Onkologi LAG3-hæmmere ændrer immunterapiens behandlingslandskab
Side 5
Highlights fra ASCO GI & GU

Side 10
Hæmatologi Highlights fra ASH 2022
Side 17
Myelomatose: Geografisk betinget?

Side 24
Share clinical knowledge and best practice to improve health and patient care.
DK / NR. 10 / 2023
sammenomkræft.dk
Rationalet for dobbelt immunterapi – aktiver og beskyt immunresponset1-7
Aktiveringsfasen
Lymfeknude. Anti-CTLA-4 antistof 1-5
Antigenpræsenterende celle
B7 CTLA-4
Anti-CTLA-4 antistof
-
• Flere T-celler aktiveres
T-celle
• Flere forskellige T-celler aktiveres
• Antallet af hukommelses T-celler øges
• PD-L1 på tumorcellerne fremmes
Effektorfasen
Tumormikromiljø. Anti-PD-1 antistof6,7
T-celle Kræftcelle -
PD-1 PD-L1/L2
Anti-PD-1 antistof
•Genetablerer og forstærker
T- celle drab
Scan QR koden og se video om virkningsmekanismen

1. Das R et. al. J Immunol (2015) 194 (3): 950–959. https://doi.org/10.4049/jimmunol.1401686
2. Pardoll D.M. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;11:252-264.
3. Wei S. et al. Cancer Discov;8(9);106986. 2018 AACR. https://pubmed.ncbi.nlm.nih.gov/30115704/
4. Wei S, et al. Immunity vol 50, 1084-1098 April 16, 2019. https://doi.org/10.1016/j.immuni.2019.03.004
5. Gao J et.al. Nat Med. 2017 May;23(5):551-555. doi: 0.1038/nm.4308. Epub 2017 Mar 27.
6. Wang C et al. Cancer Immunol Res; 2(9); 846–56. _2014. https://doi.org/10.1158/2326-6066.CIR-14-0040 AACR.
7. Brahmer JR et al. J clin oncology 2010 Jul 1;28(19):3167-75. DOI: 10.1200/JCO.2009.26.7609
ONC-DK-2300001, 20.01.2023
Onkologi Hæmatologi
5 LAG3-hæmmere ændrer immunterapiens behandlingslandskab / Marco Donia & Eva Ellebæk
7 Serum VLDL levels are associated with premenopausal breast cancer risk / Julia Debik, Tone F. Bathen & Guro F. Giskeødegård
9 Seksuel sundhed er en udfordring blandt langtidsoverlevende brystkræftpatienter / Jan Andreasen
10 Highlights From ASCO GU »Today's Science, Tomorrow's Treatment« / Jan Andreasen

11 Highlights From the 20th Anniversary of the ASCO GI meeting / Jan Andreasen
15 Danish Bladder Cancer Patients Show Similar Out comes in Clinical Practice and Clinical Trials / Lise Høj Omland
17 ASH 2022 – Greetings from New Orleans /Marie Louise de la Cour Bergmann & Jan Andreasen
18 ASH 2022 Highlights / Marie Louise de la Cour Bergmann & Jan Andreasen
21 Psoriasis artrit-patienter, TNF-hæmmere og hæmatologiske cancere / René Cordtz & Lene Dreyer
24 Er risikoen for myelomatose geografisk betinget ? / Lise Dueholm Bertelse
Indhold
TEMA
3 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
BestPractice Nordic er et uafhængigt tidsskrift, som udgives af
BestPractice Nordic ApS
Teknikerbyen 5, 2. sal 2830 Virum +45 4466 9210 redaktion@bpno.dk www.bpno.dk
Ansvarshavende redaktør Jan Andreasen

Læge og journalist +45 5151 8831 jan@bpno.dk
Redigering og produktion : Marie Louise la Cour Bergmann Redaktionel projektleder
Artiklerne i BestPractice Nordic er uafhængige af interesser. Artiklerne er den enkelte forfatters faglige perspektivering. Artiklernes budskaber er derfor ikke nødvendigvis et udtryk for redaktionens synspunkter.
Tidsskriftet udsendes til landets onkologer og hæmatologer.
Annoncer Charlotte Knudtzen
CEO & Partner 45 6139 4747 ckn@bpno.dk
Ina Bøgkjær Key Account Manager +45 6130 5072 ibo@bpno.dk
Copyright© 2023
BestPractice Nordic ApS Oplag : 735 ISSN 2597-2375
Art director
Helle Rindom
Layout og dtp Andreas Støvhase
Tryk : Strandbygaard A/S
Vi lever i en tid, hvor der sker store fremskridt inden for behandling af cancersygdomme og hæmatologiske lidelser, og hvor nye behandlingsmuligheder viser deres effekt. Igennem de senere år er vi mere og mere blevet opmærksomme på livskvalitetens betydning for patienten, både under behandlingen men især efter behandlingen, når patienten har overlevet sin sygdom. Vi lever også i en tid, hvor patienter i stigende grad vil medinddrages i beslutninger om deres behandling, hvilket kræver en anden måde at tænke på og agere i sundhedsvæsenet.

Et af de områder, hvor der sker meget nyt, er brystcancer området, hvor vi måske står foran en ny æra. Samtidig hermed er der ikke ensartede nationale retningslinjer for fokuseret patientvenlig opfølgning på tværs af de danske afdelinger, der behandler patienter med brystkræft. I dette lys har Dansk Bryst Cancer Gruppe i samarbejde med BestPractice Nordic og dieHilfe planlagt et seminar d. 13. — 14. november. Seminaret skal munde ud i et bedre, evidensbaseret og opdateret opfølgningsprogram, der medinddrager den nyeste viden om de faktorer, der har betydning for patienters helbred, livskvalitet og tilbagevenden til så normalt et liv som muligt efter behandling for brystkræft. Så derfor »save the date«.
Covid19-pandemien med de følgende globale nedlukninger synes allerede som en mørk fortid, hvilket gør, at vi igen kan mødes på internationale kongresser, deltage i faglige dialoger og ikke mindst networke. BestPractice Nordic deltog i The American Society of Hematology (ASH) årsmøde, der blev afholdt i New Orleans, hvor vi mødte flere nordiske som internationale læger inden for hæmatologien. I denne udgave bringer vi en længere reportage fra ASH, ligesom vi også bringer nyt fra såvel ASCO GU og ASGO GI 2023.
Afslutningsvis vil jeg fremhæve en artikel, der giver svaret på, om forekomsten af myelomatose er betinget af, hvor i Danmark vi bor. Hvis det bliver mellem mig og læserne, så kan jeg godt afsløre, at jeg tænkte, at der ikke er en sammenhæng. Som du kan læse, er dette ikke korrekt, for der er områder i Danmark, hvor risikoen eller forekomsten af myelomatose er større end andre steder. Artiklen giver også et bud på et svar, der er interessant i vores igangværende dialog om, hvordan miljøpåvirkninger rammer os.
Our mission is to share clinical knowledge and best practice to improve health and patient care.
Du vil på de følgende sider se, at det meste indhold i denne udgvielse er på engelsk, hvilket bliver det primære sprog fremover for BestPractice Nordic Onkologihæmatologi. Årsagen er, at vi dels har spurgt læserne, der gerne vil det engelske sprog, men også fordi det giver os mulighed for at dele viden fra jeres nordiske og internationale kolleger. Deling af ny viden mellem specialister inden for et speciale er vores DNA, og her giver det god mening at tænke såvel nationalt, nordisk og globalt.
God læselyst !
4 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
Leder
Jan Andreasen / Ansvarshavende redaktør, Læge og Journalist
Vi deler viden såvel nationalt, nordisk som globalt
LAG3-hæmmere ændrer immunterapiens behandlingslandskab
Ny immuncheck-pointhæmmer rettet mod LAG3 – relatlimab – viser lovende resultater, når den gives som fixed-dose-kombination med PD-1-hæmmeren nivolumab til behandling af metastaserende melanom hos patienter med lav PD-L1-ekspression.
MARCO DONIA er afdelingslæge på Center for Cancer Immune Therapy, Herlev Hospital. EVA ELLEBÆK er speciallæge og ph.d. i onkologi ved Nationalt Center for Cancer Immunterapi (CCIT-dk), Afdeling for Kræftbehandling på Herlev og Gentofte Hospital. Hun har speciale inden for immunterapi og modermærkekræft.
Det onkologiske behandlingslandskab blev forandret i 2011 og 2014 med godkendelsen af lægemidler, der hæmmer checkpoint-proteinerne CTLA-4 og PD-1. I årene efter fulgte adskillige opsigtsvækkende positive resultater for behandling med immun-check-pointhæmmere mod en række solide tumorer, og i dag er immuncheck-pointhæmmere blevet standardbehandling af flere cancertyper.
Lige siden har der været stor forskningsinteresse for at identificere nye checkpoints, der kan forbedre behandlingen yderligere. Der er nemlig endnu udfordringer forbundet med de nuværende behandlingsmuligheder, både med hensyn til effektmål og bivirkninger. Ikke alle patienter opnår de ønskede effekter, og flere patienter oplever hyppige og alvorlige bivirkninger. Det er især behandlinger, der kombinerer hæmning af CTLA-4 og PD-1 samtidig, der medfører bivirkninger.
Nyt lægemiddel mod hæmning af LAG3 : Relatlimab 2022 blev et år med et vigtigt gennembrud i forhold til nye behandlingsmuligheder, idet der er blevet godkendt et nyt lægemiddel, relatlimab, rettet mod hæmning af lymphocyte-activation gene 3 (LAG3). LAG3 er et overflademolekyle på T-celler, der bremser T-cellernes proliferation og funktion.
Relatlimab er en »first in class«-hæmmer af LAG3 og er blevet godkendt af Food and Drug Administration, FDA, og European Medicines Agency, EMA, som en fixed-dose-kombination med PD-1-hæmmeren nivolumab til behandling af metastaserende melanom.
RELATIVITY-047-studiet


RELATIVITY-047-studiet viser, at kombinationen af relatlimab og nivolumab giver god effekt, særligt hos patienter med lav PD-L1ekspression. EMA har kun godkendt kombinationen til patienter med malignt melanom og PD-L1-ekspression <1%.
Det er bemærkelsesværdigt, da FDA har godkendt kombinationen uden begrænsninger for PD-L1-status. Desuden har studiets forfattere konkluderet i New England Journal of Medicine, at PD-L1-ekspressionen ikke har en afgørende betydning for, om kombinationen af relatlimab og nivolumab er mere fordelagtig end monoterapi med nivolumab.
RELATIVITY-047


Relativity-047 er et globalt fase 2-3, dobbeltblindet randomiseret studie, der belyser effekten af relatlimab i fixed-dose-kombination med nivolumab hos patienter med tidligere ubehandlet metastatisk eller ikke-resektabelt melanom sammenlignet med behandling med nivolumab. Relatlimab i kombination med nivolumab administreres subkutant hver fjerde uge.




Det primære endpoint var progressionsfri overlevelse.
PD-L1 : Kombination vs. enkeltstof immunterapi
I Danmark, baseret på data fra Checkmate 067-studiet, har PD-L1 expression været anvendt til at guide valg af behandlingen siden ultimo 2016. Kombinationsbehandling med ipilimumab plus nivolumab anvendes hovedsagelig til patienter med PD-L1 expression <1%. PD-L1 expression anvendes dog normalt ikke som biomarkør ved behandling af malignt melanom andre steder i verden i dag, men dette kan ændre sig i fremtiden med indførelsen af stadigt mere komplekse behandlingsalgoritmer. I deres nye summary of product characteristic for ipilimumab samt i public assessment report for relatlimab plus nivolumab fremhæver EMA nu PD-L1 expression som et vigtigt redskab, også ved behandlingsvalg mellem ipilimumab plus nivolumab versus nivolumab monoterapi.
Onkologi
5 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
EMA vurderede, at langtidsdata (60 mdr. follow up) ikke indikerer en progressionsfri overlevelse/overlevelsesgevinst ved behandling med ipilimumab plus nivolumab versus nivolumab monoterapi hos patienter med PD-L1 positive tumores (>1%).
Det vil være interessant at se, om der observeres lignende resultater i andre tumortyper ved behandling med kombinationsimmunterapier, især dem, hvor måling af PD-L1 expression er en mere etableret del af klinisk beslutningstagning.
Immunterapi i en neoadjuverende behandling
Udover at identificere de patientgrupper, der sandsynligvis vil have gavn af dual LAG3 / PD-1-hæmning, er spørgsmålet om, hvornår man skal starte behandling, også af stor relevans for onkologer. For hver indikation er der fokus på og faglig interesse i at anvende immune checkpoint-hæmmere i tidligere og tidligere stadier af behandlingen. Oprindeligt blev immunterapi anvendt til
Referencer :
at behandle metastaserende sygdom, men i dag anvendes det også som adjuverende behandling efter operation for at forebygge relaps.
Igangværende studier belyser nu brugen af immunterapi i en neoadjuverende behandlingsstrategi, baseret på den antagelse, at der kan opnås en bedre stimulering af immunsystemet, når tumorens antigener præsenteres for T-celler i et intakt tumormikromiljø.

Fremtidig undgåelse af kirurgisk indgreb
Måske vil vi i fremtiden se, at vi for nogle cancersygdomme helt kan undgå kirurgiske indgreb, hvis der opnås en god respons på neoadjuverende immunterapi.
Kliniske undersøgelser med henblik på at belyse neoadjuverende dual LAG3/PD-1-hæmning sammenlignet med adjuverende dual LAG3/PD-1-behandling vil være af stor interesse for flere tumortyper. Dette også for at sikre, at vi opnår det fulde potentiale af behandling med checkpoint-hæmmere.
Marco Donia. LAG3 inhibitors are changing the landscape of immunotherapy- ESMO Daily Reporter. 2. Sept 2022. Hussein A. Tawbi, Dirk Schadendorf, Evan J. Lipson, Paolo A. Ascierto, Luis Matamala, Erika Castillo Gutiérrez, et alt. Relatlimab and Nivolumab versus Nivolumab in Untreated Advanced Melanoma. The New England Journal of Medicine. 2022 ; 386 : 24-34. DOI : 10.1056/NEJMoa2109970
INTERESSEKONFLIKT : Ingen.
SAVE THE DATES
DBCG seminar Lungecancerseminar
13.-14. november 2023
Milling Hotel Park,
I samarbejde med Dansk Brystcancer Gruppe afholdes et multidisciplinært seminar om opfølgning af patienter opereret for brystkræft.
27. september 2023
Aarhus Universitetshospital
Med afsæt i IASLC – 2023 World Conference on Lung Cancer (WCLC) inviterer Dansk Lunge Cancer Gruppe og BestPractice Nordic til lungecancerseminar.
6 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
2022 blev et år med et vigtigt gennembrud i forhold til nye behandlingsmuligheder, idet der er blevet godkendt et nyt lægemiddel, relatlimab, rettet mod hæmning af lymphocyte-activation gene 3 (LAG3).
Tilmeld dig her Scan QR koden og tilmeld dig
Serum VLDL levels are associated with premenopausal breast cancer risk
A recent study based on a large Norwegian population cohort shows that increased serum levels of very-low density lipoproteins (VLDLs) are associated with a decreased long-term breast cancer risk in premenopausal women.
JULIA DEBIK works as a postdoctoral fellow and researcher at the Cancer Imaging and Multiomics research group (CIMORe) and the K.G. Jebsen Center for Genetic Epidemiology, which is based at the Norwegian University of Science and Technology (NTNU) in Trondheim, Norway.
TONE F. BATHEN is a professor who is also affiliated with CIMORe, and GURO F. GISKEØDEGÅRD is an Associate Professor at the K.G. Jebsen Center for Genetic Epidemiology, NTNU, Trondheim, Norway.
Breast cancer is the most common cancer disease among women. Due to established screening protocols and more efficient treatment, breast cancer survival rates have increased during the last decades, bringing the 5-year survival rates above 90% in Norway. The prognosis is highly dependent on the stage of the disease at the time of diagnosis, and tumors may grow for years before they reach a detectable size. Novel methods for early detection and cancer prevention could increase survival and reduce the societal burden of breast cancer. It is necessary to understand the underlying etiology and biological mechanisms leading to breast cancer development and progression to achieve this.
Traditional risk factors of breast cancer
Known risk factors for breast cancer include genetic predisposition, alcohol consumption, smoking, physical inactivity, and obesity. Factors reducing the risk of breast cancer are largely related to reproductive history, such
as having children at a young age, having multiple pregnancies, breastfeeding, and early menopause. However, these risk factors alone are not sufficient to accurately predict who will develop breast cancer.
Lipoprotein subfraction analysis provides additional information to traditional lipid measurements
Lipids are important in cell signaling, membrane formation and as a cellular energy source, and lipids circulating in the blood stream reflect both ongoing cellular processes and influence from the environment. Two main forms of circulating lipids in the body are triglycerides and cholesterol, which are transported through the bloodstream in lipoproteins. Lipoproteins carry triglycerides and cholesteryl esters in their inner core, surrounded by a membrane of free cholesterol, phospholipids and apolipoproteins. Different classes of lipoproteins exist, from very-low density (VLDL), low-density (LDL), and intermediate-density (IDL) to high-density (HDL) lipoproteins.
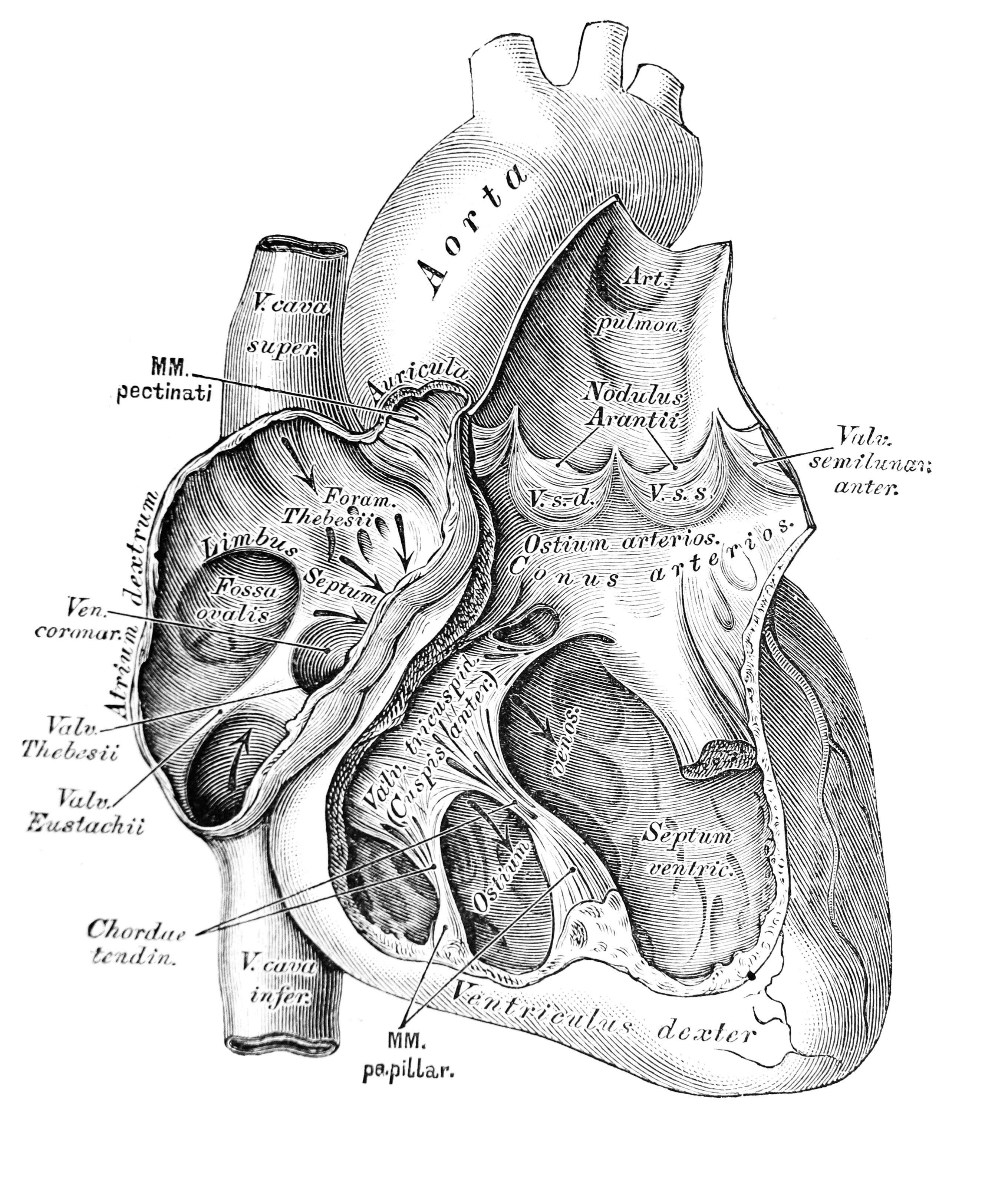
The lipoproteins exist in a range of densities within each class (Figure 1), and conventional methods for lipoprotein quantification do not reflect the delicate density range of the lipoprotein subclasses and the lipids they carry. Previous studies have shown that subfraction analysis, giving detailed information on lipoprotein size and content, provides additional information to that of traditional lipoprotein measurements. Nuclear magnetic resonance (NMR) spectroscopy provides a detailed characterization of lipoprotein subfractions in a blood sample in a fast and reproducible manner.
Lipoproteins are lipid carriers transporting triglycerides and cholesterol to cells throughout the body. Lipoproteins exist in a range of densities. Lipoprotein subfractions analysis provides a detailed image of the concentration of lipoproteins of different densities in the bloodstream and provides important information on what the lipoproteins carry.
Lipoproteins are lipid carriers transporting triglycerides and cholesterol to cells throughout the body. Lipoproteins exist in a range of densities. Lipoprotein subfractions analysis provides a detailed image of the concentration of lipoproteins of different densities in the bloodstream and provides important information on what the lipoproteins carry.
 Figure 1 – Lipoproteins
Figure 1 – Lipoproteins
Density Diameter Cholesterol Triglyceride Phospholipid Cholesteryl ester Apolipoprotein HDL LDL IDL VLDL
Figure 1 – Lipoproteins
7 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
Population biobanks facilitate large-scale prospective studies
The Trøndelag Health Study (HUNT) is a Norwegian longitudinal population health study carried out over four decades and includes questionnaire data, clinical measurements, and biological materials from over 230,000 individuals. The second wave of data collection (HUNT2) conducted between 1995-97 included 65,200 participants. By linking HUNT2 participants to the Norwegian Cancer Registry, we identified 1,199 women who developed breast cancer within a 22-year follow-up period. This provided a unique opportunity to study the association between lipoprotein subfractions and long-term breast cancer risk in a large cohort.
A nested case-control study
We conducted a nested case-control study, comparing the lipoprotein subfraction profiles of 1,199 women who later developed breast cancer and the same number of age-matched women who remained breast cancer free during the 22-year follow-up period. Serum samples were analyzed by NMR spectroscopy to achieve detailed lipoprotein subfraction profiles. We applied logistic regression to test for associations between serum lipoprotein subfractions and long-term breast cancer risk. Models were adjusted for possible confounding factors, including analysis lab, participant age, number of full-term pregnancies, age at menarche, alcohol consumption, smoking status, and body mass index (BMI). The menopausal status was unknown for a large proportion of the cohort and was estimated based on the age at participation in HUNT2.
Several VLDL subfractions inversely associated with long-term breast cancer risk
In our study cohort, 554 cases were classified as premenopausal and 645 as postmenopausal at participation in HUNT2. Postmenopausal women had significantly different lipoprotein subfraction profiles than premenopausal women, with elevated levels of most of the lipoprotein subfractions except for cholesterol and phospholipids in the largest HDL subfractions. Due to the large differences between pre- and postmenopausal women, we performed analyses separately for these groups.
For premenopausal women, we found that several VLDL subfractions were inversely associated with longterm breast cancer risk, including triglycerides, free and esterified cholesterol, and phospholipids in all VLDL particles except for the largest ones. Odds ratios for the different subfractions ranged from 0.77 to 0.83, and associations remained significant after adjusting for confounders. The traditional lipoprotein measures did not show any significant associations, demonstrating the added value of detailed subfraction analysis of lipoproteins. There were no significant associations between lipoprotein subfractions and breast cancer risk for postmenopausal women.
VLDLs are large particles produced and secreted by the liver, transporting lipids from the liver to peripheral tissues and muscles. As estrogen levels play an important role in the regulation of lipid metabolism, we hypothesize that our findings reflect hormonal activity in addition to lifestyle factors.
ORIGINAL PUBLICATION AND COAUTHORS : This article is a summary of an already-published study : Debik et al. Lipoprotein and metabolite associations to breast cancer risk in the HUNT2 study. Br J Cancer 127, 1515–1524 (2022). Coauthors: Julia Debik, Hartmut Schäfer, Trygve Andreassen, Feng Wang, Fang Fang, Claire Cannet, Manfred Spraul, Tone F. Bathen & Guro F. Giskeødegård
8 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
CONCLUSION : Our results reveal alterations in lipid metabolism of premenopausal women many years before they are diagnosed with breast cancer. In specific, increased levels of VLDLs have a protective effect against developing breast cancer.
CONFLICT OF INTEREST : None.
Seksuel sundhed er en udfordring blandt langtidsoverlevende brystkræftpatienter
I en undersøgelse foretaget af brystonkologen Solveig Katrine Smedsland fra Oslo Universitetshospital er den seksuelle sundhed blevet undersøgt blandt brystkræftpatienter, otte år efter diagnosen.
JAN ANDREASEN
Seksuel sundhed er en vigtig faktor for livskvalitet efter brystkræft, men på trods af vigtigheden er forskningen på dette område sparsom for langtidsoverlevende brystkræftpatienter. Solveig Katrine Smedsland, læge og brystonkolog på Oslo Universitetshospital, har derfor sammen med sine kolleger undersøgt den seksuelle sundhed blandt brystkræftpatienter otte år efter diagnosen. De 1.241 deltagende kvinder var på diagnosetidspunktet, i perioden 2011-2012, mellem 20 og 65 år, og de blev sammenlignet med en kontrolgruppe på i alt 17.751 kvinder.

Sammenlignet med kontrolgruppen havde kvinder med brystkræft dårligere seksuel nydelse og højere seksuelt ubehag – hvilket var særlig udtalt for premenopausale kvinder sammenlignet med gruppen af postmenopausale.
Brystkræftpatienter, der var behandlet med endokrin behandling, adjuverende kemoterapi eller aromatasehæmmere, havde dårlig seksuel sundhed på alle målte underkategorier.
Undersøgelsen dokumenterer, at udfordringer med seksuel sundhed er almindeligt hos langtidsoverlevende patienter med brystcancer og især i gruppen af premenopausale kvinder.
Nye anbefalinger fra Medicinrådet om brystcancer
Medicinrådet har på sine to seneste møder i henholdsvis januar og februar 2023 godkendt to nye behandlingsmuligheder for patienter med brystcancer.
Således er Enhertu, trastuzumab deruxtecan (T-DXd), godkendt til behandling af voksne patienter med ikke-resekterbar eller metastatisk HER2-positiv brystkræft for patienter med performancestatus 0-1 uden symptomgivende hjernemetastaser. Baggrunden for anbefalingen er, at Medicinrådet vurderer, at det er veldokumenteret, at en høj andel af patienterne har tumorsvind ved behandlingen, og at den forlænger tiden til forværring af sygdommen sammenlignet med den nuværende standardbehandling (T-DM1).
Samtidig vurderer Medicinrådet, at T-DXd forlænger patienternes levetid.
Medicinrådet anbefaler også Keytruda, pembrolizumab i kombination med kemoterapi som neoadjuverende behandling til patienter med lokalt fremskreden eller tidlig triple-negativ brystkræft, der har høj risiko for tilbagefald. Ifølge Medicinrådet er det dokumenteret, at en højere andel af patienterne har komplet tumorsvind i bryst- og lymfeknuder ved neoadjuverende behandling med pembrolizumab i kombination med kemoterapi sammenlignet med den behandling, de får i dag. Samtidig peger rådet på risikoen for alvorlige immunrelaterede bivirkninger ved behandlingen.
9 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
Denne artikel er skrevet på baggrund af en MEDtalk med Solveig Smedsland. Scan QR koden og se MEDtalken
ASCO GU »Today's Science, Tomorrow's Treatment«
Keep up with the latest updates from the 2023 ASCO Genitourinary (GU) Cancers Symposium as BestPractice Nordic brings you updates from leading oncologists who attended. Notable studies presented at the event include the IMvigor130 and the ongoing CAPItello-280 trial.

From February 16-18, the 2023 ASCO Genitourinary (GU) Cancers Symposium brought together global experts to explore innovative research, care methodologies, and new technologies for advancing progress in GU oncology. The Symposium's theme, »Today's Science, Tomorrow's Treatment,« emphasized the rapid pace and potential of therapeutic advancements in GU oncology. Throughout the event, sessions delved into new targets, concepts, and drug combinations for GU malignancies,
such as metastatic castration-resistant prostate cancer. Additionally, the Symposium highlighted fresh clinical practice approaches for managing complex care issues across various malignancies while also discussing artificial intelligence and providing updates on guidelines and key studies in prostate, bladder, and kidney cancers. BestPractice Nordic followed the congress and met with leading oncologists virtually.
Aristotle Bamias, Professor of Medical Oncology at the University of Athens, Greece, presented at ASCO GU the IMvigor130 study. This phase III study is a final Overall Survival (OS) analysis of atezolizumab (atezo) monotherapy vs chemotherapy (chemo) in untreated locally advanced or metastatic urothelial carcinoma (mUC). Aristotle Bamias explains that the benefit-risk ratio of atezolizumab vs chemotherapy support atezolizumab as first-line treatment for cisplatin-ineligible patients with PD-L1 IC2/3 mUC.
During the ACSO-GU symposium, the CAPItello-280 trial's design and study endpoints were presented. This ongoing trial aims to validate the results of the ProCAID study, which explored the safety and effects of adding capivasertib to docetaxel chemotherapy in patients with metastatic castration-resistant prostate cancer (CRPC). To learn more about this topic, you can listen to a MEDtalk with Simon Crabb, MD and Associate Professor in Medical Oncology at the Southampton Experimental Cancer Medicine Centre, University of Southampton, United Kingdom.
Scan the QR code with your phone's camera and find the MEDtalks with Aristotle Bamias and Simon Crabb on our ASCO GU congress page.

10 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
CAPItello-280 trial aims to confirm findings from ProCAID trial
JAN ANDREASEN
The phase III IMvigor130 study – Survival (OS) analysis of atezolizumab
ASCO GI 2023 – The


20th
Anniversary of the ASCO GI meeting
The ASCO Gastrointestinal Cancers Symposium, which was held in San Francisco, California from January 18-21, 2023, celebrated two decades of groundbreaking and transformative care in advancing the treatment of gastrointestinal cancer. The theme was »Applying Innovation, Transforming Care, and Advancing Equity« highlighting the recent developments in cancer screening, diagnosis, and treatment, as well as the need for new strategies to ensure that everyone has equal access to the care that is shaping the future of GI cancer treatment. At this event, BestPractice Nordic had the opportunity to meet with leading oncologists virtually and remain informed about the latest research and findings from the congress. You can find out more about the presented abstracts and short presentations on our website at bpno.dk.
11
ASCO GI Highlights
The SPOTLIGHT study: Promising Effect of Zolbetuximab plus mFOLFOX6
The SPOTLIGHT study has achieved its primary endpoint, potentially paving the way for a new first-line treatment option for individuals with Claudin 18.2 (CLDN18.2)-positive, HER2-negative, locally advanced unresectable or metastatic gastric or gastroesophageal junction (GEJ) adenocarcinoma.
Results from the SPOTLIGHT study, one of the longest phase III trials for patients with CLDN18.2+ / HER2- locally advanced unresectable or metastatic gastric or gastroesophageal junction (mG/GEJ) adenocarcinoma, were presented during the 2023 ASCO Gastrointestinal Cancers Symposium.

The SPOTLIGHT trial enrolled 550 patients with CLDN18.2+ / HER2- locally advanced unresectable or mG/GEJ adenocarcinoma in a phase III randomized study. Patients were randomly assigned to receive either zolbetuximab plus leucovorin, fluorouracil, and oxaliplatin (mFOLFOX6) or placebo plus mFOLFOX6 as their first-line treatment in a 1:1 ratio. Both groups had similar baseline characteristics. The study involved participants with a median age of 62 years, consisting of 62% men, 69% non-Asian, and 31% Asian. The majority (77%) of the participants had primary cancer instomach, and 22.6% had metastatic cancer in three or more organs.
Clinically significant improvement of PFS and OS
Kohei Shitara, MD of the National Cancer Center Hospital East, Kashiwa, Japan, stated that the median progression-free survival (PFS) was 10.6 months in the combination arm and 8.67 months in the placebo arm with a hazard ratio of 1.75 and P value of 0.0066, meeting the primary endpoint. The study also showed a PFS benefit in most subgroups. The study's positive results in terms of PFS were also reflected in the median overall survival (OS), even though OS was not the primary endpoint. The combination arm had a median OS of 18.2 months, which was significantly longer than the 15.54 months seen in the placebo arm, with a hazard ratio of 0.75 and a significant P value.
Clinical implications
Dr. Wungki Park, a medical oncologist and translational research scientist at the Memorial Sloan Kettering Cancer Center in New York suggests that the findings from the SPOTLIGHT study may lead to the development of a new treatment plan. Hence, zolbetuximab in combination with mFOLFOX6 could potentially be established as the new standard of care for patients with locally advanced (LA) unresectable or metastatic gastric or gastroesophageal junction (mG/GEJ) adenocarcinoma who have the biomarker CLDN18.2+ / HER2-.
Conclusion
The SPOTLIGHT study is a phase III trial with one of the superior OS rates for patients with CLDN18.2+ / HER2- locally advanced unresectable or metastatic gastric or gastroesophageal junction adenocarcinoma. The study has demonstrated that the combination of zolbetuximab and modified FOLFOX 6 significantly improved both PFS and OS while maintaining a tolerable safety profile. Although both groups had similar rates of adverse events, the active arm experienced more frequent nausea and vomiting.
12 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
Kohei Shitara, MD speaks during Oral Abstract Session A: Cancers of the Esophagus and Stomach at the 2023 Gastrointestinal Cancers Symposium © ASCO/Todd Buchanan 2023
JAN ANDREASEN
Colorectal cancer: Surgical induced cfDNA elevation does not impact ctDNA for MR

A recent study presented at ASCO GI 23, discovered that the increase in Cell-Free DNA levels caused by surgery does not impact the detection of circulating tumor DNA in individuals with colorectal cancer.
MEDtalk HIGHLIGHTS
During ASCO GI 2023, Stacey Cohen, a medical oncologist at the Fred Hutchinson Cancer Center and University of Washington in Seattle, presented a study evaluating the detection of circulating tumor DNA (ctDNA) in patients with stage I to III colorectal cancer immediately after surgery. The study analyzed a database of 14,425 patients with at least one ctDNA result to investigate whether the increase in cell-free DNA (cfDNA) after surgery would impact the ability to detect ctDNA for minimal residual disease (MRD). The study concludes, that although cfDNA levels increased during the first two weeks after surgery, this rise did not interfere with detecting ctDNA for MRD, which remained reliable after approximately two weeks.
No impact of cfDNA

The frequency of ctDNA was highest during the first two weeks after surgery, but positivity decreased after eight weeks, likely due to adjuvant chemotherapy. The study also demonstrated that postoperative MRD or ctDNA positivity was a reliable predictor of recurrence-free survival, with the highest positivity in stage III and the lowest in MSIhigh tumors. Even though the multivariate analysis did not impact cfDNA concentration, MRD remained the most robust predictor of recurrence-free survival.
Conclusion
The study concluded that the elevation in cfDNA after surgery did not affect the ability to detect ctDNA for MRD, and standard emerge testing windows could start as early as two weeks after surgery. However, further research is needed to investigate the small number of patients who showed ctDNA positivity in the first week after surgery.
New treatment option for refractory metastatic colorectal cancer – trifluridine/tipiracil plus bevacizumab
Positive effect of stereotactic body radiation therapy (SBRT) followed by sorafenib in patients with hepatocellular carcinoma

New option for 1. line treatment of advanced oesophagal squamous cell carcinoma – 29. Month Follow-up
Find all MEDtalks from ASCO GI at our congress site
ASCO GI 2023
Josep Tabernero
Laura Dawson
Ken Kato
JAN ANDREASEN
BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
This section is based on MEDtalks with Kohei Shitara, Wungki Park and Stacey Cohen.
Tag på online kursus når du har tid
Kurser udviklet efter danske og internationale guidelines
Lungecancer:
Nyeste tendenser ved planocellulær NSCLC


• Ætiologi, patogenese
• Klinisk præsentation, de radiologiske tegn, histopatologi
• Behandling af planocellulært lungekarcinom
• Nye tendenser i behandling af planocellulært lungekarcinom
• EGFR-, PIK3CA- og DDR-mutationer
• ALK-fusion og Rb1-signalvejen
• HER2, FGFR-1-3 og MET abnormiteter
• Nye targets NTRK-fusioner og NUT midtlinje karcinom
• Afsluttende faglig test
• Tager 3-4 timer at gennemføre
Udviklet i samarbejde med:
Edyta Maria Urbanska
lungeonkolog, afdelingslæge
Antonio Santoni-Rugiu
lungeonkolog, afdelingslæge
kr. 2.500,–
ekskl. moms
Adgang til kurset i 1 år
Immunterapi:
Undgå at overse bivirkninger
• Immunsystemets opbygning og funktion

• Immunterapi
• Bivirkninger til immuncheckpointinhibitorer
• Gennemgang af bivirkninger:
Dermatologiske, endokrinologiske, reumatologiske, neurologiske, nefrologiske, hepatiske, gastroenterologiske og kardiologiske
• Opsamling og CTCAE-oversigt
• Faglige test undervejs
• Tager 2-3 timer at gennemføre
Udviklet i samarbejde med:
Per Thor Straten professor, Nationalt Center for Cancer Immunterapi
Bent Deleuran professor, overlæge
Jeanette Kaae
ph.d., speciallæge
Rikke Holmstrøm ph.d.-stud., læge
Gratis
Adgang til kurset i 1 år
www.medelearn.dk
Faglig opdatering når det passer dig
adgang
Danish Bladder Cancer Patients Show Similar Outcomes in Clinical Practice and Clinical Trials
Two studies evaluating all Danish patients with bladder cancer treated with firstline chemotherapy and all-line pembrolizumab, respectively, have found similar outcomes and overall survival rates between patients treated in clinical practice and those from clinical trials. Inspired by these studies, a national database for bladder cancer is being created.
LISE HØJ OMLAND is a MD, PhD, employed as a chief resident physician at the Oncology Department at Rigshospitalet, Copenhagen. Her research interests are centered around bladder cancer, with a special emphasis on real-world evidence.
Real-world evidence is generated from real-world data, which refers to healthcare data derived outside the context of traditional clinical trials. In recent years, the interest in real-world evidence has increased as a source of investigating the effect of a treatment when applied to the heterogeneous patient population in routine clinical practice. This may be particularly important in bladder cancer as patients with bladder cancer are generally considered a frail patient group.
Two nationwide, population-based Danish studies have recently evaluated all Danish patients with bladder cancer treated with first-line chemotherapy and all-line pembrolizumab, respectively.1,2 This article briefly sums up the findings and potential implications.
Real-world evidence comparable to clinical results
The largest of the two studies evaluated 952 patients with metastatic bladder cancer treated with first-line chemotherapy in the period 2010 to 2016. The study showed that despite patients treated in routine clinical practice being older and in a poorer general condition than patients enrolled in clinical trials, treatment responses and overall survival were similar to reportings from clinical trials.
The other study investigated real-world pembrolizumab. It followed 139 patients treated with pembrolizumab during the first year after it was introduced as a standard treatment option in Danish oncology departments. The
study demonstrated that pembrolizumab is safe and effective when applied in routine clinical practice, with results similar to those observed in the KEYNOTE-052 and KEYNOTE-045 trials.
Legal challenges implementing real-world studies
A common interest and a close collaboration between the Danish oncology departments managing bladder cancer were essential for conducting the two real-world studies. Despite this common interest, legal constraints made data collection and transfer across the Danish regions difficult. Yet, with substantial extra efforts by the local oncologists involved in the project, this succeeded at last.
Nationwide data collection
Much can be learned from the two real-world studies. Important knowledge of patients with bladder cancer treated in routine clinical practice has been provided, which is valuable for physicians, researchers, regulatory authorities and, in the end, the patients. In addition, we have gained essential knowledge on establishing nationwide data collection. The possibility of gathering nationwide, population-based data is unique in Denmark and should be exploited even more. We hope these two studies can serve as inspiration for similar projects within other cancer types.
Prospective collaborative databases
Inspired by the two real-world studies, an initiative has been taken within the Danish bladder cancer oncology (DaBlaCa) group to establish a national database with the inclusion of prospective data on bladder cancer patients. Data collection will begin when the necessary permits are at hand.
15 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
In recent years, the interest in real-world evidence has increased as a source of investigating the effect of a treatment when applied to the heterogeneous patient population in routine clinical practice
DaBlaCa database already exists, including primarily surgical data. In the future, it may be possible to merge the two databases, thereby increasing the amount and improving the quality of data on this patient group even more.
The collaboration between the Danish oncology departments and other Nordic oncology departments managing bladder
cancer is well-established within the Nordic Urothelial Cancer Oncology Group (NUCOG). Hopefully, establishing the prospective Danish database will facilitate future collaborations across the Nordic countries.
References :
1. Omland LH, Lindberg H, Carus A, Als AB, Jensen NV, Taarnhøj GA, et al. Real-world Treatment Patterns and Overall Survival in Locally Advanced and Metastatic Urothelial Tract Cancer Patients Treated with Chemotherapy in Denmark in the Preimmunotherapy Era : A Nationwide, Populationbased Study. European Urology Open Science. 2021 ;24 : 1–8.
2. Omland LH, Stormoen DR, Dohn LH, Carus A, Als AB, Jensen NV, Taarnhøj GY, Tolver A, Pappot H. Real-world study of treatment with pembrolizumab among patients with advanced urothelial tract cancer in Denmark. Original Article. Bladder Cancer. 2021 : 413–425.
CONFLICT OF INTEREST : None.
16 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
CONCLUSION : The increasing interest in real-world evidence might be a plausible way to generate more evidence with patient groups otherwise excluded from clinical trials. Setting up nationwide databases and international collaborations are some of the possibilities with real-world studies, taking the legal restrictions into account.
Hæmatologi ASH 2022

Greetings from New Orleans
Thousands of hematologists gathered this year in warm and humid New Orleans for the 64th American Society of Hematology's (ASH) annual congress. Like many other conferences in the post-COVID19 pandemic era, ASH was a hybrid congress with the possibility of both virtual and physical participation.
As we, the BPNO team, entered the convention centre, we were greeted with a bustling atmosphere of activity and engagement. Despite the lingering pandemic, the attendees seemed eager to meet face-to-face and resume professional networking. The conference centre was abuzz with discussions on the latest research and clinical advancements in hematology, and the excitement and energy in the air were to sense. We connected with some of the leading hematologists in and outside the Nordic region. The following section summarizes the main points and insights gained from some of our meetings with the experts.
17
MARIE LOUISE LA COUR BERGMANN & JAN ANDREASEN
ASH Highlights
Breakthrough for fragile patients with CLL
During ASH, the GLOW study – a phase III trial evaluating the efficacy and safety of ibrutinib-venetoclax in older patients and/or those with comorbidities with previously untreated chronic lymphocytic leukemia (CLL) was presented. In this study, the combination of ibrutinib-venetoclax (14 months) is compared with the combination of chlorambucil-obinutuzumab (6 months) for frail patients, defined as elderly patients or patients with comorbidities such as reduced kidney function.
The study is the first to document that elderly and frail patients can achieve an improved survival with a time-limited targeted treatment compared to chemo-immunotherapy. Furthermore, the study indicates that an equally deep MRD response is not necessary when treating with a BTK inhibitor (ibrutinib) combined with a BCL2 inhibitor (venetoclax) compared to chemo-immunotherapy.
Given their distinct and complementary mechanisms of action, ibrutinib and venetoclax work synergistically to eradicate CLL by eliminating both dividing and resting leukemic subpopulations. Ibrutinib effectively inhibits tumor cell proliferation and mobilises leukemic cells from protective lymphoid niches. Further, ibrutinib increases the sensitivity of CLL cells to BCL-2 inhibition, thereby accelerating apoptotic cell killing by venetoclax.
There is, thus, not the same coalition between progression-free survival with different genetics. Authors explain this by the combination of BTK inhibitor and BCL2 inhibitor to affect different compartments of the disease such as lymph nodes, blood, and bone marrow.
We met with Carsten Utoft Niemann, chair of the Nordic CLL Groupe, at ASH. He elaborated on the connection between the ibrutinib-venetoclax combination and undetectable MRD. He pointed out that infection is still considered a major risk factor for patients with CLL but that future machine learning may be able to help identify the patients with the greatest risk of infection. By this, the treatment can be more individualized in the future. We also expect better methods for dividing patients into genetic subgroups combined with the risk of infection, which he expects will impact future clinical studies' design.
Evidence to use MRD after induction therapy of AML
Dr. Jacqueline Cloos, an expert in the field of Acute Myeloid Leukemia (AML), is part of a group called The European LeukemiaNet (ELN) MRD Working Party, which aims to improve the use of Minimal Residual Disease (MRD) as a tool in AML treatment. Recently, the group published new guidelines offering more evidence-based recommendations, particularly for using MRD after induction therapy
for intermediate-risk AML patients. The guidelines also emphasize the importance of using validated MRD tests. At ASH22, we spoke with Dr. Cloos, who explained that the ELN MRD Working Party is divided into four subgroups, each consisting of experts in flow cytometry, qPCR, next-generation sequencing, and clinical implementation of MRD. The group also strives to understand how MRD is used in real-world settings and in patients receiving fewer intensive treatments.
Dr. Cloos is particularly interested in standardizing MRD tests and improving their quality. The efforts of the ELN MRD Working Party should ultimately improve MRD for all AML patients and, hopefully, increase the usage of MRD as an intermediate endpoint for trials investigating novel drugs. The new guidelines and the ongoing work of the ELN MRD Working Party are promising steps towards better AML treatment and care.
The Future Treatment of Multiple Myeloma
Dr. Sagar Lonial from the Winship Cancer Institute of Emory University in Atlanta, USA, spoke with us at ASH22 about the exciting developments in BCMA-targeted immune therapies and CART-T cells therapy for patients suffering from multiple myeloma. This year's ASH showcased several T cell engager treatments targeting BCMA.
Even though continuous therapy with T cell engagers can cause concerns due to a higher risk of infectious complications and potential genetic mutations, Dr. Lonial expects a bright future for both T cell engagers and CAR-T cells in the treatment of multiple myeloma. The key question is the optimal treatment sequence, and Dr. Lonial believes that initiating treatment with CAR-T cell therapy and then using T cell engagers if relapse occurs may be the ideal approach. As more research is conducted, the future will reveal the answer.
With a wide range of sessions, events, and presentations, ASH22 provided a valuable opportunity for attendees to keep up-to-date with the latest developments in hematology and to network with like-minded professionals. Photo : BestPractice Nordic

18 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
Mezigdomide : Promising Efficacy in Triple-class Refractory R/R Multiple Myeloma
Mezigdomide, a novel cereblon E3 ligase modulator, has shown great promise in the treatment of relapsed and refractory multiple myeloma. This potent drug induces apoptosis in myeloma cells and has a powerful synergy with dexamethasone, explains Dr. Paul Richardson from the Dana Farber Cancer Institute, who presented preliminary results of a dose expansion study at ASH22. During the conference, we were fortunate to have the opportunity to discuss the study with Dr. Richardson.
The study involved younger patients receiving 40 milligrams of mezigdomide and dexamethasone weekly and older patients receiving 20 milligrams of mezigdomide weekly with the option to reduce doses. Patients were triple-class refractory and could have been BCMA exposed. Results suggest about 30% of high-risk synergetics and approximately 40% of extramedullary disease. Up to 30% of the patients had prior BCMA exposure, making them a very high-risk, vulnerable population in the study, with up to six prior lines of therapy.
Despite the challenges posed by this patient population, the study showed very positive results. The overall response rate was 41%, with a 50% overall response rate among the group who had prior BCMA exposure and a response rate of 30% in patients with active disease.

Dr. Richardson highlighted the favorable safety profile of mezigdomide. During the COVID-19 pandemic, just one COVID-related death during the entire duration of the dose expansion phase was registered. Moreover, the rates of other infections were relatively low, and there were no dose discontinuations due to side effects.
Overall, the study indicates very promising results for using mezigdomide in treating relapsed and refractory multiple myeloma. The drug's potent efficacy and favorable safety profile make it a promising new option for patients with this challenging disease.
R/R Large B-cell Lymphoma : Interesting Results for CAR-T Treatment
During ASH22, we had the opportunity to meet with Frederick L. Locke from the Moffitt Cancer Center in Tampa, Florida, who presented data from the ZUMA 7 randomized phase III trial. The study aimed to analyze the correlation between metabolic tumor volume and clinical outcomes in patients receiving axicabtagene ciloleucel as a second-line treatment versus standard of care.
Locke's team studied more than 1,000 patients treated with axicabtagene ciloleucel and conducted their outcomes based on the ‚»vein to vein time,« which is the duration between the collection of T cells to CAR-T infusion.
The study revealed that patients who experienced a longer vein-to-vein time had poorer outcomes, particularly in progression-free and overall survival. Based on this finding, Locke suggested that shortening the vein-to-vein time could enhance the therapy's effectiveness.
However, further research is necessary to determine potential underlying reasons for patients' extended wait before receiving their CAR-T cell infusion. One reason is that patients with more aggressive diseases needed bridging therapy, while another possibility is that delays in manufacturing contributed to the wait time.
The 2022 World Cup quarter-finals were streamed directly on a wide screen outside the congress center and gathered many attendees of the congress. Photo : BestPractice Nordic
19 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
This section is based on MEDtalks with Carsten Utoft Niemann, Jacqueline Cloos, Sagar Lonial, Paul Richardson and Frederick L. Locke. Scan the QR code and findt all MEDtalks from ASH 22.
ASH22 MEDtalks

Treatment Options for FLT3 mutant acute myeloid leukemia



Venetoclax plus obinutuzumab as 1st line treatment may be beneficial and cost-effective – also for patients without del17p/TP53-mutation
Scan the QR code and find all MEDtalks and abstracts on our ASH congress site
SAVE THE DATE
EHA og Lugano eftermiddagsseminar
Torsdag d. 17. august 2023
Århus Universitetshospital

BestPractice Nordic inviterer til eftermiddagsseminar på Århus Universitetshospital med highlights fra både EHA og Lugano. Du vil bl.a. høre oplæg fra Tarec Christoffer El-Galaly, Hans Beier Ommen, Carsten Utoft Niemann og Agoston Gyula Szabo. Det er muligt at følge mødet både fysisk og virtuelt.
Tilmeld dig her Scan QR koden og tilmeld dig
20 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
New Drugs, New Targets – Highlights from ASH22
Psoriasis artrit-patienter, TNF-hæmmere og hæmatologiske cancere
En nylig nordisk registerundersøgelse har vist, at personer med psoriasis artrit (PsA) har en let til moderat øget risiko for at udvikle hæmatologiske cancere sammenlignet med alders- og kønsmatchede individer fra den almindelige befolkning. Undersøgelsen har dog også afsløret, at patienter med PsA, der er blevet behandlet med TNF-hæmmere, ikke har en øget risiko for hæmatologiske cancere sammenlignet med PsA-patienter, der ikke er blevet behandlet med TNF-hæmmere.
RENÉ CORDTZ er uddannet læge fra Københavns Universitet og har en ph.d. inden for reumatologisk epidemiologi. Han arbejder som post.doc. ved Center of Rheumatic Research Aalborg ved Aalborg Universitetshospital. LENE DREYER er klinisk lærestolsprofessor og specialeansvarlig overlæge i reumatologi ved Aalborg Universitet og Aalborg Universitetshospital. Hun er leder af Center of Rheumatic Research Aalborg (CERRA) og medlem af Dansk Reumatologisk Database (DANBIO)’s styregruppe.
Patienter med psoriasis artrit (PsA) har en øget forekomst af adskillige komorbiditeter.1 Der findes dog ikke et entydigt klart billede af, om hæmatologiske cancere hører til i denne byrde af komorbiditeter, hvilket ellers er tilfældet ved andre reumatologiske sygdomme med inflammation, herunder reumatoid artrit og systemisk lupus erythematosus.2,3 Det er heller ikke velundersøgt, om incidensen er forhøjet for undertyper som lymfoide og myeloide maligniteter sammenlignet med generelbefolkningen.4,5
I den moderne behandling af PsA indgår TNF-hæmmere som et vigtigt element i det samlede behandlingsrepertoire. Selvom det for reumatoid artrit er velbelyst, at behandling med TNF-hæmmere ikke er associeret med en øget incidens af hæmatologiske cancere, så er det forholdsvis mindre klart, hvorvidt det også er tilfældet for PsA-patienter behandlet med TNF-hæmmere.
Idet hæmatologiske cancere er forholdsvis sjældne cancertyper, søgte vi i et nordisk forskningssamarbejde at undersøge incidensen af denne cancertype hos PsA-patienter identificeret igennem de nordiske kliniske kvalitetsregistre for artritsygdomme.6 Studiets primære formål var at undersøge incidensen af hæmatologiske cancere hos patienter behandlet med TNF-hæmmere sammenlignet med PsA-patienter, der ikke fik behandling med TNF-hæmmere eller andre biologiske lægemidler. Som et sekundært formål blev incidensen af hæmatologiske cancere hos samtlige PsA-patienter sammenlignet med generelbefolkningen.
Identifikation af PsA-patienter og kontrolgrupper
Alle patienter med PsA blev identificeret i de kliniske, reumatologiske, forsknings- og kvalitetsregistre i Danmark (DANBIO), Finland (ROB-FIN), Island (ICEBIO), Norge (NOR-DMARD) og Sverige (SRQ). Denne kohorte af
PsA-patienter blev grupperet efter, om de var behandlet med TNF-hæmmere eller ej. For Danmark og Sverige blev der fra de to landes hospitalsregistre ligeledes identificeret endnu en gruppe af PsA-patienter, der ikke fik TNF-hæmmerbehandling. Danske og svenske patienter, der havde fået behandling med TNF-hæmmere, blev hver matchet med op til ti individer fra generelbefolkningen af samme alder og køn (og for svenske patienter, bopælsregion).
Med udgangspunkt i de danske og svenske data blev der dannet en overordnet PsA-kohorte bestående af alle PsA-patienter fra DANBIO, SRQ og de to førnævnte grupper af PsA-patienter fra hospitalsregistrene. Hver PsA-patient blev også her matchet på alder og køn med 10 individer fra generelbefolkningen.
Identifikation af hæmatologiske
cancere
Ved kobling med de respektive landes cancerregistre blev tilfælde af hæmatologiske cancere identificeret. Disse blev i sekundære analyser analyseret separat, alt efter om de var lymfoide eller myeloide maligniteter.
Opfølgning af behandling med TNF-hæmmere
TNF-hæmmer-behandlede patienter blev fulgt fra datoen for deres første TNF-hæmmer-behandling, mens TNF-hæmmer-naive patienter blev fulgt fra datoen for deres første registrerede ambulante besøg i det kliniske kvalitetsregister eller anden diagnosedato for PsA registreret i hospitalsregisteret. Alle patienter blev fulgt indtil datoen for deres første hæmatologiske cancer, emigration, død eller ved datoen for data-cut (forskellig for de involverede lande), alt efter hvad der kom først. Derudover blev TNF-hæmmer-naive PsA-patienter censureret, hvis de startede i behandling med et biologisk lægemiddel.
21 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
Statistisk analyse
Med brug af data fra alle fem lande beregnede vi i en modificeret Poisson-regressionsanalyse en poolet incidensrateratio (IRR) med 95% konfidensinterval for hæmatologiske cancere hos PsA-patienter behandlet med TNF-hæmmere sammenlignet med de PsApatienter, der ikke fik TNF-hæmmere.
Med danske og svenske data blev der også beregnet en justeret IRR for hæmatologiske cancere hos TNFhæmmer-behandlede patienter sammenlignet med TNF-hæmmer-naive PsA-patienter fra hospitalsregistrene. Ydermere beregnede vi den justerede IRR for TNF-hæmmer-behandlede patienter sammenlignet med matchede kontroller fra generelbefolkningen.
For at vurdere risikoen for hæmatologisk cancer i den overordnede danske og svenske PsA-kohorte (med alle PsA-patienter fra DANBIO, SRQ samt de danske og svenske hospitalsregistre) blev der beregnet en justeret IRR sammenlignet med matchede kontroller.
I sekundære analyser undersøgte vi for hver af ovenstående sammenligninger den separate IRR for hhv. lymfoide og myeloide maligniteter.
TNF-hæmmer, hæmatologiske cancere og PsA
I alt blev 10.621 TNF-hæmmer-behandlede patienter sammenlignet med 18.387 TNF-hæmmer-naive patienter.
Størstedelen af patienterne kom fra svenske SRQ (55%) og danske DANBIO (32%). Ved behandlingens start var patienter behandlet med TNF-hæmmere i alle lande yngre end tilsvarende TNF-hæmmer-naive patienter fra samme land og havde desuden højere DAS28-CRP, mens kønsratioen var nogenlunde ens.
Sammenlignet med TNF-hæmmer-naive patienter var der ikke en øget incidens af hæmatologiske cancere hos patienter behandlet med TNF-hæmmere ; dette baseret på hhv. 63 og 40 tilfælde : IRR 1,0 (0,7 til 1,4).
Sammenlignet med de TNF-hæmmer-naive PsApatienter fra Danmarks og Sveriges hospitalsregistre var der heller ikke en øget incidens baseret på hhv. 172 og 35 tilfælde : IRR 0,8 (0,6 til 1,1).
Derimod sås en øget incidens, når TNF-hæmmerbehandlede blev sammenlignet med deres matchede kontroller fra generelbefolkningen, her baseret på 35 mod 125 tilfælde : IRR 1,4 (1,0 til 1,9).
Den øgede incidens var dog generel for hele PsAkohorten, idet den havde en IRR på 1,4 (1,2 til 1,6) sammenlignet med de matchede kontroller, her baseret på 236 mod 908 tilfælde.
Disse IRR-estimater var stort set identiske for både lymfoide og myeloide maligniteter. Derudover viste resultaterne sig særdeles robuste i adskillige sensitivitetsanalyser.
Figur 1 – Incidensrateratioer for hæmatologiske cancere hos patienter med psoriasis artrit
Figur 1 – Incidensrateratioer for hæmatologiske cancere hos patienter med psoriasis artrit
Hæmatologisk cancer
TNF-hæmmer behandlede vs bionaive (kvalitetsregistre)
TNF-hæmmer behandlede vs bionaive (hospitalsregistre)
TNF-hæmmer behandlede vs matchede kontrolindivider
PsA kohorte vs matchede kontrolindivider
Figuren viser justerede incidensrateratioer for hhv. hæmatologiske cancere, lymfoide og myeloide maligniteter. Figuren er opdelt efter, hvilke grupper der sammenlignes, hvilket konkret udfald der undersøges, samt hvilke lande der bidrog med data til den pågældende analyse. DK : Danmark, NO : Norge, SE : Sverige, FI : Finland. Figur tilpasset fra : Cordtz RL et al. Haematological malignancies in patients with psoriatic arthritis overall and treated with TNF inhibitors : a Nordic cohort study. RMD Open. 2022 Dec ;8(2).
Figuren viser justerede incidensrateratioer for hhv. hæmatologiske cancere, lymfoide og myeloide maligniteter. Figuren er opdelt efter, hvilke grupper der sammenlignes, hvilket konkret udfald der undersøges, samt hvilke lande der bidrog med data til den pågældende analyse. DK: Danmark, NO: Norge, SE: Sverige, FI: Finland. Figur tilpasset fra: Cordtz RL et al. Haematological malignancies in patients with psoriatic arthritis overall and treated with TNF inhibitors: a Nordic cohort study. RMD Open. 2022 Dec;8(2).
BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023 22
0 0,5 1,0 1,5 2,0 2,5 0 0,5 1,0 1,5 2,0 2,5 0 0,5 1,0 1,5 2,0 2,5
DK, FI, NO og SE DK og SE
Lymfoid malignitet Myeloid Malignitet
Referencer :
1. Shah K, Paris M, Mellars L, Changolkar A, Mease PJ. Real-world burden of comorbidities in US patients with psoriatic arthritis. RMD Open. 2017 ;3(2) : e000588. DOI :10.1136/rmdopen-2017-000588
2. Baecklund E, Smedby KE, Sutton LA, Askling J, Rosenquist R. Lymphoma development in patients with autoimmune and inflammatory disorders – what are the driving forces ? Semin Cancer Biol. Feb 2014 ;24 : 61-70. DOI :10.1016/j.semcancer.2013.12.001
4. Vaengebjerg S, Skov L, Egeberg
3. Gross RL, Schwartzman-Morris JS, Krathen M, et al. A comparison of the malignancy incidence among patients with psoriatic arthritis and patients with rheumatoid arthritis in a large US cohort. Arthritis Rheumatol. Jun 2014 ;66(6) : 1472-1481. DOI :10.1002/art.38385
A, Loft ND. Prevalence, Incidence, and Risk of Cancer in Patients With Psoriasis and Psoriatic Arthritis : A Systematic Review and Meta-analysis. JAMA Dermatol. Apr 1 2020 ;156(4) : 421-429. DOI :10.1001/jamadermatol.2020.0024
5. Polachek A, Muntyanu A, Lee KA, et al. Malignancy in psoriatic disease : Results from prospective longitudinal cohorts. Semin Arthritis Rheum. Feb 2021 ;51(1) : 144-149. DOI :10.1016/j.semarthrit.2020.12.008
6. Cordtz RL, Askling J, Delcoigne B, et al. Haematological malignancies in patients with psoriatic arthritis overall and treated with TNF inhibitors : a Nordic cohort study. RMD Open. Dec 2022 ; 8(2). DOI :10.1136/rmdopen-2022-002776.
INTERESSEKONFLIKTER : René Cordtz er ansat ved IQVIA uden for dette arbejde. Lene Dreyer har modtaget honorarer for oplæg/ betalt kongresrejse fra Abbvie, Eli Lilly, Galderma, og Janssen og projekt-forskningsbevilling fra BMS uden for dette projekt.
KONKLUSION : I et nordisk samarbejde viste dette registerstudie, at PsApatienter behandlet med TNF-hæmmere ikke havde en øget incidens af hæmatologiske cancere sammenlignet med de patienter, der ikke fik behandling med TNF-hæmmere. Derimod var der generelt en let til moderat øget incidens af denne kræfttype hos patienter med PsA sammenlignet med generelbefolkningen.
23 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
Er risikoen for myelomatose geografisk betinget ?

Et nyligt udgivet studie har afdækket den geografiske fordeling af myelomatosepatienter i Danmark. Studiet afslørede en ujævn fordeling med en lavere forekomst i Østdanmark og en markant højere forekomst i Syddanmark.
LISE DUEHOLM BERTELSEN er medicinstuderende på Aalborg Universitet og forskningsassistent på Hæmatologisk Afdeling, Klinisk Kræftforskningscenter på Aalborg Universitetshospital.
Myelomatose er den næsthyppigste hæmatologiske kræftsygdom og udvikles ved malign proliferation af en klonal plasmacelle i knoglemarven. Sygdommen rammer primært ældre personer, og den forventede stigende levealder vil formentlig bidrage til en større andel myelomatosepatienter i fremtiden. Forebyggende tiltag er derfor nødvendige, men forudsætter kendskab til ætiologien, der stadig er ukendt.
På nuværende tidspunkt er høj alder og mandligt køn blandt de få kendte risikofaktorer, der øger sandsynligheden for at udvikle myelomatose, men en stigende mistanke til risikofaktorer i miljøet har de seneste årtier affødt mange nye studier. Fælles for tidligere studier er, at de overvejende fokuserer på eksponeringer gennem erhverv. Kun et fåtal tager udgangspunkt i patienternes bopæl og sandsynliggør, at høj-incidens-områder kan skyldes potentielle risikofaktorer i miljøet. Imidlertid er disse studier begrænset af manglende justering for baggrundsbefolkningens alders- og kønssammensætning eller store geografiske inddelinger sammenlignet med for eksempel danske kommuner. Vores nyligt publicerede
studie gør op med disse udfordringer og undersøger den geografiske fordeling af myelomatosepatienter i Danmark på kommuneniveau.*
Geografisk fordeling af myelomatosepatienter
Studiet er baseret på data indhentet fra Dansk Myelomatose Database og inkluderer patienter med behandlingskrævende myelomatose diagnosticeret mellem år 2005 og 2020. Patienternes bopælskommune blev identificeret via det Centrale Person Register og det Danske Adresseregister. For hver af de 98 danske kommuner blev den alders- og køns-standardiserede incidensrate pr. 100.000 person-år udregnet, og dermed blev der taget højde for baggrundsbefolkningens varierende demografi.
Studiepopulationen udgjorde 5.243 myelomatosepatienter og viste en overordnet ujævn, heterogen, fordeling med hovedsageligt lave incidensrater i Østdanmark og påfaldende høje incidensrater i Syddanmark.
Fire kommuner (Vejen, Horsens, Vejle og Albertslund) havde en bemærkelsesværdig højere incidensrate i forhold til den nationale incidensrate, og særligt påfaldende
24 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
var Vejen Kommune med den højeste incidensrate på 9,6 pr. 100.000 person-år. Ud af de fire nævnte kommuner var tre (Horsens, Vejle og Vejen) forholdsvis tæt placeret i Syddanmark og udgør et potentielt hotspotområde.
Incidensen i land-, forstads- og bykommuner
Danmarks Statistik har på baggrund af en international klassificering inddelt de danske kommuner i henholdsvis land-, forstads- og bykommuner. Ud fra denne inddeling har dette studie fordelt myelomatosepatienterne på baggrund af bopælskommunen og udregnet den alders- og kønsstandardiserede incidensrate pr. 100.000 person-år for hver (land-, forstads- og by-områder).
Incidensrate-ratioen mellem land- og byområder viste en signifikant forskel med 8% øget incidensrate i landområder. Incidensrate-ratioen mellem forstads- og byområder viste en 7% øget incidensrate i forstadsområder, men forskellen var ikke signifikant.
Flytninger blandt patienterne og andre udfordringer
Selvom den geografiske udbredelse af patienter kan være et nyttigt værktøj til at undersøge, om miljøet spiller en rolle i forhold til risikoen for at udvikle en kræftsygdom, er der mange udfordringer forbundet med fremgangsmåden. Myelomatosepatienter flytter rundt i løbet af deres liv, men en sensitivitetsanalyse viste, at det drejede sig om forholdsvis få patienter. I en 25-årig periode op til diagnosetidspunktet var det kun 20% af patienterne, der havde boet i en anden kommune end den, de boede i omkring diagnosetidspunktet.
KONKLUSION
Foruden flytninger er der mange spekulationer forbundet med at undersøge miljøeksponeringer ved den geografiske fordeling baseret på adressen omkring diagnosetidspunktet. Disse spekulationer bunder hovedsageligt i tre ubekendte faktorer :
1. Hvor lang tid inden diagnosetidspunktet er de eksponeret ?
2. Hvor længe skal eksponeringen vare, før den medfører en risiko ?
3. Kan risikoen ved eksponeringen variere fra person til person ?
Imidlertid kræver afklaring af disse ubekendte, at fremtidig forskning formår at afklare, om der i det hele taget er miljøfaktorer, der øger risikoen for at udvikle myelomatose, og i så fald, hvilke faktorer der ved tilstrækkelig mistanke skal danne grundlag for videre undersøgelse.
Et behov for yderligere undersøgelser Studiet lægger i den grad op til yderligere undersøgelser af risikofaktorer i miljøet, blandt andet med fokus på det potentielle hotspotområde. En endnu mere detaljeret geografisk inddeling vil desuden udgøre et bedre fundament for undersøgelse af stoffer i miljøet i høj-incidens-områderne. Den højere forekomst i landområder advokerer også for yderligere undersøgelser med fokus på myelomatose-patienternes erhvervsfordeling og potentielle sundhedsskadelige stoffer i landbrugserhvervet.
*OPRINDELIG PUBLIKATION OG MEDFORFATTERE : Denne artikel er baseret på en publikation ved European Journal of Haematology : Bertelsen LD, Børty Nielsen L, Christensen HS, Bøgsted M, Gregersen H, Pedersen RS, Klostergaard A, Schnack BI, Pedersen PT, Abildgaard N, Hermansen E, Vangsted AJ, Severinsen MT. Geographical and ecological analyses of multiple myeloma in Denmark : Identification of potential hotspot areas and impact of urbanisation. Eur J Haematol. 2023 Mar ;110(3) : 289-295. DOI : 10.1111/ejh.13904. Epub 2022 Dec 4. PMID : 36413106. Medforfattere : Lise Dueholm Bertelsen, Lars Børty Nielsen, Heidi Søgaard Christensen, Martin Bøgsted, Henrik Gregersen, Robert Schou Pedersen, Anja Klostergaard, Brian Iversen Schnack, Per Trøllund Pedersen, Niels Abildgaard, Emil Hermansen, Annette Juul Vangsted og Marianne Tang Severinsen.
INTERESSEKONFLIKTER : Ingen.
: Resultatet af vores studie taler for, at miljøet omkring patienternes bopæl spiller en rolle i forbindelse med risikoen for udvikling af myelomatose. Desuden bekræfter den højere forekomst i landområder en udbredt mistanke til, at landbrugserhvervet og pesticider udgør potentielle risikofaktorer for myelomatose.
25 BestPractice Nordic / Onkologi og Hæmatologi / Nr. 10 / 2023
TAKE CONTROL OF RCC WITH CABOMETYX® + nivolumab
TAKE CONTROL OF THE DISEASE
Superior efficacy (OS, PFS, ORR)* vs. sunitinib demonstrated in a population reflective of real-life practice.1-6
14 months mOS gain versus sunitinib and an early separation of the Kaplan-Meier curve, sustained over time. 6-8
TAKE CONTROL OF THE TREATMENT EXPERIENCE
A well-understood tolerability profile and a low rate of AE-related discontinuations (7% both CABOMETYX® and nivolumab).1,2,5,6
Optimised CABOMETYX® dosing, easily adjusted to meet patients’ needs. 5



Indikation for CABOMETYX® : †


CABOMETYX® er indiceret som monoterapi til fremskredent nyrecellekarcinom som førstelinjebehandling hos voksne patienter med middel eller høj risiko samt voksne efter tidligere behandling med målrettet vaskulær endotelial vækstfaktor (VEGF). Indiceret som førstelinjebehandling af fremskredent nyrecellekarcinom hos voksne i kombination med nivolumab.†
Indikation for nivolumab: †
Renalcellekarcinom (RCC): nivolumab er som monoterapi indiceret til behandling af fremskredent RCC hos voksne efter tidligere behandling. Nivolumab i kombination med ipilimumab er indiceret til førstelinjebehandling af voksne patienter med fremskredent renalcellekarcinom i mellem- eller højrisikogruppen. Nivolumab i kombination med cabozantinib er indiceret til førstelinjebehandling af voksne patienter med fremskredent renalcellekarcinom.
†Her er kun vist indikation for RCC. For fuld indikation henvises til pligttekst.
CBZ-DK-0001432023-03
NIVOLUMAB
* mOS: 49.5 vs 35.5 mo p<0.0001 mPFS: 16.6 vs 8.4 mo p<0.0001 ORR: 56 vs 28%.
2.
al. New Engl J Med. 2021; 384: 829–841. 3. Heng DYC, et al. Lancet Oncol. 2013; 14: 141–148. 4.
6. Burotto M, et al. Abstract presented at ASCO GU 2023. Abstract No.603. 7. Rini BI, et al.
Presented
KCRS 2021.
Se pligttekst side 26 – 27.
1. Powles T, et al. J Clin Oncol. 2022; 40 (suppl 6): 350.
Choueiri TK, et
Hall JP, et al. Future Oncol. 2020; 16: 3045–3060. 5. Cabometyx SmPC.
Abstract 4500. Presented at ASCO 2021. 8. Choueiri TK, et al. Oral presentation.
at
Institut Produits Synthèse (IPSEN) AB, Färögatan 33, SE-164 51 Kista, Sweden

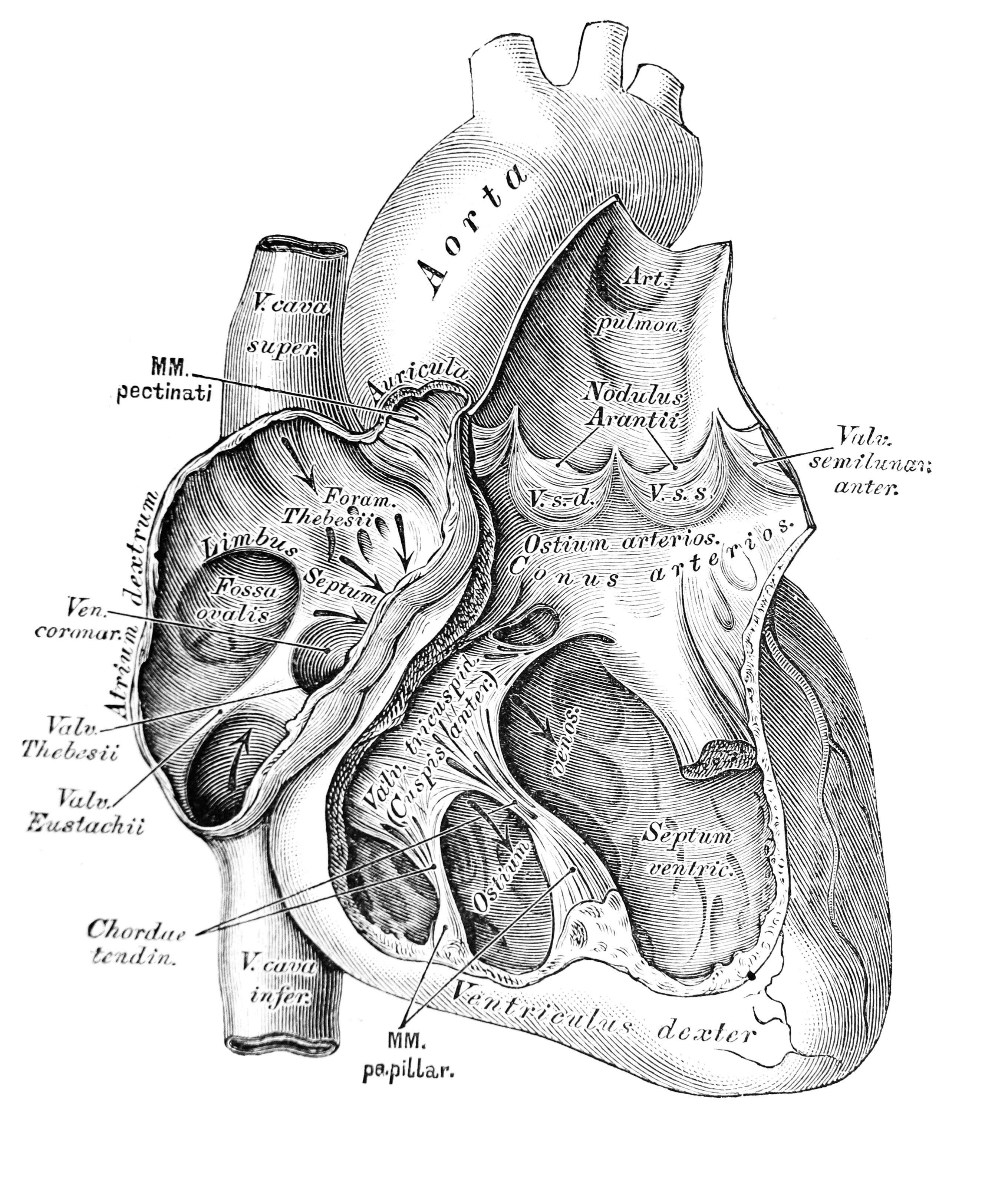















 Figure 1 – Lipoproteins
Figure 1 – Lipoproteins
































