with severe, refractory hyperhidrosis, particularly affecting the upper extremities. While often effective, the procedure carries the risk of compensatory hyperhidrosis – excessive sweating in other body regions – which can be more debilitating than the initial condition. The outcome of ETS depends not only on surgical technique but also on individual patient factors, such as preoperative expectations, environmental conditions, occupational demands, psychological status, and postoperative adaptation. The optimal level of sympathetic chain interruption remains debated, as it must be tailored to the
significant heterogeneity in almost all aspects.
These considerations highlight the urgent need for shared guidelines or at least a stronger, updated consensus. In 2024, the EACTS Guidelines Committee formed a dedicated expert group, joining forces with ESTS to broaden participation. Both societies appointed a working group of experienced members, selected based on clinical expertise and scientific publications. The EACTS group included five surgeons and F. Petrella as co-chair; the ESTS group included seven surgeons and F. Raveglia as co-chair. To ensure scientific rigor, a methodologist (Luca Bertolaccini) and a librarian (Christa Niehot) were also involved in the drafting process.
The two co-chairs and the methodologist agreed to follow the 2024 Milan Milojevic document4, which outlines a comprehensive process for developing multidisciplinary CPGs. According to this document, we have completed the “initiation phase.”
Groups formed in early 2025, with the kickoff meeting taking place on 13 March after obtaining COIs. Due to the lack of RCTs in hyperhidrosis research, we opted to develop an expert consensus document based on strong observational data rather than guidelines. The initiation phase has ended, and we are now in the

anatomical distribution of symptoms. A standardised anatomical classification, supported by expert consensus and literature review, offers a structured framework for selecting the most appropriate surgical strategy8
The EACTS/ESTS Expert Consensus Statements aim to provide comprehensive, up-to-date recommendations for surgeons involved in the management of hyperhidrosis. This expert consensus reflects the collective expertise of leading thoracic surgeons from the EACTS and ESTS. Adoption of this standardised approach to ETS, along with consistent pre- and post-operative evaluation of symptoms and quality of life, is essential for transforming expert consensus into evidencebased clinical practice.
References
1. Lee KY, Levell NJ. Turning the tide: a history and review of hyperhidrosis treatment. JRSM Open. 2014 Jan 7;5(1):2042533313505511. doi: 10.1177/2042533313505511
2. Hashmonai M, Kopelman D. History of sympathetic surgery. Clin Auton Res. 2003 Dec;13 Suppl 1:I6-9. doi: 10.1007/s10286-003-1103-5.
3. Parikh D. Pediatric Thoracic Surgery. London: Springer, 2009.
4. Greenhalgh RM, Rosengarten DS and Martin P. Role of sympathectomy for hyperhidrosis. Br Med J 1971; 1:332–334.
5. Kux E. The endoscopic approach to the vegetative nervous system and its therapeutic possibilities; especially in duodenal ulcer, angina pectoris, hypertension and diabetes. Dis Chest 1951; 20: 139–147.
6. Fritsch A, Kokoschka R and Mach K. [Results of thoracoscopic sympathectomy in hyperhidrosis of the upper extremities (author’s transl)]. Wiener klinische Wochenschrift 1975; 87: 548–550.
7. Deng B, Tan QY, Jiang YG, et al. Optimization of sympathectomy to treat palmar hyperhidrosis: the systematic review and meta-analysis of studies published during the past decade. Surg Endosc 2011; 25:1893–1901.
8. Cerfolio RJ, De Campos JR, Bryant AS, Connery CP, Miller DL, DeCamp MM, McKenna RJ, Krasna MJ. The Society of Thoracic Surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann Thorac Surg. 2011 May;91(5):1642-8. doi: 10.1016/j.athoracsur.2011.01.105.
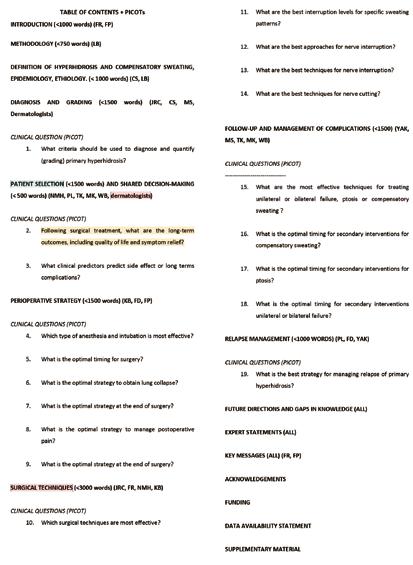
Figures 1 and 2 combined: List of questions/table of contents
writing phase. The writing phase began with the table of contents, which helped us to select the topics to be addressed.
During the
discussion, we decided that the paper on the treatment of hyperhidrosis should cover the surgical technique, the differential diagnosis between primary and secondary hyperhidrosis, selecting patients suitable for surgery, defining relevant risk factors for post-surgical side effects (especially compensatory sweating), and managing the side effects and recurrences surgically and non-
surgically (Figure 1). The table of contents was concluded by assigning each chapter to an operative working group of 2-3 people.
According to the Modified Delphi Process, to address these topics, we formulated 19 PICOT questions (Figure 2). Each PICOT was discussed in small groups, and relevant keywords – both Embase index terms and title/abstract terms – were identified. These keywords were reviewed and approved by the group. Searches were not limited by publication year and were translated for Embase, Medline (via Ovid), and Cochrane Central. PubMed was excluded due to its limited proximity operator. Results per PICOT varied from about 20 to 300.
We are currently conducting the systematic literature search. Each chapter group received a list of abstracts to select those with valid evidence based on their expertise. Comparing selections will produce a final list of accepted papers to formulate the consensus statements.
References
1. Lee ACH, Ferguson MK. Knowledge of surgical management of hyperhidrosis among primary care physicians and the general public. Interact Cardiovasc Thorac Surg. 2022 May 2;34(5):791-798.
2. Cerfolio RJ, De Campos JR, Bryant AS, et al. The Society of Thoracic Surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann Thorac Surg. 2011 May;91(5):1642-8
3. Raveglia F, Lugaresi M, Furak J, et al. Thoracic autonomic nervous system surgery current application-a survey among members of the ESTS. J Thorac Dis. 2025 Feb 28;17(2):979-990.
4. Milojevic M, Freemantle N, Hayanga JWA, et al. Harmonizing Guidelines and Other Clinical Practice Documents: A Joint Comprehensive Methodology Manual by the AATS, EACTS, ESTS, and STS. Ann Thorac Surg. 2025 Jan;119(1):83-100.
Francesco Petrella Fondazione IRCCS San Gerardo dei Tintori, Monza, Italy
Federico Raveglia IRCCS San Gerardo dei Tintori, Milan, Italy
Acquired Cardiac Disease Domain
08:30 – 09:30 Focus Session Auditorium 15
Red flags in TAVI imaging: When TAVI becomes a risky endeavour
J Trent Magruder1, Sangmin A Kim2, Vinod H Thourani2
1 Department of Cardiovascular Surgery, Piedmont Heart Institute, Athens, GA
2 Department of Cardiovascular Surgery, Marcus Valve Center, Piedmont Heart Institute, Atlanta, GA
The management of aortic stenosis (AS) has changed dramatically over the past two decades; once reserved for only high and extreme-risk patients, transcatheter aortic valve implantation (TAVI) is now utilised in all risk categories. While the preoperative evaluation for the 1st generation TAVI devices was based on 2D transthoracic echocardiography (TTE), the current algorithms use high-definition, gated, 3D computed tomography (CT) for precise TAVI planning. Excellent work by many investigators, as well as the weight of real-world experience over time, has linked certain imaging findings with risks of adverse outcomes following TAVI. These pitfalls can be grouped into at least three key areas: challenging access routes and alternative access approaches, annular anatomy and calcification, and coronary artery heights.
The first hurdle to overcome when delivering a TAVI valve is to find a way to the heart. Careful examination of access options for valve delivery remains a cornerstone of pre-TAVI imaging. Access complications are associated with significant morbidity and mortality.1,2 Transfemoral access is by far the most common approach (97% in the U.S.) and is associated with the best outcomes following TAVI as compared to alternative access, even when a peripheral vascular intervention is required. Transcaval and transcarotid access have become the preferred secondary delivery route when transfemoral access is inadequate, and has been shown to be safe and associated with a lower stroke risk than transaxillary/subclavian access.4,5 Imaging can guide the selection of the aspect of the descending aorta is applicable for transcaval puncture and closure and also appropriate which carotid artery is of adequate caliber and linearity.
Once a delivery route is chosen, imaging to determine valve sizing based on annular anatomy forms the core of pre-TAVI imaging evaluation. While appropriately large valve sizing is key to
addressing the fundamental hemodynamic problem of AS, there are many pitfalls specific to each patient which can result in hazardous situations. Traditionally, valves are sized based on systolic annular measurements, as diastolic sizing can result in a change in the selected valve size in possibly half of all patients.6 Oversizing can lead to annular rupture, which is often a fatal complication. Small aortic annuli are thought to present a heightened risk of root rupture, though this catastrophe usually occurs in the presence of other risk factors like heavy calcification.7 Subannular calcification near the muscular left ventricular outflow tract (LVOT) – for example, so-called “dagger” sometimes seen extending down from the annulus – has been associated with an increased risk of annular rupture.8 This is particularly important in those with bicuspid AV, specifically those with a Sievers 0 valve morphology. On the other hand, undersizing can lead to paravalvular regurgitation (PVR), as can increased landing zone calcium. Annular calcium in the device landing zone above 1,079 mm2 has been identified as a PVL risk factor, with an 8% increased risk of mild or greater PVL for every additional 100 mm2 of calcium.9
In addition to annular anatomy, the other key component of the aortic root assessed on pre-TAVI imaging is coronary artery anatomy, to ensure that the ostia are not occluded during valve placement by native leaflets and calcium. Traditionally, coronary artery heights of less than 10 mm are considered high risk for More recently, using computational predictive modelling, the distance from the cusp to the coronary ostium (indexed by coronary artery diameter) has been shown to be highly sensitive for predicting coronary These methods have been validated for clinical use, and we use them for decision-making on virtually every TAVI candidate at our institution.12 Computational predictive modelling can also be used to assess annular stress and the risk of root rupture, an invaluable tool particularly for heavily calcified annuli.

Surgery after TAVR implantation
08:30 – 09:30 Focus Session Hall A3
Structural valve degeneration after TAVR and SAVR
The latest release of the novel Guidelines on Heart Valve Disease by the European Society of Cardiology (ESC) and the EACTS lowered the age for routine TAVR implantation in patients with a tricuspid aortic valve to 70 years. Given the increasing life expectancy, knowledge about valve durability is of utmost importance for heart team decisions. Also, as a side note for younger patients, the Ross procedure is now endorsed for younger patients due to the excellent long-term survival and its improved valve durability.1,2
The surgical community has decades of experience regarding bioprosthetic valve durability, which will help us understand the mechanisms of valve degeneration. Typically, early cases of structural valve degeneration become evident from seven years after implantation onwards.3 This was recently observed in surgical valves with externally mounted leaflets, which were subsequently retracted from the market.4
Factors
In short, TAVI has become a remarkably safe and effective treatment in large part due to careful imaging workup and an evolving understanding over time of pitfalls to be avoided. Problems with access routes are readily detected and help to prevent intraprocedural surprises. Anatomic issues with the aortic root, like
related to valve degeneration

Factors influencing valve durability are valve/ leaflet geometry, including mechanical behaviour and valve size, leaflet tissue, haemodynamic stress measured by transvalvular gradient as well as pressure load in the closed position, and patient-related factors including age and kidney function. These factors are present in patients undergoing SAVR and TAVR. In addition, TAVR or SAVR specific factors are the presence of pledgets (SAVR) as well as the presence of the native, calcified leaflets (TAVR). While we were able to show that the absence of pledgets is beneficial for transvalvular gradients (comparing the Edwards Intuity to the Edwards Magna valve), this effect is probably also contributing to lower gradients in TAVR.5 A lower transvalvular gradient might also contribute to improved durability of TAVR valves. On the contrary, TAVR valves are typically not perfectly
small size, excess calcification, or low coronary heights, are also key considerations. Computational predictive modeling is an important tool which can help the heart team more quantitatively assess root anatomy and mitigate risky situations. Ongoing data collection and model refinement will surely improve our ability to safeguard patients with imaging before they enter the procedure suite.
References
1. Mach M, Okutucu S, Kerbel T, et al. Vascular complications in tavr: Incidence, clinical impact, and management. J Clin Med. 2021;10(21):5046. doi:10.3390/ JCM10215046/S1
2. Laakso T, Moriyama N, Raivio P, et al. Impact of Major Vascular Complication Access Site Status on Mortality After Transfemoral Transcatheter Aortic Valve Replacement ― Results From the FinnValve Registry ―. Circ Rep. 2020;2(3):182. doi:10.1253/CIRCREP.CR-20-0007
3. Isogai T, Agrawal A, Shekhar S, et al. Comparison of Outcomes Following Transcatheter Aortic Valve Replacement Requiring Peripheral Vascular Intervention or Alternative Access. J Am Heart Assoc. 2023;12(12):28878. doi:10.1161/JAHA.122.028878,
4. Junquera L, Kalavrouziotis D, Côté M, et al. Results of transcarotid compared with transfemoral transcatheter aortic valve replacement. Journal of Thoracic and Cardiovascular Surgery. 2022;163(1):69-77. doi:10.1016/J. JTCVS.2020.03.091,
5. Kirker E, Korngold E, Hodson RW, et al. Transcarotid Versus Subclavian/Axillary Access for Transcatheter Aortic Valve Replacement With SAPIEN 3. Annals of Thoracic Surgery. 2020;110(6):1892-1897. doi:10.1016/j. athoracsur.2020.05.141
6. Murphy DT, Blanke P, Alaamri S, et al. Dynamism of the aortic annulus: Effect of diastolic versus systolic CT annular measurements on device selection in transcatheter aortic valve replacement (TAVR). J Cardiovasc Comput Tomogr. 2016;10(1):37-43. doi:10.1016/J.JCCT.2015.07.008,
7. Coughlan JJ, Kiernan T, Mylotte D, Arnous S. Annular rupture during transcatheter aortic valve implantation: Predictors, management and outcomes. Interventional Cardiology: Reviews, Research, Resources. 2018;13(3):140-144. doi:10.15420/ICR.2018.20.2,
8. Girdauskas E, Owais T, Fey B, et al. Subannular perforation of left ventricular outflow tract associated with transcatheter valve implantation: Pathophysiological background and clinical implications. European Journal of Cardio-thoracic Surgery. 2017;51(1):91-96. doi:10.1093/EJCTS/EZW252, 9. Pollari F, Dell’Aquila AM, Söhn C, et al. Risk factors for paravalvular leak after transcatheter aortic valve replacement. Journal of Thoracic and Cardiovascular Surgery. 2019;157(4):1406-1415.e3. doi:10.1016/j.jtcvs.2018.08.085
10. Ribeiro HB, Webb JG, Makkar RR, et al. Predictive factors, management, and clinical outcomes of coronary obstruction following transcatheter aortic valve implantation: Insights from a large multicenter registry. J Am Coll Cardiol. 2013;62(17):1552-1562. doi:10.1016/j.jacc.2013.07.040
11. Heitkemper M, Hatoum H, Azimian A, et al. Modeling risk of coronary obstruction during transcatheter aortic valve replacement. Journal of Thoracic and Cardiovascular Surgery. 2020;159(3):829-838.e3. doi:10.1016/j. jtcvs.2019.04.091
12. Holst K, Becker T, Magruder JT, et al. Beyond Static Planning: Computational Predictive Modeling to Avoid Coronary Artery Occlusion in TAVR. Annals of Thoracic Surgery. 2025;119(1):145-151. doi:10.1016/j.athoracsur.2024.05.041
round after implantation in the native annulus, which might reduce the durability of balloonexpandable and intra-annular valves. However, supra-annular valves are protected from uneven expansion, distorted leaflet opening/ closing and faster degeneration. The effect of remnant leaflets after TAVR implantation on durability is more difficult to understand. While reduced sinus washout may lead to leaflet thrombosis, connected possibly to early degeneration, calcified leaflets may induce further calcification or thrombus formation, leading not only to valve degeneration but also to embolic events, possibly explaining reduced long-term survival in TAVR patients. Importantly, Re-Do surgery after TAVR implantation is one of the fastest-growing cardiac surgical procedures, with high technical complexity and significant surgical risk.
Future perspectives
While the heart-team community is currently discussing the durability of SAVR and TAVR, I would recommend focusing more on the specific prosthesis type rather than the implantation technique. The Notion – 1 trial
showed excellent results for TAVR regarding durability, but the majority of patients in the SAVR group received prostheses which were subsequently retracted from the market due to their impaired durability, while the CoreValve has good long-term durability due to its supraannular design.6 I would therefore strongly motivate the surgical community to contribute to international registry databases for long-term valve durability in SAVR and TAVR patients. Furthermore, device companies should be required to prolong clinical follow-up after randomised TAVR trials for at least ten years.
References
1. Oeser, C., et al., The Ross procedure in adult patients: a single-centre analysis of long-term results up to 28 years. Eur J Cardiothorac Surg, 2022. 62(2).
2. Praz, F., et al., 2025 ESC/EACTS Guidelines for the management of valvular heart disease. Eur J Cardiothorac Surg, 2025. 67(8).
3. Bismee, N.N., et al., Bioprosthetic Aortic Valve Degeneration After TAVR and SAVR: Incidence, Diagnosis, Predictors, and Management. J Cardiovasc Dev Dis, 2024. 11(12).
4. Werner, P., et al., Structural valve deterioration after aortic valve replacement with the Trifecta valve. Interact Cardiovasc Thorac Surg, 2021. 32(1): p. 39-46.
5. Capelli, C., et al., Pledget-Armed Sutures Affect the Haemodynamic Performance of Biologic Aortic Valve Substitutes: A Preliminary Experimental and Computational Study. Cardiovasc Eng Technol, 2017. 8(1): p. 17-29.
6. Thyregod, H.G.H., et al., Transcatheter or surgical aortic valve implantation: 10-year outcomes of the NOTION trial. Eur Heart J, 2024. 45(13): p. 1116-1124.
Figure 1 – Explanted TAVR prosthesis
Vinod H Thourani
Piedmont Heart Institute, Atlanta, GA
Martin Andreas Medical University of Graz, Graz, Austria
SCIENTIFIC PROGRAMME


LEARNING LABS

Take advantage of the invaluable opportunity to train with some of the world’s best cardiothoracic surgeons at the EACTS Learning Lab. These specialist hands-on workshops are designed to advance your technical abilities and include wetlabs, drylabs, simulation and practical sessions.
You will gain practical experience using the latest devices, practice on simulators and interact with expert faculty and industry proctors. EACTS Learning Lab sessions are available to EACTS members for just an additional €75 each (€100 for non-members). Spaces are limited and offered on a first-come, first served basis. Don't miss out – book today to guarantee your opportunity.
LEARNING LAB SCHEDULE
Session broadcast: EACTS 2025 trial update session Nicklas Brendborg & EACTS
09:00 – 11:00 Thoracic 09:00 – 11:00 Endoscopic Dry Lab Training

EXHIBITION FLOOR PLAN

EACTS Outreach Programme
Advancing education initiatives in underserved regions
The EACTS Outreach Programme improves the outcomes for heart patients in underserved regions by advancing education initiatives. The programme distributes grants with funding from the Edwards Lifesciences Foundation and the Every Heartbeat Matters (EHM) initiative to qualified surgeons involved in humanitarian work in underserved regions and communities. The FFF EHM grants aim to support programmes that focus on the detection, treatment and recovery of these populations,
with the goal of reducing the global burden of structural heart disease.
Recipients of the FFF Every Heartbeat Matters Grants – who must be an EACTS member – will provide education to help reduce the global burden of structural heart disease and drive progress towards global equity in surgical care.
“Many EACTS members already engage in vital educational and humanitarian programmes, particularly in Africa. The EACTS Outreach Programme will drive and
coordinate more of this important work –harnessing the expertise of EACTS members and fostering collaborations with industry partners, charities and other organisations,” said Patrick Myers, EACTS Secretary General. “Together we can improve long-term patient outcomes by opening up access to heart valve treatments around the world.”
The EACTS Outreach Committee, Chaired by Professor Carlos Mestres, Extraordinary Professor at the Department of Cardiothoracic Surgery at the University of
the Free State in South Africa, will award industry or charity-sponsored grants to EACTS members. By leveraging industry and charity contacts, EACTS aims to shift the focus from short-term missions to sustainable programmes that improve long-term patient outcomes in underserved regions, with growing interest from industry to fund such efforts.
Jee Siang Malaysia
Sue Vern Chan Malaysia
Luis
Eduardo Castro Roblin Mexico
Juan Manuel Saucedo Mexico
Rafael Quezada Angulo Mexico
Sergio Tellez Luna Mexico
Raymundo
Garcia Gonzalez Mexico
Miguel Matos
Hernandez Mexico
Oliver Huerta Del Angel Mexico
Jesus Matus Mexico
Nyamsuren Sainbayar Mongolia
Tuguldur Narankhuu Mongolia
Batbaatar Damtsag Mongolia
Sara Waguaf Morocco
Mouad Gourti Morocco
Ismail Oughebbi Morocco
Khin Maung Lwin Myanmar
Christopher Van Wyk Namibia
Manish Mallik Nepal
Ashish Kharel Nepal
Manoj Tiwari Nepal
Bas Hoogenboom Netherlands
Santosh
Gangaram-Panday Netherlands
Shanti Khargi Netherlands
Berat Avci Netherlands
Stuart Head Netherlands
Kevin Veen Netherlands
Jochem Jongenotter Netherlands
Nora Bacour Netherlands
Rogier Dolman Netherlands
Vincent Van Suylen Netherlands
Maria Agustina Bayon Netherlands
Maximiliaan Notenboom Netherlands
Adine De Keijzer Netherlands
Reda Rhellab Netherlands
Aytug Tirpan Netherlands
Jutta Arens Netherlands
Tim Mandigers Netherlands
Aria Yazdanbakhsh Netherlands
Casper Zijderhand Netherlands
Rengin Sabaoglu Netherlands
De Qing Görtzen Netherlands
Stephanie Ch’ng New Zealand
Peter Alison New Zealand
Trevor Tnay New Zealand
Fiona Doig New Zealand
Esther Ademeta Nigeria
Oluwaferanmi Morenikeji Nigeria
Theis Tonnessen Norway
Hedda Hauge Norway
Knut Eivind Kjoerstad Norway
Muhammad Chaudhary Pakistan
Vikram Kumar Pakistan
Noman Izhar Pakistan
Zara Shirazi Pakistan
Waqar Malik Pakistan
Zeeshan Afzal Pakistan
Farah Sobia Pakistan
Muhammad Bilal Pakistan
Hassan Mushtaq Pakistan
Muhammad Nisar Pakistan
Yasir Khan Pakistan
Alifa Sabir Pakistan
Raja Muhammad Ejaz Pakistan
Mian Kamal Pakistan
Marcos Fletcher Panama
Franklin Martinez Peru
Frank Garcia Rojas Peru
Tirza Intor Torres Peru
Teodoro Jr Bautista Philippines
Erwyn Novilla Philippines
Liberty Yaneza Philippines
Rudolph John De Juras Philippines
Martyna Bajek Poland
Artur Iwasieczko Poland
Remigiusz Antończyk Poland
Piotr Stepinski Poland
Dmytro Harasymiv Poland
Mikolaj Marszalek Poland
Pawel Kwinecki Poland
Anna Tomkowiak Poland
Maria Luszczyn Poland
Marcin Garbacz Poland
Szymon Pawlak Poland
Andrzej Janda Poland
Arkadiusz Niedźwiecki Poland
Dominik Mendyka Poland
Kamil Tracz Poland
Maria Konkol Poland
Paulina Kopacz Poland
Sebastian Krych Poland
Magdalena Trzebińska Poland
Jakub Piorek Poland
Adelino Leite Moreira Portugal
Joao Silva Portugal
Paulo Santos Portugal
Akosua
Fosuaa Owusu Afriyie Portugal
Helena Dias Boavida Portugal
William Jessee Qatar
Teodora
Ciurariu Astefanoaei Romania
Dan Cercel Romania
Erno Jerzicska Romania
Felix Dobritoiu Romania
Natalia Motas Romania
Vanille Loy Romania
Carolina Bors Romania
Victor Vladu Romania
Andreea Mazilu Romania
Doina Varduca Romania
Miruna Ciobanu Romania
Bashir Tsaroev Russia
Sarah Sirajuddin Saudi Arabia
Mohammed Alreshidan Saudi Arabia
Haitham Alzahrani Saudi Arabia
Mohannad Dawary Saudi Arabia
Faouzi Alimi Saudi Arabia
Ali Bargawi Saudi Arabia
Abdulmohsen Alzakari Saudi Arabia
Mostafa Ateya Saudi Arabia
Bogdan Okiljevic Serbia
Darryl Chin Singapore
Abdulrahman El Gohary Singapore
Ki Han Kim Singapore
Shirley Seah Singapore
Irwan Shah Bin Mohd
Moideen Singapore
Alicia Chia Singapore
Kenny Sin Singapore
Marcus Neo Singapore
Zong Rui Bai Singapore
Rey Chan Singapore
Peter Urban Slovakia
Livia Petrasskova Slovakia
Miha Antonic Slovenia
Veronika Krasek Slovenia
Edgar Mwanguhya South Africa
Risenge Frank Chauke South Africa
Timothy Pennel South Africa
Peter Ramoroko South Africa
Lehlohonolo Dongo South Africa
Riaan Nel South Africa
Jin Kim South Africa
Hendrik Van Der Merwe South Africa
Kaveer Sohan South Africa
Min-Seok Kim South Korea
Kwanyong Hyun South Korea
Kangmin Kim South Korea
Wooshik Kim South Korea
Eun Byul Jung South Korea
Eung Re Kim South Korea
Wan Kee Kim South Korea
Yong Jin Chang South Korea
Jinwon Shin South Korea
Se Jin Oh South Korea
Ji Seong Kim South Korea
Yoonjin Kang South Korea
Ho Jin Kim South Korea
Dong-Hee Kim South Korea
Angela Irabien Spain
Francisco Nino Gonzalez Spain
Luis Díaz Ojeda Spain
Lucía Doñate Bertolín Spain
Juan Esteban De Villareal Spain
Alberto Forteza Spain
Antonio Gonzalez Calle Spain
Jose Marin Spain
Alfonso Cañas Spain
Ignacio Sanchis Haba Spain
Maria Gomez Alfonso Spain
Elena Campos Carot Spain
Deng Siang Lee Spain
Gustavo Woll Spain
Amaya Ramírez Cervera Spain
Francisco Regueiro Mira Spain
Rocío Casais Spain
Sofia
Villavicencio Clayton Spain
Oleg Logunov Spain
Maria Sol Siliato Robles Spain
Kumaradasan Gnanakanthan Sri Lanka
Rajitha
Dilshan Munasinghe
Appuhamilage Don Sri Lanka
Palinda Bandarage Sri Lanka
Yanqi Yang Sweden
Janica Kallonen Sweden
Ruixin Lu Sweden
Claudio Caviezel Switzerland
Armelle Gaussin Switzerland
Eckhard Mauermann Switzerland
Didier Lardinois Switzerland
Selim Mosbahi Switzerland
Niccolo Landert
Switzerland
Yohan Candaux Switzerland
Martha Veit Switzerland
Lukas Glaus Switzerland
Jules Miazza Switzerland
Thierry Aymard Switzerland
Fabrizio Minervini Switzerland
Vincenzo Grimaudo Switzerland
Shengpin Yu Taiwan
Yan Yi Ngai Taiwan
Chwan-Yau Luo Taiwan
Ihsuan Cheng Taiwan
Jahongir Rajabov Tajikistan
Sarfaroz Komilov Tajikistan
Daudi Wapalila Tanzania
Thanakorn
Rojanathagoon Thailand
Saran Chiramongkol Thailand
Paradorn Jetwanna Thailand
Chanokporn Kunanusont Thailand
Thanit Kunanusont Thailand
Kornkarn Mahasawas Thailand
Thitipong Tepsuwan Thailand
Puwadon Thitivaraporn Thailand
Charat Wongwaipijarn Thailand
Surin Woragidpoonpol Thailand
Kabulo Kolela The Democratic Republic of the Congo
Sobhi Mleyhi Tunisia
Serkan Enön Turkey
Oguz Arslanturk Turkey
Cabir Yüksel Turkey
Emek Eken Turkey
Sadettin Derrnek Turkey
Niyazi Gormus Turkey
Mugisha Kyaruzi Turkey
Suat Erus Turkey
Levent Cansever Turkey
Mehmet Saricaoglu Turkey
Ulas Kumbasar Turkey
Omer Faruk Rahman Turkey
Yekta Altemur
Karamustafaoglu Turkey Ali Hasde Turkey
Mehmet Karahan Turkey
Eslem Altin Turkey
Eyüp Yardımcı Turkey
Rifat Özmen Turkey
Bedrettin Yildizeli Turkey
Gizem Kececi Ozgur Turkey
Azel Hujaz Hessen
Nejim Al-Duneyn Turkey
Ayse Cicek Turkey
İsmail Sarbay Turkey
Bahri Cilek Turkey
Imge Dulger Turkey
Ismail Dal Turkey
Ayse Karakoc Turkey
Aykut Kankoc Turkey
Erkan Kaba Turkey
Merve Yumusak Turkey
Seyda Ors Turkey
Melih Alma Turkey
Muhammed Altas Turkey
Yagmur Kahveci Turkey
Ayse Ulusoy Turkey
Izatullah Jalalzai Turkey
Nur Gizem Elipek Turkey
Basak Gorusun Turkey
Mihriban Sari Turkey
Gozde Aylin Yildiz Turkey
Salih Bilen Turkey
Erhan Özer Turkey
Atilla Pekcolaklar Turkey
Esra Yamansavcı Şirzai Turkey
Orhan Aliev Turkey
Ghazi Elshafie UK
Miray Isa Turkey
Ghattas Rizk Ukraine
Mykhailo Kryvetskyi Ukraine
Diana Furman Ukraine
Serhii Sheludko Ukraine
Vladyslav Stepanov Ukraine
Aleksandr Yachnik Ukraine
Bohdan Hel Ukraine
Yurii Hutsuliak Ukraine
Volodymyr Tanskyi Ukraine
Roman Domashych Ukraine
Maryna Tomashyk Ukraine
Ksenia Denisova Ukraine
Bei Anna Ukraine
Elina Chunikhovska Ukraine
Artemii Petlytskyi Ukraine
Vasyl Shymon Ukraine
Taras Okun Ukraine
Bohdan Hulitskyi Ukraine
Andriy Balabukha Ukraine
Anastasiia Melnyk Ukraine
Oleksii Mukha Ukraine
Dmytro Vichev Ukraine
Viktor Tytiuk Ukraine
Ajit Cheriyan United Arab Emirates
Marius Roman UK
David Waller UK
Abir Benhissoune UK
Saqib Qureshi UK
María Monteagudo Vela UK
Nikan Hoorijani UK
Ali Elbassioni UK
Shiva Mokhtassi UK
Emad Aljaaly UK
Rakesh Uppal UK
Simon Jordan UK
Felice Granato UK
Zahid Mahmood UK
Syed Aidil Hizman Syed
Nong Chek UK
Kathryn Fisher UK
Ashvini Menon UK
Fathima Mubarak UK
Hosam Ahmed UK
Alessandro Maraschi UK
Phoebe Waters UK
Amir Awwad UK
Ali Ansaripour UK
Maria Ibrahim
Mohammed Al Hammadi UK
Leila Mohamed UK
Saarim Bari UK
Katie Shiner UK
Shaurya Parekh UK
Ehimen Ataman UK
Benjamin Chapman UK
Ria Bhandari UK
Manoj Purohit UK
Alexander Reynolds UK
Nur Mousa UK
Rafe Zoubi UK
Dimitrios Pousios UK
Chun Cheong Lau UK
Sophia Shrestha UK
Ethan Alford UK
Zaidhan Khan UK
Mohamed Allam UK
Elena Lee UK
Rishita Prabhu UK
Mostafa Snosi UK
Sakshi Roy UK
Lucia Borovickova UK
Mahmoud Elkhayat UK
Sandra Ayad UK
Nikhil Sahdev UK
Rohan Pancharatnam UK
Kassem Kassem UK
Sendhil Kumaran
Balasubramanian UK
Joseph Zacharias UK
Moslem Mohamed Ahmed Fathy Fathalla
Abdelghafar UK
Kareem Hosny UK
Mostafa Wa El Sayed UK
Hanad Ahmed UK
Joshua Hon UK
Keith Buchan UK
Eshan Senanayake UK
Ahmed Shaheen UK
Sri Aurovind UK
Kathryn Edmonds UK
Kamya Mandhar UK
Aurora Sonkin UK
Iyad Al Mohtar UK
Ujjawal Kumar
David Varghese
Sarah Guo
Umar Shafiq
Abdelnour
Anastasakis
Yu Liu
Awad
Gilbert
Tharun Rajasekar


Thursday 05 - Sunday 08 March 2026
Intercontinental Sydney Harbour NSW, Australia
Program Director
Homayoun Jalali MD
t
Scan the QR code to express your interest

Fresh Perspectives at TPC
“Already familiar with European and North American approaches? Join us in Sydney for an Australian and New Zealand perspective on the challenges and opportunities shaping our daily practice.”
Publications and Guidelines Webinars
Our Guidelines Webinars present case studies demonstrating the utility of guidelinedirected care in cardiothoracic surgery, bridging theoretical knowledge with practical insights.
Watch On Demand | 2025 ESC/EACTS Guidelines for the Management of Valvular Heart Disease
Coming soon | 2025 EACTS/STS/AATS Guidelines on Temporary Mechanical Circulatory Support WATCH NOW!

Our Publications Webinars cover a wide variety of topics, from providing key resources for researchers to discussing the latest hot topics and surgical techniques shaping the field.
Watch On Demand | MMCTS Webinar: Leaflet Replacement Materials in Aortic Valve Repair
Coming soon | 28th October | MMCTS Webinar: Aneurysmatic Lesions of the Coronary Arteries: Preoperative Aspects and Surgical Management
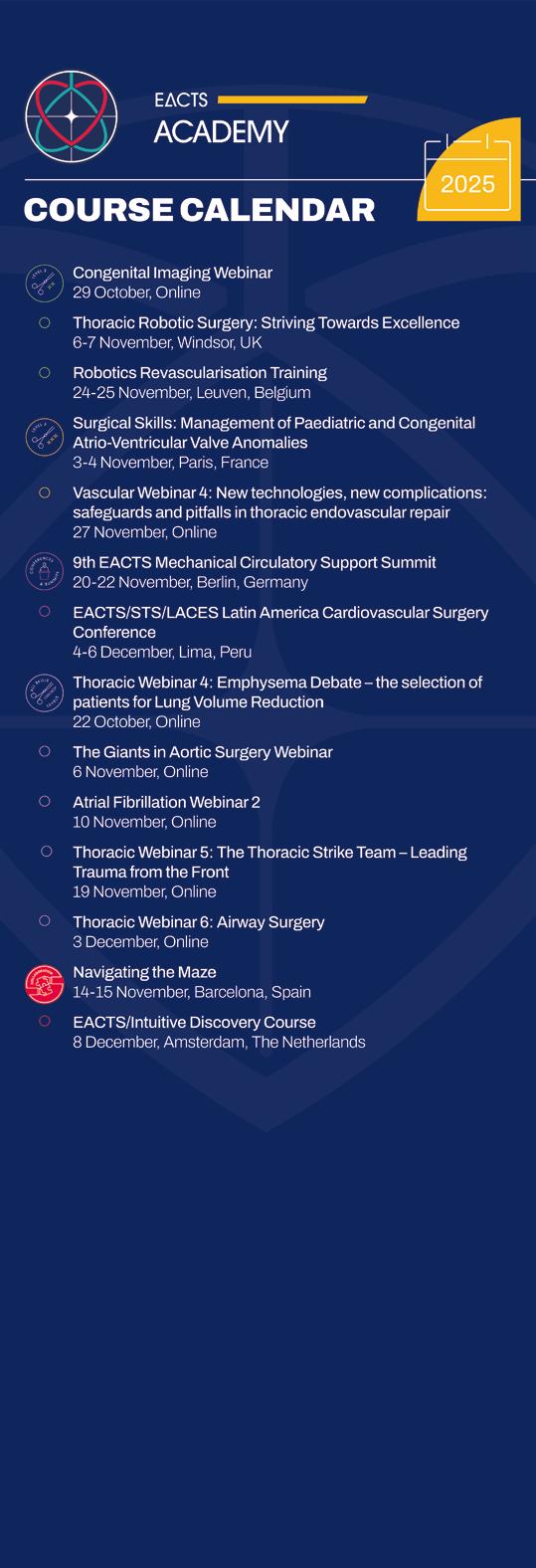

Barcelona Spain 7-10 October 20 26
