the issn 1757-4625


the issn 1757-4625


Marketing in the Digital Age What do you know about Stroke? Mental Health: Suicide and Self Harm In this issue:
volume 11 issue 4 november 2018 issn 1757-4625 the journal of the dental technologists association volume 18 issue 2 may 2025 HOURS OF






Editor: Derek Pearson
t: 07866 121597
Advertising: Rebecca Kinahan
t: 01242 461 931
e: info@dta-uk.org
DTA administration: Rebecca Kinahan
Operations Coordinator
Address: PO Box 1318, Cheltenham GL50 9EA
Telephone: 01242 461 931
Email: info@dta-uk.org Web: www.dta-uk.org
Stay connected: @DentalTechnologists Association
@The_DTA @dentaltechnologists association
Dental Technologists Association (DTA)
DTA Council:
Delroy Reeves President Joanne Stevenson
Deputy President
Tony Griffin Treasurer
Chris Fielding, Robert Leggett, Patricia MacRory and Jade Ritch.




Editorial panel: Tony Griffin Joanne Stevenson
Editorial assistant: Dr Keith Winwood Published by: Stephen Hancocks w: www.stephenhancocks.com
The Dental Technologist Association (DTA) is pleased to announce the appointment of Joanne Stevenson as the new President, following her three years of dedicated service as Deputy President supporting Delroy Reeves. The Council of the Dental Technologists Association (DTA) convened via online video conferencing on Saturday, 15th March 2025, to elect the new President and Deputy President.
After the meeting, Joanne Stevenson remarked: “It is a tremendous honour to be elected as the first female president of the DTA. I aspire to fulfil my responsibilities effectively and to guide the association toward greater achievements. I would like to extend my gratitude to the outgoing President, Delroy Reeves, for his dedicated efforts throughout the years; he has certainly left big shoes to fill.
“Congratulations to him on his new role as DTA Liaison Delegate. I also want to thank Chris Fielding for taking on the position of Deputy President; his expertise and experience in the field will undoubtedly benefit the DTA. With the support of the entire DTA management team, I am confident that we can make the association exceptional for all members.”
Joanne brings a wealth of experience and is well-equipped to lead the DTA into the future. Joanne’s expertise includes working on prosthetics such as Valplast flexible dentures, hybrid implant bars, and implantretained overdentures. Joanne is the first person to be awarded new DTA Fellowship for the quality of her work in the lab and whilst visiting surgeries for all-on-4 immediate load denture-to-bridge conversions.
The association extends its heartfelt thanks to Delroy Reeves for his outstanding leadership and contributions over the past three years as President. In Delroy’s outgoing speech he congratulated Joanne Stevenson in her new role as DTA President: “I hope my legacy will, in some ways, have a lasting impact on the dental technology profession. My wishes and desires for future developments in our esteemed and much-loved profession remain strong.
“As we introduce our new DTA President, Ms Jo Stevenson, and Deputy President, Mr Chris Fielding, to the leadership team, I extend a warm welcome to both of you.
“My best wishes for every success in your term of office.”
Delroy Reeves now takes on the title of DTA Liaison Delegate and continues his dedicated support to the profession.


Chris began his career in a commercial dental laboratory and since transitioned to full-time teaching. Currently, Chris is the Higher Education Programme Leader for Dental Technology at The City of Liverpool College.
The DTA welcomes Joanne and Chris into the leadership team and congratulates them on their new roles. The President and Deputy President serve a three-year term, supported by the DTA Treasurer and Council members. These dedicated professionals volunteer their time while actively working as registered dental technicians, always acting in the best interests of the profession.
Benefit
Full details on page 5

The DTA has reviewed the changes made by the GDC and assure all our members that all of our CPD still meets the GDC requirements. You will find this statement written on all CPD certificates moving forward:
“This verifiable continuing professional development has been provided by the Dental Technologists Association (DTA) and has been designed to meet the requirements of the General Dental Council’s criteria for verifiable continuing professional development. We confirm that the information provided on this certificate is full and accurate and that all CPD provided by the DTA has been subject to quality assurance.”


National Smile Month is a charity campaign that champions the benefits of good oral health and promoting the value of a healthy smile. Between 12 May and 12 June 2025, the Oral Health Foundation will be raising awareness of the powerful connection between diet and oral health with its theme, Feed Your Smile. A representative of the DTA will be at the launch of National Smile Month at Surveyors House in Westminster on the 9th May.
A spokesperson for the Oral Health Foundation said: “Your diet plays a crucial role in maintaining a healthy, beautiful smile, and we want to help you make smart choices that promote oral health every day. Take a look at our campaign guide (page 4) and join us in our aim to make a positive difference to the oral health of millions of people.”
Thank you to everyone who participated in the DTA annual survey and congratulations to Stephen Gale the winner of the prize draw and recipient of £100 voucher!
Join us at the Dental Technicians Hub on Saturday, 17 May, from 10:30 to 11:15 for an exciting session at the DTS. Discover the future of dental technology with Davide Accetto, the first dental technician in the UK to achieve a fully digital Immediate load using Nobel Biocare’s latest system. Davide will share his groundbreaking experience and insights during the session ‘Experience the future with digitally designed 3D printed immediate load.’ Don’t miss this opportunity to learn from a pioneer in the field and explore the cutting-edge advances in dental technology.

Come visit us at the DTS alongside the British Dental Conference and Dentistry Show at the NEC 16-17th May on stand number D02 to discover our special show offer! Our team is eager to hear your thoughts on what you’d like to see from the DTA this year and how we can continue to support our membership.
We would be thrilled to introduce and talk to you more about the exciting new DTA Rewards program, and answer any questions you may have. For more details, check out the advertisement on the inside front cover . Plus, don’t miss the chance to meet a representative from UK Special Risks on Friday, 16th May, and get answers to all your insurance-related questions

As a valued member of the Dental Technologists Association, you now have access to a range of fantastic money-saving benefits through our brand-new member benefits scheme, DTA Rewards! Take advantage of a wide range of deals including:
A Health and fitness: Stay active and save with offers on sportswear, nutrition, smartwatches, digital fitness subscriptions.
A Home and car essentials: Save on household appliances, mobile phones, car servicing, car hire, breakdown and MOTs services.
A Food and drink: Receive discounts on groceries, fine wines, dining out, take aways and beer subscriptions.
A Fashion and tech: Access savings on a range of brands online and in-store including Charles Tyrwhitt, Dell, John Lewis, ASOS and M&S.
A Entertainment: Discounts on cinema tickets, books, West End shows, magazines and streaming services.
A Travel and experiences: Looking to book a trip in the future? Save on package holidays, theme parks, day trips, luxury hotels, Airbnb, foreign currency, airport hotels and parking.





Here’s how you can make the most of DTA

Free 24/7, 365 confidential helpline
We have partnered with Health Assured to bring you a trusted and comprehensive wellbeing service. They offer a free confidential helpline, which puts you in touch with qualified counsellors and advisors who will be able to support you with, counselling support, legal guidance, bereavement support, medical information and more. What’s more, you also have free and exclusive access to the industry-leading Wisdom app –designed to improve your mental and physical health through a range of wellbeing resources and interactive features.

At some point in life, everyone will need legal assistance. Whether you’re purchasing a property or dealing with issues at work, speaking with a legal advisor could be really important. Recognising this need, we have teamed up with Lyons Davidson Solicitors to offer legal services as part of our exclusive member benefits. Lyons Davidson’s experienced legal team is always available to provide clear, friendly, and practical advice on any legal queries you may have. Their goal is to help you find solutions you can implement yourself, wherever possible.
* Terms and conditions apply to all benefits, see the DTA Rewards scheme page for more details. Offers subject to change without notice and correct at time of print. DTA Rewards is managed and run for the Dental Technologists Association by Parliament Hill Limited.










1 Sign up to DTA Rewards
Create your DTA Rewards account for free by signing up to the DTA Rewards mailing list and hear about limited time offers, product launches and competitions. Access the DTA Rewards scheme via your DTA members area.
2 Try out our Savings Calculator
Simply fill in how much you spend monthly or annually on a range of everyday categories, then the savings calculator will generate your annual personal savings total.
3 Take a look at our Ways to Save page We’ve carefully selected some offers to help you save the cost of your Dental Technologists Association membership. Explore this page by visiting the DTA Rewards scheme page via your DTA members area.
4 Looking for your favourite brands?
Browse our categories
Whether you’re looking to save money on your weekly groceries or looking for a birthday present, DTA Rewards has got an offer for you. Simply browse the range of categories or use the search engine to find what you want.
Dental Laboratories Association (DLA) Immediate Past President, Steve Campbell, dental technician and managing director at Nexus Dental Laboratory discusses the key challenges faced by technicians in the dental lab, and the ways in which new dental technology can impact and improve on workflows.
The main challenge we come up against with regards to scanning in the dental lab is achieving accurate image acquisition. This is because, whilst effective in some cases, intraoral scanners are prone to mis-stitches and, in order to achieve a more accurate outcome, a lab scanner is needed. This presents its own challenges – being a clunky and timeconsuming process. A clinical dental technician (CDT) might need to carry out a scan of a denture or impression whilst a patient is waiting, and this is not a quick process. This puts us at risk of a bottle neck in the lab, whilst we wait for scans to finish.
At Nexus Dental Lab, we are huge digital advocates, and have been fully digital for 10
years. Through digital breakthroughs, we are able to implement processes that aren’t available elsewhere and use more durable materials. As such, we are able to change everyone’s experience for the better, especially the patient’s. By utilising digital processes, once we have produced a denture, we are able to re-produce a spare at the click of a button. This transforms the lives of people in care homes, who may lose or break their dentures, which ordinarily results in a delay of two weeks and impacts both their nutrition and quality of life. However, digital processes mean that we can create a spare which is kept safe with a carer who can easily reorder a replacement from the lab.
The Cubit360 digital scanner from Mimetrik will change everything for us – it’s the

missing piece of the puzzle. The scanner is unique in that it is portable and accurate. Traditional lab scanners are impractical, bulky, expensive, and difficult to use, whereas intraoral scanners are handy but result in mis-stitch, ultimately leading to


poor fit. The Cubit360 produces a complete digital reproduction of the object in your hand. It is globally accurate without misstitches, for a simple process and an accurate fit. This completely transforms the end result for patients, eliminating discomfort and improving retention. It also changes the entire scanning experience for the professional team.
Artificial intelligence (AI) already plays a role in our workflows at Nexus. We have our own development team, and use AI at the front end. We use generative AI in design to produce a video of the patient, demonstrating their expected treatment outcome.
We carry out a lot of complex full arch work, meaning that we are aware of challenges with accuracy. Since going fully digital, we have seen things progress. Intraoral scanners have been a huge development but they have a small field of vision. It’s like doing a jigsaw but only being able to see one piece at a time. The Cubit360 can see the big picture, making it globally accurate whilst still achieving micron level precision. This changes everything for us, maximising time in the lab for the benefit of everyone. Our turnaround times are shortened, clinicians can see more patients, and
patients receive faster treatment. This is the unit that we have been looking for.
The user experience with the Cubit360 will be completely different to anything else on the market. At current, every product comes with a set workflow, and can feel quite complex and intimidating to those who are not familiar with digital solutions. In contrast, the Cubit360 system is completely open, and has a low barrier to entry, enabling the user to simply present the object and begin scanning instantly. This means that there is virtually no learning curve. When I first encountered the Cubit360, I was able to use it instinctively –this tells me that, for those who haven’t worked with any digital tech before, the system is very easy to learn.
Another advantage is its speed. The Cubit360 is scanning models and dentures in a fraction of the time we would normally need – something that was taking us 10 minutes previously, now takes 2 minutes. This is particularly important for dental technicians, as time is a valuable resource and we have a diminishing workforce. Anyone using this will feel the benefit instantly.


For the lab, this is such a transformative product – able to complement the images we receive from those who already use intraoral scanners, whilst ensuring a global scan is achieved for complete accuracy.
I genuinely think that this opens up unique new pathways, facilitating the predictable creation of highly accurate full arch scans. Ultimately, the Cubit360 creates an entirely new workflow. In the surgery, clinicians could use it to scan impressions and send them directly to the dental lab, and it can act as a stepping stone for those currently not using digital solutions, as it is an incredibly accessible option. I think a CDT armed with this unit could transform the lives of those in care homes, creating backup files for dentures. This is a new solution that can enable us to help members of society access the support they need.
A For more information about Mimetrik, please visit https://mimetrik.tech/

Following member’s requests The Technologist asks: What are the Nolan Principles? Why are they relevant to dental technologists? And who are they named after?
Michael Patrick Nolan, Baron Nolan, PC, DL, KC (10 September 1928 – 22 January 2007) was a judge in the United Kingdom, and from 1994 until 1997 was the first chairman of the Committee on Standards in Public Life.
In the words of his obituary in The Guardian, “Lord Nolan... made a profound mark on national life by substantially cleansing the Augean stable of corrupt politics as founding chairman of the Committee on Standards in Public Life.”
In January 1994, after becoming a Lord of Appeal in Ordinary and receiving a life peerage as a Law lord, he took the title Baron Nolan, of Brasted in the County of Kent. Lord Nolan chaired the Committee on Standards in Public Life from 1994 to 1997.
The committee was set up in late 1994 by John Major’s government after the cash-forquestions affair, and has conducted numerous other inquiries. Its first report in 1995 created waves by recommending full disclosure of MPs’ outside interests. He also produced a report in standards of conduct in local government in July 1997.
The principles embodied and articulated in the first report have since become embedded in public life in Britain, and are often referred to eponymously as the Nolan Principles.
1. The Seven Principles of Public Life
The Seven Principles of Public Life (also known as the Nolan Principles) apply to anyone who works as a public office-holder. This includes all those who are elected or appointed to public office, nationally and locally, and all people appointed to work in

the Civil Service, local government, the police, courts and probation services, nondepartmental public bodies (NDPBs), and in the health, education, social and care services. All public office-holders are both servants of the public and stewards of public resources. The principles also apply to all those in other sectors delivering public services.
Considering the shenanigans taking place across the global political landscape these days, it makes sense to shake these worthy ideals free of dust and bring them out into the daylight.
Holders of public office should act solely in terms of the public interest.
Holders of public office must avoid placing themselves under any obligation to people or organisations that might try inappropriately to influence them in their work. They should not act or take decisions in order to gain financial or other material benefits for themselves, their family, or their friends. They must declare and resolve any interests and relationships.
Holders of public office must act and take decisions impartially, fairly and on merit, using the best evidence and without discrimination or bias.
Holders of public office are accountable to the public for their decisions and actions and must submit themselves to the scrutiny necessary to ensure this.
Holders of public office should act and take decisions in an open and transparent manner. Information should not be withheld from the public unless there are clear and lawful reasons for so doing.
Holders of public office should be truthful.
Holders of public office should exhibit these principles in their own behaviour and treat others with respect. They should actively promote and robustly support the principles and challenge poor behaviour wherever it occurs.
A spokesperson for the Stroke Association and a stroke survivor, Judith Graham, offer insight and advice while Judith explains why she might never have had her stroke if the correct action was taken early enough. Many DTA member fall into the likeliest stroke age category and we fear that this might be a little understood and underrepresented subject.
People suffer strokes for a reason. It can affect members of the dental team and those in the general public. Strokes, which disrupt blood flow to the brain, are caused by either blocked arteries (ischemic strokes) or bleeding in the brain (haemorrhagic strokes), with high blood pressure being a major risk factor for both.
Ischemic Stroke:
This type occurs when a blood clot or plaque build-up blocks an artery, preventing blood flow to the brain.
A Thrombosis: A clot forms within a blood vessel in the brain or neck.
A Embolism: A clot travels from another part of the body to the brain.
A Atherosclerosis: Plaque build-up narrows arteries, reducing blood flow.
A This occurs when a blood vessel in the brain bursts or leaks, causing bleeding.
A A weakened area in a blood vessel wall balloons and bursts.
Arteriovenous Malformation (AVM):
A Abnormal tangles of blood vessels can rupture.
A Chronic hypertension weakens blood vessel walls, making them susceptible to rupture and bleeding.
In this case study an Oxford woman whose high blood pressure contributed to her having a stroke is warning others to check theirs – it could save their life.
Judith Graham, a retired GP, said she may never have had her stroke if her hypertension had been identified and treated. She shared her story in support of the Stroke Association’s Stroke Prevention Day awareness campaign on Thursday 30 January 2025..
Hypertension, or high blood pressure, is a condition where the force of blood against your artery walls is consistently too high, potentially damaging your heart, brain, and other vital organs. It’s a common condition, and often has no noticeable symptoms, making regular blood pressure checks crucial. Blood pressure is the force of your blood pushing against the walls of your arteries as your heart pumps blood throughout your body.
It’s measured in millimetres of mercury (mm Hg) and is expressed as two numbers: systolic (top number) and diastolic (bottom number). Systolic pressure is the pressure when your heart beats, and diastolic pressure is the pressure when your heart is at rest between beats.

Hypertension is diagnosed when your blood pressure consistently measures 130/80 mmHg or higher. Uncontrolled hypertension can lead to serious health problems, including heart disease, stroke, kidney failure, and vision loss. It can also damage the arteries that supply blood to the heart, potentially leading to chest pain (angina) and irregular heart rhythms (arrhythmias).
Judith had a stroke at a party she was hosting on New Year’s Eve 2023, nine months after retiring from The Key Medical Practice, Kidlington. She explains: “I just suddenly turned and collapsed to my knees. I didn’t feel anything else. I felt completely well but when I went to stand up I couldn’t. At the party there was a doctor I had helped to train. She said I think you’ve had a stroke.”
Judith was rushed to the John Radcliffe Hospital where the diagnosis was confirmed. She was patient there for almost two months before transferring to the Abingdon Community Hospital for rehab for further month and was supported by the Stroke Association. Her stroke has left her with difficulty walking, weakness in her right hand and reduced vision in her right eye.
Judith, who is now aged 66, continued: “The stroke appeared to come out of the blue but in fact my blood pressure unbeknown to me was very high. It shows that even though you think you are fine and feel fine, as you get older, you should really make sure to get your blood pressure checked regularly.” ... “Had I known I had high blood pressure it would have been treated earlier and I might never have had the stroke. It is all too easy because everyone is so busy to put off ensuring that basic health checks are carried out! We need to prioritise our own self-care, and not allow the world to make too many demands on us.”
New statistics from the Stroke Association show that a worryingly large proportion of

UK adults don’t know that high blood pressure is the most likely cause of stroke.
Findings from the leading stroke support charity show that 36% of people who have experience of, and therefore a connection, to stroke don’t know that high blood pressure is the biggest risk factor for the condition.
In addition, the Stroke Association has found that awareness levels are even lower amongst people who don’t have such a connection to stroke, with 43% not knowing that high blood pressure is the leading risk factor for stroke.
There are 1.4 million people in the UK who are survivors of stroke and someone has a stroke every five minutes, with high blood pressure accounting for around half of those.
Stroke survivors are frequently left with physical and mental disabilities including paralysis, problems with vision, difficulties swallowing and a struggle to communicate. Nick O’Donohue, the Stroke Association’s associate director for the South East, said: “Around 100,000 people in the UK have a stroke every year. Worryingly, this has been
increasing over the last 20 years, particularly amongst people of working age.
“The lives of the 90,000 people who survive stroke every year in the UK change in an instant as the condition impacts on their ability to live physically and mentally well.
“It is vital that everyone knows what can cause a stroke, so they can proactively look after their health to reduce the risk. We’re encouraging adults of any age to get their blood pressure checked on a regular basis. This will equip them with knowledge on whether they are at risk of having a stroke so that they can take steps to reduce their chances, if required.”
A Find out more at: www.stroke.org.uk/ stroke-prevention-day
While people of any age can have a stroke, it is most likely to impact those over the age of 65. Free blood pressure checks are available from the GP, participating pharmacies, and are also part of NHS health checks for those over the age of 40 in England and Wales.
Yet recent data from the National Audit Office found that only 44% of eligible

adults attended these health checks in the last five years.
If you have high blood pressure, and want to support the Stroke Association, get involved with its fundraising initiative, Stride for Stroke. The charity is asking people to take one step for each of the 1.4 million stroke survivors currently living in the UK, which works out as 10,000 steps per day for 140 days.
Spin or Swim for Stroke also allows participants to set a personal challenge for time or distance. Or Run 50 asks people to cover 50 miles across a month of their choice.
A Visit: https://www.stroke.org.uk/ choose-your-challenge
The Stroke Association supports stroke survivors and their families by phone, at home, and in the community.
A Find out more at: www.stroke.org.uk
Discover more, and share your thoughts on the 10 Year Health Plan here
A https://www.stroke.org.uk/get-involved/ campaigns/10-year-health-plan

To complete your CPD, store your records and print a certificate, please visit www.dta-uk.org and log in using your member details.
Q1 Reportedly, what contributed to Judith suffering from a stroke?
A High alcohol intake B High blood pressure
C Lack of exercise D She was heavy smoker
Q2 What were the symptoms when Judith had her stroke?
A Shortness of breath B Loss of vision, dizziness
C None, she simply turned and fell to her knees
D Blinding pain in her head leading to unconsciousness
Q3 What is systolic pressure?
A Blood pressure when your heart beats
B Blood pressure when your heart is at rest
C Blood pressure after a work-out
D Blood pressure when sedentary
Q4 What is diastolic pressure?
A Blood pressure when excited, such as watching a horror film
B Perfectly normal blood pressure
C Blood pressure when your heart is at rest
D Blood pressure caused by a sudden shock or extreme cold
Q5 What is the medical description of hypertension?
A When blood pressure is constantly 130/80 or higher
B When the higher number is 60 or more higher than the lower
C When the lower number drops below 50
D When the combined numbers add up to less than 170
Q6 What health problems can result from uncontrolled hypertension?
A Heart disease B Stroke C Vision loss D All of the above
Q7 What percentage of strokes are caused by high blood pressure?
A 73% B 65% C 50% D 36%
Q8 What percentage of people “with a connection to stroke” don’t know that high blood pressure is the leading cause of the condition?
A 36% B 70% C 52% D 62%
Q9 How many people in the UK suffer from a stroke every year?
A Around 270,000 B Around 100,000
C Around 180,000 D Not known, it is often misdiagnosed
Q10 Anyone can suffer a stroke, but which age group is most likely to be impacted?
A Over 55 B Over 75 C Over 80 D Over 65
On 4th March 2025, a spokesperson from the GDC announced updates to CPD processes. The Technologist shares these changes with our members.
Before looking at these changes in more detail, the DTA board is keen to point out that – with regard to the CPD updates – the association has the members’ interests in hand as its Peer Reviewed CPD is quality assured and meets all the new GDC requirements. We also provide an opportunity to catch up with CPD hours by providing access to The Technologist and Articulate CPD content dating back several months, and we will always remind members when specific CPD content is due to be taken down.
Aims:
■ To understand the requirements of GDC registration
■ Keeping up-to-date with the GDC’s CPD requirements and any changes
CPD Outcomes:
■ Effective management of self
■ Maintenance and development of knowledge and skill within your professional scope
■ CPD specific to your registration status
As part of its announcement regarding updates the GDC stated (see below) “The changes are intended to make it easier for professionals to record and submit their CPD and for providers to equip professionals with valid CPD certificates, addressing concerns raised by stakeholders about the challenges dental professionals face in meeting their CPD obligations effectively.”
The DTA’s verifiable CPD matches the Aims, Learning Outcomes and CPD Development outcomes required by the GDC, and more besides. The DTA also offers built-in reflection, an automated log book and PDP templates, making it easier to stay compliant. What’s more, our CPD articles are often written by dental technologists, and wherever possible they are written specifically around topics of interest to dental technologists, based on member feedback.
We have received information from the GDC regarding mapping (see below). It’s our understanding that it doesn’t apply to us. The GDC advises that this mapping document can be used when professionals

undertake CPD that meets the GDC’s verifiable requirements, but the CPD provider’s own evidence doesn’t include all the information needed to demonstrate that the required criteria have been met. The DTA meets all the required criteria, but we have left the mapping document advice in-situ in the interests of completeness.
Below is a reminder of the GDC’s requirements for dental technologists’ CPD. Through The Technologist and Articulate we provide over 20 hours of verifiable CPD per annum, making it easier for member registrants to comply.
Minimum Requirement:
Dental technicians must complete a minimum of 50 hours verifiable CPD, over each 5-year cycle. This means the CPD activities must be documented and verifiable, with evidence of completion.
The GDC encourages dental technicians to spread their CPD activities throughout the 5-year cycle, rather than completing a large amount of activity in a short period. (The Technologist and Articulate are each quarterly, helping to spread the activities.)
Dental technicians must complete at least 10 hours of verifiable CPD every two years.
The highly recommended core topics to be achieved within this cycle should include, as a minimum: Medical Emergencies –10 hours per 5-year cycle (2 hours per year of the cycle) Materials and Equipment –5 hours per cycle. Disinfection & Decontamination – 5 hours per cycle
Personal Development Plan:
As well as completing any required CPD, you will also need to maintain a personal
development plan, which you can use to inform your CPD priorities
Clinical Dental Technicians (CDTs):
Clinical dental technicians, along with dental therapists, dental hygienists, and orthodontic therapists, must complete 75 hours of verifiable CPD over a five-year cycle.
Renewal:
CDTs need to submit a compliant CPD statement at annual renewal and at the end of your five-year cycle.
Verifiable CPD:
CDTs must ensure they have completed at least 10 hours of verifiable CPD in the last two-year period of the 5-year cycle.
On 4th March 2025 a GDC spokesperson provided the following details regarding the new CPD updates:
We have today (4th March) announced changes to our continuing professional development (CPD) processes, after a review and feedback from stakeholders aimed at enhancing accessibility.
The changes are intended to make it easier for professionals to record and submit their CPD and for providers to equip professionals with valid CPD certificates, addressing concerns raised by stakeholders about the challenges dental

professionals face in meeting their CPD obligations effectively.
The changes are limited, to comply with the CPD scheme rules, and although we would like to go further to amend the CPD rules, this would require a change to the legislation.
Incorporating feedback from stakeholders and research findings from the review in 2024, the key improvements to the CPD scheme include simplified documentation requirements, with GDC registration numbers no longer mandatory on CPD certificates and clearer guidance on grace periods and restoration.
We have also updated the requirements for CPD mapping documents, with electronic confirmations now accepted and more flexible approaches to quality assurance verification, allowing digital confirmations alongside traditional signatures.
Stefan Czerniawski Executive Director, Strategy at the GDC, said: “We recognise that dental professionals sometimes face practical challenges in documenting their learning. By simplifying administrative requirements where we can, these changes will help people focus on what matters most – their professional development.
“There is more to be done to improve the effectiveness of the CPD and we will continue to look for opportunities to make further changes, including encouraging the government to reduce the current legislative obstacles.”
Dental professionals must still request any grace periods via their eGDC account or by email within the final six months of their CPD cycle. The fundamental requirements for CPD hours remain unchanged, maintaining the professions’ high standards of ongoing education.
For professionals who may face removal from the register due to CPD noncompliance, we have clarified our decisionmaking process, including consideration of exceptional circumstances. The updated

guidance provides clearer information about the restoration process and CPD requirements for those seeking to return to the register.
More details on the updated CPD requirements are available on our website; https://www.gdc-uk.org/educationcpd/cpd/cpd-scheme, including updated guidance documents and sample certificates.
A Registration numbers on CPD certificates
Registration numbers are helpful to have, but are no longer required.
Dental professionals are welcome to write their registration number on CPD evidence if they’d like to.
Our CPD guidance for both dental professionals and providers has been revised to reflect this and to make the policy around this clearer.
A Signatures on certificates and CPD quality assurance
We no longer require a signature on certificates to confirm the information provided is full and accurate.
We look for wording like “we confirm that the information provided on this certificate
is full and accurate and that this CPD has been subject to quality assurance”.
A CPD provider can also send an email to the dental professional to confirm the information provided is full and accurate, with either a signature or printed name. We have updated the sample CPD certificate to make this clear.
A Mapping documents
Mapping documents don’t need a signature. Dental professionals can provide an email confirmation from their CPD provider instead.
We have updated the mapping document template to reflect this.
If a dental professional is unable to complete a mapping document in full, they can submit alternative forms of evidence, like an email from the provider confirming that specified CPD criteria have been met.
A Increasing awareness of grace periods
Dental professionals need to complete their CPD activities before the end of each fiveyear cycle. If they will not be able to complete the requirements and they have good reason why they need more time, they can apply for a grace period, which can give them an additional 56 days.
Dental professionals can request a grace period via their eGDC, or via email, within the last six months of their CPD cycle.
We don’t have any powers to allow dental professionals to complete any CPD hours outside the relevant CPD cycle unless a grace period has been agreed.
A Footnote: Currently on the DTA CPD Certificates:
This verifiable continuing professional development has been provided by the Dental Technologists Association (DTA) and has been designed to meet the requirements of the General Dental Council’s criteria for verifiable continuing professional development. All CPD provided by DTA is subject to quality assurance.
To complete your CPD, store your records and print a certificate, please visit www.dta-uk.org and log in using your member details.
Q1 What is the minimum CPD requirement for dental technicians over the 5-year cycle period?
A 60 hours B 75 hours C 40 hours D 50 hours
Q2 What is the minimum CPD requirement for CDTs over the 5-year cycle period?
A 60 hours B 75 hours C 80 hours D 65 hours
Q3 What are the minimum number of hours of verifiable CPD required over a 2-year period?
A 10 hours B 15 hours C 8 hours D 12 hours
Q4 On what date were the CPD updates announced by the GDC?
A 28th February 2025 B 4th March 2025 C 1st April 2025 D 28th December 2024
Q5 Why does the GDC say it “can’t go further to amend the CPD rules”?
A It would prove too complicated
B Fear that too many changes would confuse registrants
C It would require a change to the legislation
D Unnecessary expense in new paperwork and software
Q6 Where can dental professionals request a CPD grace period?
A Via their eGDC account B By email to the GDC
C Via their team leader D a) and b) only
Q7 When can a request for a grace period be made?
A At any time during the 5-year cycle
B During the final 6-months of the 5-year cycle
C During the first 6-months of the 5-year cycle
D During the final week of the 5-year cycle
Q8 Are registration numbers still required on CPD certificates?
A Yes, they are very useful
B Sometimes, you need to check with your provider
C No, but they are useful
D Only when a registrant is trying to catch up with CPD hours during a grace period
Q9 How long is a grace period?
A A calendar month, 28-31 days B 56 days
C 40 days or less D Two months 56-62 days
Q10 Are signatures still required on certificates to confirm the information provided is full and accurate?
A No, they no longer required
B Yes, signatures are an essential factor in verification
C Signatures are required on any CPD beyond the core subjects
D b) and c) only
With Niche B2B sectors, the client often has very unique challenges with SEO, (Search Engine Optimisation). Often the volumes are not huge and the charts therefore are often a little underwhelming. The value of SEO will very much depend on elements such as how active the company is in NPD (New Product Development, which is the overall process of conceptualising, designing, planning, and commercialising a new product to bring it to market), how many product alternatives there are, and the brand – how much need there is to maintain visibility or brand position.

Rather than traditional SEO and social signals, a winning approach for dental technicians includes:
A Relationship-driven marketing (LinkedIn, industry networking, partnerships)
A Entity-based SEO (topical authority over keywords)
A AI-resistant, high-value content (case studies, white papers, expert reports)
A B2B2C strategies through dentist advocacy, not direct patient marketing
A Price-value storytelling over raw price transparency
Many industries struggle with this, but effective segmentation combined with personalised outreach (LinkedIn, industry events, partnerships) can work better than pure search optimisation. B2B buyers often make decisions based on trust and expertise, not just search results. Therefore, an omnichannel marketing strategy (a customer-centric approach that integrates all channels online and offline to provide a consistent and unified experience across every touchpoint, ensuring a seamless journey for the customer) with intelligent and wellworked campaigns is the key to success.
■
A First-party data & CRM (Customer Relationship Management)-driven engagement over cookie tracking, which refers to strategies and tactics, often using software, to manage interactions with customers and prospects, aiming to improve relationships, drive loyalty, and boost sales throughout the customer lifecycle.
If you are considering tackling SEO, or updating or creating a new website, employing additional marketing support or just more generally, reviewing your marketing strategies, you would be wise to read through the following points.
Consider the steps required to ensure their inclusion or amplification within your daily marketing activities.
Employing an SEO to tightly focus on shoring up these key campaigns with umbrella content where a single brand is used to market multiple, related products or services, and research data is essential in the visibility and dominance of the identified topics. Furthermore, as with any successful marketing campaign, building in those touch-points, will ensure that brand search queries and informational and transactional search queries will benefit from increased click though rates.
are useful, but is this approach still as effective in an AI-driven search world?
Focus on entity-based SEO which focuses on optimising content around entities (unique, well-defined things or concepts) rather than just keywords, while topical authority is about establishing a website as a reliable resource within a specific niche or topic.
Rather than chasing keywords, establish authority with in-depth resources on CAD/CAM technology, material innovations, and lab profitability strategies. AI-generated search results will prioritise expertise, depth, and trust signals over traditional keyword
stuffing – the practice of overusing specific keywords or phrases on a webpage in an unnatural way in an attempt to manipulate search engine rankings.
The opportunity to provide and maintain guides and marketing material for use within the client websites – treatment information etc., is highly valuable, providing logos and USPs or technical specifications that are relevant to their enduser, highly valuable content and enables valuable data collection for use within other campaigns, product launches and general marketing activity.
This opportunity further supports a strategy focussed on AI search assist formerly known as SGE (search generative experience.)
Getting AI to work for us and not against us is essential. For example, SGE could reduce clicks to a website by providing direct answers in search results.
Instead of just randomly aiming for these snippets, invest in exclusive, AI-resistant content—proprietary reports, gated industry insights, webinars, and in-depth research that AI summaries cannot fully replicate.
Also, structure content for AI visibility (clear, factual, well-cited data that AI models trust) and ensure the rich snippets – enhanced search results that display additional information about a webpage, like star ratings, images, or prices – are fully worked up.
Google’s Helpful Content Updates (the majority in 2023-2024) favours user-first content, but many businesses still struggle to create material that truly differentiates them. Indeed, there appears to be quite a wide misunderstanding of what helpful content actually is.
Develop highly practical, case-study-driven material. Examples:

A “3 Ways Digital Impressions Are Cutting Lab Turnaround by 40%”
A “Cost Analysis: In-House Milling vs. Outsourcing for Dental Technicians”
A “How One Dental Lab Doubled Their Efficiency with AI-Driven Inventory Management”
B2B buyers respond to data, success stories, and industry insights—not just broad helpfulness.
Ensure the content delivers in accordance to Google Content guidelines and consider the potential of auditing your content. It isn’t just good content, or just unique content, Google is asking us to create content that is going to suit the search query and the intent.
It is asking us to consider the user, they may well land on a page that instantly answers their initial search query, but is there linked content that allows them to easily navigate to supporting topics and deeper
information and is there credibility in what is being written?
Who has it been written by and is the website page experience a good one? There are additional considerations to these quite massive updates and becoming more familiar with the requirements is essential, it is a move that will only be built upon in coming years and months and as such, is essential to have this base requirement understood and effectively put into practice across all of your content creation.
Large sites are likely to require an SEO with the ability to correctly identify when to elaborate or condense a topic and additional resource to create interactive and intuitive features to the appropriate website pages, equally essential – most SEO’s within onpage experience should be able to do this.
Voice search is another element of search that most SEO’s and agencies are churning out in a mantra of Voice Search is a Game changer in terms of approaching content –to be honest, it is to some degree a game-
changer for consumer products and services. However, for a professional service or B2B product, certainly within the more advanced tertiary, technology, engineering spaces it is more the element of ensuring optimisation of long tail keywords that should be identified within the on-page and content strategy.
And to focus on AI search assist for appropriate search topics, as mentioned above, likely to produce the most successful outcome.
Price transparency in the consumer market place is essential. The consumer is searching for price information and if it isn’t readily accessible, they will often simply remove the sites that do not offer the information they
require from their own ‘prospecting list’. Dental technicians however, operate in a different market-place and to consider instead offering value transparency allows the helpful content principles to be met and further amplifying a strong sales message:
A “Why Premium Zirconia Crowns Cost More – And Why They Last Longer”
A “The True Cost of Cheap Dental Restorations: A Lab’s Perspective” This educates the market without devaluing premium services.
Prioritise first-party data strategies: the many cookie changes have required us all to adjust and evolve our privacy and cookie policies.
This global digital marketing change extends to changes required within the
technical implementation of website events:
A To allow the events to be recorded appropriately,
B To allow them to be categorised in accordance to the consent preferences (allowing some structure for the user to choose to accept/decline).
Collect insights via email newsletters, gated content, and CRM integrations, the opportunities to gain consent and to deliver personalised or advanced audience-based communication is now highly evolved and the importance of ensuring compliance and correct use of tracking will provide extremely valuable marketing segmentation and remarketing targeting opportunities controlled through audiences, personalisation and your CRM systems.
The launch of analytics tools such as Google Analytics 4 (GA4) – a next-generation

analytics platform that provides marketers with enhanced insights into user behaviour and campaign performance across websites and apps, enabling data-driven decisions and improved marketing ROI – has allowed the use of predictive analytics to understand ‘purchase’ and engagement trends and further identify predicted sales and predictive modelling in terms of forecasting behaviours.
In order to be able to make full use of these changes there are several layers of administration required to your event configuration.
These recent changes require an expert to implement and if the site has largely been self-sufficient for many years, or the site is older than four years you will likely be experiencing some disruptions and to address these sooner rather than later is a wise move.
Annie Veale is an experienced digital professional offering advanced SEO, PPC and website development services across the UK. Also, an active specialist in GA4, analytics and reporting. To contact Annie, email annie@annieveale.com

Development Outcome A&B – 60 minutes
To complete your CPD, store your records and print a certificate, please visit www.dta-uk.org and log in using your member details.
Q1 What is ‘SEO’?
A Strategic Efficiency and Organisation B Sales Effectiveness and Optimisation
C Search Engine Optimisation D Structured Economic Organisation
Q2 What is ‘NPD’?
A New Product Development B Natural Product Development
C National Product Distribution D Natural Potential Development
Q3 Which of the following is NOT the result of CRM-driven engagement?
A Improve relationships B Boost sales
C Get better prices for raw materials D Drive loyalty
Q4 According to the article, which of the following statements is true?
A Buyers only make choices based on price
B Buyers will only buy from a brand they have used before
C Buyers often make decisions based on trust and expertise
D Buyers will choose products because of marketing imagery
Q5 What does omnichannel marketing involve?
A Driving marketing through emails to existing customers
B Integrating all marketing channels online and offline
C Ensuring your message is available in all the most popular languages
D Paying to boost your website through Google, Instagram, and Facebook
Q6 What is ‘Umbrella Content’?
A Money put aside to deal with unexpected problems
B Taking out financial insurance against loss of earning
C A single brand used to market multiple related products and services
D A French marketing system in use since 1957
Q7 According to the author, what is ‘keyword stuffing’?
A The practice of only using short sharp phrases
B Using recognisable phrases from popular culture
C Using the company name is every sentence
D Overusing keywords in an unnatural way
Q8 Which of the following is NOT a rich snippet as described by the writer?
A Star ratings B Personal information about the laboratory team
C Images D Prices
Q9 What content structure helps to gain AI search assist visibility?
A Use short punchy sentences B Present product names in block capital letters
C Use clear, factual, well cited data
D Ensure that clear professional imagery is associated with any product information.
Q10 What is GA4?
A Gateway Access version 4 B Google Analytics 4
C Grammer Advancements 4 D Gradual Analytic growth 4
Aims:
■ To demonstrate the continuous nature and accelerating pace of change
■ To explain the basics of generational theory and how it seeks to explain differences between different generations
■ To provide practical illustrations of the challenges of change and how they can affect our attitudes and behaviour in both our personal and professional life
CPD Outcomes:
■ Effective communication with patients, the dental team and others across dentistry, including when obtaining consent, dealing with complaints, and raising concerns when patients are at risk;
■ Effective management of self and effective management of others or effective work with others in the dental team, in the interests of patients; providing constructive leadership where appropriate; [Effective practice and business management].
■ Maintenance and development of knowledge and skill within your field of practice; Clinical and technical areas of study: Emerging technologies and treatments:
■ Maintenance of skills, behaviours and attitudes which maintain patient confidence in you and the dental profession and put patients’ interests first. [Professional behaviours]
Development Outcomes: A, B, C & D
Kevin Lewis
This article concludes a series of three linked articles looking at the implications of change in our professional and personal lives. We have seen that these implications are often practical and/or human in nature but they may have professional, ethical and often legal consequences – many of which might not be immediately apparent. In the opening article we focused upon the increasingly fast pace of technological change, and the impact of various forms of technology. In the second article we considered generational change as part of social and demographic change, and against that background we will now explore the ways in which attitudes and behaviour are influenced by change – and vice versa.
Some of the terminology in this article relies upon having read Part 2 of this series1 but Figure 1 (on following page) provides a convenient reminder of the generational
groups that will be referred to.
The last 20 years have brought many changes in dentistry, for dental laboratories and especially technology, and of course society itself has changed beyond recognition. If we look back on the changes that have taken place in our own lives –whatever our age – we will quickly identify some changes that we actively sought or welcomed, and other changes that were imposed upon us by others and over which we had little or no control. Some of the changes may have been big and transformational, others small and insignificant, some gradual and evolutionary in nature and other sudden or “step” changes. Many readers will remember the profound changes made in 2006 to the NHS dental contract in England and Wales, and the resulting almost overnight collapse of the prescription of chrome-cobalt dentures and multi-unit crown and bridgework by NHS dentists.
And in the same year, the mandatory

1: The generational cohorts
79-96
AGE IN 2024
Born 1928-1944
SILENT GENERATION
DRIVERS re WORK ATTITUDE
Fear of Unemployment Job Security
Strong work ethic
PREFERRED LEARNING AND DEVELOPMENT STYLE
59-78
Born 1945-1965
BABY BOOMERS
Career Job for Life/Pension Home Ownership
Didactic teaching. Tell-show-do
45-58
Born 1966-1979
GENERATION X
Training Qualifications Quality of Life
Group Learning
29-44
Born 1980-1995
GEN Y [MILLENNIALS]
Portfolio Careers Rights/Entitlement Assertiveness
Interactive Coaching
13-28
Born 1996-2012
GEN Z [Post Millennials]
Mental Health
Inter-Generational Fairness
Mentoring
Regular performance feedback (and praise)
12 or Under
Born since 2012
GENERATION ALPHA
It is worth noting that 60% of Dental Technicians currently registered with the GDC are aged 55 or older: the proportion is even higher for CDTs
registration of dental technicians and CDTs with the GDC, and everything that flowed from that.
For laboratory owners it has been a roller coaster of new and changing legislation to stay on top of – whether controlled waste, or in relation to employment law, or medical devices and the requirement to register with the Medicines and Healthcare products Regulatory Agency (MHRA). In previous articles in this series over recent years we have highlighted regulations that impact every aspect of a dental laboratory’s business – some of them coming as a surprise to readers, I suspect.
Not so long ago all telephones were surgically attached to the wall and your accessibility was determined by the length of the landline cable. Then came mobile phone technology which ensured that you remained accessible to more people, more of the time (and vice versa). The smaller, lighter and more portable the devices became, the flimsier became your excuses for unavailability and the easier it became for us to parachute in and out of the lives of others without needing to be invited.
The change and challenge we experience in our busy lives – in our professional life
and at home - takes many different forms and is usually a mixture of changes we choose to make ourselves, and change determined by others, and over which we have little or no control. In the workplace the test of any manager is not seen in his or her ability to get things done in periods of stability, where everything is working in one’s favour, but at times when – for a variety of reasons – the screw turns and pressure increases. Periods of change give us decisions and adjustments to make which impact upon our well-being, our ability to cope and every aspect of our performance – whether or not we realise this at the time.
But the flip side is that the status quo is almost always easier and more comfortable than dealing with the challenge of change and importantly, change does not always announce itself at convenient times. It has a nasty habit of either arriving just when we can do without it, or taking too long to happen when we want and need it most. Organisations, leaders and individuals can all be guilty of putting their head in the sand when change comes knocking, and resistance to change can become a habit and a default reaction. As we will see, this too has its consequences and often, ones that cannot be sidestepped or ignored.
Change demands adaptation – whether we actively seek and welcome it, or have it thrust upon us. The less control an individual has over the changes, the more destabilising and stressful the change tends to be. When a number of changes occur at once, or in quick succession, the individual doesn’t get time to restore any sense of stability or re-establish homeostasis through effective “coping strategies”.
Much of the stress of change can be dissipated by having good support through times of change. The lack of such support can make change seem all the more threatening, stressful and isolating.
Giving people a sense of control is all about communication – explaining the what, when and how of the proposed changes. But the reasons for change must also be explained because the upside benefits of change may be less obvious that the downside discomfort, risks and drawbacks. Problems tend to arise when individuals are denied the opportunity to voice their concerns about proposed changes, or perhaps feel that their concerns have not been listened to or taken into account. Even something as simple as a change in business ownership creates precisely these
issues because the views of staff members are rarely sought before the deal is struck and yet their fears for what this will mean are very real. The former business owner has the proceeds of the sale to cushion any such emotions.
Individuals vary enormously in their reaction to change, but the emotional component of any individual’s response will have recognisable characteristics. Reflecting upon different moments or periods of change that you have experienced, you may be able to recognise these feelings in yourself, or in others. These emotions are not mutually exclusive and during the process of adjusting to and coping with change, the same individual may well go through phases where different emotions predominate. It is also true that the emotional response is likely to reflect the scale and nature of the change and the way in which the change is being introduced, by whom, and over what timescale.
The four main types of response, and some examples of the feelings associated with them, are illustrated in Figure 2 (below).

Change and the need to deal with it, is hardly a new challenge for the human race. It is arguably true that the pace, scale and complexity of change in the modern world is unprecedented, but equally true that past generations also thought the same of the different range of changes that they faced.
Proponents of change (and those who derive a living from it as they move from one organisation to another on lucrative consultancy and project management contracts), are often on a collision course with people working in those organisations who - rightly or mistakenly - might believe that not all of the proposed changes are necessary or desirable. The reality is that:
A Not all change is good and beneficial
A Not all change is bad and destructive
A Some change is essential, desirable and potentially highly beneficial
A Some change is not essential, unhelpful and will do more harm than good
A Proponents and champions of change are not always right and nor are they always acting in the best interests of an organisation and its staff. Their enthusiasm for the change may be blinding them to the downside risks and unintended consequences. But nor are they always wrong either.
A Those who might be resisting change or struggling to cope with it are not always wrong to feel that way, and nor are they always being difficult or obstructive. They may simply not be persuaded yet. Their lack of belief in the need for change may be blinding them to the
Apprehension
Uneasiness
Panic
Sleeplessness
Introversion
Silence
Talkativeness
Over-reaction Apathy Manifesting
Destructiveness Moodiness
Hyperactivity Rudeness Silence
Absenteeism Good Humour
potential upside benefits. But nor is their opposition always justified, and preserving the status quo may be equally undesirable or perhaps even impossible.
A Change is often resented and resisted simply because of the way it is being introduced, or the people who are proposing it.
A In many cases, the major intended benefits of a change will not be felt by the people who will be bearing the brunt of the change.
A At the heart of every change is the people who are affected by it. Carry people along with the change, involve and communicate with them, seek out and listen to their views, and you will encounter less resistance and win their respect and trust. Do the opposite and you will make life unnecessarily difficult for yourself, dragging a reluctant, resentful and distrustful workforce into an uncertain future that they have not ‘bought into’.
A Engagement and consultation with those likely to be affected by change must be “real” and tangible, not undertaken on a ‘token’ basis when key decisions have already been taken.
Change within an organisation or laboratory may be necessary for financial, strategic, competitive or operational reasons. But this will be more obvious to the owners or managers whose perspective on change and the reasons for it, may well be entirely different to the rest of the team. Managers might exaggerate the case for change and the risks of maintaining the status quo, the aim being to create a so-called “burning platform” from which people might be more prepared to jump into the unknown. There may be a tendency to feel that employees who resist the change are backward-looking dinosaurs who are being unnecessarily negative, unhelpful and uncooperative - when the real fault might lie with the manager who hasn’t adequately
communicated the reasons for and ultimate benefits of the change, or has perhaps misrepresented the position. Once the integrity, honesty and motives of the people either proposing or opposing change are in doubt, it becomes a slippery slope indeed.
Some believe that humans yearn for homeostasis / status quo and are better equipped for an immediate, specific threat (‘fight or flight’) than for the more generic threats that change can present. Some change theorists argue that people will not accept and commit to change unless you cut off any routes back to how things used to be. Yet smart, successful companies like Microsoft have realised that this radical approach is unnecessarily alienating – when the initial acceptance of Windows 10 was proving to be poor, Microsoft quickly devised “downgrade” software to allow users to go back to the much more popular Windows 7 if they were struggling with the
latest version. The downgrade became a best seller and this kind of willingness to listen and respond maintains consumer trust in the brand and demonstrates the value of flexibility.
While digital imaging has brought many benefits for clinicians and patients alike, the recent impact of the revolution in communications technology (allowing us to speak, see each other, email, engage through social media and carry out many other tasks while on the move) has been staggering and it is a perfect demonstration of the complexity and speed of change in today’s world. In her inspirational book “Thrive”, Arianna Huffington2 (co-founder of the Huffington Post) blames many of the ills of modern life upon the compulsion to fill every waking moment, to get more done, to work faster and at greater intensity and continually to search out new techniques,


technology and efficiencies in order to yield more and more productivity and minimise downtime. Digital acquaintances may get more of our time and attention than those we are physically in the presence of, and a new infectious disease of “continuous partial attention” is becoming the latest global pandemic. She also describes a personal crisis and catharsis of her own which led her to reassess her life and the relentless pursuit of “success” that had characterised it up to that point – when she appeared to be at the pinnacle of a very successful career. She warns us of
“….the stress of over-busyness, overworking, over-connecting on social media and underconnecting with ourselves and with one another. The space, the gaps, the pauses, the silence – those things that allow us to regenerate and recharge – had all but disappeared in my own life and in the lives of so many I knew.”
This is a vivid and very personal illustration of the fact that too much screen time is not the sole preserve of Gen Z and Gen Alpha, today’s youngest generations. Arianna Huffington (now 74) was aged 64 when she wrote ‘Thrive’. But we can all fall into the
Standard 7.1: You must provide good quality care based on current evidence and authoritative guidance 7.1.1 You must find out about current evidence and best practice which affect your work, premises, equipment and business and follow them.
7.1.2 If you deviate from established practice and guidance, you should record the reasons why and be able to justify your decision.
Standard 7.2: 7.2.1 You must work within your knowledge, skills, professional competence and abilities
7.2.2 You must only carry out a task or a type of treatment if you are appropriately trained, competent, confident and indemnified. Training can take many different forms. You must be sure that you have undertaken training which is appropriate for you and equips you with the appropriate knowledge and skills to perform a task safely.
7.2.3 You should only deliver treatment and care if you are
trap of living too much of our lives online rather than in the moment – precisely the outcome that was intended by the tech giants, of course.
An individual’s attitude to change can bring him/her into conflict with the law, and with third parties such as – in the case of a dental technician – the General Dental Council. None of us enjoys the luxury of being able to cherry-pick which parts of the law we are willing to comply with, and which parts we would prefer to ignore.
At one extreme the risk is that an individual will cling too closely to old/familiar ways of working and get out of date. At the other extreme the risk is that an individual will be too quick to abandon those old/familiar/ proven ways of working and plough prematurely into new approaches before carrying out the relevant due diligence and undergoing appropriate training.
The GDC’s guidance warns registrants against both of these risks – see Figure 3 below) but intuitively one might expect Baby Boomers and Gen X to be at greatest risk of becoming slower to change and more resistant to it, while Millenials (Gen Y) might have a greater tendency to push the envelope.
confident that you have had the necessary training and are competent to do so. If you are not confident to provide treatment, you must refer the patient to an appropriately trained colleague. You must only work within your mental and physical capabilities.
Standard 7.3: You must update and develop your professional knowledge and skills throughout your working life
7.3.1 You must make sure that you know how much continuing professional development (CPD) activity is required for you to maintain your registration and that you carry it out within the required time.
7.3.2 You should take part in activities that maintain update or develop your knowledge and skills. Your continuing professional development (CPD) activity should improve your practice. For more information, see the GDC’s advice on CPD.

Of course these stereotypes may be entirely wrong where some individuals are concerned.
As we have mentioned in earlier articles within this series, social media has added a whole new layer of risk for unwary dental registrants, and there are many examples of the careless use of social media leading to Fitness to Practise investigations by the GDC. The fact that one is simply behaving in the same way as many of one’s peers, does not make it right, and social media has certainly blurred the boundaries of ‘personal’ and ‘professional’ conduct in ways that many GDC registrants have clearly not thought through.
In Part 2 of this series we explored the likelihood of a generational divide when younger registrants in the first half of their career are subject to Fitness to Practise hearings. Statistically the Panels and Committee members are more likely to be older, and less likely to share (or understand) the attitudes and behaviour of the registrant.
None of us can predict what shape future change will take but as we saw in Part 1 of this series, we can be pretty sure that
technological change will continue to play an important role.4 And for the reasons we explored in Part 2, digital natives like the Millenials and post-millenials will be at the forefront of that change. Dental technology seems perfectly poised to take advantage of this synergy, given that its survival very much depends on attracting and retaining a new generation of dental technicians. They may well find the new world of dental technology much more attractive and exciting than the laboratory workplace of the past.
Much has been written and spoken about millennials in the workplace; they are sometimes dismissed as being ‘needy’ or ‘entitled’ but it is probably fairer and more accurate to say that they generally prefer to be mentored, supported and provided with regular feedback, rather than told what to do. They want their needs and feelings to be taken into account. If they feel respected and motivated they will work hard and diligently but they also place a high value a work-life balance and are prepared to demand it. Similarly their relationship with authority has been the focus of much discussion; here again they are less likely than previous generations to blindly submit to authority for its own sake, they first need to be convinced that ‘authority’ in all its
forms is acting fairly and reasonably. And it is easy to see how and why sparks might fly if that ‘authority’ consists of Baby Boomers and Gen X (as it tends to be) who were brought up not to question or challenge the established pecking order.
The post-millenials (Gen Z) are the latest addition to the workplace. They are more likely to seek ‘portfolio’ careers with their main occupation taking its place alongside side-hustles and online sub-careers as ‘infuencers’, ‘bloggers’ and the like. They live much of their lives online and that’s the main source of their communication, knowledge and attitudes. Home working lends itself to these aspirations, and they overwhelmingly favour this on the basis of ‘work-life balance’. In reality this means having the freedom to spend their time more or less on their own terms – which tends not to sit well with Boomer or Gen X employers/managers who have been brought up on more rigid, hierarchical work environments. Postmillenials are also regarded as the ‘now’ generation because they are accustomed to everything being available (and delivered to them) on demand.
Baby Boomers and Gen X saw a secure, long-term job as the central purpose around which the rest of life needs to fit; for

Kevin Lewis, BDS (Lond) LDSRCS (Eng) FDSRCS(Eng) FCGDent
Graduated in London 1971. He spent 20 years in full time general dental practice and 10 further years practising part time. He became involved in the medico-legal field in 1989, firstly as a member of the Board of Directors of Dental Protection Limited (part of the Medical Protection Society group of companies). He became a dento-legal adviser in 1992 and from 1998 was the Dental Director of Dental Protection for 18 years and also an Executive member of the Council (Board of Directors) and Executive management team of the Medical Protection Society, roles from which he stepped down in 2016. Since 2018 he has been a Special Consultant to the British Dental Association, in relation to BDA Indemnity.
He is a Founder and Ambassador for the College of General Dentistry, and was a Trustee Board member 2017-22 Kevin has been writing a regular column in the UK dental press since 1981 –originally as the Associate Editor of Dental Practice and since 2006 as the Consultant Editor of Dentistry magazine. He still writes and lectures regularly in the UK and internationally, and has been awarded honorary membership of the British, Irish and New Zealand Dental Associations. He is also an Honorary Member of the British Society for Restorative Dentistry.
the Millenials and Post-Millenials (Gens Y and Z) their life is the main purpose, around which work needs to fit.
The health of dental laboratories has always been closely intertwined with that of the dental profession, and there, too, we have almost certainly reached a tipping-point. Gone are the days when the majority of dental practices worked primarily within the NHS. But in the process of the shift towards the private sector, the era of high volume-low margins as a business model has given way to lower volumes, higher margins and a greater focus upon quality. When digital workflows are added to this seismic shift in the shape of UK dentistry it opens up many opportunities to change the business model.
The successful management of change has become an increasingly crucial life skill. Change is both constant and inevitable and
the pace of change is likely to continue its relentless acceleration. We all make change choices in our lives, to whatever extent we are free to do. But are your change choices helping you towards your personal and professional goals, or impeding you? Are you using change to give yourself a richer and more fulfilled life with more renewal time, or are you stealing it from yourself?
The challenge for us all is to understand change in its many forms and how it can affect us, and to develop strategies to harness and maximise the upside benefits while also minimising the downside risks for ourselves and those around us.
1 Living and working with change (Part 2) Generational Change, The Technologist, Vol 18, Issue 1, Feb 2025.
2 Thrive, Arianna Huffington (2015). Ebury Publishing.
3 Standards for the Dental Team. General Dental Council www.gdc-uk.org
4 Living and working with change (Part 1) Technological Change, The Technologist, Vol 17, Issue 4, Nov 2024.

To complete your CPD, store your records and print a certificate, please visit www.dtauk.org and log in using your member details.
Q1 To which generational cohort does someone born in 1955 belong?
A Generation X
B Generation Y (‘Millenial’)
C Baby Boomer
D Generation Z (‘Post-Millenial’)
Q2 In what year did the NHS dental contract changes take effect in England and Wales, triggering a sharp drop-off in the prescription of chrome-cobalt dentures and multi-unit crown and bridgework?
A 2004
B 2006
C 2008
D 2010
Q3 When was mandatory GDC registration introduced for dental technicians?
A December 31st 2004
B June 30th 2005
C January 1st 2006
D July 31st 2006
Q4 From which of the dates below were dental laboratories required to register with the Medicines and Healthcare products Regulatory Agency (MHRA)?
A January 1st 2019
B January 1st 2020
C January 1st 2021
D January 1st 2022
Q5 When did Apple introduce the first smartphone (iPhone)?
A 2003
B 2005
C 2007
D 2009
Q6 What term is used to describe the pain felt by many users when separated from their smartphone or its functionality?
A Smartlessness
B Nomophobia
C Connectlessness
D Screen Deprivation Syndrome
Q7 What is the term often used by those who are introducing or implementing change, to describe a situation where maintaining the status quo no longer appears to be a sensible or feasible option?
A Slow fuse
B Tightrope walking
C Burning platform
D Paralysis by analysis
Q8 Who wrote the bestselling 2015 book ‘Thrive’, which referred to many of the unwelcome consequences of the digital revolution ?
A Arianna Huffington
B Annabel Tissington
C Anastasia Trumpington
D Ariadne Islington
Q9 The GDC’s guidance emphasises the need to stay up to date, stating that a registrant must find out about current evidence and best practice which affect what? Select the one incorrect option from the list below.
A The premises from which you work
B The equipment you use
C The quality of the work you carry out
D Your profitability
Q10 Which generational cohort is sometimes described as the ‘now’ generation, because they have grown up in a world where most of the things they want can be made available (and delivered to them) on demand.
A Generation Y (‘Millenials’)
B Generation X
C The post-millenials (‘Gen Z’)
D The baby boomers

Dr Chris Turner MSc, BDS, MDS, FDSRCS, FCGDent Specialist in Restorative Dentistry (Rtd) Bath

Aims:
■ Understanding the links between periodontal disease, plaque, and diabetes.
■ Effective denture and crown manufacture to help reduce plaque and periodontal disease
CPD Outcomes:
■ Maintenance of knowledge within your field of practice
■ Maintenance of attitudes that put patient interest first
I read recently that by the year 2050 fifty per cent of the population of Britain will be obese, which, by my calculation will be about 35 million people. We already have about 4 million people living with diabetes, the vast majority being type 2, the weight related type, and these are already said to consume about 10 per cent of the present National Health Service budget.
How many of those 35 million obese people will develop type 2 diabetes? The vast majority! Roughly 90% of people with type 2 diabetes are either overweight or obese, highlighting the strong link between obesity and the development of this condition. If my maths
is correct, by the middle of this century there will not be much money left to treat any other people. Perhaps we need to think more about prevention.
The interesting – and now well documented and scientifically accepted fact – is that there is a two-way reversible link between diabetes mellitus and periodontal disease, the one affecting the other and vice versa as this model demonstrates (Figure 1 - below). Diabetics are at 3-4 times greater risk of developing periodontal disease than the average person, a phenomenon first described in 1928. This rises to 10 times for smokers. Thinking about how that might impact an obese smoker is enough to set our minds reeling.
There is increased evidence that the link is related to inflammation as similar blood born inflammatory products are raised in

both diseases. For dentistry, these inflammatory products come from bacteria in mature plaque, a site we can have some positive influence over.
We also know that the five medical complications of diabetes, namely, cardiac, vascular, renal, ophthalmic and neurological are exacerbated in the presence of active periodontal disease, and, when periodontal disease is treated not only does blood sugar, or glycaemic control, improve there is also diminution in the severity of these complications.
It had been thought that periodontitis is a complication of diabetes. In the light of the above evidence, when periodontitis is placed at the hub of the two diseases, it cannot be a spoke, a complication. I have concluded that periodontitis is both modifying diabetics responses and modulating those responses in the manner of a volume knob on a radio.1
Recently Miyazama et al in Japan,2 from the largest study yet of diabetics have concluded ‘good oral hygiene is a critical component of glycaemic control in diabetic patients.’
This brings us back to prevention and plaque and how the dental team’s work might influence that.
In an earlier article we examined denture sore mouth and candidiasis related to patients wearing their dentures continually. My experience with this group was that they had not been cleaned very frequently and were often covered in plaque. To date there have been no studies looking at edentulous patients and diabetes, although we might expect there to be a link given the mature plaque connection.
With this in mind, when you deliver your completed acrylic dentures, what instructions do you give about cleaning? I suggest that this would be a good place to attach an instruction leaflet rather than leaving patients to do what they think they should. You might consider what cleaning

agents both to use and not to use – and add that patients should not wear their dentures at night. I would like to see this on your letterheaded paper. After all, this is your personally manufactured product and you deserve the credit.
You will recall another dictum of mine, “patients don’t see my work but yours”. You may have to agree the words used in such advice with your client dentists, while Clinical Dental Technicians have an advantage in this respect.
Before turning to crown and bridgework in detail we should consider the role of dental plaque in periodontal disease.
The classic investigation dates back to 1965, experimental gingivitis in man, when it was shown that if plaque is left in situ without removal for 7 to 10 days, gingival inflammations always results. 3 It is this mature dental plaque that is important for diabetics.
One of the toxins secreted by mature dental plaque is osteoclast activation factor, leading to resorption of alveolar bone. High blood sugar levels are associated with increased osteoclast activity, and diabetics suffer from poor healing. Combined, these
three factors give rise to the increased bone loss seen in these patients.
It follows that not only for all patients – but especially for diabetics – it is important that the contours of the crowns you manufacture and their fit to the prepared margins are factors in plaque retention and the patient’s ability to remove plaque efficiently and effectively every day.
The tendency is always to make crowns wider in a bucco- or labio-lingual direction than the teeth they are replacing. This has been the case especially for porcelain fused to metal (PFM) crowns because the tooth reduction presented to you in the working impressions is inadequate for the widths of materials required to make the restoration. Fortunately, we now have zirconium reinforced crowns that are not only more aesthetic and have better light transmission but can also be made to narrower shoulders, usually around 0.7mm wide.
Another factor that always leads to bulky crowns is the preparation angulation of the labial face of anterior teeth. The most important factor is the fit to the margins. If this is less than perfect it will result in a plaque trap and inflammation will always result. If you are faced with requests to use
impressions where you are unable to trim dies to give an absolute, unequivocally accurate margin, patients will develop periodontal disease however hard they try to control their plaque, because the traps that have been created in the finished crowns will always be there.
The usual cause is the dentist’s failure to use retraction cord before taking impressions of sub-gingival crown margins. In my experience this is because it takes time and needs training to place retraction cords effectively.
In summary, the appliances you manufacture have a long-term effect on the health of patients. This can be directly because patients are either unable to control their plaque or have not been given instructions about cleaning dentures that become plaque covered. For people living with diabetes this is doubly important as is demonstrated by the scientific evidence about the two-way relationship with periodontal disease and that disease’s influence on their medical complications and prognosis.
References and further reading.
1 Turner CH, Diabetes mellitus and its sixth complication explained, Int J Clin Case Reports and Reviews 25: 1-6, 2025. DOI:10.31579/2690-4861/730
2 Miyazawa I et al, 2024, The relationship among obesity, diabetes and oral health. A narrative review of world health evidence Doi:10:1007/s40496-025-00397-4
3 Löe H, Theilade E, Jensen SB, Experimental gingivitis in man. J Periodontal 36: 177-187, 1965.

To complete your CPD, store your records and print a certificate, please visit www.dta-uk.org and log in using your member details.
Q1 How many people are estimated to be obese in the UK by 2050?
A Some 50 million B About 20 million
C About 35 million D Over 40 million
Q2 Roughly what percentage of people with type 2 diabetes are overweight or obese?
A 70% B 90%
C 46% D 80%
Q3 By how much are diabetics estimated to be at a greater risk of developing periodontal disease?
A 3 to 4 times B 10 times
C 5 to 6 times D 7 to 8 times
Q4 In dentistry where do inflammatory products come from?
A Gingival infection B Mature plaque
C Ulcers D Caries
Q5 Which of the following are listed as medical complications of diabetes?
A Renal B Opthalmic
C Neurological D All of the above
Q6 What date was the classic investigation ‘experimental gingivitis in man’ carried out?
A 1929 B 1938
C 1965 D 1897
Q7 How long must plaque be left in place before gingival inflammation results?
A 7 to 10 days B 15 to 18 days
C Over a month D 12 to 15 days
Q8 What does osteoclast activation lead to?
A Periodontal disease B Plaque build-up on dentures
C High glycaemic index D Resorption of alveolar bone
Q9 If a crown’s fit is less than perfect what will it lead to?
A Inflammation around the margins B Periodontal bleeding
C A dental plaque trap D Wear on the adjacent dentition
Q10 Why might you be asked to use impressions where you are unable to trim dies?
A Because the impression tray was not pushed firmly enough around the posterior teeth.
B Because the dentist has failed to use retraction cord before taking impressions of sub-gingival crown margins
C Because the impression material was old and no longer malleable enough
D Because the dentist was busy and left the impression taking to the untrained nurse.
Tracey O’Keeffe, MA (Education), BSc (Critical Care), RN, MAFHP, MCFHP
This is the last paper in this series on mental health. This article discusses suicide and self-harm and what that means to those experiencing a need to self-harm or suicidal ideations. Perhaps as a starting point, it is important to explain different terminology associated with the subject. Gibson et al. (2019) suggest that attitudes vary towards people who self-harm or who have suicidal ideations, and this can come from misunderstandings or ignorance, often gleaned from media representation, both positive and negative (Nathan and Nathan 2020). Figure 1 provides four definitions which are useful as a baseline of knowledge development around a complex and often stereotyped subject.
Some important changes have been made to words used to describe suicide and self-harm (Silverman 2016), as it is recognised that inappropriate language can be detrimental particularly when the focus is on encouraging people to seek help (Corrigan et al. 2003). The phrase “commit suicide” brings with it a sense of wrong doing or committing a crime and therefore it is now discouraged and replaced with “die by suicide”. Similarly, suggesting someone partakes in “deliberate self-harm” uses a word inviting judgment and potential blame. Figure 1 also highlights variations in the use of the word suicide with slight differences depending on the prefix. Using the correct terminology can help to nurture a sense of openness and acceptance and this could result in an individual feeling able to reach out for support and help, be that through formal or informal routes.
There can be links between self-harm and suicide but they are also different. Around 3% of those who self-harm may ultimately die by suicide (Royal College of Psychiatrists 2020). Recognising the possible connection is important, but it also clear that it should not be a predetermined assumption as selfharming can instead be a way of surviving rather than trying to end life (Sue Lambert
Trust 2022). Nevertheless, some selfharming activities can result in fatality themselves. It is important to remain openminded and not embrace myths and unproven bias (see Figure 3), instead reframing those thoughts with information to become more open.
With a death by suicide approximately every 40 seconds and around 700,000 deaths every year, it is considered a public
health problem (World Health Organisation [WHO] 2017). Certain groups are more at risk and a snapshot of prevalence indicates the significance of the issue, and indeed the fact that we are likely to come into contact with an individual who may need help (see Figure 2).
The subject is complex and often difficult to understand (Sun and Zhang 2016) both in terms of who it affects and causational factors. Both Joiner (2005) and Mind (2022) suggest there can be a sense of hopelessness or feeling unwanted or a burden on others. Causative factors can be single or an accumulation of issues, including physical or mental health concerns and traumatic experiences (American Foundation for Suicide Prevention 2022). Self-harm can also be triggered by sexual abuse, problems at work or with relationships (Royal College of Psychiatrists 2020) or bullying or cyberbullying (Compass Fostering 2020).


Certain groups of the population can be identified as more at risk than others of both suicide and self-harm. Pearlman (2015) highlights the age group 15-25 years (female more than male) for self-harming, particularly those in residential care or prison care. The risk also increases with individuals with learning disabilities, those from Asian communities, drug or alcohol dependency, and those who are gay, bisexual or transgender.
Three particular groups which can be more susceptible to risk of suicide are males, the older adult and those individuals with a dual diagnosis. The reasons for this are different, but of course they may overlap. Statistics indicate that suicide is the fourth leading cause of death in males aged 15-29, with men in the age bracket 45-49 being three times more likely than women to end their life (Simms and Scowcroft 2108, WHO 2017). Various reasons are suggested for this including a focus on physical rather than mental health and a belief that men

need to be strong and not show emotion (Baffour 2018). Groups are emerging to help men open up and create networks. One example is Alright Mate (Grassroots Suicide Prevention 2016). Another is The Heads Up Campaign (Heads Together 2022), focuses on encouraging men to be open with their friends and chat as they would about football thereby “normalising” talking about emotions in males.
Another group of concern are older adults. Passive suicide ideation is more common alongside more limited support-seeking behaviour. Some may wish to hasten the end of their life feeling depressed. Attempts at suicide are more likely to result in death

in this group too possibly due to preexisting comorbidities, frailty and a lack of desire to seek help (Harmer et al. 2021). Isolation can also increase this risk and Agerbo et al. (2007) suggests links between people living alone and suicide.
The third group to consider as high-risk is those individuals considered as having a dual diagnosis. This means having a mental health diagnosis as well as a history of substance misuse (NHS 2022a), an example being bipolar disorder and uncontrolled alcohol use (Dalton et al. 2003). Feelings of depression and paranoia can be duplicated and therefore heightened, and there are links between depression, addiction and suicide (Foy 2019). Unpicking the main causative problem can be challenging.
Adding any extra stress (positive or negative) to an individual can be considered a trigger which results in a feeling overwhelm and creates feelings of not being able to cope (Mental Help 2022). The American Foundation for Suicide Prevention (2022) highlight experiences which may result in people feeling isolated, particularly in young people with bullying. Other triggers include problems with relationships and experience of abuse (Hawton et al. 2007). Furthermore, the experience can be personal (such as sudden unemployment, bereavement, financial worries or poor health) or may be

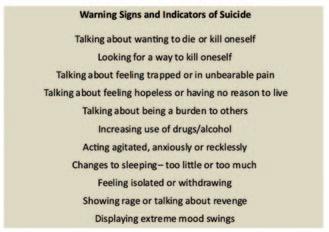
national events impacting individuals (Hawton et al. 2000). Even a perceived positive experience such as pregnancy can enhance risk, particularly if the individual is in a violent relationship, or if they are particularly young or with pre-existing mental health conditions (Nonacs 2020). Although, it may have been planned, pregnancy and childbirth is still a massive life change, and this highlights how added stress in any form can create a trigger.
Risk factors and triggers are complex and multi-dimensional. Working alongside these risks can be some more positive aspects of the person’s life which can help to counterbalance the situation (see Figure 4).
There are some cross-overs in terms of indicative signs of self-harm and suicide, but there are also some differences. Figure 5 provides some information about how thought processes that people who selfharm express. Gaining an understanding of
this, can help to recognise risk. Similarly, be aware of different ways people may selfharm and possible indicators, can create opportunity to offer help, support to signpost onward.
With regard to suicide ideations, there can also be warning signs (see Figure 6). Open dialogue may exist indicating a wish to end their life, but it could also be more covert including talk of being in unbearable pain, being a burden or feeling trapped or hopeless. Changes of behaviour can reflect a change in thought processing and altered feelings. If they are actively discussing methodology in terms of suicide or hoarding medicines, this can indicate active planning.
One aspect that people often feel anxious about is knowing how to speak to someone who is self-harming or thinking of suicide. It is important to remember to speak with them rather than to them, creating an open, safe space. The first priority must always be safety with any immediate risk to life, (whether it be theirs or someone else’s), necessitating a 999 call. Serious injury and physical harm would also require this. A calm approach acknowledging the person’s emotions can help avoid a sense of confrontation or judgement alongside a willingness to listen. The Samaritans (2023) suggest a calm, caring approach called “SHUSH” (see Figure 7). A point of note here is
recognising that asking someone directly about suicide does not increase their likelihood of carrying out the act. Conversely, it can act as providing permission for them to speak openly and freely. An open, unapologetic approach too can show care and genuine concern (Ruiz 2019).
When helping someone who is self-harming, it may be useful to ask about what has helped in the past (The Samaritans 2023). Preexisting coping strategies, such as holding ice, cubes, punching pillows, writing down thoughts, or distraction, can be used to get alleviate some their current experience or direct them to a less harmful activity.
For both self-harm and suicide, recognising our own limitations and to encourage the individual to seek professional help is vital. Sign-posting to services or more practical help such as phoning someone they need to speak with can be important. This could be family or a healthcare professional.
It can in some situations, be difficult to work with confidentiality if the person does not want help. The key concepts here are best interests and safety. Any sort of sharing should be carried out in light of GDPR regulations and therefore only the minimum necessary information should be shared. Zero Suicide Alliance (2021) highlight a framework around the work “SHARE”. As well as this they suggest that a dialogue which can be used to help encourage communication and sharing. They advocate wording similar to the following:
“In our experience it is almost always much better to involve a third party, somebody you know and trust, in your care, treatment and recovery. This might be a family member, friend, colleague or somebody important to you. This is likely to result in a better outcome and better support for yourself.
We do not have to share everything and I will respect your wishes, but I want to do all I can
to make sure you have the best possible care and support around you. Can we please discuss who else we might involve in your care?” (Zero Suicide Alliance 2021).
This stresses that only necessary information will be shared in order to get them the support and help they need but still encourages the person to think about who they might be happy to share with. Approaching each situation openly and with compassion will hopefully give the individual who is experiencing mental health problems confidence and allow them to feel confident to share. This ultimately is what could be difference between a positive start to a new journey or a potentially irreversible outcome.
This paper has looked at self-harming and suicide, a vast and complex subject. They are both often challenging and emotive areas, but the main message is one of compassion, empathy and non-judgement. This is easier with greater understanding and knowledge and hopefully this article has provided some insight. Mental health can affect anyone at any time, so suicidal ideation or self-harm behaviour is something we may all come into contact with during our lives.
– Agerbo, E., Sterne, J., Gunell, D. 2007. Combining individual and ecological data to determine compositional and contextual socioeconomic risk factors for suicide. Social Sci Med. 64:451–1. doi: 10.1016/j.socscimed.2006.08.043
– American Foundation for Suicide Prevention., 2022. Risk Factors, protective factors, and warning signs. [online] [viewed 10.3.22], Available at: Risk factors, protective factors, and warning signs | AFSP
– Baffour, F. 2018. Male Suicide: A Silent Epidemic. [online] [viewed 9.3.22] Available at: https://www.bps.org.uk/ blogs/dr-funke-baffour/male-suicide-silent-epidemic
– Compass Fostering. 2020. What to do if you think your child is self-harming. [online] [viewed 10.3.22], Available at: Different Types of Self Harm | What to do | Compass (compassfostering.com)
– Corrigan, P., Markowitz, F.E., Watson, A., Rowan, D., Kubiak, M.A. 2003. An attribution model of public discrimination towards persons with mental illness. J Health Soc Behav. 2003; 44: 162-179
– Dalton, E.J., Cate–Carter, T.D., Mundo, E., Parikh, S.V. and Kennedy, J.L. 2003. Suicide risk in bipolar patients: the role of co-morbid substance use disorders. Bipolar Disorders. 5(1), 58–61. doi: 10.1034/j.13995618.2003.00017.x
Figure 7: Supporting someone who expresses suicidal thoughts or self-harms (based on Samaritans 2023)

– Foy, C. 2019. Treating Co-Occurring Disorders to Help Prevent Suicide. [online] [viewed 11.3.22] Available at: https://fherehab.com/learning/co-occurring-disordersand-suicide/
– Gibson, R., Carson, J. and Houghton, T. 2019. Stigma towards non-suicidal self-harm: evaluating a brief educational intervention. 28 (5). https://doi.org/ 10.12968/bjon.2019.28.5.307
– Grassroots Suicide Prevention. 2016. Alright Mate. [online] [viewed 8.4.25]. Available at: Alright MateGrassroots Suicide Prevention
– Harmer, B., Lee, S., Doug, T. V. H. Saabadabi, A. 2021. Suicidal Ideation. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. PMID: 33351435
– Hawton, K., Bergen, H., Casey, D. et al. 2007. Selfharm in England: a tale of three cities. Multicentre study of self-harm. Soc Psychiatry Psychiatr Epidemiol. 42, 513-521
– Hawton, K., Harriss, L., Appleby, L., Juszczak, E., Simkin, S., McDonnell, R., Parrott, H. 2000. Effect of death of Diana, Princess of Wales on suicide and deliberate self-harm. British Journal of Psychiatry. 177 (5). 463-466. doi:10.1192/bjp.177.5.463
– Heads Together. 2022. Heads Up. [online] [10.3.22] Available at: https://www.headstogether.org.uk/ heads-up/
– Joiner, T. 2005. Why people die by suicide. Harvard University Press – Kposowa. A. J. 2003. Divorce and suicide risk. Journal of Epidemiology and Community Health. 57 (12), Letter to editor. http://dx.doi.org/10.1136/jech.57.12.993
– Mental Help. 2022. Suicide Triggers. [online] [viewed 10.3.22]. Available at: https://www.mentalhelp.net/ suicide/triggers
– Mind. 2022. What are suicidal feelings? [online] [viewed 10.3.22] Available at: What are suicidal feelings? – Mind
– Nathan, N. A. and Nathan, K. I. 2020. Suicide, Stigma and Utilising Social Media Platforms to Gauge Public Perceptions. Front. Psychiatry. 10. https://doi.org/ 10.3389/fpsyt.2019.00947
– NHS. 2022a. Dual Diagnosis. [online] [viewed 10.3.22], Available at: http://www.awp.nhs.uk/advice-support/ conditions/dual-diagnosis/
– Nonacs, R. 2020. Suicidal Ideation in Pregnancy More Common in Women with Trauma Histories. [online] [viewed 13.3.22], Available at: https://womensmental health.org/posts/suicidal-ideation-in-pregnancy-morecommon-in-women-with-trauma-histories/
–
Office for Health and Improvement Disparities. 2023. Public Health Profiles. [online] [viewed 23.2.23]. Available at: Public health profiles - OHID (phe.org.uk)
– Pearlman, J. 2015. Why do People Self-Harm? [online] [viewed 27.2.23]. Available at: Why do people selfharm? - The Mix
– Royal College of Psychiatrists. 2020. Self-harm [online] [viewed 10.3.22]. Available at: Self harm | Royal College of Psychiatrists (rcpsych.ac.uk)
– Ruiz, R. 2019. The Crisis Text Line analyzed 75 million texts to pinpoint the best way to ask if someone’s suicidal. [online] [viewed 27.2.23]. Available from: How to ask if someone is suicidal, according to data | Mashable
– Save. 2023. Warning Signs of Suicide. [online] [viewed 27.2.23]. Available at: Warning Signs of Suicide – SAVE – Simms and Scowcroft. 2018. Suicide Statistics Report: Latest Statistics for the UK and the Republic of Ireland. [online] [viewed 9.3.22]. Available at: Suicide_statistics_report_FINAL.pdf (samaritans.org)
– Sue Lambert Trust. 2022. Myths and stereotypes about self-harm. [online] [viewed 13.3.22]. Available at: https://www.suelamberttrust.org/wp-content/uploads/ 2020/11/HO12-Myths-about-self-harm-v2.pdf
– Sun, B. Q. and Zhang, J. 2016. Economic and sociological correlates of suicide: Multilevel analysis of time series data in the united kingdom. J. Forensic. Sci. 61(2):345-351. doi: 10.1111/1556-4029.13033
– The Samaritans. 2023. If you’re worried about someone else. [online] [viewed 27.2.23]. Available at: What to do if you think someone is struggling | Samaritans
– World Health Organisation. 2017. Suicide. [online] [viewed 23.2.23]. Available at: Suicide (who.int)
– Zero Suicide Alliance. 2021. Independent report. SHARE: consent, confidentiality and information sharing in mental healthcare and suicide prevention. [online] [viewed 27.2.23]. Available at: SHARE: consent, confidentiality and information sharing in mental healthcare and suicide prevention - GOV.UK (www.gov.uk)
In February 2025, Joel Mannix (left) (Head of Dental at Christie & Co) sat down with Jason Wong (right) (Chief Dental Officer for NHS England) to discuss the key trends and challenges in the dental sector. The following is The Technologist’s edited excerpt from that conversation.
Joel: How has everything been since 2024?
Jason: We have been busy trying to work on the next set of reforms for dentistry. It’s now acknowledged that NHS dentistry requires reform while making sure that patient care is at the centre of everything we do. There are a lot of things happening on the world stage as well. I think, in England, it is a case of making sure that we have the workforce to deliver the care that a patient needs.
Over the past year there’s been continued recovery. The target was to try and get back
at least to pre-pandemic levels, but I don’t think we’re quite there as we stand with NHS dentistry at the moment.
The previous administration launched a dental recovery plan. Within it, there were some short-term boosts to the sector as well as some, long-term workings aimed at improving oral health and the recruitment and retention of teams. We’ve been working through that and then, of course, the manifesto pledges that the new Government has made.
Joel: Do you expect recruitment and funding challenges to remain in the NHS
dental sector long-term?
Jason: I’m hoping it doesn’t. We are still at the stage now where two separate narratives are going on about recruitment in particular. There is one which was picked up by a lot of people that suggests that we have enough dentists in the country, but that they don’t want to do NHS treatment. But, if you look at the figures and compare us with others in Europe, we’re one of the lowest.
There was also a workforce survey carried out by the General Dental Council in

and the pictures that we have to give us more feedback. The NHS has always had a very slow path to picking up technology. We had a conference about a week and a half ago, and one of the speakers said it took, on average, 17 years of innovation research to get to the front line of the NHS, although the NHS is placing quite a bit of its technological advances on the NHS app, and if there’s some way of linking the NHS app and the NHS information system with a practice software information system, I think that could be a big move. Certainly, having the digital ability to deliver advice and information, thus putting more power in the hands of – or the phones of – our patients is a good thing. Some of these technological advances also make restorations cheaper to produce. So, that is an area the NHS is keen to explore.
Joel: In 2024, 82% of our practice sales went to independent owners. How do you see this impacting dentistry and the NHS?
Jason: That’s quite a surprising figure. The one set of definite figures that I saw were between 2007 and 2017, and on the performance list the number of providers –which is how the NHS distinguishes between someone that has a stake in the practice – had dropped from around 40% to below 10%, and the trajectory was going down much further.
Joel: Looking at the year ahead, Jason, what are your expectations for UK dentistry in 2025?
Jason: From the perspective of the NHS, I think a lot hinges on the set of reforms and how the NHS brings that on both in terms of, I suppose, 2025/26, having some kind of reform that can be put into place quickly, and then 2026 onwards or the end of 2025/26, you would hope that we will have a good picture of how NHS dentistry will be reconfigured. In terms of private dentistry, there’s a lot going on about the current cost of living and how that might impact that, especially the elective part of the market. But it is an area that seems to be

thriving. Some rely quite a bit on cosmetics and I’m not into predicting how the cosmetic market will go, but overall, while I think there’s no question that there is a definite need for NHS reform, and we’re not blinded by fake optimism, but, dentistry itself, as a sector, I think will do quite well.
One of the things I keep saying, and sometimes people disagree with this, is the overall issue is not that dentistry has failed, it’s access specifically to NHS dentistry that we’ve struggled with. The other issue is, if you look at the figures, yes, they’re down from what they were, but it wasn’t the wholesale complete change that everyone was talking about. I’m certain that, coming as I do from an area that’s a rural locality, I was aware of the problems pre-pandemic. The issue is that what we had was a recovery, but the recovery had almost become the new normal and we need to do something, first of all, to bring it back to the pre-pandemic levels. But we can’t stop there. We have to extend that in order to put the NHS on a sustainable footing.
While the reform process is not directly under my responsibility, we put quite a lot of time and advice into helping the process.
So, I think, seeing through some sort of reform programme, both short and medium and long-term, would be good. In my own areas, I want to see some change in terms of the culture of the profession. I think that, at the moment, it sort of sits in a culture of fear about what will come next, and I’m doing all I can to try and change that from a legislation perspective, talking to the regulators, as well as improving the clinical governance perspective.
We’re also looking at the well-being side of things, which has been a particular issue in dentistry that we’re trying to deal with. We’ve also been helping in terms of recruitment and retention and the workforce strategy. Some of that will be decisions made by the Government that we then feed into to try and help. My role will be to support that in every way that we can and, indeed, in other parts of the system as well, both to give advice but also to try and help with its implementation for England.
A To watch the full video interview, visit: https://www.youtube.com/watch?v=0E __0Y7yOpA
