DTA Rewards save on everyday spending

MHRA Regulation: The Facts In this issue:
We are not immune, plague and vaccination
Digital Dental Technology & Dental Technologists
Joanne Stevenson: DTA President Interview


HOURS OF VERIFIED CPD





MHRA Regulation: The Facts In this issue:
We are not immune, plague and vaccination
Digital Dental Technology & Dental Technologists
Joanne Stevenson: DTA President Interview


HOURS OF VERIFIED CPD



● are individually registered with the GDC to be able to use the titles that relate to our role in the UK
● maintain our own lifelong learning through relevant continuous professional development (as provided free to the Dental Technologists Association [DTA] members)
● ensure that we are covered by specific indemnity insurance related to our dental laboratory custom-made dental device manufacturing work, and if necessary, related clinical work and/or extended roles
● work within the GDC Scope of Practice for our registered role, along with other extended areas as confirmed by further additional training
● are, as a current GDC registered dental technologist, able to sign-off custom-made dental devices under MHRA/MDR regulations, indicating that such appliances are fit for purpose as stated on the Statement of Manufacture
● maintain and develop our dental team networks to enhance patient care
Editor: Derek Pearson t: 07866 121597
Advertising: Rebecca Kinahan
t: 01242 461 931
e: info@dta-uk.org
DTA administration: Rebecca Kinahan
Operations Coordinator
Address: PO Box 1318, Cheltenham GL50 9EA
Telephone: 01242 461 931
Email: info@dta-uk.org Web: www.dta-uk.org
Stay connected: @DentalTechnologists Association
@The_DTA @dentaltechnologists association
Dental Technologists Association (DTA)
DTA Council:
Joanne Stevenson President Chris Fielding
Deputy President Tony Griffin Treasurer
Delroy Reeves DTA Liaison Delegate
Joanne Clark, James Green, Raya Karaganeva, Robert Leggett, Patricia MacRory and Jade Ritch.
Editorial panel: Tony Griffin Joanne Stevenson
Editorial assistant: Dr Keith Winwood




The Dental Technologist Association (DTA) is delighted to announce the appointment of new Council members, Raya Karaganeva and Joanne Clark, as well as the return of James Green, following the successful elections in May 2025.
On behalf of the team, DTA President Joanne Stevenson warmly welcomes you to the management team. We extend our heartfelt congratulations on your new roles and express our sincere gratitude for your voluntary contributions to the profession, all while continuing your dedicated work as registered dental technicians.
Raya Karaganeva
Raya is a Lecturer in Dental Technology at the Queens Dental Sciences Centre, University of Greater Manchester. She qualified as a dental technician in 2015 at Manchester Metropolitan University, where she went on to complete a PhD in 2019. Her doctoral research focused on the effects of custom-made mouthguards on retention, comfort, and physiological responses during exercise. Since then, she has had a primary interest in Sports Dentistry and has worked closely with Dental Trauma UK and the DTA to disseminate knowledge and raise awareness of custom-made mouthguards. Raya has previously delivered CPD seminars for Health Education England and has

presented as an invited speaker at national and international conferences. Currently, she is involved in research projects which aim to investigate contemporary developments in dental materials and is open for collaboration.

James Green is a Maxillofacial and Dental Laboratory Manager for Great Ormond Street Hospital (GOSH) in London and Broomfield Hospital in Chelmsford, Essex.
James trained at Barts and the London, Queen Mary’s School of Medicine and Dentistry, and Lambeth College, London, and qualified as a dental technician in 2001. This was followed by a vocational training year at the Royal London Hospital and two years based at the Eastman Dental Hospital, University College London Hospitals NHS Trust, before transferring to GOSH in 2004.
He developed the auricular splint, a custommade medical device that maintains projection and dimensions following auricular reconstruction (which was published in the Annals of Plastic Surgery)
and an obturator prosthesis for children with teeth that cannot accommodate clasps due to insufficient eruption (published in the Journal of Prosthetic Dentistry).
James has delivered more than 50 invited lectures, both nationally and internationally, and authored or co-authored more than 25 peer-reviewed journal articles. His awards include the British Orthodontic Society Technicians Award (2002) and the British Orthodontic Society Award to an Orthodontic Technician for Distinguished Service (2024). James first joined the DTA council in 2008 and served as Deputy President from 2014 to 2016 and President 2016 to 2018. He is also a council member for the Orthodontic Technicians Association, where he served as Treasurer between 2007 and 2016 and Secretary since 2018.
Joanne is a prosthetics technician working in and running her family-owned dental lab in east London, alongside her brother. Joanne initially joined her family in the lab in 2003 in an admin role before studying to become a dental technician herself, completing a BTEC in dental technology at Lambeth college in 2017. Joanne now splits her time between hands-on prosthetic work and overseeing the smooth running of the lab as a whole.

Lifestyle vouchers offer DTA members a choice of everyday treats from the high-street, online, your weekly food shop, leisure and travel sectors – with access to over 300 of the UK’s biggest brand names. Save 6% at M&S, Argos, Boots, Currys, ASOS, Costa, John Lewis, Nandos, Tui, Sainsbury’s and hundreds more!















How to make the most of this saving?
Lifestyle vouchers can be redeemed online, in-store, or both depending on the retailer. This gives you the full flexibility you want to choose your redemption method while also maximising your savings. Vouchers can be split and spent across multiple big brand names. Lifestyle gives you the biggest choice of leading retailers, all in one place.


Starting a new year of CPD for 2025-2026
Your 2024-2025 CPD cycle has ended, and the GDC requires you to submit a statement by 28 August 2024, if you haven’t already done so.
You don’t need to submit your records now, but it’s essential to keep them safe in case the GDC requests them.
A If you have any concerns, reach out to the GDC promptly by calling the helpline, 0207 167 6000 or emailing renewal@gdc-uk.org

Important CPD dates:
CPD year runs from 1 August to 31 July
Then you have four weeks to make a CPD statement by 28 August.
Any CPD completed on or after 1 August counts towards the following year.
Here are some simple steps to help you when starting your new year of CPD:
1 Make sure you download your files from your 2023/2024 logbook.
2 Save your CPD certificates to your computer.
3 Add to and update your personal development plan for the year ahead.
4 You can now start taking CPD for your new 2024/2025 cycle year. Remember, on average dental technicians should complete around 10 hours per year and the GDC state that you must complete at least 10 hours over a two-year period.
5 For those that have now reached the end of your 5-year cycle and this means you should have completed 50 hours (or 75 for CDTs). You therefore might want to think about setting new goals for the new 5-year cycle ahead.
The first dental technician in the UK to achieve a fully digital Immediate load using Nobel’s latest system
Visitors were captivated by Davide Accetto’s presentation at the Dental Technicians Hub on Saturday, 17 May during DTS. As the first dental technician in the UK to achieve a fully digital Immediate load using Nobel’s latest system, Davide shared his groundbreaking experience and insights during the session and discussed the use of photogrammetry FastMap X-guide together with an IOS making it possible to CAD design and 3D print full arches on surgery day, to be screwed directly on MUAs with extreme accuracy without conventional methods. If you missed his talk during DTS, we will be sharing a filming of the session as a webinar soon. ‘Experience the future with digitally designed 3D printed immediate load.’ Don’t miss this opportunity to learn from a pioneer in the field and explore the cutting-edge advancements in dental technology.

The DTS Prize Draw
Thank you to everyone who visited our stand at the Dental Technology Showcase. Congratulations to Chris Ellis the winner of the prize draw and recipient of 12 months’ free membership!
may result from their work. Membership with the DTA offers exclusive discounted indemnity insurance in partnership with UK Special Risks.
A From the Crib to the Archwire –Orthodontic Wire – Articulate, September 2024
A Regulating Honesty and Integrity –Articulate, September 2024
Apprenticeships and routes to registration
To be a General Dental Council (GDC) registered dental technician trainees must complete an approved dental technology programme. This can be achieved through various routes, including university courses, college courses, apprenticeships, or a combination of practical training and part-time education in a commercial dental laboratory or dental hospital. The GDC maintains a list of approved qualifications and course providers on their website. We plan future interviews with education providers.
As a newly qualified dental technologist, do you understand your obligations? Once their educational requirements have been met, the dental technician must apply for registration with the GDC. This involves completing an application form and providing evidence of their qualifications and training. The GDC also requires dental technicians to have appropriate indemnity or insurance in place to cover their professional practice in order to ensure that they are protected against any claims that
In addition to these requirements, dental technicians must adhere to the GDC’s Standards for the Dental Team. These standards set out the principles, standards, and guidance that govern the conduct, performance, and ethics of dental professionals. They include putting patients’ interests first, communicating effectively with patients, obtaining valid consent, maintaining and protecting patients’ information, and working within their professional knowledge and skills. Dental technicians must also engage in continuing professional development (CPD) to maintain their registration. This involves completing a minimum of 50 hours of verifiable CPD every five years.
By meeting these requirements, dental technicians can ensure they are providing safe and effective care to their patients while also maintaining their professional standing with the GDC.
The DTA offers invaluable support to newly qualified dental technicians in meeting their professional obligations. As a member, dental technicians gain access to a wealth of resources, including comprehensive guidance on regulatory updates, technical FAQs, and business management templates. The DTA also provides a range of CPD opportunities, over 20 hours annually, ensuring that members can easily meet their CPD requirements. With the introduction of a wellbeing helpline, a comprehensive resource hub, and the DTA’s new membership benefits scheme, ‘DTA Rewards,’ (mentioned above) designed to help members save on everyday expenses – your personal interests are well-supported too.
A Flexible Dentures A Case Study –Jo Stevenson – The Technologist, November 2024
A Audit Again: Crown and Bridgework –Dr Chris Turner – The Technologist, November 2024
A Living and Working with Change Part 1: Technological Change – Kevin Lewis –The Technologist, November 2024
Show organisers celebrated the success of Dental Technology Showcase 2025, exhibitors and visitors alike found much to discover and enjoy. The DTA stand was a focus of attention keeping DTA Operations Coordinator Rebecca Kinahan and DTA Liaison Delegate Delroy Reeves busy dealing with enquiries, members dropping in, and friendly visitors. A spokesperson for the show offers more details.
DTS, co-located with The British Dental Conference & Dentistry Show (BDCDS), concluded following another year of resounding success. Held at Birmingham NEC on the 16 and 17 May, the show brought together thousands of industry professionals to explore the latest advances in dental technology and explore game-changing innovations, with countless business connections made. A highlight for many in the dental calendar, the show surpassed all expectations and received outstanding feedback from delegates and exhibitors alike. Rebbeca Peltier from DB Orthodontics said, “We love doing DTS. There are some fantastic customers, regular customers, yearly, that come to see us, and new customers too. It’s always nice to see some new faces, but we find DTS a great opportunity to showcase our products to new customers. We love all our face-to-face interactions.”
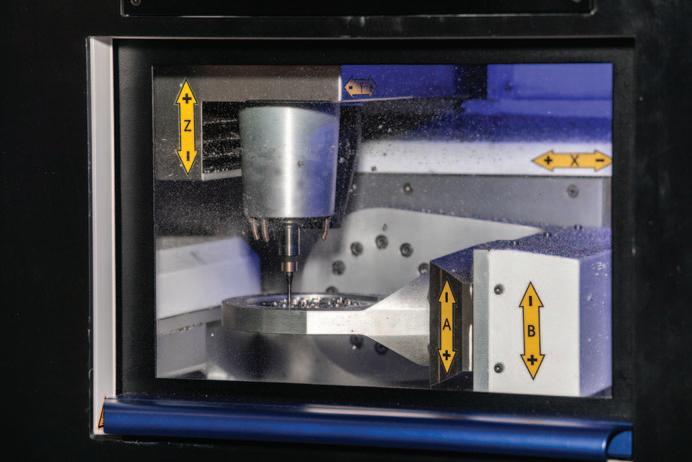
Over 80 exhibitors, including the biggest names in dental technology, showcased their latest innovations and the floor was


abuzz with excitement and inspiration. From state-of-the-art equipment to the latest in digital tools, there was something for everyone, proving DTS is the ultimate place to discover solutions that can revolutionise your lab.
The innovative Digital Dentistry Theatre, in collaboration with the IDDA, proved a must-attend destination. Live demonstrations and sessions on cuttingedge topics – from AI in diagnostics to 3D printing and digital workflows – offered attendees a hands-on glimpse into the future of dentistry. Delegates walked away with practical knowledge and inspiration to enhance their digital capabilities.
Portfolio Director, Alex Harden said: “It’s been another exceptional year, and truly inspiring to see the dental community come together to push boundaries and elevate the profession. From world-class speakers and valuable networking opportunities to the energy across the aisles, stands, and theatres – it’s been a privilege to host it all under one roof and provide a vibrant platform for professional growth and development.”
Over 50 world class speakers took to the stage across three dynamic show theatres. Covering the latest trends and topics of interest, the packed agenda included
insights into the latest trends, discoveries, and best practices in dental technology. Delegates were able to gain up to 12 free eCPD hours, a fantastic way to boost their knowledge while meeting professional development goals.
The show also proved it is more than a conference and provided multiple networking opportunities bringing together thousands of key decision-makers, thought leaders, and innovators in the dental technology sector for meaningful conversations and career-building connections. Jo Bentley from Ivoclar said: “It’s great to attend Dental Technology Showcase because we love meeting new and existing customers, and it’s a great way to showcase what we’re all about. It was a fantastic couple of days.”
A The Dental Technology Showcase 2026 will take place on 15 and 16 May, at the NEC in Birmingham. For more information on show updates visit https://the-dts.co.uk

New DTA President Joanne Stevenson looks back over her career and forward to the association’s future.
Let me introduce myself. I am a prosthetic dental technician originally from Manchester, currently residing and working in Belfast. My career as a technologist really began during my school years, guided by my careers officer. I had a strong aptitude for sciences and was keen on working in a laboratory setting but couldn’t decide on a clear career pathway. I attended interviews at microbiology labs at Christie Hospital and Scottish and Newcastle Brewery before I was eventually introduced to a dental laboratory. I was
immediately captivated by possibilities of the field, I felt it perfectly combined my passion for hands-on work with my interest in science.
Iwas able to connect with a group of dentists offering scholarships to aspiring dental students and it was they who enabled my placement in a prosthetics lab. I subsequently enrolled at Manchester Metropolitan University to pursue a BTEC National in Dental Technology, where for four years, I balanced my time between working in the lab four days a week and attending classes one day a week.
I qualified in 1995 and relocated to Belfast, where my family originated. Currently, I work in the prosthetics department at one
of the largest laboratories in Northern Ireland and my duties encompass all aspects of prosthetics, including implantretained overdentures and hybrid bridges.
I first joined the DTA council during the lockdown period after submitting an article for The Technologist publication, which led to an invitation to join the management team. After three years working as part of the team, I was elected deputy President alongside then President Delroy Reeves. My two years as deputy garnered invaluable insights and experience under Delroy’s leadership, until this year (2025) when I had the honour of being elected as the first female President of the DTA. I feel it to be both a tremendous privilege and a great responsibility to be entrusted with this role by my fellow council members, and I am

committed to leading the association with dedication and integrity.
The DTA has always been a strong advocate for our members, providing them with advice and guidance throughout their careers. I see an important part of my responsibility is to promote effective education and training, offering lifelong learning opportunities and advocating for the highest standards of practice. The management team is always looking for ways to improve the benefits for our members and provide them with as much information as possible. Just thinking about what we can do fills me with energy, we have an exciting year ahead.
Our new benefits package, ‘DTA Rewards’, designed to save our members money on day-to-day spending, can actually save them more than the cost of their membership!
We are also developing a series of free CPD digital education videos, with a focus on digital dental technology for 2025 and more to come in 2026. We are also committed to offering comprehensive Wellbeing support and have invested in a resource hub to provide our members with valuable tools and information to support their professional and personal growth, and we hope to continue adding valuable resources for our members as the profession evolves.
The field of dental technology is advancing at a remarkable pace, and I believe we will one day see dental technicians transitioning from traditional bench work to a more digital-based workflow. We have a comprehensive look at digital developments for technologists in this issue (pages 9-15) but I know that an understanding of dental anatomy and time working in an analogue format strengthens my work ethic, and the ability to work with one’s hands remains essential. While many of the labour-intensive and messy aspects of the job are being replaced by digital processes, the final finishing touches and the creation of high-end cases still require the skill and creativity of a technician.

I want to remind members of the DTA Fellowship programme which recognises dental technicians for their high-quality work in manufacturing custom-made dental device. This award is only presented to experienced DTA members who have demonstrated excellence in their field, showcasing their skill and dedication through their creations. The DTA Fellowship programme not only acknowledges these people’s contributions to the field but also inspires others in the profession to strive for the highest standards of quality and innovation.
Digital technology will continue to broaden the horizons for dental technicians, including digitally designing restorations for laboratories worldwide; it is such an exciting time to be part of the dental technology family and seeing these new career opportunities open up. We should be sharing this message with schools to incentivise the next generation and bring them to the modern, cleaner streamlined dental laboratory. The integration of AI and innovative techniques will transform the way dental devices are manufactured –while, handmade custom-made, porcelain
dental appliances may become rarer but will remain highly sought after.
I mentioned our need to reach out to the next generation, it is vital. The decline in dental technician numbers is a real concern, and while there are still several colleges offering training courses the situation is becoming particularly challenging in Northern Ireland, where training opportunities are more limited when compared to the UK mainland and too many students have had to resort to distance learning to pursue their education. The DTA is committed to supporting students throughout their studies by providing copies of The Technologist publication and offering reduced-price student memberships.
In trying to maintain a level playing field, we are committed to educating our members and raising awareness of regulations to all professional bodies ensuring compliance with the Medicines and Healthcare products Regulatory Agency (MHRA) and Medical Device Regulations (MDR) for custom-made dental devices.
We have a very informative article in this
issue of The Technologist (pages 16 to19) that explains the DTA stance in much more detail, but in summary, the laws state:
A Manufacturers of custom-made dental devices must register with the MHRA and provide each patient with a statement of manufacture for each device.
A This requirement applies to both the manufacture of dental devices in the UK and the importation of dental appliances from overseas.
A In-clinic fabrication of dental devices must also be regulated by the MHRA and the MDR.
A The GDC emphasises that compliance with the MHRA is essential for custommade dental devices in the UK, as outlined in the Standards for the Dental Team 2013.
A Registrants who sub-contract or use dental laboratories outside the UK must ensure that the manufacturer complies with the UK MDR and are liable for this responsibility.
The DTA continues to advocate for compliance with these regulations and
highlights the essential role of dental laboratories in oral healthcare. We regularly meet with regulators to discuss these important topics.
The way I see my role as President of the DTA is as a colleague and supporter of our profession, our members, and the whole dental team.
We have great relationships with all our fellow associations and work with the GDC, Chief Dental Officers and industry influencers and leaders to ensure our members are informed about technological developments, regulatory changes, and trends in the dental landscape. We see technologists as key members of the whole dental team, not just artisans working in the background but very often in the vanguard of dental developments.
Above all we members of the DTA council want to continue the excellent work and support that the DTA has always provided to our members. We are a cohesive team, each of us brings a unique vision to the association, and, working together we bring

a powerful collaboration of insight and experience to our members. We are working to enhance educational resources and training opportunities for dental technologists, we are constantly advocating for regulatory compliance and high standards in dental technology, wiping away any confusion about who should or should not be regulated and by whom, and we are striving to promote the tremendous opportunities in our profession to help attract new talent and address the decline in the number of dental technicians.
Coming into my position as President after Delroy Reeves was a humbling prospect, he left some big shoes to fill, but he is still with us as the DTA liaison delegate and we all value his contribution. We have welcomed our new council members Raya Karaganeva and Joanne Clark, as well as James Green returning to the fold, and Chris Fielding takes my place as deputy President. It is very much the DTA fielding its strongest, world class team. All I can hope is that, with their support, when my tenure as President comes to an end, the association will remain as strong as it is now and, under my leadership, will have moved on to even greater achievements.
I hope together we can continue to have a significant impact by advancing the standards of dental technology, supporting the professional growth of dental technologists, and ensuring the highest quality of care for patients as invaluable members of the dental team.
My aim is to leave a legacy of innovation, collaboration, and excellence. I am deeply grateful for this opportunity to serve as the President of the DTA and I am genuinely excited about the future of dental technology.
I look forward to working with my fellow DTA members and our entire dental community to help establish a pathway that will lead technicians to the future they rightfully deserve.
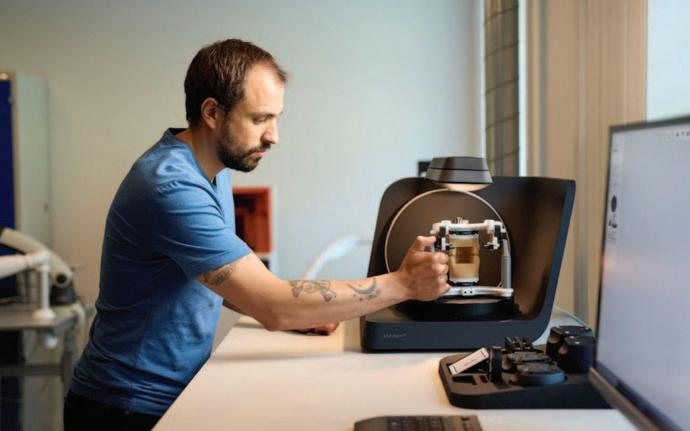
DTA Student Representative Dan Bant introduces our digital feature with an overview of what you need to consider when converting from analogue to digital in the dental laboratory.
The advice from every side is that if you don’t invest in digital you are going to be left on the platform when the train to the future pulls away and heads off towards tomorrow. Can you afford not to? the pundits ask. Perhaps not, but first and foremost, you need to take a cold and clinical look at the finances.
Step one, know your budget; there are various different routes into digital but the most important is knowing your budget before you get started. How much is your initial outlay and what is your predicted ROI (return on investment)? And, realistically, how long that might take to break even.
Step two, is your computer up to the job?
Can it handle the download portals (more of which later) and various other CAD software, such as exocad or 3Shape etc., Believe me, there’s nothing more frustrating than depending on a slow computer when controlling the efficiency of your workflow.


Step three, before raiding the kids’ piggy banks to jump on the CAD-CAM express, take time to research your choices for equipment and software. Dental shows have many examples on offer, but I think it’s best to also ask those who have already invested in certain products and get their honest opinion regarding their true value. Ask for advice as to where you might best begin your digital workflow. There will be a learning curve so it might be best to start simple and expand from there. You’ll need a little flexibility in your workplace – you must be prepared to adapt to new technologies and any new workflow systems will come with fresh problems –but there are always others who have been in the same position and have dealt with the same issues who may be able to help. Ask whether your technology provider can offer a training programme, a mentor on demand who can guide you through your first steps on your digital journey. You are lucky in the fact that you already have analogue experience at the workbench, you
understand dental anatomy in a way that cannot be replicated by AI. The digital tools you choose are simply an adjunct to skills you already possess, being aware of that might help level-out that learning curve you’re facing.
Or you can outsource your work to others. All you need to start the digital process is to download the online portals I mentioned previously to transmit your CAD cases to labs already equipped with CAM systems such as 3shape, iTero, Medit, DS core etc., and then you can outsource for all areas of work without any need to personally invest in such equipment. This can help to ease you into a full digital workflow while also allowing you to research your next move and take your time to invest in chosen areas along the way.
So, what next? Training! Let’s say you are now the proud owner of your carefully selected digital technology and it is fully integrated into your laboratory workflow. If
you have staff working with you, you must also ensure that they are trained and up to speed with the use of your selected design software, 3D printers, scanners, milling machines etc., to ensure they can get the best out your investment. I can’t stress enough that digital technology is a tool that will help make your workflow faster and more productive, but only if you understand how to use it. The most important element in any digital workflow is the human interface between the dentist’s prescription, the manufacturing process, and the device that ends up in the patient’s mouth. That human interface is you and your team.
And finally, communicate! Advise your dentists of your intention to move to a digital workflow. You might want to switch to a fully digital workflow and at that point prefer to no longer accept analogue impressions, but stop and think. First, is your clinician already working with an intraoral scanner? If not, are they ready to invest the thousands that these scanners cost? A small modern laboratory scanner could be the answer, it can read an analogue impression

both buccally and lingually in the most detailed way, ready for the CAD stage of manufacture, so that your analogue dentist can still work with you, at least until they too see the digital light.
Have the courage to make the change, but first get your digital ducks in a row. It may seem daunting at first but this is the only way the industry is moving and nobody wants to see you get left behind while that train to the future fades away into the distance.

Over the last ten years, more and more dental professionals in the UK have started to adopt digital tools. In a growing number of laboratories, technologies like intraoral scanners, CAD/CAM software, and 3D imaging systems are now used to support everyday work for more precise results and a more efficient workflow and patient outcome. However, while some laboratories have already started the digital journey, many others still rely on traditional methods. Overall, there is a long way to go to fully adopt and integrate digital tools across the sector.
Digitalisation offers a valuable opportunity for dental laboratories: It has the potential to simplify work, reduce the time taken to complete cases and thus increases
Aims:
■ To explore the latest updates in digital developments
■ Keeping up-to-date with the digital workflow
■ Digital communication
CPD Outcomes:
■ Maintenance and development of knowledge and skill within your professional scope
■ Technical areas of study
■ Emerging technologies
■ Communication with the dental team
Development Outcomes: A&C
efficiency, improve communication between laboratories and clinics as well as with patients, and provide more accurate and consistent results. That is why, “the vast majority of UK labs have adopted – or are considering adopting – digital tools to a greater or lesser extent, whether it is a 3D printer used simply for model printing or a full digital workflow.,” says Jason Longden, National Sales Manager Laboratory, Henry Schein Dental UK.
This article looks at how dental laboratories in the UK are working nowadays, how digital tools are starting to transform the way they work, and what the future might look like. It also shares thoughts from industry professionals about what they believe digital workflows can offer for both dental laboratories and patients.
Digitalisation in dentistry is evolving rapidly. New and more sophisticated equipment and tools are appearing every year, contributing to the advancement of oral health and helping to improve patient care. The dental laboratory sector in the UK is no exception to this evolution and is also undergoing change. However, digitalisation in its broadest sense is still in the early stages for many laboratories.
There are over 1,000 dental laboratories registered with the Dental Laboratories Association (DLA) in the United Kingdom,1 with an estimated total of around 1,500 laboratories across the country in 2024.2 This number has decreased over the past decade, partly due to many laboratory owners reaching retirement age. Some of these businesses have closed, while others have been taken over by larger lab groups. As a result, the number of independent laboratories has

decreased, and a few larger players are becoming more visible in the market.
At the same time, expectations from dental practices are changing. Dentists and patients are in need for faster services, reliable results, and an overall improved experience. This is encouraging more laboratories to consider investment in digital tools. However, laboratories that fully benefit from complete digital workflows are still relatively uncommon.
There is also a difference between NHSfocused laboratories and private
laboratories in terms of digital adoption. Outside of some of the large volume or milling centre dedicated laboratories, a high number of NHS laboratory workflows remain analogue to one extent or another.
“Small labs that serve NHS practices often work with tight budgets. For them, moving to fully digital workflows needs to be done in steps, with a clear plan for how to use each tool and platform effectively.” Jason Longden.
In addition, a broad number of dental laboratories in the UK that have already started to incorporate digital tools still use a
mix of traditional and digital techniques. As a result, technicians often move back and forth between manual and digital steps to complete a single case.
One of the main drivers of digital adoption among dental laboratories appears to have been the increasing use of intraoral scanners (IOS) in dental practices. As more practices are moving away from traditional impressions and adopting digital scanning, laboratories are receiving more digital files, compelling them to adapt their processes accordingly.
Along with the rise of IOS, the increased availability of CAD/CAM technology and 3D printers has also encouraged this shift. The COVID-19 pandemic seemed to be an accelerator for the adoption of digital tools in the past years, as both clinics and laboratories looked for more efficient ways to treat cases with less physical contact.
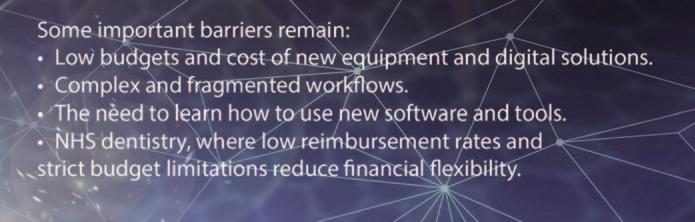
However, several barriers to digitalisation still remain.3 On the one hand, there are laboratories working primarily with the National Health Service (NHS), which need to focus more on high volumes and lower-
cost solutions, providing most of their services on an emergency basis. On the other hand, there are smaller laboratories with limited budgets and greater difficulty in incorporating new technologies – which ultimately impacts their ability to adapt and embrace digital transformation. In addition, there is a clear need for more innovation in certain workflows, such as the production of complete digital prostheses – a growing need among the older population.
Another challenge to overcome to drive the digitalisation of laboratories is the fragmentation and complexity of most current digital workflows. In addition, dental laboratory professionals need to stay up to date with the innovation and the use of new equipment and digital solutions which requires continuous education:
“Many dental practices and laboratories that have begun their transition often use multiple devices – frequently from different manufacturers – that are not seamlessly integrated. This makes it harder for dental professionals to work efficiently and fully benefit from these tools from a clinical perspective”., says Davide Fazioni, Vice

President, Global Dental Equipment & Service and Digital Workflow, Henry Schein.
Overall, the solution lies in developing both the technical and financial capacity to invest in new systems and training, given the current landscape of the sector in the country.
With an ageing population, the need for dental restorations – such as crowns, bridges, and full dentures – is expected to increase. This highlights the growing need for laboratories to deliver work quickly and accurately, and at an affordable cost. In response, digitalisation is increasingly seen as a way to meet these needs. As more laboratories explore and expand their use of digital tools, new opportunities are emerging that could reshape the profession.
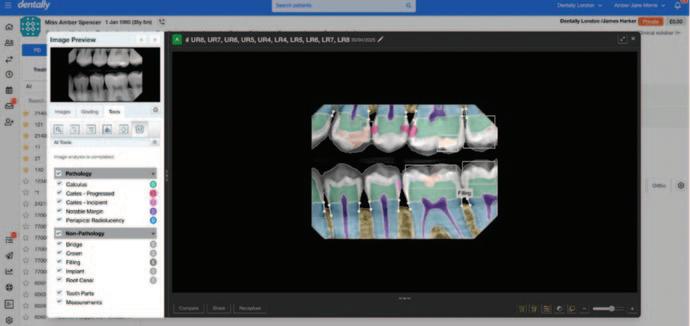
These technologies and materials can support laboratories in improving the quality of treatments, meeting deadlines more easily, and reducing costs. An additional advantage of going digital is that practices and laboratories can work more closely together. A dentist can send a scan directly to the laboratory, where a technician can start designing the case straight away. If both sides use compatible systems, the entire process – from scan to final restoration – can remain digital.
Digital workflows can also contribute to improving the patient experience, reducing the number of appointments by providing more predictable results compared to traditional analogue processes. This can also help enhance laboratory efficiency, increase chair utilisation at the practice, and reduce the environmental footprint by minimising transport needs and material waste. However, buying a machine is not enough. Even with these benefits, laboratories still need to plan digitalisation carefully, with the support of a knowledgeable and trusted partner who fully understands their needs and goals, as well as the opportunities available in the market and how to make the most of them to increase efficiency and improve results

When it comes to software, teams also must understand how to work with digital files, manage changes to workflow, and keep learning as the tools evolve. As an example, artificial intelligence (AI) is already starting to play an important role, and its impact is expected to grow over time. AI might help detect margins, suggest crown shapes, or check occlusion during the design process for dental experts. This could help save time and allow technicians to focus more on customising each case. To make that happen, dental professionals need to embrace continuous learning and collaboration.
“It’s not simply a matter of adopting the software. Practices and labs must consider how they collaborate, communicate, and adapt their workflows. Practice management software plays a critical role in this by connecting the entire practice team, streamlining processes, and ensuring information flows smoothly. That’s the key to making a digital workflow truly efficient and to delivering exceptional patient care,” states Ben Flewett, Vice President and Managing Director Henry Schein One International.
With the right elements in place – such as training, planning, and equipment – more dental laboratories in the UK could start benefiting from these advancements now and in the years ahead.
Looking ahead: What digitalisation can bring to laboratories and patients
Digital tools are gradually becoming part of the day-to-day work in dental laboratories. While most are not yet fully digital, many are taking significant steps toward adopting the technologies available in the market. Professionals need to identify the laboratory aims and thus the fitting tools that can support their workflows in an optimal way. In addition, it is crucial for the whole team to learn how to best use them in ways that improve efficiency and enhance patient care. This continuous effort is accumulative and, at the pace digitalisation in dentistry is evolving worldwide, many laboratories might be working mainly with digital equipment and tools.
Looking ahead, 3D printing and other advanced manufacturing solutions will continue to play an important role in the next phase of digital transformationespecially for crown and bridge fabrication, as well as for full digital denture workflows. These technologies could further streamline production, reduce material waste, and improve accuracy across more types of restorations.
Additionally, a key area shaping the future of digitalisation is the simplification and integration of systems. Many laboratories and practices today face the challenge of using multiple devices and software platforms that are not always compatible. This lack of integration often complicates workflows and limits the full potential of digital tools, but this will change in the near future.
“In order for customers to really use what they already purchased – or to invest in what they want to purchase – simplification is absolutely critical. We know that and we are working on the simplification of all the various software platforms dental professionals have to work with to be successful from a clinical perspective,” says Mackenzie Richter, Vice President, Global Commercial Digital Workflow Solutions at Henry Schein.

Simplification is about reducing complexity, but also about unifying fragmented digital processes into more connected, intuitive workflows. Integration across systems can help make everyday operations smoother, reduce the number of steps required, and ultimately benefit both laboratories and the practices and patients they support.
In the coming years, dental practices and laboratories will be able to access every element of the workflow – from the first appointment to the final step of treatment – through a single platform, thanks to greater connectivity between systems and equipment, regardless of brand or manufacturer.
This vision for the future includes seamless, centralised systems that digitally connect every stage of the workflow, tying together all aspects of a dental practice and laboratory. Such integration will offer laboratories the opportunity to work more efficiently, reduce turnaround times, and increase precision - ultimately improving operational efficiency and enhancing patient care.
However, achieving this will require more than just new tools and solutions, it will also depend on changes in how teams work, communicate, and adapt to new processes.
“We foresee a world in which the clinical team opens up practice management at the beginning of the day – and that is the one platform that you have to open.”
Mackenzie
Richter,
There may also be more opportunities for remote collaboration. As an example, a technician in one city could design a restoration that is then produced in another location. This increased flexibility could help laboratories expand their capabilities and support broader access to dental care, especially in communities or areas with less access to dental resources.
Dental laboratories in the UK are currently at a turning point. With continued investment in training, planning, and equipment – together with the
simplification and fully seamless integration of digital systems in the near future – the transition to full digital workflows could help laboratories evolve and thrive. This digital transition is about integrating new technologies, as well as about redefining the role laboratories will play in the dental industry.
As digital integration grows, laboratories might take on more strategic roles in treatment planning and patient care. Those who embrace it with a wellthought-out plan will be better suited to stay competitive, enhance collaboration with clinics, and provide high-quality service to patients. Ultimately, those who take the right first steps today will lead the way and help shape the future of laboratories as key contributors to improved oral health tomorrow.
1 https://dentallaboratory.org.uk/dentures/dentallaboratories-association/?utm_source=chatgpt.com
2 https://rentechdigital.com/smartscraper/businessreport-details/list-of-dental-laboratories-in-unitedkingdom
3 Committee of Public Accounts – “Fixing NHS Dentistry” report. https://committees.parliament.uk/publications/ 47347/documents/245396/default/

Development Outcomes A&C – 60 minutes
To complete your CPD, store your records and print a certificate, please visit www.dta-uk.org and log in using your member details.
Q1 How many dental laboratories are estimated to be in the UK?
A 1800 B 2300 C 1500 D At least 1000
Q2 What is said to be causing a decrease in the number of dental laboratories?
A Owners reaching retirement age
B More clinics with in-house CAD/CAM
C Some businesses taken over by larger groups
D a) and c) only
Q3 In the article, what is said to be different about NHS focused laboratories?
A They remain analogue to one extent or another
B They are largely single person businesses
C They are often based in a hospital or practice
D They use cheaper materials
Q4 Name one of the main drivers of digital adoption.
A More digital equipment coming onto the second-hand market
B The increased use of intraoral scanners in dental practices
C Computer-savvy students coming into the profession
D Better financial planning
Q5 Why was the COVID-19 pandemic considered an ‘accelerator’ for the adoption of digital tools?
A More people were working from home
B Technicians had more time to study the new technology
C Training was more accessible online
D Clinics and laboratories looked for more efficient ways to treat cases with reduced physical contact
Q6 What is specifically described as a growing need among the older generation?
A Faster treatments with less chair time
B A more aesthetic treatment outcome
C Complete digital prosthesis
D More affordable dental devices
Q7 ‘Fragmentation’ and what is recognised as a challenge to be overcome in most current digital workflows?
A Complexity
B Incompatible technology
C Fake materials
D Poorly translated user manuals
Q8 How can the digital workflow reduce dentistry’s environmental footprint?
A Minimise transport needs
B Reduce material waste
C Reduce the power needs of the laboratory
D a) and b) only
Q9 Which of the following is NOT cited as an impact of AI in the dental laboratory?
A Predict the development of dental caries
B Detect margins
C Suggest crown shapes
D Check occlusion
Q10 What did Mackenzie Richter describe as ‘absolutely critical’ for customers to use what they already purchased, or invest in what they want to purchase?
A Training
B Ongoing provider support
C Simplification
D A fully integrated digital dental workflow

by AD Griffin, MBE. DTA Treasurer

Aims:
■ To better understand the legal and registration requirements for manufacturing custom-made dental devices in the UK
■ Keeping up-to-date with GDC and MHRA law
■ Effective business management
CPD Outcomes:
■ Maintenance and development of knowledge and skill within your professional scope
■ Ethical and legal issues and developments
Development Outcome: B,C&D
Many members of the Dental Technologists’ Association (DTA) are concerned about what appears to be in-clinic manufacturing of custom-made dental devices which does not abide by current regulatory requirements. In trying to maintain a level playing field with regard to regulatory compliance, the DTA – as a professional body – continues to provide guidance to its members and raise awareness of regulations to all professional bodies responsible for the UK manufacturer of these custom-made dental devices.
According to current regulations, in order for manufacturers of custom-made dental devices to legally comply – from the inclinic manufacture of anything from a bruxism splint to a crown – by law, requires registration with the Medicines and Healthcare products Regulatory Agency (MHRA) and also requires the manufacturer to provide each patient with a statement of manufacture for each device. This relates not only to the manufacture of dental
devices in the UK but also to the importation of dental appliances from overseas, more of which later.
This statement of manufacture provides details about the device, including the manufacturer’s address, their MHRA reg number, that it’s intended use is for a specific patient, and a confirmation that it conforms to relevant standards and a registrant clinician’s prescription. It also details the materials used. The clinician who prescribed the appliance is responsible for making the patient aware of this statement and must provide it upon request.
But who should comply with the MHRA registration requirements, and are there any exceptions? Some have suggested that clinicians are exempt from registration with MHRA, as they hold the view that their own in-clinic milling is not manufacturing but rather, as per the previous MDD regulation, ‘...adapt(ing) devices already on the market to their intended purpose for an individual patient’.
Put simply, by law, this cannot be the case. The manufacturer is not exempt just because the manufacturing occurs in the dental clinic. The DTA has consistently lobbied the GDC, governments and other professional bodies with regard to this issue saying that, as it is for dental laboratories, such in-clinic fabrication should always be regulated by the MHRA. If MHRA registration is necessary for registered dental technicians, then surely it must be the same for dentists manufacturing in their clinics.
The GDC has also presented papers to indicate that compliance with the MHRA is an essential requirement for custom-made dental devices in the UK. These requirements are made very clear in the Standards for the Dental Team 2013. GDC publication. Standard 1.9.1
It states that: If you make a dental appliance, whether you are a dental technician, dentist, or any other registrant, you must understand and comply with your legal responsibilities as “manufacturer” under the Medical Device Regulations (MDR). (ref GDC published ‘Guidance on Commissioning and manufacturing dental appliances’.) This includes the legal requirement to register with the Medicines and Healthcare products Regulatory Agency (MHRA).
If you prescribe a dental appliance to be made by a person in the UK who is not a registered dental technician, you may put your registration at risk. Equally, you may put your registration at risk if you receive a dental appliance made in the UK by a person who is not a registered dental

technician. The signing off of an appliance as fit for the market by a registered dental technician assumes that they can trace by audit the manufacturing processes and that the materials used within that process are appropriate for oral cavity use.
If you decide to either sub-contract the manufacture of a dental appliance or use a dental laboratory or agent which sources dental appliances from outside the UK you take on additional responsibilities. These include a responsibility to ensure that the manufacturer or their authorised representative has complied with all relevant obligations in the UK Medical Device Regulations (MDR).
So, every GDC registrant that manufactures custom-made dental devices is required to register with the MHRA and provide the patient with the statement of manufacture, and the DTA will continue to indicate that this should continue to be seen as an oral healthcare team opportunity to work within
the law and showcase the dental laboratories’ essential role in oral healthcare.
For those who are still sceptical, then maybe the extracts from the NHS Business Authority2 will make interesting reading. See Figure 1 below
A further interesting requirement of the NHS appears later in this page,3 providing direct clinician advice on their in-house milling of custom-made dental devices (see Figure 2 overleaf ). There cannot be one requirement for NHS appliances from dental laboratories and a legal case for non-compliance for private/independent dentistry in-clinic manufacturing. It’s all manufacturing of custom-made dental devices and requires the manufacturer to register with the MHRA.
Further guidance is also provided by the government to clinicians needing to register with the MHRA because they are manufacturers of custom-made dental devices by milling in-clinic or other such manufacturing methods.4 The link provided is to GOV.UK advice on how to Register medical devices to place on the market.
It states: You must register5 if you or your company sells, leases, lends or gifts:

A Class I, IIa, IIb or III devices you have manufactured
A Class I, IIa, IIb or III devices you have refurbished or re-labelled with your own name
A Any system or procedure pack containing at least one medical device
A Custom-made devices
A IVDs you have manufactured
A IVDs undergoing performance evaluation
It is quite plain manufacturing of Custommade dental devices requires MHRA registration. It is the law, and registrants need to know that this “affect(s) your work and they need to follow the requirements...” (Standard 1.9).
Within the GDC document on custommade dental devices that require registration, the Council clearly defines a range of dental appliances that they describe as manufactured, ‘mainly outside of the mouth’. The GDC then provides a range of examples, including fixed bridges, bleaching trays, crowns, splints, retainers, etc., that they regard as custom-made dental device manufacturing, thus requiring by law for the manufacturer to register with the MHRA.
Likewise, the GDC indicates that a clinician who accepts dental appliances made in the UK by an unregistered dental technician or a dental laboratory not registered with MHRA may also put their registration at risk. The Standards for the Dental Team, standard 1.9 clearly states that as a registrant ‘You must find out about laws and regulations affecting your work and follow them’.
And finally, with regard to registrants signing off on overseas manufactured custom-made dental devices it can be impossible to verify the materials used in manufacture and the UK registrant – dental
technician or dentist – is legally liable for any problems that might result from say, an allergic reaction to alloys used in the device once placed in the patient’s mouth.
It is best to source from trusted suppliers with reputable and traceable manufactures sources. Cheap probably means suspect materials from which you could be manufacturing and then signing off custom made dental devices and for which you will be taking responsibility. This is also something that GDC registrants should be indemnified or insured to carry out.
Keeping up-to-date with such MHRA regulations is something we all as registered professionals need to do, while those wider attributes of professionalism includes displaying honesty and ethical behaviour. Within the education sector of Oral Healthcare team of professionals an updated requirement has been introduced from 2025 by the GDC called ‘Safe Practitioner – Framework’ 6 This outlines for students a range of attributes that professionals should show such as P1.12 ‘Describe the responsibility that dental practices and individual practitioners have in compliance with legal and regulatory framework’ therefore all team members are expected to know about the legal requirements and in particular for dental technicians the manufacturing of custommade dental devices under MHRA (UK MDR).
Regarding Medical Devices Regulations (MDR) which came into force 26 May 2020. Since 26 May 2021, the EU Medical Devices Regulation (Regulation 2017/745) (EU MDR) has applied in EU Member States and Northern Ireland. As these EU regulations did not take effect during the transition period, they were not EU law automatically retained by the EU (Withdrawal) Act 2018 and therefore do not apply in Great Britain. Therefore, refer
to the UK MHRA MDR regulations for custom-made dental devices.
A Please get in touch if you have any queries relating to this article, email info@dta-uk.org
1 Standards for the Dental Team 2013. GDC publication. Standard 1.9 https://www.gdc-uk.org/docs/defaultsource/information-standards-and-guidance/guidancedocuments/guidance-on-commissioning-andmanufacturing-dental-appliances79b4ee91c3a64f 12b5772a26dec28601.pdf?sfvrsn=9463dd00_10#:~:t ext=From%2026%20May%202020%20the,comply%2 0is%20a%20criminal%20offence Accessed June 2025.
2,3 NHS Business Authority. https://faq.nhsbsa.nhs.uk/ knowledgebase/article/KA-01757/en-us Accessed June 2025
4 https://www.gov.uk/guidance/register-medical-devicesto-place-on-the-market
5 https://www.gov.uk/guidance/register-medical-devicesto-place-on-the-market#who-must-register
6 The Safe Practitioner: A framework of behaviours and outcomes for dental professional education - Dental Technician https://www.gdc-uk.org/docs/defaultsource/education-and-cpd/safe-practitoner/spf-dentaltechnician.pdf?sfvrsn=75edb41e_3

To complete your CPD, store your records and print a certificate, please visit www.dta-uk.org and log in using your member details.
Q1 What is the MHRA?
A Manufacturers and Healthcare Regulation Agency
B Manufacturing for Healthcare Registration Agency
C Medicines and Healthcare products Regulatory Agency
D Medicine and Healthcare providers Regulation Agency
Q2 What does the Statement of Manufacture include?
A MHRA registration number
B The materials used
C Manufacturer’s address
D All of the above
Q3 Are clinicians exempt from registration with MHRA?
A Yes, they are adapting devices already on the market
B Yes, they are providing devices for a specific patient, not the general market
C No, by law this cannot be the case
D It is not clear, the regulation requires clarification
Q4 In the GDC Standards for the Dental Team, where is it made clear that a manufacturer has a legal requirement to register with the MHRA?
A Standard 1.9
B Standard 1.5
C Standard 1.7
D Standard 1.6
Q5 The signing off of an appliance assumes that the manufacturer can trace by audit the manufacturing processes, and what?
A That the device was manufactured by a GDC registrant
B The materials used are appropriate for oral cavity use
C That the device will be placed into the named patient
D That the device was manufactured to a registrant’s prescription, and all of the above
Q6 Are dental devices manufactured outside the UK exempt from regulation?
A Yes if they are made in the EU
B Yes if the manufacturer resides in one of six specific countries
C No, the sub-contractor must ensure the appliance complies with UK MDR requirements
D If the UK registrant is happy with the appliance they can sign it off.
Q7 What direct requirement regarding inclinic milling is demanded by the NHS?
A Practices producing such restorations must register with MHRA
B The manufacture of such restorations requires at least six-months training
C Such restorations can be manufactured by any member of the dental team under proper supervision
D Such restorations require a Statement of Manufacture
Q8 Does the in-house milling requirement by the NHS impact private/independent practices?
A No, the NHS has its own rules
B Yes, there cannot be one rule for the NHS and another for private practice
C No, independent practices are under separate requirements
D No, not if the device has specifically been made for an existing patient
Q9 The Government states that manufacturers must register with MHRA if they provide, what?
A Class I, IIa or III devices they have manufactured
B Any system or procedure pack containing at least one medical device
C Custom-made devices
D All of the above
Q10 Is not knowing about the MHRA regulatory requirements a valid excuse for not registering, as some clinicians think?
A Yes, they have enough to think about
B Clinicians are amongst the most regulated professions in healthcare, they can be trusted to act ethically at all times
C Yes, it is the regulator’s job to inform them
D No, all team members are expected to know about their legal requirements

■ Stress Part I – What is it and how does it affect us?
Tracey O’Keeffe, Coach Practitioner and Mindfulness Teacher MA (Education), BSc (Critical Care), RN, MAFHP, MCFHP
This paper, and a second one to follow, will explore stress and how we can mitigate against the damaging effects it can have on our minds and bodies. Stress is something most people can relate to and will have experienced in their lives. Indeed, Ghasemi et al. (2024, p.1) state it is “an inevitable aspect of human existence”. The world today operates as a fast-paced and pressured environment for many, and the levels of stress are rising and becoming more evident throughout the population (Candeias et al. 2024). Understanding what stress is, what can trigger it, and how we can respond rather than react may be instrumental in preventing some of the long-lasting and potentially damaging effects it can have on an well-being (Yaribeygi et al. 2017).
A seminal piece of work about stress is that of Selye (1956) who explained it as a physiological response to both physical and psychological stimuli. Charmandari et al. (2005) suggest that those stimuli may be exposure to pathogens, physical harm or chemical imbalances, although it is also acknowledged that stress can be triggered by any sort of tension, worry, or a difficult situation (World Health Organisation 2025). Essentially, anything that poses a threat or disrupts the equilibrium of the body manifests as stress and a need for the body to return to stability and balance (Ghasemi et al. 2024).
The word “stress” often brings to the mind negativity, and from the definitions and explanations above, it would seem that it predominantly brings problems. However, Seyle (1965) described it as a non-specific response from the body in order to create

change from an existing state. The Stress Curve is a well-known model based on the work Yerkes and Dodson (1908) which considers when stress moves through a positive motivating force to a negative influence (see Figure 1). What the curve shows is how positive stress, or “eustress”,
enables us to reach our optimum performance levels. Becoming “distressed” however, with an overload of stress, tips us over the brow of the curve and into possible burnout. In essence, rather than always detrimental, some degree of stress can be a stimulus for action, results and necessary

adjustment. Stress stems from the need to respond to a situation with the body activating the sympathetic nervous system into “fight or flight” mode.
Neurotransmitters and hormones (such as adrenaline and cortisol) are released which transforms the body into a state of alertness. The body senses the stress stimulus as something which needs challenging (“fight”) or something to flee from and run (“flight”). The analogy often used here is the concept of a caveman fighting a sabretooth tiger. If the body needs this physical capability, the changes within the body are useful and productive. However, if the reaction is due to a perceived but non-life threatening situation, the stress response can continue to elevate and create on-going issues (Harvard Health 2025), which will be discussed in more detail later. Stress triggers or determinants may be short-term, discrete situations or they may more long-standing historical events and experiences (Harvard Health 2025; Schneiderman et al. 2005) (see Figure 2). The variety and scope is vast, and it is worth noting that positive events such as marriage, promotion, childbirth, although not included in Figure 2, can also create stress for an individual as they adjust to change and altered personal perception and responsibility.
As shown in Figure 2, stress may be shortlived, transitory and necessary or it can remain with someone for a longer sustained period. Acute stress is usually not damaging and can in fact be beneficial. Mifsud and Reul (2018) suggest that enables further damage to the body to be prevented such as in the case of trauma or surgery. Similarly, if preparing for a particular event (such as an exam or interview) a small amount of stress can actually help with performance and alertness (as in Figure 1) (World Health Organisation 2025). However, if the acute stressor is repetitive or if it is a chronic

situation, then the health burden can increase resulting in physical and psychological problems, depending on the person’s individual situation (Schneiderman et al. 2005). If the “fight or flight” continues without moving into a recovery phase, an exhaustion stage can result leading to burnout, anxiety, and reduced stress tolerance (Seyle 1950) as well as physical health problems (Yaribeygi et al. 2017; Hasin et al. 2023; Ghasemi et al. 2024). Sometimes this can be considered as the “freeze” response where there is a level of disengagement and incapacity to act, almost as a protective factor. This is
ultimately related to physical changes within the body and the subsequent maladaptive response.
The way the body reacts to a stressful stimulus is a complex series of changes and processes involving many body systems (Carrasco and Van de Kar 2003) instigated by the autonomic nervous system (Tortora and Derrickson 2017). As well as this, there are behavioural modifications. Initially, the cardiovascular system prepares for an
emergency situation, increasing heart rate and increasing vasoconstriction in certain areas of the body. This enables oxygenated blood flow to be directed to the cardiac and skeletal muscles (for action) and the brain (for alertness). The respiratory rate also increases to match the perceived demand for oxygen (Harvard Health 2025). This activation of the sympathetic nervous system is effective when needed and it can be felt in the body with the heart racing, the breath quickening and a state of heightened arousal. Usually it is then followed by the parasympathetic nervous system coming into play once the stressor has resolved (Ulrich-Lai and Herman 2009). This reversal or “rest and digest” phase sees the slowing of the heart rate and respiratory rate with a reducing blood pressure. The circulation returns to areas such as the gut so that body can renew stores of energy. Equilibrium overall is restored.
Longer term and unrelenting stress responses in the body can result in health conditions relating to many body systems, both physical and mental, as well as behavioural adaptations or manifestations (see Figure 3). Schneiderman et al. (2005) also suggest that the more intense and severe the stressor, the greater response. This is also matched with a sense of control; the less control a person feels they have, the greater the effect of the stress on them.
As well as potential changes and risks noted in Figure 3, people may experience musculoskeletal problems like neck and back pain caused by tension (Umann et al. 2019). This can often be work-related, exacerbated by manual work or from poor posture and sedentary challenges. Psychological changes also often manifest as anxiety and depression which may be short-term or enduring (Ghasemi et al. 2024).
As a final discussion point, it is worth reenforcing that stress cannot be seen as an
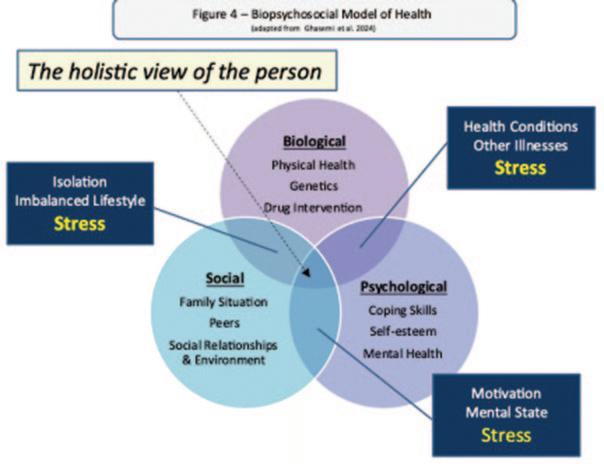
isolated phenomenon. It interacts with the individual from a biopsychosocial perspective both in terms of its origin and its solution. The biopsychosocial model of health is well-documented and utilised through healthcare, and Figure 4 demonstrates how stress as a concept sits within it. Stressors can come from biological, psychological and/or social contexts. Similarly, the way they are managed or mitigated against, can come from those three stances and each approach will vary in effectiveness for each individual situation. Indeed, Robinson (2018) notes the complexity of stimulus, appraisal and response. Stress is multidimensional and cannot be examined or solved away from the context of the situation.
Stress is inherent in life and it can be difficult to navigate through. Although our body is designed to respond in an appropriate way, the stressors we experience in day-to-day life may not warrant that response. Repetitive acute stress or long-term chronic stress can result in potentially damaging physical changes as well as maladaptive thought processes and behavioural approaches. Understanding possible management strategies is key to coping and they can be developed through self-awareness and a variety of different mechanisms which will be discussed in the next paper.
Candeias, A. A., Galindo, E., Reschke, K., Bidzan, M. and Stueck, M. 2024. Editorial: The interplay of stress, health, and well-being: unravelling the psychological and physiological processes. Frontiers in Psychology. 15. 1-4. DOI=10.3389/fpsyg.2024.1471084
Carrasco, G. A. and Van de Kar, L. D. 2003. Neuroendocrine pharmacology of stress. European Journal of Pharmacology. 463. 1. 235-272
Charmandari, E., Tsigos, C., and Chrousos, G. 2005. Endocrinology of the stress response. Annual Review of Physiology. 67. 259-284
Ghasemi, F., Beversdorf, D. Q., and Herman, K. C. 2024. Stress and stress responses: A narrative literature review from physiological mechanisms to intervention approaches. Journal of Pacific Rim Psychology. 18. 120. DOI: 10.1177/18344909241289222
Harvard Health. 2025. Stress. [online] [accessed 27.6.25]. Available at: Identifying and relieving stress - Harvard Health

Hasin, H., Johari, Y. C., Jamil, A., Nordin, E., and Hussein, W. S. 2023. The Harmful Impact of Job Stress on Mental and Physical Health. International Journal of Academic Research in Business and Social Sciences. 13. 4. 961-975
Mifsud, K. R. and Reul, J. M. H. M. 2018. Mineralocorticoid and glucocorticoid receptor-mediated control of genomic responses to stress the brain. Stress. 21. 5. 389-402
Nickerson, C. 2023. The Yerkes-Dodson Law of Arousal and Performance. [online] [accessed 28.6.25]. Available at: The Yerkes-Dodson Law of Arousal and Performance
Robinson, A. M. 2018. Let’s talk about stress: History of stress research. Review of General Psychology. 22. 3. 334-342. https://doi.org/10.1037/gpr0000137
Scheiderman, N., Ironson, G., and Siegel, S. D. 2005. Stress and Health: Psychological, Behavioural, and Biological Determinants. Annu Rev Clin Psychol. 1. 607-628.
doi:10.1146/annurev.clinpsy.1.102803.144141
Seyle. H. 1950. Stress and the general adaptation syndrome. British Medical Journal. 1. 4667. 13831392
Seyle, H. 1956. The stress of life. New York; McGraw-Hill
Seyle, H. 1965. The stress syndrome. The American Journal of nursing. 65 (3). 97-99
Tortora, G. and Derrickson, B. 2017. Tortora’s principles of anatomy and physiology. 15th edn. Singapore; John Wiley & Sons
Ulrich-Lai, Y. M., and Herman, J. P. 2009. Neural regulation of endocrine and autonomic stress responses. Nature Reviews Neuroscience. 10. 6. 397–409. https://doi.org/10.1038/ nrn2647
Umann, T., Jager, M. and Lutticke, J. 2019. Job stress as a risk factor for musculoskeletal disorders in healthcare workers: A systematic review and meta-analysis. PloS One. 14. 6. e0216857
World Health Organisation. 2025. Stress. [online] [accessed 28.6.25]. Available at: Stress
Yaribeygi, H., Panahi, Y., Sahraei, H., Johnston, T. P., and Sahebkar, A. 2017. The impact of stress on body function: a review. EXCLI Journal. 16. 1057-1072. http://dx.doi.org/10.17179/excli2017-480
Yerkes, R. M. and Dodson, J. D. 1908. The relation of strength of stimulus to rapidity of habit-formation. Punishment: Issues and experiments. 27-41.
Kevin Lewis
■ To explain the nature of choice and how/why we make decisions in different circumstances
■ To explain how we are predisposed to make certain choices, without realising this
■ To provide practical illustrations of the consequences of the choices we make and how instinctive choices can have serious implications
CPD Outcomes:
■ Effective communication with patients, the dental team and others across dentistry, including when obtaining consent, dealing with complaints, and raising concerns when patients are at risk
■ Effective management of self and effective management of others or effective work with others in the dental team, in the interests of patients; providing constructive leadership where appropriate;
[Effective practice and business management]
■ Maintenance and development of knowledge and skill within your field of practice; Clinical and technical areas of study: Emerging technologies and treatments
■ Maintenance of skills, behaviours and attitudes which maintain patient confidence in you and the dental profession and put patients’ interests first.
[Professional behaviours]
This article looks at some of the many choices we face in our personal and professional lives, and illustrates that most or all of the choices we make have a legal and/or ethical dimension, and often, professional and human consequences. Many of these consequences are not immediately apparent, nor uppermost in our mind, at the moment when we are faced with these choices.
Choices are not always binary, ie selecting one of two possible options. In many cases there are several choices. Sometimes one option is doing nothing or taking no active step to take a different course; infact that is still a choice. Some choices have to made in a split second, while others allow more time

to weigh up the options and perhaps explore new options that you weren’t previously aware of.
Three years ago, in an earlier article in this series on Legal and Ethical issues,1 we looked at the essential ingredients of professionalism. For the benefit of those who didn’t see or read that article (and for the convenience of those who did), a key section of that text is reproduced below :-
If you were to ask different people to describe a professional person, you are likely to get a range of answers (depending on who you ask). But the descriptions would probably include things like
A They are members of an acknowledged profession (accepting that the scope of this definition has widened over the years)
A They have a special level of training, knowledge and skill in their particular field
A They have achieved some kind of recognised professional qualifications
A They are good at what they do in their chosen professional field
A They enjoy an above-average level of status, respect, confidence and trust within society
But if you were then to ask those same people what was meant by ‘behaving professionally’, the focus of the description might shift away from proficiency, knowledge and practical skill levels , towards things such as
A They are principled and ethical
A They act with integrity
A They have respectable human values and maintain appropriate standards of behaviour
A They show respect for others, and their rights and dignity
A They honour the commitments they make, and take a pride in what they do
A They respect and follow the law
A They take responsibility for their actions
A They continually seek to develop, learn and improve themselves
A They demonstrate their understanding of, and their respect for, professional boundaries, ie attitudes and behaviours that are unacceptable in the context of their professional life – even if they might be acceptable in their private/personal life
There is an inherent perspective bias surrounding professionalism: those within a given profession might have a different understanding to those on the receiving

end of their professional services. Those who (perhaps by virtue of not having completed the necessary training and/or obtained the relevant qualifications) sit outside the ‘inner circle’ of the profession and/or are resentful at being excluded from it, might become disaffected or even motivated to question or undermine that exclusivity or chip away at its edges. Third parties like regulatory bodies (eg the GDC)
might have different views again and apply and enforce incongruous expectations that coincide neither with those of the providers nor the recipients of the professional service being regulated. Meanwhile funders and commissioners of services, are likely to have a very specific agenda – perhaps in the hope of securing the delivery of a service with a semblance of professionalism and all its potential benefits, without actually having to pay a premium for them.

The wisdom of hindsight will be familiar to all of us. Reflecting after the event upon whether we, or someone else, has made a sensible choice, is informed by knowing what happened as a result of that choice –and whether there might have been a different outcome, had a different choice been made. Any and every party comes to this discussion with a personal viewpoint and perhaps bias, which reflects their own individual value system. There may be subjective skews and conflicts in arriving at that view, which the individual may or may not be aware of.
All this in turn is a product of all the experiences of their lifetime from their early childhood, through all stages of their education, into their adult and working life. By that stage it has been influenced by family, teachers, peers and third parties of many different kinds (and in many cases a mix of both positive and negative influences) and there is a fascinating debate to be had regarding whether these values and
Figure 1: The text reproduced below is extracted from the GDC’s Guidance Standards for the Dental Team, these extracts having been chosen for the specific purpose of this article. To place this statement in its correct, original context you should refer to the full text of the Guidance.7
Standard 1.7: You must put patients’ interests before your own or those of any colleague, business or organisation
Principle 9 – Make sure your personal behaviour maintains patients’ confidence in you and the dental profession
Patients expect: -
– That all members of the dental team will maintain appropriate personal and professional behaviour
– That they can trust and have confidence in you as a dental professional
– That they can trust and have confidence in the dental profession
opinions are already so deeply ingrained by the time one completes any professional training and enters the profession, that it is unrealistic to expect that they can be reversed or materially modified in midcareer. This is of course a recurring question that occupies the mind of the GDC and its Professional Conduct Committee when considering whether a registrant’s failings are remediable, and if so, over what timescale.
Various pieces of research in recent years2,3 have shown that patients attach a lot less significance to things that the regulator (and to a lesser extent, the profession itself) had considered important. Also, for members of the public, the whole point of using the services of a professional person was that you could rely upon receiving care and treatment of an appropriate standard /quality – it was a ‘given’. Members of the public related much more readily to the question of whether or not the specific person treating or caring for them was ‘professional’ in the way they did it, than to any awareness or consideration of ‘professionalism’ as a broader concept. That in itself might prove to be quite an important distinction, because the reasons why somebody might raise a complaint about a dental health professional, might then be poorly aligned with the criteria that a regulator (like the GDC) might apply when investigating that complaint.
You must:
9.1 Ensure that your conduct, both at work and in your personal life, justifies patients’ trust in you and the public’s trust in the dental profession
9.2 Protect patients and colleagues from risks posed by your health, conduct or performance
9.3 Inform the GDC if you are subject to criminal proceedings or a regulatory finding is made against you anywhere in the world
9.4 Co-operate with any relevant formal or informal inquiry and give full and truthful information
The demands and expectations of any healthcare profession are necessarily different from those which might apply in other professions (such as the law, teaching, religious/faith leaders or professions such as accountants, architects, surveyors etc). Different qualities assume different levels of importance in different professions. For patient-facing roles, qualities such as compassion, kindness, caring and empathy are obviously essential, but attention to detail and an unwillingness to cut corners is equally crucial in non-patient-facing roles, as is an awareness of and attention to patient safety issues, including infection control and the responsible management of clinical and other hazardous waste. There are other underpinning principles which are shared by all kinds of professions – not least that of the paramountcy of the client/customer/patient. The principle of paramountcy is fundamental to any professional relationship and it means acting in the best interests of the client/customer/patient and placing that principle above all other considerations (whether of self-interest – commercial or otherwise - or the wider interests of employers). Without paramountcy - and by extension, unwavering respect for others and their rights – a profession cannot expect to enjoy the trust and confidence of
the public. That trust and confidence is not a right : it needs to be earned, cultivated and maintained collectively through the actions and behaviour of every individual member of the profession (see Fig 1).
An example of a fundamental tenet of this trusting relationship is the principle of ‘professional confidentiality’ and it is interesting that this is still particularly associated with the three original learned professions of mediaeval times – the Church, Medicine and the Law. The absolute confidentiality of information shared within the confines of the confessional, the consulting room/surgery, the solicitor’s office and the barrister’s chambers endures to this day.
Dentistry has inherited many of the founding principles of medicine, including this one. But the word ‘professional’ is also used as an adjective in fields far removed from healthcare, dentistry and dental technology, to describe doing something well - or consistently, dependably well. We would be mightily disappointed if the members of our national defence forces were not highly trained professionals in this sense. Painters and decorators, plasterers, plumbers and electricians might all do ‘a professional job’, and (paradoxically) footballers might even take pride in their ability to commit a ‘professional foul’ –
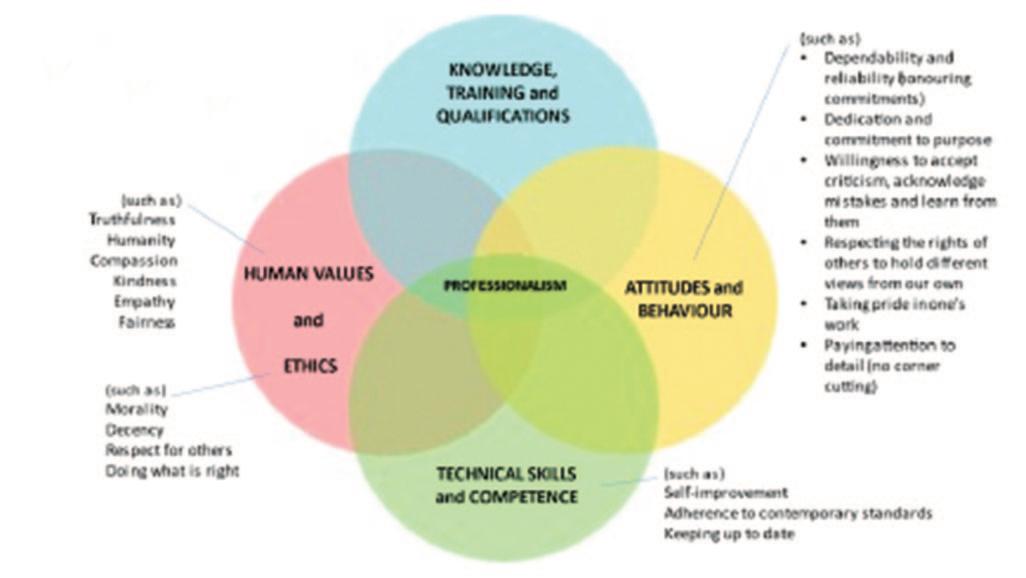
especially if they can get away with it undetected by match officials and/or VAR.
So while ‘professionalism’ might still seem an elusive and intangible concept, we are starting to tease out some elements of professionalism which are likely to sit at the heart of the choices we make. For the purposes of this discussion and ease of understanding, we might represent some of these fundamental ingredients diagrammatically (see Fig 2).
It is significant that they are represented here as four overlapping circles because none of these elements of professionalism are sufficient in isolation; there needs to be a reasonably balanced combination of all four of the elements, all of the time, because patients deserve and expect not just occasional glimpses of our professionalism - nor of the parts of it that we consider to be the most important - but the rounded totality of it. Indeed, other members of the dental team also rely upon that in their dealings with us. Being the most highly trained and qualified, and/or


most technically gifted and talented dental technologist in the universe counts for little if you have days when you are prepared to cut corners or can’t be bothered, or if you are likely to do something improper, unethical or illegal and have no insight as to why this matters. Or why your actions might bring the profession into disrepute and/or lower public confidence in dental technologists generally – and why that matters too.
Professionalism is not just a question of knowledge, training and qualifications or of being admitted to a de-facto “club”. It is a lot more nuanced than that, and manifests itself in terms of what we do, how (consistently) well we do it, and how we do it at a human level - and in the widest possible sense. But nor is professionalism binary; an individual may act unprofessionally on a particular occasion, but this is not necessarily indicative of their professionalism – or lack of professionalism – more generally. It is in that sense a careerlong journey during which we develop, enhance and fine-tune our professionalism.
Once professionalism becomes a habit, the choices we make in our private and social life will be better and more consistent. We can be relied upon to do the right thing, simply because it is the right and proper thing to do.
This is a convenient moment to remind ourselves that as a GDC registrant, the margin between our professional and personal life is somewhat blurred because the GDC can investigate any personal conduct that brings the profession into disrepute or otherwise raises concerns about a registrant’s fitness to practise. Minor motoring offences are a rare example of a criminal offence that doesn’t need to be self-reported to the GDC.4
Many factors can affect the quality of the work we carry out. Some people take an exceptional pride in their work, while others might be more prone to cut corners when they are under time pressure, or are tired or not feeling 100%, or distracted by other life
events. Here again, setting high standards and not being content with compromise or second-best is a core aspect of professionalism.
The culture of our workplace can also be important in encouraging us to pursue high standards even on the days (and especially on the days) when we don’t feel like making the extra effort and/or going the extra mile. A robust quality assurance and perhaps peer review structure can also deter the risk of corner-cutting and compromise.
A good leader/manager/business owner/employer will know which team members can and cannot be relied upon to deliver 100% whatever the pressure and whatever the circumstances.
In a previous article in this series we looked at CPD5 and the significance of the CPD choices we make. Some courses are selfevidently more about making money and maximising profits, than about pursuing quality, raising standards and selfimprovement. It is supposedly a central feature of the GDC’s approach to CPD that it is left to each individual registrant to decide what CPD they need at any moment in time (guided by their Personal Development Plan) and where, and from who, and in what format, to seek that training. It is all personal to the registrant, we are told.
But fast forward to a Professional Conduct Committee and it’s not personal any longer. Many in the profession view the GDC’s CPD requirements as a ‘distress’ activity – it’s got to be done, like it or not, so they will look for the cheapest, easiest, least demanding way to tick the relevant boxes. On the other hand, there are those who commendably invest a huge amount of time, energy and effort, money and commitment into their continual personal development.
Some registrants who for whatever reason have left it very late to complete their

minimum CPD requirement, have been shown to be completing 20 hrs a day of online courses, sometimes with several online courses running at the same time. This is not only very revealing as to the registrant’s underlying commitment to, and attitudes towards, CPD – it also introduces more serious concerns about the registrant’s honesty.
In 2014, Professor John Adams received the Lifetime Achievement Award from the Institute of Risk Management. A quarter of a century ago he wrote “Risky Business” for the Adam Smith Institute6, in which he had suggested that one can predict risk
behaviours by looking at an individual’s attitude to risk and the personal “risk thermostat” that each of us owns. He describes the concept of “virtual risks”, where in the absence of known, solid scientific evidence about given risks, individuals are at the mercy of their own judgments and attitudes, and their predispositions to view whatever evidence is available, in particular ways.
Adams (see diagram above) describes a “four-fold typology” of these predispositions. The terminology may seem unfamiliar, but it is the terminology he chose:
INDIVIDUALIST - a cheerful optimist who believes that if you can’t prove it’s
dangerous you can assume that it’s safe. He believes that science provides solutions and is confident in his ability to fix things after the event.
EGALITARIAN - a worried, cautious pessimist who believes that in a risky world, unless you can prove that it’s safe, then you should assume that it’s dangerous. He also believes that science creates new risks and there will always be unseen risks that you don’t know about.
HIERARCHIST - believes that all risks can and should be understood, quantified and managed. He doesn’t like uncertainty, so he looks for evidence, demands information, systems and processes and measurement in order to gain as much control as possible over risk and uncertainty.
FATALIST - a pragmatist who feels powerless in the face of forces that he feels unable to control. What will be, will be - and the best you can do is keep your eyes open, duck if you see something about to hit you and accept that bad stuff happens sometimes, whatever you do.
It is interesting to note in passing that the two quadrants to the left of the midline are essentially problem solving dispositions, while the two to the right rely on problem finding (ie the ability to anticipate risks and problems).
Please feel free to place a symbolic pin into your default quadrant – and then ask your
Figure 4: The text reproduced below is extracted from the GDC’s Guidance Standards for the Dental Team, these extracts having been chosen for the specific purpose of this article. To place this statement in its correct, original context you should refer to the full text of the Guidance.7
Standard 1.9: You must find out about laws and regulations that affect your work and follow them
1.9.1 You must find out about, and follow, laws and regulations affecting your work. This includes, but is not limited to, those relating to: – data protection – employment – human rights and equality – registration with other regulatory bodies.
Standard 7.1: You must provide good quality care based on current evidence and authoritative guidance
7.1.1 You must find out about current evidence and best practice which affect your work, premises, equipment and business and follow them.
7.1.2 If you deviate from established practice and guidance, you should record the reasons why and be able to justify your decision.
family, friends and colleagues whether that’s a fair assessment, or you are deluded.
Adams makes a compelling case that you should not ignore risk and simply hope for the best, but nor should you become excessively risk averse and negative. Instead he advocates an approach whereby you try to understand risks, effectively manage those that you are able to influence, and accept those that you cannot control. Your approach should be positive and pro-active, but you should not become so consumed by risk that you stop looking for solutions, perhaps because you are so busy looking for problems.
Having worked internationally in the risk field for almost 50 years, Adams fears that modern society is in danger of becoming paralysed by risk and the fear of criticism and litigation. He has argued that a generation of children have been so overprotected from risk that they have learned no mechanisms for managing risks proportionately as adults. It is a challenging and thought-provoking perspective.
Within the world of dentistry and dental technology we encounter individuals with all of the above characteristics. One dentist will think it sufficient to learn a new procedure at a half day course, and will schedule the first patient to have this procedure carried out the following day. Another more cautious dentist will attend many courses, talk to colleagues, and seek independent validation of their competence before taking the plunge. Meanwhile, many of the dentists who experience multiple clinical negligence claims and complaints seem to have no ‘risk radar’ whatsoever, or perhaps suffer from an unshakeable overconfidence – or occasionally, arrogance. This ‘blind spot’ can influence the choices they make – whether instinctive or considered - how they present and describe any risks to patients, and through the so-called ‘framing effect’ perhaps lead patients to share the clinician’s skewed and unrealistic assessment of the risks, or simply to find themselves

excessively reassured into a misplaced complacency about the risks.
It also seems extraordinary that the GDC’s approach to Scope of Practice is to leave it up to each individual registrant to assess their own competence and when they are adequately trained to carry out a new procedure.
In a fast-evolving field such as dental technology, the same considerations apply but are heightened by the rapid acceleration of the emergence of new materials, new equipment and new techniques. The relevance of Adams’ fourfold typology is obvious.
We can all have the occasional bad day –for a variety of reasons - but most of us will reflect on why it happened, learn valuable lessons and take steps to prevent a recurrence. If nothing else, an adverse experience makes us more circumspect. But if you go through life shrugging your shoulders and adopting a “stuff happens”
viewpoint you are unlikely to benefit from any reflective learning. You may even start from the premise that nothing is ever your fault.
Understanding our own ‘default’ predisposition to risk is an important part of developing a healthy, constructive approach to risk and its effective management. Spend a few moments thinking about your own approach to risk (and the attitudes of others with whom you live and work). Ask those who know you and work with you, whether they agree with your self-assessment.
Our ‘default’ predisposition to risk is important because it influences
A The choices we make
A Our approach to learning new skills –our PDP and CPD
A How we choose and introduce new equipment and techniques into our workplace
A Our response to adverse events

Graduated in London 1971. He spent 20 years in full time general dental practice and 10 further years practising part time. He became involved in the medico-legal field in 1989, firstly as a member of the Board of Directors of Dental Protection Limited (part of the Medical Protection Society group of companies). He became a dento-legal adviser in 1992 and from 1998 was the Dental Director of Dental Protection for 18 years and also an Executive member of the Council (Board of Directors) and Executive management team of the Medical Protection Society, roles from which he stepped down in 2016. Since 2018 he has been a Special Consultant to the British Dental Association, in relation to BDA Indemnity.
He is a Founder and Ambassador for the College of General Dentistry, and was a Trustee Board member 2017-22 Kevin has been writing a regular column in the UK dental press since 1981 –originally as the Associate Editor of Dental Practice and since 2006 as the Consultant Editor of Dentistry magazine. He still writes and lectures regularly in the UK and internationally, and has been awarded honorary membership of the British, Irish and New Zealand Dental Associations. He is also an Honorary Member of the British Society for Restorative Dentistry.
A Team dynamics – especially if we are in a leadership/management role. Leaders and managers set the culture of the organisation and working environment
We may break the law without realising that we are doing so. Ignorance of the law is no defence, of course, and in our working life we would effectively have chosen not to follow the GDC’s guidance -see Fig 4.
Many of the unconscious choices we make are infact a reflection of our value system, and we default to those embedded values to guide our decision making - to the point where many of our choices are subliminal and instinctive. It has been said that ethics is less about what we do, and more about what we will not do – and that is very helpful in assisting our understanding of choice, and how we exercise it.
We all make choices. From whether or not to cross the road, park illegally , exceed the speed limit or overtake, to whether or not to have our vehicle or a piece of equipment maintained / serviced, to whether or not to drink-drive, to the way we conduct
ourselves in the workplace or in our personal relationships. Whether or not we ensure that we have someone at the foot of the ladder when we are 30ft up it…the list goes on….
In our work as technologists we decide whether or not some work we have carried out, is good enough. But all of our choices have consequences and this article has tried to improve our awareness of why we make certain choices, and why it might be helpful to consider the long term legal, ethical and professional consequences.
1 Exploring Professionalism - legal, ethical and human aspects. Part One – Fundamental principles The Technologist, Vol 15 Issue 2, May 2022
2 Professionalism in healthcare professionals. Research Project. May 2014. Available from Health and Care Professions Council (HCPC) via www.hcpc-uk.org
3 Professionalism : A Mixed-Methods Research Study (July 2020), Association for Dental Education in Europe. Available from www.gdc-uk.org
4 Guidance on Reporting Matters to the General Dental Council (updated 2025) https://www.gdc-uk.org/docs/ default-source/consultations-and-responses/guidanceon-reporting-matters-to-the-gdc
5 CPD - Legal, ethical and practical implications The Technologist, Vol 17 Issue 1, Feb 2024
6 John Adams, Risky business : the management of risk and uncertainty, Adam Smith Institute, 1999
7 Standards for the Dental Team, General Dental Council www.gdc-uk.org

To complete your CPD, store your records and print a certificate, please visit www.dtauk.org and log in using your member details.
Q1 Your choices might reasonably be affected by a range of factors. Three of the most obvious ones appear below. Which one is the exception?
A The time available to make the choice
B Whether or not you have been faced with the same (or similar) choice before
C Whether or not anyone is looking and/or will find out what choice you make
D Whether or not the choice can be postponed/deferred
Q2 Three of the statements below are generally accepted descriptions of professionalism, in terms of behaving like a professional. Which one is not?
A They take responsibility for their actions
B They have high earnings levels
C They respect and follow the law
D They are principled and ethical
Q3 An individual’s value system is developed and embedded as they progress through into adulthood. Which of the following is least likely to influence it?
A Family
B Teachers and other leadership figures
C Peers, friends, colleagues and online influencers
D The Government
Q4 Which one of the following was not one of the three original “learned professions”?
A The Church/Theology
B Medicine
C Moneylenders
D The Law
Q5 Which one of the following is not a recognised aspect of the ‘paramountcy’ of a professional relationship?
A The client’s interests must always be the professional’s first consideration and priority
B Both parties respect the rights and dignity of the other
C Professional fees should always take into account the client’s ability to pay
D Commercial interests must never be allowed to influence any choice that the professional might make
Q6 Many human principles/values are shared by ethics and professionalism. Which one of the following is not?
A Morality
B Technical competence and skill
C Honesty
D Decency
Q7 In which year was Professor John Adams’s book ‘Risky Business’ published?
A 1986
B 2006
C 1999
D 2011
Q8 In the book ‘Risky Business’, what name does John Adams give to someone who tends to adopt a cautious, careful, and risk-averse approach to life?
A Egalitarian
B Individualist
C Hierarchist
D Fatalist
Q9 In Adams’ four-fold typology of risk, an individual’s default tendency towards optimism and self-confidence might lead to three of the outcomes listed below. Which one is the exception?
A Over-confidence
B Complacency and a low awareness of risk
C Arrogance
D High standards
Q10 We might break the law without taking a conscious decision to do so. In which one of the following situations does this not apply?
A Because we had never applied ourself to finding out what the law is
B Because we were not concentrating
C Because we prioritise our personal advantage over the rule of law
D Because we were tired or distracted
Dr Chris Turner, MSc, BDS, MDS, FDSRCS, FCGDent, QDR. Retired Specialist in Restorative Dentistry
If I remember correctly, psychologists claim that when we meet someone for the first time, we will have decided within 20 seconds whether we like that person or not. I have never put this theory to the test with a timer. However, I have always made sure during my career that I met the technicians who would be working with me. I was very fortunate in finding dental technologist colleagues who could provide me with the high standard of work I wanted, and I learned a great deal that stood me in good stead for many years.

Aims:
■ To better understand the importance of properly taken dental impressions
■ Effective communication between surgery and laboratory regarding what is needed for the best patient outcome
■ Effective management of self and others in the interests of the patient
CPD Outcomes:
■ Maintenance and development of knowledge and skill within your professional scope
■ Team working Development Outcome: B&C
Ikeep saying this, patients see your laboratory work not mine as the final result. I found face-to-face meetings to discuss complicated cases and to determine limitations for both of us was a most worthwhile use of time. With modern technology ZOOM could be a very useful tool for this purpose when distance is a factor, and you are receiving work by post.
On the theme of modern technology, I wonder how you are finding results with digital impression techniques and what percentage of your dental surgeon clients are using this. It looks to be the future, but I wonder how long it will be before this is the norm in the UK, and I suspect this could take a generation. There is also a question
in my mind about accuracy. Have you ever audited your digital impression results?
This brings us back to traditional impressions. How do you rate the quality of the impressions you receive, that first impression from the surgery? Before I retired, I regularly gave a course for clinicians entitled ‘The Basis of Occlusion.’ Participants were asked well in advance to bring a set of casts of their own teeth as study models. The course outline said they should be taking facebow records and mounting study casts. I expected to see perfect models, trimmed as orthodontists prefer.
Unfortunately, they were the rarity, when the models were brought at all. All too often attendees pitched up empty handed. Of course there were excuses, “I forgot”, “I thought you would provide the models”, and then there the casts themselves that were presented to me – they left a lot to be desired. The most common fault was air blows on the surfaces that required trimming before models could be correctly articulated. When it was suggested that – if you take some alginate on your finger and

rub it into the fissures before you set the tray you can avoid this problem – the usual reaction was ‘I never thought of that.’
Others were badly trimmed and clearly taken with ill-fitting trays. Needless to say, the first impressions that some of my colleagues created were not good. I was left to wonder if that was the same standard they brought to a course of treatment, what would the standard be in their treatment outcome? How might it affect the patient’s comfort and quality of life? I have also said, and I apologise if it is mantra, that restorative dentistry, both prosthodontics and crown and bridgework is sequential and consequential. By that I mean that there are a number of stages, the one being dependent on its predecessor. So, if any stage is poor there will always be an unsatisfactory end result.
This leads onto the primary impression that is sent to you. Is it fit for purpose? Does it give you the information you want for the next stage? I always thought that the blue disposable plastic trays for complete denture impressions were not fit for purpose For clinical dental technicians, if you can ever find a set of mandibular and maxillary coloured, red, yellow and purple, edentulous trays made by Bayer they were my choice for first impressions. Sadly, I think they are no longer made and I am unable to find a picture to share with you.
For crown and bridgework my preference was to take the working impression in a metal-based tray using an elastomeric impression material, Impregum, and rarely needed a special tray. The exception was for impressions over implants when sometimes it was necessary to have a hole to access screws, for example Straumann implants. Others, such as Astra-Zeneca were easier, but required accurate replacement of the impression coping into the impression. I have in mind a design of metal-based tray for implant impressions. Watch this space.
In summary, impressions matter whether they are personal interactions or those sent
to you by dental surgeons. I hope you will be able to share your expertise and be able to improve any quality deficiencies in those impressions. This may mean rejecting some. If that happens, provide your clinician with an explanation – tell them why you are turning them down. I think the mnemonic is Tell, Show, and Hope the Doing improves. Yours is a key role in the quality of dental treatment outcomes.

To complete your CPD, store your records and print a certificate, please visit www.dta-uk.org and log in using your member details.
Q1 How long do psychologists estimate it takes us to decide whether we like someone or not?
A Five minutes
B An hour or more
C 20 seconds
D A week
Q2 According to Dr Turner, what do patients see as ‘the final result’?
A A brighter, more aesthetic smile
B Your laboratory work
C Better function when eating
D Freedom from dental discomfort
Q3 How long does Dr Turner estimate it will take before digital impression taking becomes the norm in the UK?
A A generation
B Up to 10 years
C By 2030
D When the investment into digital is made by the NHS
Q4 What was the most common fault with the models attendees brought to The Basis of Occlusion course?
A Poorly trimmed margins
B Distortion caused by rushed removal
C Air blows on the surface
D Lack of depth to the posterior teeth impressions
Q5 What was Dr Turner’s answer to the model problem?
A Take care to push the impression tray higher on posterior teeth
B Rub alginate into the fissures
C Treat impressions with more care when removing
D Teach precise margin awareness in undergraduate dental courses, including time spent in the dental laboratory
From writings by Kate Stoneman from Cornell University
The editor of The Technologist is a member of the online forum Quora, which is where he found a fascinating article written by former medievalist Kate Stoneman, during which she demolishes the idea that we have developed herd immunity to the various forms of plague and can survive without vaccination – as claimed by antivaxxers. It makes a great and intelligent read. The following is an edited excerpt that loses some of the political rhetoric, while including the hint of spice.
The first thing Kate would say is that the Black Plague — by which she means the complex of three diseases caused by the bacterium Yersinia pestis — certainly has not disappeared.
The Black Death is a term which refers to one specific epidemic which lasted from 1346 to roughly 1353 and is notorious for being particularly deadly and welldocumented. However, it certainly was neither the first, nor the last, of its kind.
The Plague of Justinian in the 6th century, which killed roughly a quarter of the population of the Byzantine Empire and the
Middle East, was almost certainly Yersinia pestis. And following the mid-fourteenthcentury wave, the plague would return every ten to twenty years in Europe, right through the seventeenth century, after which time it became less common.
Today, the disease is still around, and is in fact endemic in certain parts of the world, including the Congo, Madagascar and Peru. It is not exactly unheard of in the United States either; they get about seven cases of it per year. In fact, with much of public health in the US being dismantled, Kate expects the plague to become endemic there too.

Kate hates the way “popular” science simplifies everything to the point of transforming statements that have a grain of truth to them into borderline misinformation. No, modern people are not immune to the plague. There is no “long-term genetic immunity” to the disease among the population, as has been asserted.
The series of plague pandemics that swept through Eurasia and North Africa beginning in the 14th century and subsiding in the 18th did lead to the surviving human population being slightly — and Kate underlines that slightly — more genetically robust against the pathogen, and slightly more likely to survive when infected. But the plague is still extremely deadly, and no, we are not genetically immune to it.
In its mildest, bubonic, form, the plague has a mortality rate of 50%-60% without treatment. With prompt and aggressive antibiotic treatment, that drops to 10%-15%, which is still huge. Respiratory plague has a mortality rate of nearly 100% without treatment, and around 50% with treatment. Septicaemic plague has a mortality rate of approximately 90% with or without treatment. (Septicaemic plague is basically Ebola, practically speaking, just from a different infectant.)
Kate explains: “All three forms are caused by the same bacterium, so if you contract it from someone with, say, the bubonic form, you can develop one of the other two, deadlier, forms, depending on the mode of the infection and what Yersinia decides to do once she’s inside your body.
“The bubonic plague is contracted through bites of infected fleas, with flea-carrying
rodents (usually, but not always, rats) being the vehicle by which the fleas access human hosts. Pneumonic and septicaemic forms are transmissible human-to-human, and in the case of the former, contagion is spread via coughing and sneezing. So, bottom line? The plague is still around, it is still extremely contagious and it is still extremely deadly.
“Genetics isn’t magic, by the way. Genes multitask, and even ‘positive’ mutations almost invariably have trade-offs. The same genetic variant that made humans (slightly) more resistant to the plague, also made us more susceptible to autoimmune diseases, it’s a biological give and take.
“Oh, and another reason later plague outbreaks killed fewer people than the Black Death was that there were just fewer people around to kill. The 1346–1353 outbreak was thought to have killed at least a third of the European population, although the latest research suggests it was actually closer to half. Density dropped like a rock, even in cities (especially in cities), and the population took almost 400 years to recover.”
Kate observes that public health policy is about a lot more than vaccination, and public health policies are absolutely the reason why the severity of plague pandemics declined after the 1340’s-1350’s and why they no longer happen today (so far). Most antivaxxers, unfortunately, are not just against vaccines, they are against all policies calculated to prevent the spread of disease. They are against clean water, against mass testing, against lockdowns, against social distancing, against public information about disease, and against safety regulations being imposed on private business.
But long before antibiotics and vaccines, medieval and early modern governments were stepping in to try to dampen the effects of plague pandemics. In fact, Kate traces the beginnings of this to the Black Death and its aftermath. Lockdowns,

quarantines and social distancing were invented back in the 14th century. Giovanni Boccaccio’s famous book Decameron is a collection of stories that a group of people tell each other to pass the time while isolating themselves in a castellated country villa during the Black Death.
If you know facts about the plague — as Kate does because she is a former medievalist — you’d be amazed how many public policies we have today are clearly calculated to prevent the plague from becoming endemic again. That’s what all those global deratisation programmes are about, where government workers spray train tracks and various other sites with rat poison. While people grumble about what a waste of tax money it is.
Kate explains: “In the US local laws subject property owners to fines for failure to keep their lawns trimmed and clear away garbage; no, it’s not about appearance — at least not as the first priority – it is about keeping down the rat population as are regulations imposed on grocery stores, warehouses and restaurants, and all the laws about garbage disposal.
“The human race learned the hard way, through eras of unspeakable tragedy, that rats = plague. You’ve got to keep rats away as a matter of government policy. Leave it up to antivaxxers or rugged individualists, and you’ll have people dropping in the
streets in a month. And back in an era when you couldn’t really keep rats away, a way to somewhat reduce the death toll was to act as soon as someone found a dead rat in their kitchen. Which was to put the authorities on high alert and in the case of people of means, start packing their trunks for an extended stay in the country.”
An antivaxxer implies, Kate supposes, that the best way to deal with an epidemic of a disease such as the plague is the way that they imagine people dealt with it back in the 14th century, which is to suck it up, sit tight, and do nothing. Because the alternative — a vaccinated death toll of considerably less than 30–50% of the population and no societal breakdown – is somehow – worse. Worse? How?
“By the way,” Kate said, “yes, there is a vaccine for Yersinia pestis. It is not generally available to the public, and the only people who take the jab are those who work with this organism in a lab or those who travel to areas where the plague is still endemic. For now, other public health measures, such as controlling the rat population and hygiene, have been sufficient to prevent plague outbreaks.”
Looking at the US American situation Kate has noticed that antivaxxers, and modern right-wingers in general, suffer from massive survivorship bias. Here in the UK antivaxxers line our streets chanting and
waving placards, while in the US they advocate policies that are expected to cause mass suffering or death in the belief that they, personally, will not be affected. During the COVID-19 pandemic, antivaxxers were routinely surprised when they, or people close to them, developed severe coronavirus. Many antivaxxers died.
Kate speaks directly to this antivaxxer to tell them that they are not special. A disease outbreak which kills 50% of the population (let’s say) gives them a statistical 50% chance of dying and is also likely to kill at least half his family. A pathogen does not care how “brave” or nonchalant someone is. It does not care about people’s politics, their wealth, their religion or their workout routine. Antivaxxers and their kids make excellent hosts for bacteria and viruses – fungi, too.
Kate advocates that potentially living through an epidemic that kills between one third and half the population, even if you yourself survive, would be almost unimaginably horrific. She can’t understand how someone can be cavalier about a thing like that. She says: “Apart from just being surrounded by mass death and losing one’s immediate family members — because let’s be realistic, the chances of an entire family surviving in an outbreak this deadly are nil — there are knock-on effects that exacerbate an already apocalyptic disaster.

“Half the population dying means half the people who produce the food — grow it, butcher it, package it, deliver it to you — also die. During the Black Death, crops rotted in the fields, cows and goats went unmilked, animals died. The price of whatever food was available shot through the roof — every day. This triggered a famine that lasted years.”
She continues: “This famine didn’t just affect the poor, whom antivaxxers, of course, don’t care about. Letters survive that the Queen of Sweden and Norway, Blanche of Namur, wrote to her husband, King Magnus Eriksson, who spent most of the Black Death away on this or that crusade.
“The letters describe bleak conditions at the royal palace, with the Queen and her surviving courtiers literally starving because there was no food. Everyone who had been cooking food had died, so the survivors were now dying from starvation. With even the queen herself and the most privileged nobles of the kingdom also starving.
“They were also freezing to death, by the way, because all the people who had been supplying firewood for the winter likewise either died or ran away. With most of the palace guards dead or sick, too, it was dangerous to venture outside, so even people who could, ostensibly, go out and chop some wood for the fire, balked at the idea of doing so. If this is what royalty had to go through during the Black Death, what do you think life was like for the hoi-polloi?”
Kate describes how this mass starvation triggered by the plague outbreak had in turn triggered outbreaks of other diseases, such as tuberculosis, smallpox and dysentery, because when people can’t get enough calories into their bodies their immune system is weakened.
Half the population dying means that almost all the people who care for the sick quickly die too. Remember how Kate mentioned that the bubonic plague still has a 10–15% mortality rate in the modern day with prompt and aggressive treatment?

She added: “Setting aside the fact that this is still a colossal mortality rate, you won’t get that prompt and aggressive treatment if there are no hospital beds available, and if half the doctors and nurses are dead, and if half the people who produce the medicine are also dead, and if half the law enforcement is dead, that means armed gangs are going to seize whatever medicine remains by force. If that sounds like fun to you, then may you die in “interesting times”.
“In short,” Kate says, “I don’t know how anyone can see letting something like this happen as the preferred alternative to using modern medicine and public health to... not letting something like this happen.”
We cannot let those who claim that we now have herd immunity and are immune to classic forms of plague – or politicians who tell us to do one thing then promptly do the exact opposite – win the upper hand. Ours is a global culture, we can travel long distances very quickly, an so can potential pandemics.
Kate concludes: “To refute the claims of antivaxxers I had to write a thesis. Which most people who are prone to being antivaxxers will dismiss for being too long. Like it or not, reality is very complicated. Any solution that’s simple and short, including the idea that we are immune thanks to herd immunity, is almost certainly wrong.”
traditional craftsmanship with digital efficiency in composite veneering
As ever, SHOFU focuses on manufacturing excellent dental consumables. To keep up with the growing needs of dental technicians, we will continue to develop innovative solutions for the increasing use of digitalised production processes in today’s dental laboratories.
Proper bonding makes the difference
Our new concept “CERAMAGE meets digital”, tailored to dental technicians, offers countless options to aesthetically enhance all types of restorations by composite veneering.
No matter what material you select for a framework or superstructure, or whether you make it using an analogue/manual or
digital method: CERAMAGE, CERAMAGE UP and LITE ART allow you to veneer, individualise and refine a wide variety of dental materials, e.g. PMMA, zirconia, hybrid ceramics, non-precious alloys or 3Dprinting liquids.
The secret of success is the proper adhesive bond: Combine this trio – depending on the restorative material used – with CERARESIN BOND (CRB), the bonding agent for ceramics and resins, or SHOFU Universal Primer, the bonding agent for composites and metals, zirconia and alumina. For longterm rock-solid composite veneers, combine SHOFU Universal Pre-Opaque with the Primer: The two form a well-matched system that is highly resistant to hydrolysis and thermal stress.
This combined use is very important for a durable bond in a moist environment; you no longer need mechanical retention to metal frameworks.
The flowable SHOFU Universal Pre-Opaque cures even in shadow zones with little light and increases bond strengths many times over.
The benefit for users: In all areas of veneering, you work with products that have proven their worth both individually and in combination with each other, giving you peace of mind when delivering your restorations to the dental practice.
A For more information, visit https://www .shofu.de/en/solutions/ceramagemeets-digital/

