volume 19 issue 1 february 2026
the issn 1757-4625
volume 11 issue 4 november 2018 issn 1757-4625
the journal of the dental technologists association

volume 19 issue 1 february 2026
the issn 1757-4625
volume 11 issue 4 november 2018 issn 1757-4625
the journal of the dental technologists association

In this issue:


Gut Health Scotland the Wave
Dental Technicians’ Knowledge, Attitudes and Future Views


HOURS OF VERIFIED CPD



Editor: Derek Pearson
t: 07866 121597
Advertising: Rebecca Kinahan
t: 01242 461 931
e: info@dta-uk.org
DTA administration: Rebecca Kinahan
Operations Coordinator
Address: PO Box 1318, Cheltenham GL50 9EA
Telephone: 01242 461 931
Email: info@dta-uk.org Web: www.dta-uk.org
Stay connected: @DentalTechnologists Association
@The_DTA
@dentaltechnologists association
Dental Technologists Association (DTA)
DTA Council: Joanne Stevenson President Chris Fielding
Deputy President
Tony Griffin Treasurer Delroy Reeves DTA Liaison Delegate
Joanne Clark, James Green, Raya Karaganeva, Robert Leggett, and Jade Ritch.



Editorial panel: Tony Griffin Joanne Stevenson
Editorial assistant: Dr Keith Winwood
call 01242 461 931
ISSN: 1757-4625
Views
Dear Members,
As we begin 2026, I would like to extend my sincere gratitude to all of you for your continued support and commitment to the Dental Technologists Association (DTA). Your professionalism and dedication ensure that our role within the wider dental team remains essential, respected, and forward-looking.
2025 was not a year without its challenges. We’ve heard from so many of you about navigating uncertainty, making hard decisions, and finding ways to keep moving forward when the path wasn’t always clear. Over the past year, the profession has continued to evolve, with digital workflows, new materials, and modernised regulations shaping our day-to-day practice. Amid these changes, the DTA has worked hard to advocate for our members, particularly around education, workforce sustainability, and the future of training pathways. This work will remain central to our efforts throughout 2026.
I am pleased to confirm that Headway will remain our nominated charity for another year. Their work supporting individuals and families affected by brain injury aligns

strongly with our values as a profession and as an association, and I hope you will continue to support their vital mission.
This year also saw the successful launch of a new Wellbeing Hub and DTA Rewards, together with our new partnership with Totum Benefits, giving members access to an even wider range of everyday savings. We remain committed to ensuring that DTA membership delivers meaningful value both professionally and personally, and these developments demonstrate that focus.
We have also strengthened our support for student members with the introduction of a dedicated student and newly GDCregistered area within the Members’ Area. I would like to thank our voluntary Council members for their tireless support, and all of you for your continued engagement with

the DTA. Together, we will continue to strengthen our profession and support the highest standards of dental technology across the UK.
So, as we head into 2026, I want to make you a promise: we’ll keep listening. Tell us what’s working. Tell us what isn’t. Tell us what you need next. That’s how we get better together.
Wishing you a successful and fulfilling year ahead.
Warm regards, Joanne Stevenson President, Dental Technologists Association
In a warm and ceremonial handover, Delroy Reeves addressed Council members before presenting the Chain of Office to the newly appointed President. During his presentation, he said:
“Council colleagues, this is my moment of glory. On this historic occasion of welcome, will Madame President, Mrs. Joanne Stevenson, DTA’s first female President, please be upstanding. I am extremely proud and grateful to officially welcome you, as protocol dictates, on this 8th day of November 2025, by installing you with the DTA’s Coat of Arms
Chain of Office. Wear this chain with pride, determination, and distinction as you continue to promote and represent our Dental Technologist profession. Your fellow Council colleagues are well-equipped and versatile, ready to stand with you throughout your tenure as President. We welcome you.”
The Council celebrated the appointment as a moment of progress and representation for the profession. Members expressed confidence in President Stevenson’s leadership and the direction she will bring to the Association in the coming year.



The Medicines and Healthcare products Regulatory Agency (MHRA) has begun contacting manufacturers of custom-made dental devices to outline significant changes to UK medical device registration fees, due to come into effect on 1st April 2026.
The new charges will be calculated and paid via the Device Online Registration System (DORS), and manufacturers will have 90 days from 1st April each year to submit payment. The changes form part of a wider programme to support post-market surveillance and strengthen device safety across the UK system. Manufacturers are being urged to begin preparations now to ensure compliance ahead of the deadline.
New fee structure and timelines
Under the new framework, annual fees will
be determined by the number of chargeable Global Medical Device Nomenclature (GMDN) categories registered with the MHRA.
The MHRA has confirmed that the indicative annual fee is approximately £300 per chargeable GMDN Level 2 category (or Level 1 category where Level 2 is not available). Importantly, the fee is not charged per individual device model, but per registered GMDN category. Where multiple devices are registered under the same chargeable category, only one annual fee should apply for that category.
Estimated fees currently being issued to manufacturers are indicative only. Final payable fees will not be confirmed until after 31st March 2026, based on registration data held at that point.
Manufacturers are explicitly instructed not to make payment on estimated invoices issued by the MHRA.
Payments will open through the DORS platform on 1st April 2026, and affected

organisations will have 90 days to complete payment.
A Full information on fees and routes to payment is included in MHRA’s online fee guidance, visit https://www.gov.uk/ guidance/register-medical-devices-toplace-on-the-market#fees
Who must pay the fees?
Fee estimates and reminder communications will be provided only to:
A UK-based manufacturers with a registration status of ‘Registered’
A UK Responsible Persons (UKRPs) representing non-UK manufacturers with a registration status of ‘Registered’
A Northern Ireland Authorised Representatives acting for non-EU manufacturers with a registration status of ‘Registered’
UKRPs and Northern Ireland Authorised Representatives will be responsible for collecting fees from their represented manufacturers and submitting payments via DORS. Accounts with a status of ‘Suspended’ must follow specific actions detailed in the MHRA guidance.

Given the new £300-per-category annual fee, we strongly advise all members to review exactly what devices and GMDN categories they currently have registered. In practice, some manufacturers may have multiple GMDN terms or categories registered unnecessarily, including:
A Duplicate registrations covering essentially the same device
A Legacy or obsolete device listings that are no longer placed on the market
A Slight variants or model updates that could potentially be grouped under a single appropriate GMDN category
Such duplication can artificially inflate annual fees under the new structure. Manufacturers are therefore encouraged to streamline their registrations, ensuring that:
A Only active, relevant devices remain listed
A Devices are registered under the minimum number of appropriate GMDN categories
A Duplicate or redundant entries are removed prior to the fee assessment date
The MHRA’s fee model is based on GMDN Level 2 categories (or Level 1 where Level 2 is not available).
Manufacturers must ensure accurate assignment of GMDN terms, as these determine the number of chargeable categories.
Incorrect or overly broad classification may increase fees and may also have wider implications, as GMDN data is increasingly used by NHS stakeholders for procurement and market oversight.
To support industry preparation, the GMDN Agency provides user guides and training videos via its dedicated training portal, which may help manufacturers review classifications ahead of the MHRA’s deadlines.
Training - Videos & User GuidesGMDN
A The GMDN Agency has issued separate guidance to support manufacturers in identifying Level 2 categories used by the MHRA. Visit https://www.gmdnagency .org/training/
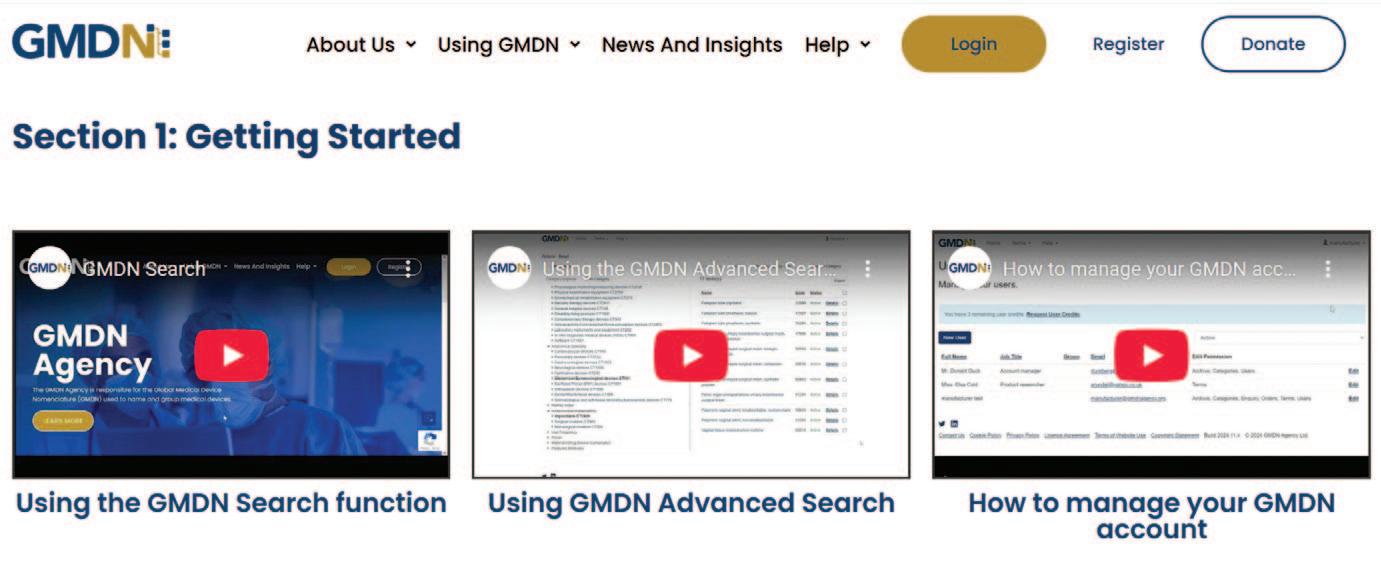
Key points include:
A GMDN Terms are mapped to multiple categories, grouped under headers, including “Device Function”
A Under Device Function, there are 22 Level 1 Categories, each with multiple Level 2 Categories
A Some Terms link only at Level 1 or across multiple categories
A Manufacturers should review GMDN assignments regularly as part of quality processes
Manufacturers with a GMDN membership can access category data directly through the “My Terms” section of their online account. Basic GMDN memberships do not provide access to category data.
1. Audit all registered devices and GMDN categories before 30th March 2026
2. Remove duplicate, obsolete, or unnecessary registrations to avoid inflated fees
3. Confirm correct GMDN term and category assignments
4. Ensure DORS account information is current and accurate
5. Review MHRA fee guidance and assess the potential budget impact of the new annual charges
If you are a student or a newly registered dental technologist (DT), this area has been specifically created to support you. It is designed to enhance and guide your career in dental technology, offering targeted content to help you understand the expectations, responsibilities, and opportunities that come with GDC registration.
This section outlines what is required of you as a registered dental technician. Browse the drop-down menus to explore key information. If you have questions or suggestions for content that would benefit others, we would welcome your feedback –we are continually working to further expand and improve these resources.
Articles from the technologist and articulate
Access a curated selection of articles tailored to your stage of practice. Start with
foundational technical pieces and progress to follow-on content designed to enhance your knowledge and confidence.
Our Health and Wellbeing Hub provides practical guidance, emotional support, and everyday tools to help you stay balanced, motivated, and resilient. Whether you need help with managing stress, seek financial advice, or require inspiration in your day-today life, the hub is designed to support both your personal and professional wellbeing.
Take advantage of exclusive member savings through DTA Rewards and our partnership with TOTUM Benefits. From dining out and weekly shopping to purchasing a car or planning a holiday, you’ll find offers that will help you make meaningful savings across a wide range of leading brands and retailers.
We invite dental technicians who have

6. Establish internal processes for timely annual review and payment
7. Monitor MHRA communications and forthcoming recorded guidance


qualified within the past three years to share their stories. Tell us what inspired your journey into dental technology, the training you undertook, how you gained worthwhile experience, the value of mentorship to your personal and professional development, and the role you are performing today. Your experiences can help guide and motivate future DTs.
A If you’d like to contribute—or even create a “Day in the Life” reel—please email us at info@dta-uk.org. Your voice plays an important part in promoting and advancing the profession.
The DTA recognises and celebrates Sue Adams’ outstanding contribution to the Association
The Dental Technologists Association (DTA) owes much of its success to those individuals who work tirelessly behind the scenes. One such person was Sue Adams, whose dedication and expertise was instrumental in shaping the organisation from its early days through to her retirement in 2019.
Sue’s journey in dentistry began as a dental nurse in Cheltenham and later took her to Riyadh in Saudi Arabia before she returned to the UK to work with the Oral Health Foundation and other dental-related businesses. From 1992 to 2019, she served as the DTA’s business manager, guiding the
association through its formative years and supporting its evolution into a respected professional body.
Sue’s leadership was pivotal during the introduction of statutory regulation for the dental team, including dental technicians and clinical dental technicians. She worked closely with the General Dental Council (GDC) to ensure compliance with regulatory requirements and championed the introduction of a structured ‘grandfather clause,’ to safeguard public trust whilst accommodating those experienced professionals without formal qualifications.
Sue played a key role in expanding member benefits. Under her management, the DTA launched high-quality Continuing Professional Development (CPD)



A Surface Finish – Articulate, March 2025
A Signs and Symptoms of Head and Neck Cancer – Articulate, March 2025
A Annie Veale: Technicians – How to be a ‘high achiever’ in SERPs (Search Engine Results Pages) – The Technologist, May 2025
programmes, all of which were free to members, meeting GDC requirements for lifelong learning. She also played a key role in creating the Dental Technologist Journal and later supported the development of Articulate, an innovative online platform combining practical videos with CPD resources.
Her influence extended to collaborating with government bodies, educational institutions and regulatory agencies, and she was a strong supporter of dental shows and conferences. Sue oversaw expansion of the DTA website, providing members with essential guidance, templates, and tools for professional development.
Beyond digital initiatives, Sue maintained a strong focus on personal member support through her team. Her efforts laid the foundation for services that continue today, including insurance, a legal helpline, and expanded member benefits such as discounts and health support.
In recognition of her exceptional contribution, the DTA Council has unanimously awarded Sue Adams Honorary DTA Membership. Her vision and commitment helped to establish a strong professional voice and have left an enduring legacy for dental technologists and clinical dental technicians alike.
Thank you, Sue, for your invaluable contribution to our profession.
Tony Griffin MBE
A Living and working with change Part 3: Attitudes and behaviour – The Technologist, May 2025
A Why does diabetes matter to us? –The Technologist, May 2025
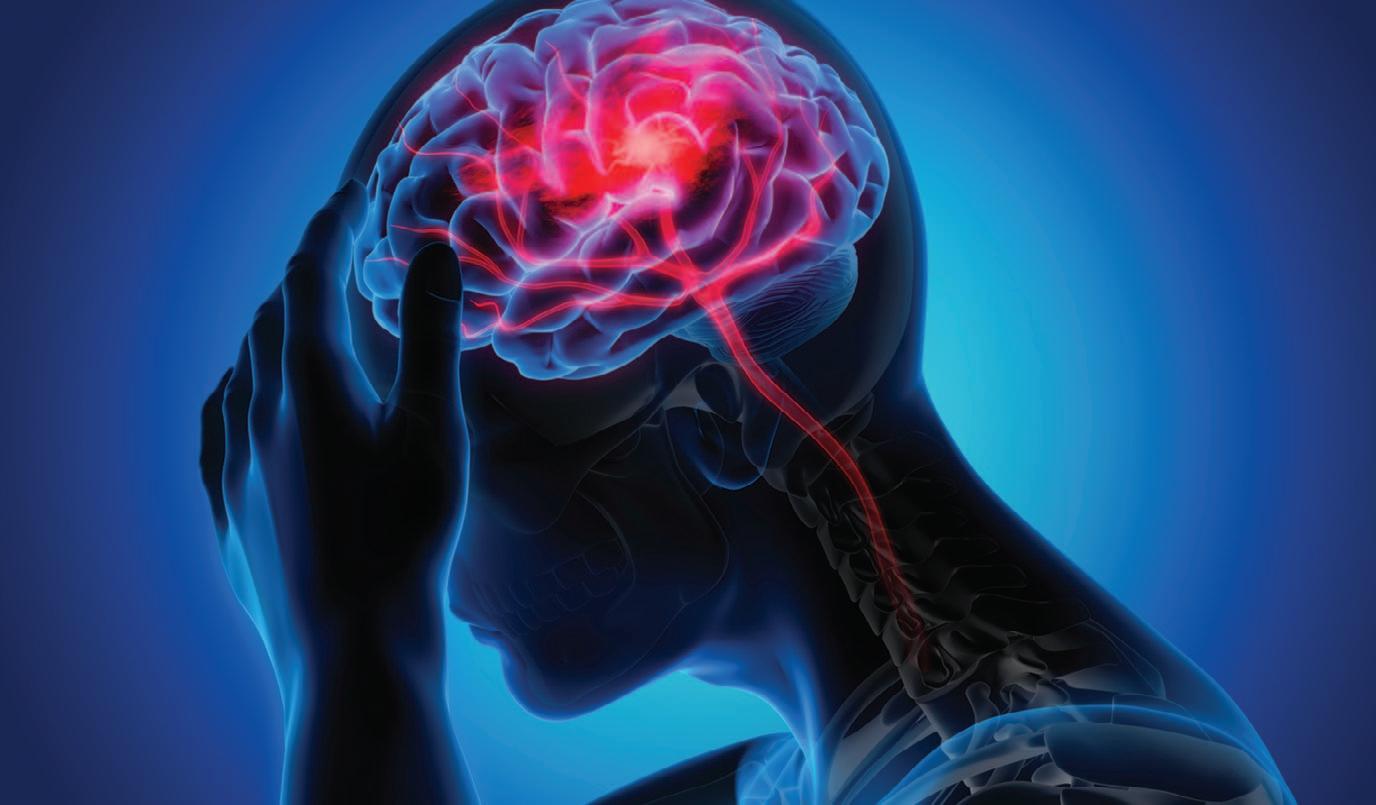
Throughout 2026, the DTA is proud to continue its support for Headway – the brain injury association, an organisation whose work remains vital to affected individuals and families across the UK.
Brain injury can alter every aspect of a person’s life — their mobility, ability to communicate, cognition, behaviour, and emotional wellbeing — and its impact is often sudden, life-changing, and long-lasting. Although it is easy to believe “it won’t happen to me”, the reality is stark: around 350,000 people are admitted to hospital with an acquired brain injury every year — that’s nearly one every 90 seconds
Headway’s 2024–2029 strategic plan sets out a clear commitment to:
A improving national awareness and understanding of brain injury; A expanding and evolving specialist support services;
A strengthening research and access to rehabilitation that helps rebuild independence and improves quality of life.
The charity continues to deliver essential services, from practical support and information to advocacy for better rehabilitation pathways. We encourage all members to support Headway in whatever way you can — whether through fundraising, raising awareness, or simply signposting someone in need. Every contribution makes a difference.
A To learn more about Headway’s work, or to access resources for yourself or your colleagues, please visit: https://www.headway.org.uk/

1 Notice is hereby given that an election of three Council Members of the Dental Technologists Association is about to be held.
2 Any member of the Company is entitled to be nominated as a candidate
3 Any person entitled to vote may take part in the nomination of any number of candidates not exceeding the number to be elected
4 Each candidate must be nominated separately by the signatures of not fewer than three Members of the Company on not more than two nomination papers to be obtained from the Returning Officer, and every nomination paper shall contain the name, registered address and title to registration both of the candidate and of the nominated and will accept office if duly elected
5 The nomination paper or papers for each candidate must be delivered by hand or by registered post to the Returning Officer on or before the 1st Day of May 2026
6 A nomination in respect of which any of these rules has not been complied with will be invalid
Delroy
Reeves as the Returning Officer
The Dental Technologists Association, PO Box 1318, Cheltenham, GL50 9EA
As we turn the page on 2025 and look ahead to a new year of opportunity and challenge, I think we can all agree that last year provided a world stage for extraordinary political turmoil, and that 2026 promises more white-water events.
We might posit that future generations will look back on the key players in recent days’ political theatre with something akin to a mixture of embarrassed laughter and shock. At least it gives our keener minds something meaty to chew and digest. I wait with interest to read the analytical thoughts that will surely follow once the dust settles, if it ever does.
It is a sense of relief to turn our attention to the calmer waters offered by our profession, to evidence-based techniques and developments shared with our peers and colleagues. Malocclusion can’t be solved by opinion but by hard facts and professional insight.
Here I’m pleased to share some key developments and reflections for dental technologists across the UK — and to highlight how our association continues to advocate for and support our profession.

GDC & Regulatory Landscape:
A The General Dental Council (GDC) has recently published its new “Scope of Practice” (November 2025), with immediate effect. For dental and clinical dental technicians, the good news is clear: nothing has been lost. The updated document is more streamlined, better structured, and easier to interpret. All previous permissions, under proper training and indemnity, remain valid.
A The clearer format and the introduction of the GDC’s “Safe Practitioner Framework” make it more straightforward for those wishing to develop their skills and expand their role — an encouraging sign for anyone looking to grow professionally.
A At the same time, the GDC has also confirmed that the 2026 Annual Retention Fee (ARF) for dental care professionals will increase from £96 to £108.
A The GDC’s new Corporate Strategy for 2026–2028 emphasises modernisation, efficiency savings across five years, and improving regulatory processes to support the profession while also protecting the public.
A A major concern for 2026 and beyond is the ongoing contraction of dentaltechnology training provision across the UK. As reported last autumn, several educational institutions have announced closure or suspension of their Dental Technology programmes — including one in Northern Ireland, another in England, and even a possible temporary suspension in Scotland.
A This trend threatens the pipeline of new, skilled dental technicians at exactly the time when demand for prosthetics, dentures, and custom-made appliances continues to rise. Without urgent intervention — both nationally and within those education sectors — we risk a looming workforce shortfall that
could impact service delivery and patient care.
A The DTA is calling on government, education providers, regulators, and oral health planners to recognise dental technology as a core element of oral healthcare infrastructure — not as an afterthought. We need stable, supported training pathways, greater capacity, and better promotion of the excitement of career pathways available within the dental technology profession in order to attract new talent. The jaded view of silent workbenches and dusty plaster rooms is fading into the past, replaced by innovation and evolution.
A Over 2025, the DTA welcomed a new leadership team and marked a historic milestone at its Autumn Council meeting on 8th November 2025, as outgoing President Delroy Reeves formally installed Joanne Stevenson as the Association’s first-ever female President.
A We also launched some exciting new benefits:
– Through DTA Rewards, our members get to experience and enjoy exclusive access to a wide variety of additional member benefits and offers from leading brands and retailers for no additional membership fee.
– A new Wellbeing Hub and Counselling Helpline, providing confidential support for mental health, stress management, and workplace wellbeing.
– Members also enjoy Totum Benefits, offering exclusive discounts and savings across a wide range of everyday products, professional services, and lifestyle essentials— supporting both your professional and personal life.
A While we continue to provide valuable member benefits:
–
Our quarterly magazine, The Technologist, remains the flagship
source of continuous professional development, helping you to meet the GDC’s mandatory requirements at no extra cost, while providing CPD relevant to everyday practice.
A As always, the DTA remains committed to representing your interests, actively monitoring regulatory change and advocating for dental technology at national and professional levels.
A Looking ahead: expect more from the DTA in 2026 — with renewed outreach to training centres, stronger advocacy on workforce shortages, and a push for recognition of dental technology’s central role in oral healthcare planning.
A If you are early in your career consider mentoring or taking on apprentices, or supporting training programmes in your area. Share your experience, encourage new entrants.
A Engage with the new Scope of Practice — review it carefully, see if there are roles within your licence you can develop further.
A Stay up to date: ensure you retain your registration, comply with CPD and GDC requirements — but also use your DTA membership to take advantage of free CPD, DTA Rewards support, and advocacy.
A Above all — stay connected. The DTA exists to represent us, as practising dental technicians. Your voice, your experience, your support help shape the future of the profession. Share valuable feedback via our membership survey QR code closing soon.

With so many offers available to DTA members through DTA Rewards it can be hard to know where to start. We include monthly offers in our DTA newsletter and why not take a look at our Ways to Save section on the DTA Rewards page.

As previously stated, we have also partnered with TOTUM to bring our members even more deals. Their memberships provide access to hundreds of offers – online and instore, as well additional benefits such as PASS proof of age ID, TOTUM Cashback, Global ID & discounts with ISIC.
The Dental Technology Showcase (DTS) 2026 returns to the NEC Birmingham on 15–16 May. We’re proud to announce that we will once again be exhibiting and speaking at this prestigious event. As the UK’s only dental lab-focused showcase, DTS provides a platform for dental laboratories to network, learn, and discover the latest innovations in the field. Attendees can connect with forward-thinking suppliers, hear from industry-leading speakers, and gain insights to help them stay ahead in a rapidly evolving sector. Book your free place via the website - https://www.the-dts.co.uk/ or via the QR code, and visit our stand; more details to follow in the May 2026 issue of The Technologist
The BDIA Dental Showcase 2026 returns to ExCeL London on 13–14 March. While traditionally aimed at the wider dental community, the organisers have indicated to the DTA that this year they are once again exploring additional content tailored specifically for dental technologists.
The organisers say: “This flagship event is celebrated for bringing together the brightest minds in the dental profession and industry, providing unmatched opportunities to explore cutting-edge products, innovative solutions, and expert insights. “With over 300 exhibitors, interactive workshops, and a comprehensive educational programme featuring leading clinicians and industry specialists, the BDIA Dental Showcase offers dental professionals the perfect platform to develop skills, expand networks, and stay ahead of the curve. Book your free place via the QR code.”

The North of England Dentistry Show is back in Manchester Central Convention Complex on 7th March 2026. The organisers promise: “The event will include the Laboratory Zone, a lecture series tailored for technicians and clinical dental technicians, showcasing the latest advances in techniques and technology. Attendees can enjoy networking opportunities and hear from some of the UK’s most inspiring speakers.”
A Stephen Kinnock MP describes the increase in ORE capacity as a ‘real step forward’
A Understanding each other’s priorities
A Looking at professionalism more broadly.
Dr Helen Phillips, GDC Chair, puts forward her thoughts
Since joining the GDC, I have prioritised meeting a lot of our stakeholders and partners. I am grateful to everyone who has given up their time, and I’m using these valuable conversations to listen, learn and ask a lot of questions. Some of this is to help me to understand where the GDC and indeed regulation fits in dentistry.
It’s immediately apparent that dentistry is practiced in a complex system. From the different types of dental settings –NHS, private, community, primary and secondary care. And the types of dentistry performed – general dental practice, preventative care, specialty care. A crucial factor in this is dental workforce, including the breadth and scope of all seven professional titles in the dental team.
As Chair of an NHS Trust for nine years and now as Chair of NHS Professionals, I see the challenges of large-scale workforce planning, recruitment and retention. There

are obvious parallels in dentistry – and some shared challenges too.
The increase in ORE capacity is a ‘real step forward’
We convened the tenth meeting of the 10th Dental Leadership Network in November, with the theme Act now, shape tomorrow: Strategic shifts in dental care I was disappointed to miss the event as I was unwell.
The Minister for Health and Care, Stephen Kinnock MP, gave a speech setting out the government’s priorities for dentistry and acknowledging the work of dental professionals across the four nations. The Minister said that he was ‘delighted’ by our recent announcement about the new ORE contract, which we expect could more than double the number of dentists joining the register via the ORE route. He described the increase in capacity as ‘a real step forward’.
In the discussions about the dental workforce, we need to be acutely aware that plans need to consider the whole dental team – there is no dentistry without dental nurses chairside; dental technicians and laboratories play a vital role; dental hygienists and dental therapists have a wide scope of practice that we should make full use of.
It is clear that no single intervention will increase the NHS dental workforce nor add capacity in regions that are currently underserved. We need to work together to tackle this.
The complexity of the systems all points to the need to understand each other’s priorities and purpose, identify the shared challenges and how we can work together as partners to tackle the issues. We each have different roles – providing insight, sharing data, working within our own governance structures to take things forward.
The GDC recently published our strategy for 2026-2028. Our vision is to be a trusted and effective regulator, supporting dental professionals to provide safe and effective care for their patients.
We have set out our vision, values, objectives, the work we will do to achieve them and how we will measure and know that we’re making progress. It’s a different strategy, and very ambitious. This is our opportunity to make a positive difference to dental regulation that will be felt by dental professionals, partners, patients and the public.
To do this, we will champion a model of regulation that supports professionalism, enables learning, and resolves issues quickly and proportionately. I want us to provide regulation that fits the times we’re in and anticipates and prepares for the future. We want to be on top of emerging issues and able to play our part in tackling shared challenges.
I am committed to nurturing relationships built on trust and support and using these to listen and to learn so that we support dental professionals to provide safe and effective care for their patients and to feel the pride that they rightly should.
Richard Susskind, an author and expert on the impact of AI on society, reminds us that the true heart of a profession is not its rituals or its regulations, but its enduring promise to put specialised knowledge to work in the service of others. Dentistry embodies that
promise every single day. In a world that is increasingly automated, accelerated, and transactional, you remain one of the few last great face-to-face professions, where skill, compassion and judgement cannot be downloaded or outsourced.
Professionalism in dentistry isn’t just about meeting standards; it is about holding yourselves to a purpose. It is the quiet courage of doing the right thing for the patient in front of you, the commitment to continual learning, and the pride of belonging to a community that safeguards the nation’s oral health. This is what sets you apart — not just as clinicians, but as professionals in the truest sense of the word.
With rights, in this case to practise, come responsibilities and you should rightly be proud of the role you play in society – we at the GDC will play our part in supporting you in every way we can to deliver on your responsibilities.
The start of a new year is a good time for reflection and looking ahead. Our Chief Executive, Tom Whiting, has set out our priorities for the years ahead and some of the things you can expect to see as we deliver our strategy, visit https://www.dental review.news/people/58-dentistryinterviews/13003-gdc-new-direction
My first three months has gone quickly – and has been a steep learning curve. I am grateful for the many conversations that I have had so far that have helped me and have candidly shared where we are doing well, and where we need to do better. I wanted to set out what you can expect from me and the GDC’s Council members in 2026.
In our strategy for 2026-2028, our vision is to be a trusted and effective regulator,

supporting dental professionals to provide safe and effective care for their patients.
We have set out our vision, values, objectives, the work we will do to achieve them and how we will measure and know that we’re making progress. It’s a different strategy, and ambitious.
Council members were heavily involved in developing the strategy and are accountable for agreeing it and setting the direction of the GDC. This means that we each have a strong interest in its delivery, and the opportunity to make a positive difference to dental regulation that will be felt by dental professionals, partners, patients and the public. Further than that, our role is to scrutinise the work of the organisation, set a positive tone and culture, and ensure that systems are in place to enable us to monitor performance.
Council’s role includes seeking assurance over the way the organisation is run and holding the Executive to account, but our relationship with the Executive runs deeper than this. We have a shared vision, and we all want to champion a model of regulation that supports professionalism, enables learning, and resolves issues quickly and proportionately.
The Executive team contributes to our committees where, together with the Council Chair of each committee, we scrutinise audit and risk, finances, and performance and remuneration. Council members also spend time with teams in the GDC to understand their challenges and priorities, and what it takes to achieve the performance we need as an organisation. We also attend significant internal events that focus on staff development and engagement so that, together, we are building regulation that fits the times we’re in and anticipates and prepares for the future.
Our new strategy is deliberately challenging, and Council’s role is to ensure that we rise to the challenge. We want to be on top of emerging issues and able to anticipate and respond to them. As we do so, we will be transparent about our progress and performance, and report on these, keeping an open dialogue about our accountability to you. If you or members of the public want to see how Council meetings are held, you can attend in person or online, and I can assure you of a warm welcome. You can request to observe a Council meeting here1.
Like me, Council is committed to nurturing relationships built on trust, using these to listen and learn so we support dental professionals to provide safe and effective care to patients. We have a great variety of opportunities to meet dental professionals and leaders across the sector, and we use these to listen and build relationships.
Last year, Council members were part of the GDC team as they and the Chief Executive met stakeholders and visited dental settings in England, Scotland, Wales and Northern Ireland. Being part of these conversations is really helpful in building our knowledge and getting to know you. Even our registrant Council members, with their firsthand and personal knowledge of dentistry, learn something new. Some parts

of dentistry move at pace, and hearing from dental professionals at the frontline of delivering safe and effective patient care in NHS, private and community dental settings is so valuable.
The GDC attends many trade shows and conferences each year. Our Council members often join the GDC’s team on the stand, answering questions from dental professionals and stakeholders, helping to explain the GDC’s role and priorities. This is such a good way of seeing the business of dentistry and hearing what’s important to professionals. I’m looking forward to doing this myself!
And, of course, the GDC convenes the Dental Leadership Network, which held its tenth event in November. I say ‘of course’, but before this Network was formed, there wasn’t a place where such a broad spectrum of dental leaders regularly came together to discuss shared challenges. Council members regularly attend, listen to the expert presenters and join in with table discussions.
Going forward, I want to see more opportunities for external stakeholders to meet and spend time with Council as a whole. Time spent sharing insights and learning from within and outside dentistry is valuable. It shows that the GDC is convening and listening and will help to build relationships and understanding.
One of the objectives in our strategy is to work collaboratively to speak up on, influence, and address issues that affect patients and the public. Dentistry can be quite fragmented; in the absence of a single coherent voice, people sometimes look to us for all the answers.
What we will do is support and enable collaboration and discussions. We need to work collaboratively with our partners in dentistry, healthcare and regulation, with the UK and devolved governments and with the dental professions. Council is also committed to achieving the standards set for us by our regulator.
To do this, we will continue to engage with GDC teams and external stakeholders alike. The GDC is determined to be recognised as a regulator that operates with greater effectiveness and works collaboratively as a valued partner. For my part, I look forward to more conversations with stakeholders in 2026. I take something away from every interaction I have and it helps me, along with other Council members, to deliver on our commitment to being a trusted and effective regulator, supporting dental professionals to provide safe and effective care.
1 https://contactus.gdc-uk.org/Enquiry/GdcCouncil/ Attendance?_gl=1*7teveg*_ga*MTk4MTExOTE4NS4xN zU1NTI0ODc1*_ga_GHXYW4GEXH*czE3NjI0MjE0NzAkb zc1OCRnMSR0MTc2MjQyMzgyNyRqNDckbDAkaDA
Kevin Lewis, BDS (Lond) LDSRCS (Eng)
FDSRCS (Eng) FFGDP (UK)
With this second article we sadly conclude our celebration of the work and career of Kevin Lewis, and salute his long-standing contribution to the members of the DTA through his informed and insightful writing.
In memory of Kevin Lewis, a great friend to the DTA and valued contributor to The Technologist over many years, over the next two issues we are republishing an article he wrote about raising concerns – but with new CPD questions.
Kevin was a true gentleman who passed away on the 30th July 2025 at the age of 76 after a long battle with liver cancer. He will be missed.

This article has been split across two consecutive issues. In the previous issue, the first part considered the principles of when and how to raise concerns (especially when they relate to other healthcare professionals), and in this issue, the second part will turn to the question of ‘safeguarding’ vulnerable individuals.
■ to understand the principles of ‘safeguarding’ and ‘vulnerability’ in adults and children
■ to raise awareness of the GDC’s expectations in terms of patient protection
■ to understand the principles and process of raising concerns
■ to understand the additional responsibilities of employers and managers
■ to effectively communicate with patients, the dental team and others across dentistry, including when obtaining consent, dealing with complaints, and raising concerns when patients are at risk
■ to effectively manage self and the effective management of others or effective work with others in the dental team, in the interests of patients; providing constructive leadership where appropriate
■ to maintain skills, behaviours and attitudes that engender patient confidence in you and the dental profession and put patients’ interests first [professional behaviours]
Development Outcome: A, C & D

s healthcare professionals there is a higher expectation placed upon us, compared to most other members of the population, that we will apply our extra knowledge and experience to protect members of the public both collectively and individually. In this respect, we are accountable to our professional regulator, the General Dental Council (GDC).
In Standards for the Dental Team,1 the GDC sets out its expectations at Principle 8, ‘Raise concerns if patients are at risk’. The GDC explains that patients have a right to expect that dental health professionals (and team members with whom they work) will act promptly to raise any relevant concerns about the welfare of vulnerable patients.
It was explained in Part 1 of this back-toback pair of articles that the phrase ‘raising concerns’ will mean different things to different people, and the threshold of what qualifies as a legitimate ‘concern’ and/or what ‘raising’ actually means in practical terms, similarly varies between individuals.

It is also true that the perspective of dental technicians and CDTs may be different to, say, a dental nurse, hygienist or dentist –sometimes because of where they work and sometimes because of what they do, who they come into contact with and what they see in the course of their work. But it is important to appreciate that Standards for the Dental Team applies, as the name suggests, to all dental registrants equally.
When reading and reflecting upon this guidance, therefore, you need to think about and interpret each paragraph in the context of your own work environment, the work you do and the contact you have with others (whether directly or indirectly).
And although in Principle 8 the GDC refers specifically to ‘patients’, we are healthcare professionals, so our public responsibility to safeguard vulnerable people does not stop at the end of the working day: because of our knowledge and training, we may recognise possible concerns that other members of the public might miss. We might be visiting an elderly care home on a domiciliary patient visit in the course of providing some full dentures for a resident, or simply visiting a relative or
friend at the same care home, in a personal capacity. The expectations placed upon us are the same, as made clear in the wording of the Standards themselves (see summary below).
Safeguarding is a term that encompasses all the things that could and should be done to minimise the risk of significant harm, abuse and exploitation, especially of children and vulnerable adults because they are more likely to have a reduced ability to look after themselves and keep themselves safe. In the case of vulnerable adults, it includes supporting them to take control of their own lives by making informed choices.
The Government has set out six principles of safeguarding to illustrate how we can all help to support and protect people in a health and social care setting. These principles are:
A empowerment – people should be helped and supported to make their own decisions regarding their care and treatment
A prevention – it is preferable to speak up before something bad happens, and much better to raise a concern and be proved wrong than to fail to act, resulting in avoidable harm to the individual concerned
A proportionality – any action we take should be proportionate to the risk: if the risk is low, we should try not to overreact as this in itself can end up undermining the interests of the person involved in other ways
A protection – in any responsible and caring society, vulnerable people deserve and should receive our support and protection
A partnership – safeguarding involves communities, groups, organisations and individuals working together to close off any gaps in preventing, detecting, reporting and taking action regarding neglect and abuse
A accountability – we all need to be accountable for what we do (and fail to do) in relation to safeguarding
It is pretty obvious that young children are considered vulnerable because they aren’t able to protect themselves in the same way as most adults could. But, in the context of dentistry, and particularly the work of dental technicians and CDTs, which adults should we be thinking of as being potentially ‘vulnerable’?
A People with a mental health condition, such as dementia or personality/behavioural disorder
A People who have learning disabilities, or are easily confused, or find it difficult to understand or remember things that they are told
A People who find it difficult to express themselves and/or communicate their wishes and concerns
A People who are ill and/or can’t carry out normal daily functions without help (this might include cleaning dentures and/or oral hygiene, or preparing food so that it
is easier to eat/chew)
A People with physical disabilities or who are physically or mentally frail
A People who are under stress or struggling to cope with a specific recent event, or with life generally
A People who, for whatever reason, are in abusive relationships or living in deprivation
But these illustrative descriptions should not lead us to assume that every elderly patient is vulnerable, for example, nor that someone who is vulnerable at one moment in time will always be so. We all need to have a working familiarity with legislation such as the Mental Capacity Act 2005, and the Data Protection Act (and the 2018 General Data Protection Regulation – which we covered in a previous article). There is an ever-present danger that we might be treating vulnerable patients without first having obtained a valid consent from them or breaching their confidentiality by discussing their personal information with
third parties without the knowledge or agreement of the patient.
The same applies to other important legislation in relation to ‘safeguarding’. There is different social care legislation relating to children (The Children and Social Work Act 20173), and adults (The Care Act 20144) and both include general principles that technicians and CDTs should be aware of and understand.
It is always easier to ‘look the other way’ and convince yourself that there is probably an innocent explanation and it would be inappropriate for you to interfere when you see something that appears troubling. But if everybody thinks in this way, this is precisely how abuse can take place almost in full view. When this happens under the noses of healthcare professionals it is impossible to justify and defend – and yet in one case after another that becomes the subject of formal investigation and attracts media attention, we find a disturbing


Graduated in London 1971. He spent 20 years in full time general dental practice and 10 further years practising part time. He became involved in the medico-legal field in 1989, firstly as a member of the Board of Directors of Dental Protection Limited (part of the Medical Protection Society group of companies). He became a dento-legal adviser in 1992 and from 1998 was the Dental Director of Dental Protection for 18 years and also an Executive member of the Council (Board of Directors) and Executive management team of the Medical Protection Society, roles from which he stepped down in 2016. Since 2018 he had been a Special Consultant to the British Dental Association, in relation to BDA Indemnity.
He was a Founder and Ambassador for the College of General Dentistry, and was a Trustee Board member 2017-22 Kevin has been writing a regular column in the UK dental press since 1981 –originally as the Associate Editor of Dental Practice and since 2006 as the Consultant Editor of Dentistry magazine. He wrote and lectured regularly in the UK and internationally, and had been awarded honorary membership of the British, Irish and New Zealand Dental Associations. Kevin also became an Honorary Member of the British Society for Restorative Dentistry.

pattern of too many organisations/agencies, and too many people in positions of knowledge and responsibility who had concerns, but did and said nothing at the time. Vulnerable people of all ages deserve better than to fall through the cracks in our society and its structure, and they are a lot safer if we all step up to the plate to share in society’s collective responsibility to look out for them.
We must obviously ensure that we treat vulnerable patients appropriately when they are receiving care and treatment from us, dealing with patients/third parties in a way that respects the dignity, confidentiality/privacy, rights and wishes of the individual in question.
But we also need to be alert to the possibility that they are being abused by others. We may tend to think of abuse in too narrow a way, our views perhaps being shaped by high-profile cases of neglect, rough/unsympathetic handling or similar abuse in care homes, or where an individual’s vulnerability has been taken
advantage of by financial scammers and other criminal behaviour (even by family members and supposed friends and carers). Such shameful cases are rightly reported widely in the media, but less obvious and more subtle forms of abuse can be psychological in nature and involve bullying, exploitation and marginalisation (acting as if they didn’t have a right to have their views taken into account).
We should reflect upon our own behaviour and actions to make sure they aren’t contributing to situations, actions and behaviour by others that can be dangerous, harmful or abusive. We must be prepared to ask questions and should be open and honest with patients about our responsibility to pass on information about potential and actual danger, harm and abuse. Above all, we must take appropriate and immediate action when we see behaviour, actions and situations that might lead to danger, harm and abuse to vulnerable individuals.
This was explained in Part One of this two-
part series on Raising Concerns, and readers are encouraged to refer back to that article for a step-by-step guide of what to do and who to contact if you do have concerns. As explained in that article, it is often very difficult to decide whether or not your concerns are genuine and justified, and sufficient in scale to merit the involvement of other bodies.
The whole point of ‘raising concerns’ is that it is not your role to investigate the concern but simply to alert an appropriate party so that they can do so, if they feel it appropriate. Very often they will have a lot more experience than you in making that assessment, and crucially, they are independent and sufficiently removed from the situation to be able to view it fairly and objectively. One should, however, be cautious about acting upon rumour and uncorroborated ‘hearsay’ and place greater weight upon things that are within your personal first-hand knowledge and experience.
You should make sure that you know who has the lead responsibility for ‘safeguarding’ in your workplace. NHS England also publishes some very helpful general guidance2 that includes the contact details of a range of organisations within and beyond the NHS and healthcare that can advise you, and where appropriate, take action.
You should have a written ‘safeguarding’ policy in your workplace and ensure that all members of your staff are aware of it and follow it consistently. This policy should set out the process to be followed in the event of concerns being raised and you should keep a record of the concerns raised, what action you took, and what the outcome was.
In England and Wales, the Government’s Disclosure and Barring Service (DBS)5 holds registers of people who are legally barred from working with and around children and/or vulnerable adults. Employers who
are registered with the DBS can request an enhanced DBS check, which in addition to confirming specified criminal convictions, also confirms whether or not a named individual is barred in this way.
The previous functions of the Criminal Records Bureau (CRB) and the Independent Safeguarding Authority (ISA) were brought together in 2012 to create the DBS, which operates as an independent agency of the Home Office. Equivalent agencies exist for both Scotland and Northern Ireland although all three hold information that covers the whole of the UK to ensure that the collective pool of information remains complete, up to date and ‘joined up’ at all times.
The issue of ‘raising concerns’ can be quite emotive and the decisions involved are not always easy. People who are younger and/or in the early years of their career in and around healthcare, generally find the principle much easier to understand and accept because it has always been a feature of their professional working environment.
Some older colleagues may even find modern terminology like ‘safeguarding’ excessive and something of an overreaction: past generations have tended to adopt a stance of ‘it’s not my job to interfere’ or ‘I should mind my own business’. Either way, we must all recognise the fast-changing world in which we live and the scrutiny that organisations and individuals working within them come under (especially in fields such as healthcare, social care, schools, and activities/ occupations that bring them into close, regular and perhaps unsupervised contact with young people and vulnerable adults). Safeguarding is certainly here to stay, and its obligations are likely to get more onerous over time, not less.
All dental registrants should be mindful of the GDC’s requirements, as set out in Standards for the Dental Team1
The GDC’s use of the word ‘must’ means that the stated duty is compulsory, rather than optional.
Standard 8.5:
You must take appropriate action if you have concerns about the possible abuse of children or vulnerable adults.
8.5.1 You must raise any concerns you may have about the possible abuse or neglect of children or vulnerable adults. You must know who to contact for further advice and how to refer concerns to an appropriate authority such as your local social services department.
8.5.2 You must find out about local procedures for the protection of children and vulnerable adults. You must follow these procedures if you suspect that a child or vulnerable adult might be at risk because of abuse or neglect.
1 Standards for the Dental Team. General Dental Council. www.gdc-uk.org
2 https://www.england.nhs.uk/ safeguarding/how-to-raise-a-safe guarding-concern/
3 http://www.legislation.gov.uk/ukpga/ 2017/16/contents/enacted/
4 https://www.scie.org.uk/care-act-2014/ safeguarding-adults/.
5 https://www.gov.uk/guidance/dbs-check -requests-guidance-for-employers/

To complete your CPD, store your records and print a certificate, please visit www.dta-uk.org and log in using your member details.
Q1 Are all GDC registrants expected to have the same perspective when raising concerns?
A Yes, it is part of their elementary training
B No, the perspective of, for example, a dental hygienist or dental technician might differ because of what they do and who they meet
C The perspectives can vary due to cultural differences
D A person’s objective view can be coloured by their attitude towards the person about whom they have concerns
Q2 Are GDC registrants only expected to safeguard vulnerable people they encounter while at work?
A Yes, anything they see beyond the workplace is not their concern
B Yes, you cannot know all the factors involved in what might seem concerning in, for example, a domestic situation
C Yes, getting involved outside the workplace might be construed as an act of abuse by the concerned registrant
D No, as healthcare professionals registrants might become aware of possible concerns that others might miss
Q3 To which members of the registered dental team do the GDC Standards for the Dental Team apply?
A Equally to all dental registrants
B Only to those who are public facing
C Only to team members in a position of authority
D Only to team members who have physical contact with patients
Q4 How many principles of safeguarding has the government set out?
A Eight
B Five
C Six
D Twelve
Q5 Which of the following is NOT one of the government’s principles of safeguarding?
A Empowerment
B Offering informed advice and guidance
C Accountability
D Prevention
Q6 Who can be considered as vulnerable?
A Young children
B People with mental health conditions
C People with learning difficulties
D People in abusive relationships and all of the above
Q7 What is listed as being an ‘ever present danger’ when working with/treating vulnerable patients?
A Not first obtaining valid consent
B Discussing their personal information with a third person without their knowledge
C Insulting them by using affectionate terms such as ‘love’ or ‘darling’
D a) and b) only
Q8 What type of abuse is ‘marginalisation’?
A Not providing an interpreter when required
B Acting as if the patient does not have the right to have their views taken into account
C Asking questions when the patient has a mouth full of instruments and can’t answer
D Insisting that the patient must only talk with the dentist, not the dental nurse
Q9 What are owners and managers required to do in the workplace regarding safeguarding?
A Have a written safeguarding policy in place
B Ensure that all members of staff are aware of the safeguarding policy and follow it
C Set out the process to be followed in the event of concerns being raised
D Keep a record of all concerns raised, and all of the above
Q10 In what year were the CRB and the ISA brought together to create the DBS?
A 2006
B 2012
C 2021
D 2018
Supported by dental group Clyde Munro, the first all-female Scots rowing team embarks on historymaking trip across the Atlantic. The team will be taking on the challenge in the iconic boat used by world-record holders – The McLean brothers.
Four determined Scots are setting off on ‘The Atlantic Challenge’ a 3,000 miles rowing trip across the Atlantic Ocean, competing alongside 35 crews from across the world in what is widely regarded as the world’s toughest rowing challenge. Their mission is clear – to become the first allfemale Scottish team of four to row any ocean, while also aiming to set a world record.
The team, named ‘Scotland the Wave’, consists of Andrena McShane-Kerr 42, Fiona Deakin 59, Heather McCallum 30, and Nicola Matthews 59. They will row in relentless shifts of two hours on, two hours off, 24 hours a day, for up to 55 days at sea, facing 40-foot waves, fierce storms, salt sores, seasickness, and extreme sleep deprivation.
Each teammate will burn more than 5,000 calories a day, consume up to 10 litres of water, and collectively complete more than 1.5 million strokes. The team’s journey has been supported by Clyde Munro Dental Group, who have provided dental care packs for the race and a free full dental check-up for each rower upon their return.
Protecting oral health is a key consideration for the rowers involved in this impressive endurance journey and where there will be frequent use of sports drinks, gels and energy bars there is an increased risk of tooth decay, enamel erosion and gum disease.
The Clyde Munro clinicians have been on hand to offer advice and guidance. drawn from the group’s specialist expertise in Sports Dentistry, delivered through SmilePlus Dental Practice & Implant Centre in Edinburgh.
Charlie Evans, Head of Clinical at Clyde Munro said: “This is a remarkable feat of endurance by the rowing team and one we are incredibly proud to support. There’s no doubt their bodies will be under a huge amount of strain, and our involvement is to support them where we can to ensure their oral health doesn’t impact on their performance, before they go, all the way out at sea and afterwards.
“For the Scotland the Wave team, it’s crucial to make sure, where possible, normal routines are kept with regards to their oral

hygiene – nobody wants a dental problem wherever they might be and certainly not in the middle of the Atlantic. My top tips for the team would be to be mindful of the frequency and timing of sugary drinks and gels to allow their saliva time to neutralise the acids that these sugars may produce.
“They should also be brushing regularly between their rowing stints with a fluoridated toothpaste. It goes without saying that they will need to drink plenty of fluids to remain hydrated.”
The rowers have all taken different paths to the Atlantic Challenge. Andrena, an accountant with a lifelong love of kayaking, mountaineering, and hill walking, assembled the team with the support of her wife and children and will raise funds for SiMBA, a charity supporting families affected by
baby loss. Nicky, a grandmother of six, has always dreamed of completing the Atlantic Challenge since she first heard about it 20 years ago. She will be raising vital funds for RNLI.
Fiona, a single mum of three, coastal rower, and B&B owner in Cromarty on the Black Isle, will take on the challenge just weeks before her 60th birthday, rowing for Breast Cancer UK in honour of family and friends affected by the disease. Heather, who works for Police Scotland, only began rowing after signing up for the challenge. An experienced adventurer, she has skydived, bungee-jumped, and volunteered in Rwanda, and she is raising funds for the Scottish Charity Air Ambulance.
A For further information about the challenge, visit https://scotlandthewave.com/

A D Griffin, MBE

A D Griffin, MBE.
Aims:
■ Gain a clearer understanding of the current GDC Scope of Practice
■ Keeping up-to-date with registration requirements
CPD Outcomes:
■ Maintenance and development of knowledge and skill within your professional scope
■ Maintain professional standards as required by the GDC guidelines
■ Put patients’ interest first
Development Outcome: C&D
The updated GDCs Scope of Practice document1 (Nov. 2025) applies to all the Dental Team members and is structured to ensure patient safety and to guide registrants.
Section One of the updated guidance needs careful reading as without an understanding of that section a real appreciation of the Section Two for each profession cannot be correctly and clearly followed.
The introduction from the GDC on the Website says that the Scope of Practice: ‘… is not an exhaustive list of all tasks that a dental professional can do.’ It continues: ‘As a dental professional, your individual scope of practice is likely to change over the course of your career, whether because of changes in the technology of dentistry, or your further training and professional development.’2
The development of the updated GDC’s Scope of Practice document has been a long process involving input from the seven registration groups. Such professional requests submitted to the GDC during the development of this document included the DTA wanting recognition of the MHRA requirements etc., (see section 1.8). The signing off of custom-made dental appliances as fit for purpose is an essential role carried out by a registered and competent Dental Technician in compliance with the MHRA MDR legislation.3 In general, the GDC want to keep many aspects of their new documents generic rather than specifically referring to other legislation, so that such GDC documents remain valid for as long as possible.
In the 2025 GDC Guidance on Scope of Practice document it is stressed that dental professionals should “Put patients’ interests first and act in their best interests”. In keeping with this section one, 1.7 c) Medical Emergencies it clearly states that: “A patient could experience a medical emergency on any premises at any time, whether they have received treatment or not.
“All members of the dental team must know their role in the event of a medical emergency, and ensure they are sufficiently trained and competent to carry out that role. If the setting in which you work changes, your role in the event of a medical emergency may change as well.”
This also includes students, evidenced by the current standard as listed in the Safe Practitioner Framework 4 ( a framework of behaviours and outcomes for dental professional education) under the heading ‘Acute Conditions’, listing C 2.4.1, indicates that students must be able to ‘Identify, assess, and manage medical emergencies’.
The need to plan one’s own life-long learning is also indicated in the trainee’s requirement in S2.7 stating: ‘Describe the principles of and demonstrate personal development planning, recording of evidence, and reflective practice.’
It is clear from the structure of the 2025 Scope of Practice that individual registrants as professionals need to look to planning their life-long learning to:
a) Keep up-to-date via Continuing Professional Development (CPD) in line with the GDC guidance, and b) Plan their own future development via a structured Personal Development Plan.
So, for example in the Scope of Practice it states...
“ With further training, dental technicians can work with patients under supervision as part of a multidisciplinary team in a clinical setting undertaking further tasks, including:
A Taking impressions, intraoral scans and measurements for the purpose of making dental appliances
A Carrying out implant frame assessments
A Recording occlusal registrations5
Dental technicians do not work independently in the clinic to:
A Perform clinical procedures related to providing removable dental appliances
A Carry out independent clinical examinations
A Identify abnormal oral mucosa and related underlying structures
A Fit removable appliances
All registrant are encouraged to carefully read the introductory part, Section One. At 1.3 for example this further explains that it is the professional’s responsibility to: “… only carry out a task or type of treatment, prescribe or plan treatment, and make decisions about a patient’s care if you are sure that you have the necessary skills and are appropriately trained, competent, and indemnified or insured.”
It further suggests that if you are not clear
how this affects you that you should ask yourself the following questions:
A Have I been trained to carry out, plan or prescribe this task or treatment?
A Am I competent to carry out, plan, prescribe, or delegate this task or treatment?
A Am I appropriately indemnified or insured to carry out, plan or prescribe this task or treatment?
Then you can find out more about what is regarded as ‘trained’ and ‘competent’ in Section 1.9 of the 2025 Scope of Practice guidance. It clearly states that as a registrant, “You must use your own professional judgment to assess whether you are trained and competent to plan and carry out any activities that you take on”. It is suggested as guideline that if you are personally unsure whether you are trained, currently competent, or appropriately indemnified, then that it is useful to discuss the situation with other registrant colleagues, HR providers or maybe your Professional body, such as the DTA.
The areas that you will need to consider are likely to be the following – along with your evidence of such focused development (built from Section one,1.3),
(i) Your indemnity or insurance providers position, as there is likely to be a need for an addition to your current policy. If your employer is providing e.g., Crown Indemnity this will not be covering you for work in other situations or businesses. Maybe the best thing to do is ask your Indemnifier or Insurance provider and get a written statement to

evidence that you have sufficient personal extra cover.
(ii) Your professional organisation as in DTA, may have guidance on its Web site for members.
(iii) Your education or training provider for any additional training beyond initial registration that is supposedly providing additional skills beyond the basic scope of practice for your registration role. (NB Do check that the course provider is currently a GDC registrant with access to the areas of patients’ care you want to be involved with.)
(iv) Your manager, employer, or mentor’s guidance that is based on clear references to such professional working that you want to develop into.
(v) Your network of colleague GDC registrants.
NB Don’t forget the need to confirm that you have no communicable diseases if you are working directly with patients.
1 2025 GDC Scope of Practice document – accessed November 2025 LINK: https://www.gdc-uk.org/ standards-guidance/standards-and-guidance/ scope-of-practice
2 Accessed November 2025: https://www.gdc-uk.org/ standards-guidance/standards-and-guidance/ scope-of-practice
3 MDR Accessed November 2025: https://www.gov.uk/ government/publications/custom-made-medicaldevices/custom-made-devices-in-great-britain
4 Safe Practitioner Framework 2023 Dental Technicians: https://www.gdc-uk.org/docs/default-source/educationand-cpd/safe-practitoner/spf-dental-technician.pdf? sfvrsn=75edb41e_3
5 Scope of Practice 2025 (as above)
To complete your CPD, store your records and print a certificate, please visit www.dta-uk.org and log in using your member details.
Q1 Why might your individual scope of practice be likely to change during your career?
A Changes in technology B Your training
C Your professional development D All of the above
Q2 The updated Scope of Practice documents involved input from how many registrant groups?
A Five B Seven C Six D Three
Q3 The manufacturer of a custom-made device must meet the particular requirements of the UK MDR 2002 legislation which relates to custom-made dental devices. Where in Part 1 of the updated Scope of Practice (2025) does it suggest that GDC registrants have a legal requirement related to manufacture of custom-made dental devices?
A 1.3 B 1.5 C 1.6 D 1.8
Q4 Why would the GDC prefer to keep many aspects of it documentation generic?
A To avoid confusing registrants
B To keep printing costs down
C They remain valid for as long as possible
D Faster turnaround of new documentation
Q5 What is advised in section 1.7 c) in the revised Scope of Practice Guidance?
A A patient could experience a medical emergency on any premises at any time, whether they have received treatment or not
B Online training is the preferred method to stay current with advice
C All members of the dental team must know their role in the event of a medical emergency, and ensure they are sufficiently trained and competent to carry out that role
D a) and c) only
Q6 In the new Scope of Practice dental technicians can undertake which tasks while under supervision?
A Take impressions
B Perform intraoral scans
C Take measurements
D All of the above for the purpose of making dental appliances
Q7 Which of the following is NOT a procedure that a dental technician can undertake?
A Taking impressions
B Recording facebows
C Carrying out intra-oral and extra-oral tracing
D Identify abnormal oral mucosa and related underlying structures
Q8 As a GDC registrant you must use your own professional judgment to assess whether you are trained and competent to plan and carry out any activities that you undertake, and so you...
A Must have evidence of being trained in a particular activity and d) only.
B Would be considered as currently competent and knowledgeable about the aspect by other relevant registrants.
C As a registered professional areas a), b) and d) are essential to be able to carry out the activities within your registration scope.
D Appropriately indemnified/insured for the activity at the site of your work and b) only.
Q9 Which message is stressed as a key part of the Scope of Practice for all dental professionals?
A Make friends with patients, this will help overcome dental phobia
B Keep the workplace light and airy to reduce stress
C Always put the patients’ interests first
D Maintain a healthy work/life balance to avoid burn-out
Q10 According to the Guidance what must individuals do in planning life-long learning
A Keep up to date with CPD and have a structured Personal Development Plan
B Talk to registered colleagues to discover the best training options
C Set aside a few hours every week to study relevant online material
D Have a fully integrated digital information workflow from your material and technology providers
Tracey O’Keeffe, Coach Practitioner and Mindfulness Teacher MA (Education), BSc (Critical Care), RN, MAFHP, MCFHP
Research in gut health and its overall impact on the human body and wellbeing has been increasing steadily, but there are still unanswered questions with new science appearing regularly on the subject (Van Hul et al. 2024). This paper will explore the concept of gut health, what it is, how we can maintain a better gut health, and ultimately how that supports our body function. It will also consider some of the potential risks of not caring for your gut health.
The term gut health is becoming more common place in everyday life as well as in medicine. Foods in supermarkets will advertise themselves as “good for the gut” or use terminology such as “tummy love”, but defining what good gut health is, is not perhaps as clear cut. Bischoff et al. (2011) suggest that just measuring gut health can be problematic requiring both a quantitative and qualitative approach. Validated biomarkers provide one element, but this cannot be removed from understanding the experience of the
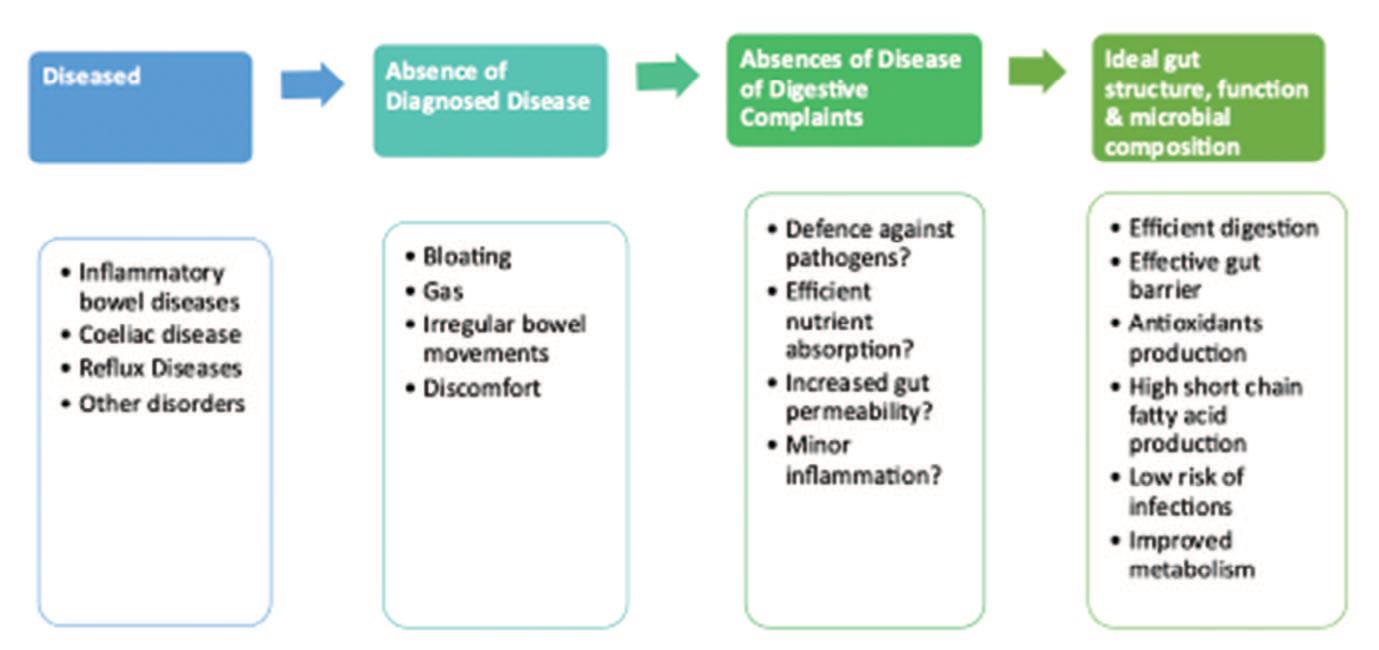
individual, their subjective view of gut health, and how these two sets of data relate to each other. Indeed, Van Hul et al. (2024) refer back to the basic confusion of what “healthy” means overall, demonstrating the complexity of diagnosing and labelling a gut as healthy or suffering with dysbiosis, the term used to describe imbalances in the microbial makeup of the gut (see Figure 1). This reflects and aligns to the World Health Organisation (2025) definition of health which takes into account a holistic, biopsychosocial view of wellbeing.
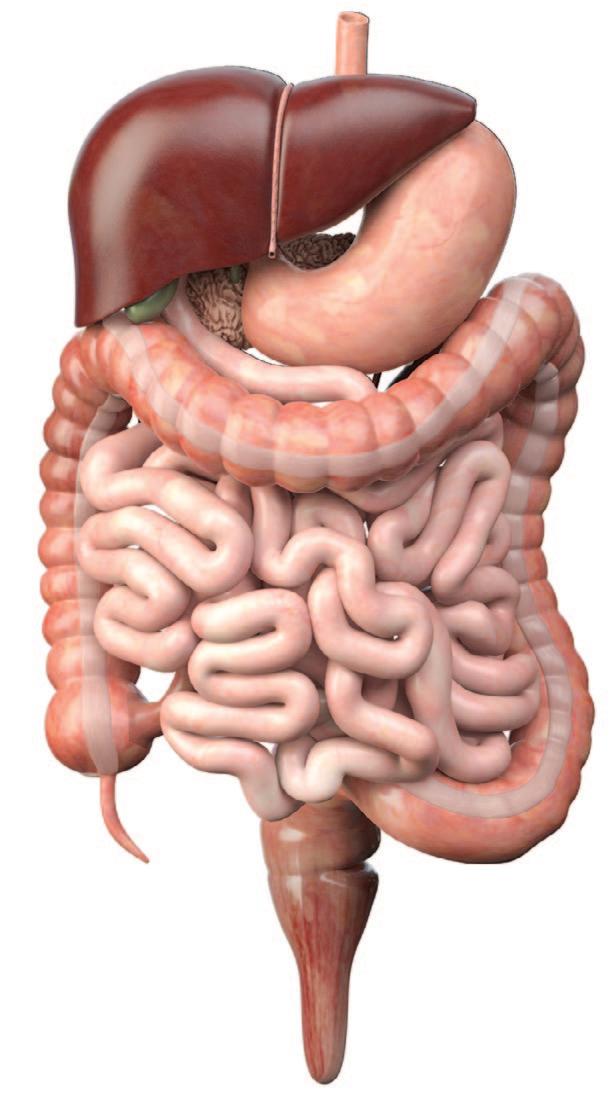
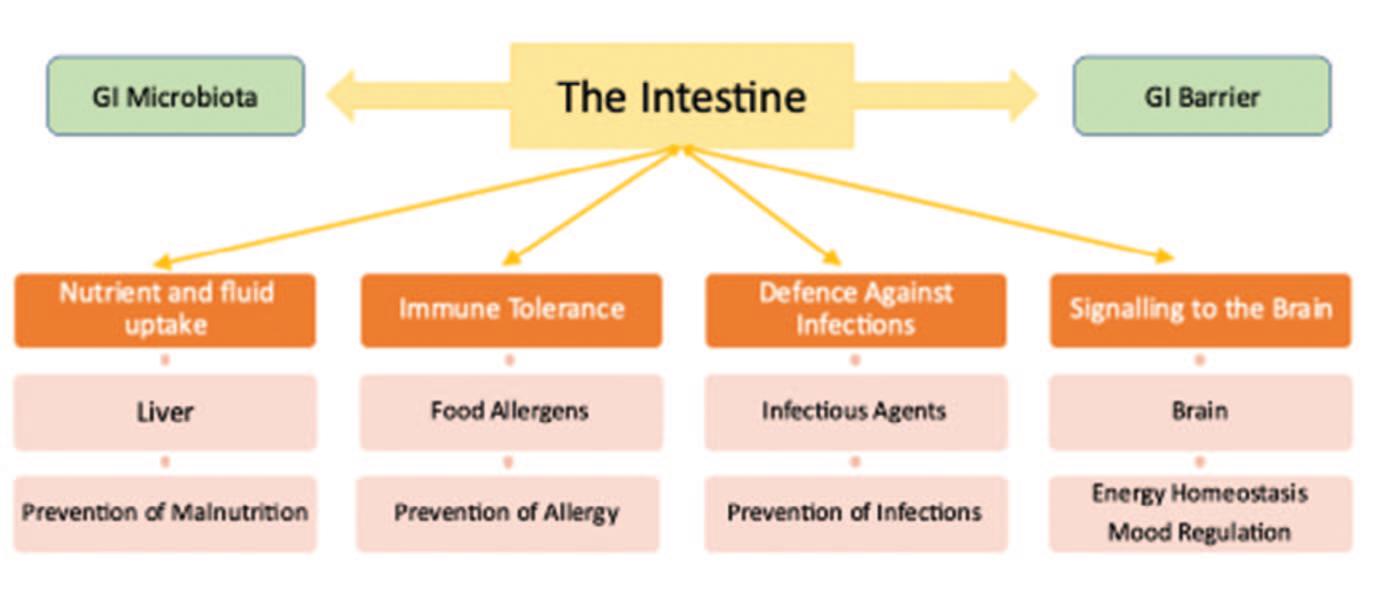
In simple terms, gut health is not just the absence of a confirmed digestive problem or a series of symptoms. It relates to a wellfunctioning gut and one which has the necessary amount of beneficial bacteria, especially in balance to the harmful, opportunistic bacteria. Furthermore, it is apparent that alongside the presence of a “good” microbiome, the integrity of the gastrointestinal (GI) barrier is important for overall health (Fasano et al. 2005; Meddings 2008).
A healthy microbiome supports immunity, infection prevention and energy homeostasis. It also contributes to the maintenance of the GI barrier. The importance of this is evident with links between GI barrier damage (or leaky gut) and the development of allergic, inflammatory or infectious disease processes (Groschwitz and Hogan 2009; Preidis and Versalovic 2009). Proving absolute causation is not always possible with current research based more upon correlation (Cani et al. 2021). However, understanding the connections between gut and health can be viewed by seeing it as four main pathways which contribute to health (Bischoff et al. 2011) (see Figure 2) and this can help visualise how powerful a healthy gut can be to overall function.

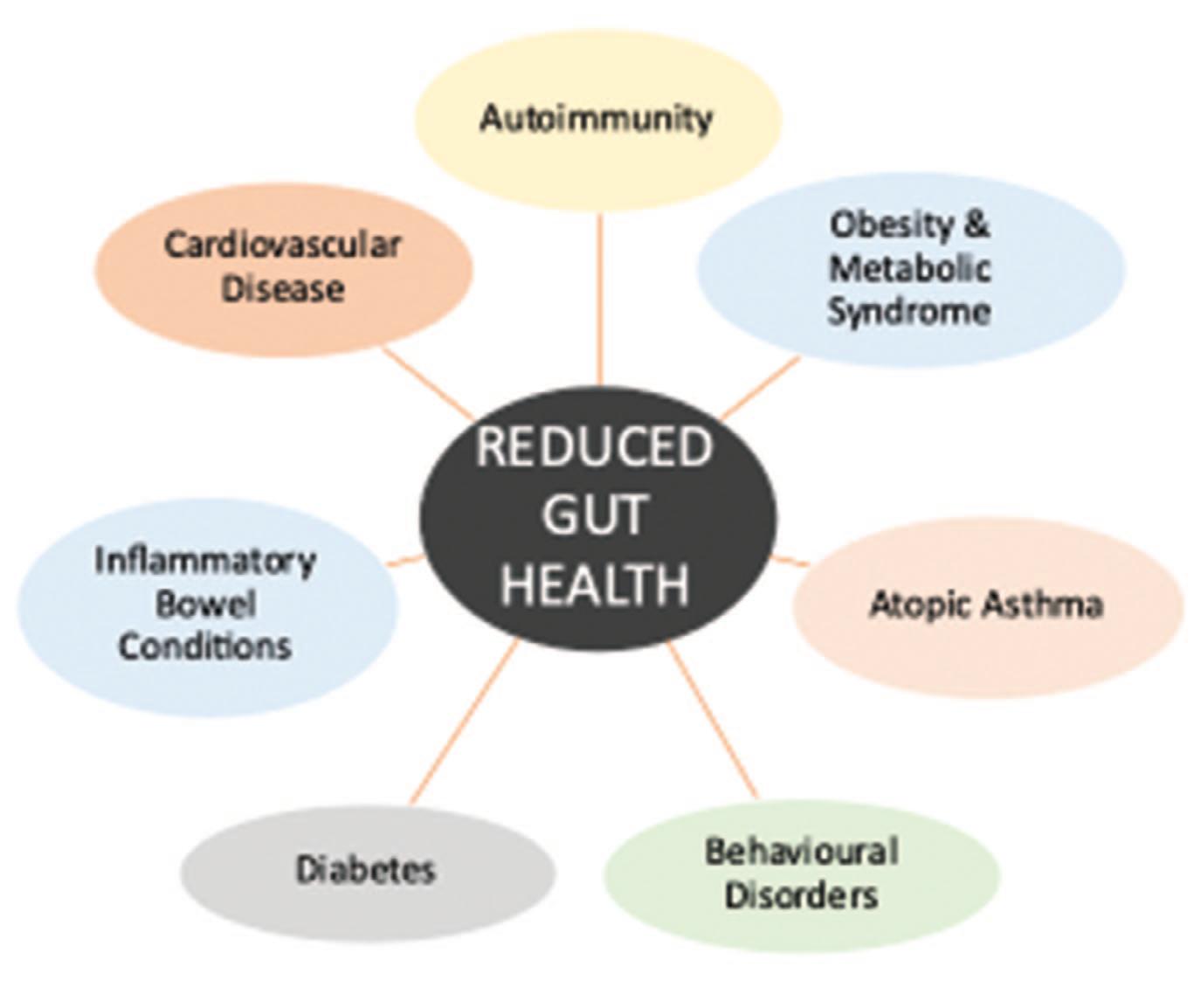
Interruptions or disruptions to these pathways are likely to cause problems throughout the body. Figure 3 highlights some of the disease processes and conditions showing links to dysregulation of gut health. With increasing numbers of people being diagnosed with long term conditions, it is important to understand if gut health plays a part in this and whether changes to lifestyle may be able to mitigate against illness or support improvement in wellbeing. Indeed, Durack and Lynch (2018) suggest that understanding the gut’s connection with remote organs and then working with modulation and rehabilitation of disturbed microbiomes may ultimately help to restore health, prevent disease, and work with chronic conditions through a new approach.
The gut hosts the largest microbial volume across the body (de Vos et al. 2022), and despite variations in between individuals,

there seems to be a core of essential species which support health (Lozupone et al. 2012).
Gut health starts early in life with theories around infants developing a unique microbiome composition which may even be originally commenced in utero (Durack and Lynch 2018). As people age the microbiome can lose both diversity and stability (Odamaki et al. 2016) unless actively addressed. Physical factors such as gut motility, stomach acidity and the production of bile acid also affect the balance and variation. However, other internal factors affect the microbial population including oxygen levels, mucus production and intestinal pH (Van Hul et al. 2024).
As well as intrinsic variables, the microbiome has to deal with external disturbances. Although the gut has some resilience to maintain homeostasis and balance, longerterm exposure can cause problems (Candela et al. 2012, Fassarella et al. 2021). These influences include diet (including processed food), overuse of antibiotics and some medications, environmental pollutants, birth
methods and stress (Van Hul et al. 2024). The microbiome balance may shift in favour of unhelpful and harmful bacteria.
Zhang (2022) suggests that positive nourishment for a healthy gut microbiome comes from an approach to food which focuses on balanced nutrition. This should include fibre-rich foods and a reduction in simple sugars and saturated fats or emulsifiers. This is particularly important for individuals with pre-existing problems such as inflammatory bowel disease. As well as reducing the diversity of the microbiome, highly processed foods can interfere with the GI barrier increasing permeability and triggering inflammatory responses via the “leaky gut” mechanism (Mu et al. 2017).
An unusual and extreme diet can also cause problems. One example would be an excessively high protein intake. This can cause
the body to focus in on protein fermentation instead of gut bacteria metabolism, ultimately reducing the ability of the body to main gut homeostasis (Zhang 2022). Indeed, David et al. (2014) suggest that the gut microbiome can be affected in only one day by high-fat, high-protein and low-fibre diets. Using a high plant-based approach to increase fibre can positively enhance gut bacteria by a natural increase in fibre (Bischoff 2011). One option for a balanced approach to nutrition is that of the Mediterranean diet (Hills et al. 2019), which can also support good cardiovascular health. There are some key messages here, but it is also complex. Hills et al. (2019) also highlight that although high fibre is a positive dietary contribution, overall high carbohydrate can result in reduced diversity of microbiome. Strangely, coffee, tea and red wine which are high in polyphenols associated with prebiotic activity, may in fact be beneficial in safe amounts with some antiinflammatory problems and an increase in diversity.
Prebiotic and probiotics work to improve the resident bacteria in colon with an overall improvement in the health of the host. Hills et al. (2019) suggest that supplementary forms may be useful in some groups of individuals. They may help with restoration of leaky gut and a healthy mucosal immune system (Bischoff et al. 2011). Similarly, maintaining adequate vitamin intake may influence gut health. Pham et al. (2021) highlight the importance of therapeutic levels of vitamins, suggesting their bi-directional role with gut microbiome. Bischoff et al. (2011) also advocate the absence of tobacco products.
Stress is also an important factor to consider in terms of lifestyle management. Increased psychological stress may increase the likelihood of leaky gut allowing antigens and toxins to enter the bloodstream (Hills et al. 2019). Mechanisms for managing stress will vary for individuals, but they include mindfulness practice, exercise generally, or finding bespoke relaxation techniques. Bischoff et al. (2011) highlight the particular
danger of chronic stress and its potential impact on poor gut homeostasis and microbiome. Through links with the enteric nervous system, dysfunctional or unbalanced microbiota can impact the nervous system. Changes in gut health can result in the neuroendocrine hormones and neurotransmitters release being adversely affected, with implications for depression or anxiety (Hills et al. 2019). This can further exacerbate any chronic stress or emotionally instability.
Some medications including overuse of nonsteroidal anti-inflammatory medication and antibiotics can interfere with gut health. Whilst necessary in some scenarios, sustained or inappropriate use can result in resistance or damage to the microbial flora of the gut. Hills et al. (2019) highlight the danger of alteration to the short chain fatty acid fermentation in the gut. Antibiotics can deplete this process and consequently affect the overall microbial homeostasis. Zhang (2022) suggests that recovery from antibiotics, with full
establishment of balance again, can take considerable months or years. Use, therefore, should be targeted, balanced and strategic, rather than indiscriminate.
It can be seen that there are interventions that can be implemented which may support positive gut health. Similarly, there are areas where changes can be made with a view to reducing damage to the GI microbiota and GI barrier (see Figure 4)
One final point of note is new more experimental treatments coming into play. One such intervention is faecal microbiota transplantation (FMT). The process involves manipulating the current gut flora of the individual by taking a donor faecal sample from a “healthier gut” of another person. Associated risks are evident and not fully explored, but there have been successful and positive results, particularly in more chronic and debilitating gut problems (Durack and Lynch 2018).
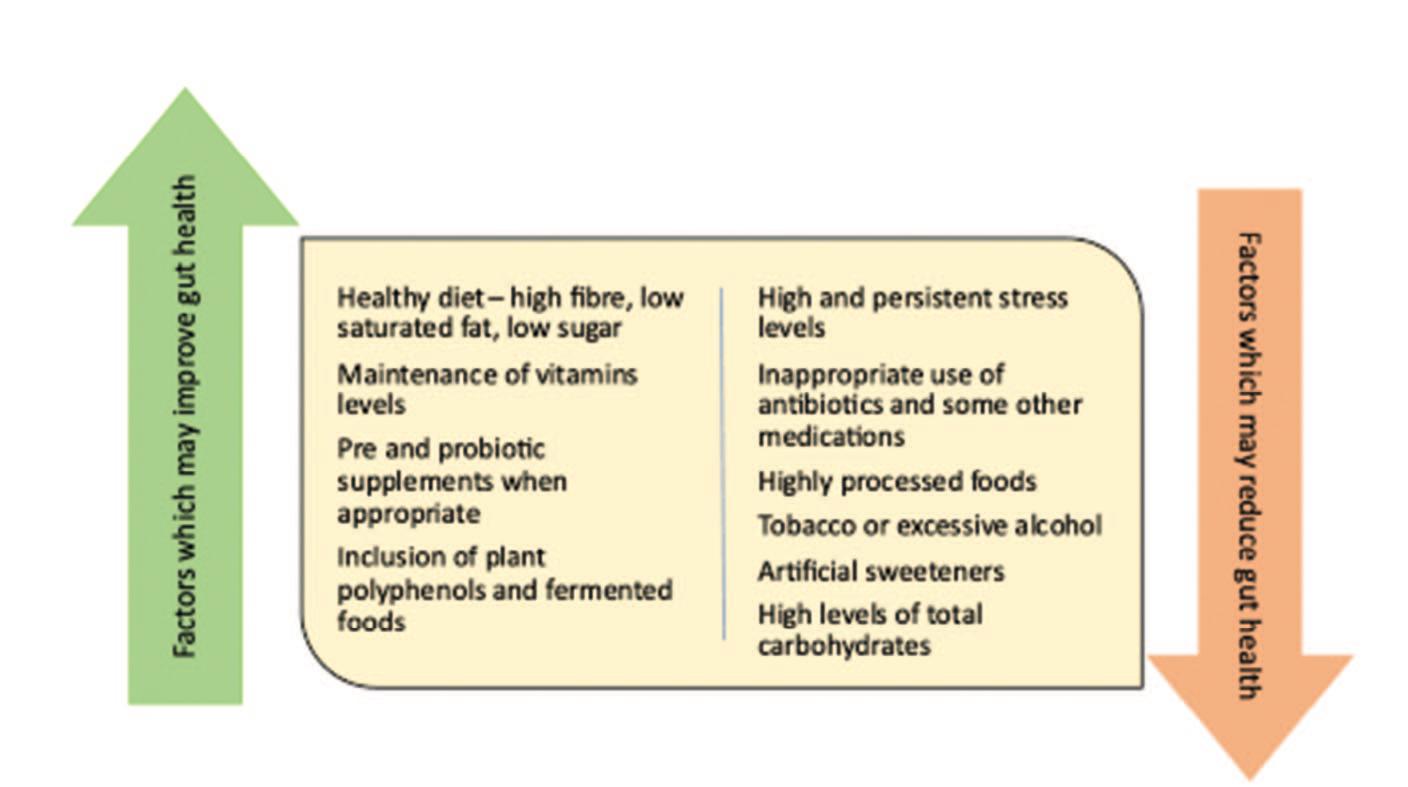
The science behind gut health and its effect on the body could still be considered in infancy. The two key elements are maintenance of a balance microbiome alongside an intact gastrointestinal barrier. There are some generic approaches that can be taken including a nutritious diet emphasising high fibre, low saturated fat and low sugar intake. Lifestyle changes which support a reduction in stress may also be beneficial. Although complex, the positive message is one of personal control over health and prevention of chronic illness. Being aware of connections between the gut and long-term conditions provides individuals an opportunity to influence their own wellbeing.
References
A Bischoff, S.C. 2011. “Gut health”: a new objective in medicine? BMC Medicine, 9 (24).1-14
A Candela, M., Biagi, E., Maccaferri, S., et al. 2012. Intestinal microbiota is a plastic factor responding to environmental changes. Trends Microbiol. 20:385–91
A Cani, P.D., Moens de Hase, E., Van Hul, M. 2021. Gut Microbiota and Host Metabolism: From Proof of Concept to Therapeutic Intervention. Microorganisms 9:1302
A David, L.A.; Maurice, C.F.; Carmody, R.N.; Gootenberg, D.B.; Buton, J.E.; Wolfe, B.E.; Ling, A.V.; Devlin, A.S.; Varma, Y.; Fischbach, M.A.; et al. 2014. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 505, 559–563
A Deehan, E.; Duar, R.M.; Armet, A.M.; Perez-Muñoz, M.E.; Jin, M.; Water, J. 2017. Modulation of the gastrointestinal microbiome with nondigestible fermentable carbohydrates to improve human health. Mirobiol. Spectr. 5 BAD-0019-2017.df
A de Vos, W.M., Tilg, H., Van Hul, M, et al. 2022. Gut microbiome and health: mechanistic insights. Gut. 71:1020–32
A Durack, J. and Lynch, S. V. 2018. The gut microbiome: Relationships with disease and opportunities for therapy. Journal of Experimental Medicine. 216. 1. 20–40
A Fasano, A, Shea-Donohue, T. 2005. Mechanisms of disease: the role of intestinal barrier function in the pathogenesis of gastrointestinal autoimmune diseases. Nat Clin Pract Gastroenterol Hepatol. 2:416-422. 18
A Fassarella, M., Blaak, E.E., Penders, J., et al. 2021. Gut microbiome stability and resilience: elucidating the response to perturbations in order to modulate gut health. Gut 70:595–605
A Groschwitz, K.R., Hogan, S.P. 2009. Intestinal barrier function: molecular regulation and disease pathogenesis. Journ Allergy Clin Immunol 124:3-20
A Hills, R. D., Pontefract, B. A., Mishcon, H. R., Black, C. A., Sutton, S. C., & Theberge, C. R. 2019. Gut Microbiome: Profound Implications for Diet and Disease. Nutrients. 11.7.1613. https://doi.org/ 10.3390/nu11071613
A Lozupone, C.A., Stombaugh, J.I., Gordon, J.I., et al. 2012. Diversity, stability and resilience of the human gut microbiota. Nature New Biol. 489:220–30
A Meddings, J. 2008. The significance of the gut barrier in disease. Gut 57:438-440. 20
A Mu, Q.; Kirby, J.; Reilly, C.M.; Luo, X.M. 2017. Leaky gut as a danger signal for autoimmune diseases. Front. Immonol. 8. 598
A Odamaki, T., K. Kato, H. Sugahara, N. Hashikura, S. Takahashi, J.Z. Xiao, F. Abe, and R. Osawa. 2016. Age-related changes in gut microbiota com position from newborn to centenarian: a crosssectional study. BMC Microbiol. 16:90. https://doi.org/10.1186/s12866-0160708-5
A Pham, V. T., Dold, S., Rehman, A., Bird, J., Steinert, R. 2021. Vitamins, the gut microbiome and gastrointestinal health in humans. Nutrition Research 95. 35-53
A Preidis, G.A., Versalovic, J. 2009. Targeting the human microbiome with antibiotics, probiotics, and prebiotics: gastroenterology enters the metagenomics era. Gastroenterology 136:2015-2031
A Van Hul, M., Cani, P.D., Petitfils, C., et al. 2024. What defines a healthy gut microbiome? Gut 73:1893–1908
A World Health Organisation. 2025. Health and Wellbeing. [accessed 8.1.26]. Available at: https://www.who.int/ data/gho/data/major-themes/healthand-well-bein
A Zhang, P. 2022. Influence of Foods and Nutrition on the Gut Microbiome and Implications for Intestinal Health. Int. J. Mol. Sci. 23. 9588. https://doi.org/ 10.3390/ijms23179588
To complete your CPD, store your records and print a certificate, please visit www.dta-uk.org and log in using your member details.
Q1 What is dysbiosis?
A Poor gut health’s effect on endocrine system
B Imbalances in the microbial make-up of the gut
C Psychological confusion caused by leaked toxins in the blood
D Toxicity caused by an ultra-processed diet
Q2 In simple terms gut health is described as what?
A A well-functioning gut
B Supports opportunistic bacteria
C Has the necessary amount of beneficial bacteria and (a
D Integrity of the GI barrier and (a and (c
Q3 How many main pathways are there between the gut and overall health?
A Six
B Three
C Four
D Five
Q4 Working with the modulation and rehabilitation of disturbed microbiomes may ultimately do what?
A Restore health
B Help lower high blood pressure
C Work with chronic disease, prevent disease, and (a only
D Reduce chances of developing Alzheimer’s disease and (c only
Q5 Which of the following is NOT listed as affecting the microbial population?
A Oxygen levels
B Lack of vitamin D
C Mucus production
D Intestinal pH
Q6 What may result from a poor diet (including processed food), overuse of antibiotics and some medications, environmental pollutants, birth methods and stress?
A Swelling in the joints
B Microbiome balance may shift in favour in favour of harmful bacteria
C Obesity
D Loss of balance in blood sugar levels leading to type 2 diabetes
Q7 The Mediterranean diet is described as providing a balanced approach to nutrition, and what?
A Good cardiovascular health
B Reduced waistline
C Improved memory
D Healthier gingivae
Q8 Why might coffee, tea, and red wine be beneficial in ‘safe amounts’
A The body can absorb them easily
B Low sugars and carbohydrate content
C They actively help reduce fatty lipids
D They are high in polyphenols
Q9 Increased psychological stress may increase the likelihood of what?
A High sugar in the gut leading to bloating and flatulence
B Leaky gut allowing antigens and toxins to enter the bloodstream
C Increase in bilirubin levels in the bloodstream
D Poor absorption of nutrients leading to fatigue
Q10 Changes in gut health resulting in neuroendocrine hormone and neurotransmitter release is described as having implications for what?
A Poor visibility due to raised glucose levels in the eyes
B Depression or anxiety
C Chronic reflux acid and potential ulcers
D Dizziness and nausea

The Technologist completes its review of Ella Cook’s dissertation based on a survey she undertook in March 2025 to investigate the views of Dental Technicians in the UK regarding the then current Scope of Practice (SoP). Ella’s research is still of interest because it provides a voice to the Dental Technicians she interviewed, but to get the latest insight into the GDC Guidance for Scope of Practice see the article by Anthony Griffin in this issue, starting on page 21.
with the Current
Figure 1 demonstrates that most respondents (61%) reported being ‘very familiar’ with their SoP, while 31% felt ‘somewhat familiar.’ A small proportion (4%) were ‘neither familiar nor unfamiliar,’ and another 4% were ‘not very familiar.’ No respondents reported being ‘not at all familiar.’
A Spearman’s rank correlation coefficient was conducted to assess the relationship between the number of years practising and familiarity with the SoP among Dental Technicians. The analysis found no statistically significant association between years of practice and familiarity with SoP (p=0.302, p>0.05). [Appendix G.1].
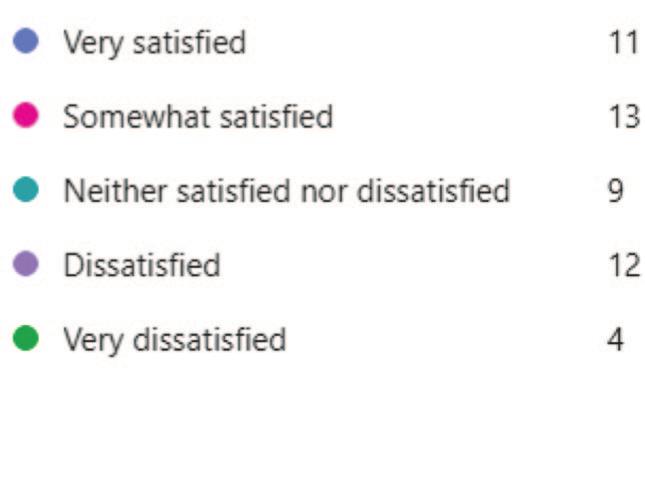
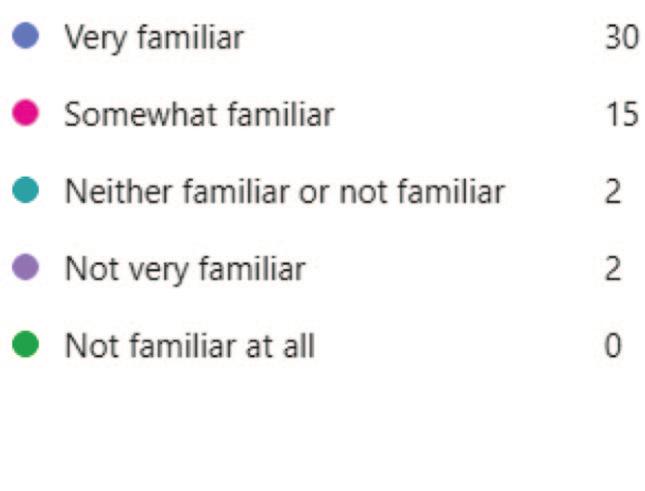
Figure 2 indicates varied satisfaction levels among respondents. While 22% were ‘very satisfied,’ and 27% were ‘somewhat satisfied,’ 18% were ‘neither satisfied nor dissatisfied’. Meanwhile, 24% were ‘dissatisfied,’ and 8% were ‘very dissatisfied.’
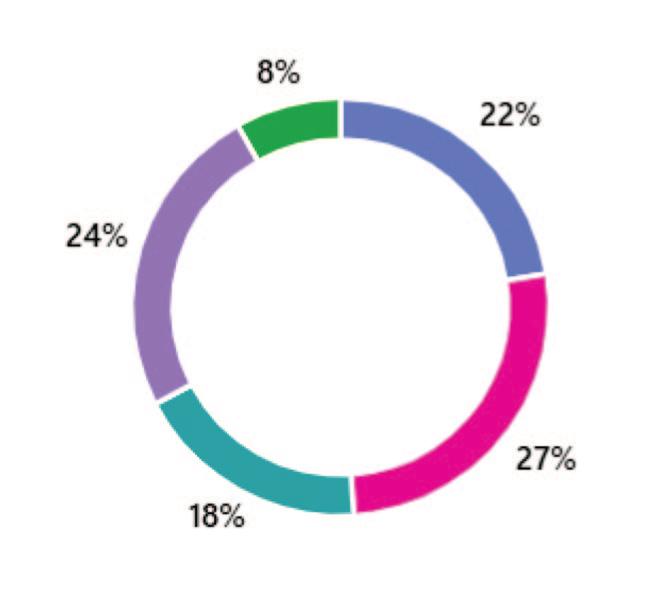

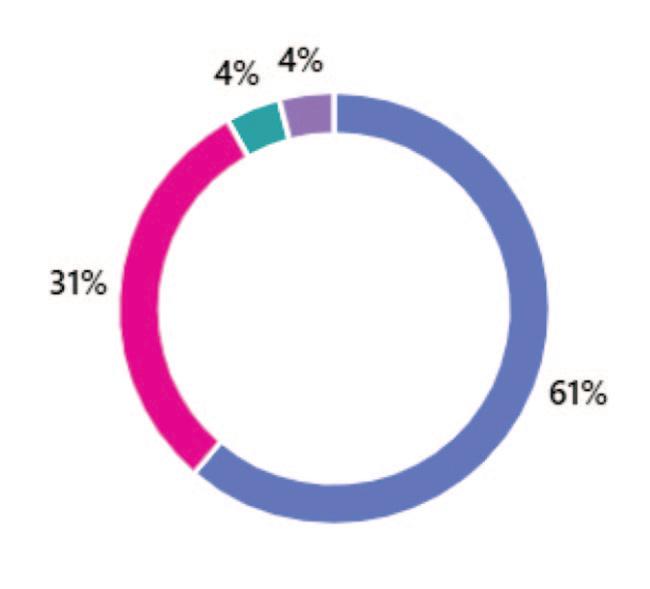
Figure 3 highlights that 24% of respondents strongly agreed that the Scope of Practice limited their ability to fully utilise their skills and training, while 18% agreed. Meanwhile, 27% were neutral, 14% disagreed, and 16% strongly disagreed.
Figures 4 and 5 show that 59% of Technicians reported being asked to work outside of their SoP. Among them, 56% identified Dentists as the primary source of these requests, while 38% reported patients as another common source. Of those who selected ‘other,’ 5% identified Laboratory Owners as the source of these requests.
5.2.5 Dental Professionals’ Understanding of Technicians’ Scope
As shown in Figure 6, 41% of Dental
: A
illustrating respondents’ perceptions of how their SoP influences their ability to utilise their skills and training
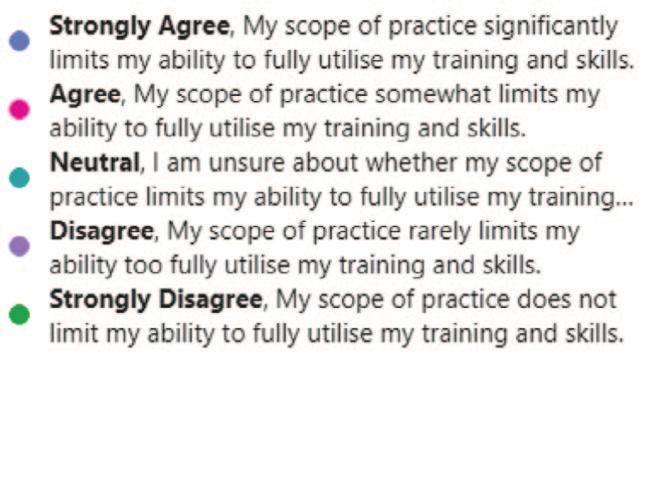
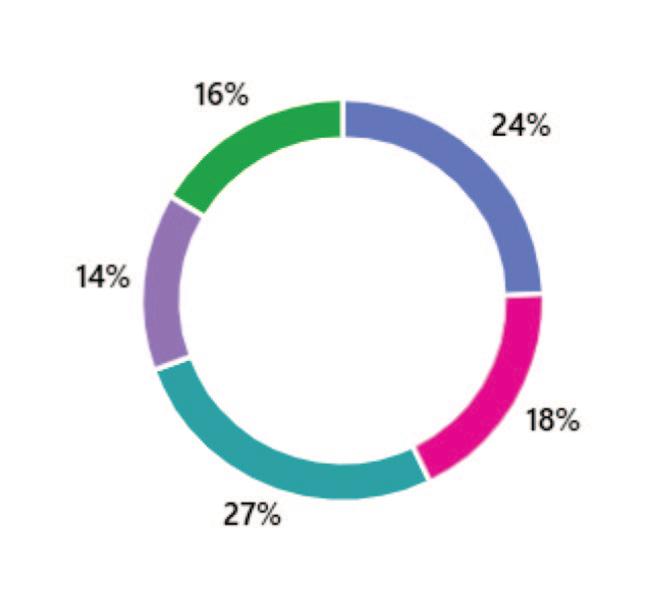

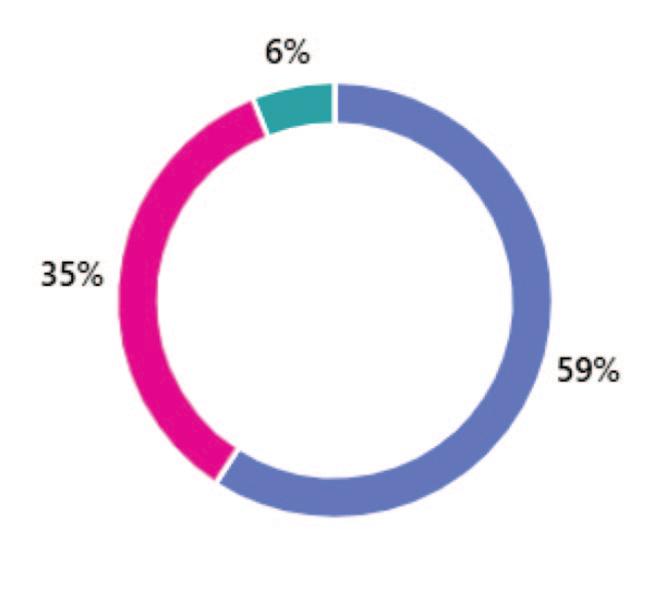
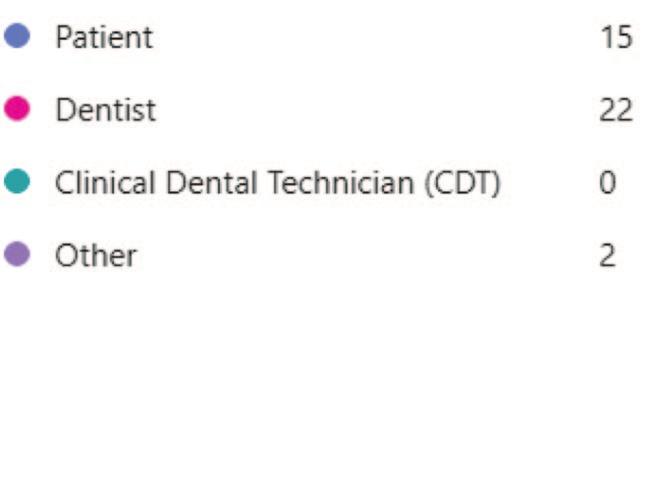
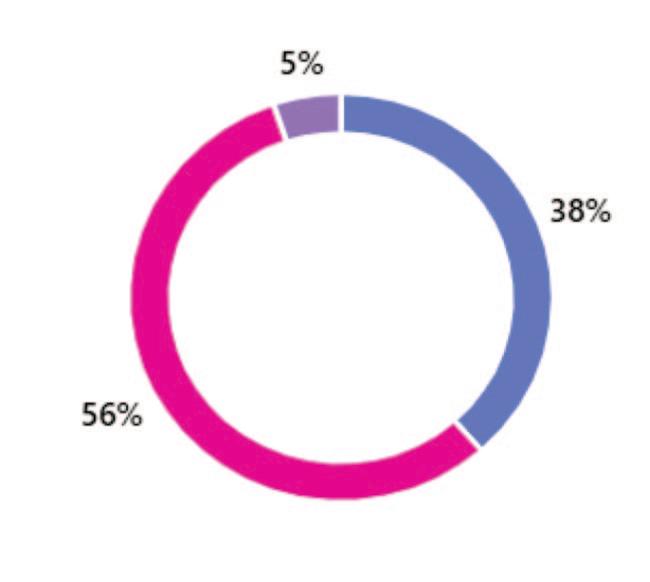
Technicians believed that other DCPs had a limited understanding of their SoP. Additionally, 27% reported a lack of understanding, while 8% felt neutral. The remaining 24% believed that other DCPs had at least some knowledge, with 8% feeling that other DCPs understood the scope well.
5.3.1 Technicians’ Views on Expanding Their Scope
Figure 7 reveals that 45% of respondents supported expanding the current SoP, while 31% were unsure, and 24% believed it should remain unchanged.
Open-text responses indicated that 50% of respondents wished to see SoP expanded to allow Technicians to take impressions.
For example, one respondent stated, “Take impressions, provide retainers, night guards & sport guards to the general public” (Participant 26).
Another said: “I feel that technicians should be able to take impressions after some basic training” (Participant 5).
Many respondents believed that being able to take impressions under certain circumstances would improve access to dental care:
“If I could do impressions, I would be able to help with relines and additions. There are no NHS dentists in our area and the elderly especially suffer because of this.” (Participant 10).
Conversely, respondents who opposed expansion felt that the current SoP accurately reflected their role: “We are manufacturers; we do not need to take impressions or work in the mouth” (Participant 12).
Other comments emphasised the existing career path for Dental Technicians who are interested in having a greater SoP: “There is already a career path to becoming a Clinical Dental Technician (CDT), which allows for a greater scope of practice” (Participant 47).
Figure 8 shows that 78% of respondents would be willing to complete additional training if the SoP were expanded. Only 10% were unwilling, and 12% were unsure.
Figure 6: A pie chart depicting how well Dental Technicians felt other DCP’s understood their SoP
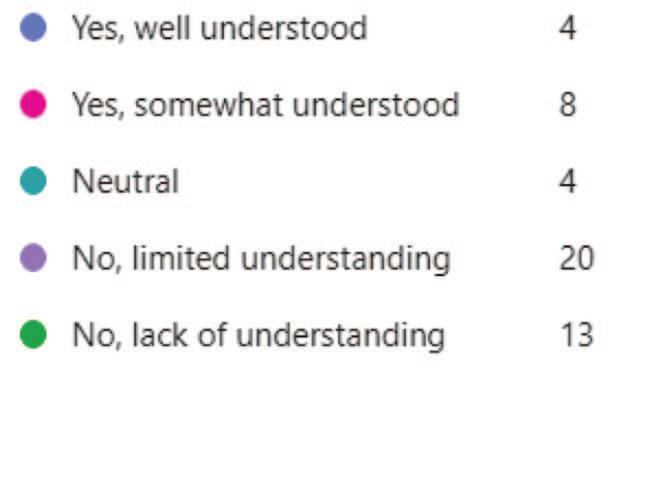
Recurring themes in free-text responses included digital technology, disparities in training and SoP, dentists’ understanding of technicians’ roles, frustrations with the GDC, and a perceived lack of recognition and respect.
5.4.1
Respondents highlighted the need for digital technologies and their impact to be included into the SoP. One stated: “The use of digital equipment would allow us to provide more products to the public” (Participant 21).
Another commented that “With new technologies, the scope may need to be expanded” (Participant 27).
Several respondents expressed concern about disparities between training and SoP, particularly in relation to the SoP of other DCPs. One stated: “Dental Nurses can now perform many Dental Technician tasks despite not having adequate training” (Participant 26).
Another mentioned that “DTs are unable to carry out tasks that GDPs are carrying out, however, GDPs have not been trained in this area” (Participant 8).
5.4.3
Participants noted that many dentists, especially newly qualified ones, lacked

technical knowledge: “Few dentists understand how to make good removable dentures” (Participant 9).
Another commented that: “Today’s generation of dentists know less and less about dental technology. They leave patients’ treatment plans down to the
technicians as they don’t have the sufficient knowledge of materials, design options” (Participant 41).
Some respondents felt that Dental Technicians are “extremely undervalued members of the dental team” (Participant 10). One commented: “With every advanced qualification I gain, the respect I receive from general dentists decreases” (Participant 1).
5.4.5
Several respondents expressed frustrations towards the GDC. One stated, “The GDC have absolutely no idea what technicians do and have never worked in or visited a laboratory in their lives” (Participant 20). Respondents criticised the GDC for
Figure 7: A pie chart depicting the percentage of Dental Technicians who believe their SoP should be expanded
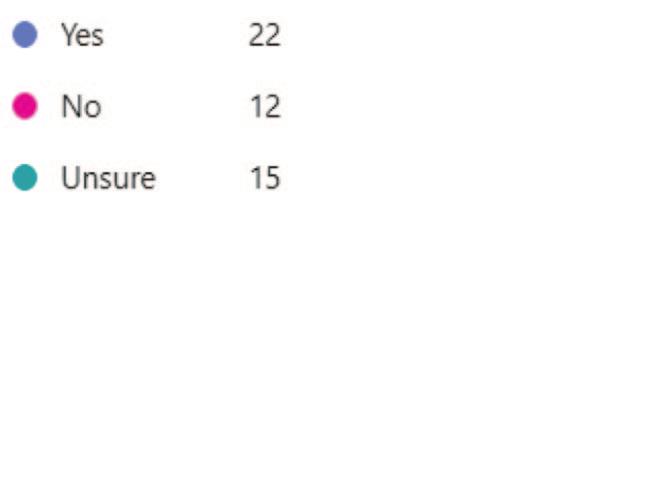
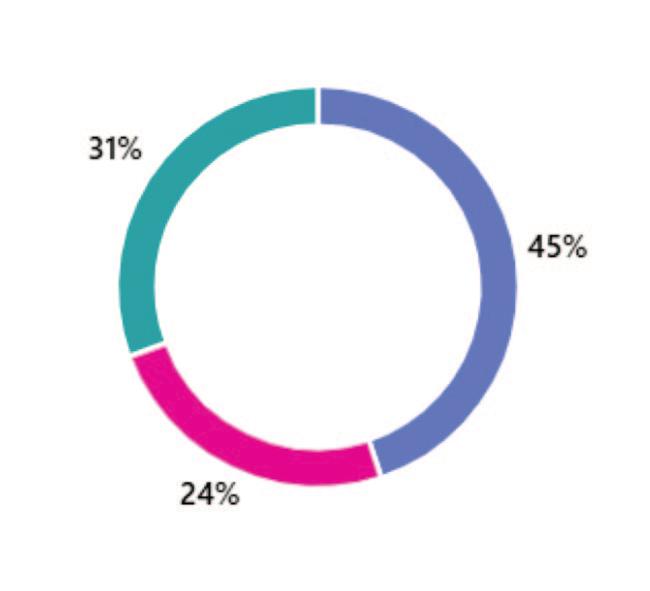
Figure 8: A pie chart showing Dental Technicians’ willingness to undergo additional training if SoP was expanded
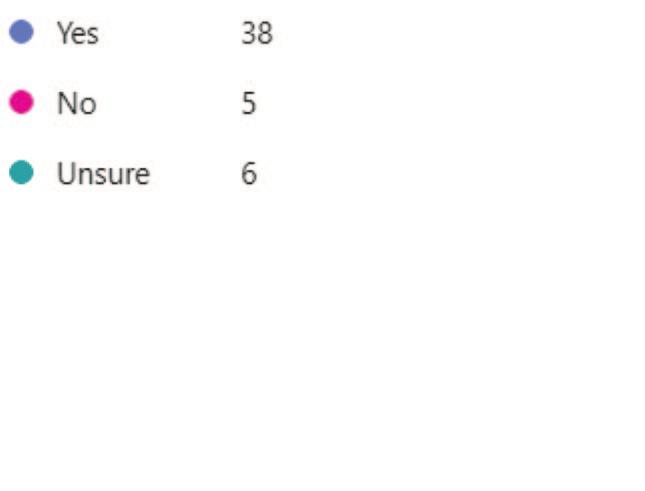
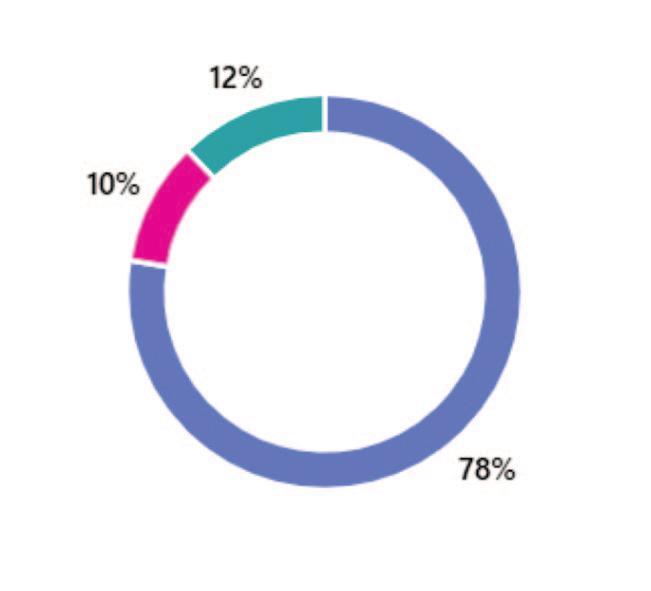
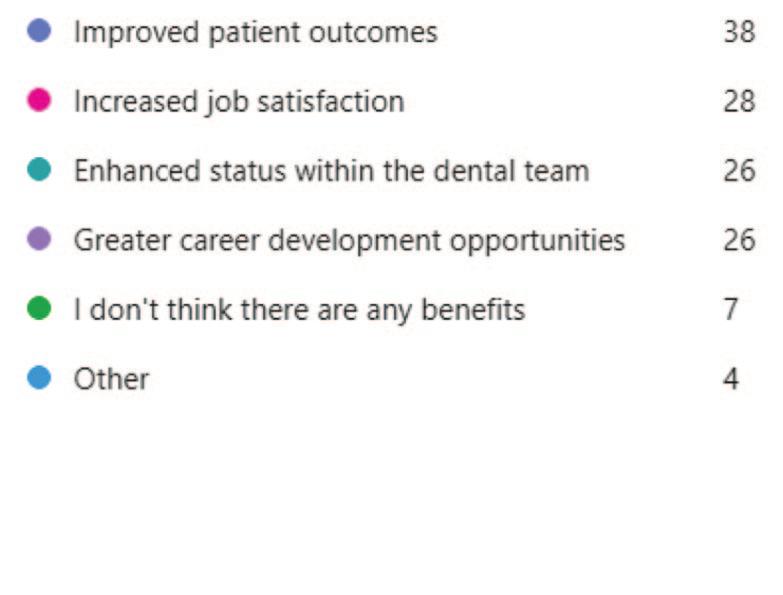
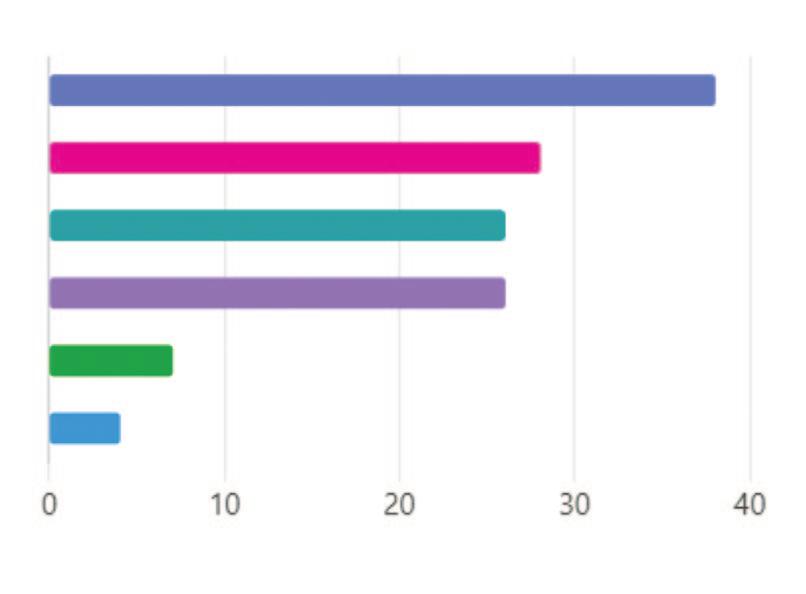
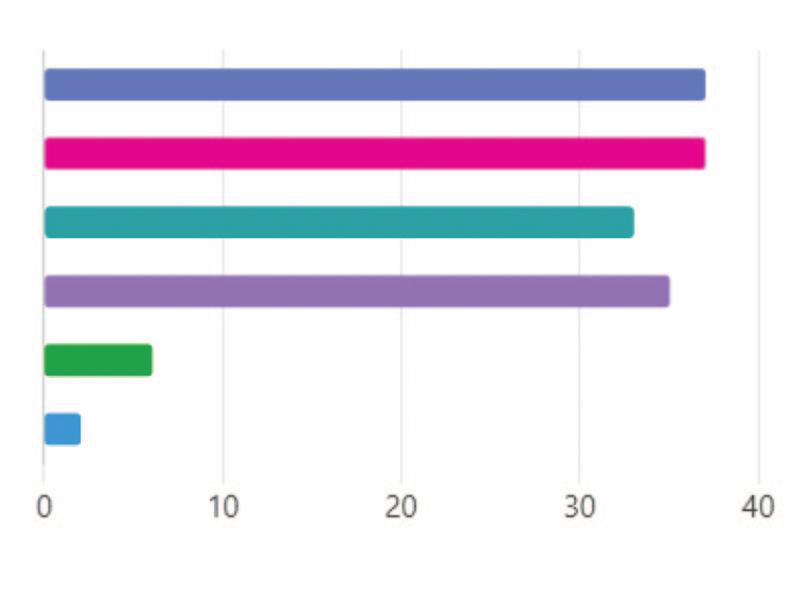
prioritising dentists over technicians: “The GDC just protects dentists and does not care about technicians” (Participant 38).
Figure 9 shows that improved patient outcomes (29%) and increased job satisfaction (22%) were the most commonly identified benefits if the SoP was to be expanded.
Figure 10 highlights that the main challenges identified by Dental Technicians if the SoP was to be expanded included additional training requirements (25%) and increased liability (25%). Issues of patient acceptance was the least frequently identified challenge identified by Dental Technicians (4%).
Most respondents (61%) report being very familiar with the SoP, suggesting that Dental Technicians have a good awareness of their role and boundaries.
This is slightly higher than the findings of the GDC Scope of Practice review (2020), which indicates that about 50% of Dental Technicians in the sample have a great or fair knowledge of the SoP guidance.
This study finds no statistically significant correlation between years of practice and familiarity. This differs from the GDC Scope of Practice review (2020), which suggests that more recently trained Dental Technicians have greater exposure to the SoP document during their training and, therefore, higher familiarity.
Satisfaction with the current SoP is mixed. While 49% of respondents express some level of satisfaction, 32% are dissatisfied or very dissatisfied. This suggests many Technicians feel restricted in their ability to fully utilise their skills and training.
The results suggest that there is considerable interest among Dental Technicians in wanting to see their SoP expanded, with 45% in favour and only 24% opposed. Impression-taking for certain cases is the most frequently suggested expansion, with 50% of respondents advocating for Technicians to perform this task following appropriate training. Free-text responses highlight that many Technicians believe this change would improve access to care, particularly for underserved areas struggling to access NHS dental services. This aligns with the concept of skill mix in dental care improving access to services (Cannell, 2016; Bullock, 2018), suggesting that Dental Technicians may be both willing, and in a position, to enhance their role. Encouragingly, 78% of respondents state they would be willing to undertake additional training if the SoP were expanded.
A concerning finding is that 59% of respondents have been asked to work beyond their SoP, predominantly by Dentists (56%), and less frequently by patients (38%). Further, over two-thirds (68%) of respondents feel that other Dental Care Professionals (DCPs) have a limited or poor understanding of the Technician’s scope.
This suggests a possible gap in awareness among other DCPs, particularly Dentists, regarding the role and scope of Dental Technicians. This could result in Technicians being asked to, or feeling pressured to carry out tasks outside of their SoP. One respondent echoes this, stating: “Dentist asking us to do the try-in at the lab for difficult cases without a dentist present. Not sure if this is really ok” (Participant 24).
This finding aligns with previous studies, which note that Dentists often lack understanding of the SoP of other DCPs. Bullock et al. (2018) identify a barrier to the greater implementation of skill mix regarding Dental Therapists due to Dentists’ limited knowledge of their role. Similarly, Leyssen et al. (2013) findings suggest that Clinical Dental Technicians (CDTs) feel both
patients and other DCPs were unaware of their role and scope. Additionally, the GDC SoP review (2020) indicated that the public is generally unaware of the SoP guidance document. These findings highlight the need for increased education on the role of Dental Technicians, particularly among Dentists, who should understand the scope of all DCPs to ensure they are referring work appropriately (GDC, 2020).
Respondents identify both potential benefits and challenges if the Scope of Practice of Dental Technicians were to be expanded. Improved patient outcomes (29%) were the most frequently identified potential benefit, once again suggesting that Dental Technicians feel they could play a role in improving access to dental care for patients.
Participants identify include additional training requirements (25%), increased liability (25%), and potential conflicts with other dental professionals (23%). However, very few Dental Technicians identify patient acceptance as a barrier, with only 4% of respondents believing this could be a potential issue. It has previously been noted that some Dentists believe that substituting roles could lead to issues of patient acceptance, for example, in the case of Dental Hygienists and Therapists in practice (Jones et al., 2007).
However, several studies suggest that patients have positive attitudes towards receiving treatment from other members of the dental team, such as Dental Hygienists and Dental Therapists (Cowpe et al., 2013; Öhrn et al., 2008; Richards, 2011; Turner et al., 2013). This aligns with the findings of this study, as Dental Technicians do not appear to view patient acceptance as a significant barrier should their SoP be expanded.
A recurring theme in free-text comments is the perception of Dental Technicians as undervalued members of the dental team. This finding is consistent with previous
studies on CDTs. For example, Curtis et al. (2019) findings indicate that CDTs feel ostracised by both other dental professionals and the GDC. Very similar views are expressed by Dental Technicians in this study. Respondents express they feel as if “The GDC just protects Dentists and does not care about Technicians” (Participant 38). Juszczyk et al. (2009) also note that 54% of Technicians working in commercial laboratories do not feel valued as part of the dental team, a feeling that goes back to before compulsory registration (Bower et al., 2004).
This suggests a long-standing perception among Dental Technicians that their role is less valued than other DCPs. Such findings could indicate the need for greater interprofessional collaboration to build stronger relationships between different DCPs.
Another recurring theme in free-text comments relates to a reduction in technical knowledge among newly qualified Dentists. This resonates with findings from Juszczyk et al. (2009), who report that Dental Technicians in the study believe newly qualified Dentists have poor technical knowledge. If this trend continues, expanding the SoP for Dental Technicians may become increasingly necessary. However, feasibility may be limited, as the


majority of Dental Technicians work in commercial laboratories away from general dental practices.
One of the main limitations of this study is the difficulty in achieving a high response rate. Due to methodological changes, an exact response rate cannot be calculated. However, the number of respondents (49) represents approximately only 1% of the total professional group (GDC, 2024). As a result, it is unclear whether the views expressed are representative of all Dental Technicians. Possible reasons for the low response rate could include survey fatigue, the timing of the survey, and a lack of interest in discussions regarding SoP (Jaggee et al., 2019; Shiyab et al., 2023).
Furthermore, the survey may have attracted respondents with strong views on the topic, potentially skewing results toward those who feel most strongly about changes in SoP (Wetzel et al., 2016).
Another limitation is the demographic distribution of respondents. A large proportion (84%) fall in the ‘more than 15 years’ of practice category. This distribution is unexpected, so more categories for years of practice could be included to further split up this group of respondents to allow for greater comparison of perspectives based on the years of practising as a Dental Technician.
Additionally, the survey does not exclude Clinical Dental Technicians (CDTs) from participating. This may be a limitation in the study methodology, as some free-text responses indicate that CDTs may have participated in the study. They have a different Scope of Practice from Dental Technicians and, therefore, may have different views on the subject. Their response could influence the results in ways that do not accurately reflect the views of Dental Technicians alone. Therefore, the study should exclude CDTs.
Finally, while this study aims to compare its findings with existing literature, there is a lack of literature surrounding the Scope of Practice for Dental Technicians. The ability to compare research is therefore hindered; comparisons are made from studies that focus on other DCPs, including Clinical Dental Technicians, Dental Hygienists, and Therapists. This could limit the strength of the comparison drawn.
Despite these limitations, the study provides qualitatively rich, valuable insights into the thoughts and feelings of Dental Technicians regarding their SoP.
The findings of this study have implications for Dental Technicians, the GDC, and the wider dental team.
For Dental Technicians, the study highlights a desire and perceived need for an expansion in Scope of Practice, particularly in relation to helping patients gain better access to dental care. However, further discussions and regulatory changes are first needed before this can happen.
The study indicates that many Dentists may not fully understand the scope of Dental Technicians. Future research could therefore focus on the knowledge of Dentists with regard to the role of Dental Technicians. This could shed light on the need for improved interprofessional education.
Given the ongoing consultation on the GDC SoP review at the time of writing, there is an opportunity to address some of the issues highlighted in this research to ensure that Dental Technicians are utilised to their full potential as members of the dental team. This could not only have a positive impact on dental care, but also on job satisfaction among Dental Technicians in the UK.
This study uses an online questionnaire to explore the knowledge, attitudes, and future views of UK Dental Technicians regarding their Scope of Practice (SoP). As far as is known, this is the first study exclusively assessing the SoP of Dental Technicians in the UK.
Findings suggest that Dental Technicians have a good awareness of their SoP. There are also a number of Dental Technicians who wish to see their SoP expand in the future so they can better support patients’ needs in the provision of certain dental devices.
The majority indicate that they are willing to undertake additional training to support this change. However, this is a complex issue governed by a number of factors, and issues such as training and regulation remain.
The study also highlights issues of the understanding of Dental Technicians’ roles among other DCPs, which may suggest a need for greater interprofessional education among dental team members. Issues of Dental Technicians feeling undervalued, both by other DCPs and the GDC, further highlight the need for greater interprofessional collaboration.
While the study has a limited number of responses, it provides a valuable foundation for future discussions on the expansion of the SoP for Dental Technicians, which is of particular relevance alongside the GDC’s ongoing review of the SoP guidance at the time of writing.
Dr Michael Sultan, founder and principal of endodontic referral practice EndoCare
As is true in all areas of systemic health, prevention and early detection are key in the fight against breast cancer. The former is all about raising awareness of the risk factors for breast cancer and educating the general population to reduce these behaviours as much as possible.
These include being overweight or obese and excessive alcohol consumption. There is also evidence that taking the contraceptive pill may increase the risk slightly, with research showing a 20-30% higher risk among women currently or recently taking a combined oral or progestogen-only contraceptive.
Unmodifiable risk factors are just as important to be aware of, although individuals have less control over them. These include age, a family history of the disease, diabetes, dense breast tissue, hormone imbalances and previous cancers.
Thanks to early detection and rapid treatment, breast cancer survival has doubled in the past 50 years. Today, 86% of people live for five years or more beyond their diagnosis. Treatment in women will vary depending on the size, stage, location and type of breast cancer identified, but may involve surgery, radiotherapy, chemotherapy, hormone therapy, targeted immunotherapy or a combination of these and more.
It is important to remember that breast cancer can affect men too, with approximately 400 individuals diagnosed every year in the UK. The disease is often detected much later in males, meaning that increased awareness of the risks and symptoms is essential to improve the statistics.
Breast cancer remains a key focus of research and treatment development, with new ideas, disease insights and management therapies frequently coming to the fore.
Heralded as a break-through in the scientific research last year, experts in Manchester reported initial success with a new way to study and develop drugs for breast cancer.
Researchers were able to preserve breast tissue outside the body, maintaining its viability for accurate testing over the following seven days.
The goal was to use this approach to investigate how different drugs and hormone therapies reacted to the cells.
More recently, research into drug therapies that can target emerging tumours before they grow in advanced cases, delaying the need for solutions like chemotherapy, has reported promising initial findings.

Dentists and their teams should be signposting patients with any concerns towards the appropriate cancer pathways, but we are not responsible for the detection, diagnosis or management of the disease. What we can do is help patients reduce and manage oral symptoms of their breast cancer or the treatment they are undergoing as a result.
For example, the literature shows that periodontal disease and tooth loss are common among postmenopausal breast cancer survivors – with up to 98% of study participants experiencing the disease. This can have a significant impact on each individual’s quality of life, creating even more challenges for them to overcome when they already have plenty to worry about.
Several of the most common cancer treatments are associated with oral complications too. Chemotherapy, for example, can often cause oral mucositis, xerostomia and salivary hypofunction, while the use of bisphosphonates can increase the risk of osteonecrosis of the jaw.

There is also much we can do to help patients reduce their chance of developing breast cancer in the first place. Research has estimated that women’s risk of breast cancer is up to three time greater when they have periodontitis. Basic yet essential on-going dental care, regular appointments and a supported at-home oral hygiene routine are, therefore, crucial for all our patients.
Breast cancer remains a prevalent and challenging disease, but enhanced understanding, continued research and treatment development are all helping to improve survival rates and quality of life for those diagnosed. For dental professionals, our role is an important one, supporting patients and optimising their oral health for a reduced risk of cancer.

● are individually registered with the GDC to be able to use the titles that relate to our role in the UK
● maintain our own lifelong learning through relevant continuous professional development (as provided free to the Dental Technologists Association [DTA] members)
● ensure that we are covered by specific indemnity insurance related to our dental laboratory custom-made dental device manufacturing work, and if necessary, related clinical work and/or extended roles
● work within the GDC Scope of Practice for our registered role, along with other extended areas as confirmed by further additional training
● are, as a current GDC registered dental technologist, able to sign-off custom-made dental devices under MHRA/MDR regulations, indicating that such appliances are fit for purpose as stated on the Statement of Manufacture
● maintain and develop our dental team networks to enhance patient care
Dental Technology Showcase is the event where over 1,500 dental lab professionals meet to shape the future of dental technology. With 60+ exhibitors, 3 theatres, 50+ expert speakers and 40+ hours of free Enhanced CPD, this is the place to unite with your dental community. Embrace new ideas, explore the innovations of tomorrow and take your lab to the next level.




