

DAILY NEWS





COLLECTIVE BEHAVIOUR AND INTELLIGENCE
In a fascinating presentation at yesterday’s Honoured Guest Lecture, behavioural biologist Professor Jens Krause (Professor for Fish Ecology in the Faculty of Life Science at the Humboldt University Berlin, Head of D epartment at the Leibniz-IGB), explained how collective behaviour - decision-making in animal groups - has produced many insights and applications for problems in the human domain such as algorithms for improved medical diagnoses and solutions for human crowd management.

In his talk, ‘Collective Behaviour and Collective Intelligence in Animals and Humans’, Professor Krause showed how simple individuals can achieve sophisticated tasks like coordinated movement, resource acquisition, and problem-solving that are beyond the capabilities of any single member.
Professor Krause and his colleagues have investigated how groups of animals (e.g., fish, birds) and humans coordinate their movements and decisions. While why they live in groups is understood, how they achieve coordinated movement (e.g., choosing direction, leadership) has been a mystery.
A central model explains group dynamics based on three social forces between individuals: 1) Zone of Repulsion: Individuals
maintain personal space around themselves; 2) Zone of Orientation/Alignment: Individuals tend to face in the same direction as nearby group members and; 3) Zone of Attraction: Individuals are drawn towards other group members further away. This model suggests that local interactions between individuals, where each pays attention only to close neighbours, can lead to global order and coordinated group movement.
In order to demonstrate how ‘a leader’ can influence individuals, his team developed an interactive robotic fish which is recognised by live fish as a conspecific and their experiment showed that the fish would follow the lead of the robotic fish. This experiment was replicated in humans and showed that people successfully guided the group without the others realising they were being led (this was even replicated successfully live on television).
Interestingly, in scenarios with conflicting information (e.g., 10 individuals instructed towards one target and 20 towards another), the conflict was almost always resolved in favour of the majority (the 20 individuals), without any explicit discussion among the group.
Professor Krause said the real-world implications of these findings include crowd dynamics, building safety (improve evacuation efficiency in emergencies) and conflict management (particularly

Chairs and Faculty:




Vinod Thourani
Michael Borger
Christian Carranza
Jessica Forcillo
EACTS TV
Watch live and recorded content from this year's Annual Meeting on EACTS TV, featuring compelling panel debates, highlights and interviews with the world’s leading cardiothoracic surgeons.
Learning Labs
Take advantage of the invaluable opportunity to train with some of the world’s best cardiothoracic surgeons at the EACTS Learning Lab. Our hands-on workshops are designed to advance your technical abilities and include wetlabs, drylabs, simulation and practical sessions.
Satellite Symposia
Join experts as they discuss the latest clinical data, current and future approaches to patient care and much more in a wide range of satellite sessions hosted by industry.

in managing demonstrations and de-escalating conflicts).
More relevantly, his research has shown that pooling independent judgement can improve medical diagnostics (Wolf M, Krause J, Carney PA, Bogart A, Kurvers RHJM (2015) Collective Intelligence Meets Medical Decision-Making: The Collective Outperforms the Best Radiologist. PLoS ONE). In this study, they investigated the performance of three well-known collective intelligence rules (“majority”, “quorum”, and “weighted quorum”) when applied to mammography screening. For any particular mammogram, these rules aggregate the independent assessments of multiple radiologists into a single decision. They found that, compared to single radiologists, any of these collective Intelligence-rules both increases true positives (i.e., recalls of patients with cancer) and decreases false positives (i.e., recalls of patients without cancer), thereby overcoming one of the fundamental limitations to decision accuracy that individual radiologists face. Therefore, collective intelligence may have the potential to improve medical decision-making in a much wider range of contexts, including many areas of diagnostic imaging and, more generally, diagnostic decisions that are based on the subjective interpretation of evidence.
His research has also found that size matters - as the group size of fish increases, the group dramatically improves their ability to survive (identify actual predators), whilst also making faster decisions as group size increases. However, additional studies have shown the opposite is true in humans, they tend to make worse and slower decisions as the group size increases.
In a personal anecdote, he cited the example of how a car nearly hit him as he automatically went to cross the road after the person next to him stepped forward. This, he said, highlighted how easily one can be influenced by others and that automatic cognitive mechanisms are at play when people copy observed actions (e.g., assuming a green light when someone else starts moving).
Professor Krause currently works within an excellence cluster in Berlin, ‘Science of Intelligence”, which brings together diverse disciplines (biology, psychology, medicine, computer science, engineering) to develop AI. Their core goal is to identify common principles between biological and artificial intelligence, based on

‘abstract intelligence principles’.
“Our idea of intelligence is very much informed by human behaviour and we think intelligence is what brains do, what neural systems do. But if you want to find commonalities between biological and artificial intelligence you need to move away from this viewpoint,” he concluded. “What could this look like? Well, life is defined by metabolism, responses to stimuli, reproduction, development, adaptation and so on, the big question is - what properties define intelligence, regardless of whether it is biological or artificial?"

A SNAPSHOT OF FRIDAY'S SESSIONS
08:30 - 09:30 Room 180/181
EACTS/EBCP - Circulating factors in perfusion
10:00 - 11:00 Hall A3
Type A IMH - A treacherous snake – ASCVTS @ EACTS session
10:00 - 11:00 Room 180/181
2025 ERAS/EACTS joint session: Advancing enhanced recovery after cardiac
11:15 - 12:00 Hall A1
Presidential Address
15:15 - 16:15 Hall A3
Specific situation in the ROSS procedure
15:15 - 16:15 Hall A1
EACTS/EAPCI - Hybrid revascularization – The best or worst of both worlds?

AN INTERVIEW WITH PROFESSOR MARKO TURINA
Yesterday, EACTS recognised one of the true pioneers, not only of cardio-thoracic surgery, but of the Association itself, by bestowing upon Professor Marko Turina an EACTS Lifetime Achievement Award. We spoke with Professor Turina about his journey from his decision to pursue medicine and surgery, through his innovative contributions to cardiac surgery, the establishment of a major European professional body and his reflections on the specialty's future.
As a young medical student at the Medical School at the University of Zagreb, Croatia, he soon developed dexterity and ability in experimental surgery, which sparked his interest in surgery. However, due to political circumstances, he was forced to leave Croatia after graduating from medical school, as he knew he could not pursue a career there.
“In 1961, I was forced to leave Croatia after graduating from medical school for purely political reasons. I was very anti-communist, coming from a conventional religious family, and I knew that I would be unable to pursue any career in Croatia,” he explained. “So, I started looking for a place to train as a student, and I had the offer from Switzerland, a small hospital in Flawil. After graduating, I wrote to the head of the University Hospital of Zürich, and they accepted me for surgical residency.”
After completing his Surgical Residency, he became a Research fellow in Biochemistry, in the Department of Pharmacology at the University of Zurich and then in 1967 became a Fellow in Cardiology at the University and a Resident in 1969. However, he wanted more advanced training and knew the place to be was
the United States.
“In 1969, the United States was absolutely the best place to go to further my training. I spent two years in the States, primarily as an Assistant Research Surgeon at the University of California, San Diego, in experimental surgery. I found the US offered the best working conditions, and although I was moderately paid, I received significant research funds of US$500,000 to develop a pump oxygenator for use in infants and newborns. At that time, it was absolutely impossible to perform open heart surgery on newborns as the priming volume of the pump oxygenators was about two litres and the infant’s blood volume was about 400 millilitres. So, it was impossible to control the perfusion. I spend a large part of my time working on a solution, and I was given very generous support by the University of California, San Diego.”
Challenges
and rewards
Developing the infant pump oxygenator, he added, was one of the most challenging yet rewarding times of his career. His device facilitated the first open-heart surgeries on infants worldwide. Another challenge was developing a so-called ‘paracorporeal artificial heart’ to support circulation in myocardial infarctions and post-cardiac surgery complications, which took him two to three years of intensive work until he could achieve long-term survivals.

rewarding. Outside of the operating theatre and research laboratory, in 1985 I became a full professor and Director of the Clinic for Cardiovascular Surgery at the University Hospital Zurich and continued in that role until 1994, when I became the Dean of the Medical School. I am the only Croatian graduate who ever became a Dean of the Medical School in Switzerland, which is quite an achievement!”

“Of course, as a doctor and as a surgeon when, you have success, when one child after other survives, when one patient after another survives, that is a tremendous satisfaction, very
The formation of EACTS
The formation of EACTS, was conceived with Francis Fonton at a US meeting, recognising the need for an international European platform for scientific exchange in cardiac surgery. After consultations with leading European surgeons, the first meeting was organised in Vienna in 1987, attended by 450 delegates. Humble beginnings for a meeting that Professor Turina acknowledges has “grown to become the largest and most important cardiothoracic surgery meeting globally.”
Visit our booth #37
Gain first experience for Endoscopic Vessel Harvesting (EVH) and Off-Pump Coronary Artery Bypass (OPCAB) Surgery at our hands-on station and engage in a peer-to-peer exchange with our clinical experts.

“The European Association for CardioThoracic Surgery was basically born out of a talk which I had with the Francis Fontan - at that time one of the leading cardiac surgeons in Europe - at a meeting in Baltimore. We both sat during lunch break and talked about how ridiculous it is that we have to travel to the United States to hear new work and to present our work. At that time in Europe, there were scientific meetings in the UK, Scandinavia, France, Germany and so on, but there was no international one. So, we decided we should try and create one.
“Professor Fontan and I selected a group of leading cardiac surgeons in Europe and asked their opinion in various countries. At that time,
we decided that membership in EACTS would be a kind of distinction for leading cardiac surgeons, similar to the American Association of Thoracic Surgery, although this was changed in later years. In the beginning, it was tough going. I wrote to about 800 prominent cardiothoracic surgeons in Europe, asking if they would like to join the meeting and become members, and about 450 came to the first meeting in Vienna in 1987. Since then, it has gone from strength to strength.”
Looking back on his career, Professor Turina offered two pieces of advice to any young medical trainee thinking about becoming a surgeon.
“Firstly, it’s important to select the proper place for your training with a top surgeon who is also devoted to teaching, which is not a simple thing. Many excellent surgeons don't teach at all. Secondly, if you want to make a scientific career in academic medicine, then spend at least one or two years in another closely related field like immunology or similar and then this will put you on the proper path in scientific development.”
Finally, he spoke about the future of the specialty, which he believes is undergoing a rapid evolution: “Cardiothoracic surgery is changing rapidly, and mostly because of the emergence of transcatheter techniques. The challenges of the future will be developing ever more minimally invasive technologies and techniques, and it is paramount that if cardio-thoracic surgery is to continue as a specialty - surgeons are at the forefront of developing the next-generation of both transcatheter and endoscopic surgical approaches.”

Founding fathers: Front row: Marko Turina and Francis Fontan. Second row: Hans Huysmans, Ramiro Rivera, Hans Borst, David Wheatley, Keyvan Moghissi, Louis Couraud, Maurizio Cotrufo, Ingolf Vogt-Moykopf
President Volkmar Falk presents Marko Turina with his EACTS Lifetime Achievement Award

LUNCH SYMPOSIUM
FRIDAY, OCTOBER 10TH, 12:15 PM - 1:30 PM, ROOM 18 & 19


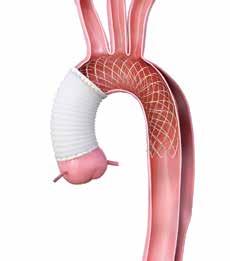
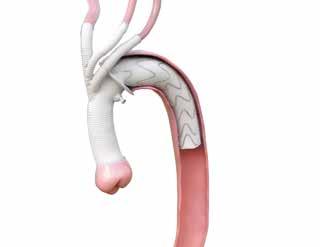
The PERSEVERE Study: One-Year Results of a Novel Aortic Arch Hybrid Prosthesis for Open Repair of Acute DeBakey Type I Dissection with Malperfusion
Dr. W. Szeto (Philadelphia, United States)
AMDS™ in DeBakey I Acute Dissection: A Hybrid Approach
Mr S. Grant (Manchester, United Kingdom)


Zone 0 Frozen Elephant Trunk: The Mainz Experience
Dr. D.-S. Dohle (Mainz, Germany)
Hybrid Arch Repair Redefined: Intermediate Results with an Available Branched FET Device
Prof. M. Pichlmaier (Munich, Germany)
Endovascular Arch Repair: Expanding the Toolbox for Cardiac Surgeons
Prof. A. Martens (Oldenburg, Germany)
World Leader in Aortic Arch Solutions



AN INTERVIEW WITH THE PRESIDENT

EACTS Daily News spoke with EACTS President, Professor Volkmar Falk (Medical Director and Director of the Department of Cardiothoracic and Vascular Surgery of the German Heart Center Berlin) about his career, his influences, the challenges facing the cardiothoracic surgery and his love of music...
Did you always want a career in medicine?
Actually, I never planned to study medicine. I wanted to become a journalist, and while I was at school, I was already writing for newspapers. After finishing school, it was mandatory in Germany at that time to do either military or civil service. Back then, I was a conscientious objector for military service and opted to work for a hospital in the ICU.
Working in the ICU gave me some fascinating insights into the medical work, and I decided to study medicine. However, medical school was rather disappointing as it was totally organized along school lines. It was not until I met my great friend and mentor, Friedrich Mohr, that I really saw my future in medicine. I was looking to do a doctoral thesis and started working with Friedrich in Bonn. When he decided to move to the University of Göttingen, it was an easy choice to join him – not because he was doing cardiac surgery – but because he was such a charismatic leader. I just felt that under his guidance, I would learn so much, and the right opportunities would emerge.
Why did you choose cardiac surgery?
First of all, you do something meaningful that has an impact on and can improve somebody else’s life. This is, at the same time, exciting and rewarding. Cardiac surgery attracted me because there’s an element of meticulous manual work that leads to an immediate result. I wouldn't go as far as to say it's an art, but it's certainly a craft that you can master with a lot of training and gaining experience. Another aspect, especially in cardiac surgery, is the time constraint; you are always working against the clock, adding a dimension of urgency. The combination of doing a complex manual task in a limited time was, and remains, appealing to me.
Who was the great influence on your career?
This is a difficult one, as I had the privilege to work with outstanding surgeons and researchers in Göttingen, Leipzig, Zurich and Berlin and many exceptional members of our international community who shared their knowledge and skills with me. But without a doubt, Friedrich Mohr has had the greatest influence on my career in cardiac surgery. Two years after I wrote my doctoral thesis with him and moved to Göttingen, he was appointed the Chief of the Leipzig Heart Center. Friedrich had built a great team around him, and I, along with five colleagues, had no hesitation in moving with him to Leipzig.
DO NOT MISS!

Since we had to build a new Heartcenter from scratch, there was a special atmosphere in the team. At the time, this part of former East Germany was still underserved with cardiac surgery, and we saw an immediate growth that by far exceeded all expectations. Importantly, we were all very open and keen to innovation, and as a result, a lot of new technologies and techniques were developed in Leipzig, much earlier than in other places in Germany. Among them are minimally invasive mitral valve repair, the use of anastomotic connectors, off-pump surgery and robotics, to name a few.
I believe that one of the key factors of our success as a group was not only our innovative spirit but also the fact that we cared for each other. Even in times of a personal crisis when you couldn't be as scientifically proliferative as you wanted to, the
Professor Volkmar Falk’s Presidential Address
Hall A1 11:15-12:00
team would help you through this. In particular, I would like to mention here my very close friend, Thomas Walther, who helped me a lot. Our careers developed side-by-side, and he has always supported me at difficult times in my life. He really was that one person who kept my career going.
What experience in your training or your career is the most valuable lesson?
I think the most valuable lesson that I have learnt from my former leaders is that when you delegate a task, then delegate it! You must trust that your team members can take responsibility. However, you must be available for back-up in case something goes wrong, and without blaming, you take on the burden together. In many ways, we learn more from our failures than our

Volkmar Falk (centre) with Friedrich Mohr (right)
successes, and when you fail, you need people around you to help you find a solution. I think that this lesson everyone from the Leipzig team learnt early in their careers. Having some sort of professional safety network around me helped me to take responsibility, but also seek advice and guidance when I was struggling. What advice would you offer to a young cardiothoracic surgery resident?
The best advice I can give is not to try to make your way through the system by yourself, but to try to find people to collaborate. Even if peers may be competitors at some stage of your career, try to form a team to make everyone grow. It is much easier to succeed as part of a team than on your own. I would also say it is important to know your limitations, but in an incremental and safe way, continuously challenge yourself to improve over time.
What do you think are the biggest challenges facing the specialty in the next decade?
There are many challenges. A lot of therapies are now shifting from open surgery to transcatheter techniques. Younger surgeons, therefore, need to acquire wire skills. If, as a specialty we want to stay in the game – these skills must become part of our curriculum. Senior surgeons must acknowledge that the new generation of surgeons must accomplish these tasks and enable them to do so. As more and more patients are treated interventionally, we are facing a growing number of more complex cases, who, after a couple of heart valve or coronary interventions, still require surgery.
The ageing population and demographic change will not only add to surgical complexity in an older and more comorbid population, but also result in a dramatic lack of workforce. Cardiac surgery, with its demanding on-call services and high demand for skilled physicians and allied health professionals, is particularly vulnerable to this development. The limited financial resources that all health care systems are facing add another dimension to the problem. The challenge will be to continue to deliver high-quality cardiovascular care with constantly diminishing resources. This is a major burden and a real challenge for the next generation.
What are your current areas of research?
From the start of my career, I was mainly involved in clinical research. The fields of minimally invasive surgery and off-pump surgery caught my early interest. From the beginning, I was very involved in robotics. During a research fellowship at Stanford University, I was working very closely with robotic companies to develop the basics of robotic coronary and mitral valve surgery. As a result, we performed the first clinical TECAB and mitral cases in Leipzig. I was also involved in one of the first transcatheter valve programs in Europe and the development of image-guided valve therapies.
Throughout my career, I've always worked very closely with engineering schools and technical universities because I was interested in developing new technologies and bringing them into clinical practice. This constant effort has also led to a professorship for translational cardiovascular technologies at the ETH in Zurich.

Among other research groups in Berlin, we have a very busy clinical and experimental research group in the field of mechanical circulatory support, which also benefits largely from close collaborations with engineering schools.
I'm actively involved in trial networks in Europe and in the US to organize investigator-initiated trials. Performing clinical trials can be really arduous at times, but I think it is by far the best way to generate new knowledge and to fill the current gaps of evidence.
For the past 15 years, I have been involved in the writing of European guidelines, which is not only very interesting but also very impactful. With one operation, you may change the life of one patient, but by writing a guideline, you may change medical practice, which can have an impact on many patients. In addition, I found it to be a great privilege to work within guideline task forces with the best experts in the respective field to evaluate the current evidence and to define the best practice for patients.
As EACTS president, what are the most rewarding and challenging aspects of the position?
First of all, it's a great honour and a reward of more than twenty-plus years that I have been working with EACTS. I presented my first international abstract at an EACTS annual meeting. I was a very young and very nervous resident and was excited to give my first lecture in English at an international meeting. I remember it was in a small room in the corner, so no

one really took notice, but I was very proud.
During the following years, I have never hesitated to take any position that was offered to me at EACTS. I was running the Techno College for many years, I served in the council for many years, and I was EACTS Treasurer for some time. Serving now as the President of our Association is something that I could not have imagined when I presented my first abstract many years ago.
EACTS is, without doubt, the best place for the scientific exchange and education in cardiac surgery on the planet, and I say that knowing what other organizations are capable of. I think the way EACTS has evolved over the last couple of years is remarkable, and that the unique way it brings international colleagues together has made the annual meeting the most successful in this field.
A particular challenge for the upcoming years is the need to secure the position of cardiac surgery in Europe and worldwide. Together with Council and the General Secretary, we are working very hard to constantly improve our connection with the European Society of Cardiology, our cardiology friends and partners. At the same time, we are increasing our transatlantic collaboration with STS, ATS and LACES, as we try to align and work together on certain projects and strengthen the position of cardiac and thoracic surgery internationally.
Another big challenge is to continuously develop the EACTS Quality Improvement Programme. We now have a professionalised data management team, and the goal is to connect as many centres throughout Europe in order to produce meaningful data that reflects the current practice and can serve as a benchmark for quality outcomes in cardiac surgery.
We also need to reinforce the interest in our specialty among the young and brightest residents, because we need them to enter cardiac surgery. There's a lot of competition with other specialties and we have to make sure the specialty stays attractive for young surgeons, in particular for female surgeons. A career in our specialty means long hours, night shifts, and weekend work, so you need dedication. We therefore need to stop lamenting about the decline of cardiac surgery and rather emphasize the merits of our specialty. The message that we need to send out is that the future of cardiac surgery is bright and offers excellent opportunities and career pathways for our residents.
Finally, how do you relax away from surgery?
I love and like to play music. I also write music, and with my various bands have recorded six albums so far. We produced the latest two records on vinyl, a very interesting process that turned out to be a lot of fun. We also produced a video for one of the songs, which is certainly more fun than making a video of a surgical case.
With our cover band, we played in Barcelona for the EACTS 30th anniversary. Playing gigs, performing your own original work at small venues here in Berlin or elsewhere, is, however, an even more rewarding experience. Excellent surgery is the result of a great team effort – so are great musical moments. Thanks to my surgical team and my band, I have experienced both.
15:15 - 16:15
12
Machine learning models using intratumoral and peritumoral radiomics for postoperative survival prediction in esophageal squamous cell carcinoma
Esophageal squamous cell carcinoma (ESCC) remains one of the most fatal malignancies globally, with East Asia accounting for 90% of cases. While esophagectomy is a primary treatment, predicting postoperative survival accurately is critical for guiding clinical decisions— particularly in determining whether neoadjuvant therapy is necessary, as it may be associated with adverse side effects. The current TNM staging system, though widely used, is limited by its reliance on pathological parameters, failing to capture tumor heterogeneity. Our study addresses this gap by developing machine learning (ML) models that integrate intratumoral and peritumoral radiomic features from preoperative CT scans, offering a new prognostic tool.
We retrospectively analyzed 443 ESCC patients who underwent esophagectomy at our institution between June 2016 and January 2020, all with preoperative contrast-enhanced CT. Patients were randomized into a training set (354 patients) and a test set (89 patients) at an 8:2 ratio. The cohort had a median age of 66 years, with 68.2% male, and most tumors were located in the middle thoracic esophagus (54.2%).
A key innovation was our focus on both intratumoral and peritumoral regions. Two radiologists used 3D Slicer to manually delineate regions of interest (ROIs): intratumoral ROIs included the primary tumor, while peritumoral ROIs encompassed

Zhi-Qiang Deng1, Chen Yang2, Hong Tao Tang3, Hao-Ji Yan4, Dong Tian,1
1 West China Hospital, Sichuan University, Chengdu, China; 2 North Sichuan Medical College, Nanchong, China; 3 West China Hospital, Sichuan University, Chengdu, China; 4 Juntendo University School of Medicine, Tokyo, Japan
surrounding lymph nodes and connective tissue (excluding major structures like the aorta). Using PyRadiomics, we extracted 851 radiomic features from each region. These features were refined through rigorous selection: excluding those with low interclass correlation coefficient (ICC < 0.85), retaining those linked to survival via Kaplan-Meier analysis (P < 0.05), and further filtering using variable importance (VIMP) and Cox regression. Notably, peritumoral features dominated the final selection—14 of 17 key features originated from peritumoral regions—
Elimination of Hemodynamic Changes During Ex Vivo Lung Perfusion Improves Dynamic Compliance

Ex vivo lung perfusion (EVLP) involves ventilating and perfusing lungs outside of the body, allowing for longer preservation, evaluation of lung function, and treatment of donor organs. Standard EVLP protocols have either utilized 100% of calculated cardiac output (CO) (ex. Lund Protocol) or lower CO targets between 30-50% (ex. Toronto Protocol).
High CO targets have been associated with increased edema formation while low flow protocols have largely resulted in lung failure. Our center’s established EVLP protocol involves perfusion of lungs
during EVLP at 30% cardiac output with evaluations performed every three hours at 50% of cardiac output. It is unclear if this increase in cardiac output improves V/Q mismatch, or if it is deleterious to the lungs. In this study, we compared our standard negative pressure ventilation EVLP protocol with evaluations performed at 50% cardiac output to a modified protocol without an increase in cardiac output during evaluations.
The perfusate used during EVLP was comprised of common hospital ingredient perfusate (CHIP) and autologous packed red blood cells with Piperacillin-Tazobactam (3.375 g), heparin (10,000 IU), and methylprednisolone (500mg). Lung protective ventilation was employed with tidal volumes of 6-8 mL/kg, a respiratory rate of 6-8 bpm, PEEP of 5-8 cmH2O, and an FiO2 of 21%.
Every three hours, an evaluation was performed. The standard/control protocol involves increasing flow from 30% to 50% CO and applying mixed sweep gas through the de-oxygenator for five minutes during evaluations. The experimental protocol only applies the mixed sweep gas with CO
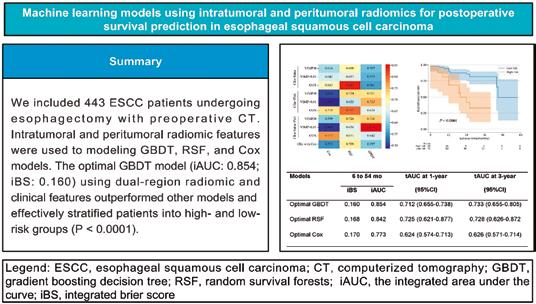
highlighting their underappreciated prognostic value.
We developed 27 models using three ML algorithms: gradient boosting decision tree (GBDT), random survival forests (RSF), and Cox regression, combined with radiomic and clinical features (preoperative complications, T stage, hemoglobin, and AST). The optimal model, a GBDT integrating dual-region radiomics and clinical features, outperformed all others. It achieved an integrated area under the curve (iAUC) of 0.854 and an integrated Brier score (iBS) of 0.160, indicating strong discrimination and calibration. For timespecific predictions, its 1-year time-dependent AUC (tAUC) was 0.712 (95% CI 0.655–0.738), and 3-year tAUC was 0.733 (95% CI 0.655–0.805). Importantly, it effectively stratified patients into high- and low-risk groups (P < 0.001), a critical tool for personalized risk assessment.

maintained at 30%. Standard lung performance characteristics were regularly assessed, including PF ratio, pulmonary vascular resistance (PVR), dynamic compliance, minute ventilation, and percentage lung weight-gain. Dynamic compliance was significantly improved in the experimental group that did not receive higher flows during evaluations. The control group’s dynamic compliance decreased after each subsequent evaluation after six hours. Similarly, minute ventilation was significantly higher in the experimental group compared to the
This study underscores two key findings: peritumoral radiomics carry significant prognostic information, reflecting tumor invasion and immune microenvironment changes that are invisible to the naked eye on CT; and ML algorithms, particularly GBDT, outperform traditional Cox regression by capturing nonlinear relationships in highdimensional data.
Clinically, this model can help clinicians identify low-risk patients who may avoid neoadjuvant therapy (reducing side effects) and intensify surveillance for high-risk individuals. Limitations include its singlecenter design and lack of neoadjuvant therapy patients, which we aim to address in multicenter studies. By leveraging both intratumoral and peritumoral radiomics, our ML model advances ESCC prognostic prediction, moving toward more precise, patientcentered care.
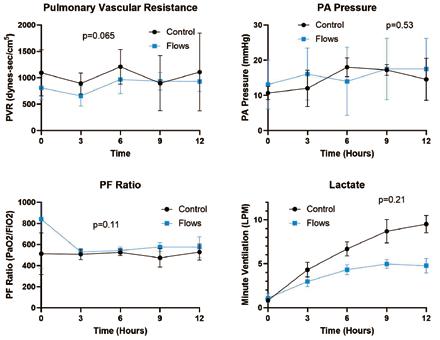
control group.
Other measures, including PVR, pulmonary artery pressures, PF ratio, and lung weight gain (72.7% weight gain for the control group, 77.1% for the experimental group), were not significantly different between groups. While lactate did not differ significantly between groups, lactate did climb more rapidly in the control group compared to the experimental group, which was performed without higher cardiac output evaluations.
Higher cardiac output targets have been associated with increased rates of edema formation, while low flow protocols have largely resulted in
early lung failure. Moderate flow perfusion targeting a CO between 20-40% of predicted CO has generally allowed for stable, prolonged EVLP. Despite their limited duration, temporary increases in CO during evaluations result in lung injury, impairing dynamic compliance, ventilation, and increasing lactate formation over 12 hours compared to a consistent CO of 30%. Modification of future protocols to eliminate hemodynamic modifications with higher CO may help to further prolong EVLP duration by reducing lung injury and improving ventilation.
Figure 1. Central image of the study.
Ryaan EL-Andari University of Alberta, Alberta, Canada
Small change, big impact: Refining the TTSS for better prognosis in blunt and polytrauma chest injuries
Blunt chest trauma remains a significant contributor to trauma-related morbidity and mortality worldwide, particularly when it occurs as part of a complex polytrauma. Rapid and accurate risk stratification is essential for guiding early interventions, optimizing resource use, and improving patient outcomes. Among the available tools, the Thoracic Trauma Severity Score (TTSS) has long been valued for its ability to correlate injury severity with prognosis.
However, clinical experience — especially in high-volume trauma centers — has revealed a persistent gap between TTSS predictions and actual outcomes in certain patient populations. This discrepancy is most evident in polytrauma cases, particularly those with concomitant head injuries, where systemic factors beyond thoracic injury itself can significantly influence prognosis.
This observation formed the basis of our research, presented during the Young Investigator Award session at EACTS 2025. We conducted a retrospective analysis of 302 patients with blunt chest trauma admitted to the cardiothoracic and trauma surgery units of our institution. Each patient was scored using the original TTSS, which incorporates the number of rib fractures, presence of pulmonary contusion or hemothorax, respiratory status, and age.
The problem became clear: while the TTSS remained effective for isolated thoracic injuries, its predictive performance declined sharply in patients with additional injuries, particularly traumatic brain injury. In these scenarios, the original TTSS underestimated the severity and failed to accurately stratify patients into appropriate risk categories.

Our proposed solution was intentionally simple — a minimal but targeted refinement of the TTSS by incorporating two readily available clinical parameters: n GCS points (derived from the Glasgow Coma Scale) n BMI points (derived from Body Mass Index) The rationale for these additions is straightforward. The GCS captures the systemic impact of neurological injury, which is a major determinant of outcome in polytrauma. BMI, meanwhile, reflects the physiological reserve and metabolic stress response, which are increasingly recognized as important factors in trauma prognosis.
To illustrate the impact, consider the case of a 45-year-old male motor vehicle accident victim with multiple rib fractures, pulmonary contusion, and a mild subdural hematoma. The original TTSS classified him as moderate risk, suggesting a relatively favorable prognosis. Yet, in practice, his recovery was complicated by prolonged ventilation and ICU stay. When scored with the refined TTSS — which accounts for his reduced GCS and elevated
Beyond the Tumour: ImmuneInflammatory Predictors of Recurrence in Young Patients with Resected NSCLC
In recent years, lung cancer in younger adults has emerged as a distinct clinical entity, marked by different histological and molecular features, more frequent advancedstage diagnoses, and a potentially more aggressive biological behaviour. However, limited data are available on prognostic factors in this population, especially following curative-intent surgery. Our multicentre study aimed to explore how immune-inflammatory biomarkers and tumour-related variables influence early and brain recurrence in young patients with resected NSCLC.
While most clinical prognostic models are designed for older patients, younger individuals with NSCLC may have different biological drivers of recurrence. Understanding which factors, clinical, pathological, or systemic, might predict relapse in this population is crucial to inform surveillance strategies and adjuvant treatment decisions. Specifically, we hypothesised that both tumour immunophenotype (i.e. PD-L1

expression) and systemic inflammation markers (i.e. neutrophilto-lymphocyte ratio, NLR) could help stratify recurrence risk beyond conventional TNM staging. This retrospective analysis included 173 young patients aged ≤50 years who underwent anatomical resection for NSCLC across three Italian thoracic centres. The median age was 46 years, and 64% were female. Most patients had adenocarcinoma histology (78%),
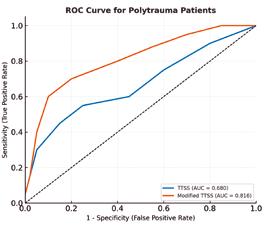
ROC curves comparing the original TTSS and Modified_TTSS for predicting mortality in polytrauma patients (n = 152). The Modified_ TTSS demonstrates significantly superior discriminatory power (AUC = 0.816) compared to the original TTSS (AUC = 0.680), with a statistically significant difference (DeLong’s test p < 0.0001).
BMI — he correctly fell into a high-risk category, prompting earlier ICU admission and more aggressive monitoring from the outset.
Statistical validation confirmed the clinical impression. Using logistic regression and ROC curve analysis, the refined TTSS achieved a significantly higher area under the curve (AUC) for predicting ICU admission, need for ventilation, and 30-day mortality. In the polytrauma subgroup (n = 152), the AUC for mortality prediction improved from 0.680 with the original TTSS to 0.816 with the modified version — a statistically significant difference (DeLong’s test p < 0.0001). This enhancement was particularly striking in patients with overlapping injury patterns, where accurate early triage is most critical.
Beyond the numbers, the clinical implications are substantial. A more accurate scoring system allows for: n Earlier and more appropriate ICU triage
n Better resource allocation in busy trauma centers
n Improved communication with patients’ families regarding prognosis
n More informed decision-making by multidisciplinary teams working under time pressure
Importantly, the proposed refinement does not require new equipment, specialized training, or additional invasive procedures. Both GCS and BMI are universally available in the first minutes to hours of trauma care, making the updated TTSS immediately implementable in a wide range of healthcare settings.
We see this as a step toward a broader principle: trauma scoring systems must evolve in parallel with shifts in injury patterns, patient demographics, and treatment capabilities. The original TTSS was developed in a different era of trauma care; its core remains valid, but its adaptability will determine its continued relevance.
Next steps will include a multicenter prospective study to validate the refined TTSS in diverse trauma systems and geographical contexts. Our hope is to build a collaborative network of cardiothoracic surgeons, trauma surgeons, and emergency physicians to refine, test, and eventually standardize this model internationally.
In conclusion, blunt chest trauma — especially within the context of polytrauma — demands nuanced risk assessment. By adding just two simple, universally available parameters, the refined TTSS delivers a meaningful leap in prognostic accuracy. This seemingly minor adjustment transforms an already valuable tool into a more robust and reliable predictor, ultimately supporting better patient-centered outcomes. We invite colleagues from across the EACTS community to join us in validating and implementing this model, with the shared goal of reducing trauma-related mortality worldwide.
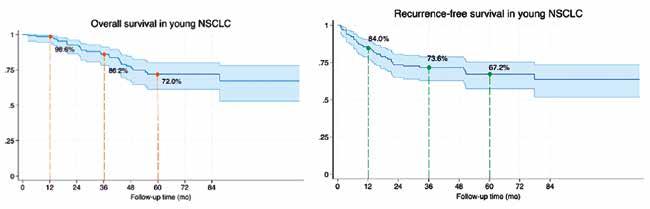
and the majority were clinical stage I (58%).
The primary endpoints were early recurrence (within 24 months) and brain recurrence as the first site.
After a median follow-up of 60 months, disease recurrence occurred in 42 patients (28%).
Among them, 50% experienced early recurrence, and brain metastases were the first site of relapse in 18 out of 21 early recurrences—highlighting the disproportionate burden of brain involvement in this subgroup.
Multivariate analysis showed that high PD-L1 expression (≥50%) and elevated NLR (≥2.45) were independently associated with early recurrence, having a 5.5-fold increased risk of early relapse.
These findings suggest that
systemic inflammation, as reflected by NLR, may contribute not only to tumour relapse but also to metastatic organotropism, particularly brain involvement. Interestingly, patients with high PD-L1 and NLR combined had the shortest median time to recurrence (13.5 mo).
Brain recurrence remains a devastating event for young patients. In our cohort, nearly one in four recurrences involved the brain, often without prior locoregional relapse. This underscores the need for closer surveillance protocols, possibly including routine brain imaging in selected high-risk individuals.
Our results advocate for a riskadapted strategy based on readily available biomarkers. Since both PD-L1 and NLR can be obtained pre- or perioperatively, their
integration into decision-making algorithms is feasible in routine clinical practice.
The clinical message is clear: not all early-stage NSCLC in young patients behaves benignly. Even among those considered low-risk by traditional criteria, inflammation and immune escape may silently drive recurrence. Incorporating biomarkers such as PD-L1 and NLR could support clinicians in (a) Tailoring follow-up intensity, (b) discussing adjuvant therapy in borderline cases, and (c) identifying candidates for immunotherapy trials.
Future prospective studies are warranted to validate these findings and explore whether modifying inflammatory status pre- or postoperatively can improve longterm outcomes.
Noha Fouda Mansoura University Faculty of Medicine, Mansoura, Egypt
Debora Brascia
Humanitas University, Milan, Italy
13:45-14:45
Is it time to revise the 2020 European mesothelioma guidelines?

Camillo Forlanini Hospital, Rome, Italy
Pleural mesothelioma (PM) is the most common form of mesothelioma, accounting for 65-70% of all cases. The incidence of PM is barely growing, with 2,417 new cases/year worldwide.
Despite asbestos having been banned in Europe since 2005, the incidence rate per 100,000 people has been reported as 0·9 for men and 0·3 for women in the USA, and as 1.7 for men and 0.4 for women in Europe.1 With an average reported lifespan from diagnosis of 9–12 months,1 malignant pleural mesothelioma is one of the most aggressive cancers, with platinum and pemetrexed chemotherapy2 the mainstay systemic treatment for early-stage resectable disease despite its modest effect on survival. In the last decades (20102020), an increase in stage I disease (from 13.5% to 15.6%) and patients who were offered treatment (from
71% to 76%) has been noticed.
According to the 2021 WHO classification of tumors of the pleura, mesothelioma can be categorized into three major types: 1)Mesothelioma in situ: recently recognized as a precursor of PM, with a median time to progression of 60 months; 2) Localized pleural mesothelioma: a solitary, localized mass that can be radically resected as in surgical specimen the borders appear circumscribed.; 3)Diffuse pleural mesothelioma, which can be divided into a) Epithelioid mesothelioma: 68-69% of cases. Median survival of 9-14 months; b) Sarcomatoid mesothelioma: 18-19% of cases. Median survival of 4-6 months; c) Biphasic mesothelioma: 12-13% of cases. Median survival of 10 months.
The latest edition of TNM (9th TNM) incorporates changes proposed in the clinical (c)T but not in the pathological (p)T component. The importance of pleural thickness measurements has been underlined, specifying that both size (total thickness) and extent of the primary tumor (involvement of anatomic structures) are mandatory in defining distinct T categories with respect to OS. Fissure involvement has been introduced in both (c)T and (p)T as a significant parameter, though
non-transmural invasion of diaphragm (T2), lung parenchyma (T2), and endothoracic fascia (T3) have been removed as T descriptors because they cannot be precisely determined based on CT.
No changes in N and M descriptors have been introduced. Stage grouping is defined as follows: Multimodality treatment is the cornerstone of therapy. Surgery has an important role in diagnosis, staging, treatment and palliation of PM patients, even if its role has been evaluated in multiple trials, mainly MARS (Treasure, Lancet Oncol 2011), MesoVATS (Rintoul, Lancet 2014) and MARS2 (Lim, Lancet 2024).
The most recent MARS2 trial has opened a significant chaotic debate on the role of surgery in mesothelioma, with several centres now adopting an approach where surgery is not utilised for surgery for all mesothelioma patients, on the basis of worsened survival with surgery in MARS2. However, some major concerns arose have been identified in the study design: one in seven patients had a non-epithelioid subtype; the clinical assessment was based on CT-scan only, no PET-CT was delivered; more than 80% of patients had the diaphragm resected; 18% of patients had a pT4 disease;
6% of patients had pN2 and 5% had cM1 disease. Moreover, a high 30–90-day mortality rate (3.8 and 8.9% respectively) was reported with a considerable number of low-volume centres involved in the trial and a significant rate of R2 resection.
In 2020, the ERS/ESTS/EACTS/ ESTRO guidelines for the management of malignant pleural mesothelioma were published by a Pan-European multidisciplinary and multisocieties team led by A. Scherpereel simultaneously in ERJ and in EJCTS. It was a tremendous effort. Since the publication of the European guidelines, many studies have changed the scenario of malignant pleural mesothelioma.
The three-year outcomes of Checkmate 743 RCT, published in Ann Oncol 2022 by S. Peters et al, showed that with non-epithelioid tumors the median overall survival (OS) was 18.1 months (95% CI, 12.2-22.8) in the nivolumab plus ipilimumab arm compared with only 8.8 months (95% CI, 7.4-10.2) in the chemotherapy arm
The phase 3 MARS-2 trial (NCT02040272) -published in Lancet 2024 by Eric Lim at al.- performed in the United Kingdom showed that at a median follow-up of 22.4 months, patients treated with chemotherapy alone had a longer median overall survival of 24.8 months (interquartile range [IQR], 12.6-37.4) compared with those who underwent surgery followed by adjuvant chemotherapy at 19.3 months (IQR, 10.0-33.7). The difference in restricted mean survival time at two years was -1.9 months (95% CI, 3.4 to -0.3; P =.019). Additionally, chemotherapy was linked with better quality of life and lower costs in the study.
Genetic mutations, particularly in the BAP1 gene, are present in up to 14% of patients and have been linked to both the development of mesothelioma and patient prognosis. Identifying these mutations can inform treatment decisions and provide insights into familial cancer risks. For such a reason, the ASCO recently updated the Mesothelioma guidelines
Giuseppe Cardillo
BECOME A MEMBER OF EACTS TODAY!
Why become a member of EACTS?
As part of our global community, you’ll gain access to world-class resources, expert-led training and a network of professionals driving innovation in cardiothoracic surgery.
Apply now to become a member of EACTS and enjoy access to all the below membership benefits.
Connect
Network with peers at the EACTS Annual Meeting – the leading global event in cardiothoracic surgery
Access exclusive member-only rates for events
NEW: EACTS mentorship programme
Learn
Free access to the European Journal of Cardio-Thoracic Surgery (EJCTS)
Reduced rates to contribute to the Interdisciplinary Cardiovascular and Thoracic Surgery journal (ICVTS)
Free access to EACTS educational webinars
Preferential rates for EACTS Academy training
Apply for exclusive fellowships and bursaries
Advance
Join task forces and committees shaping surgical standards and practice
Be part of initiatives supporting women, early-career clinicians and Allied Health Professionals
Free access to the Adult Cardiac Database
Apply for Outreach Grants
Apply for Innovation Grants
Vote at the General Assembly and help shape EACTS’ future.
Full active members pay just €300 a year.
Visit the Membership Team on the EACTS Booth in the Exhibition Hall to find out more or apply online here >>

Highlights of the Innovation Summit
‘Disruptive innovations’ at EACTS: Thinking outside the box

Friedhelm

Mark
“The term ‘Disruptive Innovation’ describes a process by which a product or service takes root in simple applications at the bottom of the market - typically by being less expensive and more accessible - and then relentlessly moves upmarket, eventually displacing established competitors.” It was first coined in the early 1990s by Harvard Business School Professor Clayton Christensen.
The annual EACTS Innovation Summit showcases ground-breaking innovations while also highlighting the challenges, particularly in regulation and finance, by fostering collaborations with businesses and academic institutions, the Summit aims to support the development of promising innovations. EACTS Daily News spoke with Professor Friedhelm Beyersdorf (Chair of the EACTS Innovation Committee) and Professor Mark Hazekamp (Deputy Chair of the EACTS Innovation Committee) who explained the meaning of ‘disruptive innovation’ and how innovations could change the future of cardiac surgery… “It is very important to understand what the terms ‘innovation’ and ‘disruptive innovation’ mean, because innovation can mean different things to different people. For most people, innovation means improving existing techniques, which, of course, is very important and must be supported. However, cardiac surgery was born out of ‘disruptive innovations’, by our grandfathers in cardiac surgery who did incredible and pioneering experiments, that created the specialty that we know today,” Professor Beyersdorf explained. “The main idea behind the Innovation Committee and Innovation Summit is to look outside the profession of cardiothoracic surgery to find new ways, new insights and new ideas that can help us to make
cardiothoracic surgery better than it already is.”
For example, Professor Hazekamp highlighted six innovation sections, namely, Artificial Intelligence (AI) + Immersive Technologies for CT Surgery, Extracorporeal Life Support/Cardiopulmonary Bypass/ Mechanical Circulatory Support, Lymphatics/ Glymphatics, Perioperative Cellular Protection and Organ Repair, Robotics Surgery and Valves of the Future, that reflect the main goals and main topics they are focused on.
“We believe that there are huge potential opportunities for cardiac surgery in AI, synthetic biology, robotics, nanotechnology, quantum technology and others, to improve patient outcomes after cardiac surgery. Surgery is still very traumatic; patients have to stay in the intensive care unit, and they need a long recovery,” Professor Hazekamp added. “But, we really have to make this better, and we really need to look outside the borders of our specialty.
For this reason, we invite people from completely other disciplines to the Innovation Summit, people who are experts in nuclear physics, biology and even economics, just to give us new insights and to make us think outside the typical box of cardiac surgery.”
Innovation Summit
The first Innovation Summit was held in April 2023 and the fourth Summit will be held in April 2026. The key to the meeting is to foster exchange between the participants. To encourage this exchange, the meeting is held in a remote place - not at an airport or in a hotel in the middle of a city. This means participants are together from breakfast to lunch to dinner, and they talk to each other all the time, all day long. The two-day meeting consists of presentations and abstracts, followed by many questions and discussions – with far more time allocated than attributed at traditional conferences. The Summit is restricted to about 80 people, with different people and specialties invited to attend,
who bring new ideas and new ways of thinking.
“The reason we invite people from completely different professions to so we can stimulate our colleagues to think in a completely different direction. The idea is that this new way of thinking, this new approach will enable us to start new approaches to surgery by listening to what other professions are doing, what kind of revolutions are happening in other industries, what can we learn from them and ultimately, can we apply these changes to enact a revolution in our field?” said Professor Beyersdorf. “It is important to note that this is not like the Techno-College, which traditionally highlights innovations to products that are already being used in a clinical setting. Our goal is to speak about the phase before that, for example, about prototypes that are being tested in animal labs, etc.”
The 2025 Innovation Summit was attended by engineers, scientists, surgeons, cardiologists and industry leaders from around the world and highlighted the latest advancements and research taking place across many scientific fields, from molecular hydrogen treatment and adventitial lymphatics to digital twins. The two-day meeting featured high-profile presenters, including Karl Jakobs, Chair of CERN, who discussed fundamental research in particle physics at CERN and applications in medicine, and Björn Schuller, Professor of Artificial Intelligence at Imperial College London, who explored challenges, breakthroughs and the boundless potential of AI in medicine and surgery.
To encourage innovation, the 2025 Innovation Summit awarded grants to the best four ‘disruptive innovations’ and the recipients are returning to the 2026 meeting to present what they have done with the money, what they have achieved, etc. The four recipients of EACTS innovation grants presented their work at this year’s Summit. Each grant recipient received €25,000 and benefits from advisory collaboration with the EACTS’ Innovation Committee Advisory Board.
“I believe the future of cardiac surgery is very exciting because change will not come from one technique or product; change will come from multiple very beneficial new developments taking place simultaneously. What will this change look like in reality? This means perioperative trauma and perioperative core mobilities will definitely decrease over the next decade. I believe advances in less invasive technologies, less blood transfusion, and having more insights into the cause of perioperative comorbidities will improve patient outcomes.”
2025, with 17 abstracts selected for presentation at the Summit.
The future
We believe that there are huge potential opportunities for cardiac surgery in AI, synthetic biology, robotics, nanotechnology, quantum technology and others, to improve patient outcomes after cardiac surgery…We have to be patient because it takes some time to safely develop these disruptive innovations. We are just at the beginning of a new era, and we are really encouraged by what we have seen so far.”
Innovation Grants – Apply Now!
The EACTS Innovation Hub was established to encourage and support disruptive developments in cardiothoracic surgery. The Hub consists of our esteemed “Innovation Committee”, access to EACTS’ own research and clinical networks, professional advice on project methodology and exclusive access to our new Innovation Grants Programme. The EACTS Innovation grant programme is intended to support early-stage, pump-priming and ‘stimulation’ research and innovation opportunities. With funding of up to €50,000 each, the EACTS Innovation Grants offer a chance to bring bold ideas to life and make a meaningful impact on cardiothoracic surgery. Funding requests will be considered for projects
This year’s recipients of the awards will present at this year’s EACTS Annual Meeting in the ‘Highlights of the Innovation Summit’ session. The successful recipients were:
n Daniel Zimpfer, Marcus Grannegger and Krishnaraj Narayanaswamy (Department of Cardiac and Thoracic Aortic Surgery, Medical University of Vienna, Austria),
n Edris Mahtab (Cardiothoracic Surgeon & Associate Professor, Leiden University Medical Center, The Netherlands)
n Joeri Van Puyvelde, Piet Claus, Elizabeth Jones, Ruth Heying, Sarah Thomis and Bart Meyns (Universitair Ziekenhuis Leuven, Belgium); and
n Tommi Pätilä (Associate Professor, Consultant in Paediatric Heart Surgery and Organ Transplantation at HUS, Helsinki; Co-founder of SpectroCor)
In addition, there are also prizes for the best abstracts presented at the Summit. Over 70 abstracts were submitted for consideration in
relevant to one or more of the EACTS Innovation priority themes, and will be assessed through established peer review processes, including members of the EACTS Innovation Committee. Through this initiative, we aim to inspire the next generation of cardiothoracic surgery advancements and harness the power of research and innovation to secure better outcomes for patients.
Strategic themes
n The Future of Robotic Surgery n Heart Valve of the Future
“I believe the future of cardiac surgery is very exciting because change will not come from one technique or product; change will come from multiple very beneficial new developments taking place simultaneously. What will this change look like in reality? This means perioperative trauma and perioperative core mobilities will definitely decrease over the next decade. I believe advances in less invasive technologies, less blood transfusion, and having more insights into the cause of perioperative comorbidities will improve patient outcomes,” Professor Beyersdorf highlighted. “For example, AI will also definitely change surgery in general in many, many aspects, both preoperative, intraoperatively and postoperatively. We are working to decrease ICU time, and maybe in 20 years, we will not need the ICU at all. That's our long-term crystal ball wish.”
“In ten years’ time, I predict that a patient with a valve problem will be evaluated by artificial intelligence so that we really know what to do in the OR, we have a surgical plan ready and that we will not need to improvise. Then he or she will be operated on by a minimal invasive approach - so no big incisions, no transfusions, no need for the ICU, no lengthy recovery, no need for rehabilitation. That would be our final goal,” added Professor Hazekamp. “Of course, we have to be patient because it takes some time to safely develop these disruptive innovations. We are just at the beginning of a new era, and we are really encouraged by what we have seen so far.”
n CPB, ECLS & MCS
n Artificial Intelligence for CT Surgery
n Perioperative Cellular Protection and Single-and MultiOrgan Repair
n Lymphatics in CT surgery
Applications opened on 1st October and will close on 1st December 2025. Please note that if your application is successful, you will be required to attend and present at the Innovation Summit (23 – 25 April 2026). In order to apply for an Innovation Grant, you must be an EACTS member. Should you require any further information or assistance, kindly email: InnovationHub@eacts.co.uk
Beyersdorf Chair of the EACTS Innovation Committee
Hazekamp Deputy Chair of the EACTS Innovation Committee
Functional outcome after recurrent laryngeal nerve injury following aortic surgery
Over the years, significant advances in surgical techniques and perioperative care have improved outcomes and reduced complications in aortic surgery. While neurological complications such as stroke and spinal cord ischemia have been extensively studied, data on recurrent laryngeal nerve (RLN) injury remain limited.
Within the broader field of thoracic aortic surgery, the reported incidence of RLN injury varies considerably, primarily depending on the type and anatomical extent of the procedure. The right RLN, which loops around the subclavian artery, is rarely injured except during interventions involving the brachiocephalic trunk at its bifurcation with the right carotid artery. By contrast, the left RLN, looping around the aortic arch and ligamentum arteriosum, is at much greater risk during operations involving the arch and proximal descending thoracic aorta. Retrospective analyses have reported incidences ranging from 1% in ascending aortic and hemiarch procedures to over 20% in extensive arch and descending aortic surgeries. The diagnosis of RLN injury is indirectly established through the detection of vocal cord paralysis on laryngoscopy. Patients typically present with hoarseness and impaired vocal function, which, if persistent, can significantly affect their quality of life. In more severe cases, dyspnea and aspiration may also occur, potentially leading to pneumonia.
Study overview
This study, presented at this year’s EACTS

Fabio Pregaldini
Paul Potratz, Eberhard Seifert, Maria Nucera, Selim Mosbahi, Murat Yildiz, Maris Bartkevics, Matthias Siepe, Florian Schoenhoff
Inselspital, Bern University Hospital, Switzerland
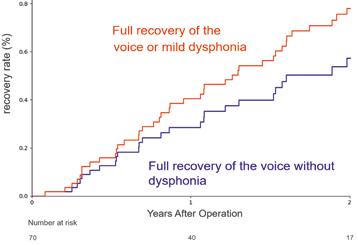
Figure: Voice recovery after recurrent laryngeal nerve injury following aortic surgery. Legend: The blue line represents patients with full recovery, while the red line shows the cumulative incidence of patients who achieved either full recovery or mild dysphonia.
Annual Meeting, aims to evaluate not only the incidence of RLN injury after aortic surgery but also the recovery rates and functional outcomes during follow-up.
We performed a retrospective single-center analysis of patients who underwent aortic arch or thoraco-abdominal surgery at Inselspital, Bern University Hospital, between 2001 and 2024. Aortic arch surgery was defined as any type of hemiarch or total arch replacement, while thoraco-abdominal procedures included those involving the proximal descending thoracic aorta. Patients were included if postoperative RLN injury was confirmed by laryngoscopy.
The primary endpoint was full recovery of voice function. Secondary endpoints included the degree of residual dysphonia, the need for speech therapy, and the requirement for interventional procedures on the vocal cords.
Results
During the study period, 2,983 patients underwent aortic arch or thoraco-abdominal
aortic surgery. Of these, 70 patients (2.3%) presented with RLN injury confirmed by laryngoscopic examination. Median follow-up was 17 months.
When stratified by type of procedure, the incidence of RLN injury was 1.7% in hemiarch and arch procedures, but considerably higher (5.3%) after thoraco-abdominal surgery. This difference reflects the more extensive anatomical exposure and manipulation required during thoraco-abdominal repairs.
The majority of patients (70%) underwent postoperative voice therapy. In 15% of cases, surgical intervention was required. Of these, 90% consisted of vocal cord augmentation, while a single patient underwent a more invasive medialization procedure. All interventions were performed between 8 and 13 months following aortic surgery, and no procedure-related complications were observed.
After a follow-up of nearly two years, 50% of patients achieved full recovery without residual dysphonia. Mild dysphonia persisted in 30% of
cases, while 13% continued to experience moderate dysphonia and 7% severe dysphonia. Overall, 80% of patients with postoperative vocal cord paralysis showed either complete recovery or only residual mild dysphonia (Figure).
Conclusion
In this large single-center experience spanning more than two decades, RLN injury was identified in 70 patients, corresponding to a complication rate of 2.3% among nearly 3,000 aortic arch and thoraco-abdominal procedures. Importantly, functional outcomes following RLN injury with vocal cord paralysis were generally favorable. Most patients benefited from speech therapy, while a subset required interventional procedures on the vocal cords. These findings highlight the importance of prompt recognition of RLN injury, systematic follow-up, and a multidisciplinary management strategy involving speech therapists and otolaryngologists.
Overall, RLN injury remains a relatively uncommon but clinically relevant complication of aortic surgery. Given its impact on phonation and quality of life, any postoperative vocal dysfunction, such as hoarseness, should prompt laryngoscopic evaluation. In cases of confirmed vocal cord paralysis, patients should be referred to a specialized otolaryngology team for structured voice therapy and, when indicated, interventional treatment. Future studies are needed to refine incidence estimates and define optimal management strategies, ultimately improving both patient outcomes and long-term quality of life after these complex surgical procedures.
I would like to sincerely thank Prof. F. Schoenhoff and Prof. M. Siepe, as well as Prof. E. Seifert from the ENT Department, for their invaluable guidance and support throughout this work.

08:30–09:30 Auditorium 15 Abstract
Dark sides & warm rides: Is cardiopulmonary bypass necessary for grafting posterior wall targets in robotic TECAB?
Minimally invasive coronary artery bypass grafting is well established, and most often applied for single-vessel grafting (LIMA to LAD) via a minimally invasive direct coronary artery bypass (MIDCAB) approach. Another technique is robotic beating-heart TECAB - totally endoscopic coronary artery bypass - the least invasive form of coronary bypass grafting. One notable benefit of TECAB is the ability to more easily and readily perform multivessel grafting, given the dexterity and visualization afforded by the robot. A sometimes perceived concern regarding minimally invasive CABG is the potential for incomplete revascularization, particularly for non-LAD targets, especially those on the posterior wall.
At our institution, robotic beating-heart TECAB using the Endowrist stabilizer is performed for a wide range of coronary targets, with over 50% of cases being for multivessel grafting. We reviewed our experience grafting posterior wall targets — defined as distal obtuse marginal (OM2/OM3) branches, posterior descending artery (PDA), or posterolateral branches (PLB) — using a left-sided robotic TECAB approach. We consider these targets to be on the “dark side” of the heart.
Between August 2013 and April 2025, 959 robotic beatingheart TECAB procedures were completed; 134 involved at least one posterior wall target grafted with an internal thoracic artery (ITA) conduit. All operations were performed through left chest ports in our standard TECAB fashion1,2 by a single surgeon and team; all current anastomoses are performed using a robotic running suture technique.1,3
In 134 TECAB cases involving posterior wall grafting, the mean age was 66 years, 16% were female, and the mean STS PROM risk score was 1.3%. The majority were performed as part of multivessel grafting (88%); of these, BITA use was 85%. All cases were performed on a beating heart. CPB without cardiac arrest (“warm ride”) was required in only five patients (3.7%) for hemodynamic support during target exposure. There were no conversions to sternotomy.
Early outcomes in this group were favorable: low complication rates (atrial fibrillation 13%, stroke 0.8%, acute kidney injury
08:30 -

Sarah Nisivaco
Husam H BalkhyMcGaw Medical Center of Northwestern University, Chicago, USA
0.8%), short ICU (mean 1.1 days) and hospital LOS (mean 2.3 days), no take-back for bleeding, and a 97% discharge-to-home rate. There was one early mortality in the group (0.8%). Longterm follow-up was complete for all patients, with mean follow-up of 45 months. Overall survival was 85%, cardiac-related mortality was 3%, and repeat cardiac surgery occurred in one patient (0.8%). Freedom from major adverse cardiac and cerebrovascular events (MACCE) was 92%.
Our findings indicate that in an experienced program, posterior wall targets are not a contraindication to robotic beating-heart TECAB. Indeed, the ability to graft these targets when needed can help achieve complete revascularization, particularly in patients with large/dominant posterior wall vessels and when PCI cannot be performed on these targets.
This series adds to our previously published work on robotic TECAB in multivessel and high-risk populations, including patients with diabetes, advanced age, and elevated STS risk scores.4-5 We continue to demonstrate that careful patient selection, a standardized approach, and a dedicated team are key to achieving reproducible results, even in complex cases or more difficult grafting strategies, such as that described here.6
This study demonstrates the feasibility and safety of posterior wall grafting via a robotic beating-heart TECAB approach and a low incidence of requiring CPB. While posterior wall grafting during beating-heart TECAB requires advanced robotic and off-pump skills, it can be incorporated into routine practice in experienced TECAB centers for select patients. As robotic technology continues to evolve and, importantly, the robotic endowrist stabilizer becomes available in newer generation systems, broader adoption of these techniques will become feasible – thus expanding the potential patient population who can benefit from a sternal-sparing revascularization approach.
Beating heart revascularization: A comparative study of microaxial flow pump devices
Recent guidelines recommend surgical revascularization for patients with severely reduced left ventricular ejection function (LVEF), despite the recognized increase in perioperative risk. In this challenging population, on-pump beating heart coronary artery bypass grafting offers a potential strategy to reduce the adverse effects associated with conventional cardioplegia and off-pump surgery. In recent years, micro-axial flow pumps such as the Impella devices have emerged as valuable tools for providing circulatory support both intraoperatively and postoperatively, representing a promising option for high-risk patients with severely impaired LVEF. A new approach, known as Impella-supported coronary bypass (ISCAB), may offer a promising solution for high-risk patients with severely reduced LVEF. However, the optimal type of Impella device for use in ISCAB procedures remains uncertain. This study aims to assess the optimal type of Impella devices (CP/5.0/5.5) for use in these procedures, assessing their impact on ventricular unloading, hemodynamic stabilization, and associated clinical outcomes within 30 days postoperatively.

Johannes Gutenberg University Mainz, Mainz, Germany
This subanalysis of a multicenter, observational, retrospective, non-randomised study aims to determine the optimal Impella device type for ISCAB in patients with severely reduced LVEF. The analysis focuses on evaluating the device’s impact on ventricular unloading, hemodynamic stability, and 30-day postoperative outcomes.
Between 2017 and 2023, six European centers enrolled 70 patients with ischemic cardiomyopathy and an LVEF between 20% and 35% who underwent ISCAB. Data were collected on baseline characteristics, perioperative variables, and postoperative complications, particularly their impact on 30-day mortality. Low cardiac output was defined as hemodynamic instability persisting despite inotropic therapy and/or Impella support.

References
1. Nisivaco S, Kitahara H, Bhasin R, Patel B, Coleman C, Balkhy HH. A decade of robotic beating-heart totally endoscopic coronary bypass (TECAB) at a single institution: Outcomes with 10-year follow-up. J Thorac Cardiovasc Surg. 2025;169(6):1753-1760.e3.
2. Nisivaco S, Bhasin R, Kitahara H, et al. Bilateral internal thoracic artery grafting in robotic beating-heart totally endoscopic coronary artery bypass: 10-year outcomes. Ann Cardiothorac Surg. 2024;13(4):354-363.
3. Balkhy HH, Nisivaco S, Hashimoto M, Torregrossa G, Grady K. Robotic Total Endoscopic Coronary Bypass in 570 Patients: Impact of Anastomotic Technique in Two Eras. Ann Thorac Surg. 2022;114(2):476-482.
4. Balkhy HH, Nisivaco S, Kitahara H, McCrorey M, Patel B. Robotic Beating Heart Totally Endoscopic Coronary Artery Bypass in Higher-Risk Patients: Can It be Done Safely? Innovations. 2018;13(2):108-113.
5. Kitahara H, Hirai T, McCrorey M, Patel B, Nisivaco S, Nathan S, Balkhy HH. Hybrid coronary revascularization: Midterm outcomes of robotic multivessel bypass and percutaneous interventions. J Thorac Cardiovasc Surg. 2019;157(5):1829-1836.e1.
6. Balkhy HH. Robotic totally endoscopic coronary artery bypass grafting: It’s now or never! JTCVS Tech. 2021;10:153-157.
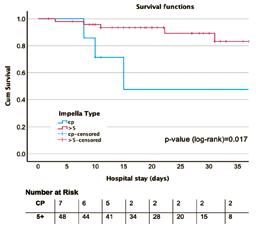
30-day mortality comparison between Impella CP and 5+
The cohort had a mean age of 65.26 ± 9.94 years. Baseline characteristics, including reoperation (p=0.011) and prolonged ICU stay (p=0.022) were associated with 30-day mortality. Rates of post-operative complications, including cardiac resuscitation, reoperation, acute renal failure requiring dialysis, major bleeding, low cardiac output and vascular problems, did not differ significantly by Impella device type. However, when these complications were associated with 30-day mortality, low cardiac output syndrome was identified as an independent risk factor for 30-day mortality (OR 0.373, 95% CI 0.1610.586, p<0.001). In addition, significant differences were observed between Impella devices with higher flow support, with a higher 30-day survival rate (85.7% vs. 57.1%),

LCO as independent risk factor of 30-days mortality
suggesting a potential advantage in hemodynamic support for the most compromised patients.
This study supports the feasibility and safety of ISCAB with Impella support in patients with severe LV dysfunction, who are not suitable candidates for conventional on-pump surgery. While the use of high-flow Impella devices suggests a trend toward improved 30-day survival, it does not show a significant impact on postoperative complications.
In high-risk revascularization cases, careful device selection may influence early outcomes, particularly in mitigating low cardiac output syndrome, a key driver of mortality in this type of patients. Further prospective, randomized studies are warranted to confirm the survival benefit suggested here.
Marta Medina
Evaluation of the effect of intraoperative hypotension on clinical outcomes after off-pump coronary artery bypass
As interest in off-pump coronary artery bypass (OPCAB) surgery continues to grow, driven by its potential to minimize the systemic side effects of cardiopulmonary bypass (CPB), an important intraoperative factor has remained underexplored: blood pressure control. While the benefits of OPCAB such as reduced neurological complications, lower transfusion requirements, and decreased renal dysfunction, are welldocumented, the hemodynamic instability often observed during these procedures poses unique anesthetic and surgical challenges. In particular, the impact of intraoperative hypotension on postoperative outcomes in OPCAB patients remains poorly defined.
In cardiac surgery more broadly, intraoperative hypotension has been repeatedly associated with adverse postoperative events. Studies focused on on-pump CABG patients have demonstrated a clear link between prolonged episodes of mean arterial pressure (MAP) below 60 mmHg and complications such as stroke, renal failure, and delirium. Yet, in OPCAB surgery, where systemic circulation is not augmented by extracorporeal support and cerebral autoregulation may be more vulnerable, the significance of hypotension is likely different, and perhaps more detrimental.
The physiology of OPCAB presents a double-edged sword: while avoiding CPB eliminates many of its harmful effects, it transfers full responsibility for maintaining organ perfusion to the native heart and vascular system during a highly dynamic surgical environment. Manipulations of the beating heart, particularly during distal anastomoses, can induce significant fluctuations in preload, afterload, and contractility. As a result, MAP can drop below critical levels—sometimes for extended periods. Intraoperative anesthetic strategies attempt to mitigate these effects through volume loading, inotropic support, and vasoactive medications, but these measures
are often reactive rather than preventive.
Despite these challenges, guidelines and evidence regarding specific blood pressure targets in OPCAB remain scarce. Much of what we know about safe intraoperative hemodynamics is derived from on-pump literature, where the role of MAP is modified by the continuous and non-pulsatile flow provided by CPB. Translating these findings to OPCAB is problematic, as the absence of extracorporeal circulation exposes organs, particularly the brain and kidneys, to the full effects of hypotension.
To address this knowledge gap, our team conducted a comprehensive investigation into the role of intraoperative hypotension in OPCAB surgery. Drawing from a large cohort of patients undergoing off-pump revascularization at a major European center for cardiac surgery, we examined the association between the duration of MAP <60 mmHg and a composite outcome of major postoperative complications, including stroke, myocardial infarction, acute renal failure, and delirium. Our methodology involved both binary and continuous analyses of hypotension burden, with a focus on doseresponse effects and risk stratification.
Our findings, presented in detail at this year’s EACTS Annual Meeting, are expected to challenge existing assumptions about


Robotic coronary artery bypass grafting (CABG) surgery has faced skepticism, but a decade of Medicare data shows its safety and durability, with evidence of longterm survival.

hemodynamic management in OPCAB. Rather than treating hypotension as an isolated or binary phenomenon, we propose a more nuanced understanding that accounts for the duration of MAP reductions. In our study, even moderate hypotensive episodes showed a measurable association with adverse outcomes, and risk appeared to rise significantly beyond a certain time threshold. Importantly, our analysis suggests that some complications (particularly postoperative delirium) may be more sensitive to hypotension than others, raising questions about the role of cerebral autoregulation and the individual vulnerability of patients.
The implications for clinical practice are considerable. Should MAP be more tightly controlled during OPCAB than previously thought? Are current intraoperative monitoring and anesthetic practices sufficient to detect and respond to meaningful hypotension in realtime? How might perfusion thresholds vary between patients with different comorbidities, such as carotid stenosis or chronic kidney disease? And crucially, is there an evidencebased MAP target specific to OPCAB that balances the risk of over-resuscitation with the need to avoid organ underperfusion?
We believe this study opens the door to a broader conversation about optimizing
intraoperative care in beating-heart surgery. Just as the cardiothoracic community has refined its understanding of myocardial protection, cerebral embolism, and bleeding management over the past decades, it is time to bring equal rigor to the study of intraoperative hemodynamics. While OPCAB avoids the inflammatory and embolic load of CPB, it introduces new variables that must be managed proactively.
As OPCAB continues to gain traction as a minimally invasive strategy, particularly in high-risk and frail patients, individualized blood pressure management may prove to be a key determinant of surgical success. Our findings highlight the need for heightened awareness of intraoperative hypotension and support further prospective research to define thresholds, monitoring techniques, and intervention strategies that can improve outcomes. We look forward to sharing our full analysis — including propensity-matching methods and dose-response modeling — during our presentation at EACTS 2025. We invite surgeons, anesthesiologists, and perioperative care teams to join the discussion on how best to translate these insights into meaningful improvements in patient safety and surgical excellence.
Five-year check-up - Robotic bypass holds its own: Long-term outcomes after single or double vessel robotic coronary artery bypass grafting in the United States
significant difference in 30-day mortality between robotic and conventional CABG (1.3% vs. 2.0%, p=0.112). Stroke was numerically lower with robotic CABG (0.4% vs. 0.9%, p=0.053). Postoperative atrial fibrillation was significantly lower amongst robotic CABG patients (18.8% vs. 22.2%, p=0.007). Median length of stay was shorter for robotic CABG (5.0 [3-6] vs. 5.0 [4-7] days, p<0.001). Rates of bleeding and one-year sternal complications were similar.
At five years, composite rates of death, acute myocardial infarction, or repeat revascularization (PCI or CABG) were comparable between robotic and conventional CABG (30.1% vs. 31.9%, HR 0.95, p=0.45). Importantly, robotic CABG patients had significantly lower all-cause mortality at five-year follow-up (22.0% vs. 25.9%, HR 0.83, p=0.012).
In 12,571 Medicare and Medicaid patients who underwent CABG for single or double vessel disease with left internal mammary artery (LIMA) or bilateral internal mammary artery (BIMA) grafting between 2012 and 2022, 18% had roboticassisted procedures, while 82% had conventional surgery through a sternotomy. In early outcomes, there was no
Despite its promise, robotic CABG has been slow to gain traction in the United States. Surgeons cite the steep learning curve, the cost of equipment, and concerns about long-term durability. Internationally, centers in Europe and Asia have more widely embraced the technology. In this United States Medicare analysis, robotic adoption of single and double vessel CABG grew only modestly over a decade, from 0.9% of CABG cases in 2012 to 1.3% in 2022. Importantly, most patients undergoing CABG in routine practice have multivessel CAD or left main disease, for which conventional CABG via sternotomy remains the gold standard, offering survival benefits that stents and medications alone do not match. Robotic CABG, by contrast, has typically been applied to patients with single or double vessel disease, with few highly experienced centers extending its use to more complex three-vessel cases. Notably, the new findings
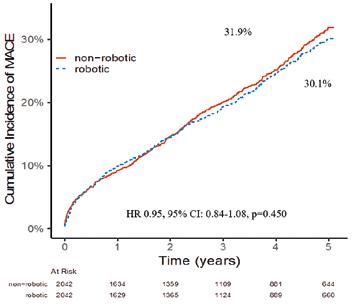
suggest that when performed in experienced centers, robotic CABG can provide those same long-term benefits while offering patients a potentially smoother recovery.
This study provides reassurance to patients and physicians that robotic technology can safely expand the landscape of heart surgery in the U.S with the necessary investments in surgical teams and infrastructure. A decade of data shows that robotic heart bypass surgery isn’t just futuristic – it’s effective and durable. 08:30–09:30
Alaa Abd El Al and Nils Hinrichs
Deutsches Herzzentrum der Charité, Berlin, Germany
Shruthi Nammalwar and Derrick Tam Cedars-Sinai Health Sciences University, Los Angeles, USA
08:30–09:30 Abstract Theatre 2
The silent cost of gender in mitral valve surgery
Mitral valve disease is the most common form of valvular heart disease, and its prevalence is expected to rise with an ageing population. Minimally invasive mitral valve surgery (MIMVS) has emerged as a transformative approach for treating mitral valve disease, offering benefits such as reduced surgical trauma, shorter hospital stays, and faster recovery compared to conventional open-heart surgery. Our new research findings reveal a persistent and measurable gender gap in the treatment of mitral valve disease in patients’ longterm outcomes.
A clear imbalance from the start Between 2010 and 2024, more than 1,500 patients underwent isolated mitral valve surgery at the Department of Cardiac Surgery, Medical University of Innsbruck. Women made up 44% of these cases, yet their profile differed markedly from men’s. On average, women were older at the time of surgery and presented in a poorer clinical condition. They had

Leo Pölzl MCI Internationale Hochschule GmbH, Innsbruck, Austria
significantly higher rates of severe symptoms - 60% of women were in NYHA class III compared with 46% of men - and their NT-proBNP levels, a marker of cardiac strain, were more than twice as high.
Women also presented with different patterns of disease. While men were most likely to present with a less complex form of mitral valve disease (predominantly Carpentier Type II), women more frequently exhibited more complex pathology: five times more cases of Type IIIa and three times higher rates of valve calcification. These anatomical and etiological differences may explain some of the disparities observed in surgical approach and outcomes.
EACTS’ Adult Cardiac Database
Using this data for research and developing databases like the ACD and EUROMACS for the cardiac surgery community, helps to identify best practices contributing to improvements in the quality of care for cardiac surgery patients.
“ My role at EACTS is to oversee, together with Edgar Daeter, the Quality Improvement Programme initiatives that we run at the Association. This consists of working with different hospitals and surgeons to look at how we can use data to generate insights to make improvement in patient management, surgery and care,” explained Paola Quattroni, EACTS
Access to minimally invasive surgery is uneven
One of the most striking findings was the surgical technique used. Minimally invasive mitral valve surgery was used in 65% of men but only 49% of women. Women were more often treated via full or partial sternotomy. Repair rates also showed a gender gap. The rates of valve repair were 85% for male and 67% for female patients. Therefore, women were twice as likely to have their valve replaced due to the intraoperative findings and despite the conduction of the operation by the same experienced surgical team. Even after adjusting for comorbidities, women remained significantly less likely to receive both MIMVS and valve repair.
Several factors may underlie this disparity. Advanced disease due to later referral, more complex disease and higher calcification rates in women may make minimally invasive repair technically more challenging.
The impact on outcomes
These disparities translate into worse results for women. Postoperatively, women spent longer in intensive care and had a significantly higher 30-day mortality rate - 2.8% versus 0.6% in men. Over five years, mortality
Quality Improvement Director. “The ACD is a collaborative registry and benchmarking tool of cardiac surgical data for centres across Europe, supporting the development of evidence-based guidelines to improve pre- and post-operative care. Based on real-world data, the database enables the identification of best practice and promotes the importance of integrating quality improvement initiatives into daily clinical practice.”
The ACD drives improvements by giving surgeons the tools to compare and benchmark their hospital’s data with other centres across Europe. This allows them to identify areas of improvement in their clinical practice, helping to improve patient outcomes. Participation in the ACD is free of charge for hospitals.
Dr Edgar Daeter, cardio-thoracic surgeon at St Antonius Hospital in Niewengein, is the Chair of the Quality Improvement Programme and ACD task force, and has been involved since the inception of the renewed ACD.
“We want to collect a limited but significant amount of data about surgical procedures. The aim is to aggregate this data for surgeons to access via an interactive viewer or tool that shows them graphs so that they can get insights from that data. They will be able to see the different trends of surgical procedures over time against certain patient groups. The interactive viewer is also a benchmarking tool for surgeons to compare their own hospital data and outcomes to data and outcomes from other hospitals. By using risk correction outcomes of types of surgery for patients with selectable risk profiles, outcomes can be benchmarked on a hospital or country level to identify potential

remained higher for women even after propensity score matching on key clinical variables. In the matched analysis, women had a 58% higher risk of death within five years of surgery. However, further analysis suggested that sex itself might not be the direct cause. When outcomes were adjusted for disease type (Carpentier classification) and the need for valve replacement, the mortality difference between men and women disappeared. This suggests that the root cause lies in the underlying pathology and the presence of disease stage-related

improvements for participating hospitals. A surgeon can see if their hospital is an outlier for a particular procedure and examine the reasons why there are differences in outcomes. By looking at the data, it might be the case that they are operating on certain patient groups with comorbidities. For example, through the database, a surgeon can look at length of stays, mortality rates, age, comorbidities etc., across different countries and healthcare systems.
Importantly, by using the database, surgeons will have a unique opportunity to find useful insights and implement improvements at their hospital.”
Dr Daeter explained that now that the database include over 55,000 procedures from about 21 international hospitals and more datasets are expected to be added soon, the QUIP team will soon organise some online community meetings for participant hospitals.
“The ACD and EUROMACS have a research pillar based on a research data request protocol, to ensure trustworthy access to de-identified data. Unique in the protocol is the opting-out system for contributing hospitals. When a research data request is submitted, all participating hospitals will receive the request and will be able to opt out from the research if
complications (e.g. atrial fibrillation, ventricular dysfunction) and how it drives surgical decisions, rather than inherent biological differences in recovery.
Why the difference matters
These findings point to a cycle where women’s distinct disease patterns: more calcification, more functional disease - lead to fewer repairs and more replacements, often through more invasive approaches. Since repair is associated with better long-term survival, the higher replacement rates in women contribute to their poorer outcomes.
Importantly, these differences are not inevitable. While anatomy and disease type can influence surgical options, earlier diagnosis and referral, coupled with techniques optimized for challenging anatomies, could help narrow the gap. Awareness among clinicians, especially referring cardiologists, about how mitral valve disease presents in women and the consequences of delay is essential. Nevertheless, the causes of this disparity are not yet fully understood. To improve outcomes for female patients, further research into sex-specific differences in mitral valve disease is warranted.
they wish. The hospitals will always be able to decide on whether to share their data or not.”
In addition to the databases work, QUIP has another dimension as a registry by briging interested communities together. With the help of the cardio-thoracic surgery community and other international registries we are keen to better understand current collection methods, auditing systems, implementation of GDPR, standardisation of cardiothoracic datasets and preparedness for implementation of the European Health Data Space.
She explained that the new database offers the opportunity to participating hospitals in a more consistent and standardised way, which will help improve data completeness and quality. This means that this data can be used much more effectively to improve best practice and inform patient care. In future, it will be possible to use the database for research. Following a trustworthy and thorough data access request process, researchers will be able to submit their study proposals, and following approval, they will be able to use the data for research purposes. For EACTS members to set up an account and access the ACD, please visit www.eacts.org/ quality-improvement/adult-cardiac-database/
Paola Quattroni
EACTS Quality Improvement Director
Edgar Daeter Chair of the Quality Improvement Programme Committee
EACTS QUIP
Cardiovascular News is the leading source of news and information for specialists in cardiovascular care.

9 DAPT de-escalation New insight on post-PCI anticoagulation

14 Profile Dipti Itchhaporia



Global
study shows disparitywidening in mitral valve disease outcomes
Degenerative mitral valve disease has doubled in prevalence globally over the last 30 years, and though improvements in surgical techniques and advances in transcatheter technologies have led to improvements in rates of mortality, these have arisen in higher income countries—leading to concern over a global disparity in care for patients with mitral valve disease.
These were among the conclusions of research presented at New York Valves 2025 (25–27 June, New York, USA), following analysis of data from the Global Burden of Disease (GBD) study—a worldwide health programme involving more than 14,000 collaborators from over 200 countries—to determine the extent of degenerative mitral valve disease from 1990 through to 2023. Guido Ascione, a cardiac surgeon and research fellow at the Cardiovascular Research Foundation (CRF) in New York, USA, presented the data which assessed the prevalence of the disease according to population-based cohort studies, population surveys and administrative data from health facilities.
For the purposes of the study, degenerative mitral valve disease was defined as an echocardiographic finding of prolapse or myxomatous degeneration of the mitral valve with mitral regurgitation (MR) ≥2, whilst cases of secondary MR, congenital, rheumatic, or those from infectious causes were excluded from the analysis.
Mortality estimates were established using information from death certificates including vital registration and autopsy data, and only cases in which degenerative mitral valve disease was the primary cause of death were taken into consideration, with estimates presented as absolute and age-standardised rates, and countries stratified based upon sociodemographic index (SDI) to determine their relative wealth.
“Primary MR progressively grew over time; from 1990 to 2023 there was a percentage increase in absolute prevalence of
+126%, and in 2023 there were globally 16 million people with primary MR and at least moderate MR,” Ascione said, noting that prevalence was higher in males than in females. Looking at age-standardised rates, Ascione commented that the data pointed to the prevalence of the disease being “actually pretty steady”, suggesting that the main driver of the increase in absolute prevalence can be ascribed to a globally ageing population or a lack of improvement in global diagnostic capabilities (i.e. access to healthcare, screening or echocardiography) over the timespan of the study. “As prevalence increases in age, the rate starts to peak after 60 years of age, and it is the highest in patients that are in between 70 and 74 years,” he detailed. “This means that in 2023, globally there were 11 million people with primary MR that were older than 70 years and four million people were actually older than 80. This has dramatic consequences when
This
has consequencesdramaticwhen we think about treatment algorithms for the future”
Continued on page 3
nerves to modulate the sympathetic signalling between the kidneys and brain to reduce blood pressure. Two devices have been approved by the US Food and Drug Administration (FDA)—the Paradise (Recor Medical) and Symplicity Spyral systems—following(Medtronic) a review of evidence from trials assessing both technologies, evidence that also contributed to the ACC/AHA guideline change. Medtronic’s Symplicity Spyral system is a minimally invasive procedure that delivers radiofrequency energy to
Continued on page 2
Hot and fresh - New techniques in aortic surgery
15:15–16:15 Congress Hall A2 (RR) Rapid Response

Arshad Quadri inQB8 Medical Technologies, Winchester, USA
VERITAS: A novel endo-root aortic stent
“Longevity is worthwhile only if it prolongs youth rather than old age.”
Allexis Carrel (1873-1944)
Since the pioneering days of open-heart surgery and deep hypothermic circulatory arrest, as well as the more recent introduction of newer cannulation techniques combined with retrograde cerebral perfusion (RCP) and antegrade cerebral perfusion (ACP), the treatment of type A aortic dissection (TAAD) has constantly evolved. Despite these developments, the mortality and neurological consequences of surgery remain in the range of 15 to 20% when considering all patient groups. And to add to it, well over 20% of patients are deemed unsuitable for
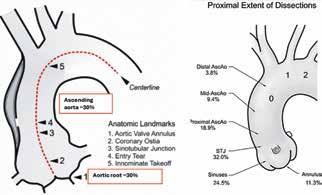
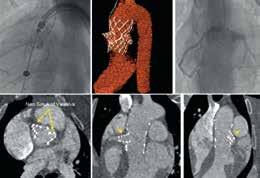
2. Veritas endograft system comprising a tri-leaflet porcine tissue valve with “trapdoor” anchoring in a non-calcified annulus, integrated with a conformable ascending aortic PTFE graft, and the “Chameleon Eyes coronary system
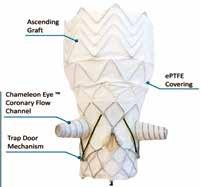
surgical treatment.
At InQb8 Medical Technologies, we have developed Veritas, a novel Aortic-Root and Ascending Aortic stent graft designed to address unmet needs in the treatment of aortic disease. Veritas represents a comprehensive endovascular solution, enabling surgeons to perform a true EndoBentall procedure—a minimally invasive alternative to conventional open surgery. And address all types of TAAD and nondissection pathologies affecting sections A, B &C of Zone 0 of the aorta (Figure 1).
The Endo-Bentall procedure, traditionally performed as open-heart surgery (OHS) with cardiopulmonary bypass (CPB) and deep hypothermic circulatory arrest (DHCS), replaces the diseased aortic root and ascending aorta and
re-implants the coronary arteries. Veritas allows this complex operation to be performed percutaneously through the femoral vessels on a beating heart, avoiding OHS, CPB, and DHCS. Veritas is an aortic valved conduit designed to enable left and right main coronary revascularization by creating neo-coronary sinuses. This innovation restores natural coronary blood flow and lowers the risk of postoperative complications. The aortic valve itself is a porcine pericardial valve that attaches to the non-calcified aortic annulus using our proprietary Trapdoor Mechanism, ensuring stability and reliability. The ascending aortic part is made with flexible, polytetrafluoroethylene (PTFE)-covered aortic stents that mould to the curvature of the ascending aorta, allowing for the best

anatomical fit (Figure 2).
We have successfully carried out the procedure in several large animal models (Figure 3), a chronic animal study is ongoing, and we plan to perform a human implantation soon.
What truly makes Veritas different from current solutions is its minimally invasive method, which removes the need for openheart surgery and complex circulatory support. This results in less invasiveness, shorter recovery times, and the ability to treat patients who are otherwise unsuitable for surgery. The global availability of Veritas could change clinical practice by greatly expanding access to life-saving treatment and improving outcomes for patients with ascending aortic disease.

Figure
Figure 3. Transfemoral total root and (top) ascending aortic replacement in a swine model.
Figure 1. Location of entry tear and proximal extent of type A aortic dissection.
EUROPEAN BOARD OF CARDIOTHORACIC SURGERY

CVCC Level 1 & 2 Examination – Updated Regulations! Easier than ever to apply, view our updated regulations. The Critical Care Certification is for surgeons who are recognised as leaders of multidisciplinary, high performing teams.
MEBCTS Level 1 Examination
The Membership of the European Board of Cardiothoracic Surgery (MEBCTS) is for surgeons at the end of national training who are ready to work independently.
FEBCTS Level 2 Examination
The Fellowship of the European Board of Cardiothoracic Surgery (FEBCTS) is for surgeons who are already practicing independently. Visit our website ebcts.org for more information
SCIENTIFIC PROGRAMME
FRIDAY 10 OCTOBER

SATURDAY 11
OCTOBER
Nursing and Allied Health Professional in cardiothoracic surgery
EACTS/ESTS joint session – surgical treatment of hyperhidrosis
Abstract session – Nursing and Allied Health Professionals 11:45 – 12:45


EXHIBITION FLOOR PLAN



TUNE IN

13:45-14:45

17:30–18:00
SATURDAY 11 OCTOBER
09:45–10:00
10:15–10:30 In focus with Gloria Farber
10:45–11:00 Next Stop: 2026 & 40 Years of EACTS
11:15–13:30 Session broadcast: EACTS 2025 trial update session

Thursday


Hands-on guidance from the
experts LEARNING LABS
Take advantage of the invaluable opportunity to train with some of the world’s best cardiothoracic surgeons at the EACTS Learning Lab. These specialist hands-on workshops are designed to advance your technical abilities and include wetlabs, drylabs, simulation and practical sessions. You will gain practical experience using the latest devices, practice on simulators and interact with expert faculty and industry proctors. EACTS Learning Lab sessions are available to EACTS members for just an additional €75 each (€100 for non-members). Spaces are limited and offered on a first-come, first served basis. Don't miss out – book today to guarantee your opportunity.

EACTS LEARNING LAB SCHEDULE
Friday 10 October
09:00 – 11:00 AV Repair – Valve Sparing Aortic Root Surgery: The Reimplantation Technique
09:00 – 11:00 Endoscopic Dry Lab Training
12:15 – 14:15 AV Repair – Annuloplasty with remodelling valve sparing root replacement and isolated aortic valve repair
12:15 – 14:15 Endoscopic Dry Lab Training
15:00 – 17:00 Left-handed Surgeons
15:00 – 17:00 Endoscopic Dry Lab Training
Saturday 11 October
09:00 – 11:00 Thoracic
09:00 – 11:00 Endoscopic Dry Lab Training
SATELLITE SYMPOSIA
These sponsored programmes do not form part of the official Annual Meeting scientific programme.
FRIDAY 10 OCTOBER

for the Lifetime Management of Patients with Complex Aortic and Mitral Valvular Heart Disease
the Aortic






Structural Heart Innovation | Science, Clinical Experience & Landmark RCT
Aortic Manipulation in Modern Cardiac Surgery: When Not to Clamp, When to Clamp, When to Cut
Trailblazing Hybrid Horizons: Redefining Aortic Innovation





Dr. Nimesh Desai
Moderator
United States of America

Dr. Fernando Fleischman
United States of America
Arch First: A New Paradigm for Proximal Control and Predictable Outcomes
Dr. Mehrdad Ghoreishi
United States of America
Cool by Design: Embracing the Non-Thermic Approach with Thoraflex™ Hybrid
Mr. Omar Nawaytou
United Kingdom
Mastering the Arch: Strategic Zoning from 0 to 3 for Precise Patient Matching
Prof. Dr. Malakh Shrestha
United States of America
Seamless Synergy: How Rapidlink™ Technology Simplifies Hybrid Arch Repair




Prof. Sabine Wipper
Austria
No Bypass, No Boundaries: Advancing Minimally Invasive Hybrid Thoracoabdominal Repair
Dr. Eric Jeng
United States of America
Starting Strong: Building a Successful Hybrid Aortic Program from the Ground Up
Prof. Aung Oo
United Kingdom
Familiar Steps, Innovative Change: Keeping Surgical Habits with Thoracoflo™
Dr. Alex Weston
United States of America
Advancing Arch First: Proven Concept Applied
Prof. Hideyuki Shimizu
Japan
Physician-driven Modification of the Stented Segment of Thoraflex™ Hybrid in complex FET cases




Introducing the ‘open mic’ programme at the EACTS booth
This year, we are excited to introduce a brand new open mic-style area at the EACTS booth (#47). Join us for an inspiring programme of engaging talks, interactive discussions, and spontaneous exchanges throughout the event!
Friday, 10 October
09:45-10:00 Avenns Medical – Heart Regeneration Is Now 10:15-10:30 Adult Cardiac Database drop-in 15:00-15:30 Sustainable cardiac surgery for the global south







Our Publications Webinars cover a wide variety of topics, from providing key resources for researchers to discussing the latest hot topics and surgical techniques shaping the field. Our Guidelines Webinars present case studies demonstrating the utility of guidelinedirected care in cardiothoracic surgery, bridging theoretical knowledge with practical insights.
9th EACTS Mechanical Circulatory Support Summit
20-22 November 2025
Hotel nhow Berlin, Berlin, Germany
The 9th EACTS Mechanical Circulatory Support Summit returns this year with interactive lectures, live-in-a-box cases and keynote presentations. The Summit is designed to attract attendees with an interest in mechanical circulatory support, including cardiologists, heart failure cardiologists, emergency and ICU specialists (ECLS), cardiac surgeons, perfusionists, heart failure nurses and VAD coordinators, paediatric cardiologists and congenital heart disease surgeons, and representatives from the medical industry (cardiac device, including ECMO development and production).
This two-and-a-half-day summit will cover an array of topics, including an update of optimal medical therapy and device treatment (OMDT), Glucagon-like peptide-1 receptor agonists, cancer treatment in LVAD patients, transcatheter aortic valve implantation (TAVI) and transcatheter edge-to-edge repair (TEER) on LVAD, big data and AI in medicine, and more.
In addition, there will also be a scientific evaluation of MCS registries (IMCARS, EUROMACS, INTERMACS, IMACS and the Stellar register) vs
multicentre studies, and discussions on the different phenotypes of cardiogenic shock (including SCAI and INTERMACS stages, AMI, postcardiotomy, acute on chronic heart failure and fulminant myocarditis). Attendees will also witness a joint EACTS /ICCAC session, ‘LVAD therapy – how to make the most out of it?’ that will focus on the power of networking, patient evaluation, selection and optimisation, and novel LVAD tools and useful wearables.
A specially designed ‘Guidelines on MCS’ session will examine the EACTS/ STS/AATS Guidelines on Temporary Mechanical Circulatory Support in Cardiac Surgery, EACTS ECD on Protected Cardiac Surgery, AATS surgical treatment of AMI complications, ISHLT guidelines on Temporary Mechanical Circulatory Support (tMCS), ESC heart failure updates, as well as examine the future perspective and unmet needs in clinical MSC guidelines.
New and recent developments will also be under the spotlight with presentations on continuous-flow biventricular assist device (CF-BiVAD) with single drive lines, CF-BiVAD with two drivelines and the surgical implantation technique for a rotary total artificial heart, as well as an update from industry, ‘What’s in the pipeline – new devices.’
A focus session on the major challenges in patients with congenital heart diseases will assess paediatric
support outside of traditional LVADs and the replacement of the pulmonary valve with pre-emptive use of Microaxial Flow Pump (mAFP). Additionally, experts will look at the impact of the combination of temporary and durable devices and the challenges during the transition from mAFP to dLVAD.
Last, but by no means least, a session entitled ‘The beauty and the beast’ will discuss complex cases and present the creative solutions in cardiology and cardiac surgery.
MCS Rising Stars Quiz
Delegates are invited to submit a team to participate in the popular MCS Rising Stars Quiz. Members of the team should be from the same country or the same institution and may have a maximum of four participants. Spaces are limited, and we may not be able to accommodate all who apply, so please register your interest by emailing clara.mealing@ eacts.co.uk and we will get back to you.
If you attended the 2025 MCS Workshop, please email registration@ eacts.co.uk to claim your €100 discount on your MCS Summit registration. Registration fees include all sessions, Welcome Reception, lunch and refreshments.
Register now!


Aortic Valve Repair: A Step-by-Step Approach 25-27 March 2026, Paris
The recent 2025 EACTS/ESC guidelines recommend aortic valve–sparing and repair procedures as the preferred treatment for root or ascending aortic aneurysms, irrespective of the severity of aortic insufficiency (Class I, Level B), and for isolated aortic insufficiency (Class IIa, Level B). Importantly, valve repair or sparing has been shown to restore life expectancy comparable to that of the general population, while being associated with fewer valve-related complications compared with valve replacement. Nevertheless, current practice shows a valve-sparing/repair rate of less than 20%, although up to 80% of valves are deemed repairable. This discrepancy highlights the urgent need to broaden the implementation of valve-sparing and repair strategies to all repairable valves.
This Level 3 EACTS course offers attendees a deep dive into a standardised and reproducible approach to aortic valve repair.

EMMANUEL
LANSAC
Course Director; La Pitié Salpétrière Sorbonne, University Hospital, Paris, France
This will include the rationale, physiological sizing and insertion techniques for incorporating an external aortic annuloplasty ring as part of any repair procedure.
The course covers n in-depth training of aortic valve repair from valve-sparing root replacement (for root aneurysms) to isolated aortic valve repair (for isolated aortic insufficiency).
n repair techniques for tricuspid, bicuspid and unicuspid valves are covered in step-by-
EACTS Outreach Programme
Advancing education initiatives in underserved regions
The EACTS Outreach Programme improves the outcomes for heart patients in underserved regions by advancing education initiatives. The programme distributes grants with funding from the Edwards Lifesciences Foundation and the Every Heartbeat Matters (EHM) initiative to qualified surgeons involved in humanitarian
work in underserved regions and communities.
The FFF EHM grants aim to support programmes that focus on the detection, treatment and recovery of these populations, with the goal of reducing the global burden of structural heart disease.
Recipients of the FFF Every Heartbeat Matters Grants – who must be an EACTS member – will provide education to help reduce the global burden of structural heart disease and drive progress towards global equity in surgical care.
“Many EACTS members already engage in
step detail.
n how to repair different valve morphologies and aortic phenotypes through s combination of technical lectures, combined with four full live surgeries and further pre-recorded live-in-a-box video sessions on different lesion sets.
n lectures on echocardiographic assessment of the aortic valve and root, evidence for aortic valve repair, guidelines and indications, repair in aortic dissections, paediatric aortic valve repair, and alternatives to repair, including the Ross procedure, will be covered by an esteemed international faculty. The programme will also include a ‘failure session’, in which attendees will discuss cases all the way from echo analysis to surgical repair, learning how to identify predictors of repair failure as well as the bailout techniques available to them when such
situations arise. Lectures on how to set up a new aortic valve repair programme will also be given.
The third day of the course will provide wet lab training, allowing attendees to practice what they have learned on cadaveric hearts within the historical laboratory of anatomy in Paris, du Fer à Moulin. There will be an international faculty to supervise, support and provide hands-on teaching during this session.
Who is this course aimed at?
Cardiac surgeons and echocardiographers (cardiologists and anaesthetists) who are willing to start, or are already part of, a valve-sparing aortic root replacement and aortic valve repair programme. Advanced residents interested in the field of valve repair are also welcomed.

vital educational and humanitarian programmes, particularly in Africa. The EACTS Outreach Programme will drive and coordinate more of this important work – harnessing the expertise of EACTS members and fostering collaborations with industry partners, charities and other organisations,” said Patrick Myers, EACTS Secretary General. “Together we can improve long-term patient outcomes by opening up access to heart valve treatments around the world.”
The EACTS Outreach Committee, Chaired by Professor Carlos Mestres, Extraordinary
Professor at the Department of Cardiothoracic Surgery at the University of the Free State in South Africa, will award industry or charitysponsored grants to EACTS members. By leveraging industry and charity contacts, EACTS aims to shift the focus from short-term missions to sustainable programmes that improve long-term patient outcomes in underserved regions, with growing interest from industry to fund such efforts.
For more information, please email: FrancisFontanFund@eacts.co.uk
PRESENCE. PRECISION. PERSPECTIVE.
