GIT












➢ Aphthous stomatitis : Allergic inflammation in children. T




➢ Herpetic stomatitis : Herpes simplex infection
➢ Vincent’s angina : Necrotizing inflammation of the mucosa of tonsils and gums caused by Treponema vincenti and Bacillus fusiformis in patients with low resistance
➢ Agranulocytic angina : Severe inflammation of the gums, and nasopharynx due to agranulocytosis
➢ Moniliasis or thrush : Oral candidiasis
A common viral disease occurs in association with or following fevers
Herpes simplex
The lesion appears as vesicles ( which contain clear serous fluid and few leucocytes ) occurs on the mucocutaneous junction of the lips, buccal mucosa and conjunctiva.
A common tumour occurring more in males more common in the lower lip. Usually a malignant ulcer with everted edges ( less commonly a polypoid growth )
Well and moderately differentiated squamous cell carcinoma.
infiltrates locally of the chin and mandible Lymphatic spread to the submental and upper cervical lymph nodes
• Def : thick white mucosal patches that cannot be scrapped off
• Cause: Chronic irritation due to : 1- excessive smoking 2- ragged tooth


3- diffuse syphilitic inflammation (3ry).
• It is squamous cell hyperplasia
• can develop into dysplasia, carcinoma in situ, and invasive carcinoma

• The stratified squamous epithelium shows acanthosis (hyperplasia of the prickle cell layer) and hyperkeratosis (increased thickness of the superficial keratinized layer)
• It can also be seen in inflammatory conditions unrelated to malignancy
• affecting immunocompromised patients.
Shallow traumatic ulcer at the edge of the tongue related to a sharp tooth.
Multiple, small, superficial painful ulcers. The pathogenesis is not clear and the ulcers are of short duration.
Common in the anterior two thirds. The edges are everted, the floor necrotic and the base indurated.
Undermined ulcer near the tip caused by coughed sputum in case of opened pulmonary tuberculosis
• Benign Tumors: Squamous cell papilloma, cavernous haemangioma, cavernous lymphangioma, fibroma, leiomyoma and myoblastoma.

• Malignant Tumors: Squamous cell carcinoma and adenocarcinoma.
More common in middle aged males its Precancerous lesions: (a) Leukoplakia. (b) Tertiary syphilis of the tongue (c) Squamous cell papilloma. Gross more common in the anterior two thirds it is a malignant ulcer with everted edges. The tumor has all grades of differentiation

Blood spread is rare.



Local spread to the floor of the mouth
Lymphatic : the submental, submaxillary and deep cervical lymph nodes
Lymphatic spread is rapid due to the rich lymphatics of the tongue and its continuous movements




•

Microscopic picture:
(a) Epithelial elements → form ducts, acini, tubules and sheets of cells. They are of ductal and myoepithelial origin. The cells lining ductal and glandular formations are cuboidal or columnar , there are spindle myoepithelial cells underlie the cubical epithelium
(b) Mesenchymal elements → Loose connective tissue, myxoid tissue, chondroid matrix and rarely bone ➢ N.B : The epithelial and mesenchymal elements are intermixed and one of them may predominate
• Behavior: ➢ slow rate of growth ➢ Recurrence after surgical removal may occur ➢ The tumor may undergo malignant change.
Called papillary cystadenoma lymphomatosum or adenolymphoma
arises in the parotid glands ( About 10% are bilateral ) most common in smokers majority arises after the age of 50 years
The cut surface shows cystic spaces with papillary projections
Cystic spaces lined by columnar cells Which also cover the papillary projections
The stroma contains lymphoid tissue with germinal centers
Cystic spaces contain mucinous gray or pale brown Secretion
















Pathological features:
o Catarrhal inflammation in which the mucosa is hyperemic, edematous and covered by excess mucous




o Petechial hemorrhage and small superficial ulcerations may occur.
Definition:Chronic gastritis is defined as the presence of chronic inflammatory changes in the mucosa leading eventually to mucosal atrophy and epithelial metaplasia

Etiology:
o Infective: Chronic infection specially by Helicobacter pylori .
o Autoimmune gastritis due to formation of antibodies against parietal cells causing their destruction and atrophy.
o Toxic effects of excess alcohol and tobacco .
o Exposure to radiations .

o Crohn's disease, amyloidosis and uremia.
Pathological features:
o Infiltration of the lamina propria by inflammatory cells mainly plasma cells and lymphocytes, occasionally accompanied by neutrophilic inflammation of the neck region of the mucosal pits.
o Atrophy of the glandular epithelium. When present, H.pyloriorganisms are found nestled within the mucus layer overlying the superficial mucosal epithelium. In the autoimmune variant, loss of parietal cells is particularly prominent.
o Gastric mucosa may show dysplasia and intestinal metaplasia. Intestinal metaplasia refers to the replacement of gastric epithelium with columnar and goblet cells of intestinal variety. This is significant, because gastrointestinal-type carcinomas seem to arise from dysplasia of this metaplastic epithelium.
Chronic superficial gastritis: The inflammatory infiltrate is limited to the foveolar region and unaccompanied by glandular atrophy. Neutrophils may be present and denoting high inflammatory activity.

Chronic atrophic gastritis: Inflammation is more extensive and accompanied by glandular atrophy.








According to the degree of atrophy, chronic atrophic gastritis is classified into mild, moderate and severe types.
Definition :Peptic ulcers are chronic, most often solitary, lesions that occur in any portion of the gastrointestinal tract exposed to the aggressive action of acidic peptic juices.
At least 98% of peptic ulcers are either in the first portion of the duodenum or in the stomach, in a ratio of about 4:1. Peptic ulcers are remitting, relapsing lesions that are most often diagnosed in middle-aged to older adults
Duodenal and gastric ulcers are the commonest with a ratio of 10:1 in Egypt.
They occur at any age but commonly between 20-40 years.
Male to female ratio is 3:1.
Sites

The first part of the duodenum (80%).
Lesser curvature of the pyloric antrum of the stomach








The lower part of the esophagus (Barrett's mucosa).
The jejunum after gastrojejunostomy.
Meckel's diverticulum if it contains ectopic gastric mucosal tissue.
Predisposing factors: Spicy and hot food, tobacco, aspirin, steroids and psychological factors as mental tension and strain.
Pathogenesis :Two conditions are key for the development of peptic ulcers
Mucosal exposure to gastric acid and pepsin. It is best perhaps to consider that peptic ulcers are created by an imbalance between the gastroduodenal mucosal defenses and the damaging forces that overcome such defenses. Both sides of the imbalance are considered
H. pylori infection, which has a strong causal relationship with peptic ulcer development
1-Hereditary predisposition:

Strong family history
More common in people with blood group o


2-Hyperacidity caused by:
Increased number of parietal cells causing hyperchlorhydia.




Chronic stress with high vagal tone causing hypersecretion of the gastric juice.
Zollinger-Ellison syndrome: Gastrinoma which is a gastrin-secretin
tumor of the pancreas causes gastric hypersecretion and hyperacidity
(3) Infection by Helicobacter pylori
1-Devitalization of the gastric mucosa caused by: (a) Impaired mucus-bicarbonate barrier (b) Decrease mucosal blood in ischemia and shock (c) Chronic gastritis specially caused by Helicobacter pylori due to enzymatic effect. (d) Duodenal-gastric reflux where bile and pancreatic juice cause mucosal injury. (e) Delayed gastric emptying
2-Traumatic effect of food on a normal or devitalized mucosa causes ulcers mainly on the lesser curvature
Acid secretion is normal or reduced.
Sites:

1-Gastric ulcers are common along the lesser curvature of the pyloric antrum.
2- Duodenal ulcers occur in the first part, more common in the anterior wall.
Size:


o Gastric ulcers are 1-3 cm in diameter, while duodenal ulcers are usually about 1 cm in diameter.
Shape:
o Rounded or oval.





o A saddle-shaped ulcer may occur in the stomach o It overrides the lesser curvature and extends on both surfaces.

Margin:
o The mucosa around the ulcer, is smooth and atrophic
Edge:
o Sloping or step-like Floor:
o Is clean and made of the serosa or the remains of the muscle layer.

Base: o Is indurated due to the extensive fibrosis

Outer serosal covering:
o Appears opaque white and puckered due to fibrosis, and adherent to the surrounding structures.

The base of the ulcer shows two layers:

o superficial layer of granulation tissue infiltrated by neutrophils. Its top part is necrotic.
o deeper layer of fibrous tissue showing remains of the muscle layer, foci of chronic inflammatory cells and endarteritis obliterans.

Hemorrhage: Causes: o The traumatic effect of food on the, granulation tissue in the floor of the ulcer o Erosion of a vessel in the floor or the wall of the ulcer. Hemorrhage causes hematemesis and melena

perforation: Occurs in 10% of the cases. o Perforation is precipitated by heavy meals or drugs as steroids and phenylbutazone. o Perforation of a gastric ulcer results in localized or diffuse peritonitis. o A duodenal ulcer may perforate into the peritoneum or penetrate into the pancreas causing pancreatitis.
Cicatricial contraction: o Causes pyloric or duodenal stenosis. o Fibrosis of a saddle shaped ulcer on the lesser curvature pull on the greater curvature constricting the stomach in the middle i.e. hour-glass stomach



Malignant change: o Occurs in 1-2% of the gastric ulcers.


















the malignant tumors that occur in the stomach, carcinoma is the most important and the most common (90% to 95%). Next in order of frequency are lymphomas (4%), carcinoids (3%), and stromal tumors (2%).




Gastric carcinoma is more common in males in the fifth and sixth decades.

The tumor is common in Japan, but rare in Africa.

Risk Factors for gastric carcinoma
o Chronic gastritis with intestinal metaplasia o Nitrites derived from nitrates (found in food and drinking water,and used as preservatives in prepared meats, may undergo nitrosation to form nitrosamines and nitrosamides o Infection with Helicobacterpylori o Diets containing foods that may generate nitrites (smoked foods, pickled vegetables and excessive salt intake) o Decreased intake of fresh vegetables and fruits (antioxidants present in these foods may inhibit nitrosation) o Partial gastrectomy o Pernicious anemia





Site
All parts of the stomach may be involved, but most gastric carcinomas occur in the antrum, pylorus, cardia and lesser curvature.

1. Polypoid or fungating carcinoma:

Large fungating mass which projects into the lumen of the stomach with surface ulceration and secondary infection.

2.Ulcerative carcinoma:
A malignant ulcer, more than 3 cm in diameter with raised everted edge and indurated base.
3.Infiltrating carcinoma: Which is either :
A- Localized type:
o Affects the pyloric region


o The wall becomes thick and rigid and the lumen is moderately reduced.
o The rest of the stomach dilates.
B-Diffuse type:


o The whole stomach wall is infiltrated by the malignant growth which shows marked fibrosis.
o The wall becomes thick and leathery and the lumen is markedly reduced "Leather bottle stomach". There is no mucosal ulceration.
1. Adenocarcinoma: The polypoid and ulcerative carcinoma are usually moderately differentiated adenocarcinoma.
This is the commonest type.





2.Mucoid carcinoma: Secrete abundant mucin.
3.Signet-ring cell carcinoma.







4.Undifferentiated carcinoma. Histological types of gastric carcinoma
histologic appearances of gastric cancer are best classified into the intestinal type and diffuse type.
intestinal variant Diffuse variant is composed of malignant cells forming neoplastic intestinal glands resembling those of colonic adenocarcinoma.
is composed of gastric-type mucous cells that generally do not form glands but rather permeate the mucosa and wall as scattered individual "signetring" cells or small clusters in an "infiltrative" growth pattern.
1.Hemorrhage: Usually chronic causing microcytic hypochromic anemia. Gastric hemorrhage is manifested as hematemesis and melena.
2.Pyloric obstruction.
3. Mucosal destruction causes hypochlorhydria or achylia. Deficiency of the intrinsic factor may cause macrocytic anemia.






The overall prognosis of gastric cancer is poor, with an average of only 10% to 15% 5-year survival, even in patients who receive a “curative” resection
Adverse prognostic factors:
include age older than 70 years; tumor location (proximal is worse than distal); venous/lymphatic invasion


The most powerful determinant of prognosis is the pathologic stage. The tumor-node-metastasis (TNM) system








Definition: Infectious disease caused by Salmonella typhi affecting mainly lymphoid tissue of the intestine.

Mode of infection:
contamination may be direct or by the way of flies.
Ingestion of food or drink contaminated by typhoid bacilli from patient or carrier.
Bacteria are carried by macrophages from the intestinal lumen to the intestinal lymphoid tissue (Peyer's patches).
- No local damage or inflammation occurs.
The organisms invade the lymphatics to the mesenteric lymph nodes and finally reach the blood stream via the thoracic duct resulting in bacteremia.
The bacteria are removed from the blood by cells of reticulo-endothelial system (in the liver, spleen, bone marrow ...etc).

By the end of the incubation period (10-14 days) the RE cells carrying the bacilli undergo necrosis and large number of bacteria enter the blood stream resulting in septicemia.






The bacteria multiply in the RE cells.
- This is accompanied by development of the pathological lesions.
Tissue Reaction:
Consists of macrophages (monocytes and histiocytes).
The reaction appears to be a delayed hypersensitivity (Type IV) reaction.
The lesions develop in the lymphoid tissue of Peyer's patches and solitary follicles. They are most marked just above the ileo-cecal valve.
1) Changes occur during the first week of disease: The mucosa and lymphoid tissue become hyperemic A large number of macrophages appear among the lymphoid tissue which become swollen and project onto the surface.

2) Changes occur during the second week of disease: Focal necrosis of the covering mucosa occurs. The foci of necrosis become confluent and end in slough formation.

3) Separation of sloughs during the third week of the disease results in ulcer formation.
4) The Ulcer: is irregularly oval. raised and its longitudinal axis is parallel to that of the intestine. Its edges are soft and undermined. The floor is smooth and necrotic. heal by granulation tissue and regeneration of surface epithelium.

5) The resultant scar is thin and stricture formation never occur. 6) The draining mesenteric lymph nodes are enlarged.
7) Cut surface shows necrosis and hemorrhage.
1. moderately enlarged.

2. shows a picture of acute splenic swelling.
3. The pulp is soft, dark red and shows greyish areas of necrosis.




4. Microscopically, red pulp is congested and crowded by macrophages.
5. Lymph follicles are compressed.
Bone marrow:
1. A tissue reaction (composed of macrophages) crowds the bone marrow & reduces formation of white blood series.
2. Leucopenia with relative or absolute monocytosis results.
Typhoid bacilli:
1.multiply in the gall bladder
2. reach the intestine in bile to be discharged in stool, so a carrier state may result after recovery.
3. may form a nucleus for gall stone formation (mixed type).
4. may induce acute or chronic cholecystitis.
Degenerative changes: caused by toxemia
Liver: Cloudy swelling, fatty change and focal necrosis.
Heart: Cloudy swelling, fatty change and dilatation of its cavities.
Muscles: Zenker's degeneration may occur in the rectus abdominus, diaphragm or intercostal muscles.
Vessels: Thrombosis in the leg veins and cerebral sinuses due to toxic endophlebitis.
Skin: Maculopapular rose rashes.
1. Intestinal hemorrhage from slough separation in 5-10%.
2. Septic peritonitis from perforation of deep ulcer.
3. Acute heart failure due to toxemia.

4. Bronchopneumonia caused by typhoid bacilli or a mixture of pathogenic bacteria.
5. Cholecystitis, gall stones and Zenker's degeneration. 6. Degenerative changes due to toxemia.
7. Typhoid osteomyelitis, localized periostitis which develops after months or years.
8. Meningitis, Encephalitis, Neuritis, Pyelonephritis and Endocarditis.


Definition: Inflammation of the colon characterized by diarrhea, tenesmus and passage of blood and mucous in stool. Types: common types are:

Gross picture:
1) Amoebae destroy the mucosa and muscularis mucosa to reach the submucosa mainly in the cecum and rectum where they multiply. 2) In the submucosa, they cause marked necrosis by their enzymes. 3) Separation of necrotic material results in small flask shaped ulcers. 4) Ulcers have: Undermined edges Yellowish necrotic floor

Variable depths The base is formed of the muscle layer 5) The mucosa in between the ulcers appears normal. 6) In the majority of cases, Healing of the above lesions occurs due to high body resistance. - However, the organism may remain in the intestinal tissue and a carrier state results. 7) In 10% of cases, The lesions progress and result in round or oval ulcers measuring up to few cm's. - Healing of these ulcers leaves smooth depressed surface and fibrous stricture may result.
Microscopic picture: The edges and floor of the ulcers consist of necrotic tissue. Inflammatory cells are few and consist of neutrophils and macrophages. The amoebae are: present in the tissues and inside the blood vessels. Rounded or oval. The nucleus is eccentric and measures 2-5 micron. 20-25 micron. The cytoplasm contains digestive vacuoles. surrounded by clear rings due to digestion of the surrounding tissues by proteolytic enzymes. Degenerated and dead amoebae stain red with eosin.

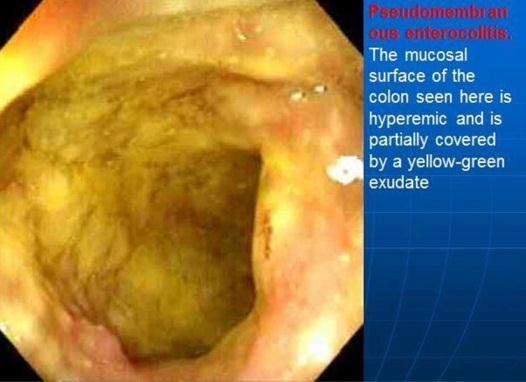
1. Ulceration causes Intestinal hemorrhage. 2. Perforation of deep ulcers causes Pericolic abscess or diffuse suppurative peritonitis. 3. Abnormal peristalsis may result in Intussusception. 4. Continual straining at stool may result in Rectal prolapse. 5. Intestinal stricture and chronic intestinal obstruction. 6. Amoeboma is a granuloma seen in the cecum and rectum as a result of amoebic infection and secondary bacterial infection. 7. Amoebic infection may spread directly to the perianal skin and vagina, and by blood to the liver causing amoebic hepatitis or amoebic abscess 8. Amoebic lung and brain abscess rarely occur. Definition: Pseudo-membranousinflammation of the colon caused by Shigella organisms.
Mode of Infection:

Ingestion of bacilli in contaminated food or drink
transmitted mainly by flies.
Gross Picture: 1) The mucosa of the colon is congested and edematous
Greyish white patches of necrosis appear.

A pseudo-membrane forms on the surface & may be stained green by bile or dark brown by blood.
Separation of parts of the membrane results in Small irregular superficial ulcers which may coalesce.
Intestinal lumen contains:
Draining lymph nodes:








Definition: Chronic non-specific inflammation of the colon of unknown etiology, begins in the rectum and gradually extends along the colon in a retrograde fashion.
The disease has a familial tendency
may be an allergic, auto-immune or psychosomatic disorder.
Active phase: The mucosa shows congestion, edema, focal hemorrhages and small ulcerations.
Chronic phase: The mucosa in between the ulcers form hyperplastic pseudo-polypoid projections, mucosal dusplasia.
The ulcers coalesce to form larger & irregular superficial ulcers.
Healing by fibrosis causes thickening of the wall and narrowing of the lumen.
Inflammation mainly affects the mucosa.
The mucosa shows congestion, edema, ulceration and infiltration by lymphocytes, plasma cells, macrophages & eosinophils.


PML and pus cells occasionally collect at the depth of the mucosal crypts forming small crypt abscesses.
The pseudo-polyps consists of: hyperplastic mucosa & granulation tissue.
With healing epithelial regeneration occurs, but may show gastric metaplasia.
1. Intestinal hemorrhage.
2. Perforation causing peritonitis.

3. Colonic stricture.

4. Peri-anal fistula.
5. Malignancy.
6. Secondary amyloidosis.

✓ Diseases of the appendix
✓ Intestinal Diverticulae

✓ Hernia and its complications


✓ Tumors of appendix
✓ Tumors of small & large intestine ✓ Megacolon and bleeding per rectum

Organisms: Streptococcus pyogenes, staphylococcus aureus and E. coli.

Pathogenesis: Infection usually from the lumen but may be blood born. Obstruction is present in a large number of cases.
Obstruction is caused by:
1. The lumen is obstructed by a foreign body as vegetable or fruit seeds or by a foecolith. This is the most common cause 2. Hyperplasia and swelling of the submucosal lymphoid tissue. 3. Post-inflammatory fibrosis of the wall. 4. Peritoneal adhesions. 5. Spasm of the muscle coat at the base of the appendix. 6. Obstruction causes mucous accumulation in the lumen.

7. The pressure is raised and causes compression and occlusion of the arteries supplying the mucosa.
8. The resulting ischemia causes devitalization of the mucosa and easy invasion by bacteria.
a) Acute catarrhal appendicitis: b) Acute suppurative appendicitis:
This is the early and mild stage of the disease.
• The appendix is slightly swollen and congested.
Microscopically: the mucosa and submucosa show hyperemia, edema, infiltration with neutrophils and increased mucous secretion.
At this stage the lesion may regress resulting in minimal fibrosis or pass to suppurative stage.
Is the common and classic picture of acute appendicitis.

• The appendix is elongated, swollen and congested.
• The lumen is narrowed and filled with purulent exudate.

• The mucosa is hyperemic, edematous and ulcerated.
• The outer serosal surface shows dilated congested vessels and yellow patches of purulent exudate.
Microscopically:
Occurs in severe cases accompanied by complete obstruction.
• Suppuration proceeds to necrosis usually at the tip followed by putrefaction.
• The appendix is dark brown to black, friable and usually perforate.
Complications:
c) Acute gangrenous appendicitis: 34
1. The mucosa shows partial shedding.
2. All coats show hyperemia, inflammatory edema and infiltration by large number of PML and pus cell.
3. The omentum and loops of the intestine may stuck by fibrinous exudate to the surface of the appendix resulting in a localized inflammatory mass "Appendicular mass".
2. Septic peritonitis mostly localized.
3. Septic thrombophlebitis of the appendicular vein causes portal pyemia.
4. Persistence of inflammatory reaction with fibrosis causes chronic appendicitis.
5. Fibrotic obstruction and distension of the lumen with mucus causes mucocele of the appendix.

6. Fistula formation.
7. Peritoneal adhesions.
4. The mass may resolve or suppuration occurs with formation of appendicular abscess.
5. The abscess may resolve or rupture on the abdominal wall, in a loop of the intestine or in the peritoneal cavity causing diffuse septic peritonitis.


6. Septic thrombophlebitis occurs in the appendicular vein and may cause portal pyemia.
• Chronic appendicitis is a fibrosed appendix resulting from healing of mild attacks of acute appendicitis.
• Fibrosis may be diffuse in the wall with a patent lumen (chronic nonobliterative appendicitis), or focal causing stenosis of the lumen.
• Marked fibrosis obliterates the lumen (chronic obliterative appendicitis).



Occur in the duodenum and the cecum and the wall consists of all intestinal coats.

Meckel's diverticulum:
It is due to failure of obliteration of the proximal part of the vitello-intestinal duct which passes from the intestine to the umbilicus in the embryo. The diverticulum forms a blind intestinal pouch 1-3 inch in length on the anti-mesenteric border of the lower ileum, 1-3 feet from the ileo-cecal valve.
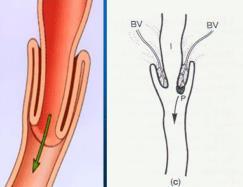
1. Degenerative changes in the muscle coat in middle and old age causing weakness of the wall specially at points of entry of blood vessels and nerves (mesenteric border).
2. Increased intra-luminal pressure due to gaseous distension in constipation.
Sites:



1. Concave border of the second part of the duodenum.
2. Mesenteric border of the jejunum and ileum.
3. Descending and sigmoid colon. This is the commonest site.
4. The diverticula are multiple and occur on the convexity of the intestine opposite the mesenteric attachment and between the longitudinal muscle bands (taeniae).
1. Acute diverticulitis is the commonest complication and may lead to formation of a pericolic abscess.
2. Intestinal hemorrhage.
3. Perforation causing septic peritonitis usually localized.
4. Fistulae with the small intestine, bladder and abdominal wall.
5. Fibrosis results in chronic intestinal obstruction.





Effects:
1. Strong peristalsis above the obstruction.
2. Distension above the obstruction by the intestinal fluids.
3. Distension interferes with venous drainage from the intestine, venous congestion occurs with extravasation of blood in the intestinal wall, lumen and peritoneal cavity.
4. Bacteria penetrate the intestinal wall causing peritonitis.
Causes:
1. Free intestinal loop or omentum enters the hernial sac.
2. Fecal content accumulated in the herniated sac.
Effects:
1. Pressure on the herniated loop against the sharp edge of the hernial ring causes venous obstruction with the development of congestion and edema.
2. Arterial occlusion results in hemorrhagic infarction or gangrene.
3. The wall becomes edematous, dark red and shows ecchymosis.

4. Peritonitis and toxemia.
Definition: Invagination of an intestinal segment (intussusceptum) into another adjacent distal segment (intussusceptien).
The condition commonly occurs in infants and children and rarely in adults.

Causes:
1- Irregular peristalsis induced by gastro-enteritis and inflammation of intestinal lymphoid tissue in babies.
2- Irritating food, overfeeding, fasting, intestinal parasites.
3- Meckel's diverticulum, polypoid tumors and rarely bilharzial polyps.
Types:
1. Ileo-cecal:

Starts at the ileo-cecal valve where a segment of the small intestine invaginates into the large intestine and may reach the rectum. This is the commonest type.

2. Enteric type (ileo-ileal): A segment of the small intestine invaginates into another distal segment. It may begin as enteric type and then the intussusceptum passes through the ileocaecal valve.
3. Colo-colonic type: Is rare.
Effects:
1. Compression of the veins causes congestion and edema in the intussusceptum.
Blood extravasated into the intestinal wall and lumen.
2. Obstruction of the arteries results in hemorrhagic infarction.
3. Blood and mucus per rectum.
III. Volvulus:
Definition: Twisting of a loop of the intestine upon itself through 180° or more. The condition occurs in the sigmoid colon and less commonly in the small intestine.
Predisposing factors:
1. Long mesocolon.
2. Loaded sigmoid colon due to constipation.
3. Peritoneal adhesions.
Effects:
1. Obstruction of the lumen and blood vessels.
2. Hemorrhagic infarction, gangrene and peritonitis.
Definition: A segment of the intestine loses its peristaltic movements.


Causes: 1. Peritonitis inhibiting the parasympathetic activity by bacterial toxins. 2. Operative trauma to the intestine stimulating the sympathetic fibers. 3. Spinal cord injuries Effects: Functional obstruction, intestinal dilatation above the obstruction, vomiting and dehydration.

Mesenteric Vascular Occlusion:
Causes: Arterial thrombosis caused by: A. Atherosclerosis B. Embolism of the superior mesenteric artery. Effects: Hemorrhagic infarction of the intestine, gangrene and acute intestinal obstruction.
Definition:
Gradual incomplete obstruction to the passage of the intestinal contents.

Causes:
1. Post-inflammatory stricture of the intestine caused by tuberculosis, amoebic and bacillary dysentery, diverticulitis, ulcerative colitis and regional enteritis.
2. Carcinoma of the colon specially of the annular type.
3. Peritoneal adhesions.
4. Hirschsprung's disease.

1. Carcinoid tumor:
• It accounts for 70% of carcinoid tumors occur in the appendix.


• The tumor appears as a small submucosal nodule at the tip of the appendix.
• The tumor does not metastasize.
2. Adenocarcinoma.
3. Malignant lymphoma.
Tumors of small intestine:
• Benign tumors: Adenoma and leiomyoma are the commonest, but fibroma, neurofibroma and hemangioma may occur.

• Malignant tumors: Rare and include:

1) Adenocarcinoma: Occurs with equal frequency in the duodenum, jejunum and ileum.
2) Carcinoid tumor (argentaffinoma): Arises from the argentaffin cells in the appendix and distal ileum.
3) Malignant Lymphoma: Usually of the non-Hodgkin's type.

Adenoma, leiomyoma, fibroma, neurofibroma and hemangioma.
They are more common than those in the small intestine.
1. Tubular adenoma (adenomatous polyp):
Common in the rectum and colon in old age.
The tumors is single or multiple, sessile or pedunculated.

The tumor consists of tubules or glands lined by tall cells showing dysplasia. Malignant change to adenocarcinoma may occur.



Common sites are the rectum and recto-sigmoid area.
The tumor is sessile, lobulated and 1-10 cm in diameter. Histologically the tumor consists of finger-like papillae, each consists of a vascular connective tissue core covered by one or multiple layers of mucin secreting columnar cells. The lesion is precancerous
3. Tubulovillous adenoma:
Show combined features of both tubular and villous adenomas.
4. Familial polyposis:
A hereditary tumor transmitted as an autosomal dominant trait.
The entire colon isstudded with hundreds polyps, usually tiny and sessile.

Histologically the polyps are commonly tubular adenomas and rarely tubulovillous adenomas.
Malignant change is common and usually occurs in young adults.
5. Hamartomatous polypi:
A hereditary autosomal dominant disease characterized by multiple gastrointestinal polypi accompanied by melanin pigmentation of the face, lips and oral mucosa.
Malignant tumors of the colon: Usually carcinoma, rarely lymphoma and sarcomas.
Carcinoma of large intestine: A common tumor specially in males occurring between the age of 50-70 years.
• Predisposing Factors:
1. Colonic adenomas specially multiple familial polyposis.
2. Pseudopolyposis of ulcerative colitis.
3. Diet rich in fat and poor in vegetable fibers.
• Sites:
About 75% of carcinomas of large intestine occur in the rectum and sigmoid colon, 25% in the rest of the colon specially in the cecum, ascending and descending colon.

• Gross Picture:
A fungating mass projecting in the lumen of the colon. Its surface may show ulceration. It is more common in the cecum.
2. Ulcerative type:

A large malignant ulcer with raised everted edges and indurated base. This type is more common in the rectum.
3.
Starts as a flat mucosal nodule which spreads around the circumference causing stenosis of the lumen with hypertrophy and dilatation in the proximal part of the colon. This type is common in the left side of the colon.
1. Adenocarcinoma: With different grades of differentiation. This is the commonest type.

2. Mucoid carcinoma.
3. Undifferentiated scirrhous carcinoma.

• Spread:
1. Direct spread:
To the urinary bladder, vagina, gall bladder, liver and pancreas.
Direct spread may lead to malignant fistulae.
2. Lymphatic spread: To the regional lymph nodes.
3. Blood spread:
To the liver, then to the lungs, brain and bones.
4. Transcelomic spread:
To the abdominal organs covered by peritoneum specially the ovaries where the metastasis are called Krükenberg tumor.
Transcelomic metastases cause hemorrhagic ascites.

A: Limited to mucosa.
B1: Extending into muscularis propria but not penetrating through it. (No nodal metastasis.)
B2: Penetrating through mascularis propria. (No nodal metastasis.)
C1: Extending into muscularis propria but not penetrating through it. (Nodal metastasis present.)
C2: Penetrating through muscularis propria. (Nodal metastasis present.)
D: (Distant metastasis.)
• Effects:
1. Intestinal hemorrhage.
2. Chronic intestinal obstruction.
3. Acute intestinal obstruction and piles.
4. Intestinal fistulae.
5. Intestinal perforation and septic peritonitis.
A rare congenital disease caused by the Auerbach's (myenteric) plexus and Meissner's (submucous) plexus in a segment of the intestine commonly the recto-sigmoid area.
Effects:

1. Partial or complete intestinal obstruction usually at birth or very early in life.
• Constipation and abdominal distension results.
2. The colon proximal to the obstruction shows hypertrophy of the muscle layer, dilatation and elongation.
• The mucosa and submucosa show chronic non-specific inflammation.
Definition: Passage of red blood in stools due to:


1. Intestinal lesions: Piles, bilharziasis, bacillary and amoebic dysentery, typhoid ulcers, tumors, anal fissures and fistulae.
2. Hemorrhagic blood diseases: Purpura, hemophilia and leukemia. 3. Scurvy and vitamin K deficiency

