














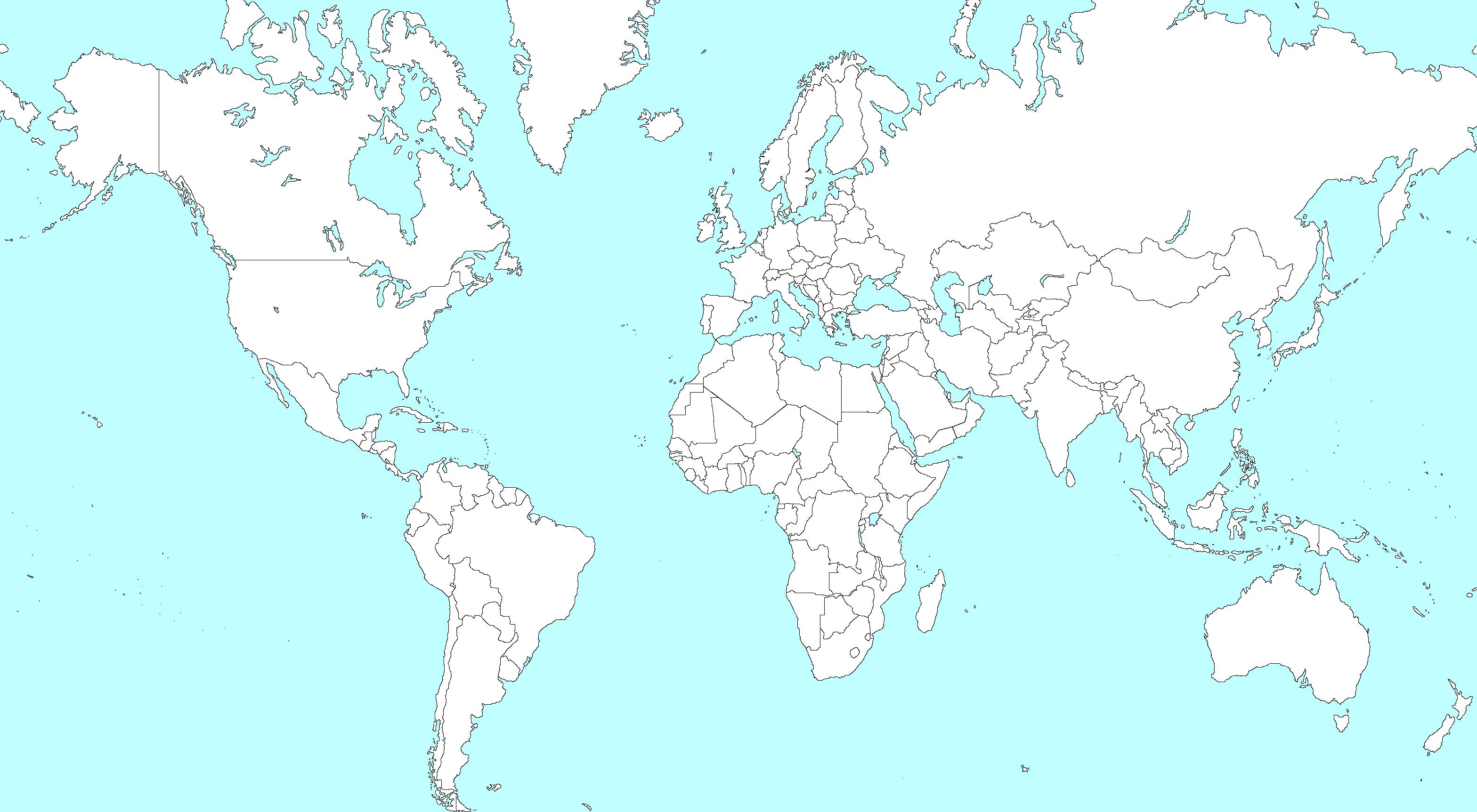
The College of Remote and Offshore Medicine is an academic not-for-profit organisation for healthcare professionals working in the remote, offshore, transit, military and security industries.

The College was founded in 2014 and is governed by a voluntary Medical Advisory Board (MAB) consisting of medical professionals from North America, Europe, Africa and the Middle East. The College has gained registration with the National Commission for Further and Higher Education of Malta to become a degree granting educational facility.
CoROM focuses on the improvement of medical training and the practice of healthcare for those working in remote, austere and difficult environments.

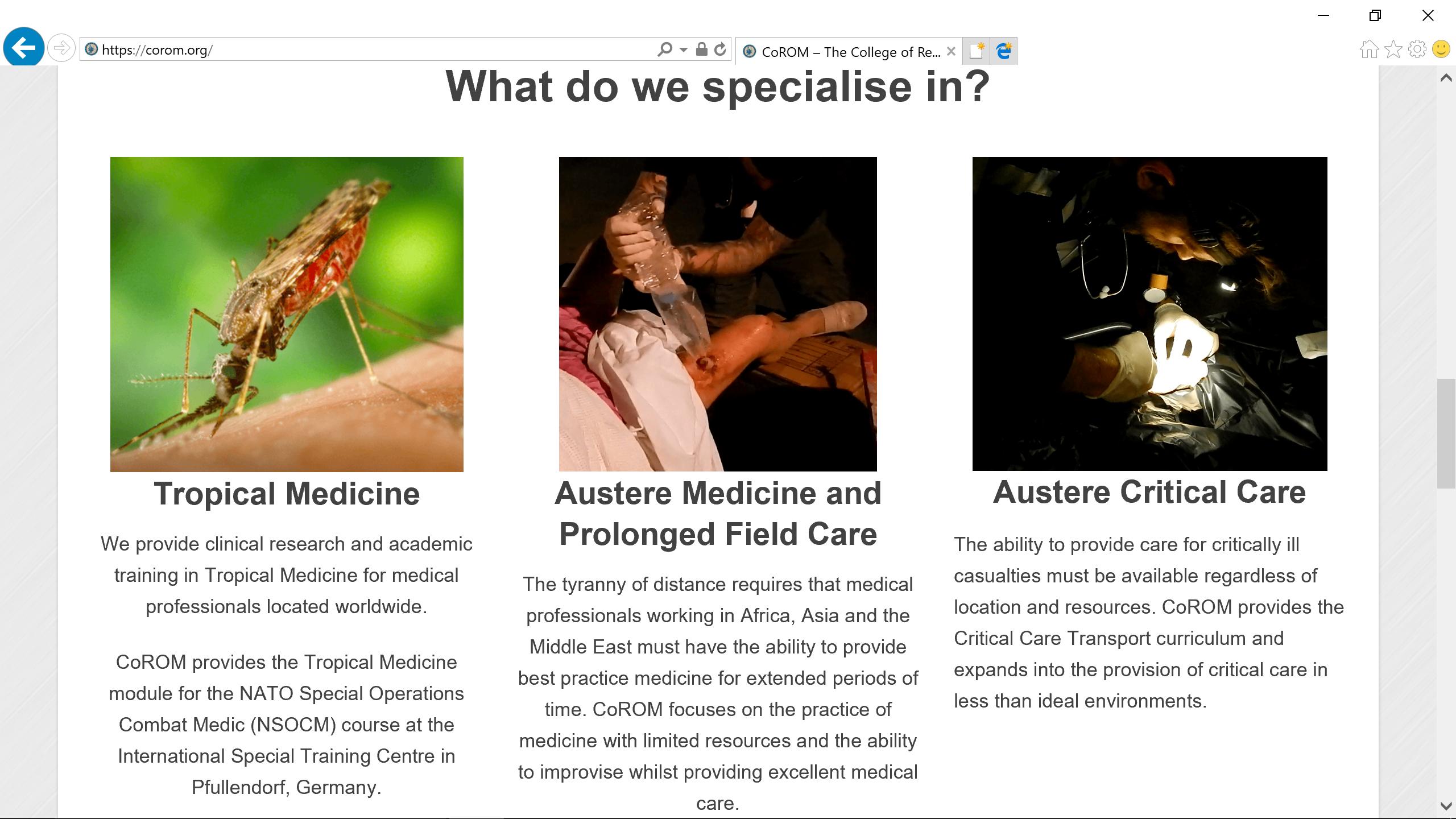
What does CoROM specialise in?
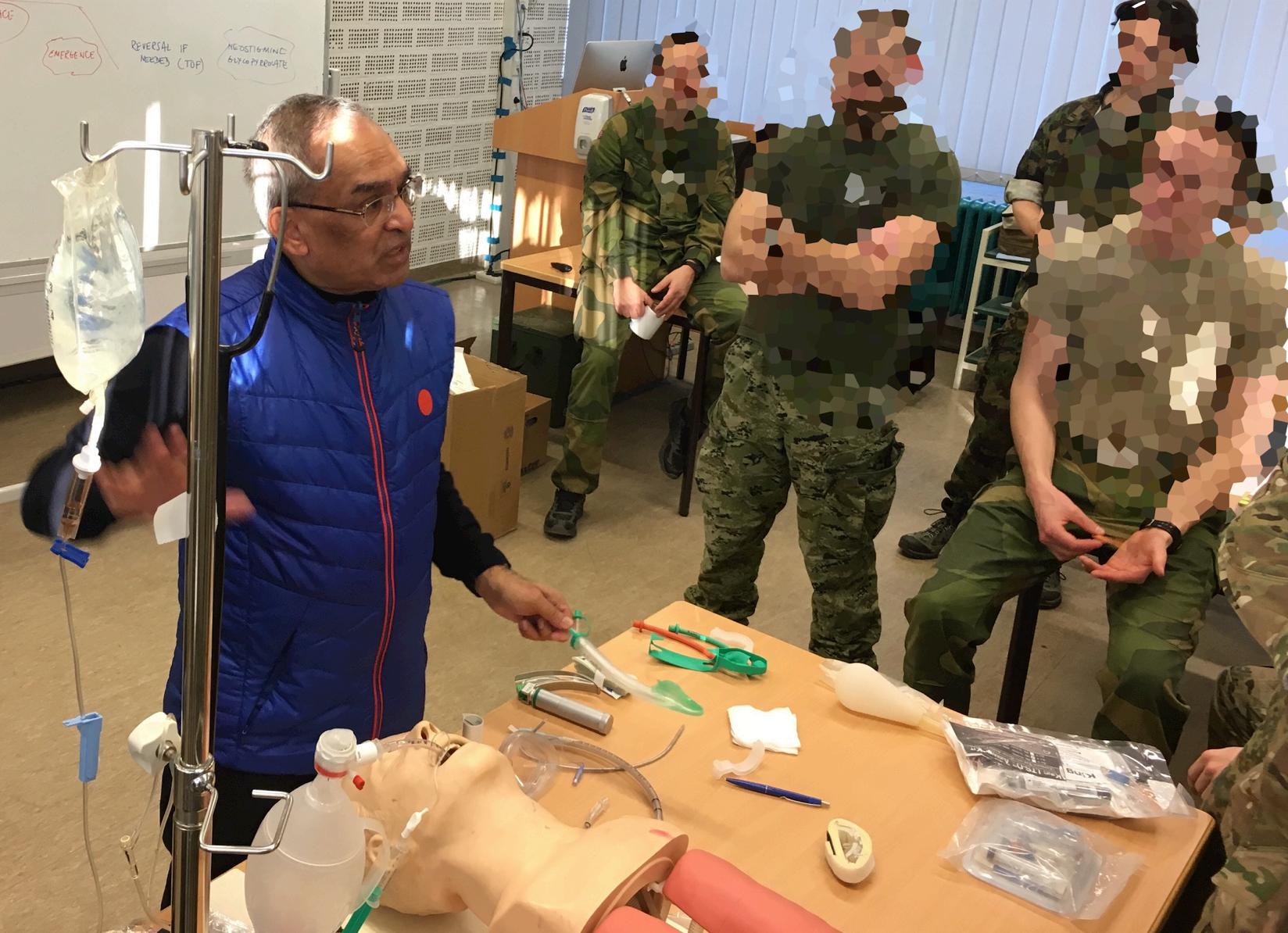
The past few months have been pretty busy for the College. Besides securing accreditation for providing EU degrees, the Ukraine Ministry of Health has asked us to be the course directors for the first paramedic course offered in Ukraine, and we have been invited back to teach on the NATO Special Operations Combat Medic course.
Starting on 1 January 2019, we are granted the right to confer undergraduate diplomas, higher diplomas and bachelor degrees. The official launch of our Diploma of Remote Paramedic Practice will launch on 1 April. The Higher Diploma will launch this autumn semester and the Bachelors in Remote Paramedic Practice will launch in early 2020. Additionally, we are working on our post graduate diplomas which will feed into the master’s degree. We will officially launch our Institute of Graduate Studies in 2020.

The MoH, in conjunction with Ternopil State Medical University, have designed and launched the first paramedic training programme in Ukraine. They have requested our College to be the course directors for the first three courses. Additionally, TSMU have been invited us back in June to run the first ITLS course in Ukraine and to set up TSMU as the first ITLS Chapter.

The NSOCM faculty have invited us back for a third year to teach the Tropical Medicine module for their programme. Additionally, we continue to support their Prolonged Field Care with three of our faculty teaching on that module. The NSOCM faculty have invited us back to run their Clinical Medicine module in 2020 as well as provide our Faculty for the PFC.
The College will be at the Special Operations Medical Association conference again this May. We will have an exhibitor’s table and will offer two pre-conference workshops: Malaria, and Tactical Medicine Review that will include the IBSC board certification exams.
We continue to grow and develop as a College and build on the efforts of our faculty. It is indeed an exciting time to be part of the CoROM family and I look forward to seeing how 2019 develops.

 Dr. Willem Stassen PhD EM Mphil EM BTEMC FP-C CCP-C
Dr. Willem Stassen PhD EM Mphil EM BTEMC FP-C CCP-C
Owing to limited critical care resources and the concentration of tertiary critical care services to urban areas, the transport of critically ill or injured patients becomes inevitable. Critical care retrieval is broadly defined as the mobilisation of specialist teams to provide life-saving care and stabilisation at a healthcare facility where the patient’s healthcare needs exceed the capability of that facility; and transport to a healthcare facility that can meet these needs.
Although, this is the case in high income countries (HICs) to some extent, low- to middle-income countries (LMICs) face particular challenges when undertaking these retrievals. LMICs often have limited road and transport infrastructure, resulting in longer transport times; have limited healthcare providers available; and limited equipment and ambulance resources. Further, critical care literature and coursework that is relevant to the LMIC setting is sparse, and access might be impossible due to pay wall policies and cost, related to economic pressures and currency fluctuations.
The College of Remote and Offshore Medicine (CoROM) aims to bridge this gap by providing high quality education to clinicians from all over the world, and improving accessibility to clinicians who are working full-time by designing courses that have an online focus, rather than extensive classroom time. By bringing together experts in retrieval, emergency medicine and critical care CoROM aims to extend its educational offering in the next academic year. We believe that by facilitating a community of shared learning, albeit virtual, we can provide opportunities for clinicians from different settings to learn from each other and build networks that can bolster the development of critical care retrieval within the respective settings. Keep an eye out for the latest news from The College on these new courses. In the meantime, you can look forward to quality education within the current course offerings.
Dr. Willem Stassen is one of the newest members of the CoROM academic board. Willem is an emergency care practitioner, primarily involved in critical care retrieval via ground, helicopter or fixed wing modes of transport. Willem holds a Masters degree in Clinical Emergency Care from the University of Cape Town, South Africa and a double PhD-degree from Karolinska Institutet, Sweden and Stellenbosch University, South Africa. Willem further holds certification as a critical care and flight paramedic with the International Board for Specialty Certification. Willem has been an instructor on the International Critical Care Paramedic course since 2015. His main research interests are telephonic disease prediction and triage, prehospital emergency care and emergency care networks, and critical care retrieval. Currently, Willem is the programme coordinator of the PhD in Emergency Medicine at the University of Cape Town, South Africa.








Emergency Medicine Services TransiRon Program 11 March – 5 April
8 April – 3 May ITLS 19-21 June
MALTA
ITLS 16 March
CRP 18 March-6 April
Pain Management 6 April
Burns 7 April
Burns 8 April
TTEMS 8-12 April
RAMS 15-19 April
FoundaRons in Crit Care 15-19 April
CC-P 22-27 April
TTEMS 27-31 May
RAMS 3-7 June
FoundaRons in Crit Care 7-11 Oct
CC-P 14-19 Oct
Remote EMT 18-23 Nov
TTEMS 25-29 Nov
Advanced TTEMS 2-6 Dec
RAMS 9-13 Dec
SEATTLE
Suturing Fundamentals 23 April
NORTH CAROLINA
SOMSA Conference 6-10 May Malaria workshop TacIcal Medicine Review with exam
CC-P: InternaRonal CriRcal Care Paramedic (with op)onal pre-study week)
CRP: CoROM Remote Paramedic*
NSOCM: NATO Special OperaRons Combat Medic course
RAMS: Remote Advanced Medical Skills
RMLS: Remote Medical Life Support
SOMSA: Special OperaRons Medicine AssociaRon ScienRfic Assembly
TTEMS: Tropical, Travel and ExpediRonary Medical Skills
TANZANIA
CRP 15 July-3 Aug
TTEMS 5-9 Aug
* The CRP course also includes 20-30 weeks of online training, plus a 400-hour clinical rotaRon.
Higher Diploma in Remote Paramedic PracIce Postgraduate CerIficate in Austere CriIcal Care

Kilimanjaro ChrisIan Medical Center (KCMC), Tanzania Remote clinics, Northern Tanzania Accident and Emergency, St. Mary’s Hospital, UK
HEMS and ambulance placement, Budapest, Hungary
Online Courses
Pharmacology for the Remote Medic
Minor Illnesses Course
Minor Emergencies Course
TacIcal Medicine Review
Level 3 Health and Safety for the Workplace
Level 3 Food Safety for the Workplace
For more information about training with CoROM, please visit corom.org
Please address newsletter correspondence to editor@corom.org.

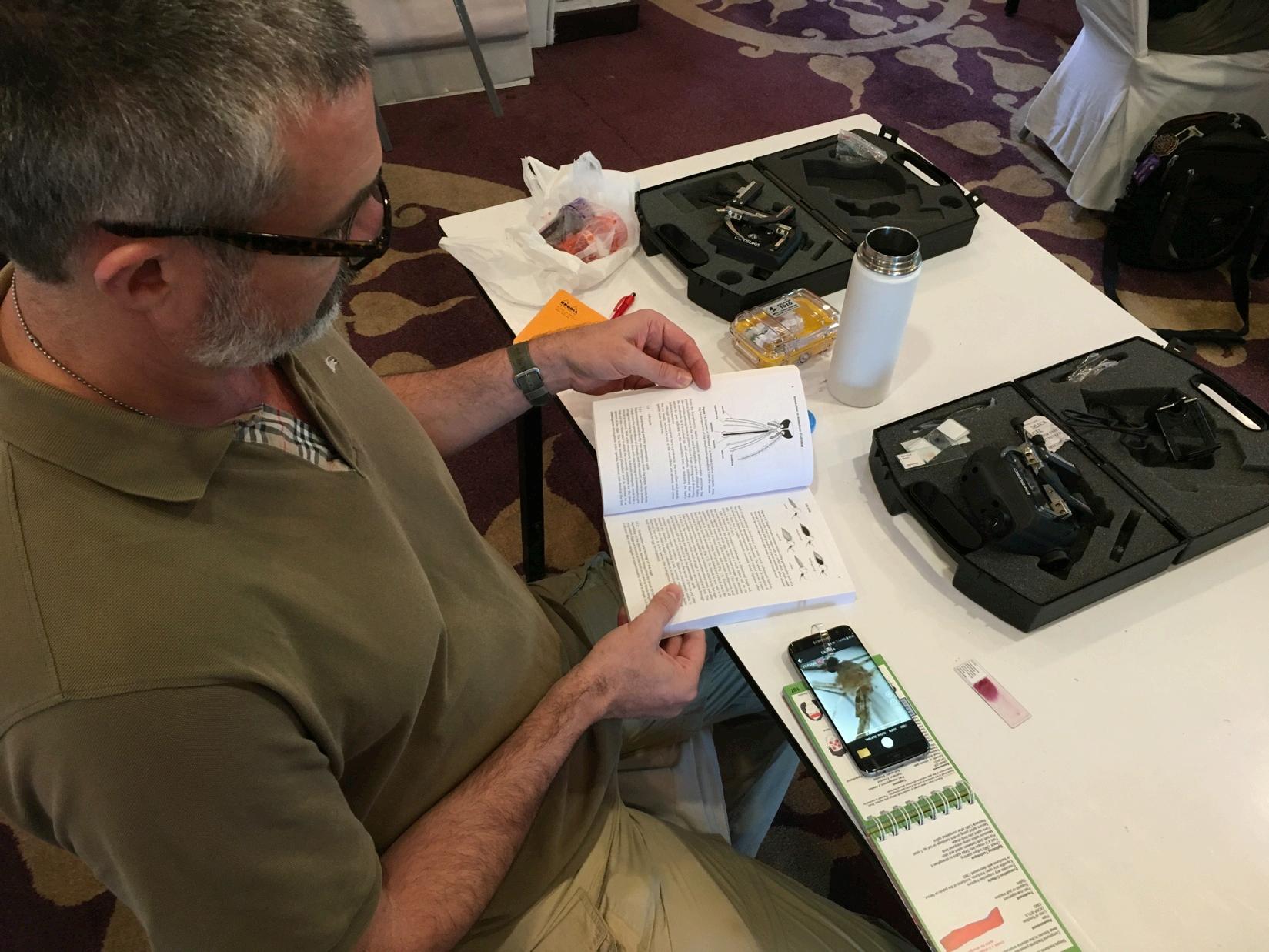
Dr. Keith Winterkorn is an American board-certified radiologist with a private practice in interventional radiology. He works in Albuquerque, New Mexico, and plans on teaching in Tanzania and Vietnam. In addition, he plans to attend the Diploma in Tropical Medicine course at the Liverpool School of Tropical Medicine.
I am an American physician who found myself at the age when many consider retiring. Yet I also found myself still eager for the challenge of something new, something that would satisfy my continued desire to help people through the practice of medicine. Years ago I had an unusual opportunity to practice ER medicine for most of a year at a small hospital on the island of St. Thomas in the Caribbean Sea. As I considered my hope for something new in my career, I also found myself longing to reconnect with that island experience....clinical practice in a resource poor land. A colleague in New Mexico in the southwestern U.S. turned out to be active in international medical relief missions. He invited me to join him on an upcoming mission to Guatemala.


That did not work out. I could not get the right time off my work schedule, and I am glad for that. I needed to update my clinical skills, especially in tropical medicine, before I could practice good medicine in a resource poor setting. I searched online. I found the TTEMS course in Malta given by CoROM. It sounded perfect to get me going in the right direction. I attended. It proved to be just the thing. The lectures were excellent, strong on the practical over the theoretical. Just what I needed. Long ago working at the ER on St. Thomas, and later participating in the early days of Interventional Radiology in remote areas of New Mexico, I learned the value of innovation, of making do with basic materials put together in new ways, the value of duct tape and pieces of wire and simple plastic tubing. The CoROM course excelled in matching the new and technologically sophisticated with the simple fact that in the field, when it all comes down on you, sometimes it’s duct tape or nothing.
At the meeting in Malta I had the good fortune to meet Dr. Francis Sakita, one of the CoROM lecturers. Dr. Sakita is Director of Emergency Medicine at the Kilimanjaro Christian Medical Center in Moshi, Tanzania. Dr. Sakita invited me to consider teaching and practicing Interventional Radiology at his center. I was able to visit Moshi in September of 2018. I hope to visit Moshi again for a few weeks in April, 2019, and in the future for longer intervals.
Two other opportunities have grown out of the CoROM course in Malta. First, I learned of the great Liverpool School of Tropical Medicine in England, which has a thirteen-week course in Tropical Medicine for medical personnel in my situation. I interviewed in Liverpool in September en route to Tanzania. My interviewer was aware of CoROM, and my experience with CoROM figured in my tentative acceptance into the Liverpool program, which I hope to attend in August, 2019.
A second opportunity grew out of sharing my experience in Malta and Tanzania with a patient of mine who is a nowretired physician from the New Mexico community. Turns out not so retired. He has become co-medical director of a hospital in Saigon, Vietnam. He has invited me to consider teaching there based on my experiences and plans. Mixing time between Vietnam and Tanzania, with maybe a visit or two home would suit me fine.
Thank you, CoROM.
Dr. Danielle Wilhelm is an American board-certified Emergency Medicine physician who is now living in Germany. She recently returned from a deployment to Iraq with an expeditionary medical unit. Since then, she has been working on her PhD in International Health in Heidelberg, Germany.


What aspect of CoROM moRvated you to join the College?
Once I finished my residency in Emergency Medicine, I found myself working almost exclusively in hospitals. However, I would find myself working in remote settings during deployments and humanitarian missions which required a different set of skills. Through my work with CoROM, I realized I could keep up those particular skills through teaching while learning new skills at the same time. I realized how much I missed the work outside of a hospital environment.
What is your favorite teaching topic at CoROM?
I really enjoy the tropical medicine topics. It’s something I don’t get to see very often in the hospital, but tropical diseases are so important to be able to identify in remote areas. This is a topic that is frequently discussed in International Health research, but it is often neglected outside of small interested groups. It’s encouraging to see this being taught to medical providers who will likely come into contact with these diseases and possibly seeing it for the first time in their careers.
Where would you like to see CoROM go in the next five years?
It would be nice to see CoROM continue to expand to other countries and other locations for instruction as it has over the last 5 years. I definitely enjoy teaching remote paramedics as I often learn quite a bit myself during these courses. Knowing this, I would also like to see a specialty course geared towards physicians who may find themselves far outside their comfort zone when supporting a remote mission or supporting paramedics working in these environments.
 Dr. Danielle Wilhelm MD MSc CoROM Faculty
Dr. Danielle Wilhelm MD MSc CoROM Faculty
Describe a medical case that has had a lasRng impact on you.
During my Emergency Medicine residency, I spent a month in The Gambia teaching ultrasound at a hospital in a small village. I was unprepared for how little resources were available, but the only way you can every really prepare for these settings is to experience it first-hand. We had an infant brought into the hospital who likely had cerebral malaria. It was my first day and I froze. I was outside of my comfort zone and didn’t even know what medications were available to give to the patient. The local nurses provided care, but I always felt I should have done more. The infant was very far progressed in the course of the disease and the unfortunate outcome would have likely been the same, regardless of what else I had done in that moment. When I explained the case to the nursing supervisor at the hospital, he told me, “You can always do something”. That has stayed with me throughout my career. I have been in situations with a patient who is rapidly deteriorating more times than I can count, but I always try to do what I can in that moment. And more often than not, there has been a good outcome. Nurses have told me that I never appear to be afraid to jump in. The reality is every Emergency Medicine physician, including myself, experiences fear when confronted with a critical patient, but the fear of looking back and wondering if there was more you could have done is even greater.
What are your three go-to medical references for remote deployments?

I’m a big fan of podcasts as I do a lot of traveling on the train. But personal favorites are ER Cast and Emergency Medicine Cases. Some of the episodes are geared towards the ER physician, but they have great ones for all emergency providers such as “Gunshot to the groin,” “Thombolytics for Frostbite,” and “Trauma- the first and last 15 minutes.” I’m also a big fan of apps, since books take up too much room and weight when traveling. Of course, that also means having a reliable electricity source. My favorite apps include ERres and Epocrates. Finally, when working all over the world you need to be able to communicate. Google Translate works well when you have a Wi-Fi connection, but dict.cc allows you to download a number of bilingual dictionaries that can be used offline.

Greetings from the land of Kilimanjaro!
In this edition of the Compass, I will be sharing a case which presented to the KCMC emergency department after being referred from a peripheral hospital. The patient was a 31 yearold female who presented with a complaint of coughing nonbloodstained sputum for one month; this was accompanied by shortness of breath in the supine position and central chest pain. The patient denied history of fever, night sweats or loss of weight. The primary survey was unremarkable except for distended jugular veins and crepitations on the right supramammary region.
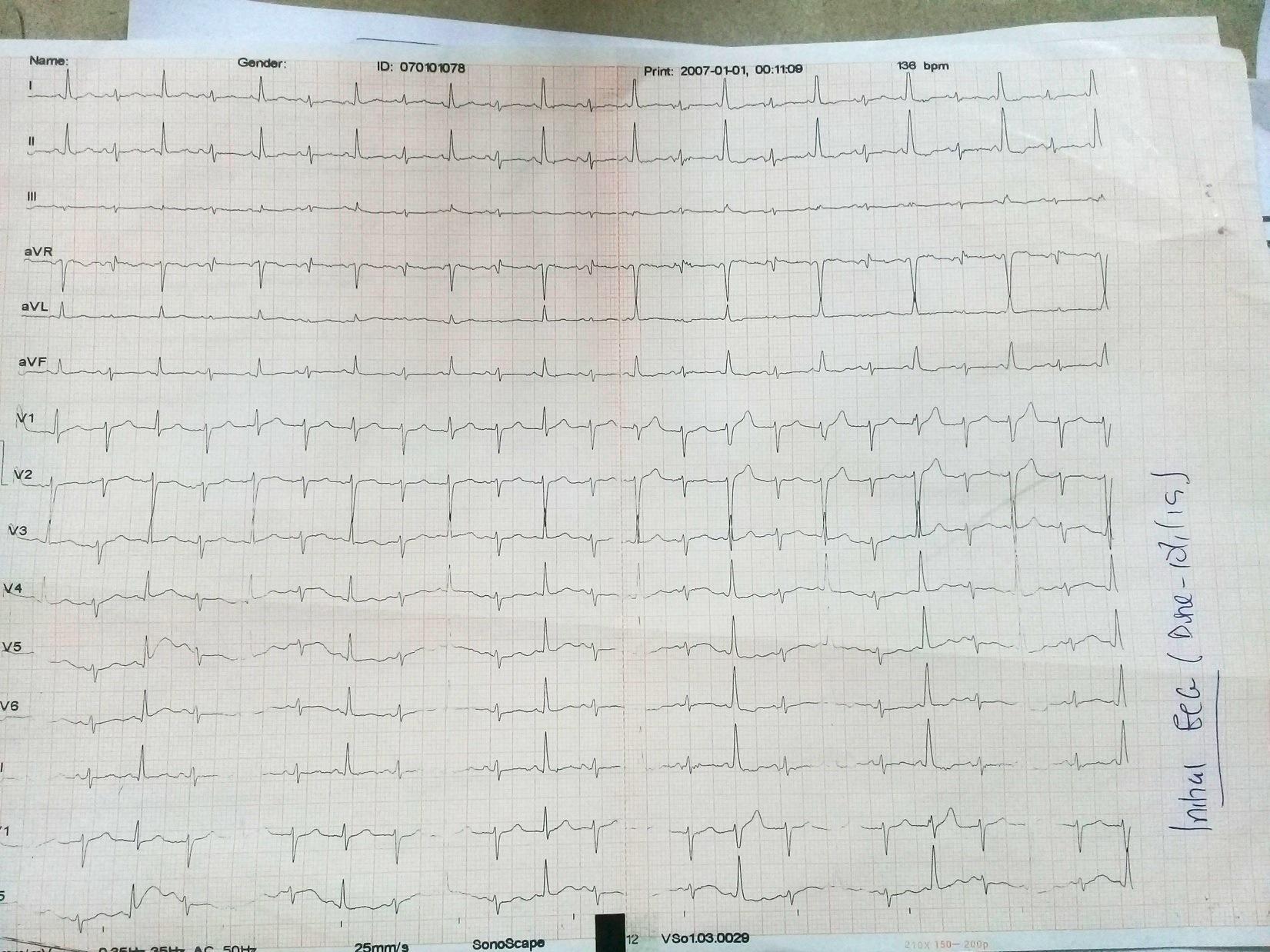
 Dr. Francis Sakita MD, MMED Emergency Physician Head of ED-KCMC CoROM Faculty
Dr. Francis Sakita MD, MMED Emergency Physician Head of ED-KCMC CoROM Faculty

Vitals signs were: BP 90/50 mmHg, HR 129, RR 30, SpO2 94% on room air, and a temperature of 37⁰C.
Secondary exam revealed muffled heart sounds and a distended abdomen due to ascites.
Bedside ECG revealed sinus tachycardia, low voltage rhythm and electrical alterans (see below).
These findings prompted us to perform a bedside cardiac ultrasound which showed massive pericardial effusion with RV collapse (see below).
Ultrasound-guided emergency pericardiocentesis through the subxiphoid region was performed and approximately 300ml of hemorrhagic fluid was drained. Immediately after draining the effusion the patient’s blood pressure and heart rate normalized.

Take home points in this case: early identification and treatment of pericardial effusion (and the skill set needed to interpret the ECGs and performing the bedside/field ultrasound) can save lives.
Follow-up: The patient was admitted at the ICU for several days where she was
The indications, tools and techniques for the decompression of a tension pneumothorax has been a lively topic of discussion for as long I’ve been a medic (22 years).
As I continue to work with healthcare practitioners across a broad international spectrum, many tips, tricks and theories float to the surface: “leave the needle in after decompression,” “take the needle out,” “leave the cannula in,” “take the cannula out,” “leave the cannula in with a 3way stopcock (or glove finger) attached,” “go lateral chest, not anterior chest,” “push the entire needle in,” “push the needle just deep enough to get air out,” “use a saline-filled syringe to visualize the air escaping,” etc. There are many who still list the late sign of tracheal deviation first when asked about signs and symptoms, and most do not consider the possibility of a needleobstructing “skin plug.” Note also the frequently-suggested notion that the immediate relief of a tension pneumothorax is not needle decompression but placement of a chest tube.
 Jason Jarvis 18D BS NREMT-P TP-C CoROM Tropical Medicine Lead The Compass editor
Jason Jarvis 18D BS NREMT-P TP-C CoROM Tropical Medicine Lead The Compass editor
The one item that was not much scrutinized – until recently – was the actual piece of equipment doing the decompressing. For decades, the 5cm (2 inch) 14-gauge angiocath has been the go-to device. Along the way, frequent failure to reach the pleural space due to the thick musculature of the anterior chest wall in the military population was addressed by simply adopting the more robust 8cm (3.25 inch) angiocath. Those who eschewed this longer, more expensive (and essentially single-purpose) needle simply shifted to the lateral chest decompression site at the 5th intercostal space along the anterior axillary line, which also happens to be the default chest tube insertion site. Besides allowing the practitioner to continue using the cheaper and more commonplace 5cm needle, the lateral decompression site possesses the advantages of being markedly thinner than the anterior chest in practically all patients, while being unobstructed by body armor plates.
A recent article* in the Journal of Special Operations Medicine studied alternative devices to the traditional 14-gauge angiocath using animal models. The device with the highest rate of procedure failure turned out to be the ubiquitous 14-gauge angiocath, while the device with the lowest rate of procedure failure was the laparoscopic trocar, carried into the field by very few that I am aware of A synopsis of their results is depicted below. Higher rate of failure Lower rate of failure



*Journal of Special Operations Medicine, Winter 2018. “Large-Caliber Alternative Devices for Decompression of Tension Pneumothorax in the Setting of Hemorrhagic Shock.” Christian S. McEvoy, et al.



It’s an exciting time here as we are about to launch the Higher Diploma in Remote Paramedic Practice (HDip RPP). It’s the culmination of several years work that has seen CoROM develop and then get approval for the programme, which has been recognized by the National Commission for Further and Higher Education in Malta. This means that the programme is a recognized third level qualification, and will carry European Credit Transfer System points, just like all other College level courses in the EU.
The programme will be of two years duration, and a student wishing to exit at the end of Year One may do so and receive a Diploma in RPP, assuming they have met the requirements.
Our official launch date is April 1st, and that is the date that will see the first cohort of students start the programme.
In addition, CoROM Faculty are busy designing not one but three post-graduate certificate programmes…more on that later.
This is a huge step for CoROM and allows us for the first time to award a formal academic qualification to the Remote and Austere Medic, which is a big step towards the recognition of this specialisation within paramedicine.

There is an old saying, “May you live in interesting times.” If you are a remote paramedic, we are living in interesting times!

At an outreach clinic in a Peruvian slum, one of your colleagues asks for your assistance interpreIng the following ECG. This paIent is most likely suffering from what condiIon?
A. Second-degree heart block type 2
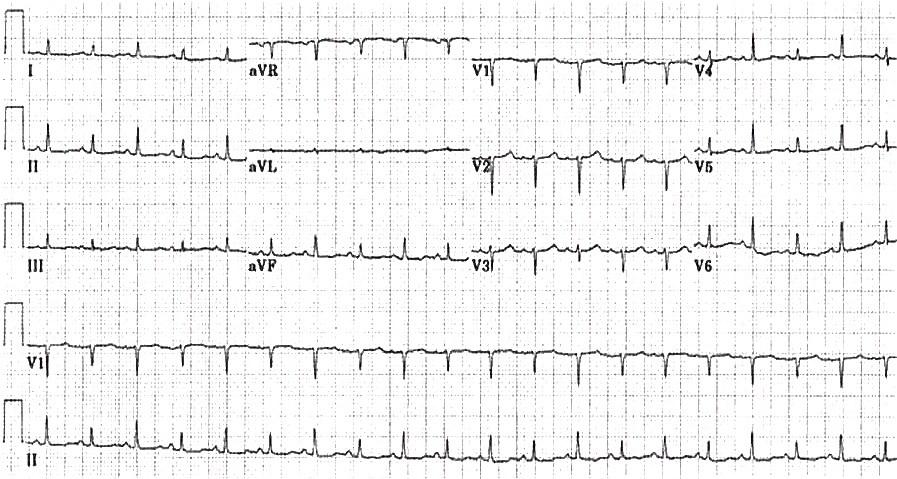
B. Severe hypothermia
C. Pulmonary embolism
D. Pericardial effusion
While gearing up for a boat dive in the Red Sea, one the divers comes to you with a burning rash on his arm, with what appears to be a small bite in the center of it. He says “something” bit him a few hours ago as he was trying on a rental wetsuit in the dive shop. He denies any constitutional symptoms, and did not see the offending creature. You most strongly suspect:
A. Lonomia caterpillar envenomaIon
B. Sandfly bite
C. Scorpion sIng
D. Recluse spider bite


Answers to “Test Yourself” from the previous issue: ECG : A. Increased intracranial pressure
Drug calculaRon: Ketamine infused at 18 drops/minute
While bivouacked on a kayak expedition around Greenland, one of the expedition members cuts her thigh with a knife while opening a food ration pack. You stop the bleeding with application of direct pressure, and note that her laceration is only 5mm in depth with no distal circulatory/sensory/motor compromise. The skin edges do not approximate in situ, so you decide to close the wound using nylon sutures. Your only remaining stock of lidocaine is a partially-full bottle containing 16mL, and it does not contain epinephrine. In order to obtain an appreciable level of vasoconstriction during the suturing procedure, how much epinephrine 1:1000 would you add to the lidocaine to create an anaesthetic solution containing the standard concentration of epinephrine 1:100,000? Answers will appear in the next ediRon of The Compass
Clinical case: Ctenocephalides genus flea (cat flea); endemic (murine) typhus


Medical References (Dr. Danielle Wilhelm’s picks)

available from Pyng Medical

The Fast1® intraosseous device offers vascular access via the manubrium, a site not available to the majority of the intraosseous devices in common use. The manubrium is a highly vascularized bone with an infusion flow rate matching most peripheral intravenous sites. The device may be inserted into the bone with or without a local anesthetic, and infusion of fluids is painless if done correctly.

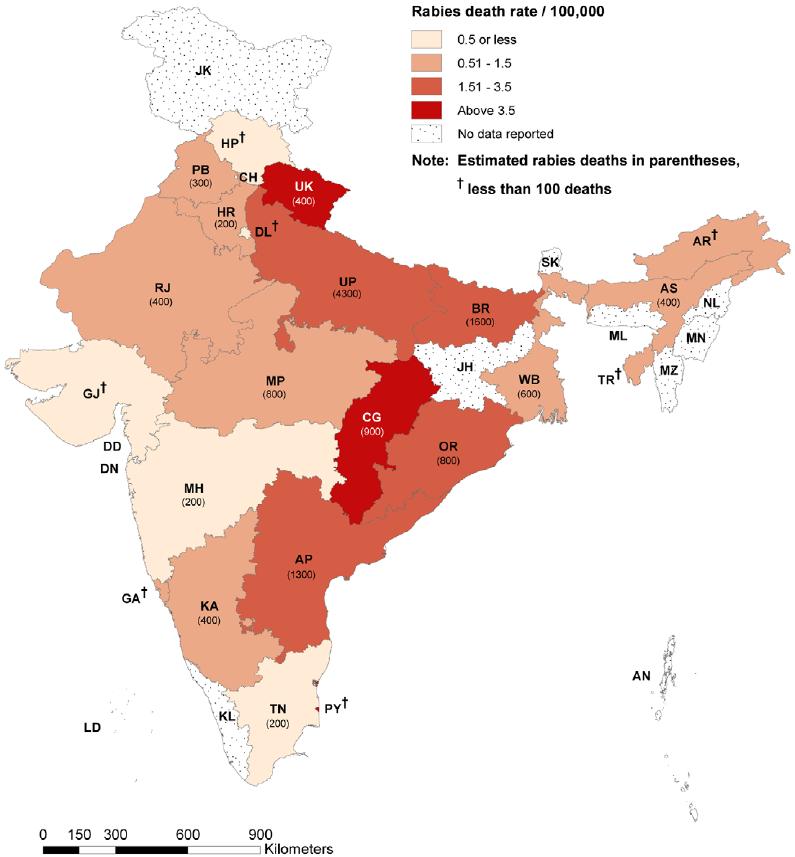
American Journal of Tropical Medicine and Hygiene. January 2019 Volume 100, Issue 1, pages 165-169. hnps://doi.org/10.4269/ajtmh.18-0711. Reeta S. Mani, et al.
Rabies, an acute progressive encephalitis, continues to be a serious public health problem in India and several other countries in Asia and Africa. Survival is rarely reported in rabies, which is considered to be almost universally fatal. We report the clinical and radiological findings of eight patients with laboratory-confirmed rabies who survive the illness. With the exception of one patient who recovered with mild sequelae, all survivors had poor functional outcomes. The reported survival from rabies in recent years may reflect an increased awareness of the disease and greater access to better critical care facilities in rabiesendemic countries. Nonetheless, there is an urgent need to focus on preventive strategies to reduce the burden of this dreadful disease in rabies-endemic countries.


Annals of Emergency Medicine. DOI: hnps://doi.org/10.1016/j.annemergmed.2018.07.018. Gonlieb, M; Goldstein, C; Ward, E.

Compared with conservative oxygen therapy, liberal oxygen therapy is associated with increased mortality without improving other patient-relevant outcomes.
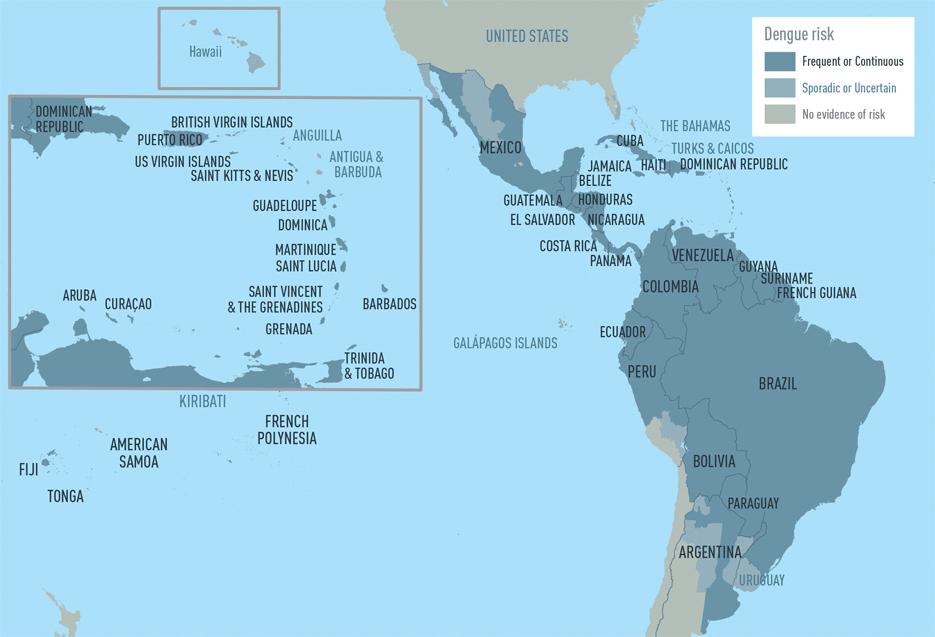
Public Library of Science.
January 22, 2019.
hnps://doi.org/10.1371/journal.pmed.1002726.
Aubree Gordon, et al.
ABSTRACT
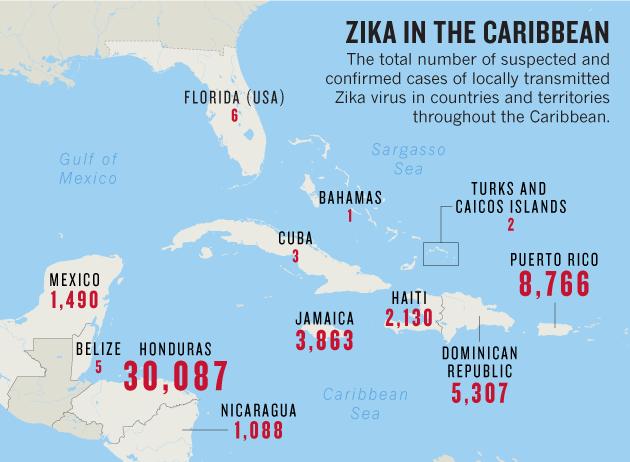
Zika virus (ZIKV) emerged in northeast Brazil in 2015 and spread rapidly across the Americas, in populations that have been largely exposed to dengue virus (DENV). The impact of prior DENV infection on ZIKV infection remains unclear. To study this potential impact, we analyzed the large 2016 Zika epidemic in Managua, Nicaragua, in a pediatric cohort with well-characterized DENV infection histories.
Journal of Anesthesiology. Volume 6, Issue 1, June 2018, pages 15-25.

Doi: 10.11648/j.ja.20180601.14. Open access.
Rabiu Musa Kutama, et al.
ABSTRACT
Nigeria is naturally blessed with both savannah and tropical rainforests vegetation and these offer a wide distribution of plants believed to possess secondary metabolites which are responsible for treating or curing various diseases. Several researches have been carried out in order to explore and identify the chemical compositions responsible for various pharmacological activities in Nigerian medicinal plants. This paper discussed the meaning and historical development of medicinal plants. A brief account of phytochemicals (alkaloids and flavonoids) were also given. The plants presented in this paper confirmed the pharmacological activities of these plants and includes: anticonvulsant, antioxidant, antibacterial, anxiolytic, anti-inflammatory, antiulcer, anticancer, antiplasmodial, antitrypanosomal, antityphoid, antitumor, antileishmanial, antidiarrhoeal, antidiabetic, antituberculosis, analgesic as well as others.

Best practice medicine in the modern era is characterized by the supremacy of double-blind randomized controlled trial studies. Before this period, clinical experience reigned supreme. A prominent member of the Norwegian THOR network said as much when he recommended PPG-2266 to me at a SOMSA medical conference two years ago.
“Read about Dr. Amosoff in PPG-2266,” he said. “He spent years doing surgeries on wounded soldiers by the trainload. Of course, his experiences don’t count for anything nowadays, because he wasn’t doing double-blind studies at the time.”
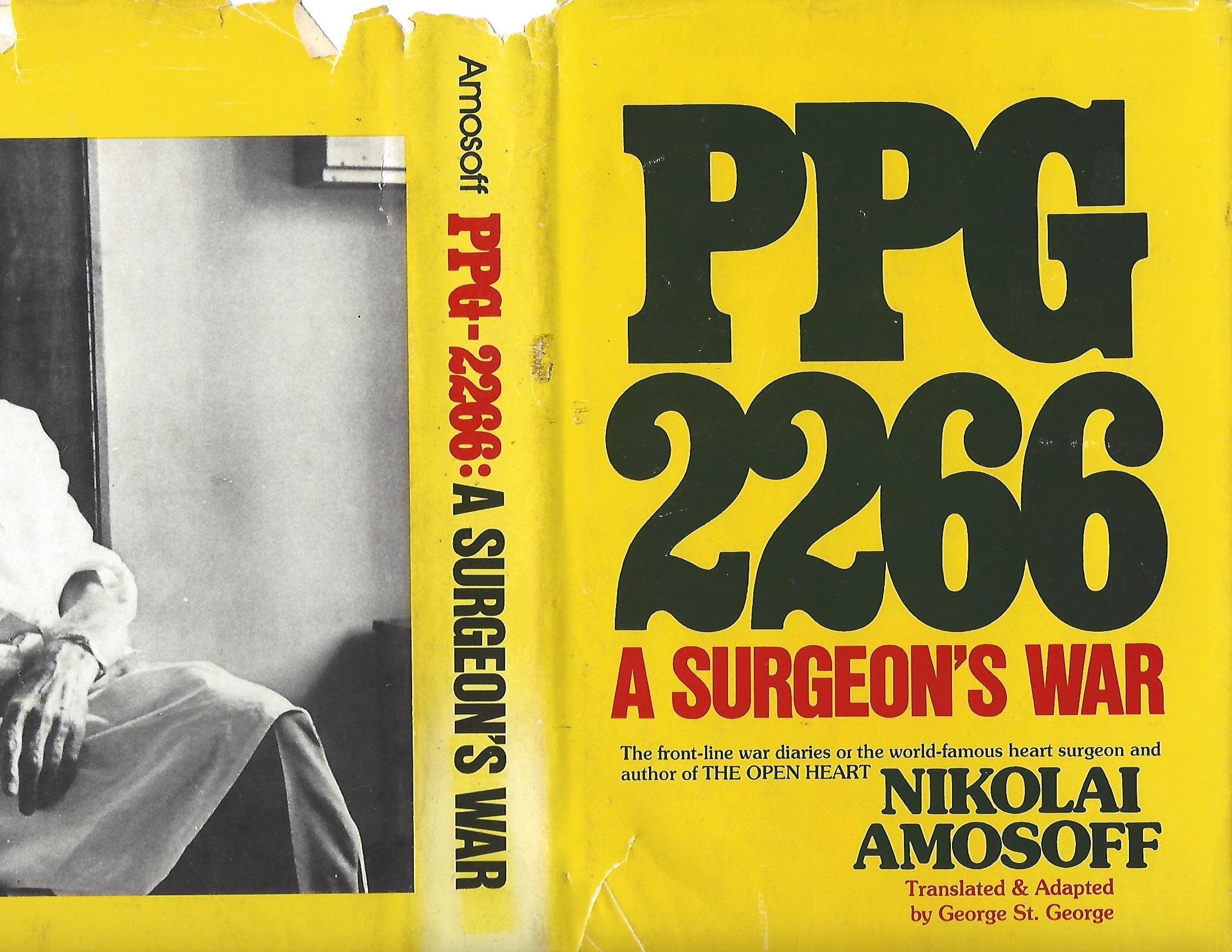
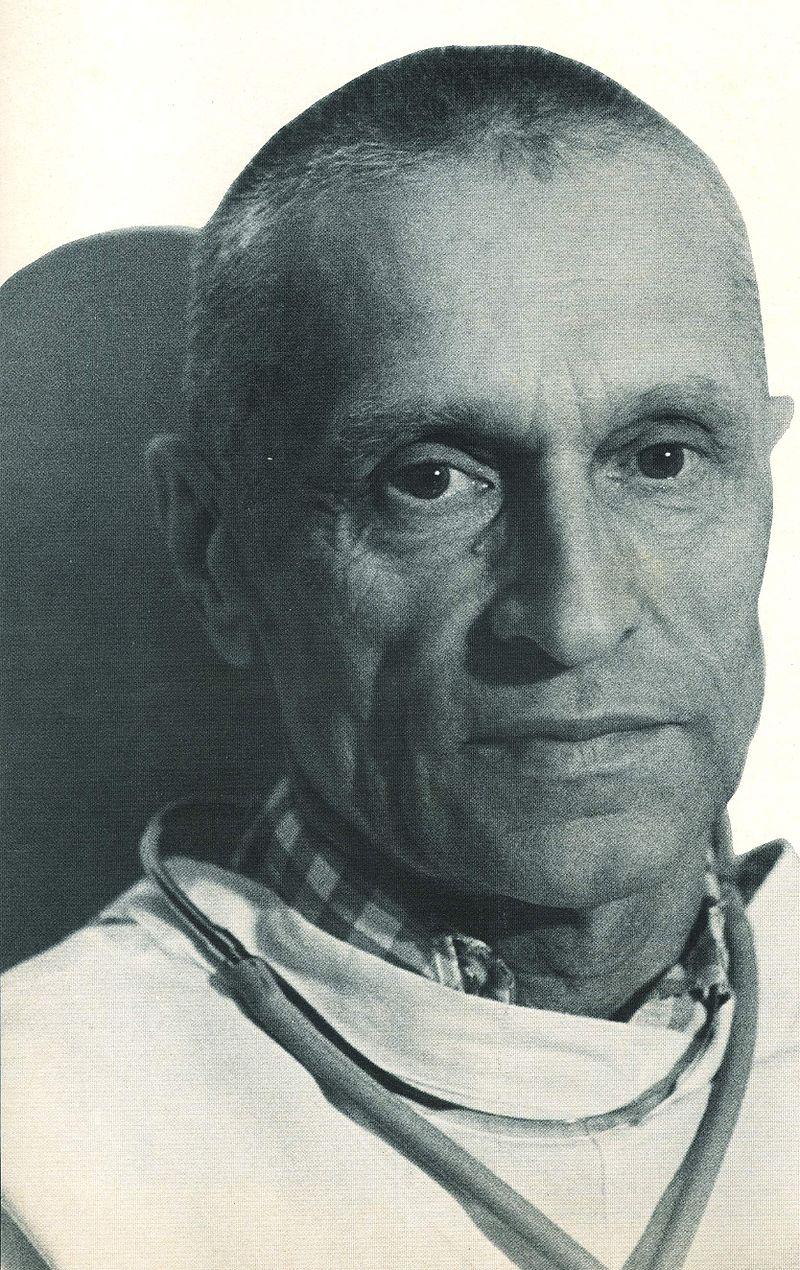
PPG-2266 (Mobile Field Hospital #2266) is the Soviet horse-drawn field hospital in which Dr. Nikolai Amosoff worked from the outset of the World War II German invasion into the Soviet Union until the fall of Berlin. The book itself is Dr. Amosoff’s translated war diaries, a treasure trove of lessons learned.
PPG-2266 follows the ever-shifting front lines of the Red Army, detailing surgical cases, lives saved and lost, mistakes made, rampant gangrene, lice and maggot infestations, uncounted amputations, and a formidable trifecta of hardships: sleep deprivation, food shortage, and the notorious Russian winters.
A keen observer of both the people around him and history, Dr. Amosoff offers the following synopsis of the progress of surgery through the ages:
“Historically, the Russian medical services have always lagged behind. The Crimean campaign...Professor Pirogoff, ‘the father of Russian surgery.’ Doctors in dirty military jackets probed all wounds to remove bullets. The results were disastrous. Almost all cases with injured bones died of infection. And of course nearly all amputees.


The Turkish war of 1878. A new theory: touch the wounds as little as possible. The results were slightly better. By then we knew of Pasteur and Lister.
The Russo-Japanese war. The Russian disgrace. Only the most pressing surgery. The goal was evacuation, evacuation of all cases. The result – gangrene.
World War I. The corrupt czar’s system could not organize military surgery. They performed only the most pressing field surgery, and then, evacuation. Gangrene took a tremendous toll. Nearly all abdominal wounds were fatal. And yet, in the West, particularly in France, things were different. All serious cases were operated on, at once, during the first few hours. And the results were remarkably successful.
During the Civil War there was practically no surgery. Fronts were changing every day. All one could hope for was evacuation of walking wounded cases. Doctors worked honestly, even though they often cursed the Bolsheviks.
Since then, there has been a great improvement. The present Medical Service of the Red Army is a far cry from our dismal past. We have enough personnel, enough equipment. It is up to us surgeons to prove our worth.”
The following passage captures the hardships endured by both the Soviet wounded and their caregivers at PPG-2266:
“But before starting to function as a surgical unit we have to feed the wounded...they counted 320 cases in 28 houses. Chapliuk has cooked the gruel, but doesn’t know how to distribute it. We left our food cans behind at Russky Brod. We start to distribute it in old helmets and water pails, and it is not until afternoon that we feed everyone - dry bread and cold gruel.
While they are setting up our dressing station, I look into the neighboring peasant huts. Absolutely horrifying scenes. All the wounded must be urgently attended to. They are lying in makeshift bandages put on by front-line medics. No way of knowing how many might be developing gangrene. Those who can move are attending to the stoves. Very dangerous. A fire would lead to a terrible tragedy, but there is no other way.
During the day we operate on only four cases. One is a chest wound. Two walking wounded actually drag him in. He is gasping for breath and has almost no pulse. We put him on the table and remove the bandage. It is horrible. The entire right side of the chest is a horrible wound...broken ribs...gray, pulsating lungs. We clean the wound and remove broken pieces of ribs, but we cannot close the wound. We just apply a tampon, put on a tight bandage, and take him to the next hut. He hasn’t a ghost of a chance, of course. In fact, we should not have wasted two hours on him.

The three other cases are amputations. Two legs to the hip, and one to the knee.
By nightfall our train arrives, all 22 carts, but there is no point in continuing our work. By midnight we call a halt. We assign several huts to each medic, ordering them to sleep there, and we doctors and nurses collapse on the floor of our dressing station, pell-mell.
The girls have spent a nightmarish day. Each was assigned 3 or 4 huts. Until dark they tried to feed their charges, listening to entreaties, reproaches, hysterics, curses. They needed water, warmth, the most primitive medical help, and we could not provide anything. One man threatened to toss a hand grenade at Anna has been bringing water up all day from a wrecked well with a pail, tying together several belts and scarves. All of them wept many times during the day, cursing superiors, doctors, and the very hour when they had decided to become military nurses.”
Watching people die is quite an experience. It makes one think. Soldiers –generally the older ones - who have religious faith, usually die easily…a small




CoROM will be running an exhibitor’s booth as well as hosting two workshops:
DetecIon and MiIgaIon of Malaria in the Austere Seong TacIcal Medicine Review & IBSC Exams
