




























As we work to put together the academic calendar for 2024, I find myself reflecting upon the state of education and the transformative journey we have embarked upon together.
The past six months have allowed me to dig in to all that is CoROM and it is from this vantage point that I would like to share my thoughts on the state of education today. Education has always been a powerful tool, enabling individuals to broaden their horizons, acquire knowledge, and unlock their true potential. We may lose property when world events overwhelm us, but knowledge can never be taken away from you.
The world around us is changing at an astonishing pace, demanding a paradigm shift in the way we approach education. The traditional model, while effective in its time, is no longer sufficient to prepare our students for the complexities of the 21st century. One of the key aspects of the state of education today is the growing emphasis on interdisciplinary learning. The boundaries between disciplines are blurring, and complex problems require a holistic approach. Paramedics today are doing things that only physicians were doing 25 years ago. As educators, we must equip our students with the skills to connect ideas across different fields, fostering innovation and creativity. By encouraging collaboration and multidisciplinary exploration, we can nurture the next generation of leaders who possess a broad perspective and the ability to tackle the multifaceted challenges that lie ahead.
Technology has opened up new avenues for teaching and learning, making education accessible to individuals around the globe. This is an enormous strength that we have to showcase CoROM’s incredible faculty, however, we must be cautious not to let technology overshadow the human element of education and neglect the strengths that the face-to-face interactions, mentorship, and a sense of community we can create by bringing students into the classroom in Malta.

In a rapidly changing world, the knowledge and skills we acquire today may become obsolete tomorrow It is no longer sufficient to view education as a onetime endeavor; rather, it is a lifelong journey of continuous growth and adaptation As an institution, we must foster a culture of curiosity and a love for learning that extends beyond the confines of the classroom By empowering our students to become self-directed learners, we equip them with the resilience and agility required to thrive in an ever-evolving landscape
The challenges we face in education today are multifaceted and complex, but they also present us with tremendous opportunities for growth and innovation. As we look to the future, we must be agile, adaptable, and open to change. Embracing new pedagogical approaches, leveraging technology, developing important collaborations, and cultivating a culture of lifelong learning will be pivotal in shaping the next generation of leaders and thinkers.
Let us continue this good work the Dean O’Kelly started and work collaboratively, pushing the boundaries of education, and empowering our students to become lifelong learners and catalysts for positive change.




From my perspective, the pace of 2023 has been nothing short of warp speed


Hard on the heels of my completion of a second transect of Africa came CoROM’s first dedicated multiday Tropical Medicine course in early June. Our Norwegian military students seemed pleased with our offering and we look forward to repeating that training in Norway and elsewhere.
Taking a break – relatively speaking – from the rigors of thesis writing to the creation of this edition of The Compass has been a welcome respite. I thank the contributors to this edition, two of whom hail from outside CoROM. The singular Dr. Geelhoed returns with a case study from Kenya during his recent surgical mission to that country. Team Rubicon cofounder Will McNulty expounds upon the humanitarian contributions of White Stork in the beleaguered country of Ukraine.

Keeping with CoROM Dean John Clark’s admonition to seek out multimodal avenues of education, two new sections grace the pages of this newsletter: Audio Files, featuring recent medical podcast episodes, and Envisioning Information, featuring YouTube links to some of my favorite education content creators
Our regular sections cover a wide gamut: the ongoing mpox outbreak, duct tape as an improvised medicine tool, notes from the latest Joint Trauma System conference, and some fascinating field medicine articles.



Finally, I am pleased to announce that CoROM will be hosting the first-ever Medicine in the Mediterranean conference in Malta in February 2024 – see the flyer on the back page of this newsletter for more information.
Jason Jarvis is CoROM’s Press Chair and an associate lecturer in Tropical Medicine. He is a paramedic and former U S Army Special Forces Medic (18D) with years of accumulated experience as an austere primary care practitioner in resource-poor countries such as Laos, Burma, Iraq and Afghanistan He recently completed his second transect of Africa, teaching predeployment medicine courses for UN peacekeeper clinicians in Ghana, Rwanda and Kenya. Based in Seattle, Jason is a freelance medical educator who teaches advanced trauma courses, minor surgical procedures, ACLS, and PALS. He is a recurrent presenter at the annual Special Operations Medical Scientific Assembly, an article reviewer for International Health, and is pursuing a master’s degree in Infectious Diseases at the London School of Hygiene and Tropical Medicine.


In the early 20th century, we strove to avoid entanglement in European wars that seemed far away and of little direct consequence. The eventual cost of that isolationist stance was 252,000 American dead, and it taught us a painful lesson: we must not hesitate to intervene early on to stop conflict lest we pay a much heavier price in blood down the road.

Along with the rest of the world, we agreed to honor the sacrifices of the Greatest Generation by preventing a recurrence of the horrors we had seen at Auschwitz, Dachau, and elsewhere. With a single voice, the international community agreed, “Never again.”

The way to avoid horrible costs in the future is to do more in the present. Our governments are leaning forward with impressive volumes of military and humanitarian assistance, but are still falling short of meeting all needs. Ordinary people across the world have stepped into the gap, providing the Ukrainian people with aid that nation-states and large traditional charities cannot. Crowdfunding is supplying Ukrainian defense forces along the frontlines with everything from tourniquets to Turkish drones. This is the critical gap that White Stork fills, and we are focused on our task. At the start of the war, White Stork managed one of the largest evacuation programs in Ukraine, safely transporting 37,829 women, children, and elderly to government reception centers in Poland.


 William McNulty White Stork Head of Mission USMC 2000-2008
William McNulty White Stork Head of Mission USMC 2000-2008
We did this because of the miles-long lines of women & children we witnessed at Polish border crossings in late February 2022. We decided on our other major line of effort - battlefield first aid kitsbecause we were surprised to learn that Ukraine was sending men and women to war without the basic medical kits that we carried in the U.S. Marines.





So now White Stork’s brave teams of international volunteers distribute Individual First Aid Kits (IFAKs) along the frontline. White Stork only delivers to end users – not aid depots – ensuring donations reach those who need them most. We respond to the demand signal of our Ukrainian partners to support the civilian population, and also provide non-lethal military aid to the frontlines. We are propelled by our strategic formal relationships with Ukrzaliznytsia (Ukrainian Railways) and Ukrposhta (Ukrainian Post Office).

We couldn’t have accomplished our mission without the support of our fiscal sponsors, Ukrainian Congress Committee of America (UCCA), and the Society of Jesus, South Poland Province. Their patronage allowed us to conduct humanitarian operations in Ukraine prior to White Stork receiving 501(c)(3) approval.





Along with our fiscal sponsors, our “Founding Funders” provided the means for us to perform these difficult tasks. We are forever grateful to Michael and Tanya Polsky of the Polsky Foundation, Anthony Melchiorre of Chatham Asset Management, Jeff Chambers and Andi Okamura, Jim and Kathy Murphy of the 125 Foundation, UCCA, and the Dorado Beach Community.
And finally, we are grateful to our friends Pauline Lewis, An-Me Chung, Jeff Menath and our colleagues at Greenberg Traurig and Kelley Drye, who provided their business expertise to help stand-up operations in those critical early days. On behalf of Grace Kim, Matt Vacca, Natalka Vivcharchyn, Dr. Darren Cuthbert, Michael Mathews, Max Cormier, Sue Johnson and the entire White Stork team, thank you to all our volunteers, donors, supporters, and partners who have demonstrated through action that “Never again” is a promise worth defending.
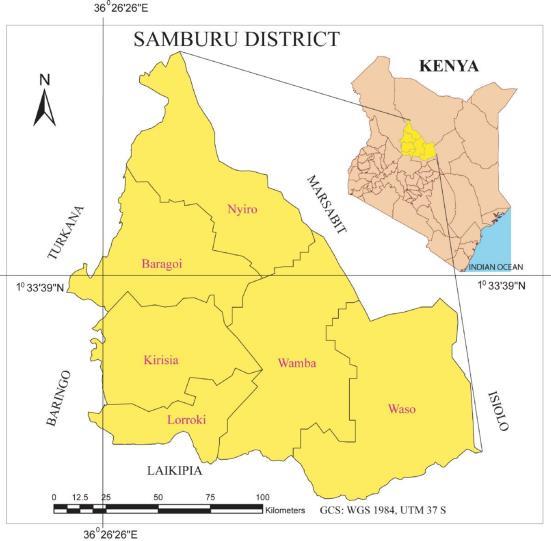
A young teenage Samburu boy was brought in by family with the story that they believe he had been bitten by a snake in the sole of the foot over a year ago.
 Glenn Geelhoed AB, BS, MD, MA, DTMH, MPH, MA, FACS
Glenn Geelhoed AB, BS, MD, MA, DTMH, MPH, MA, FACS


Although no one had seen the snake and could not describe it, that alleged event was the origin of a swelling that eventually led to chronic anesthetic, then necrotic patches and then those sites started draining, including extrusion of some small particles that looked a bit like sulfur granules.
Examination shows a woody indurated nonmobile foot that had insensate patches and spicules of parts of the bone that had been devitalized.
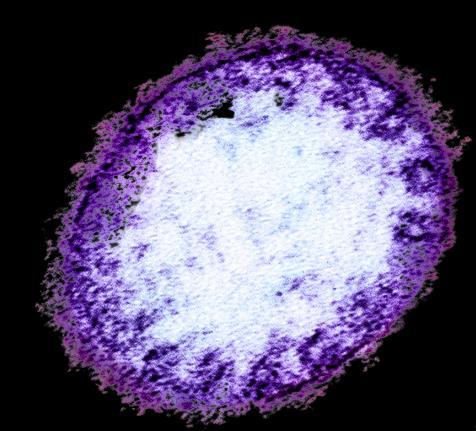
 Medial-plantar aspect of patient’s right foot
Medial-plantar aspect of patient’s right foot
Mycetoma (Madura Foot) is common in this part of the Great Rift Valley desert and this is the fourth patient with this diagnosis we have discovered in the course of two weeks in this location, but this was the youngest patient with the shortest course.

Prognosis for control of this disorder is grim, and it is gradually progressive leading to inevitable eventual amputation.


With that long-term outcome in prospect, management is focused on rehabilitation with the potential for early adaptation to a prosthesis in the future for his preservation of mobility, while maintaining him in the interval on a futile course of antifungal treatment and local wound care.
Dr. Glenn Geelhoed received his BS and AB cum laude from Calvin College and MD cum laude from the University of Michigan. He completed his surgical internship and residency through Harvard University at Peter Bent Brigham Hospital and Boston Children’s Hospital Medical Center. To assist in developing further volunteer surgical services in underserved areas of the developing world, Glenn completed masters degrees in international affairs, epidemiology, health promotion and disease prevention, anthropology, and a philosophy degree in human sciences.
He still works as a professor of surgery at George Washington University Medical Center in Washington D.C. and is a member of numerous medical, surgical, and international academic societies. Glenn is an avid game hunter and runner. He has completed more than 135 marathons across the globe. He is also a widely published author accredited with several books* and more than 500 published journal articles and chapters in books. He has two sons and five grandchildren.
*A selection of Dr. Geelhoed’s books are featured on page 21

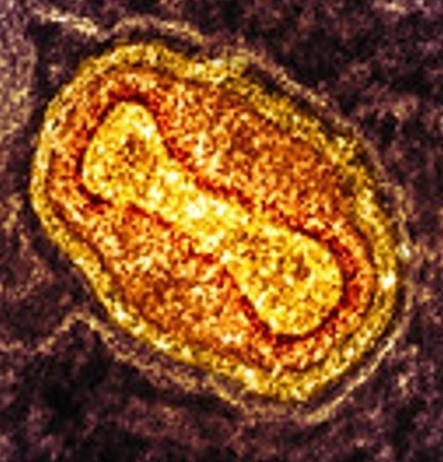
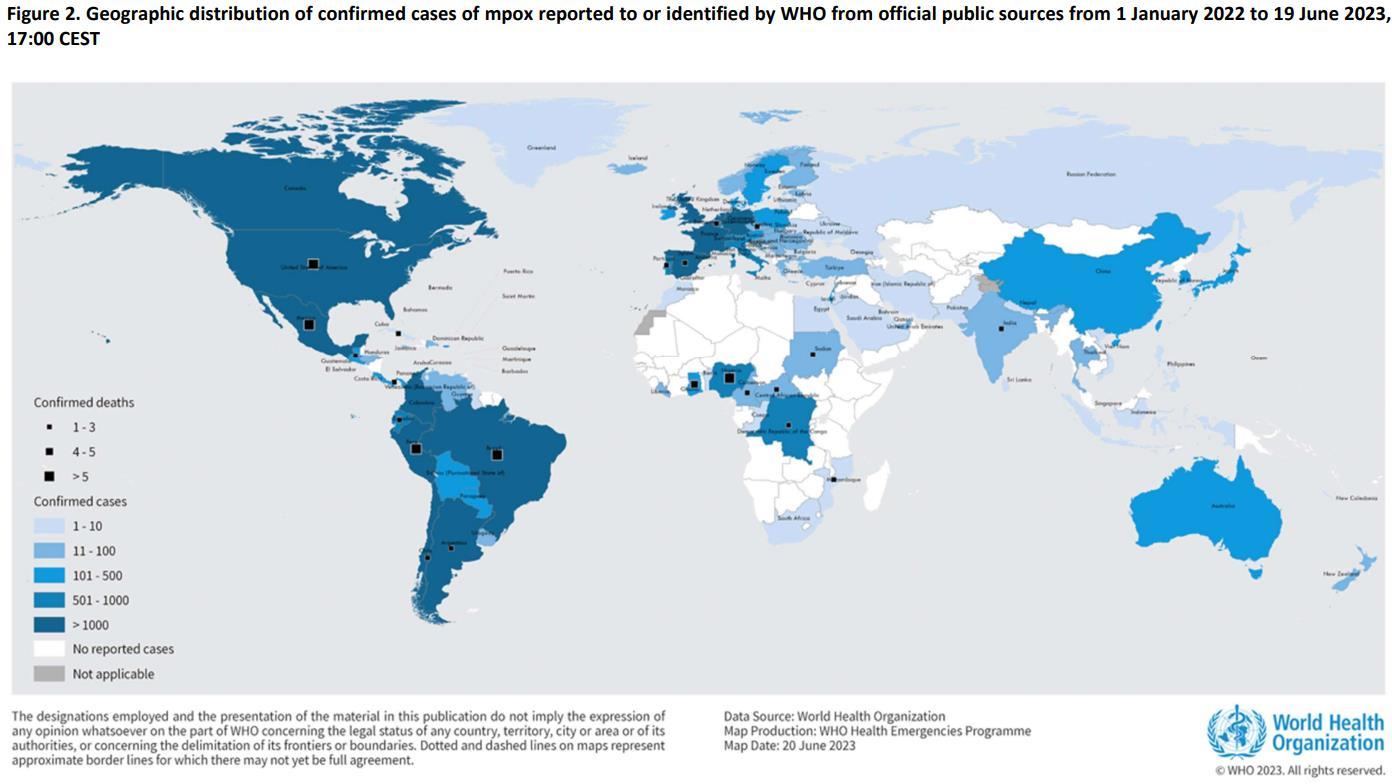
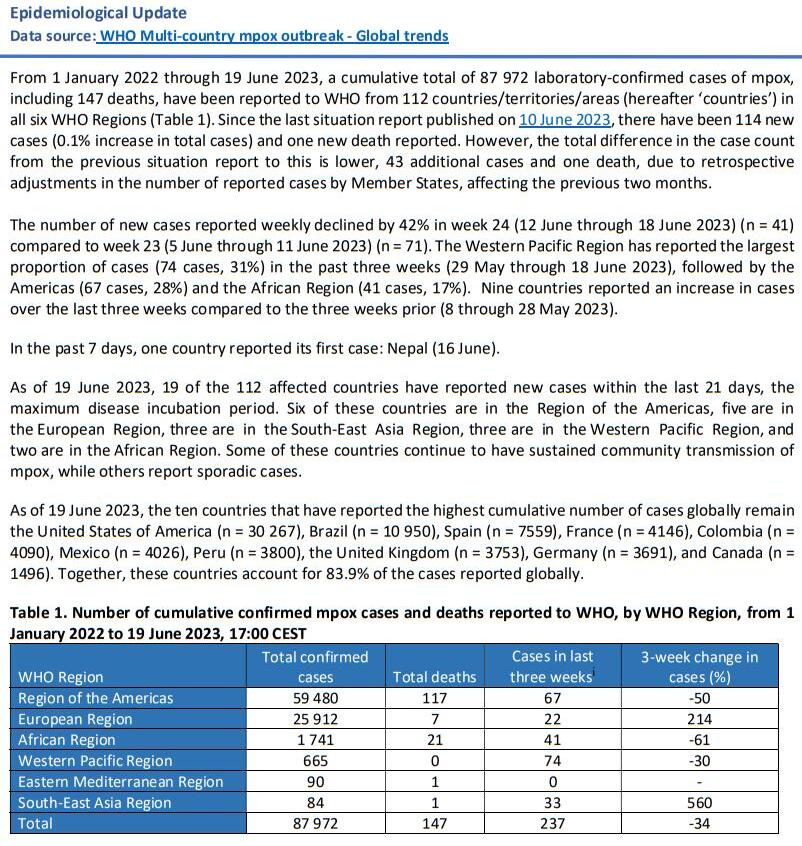
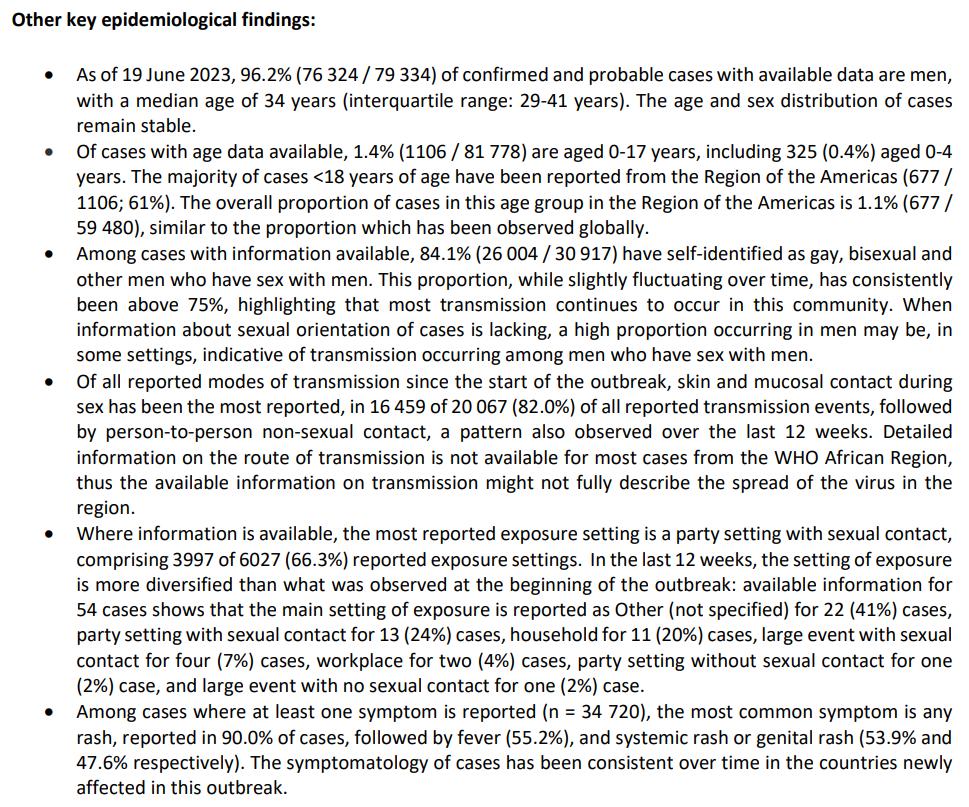
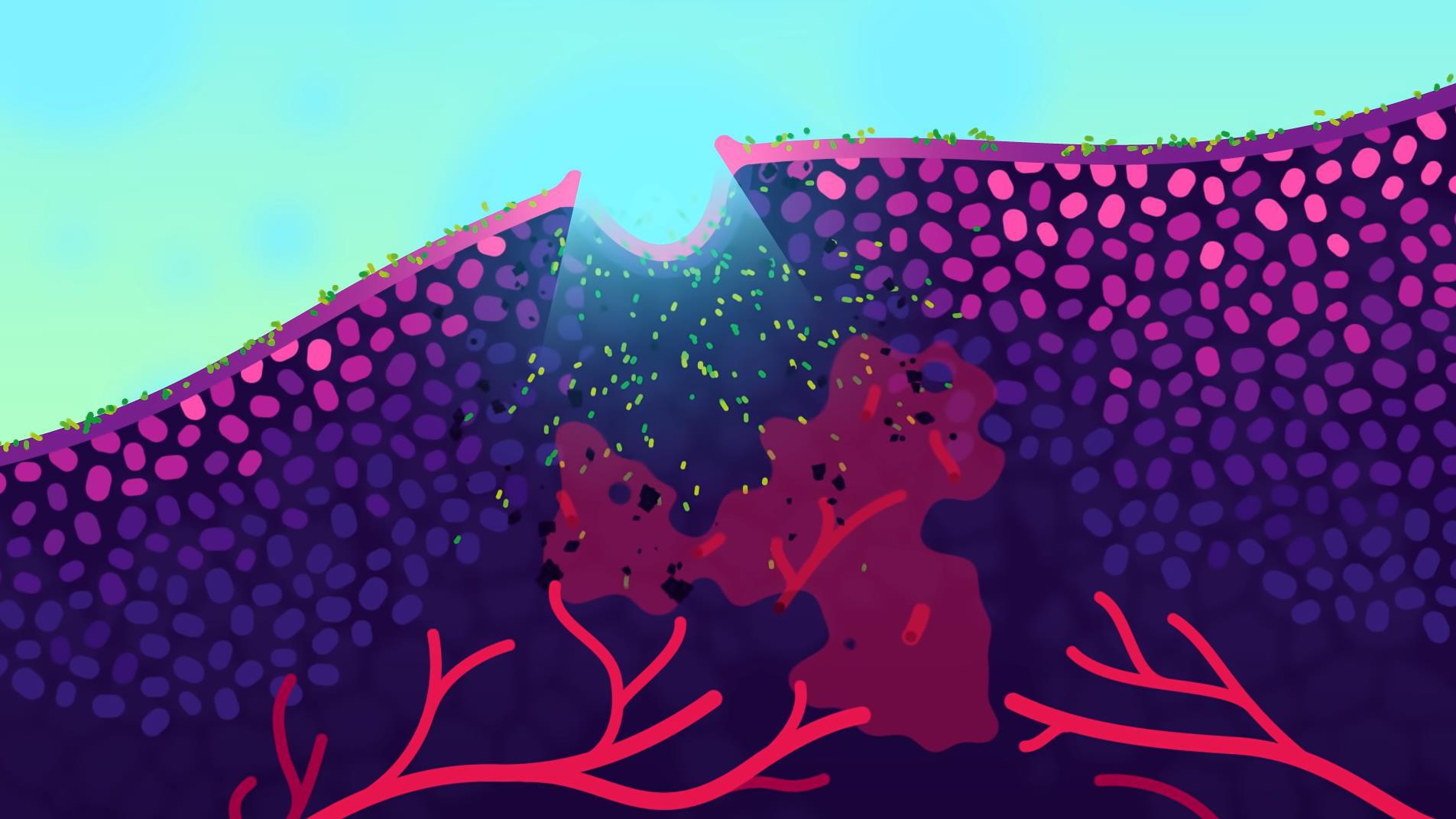
What follows are excerpts from the WHO on the current multinational mpox (monkeypox) outbreak. The primary reference is “Multi-country outbreak of mpox: external situation report 25” published on 24 June this year1 .
While the viral disease was first described in 1970, the case load has been relatively light – until now – making this an emerging infectious disease of the post-COVID era. Taking into account the probability that many readers of The Compass may be unfamiliar with clinical mpox, I have frontloaded this piece with content from the WHO’s “Clinical management and infection prevention and control for monkeypox” published on 10 June 20222 .
Jason Jarvis 18D BSc NR-Paramedic PGCert Infectious Diseases
1 https://www.who.int/publications/i/item/WHO-MPX-Clinical-and-IPC-2022.1


Those at risk of contracting mpox may be eligible to receive the modified vaccinia Ankara-Bavarian Nordic (MVA-BN) vaccine. 2 https://www.who.int/publications/m/item/multi-country-


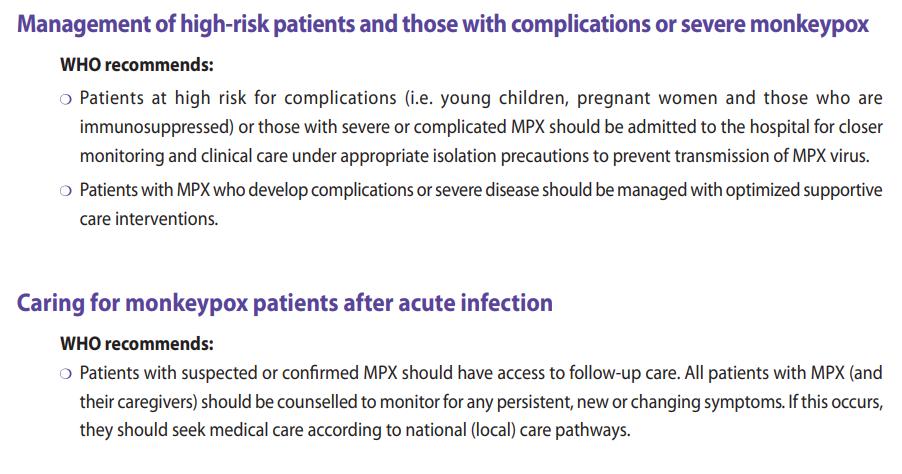
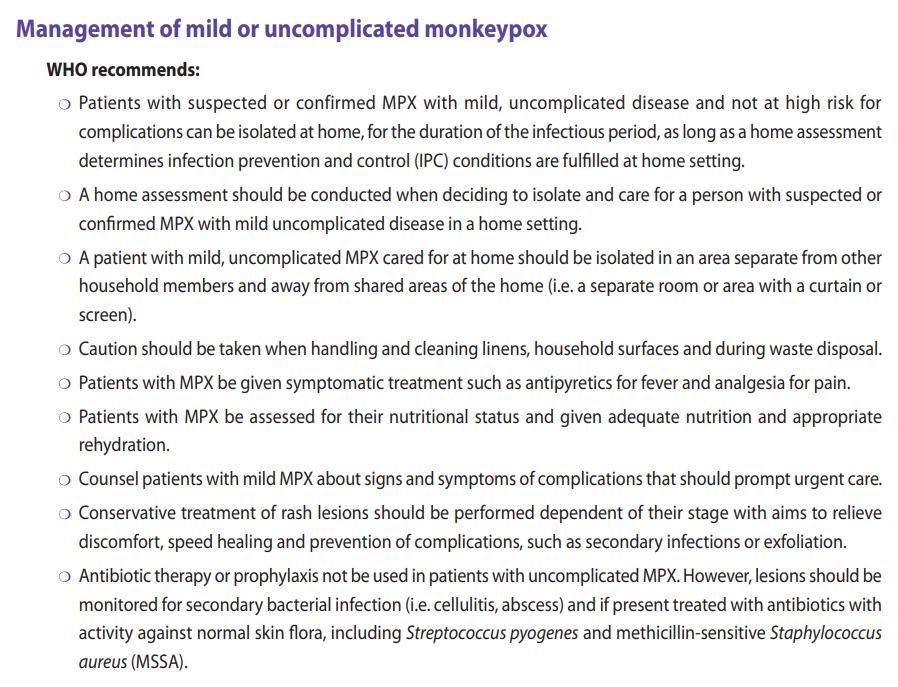
Benign manifestations of mpox are characterized by a centrifugal and vesicular rash plus fever and myalgia; severe cases of mpox may also present with skin exfoliation (similar to partial thickness burns), necrotizing soft tissue infection, pyomyositis, cervical adenopathy, ocular lesions, pneumonia, ARDS, severe dehydration, sepsis and septic shock, and encephalitis.















There have been many articles and publications discussing the use of duct tape for wilderness medicine. As Remote Medics, we can use this advice and add some rolls of duct tape to our medical kit. I like to carry one in my medical kit and one in my personal kit. I also ensure that I have two pairs of cutting devices: one pair of EMS shears in my medical ruck and a utility key chain with scissors. Redundancy is profoundly vital in austere medicine.
1. Removing warts – Published studies show that covering a plantar wart with duct tape improves outcomes.



2. Blister care – Prevention is key. Use duct tape to cover areas of the body at risk for blisters. During Special Forces selection, I used duct tape on the backs of my ankles and my hips. It prevented me from getting blisters on my hips, but I still got blisters on my feet. Once I got blisters, I used benzoin tincture and moleskin to protect them. The two options seemed to work as I completed the Qualification course without having to recycle.
3. Splinting – Duct tape can create a splint for stabilising fractures or sprains. By securing a rigid object, such as a stick or a folded newspaper, to the injured limb with duct tape, you can provide some support and immobilisation whilst evacuating the casualty.
4. Securing bandages and dressings – Duct tape can reinforce or secure bandages, particularly in areas where traditional adhesive bandages may not adhere well, such as joints or areas prone to movement. When conventional medical tape is unavailable, duct tape can be used to secure dressings or gauze pads.

5. Sling and Swathe – Duct tape can create an improvised sling to support an injured arm or shoulder. You can provide some support and immobilisation by attaching a loop of duct tape to the wrist or hand and then securing it to the chest or neck. Be sure to pad the device around the neck and the injury. https://content.instructable
 Aebhric O’Kelly M.Psy DTN FRSM FAWM FRSPH
Aebhric O’Kelly M.Psy DTN FRSM FAWM FRSPH
6. Tourniquet – Create a 50cm length of tape. Rip off another 45cm of tape and tape the two sticky sides together. Then secure this into a loop. Use a windlass to tighten this just above the catastrophic bleeding. Document the time and reassess in one hour for removal.
7. Plasters (Band-Aids) – Duct tape can be placed over a minor wound. Use gauze or other absorbable fabric and place on the wound. Use duct tape to keep the improvised bandage in place. Never place circumferentially around an extremity.
8. Waterproofing bandages – When waterproof applications are unavailable, duct tape can be used to cover regular bandages or dressings to resist moisture which can be particularly useful in a rainy or aquatic environment. I learned this whilst working on a maritime operations team in the Green Berets.

9. Chest seal - For an open chest wound, duct tape can be used to create a temporary chest seal by covering the wound with a plastic material, such as a plastic bag or plastic wrap, and securing it with duct tape.
10. Eye protection – In the absence of proper eye protection, duct tape can create an eye shield by covering the injured eye with a clean cloth or gauze pad and securing it with tape.
11. Splinting fingers or toes – Duct tape can be used to immobilise and splint injured fingers or toes by buddy-taping them together, providing support and stability. Remember to put something fluffy between the fingers.
12. Pressure dressing – For a bleeding wound that requires pressure to control, duct tape can be used to secure a folded cloth or dressing tightly over the wound, maintaining direct pressure.

https://www.survivalsullivan.com/wpcontent/uploads/2022/03/improvisedbandage-for-an-injured-arm-with-duct-tapeand-gauze-pad-768x1152.jpg


13. Stretcher – Duct tape can create a stretcher for medical evacuation. Making a solid stretcher takes 6-8 rolls of duct tape.

14. Pelvic Binder – Duct tape can support a suspected fractured pelvis. But there needs to be a way to improvise the 32 pounds of pressure required to close the open pelvic fracture, which can be improvised with a couple of tourniquets.
This list is for informational use only. Always refer to a doctor when injured.

Important tip when putting duct tape on skin: Poke holes into the duct tape where it will be placed on the skin. Use a safety pin or something similar to poke lots of holes into the tape. Do this before you put it on the casualty. These holes allow the skin to breath.
Instead of chucking a large roll of duct tape into your backpack, create a smaller and lighter option: slowly unroll the duct tape from the large commercial roll and roll it onto itself and slowly wind the tape on itself until you have 3 or 4 meters of tape rolled up. It is far lighter and takes less room. What have you used duct tape for?
Take home message: Always have a roll of duct tape in your medical and personal kit. Remember, two is one, and one is none.

Abdel-Latif A, et al. Silver duct tape occlusion in the treatment of plantar warts in adults: Is it effective? Dermatol Ther. 2020 May;33(3)

Loftus A, et al. Improvised first aid techniques for terrorist attacks. Emerg Med J. 2018 Aug;35(8):516-521
Ruskin K, Tung A. "If I Had Some Duct Tape, I Could Fix That". Anesth Analg. 2016 Nov;123(5):1072-1073.
Iserson, K. Improvised Medicine: Providing Care in Extreme Environments: Providing Care in Extreme Environments. McGraw-Hill (2016)
https://content.instructables.com/FGY/DW10/GOQY1Z48/FGYDW10GOQY1Z48.jpg


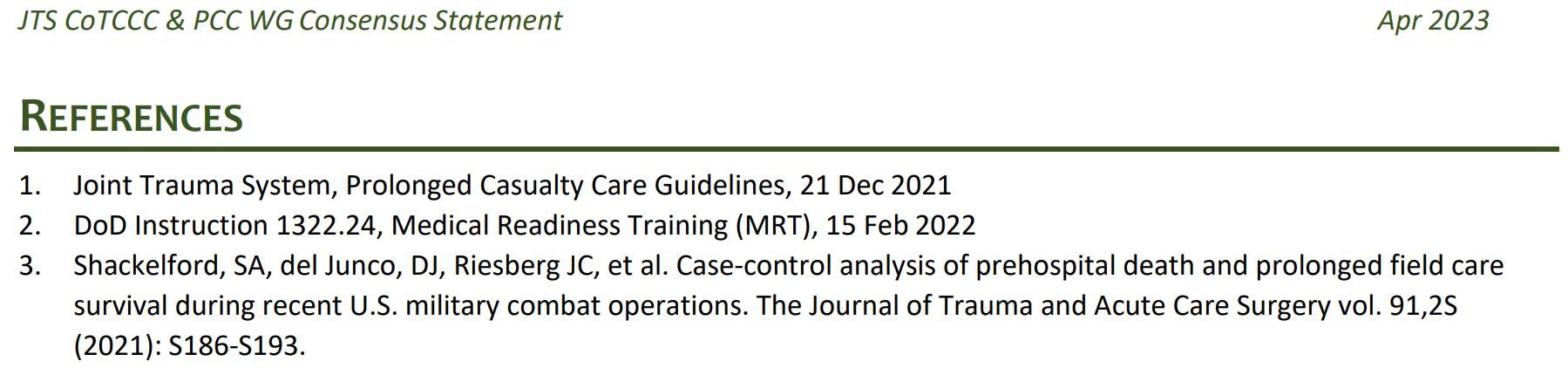
In April of 2023 a consensus statement was published on the U.S. Joint Trauma System’s website (https://jts.health.mil/). The JTS is an excellent repository of field clinical practice guidelines ranging from mechanical ventilation to snakebite treatment to setting up a walking blood bank.

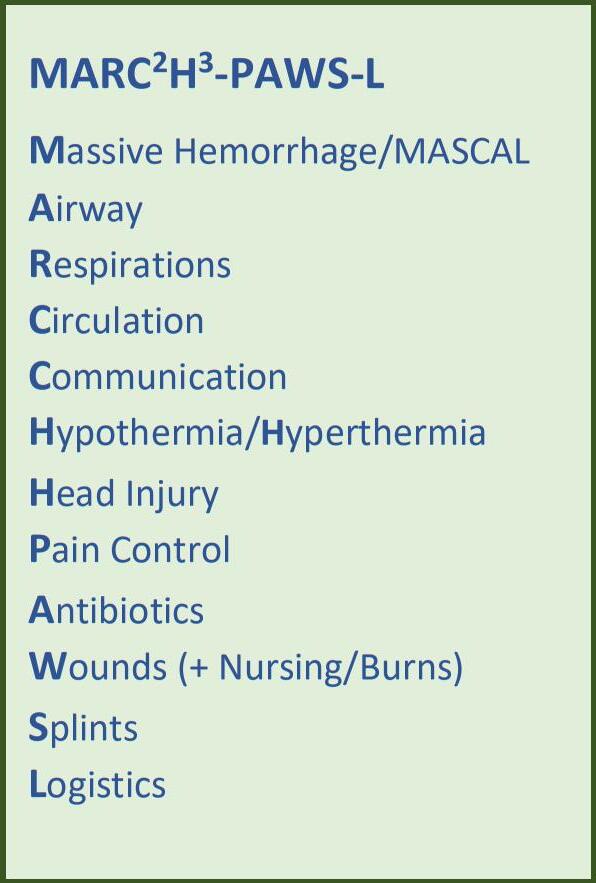
This most recent consensus statement was penned by the Committee on Tactical Combat Casualty Care and the Prolonged Casualty Care working group, and emphasizes the adage “There is no PCC before TCCC,” meaning the primary assessment and immediate threats to life must be addressed before moving into the prolonged casualty care (PCC) phase.
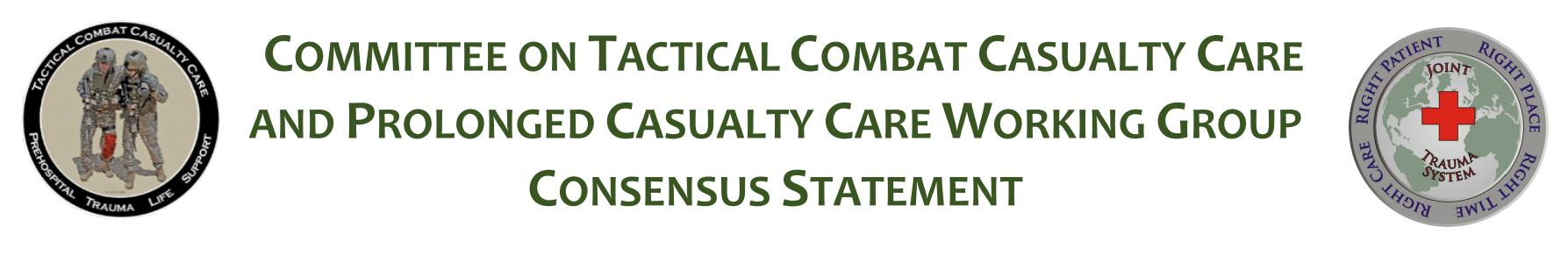

I’m not clear why this admonition needed to be stated; I can only speculate that somewhere, someone decided to put the PCC cart in front of the TCCC horse, so to speak In hospital terms, this would be analogous to an ambulance crew delivering an emergent casualty directly to the intensive care unit, entirely bypassing the emergency department
Renewed emphasis on PCC training appears in the document as well.
PCC has been an fundamental component of medical training methodology throughout my career, and continues quite robustly in both CoROM’s TTEMS and AEC courses (see course calendar on page 32). The working group’s recommendations, list of authors and a flowchart of PCC assessments and interventions appear on the following page.




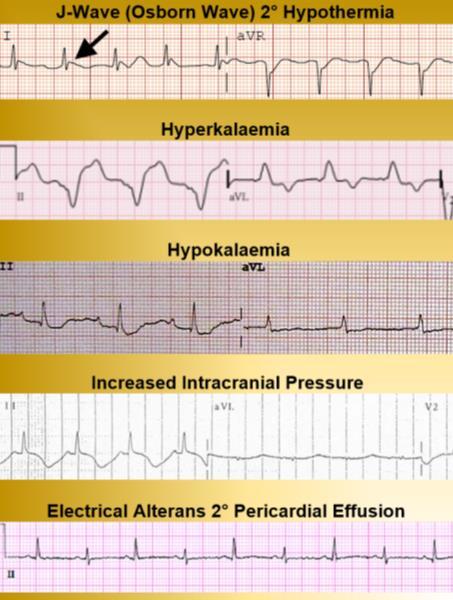
Which of the following ECGs is consistent with an epicardium that is being touched with a needle during electrocardiographically monitored pericardiocentesis?





You are in charge of drinking water procurement at a refugee camp in Namibia. 100 liters of river water has been collected and its turbidity reduced via flocculation and coagulation with aluminum salts. Your water disinfection protocol now calls for the addition of 2 mg of bleach (sodium hypochlorite) per liter of water. How many mL of 5% bleach should you add to the 100 liter stock?


One of the scientists under your care at a research station in Antarctica presents with chronic fatigue, depression and intermittent gastroenteritis. Upon examination, the 50 year-old Swedish female has splenomegaly, decreased proprioception of the hands and generalized hyporeflexia. Which of the following pathogens is most likely responsible for this syndrome?


A. Brugia malayi
B. Naegleria fowleri
C. Diphyllobothrium latum
D. Echinococcus multilocularis


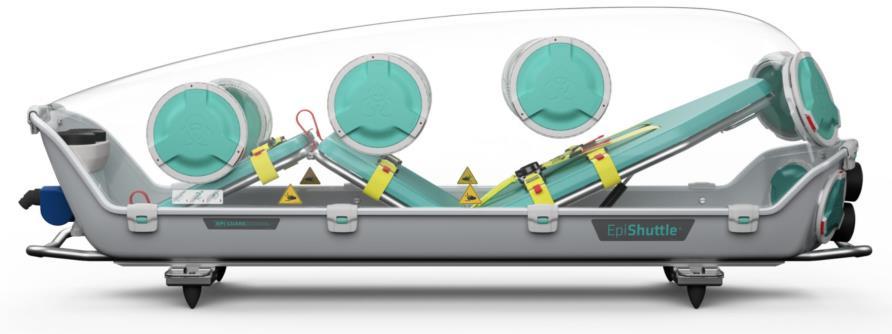
EpiShuttle®

available at https://epiguard.com/

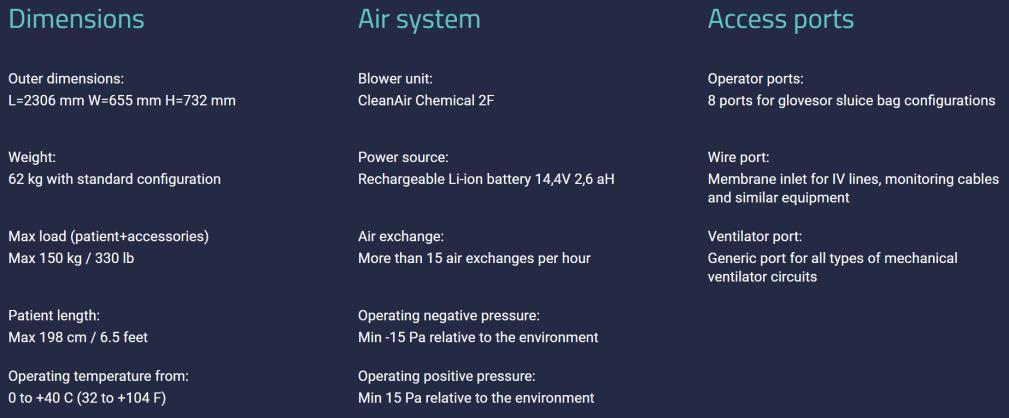
The EpiShuttle is an isolation unit designed for quick and easy transport of highly infectious and vulnerable patients.


Episode

https://open.spotify.com/episode/2e8tT7QFD3H0Gxpp9RpQKq


Episode 137: Today we have a diverse group of individuals discussing their experiences in Ukraine. Kasha, an emergency pre-hospital critical care expert, spent several months there, while Denys, a physician and medical course director, has extensive experience in training medics for the Ukrainian armed forces. Kevin, a former special agent and tactical paramedic, is currently embedded in a Ukrainian army unit conducting MEDEVAC operations. They emphasize the importance of prolonged field care (PFC) in modern warfare, cautioning against applying strategies from previous conflicts to new battlefields. They share anecdotes about challenging situations and highlight the need for medical leadership, telemedicine, proper training, and logistics in PFC. The discussion emphasizes that PFC is not limited to the military and is relevant to all medical professionals in challenging environments.
https://open.spotify.com/show/3jf8IZONKw2QiR5lkUCQDg
https://open.spotify.com/episode/419Vo5WGnpQUnKUZHo7WQh
44: Aebhric talks with Dr. Edit Gara MD PhD about the challenges found whilst providing neonatal transport.https://www.youtube.com/watch?v=t1kFC10_wZg





https://www.youtube.com/watch?v=lXfEK8G8CUI&t=513s



Structural Chemistry

Yang S, Kar S. 2023 Mar 8;1-19.
doi: 10.1007/s11224-023-02148-6.
ABSTRACT
Nipah virus (NiV) is a high-lethality RNA virus from the family of Paramyxoviridae and genus Henipavirus, classified under Biosafety Level-4 (BSL4) pathogen due to the severity of pathogenicity and lack of medications and vaccines Direct contacts or the body fluids of infected animals are the major factor of transmission of NiV As it is not an airborne infection, the transmission rate is relatively low Still, mutations of the NiV in the animal reservoir over the years, followed by zoonotic transfer, can make the deadliness of the virus manifold in upcoming years Therefore, there is no denial of the possibility of a pandemic after COVID-19 considering the severe pathogenicity of NiV, and that is why we need to be prepared with possible drugs in upcoming days Considering the time constraints, computational aided drug design (CADD) is an efficient way to study the virus and perform the drug design and test the HITs to lead experimentally Therefore, this review focuses primarily on NiV target proteins (covering NiV and human), experimentally tested studies on potential lead candidates

Journal of Special Operations Medicine

Dubecq, et al. 2023 Mar 15;23(1):84-87.
doi: 10.55460/OE4C-60HM.
ABSTRACT
Optimal pain management (TCCC), particularly in remote and appropriate treatment for prehospital analgesia of intravenous access Several (IN) analgesia in French Armed au Combat), similar to the US Medical Military Service were deployed to March 2019 and used IN ketamine a total of 259 treated casualties IN administration of ketamine 50mg appeared to be safe and effective, alone or in addition to other opioid analgesics It also had minimal side effects and led to a reduction in the doses of ketamine and morphine used by the intravenous (IV) route The French Military Medical Service supports current developments for personal devices delivering individual doses of IN ketamine However, further studies are needed to analyze its efficacy and safety in combat zones

African Journal of Emergency Medicine


Kong R, et al.
2018 Sep; 8(3): 118-122.

doi: 10.1016/j.afjem.2018.02.002.
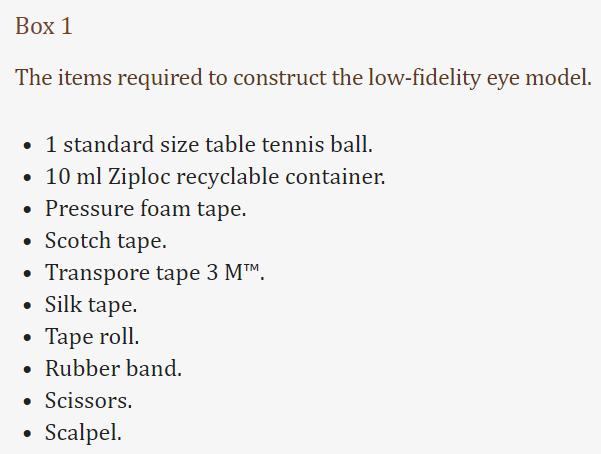
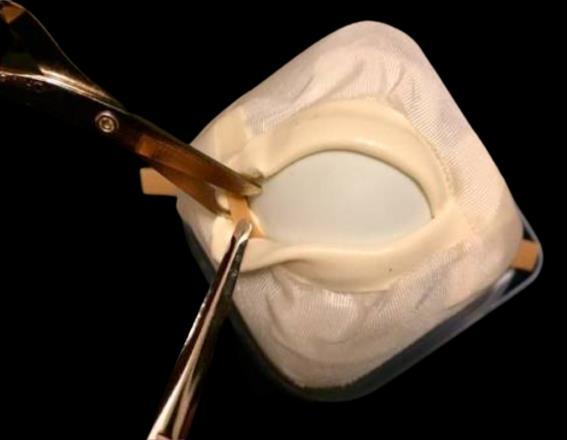
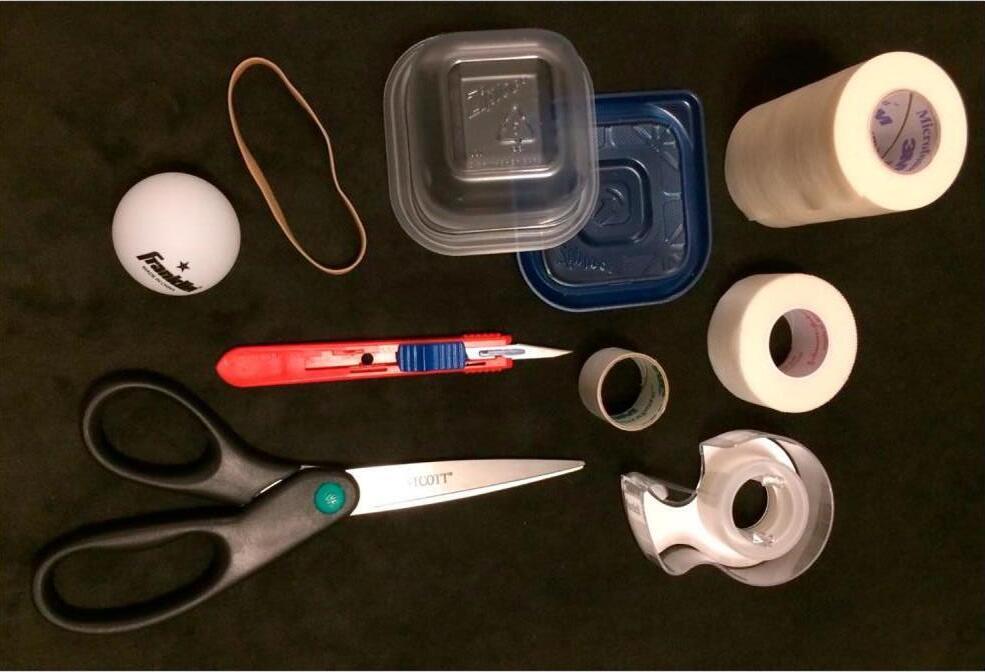
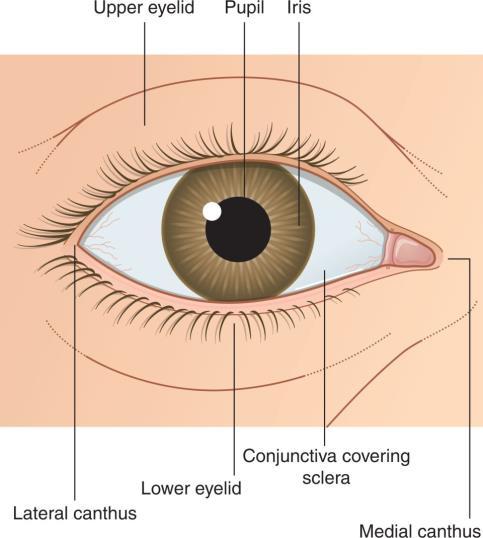
Permanent vision loss is a rare but serious complication of orbital trauma. The most reversible cause of traumatic blindness is acute ocular compartment syndrome (AOCS), usually secondary to retrobulbar haemorrhage (RBH), intra-orbital oedema or more rarely orbital emphysema. Timely diagnosis of AOCS and surgical decompression by lateral canthotomy of the ocular compartment has been shown to decrease the incidence of permanent blindness. Obtaining and maintaining procedural competency can be difficult due to the low incidence of RBH and AOCS, and the lack of access to trainers. This article discusses the construction and utilisation of a reusable non-cadaveric model, which simulates the orbital anatomy and can be used to teach and practice the lateral canthotomy procedure. This low-fidelity eye model was invented to provide clinicians with hands on training in the lateral canthotomy procedure on a reproducible non-cadaveric model. Although cadaveric models have been shown to be effective, their use has limitations: the procedure can only be performed once or twice per cadaver, and at high cost. Porcine models and commercially available high-fidelity trainers share the same limitations. This is especially problematic in resource-limited areas where it may be cost prohibitive to obtain cadavers or commercial trainers. Our low-cost reproducible low-fidelity eye model is a potential solution to this problem and can be made from materials readily available in many countries.

The American Journal of Medicine
Goddard J, deShazo R.
2023 June 21.
doi: 10.1016/j.amjmed.2023.06.002

Imported fire ants aggressively sting humans, leading to a variety of local and systemic effects. Fire ants display a behavioral adaptation to survive flooding called "rafting" bringing humans into even more contact with fire ants.

These results confirm fire ant rafts formed during flooding present a potential hazard to persons walking, wading, or boating in those areas We suggest these rafts are an under-appreciated health hazard It is reasonable to assume that people in flooded areas occasionally contact these floating rafts and are stung multiple times We provide preliminary prevention/protection recommendations for health professionals to be shared with their patients and the general public
Wilderness Medical Society Clinical Practice Guidelines

Zafren K, et al.

2023 April 30.
doi: 10.1016/j.wem.2023.02.006.
Cold and warm water immersion injuries have afflicted military personnel and civilians for centuries Nonfreezing cold injury (NFCI) can result from prolonged exposure to cold, often wet, conditions that do not cause freezing of tissue It is likely that trench foot, immersion foot, and cold immersion injury are types of NFCI Warm water immersion injuries, including warm water immersion foot (WWIF) severe tropical immersion foot (TIF), differ from NFCIs Both NFCIs warm water immersion injuries can be painful, debilitating conditions Nonfreezing cold injuries can be difficult to manage and may cause prolonged debilitating symptoms, including neuropathic pain and cold sensitivity that may be refractory to treatment Warm water immersion injuries, once recognized, can be easily treated, resolve completely, and seldom have chronic sequelae


 Review by Jason Jarvis
Review by Jason Jarvis

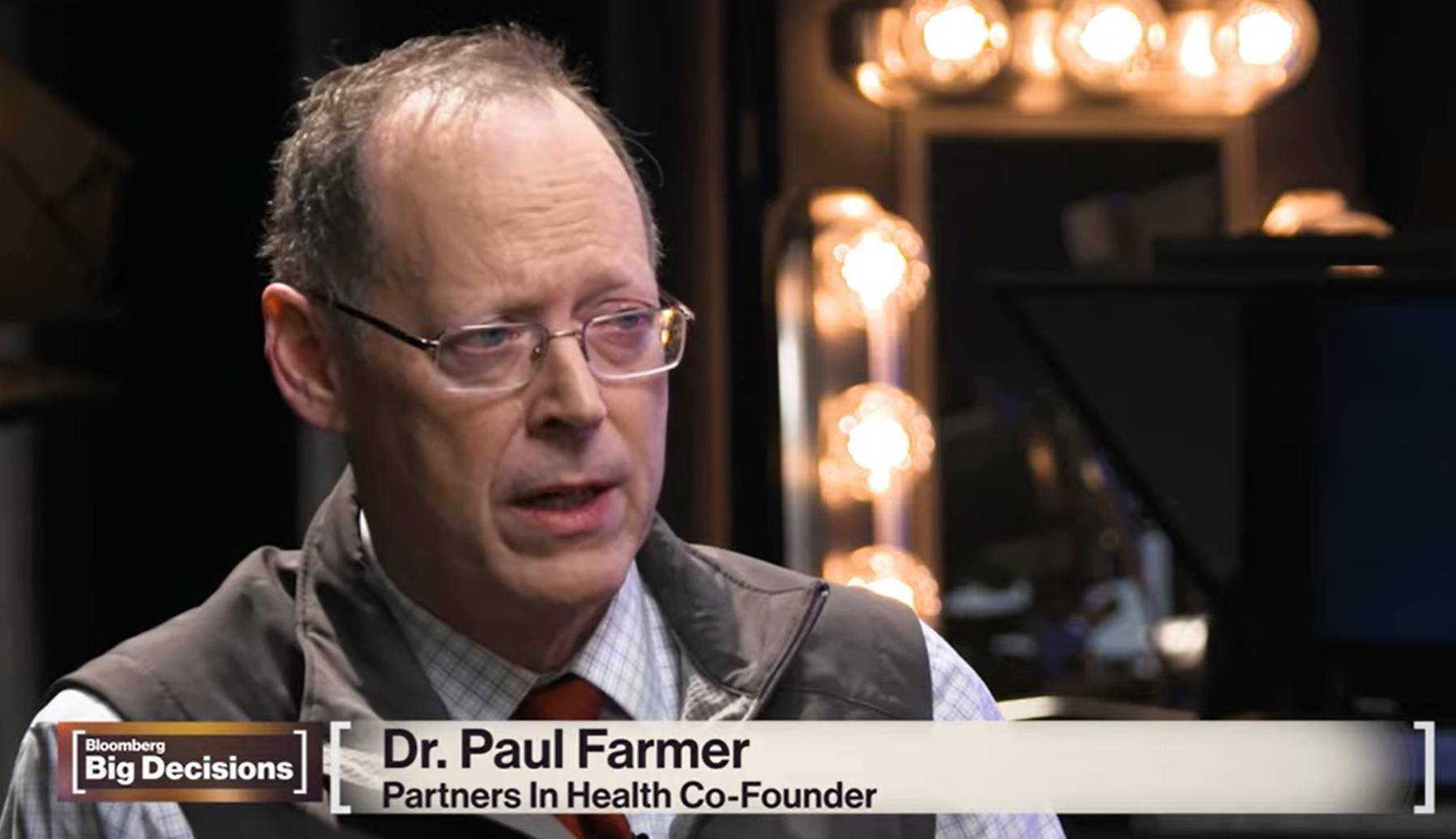
Dr. Paul Farmer stands as one of the most remarkable human beings in recent history. He embodies the modern definition of great man, which has come to mean those who transform the lives of people or society positively. In stark contrast, the premodern definition of great man typically applied to conquerors who caused untold pain and tragedy in the course of their conquests
While still a medical student, Farmer began clinical excursions into Haiti to witness firsthand “how bad things can get” and this experience was a powerful one that set the stage for his entire life.
Upon graduation from Harvard Medical School, Dr Farmer embarked upon fulltime clinical work in Haiti, essentially living in western Hispaniola fulltime. Like Dr. Gordon Seagrave (whose biography Burma Surgeon was reviewed in a past edition of The Compass) many years before him, Dr. Farmer sought out the deepest, darkest part of the inhabited world and set up his humble clinic.

Propelled forward by his charity organization Partners in Health (https://www.pih.org/) and a burning interest in infectious diseases, Dr. Farmer rose to international prominence as a leading expert in the fight against AIDS and drug-resistant tuberculosis.
Expanding far beyond the shores of Haiti, Dr. Farmer brought his vision of universal access to quality healthcare to places such as the slums of Peru and Russian prisons
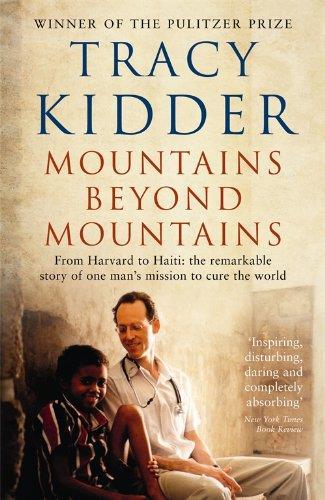
“The central character of this marvelous book is one of the most provocative, brilliant, funny, unsettling, endlessly energetic, irksome, and charming characters ever to spring to life on the page. He has embarked on an epic struggle that will take you from the halls of Harvard Medical School to a sun-scorched plateau in Haiti, from the slums of Peru to the cold gray prisons of Moscow. He wants to change the world Certainly this luminous and powerful book will change the way you see it.”
- Jonathan Harr, author of A Civil Action
Tracy Kidder author of Mountains Beyond MountainsAn excerpt from an interview with Tracy Kidder, author of Mountains Beyond Mountains
In your travels with Farmer, what most surprised and interested you? Did you learn something from the experience?
The thing about travel with Farmer is that you don’t visit the brochure sights. His itinerary is pretty much restricted to visiting hospitals, slums, and prisons. The dreadful places of the world. I hadn’t imagined that there were so many of those, and I hadn’t known just how dreadful they were.
But the trips weren’t dreary and depressing, because Farmer and his colleagues were doing something tangible, something meaningful, something that was actually improving those places. This was especially true in Haiti and Peru. I’d say that I learned two things above all. That medicine and public health are a powerful lens for looking at the world. And that a small group of determined people can actually alter some of the pictures seen through that lens.
I think that as a very young man Farmer chose to work in one of the most impoverished parts of Haiti because he was moved by the suffering he saw there. But if he’d wanted to prove a point about what is possible in public health, he couldn’t have chosen a better site. If you can do a good thing in central Haiti, it stands to reason that you can do it anywhere. And what he and his friends have done and are doing in Haiti and elsewhere - is nothing short of remarkable.
https://www.bookbrowse.com/author_interviews/full/index.cfm/autho r_number/940/tracy-kidder







The College of Remote and Offshore Medicine Foundation is an academic not-forprofit organisation for healthcare professionals working in the remote, offshore, military and security industries.


The College was founded in 2014 and is governed by a voluntary Academic Board supported by a faculty of medical professionals from four continents. The College is a Higher Education Institution registered with the Malta Further and Higher Education Authority. License No. 2018-022.
CoROM focuses on the improvement of medical training and the practice of healthcare for those working in remote, austere and resource-poor environments.
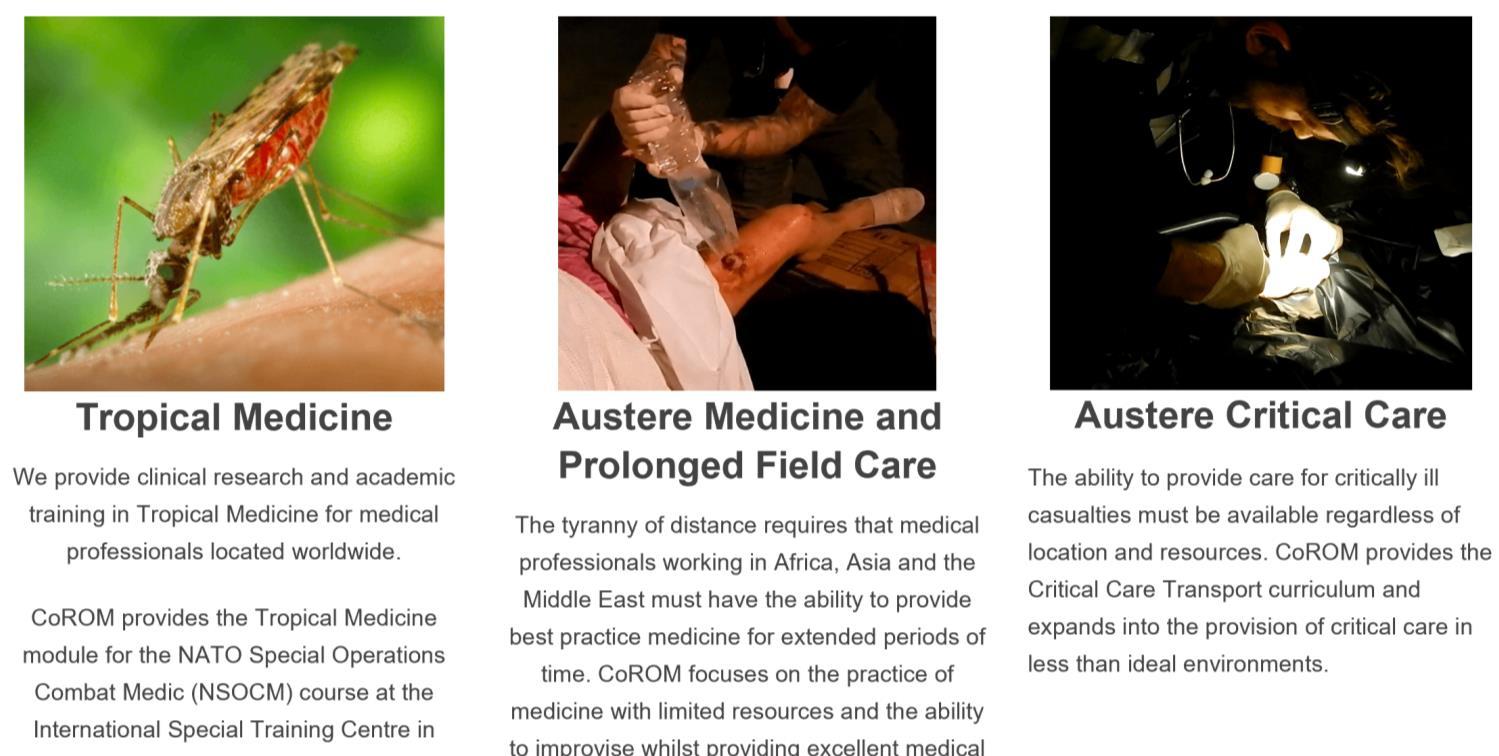
We provide clinical research and academic training in Tropical Medicine for medical professionals located worldwide.
CoROM provides the Tropical Medicine module for the NATO Special Operations Combat Medic (NSOCM) course at the International Special Training Centre in Pfullendorf, Germany.

The tyranny of distance requires that medical professionals working in Africa, Asia and the Middle East must have the ability to provide best practice medicine for extended periods of time.


CoROM focuses on the practice of medicine with limited resources and the ability to improvise whilst providing excellent medical care.


The ability to provide care for critically ill casualties must be available regardless of location and resources.
CoROM provides Critical Care Transport curriculum and expands into the provision of critical care in less than ideal environments.








MFSLR Dates TBD
TTEMS Dates TBD
NORWAY
AEC 28-31 August
NORTH CAROLINA
SOMSA Conference
13-18 May 2024

Tactical Medicine Review (O’Kelly)
Bachelor of Science Remote Paramedic Practice

Master of Science in Austere Critical Care
Master of Global Health Leadership and Practice
Doctor of Health Studies
Courses
Diploma Remote Paramedic
Higher Diploma of Remote Paramedic Practice
PG Diploma in Austere Critical Care
Diploma of Aeromedical Retrieval Medicine for Extreme
Altitude
PG Cert Tropical Medicine & Hygiene
Critical Care Transport
Aeromedical Retrieval Medicine for Extreme Altitude
Pharmacology for the Remote Medic
Minor Illnesses Course
Minor Emergencies Course
Tactical Medicine Review
Kilimanjaro Christian Medical Center (KCMC), Tanzania
Remote clinics, Northern Tanzania
Ternopil State Medical University, Ukraine
HEMS and ambulance placement, Budapest, Hungary
Kibosho District Hospital, Kilimanjaro
Ghana National Ambulance Service
TANZANIA
Clinical Tropical Medicine Dates TBD
ACC Acute Critical Care
AEC
Austere Emergency Care
ACLS Advanced Cardiac Life Support
AHA American Heart Association
APUS Austere and Prehospital
Ultrasound
ATTEMS Advanced Tropical, Travel and Expedition Medical Skills
FiCC Foundations in Critical Care (RPP203)
IBSC International Board of Specialty Certifications

MFSLR Mastering Fundamentals of Skin
PALS
Laceration Repair
Paediatric Advanced Life Support
PARSIC Prehospital Airway and Rapid Sequence Induction course
PG Cert
Postgraduate certificate
RAMS Remote Advanced Medical Skills
RMLS Remote Medical Life Support
RPP104

Fundamentals of Paramedic Practice (in-classroom)
SOMSA Special Operations Medical Association Scientific Assembly
TTEMS Tropical, Travel and Expedition
Medical Skills
For more information about training with CoROM, please visit corom.edu.mt
Contents:
Prolonged field care

Tropical medicine
Extended formulary

EMS drug cards

Calculators
Snakes & arthropods
ACLS & ECGs
Paediatric ALS
Paediatric diseases
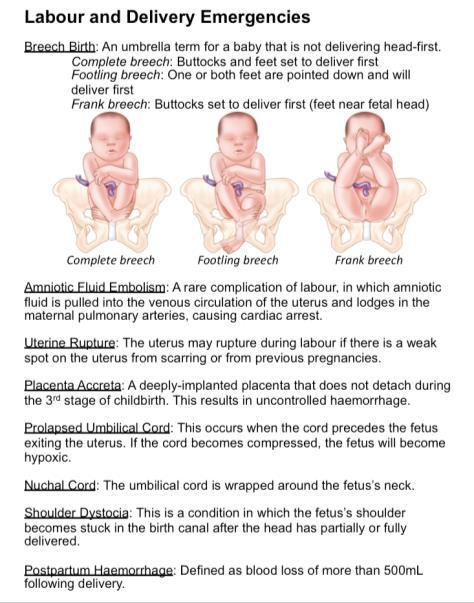
OB/Gyn
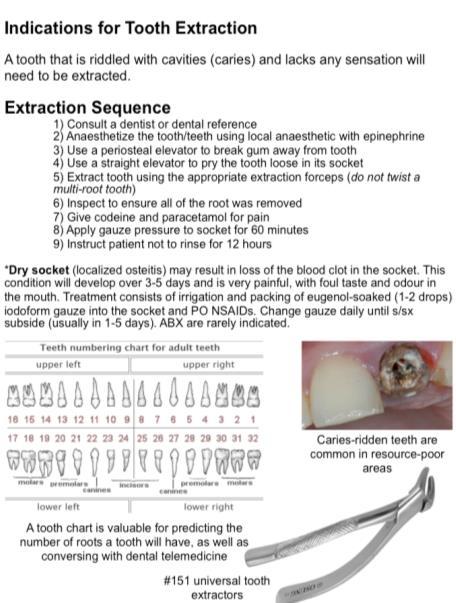
Dentistry
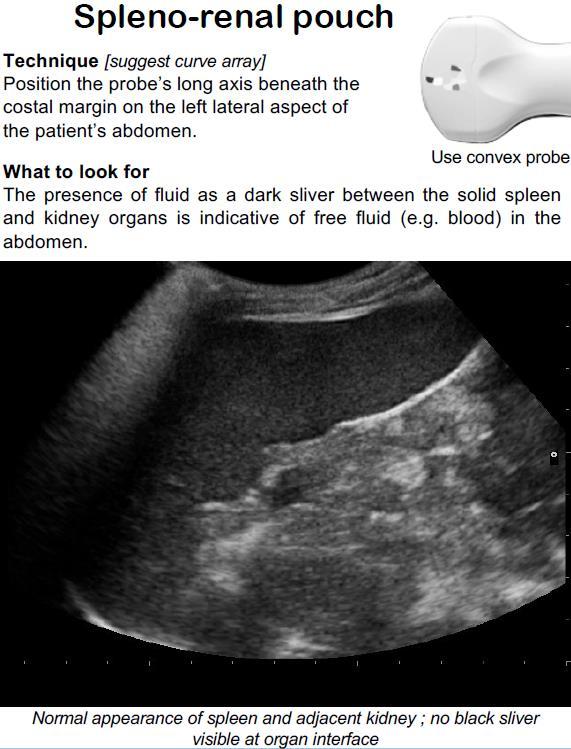
Ultrasound
Dermatology & STIs
Field laboratory
Environmental medicine
Call-for-evacuation templates

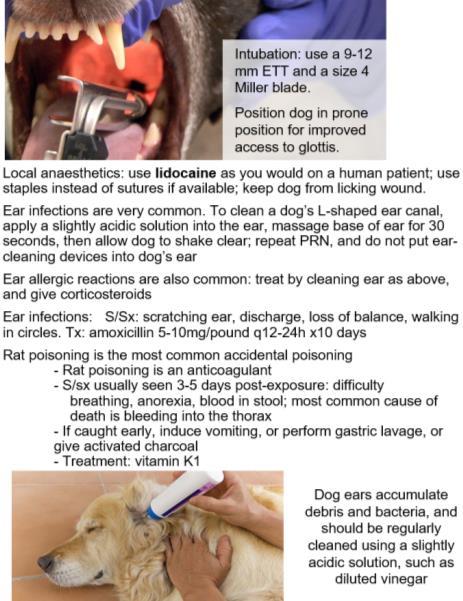
Canine medicine
…and much more!