

DAILY NEWS

Techno-College Innovation Award 2025
Congratulations to Dr Isaac George, winner of the 2025 Techno-College Innovation award in recognition of PTP technology.
2
Domain Highlights
Domain Chairs share their highlights for the packed three-day scientific programme.
6

WiCTS in Copenhagen

Residents at EACTS
Chair of WiCTS Committee, Indu Deglurkar outlines the Committee’s achievements and activities in Copenhagen.
8
EACTS Residents’ Committee Chair, Nabil Hussein, discusses this year’s Residents Programme in Copenhagen. 10

President's Choice

The highest-ranked abstracts across all four domains are presented during this special session.
12
On behalf of EACTS, I would like to welcome you all to the beautiful city of Copenhagen for the 39th EACTS Annual Meeting. Thank you for joining us. Attendees at this year’s meeting have travelled from all over the world for the most important international cardio-thoracic meeting of the year - your presence here is greatly appreciated. Over the next few days, you will witness the very best scientific presentations that will showcase our speciality’s ability to INNOVATE, DISCOVER and EDUCATE.
The Annual Meeting offers delegates a unique opportunity to connect with global experts, explore groundbreaking innovations and scientific advancements, experience unparalleled networking opportunities and discover new techniques and fresh approaches in cardiothoracic surgery.
We are joined by members of the cardiothoracic surgical community from across the world: surgeons, allied health professionals, researchers and scientists, colleagues from industry and many other professionals, giving us an opportunity to meet and learn from each other.
This year, we welcome more pre-trainees to the Annual


Meeting, part of EACTS’s commitment to supporting the next generation of surgeons. The scientific programme for pre-trainees is designed to ensure they receive the guidance and knowledge they need to thrive in their early careers.
Our third ‘Innovation Summit’ held earlier this year in Paris was a great success, with over 70 abstracts submitted and 17 selected for presentation at the Summit. These ‘disruptive technologies’ have the potential to reshape our specialty. A selection of the highest-ranked abstracts will be shared with delegates at the ‘Highlights of the Innovation Summit’ session taking place on Friday.
In the Auditorium later this morning, we will hear from our honoured guest, Jens Krause, a behavioural biologist, who will discuss the adaptive value of collective behaviour from different perspectives and through modelling approaches to explain collective intelligence and the empirical support for it in the laboratory and in the field.
More than ever, we must listen and learn from our colleagues in other specialties and in Copenhagen, we have a several joint sessions with – but not limited to – the European Heart Rhythm Association, the Society of Thoracic Surgeons, the European Society of Thoracic Surgeons, the Asian Society of Cardiovascular and Thoracic Surgery, the European Association of Cardiothoracic Anaesthesiology and Intensive Care and the Association for European Paediatric and Congenital Cardiology, among others.
There are also several sessions presenting the latest EACTS guidelines, and I encourage you to attend these sessions so you





Nimesh Desai
Joseph Bavaria Ruggero De Paulis
IN THIS ISSUE
Learning Labs
Take advantage of the invaluable opportunity to train with some of the world’s best cardiothoracic surgeons at the EACTS Learning Lab. Our hands-on workshops are designed to advance your technical abilities and include wetlabs, drylabs, simulation and practical sessions.
Continued from page 1
can learn more about major updates to guidelines on topics including valvular heart disease.
As ever, the ‘Trial Update Session’ on Saturday is an opportunity to dive deep into the latest data from current trials such the Mid-Term Outcomes of TAVI vs SAVR: Insights from the five-year UK TAVI Trial, an update on ongoing studies from mitral valve trials, FAME-3 Trial at five Years that will have implications for PCI and CABG strategies and a focus on the new pharmacological frontiers in secondary prevention after cardiac
surgery including SGLT-2 inhibitors, GLP-1 agonists, and PCSK9 inhibitors.
Over the next couple of pages, our domain Chairs share details of some of their highlight sessions. I am immensely grateful for their work, alongside their task forces, to develop an unparalleled cardio-thoracic scientific programme.
Thank you, once again, for travelling to Copenhagen. This is the highlight in the EACTS calendar, a time for you to make new connections and meet old friends, but above all a time for learning and to ultimately, achieve better outcomes for our patients.
Techno-College Award Winner 2025
Congratulations to Dr Isaac George (New York Presbyterian Hospital-Columbia University Irving Medical Center, New York, USA), winner of the 2025 Techno-College Innovation award in recognition of Photochemical Tissue Passivation (PTP) technology. Here, he describes how this point-of-care therapy strengthens venous tissue, thereby improving long-term vein graft durability…
Photochemical Tissue Passivation: How Light Can Save the Saphenous Vein Graft
DWatch live and recorded content from this year's Annual Meeting on EACTS TV, featuring compelling panel debates, highlights and interviews with the world’s leading cardiothoracic surgeons. 28
Satellite Symposia
Join experts as they discuss the latest clinical data, current and future approaches to patient care and much more in a wide range of satellite sessions hosted by industry.


urVena is advancing coronary artery bypass grafting (CABG) with its novel PTP technology, a point-of-care therapy designed to strengthen venous tissue and dramatically improve long-term vein graft durability. Despite advances in surgical techniques and medical management, CABG's efficacy remains limited primarily due to vein graft failure and the progression of atherosclerosis in native coronary arteries. Vein graft failure is ascribed to the luminal narrowing that results from intimal hyperplasia, medial thickening, and subsequent concomitant accelerated atherosclerosis. Structurally, veins are not designed to withstand arterial pressure. Vein grafts excessively expand under arterial pressure, causing irreversible injury and progressive endothelial remodeling. Vein grafts are subject to reported degeneration and occlusion rates from 20-40% in the first year and as high as 50% at five years. SVG failure is associated with a significant increase in major adverse cardiovascular events (MACE), including death, myocardial infarction (MI), and the need for repeat revascularization.
DurVena’s PTP device addresses this challenge by applying Rose Bengal dye, a photo-initiator with a long history of medical use, to the exterior of the harvested vein. The coated vein is then exposed to LED light, which activates the dye, thereby creating additional collagen crosslinks in the extracellular matrix of the vein's adventitia. The collagen crosslinks increase tissue strength and decrease elasticity without altering the histological makeup of the vein. In extensive, published pre-clinical testing of PTP in both small and large animals, a significant increase in vein stiffness (5-fold), a comparable reduction in vein expansion, and a reduction in intimal hyperplasia (a precursor to stenosis and graft failure) have been demonstrated. In addition, Durvena has also completed a first-in-human safety study demonstrating no device-related events at 30 days, 6 months, and one year.
PTP therapy is precise and localized. Rose Bengal binds non-covalently to collagen in the extracellular matrix. Upon illumination, it forms covalent crosslinks between collagen
A SNAPSHOT OF THURSDAY'S SESSIONS
10:00 - 11:00 Room 18 & 19
WiCTS – Gender Medicine: Unravelling the blind spots
13:45 - 14:45 Hall A1
From Guidelines to Treatment: Transforming ESC/EACTS guidelines into lifelong AS management
13:45 - 14:45 Hall A3
Thoraco-abdominal aortic surgery at the crossroads –STS @ EACTS session

molecules, reinforcing the tissue. The dye penetrates only about 100µm into the adventitia, forming a stable surface band. There is no change to the histological makeup of the vein. The entire process is monitored by validated software, ensuring consistent and safe application.
This novel therapy is licensed from Massachusetts General Hospital and is being developed by an accomplished team of business professionals with several successful exits and extensive experience in start-up medical device development in this market sector. Durvena has significant intellectual property protections with broad claims covering the PTP method and devices for vein graft preparation, as well as other applications, that have been issued around the world. PTP technology has broad utility applicable beyond CABG, which DurVena will explore after initial success in the CABG market. The company has received Breakthrough Designation from the FDA and expects to enroll the first patient in a US pivotal trial in the first half of 2026.
DurVena’s PTP therapy represents a paradigm shift in vein graft preparation, offering a simple and effective solution to a longstanding clinical challenge. For clinicians, it holds promise for improving patient outcomes. For strategic partners, it offers a differentiated, IP-protected platform with expansion potential across multiple medical applications.
13:45 - 14:45 Room 180 & 181
EACTS/EBCP - Perfusion in Transition: Consensus, Data and Technology and Organ care
15.15-16.15 Auditorium 12
Management of esophageal surgical disease
15.15-16.15 Auditorium 10
EACTS/AEPC joint session: Invasive treatment of congenital heart disease: Combing surgery and intervention
16:30 - 17:30 Hall A1
2025 EACTS guidelines highlights
16:30 - 17:30 Room 18 & 19
Pre-trainees
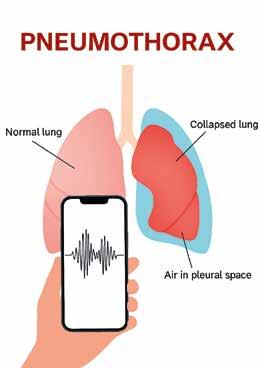
Voice-based acoustic profiling for pneumothorax detection: A non-invasive, real-time diagnostic system
Introduction
Pneumothorax (PNX), defined as the accumulation of air in the pleural cavity with partial or complete lung collapse, is a life-threatening emergency that requires immediate recognition and intervention. While chest X-rays and CT scans remain the gold standard for diagnosis, these tools are not always instantly available, especially in emergency rooms under strain, rural hospitals, disaster zones, or combat environments. Delays in recognition may lead to hypoxemia, hemodynamic compromise, or death.
This project addresses a simple yet profound question: Can we detect pneumothorax using only the human voice? Although the human ear perceives no major difference, pleural air and reduced lung volume inevitably change thoracic resonance. These shifts alter the acoustic properties of speech in ways imperceptible to the clinician but measurable with digital analysis.
Methods
We prospectively collected 59 standardised recordings from 29 patients with confirmed pneumothorax. Each patient read a short sentence (3–5 seconds) both during the pneumothorax phase and after re-expansion of the lung. Recordings were captured with common smartphones (iPhone 14 or later), under routine ward conditions, without special microphones or soundproofing. (Figure 1)
Acoustic analysis was conducted using Praat software, extracting:
n Pitch (median and mean, Hz)
n Formant frequencies (F1–F4, Hz)
n Jitter (%)
n Shimmer (%)
n Harmonics-to-noise ratio (HNR, dB)
Logistic regression models were tested. Diagnostic accuracy was assessed through ROC analysis and scoring rules.
Results
Several parameters demonstrated clear separation between pneumothorax and post-expansion states.
n Formants F2 and F3 showed strong individual diagnostic performance (AUC 0.81 and 0.85).
n Jitter, shimmer, and HNR emerged as the most reliable markers, with AUC values of 0.93, 0.89, and 0.87 respectively.
n A combined model (shimmer + jitter + HNR) achieved AUC 0.833 (95% CI: 0.752–0.908) with 75% sensitivity and 81% specificity.
n A binary cutoff rule (jitter >1.0%, HNR <16 dB, F2 >1800 Hz) identified 89.2% of cases

Örs Kaya Chest Diseases and Research Hospital, Izmir, Turkey
without false positives in controls.
Clinical implications
The ability to detect pneumothorax in seconds using only a smartphone represents a potential paradigm shift. Consider these scenarios:
n Rural ambulance services: where chest imaging is not immediately available.
n Natural disasters and war zones: where medical infrastructure is compromised and triage decisions must be made instantly.
n Remote healthcare and telemedicine: where a patient’s voice recording can be uploaded for analysis, guiding urgent decisions.
n Post-operative surveillance: where silent or recurrent pneumothorax may be detected early, without repeated exposure to radiation. By leveraging devices already in every pocket, this approach democratizes diagnosis, extending access to vulnerable populations.
Innovation and global perspective
What sets this project apart is not only its
accuracy but its accessibility. Sophisticated imaging systems cost thousands of dollars and require trained personnel. In contrast, this method relies on nothing more than a smartphone and open-source software.
From a global health perspective, such tools can bridge healthcare inequities. In lowresource settings where CT scanners are unavailable, this system could be the difference between life and death. In high-resource settings, it offers speed and efficiency, reducing diagnostic delays and healthcare costs.
Limitations and next steps
This is a pilot study with a modest sample size. Validation in larger, multicenter cohorts is essential. Additional work is needed to ensure robustness across languages, accents, and age groups.
The next step is to integrate findings into a machine learning–powered mobile application, providing automatic, real-time feedback to clinicians. We are currently expanding the dataset and developing prototypes for clinical testing.
Beyond pneumothorax, this line of research may extend to other thoracic conditions— pleural effusions, airway obstructions, or pulmonary fibrosis—where changes in sound transmission carry hidden diagnostic value.
Personal motivation
As a thoracic surgeon, I often confront the urgency of pneumothorax. Minutes matter. Yet as someone fascinated by the intersection of physics, acoustics, and medicine, I see in this project more than a diagnostic shortcut: it is a bridge between science and clinical care.
Just as Laennec’s stethoscope transformed
diagnosis two centuries ago, perhaps digital acoustic profiling can do the same in our era—transforming the everyday smartphone into a powerful clinical ally.
Conclusion
Voice-based acoustic profiling for pneumothorax detection is non-invasive, portable, fast, and inexpensive. It offers diagnostic accuracy approaching traditional methods, but with unprecedented accessibility. What began as a simple hypothesis, that pleural air changes thoracic resonance, now stands supported by measurable evidence. With further refinement, this method has the potential not only to save lives but also to redefine the future of thoracic diagnostics.
The Latest Innovation in Deflection and Control

Şeyda
Figure 1
TECHNO-COLLEGE INNOVATION AWARD
The Techno-College Innovation Award 2024 winner
We caught up with Dr Ahmad Ali Amirghof ran from the Shiraz University of Medical Sciences in Iran, who was awarded the 2024 Techno-College Innovation award in recognition of the SRAA valve, a stented Biologic Valve with the Native Right Atrial Appendage Tissue.
What was the inspiration behind developing the SRAA valve and what are the limitations of current treatments?
Despite advances in prosthetic valve technology, the ideal substitute for heart valves is still not available. The S-RAA valve was developed to address the critical limitations of existing prosthetic valves. Mechanical valves necessitate lifelong anticoagulation, exposing patients to risks of bleeding and thromboembolism. Biological valves are susceptible to structural valve deterioration, accelerated by immunemediated calcification.
These shortcomings are particularly pronounced in younger patients and in the low-pressure right-sided cardiac positions. The S-RAA valve is inspired by the concept of using native tissue to create a more biocompatible prosthesis, thereby eliminating the requirement for anticoagulation and potentially mitigating immune-driven degeneration.
What is unique about the SRAA valve (eg biological with a stent/scaffold (Shiraz frame) to mimic the complex dynamics of natural valve function)?
The S-RAA valve is distinguished by two pioneering design innovations:
First, the Living, Non-Immunogenic Leaflets: The valve's leaflets are constructed from the patient's own right atrial appendage tissue. This autologous tissue is not recognized as foreign by the body and is therefore non-immunogenic. This represents a radical departure from animaltissue bioprosthetics. Furthermore, this tissue possesses ideal physical characteristics, such as inherent flexibility, which are essential for proper valvular function. Histopathological evidence confirms the tissue remains viable post-implantation, explaining the exceptional long-term results with no observed calcification or degeneration in over 200 patients in whom the tissue has been used in the paediatric age group for Tetralogy of Fallot repair.
Second, a Dynamic, Stable Scaffold (Shiraz Frame): The valve incorporates a novel, rigid stent known as the Shiraz Frame. This is not a simple ring but an anatomical scaffold engineered to mimic the supportive structure of a native valve's annulus and commissures. This fixed skeleton is geometrically independent and renders the valve's function immune to anatomical changes in the heart's size and shape (e.g., cavity dilatation), ensuring stable performance. Another critical advantage is that the frame features long commissural posts that create an extensive coaptation surface between the leaflets. This provides a built-in safety margin, ensuring the valve remains competent and leak-proof even if the leaflets undergo minor changes like stretching or slight restriction.
How will this technology help to achieve better patient outcomes?
Its most significant impact is the potential to eliminate reoperations caused by structural valve deterioration. Unlike animal-tissue valves, which are doomed to calcify and fail, especially in the young, the S-RAA valve's autologous, living tissue has shown no evidence of calcification in long-term follow-up. For a young patient, this means the first valve replacement may be their last, sparing them a lifetime of repeat surgical procedures and their associated risks, trauma, and anxiety.
Furthermore, by avoiding a mechanical valve, patients are immediately and hopefully permanently freed from the burden of lifelong anticoagulation. This eliminates the risk of bleeding and stroke from medication, a different but constant threat that defines life with a mechanical prosthesis.
The valve provides a large, effective orifice area, which is critically important in the functional class, especially for younger patients. Furthermore, its architectural design intentionally allows for a valve-in-valve procedure should any future reintervention become necessary.
Can you briefly describe the procedure?
The device is available in 23, 25, 27, and 29 mm sizes. Selection is based on the patient's age, annular dimensions, and specifically, the size of the right atrial appendage. The width of the appendage ostium is a key measurement.
The appendage is then harvested and prepared by cutting the large internal muscle bands while leaving the smaller ones intact to facilitate movement and coaptation. The prepared appendage is placed either over the frame or, if smaller, inside it; these two options expand the pool of suitable appendages.
The proximal orifice of the tissue is sutured to the basal ring of the frame with a continuous suture line. The tips of the distal orifice are temporarily fixed to the corresponding sites on the tips of the commissural columns.
The valve is tested for competence by applying negative pressure, a process facilitated by the frame's plastic holder. If the closure is ideal and symmetrical, you proceed to suture the lateral aspects of the appendage to the columns. If any adjustment is required, it is performed at this stage before suturing the columns.
The completed valve is then implanted into the annulus using standard techniques for a prosthetic valve. Uniformly, a water test confirms perfect function with no leakage and a long coaptation surface.
Do you plan to expand the indications for the device?
Yes, we are actively expanding the indications. We have already adapted the technique for high-pressure systems by utilizing autologous pericardium instead of the appendage for mitral valve replacement, as we believe the appendage tissue cannot withstand systemic systolic pressure long-term without risk of dilation or tear.
We also employ pericardium for right-sided valves when the appendage is unsuitable. A key principle is that we do not chemically treat the pericardium; we rely on live tissue to mitigate
degeneration and calcification. While some late restriction is possible, we predict sufficient tissue reserve to maintain coaptation. Technically, working with pericardium is often easier—it offers no size or shape limitations and simplifies assembly on the frame. We shape it into a cylinder to begin the process by suturing the two ends of a pericardial piece together, and from there, the procedure is very similar.
Our early results for both tissue types are comparable, though longer follow-up in larger cohorts is needed.
We will be demonstrating the mitral valve technique with pericardium in a video session in the first day of the congress.
Regarding valve design, our focus has been on simplicity and reproducibility. While trileaflet designs are an option, we are not yet convinced of their clear advantages over the bicuspid design, so we plan to continue with the bicuspid model for the foreseeable future.
What impact has the Techno-College Innovation Award had on the ongoing development of the device?
Winning the Techno-College Innovation Award has had several profound impacts on the development of the device.
First, it significantly increased the global visibility of the innovation, introducing it to a wider surgical and scientific community far beyond our institution.
Second, it served as a strong encouragement for our entire team, reinforcing our motivation and commitment.
Third, it provided crucial validation, giving us confidence that we are on the right path with our research and technical approach.
And fourth, most importantly, it instilled a sense of responsibility. The recognition placed

an obligation on us to rigorously follow through, accelerate our efforts to make it available and practical, and inform the community about the progress and the results.
What feedback did you receive from the cardiothoracic community following your award?
The feedback from the cardiothoracic community following the award was extensive and profoundly encouraging.
Many colleagues reached out to congratulate us, viewing the concept—both the novel frame design and the use of native tissue—as a genuinely innovative approach. There was a strong sense of hope that this technology could ultimately provide patients with significantly improved valve options.
Perhaps the most significant feedback was the overarching sentiment that the device may have opened an entirely new pathway for the future of valve surgery. It was widely described as offering a fresh perspective, like a new look at the horizon, suggesting it has the potential to redefine standards and inspire a new direction in the field.





LUNCH SYMPOSIUM
THURSDAY, OCTOBER 9TH, 12:15 PM - 1:30 PM, AUDITORIUM 15
Simplifying the Complex: Versatility for Your Frozen Elephant Trunk Procedures with the LSA in Mind


Moderator
Dr. W. Szeto (Philadelphia, United States)

Once Upon a Time in Frozen Elephant Trunk…
Prof. M. Czerny (Freiburg, Germany)
Stenting the Left Subclavian Branch: First in Man Frozen Elephant Trunk with a New Custom-Made Hybrid Stent Graft System
Prof. M. Grabenwöger (Vienna, Austria)
The Bologna Experience with Custom-Made FET Device
Prof. D. Pacini (Bologna, Italy)


Moderator
Dr. A. Van Linden (Würzburg, Germany)
New Customized FET Devices: The Pisa Experience
Prof. A. Colli (Pisa, Italy)
Overview of the ARTIZEN IDE Trial: Investigating the Arcevo™ LSA Device for the Treatment of Aortic Arch Dissections and Aneurysms
Dr. F. Fleischman (Los Angeles, United States)
Simplifying the Complex.
With 20 years of experience in leading innovation with the E-vita® Open platform in the Frozen Elephant Trunk Technique, we have now developed an outer branch stent to facilitate implantation into the supra-aortic vessels. This simplifies one of the most complex aspect of the FET procedure.
Custom-Made Device
The Neo EDE™ Hybrid Arch Device is

Acquired Cardiac Disease Domain
Highlights from the Acquired Cardiac Disease Domain
In this article, we present some of the key highlights from the Acquired Cardiac Disease Domain at this year’s meeting. We spoke with Professor Filip Casselman, Chair Acquired Domain EACTS and Professor Gloria Färber, Chair-Elect Acquired Domain EACTS, who discussed the evolving role of functional and imaging-based diagnostics in guiding coronary revascularisation, bicuspid valves and aortic valve regurgitation, the expansion of the Ross procedure and more...
Coronary Task force
One of the highlighted Coronary Focus Sessions will evaluate the evolving role of functional and imaging-based diagnostics in guiding coronary revascularisation. This includes the limitations of fractional flow reserve for CABG and the potential of next-generation CT angiography. What is the best practice in conduit selection? How do we optimize surgical technique and postoperative medical management to ensure the best long-term outcomes for CABG patients? These and more topics will be answered in various sessions.
“Coronary surgery remains a large part of our job. As we gather new data from trials, registries, research and basic science, we gain new insights into the optimal techniques and optimal choice of grafts for our patients, aiming to improve their prognosis,” explained Professor Färber. “In this session, the novel aspects of optimal graft choice and patient selection will be discussed.”
She added that the emergence of new developments in diagnostics, such as CT


collective decision-making within the heart team to tackle these specific clinical situations. Also, what are the red flags in TAVI imaging that preclude percutaneous valve treatment in such a case?
“Expanding the indications for TAVI to bicuspid valves is important because usually these patients have some dilation of the aortic wall. Current transcatheter techniques neglect the ascending aorta. We have to ask whether that is an acceptable option or whether these patients may return in the future for an ascending aortic problem?’” says Professor Casselman.
Other transcatheter topics covered are particular mitral valve transcatheter techniques and newer emerging technologies. What are the difficulties and the hurdles to overcome?
patient for this indication,” said Professor Färber. “Currently, Ross is mostly for patients with rheumatic disease, (young) patients with calcified aortic valve stenosis and on indication also in endocarditis. It is particularly a valid option in younger active patients and paediatric patients, as anticoagulation in this group can be complex, and growth potential is imperative. In experienced hands, the Ross procedure provides durable, long-term surgical results.”
Other ‘teasers’
The Translational Research and Surgical Science Task Force will have a dedicated focus session on alternative solutions for organ shortage as well as a session on machine algorithms potentially applicable in this specialty.
imaging, may negate the need to do a classical coronary angiogram prior to surgery. Current imaging modalities can potentially even provide greater detail regarding coronary anatomy, atherosclerosis burden and where the optimal bypass spots are. Additional information regarding minimally invasive access may also be derived from these newer diagnostic modalities.
“These new developments bring new options for the patient, and in my personal practice, patients really ask for the less invasive approaches and faster recovery. This session will highlight how to diagnose and plan such procedures.”
Bicuspid valves and aortic valve regurgitation – new challenges in TAVI This session will provide surgeons with the contemporary knowledge needed to inform






“We will also look into the future to predict potential engineering solutions being used in research or in an experimental setting that may see daylight for clinical use in a year or two, depending on study outcomes.”
The Ross procedure
Replacing someone’s aortic valve with his own pulmonary valve has several advantages, particularly as these patients do not need any anticoagulation. The results also show low rates of endocarditis, low permanent pacemaker need and above all, excellent hemodynamics.
“Previously, the Ross procedure was performed in highly selected patients. Recently, it has had a renaissance because of the cited advantages. Ideally, there must be a consensus on the surgical technique to provide a common standard allowing us to better identify the right
The Atrial Fibrillation Task Force has an interesting session in collaboration with the European Heart Rhythm Association. Hybrid therapy for Atrial Fibrillation will be studied in depth with particular focus on the management of failures.
“We would like to urge any attendee to attend as many sessions as possible. Some people complain there are too many interesting sessions at the same time, but actually, we feel that is a sign of a strong scientific programme,” concluded Professors Casselman and Farber. “And with that, we haven’t even touched on the numerous other sessions such as trial sessions, guideline updates, hands-on training sessions, poster sessions, etc, etc. The Annual Meeting of the EACTS provides you with a four-day immersion in scientific evidence in a global networking environment. Enjoy it!”

Filip Casselman Chair of the Acquired Cardiac Disease Domain
Gloria Färber Chair-Elect of the Acquired Cardiac Disease Domain
Highlights from the Thoracic Disease Domain
This year’s packed programme from the Thoracic Disease Domain will focus on the emergence of immuno-oncology, the latest advances in robotic thoracic surgery, the rise of artificial intelligence (AI), a dedicated session on mesothelioma, and much more. We were delighted to speak with Thoracic Disease Domain Chair, Professor Korkut Bostanci (Department of Thoracic Surgery, School of Medicine, Marmara University, Istanbul, Turkey) to discuss this year’s programme...
The Thoracic Disease Domain programme has been developed by the members of the Thoracic Disease Domain and the task forces. Before October 2024, the Thoracic Disease Domain had two task forces, but this was expanded to eight last year and now includes the Airway Surgery Task Force, Chest Wall and Thoracic Trauma Task Force, Digitalization and Artificial Intelligence Task Force, Emphysema Task Force, Mediastinal Surgery Task Force, Pulmonary Surgical Oncology Task Force, Solitary Pulmonary Nodule Task Force and the Thoracic Robotic Surgery Task Force.
“Previously, we only had the Solitary Pulmonary Nodule and Thoracic Robotic Surgery Task Forces but these two Task Forces were only a small part of much larger thoracic surgery specialty,” Professor Bostanci explained. “So our previous chair, Richard Milton and the domain members, wanted to have more thoracic Task Forces to cover more of the

Korkut Bostanci
Chair
of the Thoracic Disease Domain
specialty and to broaden the reach to thoracic surgeons in Europe, which was subsequently approved by the EACTS Council. As a result, the Thoracic Disease Domain will be hosting the Techno College, 10 focus sessions, the Young Investigator Award session, four rapid response abstract sessions, five moderated E poster sessions in Copenhagen and a Learning Lab.”
One of the highlights in Copenhagen will be today’s session on the ‘Role of surgery in the era of perioperative immuno-oncology’. It will be moderated by the Chair of the Pulmonary Surgical Oncology Task Force, Dr Monica Cassiraghi and past-President of EACTS, Professor Paul Van Schil. Esteemed speakers will include past-President of EACTS, Professor Franca Melfi, who will assess the ‘Surgical challenges post chemo-IO: Techniques and complications in the minimally invasive surgery era’, and the past-President of the European Society of Thoracic Surgeons, Professor Nuria Novoa, who will examine the ‘Perioperative treatments: Surgical management from stage IB to IIIA’.
“Immuno-oncology (IO) or immunotherapy has become a game changer in the treatment of lung cancer. There are many studies assessing IO and surgery, and in this session we're going to be talking about them. It can be given before surgery as neoadjuvant, or after surgery as adjuvant treatment. There are many modalities,
GORE® TAG® Thoracic Branch Endoprosthesis
there are many drugs. In the past years, oncology pharmaceutical companies were not very much interested in attending the surgery meetings, but in the last couple of years, as immunotherapies included in the early stages of the treatment together with surgery, they are very much interested in surgical meetings as ours as well. I think this session will raise many questions and will have some fascinating discussions.”
Robotic thoracic surgery
“Robotic thoracic surgery has been popular for many years and you can do almost all thoracic interventions with a robot now. Previously, we were working through four or five ports, but now we have single port robotic surgery as well, which is sort of new, especially in Europe. So in the Thoracic Techno College, we will be having live thymectomy surgery from Rigshospitalet Copenhagen with a single port robot, performed by Professor Rene Peterson. He will also talk about ‘Single-port robotic surgery: Integration and learning curve in a robotic thoracic surgery department’ in the focus session of Robotic Surgery: Tools and Capacity.”
Mesothelioma
“From now on we will be having a new task force, Pleural Diseases Task Force, which is going to cover mesothelioma. Mesothelioma is a very difficult disease. It has been operated on by thoracic surgeons with different techniques for many years. However, currently it’s almost a non-surgical disease, especially in some countries like the UK. Some patients are still operated by pleurectomy techniques rather than extrapleural pneumonectomy, which was previously the most common technique for mesothelioma treatment. However, some
people believe the MARS 1 and 2 trials had some shortcomings. So the questions are, ‘should there be a MARS 3 trial? or is there a better way to define the surgical indications?’ To answer some of these questions, Professor Giuseppe Cardillo will ask, ‘Is it time to revise the 2020 European mesothelioma guidelines? and Ms Sara Tenconi will present, ‘What will MARS3 trial look like? More space for surgery?’
Esophageal disease
“I think for the first time as far as I remember, there will be a special session on the ‘Management of esophageal surgical disease’, and this is going to be one of the highlights. Although not in every country in Europe, many thoracic surgeons are doing esophageal surgery, and this session is a must see for all thoracic surgeons who are interested in esophageal surgery. We are honoured to have two world class speakers in this session, Dr Siva Raja from the Cleveland Clinic, who will assess ‘Endoscopic versus surgical treatment for esophageal cancer’, and Dr Patrick Seastedt from the Roswell Park Comprehensive Cancer Center, who will look at ‘The future application of AI in esophageal surgery.’”
Joint EACTS/ESTS session
Finally, there will also be a joint EACTS/ESTS session on the ‘Surgical treatment of hyperhidrosis’, as the organisations are currently working together on a project to examine this issue. Dr Francesco Petrella will present, ‘EACTS/ESTS Expert consensus statements on surgical treatment of hyperhidsrosis: The project’ and Dr Federico Raveglia will announce ‘EACTS/ESTS Expert consensus statements on surgical treatment of hyperhidsrosis: The preliminary results’.


Highlights from the Congenital Disease Domain
This year’s Congenital Disease Domain programme will debate international collaboration, showcase state-of-the-art imaging and diagnostic innovations that are transforming congenital heart disease care and explore the latest innovations and evidence surrounding right ventricle to pulmonary artery (RV PA) conduits. We spoke with Professor Vladimiro Vida (Consultant in Pediatric and Congenital Cardiac Surgery and Director of the Cardiac Surgery Training Program, University of Padua, Padua, Italy), Chair of the Congenital Disease Domain, who outlines some of the key sessions...
Professor Vida began by acknowledging that this year’s Congenital Disease Domain programme was developed through close collaboration with Professor Jurgen Hörer, the previous chair of the Congenital Disease Domain. He explained that Professor Hörer played a crucial role not only in guiding the programme’s design but also in motivating and supporting Professor Vida as he took on his new responsibilities as Chair of the Congenital Disease Domain.
The Congenital programme is structured around eight focused sessions, each carefully

Vladimiro Vida Chair of the Congenital Disease Domain
crafted to address key and current topics in congenital heart surgery. These sessions bring together world-renowned experts who will share their knowledge, experiences, and the latest advancements in this constantly evolving field. The primary goal is to provide participants with rich, relevant content that encourages engagement and the exchange of best practices for the benefit of patients.
Professor Vida explained that one of the key highlights will be the American Association for Thoracic Surgery and EACTS ‘Joint Session on the management of congenital aortic stenosis in children: “This joint session is designed to foster international collaboration, highlight divergences in practice patterns, and update practitioners on evolving guidelines and procedural innovations. This will be achieved by sharing state-of-the-art diagnostics, surgical techniques and long-term outcomes. In addition, we will compare intervention strategies, such as balloon valvuloplasty versus surgical valvuloplasty, and discuss the latest evidence, controversies and decision-making frameworks.”
There will also be a session that will showcase state-of-the-art imaging and diagnostic innovations that are transforming
Women in Cardiothoracic Surgerychampioning the role of women
The Women in Cardiothoracic Surgery (WiCTS) Committee was established in 2020 to guide the Association on how to champion the role of women in cardiothoracic surgery and create an equitable, diverse and inclusive culture throughout the organisation. We spoke with Professor Indu Deglurkar (University Hospital of Wales, Cardiff, Wales), Chair of WiCTS Committee, about the Committee’s mission, achievements and activities in Copenhagen...
“The WiCTS Committee is made up of EACTS members across Europe who believe in gender equality and opportunities for women in cardiothoracic surgery. My role as Chair and fellow Member of the WiCTS Committee is to ensure fairer opportunities for women in training, research and seeks to increase their visibility and representation within the Association. Since its creation, the committee has provided career development support, networking and structural initiatives such as fellowships and leadership training.”
She explained that since its inception, WiCTS has made considerable inroads in improving networking for women in cardiothoracic surgery and support through career development, subspecialty training, research and academia. These include a Francis Fontan Travelling Leadership Fellowship for Women in Cardiothoracic Surgery (in partnership with AtriCure). This fellowship was specifically designed to foster the development of senior leadership qualities among women in specialty – a sphere where structured guidance and mentorship in leadership have too often been
overlooked. This pioneering programme spans one year and comprises three one-week placements with chosen eminent female leaders in cardiothoracic surgery in five centres across Europe. The objective is not merely to observe, but to immerse oneself in diverse leadership environments and reflect upon the multifaceted nature of leadership within modern healthcare.
congenital heart disease care, titled ‘Precision in Practice: Emerging Imaging and Diagnostic Tools in Congenital Heart Disease’. The focus is on how emerging technologies - such as advanced fetal imaging, machine learningenabled diagnosis, real-time MRI, 3D/4D echo and fusion-guidance techniques - are enhancing precision diagnostics, surgical planning, procedural guidance, and long-term monitoring.
In addition, Professor Vida explained that the session, ‘The Right Link: Advances in The RV to PA Conduits and Reconstruction’, will explore the latest innovations and evidence surrounding RVPA conduits and surgical reconstructions in complex congenital heart disease. It will focus on refining conduit design, surgical technique and timing to improve hemodynamics, durability, and long-term outcomes, while minimising reintervention and morbidity.
“Presentations and discussions in this session will highlight that conduit longevity remains limited by degeneration and somatic mismatch, therefore optimising design and material is critical. Furthermore, we will examine issues around smart sizing and placement as these directly influence reintervention timing and ease of future surgeries, as well as focusing on emerging bioengineering and modelling tools that promise personalised solutions, thereby reducing the long-term surgical burden.”
The ‘Adult Congenital Heart Surgery Navigating Complexity, Advancing Care’ session will address the evolving complexities of surgical care in adult congenital heart disease (ACHD). It will focus on managing increasingly complex adult patients with congenital lesions, integrating advanced surgical techniques, heart
failure therapies, and transplant strategies, as well as optimising care models, team structure and outcomes in growing adult CHD programs.
“This session is designed to inform both established and emerging ACHD surgical teams on current best practices and future directions. The adult CHD population is growing and presenting with more complex anatomy and comorbidities. Therefore, integrating heart failure expertise, advanced imaging, transplant pathways and interventional options is critical to deliver optimal outcomes. Discussions will include how building and accrediting fully functional ACHD surgical programs involves robust teamwork, institutional support and specialist knowledge, and that long-term management strategies -especially for Fontan, Eisenmenger or multi-repaired patients - require individualized, multidisciplinary approaches.
In addition to the eight focused sessions, the programme will also include three abstract sessions, two rapid-fire sessions, and five moderated poster sessions. These poster sessions will feature distinguished surgeons presenting their research to the audience, fostering lively discussion and engagement.
“We will also host one learning lab, which will consist of a surgical simulation demonstrating the correction of a sinus venosus defect with partial anomalous pulmonary venous drainage via a minimally invasive axillary approach,” Professor Vida added. “This session will be coordinated by Professor Ali Dodge Kathami. We are very excited to engage both junior surgeons for this valuable learning experience and senior surgeons who wish to refine their surgical techniques.”

In addition, WiCTS has created an in-person ‘Masterclass in Leadership’ course at Windsor and a webinar series on Leadership, Gender Equity and Bias. The committee also proposes that female surgeons be more frequently present as speakers, panellists or chairs at the EACTS Annual Meetings, increasing their visibility. The Committee also hosts improved networking opportunities, and at the 38th EACTS Annual Meeting in Lisbon, Portugal, WiCTS conducted the first breakfast networking session, which was attended by 24 members from 18 countries.
WiCTS at Copenhagen
This morning, WiCTS will host a Focus session, ‘Gender Medicine: Unravelling the blind spots’ (10:0011:00, Room 18 &19), which will seek to raise awareness that biological sex and gender identity significantly impact health, disease and treatment outcomes, requiring personalised approaches.
“Historically, gender-specific factors have been neglected in research, clinical trials guidelines and practice. The assumption made in many surgical and cardiovascular studies is that male gender is ‘default’, but it has been more and more suggested that female patients have
into account. The idea behind this session is to identify some gaps in evidence and research where gender differences are under-explored, therefore promoting the integration of gender-based analysis in our surgical field. This session is an invitation to encourage the audience to question their assumptions, biases and widen their research perspectives to be more inclusive and curious about the specificities of female patients. We would like to promote inclusive research, leading to more accurate diagnoses and effective, tailored treatments for diverse patient populations. The health of women has a colossal influence on the health of subsequent generations. Hence, improving women’s health makes sense from both an economic and a social justice perspective.”
There will also be a presentation about the Committee’s collaboration with Women in Thoracic Surgery (WTS-USA). The WTS was founded in 1986 and has been championing to enhance the education of patients and opportunities for female thoracic surgeons, by enabling their members to network with each other, share ideas, professional advice and discuss challenges that they face with the purpose of finding solutions.
“I think there will be a great deal to learn from their advancement and
transfer that knowledge to develop WiCTS in EACTS. I will gain further insights from their 2nd Annual Conference next month. They certainly have a longer history and experience in the topic of gender disparities. Working together would allow collaborative sessions, networking. A collaboration between WiCTS and WTS USA is intended to maximise the impact of these groups, accelerate the process to reach gender equity via shared intellectual and human capital.”
In the WiCTS Focus Session, Dr Mario Gaudino will present, ‘Why are women under-represented in CABG Clinical Trials & what can be done about it’. Professor Deglurkar explained that this is an important discussion because for a very long time, the default patient has been ‘male’. In the 1970’s significant attention was drawn to the systematic exclusion of women from clinical trials, and this exclusion was rooted in concerns that hormonal fluctuations could complicate study outcomes, assumptions that male results were universally applicable, and fears related to undetected pregnancies.
“In addition, issues around childcare, lack of transportation, lack of adequate female investigators, communication and an increased incidence of adverse reactions were,
and continue to be, significant barriers. We believe universities, medical societies, hospitals, industry, regional ethics committees, regulatory bodies, etc, have all got an important role in addressing these barriers. Gender Medicine needs to be depoliticised and clinical guidelines must incorporate sex and gender considerations.”
Finally, Professor Deglurkar and fellow WiCTS Committee member, Dr Maroua Eid (Angers, France), will also appear on EACTS TV this afternoon (15:00–15:15), in the session, ‘Women in Cardio-thoracic Surgery’, that will explore the issues around Gender Medicine and discuss some of the improvements and how as a professional body, EACTS can address some of these challenges.
“Overall, we want to inspire more women to fulfil their surgical career ambitions. We want to promote diversity and equality within our association and spread awareness of the importance of gender equality by ensuring greater representation of women in scientific sessions at the Annual Meeting and on different organisational levels within EACTS. This can be achieved through providing mentorship for women in cardiothoracic surgery and support through career development, subspecialty training, research and academia,” she concluded. “I would actively encourage all women who participate in cardiothoracic surgery to contact WiCTS to see how we can help enhance their educational and career development opportunities through the EACTS Annual Meeting, EACTS Academy, research opportunities, and fellowships. We will be recruiting committee members and observers in the next few months.”
For more information, please email: womenscommittee@eacts. co.uk
Highlights from the Aortic Disease Domain
Highlights of the programme from the Aortic Disease Domain will include a join EACTS/STS session on thoracoabdominal aortic surgery that will explore contemporary strategies to treat this difficult patient population, another joint EACTS/ASCVTS session on Type A intramural hematomas (IMH) examining which patients benefit from immediate surgery and which patients benefit from watchful-waiting and an intriguing session on graft infections and the difficulties of how to best intervene with these patients. We caught up with Chair of the Aortic Disease Domain, Dr Florian Schoenhoff (University Hospital Bern, Switzerland), who outlined some of the topics under discussion...
“Over the past decade, thoraco-abdominal aortic surgery has evolved from being strictly open surgery or strictly endovascular surgery towards a more hybrid situation. In many cases nowadays, we start by replacing the aortic arch using a frozen elephant trunk and that leaves us with a very good proximal landing zone to continue with endovascular repair. And then depending on the morphology, depending on the age of the patient or the underlying pathology, then we either continue in an open or endovascular fashion,” Dr Schoenhoff explained. “By using this hybrid approach, we have seen that we are able to minimise the negative impact of open surgery while still maintaining longevity of the repair and good late outcomes.”
The optimal treatment of patients depends on many factors, including technical feasibility, anatomy, the age of the patient, etc. He said that some patients present with a severe kinking of the aorta or present with a chronic dissection with very small true lumen, so it is not feasible to perform an endovascular
procedure. However, he added that over time, feasibility is becoming less of a problem as newer devices are being developed that are helping surgeons mitigate such issues.
“The age of the patients is a factor because of the potential risk of developing an endoleak; the younger the patient, the more time there is for the endovascular repair to fail. So, my preference for younger patients is to perform an open repair. Then of course we have a large patient population that has connective tissue disorders - we know that the radial force that is exerted by these stentgrafts can be a problem for the aorta, which can continue to dilate around the stent grafts. Again, this may be overcome partially by newer devices. But you still need a very good proximal and distal landing zone. The best way is to create these with surgically placed Dacron grafts.”
He believes that the best outcomes come from experienced centres that have discussions within an aortic team consisting of specialists who perform both endovascular and open surgery.
“I think one of the major discussions that we will have in this session will be that we are moving away from total endovascular or open repair and towards a more hybrid solutionwhere patients over the course of their lifetime - will receive both procedures.”
Type A intramural hematomas
Until quite recently, the guidelines stated that intramural hematomas should be treated as a dissection in the same segment. However, data from a larger series of Asian patients, published over the past decade, revealed that some of these patients might be better off with ‘watchful waiting’ rather than having open surgery. The reason is that there are more patients suffering from intramural hematoma than aortic dissection in Asia than in Europe.
“So, our Asian colleagues do have more experience in treating this patient population. I believe that those patients who have persistent pain, those where you can see an entry in the aorta or patients who have pericardial effusion should undergo surgery.

in surgical patient

management at high risk for postoperative low-cardiacoutput syndrome
Postoperative low-cardiac-output-syndrome (LCOS) is an infrequent event after surgery, which may occur as an expected or unexpected complication after surgical interventions. The expected scenario is usually associated with a high-risk preoperative patient profile, usually related to already existing

descending aorta and the aortic arch, providing a landing zone for further endovascular repair with stent grafts – patients can end up with a very large segment of the aorta replaced ‘in continuity’.
One topic under discussion will be why this condition is more prevalent in the Asian population - is there inherently something different in the aorta, or is the behaviour of the aorta different in Asian patients compared to Caucasian patients? Several studies have shown that compared to Caucasian populations, the percentage of women in Asian series on aortic dissection is much higher. Asian patients present less often with ischemic heart disease, but hypertension is generally more frequent. I think this will be the main discussion going on in this session.”
Aortic graft infections
“We know that the rate of graft infections is higher the more distal the implant, so, for example, the risk of ascending aortic graft infection is much lower than in the groin. Data from the US has shown that vascular graft infections are now the most common prosthetic device infection - more than orthopaedic surgery or other surgical specialties where you put in some form of device - and this is very, very concerning.
Dr Schoenhoff believes that one of the reasons is because of the more liberal use of replacing longer segments of the aorta. This is becoming a problem today because previously, when devices were implanted, they could also be removed. Nowadays, he said, because of multiple treatments – replacing the
“For many of these patients, there is no surgical procedure that allows us to get out all of the infected material at once. And this is a really becoming more of a problem because we are more aggressive in our primary procedures. If you ask our colleagues in microbiology and infectious diseases, they would say that all graft infections require surgical intervention, and the patient cannot be considered cured until all the infected material is removed. But in more recent years, there is emerging data suggesting that in some patients, conservative treatment may be possible depending on the strain of bacteria and the duration of the infection.”
For example, a patient who does not present with any abscess formation, air or fluid collection around the graft may be conservatively treated, but if you have patients who have persistent positive blood culture and who remain symptomatic with high temperatures, chills and weight loss, these patients cannot be treated conservatively and must have surgery to remove all the infected material.
“I think the discussions will be about the option of conservative therapy, something that was not considered previously, and particularly whether there might be a case for a more liberal approach to antibiotic prophylaxis in these patients.”
“Overall, our approach when putting together the programme is to make it as interactive as possible. People are really encouraged to ask questions to the surgeons directly. One of the reasons we restrict the presentation time to eight minutes is so we can spend more time asking questions, facilitating more discussions and more debates. I think the most important thing about meetings such as EACTS is to challenge experts one-on-one, to gain insights from their experience because these things are not discussed in the literature - this is why so many people are coming to EACTS in Copenhagen this year.”
Acquired Cardiac Disease Domain


















cardiac functional compromise, with or without the contribution of the specific type and related complication of the performed surgical treatment. The occurrence of LCOS is a well-known factor directly responsible for a complicated postoperative course, leading to end-organ dysfunction and the need for maximal vaso/inotropic-active drug therapy, all predisposing factors to increased in-hospital as well as post-discharge mortality.
Prophylactic use of inotropic drugs has shown neutral results in cardiac surgery patients undergoing surgery with depressed cardiac function1,2, indicating that a different approach is warranted to impact the perioperative patient outcome in these scenarios positively. Recently, in the






interventional cardiology setting, the management of patients with similar characteristics, that is with a high chance of developing acute cardiac dysfunction or further deterioration of pre-procedural cardiac compromise during the planned procedure, has led to the application of pre-emptive application of temporary mechanical circulatory support3,4 This strategy has certainly and unquestionably allowed to accomplish complex and high-risk procedures with a “protected strategy” and positive results. In the cardiac surgery setting, the application of similar conduct has also shown a promising impact, either in patients with poor preoperative hemo-metabolic conditions or with expected complicated intraoperative cardiac recovery5,6



Several reports and evidence over the usefullness and efficacy of such a prophylactic strategy, therefore, have prompted EACTS to plan and realize a document clearly elucidating all the aspects and provide recommendations related to the application of this new concept named “Protected Cardiac Surgery”. This approach accounts for the pre-emptive application of temporary mechanical circulatory support in surgical candidates at risk of postoperative LCOS. The aim is, therefore, to prevent or significantly reduce the risks and related impact of hemodynamic instability or even cardiogenic shock and related LCOS in the postoperative period. A multidisciplinary group of worldwide experts has been asked to gather
Florian Schoenhoff Chair of the Aortic Disease Domain
Types of Protected Cardiac Surgery
Figure 2
Figure 1
Roberto Lorusso Chairman of the EACTS Expert Consensus Statement Task Force
Acquired Cardiac Disease Domain
and realize such an Expert Consensus Statement, which has explored and described all the major issues and aspects of this peculiar strategy in cardiac surgery. A structured as well as multi-disciplinary discussion and decisionmaking in the surgical planning has been presented, including patient and family-related information, over the risks and benefits, as well as the local resources and access to such a potential approach towards high-risk surgical patients. Additional information has been applied regarding the indication of the type of
Residents
Residents
at EACTS
We caught up with EACTS Residents’ Committee Chair, Dr Nabil Hussein (Birmingham Children's Hospital and Great Ormond Street Hospital, London, UK), about the important work of the committee, this year’s Residents Programme in Copenhagen and why trainee surgeons should join EACTS…
“One of the goals of EACTS is to strive so that our patients receive the best possible care. The delivery of cardiothoracic surgery is consistent across Europe; however, resident training can vary considerably,” he explained. “So, one of the roles within the Residents’ Committee is to understand European training programmes, how they differ and explore if there are ways to develop a more united approach. In the last two years, we have hosted the ‘National Trainee Summit’, where we bring national resident representatives from different countries together to discuss training and highlight areas where it can be improved. One of the key issues identified was the lack of standardisation across programmes, which has hindered the progression and mobility of residents during and after training.”
mechanical supports, also according to the kind of surgical procedure with a high likelihood of LCOS, thereby advising the appropriate planning and timely prophylactic use of such devices. To enhance the patient identification and selection for the protected cardiac surgery strategy, a dedicated and detailed classification (Figure 1) has been realized, addressing the various conditions and types of protected cardiac surgery scenarios. Furthermore, the various steps and aspects as well as circumstances of the protected cardiac surgery decision-making and application are also
described (Figure 2), whose additional features will be provided in the today presentation and released publication on the EJCTS.
References
1. Mehta RH, Leimberger JD, van Diepen S, et al. Levosimendan in Patients with Left Ventricular Dysfunction Undergoing Cardiac Surgery. New England Journal of Medicine 2017;376:2032–42.
2. Landoni G, Lomivorotov V V., Alvaro G, et al. Levosimendan for Hemodynamic Support after Cardiac Surgery. New England Journal of Medicine 2017;376:2021–31.
3. Dangas GD, Kini AS, Sharma SK, et al. Impact of hemodynamic support with Impella 2.5 versus intra-aortic balloon pump on prognostically important clinical
outcomes in patients undergoing high-risk percutaneous coronary intervention (from the PROTECT II randomized trial). Am J Cardiol 2014;113:222–8.
4. Romagnoli E, Burzotta F, Cerracchio E, et al. Impact of Impella protected-percutaneous coronary intervention on left ventricle function recovery of patients with extensive coronary disease and poor left ventricular function. Int J Cardiol 2023;387.
5. Watkins AC, Maassel NL, Ghoreishi M, et al. Preoperative Venoarterial Extracorporeal Membrane Oxygenation Slashes Risk Score in Advanced Structural Heart Disease. Annals of Thoracic Surgery 2018;106:1709–15.
6. Dobrilovic N, Lateef O, Michalak L, Delibasic M, Raman J. Extracorporeal membrane oxygenation bridges inoperable patients to definitive cardiac operation. ASAIO Journal 2019;65:43–8.
As a result, EACTS recently published The European Association for Cardio-Thoracic Surgery-Core Curriculum for the Cardiac/ Cardiovascular Surgeon1. According to Dr Hussein, this provides guidance to residents and trainers by defining the clinical and non-clinical competencies across three training stages-introductory, intermediate and advanced.
“The EACTS Core Curriculum offers a harmonised, flexible and competency-based framework for cardiac surgical training. Currently, if you train in one European country, it doesn't necessarily mean that your qualifications are recognised in another European country, which isn't great. This stifles movement and makes it difficult for resident doctors to train and gain valuable experience in

other countries. The idea of the curriculum is to raise the bar, be transparent and to set an aspirational set of guidelines that training programmes can adopt should they find it beneficial. We’ll be discussing the curriculum during the EBCTS session at the annual meeting, so please join us!”
The Residents’ Committee also helps to organise and promote training through face-toface courses, webinars and additional educational material that may be of benefit to resident doctors across Europe.
“The EACTS Academy is one of the jewels of the Association. We have a fantastic package of courses that are aligned to what residents need to know. A perfect example of this is the Foundation Courses in Adult Cardiac, Congenital and Thoracic Surgery. We understand that it can be challenging for residents to attend all our courses, so we are exploring ways to make this great education content more accessible.”
Residents in Copenhagen Dr Hussein then outlined some of the key highlights of the scientific and social programmes that residents can look forward to in Copenhagen. The scientific programme includes the third edition of the popular ‘Escape the Coffin 3.0 - Small Holes, Big Problems’, which this year will concentrate on minimally invasive cardiac, thoracic and congenital surgery.
The Residents’ Corner Award also returns, which promotes the great scientific work that has been done by residents published in the EJCTS and ICVTS. The winner will be presenting their work during our EACTS/AATS Foundation award session.
Regarding the social programme, there will be the annual Residents’ Luncheon. Each table will have two experts in specific fields, which provides a great opportunity for residents to seek guidance and develop mentorships. Dr Hussein encouraged attendees to register early for the luncheon as it is always well attended and over-subscribed. This year will also see a new ‘Open Mic’ session where a panel of experts will start prompting the audience to talk about topics around training, fellowships and mentorships. This will take place at the EACTS stand in the Exhibition Hall.
Residents Dinner
“On Friday evening, we will have a social get-together at the Residents’ Dinner. It's kindly funded by industry with approximately 50 places available. We encourage residents to sign up for the dinner as soon as possible, as last year it was completely sold out by the first morning of the meeting. It’ll be a great night with fellow residents.”
Why become a member of EACTS?
As part of our global community, you’ll gain access to world-class resources, expert-led training and a network of professionals driving innovation in cardiothoracic surgery.
Apply now to become a member of EACTS and enjoy access to all the below membership benefits.
Connect Network with peers at the EACTS Annual Meeting – the leading global event in cardiothoracic surgery
Access exclusive member-only rates for events
NEW: EACTS mentorship programme
Learn Free access to the European Journal of Cardio-Thoracic Surgery (EJCTS)
Reduced rates to contribute to the Interdisciplinary Cardiovascular and Thoracic Surgery journal (ICVTS)
Free access to EACTS educational webinars
Preferential rates for EACTS Academy training
Apply for exclusive fellowships and bursaries
Advance
Join task forces and committees shaping surgical standards and practice
Be part of initiatives supporting women, early-career clinicians and Allied Health Professionals
Free access to the Adult Cardiac Database
Apply for Outreach Grants
Apply for Innovation Grants
Vote at the General Assembly and help shape EACTS’ future.
Full active members pay just €300 a year.
Visit the Membership Team on the EACTS Booth in the Exhibition Hall to find out more or apply online here >>
“It’s based on the principle of an escape room. During the session, the audience must work together to determine the outcome of the patients that will be presented. The aim is to try and avoid an adverse outcome and get them safely through. This is a fun session that always receives great feedback. We will also have a ‘Nightmare patients unlocked’ session in which resident surgeons will present surgical cases where things go wrong, and the experts involved will give their reflections and talk about what could have been done differently, focusing on decision-making. People love seeing nightmares and how they were navigated through,, which serves as an excellent education tool to attendees.”
Additionally, there will be an artificial intelligence (AI) session that will examine the role of AI and large language models, transformational technologies that are coming into cardiothoracic surgery. There will also be a joint session with the European Association of Percutaneous Cardiovascular Interventions (EAPCI), called the Heart Team Competition. This session is designed to understand Heart Team decision-making pathways in the scenario of coronary artery disease, valvular disease and heart failure.
“Teams of resident surgeons and cardiologists will have to work through challenging cases together. The focus will be on multidisciplinary team working between surgeons and cardiologists in the form of a competition. This is the first time that we're running this, and I’m really looking forward to it.”
As ever, there will be the Young Investigator Awards for cardiac, thoracic and congenital residents - a yearly award that's given to the best presentation/paper by trainee surgeons.
Last, but by no means least, is the ‘CT Residents Showdown: European Final’. There will be three teams going head-to-head to determine this year’s European champions. It's based on the Jeopardy game format, where the team with the most money accrued will be the winner!
“Mr Richard Milton, the former Thoracic Disease Domain Chair, will be back again to host the not-to-miss event! I wonder if he’ll be dressed up again after last year’s appearance as a gladiator.”
“EACTS has so much to offer residents – the annual meeting brings everyone together, where you feel the cardiothoracic surgery community at its best. When you're a cardiothoracic surgery resident, you can become siloed in your department, but when you step out of the hospital and meet other resident colleagues, you quickly realise that we share common problems, we develop new friendships, and together we contribute to an amazing meeting,” he stated. “Being an EACTS Residents member is highly valuable - you get access to the European Journals, you get to attend all the EACTS webinars for free, you get discounts on in-person courses, and so much more. Being a Resident member, you can become part of the Residents’ Committee. This year, I will be stepping down from the committee - I have had the privilege to work with an incredible group of young, highly motivated residents who are committed to improving the experience of all resident surgeons. It has been an honour to work for my fellow residents, and I wish the committee all the best as they continue to grow from strength to strength.”
References 1. Hussein N, Eid M, Olsthoorn J, Nägele F, Loubani M, Quintana E, Borger M, van Brakel T, Sádaba JR, Clark S, Myers P. The European Association for Cardio-Thoracic Surgery-Core Curriculum for the Cardiac/Cardiovascular Surgeon. Eur J Cardiothorac Surg. 2025 Aug 2;67(8):ezaf230. doi: 10.1093/ejcts/ezaf230. PMID: 40632600
Nabil Hussein Chair of the Residents’ Committee

President's Choice:
08:30–09:30 Congress Hall A1 Plenary
Computational fluid dynamics analysis of artificial aortic valves: Impact of tilted implantation on hemodynamics


Aortic valve replacement (AVR) remains a cornerstone treatment for severe aortic valve pathologies, but the choice of prosthetic valve size and implantation strategy poses a persistent challenge. Prosthesispatient mismatch (PPM), where the implanted valve is too small relative to the patient’s body size, can lead to elevated pressure gradients, reduced survival rates, and recurrence of symptoms. To address this, annular enlargement techniques have been developed to allow implantation of larger valves such as the Manouguian, Nicks, Nunez or Yang technique. All of them are based on the opening and enlargement of the non-coronary part of the annulus, while the annular part corresponding to the left and right coronary sinuses is left intact. The enlarged part of the annulus is reconstructed by either bovine pericardium or a dacron graft. By attaching the aortic prosthesis at a higher level within the enlarged area, the implantation of a larger prosthetic valve becomes feasible. By opting for larger valves, surgeons may be forced by the new anatomy of the aortic annulus to implant the prosthesis in a tilted position. The septal side corresponding to the left and right coronary sinus remains unchanged, while the non-coronary side of the prosthesis is implanted at a high level. This leads practically to a tilted implantation of the valve. Severe tilting of the prosthesis may disrupt natural blood flow patterns, introducing turbulence, asymmetry, and abnormal shear stresses that may compromise valve durability and patient outcomes.
These trade-offs are investigated using computational fluid dynamics (CFD) to evaluate the haemodynamic performance of different valve sizes and implantation angles. The study focused on the Medtronic Avalus bioprosthetic valve, a widely used biological valve known for excellent haemodynamics after surgical aortic valve replacement. By simulating blood flow through three valve sizes – 23 mm, 25 mm, and 27 mm – under varying implantation scenarios, the research aimed to provide actionable insights for optimizing valve selection and implantation strategies.
The Role of CFD in Heart Valve Research CFD has emerged as a powerful tool in cardiovascular research, enabling detailed simulations of blood flow, pressure distribution, and mechanical stresses under physiological conditions. Unlike physical experiments, CFD allows for precise control over variables such as valve geometry, boundary conditions, and

flow dynamics, reducing the need for costly and time-intensive in vitro studies. In this study, CFD simulations were conducted using Ansys Fluent, a state-of-the-art software platform, to model the interaction between blood flow and valve structures. The simulations incorporated realistic boundary conditions and turbulence modeling to replicate physiological haemodynamics as closely as possible.
Key Findings
The study evaluated the haemodynamic performance of the three valve sizes implanted in a virtual annulus fitting a 23 mm bioprostheses. The evaluation included wall shear stress (WSS) and general shear stress thresholds associated with thrombosis and platelet activation. Two leaflet-opening configurations were analyzed to account for different flow scenarios.
23 mm Valve (Baseline): The 23 mm valve (correct size valve), implanted perpendicularly to the aortic axis, served as the baseline configuration. While it exhibited stable flow patterns, the valve showed elevated WSS and shear stress near the leaflet entry region, indicating potential risks for thrombosis and platelet activation.
25 mm Valve (Moderate Upsizing): The 25 mm valve required a tilt angle of 11.84° for implantation based on the virtual model. Despite this adjustment, the valve demonstrated improved haemodynamic performance compared to the 23 mm valve. Critical stress areas and peak velocities were reduced, and flow stability was maintained. The moderate upsizing effectively balanced the need for a larger valve with minimal disruption to natural flow patterns.
27 mm Valve (Aggressive Upsizing): To accommodate a 27 mm valve, tilted implantation at 25.58° was required. Increased tilt led to unfavorable haemodynamics, higher WSS and shear stress, particularly at the leaflet tips where contact with the aortic wall occurred. The larger tilt also restricted the effective flow area, resulting in elevated peak velocities, expanded recirculation zones, and increased turbulence. These findings suggest that aggressive upsizing may introduce more risks than benefits.
Clinical Implications:
The results highlight the importance of a balanced approach to valve sizing and implantation. Moderate upsizing to a 25 mm valve, combined with controlled tilting, offers a promising strategy for improving
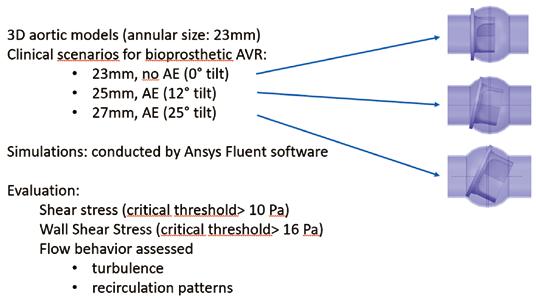
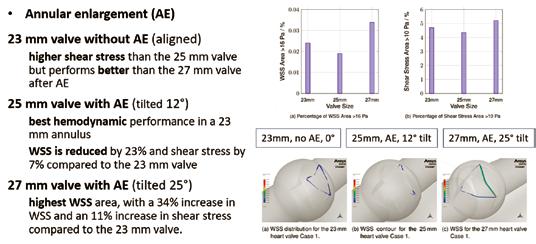
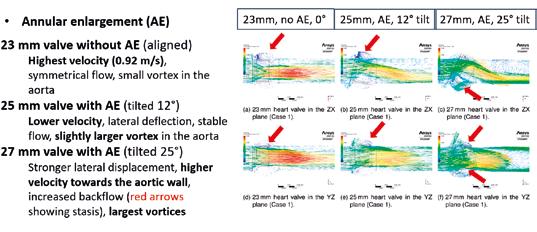
haemodynamic performance without introducing significant flow disturbances. In contrast, further upsizing to a 27 mm valve may compromise flow stability and increase the risk of adverse outcomes.
These findings have direct implications for clinical decision-making. By leveraging CFD simulations, surgeons can better predict the haemodynamic impact of different valve sizes and implantation angles, enabling more personalized and effective treatment plans. The study also underscores the need for careful consideration of tilt angles and their impact on flow dynamics, particularly when larger valves are required.
Limitations and Future Directions
While the study provides valuable insights, it is not without limitations. The simulations used an idealized aortic geometry rather than patientspecific models, which may limit the applicability of the findings to individual cases. Additionally, a Newtonian fluid model was employed, which does not fully capture the shear-thinning behavior of blood. Future research should
Friday 10 October 17:45-18:30 / Auditorium 10, Level 1, Bella Center
incorporate patient-specific geometries and more advanced fluid models to enhance the clinical relevance of CFD simulations.
Another area for future exploration is the long-term impact of tilted implantation on valve durability and patient outcomes. While this study focused on short-term haemodynamic performance, understanding the long-term effects of implantation strategies is crucial for optimizing valve design and improving patient care.
Conclusion
This research demonstrates the potential of CFD as a decision-support tool in AVR, offering a deeper understanding of the complex interplay between valve size, implantation angle, and haemodynamic performance. According to our data, implantation of significantly larger valves may lead to stronger lateral displacement, increased shear stress on the leaflets, larger vortices and stasis. Future studies are needed to explore the incidence of structural valve degeneration in a clinical setting.

MCI Innsbruck, Austria
Manuel Berger Nikolaos Bonaros
Jonna Golks
President's Choice:
08:30 - 09:30 Congress Hall A1 Plenary
10 Years of Ross-PEARS: Preliminary experience in 100 cases
The Personalized External Aortic Root Support (PEARS) technique has gained considerable acceptance within the cardiovascular surgical community over the past decade. Initially developed for patients with aortic root dilation, particularly in the context of Marfan’s syndrome, its applications have since broadened significantly. Accumulating clinical evidence now supports its utility across a wide array of aortic pathologies.
Motivated by promising early outcomes and the technical feasibility of the method, our team initiated the application of the PEARS technique to support the Ross autograft ten years ago, as the currently available surgical support grafts were cumbersome and non-anatomical supports. Today, it is well established that proper stabilization of the Ross autograft enhances the long-term durability and outcomes of the operation. However, any ideal support technique must satisfy several essential criteria:
n It must provide a firm yet flexible structure, preserving the physiological dynamics of the
aortic root;
n It should minimize additional operative time;
n It must be customizable to the patient’s individual anatomy and vascular dimensions.
Given these requirements, we identified PEARS as a promising adjunct to the Ross procedure. This could potentially make traditionally unfavourable aortic valve and root pathologies amenable to a free-root Ross if supported with a PEARS graft, which would significantly influence long-term results.
Since the first Ross-PEARS procedure in 2015, more than 200 patients worldwide have undergone this combined intervention, with over 100 cases performed at our St Thomas’ and London Bridge Hospitals in London. Although initial adoption was slow, the number of cases has grown exponentially in recent years, coinciding with an expansion in indications and increased patient referrals.
Our patient cohort has been notably diverse, encompassing a range of clinical profiles. A substantial proportion presented with
disease emergence after TEVAR: Assessing long-term risks in aortic repair patients
As the use of thoracic endovascular aortic repair (TEVAR) has risen globally, long-term outcomes and potential complications have become increasingly important for clinicians and patients alike. One underexplored consequence is the risk of developing new malignancies after TEVAR, a concern underscored by the cumulative radiation exposure from frequent postoperative computed tomography angiography (CTA) surveillance. While routine imaging is critical for detecting complications such as endoleaks1, emerging evidence suggests that intensive surveillance regimens may inadvertently elevate the risk of cancer, raising a complex challenge in balancing surveillance benefits against iatrogenic harms2
To address this critical gap, we conducted a retrospective analysis of 542 TEVAR patients, with follow-up extending up to ten years. The primary outcome was the incidence of new malignant disease, defined by imaging and/or biopsy confirmation, after TEVAR. Our approach extended beyond simple event counts, capturing the interval between TEVAR and cancer diagnosis, and scrutinizing both traditional and procedural risk factors.
Restricted cubic spline regression and multivariable competing risk models were employed to explore the relationship between CTA surveillance frequency and cancer risk. Special attention was given to cumulative imaging exposure, perioperative variables (such as X-ray and procedure time), and

predominant aortic regurgitation— traditionally a relative contraindication to the Ross procedure. Moreover, nearly 25% had undergone prior aortic valve surgery, including mechanical aortic valve replacement, bioprosthetic valve replacement, bio-Bentall procedures, or valvesparing root replacements. These findings underscore the potential of the Ross-PEARS technique for patients seeking to avoid lifelong anticoagulation, or for those already on anticoagulation who wish to discontinue it.
From a technical standpoint, the PEARS graft is integrated into the

Joseph Kletzer
Universitätsklinikum Freiburg and Universitäts-Herzzentrum, Germany.
detailed patient characteristics to distinguish genuine associations from confounding factors.
Our analysis revealed a significant doseresponse relationship between CTA frequency and subsequent risk of malignancy. Cancer hazard remained stable up to a critical threshold of approximately 1.88 CTAs per year (Figure 1); exceeding this rate was associated with a statistically significant rise in malignancy risk. Notably, this threshold aligns with radiation exposure levels identified in broader medical imaging studies as tipping points for increased lifetime cancer risk.2,3
Crucially, perioperative risk factors such as X-ray exposure or total procedure time did not display meaningful associations with malignancy onset. Instead, average CTA frequency emerged as the independent predictor of new cancers, while alternative metrics, including time intervals between scans or procedural radiation dose, showed no significant association.
Moreover, the pattern of cancers observed among our cohort mirrored organ-specific sensitivity to radiation exposure, lending mechanistic plausibility to a direct,
autograft’s proximal suture line, effectively reducing operative time. In cases involving a significant mismatch between a dilated aorta and the pulmonary artery, we performed a reduction aortoplasty by excising a longitudinal segment of the right aortic lateral wall to reconcile the discrepancy in vessel diameters. In such cases, the PEARS graft also contributes to reinforcing the reconstructed ascending aorta, extending up to the proximal aortic arch.
Post-operative recovery has been comparable to other aortic valve replacement procedures, with an
causative relationship.
These findings present a compelling reason to re-evaluate current CTA surveillance protocols following TEVAR. While frequent imaging remains indispensable for high-risk patients such as those with endoleaks or rapid aneurysm progression, our data strongly support refining surveillance strategies1: adopting risk-stratified, individualized protocols, and incorporating radiation-sparing alternatives (such as MRI or ultrasound) whenever feasible.
Clinicians should weigh the incremental cancer risk against the potential for early intervention, particularly for stable, low-risk patients in whom annual or biannual CTA may extend cumulative radiation exposure beyond safe limits. Alongside patient preferences and baseline risk factors, these nuanced protocols will be instrumental in safeguarding both short- and long-term health.
Ultimately, our study pioneers the identification of a clear, evidence-based
average hospital stay of 5–7 days. Our follow-up protocol includes a surgical consultation at six weeks post-discharge, a cardiology review with transthoracic echocardiography at three months, and a cardiac MRI at one year. Subsequent follow-up involves annual cardiology evaluations with echocardiography, with increased frequency based on clinical indications.
A notable observation emerged during follow-up: two patients required early reintervention on their pulmonary homografts within two years of the Ross-PEARS procedure. One of them involved a reoperation and the other one a balloon dilatation of the pulmonary homograft. While such events are not unprecedented, they prompted us to introduce a six-month course of low-dose ibuprofen postoperatively in all patients, aiming to mitigate inflammatory responses and delay or prevent homograft degeneration.
The Ross-PEARS operation should be considered in patients needing aortic valve replacement with an adult-sized aortic valve annulus. We also believe that the traditional concerns with severe aortic valve insufficiency and aortic root dilatation should not currently be a contraindication in this era of the Ross-PEARS operation.
threshold for safe post-TEVAR imaging, offering concrete guidance for reducing cancer risk without compromising vigilance. Optimizing surveillance not only mitigates iatrogenic harm but will shape more personalized, patientcentered follow-up care for an expanding population of aortic repair patients.
References
1. Kletzer J, Berger T, Kondov S, Bleile T, Dimov A, Werdecker V, et al. Are current follow-up intervals justified in patients with non-emergent aortic surgeries? Interdiscip Cardiovasc Thorac Surg. 2024;40(1). doi: 10.1093/icvts/ivae226. PubMed PMID: 39731738; PubMed Central PMCID: PMC11706529.
2. Albert JM. Radiation risk from CT: implications for cancer screening. AJR Am J Roentgenol. 2013;201(1):W81-7. doi: 10.2214/AJR.12.9226. PubMed PMID: 23789701.
3. Salibi PN, Agarwal V, Panczykowski DM, Puccio AM, Sheetz MA, Okonkwo DO. Lifetime attributable risk of cancer from CT among patients surviving severe traumatic brain injury. AJR Am J Roentgenol. 2014;202(2):397-400. Epub 20131226. doi: 10.2214/ AJR.12.10294. PubMed PMID: 24370078.

Figure 1: Restricted cubic spline regression of the association between average postoperative CTA frequency per year and log hazard ratio for new oncological disease following TEVAR. The solid red line represents the estimated log hazard ratio, with the shaded area indicating the 95% confidence interval. The blue dotted line marks the reference value of 1 CTA per year, while the red dashed line denotes the critical threshold of 1.88 CTAs per year, above which malignancy risk reaches statistical significance (P < 0.05). The histogram displays the distribution of the patients by average CTA frequency; CTA: Computed Tomography Angiography.
Aortic Disease Domain
Ana Redondo Palacios and Conal Austin
Ana Redondo Palacios and Conal Austin Guy’s and St Thomas’ NHS Foundation Trust, London, UK
Using Finite
Element Analysis to Evaluate the Improved Mechanical Behavior of Silk-Hybridized Three-Dimensionally-Printed Long-Segment Tracheal Substitutes


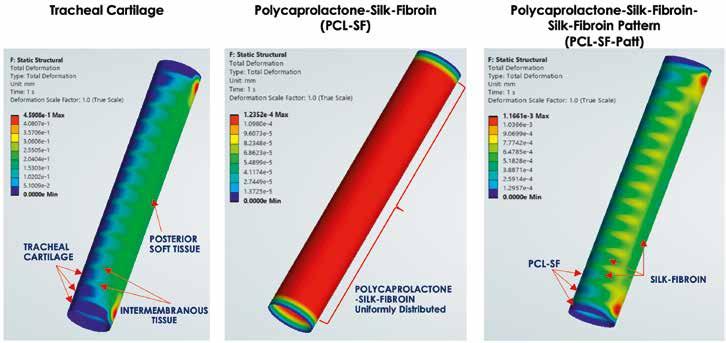
Background
Currently, there are limited management options for patients with long-segment tracheal defects greater than 6 cm. For such deformities, a primary surgical repair is not feasible due to the high tissue tension and mechanical stress generated. These conditions create an anastomotic microenvironment that promotes granulation tissue formation, occlusion, and eventual loss of airway patency.
These patients require long-segment tracheal replacement implants. Previous reconstructive strategies, such as autologous aorta or esophageal grafts, do not exhibit the mechanical strength necessary to maintain airway lumen patency during respiration. They also carry complications such as donor site morbidity. Thus, definitive management options are limited, and the need remains for an adequate long-segment tracheal replacement implant with minimal risks of mechanical failure.
Tissue-engineering using three-dimensional (3D) printing provides an avenue to generate patient-specific implants to optimize an implant’s mechanical behavior and mitigate anastomotic stress that often leads to the mechanical failure of prior reconstruction approaches.
Our research applies computational simulations to explore how hybridizing known implant materials such as polycaprolactone (PCL) with natural materials such as silk fibroin can optimize the mechanical behavior of long-segment tracheal grafts to more closely mimic the biomechanics of the native human trachea.
By applying computational methods such as Finite Element Analysis (FEA) to study the mechanics of patient-specific implants, we achieve what is often difficult to quantify in benchtop testing including simulating the complex mechanical loading environment of the human airway.
Why Silk?
Silk-fibroin, from the Bombyx mori silkworm, has exceptional tensile strength and is biocompatible. Hybridizing silk-fibroin with PCL allows us to optimize implant designs to mimic the native human trachea’s innate mechanical behavior. Integrating silk-fibroin hybrids in a geometric patterned fashion allows us to design a graft with lateral rigidity and longitudinal flexibility similar to the native trachea.
Role of Finite Element Analysis (FEA) and Computational Simulations:
Finite Element Analysis allows us to:
n Simulate intrathoracic loading conditions such as intraluminal radial pressures during inspiration.
n Evaluate the deformation and stress distributions of different implant designs and compare with the mechanical behavior of the native human trachea.
n Identify weak points before fabrication or implantation.
Computational simulation evaluations are cost-effective, efficient, and shorten the overall implant design and development process.
Methods:
We created three computational models:
1. Control – standard human trachea including cartilaginous rings, inter-membranous muscle, and membranous tracheal posterior
2. Hybrid – 3D-printed implant uniformly composed of a polycaprolactone-silk-fibroin hybrid bio-ink.
3. Patterned Hybrid – 3D-printed implant composed of polycaprolactone-silk-fibroin in locations matching the hyaline tracheal cartilage c-rings of human trachea alternated with silk-fibroin in locations of intermembraneous and posterior soft tissue regions of the native human trachea.
Boundary conditions included the proximal and distal ends of the trachea as fixed supports and an internal radial pressure simulating airway intraluminal inspiratory pressure.
Results
n Deformation: By alternating PCL-SF to mimic tracheal cartilage tissue with SF to mimic tracheal intermembranous and posterior soft tissue, our implant design permits both the longitudinal flexibility and the lateral rigidity seen in native human trachea biomechanics.
Clinical Implications
From a surgeon’s perspective, an ideal tracheal substitute laterally rigid strength anteriorly to maintain airway lumen
EACTS Outreach Programme
Advancing education initiatives in underserved regions
The EACTS Outreach Programme improves the outcomes for heart patients in underserved regions by advancing education initiatives. The programme distributes grants with funding from the Edwards Lifesciences Foundation and the Every Heartbeat Matters (EHM) initiative to qualified surgeons involved in humanitarian
work in underserved regions and communities.
The FFF EHM grants aim to support programmes that focus on the detection, treatment and recovery of these populations, with the goal of reducing the global burden of structural heart disease.
Recipients of the FFF Every Heartbeat Matters Grants – who must be an EACTS member – will provide education to help reduce the global burden of structural heart disease and drive progress towards global equity in surgical care.
“Many EACTS members already engage in
patency and connective tissue and muscle interspersed and located posteriorly for longitudinal flexibility. These characteristics permit expansion and contraction vertically during respiration and neck flexion-extension movements. Our implant design meets these criteria suggesting potential to reduce granulation tissue formation at the anastomoses-wellknown failure points in airway prostheses.
Next Steps
Our ongoing work focuses on:
n Computational Fluid Dynamics Studies: Simulating internal airflow of various implant designs to confirm intact airway mechanics.
n Optimizing implant design into porous scaffolds to balance mechanical strength with porosity that permits vascular ingrowth, nutrient exchange, and tissue integration. n in vivo preclinical testing to assess host tissue integration and long-term patency.
n Patient-specific customization: Currently, we are refining the engineering workflow to design custom implants directly from CT-radiographic imaging of a patient’s airway.
n The applications of FEA to further optimize reconstruction implants extends beyond tracheal reconstruction including bronchial replacements, chest wall reconstruction, vascular grafts, and other tubular organsrequiring a balance of strength, compliance, and bio-integration.
Conclusion:
This study illustrates the power of applying computational methods to advance surgical reconstruction. Finite Element Analysis not only accelerates design iteration but also helps predict clinical performance – allowing surgeons to engineer the optimal implant. The silk-hybridized, 3D-printed longsegment tracheal substitute represents a step toward a truly durable, custom-tailored airway reconstruction option, potentially transforming care for patients with devastating tracheal defects.
vital educational and humanitarian programmes, particularly in Africa. The EACTS Outreach Programme will drive and coordinate more of this important work –harnessing the expertise of EACTS members and fostering collaborations with industry partners, charities and other organisations,” said Patrick Myers, EACTS Secretary General. “Together we can improve long-term patient outcomes by opening up access to heart valve treatments around the world.”
The EACTS Outreach Committee, Chaired by Professor Carlos Mestres, Extraordinary
Professor at the Department of Cardiothoracic Surgery at the University of the Free State in South Africa, will award industry or charitysponsored grants to EACTS members. By leveraging industry and charity contacts, EACTS aims to shift the focus from short-term missions to sustainable programmes that improve long-term patient outcomes in underserved regions, with growing interest from industry to fund such efforts.
For more information, please email: FrancisFontanFund@eacts.co.uk
Figure 1. FEA comparing total deformation of the human trachea (left) with a homogenous polymer (center), and silk-hybridized in a patterned fashion (right) under radial compression.
Sujata Syamal Harvard University, USA
Clauden Louis Winter Haven Hospital, USA
Interventional palliation followed by surgical repair – the surgeons’ perspective
It is time to acknowledge that congenital cardiologists and congenital cardiac surgeons share the same goal: to provide the best possible care for patients with congenital heart disease – together. The days when cardiologists and surgeons were in competition with each other should be behind us, and everyone involved in the care of these patients understands this.
In an era where percutaneous interventions are becoming increasingly common, the concept of a "heart team," as established in adult cardiac care, is gaining importance in the congenital field as well. This collaborative approach allows for tailored patient management: those undergoing complex surgery may later require catheter-based interventions that surgeons would prefer to avoid re-operating, while others may need surgical intervention following a failed catheter procedure.
Today, low early mortality is expected even in the most complex congenital cardiac cases. Yet, in some instances, despite a technically perfect surgical result, mortality may still occur. Therefore, a hybrid strategy – beginning with less invasive palliative interventions followed by definitive surgical repair – can be a promising approach.
Some palliative interventional procedures have already become standard practice in many centers, such as ductal stenting. The technique of stenting the ductus arteriosus in

Julie Cleuziou
Deutsches Herzzentrum München
German Heartcenter Munich, Munich, Germany
neonates with duct-dependent pulmonary circulation can, in some cases, replace the traditional surgical systemic-to-pulmonary shunt. The Congenital Catheterization Research Collaborative conducted a multicenter study comparing 156 neonates who received surgical shunts with 35 neonates who underwent ductal stenting for pulmonary atresia1. The results showed that ductal stenting offered comparable clinical outcomes to surgical shunt -implantation. Rates of procedural complications, interstage mortality, and pulmonary artery growth were similar in both groups, although the ductal stent group
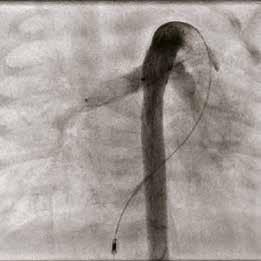


had a higher rate of re-interventions.
Another palliative option for patients with reduced or absent pulmonary blood flow is right ventricular outflow tract stenting. An Australian study including 20 infants with a median age of 14 days (IQR 7–32) and a median weight of 2.7 kg (IQR 2.1–3.4), undergoing primary right ventricular outflow tract stenting, reported no deaths within 30 days2. However, 13 patients (65%) required further interventions before definitive repair. A drawback of placing stents within the myocardium is the difficulty of explanting them, which might not always be feasible. Furthermore, patients with prior right
“From a surgeon’s perspective, palliative interventions do have a place in the treatment of congenital heart disease. So far, results indicate that interventional palliative procedures are feasible and may even contribute to reduced early mortality. However, multiple re-interventions are often required before definitive surgical repair can be undertaken. Nevertheless, due to the lack of large-scale studies, several important questions remain unanswered.”
ventricular outflow tract stenting tend to have higher rates of transannular patches and conduit implantation at time of repair2
A less common but promising strategy involves palliating patients with hypoplastic left heart syndrome or borderline left heart hypoplasia. Instead of undergoing a complex and high-risk surgery, patients receive a ductal stent and flow restrictors in both pulmonary arteries. Based on the “hybrid stage 1 Norwood” concept – which includes surgical bilateral pulmonary artery banding and ductal stenting – a fully interventional approach has been introduced. While this may not replace the traditional Norwood stage 1 procedure entirely, it provides patients, parents, and heart teams with valuable time before the next stage. Boston Children’s Hospital reported on 17 neonates who received flow restrictors. The procedure was technically feasible in all cases, and 76% of the patients progressed to the intended surgical stage3. Compared with a similar cohort undergoing the hybrid stage 1 procedure, those treated by interventional means had a significantly lower 6-month all-cause mortality risk (adjusted hazard ratio, 0.26 [95% CI, 0.08–0.82]).
In conclusion, from a surgeon’s perspective, palliative interventions do have a place in the treatment of congenital heart disease. So far, results indicate that interventional palliative procedures are feasible and may even contribute to reduced early mortality. However, multiple re-interventions are often required before definitive surgical repair can be undertaken. Nevertheless, due to the lack of large-scale studies, several important questions remain unanswered:
n Does ductal stenting affect pulmonary artery growth?
n Is right ventricular outflow tract stenting associated with longer cardiopulmonary bypass and cross-clamp times?
n Does right ventricular outflow tract stenting lead to a higher rate of conduit placement?
n Do flow restrictors increase the likelihood of pulmonary artery injury requiring surgical repair at subsequent stages of univentricular palliation?
References
1. Bauser-Heaton H, Qureshi AM, Goldstein BH, Glatz AC, Ligon RA, Gartenberg A, Aggarwal V, Shashidharan S, McCracken CE, Kelleman MS, Petit CJ. Comparison of Patent Ductus Arteriosus Stent and Blalock–Taussig Shunt as Palliation for Neonates with Sole Source Ductal-Dependent Pulmonary Blood Flow: Results from the Congenital Catheterization Research Collaborative. Pediatric Cardiology (2022) 43:121–131.
2. Luxford JC, Adams PE, Roberts PA, Mervis J. Right Ventricular Outflow Tract Stenting is a Safe and Effective Bridge to Definitive Repair in Symptomatic Infants with Tetralogy of Fallot. Heart, Lung and Circulation (2023) 32, 638–644.
3. Sperotto F, Lang N, Nathan M, Kaza A, Hoganson DM, Valencia E, Odegard K, Allan CK, da Cruz EM, del Nido PJ, Emani SM, Baird. Transcatheter Palliation with Pulmonary Artery Flow Restrictors in Neonates with Congenital Heart Disease: Feasibility, Outcomes, and Comparison with a Historical Hybrid Stage 1 Cohort. Circ Cardiovasc Interv. 2023 Dec;16(12):e013383.
Surgical extraction of an RVOT stent
Palliative intervention in a patient with hypoplastic left heart syndrome. * Ductal stent, # pulmonary flow restrictors
Ductal stent in a patient with pulmonary stenosis
17:45 - 18:45 Focus Session Auditorium 15
Optimal CABG approach
Coronary artery surgery is rapidly changing. Like in other medical and surgical specialties, patients are now demanding both an excellent outcome and a less invasive approach. Over time, percutaneous coronary interventions and medical therapy have gained ground as alternatives to bypass surgery, with recent clinical trials such as ISCHEMIA and FAME 3 suggesting that an individualized, targeted, and potentially hybrid approach to multivessel coronary artery disease will play a significant role in the future.


The coronary surgeon’s best bypass conduits are the internal thoracic arteries. Over two decades, our group has offered multiarterial MICS CABG as a surgical approach to treat multivessel coronary artery disease.1 The conventional MICS CABG operation, however, is technically difficult. Robotic technology enables the surgeon to more easily enter the sphere of nonsternotomy multiarterial CABG by allowing the harvest of both internal thoracic arteries (robotically over their full length), keeping the grafts pedicled (without the need for proximally source them), and by anastomosing them (using MICS CABG techniques) on the left anterior descending and left circumflex territories. Prior to the patient going home, graft
2024 ESC Chronic Coronary Syndrome Guidelines: Indications and PatientCentered Approach
The 2025 European Society of Cardiology (ESC) guidelines for chronic coronary syndromes (CCS) mark an important step forward in managing patients with stable coronary artery disease. Unlike the 2019 guidelines, where input from surgeons was limited, this update features much stronger involvement from the surgical community and includes formal endorsement by the European Association for CardioThoracic Surgery. These guidelines incorporate the latest advances in diagnostics, risk assessment, and treatment strategies. They also put a clear focus on personalized, patientcentered care and emphasize the importance of shared decisionmaking between healthcare providers and patients, reflecting a more tailored approach to treatment.
Medical Management
Optimal medical therapy remains central to managing CCS in the current guidelines. All patients should receive statins, targeting LDL
validation is usually performed, during which the right coronary artery can either be stented or left to medical management.2
Up to four grafts can be performed this way, depending on individual coronary anatomy. With this approach, patients not only avoid a sternotomy, but also cardiopulmonary bypass, cardiac anoxia, aortic manipulations, vein grafts, radial harvest, Y- or T-grafts, as well as significant blood loss. Patients leave hospital and return to work earlier, with two angiographicallyproven internal thoracic artery grafts on their left heart
agonists for type 2 diabetes with obesity.

cholesterol below 55 mg/dL. ACE inhibitors are advised for heart failure, diabetes, or hypertension. Betablockers and calcium channel blockers are first-line for angina, with other antianginals chosen based on individual needs. New recommendations include SGLT2 inhibitors and GLP-1 receptor

Instead of a strict stepwise approach, the guidelines now promote selecting antianginal drugs according to ischemia mechanisms, comorbidities, and patient tolerance, enabling more personalized treatment.
Revascularization
The guidelines reaffirm the central role of revascularization in CCS, particularly for patients at high risk of adverse outcomes. CABG remains the preferred strategy for patients with multivessel disease, left main disease, diabetes, or impaired left ventricular function. The guidelines emphasize that the decision to revascularize must be based on a careful assessment of ischemic burden, anatomical complexity, comorbidities, and patient preferences. Markedly, the threshold for intervention in asymptomatic or minimally symptomatic patients has increased, reflecting evidence that routine revascularization (particularly PCI) does not always improve outcomes over optimal medical therapy.
Concerning the management of patients with left ventricular dysfunction, the REVIVED-BCIS2 trial found that PCI offers no significant benefit over guideline-
circulation, feeding up to four distal anastomoses (Figure 1). Recently, the Minimally Invasive versus STernotomy (MIST) trial demonstrated several benefits of a nonsternotomy approach for multivessel CABG, including its primary outcome of better postoperative recovery, as well as the safety and feasibility of performing complete revascularization by using multiple grafts without sternotomy.3,4 Surgeons must now find ways to provide advanced and less invasive multiarterial coronary bypass in a manner that is less invasive, associated with better recovery and outcomes and, importantly, more widely diffusible. The presentation titled Optimal CABG Approach during the session “Heart Team: Myocardial Revascularization decision making in practice” at the EACTS Annual Meeting, on Friday, October 9 at 17:45, will describe this novel way of surgically approaching multivessel and/or left main coronary artery disease.
References
1. McGinn JT Jr, Usman S, Lapierre H, Pothula VR, Mesana TG, Ruel M. Minimally invasive coronary artery bypass grafting: dual-center experience in 450 consecutive patients. Circulation. 2009 Sep 15;120(11 Suppl):S78-84. doi: 10.1161/CIRCULATIONAHA.108.840041.
2. Issa HMN, Parisi A, Goubran D, Ruel M. The 10 Commandments of Robotic Bilateral Internal Thoracic Artery Harvesting. Innovations (Phila). 2025 Jun 30:15569845251350280. doi: 10.1177/15569845251350280.
3. Guo MH, Wells GA, Glineur D, Fortier J, Davierwala PM, Kikuchi K, Lemma MG, Mishra YK, McGinn J, Ramchandani M, Rabindra P, Nambala S, Chiu KM, Kiaii B, Gibson S, Ruel M. Minimally Invasive coronary surgery compared to STernotomy coronary artery bypass grafting: The MIST trial. Contemp Clin Trials. 2019 Mar;78:140-145. doi: 10.1016/j.cct.2019.01.006.
4. Ruel M, Nambala S, Verevkin A, Rabindranauth P, Kikuchi K, Davierwala P, Lemma M, Ponnambalam M, Guo M, Borger M, Whitlock R, Wells GA. Minimally Invasive Compared to Sternotomy Coronary Artery Bypass Grafting: Primary Results from the MIST Randomized Controlled Trial. Presented at the 105th Annual Meeting of the American Association for Thoracic Surgery, Seattle, May 2025.
directed medical therapy (GDMT) for patients with ischemic cardiomyopathy and left ventricular dysfunction. In contrast, the STICH trial showed that CABG plus GDMT significantly lowers all-cause and cardiovascular mortality compared to GDMT alone in patients with CAD, LVEF ≤35%, and no left main disease (LMD) over nearly 10 years. As a result, PCI for patients with LVEF <35% and high surgical risk is now a IIb rather than IIa recommendation.
Mode of revascularization
Following the revision of the 2018 ESC/EACTS recommendations for LMD, the ESC has reviewed the evidence and, in the latest guidelines, gives precedence to CABG over PCI for most patients with LMSD. In cases where both procedures are suitable, a Heart Team should weigh treatment options to optimize outcomes and quality of life.
In complex cases where CABG and PCI are equally recommended, a multidisciplinary Heart Team should determine the best treatment for improving patient outcomes and quality of life.
Nevertheless, revascularization decisions should be patientcentered, considering individual preferences, health literacy, cultural background, and social support
whenever possible.
For the management of graft failure after coronary artery bypass grafting, there are new IIa recommendations for redo CABG for patients without a patent LIMA graft to the LAD, and for PCI of the bypassed native artery over PCI of the bypass graft.
Practical Takeaways for Cardiac Surgeons
For cardiac surgeons, the 2025 guidelines underscore the importance of early and ongoing collaboration within the Heart Team. Surgeons play a vital role in patient selection, risk assessment, and shared decisionmaking, particularly for patients with complex coronary anatomy or high surgical risk.
It is imperative that surgeons not only continue to perfectionate the surgical techniques and perioperative care of patients with coronary artery disease, but also that they embark in prospective, good-quality research to fill existing knowledge gaps.
Unfortunately, many important aspects of myocardial revascularization, such as the procedural aspects of both PCI and CABG are absent in the current guidelines, signalling the need for further updates and partnership between ESC and EACTS to produce recommendations in these areas.
Figure. Male patient one week after robotic-assisted CABG using both internal thoracic arteries.
Rafael Sádaba Navarra University Hospital, Pamplona, Spain
Gathering real-world evidence to improve outcomes at EACTS
15:15 - 16:15
Focus Session Room 180/181
16:30 - 17:30 Focus Session Room 180/181
Today, there will be two special Focus Sessions discussing the importance of gathering real-world evidence based on the collection and use of high-quality data to improve patient outcomes. The session, ‘Advancing cardio-thoracic surgery through data and insights’, will explore how using high-quality multi-centre data can help generate insights for quality improvement and research.
“Our sessions in Copenhagen will demonstrate how correctly collecting as muchinformation as possible on a small set of variables, can inform us about patient characteristics and outcomes from surgery, resulting inimprovements in cardio-thoracic surgery and patient care,” explained Paola Quattroni, EACTS Quality Improvement Director. “Our presenters will discuss the importance of collecting data in a standardized way, demonstrate how this data can be used, and show how it ultimately leads to improved patient outcomes.”
Professor of Thoracic Surgery, Rishindra Reddy, looks forward to sharing his insights from the Michigan Quality Improvement Initiative during today’s session and how he brought together different hospitals and communities to better understand data and improve outcomes.
“I am excited to share the insights of our Cardiothoracic Surgery Quality Collaborative from the State of Michigan with the European and broader cardiothoracic community. We have led the United States in certain quality

metrics with a combination of programmes ranging from large academic centres to single surgeons in small hospitals, all performing cardiac and thoracic surgery at a very high level with reduced blood transfusions, early extubation after cardiac surgery, high rates of IMA use for coronary bypass, and improved lymph node dissection for lung cancer, among many other key quality metrics.”
The session will also look at how embracing new tools, such as robotics in cardiac surgery and artificial intelligence, can advance research and surgical outcomes. For example,
Dr Johannes Bonatti from the University of Pittsburgh will present how a community-led working group is developing standards for the collection of robotics cardiac surgery data.
Dr Zain Khalpey from the University of Arizona will explain how his team has developed AI
tools that collect real-time data in the OR and perform analytics for quality improvement and research purposes.
Mechanical circulatory support registries
The session, ‘Use of real-world data for research in mechanical circulatory support’, will concentrate on how real-world data from clinical registries offer valuable insights into the use and impact of mechanical circulatory support devices, particularly in complex populations such as heart failure patients. Clinical registries provide a platform for understanding the use of devices, patient characteristics, and clinical outcomes in diverse populations. This session will delve into recent developments of international clinical registries, including the EACTS European Registry for Mechanical Circulatory Support (EUROMACS), which continues to be the main European resources of data from patients with durable MCS, and the US-based International Registry for Mechanically Assisted Circulatory Support (IMACS), and will highlight important research studies that can inform management of heart failure patients.
Professor José Golzalez Costello, Associate Professor at the University of Barcelona and
Visit us at booth #54 to pick up the new INTUI CABG Guidebook and the updated CABG Guidebook for Legacy software. → New insights. → Smarter layout. → Same trusted guidance. Defining quality. Transforming lives.
multinational database, with collaboration from a diverse group of international authors”.
“Overall, these sessions are designed to support investigator-initiated research proposals and have the uniqueness of integrating patients from all the different registries around the world. I look forward to welcoming delegates to these sessions and listening to the fascinating presentations and subsequent discussions,” Quattroni added.
EACTS’ Adult Cardiac Database
Using this data for research and developing databases like the ACD and EUROMACS for the cardiac surgery community, helps to identify best practices contributing to improvements in the quality of care for cardiac surgery patients.
“My role at EACTS is to oversee, together with Edgar Daeter, the Quality Improvement Programme initiatives that we run at the
Paola Quattroni EACTS Quality Improvement Director
LEARNING LABS
Hands-on guidance from the experts
Take advantage of the invaluable opportunity to train with some of the world’s best cardiothoracic surgeons at the EACTS Learning Lab. These specialist hands-on workshops are designed to advance your technical abilities and include wetlabs, drylabs, simulation and practical sessions. You will gain practical experience using the latest devices, practice on simulators and interact with expert faculty and industry proctors. EACTS Learning Lab sessions are available to EACTS members for just an additional €75 each (€100 for non-members).

Spaces are limited and offered on a first-come, first served basis. Don't miss out – book today to guarantee your opportunity.
EACTS LEARNING LAB SCHEDULE
Thursday 9 October
08:30 – 10:30 The axillary approach for repair of congenital heart defects
08:30 – 10:30 Endoscopic Dry Lab Training
11:15 – 13:15 Mitral Valve
11:15 – 13:15 Endoscopic Dry Lab Training
13:45 – 15:45 Coronary
13:45 – 15:45 Endoscopic Dry Lab Training
16:15 – 18:15 Transcatheter
16:15 – 18:15 Endoscopic Dry Lab Training
Dr Edgar Daeter, cardio-thoracic surgeon at St Antonius Hospital in Niewengein, is the Chair of the Quality Improvement Programme and ACD task force, and has been involved since the inception of the renewed ACD.
“We want to collect a limited but significant amount of data about surgical procedures. The aim is to aggregate this data for surgeons to access via an interactive viewer or tool that shows them graphs so that they can get insights from that data. They will be able to see the different trends of surgical procedures over time against certain patient groups. The interactive viewer is also a benchmarking tool for surgeons to compare their own hospital data and outcomes to data and outcomes from other hospitals. By using risk correction outcomes of types of surgery for patients with selectable risk profiles, outcomes can be benchmarked on a hospital or country level to identify potential improvements for participating hospitals. A surgeon can see if their hospital is an outlier for a particular procedure and examine the reasons

why there are differences in outcomes. By looking at the data, it might be the case that they are operating on certain patient groups with comorbidities. For example, through the
Friday 10 October
09:00 – 11:00 AV Repair – Valve Sparing Aortic Root Surgery: The Reimplantation Technique
09:00 – 11:00 Endoscopic Dry Lab Training
12:15 – 14:15 AV Repair – Annuloplasty with remodelling valve sparing root replacement and isolated aortic valve repair
12:15 – 14:15 Endoscopic Dry Lab Training
15:00 – 17:00 Left-handed Surgeons
15:00 – 17:00 Endoscopic Dry Lab Training
Saturday 11 October
09:00 – 11:00 Thoracic
09:00 – 11:00 Endoscopic Dry Lab Training
database, a surgeon can look at length of stays, mortality rates, age, comorbidities etc., across different countries and healthcare systems.
Importantly, by using the database, surgeons will have a unique opportunity to find useful insights and implement improvements at their hospital.”
Dr Daeter explained that now that the database include over 55,000 procedures from about 21 international hospitals and more datasets are expected to be added soon, the QUIP team will soon organise some online community meetings for participant hospitals.
“The ACD and EUROMACS have a research pillar based on a research data request protocol, to ensure trustworthy access to de-identified data. Unique in the protocol is the opting-out system for contributing hospitals. When a research data request is submitted, all participating hospitals will receive the request and will be able to opt out from the research if they wish. The hospitals will always be able to decide on whether to share their data or not.”
In addition to the databases work, QUIP has another dimension as a registry by briging
interested communities together. With the help of the cardio-thoracic surgery community and other international registries we are keen to better understand current collection methods, auditing systems, implementation of GDPR, standardisation of cardiothoracic datasets and preparedness for implementation of the European Health Data Space. She explained that the new database offers the opportunity to participating hospitals in a more consistent and standardised way, which will help improve data completeness and quality. This means that this data can be used much more effectively to improve best practice and inform patient care. In future, it will be possible to use the database for research. Following a trustworthy and thorough data access request process, researchers will be able to submit their study proposals, and following approval, they will be able to use the data for research purposes.
For EACTS members to set up an account and access the ACD, please visit www.eacts.org/ quality-improvement/adult-cardiac-database/
Edgar Daeter Chair of the Quality Improvement Programme Committee
9th EACTS Mechanical Circulatory Support Summit
20-22 November 2025
Hotel nhow Berlin, Berlin, Germany
The 9th EACTS Mechanical Circulatory Support Summit returns this year with interactive lectures, live-in-a-box cases and keynote presentations. The Summit is designed to attract attendees with an interest in mechanical circulatory support, including cardiologists, heart failure cardiologists, emergency and ICU specialists (ECLS), cardiac surgeons, perfusionists, heart failure nurses and VAD coordinators, paediatric cardiologists and congenital heart disease surgeons, and representatives from the medical industry (cardiac device, including ECMO development and production).
This two-and-a-half-day summit will cover an array of topics, including an update of optimal medical therapy and device treatment (OMDT), Glucagon-like peptide-1 receptor agonists, cancer treatment in LVAD patients, transcatheter aortic valve implantation (TAVI) and transcatheter edge-to-edge repair (TEER) on LVAD, big data and AI in medicine, and more.
In addition, there will also be a scientific evaluation of MCS registries (IMCARS, EUROMACS, INTERMACS, IMACS and the Stellar

register) vs multicentre studies, and discussions on the different phenotypes of cardiogenic shock (including SCAI and INTERMACS stages, AMI, postcardiotomy, acute on chronic heart failure and fulminant myocarditis). Attendees will also witness a joint EACTS /ICCAC session, ‘LVAD therapy – how to make the most out of it?’ that will focus on the power of networking, patient evaluation, selection and optimisation, and novel LVAD tools and useful wearables.
A specially designed ‘Guidelines on MCS’ session will examine the EACTS/STS/AATS Guidelines on Temporary Mechanical Circulatory Support in Cardiac Surgery, EACTS ECD on Protected Cardiac Surgery, AATS surgical treatment of AMI complications, ISHLT guidelines on Temporary Mechanical Circulatory Support (tMCS), ESC heart failure updates, as well as examine the future perspective and unmet needs in clinical MSC guidelines.
New and recent developments will also be under the spotlight with presentations on continuous-flow biventricular assist device (CFBiVAD) with single drive lines, CF-BiVAD with two drivelines and the surgical implantation technique for a rotary total artificial heart, as well as an update from industry, ‘What’s in
the pipeline – new devices.’
A focus session on the major challenges in patients with congenital heart diseases will assess paediatric support outside of traditional LVADs and the replacement of the pulmonary valve with pre-emptive use of Microaxial Flow Pump (mAFP). Additionally, experts will look at the impact of the combination of temporary and durable devices and the challenges during the transition from mAFP to dLVAD.

Last, but by no means least, a session entitled ‘The beauty and the beast’ will discuss complex cases and present the creative solutions in cardiology and cardiac surgery.
MCS Rising Stars Quiz
Delegates are invited to submit a team to participate in the popular MCS Rising Stars Quiz. Members of the team should be from the same country or the same institution and may have a maximum of four participants. Spaces are limited, and we may not be able to accommodate all who apply, so please register your interest by emailing clara.mealing@ eacts. co.uk and we will get back to you.
If you attended the 2025 MCS Workshop, please email registration@eacts.co.uk to claim your €100 discount on your MCS Summit registration. Registration fees include all sessions, Welcome Reception, lunch and refreshments. Register now!
Custom Surgical Instruments, Implants & Accessories
Quality Refined since 1927
Visit Kapp at EACTS Annual Meeting - Shell #70

The Original Cosgrove® Mitral Valve Retractor System
• Universal Self-retaining Heart Retractor
• Mitral Valve Repair or Replacement Surgery
• Exceptional Exposure for Right & Left Atrium

Kapp is the EXCLUSIVE Manufacturer of the ORIGINAL Cosgrove Design


McCarthy Mini-Sternotomy Retractor w/ Universal Lift
Designed to provide excellent exposure for valve operations, Maze procedures or other intra-cardiac procedures. Also used for mini sternotomy procedures or coronary artery bypass operations, based upon the patient’s size. The removable lift increases exposure for valve procedures.
• Mounted on a 5 inch modified chest spreader.
• Small, durable, with unique smaller blades for ease of access and retracting for either proximal or distal mini-sternotomy procedures.
• Provides optimal surgical exposure for minimally invasive procedures.












Sterile Adhesive Organizer
• Keeps sterile tethered appliances on the surgical field from falling to the floor with 4 hook & loop closures
• Latex free self adhesive back for attachment to the surgical field
• Economical - Saves pre-op time
• Several sizes, configurations, colors
• Sterile shelf life 2 years
• New users call for FREE SAMPLES

Rosenkranz™ Pediatric Open Heart Retractor
A unique small retractor with attachable, self-retaining atrial and ventricular retractor blades that provide excellent and consistent exposure of all heart chambers during heart valve replacement for congenital heart defect surgery. The Rosenkranz™ Pediatric Open Heart Retractor enhances visualization of the intracardiac anatomy and comes in two small sizes for pediatric and small child use.
Gillinov Self-Retaining Maze Retractor
The Gillinov Self-Retaining Maze Retractor/attachment is designed to provide exposure of the pulmonary veins and atrial appendage during the Maze procedure or operations for atrial fibrillation that include pulmonary vein ablation. The visualization of these structures is greatly enhanced with this retractor.

SCIENTIFIC PROGRAMME
THURSDAY 9 OCTOBER


FRIDAY 10 OCTOBER
11 OCTOBER
16:30 - 17:30 Focus Session Hall A1
ESC/EACTS Guidelines for the Management of Valvular Heart Disease
Key points
n Surgery remains the preferred choice for patients with primary mitral regurgitation.
n A new class IIa recommendation for surgery and a IIb recommendation for transcatheter procedures for patients with atrial secondary mitral regurgitation.
n A new class I recommendation for mitral valve repair surgery in patients with asymptomatic primary mitral regurgitation, who meet certain diagnostic criteria.
n A change in the age cut-off from 75 to 70 years, in favour of TAVI for patients with tricuspid aortic valve stenosis.
n An upgrade in the recommendation (IIa) for aortic valve repair, in experienced centres, for patients with aortic regurgitation.
EACTS and the European Society of Cardiology (ESC) have published new guidelines which will have a significant impact on the worldwide care of patients with valvular heart disease (VHD). The two organisations have worked in close collaboration to develop the 2025 ESC/EACTS Guidelines for the Management of Valvular Heart Disease, drawing on the latest clinical evidence available.
The guidelines recommend lowering the age cut-off for transcatheter aortic valve implementation (TAVI) for tricuspid aortic valve patients from 75 to 70 years. This

recommendation reflects a growing body of clinical evidence, including extended follow-up results from multicentric randomised trials, demonstrating outcomes with TAVI comparable to SAVR, particularly in terms of hard clinical endpoints.
The guidelines address several important issues for surgeons taking care of VHD patients, including setting out clear diagnostic criteria for patients with aortic stenosis, better defining the role of CT angiography in preoperative assessment of coronary artery disease, and management of patients with
mixed or multiple valvular disease.
In addition, this is the first time that any guideline document provides a definition of atrial secondary mitral regurgitation. These guidelines include a IIa recommendation for surgery and a IIb recommendation for transcatheter procedures for these patients. Michael Borger, EACTS-appointed co-chair of the guidelines Task Force, which developed the VHD guidelines, explained: “This is particularly important for us as surgeons, because we are able to offer a therapy that really treats the actual etiology of the disease. We're able to offer repair of the mitral and frequently the tricuspid valve, in addition to an ablation procedure against atrial fibrillation (AF) and a closure of the left atrial appendage, all in one procedure. And the results for surgery, although preliminary and not randomised, seem to be better than for transcatheter procedures.”
The guidelines also clearly reiterate that surgery is the procedure of choice for patients with primary mitral regurgitation, with transcatheter therapy being an option only for those patients who are not appropriate candidates for surgery.
A new class I recommendation for mitral valve repair surgery in patients with asymptomatic primary mitral regurgitation, who meet certain diagnostic criteria, stresses the benefits of early intervention, instead of monitoring for the emergence of traditional class I triggers (i.e. symptoms or LV dysfunction). The guidelines stress that delaying surgery until symptoms or LV dysfunction have taken place will likely have an adverse impact on life expectancy following surgery. Patients with primary mitral
regurgitation who undergo earlier mitral valve repair can benefit from the same long-term life expectancy as people who do not suffer from VHD. Further additions to the guidelines, which will replace the previous 2021 version, include:
n A clearer definition regarding when a concomitant tricuspid valve repair procedure is recommended.
n A new class I recommendation to close the left atrial appendage for VHD patients with AF. There is an increasing amount of data showing that AF has a negative impact on patients and that left atrial appendage closure reduces the risk of stroke.
Concomitant surgical atrial ablation is also mentioned prominently in the text as a method to mitigate those negative outcomes associated with AF.
n An expanded chapter on mixed and multivalve disease, which stresses the importance of involving the Heart Team in discussions about treatment, where surgery is often the most reasonable option.
Michael Borger said, “These guidelines are of global significance for everyone working in the field of VHD. The Task Force, which included both surgeons and cardiologists, has worked together closely over the past two years using the latest data available to develop these recommendations to support Heart Teams everywhere. These guidelines demonstrate the importance of collaboration between cardiologists and surgeons for the benefit of patients. I highly recommend these guidelines to Heart Teams in Europe and across the world to support your clinical decision making.”


Michel Borger Leipzig Heart Center, Leipzig, Germany
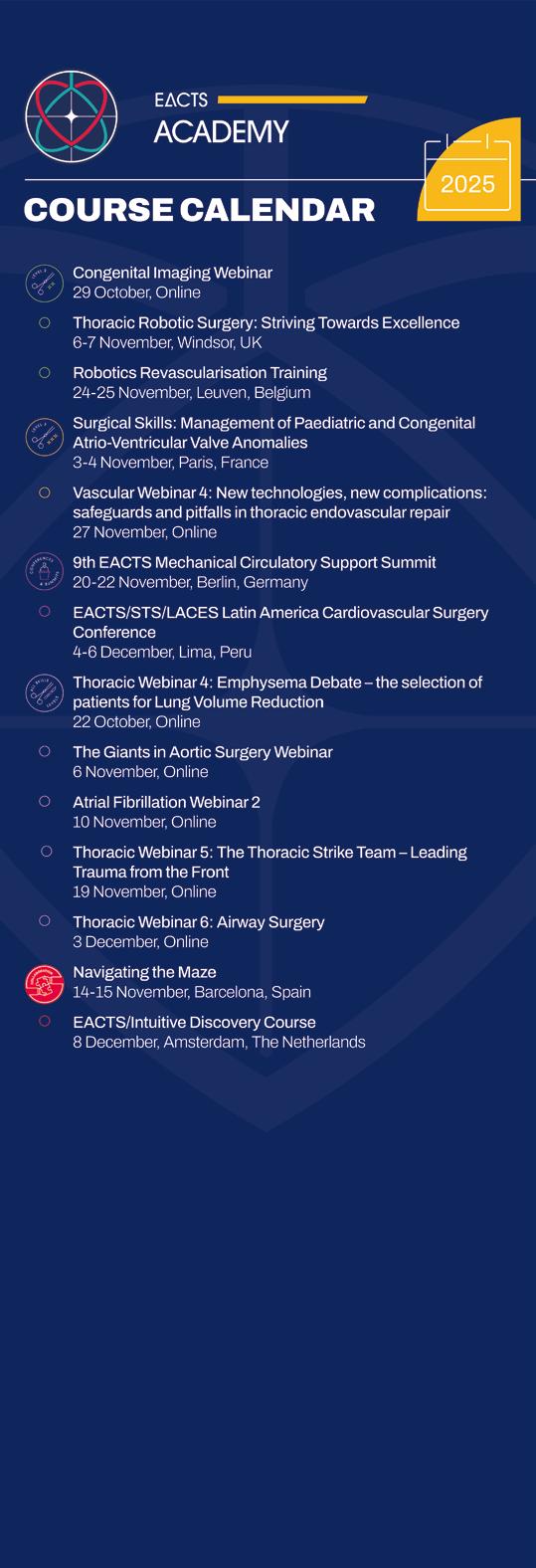

Heritable thoracic aortic disease – risk assessment and precision aortic medicine
17:45-18:45 Focus Session Hall A3
PEARS or David – Decision making in my practice
The surgical treatment of aortic root dilatation has advanced greatly over the past three decades. Where once the Bentall operation—with its composite graft and mechanical valve replacement— was standard, today the priority is preservation of the native valve. This reflects a broader philosophy: surgery should correct disease while maintaining natural anatomy, limiting prosthetic material, and avoiding anticoagulation.
Two valve-sparing operations now define this field. The David reimplantation procedure, with over thirty years of follow-up, is the benchmark for durability. The Personalised External Aortic Root Support (PEARS)—pioneered by Professor Tom Treasure and refined by Dr Conal Austin—offers a preventative strategy to stabilise the root before cusp damage occurs. One is reconstructive, the other preventative.
For the practising surgeon, the challenge is not simply technical mastery but deciding which operation suits each patient. In my practice,

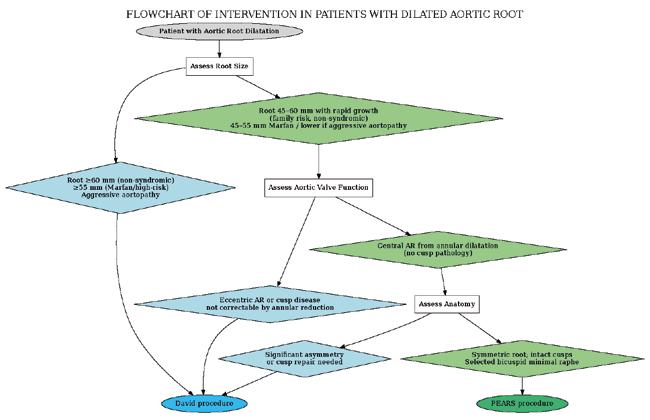
decision-making depends on anatomy, disease trajectory, and patient priorities—balancing proven durability against the advantages of earlier, low-risk intervention.
Understanding the Two Approaches
The David procedure involves
excising the dilated root, reimplanting the valve within a Dacron graft, and reattaching the coronaries. It restores root geometry and annular stability. Freedom from reoperation at 15–20 years exceeds 90%.
The PEARS procedure places a patient-specific mesh sleeve around the root without opening the aorta or

Critical Care Examination Applications opening 15th October!
CVCC Level 1 & 2 Examination – Updated Regulations!
Easier than ever to apply, view our updated regulations. The Critical Care Certification is for surgeons who are recognised as leaders of multidisciplinary, high performing teams.
MEBCTS Level 1 Examination
The Membership of the European Board of Cardiothoracic Surgery (MEBCTS) is for surgeons at the end of national training who are ready to work independently.
FEBCTS Level 2 Examination
The Fellowship of the European Board of Cardiothoracic Surgery (FEBCTS) is for surgeons who are already practicing independently.
disturbing the valve. It prevents further dilatation, and the porous mesh permits tissue ingrowth and integration.
Timing and Valve Function
Timing and valve status are decisive. The David procedure is suited to patients who have exceeded surgical thresholds and whose roots cannot be reduced safely, even with the ~10% reduction achievable with PEARS. Typically, this means roots ≥60 mm in non-syndromic patients, ≥55 mm in Marfan syndrome, and earlier in aggressive aortopathies. Moderate-to-severe regurgitation, especially eccentric or l inked to cusp disease not correctable by annular reduction, also favours David. PEARS is most useful in the “grey zone,” before or just at threshold. I consider it in younger patients with connective tissue disorders, roots in the mid-40s to early-50s range, rapid growth, or strong family history. Mild-to-moderate central regurgitation can also be addressed if due to annular dilatation, as the mesh may reduce annular size by 10-15%.
In this setting, PEARS avoids bypass and may prevent progression to cusp damage.
Anatomical and Technical Factors
The David procedure tolerates root asymmetry and cusp pathology because reimplantation allows cusp repair. PEARS requires intact leaflets with coaptation restorable by annular downsizing. It works best in symmetric dilatation with central regurgitation from annular enlargement, and in selected bicuspid valves with minor raphe disease. By contrast, intrinsic cusp pathology— prolapse, restriction, calcification—or eccentric regurgitation not correctable by annular reduction favours David. Coronary anatomy also matters. David requires mobilisation and reimplantation of the coronaries, while PEARS leaves them untouched, though orientation affects sleeve design.
Technically, the David is complex, requiring bypass and cross-clamping but offering a durable one-stage repair. PEARS is performed on a beating heart with shorter times. It is
simpler, but the accurate placement of the mesh is essential for long-term success and to avoid coronary complications.
Risk–Benefit Profile
The David procedure carries a low perioperative risk, with complications mainly related to precision: bleeding, coronary ischaemia, or late cusp degeneration if repair is imperfect. Its durability is excellent, with outcomes beyond two decades.
PEARS has low early mortality and morbidity, faster recovery, no anticoagulation, and valve preservation. Its limitations are less mature long-term data and a small risk of late conversion to root replacement. Conversion may be more demanding due to mesh ingrowth and adhesions, but remains feasible in experienced centres.
Patient Perspective and Shared Decision-Making
Patients bring clear priorities. Some prefer to delay bypass with a less invasive option; others want the reassurance of a single David operation. For young Marfan or Loeys–Dietz patients with moderate dilatation and competent valves, I emphasise PEARS as a way to stabilise the disease while preserving options. For those with advanced enlargement or significant eccentric regurgitation, the David procedure is my recommendation.
Shared decision-making is essential. Lifestyle, pregnancy plans, lifelong imaging, and tolerance for reoperation all influence the final choice.
Conclusion
The choice between PEARS and the David procedure is not a competition but a continuum of care. PEARS allows earlier, low-risk intervention while keeping future options open. David remains the definitive solution for advanced disease, especially where valve pathology coexists, offering unmatched stability.
In practice, the art lies in recognising when a patient stands at the fulcrum between the two—where anatomy, timing, and personal priorities converge—and guiding them toward the operation that best secures their future.
Gianluca Lucchese
St Thomas’ Hospital & Cleveland Clinic, London, UK
15:15–16:15
Auditorium 15 Abstract
High sensitivity, high stakes: Redefining troponin thresholds after isolated CABG
CABG remains the gold standard treatment for extensive coronary disease due to its significant long-term mortality benefits, symptom reduction and protection against non-fatal cardiac events. However, CABG is an invasive procedure that often causes a transient rise in postoperative cardiac biomarkers, such as high-sensitivity cardiac troponin I (hs-cTnI). Extremely high troponin after CABG is concerning for graft failure, poor myocardial protection, or incomplete revascularization. There is no clear consensus on the clinically significant hs-cTnI after CABG that should indicate additional intervention. Current hs-cTnI thresholds defining postoperative myocardial infarction (MI) by guidelines have provoked controversy for their impact on major trials comparing PCI to CABG.
The Vascular Events in Surgery
We conducted a secondary analysis of the VISION Study to examine the hs-cTnI threshold associated with all-cause mortality in isolated CABG, and compare these thresholds between OPCAB and ONCAB. The statistical methods mirrored the original VISION study.
The VISION Study enrolled 6,505 patients (OPCAB=1,141, ONCAB=5,364) who underwent isolated CABG and were eligible for our subanalysis. Patients undergoing OPCAB were less likely to have had a previous MI (p<0.001), had a lower median EuroSCORE II (p=0.002) and presented with less advanced NYHA status (p<0.001) and CCS angina class (p<0.001) compared to ONCAB.

The median peak hs-cTnI was significantly lower at 640 ng/L ([IQR 264-1,689], 25x upper reference limit [URL]) after OPCAB, compared to differentially associated with all-cause mortality than in ONCAB.
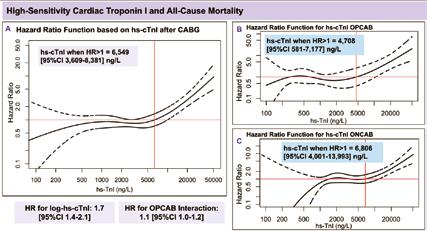
complications of CABG is postoperative MI, which may also constitute treatment failure due to graft failure, technical error, or distal occlusion. Previous studies have shown that hs-cTnI is prognostic of adverse outcomes even in the absence of supportive clinical or imaging findings. However, existing guidelines by the SCAI-2, UDMI, and ARC-2 present conflicting definitions of
exceeds current guideline thresholds for perioperative MI and (ii) guides early definitive testing and management. Our findings also allow for more accurate outcome measurements in trials comparing CABG to PCI. Our median hs-cTnI level was 94x URL, with 61% of patients exceeding the SCAI-2 definition of MI. This implies that previous uses of SCAI-2, such as in the EXCEL trial, may have



FIGURE
EXHIBITION FLOOR PLAN

Introducing the ‘open mic’ programme at the EACTS booth
This year, we are excited to introduce a brand new open mic-style area at the EACTS booth (#47). Join us for an inspiring programme of engaging talks, interactive
Your guide to what's on
TUNE IN

Watch live and recorded content from this year's Annual Meeting on EACTS TV. Educational and entertaining, EACTS TV features compelling panel debates, Annual Meeting highlights and interviews with the world’s leading cardiothoracic surgeons.
Thursday 9 OCTOBER
09:45–10:00 Your daily briefing: Thursday
10:15–10:30 In focus with robotics
10:45–11:00 Techno-College unpacked
11:15-12:15 Session broadcast: Honoured Guest
14:00–14:15 What to expect as a Resident at the Annual Meeting
14:30–14:45 What’s new in innovation
15:00–15:15 WiCTS: Gender Medicine: Under representation of female patients in clinical trials
15:30–15:45
Innovation and sustainability - from emergency to scheduled approach, from nightmare to differential treatment
16:00–16:15 The big debate: centralisation of centres for care
16:30–17:00 Latin Heart Rounds
17:30–18:00 Science Friction
Korkut Bostanci
Nico Bonaros
Polina Danchenko
Wouter Oosterlinck
Joerg Kempfert Niv Ad
Marion Durand
Hazem Fallouh
Jens Krause
Felix Nägele Polina Danchenko
Gowthan Santhirakumaran
Friedhelm Beyersdorf
Joe Bavaria
Can Gollmann-Tepeköylü
Indu Deglurkar Maroua Eid
Gloria Faerber
Daniel Zimpfer
Evgenij Potapov
Jan Gummert
Zuzana Tucnova
Boulos Asfour
Richard Milton
Filip Casselman
Jose Luis Pomar (Moderator)
Lorenzo Galletti
Daniel Pereda
Mateo Marin
Chris Malaisrie
Patrick Myers
Nabil Hussein Maroua Eid
FRIDAY 10 OCTOBER
08:45–9:15
CABG Nightmares – Practical Solutions for Complex Cases
09:45–10:00 Your daily briefing: Friday
10:15–10:30 In focus with Thoracic
10:45–11:00 Bridging the gap in Allied Health Professional education with industry
Miia Lehtinen
Can Gollmann-Tepeköylü
Miguel Sousa Uva
Virginia Litle
Daniel Zimpfer
Miia Lehtinen
Raphael Bueno
Cristina Ruizsegria
Richard Thomson
Sara Zaher
11:15–12:15 Session broadcast: Presidential Address Volkmar Falk
12:30–13:15 CT Residents Showdown: European Final
Richard Milton Nabil Hussein
13:45-14:45 Session broadcast: Managing DOACs in urgent and emergent scenarios and optimizing secondary prevention — A case-based session
15:30–16:00 Meet the giants in CT Surgery Paul Sergeant
16:15–16:30 Interview with the EJCTS Editor-in-Chiefs Mario Gaudino
17:00–17:15 Francis Fontan Fund and Outreach Programmes
17:30–18:00 Science Friction
SATURDAY 11 OCTOBER
09:45–10:00 Your daily briefing: Saturday
10:15–10:30 In focus with Gloria Farber
10:45–11:00 Next Stop: 2026 & 40 Years of EACTS
11:15–13:30 Session broadcast: EACTS 2025 trial update session
Matthias Siepe
Carlos Mestres
Peter Licht
Alicja Zientara
Florian Schoenhoff
Francesca Gatta
Vladimiro Vida
Luca Di Marco
Soi Avgeridou
Gloria Farber
Rafael Sadaba
Sharon Pidgeon
Nicklas Brendborg & EACTS
The 39th EACTS
Annual Meeting Social Media Ambassadors
Our Social Media Ambassadors for the 39th EACTS Annual will keep you informed of all the latest news from Copenhagen during and after #EACTS2025



SATELLITE SYMPOSIA













Rethinking multivalvular disease: bridging technology and technique, in aortic, mitral, and tricuspid surgery
Structural Heart Innovation | Science, Clinical Experience & Landmark RCT
Aortic Manipulation in Modern Cardiac Surgery: When Not to Clamp, When to Clamp, When to Cut


THE ROLE OF THE SECRETARY GENERAL
The Secretary General of EACTS plays a crucial role in representing cardiothoracic surgeons and the future direction of the Association. We spoke with the current Secretary General of EACTS, Patrick Myers (Zurich University Hospital in Switzerland) about his roles and responsibilities, achievements and future challenges...
As Secretary General, what are your key duties and responsibilities?
My main duties and responsibilities are to serve as the voice of the Council. I'm the one who has an overview of all that's going on within EACTS, overseeing the strategic direction and acting as an external representation of the Association. That means that I have to lead some of the major initiatives, such as the annual meeting, our educational programmes and, along with Council, organise our strategic vision for the next five years. I work very closely with the Executive Committee, Council and our Windsor office to make sure that we align our mission and our strategic plan, as well as representing EACTS in collaborations with other surgical societies around the world, other specialties such as cardiology, being in contact with regulatory bodies, and working with our partners in industry.
I'm a practising cardiac surgeon and so I have to fit this in around my schedule. Luckily, I have a fairly adaptable schedule so I can commit enough time to taking care of what EACTS needs, but at the same time, being in the operating room, so I have enough time to dedicate to my patients, and family.
And what particular skill set do you need to perform this role?
The role requires balance – a mixture of a strategic vision and practical leadership. During the pandemic, we were a ‘bare bones’ Association, and the Windsor staff was at a minimum, and as an Association, we were not far from disappearing. However, with the help of my predecessor, Professor Rafael Sádaba, we rebuilt the team in Windsor, and we now have a completely professionalised team. This allows us to focus on our strategic vision, think about how we develop our Association and specialty, and how we want to help our members to get better outcomes for the patients.
What skills do I need? It helps that I am Swiss – as the role requires communication and diplomacy! We have developed very close relationships with the other surgical societies around the world, producing guidelines and position statements, etc. Importantly, we also have a much closer relationship with the cardiology associations. Overall, the role requires that I have an understanding of policy, education and surgical innovation because that is crucial to the future direction of our Association, and what our members need to improve their practice.
What do you believe you've achieved so far, and what do you hope to achieve in the next three years?
I'm very proud of what we've achieved so far. Firstly, EACTS is a team, and we really can rely on our fantastic membership and our outstanding professional staff in Windsor. These are not my achievements, but a recognition that our members give their time to take on different roles for the benefit of the Association. For example, under the leadership of Friedhelm Beyersdorf and Mark Hazekamp,
we have developed the ‘Innovation Hub’ that was part of our strategic plan. We have also developed the Francis Fontan Fellowships, under the guidance of Ruggero De Paulis and Peter Licht, and others, so now we have a fantastic offering of fellowships to our members.
I am also proud that we have strengthened our global collaborations with surgical and cardiology associations so that we're now working together for our patients, developing educational programmes together, for example, in Latin America. We're now looking to develop that in Africa. I think EACTS is often seen as an ‘old boys club’ and that it's always the same people who get positions within the Association. What I have strived to do is to address issues around governance and transparency, to improve how we operate internally, to develop a professional behaviour policy and to have an open process for all the nominations within the Association, so that everybody can feel included.
As a charity, we only function because people are willing to give their free time on a voluntary basis to commit to doing extra work for our specialty. It's incredibly rewarding to do that, but it's not always easy to find people who can do that on a consistent basis. I am very proud of our membership - we have so many members who are interested and really energised to give back to our specialty – who are not driven by gaining any personal benefits from their roles within the Association.
But we have much more to do. For example, women are under-represented within our specialty, so we have to help them in mentoring so that they reach, so that everybody can reach, that level where they can contribute back to the specialty through EACTS. It is not instantaneous and it takes years of developing these relationships and mentoring. For instance, myself, Rafael Sádaba (current vice president of EACTS), Matthias Siepe (Editor-inChief for the European Journal of CardioThoracic Surgery), and Peyman Nia (Editor-inChief – Interdisciplinary CardioVascular and Thoracic Surgery journal) were all serving together in the Resident’s Committee 15 years ago, and we all continued working within the Association. To improve and continue this development, we have ensured the Residents’ Committee is part of our Programme Committee for our annual meeting.
If our residents can see what work is involved in developing our annual meeting, the largest cardiothoracic meeting in the world, then at this very early stage in their career, they can participate and contribute to it, and become involved in sessions that are innovative, thought-provoking and with completely different formats.
What do you most enjoy or find most rewarding as Secretary General?
The people - I get to work along some of the most passionate, innovative, dedicated individuals in cardiothoracic surgery, from residents, early career surgeons to the most senior thought leaders. There is this real

energy, and that energy shapes the future of our specialty. It's a privilege to serve a community that's so committed to excellence in patient care and science.
And what do you find most frustrating about the role?
They are only 24 hours in a day and sometimes I just don't have the time to respond to all of the mountains of emails I get every day, even if my goal is to get my inbox back to zero! We have lots of ideas and lots of passionate people making these ideas happen, but change takes time, particularly in such a large international organisation. Sometimes the pace of progress feels a little bit slower than it should be. But, I've learned that persistence, patience and partnerships go a long way in building these lasting improvements. I am very proud of where EACTS is today. I hear so much positive feedback from people, that is quite rewarding.
"I've
learned that persistence, patience and partnerships go a long way in building these lasting improvements. I am very proud of where EACTS is today. I hear so much positive feedback from people, that is quite rewarding."
How important are the team in Windsor and Council in helping you achieve your goals and aims as an Association?
They are absolutely essential. Our Windsorbased staff perform all the operational day-to-day functions, allowing Council to focus on our wider strategic goals. The team in Windsor are highly professional, very committed and working behind the scenes - they’re the ones who really make everything run smoothly. Council is essential to my role in that I consider each member as a mentorpeople whom I can bounce ideas off and learn from. As an organisation, we are striving to have representation from all around Europe and to be as gender diverse as we can be. To achieve these goals, Council offers invaluable support, advice and feedback for these important initiatives, and others that we're working on.
What do you believe are the major challenges that face our speciality over the next decade?
Our five-year strategic plan highlights several key challenges – crucially, that we need to train and retain the next generation of surgeons. The growing complexity of patient care requires multidisciplinary collaboration. In addition, we need to face the challenges from the rapid pace of technological change, especially from the transcatheter therapies and artificial intelligence (AI). We need to
understand how these technologies are going to impact our specialty. There is a lot of pressure for transcatheter therapies, and the data from the early results are very good, however, the long-term results are questionable, as we have seen with coronary stents in the past. Therefore, we need to ensure that the training and education that we deliver evolves ‘in step’ with these innovations. In addition, we need to gather more data to strengthen our quality improvement programme to ultimately improve clinical practice and outcomes for our patients. Finally, it’s important that we not only represent surgeons but we must continue to advocate for our patients and what are the most effective therapies, particularly as we have a rapidly evolving healthcare system throughout Europe.
As an experienced cardiothoracic surgeon, what advice would you offer to a young cardiothoracic surgery trainee? The future is bright. There are so many different innovations in cardiothoracic surgery today, and the specialty is going to grow over time. It will change, but it's the most rewarding specialty. There are very few jobs where you can actually hold your patient's heart in your hands. That's quite a responsibility. So, I would say to a cardiothoracic trainee: ‘Stay curious, stay humble, stay connected, learn from every case, learn from every colleague and also learn from every one of your mistakes. You'll make some mistakes along the way, you'll make many, so learn from those’. Residents should seek mentors, not just one; they will need several mentors who'll challenge them, but who will also support them.
There are many ways to build a career. I never thought that I'd be a private practice surgeon. I always thought that I would be an academic congenital surgeon. Don't think that there's just one career that's lying ahead of you, there are many - be it in clinical practice, research, education or leadership. But remember, the patient comes first, whatever you're doing. The patient is the most important person in your career. If you do good to your patients, all the rest will fall into line.
How do you relax in your spare time? I like spending time with my children, although now that they're adolescents, they do their own thing more and more. But seeing them grow into their own little people is such a joy. I'm a keen runner and run a half marathon three or four times a year. I have run one marathon, but clearly that's too long a distance for me! I'm in Switzerland, so I like going hiking in the mountains. I love getting lost in a nice book, and I just finished reading reading Craig Smith's ‘Nobility in Small Things: A Surgeon's Path’.
I would like to say to our members, please become an active participant in EACTS - we'd love to have you contribute in whatever way you can. The more you contribute, the more EACTS will grow and become useful for all our members. So, please help out if you can!


